Tue, Apr 23, 2024
Volume 29, Issue 4 (9-2019)
JHNM 2019, 29(4): 218-227 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zahedi R, Baghaei M, Yeganehfarzand M R, Kazemnezhad Leili E. The Relationship of Health Literacy and Adherence to Self-care Behaviors in Patients With Metabolic Syndrome. JHNM 2019; 29 (4) :218-227
URL: http://hnmj.gums.ac.ir/article-1-774-en.html
URL: http://hnmj.gums.ac.ir/article-1-774-en.html
1- Nursing (MSN), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. , rezazahedi1991@gmail.com
2- Instructor, Department of Nursing (Medical-Surgical), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
3- Associate Professor, Social Determinants of Health Research Center (SDHRC), Bio-Statistics, Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Nursing (Medical-Surgical), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
3- Associate Professor, Social Determinants of Health Research Center (SDHRC), Bio-Statistics, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 600 kb]
(674 Downloads)
| Abstract (HTML) (2838 Views)
Full-Text: (1188 Views)
Introduction
long with the increasing obesity and sedentary lifestyle, metabolic syndrome has become a tremendous and growing challenge for health care services all over the world [1]. This syndrome is associated with cardiovascular risk factors, such as abdominal obesity, high blood pressure, impaired glucose tolerance or disruption of insulin metabolism, and lipid disorders (increased triglycerides and low high-density lipoprotein) [2]. Therefore, patients with metabolic syndrome are prone to catch cardiovascular diseases and type 2 diabetes 5-10 years after the diagnosis of the syndrome. Also, they are more susceptible to stroke and myocardial infarction. Eventually, the mortality rate in this syndrome regardless of having a history of cardiovascular diseases is twice as non-afflicted people [1].
Economic burden of metabolic syndrome is also noteworthy because the annual health expenditure of patients with metabolic syndrome is (60%) more than non-afflicted people [3]. For instance, the annual health cost of a patient with metabolic syndrome is $4000 in America [4]. It is estimated that around (25%) of people in Europe and (32%) of people in America have this syndrome. This figure rises to (40%) for older people [5]. The prevalence of this syndrome in Iran has been estimated (38%) according to the International Diabetes Federation (IDF) and (29%) according to National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) [6]. Thus, it is critical to pay more attention to the prevention and treatment of metabolic syndrome as well as using practical approaches towards this syndrome in society [7].
The exact etiology of this syndrome is unknown. But, genetics and environmental factors such as inappropriate diet and obesity are already regarded as its associated factors [8]. Accordingly, for decreasing the risk of metabolic syndrome, medicinal therapy, and correction of lifestyle in observing diet are recommendations [9]. Evidence supports the effectiveness of early changes in lifestyle and use of necessary medications in preventing heart diseases and diabetes in the patients with this syndrome and noticeable reduction of their mortality rate with the use of statins [10, 11]. Observing these items require the active participation of high-risk patients [12]. So, self-care behavior, including learning and active performance of required skills, is considered as the cornerstone of long-term care management [13]. It is recommended that the patients with this syndrome be encouraged to do self-care behavior to control and treat this illness [14].
The expected self-care behaviors in patients with metabolic syndrome are usually a set of defined behaviors, including having a healthy diet, doing exercise, using medications, and so on which has to be followed by the patients every day to gain better control of the disease [15]. According to the study of Hamadzadeh et al. in Tehran, a large percentage of diabetics had an average or low self-care behaviors [16]. Zinat Motlagh et al. reported that only a small percentage of patients with high blood pressure had adherence to observing diet and exercise [17]. These findings may be because of the nature of self-care behavior, which is a process. This process needs knowledge and skills to do the recommended behavior by the patient [18]. People with high health literacy are capable of acquiring the correct and accurate information from different sources to understand their situation and also self-care behaviors [19]. According to the results of the national study done by Tavousi, these conditions indicate inadequate health literacy in (44.4%)of the studied people [20]. The results of research done in Rasht City also shows adequate health literacy, just, in (41.6%) of people with high blood pressure [21].
On the other hand, the studies on the relationship between health literacy and self-care behaviors yielded contradictory results [22-25]. Regarding the high prevalence of metabolic syndrome in the country and the low level of self-care behaviors in patients with chronic diseases, patients with metabolic syndrome need special attention [6, 14]. Therefore, this study aimed to examine the relationship between health literacy and self-care behaviors in patients with metabolic syndrome. It is hoped that the findings of this study be an appropriate guideline for health services managers and clinical nurses to take proper interventions towards health literacy promotion and also increase the level of self-care behavior of patients with metabolic syndrome.
Materials and Methods
This analytical cross-sectional study was conducted on the patients with metabolic syndrome who referred to selected specialist clinics of educational university hospitals affiliated to Guilan University of Medical Sciences and other health centers in Rasht City, Iran.
The sample size was estimated as 166 according to Raiesi et al. study (using the correlation coefficient of observing diet and the score of health literacy [r=0.22]), with the confidence interval of (95%) and power of (85%) [18]. To control the effect of confounding variables, the researcher added (10%) to the sample size, and eventually, 184 samples were recruited for the study. The inclusion criteria included having metabolic syndrome according to National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) (the existence of at least 3 out of 5 criteria, including waist circumference ≥88 cm in women and ≥102cm in men; blood pressure ≥130.85mm Hg; fasting blood glucose ≥100; blood triglyceride level ≥150mg/dL; and high density lipoprotein >50mg/dL in women and >40 in men) [26]; being 18-65 years old; having reading and writing ability; using at least one medicine to control metabolic syndrome symptoms; lacking disabling diseases like myocardial infarction, stroke, and remembering the frequency of doing self-care behaviors in the last seven days.
The sampling was done in the health centers in the morning shift. At first, all patients referred to clinics with relevant test results (triglyceride, cholesterol, high-density lipoprotein, and fasting blood glucose) were selected during three months before data gathering. Then, their systolic and diastolic blood pressure (using digital barometer device model Beurer BM20, according to mm Hg) and waist circumference (using an inelastic measuring tape) were measured and recorded. The sampling was done in June and July of 2016.
The study data were collected with a 3-part tool, including personal and disease-related information questionnaire, Hypertension Self-Care Activity Level Effects (H-SCALE), and Health Literacy for Iranian Adults (HELIA).
The personal information questionnaire collected information about age, gender, marital status, level of education, employment status of the samples as well as their disease-related information, including how long the patient had diabetes, high blood pressure, and high blood lipids, history of receiving instructions about these disorders and weight control. H-SCALE, designed by Seymour and Warren-Findlow in 2011, was the second part of the study instrument which contained 31 questions for measuring the adherence to self-care behaviors in observing medications (three questions), observing diet (12 questions), doing exercise (two questions), smoking (one question), alcohol drinking (three questions), and observing weight control (ten questions) in the last seven days before sampling [27]. In this study, two questions about adherence to a low sugar diet were added to observing diet questions. The questions in all subscales except weight control were rated from zero to seven (based on the frequency of the behaviors done in the week days). Regarding the weight control subscale, the questions were rated based on a five-point Likert-type scale from five = always to one = never.
Finally, the samples were categorized based on their obtained scores into two groups. The adherence group to the self-care behaviors were those who obtained 21 score in medication adherence (range: 0-21), ≥6 score in diet adherence (range: 0-7), ≥8 score in doing exercise (range: 0-14), zero score in smoking (range: 0-7), zero score in drinking alcohol (range: 0-21), and ≥40 score in weight control (range: 10-50). The others were in the non-adherence group.
The validity of this questionnaire after translation and back-translation was evaluated with content validation method (with receiving opinions of nine nursing specialists and one endocrinologist). Quantitative methods of content validity by determining CVI and CVR confirmed the validity of all questions but two questions in the diet section that were removed from the questions because of low score obtained (0.62) in the clarity of phrase. The reliability of the scale was evaluated by performing a pilot study on 20 eligible people (to be in the study), using the test-retest method with a two-week interval. Comparing the results of the two tests showed no significant differences between the phases. The internal consistency of the tool was evaluated by calculating the Cronbach alpha coefficients in all subscales and confirmed by obtaining an alpha coefficient of more than 0.7.
The third part of the instrument was HELIA questionnaire that measured the samples’ health literacy [25]. This 33-item tool evaluates health literacy in dimensions of access (six items), reading skill (four items), understanding (seven items), appraisal (four items), decision making and application of health information (12 items). The items were rated according to 5-point Likert-type scale in all dimensions, except reading, from never (score one), hardly (score two), sometimes (score three), mostly (score four), and always (score five). The reading items are rated based on a five-option scale with answers of “absolutely hard”, “hard”, “not hard-not easy”, “easy”, and “absolutely easy”. The scores gained in this instrument, after calculating it in percentage (with the range of 0-100), were categorized in four levels of inadequate health literacy (0-50), not enough (50.1-66), adequate (66.1-84), and high (84.1-100). This questionnaire has been customized for Iran [28].
The study data were collected after receiving a written letter of consent from participants. The analyses were done by descriptive statistics, the Chi-square test, and multiple logistic regression in SPSS V. 22. The significance level was set at P level less than 0.05.
Results
The Mean±SD age of the study samples was 52.5±7.6 years. They were mostly men (55.4%), married (95.1%), employed (35.9%), and had a diploma or under diploma education (60.3%). The Mean±SD duration of having diabetes, high blood pressure, and high blood lipids in the samples were respectively 5.41±5.25, 5.21±4.49, and 4.93±4.41 years. The percentages of the samples who had a history of receiving education about self-care behavior in managing blood pressure, diabetes, high blood lipids, and losing weight were (27.2%), (20.7%), (10.9%), and (9.8%), respectively.
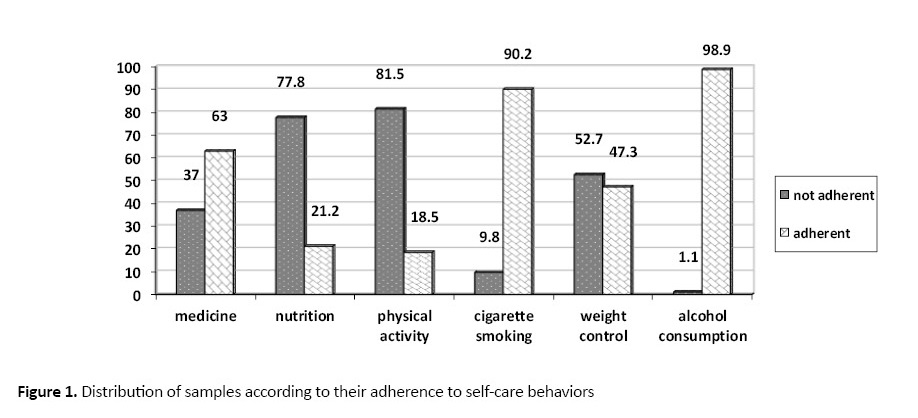
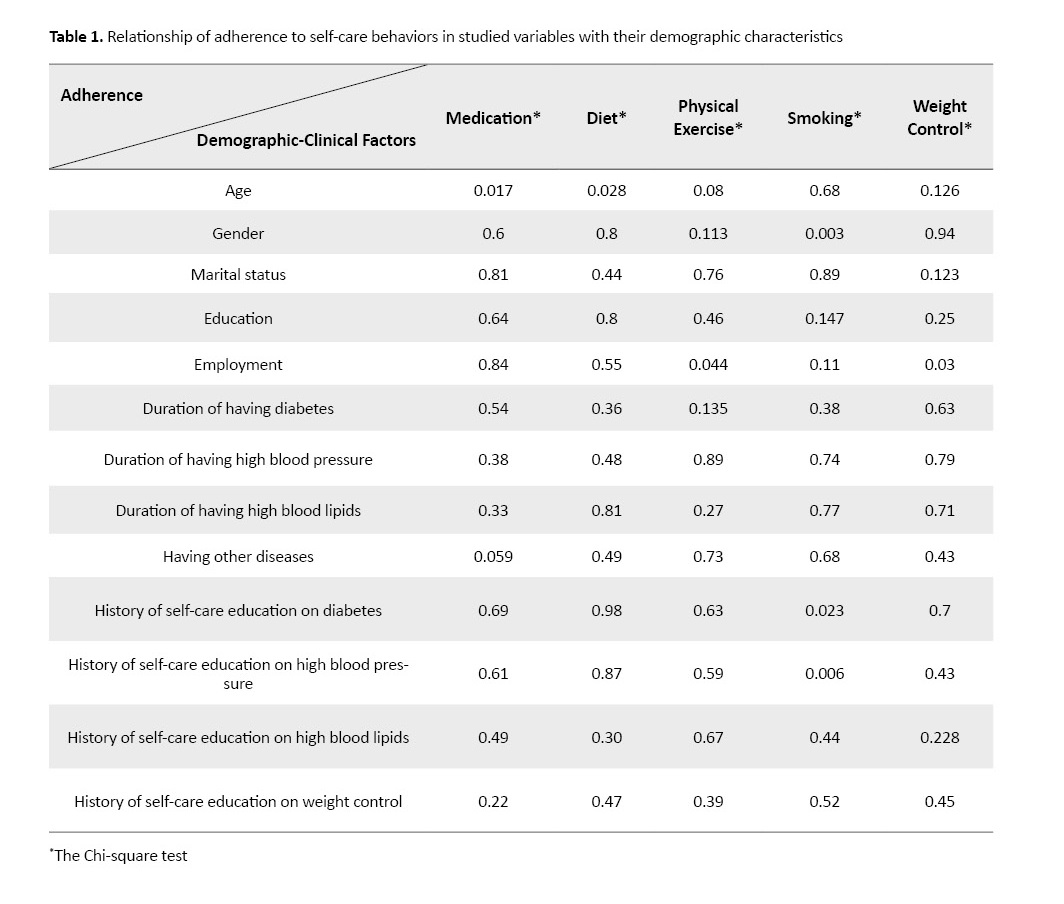
Table 1 presents the adherence level of the samples to self-care behaviors. Figure 1 shows the relationship of adherence to self-care behaviors in studied samples with regard to their demographic variables.
long with the increasing obesity and sedentary lifestyle, metabolic syndrome has become a tremendous and growing challenge for health care services all over the world [1]. This syndrome is associated with cardiovascular risk factors, such as abdominal obesity, high blood pressure, impaired glucose tolerance or disruption of insulin metabolism, and lipid disorders (increased triglycerides and low high-density lipoprotein) [2]. Therefore, patients with metabolic syndrome are prone to catch cardiovascular diseases and type 2 diabetes 5-10 years after the diagnosis of the syndrome. Also, they are more susceptible to stroke and myocardial infarction. Eventually, the mortality rate in this syndrome regardless of having a history of cardiovascular diseases is twice as non-afflicted people [1].
Economic burden of metabolic syndrome is also noteworthy because the annual health expenditure of patients with metabolic syndrome is (60%) more than non-afflicted people [3]. For instance, the annual health cost of a patient with metabolic syndrome is $4000 in America [4]. It is estimated that around (25%) of people in Europe and (32%) of people in America have this syndrome. This figure rises to (40%) for older people [5]. The prevalence of this syndrome in Iran has been estimated (38%) according to the International Diabetes Federation (IDF) and (29%) according to National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) [6]. Thus, it is critical to pay more attention to the prevention and treatment of metabolic syndrome as well as using practical approaches towards this syndrome in society [7].
The exact etiology of this syndrome is unknown. But, genetics and environmental factors such as inappropriate diet and obesity are already regarded as its associated factors [8]. Accordingly, for decreasing the risk of metabolic syndrome, medicinal therapy, and correction of lifestyle in observing diet are recommendations [9]. Evidence supports the effectiveness of early changes in lifestyle and use of necessary medications in preventing heart diseases and diabetes in the patients with this syndrome and noticeable reduction of their mortality rate with the use of statins [10, 11]. Observing these items require the active participation of high-risk patients [12]. So, self-care behavior, including learning and active performance of required skills, is considered as the cornerstone of long-term care management [13]. It is recommended that the patients with this syndrome be encouraged to do self-care behavior to control and treat this illness [14].
The expected self-care behaviors in patients with metabolic syndrome are usually a set of defined behaviors, including having a healthy diet, doing exercise, using medications, and so on which has to be followed by the patients every day to gain better control of the disease [15]. According to the study of Hamadzadeh et al. in Tehran, a large percentage of diabetics had an average or low self-care behaviors [16]. Zinat Motlagh et al. reported that only a small percentage of patients with high blood pressure had adherence to observing diet and exercise [17]. These findings may be because of the nature of self-care behavior, which is a process. This process needs knowledge and skills to do the recommended behavior by the patient [18]. People with high health literacy are capable of acquiring the correct and accurate information from different sources to understand their situation and also self-care behaviors [19]. According to the results of the national study done by Tavousi, these conditions indicate inadequate health literacy in (44.4%)of the studied people [20]. The results of research done in Rasht City also shows adequate health literacy, just, in (41.6%) of people with high blood pressure [21].
On the other hand, the studies on the relationship between health literacy and self-care behaviors yielded contradictory results [22-25]. Regarding the high prevalence of metabolic syndrome in the country and the low level of self-care behaviors in patients with chronic diseases, patients with metabolic syndrome need special attention [6, 14]. Therefore, this study aimed to examine the relationship between health literacy and self-care behaviors in patients with metabolic syndrome. It is hoped that the findings of this study be an appropriate guideline for health services managers and clinical nurses to take proper interventions towards health literacy promotion and also increase the level of self-care behavior of patients with metabolic syndrome.
Materials and Methods
This analytical cross-sectional study was conducted on the patients with metabolic syndrome who referred to selected specialist clinics of educational university hospitals affiliated to Guilan University of Medical Sciences and other health centers in Rasht City, Iran.
The sample size was estimated as 166 according to Raiesi et al. study (using the correlation coefficient of observing diet and the score of health literacy [r=0.22]), with the confidence interval of (95%) and power of (85%) [18]. To control the effect of confounding variables, the researcher added (10%) to the sample size, and eventually, 184 samples were recruited for the study. The inclusion criteria included having metabolic syndrome according to National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) (the existence of at least 3 out of 5 criteria, including waist circumference ≥88 cm in women and ≥102cm in men; blood pressure ≥130.85mm Hg; fasting blood glucose ≥100; blood triglyceride level ≥150mg/dL; and high density lipoprotein >50mg/dL in women and >40 in men) [26]; being 18-65 years old; having reading and writing ability; using at least one medicine to control metabolic syndrome symptoms; lacking disabling diseases like myocardial infarction, stroke, and remembering the frequency of doing self-care behaviors in the last seven days.
The sampling was done in the health centers in the morning shift. At first, all patients referred to clinics with relevant test results (triglyceride, cholesterol, high-density lipoprotein, and fasting blood glucose) were selected during three months before data gathering. Then, their systolic and diastolic blood pressure (using digital barometer device model Beurer BM20, according to mm Hg) and waist circumference (using an inelastic measuring tape) were measured and recorded. The sampling was done in June and July of 2016.
The study data were collected with a 3-part tool, including personal and disease-related information questionnaire, Hypertension Self-Care Activity Level Effects (H-SCALE), and Health Literacy for Iranian Adults (HELIA).
The personal information questionnaire collected information about age, gender, marital status, level of education, employment status of the samples as well as their disease-related information, including how long the patient had diabetes, high blood pressure, and high blood lipids, history of receiving instructions about these disorders and weight control. H-SCALE, designed by Seymour and Warren-Findlow in 2011, was the second part of the study instrument which contained 31 questions for measuring the adherence to self-care behaviors in observing medications (three questions), observing diet (12 questions), doing exercise (two questions), smoking (one question), alcohol drinking (three questions), and observing weight control (ten questions) in the last seven days before sampling [27]. In this study, two questions about adherence to a low sugar diet were added to observing diet questions. The questions in all subscales except weight control were rated from zero to seven (based on the frequency of the behaviors done in the week days). Regarding the weight control subscale, the questions were rated based on a five-point Likert-type scale from five = always to one = never.
Finally, the samples were categorized based on their obtained scores into two groups. The adherence group to the self-care behaviors were those who obtained 21 score in medication adherence (range: 0-21), ≥6 score in diet adherence (range: 0-7), ≥8 score in doing exercise (range: 0-14), zero score in smoking (range: 0-7), zero score in drinking alcohol (range: 0-21), and ≥40 score in weight control (range: 10-50). The others were in the non-adherence group.
The validity of this questionnaire after translation and back-translation was evaluated with content validation method (with receiving opinions of nine nursing specialists and one endocrinologist). Quantitative methods of content validity by determining CVI and CVR confirmed the validity of all questions but two questions in the diet section that were removed from the questions because of low score obtained (0.62) in the clarity of phrase. The reliability of the scale was evaluated by performing a pilot study on 20 eligible people (to be in the study), using the test-retest method with a two-week interval. Comparing the results of the two tests showed no significant differences between the phases. The internal consistency of the tool was evaluated by calculating the Cronbach alpha coefficients in all subscales and confirmed by obtaining an alpha coefficient of more than 0.7.
The third part of the instrument was HELIA questionnaire that measured the samples’ health literacy [25]. This 33-item tool evaluates health literacy in dimensions of access (six items), reading skill (four items), understanding (seven items), appraisal (four items), decision making and application of health information (12 items). The items were rated according to 5-point Likert-type scale in all dimensions, except reading, from never (score one), hardly (score two), sometimes (score three), mostly (score four), and always (score five). The reading items are rated based on a five-option scale with answers of “absolutely hard”, “hard”, “not hard-not easy”, “easy”, and “absolutely easy”. The scores gained in this instrument, after calculating it in percentage (with the range of 0-100), were categorized in four levels of inadequate health literacy (0-50), not enough (50.1-66), adequate (66.1-84), and high (84.1-100). This questionnaire has been customized for Iran [28].
The study data were collected after receiving a written letter of consent from participants. The analyses were done by descriptive statistics, the Chi-square test, and multiple logistic regression in SPSS V. 22. The significance level was set at P level less than 0.05.
Results
The Mean±SD age of the study samples was 52.5±7.6 years. They were mostly men (55.4%), married (95.1%), employed (35.9%), and had a diploma or under diploma education (60.3%). The Mean±SD duration of having diabetes, high blood pressure, and high blood lipids in the samples were respectively 5.41±5.25, 5.21±4.49, and 4.93±4.41 years. The percentages of the samples who had a history of receiving education about self-care behavior in managing blood pressure, diabetes, high blood lipids, and losing weight were (27.2%), (20.7%), (10.9%), and (9.8%), respectively.
Table 1 presents the adherence level of the samples to self-care behaviors. Figure 1 shows the relationship of adherence to self-care behaviors in studied samples with regard to their demographic variables.
The highest Mean±SD value of health literacy of the samples was seen in understanding dimension (85.81±15.17) and next in decision making and behavior (81.57±15.66), access (72.94±23.20), appraisal (71.64±23.17), and reading (69.97±26.94). The Mean±SD total score of samples’ health literacy was 76.39±15.56. Most of the samples had adequate health literacy (44.6%). Table 2 presents the relationship of health literacy level with adherence to self-care behaviors in the studied samples.
According to logistic regression analysis, access dimension was the predictor of a dherence to weight control (P=0.011) and decision making and behavior was the predictor of adherence to using medications (P=0.002), diet, cigarette smoking, and weight control (P=0.001, P=0.001, and P=0.001, respectively). Also, age variable in two age ranges of 50-60 years and older than 60 years (P=0.006), compared to age range of below 50 years (P=0.0029) was the predictor of adherence to using medication; retired people compared to employed people was the predictor of adherence to exercise and weight control (P=0.042); female gender compared to male gender was the predictor of adherence to smoking (P=0.007); not having diabetes compared to five years of having diabetes was the predictor of adherence to exercise (P=0.039) (Table 3).
Discussion
The results of this study indicated that a considerable percentage of the studied samples were not adherent to self-care behaviors in observing a healthy diet and doing exercise and controlling their weight. This result, which is consistent with some studies, shows these patients should receive self-care promoting interventions because adherence to self-care behaviors is crucial [17, 27]. For instance, appropriate self-care behaviors can reduce the risk of cardiovascular side-effects that are responsible for the death of (70-80%) of them [29].
On the other hand, the results show an increase in adherence to self-care behaviors in using the medicine in older people. This result agrees with the outcome of some other studies [17, 27]. These results are obtained with regard to the possibility of the existence of other diseases in older people such as cognitive problems (Alzheimer and dementia), physical limitations, vision and hearing impairment, and low literacy that each of them can weaken adherence to medicine usage in these ages [30]. Of course, older people are usually affected by several simultaneous and chronic illnesses, and their understanding of the potential disability of the disease may make them more sensitiveness towards using medications. In addition, more attention of the family members towards the elderly can be another factor in their adherence to using medications [31].
Also, the over 60 year’s age samples in this study had a weaker adherence to diet compared to other age groups. These findings are consistent with Elbur study results. This researcher believed that cultural elements were among the responsible factors for the weak adherence to diet in this age group [32]. This argument is acceptable considering that most participants in this study were men and preparing and cooking food is mainly a responsibility of women in Iranian culture.
Findings of this study indicated that retired people had more adherence to exercise and weight control tasks compared to employed people and housekeeper(P=0.008). It should be noted that retired people, regardless of their history of employment and its related social relations, have lower levels of occupational and routine life concerns, than employed people. Therefore, this group of people may have more time for arranging and performing physical activity plans. However, the result of Zinat Motlagh study shows no significant relationship between self-care behavior and employment condition in the studied samples [17].
Adequate and high health literacy in most of the samples of this study, which is similar to the results of Haghighi study, is a promising finding. Experts believe that people with a high level of health literacy are capable of experiencing better and more appropriate health services because of their cooperation with health centers and following healthy instructions [33, 34]. However, the results of this study are inconsistent with Izadirad study results [35]. The discrepancy in the findings can be related to the study population and samples. This study was conducted on patients with metabolic syndrome in a city in North of Iran (Rasht) and with the samples’ Mean±SD age of 52.5±7.6 years. However, Izadirad et al. conducted their study in a southern province (Baluchestan) on younger samples [36].
A positive and significant relationship exists between total level of health literacy and all dimensions of it, including reading, access, understanding, appraisal, and decision making and behavior only with adherence to self-care behavior in losing weight. This is one of the noteworthy findings of this study. So that the people with a higher level of total health literacy and its dimensions had more adherence in losing weight measures. This finding was not consistent with the results of many studies. For instance, Seyed Shohadaei study indicates a significant relationship between health literacy and self-care dimensions in using medication and diet [22].
Raiesi et al. found only a direct and significant relationship between health literacy and self-care behavior in using medications and doing exercise [18]. Ghaedi et al. study also indicates an indirect and significant relationship between health literacy and self-care behavior in observing diet and doing exercise [25]. The discrepancies in the findings of the mentioned studies with this study may be due to the differences in the study instrument used for evaluating health literacy.
Finally, examining the relationship of health literacy with adherence to self-care behaviors in patients with metabolic syndrome with regression test indicated that the total level of health literacy did not have the predicting ability for self-care behavior. But, in our study, the decision making and behavior dimension of health literacy could predict the self-care behaviors of using medications, observing a healthy diet, smoking, and controlling weight.
Yokokawa also found in his study that decision-making dimension of health literacy had a significant statistical relationship with the characteristic of a healthy lifestyle [37]. This finding, which indicates the effect of patients’ taking part in joint therapy decision making to improve self-care behaviors, is justifiable. However, patients with metabolic syndrome need knowledge and proper attitude for successful control of the syndrome and promotion of their adherence to self-care behavior. Therefore, it is necessary that in disease prevention and improving health plans, health, and treatment authorities pay more attention to decision making dimension of health literacy. Also, it is suggested that the skills and learning capacities of patients in using social networks, especially the Internet, social media, and communicating skills be developed.
The uncontrollable limitations of this study were the non-random sampling method and collecting data using the self-reporting method in the crowded environment of clinics that made it difficult for the sample to remind self-care behavior in the last week.
Ethical Considerations
Compliance with ethical guidelines
After obtaining permission from the Ethics Committee of Deputy for Research and Technology of Guilan University of Medical Sciences (IR.GUMS.REC.1394.633) and receiving a letter of introduction.
Funding
The present paper was extracted from the Master thesis of Reza Zahedi, in Social Determinants of Health Research Center (SDHRC) at Guilan University of Medical Sciences (Registration No.: 94122505). This study was financially supported by the Social Determinants of Health Research Center of Guilan University of Medical Sciences.
Authors contributions
All authors equally contributed in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We want to appreciate the respectable Deputy for the Research and Technology of Guilan University of Medical Sciences, the Social Determinants of Health Research Center, all colleagues of university hospitals of Dr. Heshmat and Razi in Rasht, particularly the specialist clinics of these centers, and finally all patients taking part in this study.
References
The results of this study indicated that a considerable percentage of the studied samples were not adherent to self-care behaviors in observing a healthy diet and doing exercise and controlling their weight. This result, which is consistent with some studies, shows these patients should receive self-care promoting interventions because adherence to self-care behaviors is crucial [17, 27]. For instance, appropriate self-care behaviors can reduce the risk of cardiovascular side-effects that are responsible for the death of (70-80%) of them [29].
On the other hand, the results show an increase in adherence to self-care behaviors in using the medicine in older people. This result agrees with the outcome of some other studies [17, 27]. These results are obtained with regard to the possibility of the existence of other diseases in older people such as cognitive problems (Alzheimer and dementia), physical limitations, vision and hearing impairment, and low literacy that each of them can weaken adherence to medicine usage in these ages [30]. Of course, older people are usually affected by several simultaneous and chronic illnesses, and their understanding of the potential disability of the disease may make them more sensitiveness towards using medications. In addition, more attention of the family members towards the elderly can be another factor in their adherence to using medications [31].
Also, the over 60 year’s age samples in this study had a weaker adherence to diet compared to other age groups. These findings are consistent with Elbur study results. This researcher believed that cultural elements were among the responsible factors for the weak adherence to diet in this age group [32]. This argument is acceptable considering that most participants in this study were men and preparing and cooking food is mainly a responsibility of women in Iranian culture.
Findings of this study indicated that retired people had more adherence to exercise and weight control tasks compared to employed people and housekeeper(P=0.008). It should be noted that retired people, regardless of their history of employment and its related social relations, have lower levels of occupational and routine life concerns, than employed people. Therefore, this group of people may have more time for arranging and performing physical activity plans. However, the result of Zinat Motlagh study shows no significant relationship between self-care behavior and employment condition in the studied samples [17].
Adequate and high health literacy in most of the samples of this study, which is similar to the results of Haghighi study, is a promising finding. Experts believe that people with a high level of health literacy are capable of experiencing better and more appropriate health services because of their cooperation with health centers and following healthy instructions [33, 34]. However, the results of this study are inconsistent with Izadirad study results [35]. The discrepancy in the findings can be related to the study population and samples. This study was conducted on patients with metabolic syndrome in a city in North of Iran (Rasht) and with the samples’ Mean±SD age of 52.5±7.6 years. However, Izadirad et al. conducted their study in a southern province (Baluchestan) on younger samples [36].
A positive and significant relationship exists between total level of health literacy and all dimensions of it, including reading, access, understanding, appraisal, and decision making and behavior only with adherence to self-care behavior in losing weight. This is one of the noteworthy findings of this study. So that the people with a higher level of total health literacy and its dimensions had more adherence in losing weight measures. This finding was not consistent with the results of many studies. For instance, Seyed Shohadaei study indicates a significant relationship between health literacy and self-care dimensions in using medication and diet [22].
Raiesi et al. found only a direct and significant relationship between health literacy and self-care behavior in using medications and doing exercise [18]. Ghaedi et al. study also indicates an indirect and significant relationship between health literacy and self-care behavior in observing diet and doing exercise [25]. The discrepancies in the findings of the mentioned studies with this study may be due to the differences in the study instrument used for evaluating health literacy.
Finally, examining the relationship of health literacy with adherence to self-care behaviors in patients with metabolic syndrome with regression test indicated that the total level of health literacy did not have the predicting ability for self-care behavior. But, in our study, the decision making and behavior dimension of health literacy could predict the self-care behaviors of using medications, observing a healthy diet, smoking, and controlling weight.
Yokokawa also found in his study that decision-making dimension of health literacy had a significant statistical relationship with the characteristic of a healthy lifestyle [37]. This finding, which indicates the effect of patients’ taking part in joint therapy decision making to improve self-care behaviors, is justifiable. However, patients with metabolic syndrome need knowledge and proper attitude for successful control of the syndrome and promotion of their adherence to self-care behavior. Therefore, it is necessary that in disease prevention and improving health plans, health, and treatment authorities pay more attention to decision making dimension of health literacy. Also, it is suggested that the skills and learning capacities of patients in using social networks, especially the Internet, social media, and communicating skills be developed.
The uncontrollable limitations of this study were the non-random sampling method and collecting data using the self-reporting method in the crowded environment of clinics that made it difficult for the sample to remind self-care behavior in the last week.
Ethical Considerations
Compliance with ethical guidelines
After obtaining permission from the Ethics Committee of Deputy for Research and Technology of Guilan University of Medical Sciences (IR.GUMS.REC.1394.633) and receiving a letter of introduction.
Funding
The present paper was extracted from the Master thesis of Reza Zahedi, in Social Determinants of Health Research Center (SDHRC) at Guilan University of Medical Sciences (Registration No.: 94122505). This study was financially supported by the Social Determinants of Health Research Center of Guilan University of Medical Sciences.
Authors contributions
All authors equally contributed in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We want to appreciate the respectable Deputy for the Research and Technology of Guilan University of Medical Sciences, the Social Determinants of Health Research Center, all colleagues of university hospitals of Dr. Heshmat and Razi in Rasht, particularly the specialist clinics of these centers, and finally all patients taking part in this study.
References
- Kaur J. A comprehensive review on metabolic syndrome. Cardiology Research and Practice. 2014; 2014(943162):1-21. [DOI:10.1155/2014/943162] [PMID] [PMCID]
- Mann Dl, Zipes Dp, Libby P, Bonow R. Braunwald’s textbook of cardiovascular medicine. Philadephia: Elsevier Saunders; 2015.
- Mahabaleshwarkar R, Taylor YJ, Spencer MD, Mohanan S. Prevalence of metabolic syndrome in a large integrated health care system in north carolina. North Carolina Medical Journal. 2016; 77(3):168-74. [DOI:10.18043/ncm.77.3.168] [PMID]
- Homayounfar R, Ehrampoush E, Koohpaye SA, Meshkibaf MH, Taghizade S, Almasi A, et al. [Diet-induced metabolic syndrome model in rats (Persian)]. Journal of Fasa University of Medical Sciences. 2013; 2(4):288-96.
- Soosova M, Hrehova J. The effect of education on lifestyle changes and metabolic syndrome components. Central European Journal of Nursing and Midwifery. 2014; 5(4):161-8. [DOI:10.15452/CEJNM.2014.05.0012]
- Maleki F, Sayehmiri F, Kiani F, sayehmiri K, Nasiri S. [Metabolic syndrome prevalence in Iran: A systematic review and meta analysis (Persian)]. Journal of Kermanshah University of Medical Sciences. 2014; 18(4):242-50.
- Dalvand S, Niksima SH, Meshkani R, Gheshlagh RG, Sadegh-Nejadi S, Kooti W. Prevalence of metabolic syndrome among Iranian population: A systematic review and meta-analysis. Iranian Journal of Public Health. 2017; 46(4):456-67.
- Nanri A , Tomita K, Matsushita Y, Ichikawa F, Yamamoto M, Nagafuchi Y, et al. Effect of six months lifestyle intervention in Japanese men with metabolic syndrome: Randomized controlled trial. Journal of Occupational Health. 2012; 54(3):215-22. [DOI:10.1539/joh.11-0238-OA] [PMID]
- Ghasemifard N , Fallahi E, Barak F, Saneei P, Hassanzadeh keshteli A, et al. [The association between dietary approaches to stop hypertension diet and metabolic syndrome in women (Persian)]. Hamadan University of Medical Sciences. 2014; 21(2):112-21.
- Lin CH, Chiang SL, Heitkemper MM, Hung YJ, Lee MS, Tzeng WC, et al. Effects of telephone-based motivational interviewing in lifestyle modification program on reducing metabolic risks in middle-aged and older women with metabolic syndrome: A randomized controlled trial. International Journal of Nursing Studies. 2016; 60:12-23. [DOI:10.1016/j.ijnurstu.2016.03.003] [PMID]
- Heidari Z, Hosseinpanah F, Mehrabi Y, Azizi F. Evaluation of power of components of metabolic syndrome for prediction of its development: A 6.5 year longitudinal study in Tehran Lipid and Glucose Study (TLGS). Iranian Journal of Endocrinology and Metabolism. 2010; 11(5):530-42. [DOI:10.1038/ejcn.2010.111] [PMID]
- Karalis DG . Achieving optimal lipid goals in the metabolic syndrome: A global health problem. Atherosclerosis. 2014; 237(1):191-3. [DOI:10.1016/j.atherosclerosis.2014.07.039] [PMID]
- Baljani E, Salimi S, Rahimi J, Amanpour E, Parkhashjou M, Sharifnejad A, et al. [The effect of education on promoting self efficacy in patients with cardiovascular disease (Persian)]. Journal of Kermanshah University of Medical Sciences. 2012; 16(3):227-35.
- Kim CJ, Park JW, Park HR. Effects of a community‐based intervention on cardio‐metabolic risk and self‐care behaviour in older adults with metabolic syndrome. International Journal of Nursing Practice. 2014; 20(2):212-20. [DOI:10.1111/ijn.12139] [PMID]
- Vieira CM, Chvatal VL, Cordeiro SN, Turato ER. Nutrition and self-care practices of patients with chronic Metabolic Syndrome: A qualitative study. Acta Paul Enferm. 2012; 25(4):537-42. [DOI:10.1590/S0103-21002012005000017]
- Mohebbi S, Azadbakht L, Feyzi A, Sharifirad G, Hozoori M. [An assessment of the correlation between nutritional self-management and health promotion model constructs in women with metabolic syndrome, 2012 (Persian)]. Qom University of Medical Sciences Journal. 2013; 7(5):42-52.
- Hamadzadeh S, Ezatti ZH, Abedsaeidi ZH, Nasiri N. [Coping styles and self-care behaviors among diabetic patients (Persian)]. Iran Journal of Nursing. 2013; 25(80):24-33.
- Zinat Motlagh SF, Chaman R, Sadeghi E, Eslami AA. [Self-care behaviors and related factors in hypertensive patients (Persian)]. Iranian Red Crescent Medical Journal. 2016; 18(6):e35805. [DOI:10.5812/ircmj.35805] [PMID] [PMCID]
- Reisi M, Mostafavi F, Javadzade H, Mahaki B, Tavassoli E, Sharifirad G. [Communicative and critical health literacy and self-care behaviors in patients with type 2 diabetes (Persian)]. Iranian Journal of Diabetes and Metabolism. 2016; 14(3):199-208.
- Reisi M, Mostafavi F, Javadzade SH, Mahaki B, Sharifirad G. [Assessment of some predicting factors of self-efficacy in patients with type 2 diabetes (Persian)]. Iranian Journal of Endocrinology and Metabolism. 2015; 17(1):44-52. [DOI:10.5001/omj.2016.10] [PMID] [PMCID]
- Tavousi M, Haeri MA, Rafiefar S, Solimanian A, Sarbandi F, Ardestani M, et al. [A health literacy in Iran: Finding from a national study (Persian)]. Payesh. 2016; 15(1):95-102.
- Darvishpour J, Omidi S, Farmanbar R. The relationship between health literacy and hypertension treatment control and follow-up. Caspian Journal of Health Research. 2016; 2(1):1-8. [DOI:10.18869/acadpub.cjhr.2.1.1]
- Seyedoshohadaee M, Barasteh S, Jalalinia F, Eghbali M, Nezami M. [The relationship between health literacy and self-care behaviors in patients with type 2 diabetes (Persian)]. Iranian Journal of Nursing Research. 2016; 10(4):43-51.
- Liu YB, Liu L, Li YF, Chen YL. Relationship between health literacy, health-related behaviors and health status: A survey of elderly Chinese. International Journal of Environmental Research and Public Health. 2015; 12(8):9714-25. [DOI:10.3390/ijerph120809714] [PMID] [PMCID]
- Al Sayah F, Majumdar SR, Egede LE, Johnson JA. Associations between health literacy and health outcomes in a predominantly low-income African American population with type 2 diabetes. Journal of Health Communication. 2015; 20(5):581-8. [DOI:10.1080/10810730.2015.1012235] [PMID]
- Ghaedi M, Banihashemi F, Latifi M, Soleymaninejad M. [The relationship between health literacy and self-care among patients with type 2 diabetes residing in the city of Bastak (Persian)]. Iranian Journal of Endocrinology and Metabolism. 2016; 18(2):90-6.
- Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American heart association/national heart, lung, and blood institute scientific statement. Circulation. 2005; 112(17):2735-52. [DOI:10.1161/CIRCULATIONAHA.105.169404] [PMID]
- Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. Journal of the National Medical Association. 2011; 103(6):503-12. [DOI:10.1016/S0027-9684(15)30365-5]
- Montazeri A, Tavousi M. Ra hshani F, Azin SA, Jahangiri K, Ebadi M, et al. [Health Literacy for Iranian Adults (HELIA): Development and psychometric properties (Persian)]. Payesh. 2014; 13(5):589-99.
- Mohebi S, Azadbakhat L, Feyzi A, Hozoori M, Sharifirad G. [Effect of social support from husband on the control of risk factors for metabolic syndrome (Persian)]. Iranian Journal of Endocrinology and Metabolism. 2014; 16(1):11-9.
- Arrelias CC, Faria HT, Teixeira CR, Santos MA, Zanetti ML. Adherence to diabetes mellitus treatment and sociodemographic, clinical and metabolic control variables. Acta Paulista de Enfermagem. 2015; 28(4):315-22. [DOI:10.1590/1982-0194201500054]
- Wang W, Lau Y, Loo A, Chow A, Thompson DR. Medication adherence and its associated factors among Chinese community-dwelling older adults with hypertension. Heart & Lung. 2014; 43(4):278-83. [DOI:10.1016/j.hrtlng.2014.05.001] [PMID]
- Elbur AI. Level of adherence to lifestyle changes and medications among male hypertensive patients in two hospitals in Taif; Kingdom of Saudi Arabia. International Journal of Pharmacy and Pharmaceutical Sciences. 2015; 7(4):168-72.
- Haghighi ST, Lamyian M, Granpaye L. Assessment of the level of health literacy among fertile Iranian women with breast cancer. Electronic Physician. 2015; 7(6):1359-64. [PMID] [PMCID]
- Mahmoudi H, Taheri A. [Relation between information literacy and health literacy of students in Ferdowsi university of Mashhad (Persian)]. Human Information Interaction. 2015; 2(2):31-41.
- Izadirad H, Zareban I. [The relationship of health literacy with health status, preventive behaviors and health services utilization in Baluchistan, Iran (Persian)]. Journal of Education and Community Health. 2015; 2(3):43-50. [DOI:10.20286/jech-02036]
- Yokokawa H, Fukuda H, Yuasa M, Sanada H, Hisaoka T, Naito T. Association between health literacy and metabolic syndrome or healthy lifestyle characteristics among community-dwelling Japanese people. Diabetology & Metabolic Syndrome. 2016; 8:30. [DOI:10.1186/s13098-016-0142-8] [PMID] [PMCID]
Article Type : Applicable |
Subject:
General
Received: 2019/07/28 | Accepted: 2019/08/10 | Published: 2019/10/1
Received: 2019/07/28 | Accepted: 2019/08/10 | Published: 2019/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |