Wed, Jan 28, 2026
Volume 35, Issue 4 (9-2025)
JHNM 2025, 35(4): 270-278 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hossaini K S, mazlom R, ShariatMoghani S, Akhlaghi F, Soleimanpour S, Jahani Shoorab N. The Effect of Using Topical Breast Milk on the Healing of Episiotomy. JHNM 2025; 35 (4) :270-278
URL: http://hnmj.gums.ac.ir/article-1-2405-en.html
URL: http://hnmj.gums.ac.ir/article-1-2405-en.html
Kobra sadat Hossaini1 

 , Reza Mazlom2
, Reza Mazlom2 

 , Sediqah ShariatMoghani3
, Sediqah ShariatMoghani3 

 , Farideh Akhlaghi4
, Farideh Akhlaghi4 

 , Saman Soleimanpour5
, Saman Soleimanpour5 

 , Nahid Jahani Shoorab *6
, Nahid Jahani Shoorab *6 




 , Reza Mazlom2
, Reza Mazlom2 

 , Sediqah ShariatMoghani3
, Sediqah ShariatMoghani3 

 , Farideh Akhlaghi4
, Farideh Akhlaghi4 

 , Saman Soleimanpour5
, Saman Soleimanpour5 

 , Nahid Jahani Shoorab *6
, Nahid Jahani Shoorab *6 


1- Master of Midwifery (MSc), Department of Midwifery, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Instructor, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Instructor, Department of Midwifery, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Professor, Department of Obstetrics, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
5- Associate Professor, Department of Microbiology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
6- Associate Professor, Nursing and Midwifery Care Research Centre, Mashhad University of Medical Sciences, Mashhad, Iran. ,jahanishn@mums.ac.ir
2- Instructor, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Instructor, Department of Midwifery, School of Nursing and Midwifery, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Professor, Department of Obstetrics, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
5- Associate Professor, Department of Microbiology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
6- Associate Professor, Nursing and Midwifery Care Research Centre, Mashhad University of Medical Sciences, Mashhad, Iran. ,
Full-Text [PDF 610 kb]
(317 Downloads)
| Abstract (HTML) (502 Views)
Full-Text: (366 Views)
Introduction
Episiotomy is an incision in the perineum performed to widen the vaginal opening at the second stage of delivery. The American College of Obstetricians and Gynecologists (ACOG) recommends elective episiotomy over routine episiotomy [1]. The studies have reported the episiotomy rates of 19.4% in South Brazil [2], 49% in Ethiopia [3], 92.7% in Romania [4], 95% in Iran [5], and 67% in the Middle East [6]. The repair stage of episiotomy wound healing starts in the first 48 hours and can last for 14 days, increasing the resistance in the newly-created tissue of the healing site during the collagen structure remodeling [7]. Infection of the episiotomy site and delayed healing are among the complications caused by its special anatomical position and proximity to the anus [8]. Improper wound healing and wound dehiscence due to infection usually occur 7-10 days after healing [9]. Delay in the healing of the episiotomy site leads to unpleasant anatomical results, such as skin sensitivity, vaginal narrowing, vaginal prolapse, vaginal opening asymmetry, rectovaginal fistulas, and a higher risk of site infection [10, 11]. Episiotomy does not heal fully up to three weeks after delivery, and wound healing is delayed in 41% of cases [12]. Perineal infections and deformities caused by the delay in perineal healing are the causes of marital and psycho-social problems due to sexual disorders [13]. Accelerating wound healing can reduce pain in the perineal site [14] and make women recover faster after delivery and return to daily activities [12]. Several factors, such as diabetes, vaginal examinations, vaginal hematoma, length of episiotomy incision >3 cm, and anemia, delay recovery [15, 16]. Numerous medicinal methods have been proposed to improve and speed up wound healing, such as topical phenytoin, gentamicin solutions [16], or herbal medicines [17], but the side effects of chemical or even herbal medicines limit their use [14].
Human milk is rich in leukocytes, which cause active immunity. The complement system, macrophages, lymphocytes, lactoferrin, lactoperoxidase, and lysozymes are defense factors in colostrum and breast milk [18]. The topical use of breast milk for perineal healing in the first to seventh days after delivery has been reported to be more effective than disinfection with soap [19]. Some studies have also reported that the topical use of breast milk on the episiotomy site led to higher healing [20, 21]. These studies assessed episiotomy healing at the seventh day of postpartum, while the proliferative phase is performed at least until the second week, and the control of the episiotomy site is recommended in the second week after delivery [22]. Additionally, the studies have only included women without infection risk factors. Mothers who are exposed to infection are not able to breastfeed and take care of their infant. In a study of late repair of episiotomy, 73.3% of neonates did not receive adequate care [23]. Keeping this in mind, and considering the effectiveness of breast milk against gram-negative and positive bacteria [24], this study aims to determine the topical effect of breast milk on the healing of the episiotomy site in primiparous women at risk of infection.
Materials and Methods
This is a randomized clinical trial. This study was conducted on 78 primiparous women who were admitted to the delivery rooms of two teaching hospitals affiliated with Mashhad University of Medical Sciences, Mashhad, Iran, in 2021-2022. The eligible participants were randomly assigned to two groups of intervention (group B) and control (group A) using the Sealed Envelope website. The inclusion criteria were being primiparous, singleton pregnancy, cephalic presentation, gestational age of 38-42 weeks, no bleeding or fetal distress in labor, no special diet (vegetarian or under diet), no smoking and use of special drugs (e.g. anticoagulants, antidepressants, benzodiazepines, alcohol), no history of reconstructive surgery, vaginal and perineum lesions, and having at least two concurrent predisposing factors of infection (delivery process for >8 hours, hospitalization after delivery for >5 days, Body Mass Index (BMI) >28 kg/m2, vaginal examination >3 times per day, age >30 years, episiotomy length >3 cm, premature rupture of membranes in >18 hours before delivery, experience <10 years in delivery, chronic hypertension, anemia, overt or gestational diabetes treated with insulin and metformin, and immunosuppressive drug use) [9]. The exclusion criteria were the infant’s death, birth of an infant with an abnormality, the mother’s non-visit of the midwifery clinic on days 5 and 10, non-adherence to health instructions given by the researcher (at least one day), puerperal fever, third- or fourth-degree perineal tear, episiotomy other than mediolateral, curettage or erosion after delivery, and use of anticoagulants, antidepressants, benzodiazepines, and taking other measures for wound healing (e.g. the use of herbal medicines).
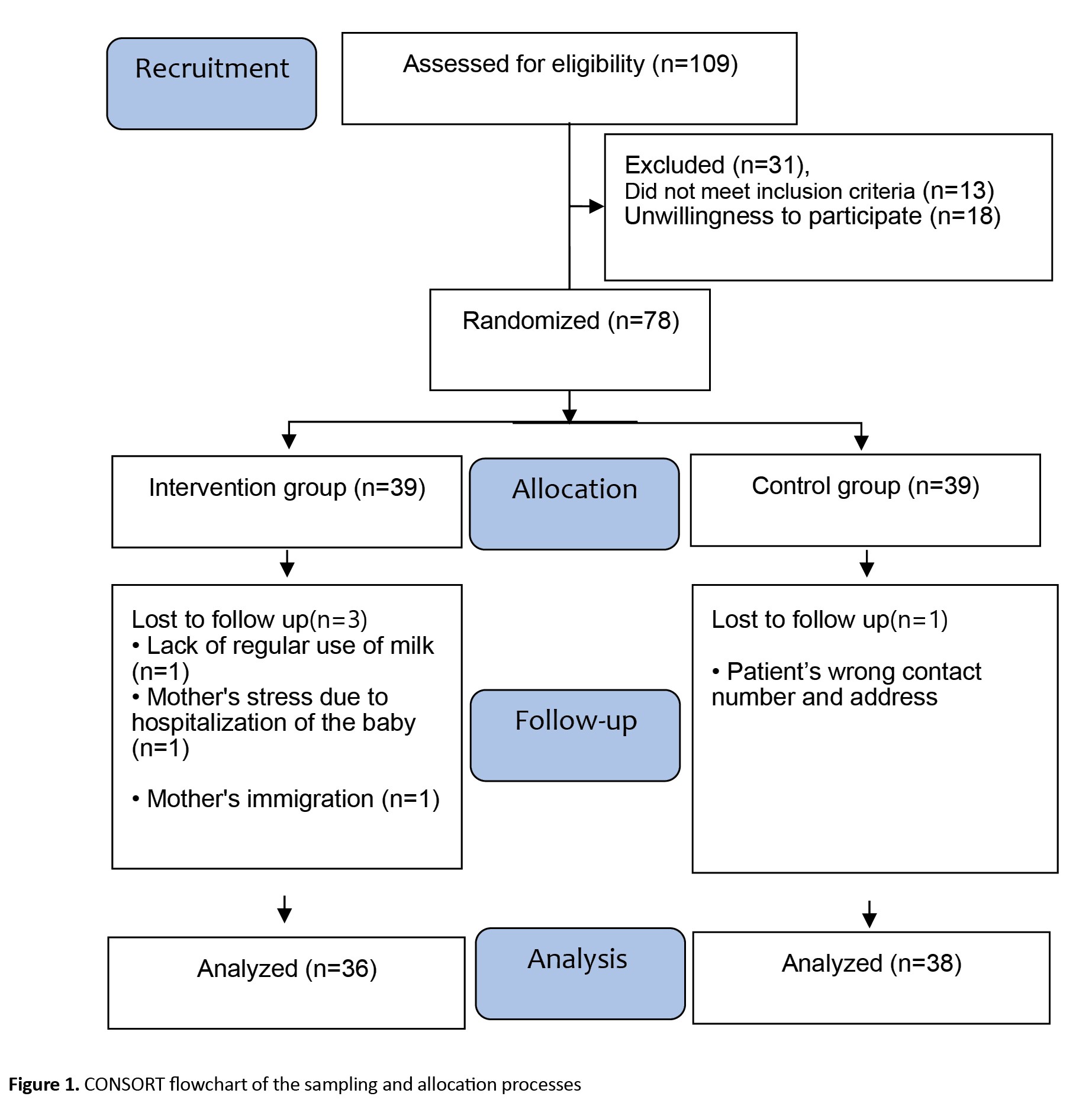
The sample size was estimated using a pilot study on 20 individuals (10 from the intervention group and 10 from the control group) based on the Redness, Edema, Ecchymosis, Discharge, and Approximation (REEDA) criteria for the fifth and tenth days. The sample size was examined for each REEDA criterion in the two groups. The largest size belonged to bruising on day 10 and was equivalent to 35 per group at a 95% confidence interval (CI) with a test power of 80%. The mean REEDA score was 0.83 in the intervention group and 0.94 in the control group. Furthermore, the standard deviations of the intervention group (S1) and control group (S2) were 0.11 and 0.20, respectively. The estimated values were increased by 10% to increase certainty and consider possible dropout during the research, and reached 39 per group. The eligible participants were included in the study after being informed of the study objectives, assured of confidentiality, and signing a written consent form. During the study, four mothers were excluded from the study (Figure 1). Data collection tools included a demographic/obstetric form, the REEDA scale, and a sterile graduated swab to examine the length and depth of the episiotomy. The demographic/obstetric form surveyed six demographic items (age, woman’s and husband’s education levels, woman’s and husband’s jobs, monthly income) and six obstetric items (last menstrual period, history of abortion, history of Ectopic Pregnancy [EP], mother’s weight and height, and BMI). This questionnaire was used after determining its face and content validity based on the opinions of 10 faculty members of the School of Nursing and Midwifery. The REEDA scale is a valid tool to examine the degree of wound healing with five criteria: Redness, edema, ecchymosis, discharge, and approximation. Each criterion receives a score from 0 (absence) to 3 (severe state). The total score ranges from 0 (full healing) to 15 (no healing) [25]. Many studies in Iran have also used this tool since it covers all critical aspects in healing perineal wounds [26, 27]. The qualitative content validity of this tool in our study was confirmed based on the opinions of 10 faculty members of the School of Nursing and Midwifery. To confirm reliability, the REEDA scale was completed separately by two researchers with similar experience and educational level, and their agreement was confirmed with a coefficient of 0.9.
The researcher was present at the mother’s bedside during the active phase of labor. She completed the demographic and midwifery form on behalf of the mother through interview, observation, and examination. Furthermore, the length and depth of the episiotomy incision were measured and recorded using a sterile graduated swab immediately after delivery and removal of the placenta. During the episiotomy repair, the number of catgut chromic sutures for skin closure was recorded. After the healing of the episiotomy, all mothers received care and necessary information about personal hygiene (drying the perinea after going to the bathroom, keeping nails short, bathing, using a hair dryer on the suture site, changing menstrual pads after going to the bathroom, using normal saline irrigation solution after defecation, washing hands before and after breastfeeding, and expressing milk), and how to take care of the perineum and sutures. According to this routine care in the hospital, the control group was asked to wash with normal saline twice daily, every 12 hours, for 10 days. The intervention group was taught to wash with normal saline for 10 days, like the control group, and take 2 mL of their milk each time with a 5 mL syringe, drip milk on the perineal wound using a 2 mL needleless syringe (0.25 mL in the first three days), and then press the site gently with the sterile gauze for three minutes in such a way that the pain could be tolerated. The volume of milk for washing was based on Nuraini et al.’s study [19]. Two hours after delivery, the researcher used the REEDA scale to check the perineal wound healing under sufficient light when the mother was in the lithotomy position. The mothers of both groups received necessary explanations about completing the follow-up checklists (daily record of intervention implementation, health recommendations, eating status, and physical activity). They were recommended to visit the midwifery clinics where they gave birth for follow-up care on the 5th and 10th days of delivery. Thereafter, all participants received the normal saline serum and the follow-up checklists. In addition to the irrigation serum, the intervention group received 20 pieces of sterile dental gauze (2×2 cm) and two 5 cc syringes.
Data was analyzed by SPSS software, version 21 using descriptive statistics (mean, frequency, percentage), the chi-square test, Fisher’s exact test, Mann-Whitney U test, Friedman’s test, and independent t-test. The significance level was set at 0.05.
Results
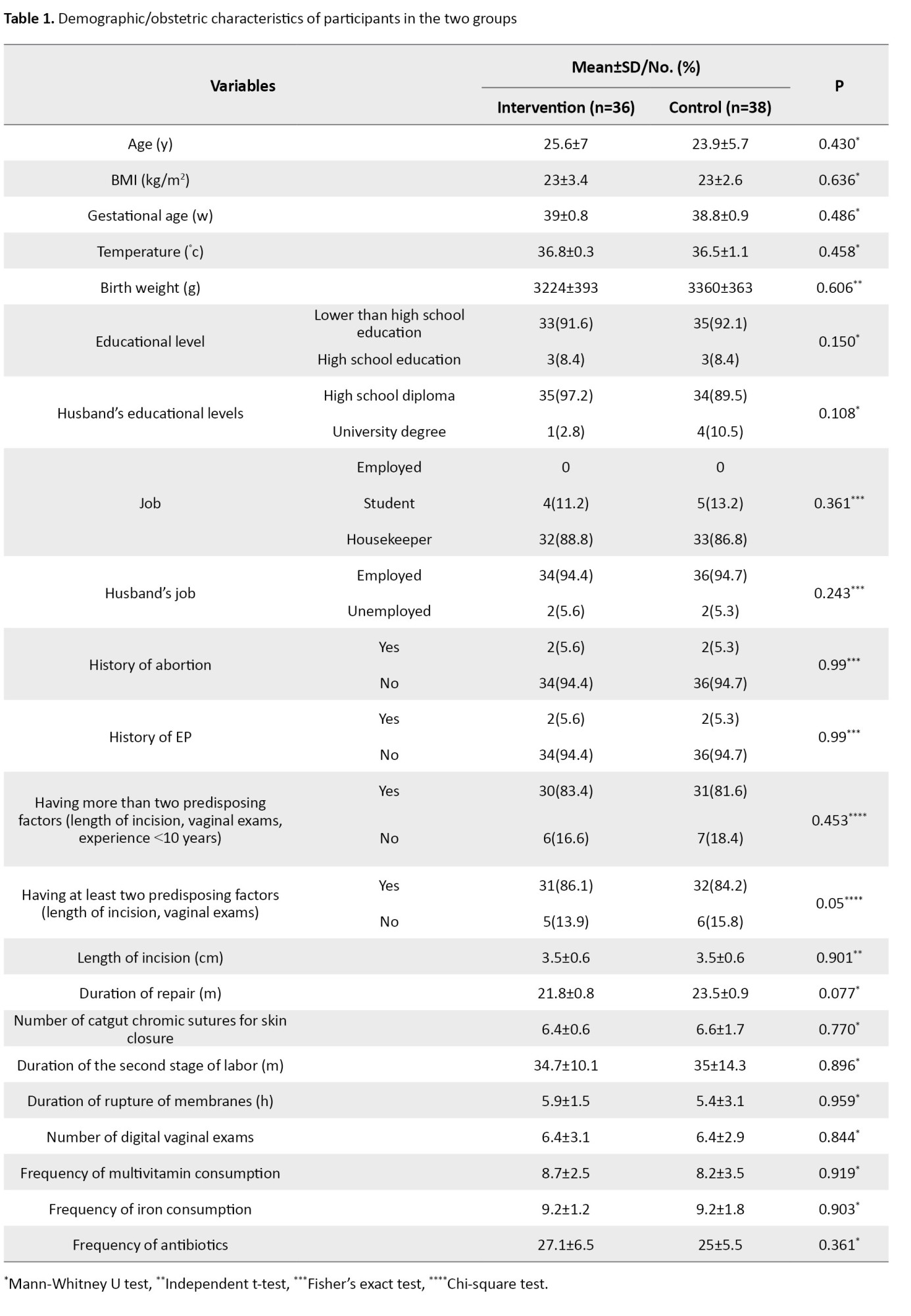
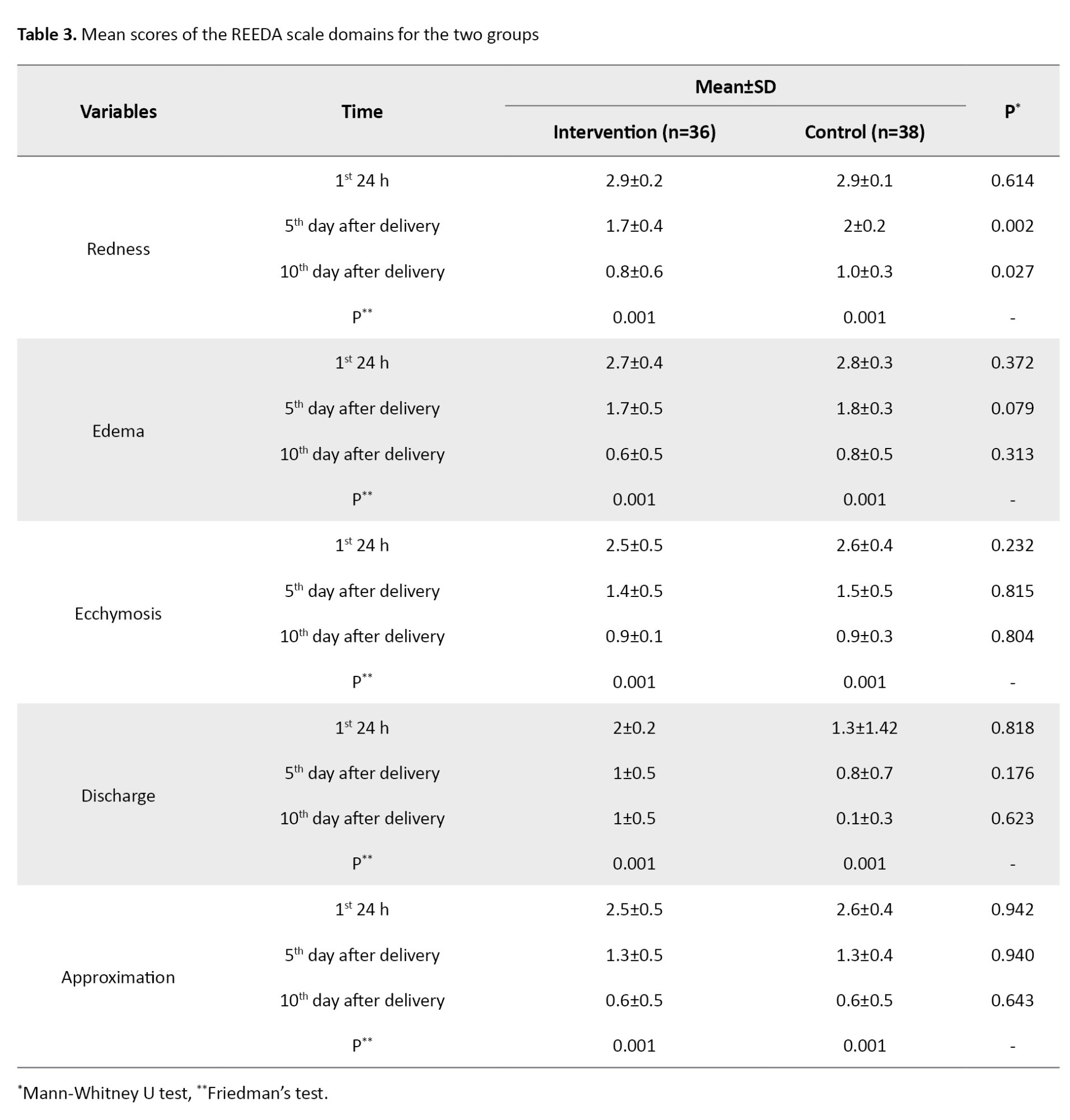
As shown in Table 1, the two groups were not significantly different regarding demographic/obstetric variables.
The mean total score of the REEDA scale for the two groups is shown in Table 2
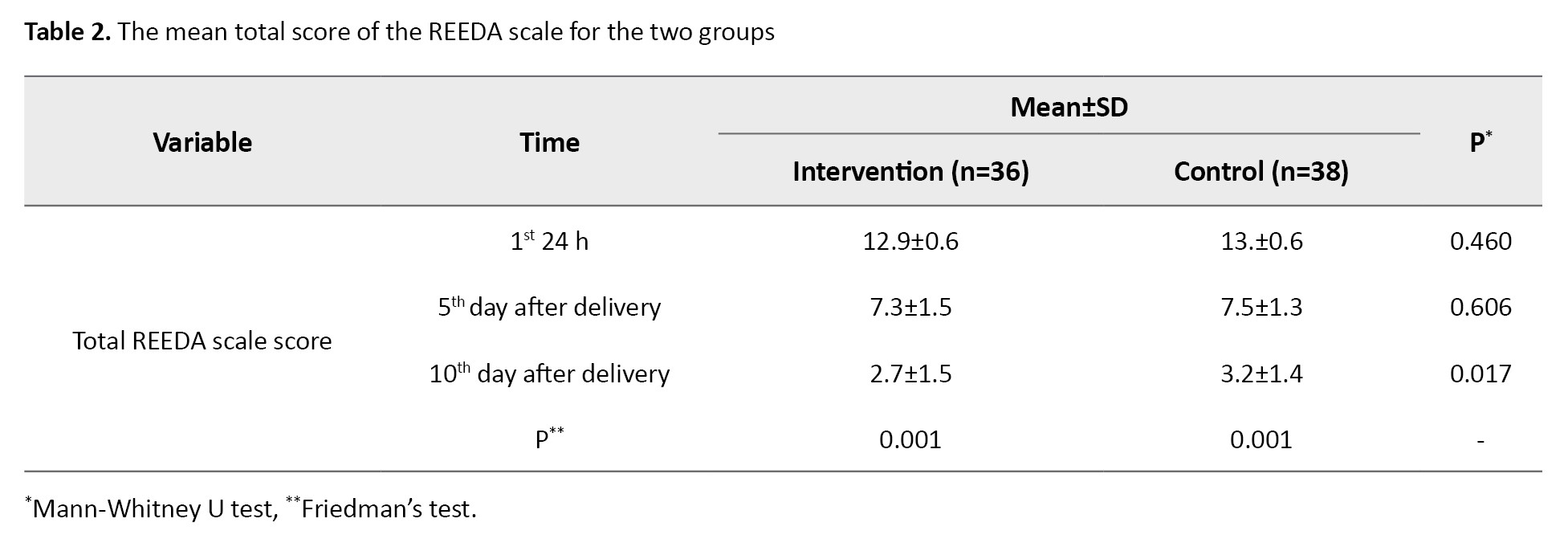
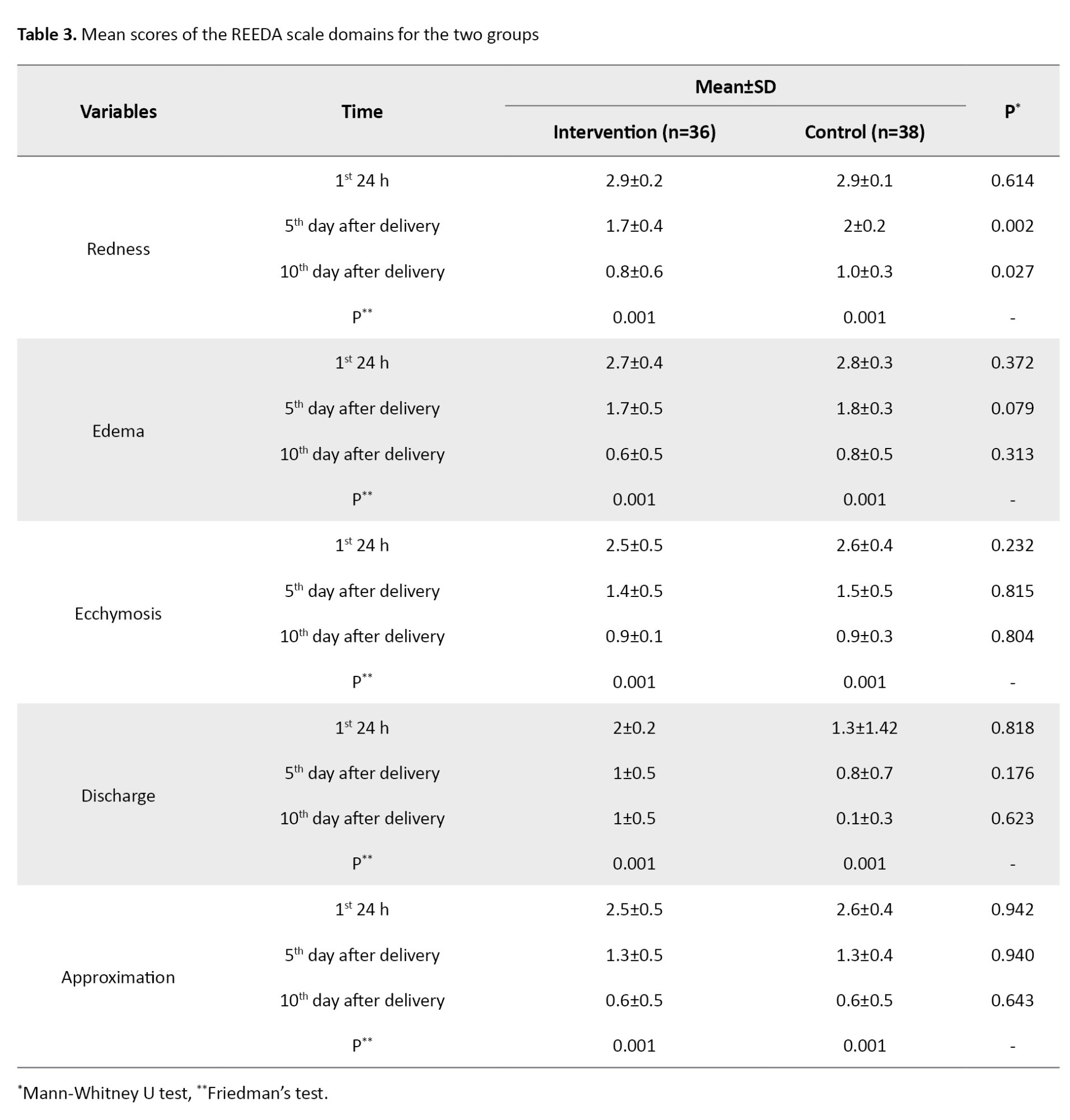
Based on the results, the total score was similar between the two groups before delivery and five days after delivery but there was a significant decline in the intervention group on the 10th day after delivery compared to the control group (P=0.017) (Table 2). The mean scores of the REEDA scale domains for the two groups are shown in Table 3.
Discussion
To our knowledge, this is the first study on the topical effect of breast milk on the healing of episiotomy site in primiparous women at risk of episiotomy site infection. Based on the results, the healing process of episiotomy wounds was significantly faster in the group that received topical breast milk on the tenth day after delivery than in the control group. Furthermore, there was significantly more redness around the wound site on the 5th and 10th days after delivery in the intervention than in the control group. The difference between groups was not significant in other REEDA criteria. Also, despite having at least two risk factors for episiotomy infection in participants, episiotomy site infection did not occur in any mothers in the intervention group compared to the control group.
The frequency of episiotomy site infection (grade 2 and higher) is reported to be less than 1% [28]. This rate is very diverse in different hospitals because many factors can affect it, such as hygiene, medical problems (e.g. diabetes), number of vaginal examinations, and the duration of the second stage of labor [8, 16]. In our study, all participants had two common risk factors (Length of incision, vaginal exams). Also, they were homogeneous in terms of three risk factors (Length of incision, vaginal exams, and experience <10 years) and did not have any other risk. A study on 60 Indonesian women with perineal wounds evaluated the effect of topical breast milk. At the end of the seventh day, the intervention group’s wound healing rate (obtaining a score of 7) was more than twice that of the control group, in which perineal washing was done using antiseptic soap [19]. This is consistent with the results of our study. The mentioned study did not investigate and compare the total healing score between the two groups, and only mentioned the percentage of improvement; hence, it was impossible to compare the healing scores between the two studies. However, no high wound healing was reported in our study, probably due to the difference in the participants. In our study, participants had predisposing factors for episiotomy site infection, whereas the participants in the mentioned study did not have such factors.
In the present study, wound site redness was the only REEDA criterion that showed a significant difference between the intervention and control groups, which indicated more redness in the intervention group on the 5th and 10th days after delivery. In a study on the healing of the episiotomy site, most of the REEDA criteria showed improvement [16]. The discrepancy can be due to differences in participants.
In a study on 40 postnatal women [21], the effect of topical milk was reported to be effective in episiotomy wound healing, and they reported mean score of 5 degrees of wound healing compared to the control group. The participants with the risk factor of infection were excluded, and the method was not explained clearly; for example, the amount of consumed milk and the routine care in the control group were not clear. In our study, we examined the healing of the episiotomy site for 10 days after delivery, which is the time of the second visit for postpartum care based on the national guidelines. In the mentioned study’s follow-up period, 5 degrees of healing based on the REEDA scale occurred until the fifth day after delivery, and about 10 degrees of healing occurred until the tenth day. No episiotomy site infection was reported in their intervention group. Additionally, in this study, the rate of wound infection was reported.
It should be noted that during the wound healing process, monocytes enter the site after 48-72 hours and produce cytokines such as Fibroblast Growth Factors (FGFs), Epidermal Growth Factors (EGFs), Interleukin-6 (IL-6), and IL-1, which play roles in the third stage of healing or proliferation after differentiating into macrophages [29]. Human milk contains countless cytokines, including FGF, EGF, and IL-6 [25]. Furthermore, it is antimicrobial and limits the growth of Escherichia coli [30]. An animal study reported that topical milk ointment (prepared from cow’s milk) caused faster skin wound healing, and that 5% milk ointment achieved quicker wound healing compared to phenytoin ointment. This histological study confirmed the increase in collagen tissue and fibroblasts and the reduction of inflammatory evidence in milk ointment users [24].
The strength of our study was the use of breast milk for the healing of episiotomy site in women prone to episiotomy site infection with maximum control of variables affecting the infection. The researcher was present at the patient’s bedside in the active phase. However, there were limitations such as the impossibility of precise control over the topical use of milk. In this regard, future studies are recommended to use milk ointment with a specific percentage. Different types of episiotomy site infection risk factors, diets, and the immune systems of the participants were other limitations of the present study. To overcome it, random group assignment was used.
In conclusion, the topical use of breast milk is effective in healing episiotomy wounds. Since breast milk is available and cost-effective with no side effects, mothers, especially those prone to episiotomy site infection, can receive the necessary training about the topical use of breast milk to heal the episiotomy wound quickly.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran (Code: IR.MUMS.NURSE.REC.1399.071) and registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20210121050098N1). The procedures were in accordance with the ethical principles of the Declaration of Helsinki. All participants signed a written informed consent form before participating in this study.
Funding
This article was extracted from the master’s thesis of the Kobra Sadat Hossaini, approved by the Department of Midwifery, School of Nursing and Midwifery, Mashhad University of Medical Sciences and financially supported by Mashhad University of Medical Sciences, Mashhad, Iran (Grant No.: 991239).
Authors' contributions
Conceptualization and investigation: Kobra Sadat Hossaini, Nahid Jahani Shoorab, Sediqah ShariatMoghani and Farideh Akhlaghi; Data collection and writing the initial draft: Kobra Sadat Hossaini; Data analyses: Reza Mazlom; Final approval: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research of Mashhad University of Medical Sciences, Mashhad, Iran, for the financial support, and the staff of Ommol-banin and Hasheminejad hospitals and all participants for their cooperation in this study.
References
Episiotomy is an incision in the perineum performed to widen the vaginal opening at the second stage of delivery. The American College of Obstetricians and Gynecologists (ACOG) recommends elective episiotomy over routine episiotomy [1]. The studies have reported the episiotomy rates of 19.4% in South Brazil [2], 49% in Ethiopia [3], 92.7% in Romania [4], 95% in Iran [5], and 67% in the Middle East [6]. The repair stage of episiotomy wound healing starts in the first 48 hours and can last for 14 days, increasing the resistance in the newly-created tissue of the healing site during the collagen structure remodeling [7]. Infection of the episiotomy site and delayed healing are among the complications caused by its special anatomical position and proximity to the anus [8]. Improper wound healing and wound dehiscence due to infection usually occur 7-10 days after healing [9]. Delay in the healing of the episiotomy site leads to unpleasant anatomical results, such as skin sensitivity, vaginal narrowing, vaginal prolapse, vaginal opening asymmetry, rectovaginal fistulas, and a higher risk of site infection [10, 11]. Episiotomy does not heal fully up to three weeks after delivery, and wound healing is delayed in 41% of cases [12]. Perineal infections and deformities caused by the delay in perineal healing are the causes of marital and psycho-social problems due to sexual disorders [13]. Accelerating wound healing can reduce pain in the perineal site [14] and make women recover faster after delivery and return to daily activities [12]. Several factors, such as diabetes, vaginal examinations, vaginal hematoma, length of episiotomy incision >3 cm, and anemia, delay recovery [15, 16]. Numerous medicinal methods have been proposed to improve and speed up wound healing, such as topical phenytoin, gentamicin solutions [16], or herbal medicines [17], but the side effects of chemical or even herbal medicines limit their use [14].
Human milk is rich in leukocytes, which cause active immunity. The complement system, macrophages, lymphocytes, lactoferrin, lactoperoxidase, and lysozymes are defense factors in colostrum and breast milk [18]. The topical use of breast milk for perineal healing in the first to seventh days after delivery has been reported to be more effective than disinfection with soap [19]. Some studies have also reported that the topical use of breast milk on the episiotomy site led to higher healing [20, 21]. These studies assessed episiotomy healing at the seventh day of postpartum, while the proliferative phase is performed at least until the second week, and the control of the episiotomy site is recommended in the second week after delivery [22]. Additionally, the studies have only included women without infection risk factors. Mothers who are exposed to infection are not able to breastfeed and take care of their infant. In a study of late repair of episiotomy, 73.3% of neonates did not receive adequate care [23]. Keeping this in mind, and considering the effectiveness of breast milk against gram-negative and positive bacteria [24], this study aims to determine the topical effect of breast milk on the healing of the episiotomy site in primiparous women at risk of infection.
Materials and Methods
This is a randomized clinical trial. This study was conducted on 78 primiparous women who were admitted to the delivery rooms of two teaching hospitals affiliated with Mashhad University of Medical Sciences, Mashhad, Iran, in 2021-2022. The eligible participants were randomly assigned to two groups of intervention (group B) and control (group A) using the Sealed Envelope website. The inclusion criteria were being primiparous, singleton pregnancy, cephalic presentation, gestational age of 38-42 weeks, no bleeding or fetal distress in labor, no special diet (vegetarian or under diet), no smoking and use of special drugs (e.g. anticoagulants, antidepressants, benzodiazepines, alcohol), no history of reconstructive surgery, vaginal and perineum lesions, and having at least two concurrent predisposing factors of infection (delivery process for >8 hours, hospitalization after delivery for >5 days, Body Mass Index (BMI) >28 kg/m2, vaginal examination >3 times per day, age >30 years, episiotomy length >3 cm, premature rupture of membranes in >18 hours before delivery, experience <10 years in delivery, chronic hypertension, anemia, overt or gestational diabetes treated with insulin and metformin, and immunosuppressive drug use) [9]. The exclusion criteria were the infant’s death, birth of an infant with an abnormality, the mother’s non-visit of the midwifery clinic on days 5 and 10, non-adherence to health instructions given by the researcher (at least one day), puerperal fever, third- or fourth-degree perineal tear, episiotomy other than mediolateral, curettage or erosion after delivery, and use of anticoagulants, antidepressants, benzodiazepines, and taking other measures for wound healing (e.g. the use of herbal medicines).
The sample size was estimated using a pilot study on 20 individuals (10 from the intervention group and 10 from the control group) based on the Redness, Edema, Ecchymosis, Discharge, and Approximation (REEDA) criteria for the fifth and tenth days. The sample size was examined for each REEDA criterion in the two groups. The largest size belonged to bruising on day 10 and was equivalent to 35 per group at a 95% confidence interval (CI) with a test power of 80%. The mean REEDA score was 0.83 in the intervention group and 0.94 in the control group. Furthermore, the standard deviations of the intervention group (S1) and control group (S2) were 0.11 and 0.20, respectively. The estimated values were increased by 10% to increase certainty and consider possible dropout during the research, and reached 39 per group. The eligible participants were included in the study after being informed of the study objectives, assured of confidentiality, and signing a written consent form. During the study, four mothers were excluded from the study (Figure 1). Data collection tools included a demographic/obstetric form, the REEDA scale, and a sterile graduated swab to examine the length and depth of the episiotomy. The demographic/obstetric form surveyed six demographic items (age, woman’s and husband’s education levels, woman’s and husband’s jobs, monthly income) and six obstetric items (last menstrual period, history of abortion, history of Ectopic Pregnancy [EP], mother’s weight and height, and BMI). This questionnaire was used after determining its face and content validity based on the opinions of 10 faculty members of the School of Nursing and Midwifery. The REEDA scale is a valid tool to examine the degree of wound healing with five criteria: Redness, edema, ecchymosis, discharge, and approximation. Each criterion receives a score from 0 (absence) to 3 (severe state). The total score ranges from 0 (full healing) to 15 (no healing) [25]. Many studies in Iran have also used this tool since it covers all critical aspects in healing perineal wounds [26, 27]. The qualitative content validity of this tool in our study was confirmed based on the opinions of 10 faculty members of the School of Nursing and Midwifery. To confirm reliability, the REEDA scale was completed separately by two researchers with similar experience and educational level, and their agreement was confirmed with a coefficient of 0.9.
The researcher was present at the mother’s bedside during the active phase of labor. She completed the demographic and midwifery form on behalf of the mother through interview, observation, and examination. Furthermore, the length and depth of the episiotomy incision were measured and recorded using a sterile graduated swab immediately after delivery and removal of the placenta. During the episiotomy repair, the number of catgut chromic sutures for skin closure was recorded. After the healing of the episiotomy, all mothers received care and necessary information about personal hygiene (drying the perinea after going to the bathroom, keeping nails short, bathing, using a hair dryer on the suture site, changing menstrual pads after going to the bathroom, using normal saline irrigation solution after defecation, washing hands before and after breastfeeding, and expressing milk), and how to take care of the perineum and sutures. According to this routine care in the hospital, the control group was asked to wash with normal saline twice daily, every 12 hours, for 10 days. The intervention group was taught to wash with normal saline for 10 days, like the control group, and take 2 mL of their milk each time with a 5 mL syringe, drip milk on the perineal wound using a 2 mL needleless syringe (0.25 mL in the first three days), and then press the site gently with the sterile gauze for three minutes in such a way that the pain could be tolerated. The volume of milk for washing was based on Nuraini et al.’s study [19]. Two hours after delivery, the researcher used the REEDA scale to check the perineal wound healing under sufficient light when the mother was in the lithotomy position. The mothers of both groups received necessary explanations about completing the follow-up checklists (daily record of intervention implementation, health recommendations, eating status, and physical activity). They were recommended to visit the midwifery clinics where they gave birth for follow-up care on the 5th and 10th days of delivery. Thereafter, all participants received the normal saline serum and the follow-up checklists. In addition to the irrigation serum, the intervention group received 20 pieces of sterile dental gauze (2×2 cm) and two 5 cc syringes.
Data was analyzed by SPSS software, version 21 using descriptive statistics (mean, frequency, percentage), the chi-square test, Fisher’s exact test, Mann-Whitney U test, Friedman’s test, and independent t-test. The significance level was set at 0.05.
Results
As shown in Table 1, the two groups were not significantly different regarding demographic/obstetric variables.
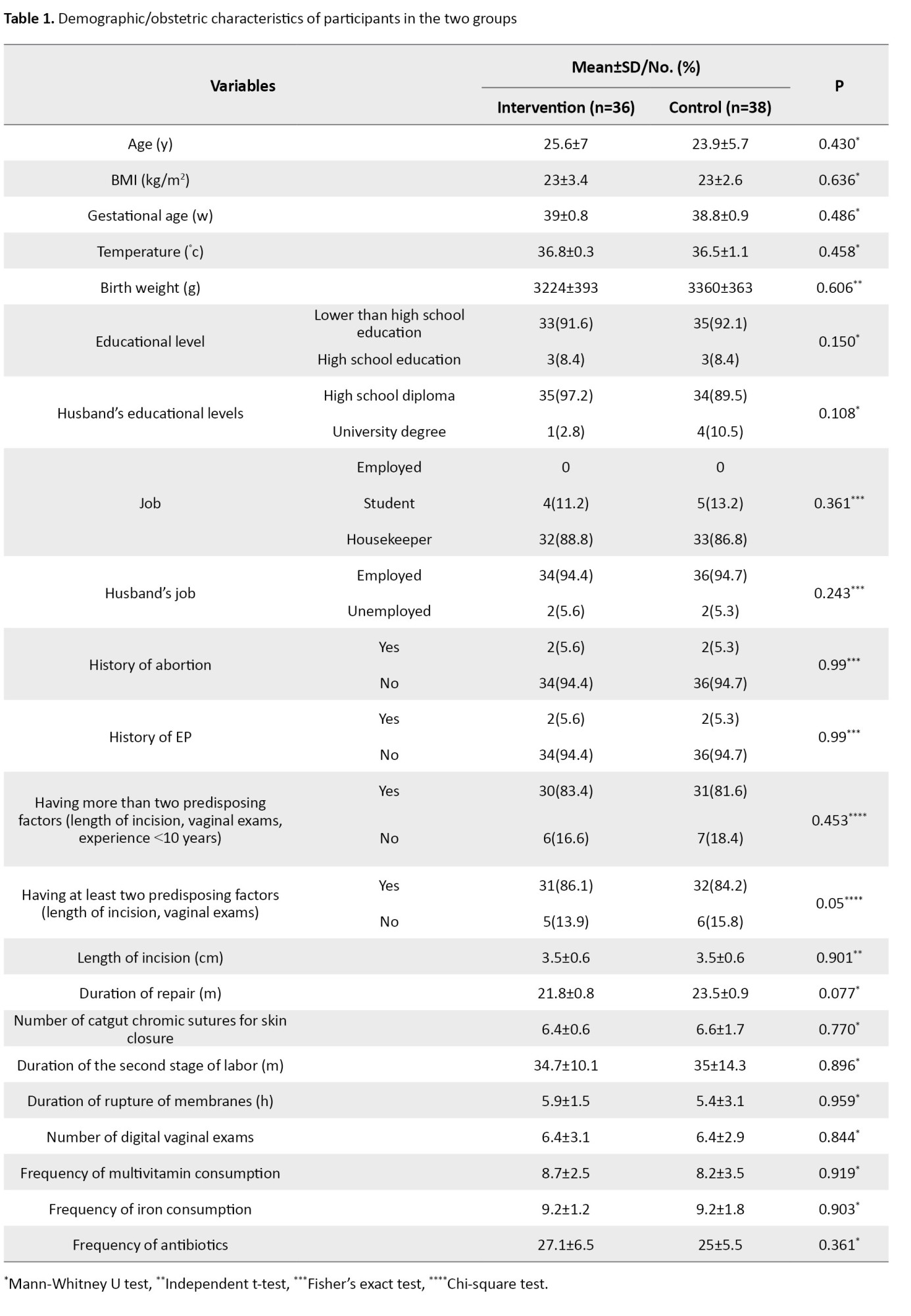
The mean total score of the REEDA scale for the two groups is shown in Table 2
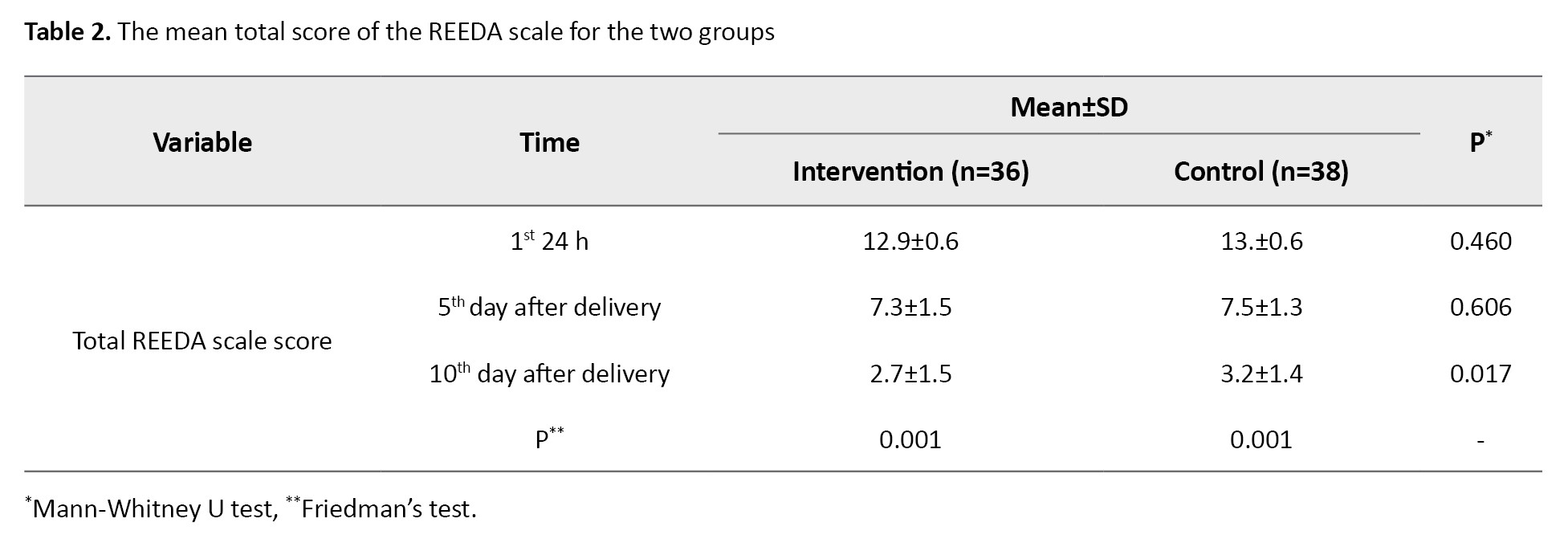
Based on the results, the total score was similar between the two groups before delivery and five days after delivery but there was a significant decline in the intervention group on the 10th day after delivery compared to the control group (P=0.017) (Table 2). The mean scores of the REEDA scale domains for the two groups are shown in Table 3.
Discussion
To our knowledge, this is the first study on the topical effect of breast milk on the healing of episiotomy site in primiparous women at risk of episiotomy site infection. Based on the results, the healing process of episiotomy wounds was significantly faster in the group that received topical breast milk on the tenth day after delivery than in the control group. Furthermore, there was significantly more redness around the wound site on the 5th and 10th days after delivery in the intervention than in the control group. The difference between groups was not significant in other REEDA criteria. Also, despite having at least two risk factors for episiotomy infection in participants, episiotomy site infection did not occur in any mothers in the intervention group compared to the control group.
The frequency of episiotomy site infection (grade 2 and higher) is reported to be less than 1% [28]. This rate is very diverse in different hospitals because many factors can affect it, such as hygiene, medical problems (e.g. diabetes), number of vaginal examinations, and the duration of the second stage of labor [8, 16]. In our study, all participants had two common risk factors (Length of incision, vaginal exams). Also, they were homogeneous in terms of three risk factors (Length of incision, vaginal exams, and experience <10 years) and did not have any other risk. A study on 60 Indonesian women with perineal wounds evaluated the effect of topical breast milk. At the end of the seventh day, the intervention group’s wound healing rate (obtaining a score of 7) was more than twice that of the control group, in which perineal washing was done using antiseptic soap [19]. This is consistent with the results of our study. The mentioned study did not investigate and compare the total healing score between the two groups, and only mentioned the percentage of improvement; hence, it was impossible to compare the healing scores between the two studies. However, no high wound healing was reported in our study, probably due to the difference in the participants. In our study, participants had predisposing factors for episiotomy site infection, whereas the participants in the mentioned study did not have such factors.
In the present study, wound site redness was the only REEDA criterion that showed a significant difference between the intervention and control groups, which indicated more redness in the intervention group on the 5th and 10th days after delivery. In a study on the healing of the episiotomy site, most of the REEDA criteria showed improvement [16]. The discrepancy can be due to differences in participants.
In a study on 40 postnatal women [21], the effect of topical milk was reported to be effective in episiotomy wound healing, and they reported mean score of 5 degrees of wound healing compared to the control group. The participants with the risk factor of infection were excluded, and the method was not explained clearly; for example, the amount of consumed milk and the routine care in the control group were not clear. In our study, we examined the healing of the episiotomy site for 10 days after delivery, which is the time of the second visit for postpartum care based on the national guidelines. In the mentioned study’s follow-up period, 5 degrees of healing based on the REEDA scale occurred until the fifth day after delivery, and about 10 degrees of healing occurred until the tenth day. No episiotomy site infection was reported in their intervention group. Additionally, in this study, the rate of wound infection was reported.
It should be noted that during the wound healing process, monocytes enter the site after 48-72 hours and produce cytokines such as Fibroblast Growth Factors (FGFs), Epidermal Growth Factors (EGFs), Interleukin-6 (IL-6), and IL-1, which play roles in the third stage of healing or proliferation after differentiating into macrophages [29]. Human milk contains countless cytokines, including FGF, EGF, and IL-6 [25]. Furthermore, it is antimicrobial and limits the growth of Escherichia coli [30]. An animal study reported that topical milk ointment (prepared from cow’s milk) caused faster skin wound healing, and that 5% milk ointment achieved quicker wound healing compared to phenytoin ointment. This histological study confirmed the increase in collagen tissue and fibroblasts and the reduction of inflammatory evidence in milk ointment users [24].
The strength of our study was the use of breast milk for the healing of episiotomy site in women prone to episiotomy site infection with maximum control of variables affecting the infection. The researcher was present at the patient’s bedside in the active phase. However, there were limitations such as the impossibility of precise control over the topical use of milk. In this regard, future studies are recommended to use milk ointment with a specific percentage. Different types of episiotomy site infection risk factors, diets, and the immune systems of the participants were other limitations of the present study. To overcome it, random group assignment was used.
In conclusion, the topical use of breast milk is effective in healing episiotomy wounds. Since breast milk is available and cost-effective with no side effects, mothers, especially those prone to episiotomy site infection, can receive the necessary training about the topical use of breast milk to heal the episiotomy wound quickly.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran (Code: IR.MUMS.NURSE.REC.1399.071) and registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20210121050098N1). The procedures were in accordance with the ethical principles of the Declaration of Helsinki. All participants signed a written informed consent form before participating in this study.
Funding
This article was extracted from the master’s thesis of the Kobra Sadat Hossaini, approved by the Department of Midwifery, School of Nursing and Midwifery, Mashhad University of Medical Sciences and financially supported by Mashhad University of Medical Sciences, Mashhad, Iran (Grant No.: 991239).
Authors' contributions
Conceptualization and investigation: Kobra Sadat Hossaini, Nahid Jahani Shoorab, Sediqah ShariatMoghani and Farideh Akhlaghi; Data collection and writing the initial draft: Kobra Sadat Hossaini; Data analyses: Reza Mazlom; Final approval: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research of Mashhad University of Medical Sciences, Mashhad, Iran, for the financial support, and the staff of Ommol-banin and Hasheminejad hospitals and all participants for their cooperation in this study.
References
- Modi DA, Vaishnav PP. Routine versus selective use of episiotomy in primigravida: A prospective non-randomized case-control study. Int J Reprod Contracept Obstet Gynecol. 2020; 9(3):1003-6. [DOI:10.18203/2320-1770.ijrcog20200864]
- Cesar JA, Marmitt LP, Mendoza-Sassi RA. Episiotomy in Southern Brazil: Prevalence, trend, and associated factors. Rev Saude Publica. 2022; 56:26. [DOI:10.11606/s1518-8787.2022056003908] [PMID]
- Kebede E, Fantahun Y, Hassen S. Prevalence of episiotomy and factors associated with its practice in three teaching hospitals, Addis Ababa, Ethiopia. Ethiopian J Reprod Health. 2023; 15(2):47-58. [DOI:10.69614/ejrh.v15i2.653]
- Azu TD, Abraham SA, Doe PF, Amoadu M, Owusu G. Prevalence and predictors of episiotomy among puerperal women accessing postnatal care in the Kumasi Metropolis. BMC Pregnancy Childbirth. 2024; 24(1):750. [DOI:10.1186/s12884-024-06967-1] [PMID]
- Abedzadeh-Kalahroudi M, Talebian A, Sadat Z, Mesdaghinia E. Perineal trauma: Incidence and its risk factors. J Obstet Gynaecol. 2019; 39(2):206-11. [DOI:10.1080/01443615.2018.1476473] [PMID]
- Ghiasvand M, Nahidi F, Sedigh Mobarakabadi S, Broumandnia N, Sharifnia H. Prevalence and meta-analysis of episiotomy in the Middle East. Iran J Obstet Gynecol Infertil. 2021; 24(4):90-9. [DOI:10.22038/ijogi.2021.18439]
- Orlińska K, Komosińska-Vassev K, Olczyk K, Glaesel M, Olczyk P. Wound healing-characteristics of the ideal dressing. Ann Acad Med Siles. 2023; 77:197-203. [DOI:10.18794/aams/173203]
- Okeahialam NA, Thakar R, Sultan AH. Postpartum perineal wound infection and its effect on anal sphincter integrity: Results of a prospective observational study. Acta Obstet Gynecol Scand. 2023; 102(4):473-9. [DOI:10.1111/aogs.14515] [PMID]
- Prasad I, Sinha S, Singh S, Agarwal M, Asiya A. A catastrophic outcome of ineffectual episiotomy causing acquired vaginal atresia: A case report. Cureus. 2023; 15(5):e39574. [DOI:10.7759/cureus.39574] [PMID]
- Laki E, Torkzahrani S, Mojab F, Heydari A, Soltani Kermanshahi M. [The effect frankincense ointment on pain intensity and episiotomy wound healing in primiparous women (Persian)]. Iran J Obstet Gynecol Infertil. 2019; 22(2):42-51. [DOI:10.22038/ijogi.2019.13201]
- Jahani Shourab N, Mirteimouri M, Latifnejad Roudsari R. [A case series of severe perineal lacerations during normal childbirth (Persian)]. The Iranian J Obstet Gynecol Infertil. 2018; 21(8):103-14. [DOI:10.22038/ijogi.2018.11978]
- Goodarzi G, Rajabian S, Ahmadian M, Kalateh A. Comparing the incidence of episiotomy site infection in two groups of primiparas with and without taking prophylactic antibiotics after normal vaginal delivery referred to bent al-huda hospital in Bojnourd. J Obstet Gynecol Cancer Res. 2020; 5(2):31-8. [DOI:10.30699/jogcr.5.2.31]
- Jahani Shoorab N, Mirteimouri M, Taghipour A, Latifnejad Roudsari R. Women's experiences of emotional recovery from childbirth-related perineal trauma: A qualitative content analysis. Int J Community Based Nurs Midwifery. 2019; 7(3):181-91. [DOI:10.30476/IJCBNM.2019.44993] [PMID]
- Moradi M, Niazi A, Mazloumi E, Mousavi SF, Lopez V. Effect of lavender on episiotomy wound healing and pain relief: A systematic review. Evidence Based Care. 2020; 10(1):61-9. [DOI:10.22038/ebcj.2020.46285.2265]
- Jahani Shoorab N, Taghipour A, Esmaily H, Latifnejad Roudsari R. Development and psychometric properties of the women's recovery of postnatal perineal injuries questionnaire (WRPPIQ). Int J Community Based Nurs Midwifery. 2020; 8(4):311-23. [DOI:10.30476/ijcbnm.2020.85610.1279] [PMID]
- Cai C, Shan S, Chen X, Yao X, Liu Y, Jiang H. Analysis of risk factors and prediction model construction for poor healing of perineal wounds after vaginal delivery: A retrospective case-control study. Int J Nurs Stud Adv. 2025; 8:100326. [DOI:10.1016/j.ijnsa.2025.100326] [PMID]
- Sayahi M, Jahangirimehr A, Hatami Manesh Z, Mojab F, Nikbina M. The effect of Camellia sinensis ointment on perineal pain and episiotomy wound healing in primiparous women: A triple-blind randomized clinical trial. Plos One. 2024; 19(8):e0305048. [DOI:10.1371/journal.pone.0305048] [PMID]
- Demirtaş MS, Yalçın SS. The use of human milk for therapeutic purposes other than nutrition. Turk Arch Pediatr. 2022; 57(3):255-66. [DOI:10.5152/TurkArchPediatr.2022.22075] [PMID]
- Nuraini S, Saadah S, Rismawati S. The effect of breastmilk topical on perineal wound healing on 1-7 days postpartum mothe. MANR. 2019; 1(2):68-75. [DOI:10.31983/manr.v1i2.5288]
- Admasari Y, Santoso B, Suherni T, Mashoedi ID, Mardiyono M. Breast milk as an alternative for postpartum perineal care. Belitung Nur J. 2017; 3(3):238-45. [DOI:10.33546/bnj.101]
- Patel A, Makwana A, Tiwari A. Effect of topical application of breast milk on episiotomy wound healing: A quasi-experimental study. J Clin Diagn Res. 2023; 17(5):LC24-7. [DOI:10.7860/JCDR/2023/60358.17886]
- Spielman AF, Griffin MF, Parker J, Cotterell AC, Wan DC, Longaker MT. Beyond the scar: A basic science review of wound remodeling. Adv Wound Care. 2023; 12(2):57-67. [DOI:10.1089/wound.2022.0049] [PMID]
- Tessier JM, Sanders J, Sartelli M, Ulrych J, De Simone B, Grabowski J, et al. Necrotizing soft tissue infections: A focused review of pathophysiology, diagnosis, operative management, antimicrobial therapy, and pediatrics. Surg Infect. 2020; 21(2):81-93. [DOI:10.1089/sur.2019.219] [PMID]
- Steen M, Cooper K. A tool for assessing perineal trauma. J Wound Care. 1997; 6(9):432-6. [DOI:10.12968/jowc.1997.6.9.432] [PMID]
- Azhari S, Aradmehr M, Rakhshandeh H, Tara F, Shakeri MT. [The effects of chamomile cream on wound healing of episiotomy in primiparous women (Persian)]. Iran J Obstet Gynecol Infertil. 2014; 17(93):16-26. [DOI:10.22038/ijogi.2014.2747]
- Taleb S, Saeedi M. The effect of the Verbascum Thapsus on episiotomy wound healing in nulliparous women: A randomized controlled trial. BMC Complement Med Ther. 2021; 21(1):166. [DOI:10.1186/s12906-021-03339-6] [PMID]
- Puissegur A, Accoceberry M, Rouzaire M, Pereira B, Herault M, Bruhat C, et al. Risk factors for perineal wound breakdown in early postpartum: A retrospective case-control study. J Clin Med. 2023; 12(8):3036. [DOI:10.3390/jcm12083036] [PMID]
- Takahashi T, Ueno HM, Yamaide F, Nakano T, Shiko Y, Kawasaki Y, et al. Comparison of 30 cytokines in human breast milk between 1989 and 2013 in Japan. Nutrients. 2023; 15(7):1735. [DOI:10.3390/nu15071735] [PMID]
- Yalçın SS, Demirtaş MS, Yalçın S. Breastfeeding while pregnant: A country-wide population study. Breastfeed Med. 2021; 16(10):827-34. [DOI:10.1089/bfm.2021.0073] [PMID]
- Singh A, Duche RT, Wandhare AG, Sian JK, Singh BP, Sihag MK, et al. Milk-derived antimicrobial peptides: Overview, applications, and future perspectives. Probiotics Antimicrob Proteins. 2023; 15(1):44-62. [Doi:10.1007/s12602-022-10004-y] [PMID]
Article Type : Research |
Subject:
Special
Received: 2024/08/14 | Accepted: 2024/11/30 | Published: 2025/09/8
Received: 2024/08/14 | Accepted: 2024/11/30 | Published: 2025/09/8
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |