Sun, Nov 23, 2025
Volume 35, Issue 4 (9-2025)
JHNM 2025, 35(4): 279-285 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
garaleah E M, Alkhotoba G H A, Alma’aytah N. Prevalence and Risk Factors of Postpartum Depression among Women in Southern Jordan: A Cross-Sectional Study. JHNM 2025; 35 (4) :279-285
URL: http://hnmj.gums.ac.ir/article-1-2448-en.html
URL: http://hnmj.gums.ac.ir/article-1-2448-en.html
1- Maternity and Newborn Health (MSc), Department of Allied Medical Sciences, Karak University College, Al-Balqa Applied University, Karak, Jordan. , Ehoudgaraleah@bau.edu.jo
2- Pediatric Health(MSc), Karak University College, Al-Balqa Applied University, Karak, Jordan.
3- Maternity and Newborn Health (MSc), Department of Allied Medical Sciences, Karak University College, Al-Balqa Applied University, Karak, Jordan.
2- Pediatric Health(MSc), Karak University College, Al-Balqa Applied University, Karak, Jordan.
3- Maternity and Newborn Health (MSc), Department of Allied Medical Sciences, Karak University College, Al-Balqa Applied University, Karak, Jordan.
Full-Text [PDF 452 kb]
(177 Downloads)
| Abstract (HTML) (275 Views)
Full-Text: (87 Views)
Introduction
Postpartum Depression (PPD) is a common mental health disorder affecting 10–20% of women globally, with rates exceeding 30% in some low- and middle-income countries [1, 2]. In Jordan, the prevalence ranges from 22% to 30%, with approximately 45% of cases classified as moderate to severe [3, 4]. PPD negatively impacts maternal well-being, infant development, and family dynamics. Neurological and emotional changes associated with PPD can impair maternal bonding, increasing the risk of emotional, behavioral, and cognitive difficulties in children [4–6]. Several factors are associated with PPD, including unplanned pregnancies, low socioeconomic status, poor social support, and marital stress [7–9]. Adolescent mothers are at greater risk, particularly when experiencing family conflict or financial hardship [10-12]. Additionally, research suggests a potential link between parity and increased risk of PPD. A systematic review reported that women with more than one child were 1.5-2 times more likely to develop PPD symptoms [13, 14], while studies from Japan and Spain found that parity was associated with 30–50% higher rates of depressive symptoms [15, 16].
Despite international findings, the relationship between parity and PPD remains under-investigated in Jordan. Given the country’s unique social and healthcare context, including limited access to mental health services, parity may play a distinct role in shaping maternal mental health outcomes [17, 18]. Therefore, this study aims to examine whether multiparous women in Jordan are at greater risk of developing PPD. The goal is to identify the risk factors associated with PPD among southern Jordanian women. Understanding this relationship is crucial for identifying at-risk groups and informing the development of targeted interventions that promote maternal and infant well-being.
Materials and Methods
This quantitative cross-sectional study was conducted in the southern governorates of Jordan, targeting postpartum women who attended maternal and child health clinics or those accessible through social media platforms, such as Facebook and WhatsApp. A total of 434 women participated in the study from August to December 2023. They were mothers aged 20-45 years, with at least one child, and no reported history of psychological symptoms prior to marriage. Women who reported a history of severe mental illness, inability to complete the questionnaires, or had medical conditions that could confound the results were excluded. The sample size was determined using G*Power software, version 3.1. Based on a medium effect size of 0.3, an alpha value of 0.05, and a test power of 0.80, the required sample size was calculated to be 384. To ensure sufficient data quality and to account for a 13% sample dropout rate, the sample size increased to 434.
Data collection was performed using a structured, self-administered questionnaire that included two sections: a sociodemographic/obstetric form and the Edinburgh Postnatal Depression Scale (EPDS). The sociodemographic/obstetric form surveyed age, parity, educational level, employment status, family income, history of smoking, age at marriage, number of previous pregnancies and abortions, and number of children living with parents. The EPDS is a valid 10-item scale developed by Cox et al. [19], with each item rated on a four-point Likert scale and a total score ranging from 0 to 30. A cut-off point of 13 was used to indicate probable PPD. In this study, the validated Arabic version of EPDS was used. The translation was done by two independent translators and reviewed by a bilingual expert panel specialized in mental health. A pilot test was conducted on 15 Jordanian women (not included in the final sample) to assess clarity and cultural adaptability. The internal consistency of the Arabic EPDS was found to be high (Cronbach’s α coefficient=0.82). Previous studies have confirmed the validity of the Arabic EPDS in other Arab countries [20]. Data collection was conducted in-person (for women attending maternal and child health services) or online (for women reachable through social media platforms).
Statistical analysis was performed in IBM SPSS software, version 29. Descriptive statistics were used to present participants’ characteristics. Categorical variables were expressed as frequency (percentage), while continuous variables were reported as Mean±SD. Independent t-tests and one-way Analysis of Variance (ANOVA) were used to compare the groups based on depression levels. Pearson’s correlation test was used to explore associations between continuous variables. The assumptions of normality were tested using the Shapiro–Wilk test. P<0.05 was considered statistically significant.
Results
The socio-demographic and obstetric characteristics of participants are presented in Table 1.
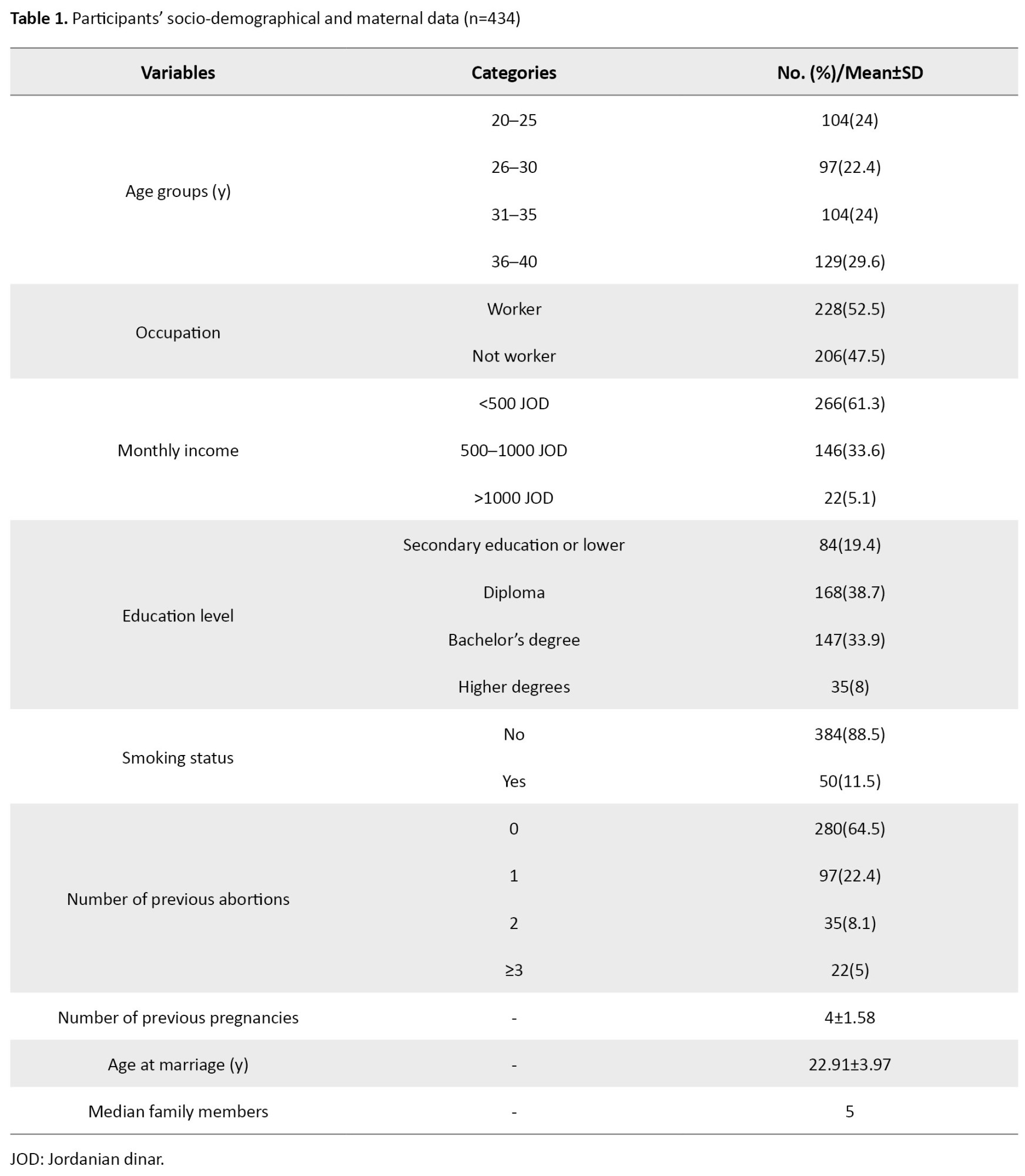
The majority were aged 36–40 years (29.6%), and more than half were employed (52.5%). Most participants reported a monthly income of <500 Jordanian dinar (61.3%), and 38.7% had a diploma. Regarding health behaviors, the majority were non-smokers (88.5%), with no history of abortions (64.5%), and their mean number of previous pregnancies was 4±1.58. Their mean age at marriage was 22.91±3.97 years, and the median family size was 5 (Table 1).
The mean EPDS score was 15.57±4.71. A total of 324 women (74.7%) scored 13 or above, indicating that they were at risk of PPD development, whereas 110 women (25.3%) were not at risk (Table 2).
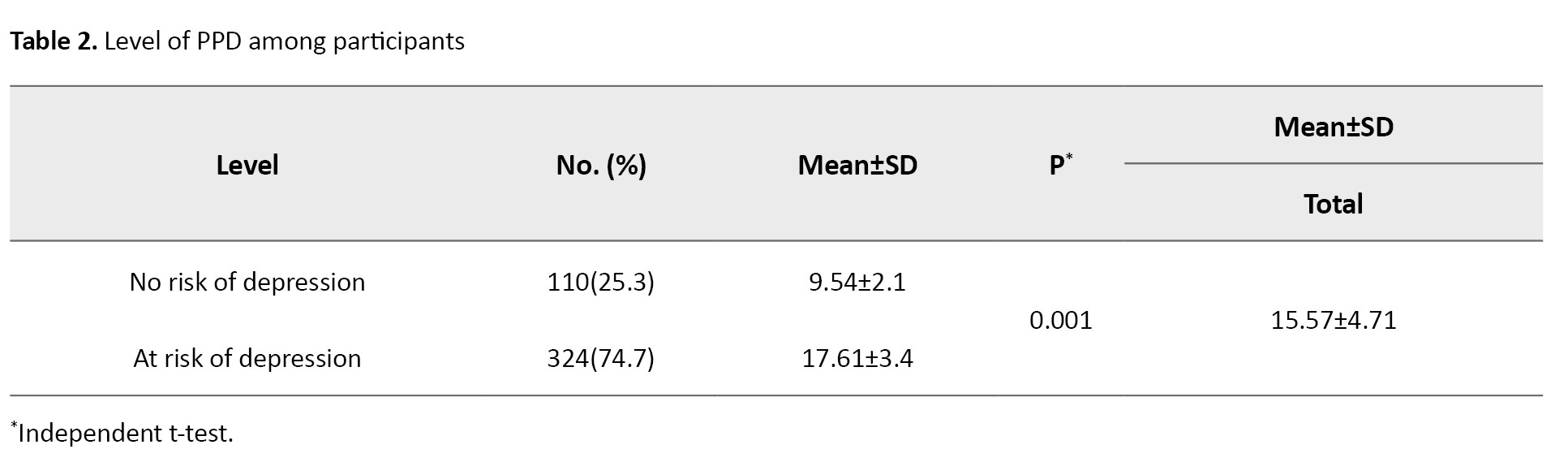
The independent t-test results revealed a statistically significant difference in the EPDS score between the two groups at risk and at no risk of PPD development (P=0.001).
The ANOVA results showed that the EPDS score was significantly different based on educational level (P=0.009), where women with secondary education or lower level had higher scores than those with higher education levels. The EPDS score was not significantly different based on the number of previous abortions, age, occupation, monthly income, or smoking (Table 3).

The results of Pearson’s correlation test for the association of socio-demographic and obstetric variables with the EPDS score are presented in Table 4.
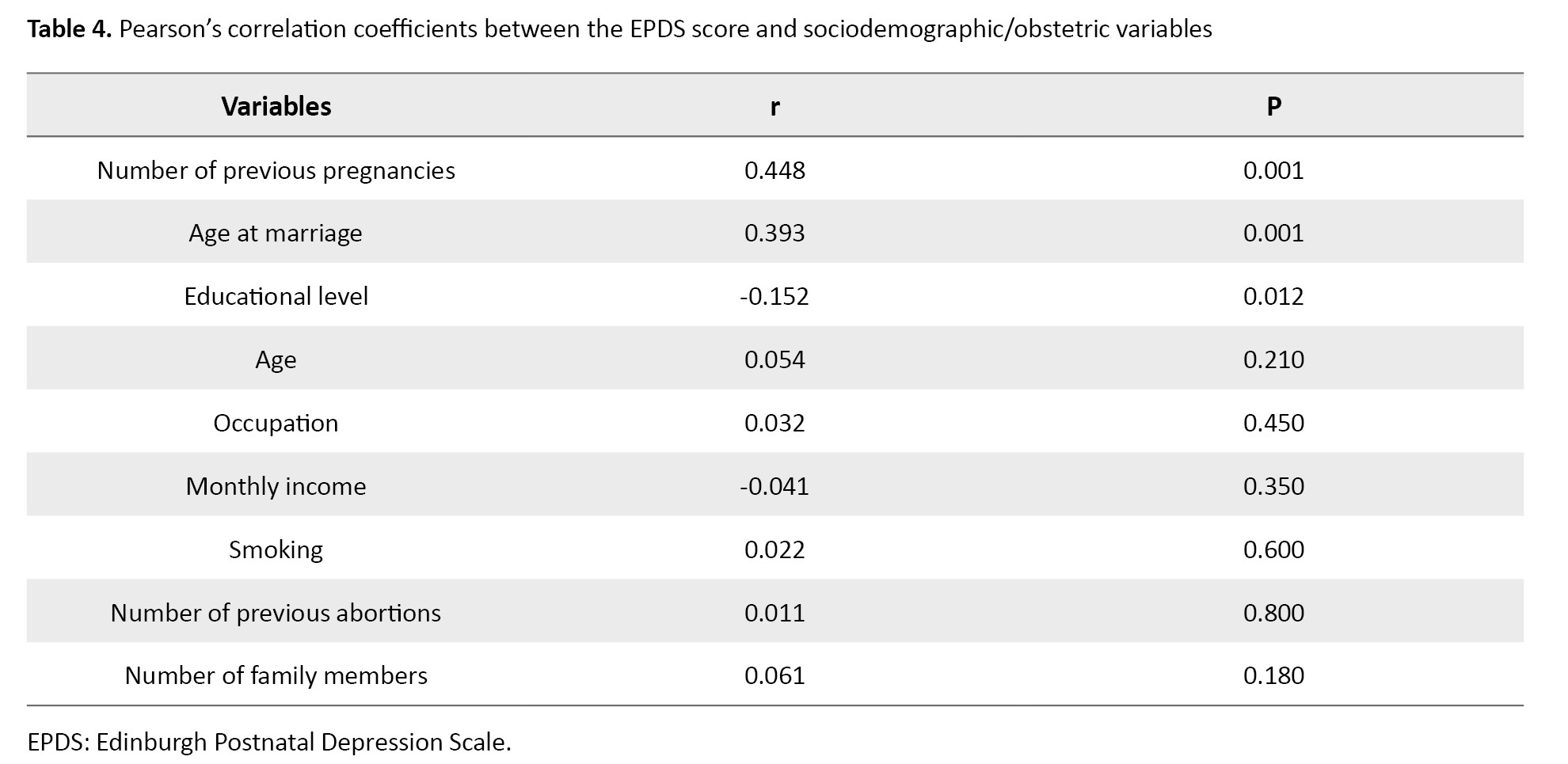
The results revealed moderate positive associations between the EPDS score and number of previous pregnancies (r=0.448, P=0.001), and age at marriage (r=0.393, P=0.001) and negative associations between the EPDS score and educational level(r=-0.152, P=0.012). These findings suggest that parity and maternal age at marriage are moderately related to the severity of PPD symptoms. Other socio-demographic factors showed no significant relationship with the EPDS score.
Discussion
This study examined the prevalence and factors associated with PPD among Jordanian women. The results indicate that the number of previous pregnancies, age at marriage, and educational level in women were significantly associated with their EPDS score. These results are consistent with the results of other similar studies [21, 22]. Women with higher parity and older age at marriage exhibited higher EPDS scores, suggesting a moderate positive relationship with PPD symptoms. These findings are consistent with the results of a study conducted in Japan [23]. Educational level was also significantly associated with PPD, where women with secondary education or lower level showed higher EPDS scores compared to those with higher education, which is consistent with the findings of Miyake et al. [24], and findings of studies conducted in Japan and Iran, where lower education was reported as a risk factor for PPD [23, 25], suggesting that cultural and societal expectations may modulate the relationship between education and maternal mental health. Although those with low monthly income had higher EPDS scores compared to those with higher income, the difference was not statistically significant. This contrasts with the results of Segre et al. [26]. No significant association was found between smoking or history of abortion and the EPDS score. These findings contrast with the results of Dindar et al. [27].
Limitations of this study included the use of a convenience sampling method and an online survey method, which may limit generalizability. Future studies with a longitudinal design and larger, more diverse populations are recommended to confirm the reported associations. Our findings underscore the importance of early identification of women at higher risk of PPD in Jordan, particularly those with higher parity, older age of marriage, or lower educational levels, to facilitate timely interventions. The study emphasizes the need for targeted postpartum care, including educational programs and supportive interventions, to mitigate the impact of PPD, especially among women at higher risk. Additional qualitative studies should be conducted to explore the specific challenges faced by Jordanian women. Applying targeted interventions and policies may help alleviate the burden of PPD and enhance maternal well-being in this population.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Al-Balqa Applied University, Karak, Jordan. Written informed consent was obtained from all participants prior to the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Data collection and data analysis: Ehoud Garaleah; Draft preparation: Ehoud Garaleah and Ghayda Alkhotoba; Supervision: Nooralhuda Alma’aytah and Ehoud Garaleah; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the women who participated in this research for their cooperation.
References
Postpartum Depression (PPD) is a common mental health disorder affecting 10–20% of women globally, with rates exceeding 30% in some low- and middle-income countries [1, 2]. In Jordan, the prevalence ranges from 22% to 30%, with approximately 45% of cases classified as moderate to severe [3, 4]. PPD negatively impacts maternal well-being, infant development, and family dynamics. Neurological and emotional changes associated with PPD can impair maternal bonding, increasing the risk of emotional, behavioral, and cognitive difficulties in children [4–6]. Several factors are associated with PPD, including unplanned pregnancies, low socioeconomic status, poor social support, and marital stress [7–9]. Adolescent mothers are at greater risk, particularly when experiencing family conflict or financial hardship [10-12]. Additionally, research suggests a potential link between parity and increased risk of PPD. A systematic review reported that women with more than one child were 1.5-2 times more likely to develop PPD symptoms [13, 14], while studies from Japan and Spain found that parity was associated with 30–50% higher rates of depressive symptoms [15, 16].
Despite international findings, the relationship between parity and PPD remains under-investigated in Jordan. Given the country’s unique social and healthcare context, including limited access to mental health services, parity may play a distinct role in shaping maternal mental health outcomes [17, 18]. Therefore, this study aims to examine whether multiparous women in Jordan are at greater risk of developing PPD. The goal is to identify the risk factors associated with PPD among southern Jordanian women. Understanding this relationship is crucial for identifying at-risk groups and informing the development of targeted interventions that promote maternal and infant well-being.
Materials and Methods
This quantitative cross-sectional study was conducted in the southern governorates of Jordan, targeting postpartum women who attended maternal and child health clinics or those accessible through social media platforms, such as Facebook and WhatsApp. A total of 434 women participated in the study from August to December 2023. They were mothers aged 20-45 years, with at least one child, and no reported history of psychological symptoms prior to marriage. Women who reported a history of severe mental illness, inability to complete the questionnaires, or had medical conditions that could confound the results were excluded. The sample size was determined using G*Power software, version 3.1. Based on a medium effect size of 0.3, an alpha value of 0.05, and a test power of 0.80, the required sample size was calculated to be 384. To ensure sufficient data quality and to account for a 13% sample dropout rate, the sample size increased to 434.
Data collection was performed using a structured, self-administered questionnaire that included two sections: a sociodemographic/obstetric form and the Edinburgh Postnatal Depression Scale (EPDS). The sociodemographic/obstetric form surveyed age, parity, educational level, employment status, family income, history of smoking, age at marriage, number of previous pregnancies and abortions, and number of children living with parents. The EPDS is a valid 10-item scale developed by Cox et al. [19], with each item rated on a four-point Likert scale and a total score ranging from 0 to 30. A cut-off point of 13 was used to indicate probable PPD. In this study, the validated Arabic version of EPDS was used. The translation was done by two independent translators and reviewed by a bilingual expert panel specialized in mental health. A pilot test was conducted on 15 Jordanian women (not included in the final sample) to assess clarity and cultural adaptability. The internal consistency of the Arabic EPDS was found to be high (Cronbach’s α coefficient=0.82). Previous studies have confirmed the validity of the Arabic EPDS in other Arab countries [20]. Data collection was conducted in-person (for women attending maternal and child health services) or online (for women reachable through social media platforms).
Statistical analysis was performed in IBM SPSS software, version 29. Descriptive statistics were used to present participants’ characteristics. Categorical variables were expressed as frequency (percentage), while continuous variables were reported as Mean±SD. Independent t-tests and one-way Analysis of Variance (ANOVA) were used to compare the groups based on depression levels. Pearson’s correlation test was used to explore associations between continuous variables. The assumptions of normality were tested using the Shapiro–Wilk test. P<0.05 was considered statistically significant.
Results
The socio-demographic and obstetric characteristics of participants are presented in Table 1.
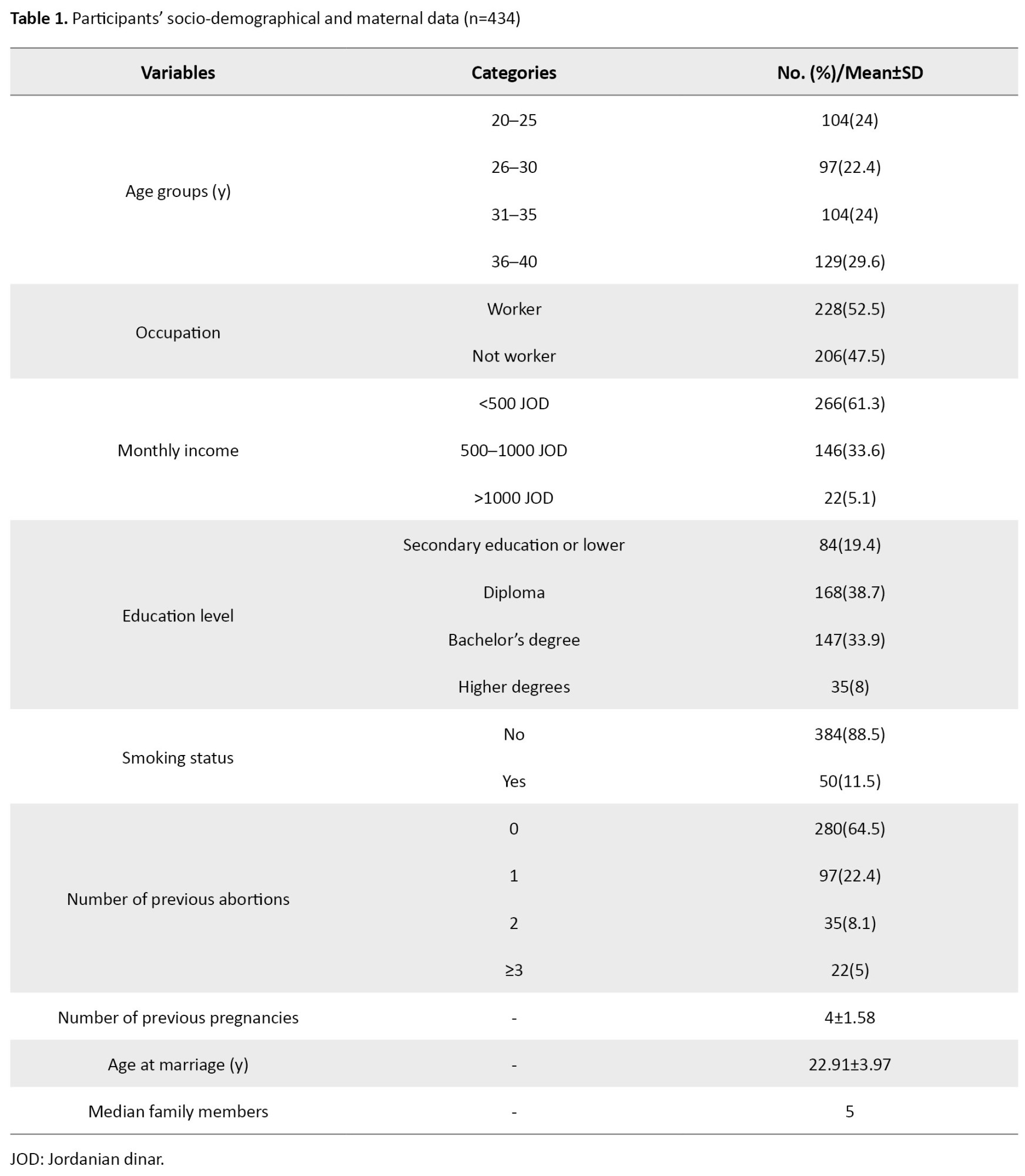
The majority were aged 36–40 years (29.6%), and more than half were employed (52.5%). Most participants reported a monthly income of <500 Jordanian dinar (61.3%), and 38.7% had a diploma. Regarding health behaviors, the majority were non-smokers (88.5%), with no history of abortions (64.5%), and their mean number of previous pregnancies was 4±1.58. Their mean age at marriage was 22.91±3.97 years, and the median family size was 5 (Table 1).
The mean EPDS score was 15.57±4.71. A total of 324 women (74.7%) scored 13 or above, indicating that they were at risk of PPD development, whereas 110 women (25.3%) were not at risk (Table 2).
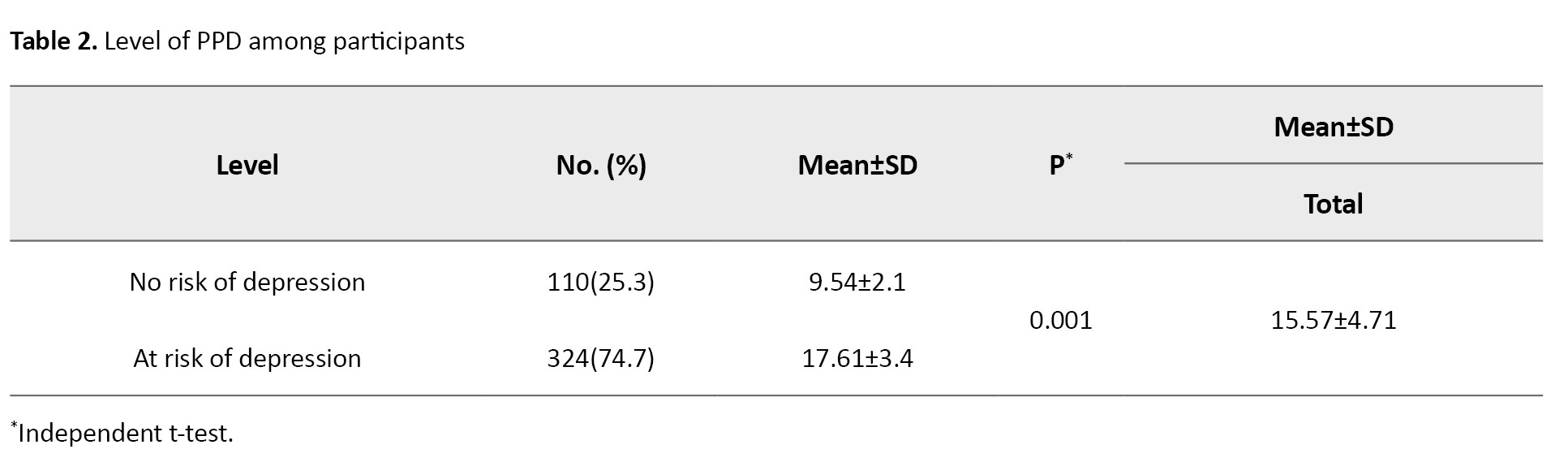
The independent t-test results revealed a statistically significant difference in the EPDS score between the two groups at risk and at no risk of PPD development (P=0.001).
The ANOVA results showed that the EPDS score was significantly different based on educational level (P=0.009), where women with secondary education or lower level had higher scores than those with higher education levels. The EPDS score was not significantly different based on the number of previous abortions, age, occupation, monthly income, or smoking (Table 3).

The results of Pearson’s correlation test for the association of socio-demographic and obstetric variables with the EPDS score are presented in Table 4.
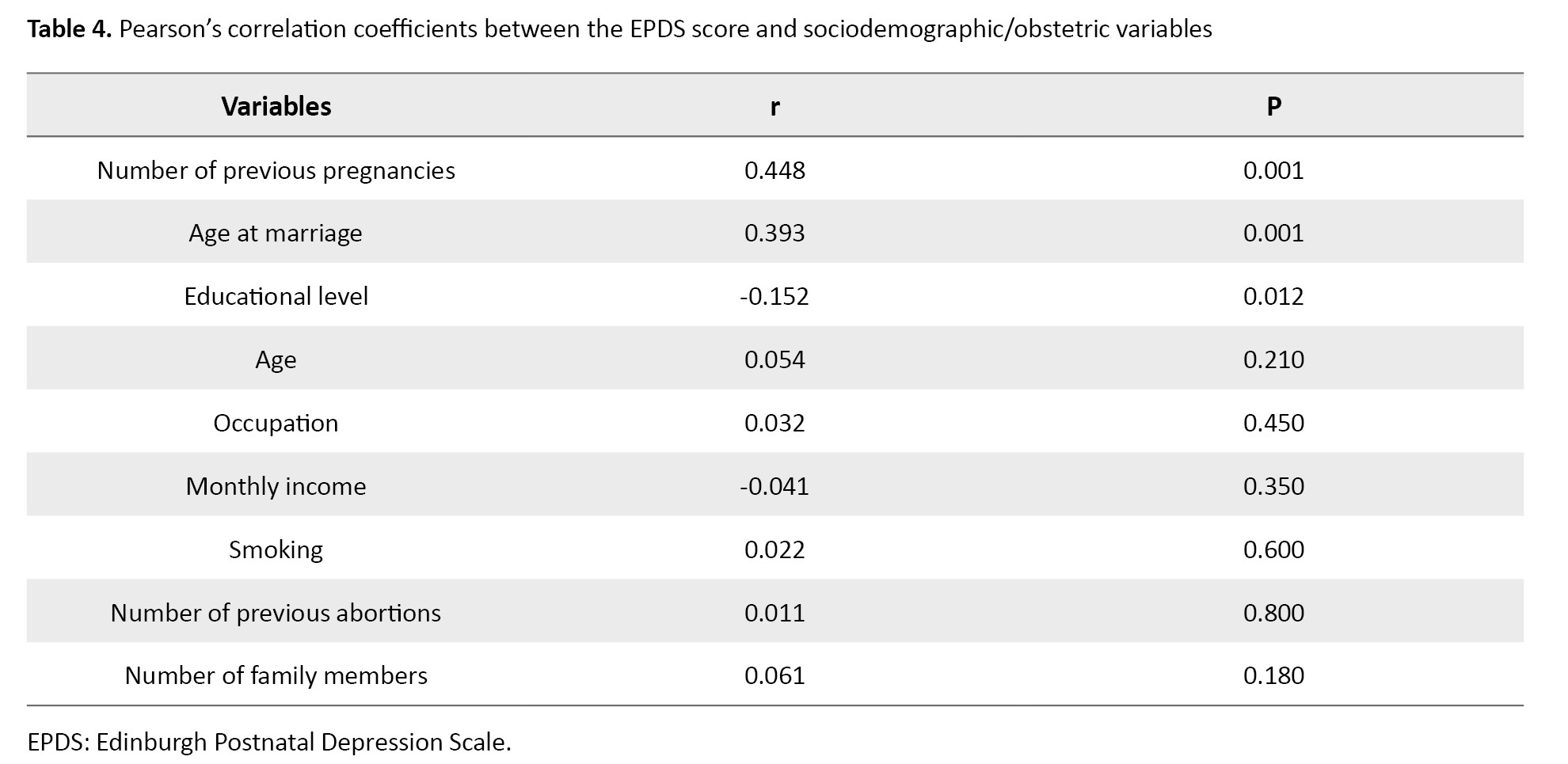
The results revealed moderate positive associations between the EPDS score and number of previous pregnancies (r=0.448, P=0.001), and age at marriage (r=0.393, P=0.001) and negative associations between the EPDS score and educational level(r=-0.152, P=0.012). These findings suggest that parity and maternal age at marriage are moderately related to the severity of PPD symptoms. Other socio-demographic factors showed no significant relationship with the EPDS score.
Discussion
This study examined the prevalence and factors associated with PPD among Jordanian women. The results indicate that the number of previous pregnancies, age at marriage, and educational level in women were significantly associated with their EPDS score. These results are consistent with the results of other similar studies [21, 22]. Women with higher parity and older age at marriage exhibited higher EPDS scores, suggesting a moderate positive relationship with PPD symptoms. These findings are consistent with the results of a study conducted in Japan [23]. Educational level was also significantly associated with PPD, where women with secondary education or lower level showed higher EPDS scores compared to those with higher education, which is consistent with the findings of Miyake et al. [24], and findings of studies conducted in Japan and Iran, where lower education was reported as a risk factor for PPD [23, 25], suggesting that cultural and societal expectations may modulate the relationship between education and maternal mental health. Although those with low monthly income had higher EPDS scores compared to those with higher income, the difference was not statistically significant. This contrasts with the results of Segre et al. [26]. No significant association was found between smoking or history of abortion and the EPDS score. These findings contrast with the results of Dindar et al. [27].
Limitations of this study included the use of a convenience sampling method and an online survey method, which may limit generalizability. Future studies with a longitudinal design and larger, more diverse populations are recommended to confirm the reported associations. Our findings underscore the importance of early identification of women at higher risk of PPD in Jordan, particularly those with higher parity, older age of marriage, or lower educational levels, to facilitate timely interventions. The study emphasizes the need for targeted postpartum care, including educational programs and supportive interventions, to mitigate the impact of PPD, especially among women at higher risk. Additional qualitative studies should be conducted to explore the specific challenges faced by Jordanian women. Applying targeted interventions and policies may help alleviate the burden of PPD and enhance maternal well-being in this population.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Al-Balqa Applied University, Karak, Jordan. Written informed consent was obtained from all participants prior to the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Data collection and data analysis: Ehoud Garaleah; Draft preparation: Ehoud Garaleah and Ghayda Alkhotoba; Supervision: Nooralhuda Alma’aytah and Ehoud Garaleah; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the women who participated in this research for their cooperation.
References
- Mohammad KI, Sabbah H, Aldalaykeh M, ALBashtawy M, Z Abuobead K, Creedy D, et al. Informative title: Effects of social support, parenting stress and self-efficacy on postpartum depression among adolescent mothers in Jordan. J Clin Nurs. 2021; 30(23-24):3456-65. [DOI:10.1111/jocn.15846] [PMID]
- Mohammad KI, Gamble J, Creedy DK. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery. 2011; 27(6):e238-45. [DOI:10.1016/j.midw.2010.10.008] [PMID]
- Ayoub K, Shaheen A, Hajat S. Postpartum depression in the Arab region: A systematic literature review. Clin Pract Epidemiol Ment Health. 2020; 16(Suppl-1):142-55. [DOI:10.2174/1745017902016010142] [PMID]
- Kantrowitz-Gordon I. Internet confessions of postpartum depression. Issues Ment Health Nurs. 2013; 34(12):874-82. [DOI:10.3109/01612840.2013.806618] [PMID]
- Liu S, Yan Y, Gao X, Xiang S, Sha T, Zeng G, He Q. Risk factors for postpartum depression among Chinese women: Path model analysis. BMC Pregnancy Childbirth. 2017; 17(1):133. [DOI:10.1186/s12884-017-1320-x] [PMID]
- Green K, Broome H, Mirabella J. Postnatal depression among mothers in the United Arab Emirates: Socio-cultural and physical factors. Psychol Health Med. 2006; 11(4):425-31. [DOI:10.1080/13548500600678164] [PMID]
- Zhao XH, Zhang ZH. Risk factors for postpartum depression: An evidence-based systematic review of systematic reviews and meta-analyses. Asian J Psychiatr. 2020; 53:102353. [DOI:10.1016/j.ajp.2020.102353] [PMID]
- Stewart DE, Robertson E, Dennis CL, Grace SL, Wallington T. Postpartum depression: Literature review of risk factors and interventions. Toronto: University Health Network; 2003. [Link]
- Davis K, Pearlstein T, Stuart S, O'Hara M, Zlotnick C. Analysis of brief screening tools for the detection of postpartum depression: Comparisons of the PRAMS 6-item instrument, PHQ-9, and structured interviews. Arch Womens Ment Health. 2013; 16(4):271-7. [DOI:10.1007/s00737-013-0345-z] [PMID]
- Zineb S. Validation of the Arabic version of the Edinburgh Postnatal Depression Scale and prevalence of postnatal depression on an Algerian sample. Formats Citation. 2020; 12(1):341-51. [Link]
- Sakemi Y, Nakashima T, Watanabe K, Ochiai M, Sawano T, Inoue H, et al. Changing risk factors for postpartum depression in mothers admitted to a perinatal center. Pediatr Neonatol. 2023; 64(3):319-26. [DOI:10.1016/j.pedneo.2022.09.013] [PMID]
- Wei J, Wu QJ, Zhang TN, Shen ZQ, Liu H, Zheng DM, et al. Complications in multiple gestation pregnancy: A cross-sectional study of ten maternal-fetal medicine centers in China. Oncotarget. 2016; 7(21):30797-803. [DOI:10.18632/oncotarget.9000] [PMID]
- Hoque M, Hoque E, Kader SB. Pregnancy complications of grandmultiparity at a rural setting of South Africa. Iran J Reproduct Med. 2008; 6(1):25-30. [Link]
- Santana DS, Surita FG, Cecatti JG. Multiple pregnancy: Epidemiology and association with maternal and perinatal morbidity. Rev Bras Ginecol Obstet. 2018; 40(9):554-62. [DOI:10.1055/s-0038-1668117] [PMID]
- Lazarov S, Lazarov L, Lazarov N. Complications of multiple pregnancies: Overview. Trakia J Sci. 2016; 1:108-11. [Link]
- Kadir S, Shakoor S, Raza S, Malik A. Antenatal complications in grand multipara presented at tertiary care hospital. Ann Punjab Med Coll. 2021; 15(1):69-72. [DOI:10.29054/apmc/2021.862]
- Wang W, Ren D, Wang CS, Li T, Yao HC. High sensitivity C-reactive protein to prealbumin ratio measurement as a marker of the prognosis in acute coronary syndrome. Sci Rep. 2019; 9(1):11583. [DOI:10.1038/s41598-019-48189-y] [PMID]
- Shinohara S, Horiuchi S, Shinohara R, Otawa S, Kushima M, Miyake K, et al. Multiple pregnancy as a potential risk factor for postpartum depression: The Japan environment and children's study. J Affect Disord. 2023; 329:218-24. [DOI:10.1016/j.jad.2023.02.088] [PMID]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987; 150:782-6. [DOI:10.1192/bjp.150.6.782] [PMID]
- Ghubash R, Abou-Saleh MT, Daradkeh TK. The validity of the Arabic Edinburgh postnatal depression scale. Soc Psychiatry Psychiatr Epidemiol. 1997; 32(8):474-6. [DOI: 10.1007/BF00789142] [PMID]
- Al Dallal F, Grant I. Postnatal depression among Bahraini women: Prevalence of symptoms and psychosocial risk factors. East Mediterranean Health J. 18(5):439-45. [DOI:10.26719/2012.18.5.432]
- Muraca GM, Joseph KS. The association between maternal age and depression. J Obstet Gynaecol Can. 2014; 36(9):803-10. [DOI:10.1016/S1701-2163(15)30482-5] [PMID]
- Matsumura K, Hamazaki K, Tsuchida A, Kasamatsu H, Inadera H; Japan environment and children’s study (JECS) Group. Education level and risk of postpartum depression: Results from the Japan environment and children's study (JECS). BMC Psychiatry. 2019; 19(1):419. [DOI:10.1186/s12888-019-2401-3] [PMID]
- Miyake Y, Tanaka K, Arakawa M. Associations of job type, income, and education with postpartum depressive symptoms: The Kyushu Okinawa maternal and child health study. Psychiatry Res. 2020; 291:113224. [DOI:10.1016/j.psychres.2020.113224] [PMID]
- Cheraghi M, Najafian M, Amoori N, Bazargan A, Cheraghi M, Motaghi M. Risk factors of postpartum depression in Ramhormoz city, Iran. Neuropsychiatria Neuropsychologia Neuropsychiatry Neuropsychology. 2015; 10(1):1-4. [Link]
- Segre LS, O'Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression: The relative significance of three social status indices. Soc Psychiatry Psychiatr Epidemiol. 2007; 42(4):316-21. [DOI:10.1007/s00127-007-0168-1] [PMID]
- Dindar I, Erdogan S. Screening of Turkish women for postpartum depression within the first postpartum year: The risk profile of a community sample. Public Health Nurs. 2007; 24(2):176-83. [DOI:10.1111/j.1525-1446.2007.00636.x] [PMID]
Article Type : Research |
Subject:
Special
Received: 2024/11/28 | Accepted: 2025/05/3 | Published: 2025/09/8
Received: 2024/11/28 | Accepted: 2025/05/3 | Published: 2025/09/8
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |