Thu, Apr 25, 2024
Volume 29, Issue 1 (1-2019)
JHNM 2019, 29(1): 50-55 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salimi Kivi M, Jamei-Moghadam M, Khoshlahni H, Heidarzadeh M, Kamran A, Shahabi H. Psychological Changes in Patients With Multiple Sclerosis. JHNM 2019; 29 (1) :50-55
URL: http://hnmj.gums.ac.ir/article-1-821-en.html
URL: http://hnmj.gums.ac.ir/article-1-821-en.html
Mahsa Salimi Kivi1 
 , Masomeh Jamei-Moghadam1
, Masomeh Jamei-Moghadam1 
 , Hekmat Khoshlahni2
, Hekmat Khoshlahni2 
 , Mehdi Heidarzadeh *
, Mehdi Heidarzadeh * 

 3, Aziz Kamran4
3, Aziz Kamran4 

 , Hosein Shahabi2
, Hosein Shahabi2 


 , Masomeh Jamei-Moghadam1
, Masomeh Jamei-Moghadam1 
 , Hekmat Khoshlahni2
, Hekmat Khoshlahni2 
 , Mehdi Heidarzadeh *
, Mehdi Heidarzadeh * 

 3, Aziz Kamran4
3, Aziz Kamran4 

 , Hosein Shahabi2
, Hosein Shahabi2 

1- Student Research Committee, Midwifery (BSc.), Khalkhal Medical College, Ardabil University of Medical Sciences, Ardabil, Iran.
2- Nursing (BSc.), Student Research Committee, Ardabil University of Medical Sciences, Ardabil, Iran.
3- Assistant Professor, Department of Critical Care, School of Nursing and Midwifery, Ardabil University of Medical Sciences, Ardabil, Iran. , m.mahda@gmail.com
4- Associate Professor, Educational Development Professor, Ardabil University of Medical Sciences, Ardabil, Iran
2- Nursing (BSc.), Student Research Committee, Ardabil University of Medical Sciences, Ardabil, Iran.
3- Assistant Professor, Department of Critical Care, School of Nursing and Midwifery, Ardabil University of Medical Sciences, Ardabil, Iran. , m.mahda@gmail.com
4- Associate Professor, Educational Development Professor, Ardabil University of Medical Sciences, Ardabil, Iran
Full-Text [PDF 493 kb]
(855 Downloads)
| Abstract (HTML) (3289 Views)
Discussion
The study results indicate that the study subjects experienced a moderate level of posttraumatic growth. Few studies have examined the posttraumatic growth in patients with MS by using PTGI. The study of Ackroyd reported that the MS patients experienced some degrees of growth [19]. Comparing various studies, the mean score of posttraumatic growth in the present study was higher than the scores in other studies on patients with MS [19], cancer [24, 25] and non-clinical stressful events [26, 27]. This finding suggests that Iranian people who experience MS stressful incident will experience more positive psychological changes as well. However, in studies that have examined the posttraumatic growth in patients with cancer and myocardial infarction in Iranian society [28, 29], the PTGI score was lower than in the present study. It seems that stressful events such as cancer that are more severe and make people feeling closer to death will also cause more psychological changes.
Evaluating the posttraumatic growth items reveals that the highest growth rate belonged respectively to the dimensions of spiritual changes, relating to others, appreciation of life, personal strengthening, and new possibilities. These results were similar to the results of previous studies that have examined the posttraumatic growth in Iranian samples with cancer [28] and myocardial infarction [29] which have reported the spiritual changes and relating to others as two very important dimensions of positive changes after the occurrence of a stressful event. However, in studies conducted in modern societies, other aspects of posttraumatic growth have been reported as the priority changes [24, 26, 27].
In a study by Morris, the dimensions of appreciating the life and spirituality have achieved the highest and lowest scores, respectively [24]. This difference indicate that due to religious and traditional structure of Iran society [30], after a stressful event, the tendency toward the source of spirituality and relating to others (given that the supports of family and kinships are the greatest support in such situations) are the common strategy in Iranian society that is associated with their significant growth in this area.
Evaluating the demoralization revealed that the patients experience some degree of demoralization after developing MS. Moreover, a significant inverse correlation was seen between the score of demoralization and posttraumatic growth and its dimensions; so that the posttraumatic growth score increased by reducing the demoralization. In a study by Li, it was found that cancer patients experience both positive and negative aspects of psychological changes; so that some degree of demoralization and posttraumatic growth was reported in them. In addition, they observed an inverse relationship between posttraumatic growth and demoralization; so that by reducing the score of demoralization, the posttraumatic growth score increased [31].
In a study conducted by Mohr, it was found that patients with MS experienced both positive and negative aspects of changes in living with the disease [17]. In a study it was found that the developing of cancer lead to the demoralization in involved patients. Since the tool used in both studies were the same, it was observed that the demoralization score in patients with MS in this study was higher than its score in patients with cancer in the study by Li [32]. Because few studies have been conducted on demoralization in MS patients in different parts of the world, there is little information on factors affecting the demoralization, and further studies are required in this area.
The notable finding in our study was the weak relationship between the dimension of spirituality and demoralization, which their correlation coefficient was significantly low in comparison with other aspects of posttraumatic growth. Thus, demoralization explains only 5% of changes of spiritual dimension in patients with MS. This suggests that Iranian patients with MS, at every level of psychological disorders, will be inclined to spirituality according to the religious context. Previous studies [33, 34] have reported that during stressful incidents, the affected patients use spirituality as a coping strategy. It seems that tendency to spirituality in MS patients, even in the presence of demoralization, is a coping strategy in the first step and then, the patients will achieve a significant spiritual growth.
Although this study has provided valuable information on psychological changes in patients with MS, it has some limitations, too. Due to lack of access to all patients in the city, the study samples were recruited by convenience sampling method that affects the generalizability of the results. This study was merely a descriptive-correlational study that provided some information in relation to the strong relationship between demoralization and posttraumatic growth. However, further studies should be conducted as clinical trials to determine the cause and effect impacts of these variables.
The results of this study indicate that MS patients in Ardabil experienced both negative changes (demoralization) and positive changes (posttraumatic growth) in the psychological context. In addition, a significant inverse correlation was found between these two variables, so that by reducing demoralization, the posttraumatic growth increases. Given that demoralization is a major obstacle in creating positive psychological changes in MS patients, nurses, psychology counselors and other caregivers in the community can consider this concept and by reducing demoralization, can alleviate the patients’ psychological problems and provide the context to bring positive changes for them.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Ardabil University of Medical Sciences (IR.ARUMS.REC.1394.99).
Funding
This study was part of a research project approved by the Student Research Committee of Ardabil University of Medical Sciences.
Authors contributions
The authors contributions is as follows: Data collection: Mahsa Salimi Kivi, Masomeh Jamei-Moghadam and Hosein Shahabi; Importing data in computer: Masomeh Jamei-Moghadam; Data analysis and interpretation: Mahsa Salimi Kivi, Mehdi Heidarzadeh and Aziz Kamran; Design: Mehdi Heidarzadeh and Mahsa Salimi Kivi; Writing: Mahsa Salimi Kivi and Mehdi Heidarzadeh; Critical revision of the manuscript: Aziz Kamran; and Leader of research team: Mehdi Heidarzadeh.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
We would like to thank the officials and employees of School of Nursing and Midwifery of Khalkhal, Alavi Hospital Emergency Department and the MS Society of Ardabil and all the study participants.
References
Full-Text: (1093 Views)
Introduction
Multiple Sclerosis (MS) is a disease caused by reduced speed of neurotransmission. It is also the most common cause of disability that lead to several physical and mental problems and family and social dysfunction for the involved people. The disease has currently affected more than 1.3 million people worldwide [1]. In recent years, studies in the Middle East and Iran have suggested a relatively high and increasing prevalence of MS [2]. People with MS experience symptoms and side effects such as fatigue, physical disability, cognitive impairment, pain, and depression [3]. One of the serious complications of the disease is the development of disability, particularly in young patients. Thus, MS is currently considered as the second leading cause of disability in young people in Iran. Given that the most people in this age are at the peak of their individual, social, and family responsibilities, the disease creates serious problems for them [4].
One of the psychiatric disorders in dealing with stressful events is demoralization. Demoralization refers to an inhibitory reaction in response to overwhelming stresses, which appears following perceived inability related to the continuing adaptation and concern, disappointment and feelings of inadequacy [5]. This concept has been suggested for the first time in 1970 by Frank to describe a situation of perceived incompetence, failure to comply, hopelessness, existential despair and meaninglessness of life that occur frequently following the treatment of health problems in people [6].
The clinical features of the demoralization syndrome include sense of dysmorphic body, physical disability, chronic diseases, social isolation, depression, feeling of inadequacy and mistrust, confusion, loss of self-confidence and despair [7]. Demoralization is a kind of distress that has a high correlation with physical disorders [5]. It can act as a major obstacle in the recovery of the patients [8]. Kissane et al. believed that “in the event of demoralization, negative thoughts are developed in people about the ability to make influence on issues, and thus, they will lack appropriate motivation and morale for doing efforts to test new ways of coping in the future, and gradually would go down into social isolation” [9].
Although, few studies related to demoralization in MS patients have been conducted, other studies have reported that severe and incurable diseases, such as immune deficiency syndromes, can lead to demoralization syndrome [10]. Meanwhile, some studies have also reported the occurrence rate of demoralization as 13% in people with chronic diseases [11, 12]. Many scientific evidence and documents obtained over the past 30 years suggest that trauma and stressful events not only lead to health threats [13-15], but also may act as facilitating factors for positive psychological changes [14]. Thus in the stressful conditions of the present life, people would also may grow [15].
In other words, despite the fact that stressful events in people’s lives may lead to adverse effects in various physical, mental and social aspects, in the meantime, dealing with these events will lead to the growth of various human aspects. The term “posttraumatic growth” is defined as “a subjective experience of positive psychological changes that is created by a person due to coping with highly challenging situations in the life” [16]. The term “posttraumatic” emphasizes that growth occurs after a very stressful event and not after any minor stress or during normal development process. The term “growth” refers to the fact that the person will achieve a progress that is beyond his level of compatibility, mental performance or awareness. This suggests that new positive achievements and further and meaningful benefits will be seen in people’s life compared to the pre-crisis status [15].
Developing MS as a stressful event, following by physical, mental and social problems can be the source of many positive effects for the involved people and coping with this disease can also be associated with beneficial psychological effects [17]. Mohr and Pakenham studies highlight the growth concepts such as deepening of relationships, appreciating the life, increased spirituality, becoming stronger, new opportunities, and changes in life priorities [17, 18]. In studies that have examined the posttraumatic growth in patients with MS by quantitative method, some degrees of posttraumatic growth have been also reported [19, 20].
Given that demoralization in patients with chronic diseases impairs their healing process and coping with the conditions of disease, it is highly important to recognize and solve it. However, the review of literature reveals no relevant study on patients with multiple sclerosis, especially in Iranian society. Since few studies have examined the positive psychological effects (posttraumatic growth) and demoralization in patients with MS, especially in Iranian society, we aimed to explore the concept of posttraumatic growth and its dimensions as well as the concept of demoralization in patients with MS.
Materials and Methods
This study was a cross-sectional research. The study population consisted of all patients with MS who were the members of the MS Society in the city of Ardebil in the north of Iran. By convenience sampling method, all eligible patients willing to participate in the study were entered into the study (From February to June 2016) after explaining the study objectives and ensuring them about the confidentiality of information. The study inclusion criteria were as follows: diagnosis of MS by a neurologist, at least 6 months passed of their initial diagnosis, and ability to communicate and respond to questions. The patients with cognitive disorders (according to the patient history and medical records) as well as those unwilling to participate were excluded from the study.
Considering sample size formula for correlational studies [21] and using a two-sided significance level of 5% and a power analysis of 80% with correlation coefficient of r=-0.3 (calculated from the data of 20 participants in a pilot study), the minimum required sample was estimated as 85. There were a total of 597 patients with MS in Ardabil, of which 160 eligible patients were included in the study, and 14 patients were excluded from the study due to failure in answering the study questions. Finally, the data from 146 eligible patients were analyzed in SPSS V. 22. For this purpose, descriptive statistics (mean, standard deviation, minimum and maximum) and inferential statistics (Pearson correlation coefficient) were used to classify the data and find correlation of posttraumatic growth and demoralization in MS patients.
In this study, the relevant data were collected using questionnaire through interviews. The questionnaire used in this study included a demographic characteristics questionnaire, posttraumatic growth inventory, and demoralization scale. The Post-Traumatic Growth Inventory (PTGI) was designed in 1996 by Tedeschi and Calhoun in the United States to assess the concept of posttraumatic growth. It has 21 items that assess the psychological growth rate after facing a stressful event in 5 areas of personal strengthening, relating to others, appreciation of life, spiritual changes, and new possibilities. The tool was scored on a 6-point Likert-type scale from 0=no, 1=very little, 2=little, 3=moderately, 4=much, and 5=very much. The total score ranges from 0 to 105, where higher scores indicate higher posttraumatic growth and lower scores represented lower posttraumatic growth [22].
Heidarzadeh reported the psychometric characteristics of the posttraumatic growth inventory as valid for use in Iranian samples who experienced stressful events [23]. The demoralization scale was designed by Kissane et al. in 2004. It has 24 items with 5-point Likert-type rating scale that each item score ranges from 0 to 4. Higher scores indicate higher demoralization [9]. The tool was translated by the researchers, and its content validity was confirmed by 10 experts, including 4 nurses working in wards associated with the MS disease, 5 nursing faculty members and one neurologist. In addition, the internal consistency of the tool was confirmed with Cronbach α coefficient of 0.83.
Results
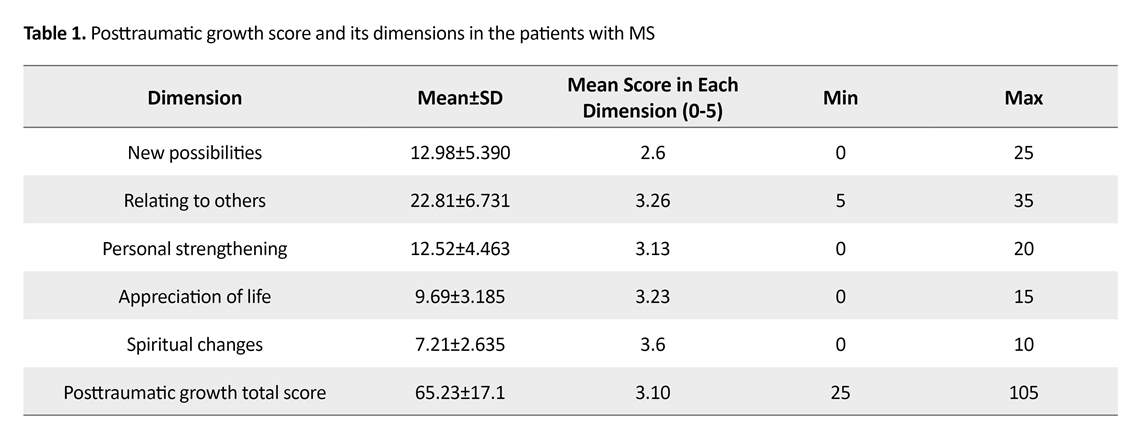
The Mean±SD of the subjects was 33.59±8.70 years (age range: 18 to 57 years). Most subjects were female (67.8%), married (67.1%), with an average income level (52.7%) and receiving some degree of help in daily activities due to their disability. Their mean duration of developing MS was 67 months (range: 6 months to 20 years.) The Post-Traumatic Growth Inventory (PTGI) Mean±SD scores in patients with MS were 65.23±17.1.
It was also found that the mean scores from highest to lowest belonged to the dimensions of spiritual changes, relating to others, appreciation of life, personal strengthening, and new possibilities, respectively (Table 1). The results also indicate that the Mean±SD score of demoralization was 34.71±18.22. Meanwhile, an inverse and significant relationship was found between demoralization and posttraumatic growth (P<0.001; r=-0.57) and its dimensions (P<0.001; r=-0.23 to -0.55) (Table 2).
Multiple Sclerosis (MS) is a disease caused by reduced speed of neurotransmission. It is also the most common cause of disability that lead to several physical and mental problems and family and social dysfunction for the involved people. The disease has currently affected more than 1.3 million people worldwide [1]. In recent years, studies in the Middle East and Iran have suggested a relatively high and increasing prevalence of MS [2]. People with MS experience symptoms and side effects such as fatigue, physical disability, cognitive impairment, pain, and depression [3]. One of the serious complications of the disease is the development of disability, particularly in young patients. Thus, MS is currently considered as the second leading cause of disability in young people in Iran. Given that the most people in this age are at the peak of their individual, social, and family responsibilities, the disease creates serious problems for them [4].
One of the psychiatric disorders in dealing with stressful events is demoralization. Demoralization refers to an inhibitory reaction in response to overwhelming stresses, which appears following perceived inability related to the continuing adaptation and concern, disappointment and feelings of inadequacy [5]. This concept has been suggested for the first time in 1970 by Frank to describe a situation of perceived incompetence, failure to comply, hopelessness, existential despair and meaninglessness of life that occur frequently following the treatment of health problems in people [6].
The clinical features of the demoralization syndrome include sense of dysmorphic body, physical disability, chronic diseases, social isolation, depression, feeling of inadequacy and mistrust, confusion, loss of self-confidence and despair [7]. Demoralization is a kind of distress that has a high correlation with physical disorders [5]. It can act as a major obstacle in the recovery of the patients [8]. Kissane et al. believed that “in the event of demoralization, negative thoughts are developed in people about the ability to make influence on issues, and thus, they will lack appropriate motivation and morale for doing efforts to test new ways of coping in the future, and gradually would go down into social isolation” [9].
Although, few studies related to demoralization in MS patients have been conducted, other studies have reported that severe and incurable diseases, such as immune deficiency syndromes, can lead to demoralization syndrome [10]. Meanwhile, some studies have also reported the occurrence rate of demoralization as 13% in people with chronic diseases [11, 12]. Many scientific evidence and documents obtained over the past 30 years suggest that trauma and stressful events not only lead to health threats [13-15], but also may act as facilitating factors for positive psychological changes [14]. Thus in the stressful conditions of the present life, people would also may grow [15].
In other words, despite the fact that stressful events in people’s lives may lead to adverse effects in various physical, mental and social aspects, in the meantime, dealing with these events will lead to the growth of various human aspects. The term “posttraumatic growth” is defined as “a subjective experience of positive psychological changes that is created by a person due to coping with highly challenging situations in the life” [16]. The term “posttraumatic” emphasizes that growth occurs after a very stressful event and not after any minor stress or during normal development process. The term “growth” refers to the fact that the person will achieve a progress that is beyond his level of compatibility, mental performance or awareness. This suggests that new positive achievements and further and meaningful benefits will be seen in people’s life compared to the pre-crisis status [15].
Developing MS as a stressful event, following by physical, mental and social problems can be the source of many positive effects for the involved people and coping with this disease can also be associated with beneficial psychological effects [17]. Mohr and Pakenham studies highlight the growth concepts such as deepening of relationships, appreciating the life, increased spirituality, becoming stronger, new opportunities, and changes in life priorities [17, 18]. In studies that have examined the posttraumatic growth in patients with MS by quantitative method, some degrees of posttraumatic growth have been also reported [19, 20].
Given that demoralization in patients with chronic diseases impairs their healing process and coping with the conditions of disease, it is highly important to recognize and solve it. However, the review of literature reveals no relevant study on patients with multiple sclerosis, especially in Iranian society. Since few studies have examined the positive psychological effects (posttraumatic growth) and demoralization in patients with MS, especially in Iranian society, we aimed to explore the concept of posttraumatic growth and its dimensions as well as the concept of demoralization in patients with MS.
Materials and Methods
This study was a cross-sectional research. The study population consisted of all patients with MS who were the members of the MS Society in the city of Ardebil in the north of Iran. By convenience sampling method, all eligible patients willing to participate in the study were entered into the study (From February to June 2016) after explaining the study objectives and ensuring them about the confidentiality of information. The study inclusion criteria were as follows: diagnosis of MS by a neurologist, at least 6 months passed of their initial diagnosis, and ability to communicate and respond to questions. The patients with cognitive disorders (according to the patient history and medical records) as well as those unwilling to participate were excluded from the study.
Considering sample size formula for correlational studies [21] and using a two-sided significance level of 5% and a power analysis of 80% with correlation coefficient of r=-0.3 (calculated from the data of 20 participants in a pilot study), the minimum required sample was estimated as 85. There were a total of 597 patients with MS in Ardabil, of which 160 eligible patients were included in the study, and 14 patients were excluded from the study due to failure in answering the study questions. Finally, the data from 146 eligible patients were analyzed in SPSS V. 22. For this purpose, descriptive statistics (mean, standard deviation, minimum and maximum) and inferential statistics (Pearson correlation coefficient) were used to classify the data and find correlation of posttraumatic growth and demoralization in MS patients.
In this study, the relevant data were collected using questionnaire through interviews. The questionnaire used in this study included a demographic characteristics questionnaire, posttraumatic growth inventory, and demoralization scale. The Post-Traumatic Growth Inventory (PTGI) was designed in 1996 by Tedeschi and Calhoun in the United States to assess the concept of posttraumatic growth. It has 21 items that assess the psychological growth rate after facing a stressful event in 5 areas of personal strengthening, relating to others, appreciation of life, spiritual changes, and new possibilities. The tool was scored on a 6-point Likert-type scale from 0=no, 1=very little, 2=little, 3=moderately, 4=much, and 5=very much. The total score ranges from 0 to 105, where higher scores indicate higher posttraumatic growth and lower scores represented lower posttraumatic growth [22].
Heidarzadeh reported the psychometric characteristics of the posttraumatic growth inventory as valid for use in Iranian samples who experienced stressful events [23]. The demoralization scale was designed by Kissane et al. in 2004. It has 24 items with 5-point Likert-type rating scale that each item score ranges from 0 to 4. Higher scores indicate higher demoralization [9]. The tool was translated by the researchers, and its content validity was confirmed by 10 experts, including 4 nurses working in wards associated with the MS disease, 5 nursing faculty members and one neurologist. In addition, the internal consistency of the tool was confirmed with Cronbach α coefficient of 0.83.
Results
The Mean±SD of the subjects was 33.59±8.70 years (age range: 18 to 57 years). Most subjects were female (67.8%), married (67.1%), with an average income level (52.7%) and receiving some degree of help in daily activities due to their disability. Their mean duration of developing MS was 67 months (range: 6 months to 20 years.) The Post-Traumatic Growth Inventory (PTGI) Mean±SD scores in patients with MS were 65.23±17.1.
It was also found that the mean scores from highest to lowest belonged to the dimensions of spiritual changes, relating to others, appreciation of life, personal strengthening, and new possibilities, respectively (Table 1). The results also indicate that the Mean±SD score of demoralization was 34.71±18.22. Meanwhile, an inverse and significant relationship was found between demoralization and posttraumatic growth (P<0.001; r=-0.57) and its dimensions (P<0.001; r=-0.23 to -0.55) (Table 2).
Discussion
The study results indicate that the study subjects experienced a moderate level of posttraumatic growth. Few studies have examined the posttraumatic growth in patients with MS by using PTGI. The study of Ackroyd reported that the MS patients experienced some degrees of growth [19]. Comparing various studies, the mean score of posttraumatic growth in the present study was higher than the scores in other studies on patients with MS [19], cancer [24, 25] and non-clinical stressful events [26, 27]. This finding suggests that Iranian people who experience MS stressful incident will experience more positive psychological changes as well. However, in studies that have examined the posttraumatic growth in patients with cancer and myocardial infarction in Iranian society [28, 29], the PTGI score was lower than in the present study. It seems that stressful events such as cancer that are more severe and make people feeling closer to death will also cause more psychological changes.
Evaluating the posttraumatic growth items reveals that the highest growth rate belonged respectively to the dimensions of spiritual changes, relating to others, appreciation of life, personal strengthening, and new possibilities. These results were similar to the results of previous studies that have examined the posttraumatic growth in Iranian samples with cancer [28] and myocardial infarction [29] which have reported the spiritual changes and relating to others as two very important dimensions of positive changes after the occurrence of a stressful event. However, in studies conducted in modern societies, other aspects of posttraumatic growth have been reported as the priority changes [24, 26, 27].
In a study by Morris, the dimensions of appreciating the life and spirituality have achieved the highest and lowest scores, respectively [24]. This difference indicate that due to religious and traditional structure of Iran society [30], after a stressful event, the tendency toward the source of spirituality and relating to others (given that the supports of family and kinships are the greatest support in such situations) are the common strategy in Iranian society that is associated with their significant growth in this area.
Evaluating the demoralization revealed that the patients experience some degree of demoralization after developing MS. Moreover, a significant inverse correlation was seen between the score of demoralization and posttraumatic growth and its dimensions; so that the posttraumatic growth score increased by reducing the demoralization. In a study by Li, it was found that cancer patients experience both positive and negative aspects of psychological changes; so that some degree of demoralization and posttraumatic growth was reported in them. In addition, they observed an inverse relationship between posttraumatic growth and demoralization; so that by reducing the score of demoralization, the posttraumatic growth score increased [31].
In a study conducted by Mohr, it was found that patients with MS experienced both positive and negative aspects of changes in living with the disease [17]. In a study it was found that the developing of cancer lead to the demoralization in involved patients. Since the tool used in both studies were the same, it was observed that the demoralization score in patients with MS in this study was higher than its score in patients with cancer in the study by Li [32]. Because few studies have been conducted on demoralization in MS patients in different parts of the world, there is little information on factors affecting the demoralization, and further studies are required in this area.
The notable finding in our study was the weak relationship between the dimension of spirituality and demoralization, which their correlation coefficient was significantly low in comparison with other aspects of posttraumatic growth. Thus, demoralization explains only 5% of changes of spiritual dimension in patients with MS. This suggests that Iranian patients with MS, at every level of psychological disorders, will be inclined to spirituality according to the religious context. Previous studies [33, 34] have reported that during stressful incidents, the affected patients use spirituality as a coping strategy. It seems that tendency to spirituality in MS patients, even in the presence of demoralization, is a coping strategy in the first step and then, the patients will achieve a significant spiritual growth.
Although this study has provided valuable information on psychological changes in patients with MS, it has some limitations, too. Due to lack of access to all patients in the city, the study samples were recruited by convenience sampling method that affects the generalizability of the results. This study was merely a descriptive-correlational study that provided some information in relation to the strong relationship between demoralization and posttraumatic growth. However, further studies should be conducted as clinical trials to determine the cause and effect impacts of these variables.
The results of this study indicate that MS patients in Ardabil experienced both negative changes (demoralization) and positive changes (posttraumatic growth) in the psychological context. In addition, a significant inverse correlation was found between these two variables, so that by reducing demoralization, the posttraumatic growth increases. Given that demoralization is a major obstacle in creating positive psychological changes in MS patients, nurses, psychology counselors and other caregivers in the community can consider this concept and by reducing demoralization, can alleviate the patients’ psychological problems and provide the context to bring positive changes for them.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Ardabil University of Medical Sciences (IR.ARUMS.REC.1394.99).
Funding
This study was part of a research project approved by the Student Research Committee of Ardabil University of Medical Sciences.
Authors contributions
The authors contributions is as follows: Data collection: Mahsa Salimi Kivi, Masomeh Jamei-Moghadam and Hosein Shahabi; Importing data in computer: Masomeh Jamei-Moghadam; Data analysis and interpretation: Mahsa Salimi Kivi, Mehdi Heidarzadeh and Aziz Kamran; Design: Mehdi Heidarzadeh and Mahsa Salimi Kivi; Writing: Mahsa Salimi Kivi and Mehdi Heidarzadeh; Critical revision of the manuscript: Aziz Kamran; and Leader of research team: Mehdi Heidarzadeh.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
We would like to thank the officials and employees of School of Nursing and Midwifery of Khalkhal, Alavi Hospital Emergency Department and the MS Society of Ardabil and all the study participants.
References
- Kingwell E, Bajdik C, Phillips N, Zhu F, Oger J, Hashimoto S, et al. Cancer risk in multiple sclerosis: Findings from British Columbia, Canada. Brain. 2012; 135(10):2973-9. [DOI:10.1093/brain/aws148] [PMID]
- Elhami SR, Mohammad K, Sahraian MA, Eftekhar H. A 20-year incidence trend (1989–2008) and point prevalence (March 20, 2009) of multiple sclerosis in Tehran, Iran: A population-based study. Neuroepidemiology. 2011; 36(3):141-7. [DOI:10.1159/000324708] [PMID]
- Brunner LS. Brunner & Suddarth’s textbook of medical-surgical nursing. Philadelphia: Lippincott Williams & Wilkins; 2010.
- Kessler TM, Fowler CJ, Panicker JN. Sexual dysfunction in multiple sclerosis. Expert Review of Neurotherapeutics. 2009; 9(3):341-50. [DOI:10.1586/14737175.9.3.341] [PMID]
- Vehling S, Mehnert A. Symptom burden, loss of dignity, and demoralization in patients with cancer: A mediation model. Psycho‐Oncology. 2014; 23(3):283-90. [DOI:10.1002/pon.3417] [PMID]
- Frank JD. Psychotherapy: The restoration of morale. American Journal of Psychiatry. 1974; 131(3):271-4. [DOI:10.1176/ajp.131.3.271] [PMID]
- Marchesi C, Maggini C. Socio-demographic and clinical features associated with demoralization in medically ill in-patients. Social Psychiatry and Psychiatric Epidemiology. 2007; 42(10):824-9. [DOI:10.1007/s00127-007-0230-z] [PMID]
- Cavelti M, Kvrgic S, Beck EM, Rüsch N, Vauth R. Self-stigma and its relationship with insight, demoralization, and clinical outcome among people with schizophrenia spectrum disorders. Comprehensive Psychiatry. 2012; 53(5):468-79. [DOI:10.1016/j.comppsych.2011.08.001] [PMID]
- Kissane DW, Wein S, Love A, Lee XQ. The demoralization scale: A report of its development and preliminary validation. Journal of Palliative Care. 2004; 20(4):269-76. [PMID]
- Briggs L, Macleod S. Demoralization or clinical depression? Enhancing understandings of psychological distress in resettled refugees and migrants. World Cultural Psychiatry Research Review. 2010; 5(2):86-98.
- Robinson S, Kissane DW, Brooker J, Burney S. A systematic review of the demoralization syndrome in individuals with progressive disease and cancer: A decade of research. Journal of Pain and Symptom Management. 2015; 49(3):595-610. [DOI:10.1016/j.jpainsymman.2014.07.008] [PMID]
- Robinson S, Kissane DW, Brooker J, Burney S. A review of the construct of demoralization: History, definitions, and future directions for palliative care. American Journal of Hospice and Palliative Medicine. 2016; 33(1):93-101. [DOI:10.1177/1049909114553461] [PMID]
- Zamanzadeh V, Heydarzadeh M, Oshvandi Kh, Argani H, Abedi Azar S. [Effect of physical exercises on quality of life in hemodialysis patients (Persian)]. Medical Journal of Tabriz University of Medical Sciences. 2008; 30(1):51-5.
- Schroevers MJ, Helgeson VS, Sanderman R, Ranchor AV. Type of social support matters for prediction of posttraumatic growth among cancer survivors. Psycho‐Oncology. 2010; 9(1):46-53. [DOI:10.1002/pon.1501] [PMID]
- Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004; 15(1):1-18. [DOI:10.1207/s15327965pli1501_01]
- Zwahlen D, Hagenbuch N, Carley MI, Jenewein J, Buchi S. Posttraumatic growth in cancer patients and partners-effects of role, gender and the dyad on couples’ posttraumatic growth experience. Psycho‐Oncology. 2010; 19(1):12-20. [DOI:10.1002/pon.1486] [PMID]
- Mohr DC, Dick LP, Russo D, Pinn J, Boudewyn AC, Likosky W, et al. The psychosocial impact of multiple sclerosis: Exploring the patient’s perspective. Health Psychology. 1999; 18(4):376-82. [DOI:10.1037/0278-6133.18.4.376] [PMID]
- Pakenham KI. The nature of benefit finding in Multiple Sclerosis (MS). Psychology, Health & Medicine. 2007; 12(2):190-6. [DOI:10.1080/13548500500465878] [PMID]
- Ackroyd K, FortuneDG, Price S, Howell S, Sharrack B, Isaac CL. Adversarial growth in patients with multiple sclerosis and their partners: Relationships with illness perceptions, disability and distress. Journal of Clinical Psychology in Medical Settings. 2011; 18(4):372-9. [DOI:10.1007/s10880-011-9265-0] [PMID]
- Hart SL, Vella L, Mohr DC. Relationships among depressive symptoms, benefit-finding, optimism, and positive affect in multiple sclerosis patients after psychotherapy for depression. Health Psychology. 2008; 27(2):230-8. [DOI:10.1037/0278-6133.27.2.230] [PMID] [PMCID]
- Hulley SB, Cummings SR, Browner WS, Grady D, Newman TB. Designing clinical research: An epidemiologic approach. Philadelphia: Lippincott Williams & Wilkins; 2013.
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996; 9(3):455-71. [DOI:10.1002/jts.2490090305]
- Heidarzadeh M, Naseri P, Shamshiri M, Dadkhah B, Rassouli M, Gholchin M. Evaluating the factor structure of the persian version of posttraumatic growth inventory in cancer patients. Asian Nursing Research. 2017; 11(3):180-6. [DOI:10.1016/j.anr.2017.07.003] [PMID]
- Morris BA, Shakespeare Finch J, Scott JL. Posttraumatic growth after cancer: The importance of health-related benefits and newfound compassion for others. Supportive Care in Cancer. 2012; 20(4):749-56. [DOI:10.1007/s00520-011-1143-7] [PMID]
- Bellizzi KM, Smith AW, Reeve BB, Alfano CM, Bernstein L, Meeske K, et al. Posttraumatic growth and health-related quality of life in a racially diverse cohort of breast cancer survivors. Journal of Health Psychology. 2010; 15(4):615-26. [DOI:10.1177/1359105309356364] [PMID]
- Hooper LM, Marotta SA, Depuy V. A confirmatory factor analytic study of the posttraumatic growth inventory among a sample of racially diverse college students. Journal of Mental Health. 2009; 18(4):335-43. [DOI:10.1080/09638230802522502]
- Lee JA, Luxton DD, Reger GM, Gahm GA. Confirmatory factor analysis of the Posttraumatic Growth Inventory with a sample of soldiers previously deployed in support of the Iraq and Afghanistan wars. Journal of Clinical Psychology. 2010; 66(7):813-9. [DOI:10.1002/jclp.20692] [PMID]
- Heidarzadeh M, Rassouli M, Shahbolaghi FM, Majd HA, Karam AM, Mirzaee H, et al. Posttraumatic growth and its dimensions in patients with cancer. Middle East Journal of Cancer. 2014; 5(1):23-9.
- Rahimi R, Heidarzadeh M, Shoaee R. The relationship between posttraumatic growth and social support in patients with myocardial infarction. Canadian Journal of Cardiovascular Nursing. 2016; 26 (2):19-24. [PMID]
- Heidarzadeh M, Hassani P, Ghahramanian A, Ilnaz Y. [Quality of life and social support in congestive heart failure patients and healthy people (Persian)]. Holistic Nursing and Midwifery Journal. 2013; 23(1):13-21.
- Li YC, Yeh PC, Chen HW, Chang YF, Pi SH, Fang CK. Posttraumatic growth and demoralization after cancer: The effects of patients’ meaning-making. Palliative and Supportive Care. 2015; 13(5): 1449-58. [DOI:10.1017/S1478951515000048] [PMID]
- Li YC, Ho CH, Wang HH. Demoralization in cancer patients and related factors in Taiwan. Cancer Nursing. 2017; 40(1):E54-E60. [DOI:10.1097/NCC.0000000000000352] [PMID]
- Farsi Z, Dehghan Nayeri N, Negarandeh R. Coping strategies of adults with leukemia undergoing hematopoieticstem cell transplantation in Iran: A qualitative study. Nursing & Health Sciences. 2010; 12(4):485-92. [DOI:10.1111/j.1442-2018.2010.00563.x] [PMID]
- Heidarzadeh M, Rassouli M, Ghanavati A, Mirzaei H, Tahmasebi M. Spiritual growth in cancer patients: A qualitative study. Bulletin of Environment, Pharmacology and Life Sciences. 2014; 3(9):92-7.
Article Type : Research |
Subject:
Special
Received: 2018/06/6 | Accepted: 2018/10/25 | Published: 2019/01/1
Received: 2018/06/6 | Accepted: 2018/10/25 | Published: 2019/01/1
References
1. Kingwell E, Bajdik C, Phillips N, Zhu F, Oger J, Hashimoto S, et al. Cancer risk in multiple sclerosis: Findings from British Columbia, Canada. Brain. 2012; 135(10):2973-9. [DOI:10.1093/brain/aws148] [PMID] [DOI:10.1093/brain/aws148]
2. Elhami SR, Mohammad K, Sahraian MA, Eftekhar H. A 20-year incidence trend (1989–2008) and point prevalence (March 20, 2009) of multiple sclerosis in Tehran, Iran: A population-based study. Neuroepidemiology. 2011; 36(3):141-7. [DOI:10.1159/000324708] [PMID] [DOI:10.1159/000324708]
3. Brunner LS. Brunner & Suddarth's textbook of medical-surgical nursing. Philadelphia: Lippincott Williams & Wilkins; 2010.
4. Kessler TM, Fowler CJ, Panicker JN. Sexual dysfunction in multiple sclerosis. Expert Review of Neurotherapeutics. 2009; 9(3):341-50. [DOI:10.1586/14737175.9.3.341] [PMID] [DOI:10.1586/14737175.9.3.341]
5. Vehling S, Mehnert A. Symptom burden, loss of dignity, and demoralization in patients with cancer: A mediation model. Psycho‐Oncology. 2014; 23(3):283-90. [DOI:10.1002/pon.3417] [PMID] [DOI:10.1002/pon.3417]
6. Frank JD. Psychotherapy: The restoration of morale. American Journal of Psychiatry. 1974; 131(3):271-4. [DOI:10.1176/ajp.131.3.271] [PMID] [DOI:10.1176/ajp.131.3.271]
7. Marchesi C, Maggini C. Socio-demographic and clinical features associated with demoralization in medically ill in-patients. Social Psychiatry and Psychiatric Epidemiology. 2007; 42(10):824-9. [DOI:10.1007/s00127-007-0230-z] [PMID] [DOI:10.1007/s00127-007-0230-z]
8. Cavelti M, Kvrgic S, Beck EM, Rüsch N, Vauth R. Self-stigma and its relationship with insight, demoralization, and clinical outcome among people with schizophrenia spectrum disorders. Comprehensive Psychiatry. 2012; 53(5):468-79. [DOI:10.1016/j.comppsych.2011.08.001] [PMID] [DOI:10.1016/j.comppsych.2011.08.001]
9. Kissane DW, Wein S, Love A, Lee XQ. The demoralization scale: A report of its development and preliminary validation. Journal of Palliative Care. 2004; 20(4):269-76. [PMID] [PMID]
10. Briggs L, Macleod S. Demoralization or clinical depression? Enhancing understandings of psychological distress in resettled refugees and migrants. World Cultural Psychiatry Research Review. 2010; 5(2):86-98.
11. Robinson S, Kissane DW, Brooker J, Burney S. A systematic review of the demoralization syndrome in individuals with progressive disease and cancer: A decade of research. Journal of Pain and Symptom Management. 2015; 49(3):595-610. [DOI:10.1016/j.jpainsymman.2014.07.008] [PMID] [DOI:10.1016/j.jpainsymman.2014.07.008]
12. Robinson S, Kissane DW, Brooker J, Burney S. A review of the construct of demoralization: History, definitions, and future directions for palliative care. American Journal of Hospice and Palliative Medicine. 2016; 33(1):93-101. [DOI:10.1177/1049909114553461] [PMID] [DOI:10.1177/1049909114553461]
13. Zamanzadeh V, Heydarzadeh M, Oshvandi Kh, Argani H, Abedi Azar S. [Effect of physical exercises on quality of life in hemodialysis patients (Persian)]. Medical Journal of Tabriz University of Medical Sciences. 2008; 30(1):51-5.
14. Schroevers MJ, Helgeson VS, Sanderman R, Ranchor AV. Type of social support matters for prediction of posttraumatic growth among cancer survivors. Psycho‐Oncology. 2010; 9(1):46-53. [DOI:10.1002/pon.1501] [PMID] [DOI:10.1002/pon.1501]
15. Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004; 15(1):1-18. [DOI:10.1207/s15327965pli1501_01] [DOI:10.1207/s15327965pli1501_01]
16. Zwahlen D, Hagenbuch N, Carley MI, Jenewein J, Buchi S. Posttraumatic growth in cancer patients and partners-effects of role, gender and the dyad on couples' posttraumatic growth experience. Psycho‐Oncology. 2010; 19(1):12-20. [DOI:10.1002/pon.1486] [PMID] [DOI:10.1002/pon.1486]
17. Mohr DC, Dick LP, Russo D, Pinn J, Boudewyn AC, Likosky W, et al. The psychosocial impact of multiple sclerosis: Exploring the patient's perspective. Health Psychology. 1999; 18(4):376-82. [DOI:10.1037/0278-6133.18.4.376] [PMID] [DOI:10.1037/0278-6133.18.4.376]
18. Pakenham KI. The nature of benefit finding in Multiple Sclerosis (MS). Psychology, Health & Medicine. 2007; 12(2):190-6. [DOI:10.1080/13548500500465878] [PMID] [DOI:10.1080/13548500500465878]
19. Ackroyd K, FortuneDG, Price S, Howell S, Sharrack B, Isaac CL. Adversarial growth in patients with multiple sclerosis and their partners: Relationships with illness perceptions, disability and distress. Journal of Clinical Psychology in Medical Settings. 2011; 18(4):372-9. [DOI:10.1007/s10880-011-9265-0] [PMID] [DOI:10.1007/s10880-011-9265-0]
20. Hart SL, Vella L, Mohr DC. Relationships among depressive symptoms, benefit-finding, optimism, and positive affect in multiple sclerosis patients after psychotherapy for depression. Health Psychology. 2008; 27(2):230-8. [DOI:10.1037/0278-6133.27.2.230] [PMID] [PMCID] [DOI:10.1037/0278-6133.27.2.230]
21. Hulley SB, Cummings SR, Browner WS, Grady D, Newman TB. Designing clinical research: An epidemiologic approach. Philadelphia: Lippincott Williams & Wilkins; 2013.
22. Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996; 9(3):455-71. [DOI:10.1002/jts.2490090305] [DOI:10.1002/jts.2490090305]
23. Heidarzadeh M, Naseri P, Shamshiri M, Dadkhah B, Rassouli M, Gholchin M. Evaluating the factor structure of the persian version of posttraumatic growth inventory in cancer patients. Asian Nursing Research. 2017; 11(3):180-6. [DOI:10.1016/j.anr.2017.07.003] [PMID] [DOI:10.1016/j.anr.2017.07.003]
24. Morris BA, Shakespeare Finch J, Scott JL. Posttraumatic growth after cancer: The importance of health-related benefits and newfound compassion for others. Supportive Care in Cancer. 2012; 20(4):749-56. [DOI:10.1007/s00520-011-1143-7] [PMID] [DOI:10.1007/s00520-011-1143-7]
25. Bellizzi KM, Smith AW, Reeve BB, Alfano CM, Bernstein L, Meeske K, et al. Posttraumatic growth and health-related quality of life in a racially diverse cohort of breast cancer survivors. Journal of Health Psychology. 2010; 15(4):615-26. [DOI:10.1177/1359105309356364] [PMID] [DOI:10.1177/1359105309356364]
26. Hooper LM, Marotta SA, Depuy V. A confirmatory factor analytic study of the posttraumatic growth inventory among a sample of racially diverse college students. Journal of Mental Health. 2009; 18(4):335-43. [DOI:10.1080/09638230802522502] [DOI:10.1080/09638230802522502]
27. Lee JA, Luxton DD, Reger GM, Gahm GA. Confirmatory factor analysis of the Posttraumatic Growth Inventory with a sample of soldiers previously deployed in support of the Iraq and Afghanistan wars. Journal of Clinical Psychology. 2010; 66(7):813-9. [DOI:10.1002/jclp.20692] [PMID] [DOI:10.1002/jclp.20692]
28. Heidarzadeh M, Rassouli M, Shahbolaghi FM, Majd HA, Karam AM, Mirzaee H, et al. Posttraumatic growth and its dimensions in patients with cancer. Middle East Journal of Cancer. 2014; 5(1):23-9.
29. Rahimi R, Heidarzadeh M, Shoaee R. The relationship between posttraumatic growth and social support in patients with myocardial infarction. Canadian Journal of Cardiovascular Nursing. 2016; 26 (2):19-24. [PMID] [PMID]
30. Heidarzadeh M, Hassani P, Ghahramanian A, Ilnaz Y. [Quality of life and social support in congestive heart failure patients and healthy people (Persian)]. Holistic Nursing and Midwifery Journal. 2013; 23(1):13-21.
31. Li YC, Yeh PC, Chen HW, Chang YF, Pi SH, Fang CK. Posttraumatic growth and demoralization after cancer: The effects of patients' meaning-making. Palliative and Supportive Care. 2015; 13(5): 1449-58. [DOI:10.1017/S1478951515000048] [PMID] [DOI:10.1017/S1478951515000048]
32. Li YC, Ho CH, Wang HH. Demoralization in cancer patients and related factors in Taiwan. Cancer Nursing. 2017; 40(1):E54-E60. [DOI:10.1097/NCC.0000000000000352] [PMID] [DOI:10.1097/NCC.0000000000000352]
33. Farsi Z, Dehghan Nayeri N, Negarandeh R. Coping strategies of adults with leukemia undergoing hematopoieticstem cell transplantation in Iran: A qualitative study. Nursing & Health Sciences. 2010; 12(4):485-92. [DOI:10.1111/j.1442-2018.2010.00563.x] [PMID] [DOI:10.1111/j.1442-2018.2010.00563.x]
34. Heidarzadeh M, Rassouli M, Ghanavati A, Mirzaei H, Tahmasebi M. Spiritual growth in cancer patients: A qualitative study. Bulletin of Environment, Pharmacology and Life Sciences. 2014; 3(9):92-7.
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |