Mon, Dec 29, 2025
Volume 35, Issue 3 (6-2025)
JHNM 2025, 35(3): 179-187 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tabrizi M, Adib M, Khaleghdoost Mohamadi T, Maroufizadeh S. Nurses' Performance and Related Factors in End-of-Life Care in the Intensive Care Unit: A Cross-sectional Study. JHNM 2025; 35 (3) :179-187
URL: http://hnmj.gums.ac.ir/article-1-2423-en.html
URL: http://hnmj.gums.ac.ir/article-1-2423-en.html
1- Nursing (Msc), Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Associate Professor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,adibm.2211@gmail.com
3- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
2- Associate Professor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 491 kb]
(304 Downloads)
| Abstract (HTML) (530 Views)
Full-Text: (165 Views)
Introduction
Death is an inevitable part of life, making it essential for healthcare providers to deliver high-quality End-of-life (EOL) care when treatment is no longer effective [1, 2]. EOL care offers comprehensive support—addressing physical, emotional, spiritual, psychological, and social needs—to patients with terminal illnesses and their families, aiming to improve quality of life [3-6]. In addition to pain management, key elements of EOL care include emotional support, effective communication, and helping patients and families prepare for death with dignity [7].
Implementing a structured EOL care program can avoid unnecessary medical interventions, ease patient suffering, reduce psychological distress in family members after death, and lower the economic and social burdens on society; in contrast, inadequate EOL care can result in intense grief, Post-traumatic Stress Disorder (PTSD) among family members, and emotional or moral distress for healthcare providers [3, 8]. However, ethical considerations surrounding EOL care continue to be debated in the healthcare community [9]. The demand for EOL care is rising due to the aging population, limited medical and social support services, and a growing prevalence of chronic degenerative conditions [10]. Over the next five decades, the global death rate is projected to rise significantly, with many individuals expected to pass away from progressive chronic illnesses, highlighting the urgent need for comprehensive EOL systems that address the needs and expectations of both patients and their families [11].
Approximately 56.8 million people are estimated to require EOL care annually, yet only 14% receive it adequately [12]. About 94% of those needing such care are adults, with 69% being over 60% and 25% between the ages of 15 and 59 [4]. Around 11% of EOL patients spend more than one week in Intensive Care Units (ICUs) during the last six months of life, and approximately 20% of terminally ill individuals remain in the ICU for at least three days at the end of life [13, 14].
Improving EOL care in the ICU is vital for critically ill patients. Key elements include effective communication, pain, anxiety relief, and family support [15]. Nurses play a central role due to their close interaction with patients and families. High-quality nursing care can lead to a peaceful death and a meaningful family experience [16]. However, an Australian study found that while ICU nurses excelled in sharing information and adjusting to the environment, they were less effective in providing emotional support and symptom management [9].
Considering the contradictions in the results of the studies, as well as the cultural differences, the prevailing management atmosphere, the conditions, and facilities, as well as the training courses completed by nurses, which can lead to differences in the skill level of nurses in caring for patients at the EOL and because very few studies have been done on the performance of nurses regarding EOL care in Iran. Therefore, we decided to conduct a study to determine the factors related to the performance of ICU nurses in EOL care in the educational-medical centers of Rasht City.
Materials and Methods
The current research is a descriptive-analytical cross-sectional study. The census method selected 220 working nurses in the ICUs of six educational medical centers affiliated with Guilan University of Medical Sciences in Rasht City, Iran.
The inclusion criteria included having at least a bachelor’s degree, at least 6 months of work experience in the research department, and consent to participate in this study. The data collection tool was the standard questionnaire of EOL care performance of ICU nurses, which included individual, social, and organizational characteristics and measured the performance of nurses in EOL care.
A questionnaire of personal, social, and organizational characteristics includes questions such as age, sex, marital status, education level, position, service history in the ICU, frequency of caring for a dying patient in the hospital, history of caring for dying family members or friends and passing a training course related to EOL care.
The questionnaire to measure nurses’ performance regarding EOL care was a researcher-made questionnaire based on a similar previous study [9]. It has 51 phrases and 6 subscales: Providing information to patients (statements 1-10), making patient-centered and family-centered decisions (statements 11-15), adjusting the environment around patients (statements 16-25), emotional supports (statements 26-37), the management of signs and symptoms of patients (statements 38-47), and spiritual care (statements 48-51). The answers to the phrases are “never,” “rarely,” “sometimes,” “usually,” and “always,” scoring 1 to 5, and the total range of scores from the questionnaire is between 51 and 255. A higher score indicates a better performance.
After completing the tool design, it entered the validity and reliability phase. The faculty members of Guilan University of Medical Sciences confirmed the instrument’s validity. The mean Content Validity Ratio (CVR=0.83) and Content Validity Index (CVI=0.95) were obtained.
The Cronbach α coefficient and Intra Class Coefficient (ICC) were used to check the nurses’ performance questionnaire’s internal consistency and test re-test reliability regarding EOL care. Internal consistency reliability was calculated in 25 nurses, and test re-test reliability was calculated in 15 nurses at an interval of two weeks. The value of the Cronbach α coefficient for the whole questionnaire was 0.961, and for its subscales were as follows: Information sharing, 0.920; patients-centered and family-centered decision-making, 0.874; environment adjustment, 0.858; emotional support, 0.943; control of signs and symptoms, 0.827; and spiritual support, 0.961. According to the Cronbach α coefficient values, the internal consistency of the entire questionnaire and its subscales was good to excellent. The ICC values for the whole questionnaire were 0.983, and for its subscales were as follows: Information sharing, 0.981; patient-centered and family-centered decision-making, 0.955; environment adjustment, 0.971; emotional support, 0.970; control of signs and symptoms, 0.962; and spiritual support, 0.804.
Data collection was done in May 2022, and after explaining the purpose of the research and getting familiar with the working method, the questionnaire was administered to all working nurses in the ICUs of these hospitals and collected after completion. The questionnaires were completed by the research samples and collected after half an hour. To maintain confidentiality and reduce bias, the questionnaires were anonymous. In addition, sampling was done after the end of the shift delivery, so there was no intervention in the nursing care process.
In this study, the values of quantitative variables were shown as “Mean±SD” and “median (interquartile range),” and the values of qualitative variables were shown as “frequency (percentage).” The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to check the normality of the total performance score of nurses regarding EOL care. A 1-sample t-test was used to compare the converted mean score of nurses’ total performance regarding EOL care. In univariate analysis, an independent t-test and Pearson correlation coefficient were used to investigate the relationship between the total performance score of nurses regarding EOL care and their personal and occupational characteristics. Also, in the multivariate analysis, the multiple linear regression model was used to determine the factors related to the total performance score of nurses regarding EOL care. The data were analyzed using SPSS software, version 16, and the significance level was set at 0.05.
Results
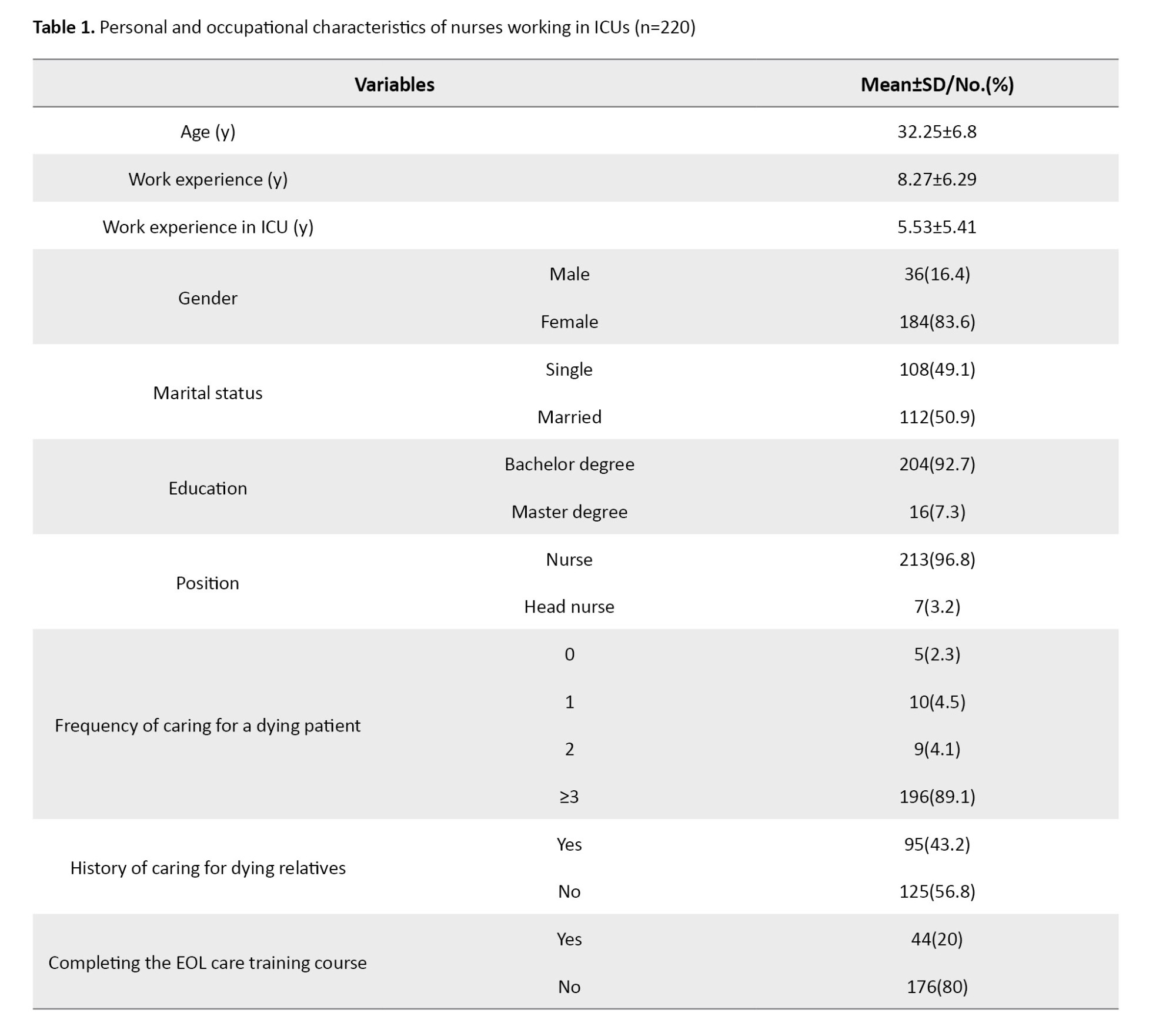
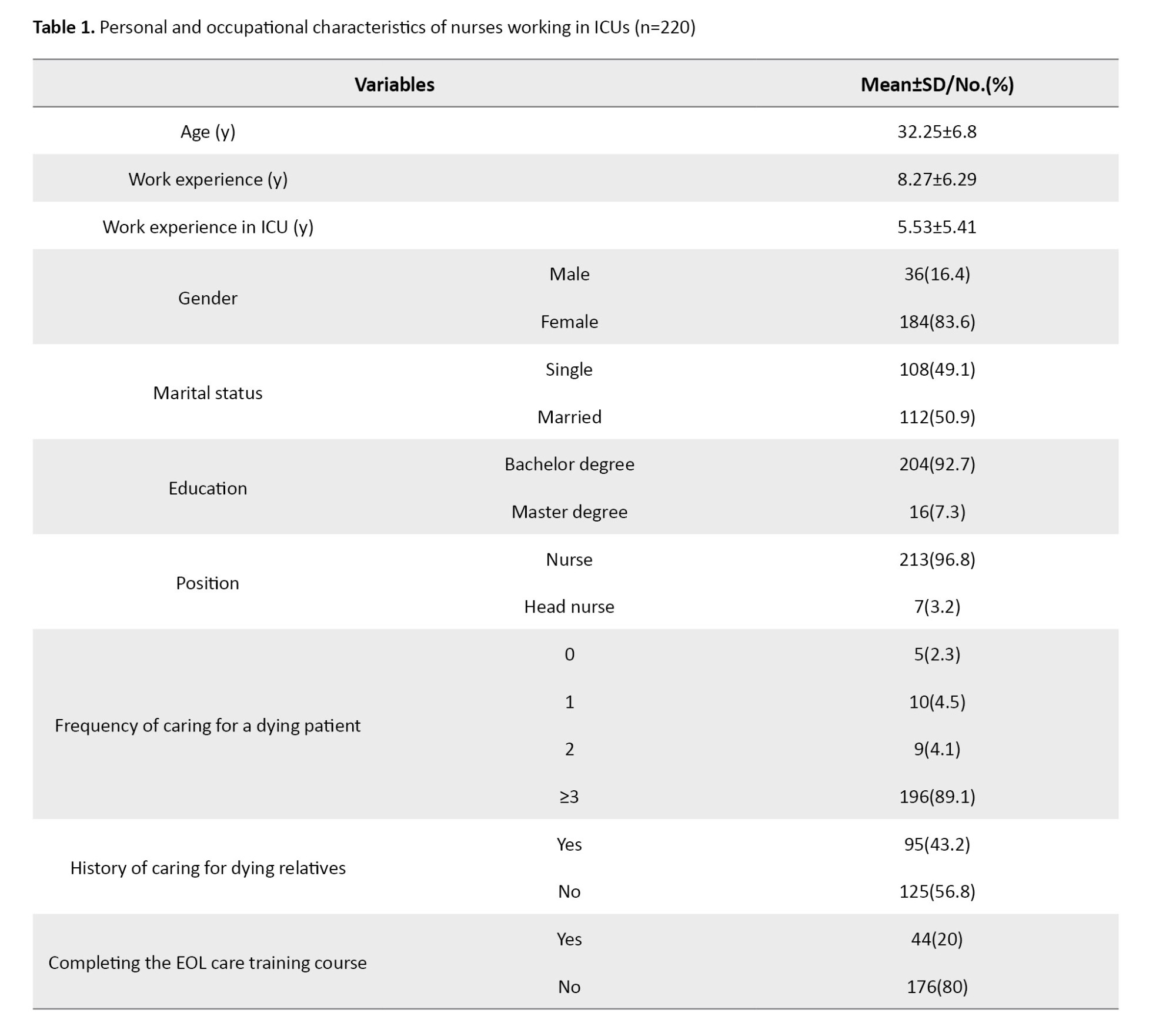
The results showed the mean age of the nurses was 32.25±6.80 years. The mean work experience was 8.27±6.29 years, and their mean work experience in the ICU was 5.53±5.41 years. Of the 220 nurses studied, 16.4% were male, 50.9% were married, 7.3% had a master’s degree, 43.2% had a history of caring for dying relatives, and 20.0% had a history of passing the EOL care training course (Table 1).
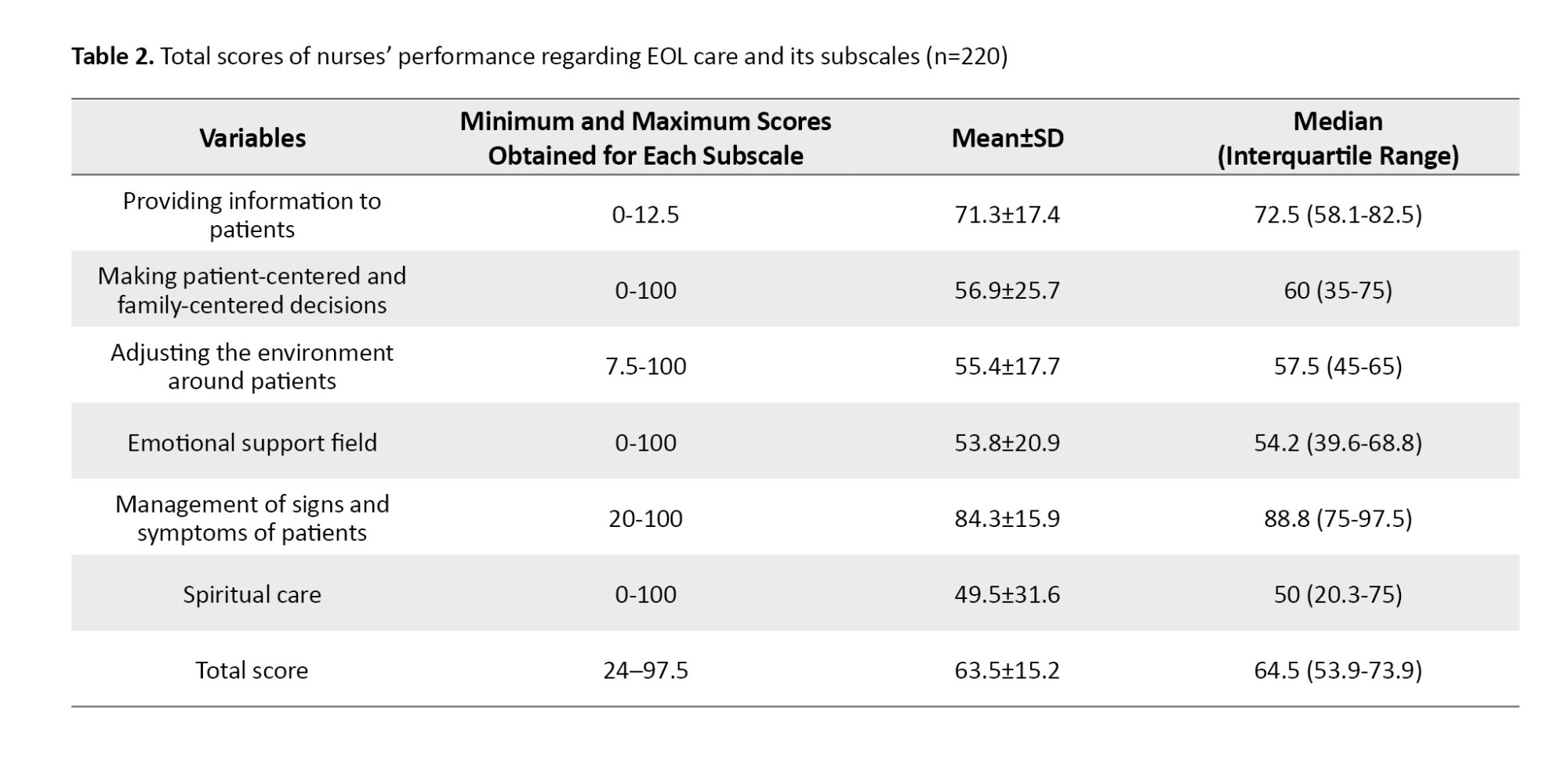
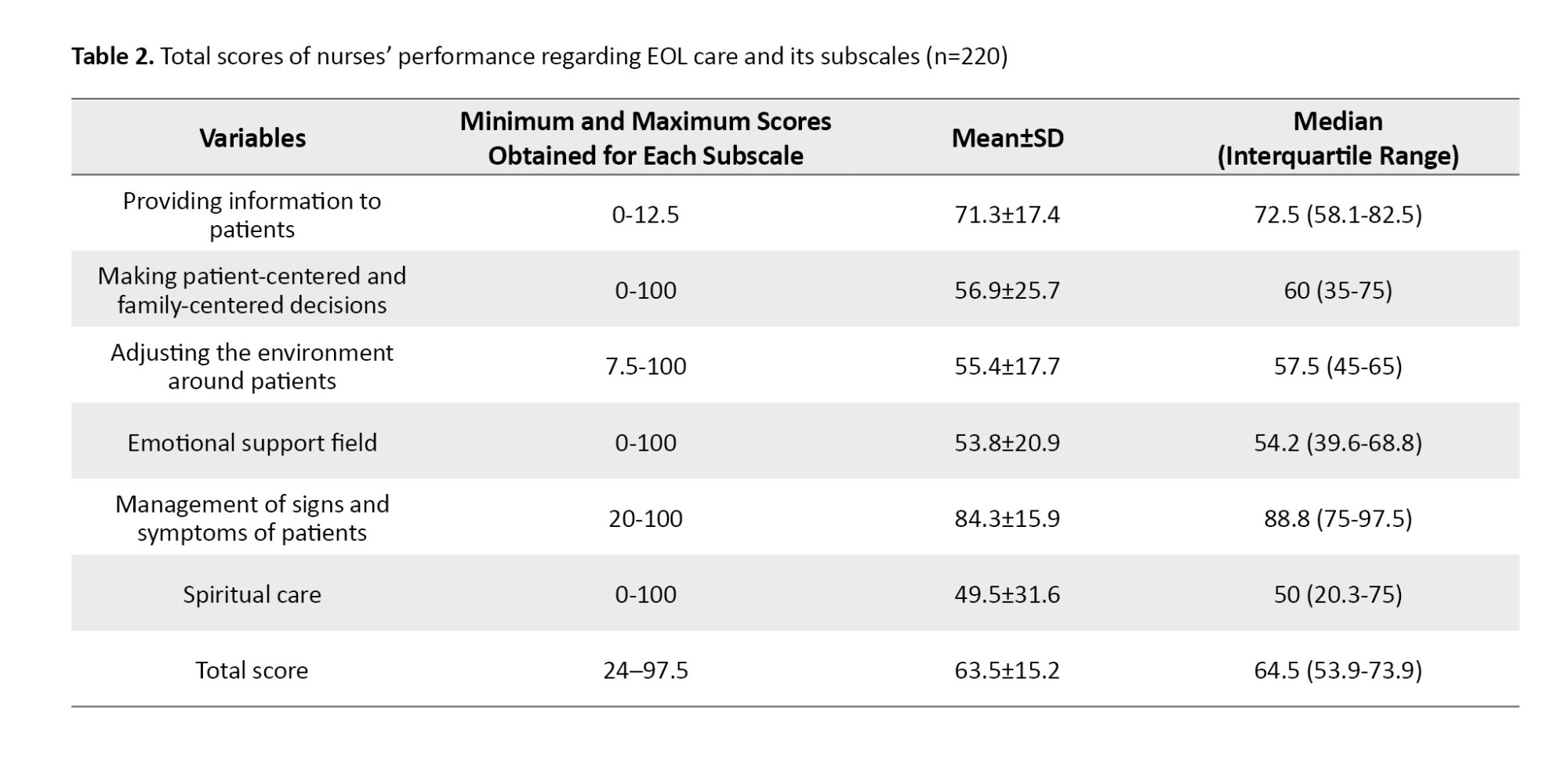
The scores for each subscale were calculated on a scale of 100, and the average scores for each subscale out of a possible 100 are reported in Table 2. The converted mean score of the nurses’ total performance in EOL care was equal to 63.5±15.2, and their median score was 64.5 (interquartile range: 53.9-73.9). According to the results, the highest values of nurses’ performance scores regarding EOL care were respectively related to the field of management of patient’s signs and symptoms and the field of providing information, and the lowest values were associated with the field of spiritual care.
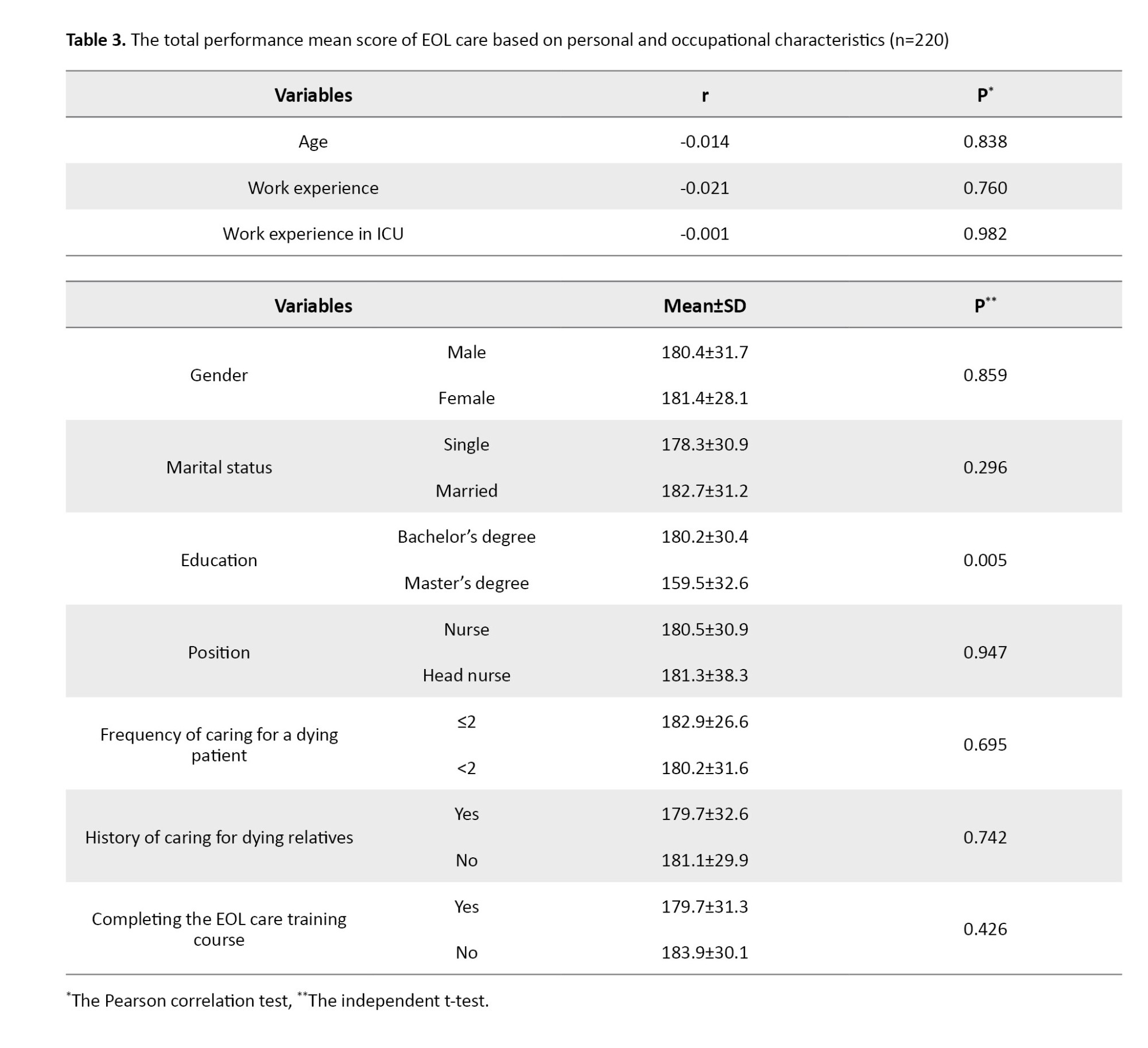
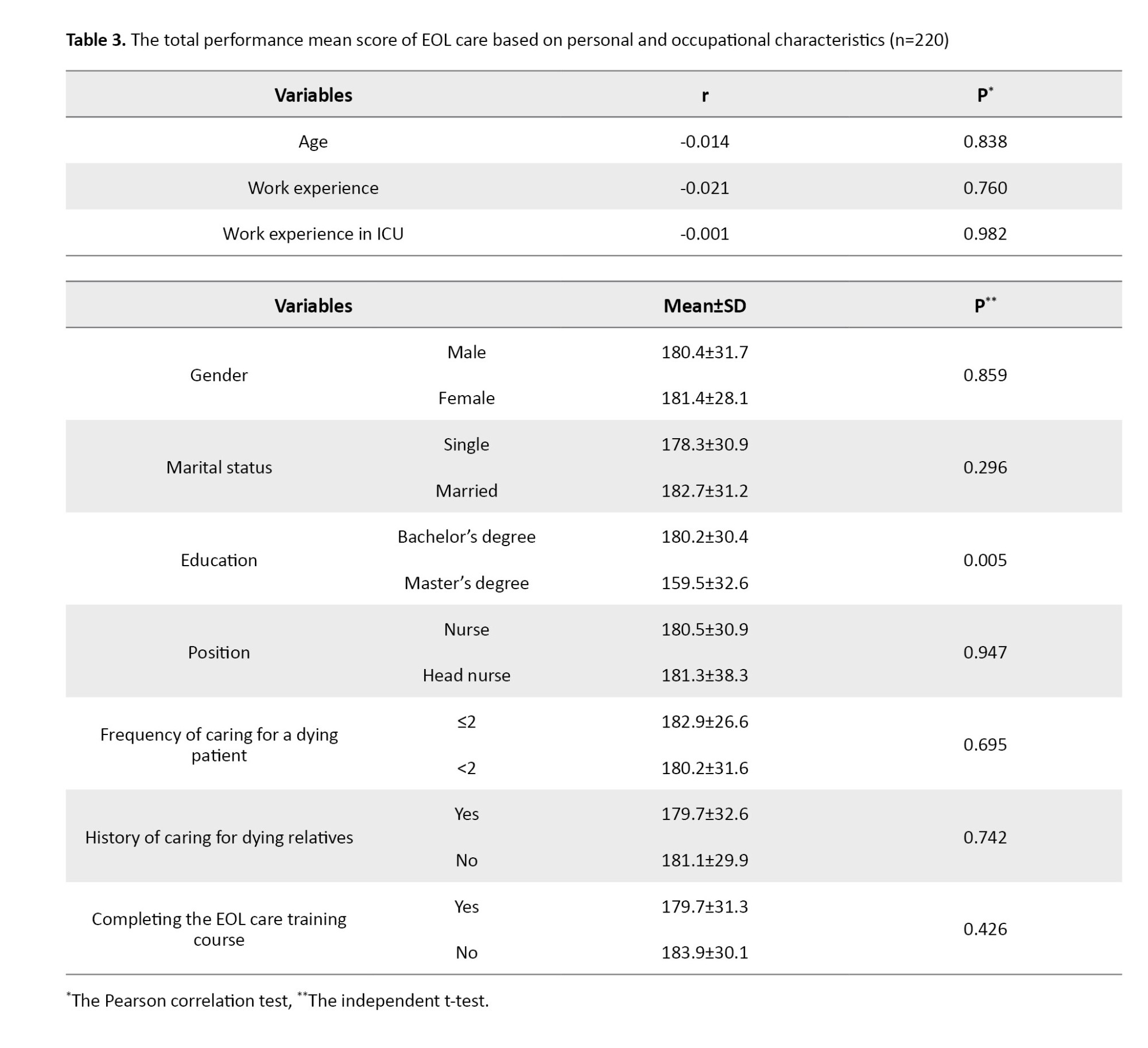
According to the findings, the mean total performance score for EOL care in nurses with master’s education was significantly lower than that of nurses with bachelor’s (P=0.005). Other personal and occupational characteristics of nurses had no statistically significant relationship with the total score (Table 3).
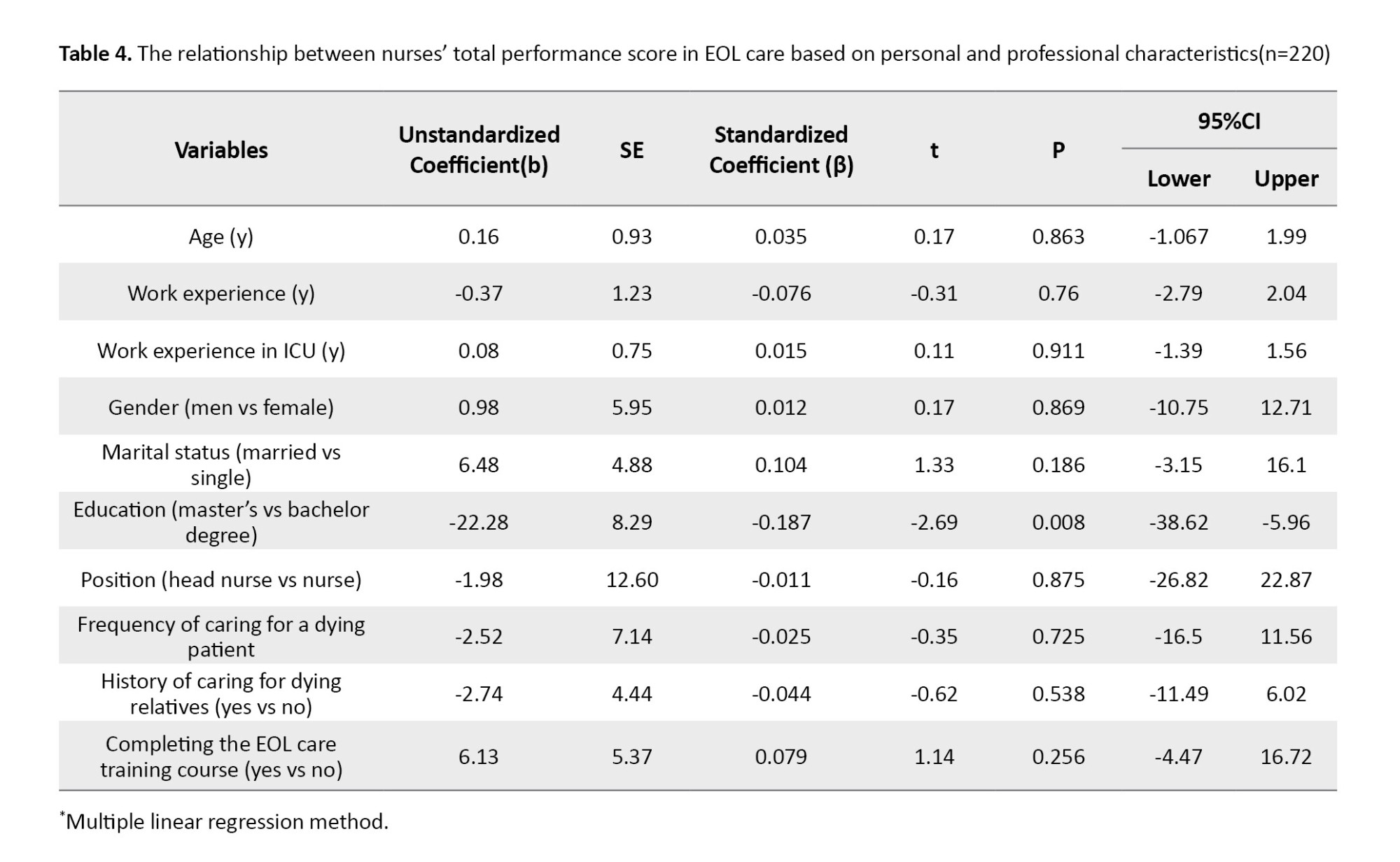
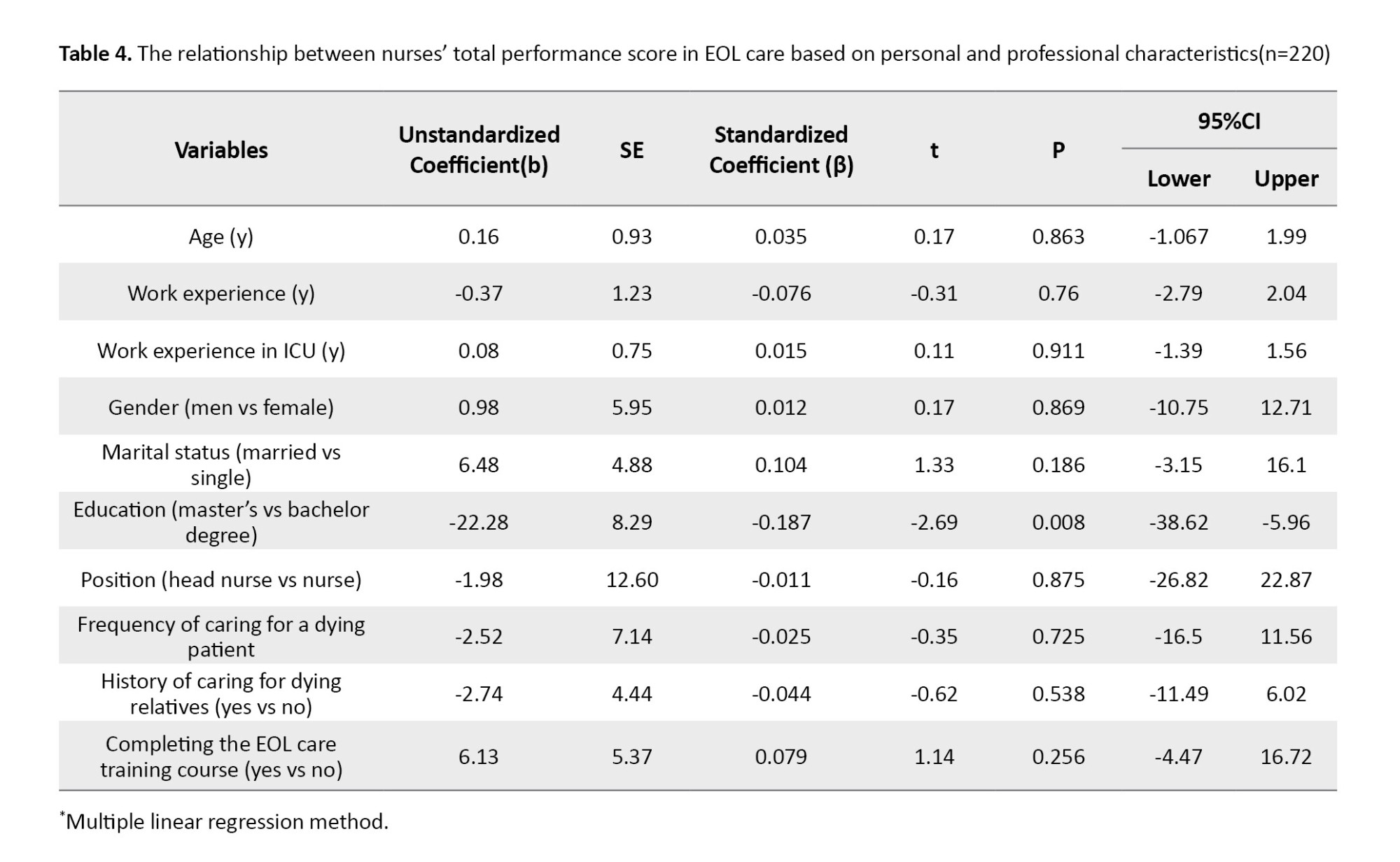
According to the findings, the total performance score of nurses regarding EOL care in nurses with master’s education was significantly 22.28 units lower than nurses with bachelor’s education (b=-22.28, 95% CI, -38.62 to -5.96, P=0.008). Nurses’ other personal and occupational characteristics had no statistically significant relationship with their total performance score regarding EOL care. The coefficient of determination (R2) was 0.05, which indicates that 5.0% of the variations in the total performance score of nurses regarding EOL care were explained by their personal and occupational characteristics (Table 4).
Discussion
This study was conducted to determine the factors related to the performance of ICU nurses in EOL care in the educational medical centers of Rasht City. In the current study, the mean performance score of ICU nurses in EOL care was 63.5±15.2. In our study, contrary to many studies [2, 9, 17, 18], the mean performance score of nurses was higher. Nurses’ high mean performance score may indicate the importance of EOL care for Iranian nurses.
Based on the findings of Ranse et al.’s study, environmental limitations (e.g. poor space design and lack of privacy) and concerns about respecting patients’ wishes (e.g. uncertainty about deciding on the desired treatment and advance directives) were among the influential factors in this field [9]. In addition, nurses have mentioned environmental conditions, time, place, and limited resources as factors affecting their ability to provide suitable services [19]. In this regard, Park et al.’s study showed that supportive and practical death education programs should be designed based on nurses’ professional experience and work environment, enabling them to provide better EOL care [20]. Iranian nurses seem adaptable to the environment in which they assume the role of care.
In the present study, the mean total converted score of ICU nurses’ performance in the emotional support of patients was higher than the mean score for this questionnaire subscale. According to previous studies, many nurses managing EOL care patients may suffer from fear, uncertainty, and emotional exhaustion [21, 22]. In the present study, the mean total converted score of critical care nurses’ performance in patient- and family-centered decision-making in EOL care was higher than the mean score for this questionnaire subscale. According to the results of the study by Ranse et al., the personal values of nurses and the preferences of patients and families are important issues in EOL care. Also, the empowerment of critical care nurses through the development of knowledge, skills, and the ability to participate in interpersonal relationships are issues that have been emphasized in this field. In addition, strategies such as standardizing patient and family preference documentation in patient care plans help critical care nurses identify patient and family preferences [9]. Given the good score of this area in the present study, it can be hoped that nurses’ EOL care decisions depend on the family’s decision.
In the present study, the mean total converted score of the performance of ICU nurses in the field of control of symptoms and signs of patients in EOL care received the highest mean score. According to the results of the study by Lim, the control of symptoms and signs of patients in EOL care focuses on goals that primarily provide comfort and dignity to patients. Appropriate actions in this regard can be managing pain and other symptoms and providing emotional, social, spiritual, and practical support. Common symptoms in late life include pain, dyspnea, delirium, and respiratory secretions. Such symptoms should be treated quickly with appropriate medications and explanations to the patient and family [23]. Beckstrand and his colleagues also showed that the signs and symptoms of the disease can include mental, psychological, and physical concerns or symptoms of pain, fatigue, and nausea [24]. To provide quality EOL care, nurses need to understand the ethical principles applied in EOL care interventions. Teaching skills to the patient helps the patient to face the positive symptoms of his disease by acquiring self-management skills of symptoms and with negative symptoms by learning how to communicate properly verbally and non-verbally with others and express emotional expressions so that learning social and life skills leads to patient self-help, and will motivate him to actively participate in controlling the symptoms of his disease and will lead to the development of self-management skills [25, 26].
In the current study, the mean total converted score of ICU nurses’ performance in the field of spiritual support of patients in EOL care received the lowest mean score compared to other fields. Gurdogan et al in their study showed that spirituality and spiritual care are important components in providing nursing care. In a similar study, nurses had the lowest average score in spirituality [22]. Also, in a study conducted on nurses in Taiwan, the mean total score was reported as high [27]. Providing physical and spiritual care for terminally ill patients, as well as supporting their families, is one of the primary duties of a nurse. Therefore, nurses should pay attention to the condition of each patient. To do this, they must be aware of the patient’s feelings and thoughts as well as his attitude towards death [22].
Based on the present study’s findings, the mean total performance score for EOL care in nurses with a master’s degree was significantly lower than that of nurses with a bachelor’s degree. However, nurses’ other personal and occupational characteristics had no statistically significant relationship with the total score of their performance regarding EOL care. The results of some studies were inconsistent with the results of the present study [22, 28, 29]. This difference can probably be because nurses with a higher degree are more likely to be in charge of the department and are more engaged in management work.
To enhance the quality of EOL care, nurses should strengthen their skills in adapting to environmental limitations, providing emotional support to patients and families, and effectively managing patients’ symptoms. Advanced training in spiritual care and addressing patients’ physical and emotional needs is also essential. Implementing standardized methods for documenting patient and family preferences and involving them in the decision-making process can further improve the quality of care. Additionally, nurses with higher academic qualifications should participate in specialized training programs to balance their managerial and clinical responsibilities, ensuring a more effective role in service delivery.
The findings of this study showed that, in general, nurses had a high mean total score of EOL care performance, which was significantly lower in nurses with a master’s degree than in nurses with a bachelor’s degree. This difference could be due to the lack of focus of nurses with higher education levels on the patient’s bedside and providing direct care to dying patients. It seems that most people with higher education levels are in charge of the ward or are involved in managerial work, and it is suggested that in future research, people who are not directly involved in the care of these patients should be excluded from the study. Using a questionnaire to assess nurses’ performance was one of the limitations of this study, and based on this, it is suggested that future studies use the observation method to evaluate nurses’ performance.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1401.030). Written informed consent was obtained from all Research units. All ethical principles were considered.
Funding
This study was extracted from the master’s thesis Maryam Tabrizi, approved by the Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Study design and supervision: Masoomeh Adib; Data collection: Maryam Tabrizi; Data analysis: Saman Maroufizadeh; Draft preparation: Maryam Tabrizi, Masoomeh Adib, and Tahereh Khaleghdoost Mohamadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers sincerely thank and appreciate the cooperation and support of the Deputy of Research and Technology of Guilan University of Medical Sciences, Rasht, Iran. Also, we are extremely grateful for the cooperation and assistance of all the participating nurses in this study.
References
Death is an inevitable part of life, making it essential for healthcare providers to deliver high-quality End-of-life (EOL) care when treatment is no longer effective [1, 2]. EOL care offers comprehensive support—addressing physical, emotional, spiritual, psychological, and social needs—to patients with terminal illnesses and their families, aiming to improve quality of life [3-6]. In addition to pain management, key elements of EOL care include emotional support, effective communication, and helping patients and families prepare for death with dignity [7].
Implementing a structured EOL care program can avoid unnecessary medical interventions, ease patient suffering, reduce psychological distress in family members after death, and lower the economic and social burdens on society; in contrast, inadequate EOL care can result in intense grief, Post-traumatic Stress Disorder (PTSD) among family members, and emotional or moral distress for healthcare providers [3, 8]. However, ethical considerations surrounding EOL care continue to be debated in the healthcare community [9]. The demand for EOL care is rising due to the aging population, limited medical and social support services, and a growing prevalence of chronic degenerative conditions [10]. Over the next five decades, the global death rate is projected to rise significantly, with many individuals expected to pass away from progressive chronic illnesses, highlighting the urgent need for comprehensive EOL systems that address the needs and expectations of both patients and their families [11].
Approximately 56.8 million people are estimated to require EOL care annually, yet only 14% receive it adequately [12]. About 94% of those needing such care are adults, with 69% being over 60% and 25% between the ages of 15 and 59 [4]. Around 11% of EOL patients spend more than one week in Intensive Care Units (ICUs) during the last six months of life, and approximately 20% of terminally ill individuals remain in the ICU for at least three days at the end of life [13, 14].
Improving EOL care in the ICU is vital for critically ill patients. Key elements include effective communication, pain, anxiety relief, and family support [15]. Nurses play a central role due to their close interaction with patients and families. High-quality nursing care can lead to a peaceful death and a meaningful family experience [16]. However, an Australian study found that while ICU nurses excelled in sharing information and adjusting to the environment, they were less effective in providing emotional support and symptom management [9].
Considering the contradictions in the results of the studies, as well as the cultural differences, the prevailing management atmosphere, the conditions, and facilities, as well as the training courses completed by nurses, which can lead to differences in the skill level of nurses in caring for patients at the EOL and because very few studies have been done on the performance of nurses regarding EOL care in Iran. Therefore, we decided to conduct a study to determine the factors related to the performance of ICU nurses in EOL care in the educational-medical centers of Rasht City.
Materials and Methods
The current research is a descriptive-analytical cross-sectional study. The census method selected 220 working nurses in the ICUs of six educational medical centers affiliated with Guilan University of Medical Sciences in Rasht City, Iran.
The inclusion criteria included having at least a bachelor’s degree, at least 6 months of work experience in the research department, and consent to participate in this study. The data collection tool was the standard questionnaire of EOL care performance of ICU nurses, which included individual, social, and organizational characteristics and measured the performance of nurses in EOL care.
A questionnaire of personal, social, and organizational characteristics includes questions such as age, sex, marital status, education level, position, service history in the ICU, frequency of caring for a dying patient in the hospital, history of caring for dying family members or friends and passing a training course related to EOL care.
The questionnaire to measure nurses’ performance regarding EOL care was a researcher-made questionnaire based on a similar previous study [9]. It has 51 phrases and 6 subscales: Providing information to patients (statements 1-10), making patient-centered and family-centered decisions (statements 11-15), adjusting the environment around patients (statements 16-25), emotional supports (statements 26-37), the management of signs and symptoms of patients (statements 38-47), and spiritual care (statements 48-51). The answers to the phrases are “never,” “rarely,” “sometimes,” “usually,” and “always,” scoring 1 to 5, and the total range of scores from the questionnaire is between 51 and 255. A higher score indicates a better performance.
After completing the tool design, it entered the validity and reliability phase. The faculty members of Guilan University of Medical Sciences confirmed the instrument’s validity. The mean Content Validity Ratio (CVR=0.83) and Content Validity Index (CVI=0.95) were obtained.
The Cronbach α coefficient and Intra Class Coefficient (ICC) were used to check the nurses’ performance questionnaire’s internal consistency and test re-test reliability regarding EOL care. Internal consistency reliability was calculated in 25 nurses, and test re-test reliability was calculated in 15 nurses at an interval of two weeks. The value of the Cronbach α coefficient for the whole questionnaire was 0.961, and for its subscales were as follows: Information sharing, 0.920; patients-centered and family-centered decision-making, 0.874; environment adjustment, 0.858; emotional support, 0.943; control of signs and symptoms, 0.827; and spiritual support, 0.961. According to the Cronbach α coefficient values, the internal consistency of the entire questionnaire and its subscales was good to excellent. The ICC values for the whole questionnaire were 0.983, and for its subscales were as follows: Information sharing, 0.981; patient-centered and family-centered decision-making, 0.955; environment adjustment, 0.971; emotional support, 0.970; control of signs and symptoms, 0.962; and spiritual support, 0.804.
Data collection was done in May 2022, and after explaining the purpose of the research and getting familiar with the working method, the questionnaire was administered to all working nurses in the ICUs of these hospitals and collected after completion. The questionnaires were completed by the research samples and collected after half an hour. To maintain confidentiality and reduce bias, the questionnaires were anonymous. In addition, sampling was done after the end of the shift delivery, so there was no intervention in the nursing care process.
In this study, the values of quantitative variables were shown as “Mean±SD” and “median (interquartile range),” and the values of qualitative variables were shown as “frequency (percentage).” The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to check the normality of the total performance score of nurses regarding EOL care. A 1-sample t-test was used to compare the converted mean score of nurses’ total performance regarding EOL care. In univariate analysis, an independent t-test and Pearson correlation coefficient were used to investigate the relationship between the total performance score of nurses regarding EOL care and their personal and occupational characteristics. Also, in the multivariate analysis, the multiple linear regression model was used to determine the factors related to the total performance score of nurses regarding EOL care. The data were analyzed using SPSS software, version 16, and the significance level was set at 0.05.
Results
The results showed the mean age of the nurses was 32.25±6.80 years. The mean work experience was 8.27±6.29 years, and their mean work experience in the ICU was 5.53±5.41 years. Of the 220 nurses studied, 16.4% were male, 50.9% were married, 7.3% had a master’s degree, 43.2% had a history of caring for dying relatives, and 20.0% had a history of passing the EOL care training course (Table 1).
The scores for each subscale were calculated on a scale of 100, and the average scores for each subscale out of a possible 100 are reported in Table 2. The converted mean score of the nurses’ total performance in EOL care was equal to 63.5±15.2, and their median score was 64.5 (interquartile range: 53.9-73.9). According to the results, the highest values of nurses’ performance scores regarding EOL care were respectively related to the field of management of patient’s signs and symptoms and the field of providing information, and the lowest values were associated with the field of spiritual care.
According to the findings, the mean total performance score for EOL care in nurses with master’s education was significantly lower than that of nurses with bachelor’s (P=0.005). Other personal and occupational characteristics of nurses had no statistically significant relationship with the total score (Table 3).
According to the findings, the total performance score of nurses regarding EOL care in nurses with master’s education was significantly 22.28 units lower than nurses with bachelor’s education (b=-22.28, 95% CI, -38.62 to -5.96, P=0.008). Nurses’ other personal and occupational characteristics had no statistically significant relationship with their total performance score regarding EOL care. The coefficient of determination (R2) was 0.05, which indicates that 5.0% of the variations in the total performance score of nurses regarding EOL care were explained by their personal and occupational characteristics (Table 4).
Discussion
This study was conducted to determine the factors related to the performance of ICU nurses in EOL care in the educational medical centers of Rasht City. In the current study, the mean performance score of ICU nurses in EOL care was 63.5±15.2. In our study, contrary to many studies [2, 9, 17, 18], the mean performance score of nurses was higher. Nurses’ high mean performance score may indicate the importance of EOL care for Iranian nurses.
Based on the findings of Ranse et al.’s study, environmental limitations (e.g. poor space design and lack of privacy) and concerns about respecting patients’ wishes (e.g. uncertainty about deciding on the desired treatment and advance directives) were among the influential factors in this field [9]. In addition, nurses have mentioned environmental conditions, time, place, and limited resources as factors affecting their ability to provide suitable services [19]. In this regard, Park et al.’s study showed that supportive and practical death education programs should be designed based on nurses’ professional experience and work environment, enabling them to provide better EOL care [20]. Iranian nurses seem adaptable to the environment in which they assume the role of care.
In the present study, the mean total converted score of ICU nurses’ performance in the emotional support of patients was higher than the mean score for this questionnaire subscale. According to previous studies, many nurses managing EOL care patients may suffer from fear, uncertainty, and emotional exhaustion [21, 22]. In the present study, the mean total converted score of critical care nurses’ performance in patient- and family-centered decision-making in EOL care was higher than the mean score for this questionnaire subscale. According to the results of the study by Ranse et al., the personal values of nurses and the preferences of patients and families are important issues in EOL care. Also, the empowerment of critical care nurses through the development of knowledge, skills, and the ability to participate in interpersonal relationships are issues that have been emphasized in this field. In addition, strategies such as standardizing patient and family preference documentation in patient care plans help critical care nurses identify patient and family preferences [9]. Given the good score of this area in the present study, it can be hoped that nurses’ EOL care decisions depend on the family’s decision.
In the present study, the mean total converted score of the performance of ICU nurses in the field of control of symptoms and signs of patients in EOL care received the highest mean score. According to the results of the study by Lim, the control of symptoms and signs of patients in EOL care focuses on goals that primarily provide comfort and dignity to patients. Appropriate actions in this regard can be managing pain and other symptoms and providing emotional, social, spiritual, and practical support. Common symptoms in late life include pain, dyspnea, delirium, and respiratory secretions. Such symptoms should be treated quickly with appropriate medications and explanations to the patient and family [23]. Beckstrand and his colleagues also showed that the signs and symptoms of the disease can include mental, psychological, and physical concerns or symptoms of pain, fatigue, and nausea [24]. To provide quality EOL care, nurses need to understand the ethical principles applied in EOL care interventions. Teaching skills to the patient helps the patient to face the positive symptoms of his disease by acquiring self-management skills of symptoms and with negative symptoms by learning how to communicate properly verbally and non-verbally with others and express emotional expressions so that learning social and life skills leads to patient self-help, and will motivate him to actively participate in controlling the symptoms of his disease and will lead to the development of self-management skills [25, 26].
In the current study, the mean total converted score of ICU nurses’ performance in the field of spiritual support of patients in EOL care received the lowest mean score compared to other fields. Gurdogan et al in their study showed that spirituality and spiritual care are important components in providing nursing care. In a similar study, nurses had the lowest average score in spirituality [22]. Also, in a study conducted on nurses in Taiwan, the mean total score was reported as high [27]. Providing physical and spiritual care for terminally ill patients, as well as supporting their families, is one of the primary duties of a nurse. Therefore, nurses should pay attention to the condition of each patient. To do this, they must be aware of the patient’s feelings and thoughts as well as his attitude towards death [22].
Based on the present study’s findings, the mean total performance score for EOL care in nurses with a master’s degree was significantly lower than that of nurses with a bachelor’s degree. However, nurses’ other personal and occupational characteristics had no statistically significant relationship with the total score of their performance regarding EOL care. The results of some studies were inconsistent with the results of the present study [22, 28, 29]. This difference can probably be because nurses with a higher degree are more likely to be in charge of the department and are more engaged in management work.
To enhance the quality of EOL care, nurses should strengthen their skills in adapting to environmental limitations, providing emotional support to patients and families, and effectively managing patients’ symptoms. Advanced training in spiritual care and addressing patients’ physical and emotional needs is also essential. Implementing standardized methods for documenting patient and family preferences and involving them in the decision-making process can further improve the quality of care. Additionally, nurses with higher academic qualifications should participate in specialized training programs to balance their managerial and clinical responsibilities, ensuring a more effective role in service delivery.
The findings of this study showed that, in general, nurses had a high mean total score of EOL care performance, which was significantly lower in nurses with a master’s degree than in nurses with a bachelor’s degree. This difference could be due to the lack of focus of nurses with higher education levels on the patient’s bedside and providing direct care to dying patients. It seems that most people with higher education levels are in charge of the ward or are involved in managerial work, and it is suggested that in future research, people who are not directly involved in the care of these patients should be excluded from the study. Using a questionnaire to assess nurses’ performance was one of the limitations of this study, and based on this, it is suggested that future studies use the observation method to evaluate nurses’ performance.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1401.030). Written informed consent was obtained from all Research units. All ethical principles were considered.
Funding
This study was extracted from the master’s thesis Maryam Tabrizi, approved by the Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Study design and supervision: Masoomeh Adib; Data collection: Maryam Tabrizi; Data analysis: Saman Maroufizadeh; Draft preparation: Maryam Tabrizi, Masoomeh Adib, and Tahereh Khaleghdoost Mohamadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers sincerely thank and appreciate the cooperation and support of the Deputy of Research and Technology of Guilan University of Medical Sciences, Rasht, Iran. Also, we are extremely grateful for the cooperation and assistance of all the participating nurses in this study.
References
- Osei EA, Aquah AA, Appiah S, Nasreen L, Oware J, Sarpong C, et al. Enhancing end-of-life care in Ghana: Nurse strategies and practices in addressing patient needs. BMC Palliat Care. 2025; 24(1):70.[DOI:10.1186/s12904-025-01706-5] [PMID]
- Aghaei M, Mohajjel Aghdam A, Bodaghi S, Azami Agdash S. [Knowledge and attitude of nurses toward caring for end of life patients (Persian)]. Iran J Nurs. 2017; 30(107):74-82 [DOI:10.29252/ijn.30.107.74]
- Huffman JL, Harmer B. End-of-life care. 2023 Feb 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. [PMID]
- Xia L, Kongsuwan W. Factors relating to nurses’ end-of-life care. J Biosci Med. 2020; 8(6):189-200. [Link]
- Giwangkancana GW, Anina HN, Sukandar H. Predicting end-of-life in a hospital setting. J Multidiscip Healthc. 2024; 17:619-27. [DOI:10.2147/JMDH.S443425] [PMID]
- Culberson JW, Kopel J, Sehar U, Reddy PH. Urgent needs of caregiving in ageing populations with Alzheimer's disease and other chronic conditions: Support our loved ones. Ageing Res Rev. 2023; 90:102001. [DOI:10.1016/j.arr.2023.102001] [PMID]
- White KR, Coyne PJ, Patel UB. Are nurses adequately prepared for end-of-life care? J Nurs Scholarsh. 2001; 33(2):147-51. [DOI:10.1111/j.1547-5069.2001.00147.x] [PMID]
- Gerritsen RT, Koopmans M, Hofhuis JG, Curtis JR, Jensen HI, Zijlstra JG, et al. Comparing quality of dying and death perceived by family members and nurses for patients dying in US and Dutch ICUs. Chest. 2017; 151(2):298-307. [DOI:10.1016/j.chest.2016.09.003] [PMID]
- Ranse K, Yates P, Coyer F. End-of-life care practices of critical care nurses: A national cross-sectional survey. Aust Crit Care. 2016; 29(2):83-9. [DOI:10.1016/j.aucc.2015.07.001] [PMID]
- Chan CWH, Chow MCM, Chan S, Sanson-Fisher R, Waller A, Lai TTK, et al. Nurses' perceptions of and barriers to the optimal end-of-life care in hospitals: A cross-sectional study. J Clin Nurs. 2020; 29(7-8):1209-19. [DOI:10.1111/jocn.15160] [PMID]
- Akdeniz M, Yardımcı B, Kavukcu E. Ethical considerations at the end-of-life care. SAGE Open Med. 2021; 9:20503121211000918.[DOI:10.1177/20503121211000918] [PMID]
- Wang W, Wu C, Bai D, Chen H, Cai M, Gao J, et al. A meta-analysis of nursing students' knowledge and attitudes about end-of-life care. Nurse Educ Today. 2022; 119:105570. [DOI:10.1016/j.nedt.2022.105570] [PMID]
- Beckstrand RL, Kirchhoff KT. Providing end-of-life care to patients: Critical care nurses’ perceived obstacles and supportive behaviors. Am J Crit Care. 2005; 14(5):395-403. [DOI:10.4037/ajcc2005.14.5.395] [PMID]
- AACN. AACN Core curriculum for high acuity, progressive, and critical care nursing. Amsterdam: Elsevier - Health Sciences Division; 2017. [Link]
- Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: Collaboration, moral distress, and ethical climate. Crit Care Med. 2007; 35(2):422-9.[DOI:10.1097/01.CCM.0000254722.50608.2D] [PMID]
- Ranse K, Yates P, Coyer F. Modelling end-of-life care practices: Factors associated with critical care nurse engagement in care provision. Intensive Crit Care Nurs. 2016; 33:48-55. [DOI:10.1016/j.iccn.2015.11.003] [PMID]
- Ceyhan Ö, Özen B, Zincir H, Şimşek N, Başaran M. How intensive care nurses perceive good death. Death Stud. 2018; 42(10):667-72.[DOI:10.1080/07481187.2018.1430084] [PMID]
- Choi J, Gu M, Oh S, Sok S. Relationship between End-of-Life Care Stress, Death Anxiety, and Self-Efficacy of Clinical Nurses in South Korea. Int J Environ Res Public Health. 2022; 19(3):1082. [DOI:10.3390/ijerph19031082] [PMID]
- Ranse K, Yates P, Coyer F. Factors influencing the provision of end-of-life care in critical care settings: Development and testing of a survey instrument. J Adv Nurs. 2015; 71(3):697-709. [DOI:10.1111/jan.12576] [PMID]
- Park HJ, Lee YM, Won MH, Lim SJ, Son YJ. Hospital nurses' perception of death and self-reported performance of end-of-life care: Mediating role of attitude towards end-of-life care. Healthcare (Basel). 2020; 8(2):142. [DOI:10.3390/healthcare8020142] [PMID]
- Lee YY, Ranse K, Silvester W, Mehta A, Van Haren F. Attitudes and self-reported end-of-life care of Australian and New Zealand intensive care doctors in the context of organ donation after circulatory death. Anaesth Intensive Care. 2018; 46(5):488-97. [DOI:10.1177/0310057X1804600510] [PMID]
- Gurdogan EP, Kurt D, Aksoy B, Kınıcı E, Şen A. Nurses' perceptions of spiritual care and attitudes toward the principles of dying with dignity: A sample from Turkey. Death Stud. 2017; 41(3):180-7. [DOI:10.1080/07481187.2016.1231242] [PMID]
- Lim RB. End-of-life care in patients with advanced lung cancer. Ther Adv Respir Dis. 2016; 10(5):455-67.[DOI:10.1177/1753465816660925] [PMID]
- Beckstrand RL, Hadley KH, Luthy KE, Macintosh JLB. Critical care nurses' suggestions to improve end-of-life care obstacles: Minimal change over 17 years. Dimens Crit Care Nurs. 2017; 36(4):264-70.[DOI:10.1097/DCC.0000000000000252] [PMID]
- Buller H, Virani R, Malloy P, Paice J. End-of-life nursing and education consortium communication curriculum for nurses. J Hosp Palliat Nurs. 2019; 21(2):E5-12. [DOI:10.1097/NJH.0000000000000540] [PMID]
- Walker PH, Neuman BM. Blueprint for use of nursing models: Education, research, practice, and administration. Burlington: Jones & Bartlett Learning; 1996. [Link]
- Wu LF, Lin LY. Exploration of clinical nurses' perceptions of spirituality and spiritual care. J Nurs Res. 2011; 19(4):250-6. [DOI:10.1097/JNR.0b013e318236cf78] [PMID]
- Wong KF, Lee LY, Lee JK. Hong Kong enrolled nurses’ perceptions of spirituality and spiritual care. Int Nurs Rev. 2008; 55(3):333-40. [DOI:10.1111/j.1466-7657.2008.00619.x] [PMID]
- Ibdah R, Zeilani R, Atout M. Jordanian nurses’ perspectives of spirituality and spiritual care: A qualitative study. Cancer Nurs. 2024; 47(1):E38-46. [DOI:10.1097/NCC.0000000000001159] [PMID]
Article Type : Research |
Subject:
General
Received: 2024/10/2 | Accepted: 2025/05/4 | Published: 2025/06/10
Received: 2024/10/2 | Accepted: 2025/05/4 | Published: 2025/06/10
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |