Thu, Apr 25, 2024
Volume 29, Issue 1 (1-2019)
JHNM 2019, 29(1): 29-35 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghiasmand M, Moghadamnia M T, Pourshaikhian M, Kazemnezhad Leyli E. Emotional Triggers of Acute Myocardial Infarction. JHNM 2019; 29 (1) :29-35
URL: http://hnmj.gums.ac.ir/article-1-663-en.html
URL: http://hnmj.gums.ac.ir/article-1-663-en.html
1- Critical Care Nursing (MSN.), Guilan Social Security Organization, Rasul-e Akram Hospital, Rasht, Iran.
2- Assistant Professor, Social Determinents of Health Research Center (SDHRC), Department of Nursing (Medical-Surgical), Guilan University of Medical Sciences, Rasht, Iran. , moghadamnia@gums.ac.ir
3- Assistant Professor, Social Determinents of Health Research Center (SDHRC), Department of Nursing (Medical-Surgical), Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Social Determinants of Health Research Center (SDHRC), Department of Bio-Statistics, Guilan University of Medical Sciences, Rasht, Iran.
2- Assistant Professor, Social Determinents of Health Research Center (SDHRC), Department of Nursing (Medical-Surgical), Guilan University of Medical Sciences, Rasht, Iran. , moghadamnia@gums.ac.ir
3- Assistant Professor, Social Determinents of Health Research Center (SDHRC), Department of Nursing (Medical-Surgical), Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Social Determinants of Health Research Center (SDHRC), Department of Bio-Statistics, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 638 kb]
(723 Downloads)
| Abstract (HTML) (4094 Views)
Discussion
This study was conducted with the aim of identifying emotional triggers in patients with acute MI, and the results showed that quarrels, hearing unexpected news and partner bereavement had significant association with acute MI risk. According to results, quarrels doubled the risk of acute MI. Colombo also reported that quarrels at work or at home can increase the risk of developing MI [12]. Hearing unexpected news also doubles the risk of acute MI which is consistent with the findings of Masoumi [20].
This can be due to the release of catecholamines and increased heart rate. The risk of having acute MI was less associated with the loss of a loved one. In the studies of Carey [22] and Mostofsky [29], the effect of bereavement on MI was higher (2 times). The participants in Carey study were 60 to 89 years old, while in Mostofsky study, the subjects ‘ average age was 61.6 years. The reason for this difference may be because of difference in calculation of hazard period. In our study, the hazard period was the first 24 hours before MI onset, while in Mostofsky and Carey studies, the hazard period was one month prior to MI. Despite the high incidence of anger among subjects in this study, it had no significant association with the increase of acute MI risk. Edmondson [13], Strike [18], and Bulkey [30] reported the odds ratio of developing MI after anger as two times. The reason for the different results may be because of non-classification of anger levels and its discrimination with repressed anger. It seems that by categorizing anger episodes, different results can be obtained.
In our study, impaired sleep was not a predictor of acute MI. Clark showed that in women over age 60, disturbed sleep showed a consistently higher risk of long-term acute MI, which is not in agreement with our results [31]. This inconsistency may be due to the fact that the majority of participants in our study was middle-aged, and this age period, sleep disorders are more common. Or maybe it is because of non-classification of sleeping problems, participants’ inappropriate beliefs about sleeplessness, or their inaccurate self-report of impaired sleep duration.
Results of our study indicated that job loss had no significant effect on acute MI development. This result is not in agreement with the results of Gallo [32]. They reported that job loss among workers over 50 years of age had a more than twofold increase in the risk of subsequent MI. In our study, most of the subjects were middle-aged or retired and women were housewives, and the number of exposures to this trigger was very low. Hence, this result cannot be conclusive.
About the trigger of partner bereavement, the risk of having acute MI was low. Mostofsky reported the incidence rate of acute MI onset 21-fold more within first few days of mourning for losing the loved ones in the first six months [19]. Carey reported that mourning can double the MI risk 1 month after the death of the spouse. The risk was also two-fold after three months [22]. The reason for low rate of MI in our study was related to few people exposed to this trigger and short hazard period.
In examining the effect of watching exciting sports matches on TV, no significant relationship was found. However, Borges reported that the incidence of MI increased during the period of FIFA World Cup Football in individuals aged over 35 [21]. Perhaps the reason for this inconsistency is the few people in our study who exposed to this trigger or lack of world cup matches at the time of study. Based on our results, just quarrel and unexpected news can increase two fold the risk of MI, also losing a loved one has a little association with MI.
According to the findings, it is recommended that unexpected news be given to individuals gradually, and since quarrels are the triggers of MI, people should avoid stressful environments. The death of a loved one although had low impact on MI risk. In his regard, relaxation techniques should be taught to at-risk people. It is suggested that emotional triggers be taught to patients with angina pectoris to increase their awareness, thereby reducing the incidence of MI in them. One of the limitations of this study was failure to remember the correct time of hazard and control periods by the patients.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by Ethics Committee of Guilan University of Medical Sciences (code: IR.GUMS.REC.1394.218).
Funding
This research was approved by Research Center on Social Determinants on Health Research Center (SDHRC) of Guilan University of Medical Sciences and extracted from a master thesis of Maryam Ghiasmand, department of medical surgical nursing of Guilan University of Medical Sciences (registration number: 922349).
Authors contributions
The authors contributions is as follows: Conceptualization: Mohammad Taghi Moghadamnia; Methodology: All authors; Investigation: Maryam Ghiasmand and Mohammad Taghi Moghadamnia; Writing original draft: All authors; Writing-review & editing: Majid Pourshaikhian and Mohammad Taghi Moghadamnia; Funding acquisition: All authors; and Resources: All authors; Supervision: Mohammad Taghi Moghadamnia.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Professors, authorities and personnel of Dr. Heshmat Medical Center and Rasul-e Akram Hospital in Rasht.
References
Full-Text: (852 Views)
Introduction
Cardiovascular diseases are a serious threat to human community [1]. About one-third of annual deaths in the United States occur due to cardiovascular diseases, as one heart attack occurs every 34 seconds [2], and most deaths from heart attacks occur in people aged 45-65 years [3]. About 70-80% of heart attacks occur outside the hospital, where 50-65% of the cases had no history of heart problem [4]. The World Health Organization (WHO) has reported that the prevalence of cardiovascular diseases is on the rise and is expected to reach 46.4% by 2020 [5]. The number of patients with cardiovascular problems in Rasht, Iran was 7639 in 2008, and reached 8485 in 2009 [6].
One of the most important cardiovascular diseases is coronary heart disease or Myocardial Infarction (MI) [7]. There are two types of factors contributing in the MI occurrence. The first is chronic risk factors that are further categorized as non-modifiable (e.g. gender, age, race, family history), and modifiable risk factors (e.g. high cholesterol, obesity, physical inactivity, diabetes, smoking, stress and alcohol) [8-11]. The second is acute risk factors which are called “triggers” and received less attention in scientific research [12]. They are actually external stimuli that trigger the onset of internal mechanisms such as biomechanical, prothrombotic and vasoconstrictive ones and lead to sclerotic plaque rupture, acute MI, or other coronary syndromes [8]. These external triggers can make pathological changes and there is a direct relationship between exposure to these triggers and the onset of the disease [12].
Acute triggers are classified into four categories: emotional, environmental, physical and chemical [13-18]. Among these, emotional triggers can cause MI by affecting the emotional stressors such as anger and anxiety, depression [12, 13, 19], earthquake, war [18], work-related stress [17], unexpected news [20], and watching sport games [21]. Emotional triggers also reduce sleep, appetite and rest and increase cortisol levels and are associated with cardiovascular diseases [22]. This means that they increase the sympathetic activity, increase the vascular resistance and cause disturbances in the vulnerable coronary plaque, and stimulate inflammation and prothrombotic responses. They also increase heart rate, hypertension, cardiac contractions and endothelial dysfunction [4, 23].
In examining the acute MI triggers, the time period for developing a disease, “hazard period”, is important. Hazard period ranges from a few minutes to 24 hours before the onset of MI [18]. At this period, a disease can occur which is immediately before the onset of symptoms [24]. The hazard period of a trigger is compared to other time periods such as “control period”. The control period is actually the period when the symptoms has not yet observed, and is for examining the trigger and comparing it with the previous weeks before the onset of MI or even up to past 12 months [24].
Regarding the high prevalence of acute MI in society and its implications, and because of the limited studies on emotional triggers, it is necessary to study them for health promotion. Colombo reported that the incidence of cardiovascular diseases and its mortality rate increased by 35% in the first week of 1994 earthquake in California [12]. In another study with 10 years of follow-up, it was shown that some potential levels of anger and anxiety are associated with a prolonged increase in MI and other cardiovascular diseases [25].
Results have also indicated an association between sleep disorders and risk of MI [26], and between partner bereavement and acute MI [22]. Therefore, with appropriate training programs, steps can be taken to raise awareness of at-risk people for acute MI. Appropriate pathological understanding of the process of coronary heart disease and clinical therapies allows the nurses to anticipate an intervention program [10]. Since the symptoms of MI are sudden and can cause disability, understanding the disease process can delay its onset. On the other hand, the issue of triggers and the effect of emotional triggers on the onset of acute MI is unknown. In this regard, the purpose of this study is to identify the emotional triggers of acute MI for the awareness of at-risk people or preventing its onset.
Materials and Methods
This was a case cross-over [27] and the sample size (n=269) was estimated based on results of Colombo study [12] (OR=4.3), Harrison Internal Medicine data on MI patients [9], number of American people aged 50 to 80 years according to American census [28], 95% confidence interval, 80% test power, and P value less than 0.05. We used the convenience sampling method which started from September 2015 to February 2016 for 5 months. Emotional triggers in these patients with MI were anger, sleep disorders, quarrels, unexpected news, watching sport games, job loss, and partner bereavement at the hazard period. These triggers were compared with the control period and analyzed, i.e. each patient was her own control during the period before the MI. The first 24 hours before MI onset was considered as the hazard period [12, 15].
To examine the effects of emotional triggers, based on their nature and effects, three control periods were set. In this regard, the effects of anger, impaired sleep, quarrels, hearing unexpected news, and watching sport games were examined in 1, 2, and 5-day control periods; while for measuring the effect of job loss, the control periods were 1 week before, 2 weeks before, and more than 4 weeks period before MI onset; and the effect of partner bereavement was assessed 1 month, 1-6 months, and 6-12 months before the MI onset [13, 19].
The inclusion criteria were as follows: diagnosis of acute MI according to the patient’s therapist, changes in the ECG and cardiac enzymes based on the patient’s records, having age above 18 years, no cognitive impairment or anxiety and mental disorders based on the patient’s records, willingness to participate in the study, having passed at least 24 hours from the admission, and having a stable condition. Based on these criteria and using convenience sampling method, 275 patients were entered into the study. Of them, 6 patients were excluded from the study (5 were not interested to participate, and one due to misdiagnosis). Then, the final sample size was 269.
The data collection tool was a researcher-designed questionnaire with 20 questions. The first 13 questions collected demographic characteristics of the patients such as age, gender, marital status, income, education, history of diabetes, hypertension, overweight based on BMI>25; as well as history of alcohol, tobacco, or opium use; history of tea and coffee consumption; and history of heart attack. The next 7 questions assessed emotional triggers (anger, insomnia, quarrel, unexpected news, job loss, partner bereavement, watching exciting shows), estimated hazard period and control period. The measurement criterion was the patient’s exposure or non-exposure to the triggers. The mean and standard deviations of the triggers are based on the time of hazard period.
The time unit for hazard period was hour (hours each subject exposed to the triggers during the last 24 hours and hours before the onset of acute MI) and for control period, it was day, week or month which was reported by the patients at the times of exposure or non-exposure to the triggers. The content validity method was used to determine the validity of the questionnaire, so it was sent to 10 Nursing Faculty members for evaluation. According to the values of the lawshe table, its validity was reported 0.96 which is acceptable. For testing its reliability, test-retest technique was applied. The Kappa coefficient for all demographic variables and questions related to the emotional triggers was equal to 1, indicating the agreement between raters (patients).
The study data were collected by the presence of the researcher at the study location after obtaining the informed consent from the patients. The researcher attended in randomly different shifts of morning, evening, and night on certain days of the week. The questionnaires were completed by the researcher through the interview with the patients. Descriptive statistics were used to describe the data. Cochran test was used to assess significant differences of each trigger in four periods including hazard period and three control periods. Generalized Estimating Equations (GEE) method of logistic regression analysis was used to determine the variables associated with the onset of acute MI. All data were analyzed in SPSS V. 21. The significance level was set at P<0.05.
Results
The Mean±SD age of the participants was 60.3±12.2 years. Most cases of acute MI were observed among married men. The average income of the subjects was $ 800 a month. In terms of education, 38.3% of the study patients were illiterate; 24.9% had primary education; 13% intermediate education; 15.6% high school diploma; and 8.2% academic education. In terms of underlying diseases, 36.4% had a history of diabetes; 43.9% a history of hypertension; 59.5% had BMI above 25; 37.5% a history of smoking; 8.2% a history of alcohol use; 19.3% a history of drug addiction; 50.2% a history of tea consumption more than three cups per day; and 16.4% a history of stroke.
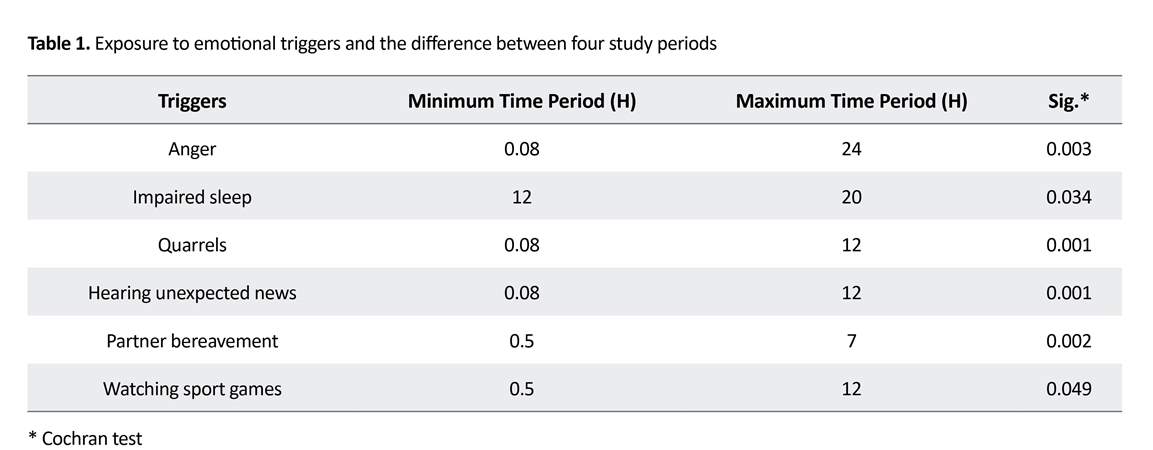
There is a significant difference between MI patients exposed to the triggers of anger, impaired sleep, quarrels, hearing unexpected news, partner bereavement, and watching sport games in four study periods (one hazard period and three control periods) based on Cochran test. In addition, there was a difference between patients with far time period versus people with near time period exposure (Table 1). Results also reported that before acute MI onset 32% of the subjects had exposure to anger (4.99±5.50 h); 36.8% had sleep disorders (13.1±2.4 h); 17.1% exposed to quarrels (4.71±4.85 h) ; 21.6% to unexpected (bad or good) news (5.78±5.01 h); 1.5% to the death of a loved one (1.9±2.9 h); and 3% by watching sport games (5.17±4.80 h).
Cardiovascular diseases are a serious threat to human community [1]. About one-third of annual deaths in the United States occur due to cardiovascular diseases, as one heart attack occurs every 34 seconds [2], and most deaths from heart attacks occur in people aged 45-65 years [3]. About 70-80% of heart attacks occur outside the hospital, where 50-65% of the cases had no history of heart problem [4]. The World Health Organization (WHO) has reported that the prevalence of cardiovascular diseases is on the rise and is expected to reach 46.4% by 2020 [5]. The number of patients with cardiovascular problems in Rasht, Iran was 7639 in 2008, and reached 8485 in 2009 [6].
One of the most important cardiovascular diseases is coronary heart disease or Myocardial Infarction (MI) [7]. There are two types of factors contributing in the MI occurrence. The first is chronic risk factors that are further categorized as non-modifiable (e.g. gender, age, race, family history), and modifiable risk factors (e.g. high cholesterol, obesity, physical inactivity, diabetes, smoking, stress and alcohol) [8-11]. The second is acute risk factors which are called “triggers” and received less attention in scientific research [12]. They are actually external stimuli that trigger the onset of internal mechanisms such as biomechanical, prothrombotic and vasoconstrictive ones and lead to sclerotic plaque rupture, acute MI, or other coronary syndromes [8]. These external triggers can make pathological changes and there is a direct relationship between exposure to these triggers and the onset of the disease [12].
Acute triggers are classified into four categories: emotional, environmental, physical and chemical [13-18]. Among these, emotional triggers can cause MI by affecting the emotional stressors such as anger and anxiety, depression [12, 13, 19], earthquake, war [18], work-related stress [17], unexpected news [20], and watching sport games [21]. Emotional triggers also reduce sleep, appetite and rest and increase cortisol levels and are associated with cardiovascular diseases [22]. This means that they increase the sympathetic activity, increase the vascular resistance and cause disturbances in the vulnerable coronary plaque, and stimulate inflammation and prothrombotic responses. They also increase heart rate, hypertension, cardiac contractions and endothelial dysfunction [4, 23].
In examining the acute MI triggers, the time period for developing a disease, “hazard period”, is important. Hazard period ranges from a few minutes to 24 hours before the onset of MI [18]. At this period, a disease can occur which is immediately before the onset of symptoms [24]. The hazard period of a trigger is compared to other time periods such as “control period”. The control period is actually the period when the symptoms has not yet observed, and is for examining the trigger and comparing it with the previous weeks before the onset of MI or even up to past 12 months [24].
Regarding the high prevalence of acute MI in society and its implications, and because of the limited studies on emotional triggers, it is necessary to study them for health promotion. Colombo reported that the incidence of cardiovascular diseases and its mortality rate increased by 35% in the first week of 1994 earthquake in California [12]. In another study with 10 years of follow-up, it was shown that some potential levels of anger and anxiety are associated with a prolonged increase in MI and other cardiovascular diseases [25].
Results have also indicated an association between sleep disorders and risk of MI [26], and between partner bereavement and acute MI [22]. Therefore, with appropriate training programs, steps can be taken to raise awareness of at-risk people for acute MI. Appropriate pathological understanding of the process of coronary heart disease and clinical therapies allows the nurses to anticipate an intervention program [10]. Since the symptoms of MI are sudden and can cause disability, understanding the disease process can delay its onset. On the other hand, the issue of triggers and the effect of emotional triggers on the onset of acute MI is unknown. In this regard, the purpose of this study is to identify the emotional triggers of acute MI for the awareness of at-risk people or preventing its onset.
Materials and Methods
This was a case cross-over [27] and the sample size (n=269) was estimated based on results of Colombo study [12] (OR=4.3), Harrison Internal Medicine data on MI patients [9], number of American people aged 50 to 80 years according to American census [28], 95% confidence interval, 80% test power, and P value less than 0.05. We used the convenience sampling method which started from September 2015 to February 2016 for 5 months. Emotional triggers in these patients with MI were anger, sleep disorders, quarrels, unexpected news, watching sport games, job loss, and partner bereavement at the hazard period. These triggers were compared with the control period and analyzed, i.e. each patient was her own control during the period before the MI. The first 24 hours before MI onset was considered as the hazard period [12, 15].
To examine the effects of emotional triggers, based on their nature and effects, three control periods were set. In this regard, the effects of anger, impaired sleep, quarrels, hearing unexpected news, and watching sport games were examined in 1, 2, and 5-day control periods; while for measuring the effect of job loss, the control periods were 1 week before, 2 weeks before, and more than 4 weeks period before MI onset; and the effect of partner bereavement was assessed 1 month, 1-6 months, and 6-12 months before the MI onset [13, 19].
The inclusion criteria were as follows: diagnosis of acute MI according to the patient’s therapist, changes in the ECG and cardiac enzymes based on the patient’s records, having age above 18 years, no cognitive impairment or anxiety and mental disorders based on the patient’s records, willingness to participate in the study, having passed at least 24 hours from the admission, and having a stable condition. Based on these criteria and using convenience sampling method, 275 patients were entered into the study. Of them, 6 patients were excluded from the study (5 were not interested to participate, and one due to misdiagnosis). Then, the final sample size was 269.
The data collection tool was a researcher-designed questionnaire with 20 questions. The first 13 questions collected demographic characteristics of the patients such as age, gender, marital status, income, education, history of diabetes, hypertension, overweight based on BMI>25; as well as history of alcohol, tobacco, or opium use; history of tea and coffee consumption; and history of heart attack. The next 7 questions assessed emotional triggers (anger, insomnia, quarrel, unexpected news, job loss, partner bereavement, watching exciting shows), estimated hazard period and control period. The measurement criterion was the patient’s exposure or non-exposure to the triggers. The mean and standard deviations of the triggers are based on the time of hazard period.
The time unit for hazard period was hour (hours each subject exposed to the triggers during the last 24 hours and hours before the onset of acute MI) and for control period, it was day, week or month which was reported by the patients at the times of exposure or non-exposure to the triggers. The content validity method was used to determine the validity of the questionnaire, so it was sent to 10 Nursing Faculty members for evaluation. According to the values of the lawshe table, its validity was reported 0.96 which is acceptable. For testing its reliability, test-retest technique was applied. The Kappa coefficient for all demographic variables and questions related to the emotional triggers was equal to 1, indicating the agreement between raters (patients).
The study data were collected by the presence of the researcher at the study location after obtaining the informed consent from the patients. The researcher attended in randomly different shifts of morning, evening, and night on certain days of the week. The questionnaires were completed by the researcher through the interview with the patients. Descriptive statistics were used to describe the data. Cochran test was used to assess significant differences of each trigger in four periods including hazard period and three control periods. Generalized Estimating Equations (GEE) method of logistic regression analysis was used to determine the variables associated with the onset of acute MI. All data were analyzed in SPSS V. 21. The significance level was set at P<0.05.
Results
The Mean±SD age of the participants was 60.3±12.2 years. Most cases of acute MI were observed among married men. The average income of the subjects was $ 800 a month. In terms of education, 38.3% of the study patients were illiterate; 24.9% had primary education; 13% intermediate education; 15.6% high school diploma; and 8.2% academic education. In terms of underlying diseases, 36.4% had a history of diabetes; 43.9% a history of hypertension; 59.5% had BMI above 25; 37.5% a history of smoking; 8.2% a history of alcohol use; 19.3% a history of drug addiction; 50.2% a history of tea consumption more than three cups per day; and 16.4% a history of stroke.
There is a significant difference between MI patients exposed to the triggers of anger, impaired sleep, quarrels, hearing unexpected news, partner bereavement, and watching sport games in four study periods (one hazard period and three control periods) based on Cochran test. In addition, there was a difference between patients with far time period versus people with near time period exposure (Table 1). Results also reported that before acute MI onset 32% of the subjects had exposure to anger (4.99±5.50 h); 36.8% had sleep disorders (13.1±2.4 h); 17.1% exposed to quarrels (4.71±4.85 h) ; 21.6% to unexpected (bad or good) news (5.78±5.01 h); 1.5% to the death of a loved one (1.9±2.9 h); and 3% by watching sport games (5.17±4.80 h).
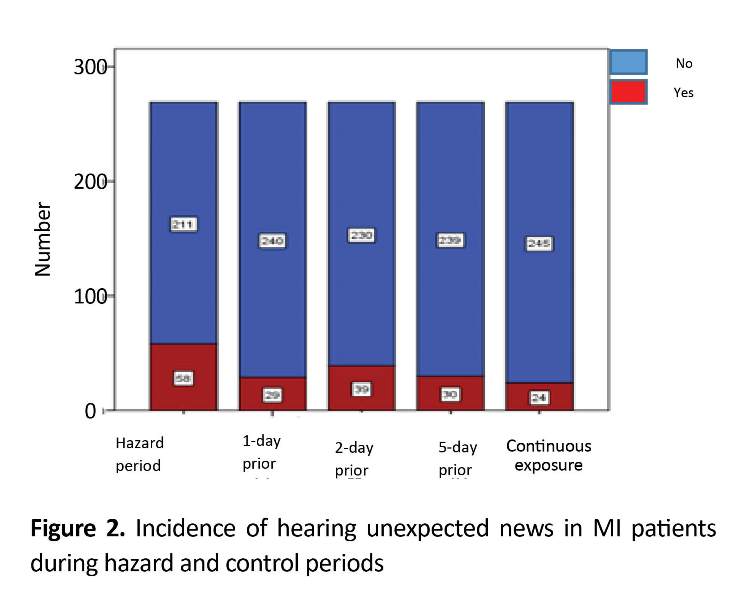
GEE model results showed that quarrel (95% CI 1.19-3.38, OR=2.01, P=0.008) and hearing unexpected news (95% CI 1.35-3.53, OR=2.19, P=0.001) prior to acute MI onset doubled the risk of acute MI. The death of loves ones before acute MI onset showed very low predictability (95%CI 0.08-0.84, OR=0.27, P=0.024). Despite the high incidence of anger and impaired sleep among subjects, these triggers could not predict acute MI risk. Job loss and watching sport games also had no significant association with the increase of acute MI risk (Table 2). Incidence of exposure to quarrels and unexpected news during hazard and control periods are illustrated in Figure 1 and 2.
Discussion
This study was conducted with the aim of identifying emotional triggers in patients with acute MI, and the results showed that quarrels, hearing unexpected news and partner bereavement had significant association with acute MI risk. According to results, quarrels doubled the risk of acute MI. Colombo also reported that quarrels at work or at home can increase the risk of developing MI [12]. Hearing unexpected news also doubles the risk of acute MI which is consistent with the findings of Masoumi [20].
This can be due to the release of catecholamines and increased heart rate. The risk of having acute MI was less associated with the loss of a loved one. In the studies of Carey [22] and Mostofsky [29], the effect of bereavement on MI was higher (2 times). The participants in Carey study were 60 to 89 years old, while in Mostofsky study, the subjects ‘ average age was 61.6 years. The reason for this difference may be because of difference in calculation of hazard period. In our study, the hazard period was the first 24 hours before MI onset, while in Mostofsky and Carey studies, the hazard period was one month prior to MI. Despite the high incidence of anger among subjects in this study, it had no significant association with the increase of acute MI risk. Edmondson [13], Strike [18], and Bulkey [30] reported the odds ratio of developing MI after anger as two times. The reason for the different results may be because of non-classification of anger levels and its discrimination with repressed anger. It seems that by categorizing anger episodes, different results can be obtained.
In our study, impaired sleep was not a predictor of acute MI. Clark showed that in women over age 60, disturbed sleep showed a consistently higher risk of long-term acute MI, which is not in agreement with our results [31]. This inconsistency may be due to the fact that the majority of participants in our study was middle-aged, and this age period, sleep disorders are more common. Or maybe it is because of non-classification of sleeping problems, participants’ inappropriate beliefs about sleeplessness, or their inaccurate self-report of impaired sleep duration.
Results of our study indicated that job loss had no significant effect on acute MI development. This result is not in agreement with the results of Gallo [32]. They reported that job loss among workers over 50 years of age had a more than twofold increase in the risk of subsequent MI. In our study, most of the subjects were middle-aged or retired and women were housewives, and the number of exposures to this trigger was very low. Hence, this result cannot be conclusive.
About the trigger of partner bereavement, the risk of having acute MI was low. Mostofsky reported the incidence rate of acute MI onset 21-fold more within first few days of mourning for losing the loved ones in the first six months [19]. Carey reported that mourning can double the MI risk 1 month after the death of the spouse. The risk was also two-fold after three months [22]. The reason for low rate of MI in our study was related to few people exposed to this trigger and short hazard period.
In examining the effect of watching exciting sports matches on TV, no significant relationship was found. However, Borges reported that the incidence of MI increased during the period of FIFA World Cup Football in individuals aged over 35 [21]. Perhaps the reason for this inconsistency is the few people in our study who exposed to this trigger or lack of world cup matches at the time of study. Based on our results, just quarrel and unexpected news can increase two fold the risk of MI, also losing a loved one has a little association with MI.
According to the findings, it is recommended that unexpected news be given to individuals gradually, and since quarrels are the triggers of MI, people should avoid stressful environments. The death of a loved one although had low impact on MI risk. In his regard, relaxation techniques should be taught to at-risk people. It is suggested that emotional triggers be taught to patients with angina pectoris to increase their awareness, thereby reducing the incidence of MI in them. One of the limitations of this study was failure to remember the correct time of hazard and control periods by the patients.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by Ethics Committee of Guilan University of Medical Sciences (code: IR.GUMS.REC.1394.218).
Funding
This research was approved by Research Center on Social Determinants on Health Research Center (SDHRC) of Guilan University of Medical Sciences and extracted from a master thesis of Maryam Ghiasmand, department of medical surgical nursing of Guilan University of Medical Sciences (registration number: 922349).
Authors contributions
The authors contributions is as follows: Conceptualization: Mohammad Taghi Moghadamnia; Methodology: All authors; Investigation: Maryam Ghiasmand and Mohammad Taghi Moghadamnia; Writing original draft: All authors; Writing-review & editing: Majid Pourshaikhian and Mohammad Taghi Moghadamnia; Funding acquisition: All authors; and Resources: All authors; Supervision: Mohammad Taghi Moghadamnia.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Professors, authorities and personnel of Dr. Heshmat Medical Center and Rasul-e Akram Hospital in Rasht.
References
- Nikpazhoh A. [Guide line for prevention and treatment Cardio Vascular disease (Persian)]. Tehran: Institute of Contemporary Iranian prevention and Health Promotion; 2010.
- Schwartz BG, French WJ, Mayeda GS, Burstein S, Economides C, Bhandari AK, et al. Emotional stressors trigger cardiovascular events. International Journal of Clinical Practice. 2012; 66(7):631-9. [DOI:10.1111/j.1742-1241.2012.02920.x] [PMID]
- Gaziano TH, Prabhakaran D, Gaziano M. Global burden of cardiovascular disease. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, editors. Braunwald heart disease: A textbook of cardiovascular Medicine. Amsterdam: Elsevier; 2015.
- Bersten A. Oh's Intensive care manual. Amsterdam: Elsevier; 2013.
- Vahedian Azimi A, Sadeghi M, Movafegh A, Sorouri Zanjani R, Hasani D, Salehmoghaddam AR, et al. [The relationship between perceived stress and the top five heart disease characteristics in patients with myocardial infarction (Persian)]. Journal of Zanjan University of Medical Sciences. 2012; 20(78):100-12.
- Moaddab F. [Survey of predictive factors of self-care in patients’ whit Heart Failure that referred to Dr. Heshmat Hospital of Rasht 1392 Guilan university of medical science (Persian)] [MSc. thesis]. Tehran: Shahid Beheshti University of Medical Sciences; 2013.
- Rafati M, Ghotbi M, Ahmadnia H. [Principle of prevention and care of disease, set of instruction (Persian)]. Tehran: Sepid Barg; 2008.
- Čulić V. Acute risk factors for myocardial infarction. International Journal of Cardiology. 2007; 117(2):260-9. [DOI:10.1016/j.ijcard.2006.05.011] [PMID]
- Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrisons Manual of Medicine. New York: McGraw-Hill Education; 2013.
- Urden LD, Stacy KM, Lough ME. Critical care nursing: Diagnosis and management. Maryland Heights: Mosby; 2013.
- Marx J, Walls R, Hockberger R. Rosen’s emergency medicine-concepts and clinical practice. Amsterdam: Elsevier; 2013.
- Colombo A, Proietti R, Culic V, Lipovetzky N, Viecca M, Danna P. Triggers of acute myocardial infraction: Neglected piece of the puzzle. Italian Federation of Cardiology. 2014; 15(1):1-7. [DOI: 10.2459/JCM.0b013e3283641351 ] [PMID]
- Edmondson D, Newman JD, Whang W, Davidson KW. Emotional triggers in myocardial infarction: Do they matter? European Heart Journal. 2012; 34(4):300-6. [DOI:10.1093/eurheartj/ehs398] [PMID] [PMCID]
- Glozier N, Tofler GH, Colquhoun DM, Bunker SJ, Clarke DM, Hare DL, et al. Psychosocial risk factors for coronary heart disease. Medical Journal of Australia. 2013; 199(3):179-80. [DOI:10.5694/mja13.10440] [PMID]
- Lindau ST, Abramsohn EM, Bueno H, D’onofrio G, Lichtman JH, Lorenze NP, et al. Sexual activity and counseling in the first month after acute myocardial infarction among younger adults in the United States and Spain: A prospective, observational study. Circulation. 2014; 130(25):2302-9. [DOI:10.1161/CIRCULATIONAHA.114.012709] [PMID] [PMCID]
- Lipovetzky N, Hod H, Roth A, Kishon Y, Sclarovsky S, Green MS. Heavy meals as a trigger for a first event of the acute coronary syndrome: A case-crossover study. Israel Medical Association Journal. 2004; 6(12):728-31. [PMID]
- Mittleman MA, Mostofsky E. Physical, psychological and chemical triggers of acute cardiovascular events: Preventive strategies. Circulation. 2011; 124(3):346-54. [DOI:10.1161/CIRCULATIONAHA.110.968776] [PMID] [PMCID]
- Strike PC, Steptoe A. Behavioral and emotional triggers of acute coronary syndromes: A systematic review and critique. Psychosomatic Medicine. 2005; 67(2):179-86. [DOI:10.1097/01.psy.0000155663.93160.d2] [PMID]
- Mostofsky E, Maclure M, Sherwood j, Mittleman M. Risk of acute myocardial infraction after the death of a significant persons in ons life:the determinants of myocardial infraction onest study. American Heart Association. 2012; 125(3):491-6. [DOI: 10.1161/CIRCULATIONAHA.111.061770] [PMID] [PMCID]
- Masoomi M, Zare J, Kahnooj M, Mirzazadeh A, Sheikhvatan M. Sex differences in potential daily triggers of the onset of acute myocardial infarction: A case-crossover analysis among an Iranian population. Journal of Cardiovascular Medicine. 2010; 11(10):723-6. [DOI:10.2459/JCM.0b013e32833892da]
- Borges D, Monterio R, Schmidt A, Filho A. [Worde soccer as a triggers of cardiovascular evrnt (Portuguese)]. Sociedade Brasileira de Cardiologia. 2013; 100(6):546-52. [DOI:10.5935/abc.20130105] [PMID]
- Carey I, Shah S, Dewild s, Harris T, Victor ch, Cook D. Increased risk of acute cardiovascular event s after partner breavment amatched cohort study. JAMA Internal Medicine. 2014; 174(4):598-605.
- Maiese A, Gitto L, dell’Aquila M, Serinelli S, Bolino G. Association between the intake of cocaine and a strong physical and emotional stress: A case report of a sudden death. European Journal of Forensic Sciences. 2016; 3(1):35-7. [DOI:10.5455/ejfs.189757]
- Dahabreh IJ, Paulus JK. Association of episodic physical and sexual activity with triggering of acute cardiac events: Systematic review and meta-analysis. The Latest Medical Research, Reviews, and Guidelines. 2011; 305(12):1225-33.
- Smeijers L, Mostofsky E, Tofler GH, Muller JE, Kop WJ, Mittleman MA. Association between high levels of physical exertion, anger, and anxiety immediately before myocardial infarction with mortality during 10-year follow-up. Journal of the American College of Cardiology. 2015; 66(9):1083-4. [DOI:10.1016/j.jacc.2015.06.1317] [PMID]
- Wang X, Liu X, Song Q, Wu S. Sleep duration and risk of myocardial infarction and all-cause death in a Chinese population: The kailuan study. Sleep Medicine. 2016; 19:13-6. [DOI:10.1016/j.sleep.2015.09.027] [PMID]
- Ghorbani M, Yonesian M. [Survey methodology case-crossover study in epidemiology (Persian)]. Iranian Journal of Epidemiology. 2008; 1(1):59-69.
- Census.gov. US population. [Internet]. 2015 [Accessed 2015 April 19]. Available from: http://www.census.gov/popclock/
- Mostofsky E, Penner E, Mittleman M. Outbursts of anger as a trigger of acute cardiovascular events: A systematic review and meta-analysis. European Heart Journal. 2014; 35(21):1404-10. [DOI:10.1093/eurheartj/ehu033] [PMID] [PMCID]
- Bulkey Th, Hoo SS, Fethney J. Triggers of acute coronary occlusion by episodes of anger. Europian Heart Journal. 2015; 4(6):493-8
- Clark A, Lange T, Hallqvist J. Sleep impairment and prognosis of acute myocardial infarction: A prospective cohort study. Sleep. 2014; 37(5):851-8. [DOI:10.5665/sleep.3646] [PMID] [PMCID]
- Gallo WT, Teng HM, Falba TA, Kasl SV, Krumholz HM, Bradley EH. The impact of late career job loss on myocardial infarction and stroke: A 10 year follow up using the health and retirement survey. Occupational and Environmental Medicine. 2006; 63(10):683-7. [DOI:10.1136/oem.2006.026823] [PMID] [PMCID]
Article Type : Applicable |
Subject:
Special
Received: 2018/03/15 | Accepted: 2018/09/28 | Published: 2019/01/1
Received: 2018/03/15 | Accepted: 2018/09/28 | Published: 2019/01/1
References
1. Nikpazhoh A. [Guide line for prevention and treatment Cardio Vascular disease (Persian)]. Tehran: Institute of Contemporary Iranian prevention and Health Promotion; 2010.
2. Schwartz BG, French WJ, Mayeda GS, Burstein S, Economides C, Bhandari AK, et al. Emotional stressors trigger cardiovascular events. International Journal of Clinical Practice. 2012; 66(7):631-9. [DOI:10.1111/j.1742-1241.2012.02920.x] [PMID] [DOI:10.1111/j.1742-1241.2012.02920.x]
3. Gaziano TH, Prabhakaran D, Gaziano M. Global burden of cardiovascular disease. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, editors. Braunwald heart disease: A textbook of cardiovascular Medicine. Amsterdam: Elsevier; 2015.
4. Bersten A. Oh's Intensive care manual. Amsterdam: Elsevier; 2013.
5. Vahedian Azimi A, Sadeghi M, Movafegh A, Sorouri Zanjani R, Hasani D, Salehmoghaddam AR, et al. [The relationship between perceived stress and the top five heart disease characteristics in patients with myocardial infarction (Persian)]. Journal of Zanjan University of Medical Sciences. 2012; 20(78):100-12.
6. Moaddab F. [Survey of predictive factors of self-care in patients' whit Heart Failure that referred to Dr. Heshmat Hospital of Rasht 1392 Guilan university of medical science (Persian)] [MSc. thesis]. Tehran: Shahid Beheshti University of Medical Sciences; 2013.
7. Rafati M, Ghotbi M, Ahmadnia H. [Principle of prevention and care of disease, set of instruction (Persian)]. Tehran: Sepid Barg; 2008.
8. Čulić V. Acute risk factors for myocardial infarction. International Journal of Cardiology. 2007; 117(2):260-9. [DOI:10.1016/j.ijcard.2006.05.011] [PMID] [DOI:10.1016/j.ijcard.2006.05.011]
9. Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrisons Manual of Medicine. New York: McGraw-Hill Education; 2013.
10. Urden LD, Stacy KM, Lough ME. Critical care nursing: Diagnosis and management. Maryland Heights: Mosby; 2013. [PMID]
11. Marx J, Walls R, Hockberger R. Rosen's emergency medicine-concepts and clinical practice. Amsterdam: Elsevier; 2013.
12. Colombo A, Proietti R, Culic V, Lipovetzky N, Viecca M, Danna P. Triggers of acute myocardial infraction: Neglected piece of the puzzle. Italian Federation of Cardiology. 2014; 15(1):1-7. [DOI: 10.2459/JCM.0b013e3283641351 ] [PMID] [DOI:10.2459/JCM.0b013e3283641351]
13. Edmondson D, Newman JD, Whang W, Davidson KW. Emotional triggers in myocardial infarction: Do they matter? European Heart Journal. 2012; 34(4):300-6. [DOI:10.1093/eurheartj/ehs398] [PMID] [PMCID] [DOI:10.1093/eurheartj/ehs398]
14. Glozier N, Tofler GH, Colquhoun DM, Bunker SJ, Clarke DM, Hare DL, et al. Psychosocial risk factors for coronary heart disease. Medical Journal of Australia. 2013; 199(3):179-80. [DOI:10.5694/mja13.10440] [PMID] [DOI:10.5694/mja13.10440]
15. Lindau ST, Abramsohn EM, Bueno H, D'onofrio G, Lichtman JH, Lorenze NP, et al. Sexual activity and counseling in the first month after acute myocardial infarction among younger adults in the United States and Spain: A prospective, observational study. Circulation. 2014; 130(25):2302-9. [DOI:10.1161/CIRCULATIONAHA.114.012709] [PMID] [PMCID] [DOI:10.1161/CIRCULATIONAHA.114.012709]
16. Lipovetzky N, Hod H, Roth A, Kishon Y, Sclarovsky S, Green MS. Heavy meals as a trigger for a first event of the acute coronary syndrome: A case-crossover study. Israel Medical Association Journal. 2004; 6(12):728-31. [PMID] [PMID]
17. Mittleman MA, Mostofsky E. Physical, psychological and chemical triggers of acute cardiovascular events: Preventive strategies. Circulation. 2011; 124(3):346-54. [DOI:10.1161/CIRCULATIONAHA.110.968776] [PMID] [PMCID] [DOI:10.1161/CIRCULATIONAHA.110.968776]
18. Strike PC, Steptoe A. Behavioral and emotional triggers of acute coronary syndromes: A systematic review and critique. Psychosomatic Medicine. 2005; 67(2):179-86. [DOI:10.1097/01.psy.0000155663.93160.d2] [PMID] [DOI:10.1097/01.psy.0000155663.93160.d2]
19. Mostofsky E, Maclure M, Sherwood j, Mittleman M. Risk of acute myocardial infraction after the death of a significant persons in ons life:the determinants of myocardial infraction onest study. American Heart Association. 2012; 125(3):491-6. [DOI: 10.1161/CIRCULATIONAHA.111.061770] [PMID] [PMCID] [DOI:10.1161/CIRCULATIONAHA.111.061770]
20. Masoomi M, Zare J, Kahnooj M, Mirzazadeh A, Sheikhvatan M. Sex differences in potential daily triggers of the onset of acute myocardial infarction: A case-crossover analysis among an Iranian population. Journal of Cardiovascular Medicine. 2010; 11(10):723-6. [DOI:10.2459/JCM.0b013e32833892da] [DOI:10.2459/JCM.0b013e32833892da]
21. Borges D, Monterio R, Schmidt A, Filho A. [Worde soccer as a triggers of cardiovascular evrnt (Portuguese)]. Sociedade Brasileira de Cardiologia. 2013; 100(6):546-52. [DOI:10.5935/abc.20130105] [PMID] [DOI:10.5935/abc.20130105]
22. Carey I, Shah S, Dewild s, Harris T, Victor ch, Cook D. Increased risk of acute cardiovascular event s after partner breavment amatched cohort study. JAMA Internal Medicine. 2014; 174(4):598-605. [DOI:10.1001/jamainternmed.2013.14558] [PMID]
23. Maiese A, Gitto L, dell'Aquila M, Serinelli S, Bolino G. Association between the intake of cocaine and a strong physical and emotional stress: A case report of a sudden death. European Journal of Forensic Sciences. 2016; 3(1):35-7. [DOI:10.5455/ejfs.189757] [DOI:10.5455/ejfs.189757]
24. Dahabreh IJ, Paulus JK. Association of episodic physical and sexual activity with triggering of acute cardiac events: Systematic review and meta-analysis. The Latest Medical Research, Reviews, and Guidelines. 2011; 305(12):1225-33. [DOI:10.1001/jama.2011.336]
25. Smeijers L, Mostofsky E, Tofler GH, Muller JE, Kop WJ, Mittleman MA. Association between high levels of physical exertion, anger, and anxiety immediately before myocardial infarction with mortality during 10-year follow-up. Journal of the American College of Cardiology. 2015; 66(9):1083-4. [DOI:10.1016/j.jacc.2015.06.1317] [PMID] [DOI:10.1016/j.jacc.2015.06.1317]
26. Wang X, Liu X, Song Q, Wu S. Sleep duration and risk of myocardial infarction and all-cause death in a Chinese population: The kailuan study. Sleep Medicine. 2016; 19:13-6. [DOI:10.1016/j.sleep.2015.09.027] [PMID] [DOI:10.1016/j.sleep.2015.09.027]
27. Ghorbani M, Yonesian M. [Survey methodology case-crossover study in epidemiology (Persian)]. Iranian Journal of Epidemiology. 2008; 1(1):59-69.
28. Census.gov. US population. [Internet]. 2015 [Accessed 2015 April 19]. Available from: http://www.census.gov/popclock/
29. Mostofsky E, Penner E, Mittleman M. Outbursts of anger as a trigger of acute cardiovascular events: A systematic review and meta-analysis. European Heart Journal. 2014; 35(21):1404-10. [DOI:10.1093/eurheartj/ehu033] [PMID] [PMCID] [DOI:10.1093/eurheartj/ehu033]
30. Bulkey Th, Hoo SS, Fethney J. Triggers of acute coronary occlusion by episodes of anger. Europian Heart Journal. 2015; 4(6):493-8
31. Clark A, Lange T, Hallqvist J. Sleep impairment and prognosis of acute myocardial infarction: A prospective cohort study. Sleep. 2014; 37(5):851-8. [DOI:10.5665/sleep.3646] [PMID] [PMCID] [DOI:10.5665/sleep.3646]
32. Gallo WT, Teng HM, Falba TA, Kasl SV, Krumholz HM, Bradley EH. The impact of late career job loss on myocardial infarction and stroke: A 10 year follow up using the health and retirement survey. Occupational and Environmental Medicine. 2006; 63(10):683-7. [DOI:10.1136/oem.2006.026823] [PMID] [PMCID] [DOI:10.1136/oem.2006.026823]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |