Thu, Apr 25, 2024
Volume 30, Issue 1 (1-2020)
JHNM 2020, 30(1): 9-16 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rostamkhan S, Mokhtari Lakeh N, Asiri S, Kazemnezhad Leili E. Breastfeeding Status up to 2-Year-Olds and Its’ Associated Factors Based on Behaviors, Attitudes, Subjective Norms, and Enabling Factors(BASNEF) Model. JHNM 2020; 30 (1) :9-16
URL: http://hnmj.gums.ac.ir/article-1-810-en.html
URL: http://hnmj.gums.ac.ir/article-1-810-en.html
1- Nursing (MSN), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- PhD. Candidate in Educational Administration, Social Determinants of Health Research Center (SDHRC), Instructor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. , lakenasrin@gmail.com
3- PhD. Candidate in Gerontology, Social Determinants of Health Research Center (SDHRC), Instructor,Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Social Determinants of Health Research Center (SDHRC), Biostatistics, Guilan University of Medical Sciences, Rasht, Iran.
2- PhD. Candidate in Educational Administration, Social Determinants of Health Research Center (SDHRC), Instructor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. , lakenasrin@gmail.com
3- PhD. Candidate in Gerontology, Social Determinants of Health Research Center (SDHRC), Instructor,Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Social Determinants of Health Research Center (SDHRC), Biostatistics, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 487 kb]
(728 Downloads)
| Abstract (HTML) (2926 Views)
Full-Text: (894 Views)
Introduction
Breast milk is the primary food for children under 2 years of age. Furthermore, nutrition is a major factor in the biopsychological development of infants [1, 2]. The World Health Organization (WHO), therefore, recommends exclusive breastfeeding guidelines for at least 6 months and its continuation along with supplemental feeding for up to 2 years to provide optimal growth for all infants [3, 4]. Breast milk can protect infants against diseases, such as respiratory tract infections, urinary tract infections, bacterial infection, allergies, gastrointestinal diseases, eczema, middle ear infections, and malnutrition [5]. According to the United Nations Children’s Fund (UNICEF), 52% of infants are breastfed and supplemented by the age of 6-9 months. Moreover, 46% of the world’s children between the ages of 20 and 23 are still breastfed, with the highest rate (69%) reported in South Asia and the lowest rate (24%) in the Middle East and North Africa. Although the breastfeeding rate has improved in some countries over the past 10 years, it is still well below the recommended level [6].
A study in Iran revealed that 90% of infants were breastfed during the first year and 57% during the first two years [7]. Another study in 2012 in one of the northern cities of Iran reported a 21.3% incidence of exclusive breastfeeding [8]. This rate in some other cities of Iran has been reported up to 79% [9]. According to Olang et al. only 56% and 25% of Iranian children aged ≤4 and ≤6 months had exclusive breastfeeding, respectively [10].
Various studies have reported several factors affecting exclusive breastfeeding and breastfeeding duration. Such factors include race, age, occupation and maternal literacy level, socioeconomic factors, inadequate breast milk, childhood obesity, maternal obesity, smoking, multiple pregnancy, delivery type, pregnancy type, number of breastfeeding times and the mother’s willingness to breastfeed, birth weight, number of children, nurses’ performance, the tips that mothers receive from friends and healthcare workers, social support, and breastfeeding adequacy [11-13].
Inadequate milk production is among the significant causes of non-continuation of breastfeeding in the first 6 months; it has a greater frequency in the first 4 months of life [14]. To succeed in changing health behaviors, health educators must be aware of the factors influencing the formation of behavior and that theory can facilitate this process. Hubly introduced the Behaviors, Attitudes, Subjective Norms, Enabling Factors (BASNEF) model to understand behavioral changes in health communication. According to this model, individuals commit a new behavior when they believe that the behavior has health, financial, and other benefits (evaluation of the consequences of the behavior). Then, this assessment shapes their attitude toward that behavior. Accordingly, significant others can influence one’s decision to have new behaviors and act as a barrier or facilitator of the behavior (subjective norm).
An individual’s subjective norms are also determined by normative beliefs, i.e. the extent to which the new behavior is accepted or rejected by significant others. The combination of attitudes towards behavior and subjective norms can shape a person’s decision to adopt a new behavior (behavioral intention). However, factors like skill, money, cost, etc. can be effective in transforming behavioral intention into effective behavior. These factors must be present so that the behavior can occur [15]. Breastfeeding behavior is no exception. Any attempt and planning without investigating the causes of breastfeeding and understanding different breastfeeding behaviors are impractical. Cross-sectional and retrospective studies, the lack of evaluating rural population’s attitudes towards urban population, low sample size, disregarding the examination of premature and ill infants, accessibility to mothers only by phone calls and invitations, and the non-exploration of enabling factors and subjective norms are among the limitations of similar studies.
With the expansion of the health network, valuable measures have been taken in Iran to promote breastfeeding; however, breastfeeding inhibitors are rooted in the bio-socio-cultural issues of society, more efforts are required to determine these factors and to increase the mothers’ awareness of the benefits and techniques of breastfeeding in different parts of the country. Thus, this study aimed to investigate the breastfeeding status of ≤2-year-olds in Iran and its associated factors based on the BASNEF model.
Materials and Methods
This analytical and cross-sectional study was conducted in 2016. The study population consisted of mothers with babies aged 6-24 months referring to the comprehensive health centers in Rasht City, Iran (N=1725). The sample size was determined as 180, according to Charkazi et al. study on breastfeeding prevalence (86.4%) and considering a 5% error, and 95% confidence interval [16]. Additionally, 18 other variables were studied in addition to breastfeeding; thus, 270 samples were determined considering 5 samples per variable.
The inclusion criteria had active health records and willingness to participate in the study. First, mothers were given the necessary explanations about the study purposes by phone and were invited to participate in the study. If accepted, the date and time of the interview were determined. Then, written informed consent was obtained from them. For illiterate or less educated mothers, verbal consent was obtained after providing verbal explanations. In total, 1006 samples were excluded due to inactivity, and 449 mothers had no willingness to participate in the study. Sampling was performed using a two-stage cluster random sampling technique. Consequently, the number of clusters (health centers) was initially determined. In this regard, 16 out of 38 centers were selected from the north, west, east, and west of Rasht City. The health center No.9, where the validity and reliability of the used questionnaire were tested, was excluded from the study. Then, from each center, eligible samples were selected during working hours from 8 AM to 2 PM among those referring to the centers.
For collecting the required data, a 6-part questionnaire adapted from the studies of Charkazi et al. [16] and Sharifirad et al. [17] was used. The first part (12 items) surveys the demographic characteristics of study samples. The second part (4 items) measures breastfeeding behaviors. Next part (18 items) assesses the breastfeeding knowledge of mothers rated on three scales (1=Yes, 0=No, 0=No idea); based on the obtained scores, mothers’ knowledge is categorized into three levels of good (score >14 or >75%), moderate (score 8-14 or 50%-75%), and poor (score <8 or <50%) [16]. Part 4 (19 items) measures the attitude of mothers towards breastfeeding on a 5-point Likert-type scale ranging from definitely disagree to agree (0-4). Reverse expressions were given reverse scoring. The total achievable score ranges from 0 to 36. Scores <18 indicate undesirable attitudes and scores ≥18 demonstrate a desirable attitude. Part 5 (5 items) evaluates enabling factors answered by yes/no. The correct and incorrect answers are dedicated one and zero points, respectively. The final part surveys subjective norms (trustworthy people who influence mothers’ decisions about breastfeeding behavior) with one question answered on a 5-point scale. The mothers are requested to prioritize among those who are effective in their breastfeeding behavior [16].
To evaluate the validity of the questionnaire, it was provided to 10 members of the nursing faculty. The quantitative validity of the instrument was confirmed by Content Validity Ratio (CVR) and Content Validity Index (CVI) determination. The test-retest reliability of the tool was twice measured for 1 week via a pilot study on 15 samples. Responses were similar in ˃95% of the samples in the two phases. The reliability of the two constructs of enabling factors and subjective norms using the Kappa test was confirmed with the kappa coefficient of 0.8.
After approval by the Deputy for Research and obtaining ethical approval (no. 922360), the researcher visited the centers and collected data by the questionnaire. The collected data were analyzed in SPSS. For data analysis, we applied descriptive statistics and the Chi-squared test, Fisher’s Exact test, and multivariate logistic regression analysis (backward elimination method).
Breast milk is the primary food for children under 2 years of age. Furthermore, nutrition is a major factor in the biopsychological development of infants [1, 2]. The World Health Organization (WHO), therefore, recommends exclusive breastfeeding guidelines for at least 6 months and its continuation along with supplemental feeding for up to 2 years to provide optimal growth for all infants [3, 4]. Breast milk can protect infants against diseases, such as respiratory tract infections, urinary tract infections, bacterial infection, allergies, gastrointestinal diseases, eczema, middle ear infections, and malnutrition [5]. According to the United Nations Children’s Fund (UNICEF), 52% of infants are breastfed and supplemented by the age of 6-9 months. Moreover, 46% of the world’s children between the ages of 20 and 23 are still breastfed, with the highest rate (69%) reported in South Asia and the lowest rate (24%) in the Middle East and North Africa. Although the breastfeeding rate has improved in some countries over the past 10 years, it is still well below the recommended level [6].
A study in Iran revealed that 90% of infants were breastfed during the first year and 57% during the first two years [7]. Another study in 2012 in one of the northern cities of Iran reported a 21.3% incidence of exclusive breastfeeding [8]. This rate in some other cities of Iran has been reported up to 79% [9]. According to Olang et al. only 56% and 25% of Iranian children aged ≤4 and ≤6 months had exclusive breastfeeding, respectively [10].
Various studies have reported several factors affecting exclusive breastfeeding and breastfeeding duration. Such factors include race, age, occupation and maternal literacy level, socioeconomic factors, inadequate breast milk, childhood obesity, maternal obesity, smoking, multiple pregnancy, delivery type, pregnancy type, number of breastfeeding times and the mother’s willingness to breastfeed, birth weight, number of children, nurses’ performance, the tips that mothers receive from friends and healthcare workers, social support, and breastfeeding adequacy [11-13].
Inadequate milk production is among the significant causes of non-continuation of breastfeeding in the first 6 months; it has a greater frequency in the first 4 months of life [14]. To succeed in changing health behaviors, health educators must be aware of the factors influencing the formation of behavior and that theory can facilitate this process. Hubly introduced the Behaviors, Attitudes, Subjective Norms, Enabling Factors (BASNEF) model to understand behavioral changes in health communication. According to this model, individuals commit a new behavior when they believe that the behavior has health, financial, and other benefits (evaluation of the consequences of the behavior). Then, this assessment shapes their attitude toward that behavior. Accordingly, significant others can influence one’s decision to have new behaviors and act as a barrier or facilitator of the behavior (subjective norm).
An individual’s subjective norms are also determined by normative beliefs, i.e. the extent to which the new behavior is accepted or rejected by significant others. The combination of attitudes towards behavior and subjective norms can shape a person’s decision to adopt a new behavior (behavioral intention). However, factors like skill, money, cost, etc. can be effective in transforming behavioral intention into effective behavior. These factors must be present so that the behavior can occur [15]. Breastfeeding behavior is no exception. Any attempt and planning without investigating the causes of breastfeeding and understanding different breastfeeding behaviors are impractical. Cross-sectional and retrospective studies, the lack of evaluating rural population’s attitudes towards urban population, low sample size, disregarding the examination of premature and ill infants, accessibility to mothers only by phone calls and invitations, and the non-exploration of enabling factors and subjective norms are among the limitations of similar studies.
With the expansion of the health network, valuable measures have been taken in Iran to promote breastfeeding; however, breastfeeding inhibitors are rooted in the bio-socio-cultural issues of society, more efforts are required to determine these factors and to increase the mothers’ awareness of the benefits and techniques of breastfeeding in different parts of the country. Thus, this study aimed to investigate the breastfeeding status of ≤2-year-olds in Iran and its associated factors based on the BASNEF model.
Materials and Methods
This analytical and cross-sectional study was conducted in 2016. The study population consisted of mothers with babies aged 6-24 months referring to the comprehensive health centers in Rasht City, Iran (N=1725). The sample size was determined as 180, according to Charkazi et al. study on breastfeeding prevalence (86.4%) and considering a 5% error, and 95% confidence interval [16]. Additionally, 18 other variables were studied in addition to breastfeeding; thus, 270 samples were determined considering 5 samples per variable.
The inclusion criteria had active health records and willingness to participate in the study. First, mothers were given the necessary explanations about the study purposes by phone and were invited to participate in the study. If accepted, the date and time of the interview were determined. Then, written informed consent was obtained from them. For illiterate or less educated mothers, verbal consent was obtained after providing verbal explanations. In total, 1006 samples were excluded due to inactivity, and 449 mothers had no willingness to participate in the study. Sampling was performed using a two-stage cluster random sampling technique. Consequently, the number of clusters (health centers) was initially determined. In this regard, 16 out of 38 centers were selected from the north, west, east, and west of Rasht City. The health center No.9, where the validity and reliability of the used questionnaire were tested, was excluded from the study. Then, from each center, eligible samples were selected during working hours from 8 AM to 2 PM among those referring to the centers.
For collecting the required data, a 6-part questionnaire adapted from the studies of Charkazi et al. [16] and Sharifirad et al. [17] was used. The first part (12 items) surveys the demographic characteristics of study samples. The second part (4 items) measures breastfeeding behaviors. Next part (18 items) assesses the breastfeeding knowledge of mothers rated on three scales (1=Yes, 0=No, 0=No idea); based on the obtained scores, mothers’ knowledge is categorized into three levels of good (score >14 or >75%), moderate (score 8-14 or 50%-75%), and poor (score <8 or <50%) [16]. Part 4 (19 items) measures the attitude of mothers towards breastfeeding on a 5-point Likert-type scale ranging from definitely disagree to agree (0-4). Reverse expressions were given reverse scoring. The total achievable score ranges from 0 to 36. Scores <18 indicate undesirable attitudes and scores ≥18 demonstrate a desirable attitude. Part 5 (5 items) evaluates enabling factors answered by yes/no. The correct and incorrect answers are dedicated one and zero points, respectively. The final part surveys subjective norms (trustworthy people who influence mothers’ decisions about breastfeeding behavior) with one question answered on a 5-point scale. The mothers are requested to prioritize among those who are effective in their breastfeeding behavior [16].
To evaluate the validity of the questionnaire, it was provided to 10 members of the nursing faculty. The quantitative validity of the instrument was confirmed by Content Validity Ratio (CVR) and Content Validity Index (CVI) determination. The test-retest reliability of the tool was twice measured for 1 week via a pilot study on 15 samples. Responses were similar in ˃95% of the samples in the two phases. The reliability of the two constructs of enabling factors and subjective norms using the Kappa test was confirmed with the kappa coefficient of 0.8.
After approval by the Deputy for Research and obtaining ethical approval (no. 922360), the researcher visited the centers and collected data by the questionnaire. The collected data were analyzed in SPSS. For data analysis, we applied descriptive statistics and the Chi-squared test, Fisher’s Exact test, and multivariate logistic regression analysis (backward elimination method).
Results
Most study participants aged 27-30 years (mean age: 29.93±5.53 years); 53% of mothers’ babies aged 6-12 months, 28.5% aged 13-18 months, and 18.15% aged 19-24 months. Most mothers (91.1%) were covered by insurance, and 29.3% had been referred to the health centers for prenatal care; 77.4% of mothers had cesarean section; most of the infants (58.1%) were first children of the families, and had no underlying disease (88.5%). Most families (47.8%) had a monthly income of 150-300 $. Among infants with discontinued breastfeeding, 18.9% lacked breast milk consumption; in 6.3% of mothers, physician recommendation was the most common reason to discontinue breastfeeding. The prevalence of breastfeeding was 56.3%, formula feeding 19.6%, combined breastfeeding, and formula feeding 23%, and for other kinds of milk, it was 1.1%. Furthermore, 61.5% of the study infants had exclusive breastfeeding.
Most study participants aged 27-30 years (mean age: 29.93±5.53 years); 53% of mothers’ babies aged 6-12 months, 28.5% aged 13-18 months, and 18.15% aged 19-24 months. Most mothers (91.1%) were covered by insurance, and 29.3% had been referred to the health centers for prenatal care; 77.4% of mothers had cesarean section; most of the infants (58.1%) were first children of the families, and had no underlying disease (88.5%). Most families (47.8%) had a monthly income of 150-300 $. Among infants with discontinued breastfeeding, 18.9% lacked breast milk consumption; in 6.3% of mothers, physician recommendation was the most common reason to discontinue breastfeeding. The prevalence of breastfeeding was 56.3%, formula feeding 19.6%, combined breastfeeding, and formula feeding 23%, and for other kinds of milk, it was 1.1%. Furthermore, 61.5% of the study infants had exclusive breastfeeding.
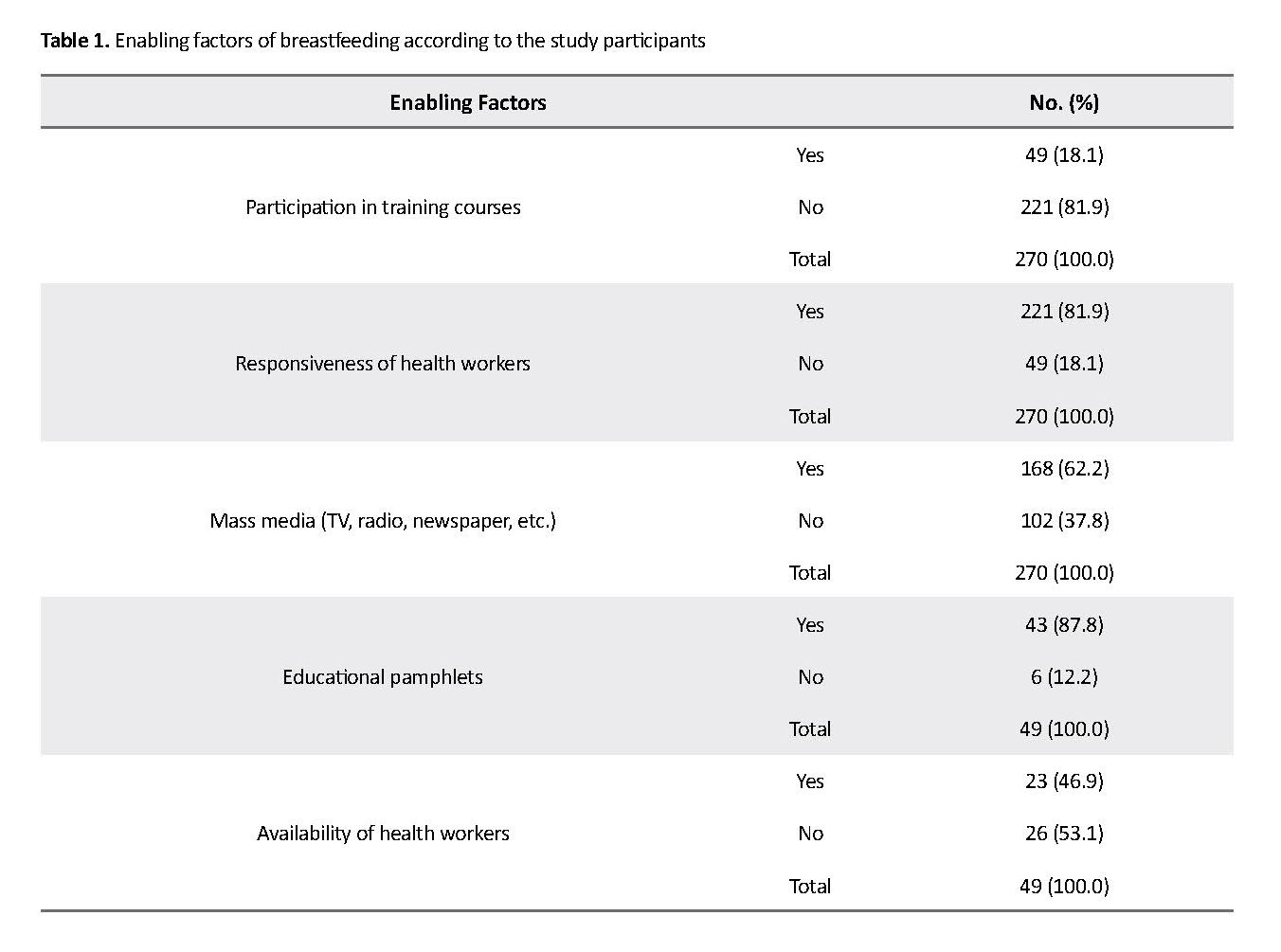
In terms of breastfeeding knowledge, 25.6%, 50%, and 24.4% were at good, moderate, and poor levels, respectively. Regarding attitude towards breastfeeding, 61.9% and 38.1% had undesirable and desirable attitudes, respectively. The majority of mothers (81.9%) had not participated in training courses on breastfeeding and its proper techniques; however, the responsiveness of health workers who were included in part 5 of the questionnaire (enabling factors) was equal to 81.9%. The enabling factors according to the study participants, are presented in Table 1.
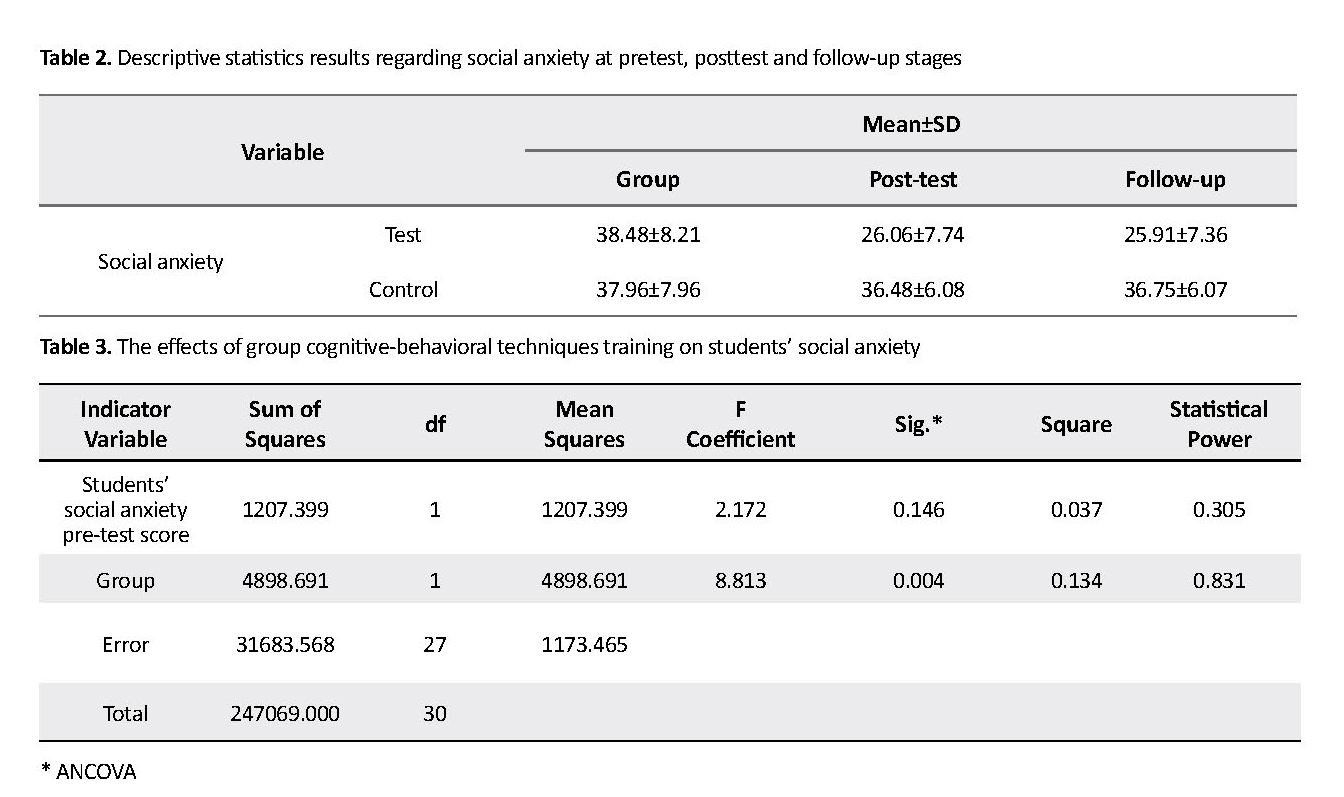
According to Fisher’s exact test results, breastfeeding status based on the infant’s age was significant (P=0.036); infants aged 19-24 months had more favorable breastfeeding status. There was no significant relationship between breastfeeding status and other individual and social variables. Breastfeeding status based on mothers’ attitudes was significant (P=0.029). In other words, the mothers with a desirable attitude had favorable breastfeeding; however, breastfeeding status was not significant based on mothers’ knowledge. There was no statistically significant relationship between breastfeeding status and subjective norms. Breastfeeding status based on subjective norms is presented in Table 2. The collected results also reported no significant association between breastfeeding status and enabling factors (Table 3).
For evaluating the predictor variables of breastfeeding, a multivariate logistic regression model with backward method was used. All variables with P<0.25 in the univariate analysis were included in the initial logistic model. Regression model indicated that the variables of infant’s age (OR=1.582, 95% CI=1.133- 2.207, P=0.007), family income (OR=0.65, 95% CI=0.489-0.865, P=0.003), and breastfeeding knowledge (OR=1.3, 95% CI=1.101-1.428, P=0.001) contributed to breastfeeding status (Table 4).
According to Fisher’s exact test results, breastfeeding status based on the infant’s age was significant (P=0.036); infants aged 19-24 months had more favorable breastfeeding status. There was no significant relationship between breastfeeding status and other individual and social variables. Breastfeeding status based on mothers’ attitudes was significant (P=0.029). In other words, the mothers with a desirable attitude had favorable breastfeeding; however, breastfeeding status was not significant based on mothers’ knowledge. There was no statistically significant relationship between breastfeeding status and subjective norms. Breastfeeding status based on subjective norms is presented in Table 2. The collected results also reported no significant association between breastfeeding status and enabling factors (Table 3).
For evaluating the predictor variables of breastfeeding, a multivariate logistic regression model with backward method was used. All variables with P<0.25 in the univariate analysis were included in the initial logistic model. Regression model indicated that the variables of infant’s age (OR=1.582, 95% CI=1.133- 2.207, P=0.007), family income (OR=0.65, 95% CI=0.489-0.865, P=0.003), and breastfeeding knowledge (OR=1.3, 95% CI=1.101-1.428, P=0.001) contributed to breastfeeding status (Table 4).
Discussion
Among the studied variables, infant age, family income, and mothers’ knowledge were the predictors of breastfeeding status. Increasing mothers’ knowledge of breastfeeding by considering the role of husband, health workers, and grandmothers can help in choosing breast milk to feed ≤2-year-olds. Latifi et al. [13] investigated the breastfeeding status of mothers with infants aged 8-24 months in northern Iran and its related factors using the BASNEF model. They reported the common reasons for discontinuation of breastfeeding as follows: the lack of breastmilk, crying and restlessness of the baby, child’s illness, mother’s illness, difficulty of breastfeeding, mother’s occupation, and doctor’s advice. In our study, mothers’ knowledge of breastfeeding was at a moderate level, which is consistent with the results of Mary [18]. However, Vaaler et al. [19] explored breastfeeding attitudes and behavior among mothers living in Texas. They concluded that most of the subjects had positive and favorable attitudes toward breast milk and infant formula. Such discrepancy can be due to different cultural backgrounds, the interval between their study and the present study, and the use of different research tools.
Masoumi et al. [20] studied the effect of exclusive breastfeeding counseling on the knowledge and attitude of mothers with preterm infants. Accordingly, they found a significant relationship between breastfeeding and mothers’ knowledge and attitude. Kornides and Kitsantas [21] reported that interventions to increase mothers’ knowledge and support from family and health care staff are effective in breastfeeding behavior. Rahimi et al. [22] investigated pregnant women’s beliefs about exclusive breastfeeding by the end of 6 months. The revealed that emotional communication with the infant was the most essential positive behavioral belief, while breast deformity and fatigue were negative behavioral beliefs in pregnant mothers about exclusive breastfeeding. These findings suggest that promoting positive beliefs and correcting false beliefs, increasing mothers’ knowledge and attitudes towards the benefits of breastfeeding, as well as teaching proper breastfeeding methods during pregnancy and after childbirth can significantly improve breastfeeding continuation.
Regarding enabling factors, the responsiveness of health workers and mass media have been higher considered in our study. Bai et al. [23] reported perceived social support from family, friends, and health workers during exclusive breastfeeding as the most crucial subjective norm. Rempel and Rempel indicated the unique role of fathers in understanding, encouraging, and valuing the breastfeeding mothers, and sharing housework and child care, in this regard [24].
According to Jiang et al. direct support and training by professional caregivers can have a very positive effect on increasing the breastfeeding period [25]. Negin et al. in a systemic review, reported that grandmothers have a significant impact on important health behaviors, including exclusive breastfeeding [26]. Programs aiming to promote exclusive breastfeeding should incorporate grandmothers in their interventions to maximize the effect. People close to the mother appear to have a significant influence on her breastfeeding behavior. Better attitudes to breastfeeding are provided when caregivers are the relatives of mothers; therefore, the husband, the mother-in-law and those who have close relations with the mother should be included in the educational and counseling programs.
In this study, the optimal breastfeeding prevalence based on infant age and pregnancy care location was significant. Mothers who received pregnancy care only in the health center had a higher percentage of favorable breastfeeding behavior. However, this finding was not statistically significant based on other variables. Mothers who reported a desirable attitude indicated favorable breastfeeding behavior. Among the studied variables, infant age, family income, and mother’s knowledge were the predictors of breastfeeding status; with their increase, the odds of optimal breastfeeding increases. Veghari and Rahmati found that exclusive breastfeeding significantly enhances with increased mother’s educational level [27].
Breastfeeding duration had a significant positive relationship with household size, birth order, maternal age, and infant nutrition status; however, literate mothers had a shorter duration of breastfeeding. In the study of Jafari Asl et al. a significant relationship between breastfeeding duration and the mother’s attitude towards breastfeeding was reported [5]. Mogre and Dery suggested that, in addition to knowledge, infant’s age and mothers’ education were the determinants of exclusive breastfeeding practice [28]. According to Titaley et al. delayed initiation and non-exclusive breastfeeding were higher in wealthy families [29]. Ranjabaran et al. also argued that breast milk feeding was lower in high-income families [9].
The obtained results highlighted that, in addition to the mothers’ knowledge, support, and encouragement from husband, mother, and mother-in-law had positive effects on mothers’ breastfeeding behavior, as subjective norms. More attention should be paid to these factors in breastfeeding programs. Given that the survey instrument in this study was a questionnaire, limitations, like failure to accurately reflect maternal behavior, may have affected the achieved outcomes. Considering the relationship between breastfeeding knowledge and breastfeeding status, we suggest that interventional studies be conducted to find the most robust methods to raise awareness in the mothers of children under 2 years of age.
Conclusion
Raising the mothers’ knowledge of breastfeeding by considering the role of husbands, health workers, and grandmothers could help in choosing breast milk for feeding infants aged ≤2 years.
Ethical Considerations
Compliance with ethical guidelines
The Social Determinants of Health Research Center (SDHRC) of Guilan University of Medical Sciences
Funding
This research was supported by the Vice-Chancellor of Research and Technology of Guilan University of Medical Sciences (Grant No. 922360).
Authors contributions
The study plan: Somayeh Rostamkhan and Nasrin Mokhtari Lakeh; Manuscript drafting: Shahla Asiri; The essential revision: Ehsan Kazemnezhad Leili.
Conflict of interest
The authors declared noconflicts of interest.
Acknowledgements
The authors would like to thank the staff of health centers in Rasht and all the mothers who participated in this study for their valuable cooperation.
References
Yaghini SO, Khameh S, Danesh F, Modaresi MR, Saneian H. [Determinants of exclusive breast milk feeding of infants in Isfahan, Iran (Persian)]. Journal of Isfahan Medical School. 2011; 28(117):1126-39.
World Health Organization. Breastfeeding [Internet]. 2018 [Updated 2018 December 31]. Available from: https://www.who.int/nutrition/topics/exclusive_breastfeeding/en/
World Health Organization. Exclusive breastfeeding-worledheslth organization [Internet]. 2014. Available from: www.who.int.nutrition.topics.exclusive-breastfeeding.en
Poorshaban F, Pakseresht S, Bostani Khalesi Z, Kazemnejad Leili E. Factors associated with breastfeeding self-efficacy of mothers within 6 weeks of delivery. Journal of Holistic Nursing and Midwifery. 2017; 27(1):27-34. [DOI:10.18869/acadpub.hnmj.27.1.27]
Jafari Asl M, Fadakar Sogheh R, Ghavi A, Ahmad Shearbafi M. [Related factors to continued breastfeeding in infants (Persian)]. Journal of Holistic Nursing and Midwifery. 2014; 24(2):1-8.
Masoudifard M, Daroogheh L, Yousefian A, Lame E. [Effective factors on using artificial milk in under-one children in Aran-Bidgol (Persian)]. Journal of Qazvin University of Medical Sciences. 2012; 16(3):78-84.
Bastani F. [The importance of breast feeding (component of success in breast feeding) (Persian)]. 1st ed. Tehran: Mahtab; 2009.
Ziaie T, Ghanbari A, Hassanzadeh Rad A, Yazdani MA. [Investigating risk factors of failure in exclusive breastfeeding in less than one-year-old children referred to health centers in Rasht City (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2012; 15(18):32-9.
Ranjbaran M, Jafari Manesh H, Panahi M, Baderan M, Shamsi M, Nakhaei M, et al. [The survey of exclusive breast feeding and some socio-economical determinants in Shazand-Arak in 2014 (Persian)]. Journal of Community Health. 2014; 8(2):10-8.
Olang B, Farivar K, Heidarzadeh A, Strandvik B, Yngve A. Breastfeeding in Iran: Prevalence, duration and current recommendations. International Breastfeeding Journal. 2009; 4:8. [DOI:10.1186/1746-4358-4-8] [PMID] [PMCID]
Walker A. Breast milk as the gold standard for protective nutrients. The Journal of Pediatrics. 2010; 156(2 Suppl):S3-S7. [DOI:10.1016/j.jpeds.2009.11.021] [PMID]
Spiby H, McCormick F, Wallace L, Renfrew MJ, D’Souza L, Dyson L. A systematic review of education and evidence-based practice interventions with health professionals and breast feeding counsellors on duration of breast feeding. Midwifery. 2009; 25(1):50-61. [DOI:10.1016/j.midw.2007.01.006] [PMID]
Latifi M, Saggar R, Seyyedghasemi NS, Moghaddam Z, Soleymaninejad M, Ghaedi M, et al. [Investigating of breast feeding situation in mothers who have 8-24 months infant and its related factors based on BNAASNEF model constructs in Aq qala City (Persian)]. Journal of Prevention and Health. 2016; 1(1):64-73.
Mannel R, Martens PJ, Walker M, editors. Core curriculum for lactation consultant practice. 3rd ed. Burlington, MA: Jones & Bartlett Publishers; 2012.
Saffari M, Shojaeizadeh D, Ghofranipour F, Heydarnia AR, Pakpoor Hajiagha A. [Theories, models and education methods of health promotion and health (Persian)]. Tehran: Assare Sobhan; 2010.
Charkazi A, Miraeiz SZ, Razzaghnejad A, Shahnazi H, Hasanzadeh A, Badleh MT. Breastfeeding status during the first two years of infants’ life and its risk factors based on BASNEF model structures in Isfahan. Journal of Education and Health Promotion. 2013; 2:9. [DOI:10.4103/2277-9531.107938] [PMID] [PMCID]
Sharifirad GR, Golshiri P, Shahnazi H, Barati M, Hasanzadeh A, Charkazi AR, et al. [The impact of educational program based on BASNEF model on breastfeeding behavior of pregnant mothers in Arak (Persian)]. Journal of Arak University of Medical Sciences. 2010; 13(1):63-70.
Jennifer Jothi Mary A. A study to assess the knowledge and attitude regarding to breast feeding among antenatal women attending antenatal OPD, in Christian Medical College, Vellore. Asian Journal of Nursing Education and Research. 2013; 3(3):188-9.
Vaaler ML, Stagg J, Parks SE, Erickson T, Castrucci BC. Breast-feeding attitudes and behavior among WIC mothers in Texas. Journal of Nutrition Education and Behavior. 2010; 42(3 Suppl):S30-S8. [DOI:10.1016/j.jneb.2010.02.001] [PMID]
Masoumi SZ, Ahmadi Sh, Parsa P, Roshanaei Gh, Basiri B. [Effects of counseling on adherence to exclusive breastfeeding in mothers of hospitalized late preterm infants in Fatemieh Hospital, Hamadan, Iran, 2014 (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2015; 23(3):72-81.
Kornides M, Kitsantas P. Evaluation of breastfeeding promotion, support, and knowledge of benefits on breastfeeding outcomes. Journal of Child Health Care. 2013; 17(3):264-73. [DOI:10.1177/1367493512461460] [PMID] [PMCID]
Rahimi T, Dehdari T, Shojaei S, Sadat Hashemi BS, Akbari Z, Daryafti H. [Beliefs of pregnant women in Qom City about exclusive breastfeeding until 6 months of age, Iran (Persian)]. Qom University of Medical Sciences Journal. 2016:10(2):60-9.
Bai Y, Middlestadt SE, Peng CY, Fly AD. Predictors of continuation of exclusive breastfeeding for the first six months of life. Journal of Human Lactation. 2010; 26(1):26-34. [DOI:10.1177/0890334409350168] [PMID]
Rempel LA, Rempel JK. The breastfeeding team: The role of involved fathers in the breastfeeding family. Journal of Human Lactation. 2011; 27(2):115-21. [DOI:10.1177/0890334410390045] [PMID]
Jiang H, Li M, Yang D, Wen LM, Hunter C, He G, et al. Awareness, intention, and needs regarding breastfeeding: Findings from first-time mothers in Shanghai, China. Breastfeeding Medicine. 2012; 7(6):526-34. [DOI:10.1089/bfm.2011.0124] [PMID] [PMCID]
Negin J, Coffman J, Vizintin P, Raynes-Greenow C. The influence of grandmothers on breastfeeding rates: A systematic review. Biomed Central Pregnancy and Childbirth. 2016; 16:91. [DOI:10.1186/s12884-016-0880-5] [PMID] [PMCID]
Veghari GR, Rahmati R. [Breastfeeding status and some of its related factors in the Golestan Province (Persian)]. Iran Journal of Nursing. 2011; 24(71):8-18.
Mogre V, Dery M, Gaa PK. Knowledge, attitudes and determinants of exclusive breastfeeding practice among Ghanaian rural lactating mothers. International Breastfeeding Journal. 2016; 11:12. [DOI:10.1186/s13006-016-0071-z] [PMID] [PMCID]
Titaley CR, Loh PC, Prasetyo S, Ariawan I, Shankar AH. Socio-economic factors and use of maternal health services are associated with delayed initiation and non-exclusive breastfeeding in Indonesia: Secondary analysis of Indonesia Demographic and Health Surveys 2002/2003 and 2007. Asia Pacific Journal of Clinical Nutrition. 2014; 23(1):91-104. [DOI:10.6133/apjcn.2014.23.1.18] [PMID]
Among the studied variables, infant age, family income, and mothers’ knowledge were the predictors of breastfeeding status. Increasing mothers’ knowledge of breastfeeding by considering the role of husband, health workers, and grandmothers can help in choosing breast milk to feed ≤2-year-olds. Latifi et al. [13] investigated the breastfeeding status of mothers with infants aged 8-24 months in northern Iran and its related factors using the BASNEF model. They reported the common reasons for discontinuation of breastfeeding as follows: the lack of breastmilk, crying and restlessness of the baby, child’s illness, mother’s illness, difficulty of breastfeeding, mother’s occupation, and doctor’s advice. In our study, mothers’ knowledge of breastfeeding was at a moderate level, which is consistent with the results of Mary [18]. However, Vaaler et al. [19] explored breastfeeding attitudes and behavior among mothers living in Texas. They concluded that most of the subjects had positive and favorable attitudes toward breast milk and infant formula. Such discrepancy can be due to different cultural backgrounds, the interval between their study and the present study, and the use of different research tools.
Masoumi et al. [20] studied the effect of exclusive breastfeeding counseling on the knowledge and attitude of mothers with preterm infants. Accordingly, they found a significant relationship between breastfeeding and mothers’ knowledge and attitude. Kornides and Kitsantas [21] reported that interventions to increase mothers’ knowledge and support from family and health care staff are effective in breastfeeding behavior. Rahimi et al. [22] investigated pregnant women’s beliefs about exclusive breastfeeding by the end of 6 months. The revealed that emotional communication with the infant was the most essential positive behavioral belief, while breast deformity and fatigue were negative behavioral beliefs in pregnant mothers about exclusive breastfeeding. These findings suggest that promoting positive beliefs and correcting false beliefs, increasing mothers’ knowledge and attitudes towards the benefits of breastfeeding, as well as teaching proper breastfeeding methods during pregnancy and after childbirth can significantly improve breastfeeding continuation.
Regarding enabling factors, the responsiveness of health workers and mass media have been higher considered in our study. Bai et al. [23] reported perceived social support from family, friends, and health workers during exclusive breastfeeding as the most crucial subjective norm. Rempel and Rempel indicated the unique role of fathers in understanding, encouraging, and valuing the breastfeeding mothers, and sharing housework and child care, in this regard [24].
According to Jiang et al. direct support and training by professional caregivers can have a very positive effect on increasing the breastfeeding period [25]. Negin et al. in a systemic review, reported that grandmothers have a significant impact on important health behaviors, including exclusive breastfeeding [26]. Programs aiming to promote exclusive breastfeeding should incorporate grandmothers in their interventions to maximize the effect. People close to the mother appear to have a significant influence on her breastfeeding behavior. Better attitudes to breastfeeding are provided when caregivers are the relatives of mothers; therefore, the husband, the mother-in-law and those who have close relations with the mother should be included in the educational and counseling programs.
In this study, the optimal breastfeeding prevalence based on infant age and pregnancy care location was significant. Mothers who received pregnancy care only in the health center had a higher percentage of favorable breastfeeding behavior. However, this finding was not statistically significant based on other variables. Mothers who reported a desirable attitude indicated favorable breastfeeding behavior. Among the studied variables, infant age, family income, and mother’s knowledge were the predictors of breastfeeding status; with their increase, the odds of optimal breastfeeding increases. Veghari and Rahmati found that exclusive breastfeeding significantly enhances with increased mother’s educational level [27].
Breastfeeding duration had a significant positive relationship with household size, birth order, maternal age, and infant nutrition status; however, literate mothers had a shorter duration of breastfeeding. In the study of Jafari Asl et al. a significant relationship between breastfeeding duration and the mother’s attitude towards breastfeeding was reported [5]. Mogre and Dery suggested that, in addition to knowledge, infant’s age and mothers’ education were the determinants of exclusive breastfeeding practice [28]. According to Titaley et al. delayed initiation and non-exclusive breastfeeding were higher in wealthy families [29]. Ranjabaran et al. also argued that breast milk feeding was lower in high-income families [9].
The obtained results highlighted that, in addition to the mothers’ knowledge, support, and encouragement from husband, mother, and mother-in-law had positive effects on mothers’ breastfeeding behavior, as subjective norms. More attention should be paid to these factors in breastfeeding programs. Given that the survey instrument in this study was a questionnaire, limitations, like failure to accurately reflect maternal behavior, may have affected the achieved outcomes. Considering the relationship between breastfeeding knowledge and breastfeeding status, we suggest that interventional studies be conducted to find the most robust methods to raise awareness in the mothers of children under 2 years of age.
Conclusion
Raising the mothers’ knowledge of breastfeeding by considering the role of husbands, health workers, and grandmothers could help in choosing breast milk for feeding infants aged ≤2 years.
Ethical Considerations
Compliance with ethical guidelines
The Social Determinants of Health Research Center (SDHRC) of Guilan University of Medical Sciences
Funding
This research was supported by the Vice-Chancellor of Research and Technology of Guilan University of Medical Sciences (Grant No. 922360).
Authors contributions
The study plan: Somayeh Rostamkhan and Nasrin Mokhtari Lakeh; Manuscript drafting: Shahla Asiri; The essential revision: Ehsan Kazemnezhad Leili.
Conflict of interest
The authors declared noconflicts of interest.
Acknowledgements
The authors would like to thank the staff of health centers in Rasht and all the mothers who participated in this study for their valuable cooperation.
References
Yaghini SO, Khameh S, Danesh F, Modaresi MR, Saneian H. [Determinants of exclusive breast milk feeding of infants in Isfahan, Iran (Persian)]. Journal of Isfahan Medical School. 2011; 28(117):1126-39.
World Health Organization. Breastfeeding [Internet]. 2018 [Updated 2018 December 31]. Available from: https://www.who.int/nutrition/topics/exclusive_breastfeeding/en/
World Health Organization. Exclusive breastfeeding-worledheslth organization [Internet]. 2014. Available from: www.who.int.nutrition.topics.exclusive-breastfeeding.en
Poorshaban F, Pakseresht S, Bostani Khalesi Z, Kazemnejad Leili E. Factors associated with breastfeeding self-efficacy of mothers within 6 weeks of delivery. Journal of Holistic Nursing and Midwifery. 2017; 27(1):27-34. [DOI:10.18869/acadpub.hnmj.27.1.27]
Jafari Asl M, Fadakar Sogheh R, Ghavi A, Ahmad Shearbafi M. [Related factors to continued breastfeeding in infants (Persian)]. Journal of Holistic Nursing and Midwifery. 2014; 24(2):1-8.
Masoudifard M, Daroogheh L, Yousefian A, Lame E. [Effective factors on using artificial milk in under-one children in Aran-Bidgol (Persian)]. Journal of Qazvin University of Medical Sciences. 2012; 16(3):78-84.
Bastani F. [The importance of breast feeding (component of success in breast feeding) (Persian)]. 1st ed. Tehran: Mahtab; 2009.
Ziaie T, Ghanbari A, Hassanzadeh Rad A, Yazdani MA. [Investigating risk factors of failure in exclusive breastfeeding in less than one-year-old children referred to health centers in Rasht City (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2012; 15(18):32-9.
Ranjbaran M, Jafari Manesh H, Panahi M, Baderan M, Shamsi M, Nakhaei M, et al. [The survey of exclusive breast feeding and some socio-economical determinants in Shazand-Arak in 2014 (Persian)]. Journal of Community Health. 2014; 8(2):10-8.
Olang B, Farivar K, Heidarzadeh A, Strandvik B, Yngve A. Breastfeeding in Iran: Prevalence, duration and current recommendations. International Breastfeeding Journal. 2009; 4:8. [DOI:10.1186/1746-4358-4-8] [PMID] [PMCID]
Walker A. Breast milk as the gold standard for protective nutrients. The Journal of Pediatrics. 2010; 156(2 Suppl):S3-S7. [DOI:10.1016/j.jpeds.2009.11.021] [PMID]
Spiby H, McCormick F, Wallace L, Renfrew MJ, D’Souza L, Dyson L. A systematic review of education and evidence-based practice interventions with health professionals and breast feeding counsellors on duration of breast feeding. Midwifery. 2009; 25(1):50-61. [DOI:10.1016/j.midw.2007.01.006] [PMID]
Latifi M, Saggar R, Seyyedghasemi NS, Moghaddam Z, Soleymaninejad M, Ghaedi M, et al. [Investigating of breast feeding situation in mothers who have 8-24 months infant and its related factors based on BNAASNEF model constructs in Aq qala City (Persian)]. Journal of Prevention and Health. 2016; 1(1):64-73.
Mannel R, Martens PJ, Walker M, editors. Core curriculum for lactation consultant practice. 3rd ed. Burlington, MA: Jones & Bartlett Publishers; 2012.
Saffari M, Shojaeizadeh D, Ghofranipour F, Heydarnia AR, Pakpoor Hajiagha A. [Theories, models and education methods of health promotion and health (Persian)]. Tehran: Assare Sobhan; 2010.
Charkazi A, Miraeiz SZ, Razzaghnejad A, Shahnazi H, Hasanzadeh A, Badleh MT. Breastfeeding status during the first two years of infants’ life and its risk factors based on BASNEF model structures in Isfahan. Journal of Education and Health Promotion. 2013; 2:9. [DOI:10.4103/2277-9531.107938] [PMID] [PMCID]
Sharifirad GR, Golshiri P, Shahnazi H, Barati M, Hasanzadeh A, Charkazi AR, et al. [The impact of educational program based on BASNEF model on breastfeeding behavior of pregnant mothers in Arak (Persian)]. Journal of Arak University of Medical Sciences. 2010; 13(1):63-70.
Jennifer Jothi Mary A. A study to assess the knowledge and attitude regarding to breast feeding among antenatal women attending antenatal OPD, in Christian Medical College, Vellore. Asian Journal of Nursing Education and Research. 2013; 3(3):188-9.
Vaaler ML, Stagg J, Parks SE, Erickson T, Castrucci BC. Breast-feeding attitudes and behavior among WIC mothers in Texas. Journal of Nutrition Education and Behavior. 2010; 42(3 Suppl):S30-S8. [DOI:10.1016/j.jneb.2010.02.001] [PMID]
Masoumi SZ, Ahmadi Sh, Parsa P, Roshanaei Gh, Basiri B. [Effects of counseling on adherence to exclusive breastfeeding in mothers of hospitalized late preterm infants in Fatemieh Hospital, Hamadan, Iran, 2014 (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2015; 23(3):72-81.
Kornides M, Kitsantas P. Evaluation of breastfeeding promotion, support, and knowledge of benefits on breastfeeding outcomes. Journal of Child Health Care. 2013; 17(3):264-73. [DOI:10.1177/1367493512461460] [PMID] [PMCID]
Rahimi T, Dehdari T, Shojaei S, Sadat Hashemi BS, Akbari Z, Daryafti H. [Beliefs of pregnant women in Qom City about exclusive breastfeeding until 6 months of age, Iran (Persian)]. Qom University of Medical Sciences Journal. 2016:10(2):60-9.
Bai Y, Middlestadt SE, Peng CY, Fly AD. Predictors of continuation of exclusive breastfeeding for the first six months of life. Journal of Human Lactation. 2010; 26(1):26-34. [DOI:10.1177/0890334409350168] [PMID]
Rempel LA, Rempel JK. The breastfeeding team: The role of involved fathers in the breastfeeding family. Journal of Human Lactation. 2011; 27(2):115-21. [DOI:10.1177/0890334410390045] [PMID]
Jiang H, Li M, Yang D, Wen LM, Hunter C, He G, et al. Awareness, intention, and needs regarding breastfeeding: Findings from first-time mothers in Shanghai, China. Breastfeeding Medicine. 2012; 7(6):526-34. [DOI:10.1089/bfm.2011.0124] [PMID] [PMCID]
Negin J, Coffman J, Vizintin P, Raynes-Greenow C. The influence of grandmothers on breastfeeding rates: A systematic review. Biomed Central Pregnancy and Childbirth. 2016; 16:91. [DOI:10.1186/s12884-016-0880-5] [PMID] [PMCID]
Veghari GR, Rahmati R. [Breastfeeding status and some of its related factors in the Golestan Province (Persian)]. Iran Journal of Nursing. 2011; 24(71):8-18.
Mogre V, Dery M, Gaa PK. Knowledge, attitudes and determinants of exclusive breastfeeding practice among Ghanaian rural lactating mothers. International Breastfeeding Journal. 2016; 11:12. [DOI:10.1186/s13006-016-0071-z] [PMID] [PMCID]
Titaley CR, Loh PC, Prasetyo S, Ariawan I, Shankar AH. Socio-economic factors and use of maternal health services are associated with delayed initiation and non-exclusive breastfeeding in Indonesia: Secondary analysis of Indonesia Demographic and Health Surveys 2002/2003 and 2007. Asia Pacific Journal of Clinical Nutrition. 2014; 23(1):91-104. [DOI:10.6133/apjcn.2014.23.1.18] [PMID]
Article Type : Applicable |
Subject:
Special
Received: 2019/10/28 | Accepted: 2019/12/5 | Published: 2020/01/1
Received: 2019/10/28 | Accepted: 2019/12/5 | Published: 2020/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |