Thu, Apr 25, 2024
Volume 28, Issue 2 (3-2018)
JHNM 2018, 28(2): 115-120 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kamalifard M, Bayati Payan S, Panahi S, Hasanpoor S, Babapour Kheiroddin J. Paternal Postpartum Depression and Its Relationship With Maternal Postpartum Depression. JHNM 2018; 28 (2) :115-120
URL: http://hnmj.gums.ac.ir/article-1-972-en.html
URL: http://hnmj.gums.ac.ir/article-1-972-en.html
Mahin Kamalifard1 
 , Somayeh Bayati Payan *
, Somayeh Bayati Payan * 
 2, Samira Panahi1
2, Samira Panahi1 
 , Shirin Hasanpoor1
, Shirin Hasanpoor1 
 , Jalil Babapour Kheiroddin3
, Jalil Babapour Kheiroddin3 


 , Somayeh Bayati Payan *
, Somayeh Bayati Payan * 
 2, Samira Panahi1
2, Samira Panahi1 
 , Shirin Hasanpoor1
, Shirin Hasanpoor1 
 , Jalil Babapour Kheiroddin3
, Jalil Babapour Kheiroddin3 

1- Department of Midwifery, Instructor, Faculty of Nursery and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Midwifery, Instructor, Faculty of Nursery and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran , sobayati@yahoo.com
3- Department of Psychology, Professor, Faculty of Psychology and Educational Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Midwifery, Instructor, Faculty of Nursery and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran , sobayati@yahoo.com
3- Department of Psychology, Professor, Faculty of Psychology and Educational Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
Full-Text [PDF 531 kb]
(2017 Downloads)
| Abstract (HTML) (4440 Views)
Full-Text: (2342 Views)
Introduction
The transition to parenthood is a stressful experience for parents [1], which creates many challenges and concerns in the life of the couple [2, 3]. Maternal Postpartum Depression (PPD) has been studied by many researchers, but although men may also develop depression after childbirth, this problem remains an unknown phenomenon [4, 5]. Since fathers today play a more active role in the care of their infants compared to previous generations, it is essential and inevitable to take into account their mental health as well [6, 7].
Depression symptoms in men are not as apparent as in women and may be followed by isolation, anxiety and restlessness, pessimism, hostility, violence, alcohol, as well as illegal substance use and illicit relations instead of grief [5, 7, 8]. Father’s PPD has a mysterious start and a gradual progression [4]. The prevalence of PPD differs in different societies and researches. It has been reported to be between 30% and 40% among Iranian mothers [9, 10]. PPD was relatively common in fathers [11]. The PPD rate in the first year postpartum ranged from 1.2 to 27.5 % in Ireland, Poland, and several other countries [6], with the figure being 8.2% in Canada, 12.5% in China, and 5–10% in a review study [12-14].
Many studies showed that a father’s anxiety and depression were associated with increased risk of emotional-psychological disorders in the father and family members, along with marital maladjustment, excessive reproach, higher distress levels, and mood problems in infants. Other reasons include anti-social behaviors in children, hyperactivity, behavioral problems, especially in boys, increased health costs [11, 14, 15], and the probability of infanticide [1]. The results of the studies examining the risk factors for father’s PPD are contradictory. Some reported factors include unwanted pregnancy, birth of daughter [16], marital incompatibility [12], having other children, old age, pregnancy anxiety, low education, spouse’s depression during pregnancy and postpartum [4, 11], and maternal PPD [17]. The biological factors include changes in levels of testosterone, estrogen, cortisol, vasopressin, and prolactin, while the ecological factors include changes in lifestyle, marital relationships, difficulty in establishing attachment behaviors with the fetus, and lack of proper pattern for playing the parental role [1].
According to the World Health Organization’s (WHO) recommendation, depression can be diagnosed and treated in primary health care centers, and midwives have a good opportunity to diagnose father’s PPD because of their proximity to families [5, 18]. There is inadequate information on father’s PPD and its prevalence and risk factors, and researchers believe that more research is required among families with different ethnic, cultural, and economic backgrounds. This is to increase their level of awareness in this area and develop diagnostic tools and therapeutic programs [1, 4, 18]. Considering the prevalence of father’s PPD reported in some foreign studies, its adverse effects, multi-factorial nature, and inaccessibility of basic information in the country, the present study aimed at determining father’s depression and its related factors. It aimed to find out, in particular, maternal PPD among couples covered by health centers of the Shahid Beheshti University of Medical Sciences in Tehran.
Materials and Methods
This is an analytical cross-sectional study that was performed on all eligible couples who were referred to health centers of the Shahid Beheshti University of Medical Sciences six to 12 weeks after the birth of their child. The cluster sampling method was used. At first, about 10% of the health centers (a total of seven centers) were randomly selected using the drawing method from a total of 72 health centers covered by the Shahid Beheshti University of Tehran in all four urban areas (two from north, two from east, two from west, and one from northwest of Tehran, respectively). Then samples of each health center were selected from eligible couples on a regular basis from December 2012 to May 2013. To calculate the sample size, a pilot study was carried out on 30 eligible fathers in two health centers. Then, the sample size was estimated to be 200 using the formula for estimating the ratio and the p value of 0.07, obtained from the study as well as by taking into account q=0.93, z=1.96, d=0.05, and design effect=2. Finally, to increase the reliability of the study and the probability of drop-outs, the sampling continued until selection of up to 230 couples. After collecting the questionnaires and deleting the incomplete submissions, a total of 205 couples were analyzed.
The inclusion criteria of the couples included: being Iranian and a resident of Tehran with at least elementary education; six to 12 weeks after birth of the child; couples should be living together; and a healthy newborn without any history of admission. Other criteria included no history of mental disease, depression, or chronic diseases causing symptoms of depression, non-use of drugs as well as drugs affecting the human psyche, and no incidence of mood disorders in the last six months. This was done according to the statements by the participants. After meeting with couples and giving a full description of the research, its objectives and the confidentiality of information, the researcher received their written consent, provided them with questionnaires, and requested them to answer questions separately without interacting with each other. They were to be submitted later. Sampling was performed on weekdays during office hours.
The instrument used to collect data from the fathers included the self-reporting EPDS and a researcher-made questionnaire on sociodemographic factors and fertility. The Edinburgh Scale was only used for mothers. This scale underwent psychometric assessment in Iran [19] and consisted of 10 multiple-choice questions with a score of 0–3 and the total score range varied from 0 to 30. This instrument has been validated in several regions, including Australia, Hong Kong, and Vietnam for men [20-22]. However, in the case of fathers, its content validity was verified by nine faculty members of the Tabriz University of Medical Sciences and its reliability was investigated using internal consistency. Cronbach’s alpha of 0.79 was obtained based on the pilot study. Also, Massoudi showed, in a study, that a score of 12≤ [3] was indicative of PPD for couples, which does not necessarily mean a definitive clinical diagnosis of depression.
The researcher-made questionnaire on the father’s demographic characteristics consisted of 21 questions with 12 items being related to social-demographic characteristics and nine questions related to fertility characteristics. At the end of the study, data analysis was performed using descriptive statistics (mean, standard deviation, and frequency-percent) and inferential statistics (Pearson correlation coefficient, Chi-square, and linear regression) in SPSS software V. 17. This study was carried out after obtaining permission from the Vice-Chancellor of Research and Technology of the Tabriz University of Medical Sciences and the Vice-Chancellor for Health of the Shahid Beheshti University of Medical Sciences in Tehran. This research was approved with ethical code 91129.
Results
The findings of the present research showed that the mean age of fathers and their wives was 32.63±0.5 and 28.24±4.47 years, respectively. The majority of fathers (39.5%) had university education. Most of them were Farsi speakers (44.9%) and self-employed (43.4%). A total of 55.1% of them were first-time fathers and there was no history of an abortion in 86.8% of the cases. A total of 84.9%, 71.9%, and 87.3% of pregnancies were wanted, uncomplicated, and full-term, respectively. Most of the babies (53.2%) were boys and 88.3% of the parents were satisfied with the gender of their infants. A total of 42% of them were tenants and 52.9% had economic status in moderate level. Also, 58.2% of fathers mentioned their wives as the first source of social support. The overall mean of depression in the fathers was 5.96±4.43. Twenty-four of the fathers scored 12 or higher on the Edinburgh scale, indicating the presence of symptoms of depression. Also, the percentage of maternal PPD was determined in 33.2% of the cases. The results of the Pearson correlation test showed a direct and significant statistical relationship among the PPD scores of the parents (P=0.001, r=0.29). As a result, the paternal depression score increased in proportion to the increase in the maternal depression score.
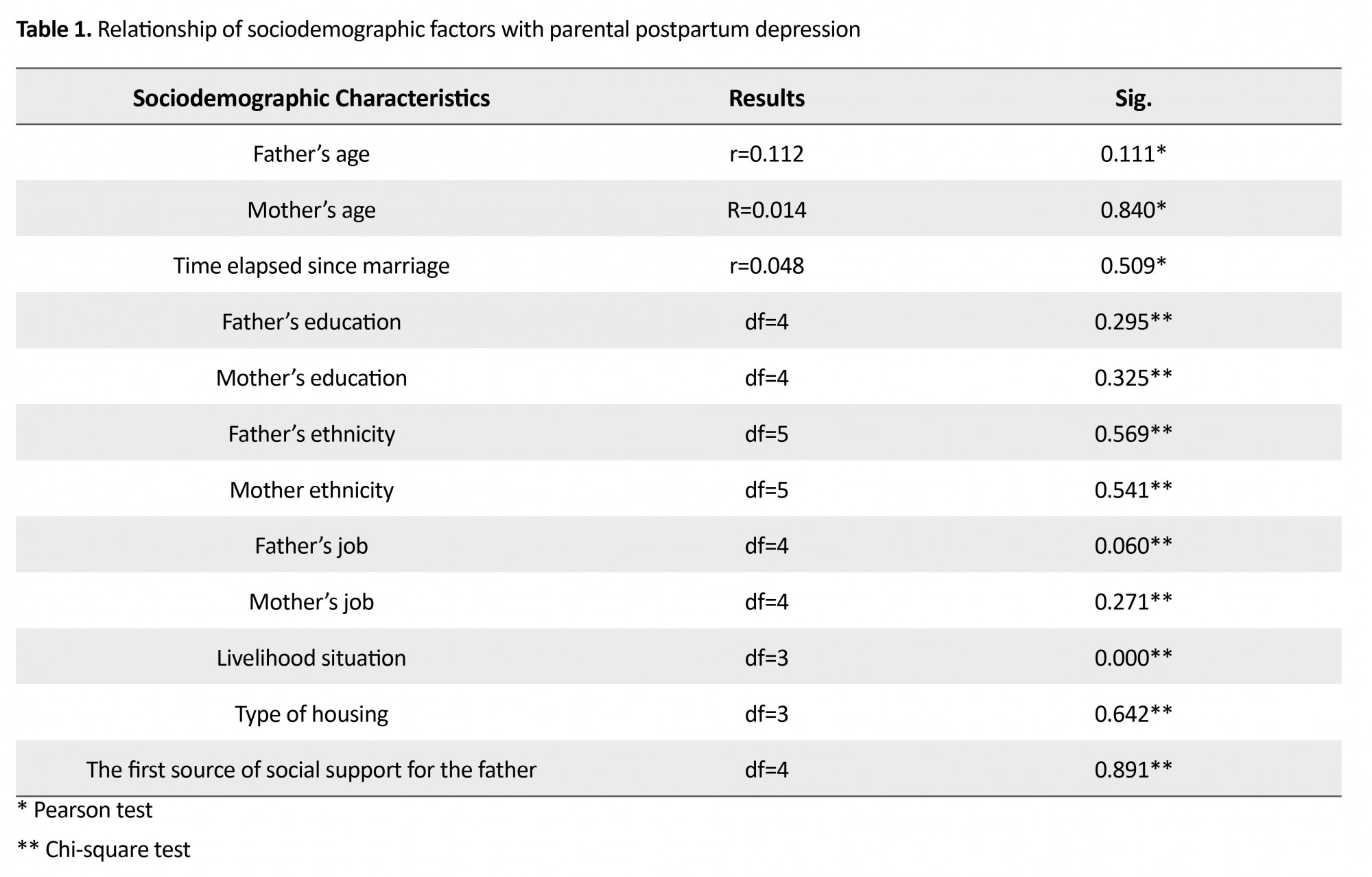
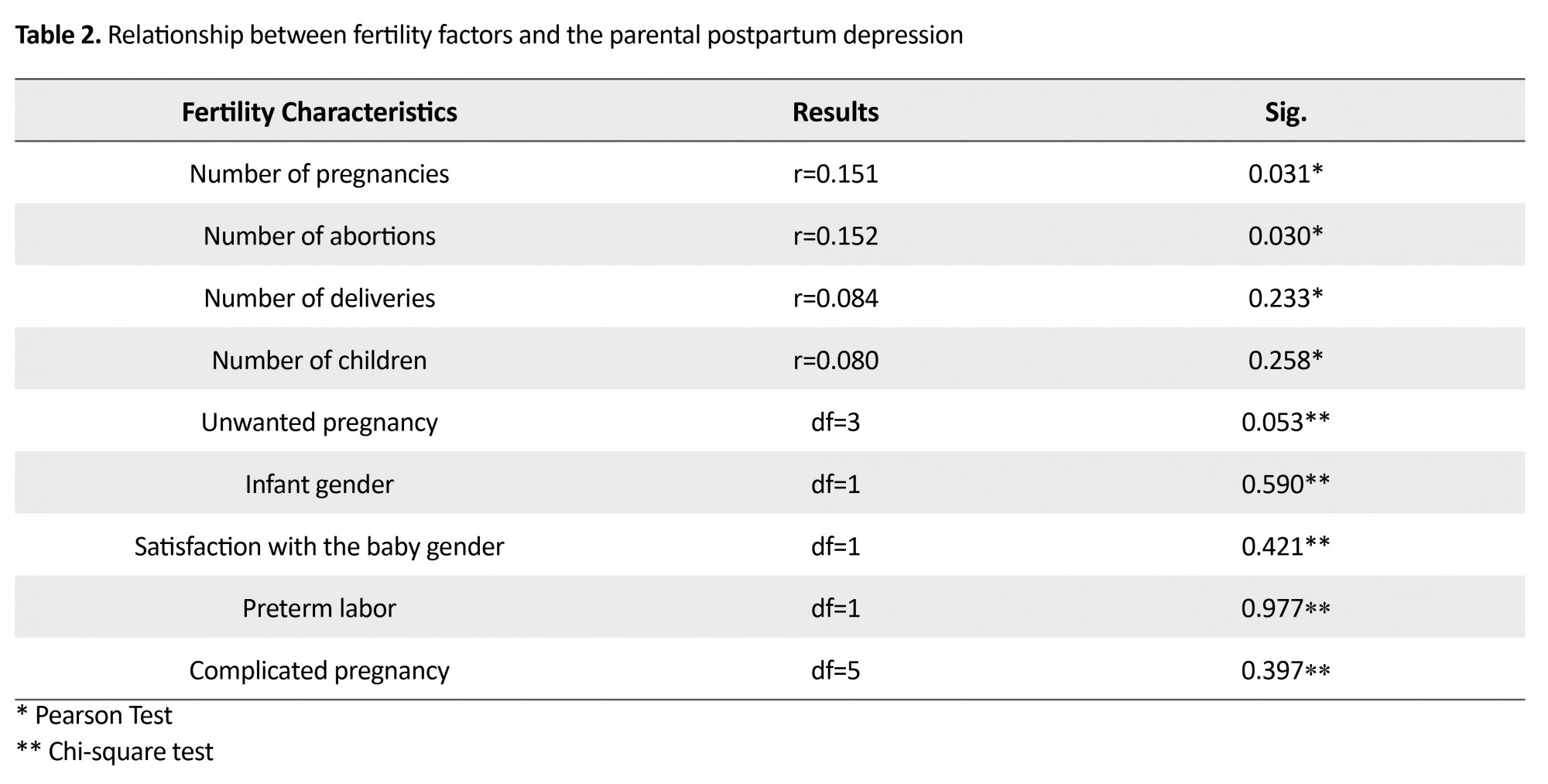
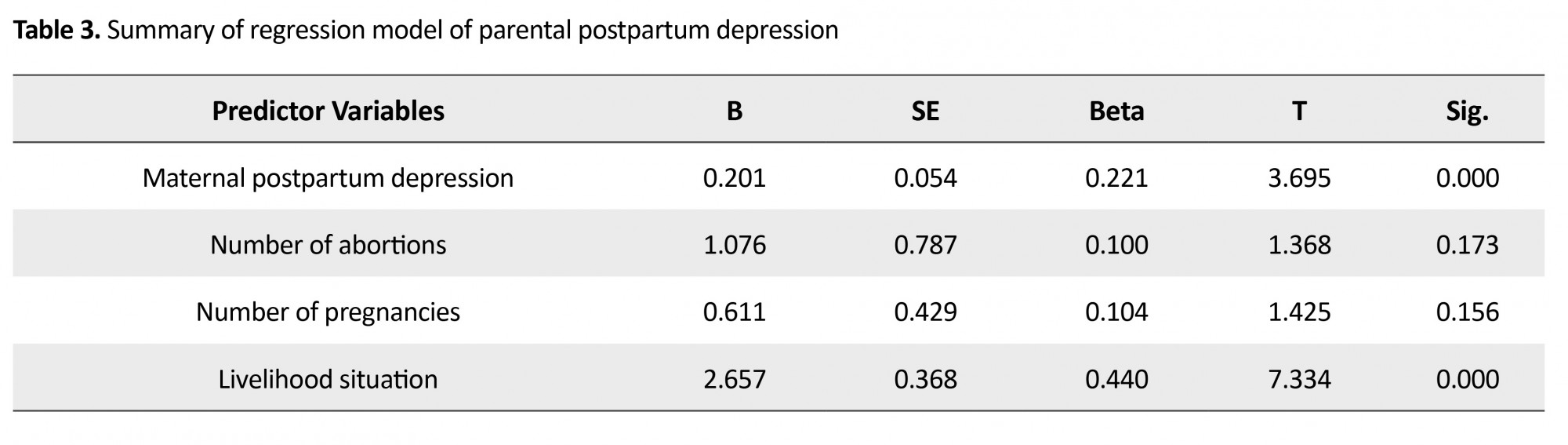
The chi-square test showed a significant statistical relationship between the family livelihood situation and PPD while determining the relationship between the sociodemographic factors and paternal PPD (Table 1) (P=0.001, df=3 x2=29.8). Half of the fathers who were barely making ends meet were depressed, and there was no depression in any of the fathers who had high economic status. There was no significant relationship between other sociodemographic variables and paternal depression. Among the fertility factors (Table 2), the Pearson correlation test showed a direct and significant relationship between the number of abortions (r=0.152, P=0.03) and the number of wife’s pregnancies (r=0.151, P=0.031) with parental PPD. There was no significant relationship between other fertility factors and paternal PPD. The multiple linear regression analysis was then conducted to determine the contribution of each of the variables associated with paternal depression in explaining its changes (Table 3). Independent variables, based on the determination coefficient (R2), significantly explained about 30% of changes in the overall paternal PPD (P=0.001). Of this, only the maternal PPD and family livelihood situation variables could predict significant paternal depression.
The transition to parenthood is a stressful experience for parents [1], which creates many challenges and concerns in the life of the couple [2, 3]. Maternal Postpartum Depression (PPD) has been studied by many researchers, but although men may also develop depression after childbirth, this problem remains an unknown phenomenon [4, 5]. Since fathers today play a more active role in the care of their infants compared to previous generations, it is essential and inevitable to take into account their mental health as well [6, 7].
Depression symptoms in men are not as apparent as in women and may be followed by isolation, anxiety and restlessness, pessimism, hostility, violence, alcohol, as well as illegal substance use and illicit relations instead of grief [5, 7, 8]. Father’s PPD has a mysterious start and a gradual progression [4]. The prevalence of PPD differs in different societies and researches. It has been reported to be between 30% and 40% among Iranian mothers [9, 10]. PPD was relatively common in fathers [11]. The PPD rate in the first year postpartum ranged from 1.2 to 27.5 % in Ireland, Poland, and several other countries [6], with the figure being 8.2% in Canada, 12.5% in China, and 5–10% in a review study [12-14].
Many studies showed that a father’s anxiety and depression were associated with increased risk of emotional-psychological disorders in the father and family members, along with marital maladjustment, excessive reproach, higher distress levels, and mood problems in infants. Other reasons include anti-social behaviors in children, hyperactivity, behavioral problems, especially in boys, increased health costs [11, 14, 15], and the probability of infanticide [1]. The results of the studies examining the risk factors for father’s PPD are contradictory. Some reported factors include unwanted pregnancy, birth of daughter [16], marital incompatibility [12], having other children, old age, pregnancy anxiety, low education, spouse’s depression during pregnancy and postpartum [4, 11], and maternal PPD [17]. The biological factors include changes in levels of testosterone, estrogen, cortisol, vasopressin, and prolactin, while the ecological factors include changes in lifestyle, marital relationships, difficulty in establishing attachment behaviors with the fetus, and lack of proper pattern for playing the parental role [1].
According to the World Health Organization’s (WHO) recommendation, depression can be diagnosed and treated in primary health care centers, and midwives have a good opportunity to diagnose father’s PPD because of their proximity to families [5, 18]. There is inadequate information on father’s PPD and its prevalence and risk factors, and researchers believe that more research is required among families with different ethnic, cultural, and economic backgrounds. This is to increase their level of awareness in this area and develop diagnostic tools and therapeutic programs [1, 4, 18]. Considering the prevalence of father’s PPD reported in some foreign studies, its adverse effects, multi-factorial nature, and inaccessibility of basic information in the country, the present study aimed at determining father’s depression and its related factors. It aimed to find out, in particular, maternal PPD among couples covered by health centers of the Shahid Beheshti University of Medical Sciences in Tehran.
Materials and Methods
This is an analytical cross-sectional study that was performed on all eligible couples who were referred to health centers of the Shahid Beheshti University of Medical Sciences six to 12 weeks after the birth of their child. The cluster sampling method was used. At first, about 10% of the health centers (a total of seven centers) were randomly selected using the drawing method from a total of 72 health centers covered by the Shahid Beheshti University of Tehran in all four urban areas (two from north, two from east, two from west, and one from northwest of Tehran, respectively). Then samples of each health center were selected from eligible couples on a regular basis from December 2012 to May 2013. To calculate the sample size, a pilot study was carried out on 30 eligible fathers in two health centers. Then, the sample size was estimated to be 200 using the formula for estimating the ratio and the p value of 0.07, obtained from the study as well as by taking into account q=0.93, z=1.96, d=0.05, and design effect=2. Finally, to increase the reliability of the study and the probability of drop-outs, the sampling continued until selection of up to 230 couples. After collecting the questionnaires and deleting the incomplete submissions, a total of 205 couples were analyzed.
The inclusion criteria of the couples included: being Iranian and a resident of Tehran with at least elementary education; six to 12 weeks after birth of the child; couples should be living together; and a healthy newborn without any history of admission. Other criteria included no history of mental disease, depression, or chronic diseases causing symptoms of depression, non-use of drugs as well as drugs affecting the human psyche, and no incidence of mood disorders in the last six months. This was done according to the statements by the participants. After meeting with couples and giving a full description of the research, its objectives and the confidentiality of information, the researcher received their written consent, provided them with questionnaires, and requested them to answer questions separately without interacting with each other. They were to be submitted later. Sampling was performed on weekdays during office hours.
The instrument used to collect data from the fathers included the self-reporting EPDS and a researcher-made questionnaire on sociodemographic factors and fertility. The Edinburgh Scale was only used for mothers. This scale underwent psychometric assessment in Iran [19] and consisted of 10 multiple-choice questions with a score of 0–3 and the total score range varied from 0 to 30. This instrument has been validated in several regions, including Australia, Hong Kong, and Vietnam for men [20-22]. However, in the case of fathers, its content validity was verified by nine faculty members of the Tabriz University of Medical Sciences and its reliability was investigated using internal consistency. Cronbach’s alpha of 0.79 was obtained based on the pilot study. Also, Massoudi showed, in a study, that a score of 12≤ [3] was indicative of PPD for couples, which does not necessarily mean a definitive clinical diagnosis of depression.
The researcher-made questionnaire on the father’s demographic characteristics consisted of 21 questions with 12 items being related to social-demographic characteristics and nine questions related to fertility characteristics. At the end of the study, data analysis was performed using descriptive statistics (mean, standard deviation, and frequency-percent) and inferential statistics (Pearson correlation coefficient, Chi-square, and linear regression) in SPSS software V. 17. This study was carried out after obtaining permission from the Vice-Chancellor of Research and Technology of the Tabriz University of Medical Sciences and the Vice-Chancellor for Health of the Shahid Beheshti University of Medical Sciences in Tehran. This research was approved with ethical code 91129.
Results
The findings of the present research showed that the mean age of fathers and their wives was 32.63±0.5 and 28.24±4.47 years, respectively. The majority of fathers (39.5%) had university education. Most of them were Farsi speakers (44.9%) and self-employed (43.4%). A total of 55.1% of them were first-time fathers and there was no history of an abortion in 86.8% of the cases. A total of 84.9%, 71.9%, and 87.3% of pregnancies were wanted, uncomplicated, and full-term, respectively. Most of the babies (53.2%) were boys and 88.3% of the parents were satisfied with the gender of their infants. A total of 42% of them were tenants and 52.9% had economic status in moderate level. Also, 58.2% of fathers mentioned their wives as the first source of social support. The overall mean of depression in the fathers was 5.96±4.43. Twenty-four of the fathers scored 12 or higher on the Edinburgh scale, indicating the presence of symptoms of depression. Also, the percentage of maternal PPD was determined in 33.2% of the cases. The results of the Pearson correlation test showed a direct and significant statistical relationship among the PPD scores of the parents (P=0.001, r=0.29). As a result, the paternal depression score increased in proportion to the increase in the maternal depression score.
The chi-square test showed a significant statistical relationship between the family livelihood situation and PPD while determining the relationship between the sociodemographic factors and paternal PPD (Table 1) (P=0.001, df=3 x2=29.8). Half of the fathers who were barely making ends meet were depressed, and there was no depression in any of the fathers who had high economic status. There was no significant relationship between other sociodemographic variables and paternal depression. Among the fertility factors (Table 2), the Pearson correlation test showed a direct and significant relationship between the number of abortions (r=0.152, P=0.03) and the number of wife’s pregnancies (r=0.151, P=0.031) with parental PPD. There was no significant relationship between other fertility factors and paternal PPD. The multiple linear regression analysis was then conducted to determine the contribution of each of the variables associated with paternal depression in explaining its changes (Table 3). Independent variables, based on the determination coefficient (R2), significantly explained about 30% of changes in the overall paternal PPD (P=0.001). Of this, only the maternal PPD and family livelihood situation variables could predict significant paternal depression.
Discussion
The present research showed a direct correlation between the paternal and maternal depression scores. The latter was considered one of the predictors of parental PPD. Paulson and Bazemore also reported in their studies a positive and moderate correlation between parental and maternal depression [23]. In cases where a woman suffers from PPD, fathers are expected to be more involved in family affairs than before. In the event of prolonged maternal depression, a man’s mental adaptation becomes disrupted due to lack of adequate support; his stress increases and predisposes him to depression [4, 16, 17]. However, Nishimura and Ohashi reported no correlation between couples depressed in Japan. They attributed it to the existence of supportive traditions in their country, according to which a father lives away for a while from his wife after childbirth [17]. In this research, among the sociodemographic factors, a significant relationship was observed only between the family livelihood situation and father’s PPD. Another study showed that there was a relationship between the economic situation and a father’s Edinburgh scores, but it did not predict the paternal PPD [24]. In many societies, it is the man’s duty to guarantee the family’s financial security. After the birth of the child, due to the increased financial burden on the family, more emphasis was placed on the breadwinning role of the man, and the father had less opportunity to perform parental duties. In the face of functional weaknesses in the professional and gender roles, the risk of psychiatric distresses increases [7, 25].
The results also showed that there was no significant relationship between the father’s PPD and other sociodemographic factors. de Montigny’s research also showed no relationship between the father’s PPD and demographic factors, including age, education, and marriage duration [12]. Among fertility factors, the number of abortions was significantly correlated with the father’s PPD. De Montigny also showed that paternal PPD was associated with a history of abortion, which could not predict PPD, as in this study [12]. Mothers who have had a history of abortion have a greater sense of failure, disappointment, and incompetence [26, 27], and since the mental situation of couples has an effect on both of them, the father may experience these feelings. In the present study, there was no relationship between the number of children and the delivery with PPD, which was consistent with Lashkaripour’s study conducted on mothers [28].
In contrast to Gao’s [16] study, the father’s depression was not significantly related to unwanted pregnancy in the present research. Also, there was no significant relationship between a father’s PPD and preterm labor, which was consistent with the result of Nishimura and Ohashi’s study [17]. In general, a complex combination of various variables is involved for depression to occur. This is likely affected by the existing cultural and social differences of people in different societies. The contradictory findings of previous studies show the need for further studies in various statistical societies.
The non-generalizability of the results of the present study in the context of other cities and villages in Iran along with its cross-sectional design were among some of the limitations of the research. Therefore, further longitudinal and cohort studies are recommended in various cultural and social environments. Also, there is a need to investigate other PPD-related factors. In the present research, a significant number of fathers had symptoms of PPD. Considering the clinical significance of this phenomenon and its relationship with the mother’s PPD and some other factors, it is recommended that in addition to raising public awareness and implementing educational programs on childbirth, fathers must also be investigated for mood disorders and predisposing factors during this period, especially when their wives are depressed.
Acknowledgments
This article is the result of a master’s thesis wich the authors would like to appreciate the Vice-Chancellor of the Research and Student Research Committee of Tabriz University of Medical Sciences for funding the research, officials of the Nursing and Midwifery Faculty of Tabriz, Deputy of Health of the University of Medical Sciences Shahid Beheshti, all the staff of the health centers and dear ones who helped us in this regard.
Conflict of Interest
The authors declared no conflicts of interest. All authors have agreed on the final version and meet at least one of the ICMJE authorship criteria, including substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content.
References
The present research showed a direct correlation between the paternal and maternal depression scores. The latter was considered one of the predictors of parental PPD. Paulson and Bazemore also reported in their studies a positive and moderate correlation between parental and maternal depression [23]. In cases where a woman suffers from PPD, fathers are expected to be more involved in family affairs than before. In the event of prolonged maternal depression, a man’s mental adaptation becomes disrupted due to lack of adequate support; his stress increases and predisposes him to depression [4, 16, 17]. However, Nishimura and Ohashi reported no correlation between couples depressed in Japan. They attributed it to the existence of supportive traditions in their country, according to which a father lives away for a while from his wife after childbirth [17]. In this research, among the sociodemographic factors, a significant relationship was observed only between the family livelihood situation and father’s PPD. Another study showed that there was a relationship between the economic situation and a father’s Edinburgh scores, but it did not predict the paternal PPD [24]. In many societies, it is the man’s duty to guarantee the family’s financial security. After the birth of the child, due to the increased financial burden on the family, more emphasis was placed on the breadwinning role of the man, and the father had less opportunity to perform parental duties. In the face of functional weaknesses in the professional and gender roles, the risk of psychiatric distresses increases [7, 25].
The results also showed that there was no significant relationship between the father’s PPD and other sociodemographic factors. de Montigny’s research also showed no relationship between the father’s PPD and demographic factors, including age, education, and marriage duration [12]. Among fertility factors, the number of abortions was significantly correlated with the father’s PPD. De Montigny also showed that paternal PPD was associated with a history of abortion, which could not predict PPD, as in this study [12]. Mothers who have had a history of abortion have a greater sense of failure, disappointment, and incompetence [26, 27], and since the mental situation of couples has an effect on both of them, the father may experience these feelings. In the present study, there was no relationship between the number of children and the delivery with PPD, which was consistent with Lashkaripour’s study conducted on mothers [28].
In contrast to Gao’s [16] study, the father’s depression was not significantly related to unwanted pregnancy in the present research. Also, there was no significant relationship between a father’s PPD and preterm labor, which was consistent with the result of Nishimura and Ohashi’s study [17]. In general, a complex combination of various variables is involved for depression to occur. This is likely affected by the existing cultural and social differences of people in different societies. The contradictory findings of previous studies show the need for further studies in various statistical societies.
The non-generalizability of the results of the present study in the context of other cities and villages in Iran along with its cross-sectional design were among some of the limitations of the research. Therefore, further longitudinal and cohort studies are recommended in various cultural and social environments. Also, there is a need to investigate other PPD-related factors. In the present research, a significant number of fathers had symptoms of PPD. Considering the clinical significance of this phenomenon and its relationship with the mother’s PPD and some other factors, it is recommended that in addition to raising public awareness and implementing educational programs on childbirth, fathers must also be investigated for mood disorders and predisposing factors during this period, especially when their wives are depressed.
Acknowledgments
This article is the result of a master’s thesis wich the authors would like to appreciate the Vice-Chancellor of the Research and Student Research Committee of Tabriz University of Medical Sciences for funding the research, officials of the Nursing and Midwifery Faculty of Tabriz, Deputy of Health of the University of Medical Sciences Shahid Beheshti, all the staff of the health centers and dear ones who helped us in this regard.
Conflict of Interest
The authors declared no conflicts of interest. All authors have agreed on the final version and meet at least one of the ICMJE authorship criteria, including substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content.
References
- Kim P, Swain J. Sad dads: Paternal postpartum depression. Psychiatry (Edgmont). 2007; 4(2):35-47. PMID: 20805898
- John WS, Cameron C, McVeigh C. Meeting the challenge of new fatherhood during the early weeks. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2005; 34(2):180-9. doi: 10.1177/0884217505274699
- Massoudi P. Depression and distress in Swedish fathers in the postnatal period– prevalence, correlates, identificaton, and support [PhD thesis]. Gothenburg: University of Gothenburg; 2013.
- Goodman JH. Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. Journal of Advanced Nursing. 2004; 45(1):26-35. doi: 10.1046/j.1365-2648.2003.02857.x
- Melrose S. Paternal postpartum depression: How can nurses begin to help? Contemporary Nurse. 2010; 34(2):199-210. doi: 10.5172/conu.2010.34.2.199
- Wilson CC. Paternal postpartum distress: A discourse analytic study [PhD Thesis]. Hull: University of Hul; 2008.
- Veskrna L. Peripartum depression –does it occur in fathers and does it matter? Journal of Men's Health. 2010; 7(4):420–30. doi: 10.1016/j.jomh.2010.10.004
- Spector AZ. Fatherhood and depression: A review of risks, effects, and clinical application. Issues in Mental Health Nursing. 2006; 27(8):867-83. doi: 10.1080/01612840600840844
- Hosseini H, Naghibi AH, Khademloo M. [Post partum depression and its relationship with some related factors (Persian)]. Journal of Babol University of Medical Sciences. 2008; 10(2):76-81.
- Rubintan N, Esmaeelpur K, Mahmudalilu M, Seyedrasuli E. [The relationship of type of delivery and infant feeding with postpartum depression (Persian)]. Medical Journal of Tabriz University of Medical Science & Health Service. 2012; 34(3):52-6.
- Ramchandani PG, Stein A, Oconnor T, Heron J, Murray L, Evans J. Depression in men in the postnatal period and later child psychopathology: a population cohort study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008; 47(4): 390-8. doi: 10.1097/chi.0b013e31816429c2
- de Montigny F, Girard ME, Lacharité C, Dubeau D, Devault A. Psychosocial factors associated with paternal postnatal depression. Journal of Affective Disorders. 2013; 150(1):44–9. doi: 10.1016/j.jad.2013.01.048
- Mao Q, Zhu LX, Su XY. A comparison of postnatal depression and related factors between Chinese new mothers and fathers. Journal of Clinical Nursing. 2011; 20(5-6):645–52. doi: 10.1111/j.1365-2702.2010.03542.x
- Ramchandani P, Psychogiou L, Vlachos H, Iles J, Sethna V, Netsi E, et al. Paternal depression: an examination of its links with father, child and family functioning in the postnatal period. Depression and Anxiety. 2011; 28(6):471-7. doi: 10.1002/da.20814
- Ramchandani P, Stein A, Evans J, O’Connor T. Paternal depression in the postnatal period and child development: a prospective population study. Lancet. 2005; 365(9478):2201-5. doi: 10.1016/s0140-6736(05)66778-5
- Gao L, Chan S, Mao Q. Depression, perceived stress,and social support among first-time Chinese mothers and fathers in the postpartum period. Research in Nursing & Health. 2009; 32(1):50–8. doi: 10.1002/nur.20306
- Nishimura A, Ohashi K. Risk factors of paternal depression in the early postnatal period in Japan. Nursing & Health Sciences. 2010; 12(2):170-6. doi: 10.1111/j.1442-2018.2010.00513.x
- Schumacher M, Zubaran C, White G. Bringing birth-related paternal depression to the fore. Women and Birth. 2008; 21(2):65-70. doi: 10.1016/j.wombi.2008.03.008
- Ahmadi Kani Golzar A, GoliZadeh Z. [Validation of Edinburgh Postpartum Depression Scale (EPDS) for screening postpartum depression in Iran (Persian)]. Iranian Journal of Psychiatric Nursing. 2015; 3(3):1-10.
- Lai BP, Tang AK, Lee DT, Yip AS, Chung TK. Detecting postnatal depression in Chinese men: A comparison of three instruments. Psychiatry Research. 2010; 180(2-3):80-5. doi: 10.1016/j.psychres.2009.07.015
- Matthey S, Barnett B, Kavanagh DJ, Howie P. Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. Journal of Affective Disorders. 2001; 64(2-3):175-84. doi: 10.1016/s0165-0327(00)00236-6
- Tran TD, Tran T, Fisher J. Validation of three psychometric instruments for screening for perinatal common mental disorders in men in the north of Vietnam. Journal of Affective Disorders. 2012; 136(1-2):104-9. doi: 10.1016/j.jad.2011.08.012
- Paulson J, Bazemore S. Prenatal and postpartum depression in fathers and its association with maternal depression. JAMA. 2010; 303(19):1961-9. doi: 10.1001/jama.2010.605
- Bielawska-Batorowicz E, Kassakowska-Petrycka K. Depressive mood in men after the birth of their offspring in relation to a partner’s depression, social support, father’s personality and prenatal expectations. Journal of Reproductive and Infant Psychology. 2006; 24(1):21-9. doi: 10.1080/02646830500475179
- Anderson EA, Kohler JK, Letiecq BL. Predictors of depression among low-Income, nonresidential fathers. Journal of Family Issues. 2005; 26(5):547-67. doi: 10.1177/0192513x04272753
- Kiani F, Khadivzade T, Sargolzaei M, Behnam H. [Relationship between marital satisfaction during pregnancy and postpartum depression (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2009; 13(5):37-44.
- Astaraki L. [Survey of parental – fetal attachment and associated factors in pregnant women of health and medical centers and their husbands, affiliated to Tehran universities of medical science in Tehran (Persian)] [MSc. Thesis]. Tehran: Tehran University of Medical Sciences; 2011
- Lashkaripour K, Bakhshani NM, Hokmabadi S, Sajjadi SAR, Sarasiyabi AS. [Postpartum depression and related factors: A 4.5 months study (Persian)]. Journal of Fundamentals of Mental Health. 2012; 13(4):404-12.
Article Type : Research |
Subject:
Special
Received: 2018/03/19 | Accepted: 2018/03/19 | Published: 2018/03/19
Received: 2018/03/19 | Accepted: 2018/03/19 | Published: 2018/03/19
References
1. Kim P, Swain J. Sad dads: Paternal postpartum depression. Psychiatry (Edgmont). 2007; 4(2):35-47. PMID: 20805898
2. John WS, Cameron C, McVeigh C. Meeting the challenge of new fatherhood during the early weeks. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2005; 34(2):180-9. doi: 10.1177/0884217505274699 [DOI:10.1177/0884217505274699]
3. Massoudi P. Depression and distress in Swedish fathers in the postnatal period– prevalence, correlates, identificaton, and support [PhD thesis]. Gothenburg: University of Gothenburg; 2013.
4. Goodman JH. Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. Journal of Advanced Nursing. 2004; 45(1):26-35. doi: 10.1046/j.1365-2648.2003.02857.x [DOI:10.1046/j.1365-2648.2003.02857.x]
5. Melrose S. Paternal postpartum depression: How can nurses begin to help? Contemporary Nurse. 2010; 34(2):199-210. doi: 10.5172/conu.2010.34.2.199 [DOI:10.5172/conu.2010.34.2.199]
6. Wilson CC. Paternal postpartum distress: A discourse analytic study [PhD Thesis]. Hull: University of Hul; 2008.
7. Veskrna L. Peripartum depression –does it occur in fathers and does it matter? Journal of Men's Health. 2010; 7(4):420–30. doi: 10.1016/j.jomh.2010.10.004 [DOI:10.1016/j.jomh.2010.10.004]
8. Spector AZ. Fatherhood and depression: A review of risks, effects, and clinical application. Issues in Mental Health Nursing. 2006; 27(8):867-83. doi: 10.1080/01612840600840844 [DOI:10.1080/01612840600840844]
9. Hosseini H, Naghibi AH, Khademloo M. [Post partum depression and its relationship with some related factors (Persian)]. Journal of Babol University of Medical Sciences. 2008; 10(2):76-81.
10. Rubintan N, Esmaeelpur K, Mahmudalilu M, Seyedrasuli E. [The relationship of type of delivery and infant feeding with postpartum depression (Persian)]. Medical Journal of Tabriz University of Medical Science & Health Service. 2012; 34(3):52-6.
11. Ramchandani PG, Stein A, Oconnor T, Heron J, Murray L, Evans J. Depression in men in the postnatal period and later child psychopathology: a population cohort study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008; 47(4): 390-8. doi: 10.1097/chi.0b013e31816429c2 [DOI:10.1097/CHI.0b013e31816429c2]
12. de Montigny F, Girard ME, Lacharité C, Dubeau D, Devault A. Psychosocial factors associated with paternal postnatal depression. Journal of Affective Disorders. 2013; 150(1):44–9. doi: 10.1016/j.jad.2013.01.048 [DOI:10.1016/j.jad.2013.01.048]
13. Mao Q, Zhu LX, Su XY. A comparison of postnatal depression and related factors between Chinese new mothers and fathers. Journal of Clinical Nursing. 2011; 20(5-6):645–52. doi: 10.1111/j.1365-2702.2010.03542.x [DOI:10.1111/j.1365-2702.2010.03542.x]
14. Ramchandani P, Psychogiou L, Vlachos H, Iles J, Sethna V, Netsi E, et al. Paternal depression: an examination of its links with father, child and family functioning in the postnatal period. Depression and Anxiety. 2011; 28(6):471-7. doi: 10.1002/da.20814 [DOI:10.1002/da.20814]
15. Ramchandani P, Stein A, Evans J, O'Connor T. Paternal depression in the postnatal period and child development: a prospective population study. Lancet. 2005; 365(9478):2201-5. doi: 10.1016/s0140-6736(05)66778-5 [DOI:10.1016/S0140-6736(05)66778-5]
16. Gao L, Chan S, Mao Q. Depression, perceived stress,and social support among first-time Chinese mothers and fathers in the postpartum period. Research in Nursing & Health. 2009; 32(1):50–8. doi: 10.1002/nur.20306 [DOI:10.1002/nur.20306]
17. Nishimura A, Ohashi K. Risk factors of paternal depression in the early postnatal period in Japan. Nursing & Health Sciences. 2010; 12(2):170-6. doi: 10.1111/j.1442-2018.2010.00513.x [DOI:10.1111/j.1442-2018.2010.00513.x]
18. Schumacher M, Zubaran C, White G. Bringing birth-related paternal depression to the fore. Women and Birth. 2008; 21(2):65-70. doi: 10.1016/j.wombi.2008.03.008 [DOI:10.1016/j.wombi.2008.03.008]
19. Ahmadi Kani Golzar A, GoliZadeh Z. [Validation of Edinburgh Postpartum Depression Scale (EPDS) for screening postpartum depression in Iran (Persian)]. Iranian Journal of Psychiatric Nursing. 2015; 3(3):1-10.
20. Lai BP, Tang AK, Lee DT, Yip AS, Chung TK. Detecting postnatal depression in Chinese men: A comparison of three instruments. Psychiatry Research. 2010; 180(2-3):80-5. doi: 10.1016/j.psychres.2009.07.015 [DOI:10.1016/j.psychres.2009.07.015]
21. Matthey S, Barnett B, Kavanagh DJ, Howie P. Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. Journal of Affective Disorders. 2001; 64(2-3):175-84. doi: 10.1016/s0165-0327(00)00236-6 [DOI:10.1016/S0165-0327(00)00236-6]
22. Tran TD, Tran T, Fisher J. Validation of three psychometric instruments for screening for perinatal common mental disorders in men in the north of Vietnam. Journal of Affective Disorders. 2012; 136(1-2):104-9. doi: 10.1016/j.jad.2011.08.012 [DOI:10.1016/j.jad.2011.08.012]
23. Paulson J, Bazemore S. Prenatal and postpartum depression in fathers and its association with maternal depression. JAMA. 2010; 303(19):1961-9. doi: 10.1001/jama.2010.605 [DOI:10.1001/jama.2010.605]
24. Bielawska-Batorowicz E, Kassakowska-Petrycka K. Depressive mood in men after the birth of their offspring in relation to a partner's depression, social support, father's personality and prenatal expectations. Journal of Reproductive and Infant Psychology. 2006; 24(1):21-9. doi: 10.1080/02646830500475179 [DOI:10.1080/02646830500475179]
25. Anderson EA, Kohler JK, Letiecq BL. Predictors of depression among low-Income, nonresidential fathers. Journal of Family Issues. 2005; 26(5):547-67. doi: 10.1177/0192513x04272753 [DOI:10.1177/0192513X04272753]
26. Kiani F, Khadivzade T, Sargolzaei M, Behnam H. [Relationship between marital satisfaction during pregnancy and postpartum depression (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2009; 13(5):37-44.
27. Astaraki L. [Survey of parental – fetal attachment and associated factors in pregnant women of health and medical centers and their husbands, affiliated to Tehran universities of medical science in Tehran (Persian)] [MSc. Thesis]. Tehran: Tehran University of Medical Sciences; 2011
28. Lashkaripour K, Bakhshani NM, Hokmabadi S, Sajjadi SAR, Sarasiyabi AS. [Postpartum depression and related factors: A 4.5 months study (Persian)]. Journal of Fundamentals of Mental Health. 2012; 13(4):404-12.
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |