Mon, Dec 1, 2025
Volume 34, Issue 3 (6-2024)
JHNM 2024, 34(3): 281-291 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aflaki T, Olfati F, Mirzadeh M, Jourabchi Z. The Effect of Education Based on Health Belief Model on Self-Care Behaviors of Women with High Blood Pressure in Pregnancy. JHNM 2024; 34 (3) :281-291
URL: http://hnmj.gums.ac.ir/article-1-2377-en.html
URL: http://hnmj.gums.ac.ir/article-1-2377-en.html
1- Midwifery (MS), Student Research Committee, Qazvin University of Medical Science, Qazvin, Iran.
2- Associate Professor, Department of Reproductive Health, Social Determinants of Health Research Center, Research Institute for Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran.
3- Assistant Professor, Department of Community Medicine, Metabolic Disease Research Center, Qazvin University of Medical Science, Qazvin, Iran.
4- Associate Professor, Department of Community Health, Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Science, Qazvin, Iran. ,zinat.jourabchi@ymail.com
2- Associate Professor, Department of Reproductive Health, Social Determinants of Health Research Center, Research Institute for Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran.
3- Assistant Professor, Department of Community Medicine, Metabolic Disease Research Center, Qazvin University of Medical Science, Qazvin, Iran.
4- Associate Professor, Department of Community Health, Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Science, Qazvin, Iran. ,
Keywords: Health belief model (HBM), Self-care behaviors, Hypertension in pregnancy, Chronic hypertension
Full-Text [PDF 644 kb]
(519 Downloads)
| Abstract (HTML) (1227 Views)
Full-Text: (841 Views)
Introduction
According to the American College of Obstetricians and Gynecologists (ACOG), “gestational hypertension” is defined as “systolic blood pressure above 140 and diastolic blood pressure above 90 mm Hg, which occurs after the 20th week of pregnancy (or within 12 weeks after delivery). This type of hypertension is without the presence of protein in the urine or dysfunction of internal organs such as the liver; however, if hypertension occurs before the 20th week of pregnancy and remains stable until 12 weeks after delivery, it is called “chronic hypertension”. If the systolic blood pressure is above 160 mm Hg or the diastolic blood pressure is above 110 mm Hg, it is called “severe hypertension” in pregnancy [1, 2]. The global prevalence of hypertension in pregnant women is reported to be about 5-10% [3, 4]. Prevalence of hypertension among pregnant women in the US is 13.8% [5]; in Ireland, about 6% [6], and in Iran, 6% [7]. Hypertension in pregnancy is an important risk factor for the mother and the fetus [3].
Many studies have shown the role of self-care in hypertension management [8, 9, 10]. Self-care behaviors can be one of the most important strategies to control blood pressure and maintain its normal level [11]. Self-care management for controlling blood pressure refers to the use of knowledge and skills to prevent the occurrence of hypertension or reduce its severity. Effective factors for self-care management of hypertension include: Correct and regular use of medications, lifestyle modification (such as following a low-salt and low-fat diet), performing regular sports activities, avoiding alcohol consumption, appropriate weight control, blood pressure measurement and control, managing and reducing stress, and giving importance to care and visiting doctors [12, 13]. Although many studies have shown the positive and favorable effect of self-care behaviors in controlling high hypertension, many people with hypertension in the world still do not follow self-care behaviors. It is suggested that self-care behaviors should be taught using appropriate educational programs and models in patients with hypertension [14, 15, 16, 17]. One of the prominent models in this field is the health belief model (HBM) which has six components of perceived sensitivity, perceived severity, perceived benefits, perceived barriers, cues to actions, and self-efficacy [18, 19]. A study in Iran showed the significant relationship of the components of perceived barriers, self-efficacy and cues to action with self-care behaviors in patients with hypertension, and recommended that the HBM-based educational programs should be developed to promote self-care behaviors to control high blood pressure [20]. On the other hand, the use of HBM can increase the self-efficacy of hypertensive patients; the increase in perceived sensitivity and severity of hypertensive patients can improve their self-care behaviors [21].
To our knowledge, there is no study on the effect of HBM-based educational programs on self-care behaviors of pregnant women with hypertension. Therefore, this study aims to assess the effectiveness of an HBM-based educational program in improving the self-care behaviors of pregnant women with hypertension.
Materials and Methods
This is a quasi-experimental study with a pre-test/post-test design that was conducted on women with hypertension in pregnancy who referred to one of the specialized women’s hospitals in Rasht, Iran, during January-August 2020. The sample size was determined to be 90 by considering the first type error level of 0.05, the second type error level of 0.2, the Mean±SD scores of 20.72±1.75 and 22.32±2.94 for systolic pressure [12], and a 20% sample drop. Eligible samples were selected using a convenience sampling method. The inclusion criteria were gestational age up to 28 weeks, blood pressure of ≥140 and ≥90, singleton pregnancy, absence of proteinuria and preeclampsia, no addiction to drugs, smoking and alcohol, no neurological and mental diseases according to medical records, not having abnormal bleeding, age <45 years, reading and writing literacy, and willingness to participate in the study. The exclusion criteria were unwillingness to continue participating in the study and withdrawing for any reason during the study process. The data collection tools included a demographic/obstetric form, an HBM questionnaire, and the hypertension in pregnancy self-care profile.
The demographic/obstetric form surveys age, weight, insurance status (based on the patient’s medical file), educational level, occupation, place of residence, economic status, wanted/unwanted pregnancy, time of previous delivery, history of infertility, history of using assisted reproductive technologies (ARTs), and information about blood pressure based on the self-reports. The HBM questionnaire was designed by the researcher according to a previous study [22] and the scoring method was based on Khorsandi et al.’s study [23]. The questionnaire had two parts. The first part included items measuring knowledge (6 items) and the second part with 42 items measured perceived sensitivity (6 items), perceived severity (6 items), perceived benefits (6 items), perceived barriers (6 items), cues to actions (6 items), and self-efficacy (6 items). The items were rated on a five-point Likert scale as 1 (completely disagree), 2 (disagree), 3 (no idea), 4 (agree), and 5 (completely agree). The total score ranges from 42 to 210, with higher scores indicating better status. To determine the validity of this tool, face validity and content validity were measured. The initial draft was sent to 11 faculty members and experts in midwifery and health education from Qazvin University of Medical Sciences. The content validity ratio (CVR) was obtained as 0.87 and the content validity index (CVI) was 0.95. To determine the reliability using Cronbach’s α coefficient, the initial draft was completed by 20 mothers with hypertension in pregnancy who were not among the samples. Cronbach’s α was obtained 0.83 for the knowledge subscale, 0.7 for perceived sensitivity, 0.83 for perceived severity, 0.7 for perceived benefits, 0.7 for perceived barriers, 0.7 for cues to actions, 0.78 for self-efficacy, and 0.74 for the whole scale. The hypertension in pregnancy self-care profile was developed based on the scale designed by Han et al. [24], and its Persian version was validated by Ghanei Gheshlagh et al. [25]. It had 19 items measuring hypertension self-care behaviors in 4 areas of diet/physical activity (9 items), drug regimen/physician visit (4 items), food labeling (2 items), disease/stress management (4 items). The items were rated on a four-point Likert scale as 1 (never), 2 (sometimes), 3 (often), and 4 (always). The score ranged 9-36 for diet/physical activity, 4-16 for drug regimen/ physician visit, 2-8 for food labeling, and 4-16 for disease/stress management. The total score ranged 19-76, with higher scores indicating higher self-care behaviors for hypertension in pregnancy. The CVI was 0.94. Moreover, Cronbach’s α was obtained 0.76 for diet/physical activity, 0.84 for drug regimen/doctor visit, 0.93 for food labeling, and 0.70 for disease/stress management, and 0.80 for the whole scale.
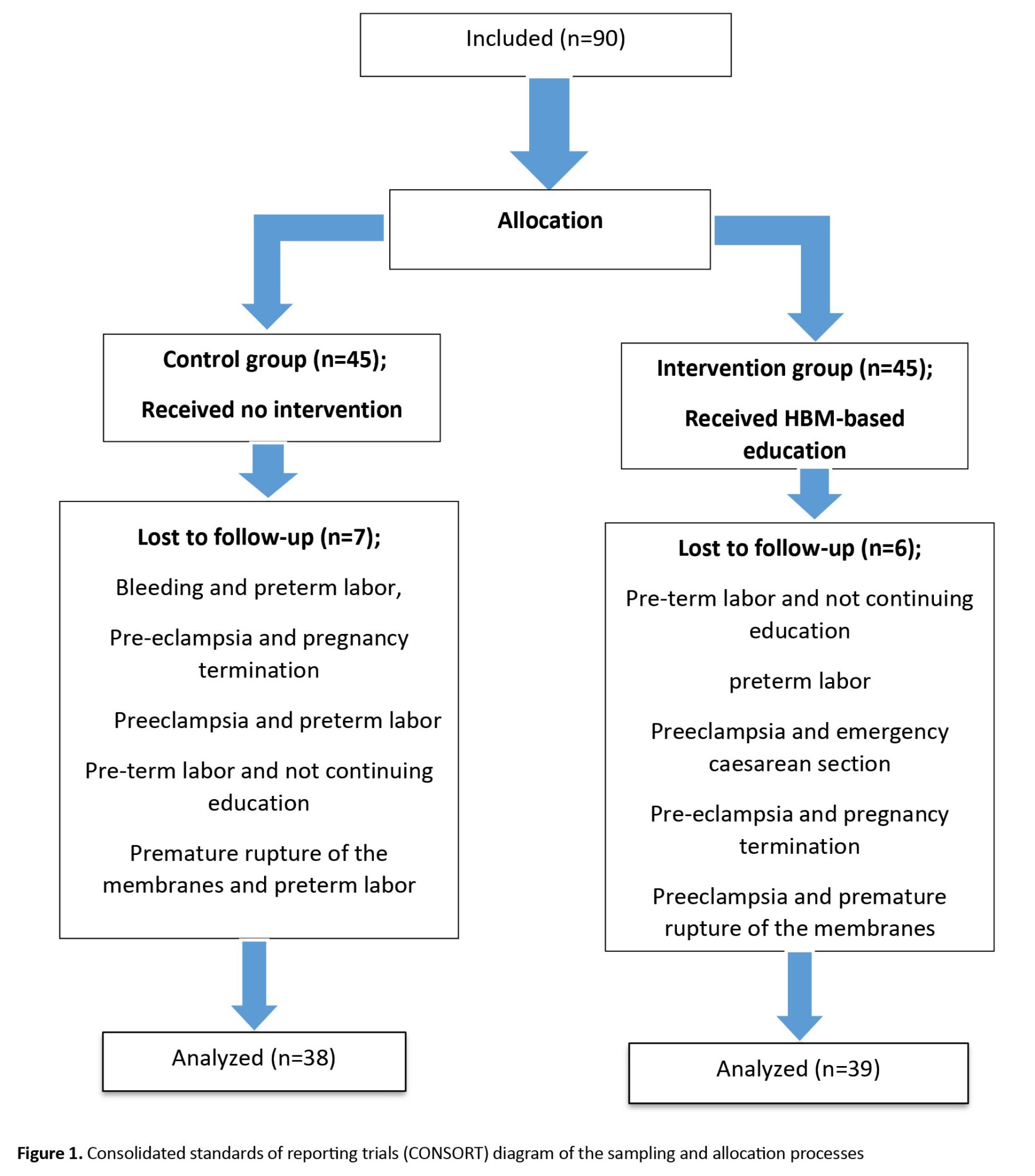
The participants were randomly divided into two groups of intervention and control using the random allocation software (Figure 1). Both groups received information from their health care providers during the study, while the intervention group was also given HBM-based education by the researcher. The content of the educational sessions was reviewed and approved by five faculty members of the schools of midwifery and health at Qazvin University of Medical Sciences (Table 1).
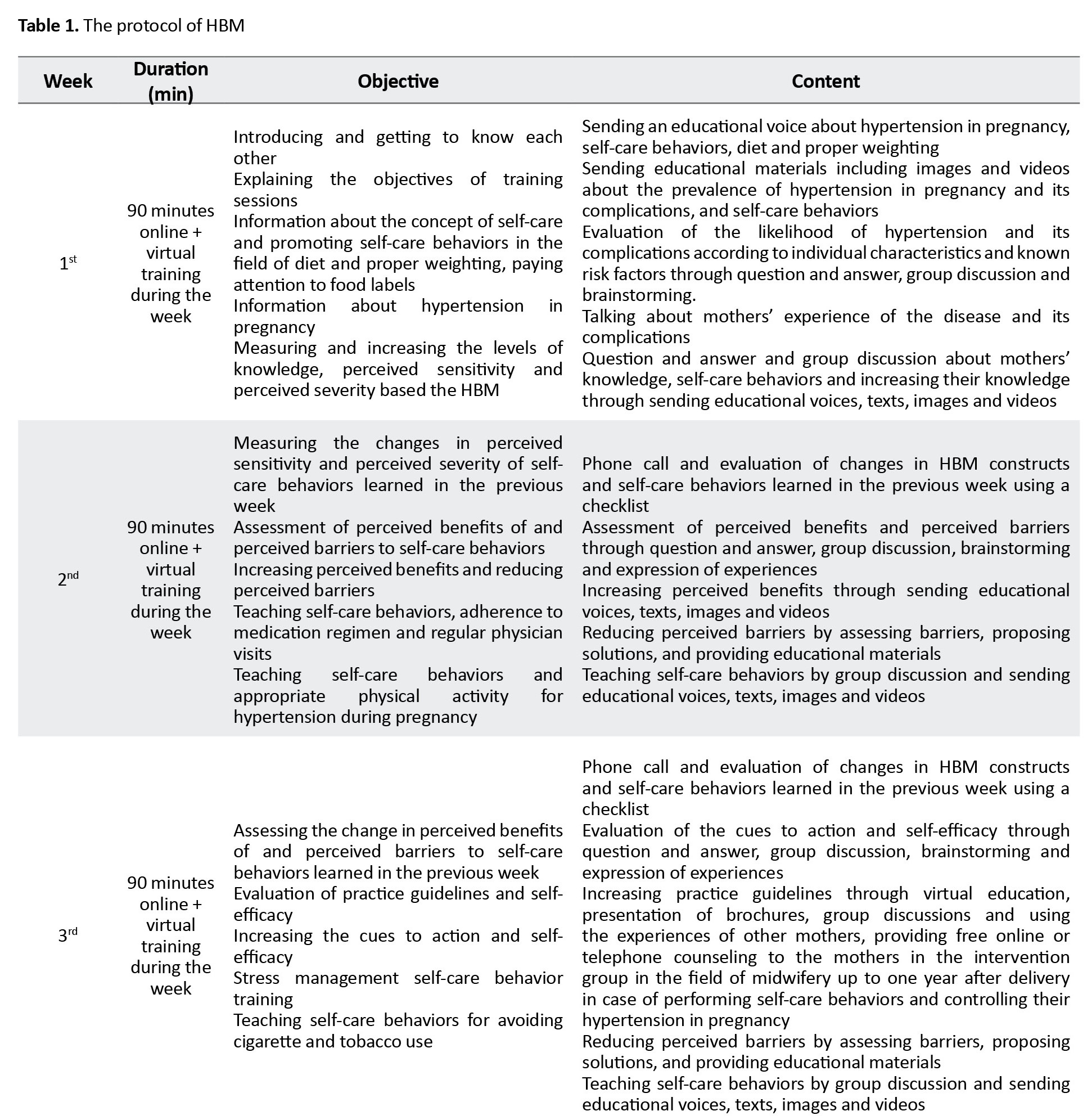
Due to the COVID-19 pandemic at the time of the study, educational sessions were conducted virtually and on WhatsApp. First, groups of 5-15 were created in WhatsApp. Then, the date and time of the meetings were determined in consultation with the group members and they were requested to become online at the determined time. Additional files including pictures, pamphlets and related educational videos were also shared in the groups. The intervention was provided at 3 sessions for three weeks and each session lasted for 90 minutes.
One month after the end of the intervention, the post-test assessment was performed in both groups. During this period, both groups received the usual prenatal care. After the end of the research, to comply with the ethical principles, the educational pamphlet was also given to the control group. After collecting the data, they were entered into SPSS software, version 25 and analyzed. Descriptive statistics such as Mean±SD, percentage, and frequency were used to describe data. Data analysis was done using chi-square test, independent t-test, Cohen’s d (effect size), and ANCOVA. The significance level was set at 0.05.
Results
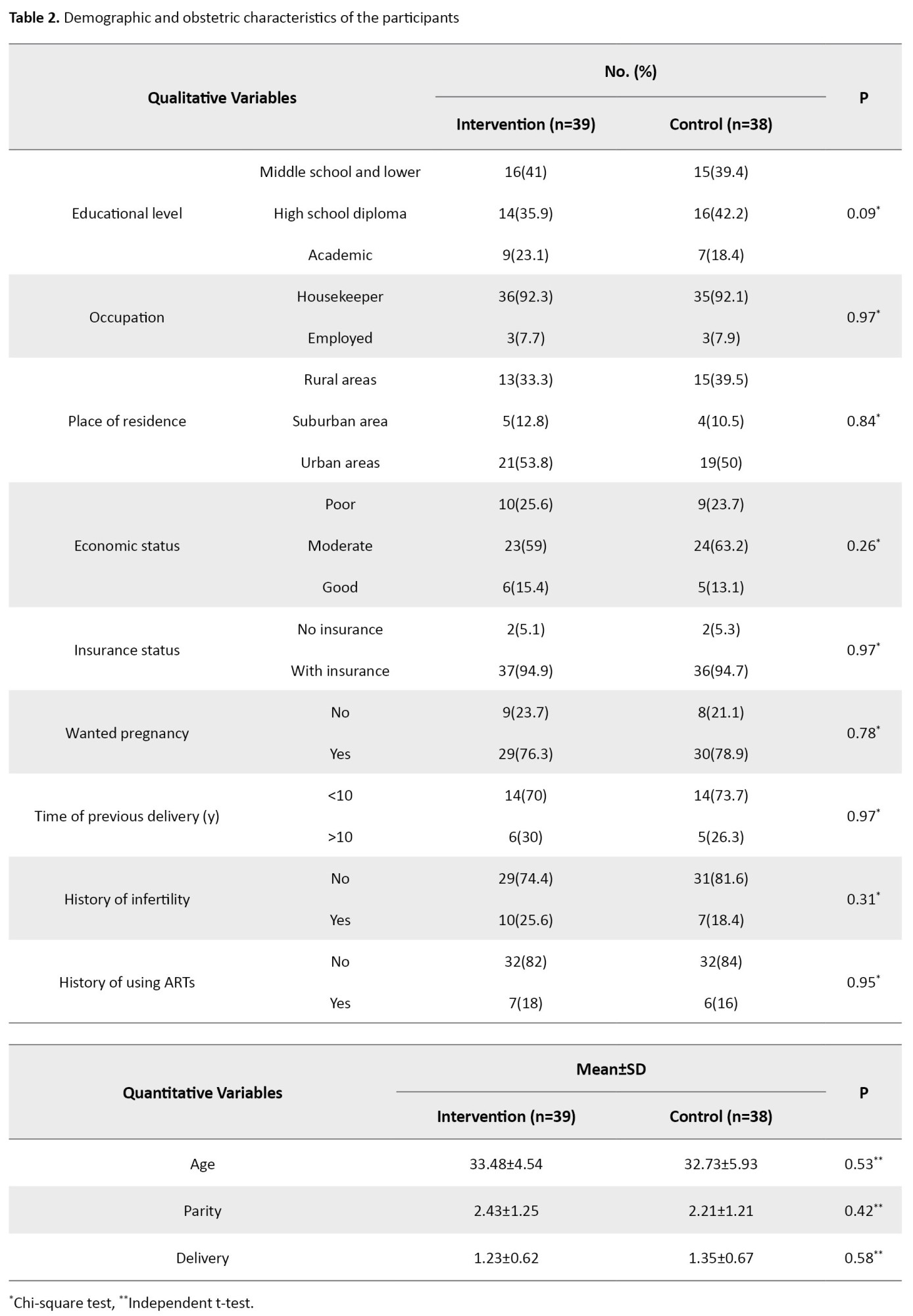
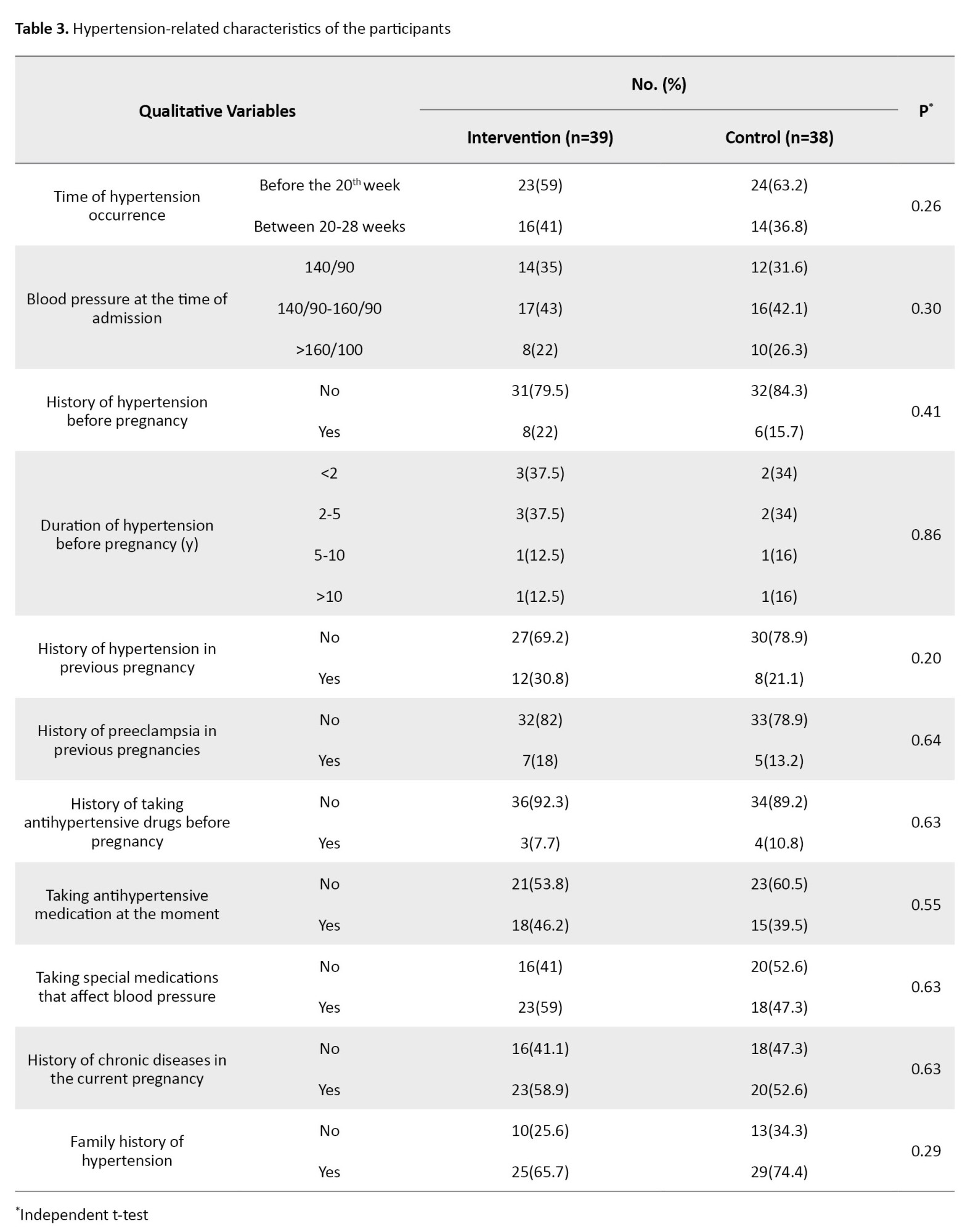
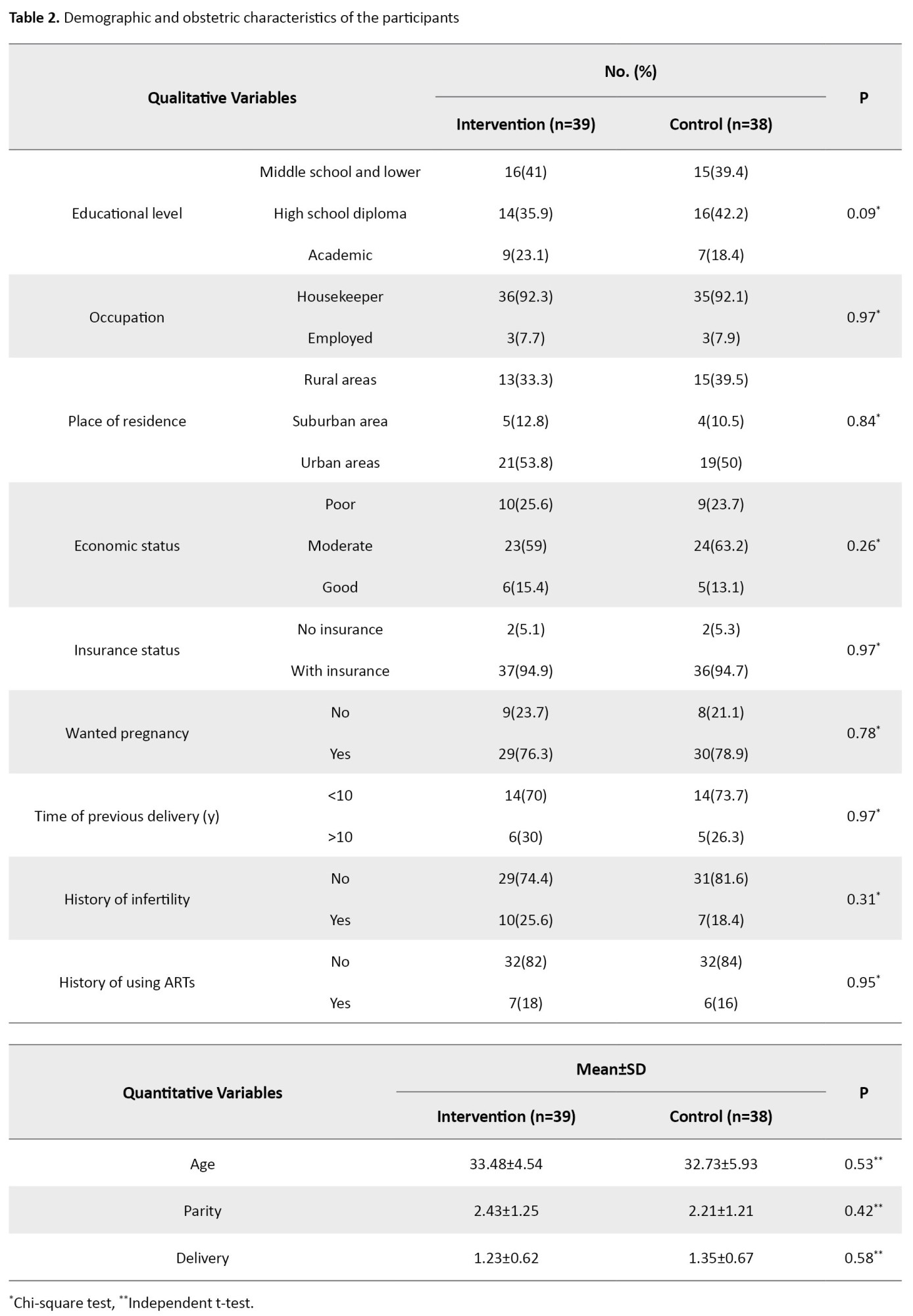
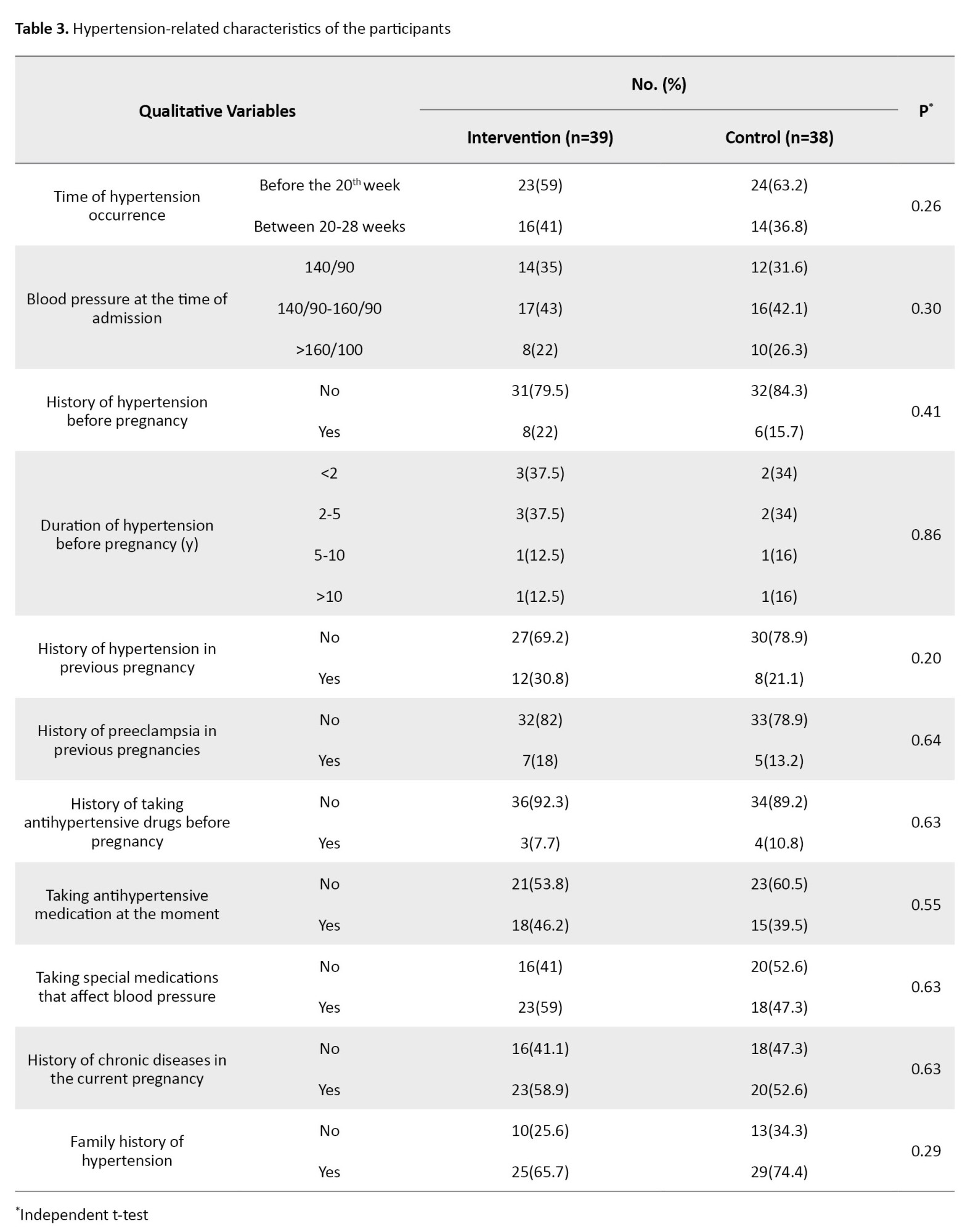
The final data analysis was done on 39 women in the intervention group and 38 women in the control group. Based on the demographic and obstetric variables, there were no significant differences between the two groups. There was also no significant difference regarding blood pressure level (Table 2).
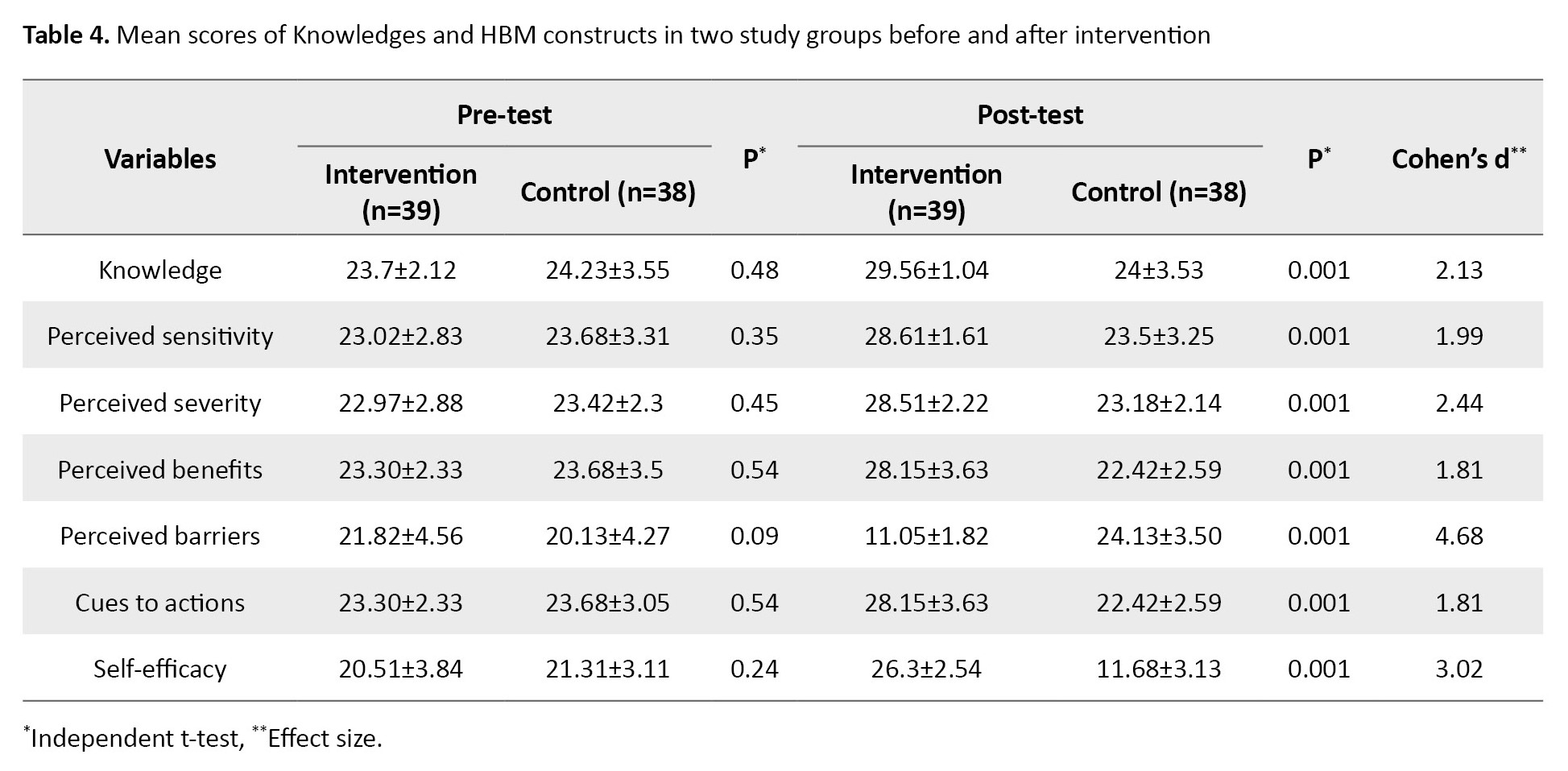
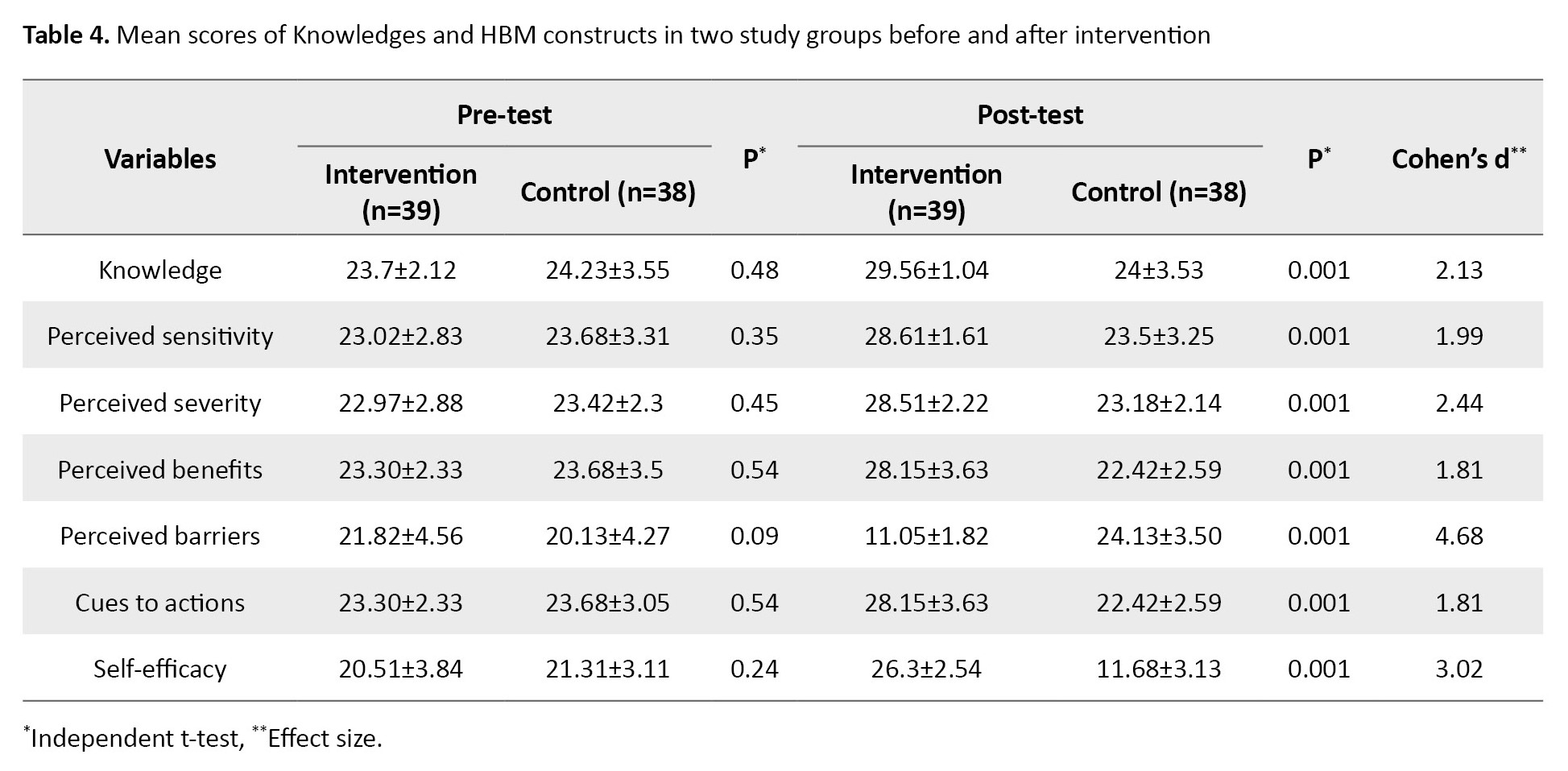
According to the independent t-test results, the mean scores of knowledges and the HBM constructs were not significantly different between the two groups before the intervention. However, one month after the intervention, the mean scores showed statistically significant differences (P=0.001). The mean scores of knowledge, perceived sensitivity, perceived severity, perceived benefits, cues to action, and self-efficacy increased in the intervention group, while the mean score of perceived barriers decreased (Table 3).
The mean score of knowledge after the intervention in the intervention group was 29.56±1.04, which was significantly higher compared to the control group that was 24±3.53 (P=0.001). The Cohen’s d value was 2.13. The mean perceived sensitivity score after the intervention in the intervention group was 28.61±1.61, which was significantly higher compared to the control group (23.50±3.25) (P=0.001, Cohen’s d=1.99). The mean score of perceived severity after the intervention in the intervention group was 28.51±2.22, which was significantly higher compared to the control group that was 23.18±2.14 (P=0.001, Cohen’s d=2.44). The mean score of perceived benefits after the intervention in the intervention group was 28.15±3.63, which was significantly higher compared to the control group that was 22.42±2.59 (P=0.001, Cohen’s d=1.81). The mean score of perceived barriers after the intervention in the intervention group was 11.05±1.82, which was significantly lower compared to the control group (24.13±3.50) (P=0.001, Cohen’s d=4.68). The mean score of cues to action after the intervention in the intervention group was 28.15±3.63, which was significantly higher compared to the control group, 22.42±2.59 (P=0.001, Cohen’s d=1.81). The mean self-efficacy score after the intervention in the intervention group was 26.30±2.54, which was significantly higher compared to the control group, 17.68±3.13 (P=0.001, Cohen’s d=3.02). For more information (Table 4).
According to the results in Table 5, the mean score of diet/physical activity after the intervention in the intervention group was 31±2.32, which was significantly higher compared to the control group, 19.39±3.14 (P=0.001, Cohen’s d=4.20).
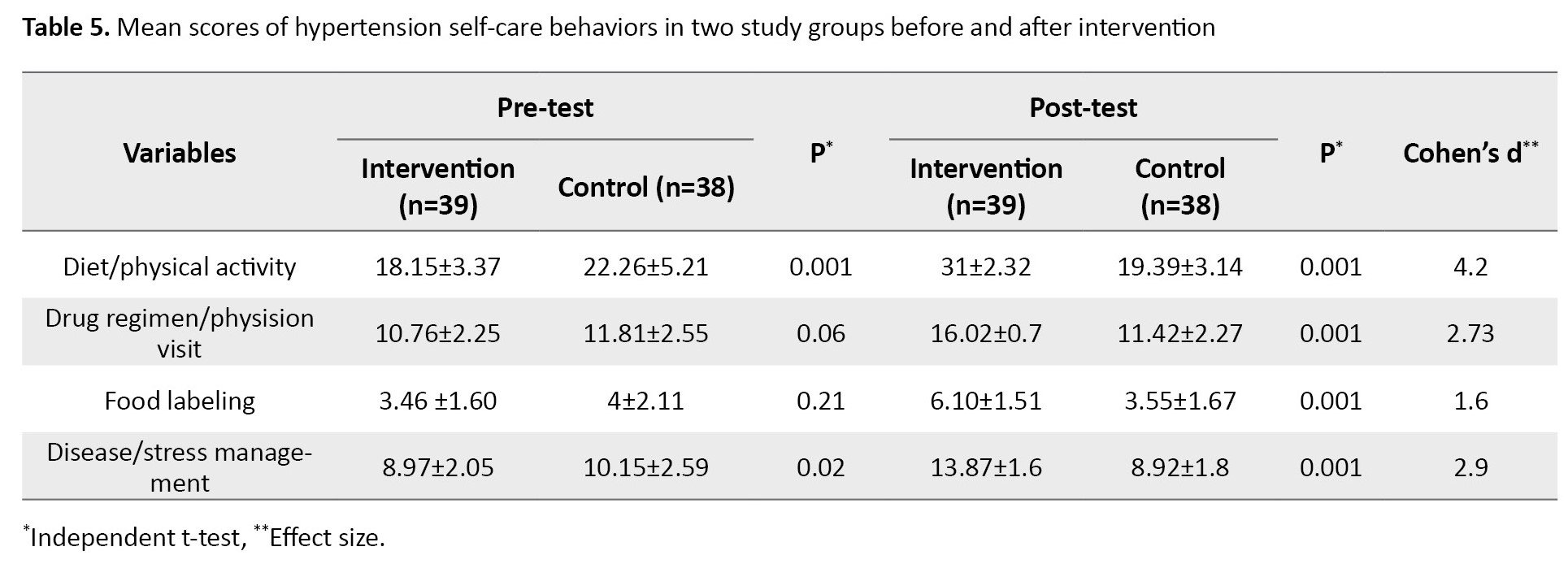
The mean score of drugs regimen/physision visit after the intervention was 16.02±0.70 in the intervention group and 11.42±2.27 in the control (P=0.001, Cohen’s d=2.73). The mean score of food labeling after the intervention was 6.10±1.51 in the intervention group and 3.55±1.67 in the control group (P=0.001, Cohen’s d=1.60). The mean score of disease/stress management after the intervention was 13.87±1.60 in the intervention group and 8.92±1.80 in the control group (P=0.001, Cohen’s d=2.90).
Discussion
The purpose of this research was the assessment of the effect of an HBM-based educational intervention on the self-care behaviors of women with hypertension in pregnancy. The results showed that the use of an educational intervention based on the HBM constructs increased knowledge, perceived sensitivity, perceived severity, perceived benefits, cues to action, and self-efficacy, reduced perceived barriers, and promoted self-care behaviors of hypertensive pregnant women.
Our results are consistent with the results of Jahani et al., who showed that the scores of knowledges, HBM constructs, self-care behavior significantly increased in hypertensive patients after the educational intervention [26]. In addition, the results are in line with the findings of a similar study on patients with tuberculosis [27]. When hypertensive women’ knowledge, perceived sensitivity and perceived severity increase, they are more likely to find a solution to control their disease. By performing self-care behaviors that are cost effective, they can easily control hypertension in pregnancy and prevent its complications.
In this study, the virtual method and educational images and videos were used for teaching self-care behaviors to hypertensive pregnant women. The results of a study also showed that teaching exercise online during pregnancy as a self-care behavior helped women to control their systolic blood pressure before and immediately after delivery [28]. In Kurt et al.’s study, it was shown that self-management and performing self-care behaviors could increase hypertensive patients’ awareness of high blood pressure, compliance with treatment, and proper control of their blood pressure [9]. These are also consistent with our results.
The findings of this study regarding the significant difference in the score of cues to action between two intervention and control groups after education are consistent with the results of Eftekhar Ardebili [29]. The increase in cues to action in the intervention group can be explained by the fact that this group, in addition to radio and TV educational programs, had access to virtual education, midwives and health personnel, brochures, and group discussions with other pregnant mothers suffering from hypertension in pregnancy. They also received one year of free online midwifery counseling by the researcher as a reward for participating in the educational classes.
In the present study, one month after the intervention, the mean score of self-efficacy in the intervention group increased compared to the control group; in the control group, the level of self-efficacy decreased even compared to baseline. The HBM-based education caused hypertensive pregnant mothers to have more perceived sensitivity and severity regarding their disease, and their perceived benefits of self-care increased while their perceived barriers decreased. Therefore, they perceived more self-efficacy and ability to perform hypertension self-care behaviors. This is consistent with the results of some studies [8, 30].
Our results also showed significant increase in self-care behaviors of the intervention group in the areas of diet/physical activity, drug regimen/doctor visit, food labeling, and disease/stress management after education, which is consistent with the results of some studies [31, 32]. Regarding the diet/physical activity, the results are also consistent with the results of Abdolaliyan [33]. Physical activity of pregnant women was lower than average level. The use of the HBM constructs, especially the perceived benefits and perceived barriers can play an important role in promoting the physical activity of hypertensive pregnant women. Regarding food labeling, the results are also consistent with the results of other studies [34, 35]. as well Makhija et al. showed that stress is one of the effective factors in increasing blood pressure in pregnancy, and yoga exercise during pregnancy is an effective way to manage stress and reduce hypertension and its complications [36]. In Verma et al.’s study, the positive effects of self-care behaviors and lifestyle modification such as healthy diet, weight management, and physical activity as well as stress control on the prevention and treatment of hypertension were also suggested [13].
In conclusion, it seems that education based on the HBM constructs can increase self-care behaviors in pregnant mothers with hypertension. However, it is recommended to conduct more studies so that it can also be used for patients at the bedside. It is also recommended to compare this educational approach with other educational methods in future studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Qazvin University of Medical Sciences (Code: IR.QUMS.REC.1398.152). In this study, all ethical considerations, such as obtaining informed consent from the participants, ensuring the confidentiality of their information, their right to leave the study, were considered.
Funding
This article was extracted from a master’s thesis of Tahereh Aflaki, approved by Department of Midwifery School of Nursing and Midwifery, Qazvin University of Medical Science.
Authors' contributions
Conceptualization and study design: Tahereh Aflaki, Forouzan Olfati and Zinat Jourabchi; Intervention and sampling: Tahereh Aflaki; Supervision: Zinat Jourabchi; Data analysis: Tahereh Aflaki and Moniralsadat Mirzadeh; Initial draft preparation: Tahereh Aflaki and Zinat Jourabchi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
References
According to the American College of Obstetricians and Gynecologists (ACOG), “gestational hypertension” is defined as “systolic blood pressure above 140 and diastolic blood pressure above 90 mm Hg, which occurs after the 20th week of pregnancy (or within 12 weeks after delivery). This type of hypertension is without the presence of protein in the urine or dysfunction of internal organs such as the liver; however, if hypertension occurs before the 20th week of pregnancy and remains stable until 12 weeks after delivery, it is called “chronic hypertension”. If the systolic blood pressure is above 160 mm Hg or the diastolic blood pressure is above 110 mm Hg, it is called “severe hypertension” in pregnancy [1, 2]. The global prevalence of hypertension in pregnant women is reported to be about 5-10% [3, 4]. Prevalence of hypertension among pregnant women in the US is 13.8% [5]; in Ireland, about 6% [6], and in Iran, 6% [7]. Hypertension in pregnancy is an important risk factor for the mother and the fetus [3].
Many studies have shown the role of self-care in hypertension management [8, 9, 10]. Self-care behaviors can be one of the most important strategies to control blood pressure and maintain its normal level [11]. Self-care management for controlling blood pressure refers to the use of knowledge and skills to prevent the occurrence of hypertension or reduce its severity. Effective factors for self-care management of hypertension include: Correct and regular use of medications, lifestyle modification (such as following a low-salt and low-fat diet), performing regular sports activities, avoiding alcohol consumption, appropriate weight control, blood pressure measurement and control, managing and reducing stress, and giving importance to care and visiting doctors [12, 13]. Although many studies have shown the positive and favorable effect of self-care behaviors in controlling high hypertension, many people with hypertension in the world still do not follow self-care behaviors. It is suggested that self-care behaviors should be taught using appropriate educational programs and models in patients with hypertension [14, 15, 16, 17]. One of the prominent models in this field is the health belief model (HBM) which has six components of perceived sensitivity, perceived severity, perceived benefits, perceived barriers, cues to actions, and self-efficacy [18, 19]. A study in Iran showed the significant relationship of the components of perceived barriers, self-efficacy and cues to action with self-care behaviors in patients with hypertension, and recommended that the HBM-based educational programs should be developed to promote self-care behaviors to control high blood pressure [20]. On the other hand, the use of HBM can increase the self-efficacy of hypertensive patients; the increase in perceived sensitivity and severity of hypertensive patients can improve their self-care behaviors [21].
To our knowledge, there is no study on the effect of HBM-based educational programs on self-care behaviors of pregnant women with hypertension. Therefore, this study aims to assess the effectiveness of an HBM-based educational program in improving the self-care behaviors of pregnant women with hypertension.
Materials and Methods
This is a quasi-experimental study with a pre-test/post-test design that was conducted on women with hypertension in pregnancy who referred to one of the specialized women’s hospitals in Rasht, Iran, during January-August 2020. The sample size was determined to be 90 by considering the first type error level of 0.05, the second type error level of 0.2, the Mean±SD scores of 20.72±1.75 and 22.32±2.94 for systolic pressure [12], and a 20% sample drop. Eligible samples were selected using a convenience sampling method. The inclusion criteria were gestational age up to 28 weeks, blood pressure of ≥140 and ≥90, singleton pregnancy, absence of proteinuria and preeclampsia, no addiction to drugs, smoking and alcohol, no neurological and mental diseases according to medical records, not having abnormal bleeding, age <45 years, reading and writing literacy, and willingness to participate in the study. The exclusion criteria were unwillingness to continue participating in the study and withdrawing for any reason during the study process. The data collection tools included a demographic/obstetric form, an HBM questionnaire, and the hypertension in pregnancy self-care profile.
The demographic/obstetric form surveys age, weight, insurance status (based on the patient’s medical file), educational level, occupation, place of residence, economic status, wanted/unwanted pregnancy, time of previous delivery, history of infertility, history of using assisted reproductive technologies (ARTs), and information about blood pressure based on the self-reports. The HBM questionnaire was designed by the researcher according to a previous study [22] and the scoring method was based on Khorsandi et al.’s study [23]. The questionnaire had two parts. The first part included items measuring knowledge (6 items) and the second part with 42 items measured perceived sensitivity (6 items), perceived severity (6 items), perceived benefits (6 items), perceived barriers (6 items), cues to actions (6 items), and self-efficacy (6 items). The items were rated on a five-point Likert scale as 1 (completely disagree), 2 (disagree), 3 (no idea), 4 (agree), and 5 (completely agree). The total score ranges from 42 to 210, with higher scores indicating better status. To determine the validity of this tool, face validity and content validity were measured. The initial draft was sent to 11 faculty members and experts in midwifery and health education from Qazvin University of Medical Sciences. The content validity ratio (CVR) was obtained as 0.87 and the content validity index (CVI) was 0.95. To determine the reliability using Cronbach’s α coefficient, the initial draft was completed by 20 mothers with hypertension in pregnancy who were not among the samples. Cronbach’s α was obtained 0.83 for the knowledge subscale, 0.7 for perceived sensitivity, 0.83 for perceived severity, 0.7 for perceived benefits, 0.7 for perceived barriers, 0.7 for cues to actions, 0.78 for self-efficacy, and 0.74 for the whole scale. The hypertension in pregnancy self-care profile was developed based on the scale designed by Han et al. [24], and its Persian version was validated by Ghanei Gheshlagh et al. [25]. It had 19 items measuring hypertension self-care behaviors in 4 areas of diet/physical activity (9 items), drug regimen/physician visit (4 items), food labeling (2 items), disease/stress management (4 items). The items were rated on a four-point Likert scale as 1 (never), 2 (sometimes), 3 (often), and 4 (always). The score ranged 9-36 for diet/physical activity, 4-16 for drug regimen/ physician visit, 2-8 for food labeling, and 4-16 for disease/stress management. The total score ranged 19-76, with higher scores indicating higher self-care behaviors for hypertension in pregnancy. The CVI was 0.94. Moreover, Cronbach’s α was obtained 0.76 for diet/physical activity, 0.84 for drug regimen/doctor visit, 0.93 for food labeling, and 0.70 for disease/stress management, and 0.80 for the whole scale.
The participants were randomly divided into two groups of intervention and control using the random allocation software (Figure 1). Both groups received information from their health care providers during the study, while the intervention group was also given HBM-based education by the researcher. The content of the educational sessions was reviewed and approved by five faculty members of the schools of midwifery and health at Qazvin University of Medical Sciences (Table 1).
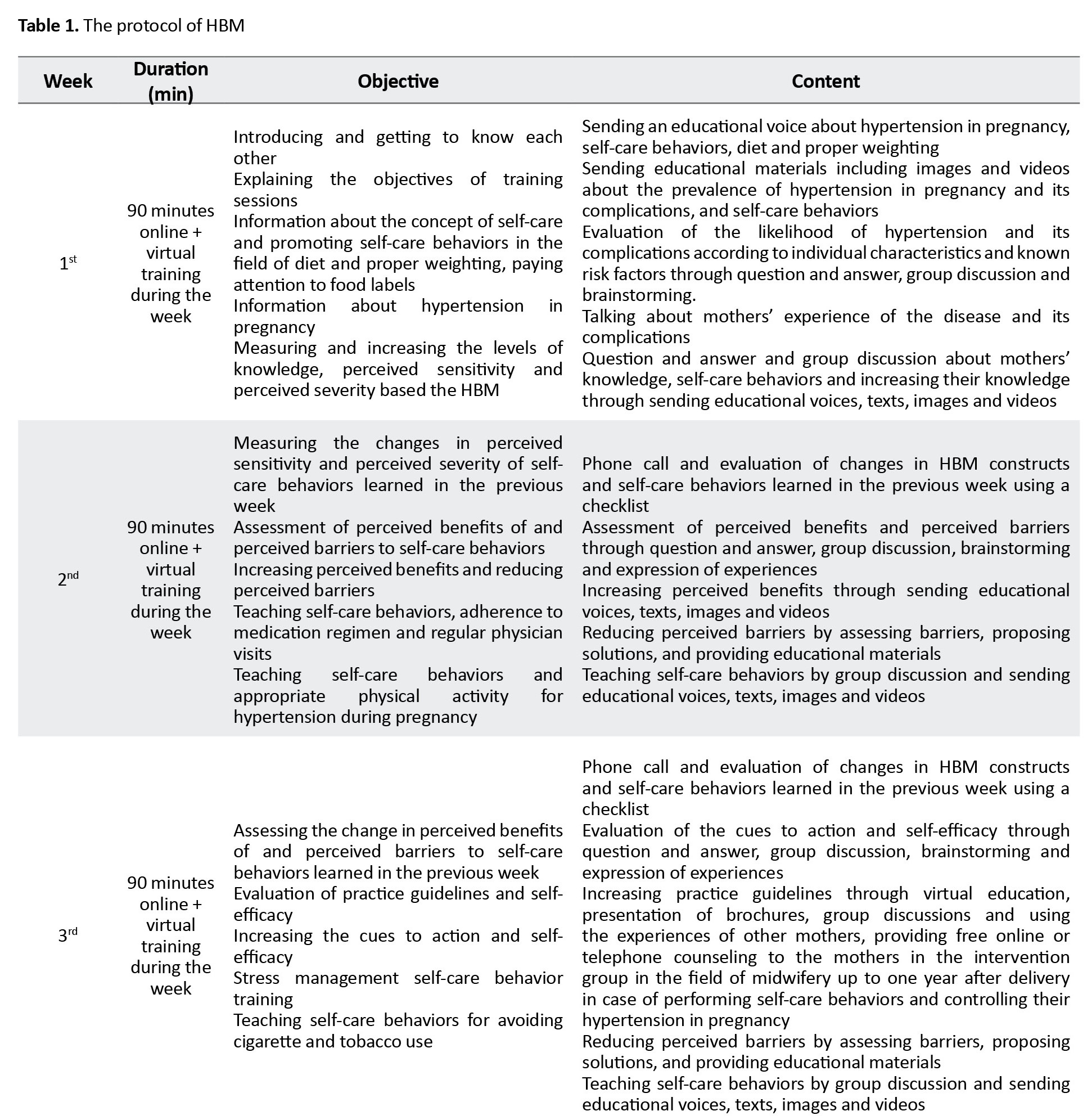
Due to the COVID-19 pandemic at the time of the study, educational sessions were conducted virtually and on WhatsApp. First, groups of 5-15 were created in WhatsApp. Then, the date and time of the meetings were determined in consultation with the group members and they were requested to become online at the determined time. Additional files including pictures, pamphlets and related educational videos were also shared in the groups. The intervention was provided at 3 sessions for three weeks and each session lasted for 90 minutes.
One month after the end of the intervention, the post-test assessment was performed in both groups. During this period, both groups received the usual prenatal care. After the end of the research, to comply with the ethical principles, the educational pamphlet was also given to the control group. After collecting the data, they were entered into SPSS software, version 25 and analyzed. Descriptive statistics such as Mean±SD, percentage, and frequency were used to describe data. Data analysis was done using chi-square test, independent t-test, Cohen’s d (effect size), and ANCOVA. The significance level was set at 0.05.
Results
The final data analysis was done on 39 women in the intervention group and 38 women in the control group. Based on the demographic and obstetric variables, there were no significant differences between the two groups. There was also no significant difference regarding blood pressure level (Table 2).
According to the independent t-test results, the mean scores of knowledges and the HBM constructs were not significantly different between the two groups before the intervention. However, one month after the intervention, the mean scores showed statistically significant differences (P=0.001). The mean scores of knowledge, perceived sensitivity, perceived severity, perceived benefits, cues to action, and self-efficacy increased in the intervention group, while the mean score of perceived barriers decreased (Table 3).
The mean score of knowledge after the intervention in the intervention group was 29.56±1.04, which was significantly higher compared to the control group that was 24±3.53 (P=0.001). The Cohen’s d value was 2.13. The mean perceived sensitivity score after the intervention in the intervention group was 28.61±1.61, which was significantly higher compared to the control group (23.50±3.25) (P=0.001, Cohen’s d=1.99). The mean score of perceived severity after the intervention in the intervention group was 28.51±2.22, which was significantly higher compared to the control group that was 23.18±2.14 (P=0.001, Cohen’s d=2.44). The mean score of perceived benefits after the intervention in the intervention group was 28.15±3.63, which was significantly higher compared to the control group that was 22.42±2.59 (P=0.001, Cohen’s d=1.81). The mean score of perceived barriers after the intervention in the intervention group was 11.05±1.82, which was significantly lower compared to the control group (24.13±3.50) (P=0.001, Cohen’s d=4.68). The mean score of cues to action after the intervention in the intervention group was 28.15±3.63, which was significantly higher compared to the control group, 22.42±2.59 (P=0.001, Cohen’s d=1.81). The mean self-efficacy score after the intervention in the intervention group was 26.30±2.54, which was significantly higher compared to the control group, 17.68±3.13 (P=0.001, Cohen’s d=3.02). For more information (Table 4).
According to the results in Table 5, the mean score of diet/physical activity after the intervention in the intervention group was 31±2.32, which was significantly higher compared to the control group, 19.39±3.14 (P=0.001, Cohen’s d=4.20).
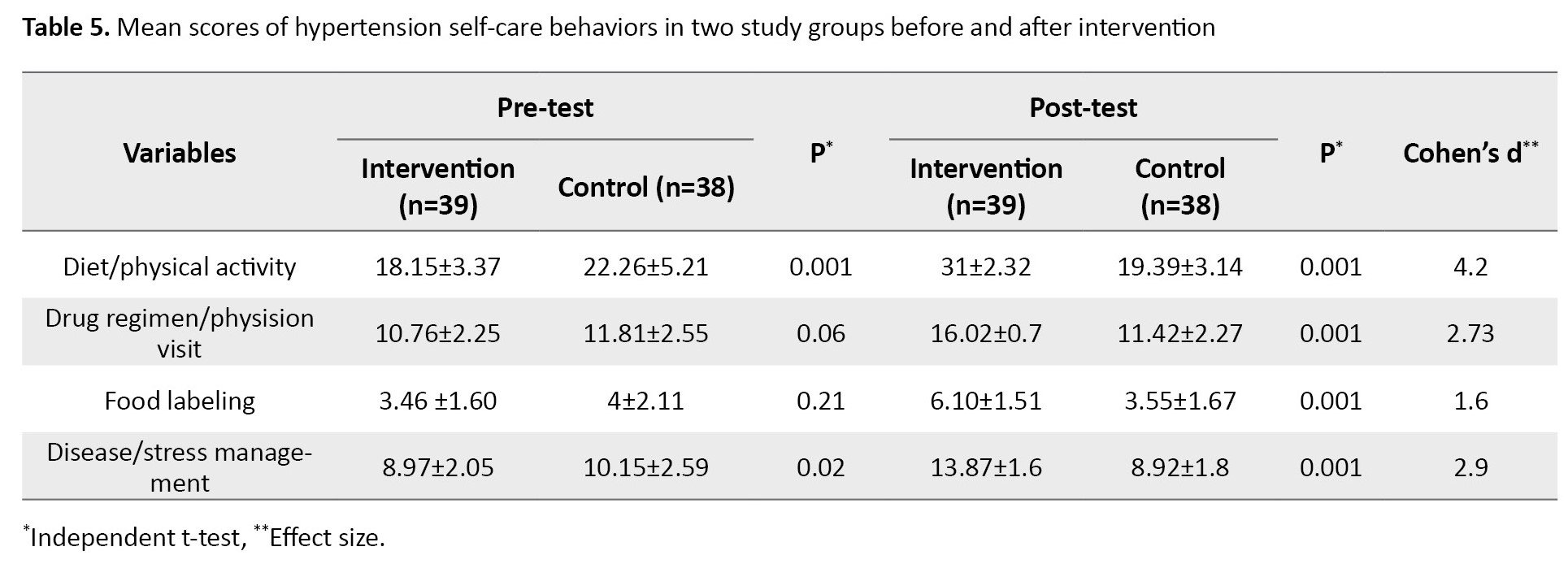
The mean score of drugs regimen/physision visit after the intervention was 16.02±0.70 in the intervention group and 11.42±2.27 in the control (P=0.001, Cohen’s d=2.73). The mean score of food labeling after the intervention was 6.10±1.51 in the intervention group and 3.55±1.67 in the control group (P=0.001, Cohen’s d=1.60). The mean score of disease/stress management after the intervention was 13.87±1.60 in the intervention group and 8.92±1.80 in the control group (P=0.001, Cohen’s d=2.90).
Discussion
The purpose of this research was the assessment of the effect of an HBM-based educational intervention on the self-care behaviors of women with hypertension in pregnancy. The results showed that the use of an educational intervention based on the HBM constructs increased knowledge, perceived sensitivity, perceived severity, perceived benefits, cues to action, and self-efficacy, reduced perceived barriers, and promoted self-care behaviors of hypertensive pregnant women.
Our results are consistent with the results of Jahani et al., who showed that the scores of knowledges, HBM constructs, self-care behavior significantly increased in hypertensive patients after the educational intervention [26]. In addition, the results are in line with the findings of a similar study on patients with tuberculosis [27]. When hypertensive women’ knowledge, perceived sensitivity and perceived severity increase, they are more likely to find a solution to control their disease. By performing self-care behaviors that are cost effective, they can easily control hypertension in pregnancy and prevent its complications.
In this study, the virtual method and educational images and videos were used for teaching self-care behaviors to hypertensive pregnant women. The results of a study also showed that teaching exercise online during pregnancy as a self-care behavior helped women to control their systolic blood pressure before and immediately after delivery [28]. In Kurt et al.’s study, it was shown that self-management and performing self-care behaviors could increase hypertensive patients’ awareness of high blood pressure, compliance with treatment, and proper control of their blood pressure [9]. These are also consistent with our results.
The findings of this study regarding the significant difference in the score of cues to action between two intervention and control groups after education are consistent with the results of Eftekhar Ardebili [29]. The increase in cues to action in the intervention group can be explained by the fact that this group, in addition to radio and TV educational programs, had access to virtual education, midwives and health personnel, brochures, and group discussions with other pregnant mothers suffering from hypertension in pregnancy. They also received one year of free online midwifery counseling by the researcher as a reward for participating in the educational classes.
In the present study, one month after the intervention, the mean score of self-efficacy in the intervention group increased compared to the control group; in the control group, the level of self-efficacy decreased even compared to baseline. The HBM-based education caused hypertensive pregnant mothers to have more perceived sensitivity and severity regarding their disease, and their perceived benefits of self-care increased while their perceived barriers decreased. Therefore, they perceived more self-efficacy and ability to perform hypertension self-care behaviors. This is consistent with the results of some studies [8, 30].
Our results also showed significant increase in self-care behaviors of the intervention group in the areas of diet/physical activity, drug regimen/doctor visit, food labeling, and disease/stress management after education, which is consistent with the results of some studies [31, 32]. Regarding the diet/physical activity, the results are also consistent with the results of Abdolaliyan [33]. Physical activity of pregnant women was lower than average level. The use of the HBM constructs, especially the perceived benefits and perceived barriers can play an important role in promoting the physical activity of hypertensive pregnant women. Regarding food labeling, the results are also consistent with the results of other studies [34, 35]. as well Makhija et al. showed that stress is one of the effective factors in increasing blood pressure in pregnancy, and yoga exercise during pregnancy is an effective way to manage stress and reduce hypertension and its complications [36]. In Verma et al.’s study, the positive effects of self-care behaviors and lifestyle modification such as healthy diet, weight management, and physical activity as well as stress control on the prevention and treatment of hypertension were also suggested [13].
In conclusion, it seems that education based on the HBM constructs can increase self-care behaviors in pregnant mothers with hypertension. However, it is recommended to conduct more studies so that it can also be used for patients at the bedside. It is also recommended to compare this educational approach with other educational methods in future studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Qazvin University of Medical Sciences (Code: IR.QUMS.REC.1398.152). In this study, all ethical considerations, such as obtaining informed consent from the participants, ensuring the confidentiality of their information, their right to leave the study, were considered.
Funding
This article was extracted from a master’s thesis of Tahereh Aflaki, approved by Department of Midwifery School of Nursing and Midwifery, Qazvin University of Medical Science.
Authors' contributions
Conceptualization and study design: Tahereh Aflaki, Forouzan Olfati and Zinat Jourabchi; Intervention and sampling: Tahereh Aflaki; Supervision: Zinat Jourabchi; Data analysis: Tahereh Aflaki and Moniralsadat Mirzadeh; Initial draft preparation: Tahereh Aflaki and Zinat Jourabchi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
References
- Battarbee AN, Sinkey RG, Harper LM, Oparil S, Tita AT. Chronic hypertension in pregnancy. Am J Obstet Gynecol. 2020; 222(6):532-41. [DOI:10.1016/j.ajog.2019.11.1243] [PMID]
- Nobles CJ, Mendola P, Mumford SL, Silver RM, Kim K, Andriessen VC, et al. Preconception blood pressure and its change into early pregnancy: early risk factors for preeclampsia and gestational hypertension. Hypertension. 2020; 76(3):922-9. [DOI:10.1161/HYPERTENSIONAHA.120.14875] [PMID]
- Papademetriou V, Stavropoulos K, Patoulias D, Papadopoulos C, Georgios K, Toumpourleka M, et al. Hypertension in pregnancy: Unanswered questions. Curr Pharm Des. 2021; 27(36):3795-803. [PMID]
- Wang W, Xie X, Yuan T, Wang Y, Zhao F, Zhou Z, et al. Epidemiological trends of maternal hypertensive disorders of pregnancy at the global, regional, and national levels: A population-based study. BMC Pregnancy Childbirth. 2021; 21(1):364. [DOI:10.1186/s12884-021-03809-2] [PMID]
- Bello NA, Zhou H, Cheetham TC, Miller E, Getahun DT, Fassett MJ, et al. Prevalence of hypertension among pregnant women when using the 2017 American College of Cardiology/American Heart Association blood pressure guidelines and association with maternal and fetal outcomes. JAMA Netw Open. 2021; 4(3):e213808. [DOI:10.1001/jamanetworkopen.2021.3808] [PMID]
- Corrigan L, O’Farrell A, Moran P, Daly D. Hypertension in pregnancy: Prevalence, risk factors and outcomes for women birthing in Ireland. Pregnancy Hypertens. 2021; 24:1-6. [DOI:10.1016/j.preghy.2021.02.005] [PMID]
- Tavakolipoor S, Beigi M, Nekuei N, Shafiei F. The prevalence of pregnancy hypertensive disorders and their related factors in the second and third level hospitals affiliated to Isfahan University of Medical Sciences, Isfahan, Iran. J Midwifery Reprod Health. 2019; 7(3):1736-41. [DOI:10.22038/JMRH.2019.32423.1353]
- Khademian Z, Kazemi Ara F, Gholamzadeh S. The effect of self care education based on orem's nursing theory on quality of life and self-efficacy in patients with hypertension: A quasi-experimental study. Int J Community Based Nurs Midwifery. 2020; 8(2):140-9. [PMID]
- Kurt D, Gurdogan EP. The effect of self-management support on knowledge level, treatment compliance and selfcare management in patients with hypertension. Aust J Adv Nurs. 2022; 39(3):14-23. [DOI:10.37464/2020.393.543]
- Pahria T, Nugroho C, Yani DI. Factors influencing self-care behaviors in hypertension patients with complications. Vasc Health Risk Manag. 2022; 18:463-71. [DOI:10.2147/VHRM.S366811] [PMID]
- Pourmand G, Doshmangir L, Ahmadi A, Noori M, Rezaeifar A, Mashhadi R, et al. An application of the theory of planned behavior to self-care in patients with hypertension. BMC Public Health. 2020; 20(1):1290. [DOI:10.1186/s12889-020-09385-y] [PMID]
- Chang AK, Lee EJ. Factors affecting self-care in elderly patients with hypertension in Korea. Int J Nurs Pract. 2015; 21(5):584-91. [DOI:10.1111/ijn.12271] [PMID]
- Verma N, Rastogi S, Chia YC, Siddique S, Turana Y, Cheng Hm, et al. Non-pharmacological management of hypertension. J Clin Hypertens (Greenwich). 2021; 23(7):1275-83. [DOI:10.1111/jch.14236] [PMID]
- Abedini S, Pourjalil F, Mohseni S. The impact of an educational program based on the BASNEF model on knowledge and self-care behaviors of patients with hypertension. Health Scope. 2020; 9(4):e95588. [DOI:10.5812/jhealthscope.95588]
- Adinkrah E, Bazargan M, Wisseh C, Assari S. Adherence to hypertension medications and lifestyle recommendations among underserved African American middle-aged and older adults. Int J Environ Res Public Health. 2020; 17(18):6538. [DOI:10.3390/ijerph17186538] [PMID]
- Hussen FM, Adem HA, Roba HS, Mengistie B, Assefa N. Self-care practice and associated factors among hypertensive patients in public health facilities in Harar Town, Eastern Ethiopia: A cross-sectional study. SAGE Open Med. 2020; 8. [DOI:10.1177/2050312120974145] [PMID]
- Zangiabadi A, Esmaili AS, Tabatabaei SVA, Movahed E, SHhankestani H. Factors regarding adherence to medication in patients with hypertension based on health belief model in the South of Kerman, Iran, in 2019. J Community Health Res. 2022. [DOI:10.18502/jchr.v11i2.9995]
- Mohebi S. Dashti Z, Ramezani T, Hozoori M. [The educational needs of menopausal women with hypertension on healthy nutritional behaviors using the health belief model (Persian)]. Zanko J Med Sci 2017; 18(57):33-43. [Link]
- Zahmatkesh Rokhi N, Ebrahimzadeh Zagami S, Mazloum SR, Moradi M. [The effect of health belief model-based education on high-risk physical inactivity behavior in female students of Mashhad University of Medical Sciences (Persian)]. Nurs Midwifery J 2022; 19(11):846-56. [DOI:10.52547/unmf.19.11.846]
- Hazavehei MM, Dashti S, Moeini B, Faradmal J, Shahrabadi R, Yazdi AH. [Factors related to self-care behaviors in hypertensive individuals based on health belief model (Perian)]. Koomesh. 2015; 17(1):37-44. [Link]
- Larki A, Tahmasebi R, Reisi M. Factors predicting self-care behaviors among low health literacy hypertensive patients based on health belief model in Bushehr District, South of Iran. Int J Hypertens. 2018; 2018:1-7. [DOI:10.1155/2018/9752736] [PMID]
- Sadeghi R, Mohseni M, Khanjani N. [The effect of an educational intervention according to hygienic belief model in improving care and controlling among patients with hypertension (Persian)]. J Rafsanjan Univ Med Sci. 2014; 13(4):383-94. [Link]
- Khorsandi M, Fekrizadeh Z, Roozbahani N. Investigation of the effect of education based on the health belief model on the adoption of hypertension-controlling behaviors in the elderly. Clin Interv Aging. 2017; 12:233-40. [DOI:10.2147/CIA.S117142] [PMID]
- Han HR, Lee H, Commodore-Mensah Y, Kim M. Development and validation of the hypertension self-care profile: a practical tool to measure hypertension self-care. J Cardiovasc Nurs. 2014; 29(3):E11-20. [DOI:10.1097/JCN.0b013e3182a3fd46] [PMID]
- Ghanei Gheshlagh RG, Parizad N, Ghalenoee M, Dalvand S, Baghi V, Najafi F, et al. Psychometric features of Persian version of self-efficacy tool for patients with hypertension. Int Cardiovasc Res J. 2018; 12(2):50-6. [Link]
- Jahani B, Shakerinejad G, Karami KB, Haghighizadeh MH. Effect of self-care behaviors education on hypertensive patients in Ahwaz; based on Health Belief Model. World J Pharm Res. 2015; 4(5):109-20. [Link]
- Hosseinalipour SA, Mohammadbeigi A, Rahbar A, Mohebi S. [The impact of educational intervention based on extended health belief model with social support on promoting self-care behaviors in patients with smear positive pulmonary TB (Persian)]. Qom Univ Med Sci J. 2021; 15 (5):312-21. [DOI:10.32598/qums.15.5.1829.1]
- Silva-Jose C, Sánchez-Polán M, Diaz-Blanco Á, Coterón J, Barakat R, Refoyo I. Effectiveness of a virtual exercise program during COVID-19 confinement on blood pressure control in healthy pregnant women. Front Physiol. 2021; 12:645136. [DOI:10.3389/fphys.2021.645136] [PMID]
- Eftekhar Ardebili H, fathi S, Moradi H, Mahmoudi M, mahery AB. [Effect of educational intervention based on the health belief model in blood pressure control in hypertensive women (Persian)]. J Mazandaran Univ Med Sci. 2014; 24 (119):62-71. [Link]
- Tan FCJH, Oka P, Dambha-Miller H, Tan NC. The association between self-efficacy and self-care in essential hypertension: A systematic review. BMC Fam Pract. 2021; 22(1):44. [Link]
- Azadi NA, Ziapour A, Lebni JY, Irandoost SF, Abbas J, Chaboksavar F. The effect of education based on health belief model on promoting preventive behaviors of hypertensive disease in staff of the Iran University of Medical Sciences. ArchPublic Health. 2021; 79(1):69. [DOI:10.1186/s13690-021-00594-4] [PMID]
- Rasouli M, Pourheidari M, Gardesh ZH. Effect of self-care before and during pregnancy to prevention and control preeclampsia in high-risk women. Int J Prev Med. 2019; 10(1):21-30. [DOI:10.4103/ijpvm.IJPVM_300_17] [PMID]
- Abdolaliyan N, Shahnazi H, Kzemi A, Hasanzadeh A. Determinants of the self-efficacy of physical activity for maintaining weight during pregnancy: The application of the health belief model. J Educ Health Promot. 2017; 6(1):93-8. [DOI:10.4103/jehp.jehp_175_16] [PMID]
- Arfaoui L, Alkhaldy A, Alareeshi A, AlSaadi G, Alhendi S, Alghanmi A, et al. Assessment of knowledge and self-reported use of nutrition facts labels, nutrient content, and health claims among Saudi adult consumers. J Multidiscip Healthcare. 2021; 2021:2959-72. [DOI:10.2147/JMDH.S327700] [PMID]
- Moore SG, Donnelly JK, Jones S, Cade JE. Effect of educational interventions on understanding and use of nutrition labels: A systematic review. Nutrients. 2018; 10(10):1432. [DOI:10.3390/nu10101432] [PMID]
- Makhija A, Khatik N, Raghunandan C. A randomized control trial to study the effect of integrated yoga on pregnancy outcome in hypertensive disorder of pregnancy. Complement Ther Clin Pract. 2021; 43:101366. [DOI:10.1016/j.ctcp.2021.101366] [PMID]
Article Type : Research |
Subject:
General
Received: 2024/06/12 | Accepted: 2024/06/21 | Published: 2024/07/1
Received: 2024/06/12 | Accepted: 2024/06/21 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |