Thu, Apr 25, 2024
Volume 28, Issue 2 (3-2018)
JHNM 2018, 28(2): 121-128 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pourkhani S, Chehrzad M M, Reza Masouleh S, Kazem Nezhad Leyli E. The Effect of Family-Based Care on Stress, Anxiety, and Depression of Mothers With Premature Infants . JHNM 2018; 28 (2) :121-128
URL: http://hnmj.gums.ac.ir/article-1-973-en.html
URL: http://hnmj.gums.ac.ir/article-1-973-en.html
The Effect of Family-Based Care on Stress, Anxiety, and Depression of Mothers With Premature Infants
1- Nursing (MSc.), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
2- Social Determinants of Health Research Center (SDHRC), PhD Candidate, Department of Nursing, Instructor, Guilan University of Medical Sciences, Rasht, Iran , chehrzad@yahoo.com
3- Social Determinants of Health Research Center (SDHRC), Department of Nursing, Instructor, Guilan University of Medical Sciences, Rasht, Iran
4- Social Determinants of Health Research Center (SDHRC), Bio-Statistics, Associate Professor, Guilan University of Medical Sciences, Rasht, Iran
2- Social Determinants of Health Research Center (SDHRC), PhD Candidate, Department of Nursing, Instructor, Guilan University of Medical Sciences, Rasht, Iran , chehrzad@yahoo.com
3- Social Determinants of Health Research Center (SDHRC), Department of Nursing, Instructor, Guilan University of Medical Sciences, Rasht, Iran
4- Social Determinants of Health Research Center (SDHRC), Bio-Statistics, Associate Professor, Guilan University of Medical Sciences, Rasht, Iran
Full-Text [PDF 513 kb]
(1110 Downloads)
| Abstract (HTML) (4088 Views)
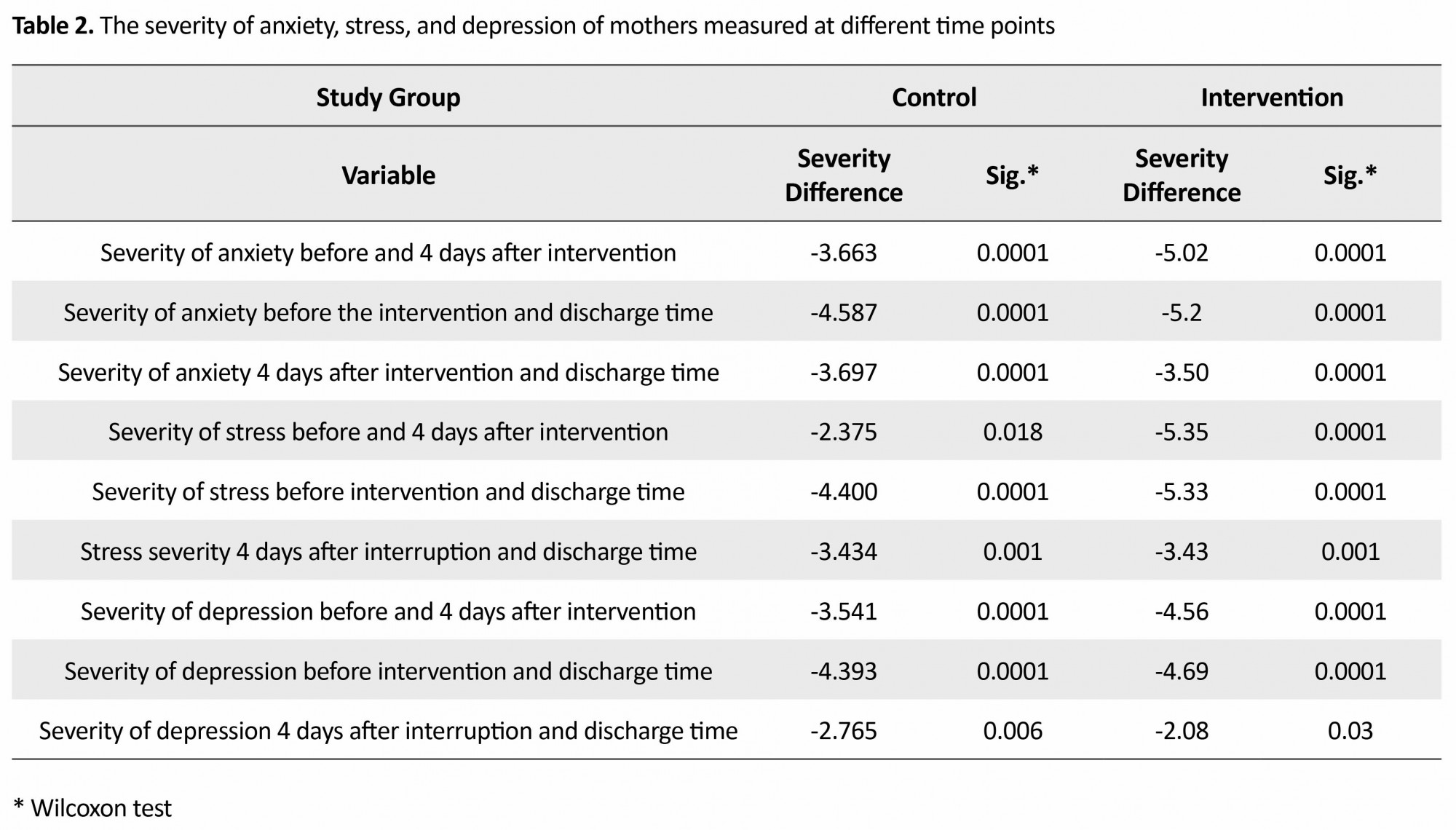
There was a significant statistical difference between the severity of stress in the control group before the intervention, 4 days after the intervention (P=0.018) and discharge time (P=0.0001) and also between 4 days after the intervention and the discharge time (P=0.001). Moreover, there was a significant statistical difference between the intensity of stress, before the intervention, 4 days after the intervention (P=0.0001), and discharge time (P=0.0001) and also between 4 days after the intervention and at discharge time (P=0.0001).
With regard to the severity of depression before the intervention, there was a significant statistical difference between 4 days after the intervention time (P=0.0001) and discharge time (P=0.0001) and also between 4 days after the intervention time and discharge time (P=0.006) in the control group. Moreover, in the intervention group, there was a significant statistical difference in the severity of depression before the intervention, 4 days after the intervention (P=0.0001) and at discharge time (P=0.0001) and also between 4 days after the intervention and discharge time (P=0.038).
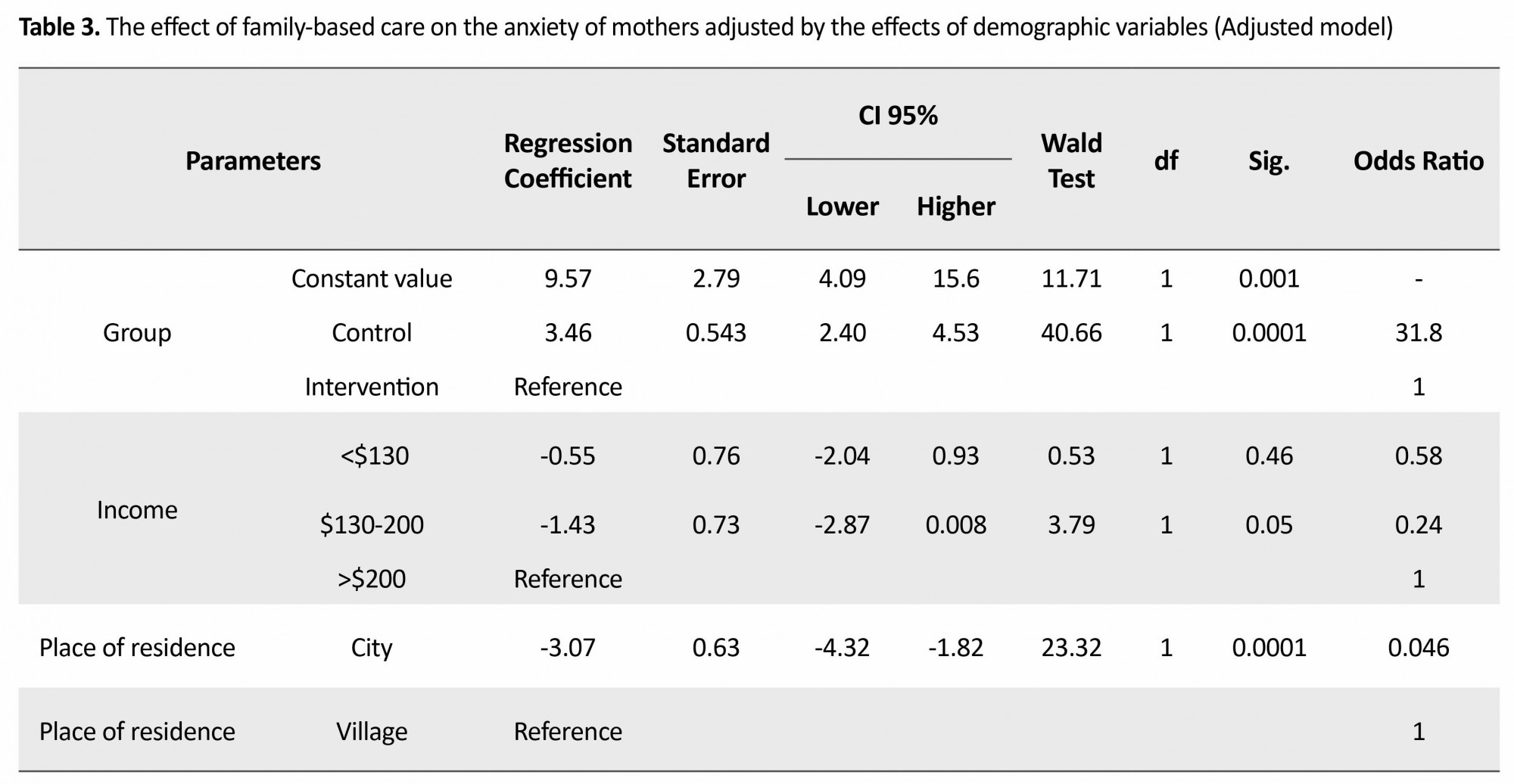
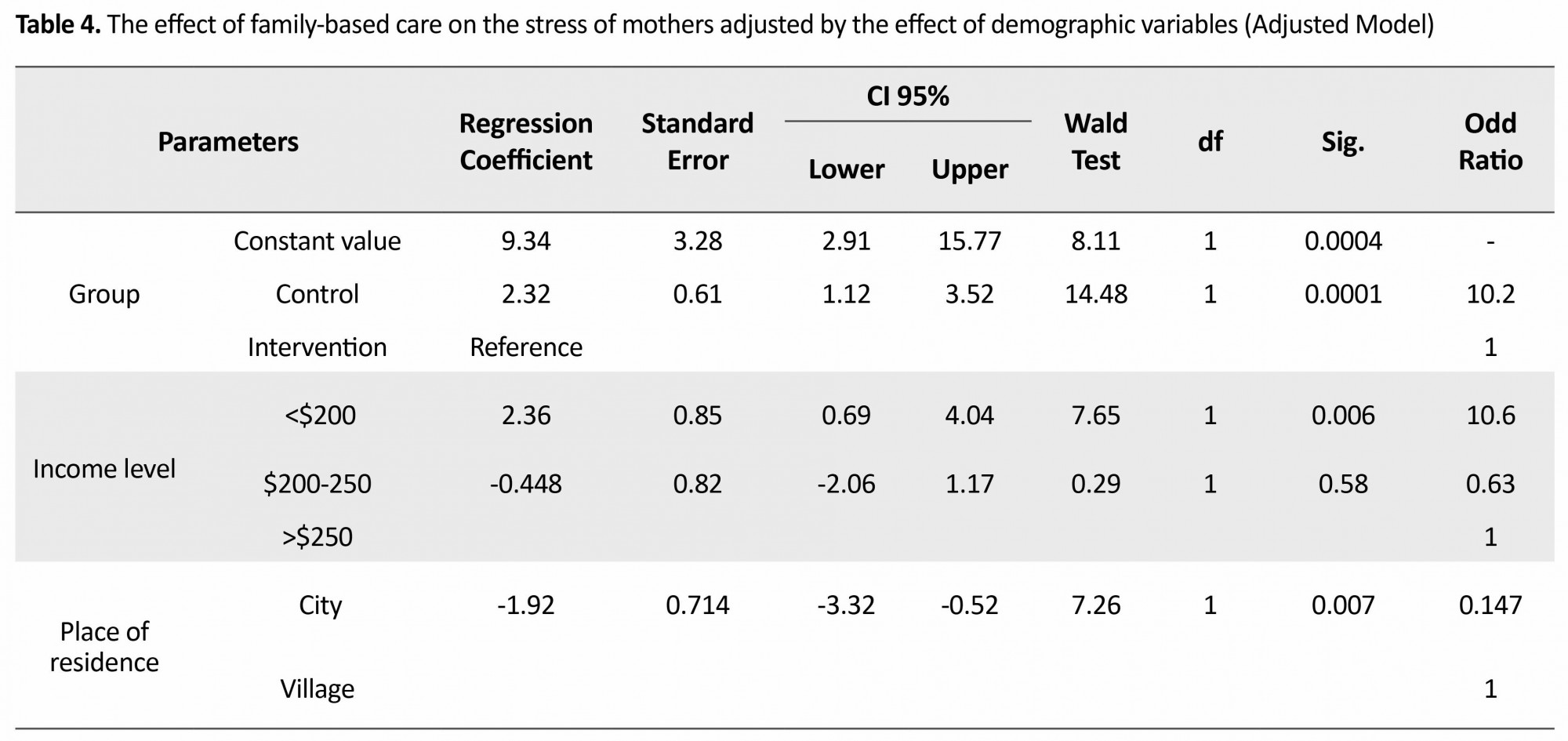
Findings in present study also showed that after adjusting the effects of demographic variables before the intervention, the statistical differences in anxiety, stress, and depression were not significant between control and intervention groups while the effect of family-based intervention on the severity of anxiety was significant (P=0.0001) in such a way that the control group on average (4.3±0.53) was more anxious than the intervention group (95% CI=2.4-4.5). With regard to the stress, the difference was statistically significant (P=0.0001) in such a way that the control group had a higher stress level (2.3±0.61) than the intervention group (95% CI=1.1-3.5). The effects of family-based care on the severity of depression were significant (P=0.0001), where the severity of depression in the control group was more (1.7±0.44) than the intervention group (95% CI=0.84-2.5). Income and residence were also the factors influencing the severity of anxiety, stress, and depression of mothers as represented in Tables 3,4, and 5.
Discussion
The present study shows that implementing family-based care reduces the levels of anxiety, stress, and depression in mothers. There is also a statistically significant difference between the intervention and control groups in reducing the amount and severity of anxiety, stress, and depression of mothers before the intervention, 4 days after intervention, and at the time of discharge.
In line with the present research, the results of Ayeen showed that mean level of anxiety in mothers in the intervention group, 4 days after the admission, at the time of discharge, and the average level of children’s anxiety in the intervention group 4 days after admission was significantly lower than in the control group and at the time of admission [14]. Similarly, the results of O’Brien showed that stress during discharge in the intervention group significantly decreased compared with the control group [15]. In line with the current study, Melnyk showed that mothers in the intervention group experience lower levels of stress, anxiety, and depression during the hospital stay and discharge compared with the control group. In addition, the rate of participation and interaction of the mother with the infant in the intervention group was more than the control group [16]. Moreover, Zeinali reported that family-based care is effective in fulfilling the required information of the parents of hospitalized children [10]. The study of Gooding indicates the impact of family-based care provision and parental involvement in reducing the amount of stress, anxiety, and depression [17].
Likewise, Obeidat showed that the intensity of stress, anxiety, and depression perceived by parents with premature infants was more than that in parents with mature normal infants [12]. He also reported that providing interventions such as family-based care and parenting support during hospitalization were effective in reducing the parents’ stress level, anxiety, and depression [12]. Benzies, in a systematic review study, showed that providing educational and sociopsychological interventions generally reduces parental anxiety and depression [18]. According to Akbarbegloo et al. providing information to parents results in their control and power feeling over their position and their increased participation in taking care of their children [19]. In another study, Cockcroft showed that levels of stress, anxiety, and depression of mothers could be reduced by providing family-focused care and active presence of mothers alongside their infants [20]. According to these results, providing family-based care can help reduce the amount of stress, anxiety, and depression in mothers. These results indicate the usefulness of materials provided to mothers can encourage them to participate more in taking care of their infants.
A few limitations of this study are mothers’ personality traits, characters, and physical problems, which might influence the results of implementing family-based care. Further, the results of this study cannot be generalized. It is recommended that future quasi-experimental studies should be conducted on the ways of contributing mothers in the hospitalized newborns’ care such as hugging and massage and benefits of such studies should be explained to the family and health care staff. Future studies are recommended to determine the effects of educational-supportive programs on the stress, anxiety, and depression of fathers of premature infants.
Acknowledgments
This article is the result of a research project that was funded by the Social Determinants of Health Research Center of Guilan University of Medical Sciences. Hereby, we express our sincere gratitude to the Research Deputy of the University for supporting this research as part of a master’s thesis (Pediatric Nursing major). We also appreciate the cooperation of the staff of NICUs of Rasht Medical Educational health centers.
Conflict of Interest
No conflict of interest has been declared by the authors. All authors have agreed on the final version and meet at least one of the ICMJE authorship criteria, including substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content.
References
Full-Text: (1322 Views)
Introduction
Every year, about 15 million premature babies are born worldwide comprising more than 10% of all infants born [1]. The prevalence of premature birth varies in different societies. The statistics show that 8-10% of newborns in the United States and 5-7% of newborns in Europe are premature, and Iran is also among the areas with a high prevalence of preterm labor (about 12%) [2].
Giving birth to premature infant requires early separation of infant from mother and long-term admission to the Neonatal Intensive Care Unit (NICU); this separation hurts both mother and infant. According to the World Health Organization (WHO), the average days of hospitalization of premature infants of less than 32 weeks is 35 days [2, 3]. Premature infant admission in the NICU is a psychological crisis for the family, particularly the mother, and brings about anxiety and disability for the mother. This feeling of anxiety, stress, and depression increases and intensifies with the prolonged admission of the premature infant [4, 5]. Several Studies suggested that high levels of anxiety in mothers of premature infants were noticeable at birth and even months later, creating a stressful situation for mothers of premature infants [1-3].
Stress and worry of mothers of premature infants about infant’s survival and health affect their ability and maternal role. Most of them do not know how to cope with fear, anxiety, and fatigue. It is very hard for mothers to deal with these emotions without help and support of others. Fatigue and insomnia also lead to mothers’ impatience [6]. About 70-80% of mothers of premature infants tolerate high levels of psychological stress that manifests as fear, restlessness, cry, guiltiness, anxiety, depression, inattention, and disappointment [3]. Thus, providing the conditions for mother’s presence next to her baby and the possibility of caring will have great benefits for the infant and mother [7]. In this case, mothers may feel more able and self-confident and try harder and to the best in playing their parenting role [8].
One of the ways to empower parents in caring their babies is doing family-based care [9]. Family-based care provides communication between family and health care staff. In this regard, family members are considered as full-time partners in providing health care for their infants. Family-based care supports families by giving priority to the values and needs of the family, develops collaborative communication, and empowers the whole family. To provide this kind of care, medical staff should have a respectable attitude and function to work together with families. Moreover, the health care system should provide opportunities for family participation in policy- and decision-making with the support of the staff, establishment of adequate facilities, innovation, and services available [10]. This type of care will have many benefits to the family, including acquiring skill and sense of competence for infant care after discharge, keeping and maintaining family relationships, reducing emotional stress, and increasing the sense of security in the infant [9]. Similarly, the results of the study by Ali Abadi indicate that the participation of mothers in the care of premature infants was effective in reducing maternal anxiety and suggest that family-based care strategy by the authorities should be implemented by providing appropriate substrates in the clinical settings [11]. Further, the study of Obeidat indicates that stress, anxiety, and depression are perceived more by the parents of premature infants than that of parents with mature infant and providing interventions such as family-based care and parenting support have been effective during the hospital stay in reducing the levels of parental stress, anxiety, and depression [12].
In light of these ideas and given the increasing prevalence of premature infant birth and the psychological responses of the mothers of these infants such as depression, irritability, anxiety, loss of self-esteem, fear of changes in parenting roles, the researchers attempted to determine the effect of family-based care on stress, anxiety, and depression of mothers of premature infants hospitalized in neonate wards.
Materials and Methods
The present study is a quasi-experimental study conducted in the neonatal wards of Medical Educational health centers of Rasht City from December 2014 to June 2015. The required sample size to compare anxiety, stress, and depression between intervention and control groups by providing family-based intervention in mothers of premature infants was estimated according to the study of Khalilzadeh et al. and taking into account the standard deviation of the anxiety score of intervention and control groups (S1=6.58, S2=7.11), the mean difference in anxiety score (d=6.5) [9], confidence interval of 99%, and test power of 95%.
Samples of this study were selected by consecutive sampling method and divided into intervention and control groups. First, the control group samples, fulfilling the inclusion criteria, were consecutively selected within 3 months and received the routine maternity care in the department.
In the next step, samples of the intervention group, fulfilling the inclusion criteria, were consecutively selected within 3 months and received family-based care by the researcher during the hospitalization period. The inclusion criteria for mothers were as follows: being over 18 years, being literate, fluent in Persian, no history of previous infant hospitalized in neonatal ward, no history of caring for a premature infant, no physical disorder that disrupts everyday activities, and lack of obvious nervous and psychological problems leading to use of medicine(according to their personal statements). Based on the contents of the medical records, the neonatal inclusion criteria were having a fetal age of 28-35 weeks, birth weight less than 2500 g, single birth, and without congenital anomalies.
In the intervention group, a care booklet containing the protocol of family-based care of the infant was provided to mothers at the beginning of the program. They were asked to keep the care booklet throughout their hospital stay. The intervention program was implemented in three stages. The first stage was family-based care at the start of infant care by mother. The second stage was before the fourth day and the third stage was before the infant’s discharge with the mother’s practical participation in taking care of the infant. The researcher trained mother at each stage of family-based care in 1-2 hours, keeping in mind the mother’s condition. The feedbacks were taken from the mothers during the work shift. The stages of family-based care for mothers were as follows:
In the first stage, i.e. in the initial care of the infant, neonatal unit and its required equipment, and the necessary knowledge regarding appearance, characteristics, and behavior of premature infants were explained in the presence of a researcher and mother beside the infant. Moreover, sleep and awakening patterns of premature infants, symptoms of stress in premature infants and how to treat them, the role of mother in the care of premature infants in the mothers’ room (to prevent possible noise pollution in the ward) were explained and training provided.
In the second stage, before the fourth day after the intervention, the issues such as the best time to interact with the infant, principles and methods for daily routine care, including nutrition, keeping body temperature and proper clothing, diaper change, and umbilical cord care, were demonstrated to the mother. Next, the mother performed the care learned in the presence of the researcher.
In the last step and before the infant’s discharge, the role of mothers in preparing the infant’s transfer from the hospital to the house, and how to make effective and continuous communication with the infant were emphasized. Furthermore, mothers were taught about the required screening tests (e.g. auditory, visual, and intelligence tests), vaccination, medications such as multivitamins with their correct dose and the method of administration, how to bathe, how to communicate with infants centers in special circumstances, and neonatal physician training.
Depression Anxiety and Stress Scale (DASS-21) was used to determine the effect of family-based care on mothers’ depression, anxiety, and stress. This instrument was completed by the mother at the start of maternity care, 4 days after the intervention, and the day of discharge. This is the standard tool designed by Lovibond and has also been validated in Iran [13]. The research instrument has 21 questions for three emotional states, namely anxiety, stress, and depression. Each scale contained 7 questions which is rated based on 4-point Likert-type scale (never, few times, sometimes, and always), where never assigned 0 and always assigned 3. Based on scores obtained, severity of depression, anxiety, and stress was judged. In the case of depression, a score of 0 to 4 means normal state and lack of depression, score 5 or 6 represents mild depression and scores 7 to 10 represent moderate depression, scores 11 to 13 indicates severe depression, and the score of 14 or higher indicates very severe depression.
In the case of anxiety, score 0-3 indicates normal level and lack of anxiety, score 4-5 indicates mild anxiety, 6 or 7 indicates moderate anxiety, score 8-9 indicates severe anxiety, and the score of 10 and higher indicates very severe anxiety. Finally, in the case of stress, a score of 0-7 is normal and means lack of stress, score 8-9 mild stress, score 10-12 moderate stress, score 13-16 severe stress, and score 17 and higher very severe stress.
After collecting information, the data were analyzed using SPSS version 20. To assess the levels of anxiety, stress, and depression in the two studied groups, first the Kolmogorov-Smirnov test was used to check the normal distribution of the above variables. Since the variables followed the normal distribution, the independent t-test was used to compare the variables in the two studied groups. The Mann-Whitney test was employed to compare qualitative ordinal variables of severity of anxiety, stress, and depression in both groups. In addition, the Wilcoxon test was used to compare the ordinal decrease of these variables before and after the intervention. To investigate the effect of family-based care on the severity of anxiety, stress, and depression of mothers, the generalized linear model was used as generalized estimating equation method by adjusting the effects of individual and social intervening variables. P<0.05 was considered the significance level of the study tests.
Results
The findings indicate mean age of the subjects in the control group was 29.70±5.19 years, they were all married, their degree of education was mostly (47.5%) under diploma, almost all (90%) were housewives, mostly (57.5%) had their first delivery, mostly (60%) delivered their first born alive child and their first child (60%), monthly earnings of nearly half of them (42.5%) was below $200, mostly (60%) resided in the city, and most of them (62.2%) were admitted to the hospital. Finally, the mean duration of neonate’s hospital stay was 9.10±5.02 days. In the intervention group, the mean age of the mothers was 28.85±6.55 years, they were all married, their degree of education was mostly (42.5%) diploma, 92.5% were housewives, mostly (47.5%) had their first delivery, 55% delivered their first born alive child and their first child (65%), monthly income of nearly half of them (47.5%) was less than $200, 70% resided in the city, and most of them (57.5%) did not stay in the hospital. The mean duration of neonates’ hospitalization was 10.15±6.73 days. Based on the statistical test, no significant difference in individual and social variables was found between two groups.
The results indicate no significant statistical difference between the mean scores for anxiety, stress, and depression in both studied groups before the intervention. However, a significant statistical difference was observed between the mean scores in two studied groups 4 days after the intervention and on the day of discharge (Table 1). The information in Table 2 indicates a significant statistical difference between the severity of anxiety changes before the intervention, 4 days after intervention (P=0.0001), and during discharge (P=0.0001) as well as between the severity of anxiety changes, 4 days after the intervention and at discharge time (P=0.0001).
Every year, about 15 million premature babies are born worldwide comprising more than 10% of all infants born [1]. The prevalence of premature birth varies in different societies. The statistics show that 8-10% of newborns in the United States and 5-7% of newborns in Europe are premature, and Iran is also among the areas with a high prevalence of preterm labor (about 12%) [2].
Giving birth to premature infant requires early separation of infant from mother and long-term admission to the Neonatal Intensive Care Unit (NICU); this separation hurts both mother and infant. According to the World Health Organization (WHO), the average days of hospitalization of premature infants of less than 32 weeks is 35 days [2, 3]. Premature infant admission in the NICU is a psychological crisis for the family, particularly the mother, and brings about anxiety and disability for the mother. This feeling of anxiety, stress, and depression increases and intensifies with the prolonged admission of the premature infant [4, 5]. Several Studies suggested that high levels of anxiety in mothers of premature infants were noticeable at birth and even months later, creating a stressful situation for mothers of premature infants [1-3].
Stress and worry of mothers of premature infants about infant’s survival and health affect their ability and maternal role. Most of them do not know how to cope with fear, anxiety, and fatigue. It is very hard for mothers to deal with these emotions without help and support of others. Fatigue and insomnia also lead to mothers’ impatience [6]. About 70-80% of mothers of premature infants tolerate high levels of psychological stress that manifests as fear, restlessness, cry, guiltiness, anxiety, depression, inattention, and disappointment [3]. Thus, providing the conditions for mother’s presence next to her baby and the possibility of caring will have great benefits for the infant and mother [7]. In this case, mothers may feel more able and self-confident and try harder and to the best in playing their parenting role [8].
One of the ways to empower parents in caring their babies is doing family-based care [9]. Family-based care provides communication between family and health care staff. In this regard, family members are considered as full-time partners in providing health care for their infants. Family-based care supports families by giving priority to the values and needs of the family, develops collaborative communication, and empowers the whole family. To provide this kind of care, medical staff should have a respectable attitude and function to work together with families. Moreover, the health care system should provide opportunities for family participation in policy- and decision-making with the support of the staff, establishment of adequate facilities, innovation, and services available [10]. This type of care will have many benefits to the family, including acquiring skill and sense of competence for infant care after discharge, keeping and maintaining family relationships, reducing emotional stress, and increasing the sense of security in the infant [9]. Similarly, the results of the study by Ali Abadi indicate that the participation of mothers in the care of premature infants was effective in reducing maternal anxiety and suggest that family-based care strategy by the authorities should be implemented by providing appropriate substrates in the clinical settings [11]. Further, the study of Obeidat indicates that stress, anxiety, and depression are perceived more by the parents of premature infants than that of parents with mature infant and providing interventions such as family-based care and parenting support have been effective during the hospital stay in reducing the levels of parental stress, anxiety, and depression [12].
In light of these ideas and given the increasing prevalence of premature infant birth and the psychological responses of the mothers of these infants such as depression, irritability, anxiety, loss of self-esteem, fear of changes in parenting roles, the researchers attempted to determine the effect of family-based care on stress, anxiety, and depression of mothers of premature infants hospitalized in neonate wards.
Materials and Methods
The present study is a quasi-experimental study conducted in the neonatal wards of Medical Educational health centers of Rasht City from December 2014 to June 2015. The required sample size to compare anxiety, stress, and depression between intervention and control groups by providing family-based intervention in mothers of premature infants was estimated according to the study of Khalilzadeh et al. and taking into account the standard deviation of the anxiety score of intervention and control groups (S1=6.58, S2=7.11), the mean difference in anxiety score (d=6.5) [9], confidence interval of 99%, and test power of 95%.
Samples of this study were selected by consecutive sampling method and divided into intervention and control groups. First, the control group samples, fulfilling the inclusion criteria, were consecutively selected within 3 months and received the routine maternity care in the department.
In the next step, samples of the intervention group, fulfilling the inclusion criteria, were consecutively selected within 3 months and received family-based care by the researcher during the hospitalization period. The inclusion criteria for mothers were as follows: being over 18 years, being literate, fluent in Persian, no history of previous infant hospitalized in neonatal ward, no history of caring for a premature infant, no physical disorder that disrupts everyday activities, and lack of obvious nervous and psychological problems leading to use of medicine(according to their personal statements). Based on the contents of the medical records, the neonatal inclusion criteria were having a fetal age of 28-35 weeks, birth weight less than 2500 g, single birth, and without congenital anomalies.
In the intervention group, a care booklet containing the protocol of family-based care of the infant was provided to mothers at the beginning of the program. They were asked to keep the care booklet throughout their hospital stay. The intervention program was implemented in three stages. The first stage was family-based care at the start of infant care by mother. The second stage was before the fourth day and the third stage was before the infant’s discharge with the mother’s practical participation in taking care of the infant. The researcher trained mother at each stage of family-based care in 1-2 hours, keeping in mind the mother’s condition. The feedbacks were taken from the mothers during the work shift. The stages of family-based care for mothers were as follows:
In the first stage, i.e. in the initial care of the infant, neonatal unit and its required equipment, and the necessary knowledge regarding appearance, characteristics, and behavior of premature infants were explained in the presence of a researcher and mother beside the infant. Moreover, sleep and awakening patterns of premature infants, symptoms of stress in premature infants and how to treat them, the role of mother in the care of premature infants in the mothers’ room (to prevent possible noise pollution in the ward) were explained and training provided.
In the second stage, before the fourth day after the intervention, the issues such as the best time to interact with the infant, principles and methods for daily routine care, including nutrition, keeping body temperature and proper clothing, diaper change, and umbilical cord care, were demonstrated to the mother. Next, the mother performed the care learned in the presence of the researcher.
In the last step and before the infant’s discharge, the role of mothers in preparing the infant’s transfer from the hospital to the house, and how to make effective and continuous communication with the infant were emphasized. Furthermore, mothers were taught about the required screening tests (e.g. auditory, visual, and intelligence tests), vaccination, medications such as multivitamins with their correct dose and the method of administration, how to bathe, how to communicate with infants centers in special circumstances, and neonatal physician training.
Depression Anxiety and Stress Scale (DASS-21) was used to determine the effect of family-based care on mothers’ depression, anxiety, and stress. This instrument was completed by the mother at the start of maternity care, 4 days after the intervention, and the day of discharge. This is the standard tool designed by Lovibond and has also been validated in Iran [13]. The research instrument has 21 questions for three emotional states, namely anxiety, stress, and depression. Each scale contained 7 questions which is rated based on 4-point Likert-type scale (never, few times, sometimes, and always), where never assigned 0 and always assigned 3. Based on scores obtained, severity of depression, anxiety, and stress was judged. In the case of depression, a score of 0 to 4 means normal state and lack of depression, score 5 or 6 represents mild depression and scores 7 to 10 represent moderate depression, scores 11 to 13 indicates severe depression, and the score of 14 or higher indicates very severe depression.
In the case of anxiety, score 0-3 indicates normal level and lack of anxiety, score 4-5 indicates mild anxiety, 6 or 7 indicates moderate anxiety, score 8-9 indicates severe anxiety, and the score of 10 and higher indicates very severe anxiety. Finally, in the case of stress, a score of 0-7 is normal and means lack of stress, score 8-9 mild stress, score 10-12 moderate stress, score 13-16 severe stress, and score 17 and higher very severe stress.
After collecting information, the data were analyzed using SPSS version 20. To assess the levels of anxiety, stress, and depression in the two studied groups, first the Kolmogorov-Smirnov test was used to check the normal distribution of the above variables. Since the variables followed the normal distribution, the independent t-test was used to compare the variables in the two studied groups. The Mann-Whitney test was employed to compare qualitative ordinal variables of severity of anxiety, stress, and depression in both groups. In addition, the Wilcoxon test was used to compare the ordinal decrease of these variables before and after the intervention. To investigate the effect of family-based care on the severity of anxiety, stress, and depression of mothers, the generalized linear model was used as generalized estimating equation method by adjusting the effects of individual and social intervening variables. P<0.05 was considered the significance level of the study tests.
Results
The findings indicate mean age of the subjects in the control group was 29.70±5.19 years, they were all married, their degree of education was mostly (47.5%) under diploma, almost all (90%) were housewives, mostly (57.5%) had their first delivery, mostly (60%) delivered their first born alive child and their first child (60%), monthly earnings of nearly half of them (42.5%) was below $200, mostly (60%) resided in the city, and most of them (62.2%) were admitted to the hospital. Finally, the mean duration of neonate’s hospital stay was 9.10±5.02 days. In the intervention group, the mean age of the mothers was 28.85±6.55 years, they were all married, their degree of education was mostly (42.5%) diploma, 92.5% were housewives, mostly (47.5%) had their first delivery, 55% delivered their first born alive child and their first child (65%), monthly income of nearly half of them (47.5%) was less than $200, 70% resided in the city, and most of them (57.5%) did not stay in the hospital. The mean duration of neonates’ hospitalization was 10.15±6.73 days. Based on the statistical test, no significant difference in individual and social variables was found between two groups.
The results indicate no significant statistical difference between the mean scores for anxiety, stress, and depression in both studied groups before the intervention. However, a significant statistical difference was observed between the mean scores in two studied groups 4 days after the intervention and on the day of discharge (Table 1). The information in Table 2 indicates a significant statistical difference between the severity of anxiety changes before the intervention, 4 days after intervention (P=0.0001), and during discharge (P=0.0001) as well as between the severity of anxiety changes, 4 days after the intervention and at discharge time (P=0.0001).
There was a significant statistical difference between the severity of stress in the control group before the intervention, 4 days after the intervention (P=0.018) and discharge time (P=0.0001) and also between 4 days after the intervention and the discharge time (P=0.001). Moreover, there was a significant statistical difference between the intensity of stress, before the intervention, 4 days after the intervention (P=0.0001), and discharge time (P=0.0001) and also between 4 days after the intervention and at discharge time (P=0.0001).
With regard to the severity of depression before the intervention, there was a significant statistical difference between 4 days after the intervention time (P=0.0001) and discharge time (P=0.0001) and also between 4 days after the intervention time and discharge time (P=0.006) in the control group. Moreover, in the intervention group, there was a significant statistical difference in the severity of depression before the intervention, 4 days after the intervention (P=0.0001) and at discharge time (P=0.0001) and also between 4 days after the intervention and discharge time (P=0.038).
Findings in present study also showed that after adjusting the effects of demographic variables before the intervention, the statistical differences in anxiety, stress, and depression were not significant between control and intervention groups while the effect of family-based intervention on the severity of anxiety was significant (P=0.0001) in such a way that the control group on average (4.3±0.53) was more anxious than the intervention group (95% CI=2.4-4.5). With regard to the stress, the difference was statistically significant (P=0.0001) in such a way that the control group had a higher stress level (2.3±0.61) than the intervention group (95% CI=1.1-3.5). The effects of family-based care on the severity of depression were significant (P=0.0001), where the severity of depression in the control group was more (1.7±0.44) than the intervention group (95% CI=0.84-2.5). Income and residence were also the factors influencing the severity of anxiety, stress, and depression of mothers as represented in Tables 3,4, and 5.
Discussion
The present study shows that implementing family-based care reduces the levels of anxiety, stress, and depression in mothers. There is also a statistically significant difference between the intervention and control groups in reducing the amount and severity of anxiety, stress, and depression of mothers before the intervention, 4 days after intervention, and at the time of discharge.
In line with the present research, the results of Ayeen showed that mean level of anxiety in mothers in the intervention group, 4 days after the admission, at the time of discharge, and the average level of children’s anxiety in the intervention group 4 days after admission was significantly lower than in the control group and at the time of admission [14]. Similarly, the results of O’Brien showed that stress during discharge in the intervention group significantly decreased compared with the control group [15]. In line with the current study, Melnyk showed that mothers in the intervention group experience lower levels of stress, anxiety, and depression during the hospital stay and discharge compared with the control group. In addition, the rate of participation and interaction of the mother with the infant in the intervention group was more than the control group [16]. Moreover, Zeinali reported that family-based care is effective in fulfilling the required information of the parents of hospitalized children [10]. The study of Gooding indicates the impact of family-based care provision and parental involvement in reducing the amount of stress, anxiety, and depression [17].
Likewise, Obeidat showed that the intensity of stress, anxiety, and depression perceived by parents with premature infants was more than that in parents with mature normal infants [12]. He also reported that providing interventions such as family-based care and parenting support during hospitalization were effective in reducing the parents’ stress level, anxiety, and depression [12]. Benzies, in a systematic review study, showed that providing educational and sociopsychological interventions generally reduces parental anxiety and depression [18]. According to Akbarbegloo et al. providing information to parents results in their control and power feeling over their position and their increased participation in taking care of their children [19]. In another study, Cockcroft showed that levels of stress, anxiety, and depression of mothers could be reduced by providing family-focused care and active presence of mothers alongside their infants [20]. According to these results, providing family-based care can help reduce the amount of stress, anxiety, and depression in mothers. These results indicate the usefulness of materials provided to mothers can encourage them to participate more in taking care of their infants.
A few limitations of this study are mothers’ personality traits, characters, and physical problems, which might influence the results of implementing family-based care. Further, the results of this study cannot be generalized. It is recommended that future quasi-experimental studies should be conducted on the ways of contributing mothers in the hospitalized newborns’ care such as hugging and massage and benefits of such studies should be explained to the family and health care staff. Future studies are recommended to determine the effects of educational-supportive programs on the stress, anxiety, and depression of fathers of premature infants.
Acknowledgments
This article is the result of a research project that was funded by the Social Determinants of Health Research Center of Guilan University of Medical Sciences. Hereby, we express our sincere gratitude to the Research Deputy of the University for supporting this research as part of a master’s thesis (Pediatric Nursing major). We also appreciate the cooperation of the staff of NICUs of Rasht Medical Educational health centers.
Conflict of Interest
No conflict of interest has been declared by the authors. All authors have agreed on the final version and meet at least one of the ICMJE authorship criteria, including substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content.
References
- Blencowe H, Cousens S, Oestergaard M, Chou D, Moller AB, Narwal R, et al. National, regional and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. The Lancet. 2012; 379(9832):2162-72. doi: 10.1016/s0140-6736(12)60820-4
- Martin JA, Hamilton BE, Ventura SJ, Osterman MA, Osterman JK, Wilson EC, et al. Births: Final data for 2010. National Vital Statistics Reports. 2012; 61(1):1-72. PMID: 24974589
- Reihani T, Sekhavat pour Z, Heidarzadeh M, Mousavi M, Mazlom R. [Investigating the effects of spiritual self-care training on psychological stress of mothers with preterm infants admitted in neonatal intensive care unit (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2014; 17(97):18-28. doi: 10.22038/IJOGI.2014.2826
- Gangi S, Dente D, Bacchio E, Giampietro S, Terrin G, De Curtis M. Posttraumatic stress disorder in parents of premature birth neonates. Procedia - Social and Behavioral Sciences. 2013; 82:882–5. doi: 10.1016/j.sbspro.2013.06.365
- Carvalho AE, Linhares MB, Padovani FH and Martinez FE. Anxiety and depression in mothers of preterm infants and psychological intervention during hospitalization in neonatal ICU. The Spanish journal of psychology. 2009; 12(1):161-70. doi: 10.1017/s1138741600001578
- Arzani A,Valizadeh L, Zamanzadeh V, Eisa Mohammadi E. [Mothers' experiences of caring for prematurely born infants: growth sparks in the face of caregiver burden (Persian)]. Journal of Qualitative Research in Health Sciences. 2014; 3(3): 217-29.
- Pineda RG, Stransky KE, Rogers C, Duncan MH, Smith GC, Neil J, et al. The single-patient room in the NICU: Maternal and family effects. Journal of Perinatology. 2012; 32(7):545–51.
- Franck LS, Oulton K, Nderitu S, Lim M, Fang S, Kaiser A. Parent involvement in pain management for NICU infants: A randomized controlled trial. Journal of Pediatrics. 2011; 128(3):510-8. doi: 10.1542/peds.2011-0272
- Khalilzadeh H, Khorsandi F, Feizi A, Khalakbari H. [The Effect Of Family-centered Care On Anxeity Of Hospitalized Childs Parents With Urinery Tract Infection In Pediatric Ward Of Shahid Motahary Medical Training Center in Urmia (Persian)]. Journal of Urmia Nursing & Midwifery Faculty. 2013; 11(1):34-37.
- Zeinali J, Mirhaghjou S N, Mirzaei M, Alhani F, Kazem Nezhad Leili E, Dehghani M. [The effect of family centered care on meeting parental information needs of hospitalized children (Persian)]. Journal of Holistic Nursing And Midwifery. 2012; 22(1):30-7.
- Aliabadi T, Bastani F, Haghani H. [Effect of mothers’ participation in preterm infants’ care in NICU on readmission rates (Persian)]. Hayat. 2011; 17(2):71-7.
- Obeidat HM, Bond EA, Callister LC. The parental experience of having an infant in the newborn intensive care unit. Journal of Perinatal Education. 2009; 18(3):23–9. doi: 10.1624/105812409x461199
- Sahebi A, Asghari MJ, Salari RS. [Validation of Depression Anxiety and Stress Scale (DASS-21) for an Iranian Population (Persian)]. Journal Psychology. Developmental Psychology. 2006; 4:299-312.
- Ayeen F, Alhani F, Mohammadi A, Kazemnejad A. [Needs of Mother's of hospitalized Childes: Rights claimed by the mothers of nursing services (Persian)]. Special Journal of Medical Ethics and Medical History. 2010; 4:70- 81.
- O’Brien K, Bracht M, Macdonell K, McBride T, Robson K, O’Leary L. A pilot cohort analytic study of Family Integrated Care in a Canadian neonatal intensive care unit. BMC Pregnancy and Childbirth. 2013; 13(1):2-8. doi: 10.1186/1471-2393-13-s1-s12
- Melnyk BM, Fischbeck-Feinstein N, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants' length of stay and improving parents' mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: Arandomized controlled trial. Pediatrics. 2008; 118(5): 1414-37. doi: 10.1542/peds.2005-2580
- Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: Origins, advances, impact. Seminars in Perinatology. 2011; 35(1):20–8. doi: 10.1053/j.semperi.2010.10.004
- Benzies KM, Magill-Evans JE, Hayden K, Ballantyne M. Key components of early intervention programs for preterm infants and their parents: A systematic review and meta-analysis. BMC Pregnancy and Childbirth. 2013; 13(Suppl 1):S10. doi: 10.1186/1471-2393-13-s1-s10
- Akbarbegloo M, Valizadeh L, Asadollahi M. [Mothers and nurses viewpoint about importance and perceived nursing supports for parents with hospitalized premature newborn in natal intensive care unit (Persian)]. Journal of Critical Care Nursing. 2009; 2(2):71-4.
- Cockcroft S. How can family centred care be improved to meet the needs of parents with a premature baby in neonatal intensive care? Journal of Neonatal Nursing. 2012; 18(3):105–10. doi: 10.1016/j.jnn.2011.07.008
Article Type : Research |
Subject:
Special
Received: 2018/03/19 | Accepted: 2018/03/19 | Published: 2018/03/19
Received: 2018/03/19 | Accepted: 2018/03/19 | Published: 2018/03/19
References
1. Blencowe H, Cousens S, Oestergaard M, Chou D, Moller AB, Narwal R, et al. National, regional and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. The Lancet. 2012; 379(9832):2162-72. doi: 10.1016/s0140-6736(12)60820-4 [DOI:10.1016/S0140-6736(12)60820-4]
2. Martin JA, Hamilton BE, Ventura SJ, Osterman MA, Osterman JK, Wilson EC, et al. Births: Final data for 2010. National Vital Statistics Reports. 2012; 61(1):1-72. PMID: 24974589
3. Reihani T, Sekhavat pour Z, Heidarzadeh M, Mousavi M, Mazlom R. [Investigating the effects of spiritual self-care training on psychological stress of mothers with preterm infants admitted in neonatal intensive care unit (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2014; 17(97):18-28. doi: 10.22038/IJOGI.2014.2826
4. Gangi S, Dente D, Bacchio E, Giampietro S, Terrin G, De Curtis M. Posttraumatic stress disorder in parents of premature birth neonates. Procedia - Social and Behavioral Sciences. 2013; 82:882–5. doi: 10.1016/j.sbspro.2013.06.365 [DOI:10.1016/j.sbspro.2013.06.365]
5. Carvalho AE, Linhares MB, Padovani FH and Martinez FE. Anxiety and depression in mothers of preterm infants and psychological intervention during hospitalization in neonatal ICU. The Spanish journal of psychology. 2009; 12(1):161-70. doi: 10.1017/s1138741600001578 [DOI:10.1017/S1138741600001578]
6. Arzani A,Valizadeh L, Zamanzadeh V, Eisa Mohammadi E. [Mothers' experiences of caring for prematurely born infants: growth sparks in the face of caregiver burden (Persian)]. Journal of Qualitative Research in Health Sciences. 2014; 3(3): 217-29.
7. Pineda RG, Stransky KE, Rogers C, Duncan MH, Smith GC, Neil J, et al. The single-patient room in the NICU: Maternal and family effects. Journal of Perinatology. 2012; 32(7):545–51. [DOI:10.1038/jp.2011.144] [PMID] [PMCID]
8. Franck LS, Oulton K, Nderitu S, Lim M, Fang S, Kaiser A. Parent involvement in pain management for NICU infants: A randomized controlled trial. Journal of Pediatrics. 2011; 128(3):510-8. doi: 10.1542/peds.2011-0272 [DOI:10.1542/peds.2011-0272]
9. Khalilzadeh H, Khorsandi F, Feizi A, Khalakbari H. [The Effect Of Family-centered Care On Anxeity Of Hospitalized Childs Parents With Urinery Tract Infection In Pediatric Ward Of Shahid Motahary Medical Training Center in Urmia (Persian)]. Journal of Urmia Nursing & Midwifery Faculty. 2013; 11(1):34-37.
10. Zeinali J, Mirhaghjou S N, Mirzaei M, Alhani F, Kazem Nezhad Leili E, Dehghani M. [The effect of family centered care on meeting parental information needs of hospitalized children (Persian)]. Journal of Holistic Nursing And Midwifery. 2012; 22(1):30-7.
11. Aliabadi T, Bastani F, Haghani H. [Effect of mothers' participation in preterm infants' care in NICU on readmission rates (Persian)]. Hayat. 2011; 17(2):71-7.
12. Obeidat HM, Bond EA, Callister LC. The parental experience of having an infant in the newborn intensive care unit. Journal of Perinatal Education. 2009; 18(3):23–9. doi: 10.1624/105812409x461199 [DOI:10.1624/105812409X461199]
13. Sahebi A, Asghari MJ, Salari RS. [Validation of Depression Anxiety and Stress Scale (DASS-21) for an Iranian Population (Persian)]. Journal Psychology. Developmental Psychology. 2006; 4:299-312.
14. Ayeen F, Alhani F, Mohammadi A, Kazemnejad A. [Needs of Mother's of hospitalized Childes: Rights claimed by the mothers of nursing services (Persian)]. Special Journal of Medical Ethics and Medical History. 2010; 4:70- 81.
15. O'Brien K, Bracht M, Macdonell K, McBride T, Robson K, O'Leary L. A pilot cohort analytic study of Family Integrated Care in a Canadian neonatal intensive care unit. BMC Pregnancy and Childbirth. 2013; 13(1):2-8. doi: 10.1186/1471-2393-13-s1-s12 [DOI:10.1186/1471-2393-13-S1-S12]
16. Melnyk BM, Fischbeck-Feinstein N, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants' length of stay and improving parents' mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: Arandomized controlled trial. Pediatrics. 2008; 118(5): 1414-37. doi: 10.1542/peds.2005-2580 [DOI:10.1542/peds.2005-2580]
17. Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: Origins, advances, impact. Seminars in Perinatology. 2011; 35(1):20–8. doi: 10.1053/j.semperi.2010.10.004 [DOI:10.1053/j.semperi.2010.10.004]
18. Benzies KM, Magill-Evans JE, Hayden K, Ballantyne M. Key components of early intervention programs for preterm infants and their parents: A systematic review and meta-analysis. BMC Pregnancy and Childbirth. 2013; 13(Suppl 1):S10. doi: 10.1186/1471-2393-13-s1-s10 [DOI:10.1186/1471-2393-13-S1-S10]
19. Akbarbegloo M, Valizadeh L, Asadollahi M. [Mothers and nurses viewpoint about importance and perceived nursing supports for parents with hospitalized premature newborn in natal intensive care unit (Persian)]. Journal of Critical Care Nursing. 2009; 2(2):71-4.
20. Cockcroft S. How can family centred care be improved to meet the needs of parents with a premature baby in neonatal intensive care? Journal of Neonatal Nursing. 2012; 18(3):105–10. doi: 10.1016/j.jnn.2011.07.008 [DOI:10.1016/j.jnn.2011.07.008]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |