Fri, Jul 12, 2024
Volume 34, Issue 3 (6-2024)
JHNM 2024, 34(3): 270-280 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Karki R, Joshi S, Kaphle M. Complementary Feeding Practices Among Mothers of 6 to 24-month-old Children in Rural Nepal: A Cross-sectional Study. JHNM 2024; 34 (3) :270-280
URL: http://hnmj.gums.ac.ir/article-1-2376-en.html
URL: http://hnmj.gums.ac.ir/article-1-2376-en.html
1- Central Department of Public Health, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal. , karkirajesh2022@gmail.com
2- Department of Public Health, Yeti Health Science Academy, Purbanchal University, Kathmandu, Nepal.
3- Department of Public Health, People’s Dental College and Hospital, Tribhuvan University, Kathmandu, Nepal.
2- Department of Public Health, Yeti Health Science Academy, Purbanchal University, Kathmandu, Nepal.
3- Department of Public Health, People’s Dental College and Hospital, Tribhuvan University, Kathmandu, Nepal.
Full-Text [PDF 502 kb]
(37 Downloads)
| Abstract (HTML) (133 Views)
Full-Text: (17 Views)
Introduction
The first six months are crucial for infant development, and the World Health Organization (WHO) recommends exclusive breastfeeding during this period. However, as breastfeeding alone may become insufficient afterward, the introduction of complementary feeding is advised [1]. Effective breastfeeding and complementary feeding practices play a vital role in reducing under-five mortality. Research shows that growth faltering can start at 3 months and persist for 2 years. Despite optimal breastfeeding, children may be at risk of stunting if they lack adequate dietary intake, variety, and meal frequency after 6 months of age [2].
This critical period extends from 6 to 18-24 months and significantly impacts the global prevalence of malnutrition in children under five years [3]. Complementary feeding, as defined by WHO and the United Nations Children’s Fund (UNICEF), involves the introduction of solid, semi-solid, or other foods alongside breastfeeding [4].
The initial 1000 days of life are crucial for long-term health and development, especially from 6 to 24 months, which is particularly sensitive. During this phase, complementary feeding plays an increasingly vital role, emphasizing the importance of consuming nutritious foods [5]. According to WHO, introducing complementary foods in a timely manner can save the lives of over 820000 children every year. In 2008, WHO designed various measures to assess the effectiveness of infant and young child feeding (IYCF) practices. However, these measurements reveal that many children in low- and middle-income countries frequently lack adequate complementary feeding [6, 7].
Nepal actively addresses malnutrition through policies and programs, yet it has remained a significant public health issue. High rates of underweight children (19%) and alarming anemia prevalence (43% in under-five, 65% in the 6-23 months age group) persist [8]. One primary cause of malnutrition is inadequate or limited maternal knowledge regarding what, when, and how to feed a child, rather than food unavailability [9]. Additional factors include maternal education, nutritional counseling, food security, number of children, maternal health services, decision-making power, poverty, lack of access to clean water and sanitation, poor hygiene practices, and inadequate care and feeding practices [8, 10]. Complementary feeding practices in Nepal have made limited progress over the past 15 years, with an average yearly growth rate of only 1% to 2% [11]. Regular assessments of infant and young child feeding practices are crucial for evidence-based decision-making to combat undernourishment [12]. Therefore, this study aims to identify the prevalence of complementary feeding practices and associated factors among mothers with children aged 6-24 months. To our knowledge, this is the first study conducted on complementary feeding practices in this rural area. Analyzing the current prevalence of complementary feeding practices and uncovering the factors can provide baseline information for the concerned municipalities to develop effective public health intervention programs.
Materials and Methods
A community-based cross-sectional study was conducted in Surma Rural Municipality, Sudurpashchim Province (Far-West Province), Nepal, in 2023. Mothers with children aged between 6 and 24 months were recruited from the study area. The sample size was calculated considering a 95% confidence interval (CI), a proportion of timely initiation of complementary feeding estimated at 53% based on previous research [10], and a desired margin of error of 5%. This calculation resulted in a sample size of 384. A total of 381 mothers from the selected sample actively participated, achieving a response rate of 99.2%.
Only eligible mothers permanently residing in Surma Municipality with children aged 6-24 months, who were available during data collection and willing to participate, were included. Individuals who did not provide consent and family members other than mothers were excluded from the study.
Study participants were selected using purposive sampling due to the challenges of tracing respondents’ houses within limited time and resources. Before their selection, the female community health volunteers (FCHVs) were contacted and informed about the study’s objectives. The FCHVs provided a list of households with mothers having children between 6-24 months. Subsequently, each household, including the mothers of the children, was visited as per the provided list. Assistance from the FCHVs was sought to locate the homes. When the mothers were unavailable during the initial data collection, a second visit to the same household was attempted. However, if the mothers were still absent during the second attempt, they were excluded from the study.
Face-to-face interviews were conducted by trained researchers using the Nepali language from March 27th to April 7th, 2023. After conducting an extensive literature review, a researcher-made questionnaire was used to assess the information on the sociodemographic characteristics of the mother and child and maternal factors. The practice of complementary feeding was evaluated using the WHO guidelines [6]. The questionnaire included 17 questions covering initiation time, additional breastfeeding, meal frequency, dietary diversity, and hygiene practices. To determine the quantity of food and evaluate the minimum acceptable diet, a 250-mL cup was provided to mothers, allowing them to indicate the amount of food they fed to their children. The nutritional status of children was measured using the mid-upper arm circumference (MUAC) tape.
To ensure the validity of the instrument, three experts in public health and nutrition participated in the validation process and evaluated the questionnaire based on criteria such as clarity, relevance, appropriateness, and cultural sensitivity. Additionally, a pilot study was conducted among 40 respondents at Jaya Prithvi Municipality to enhance the reliability of the questionnaire. We evaluated the participants’ understanding of the questionnaire during the pilot study. We assessed if the questions were clear, easy to answer, and understandable. Also, we checked for redundancy and identified any questions that might be confusing or unnecessary. Based on this feedback, we refined the questionnaire to improve its clarity, ease of use, and overall flow. This condition allowed us to assess the consistency and stability of the questionnaire’s results. Based on the feedback and data collected during the pilot study, necessary modifications were made to improve the instrument’s reliability.
Children aged 6-24 months who were introduced to solid or semi-solid food precisely at 6 months of age, fed at the required frequency, given the appropriate quantity of food for their age, and provided with at least 4 out of the 7 food categories outlined in the WHO feeding practice guidelines were considered to have appropriate complementary feeding practices [6]. Data coding and entering to software was done after data collection. Descriptive statistics were employed for categorical variables. The Pearson’s chi-square test assessed the association between independent variables and the practice of complementary feeding (appropriate and inappropriate). The most prevalent predictors for complementary feeding practices were determined using multivariate logistic regression analysis, incorporating variables that demonstrated a significant association at the bivariate level. All statistical significance was determined at a significance level of P<0.05. All analyses were performed using IBM SPSS statistics software, version 26.
Results
The sociodemographic characteristics of mothers are presented in Table 1.
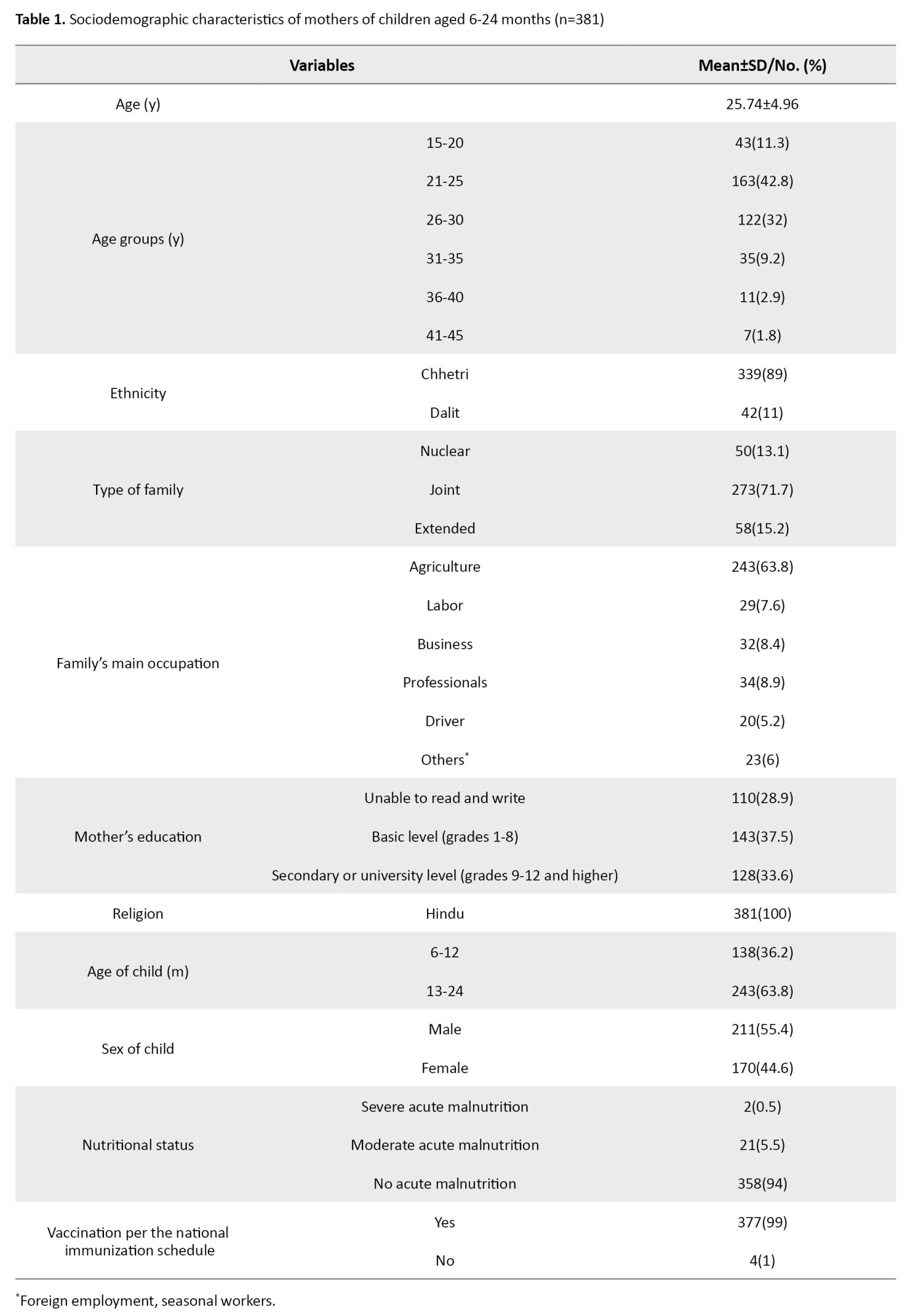
Among the 381 respondents, the majority (42.8%) belonged to the age group of 21-25 years, with a mean age of 25.74±4.96 years. The ethnicity of most respondents was Chhetri (89%), and all participants identified as Hindus. In addition, a significant number of respondents (71.7%) lived in joint families, with agriculture being the primary source of income for the majority (63.8%). Moreover, a majority of the respondents (37.5%) had received only basic level education.
Regarding the children, the majority (63.8%) fell within the age range of 13-24 months, and 55.4% were male. Notably, 94% of the children showed no signs of acute malnutrition, and 99% of the children had received vaccinations in accordance with the national immunization schedule.
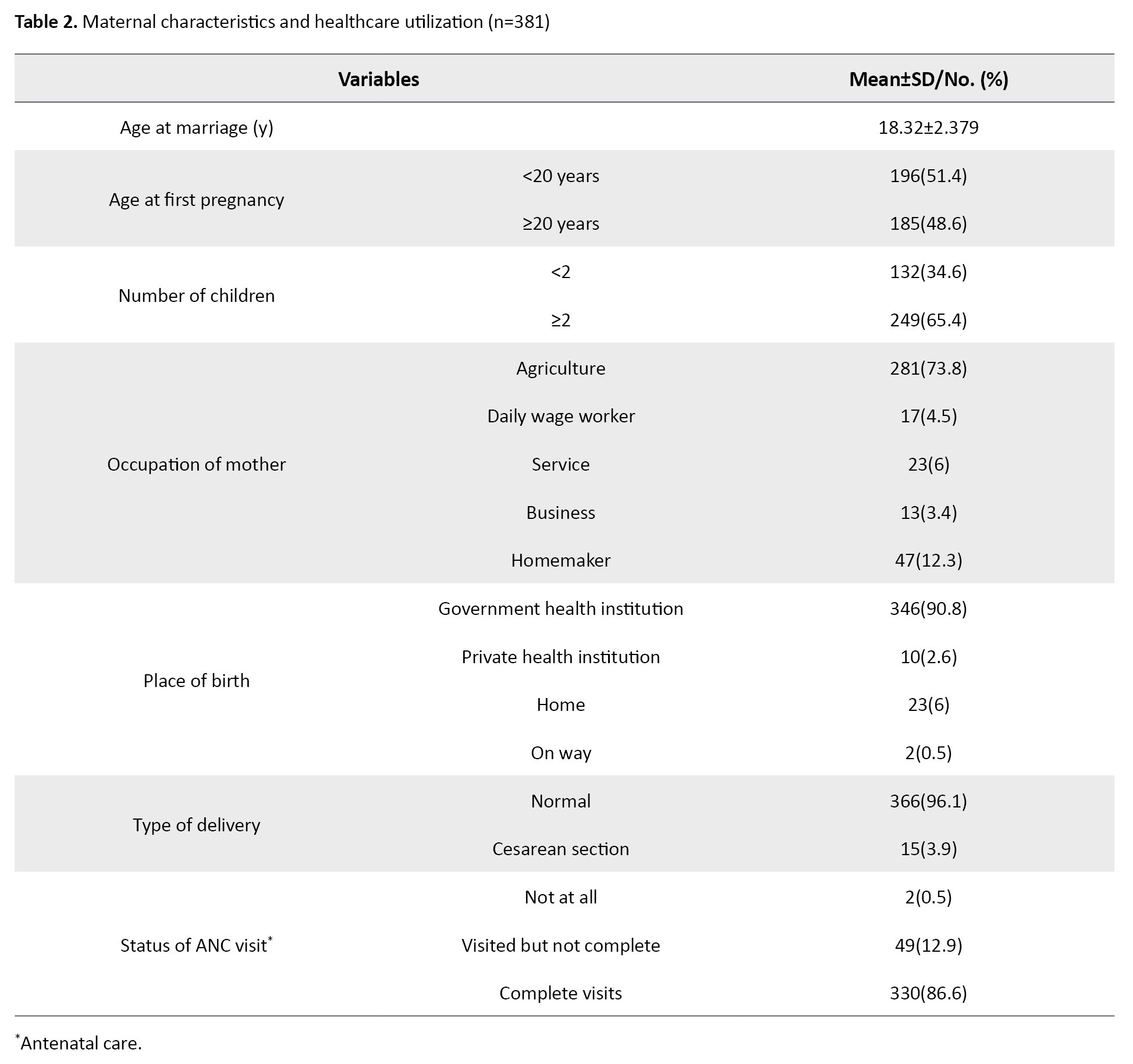
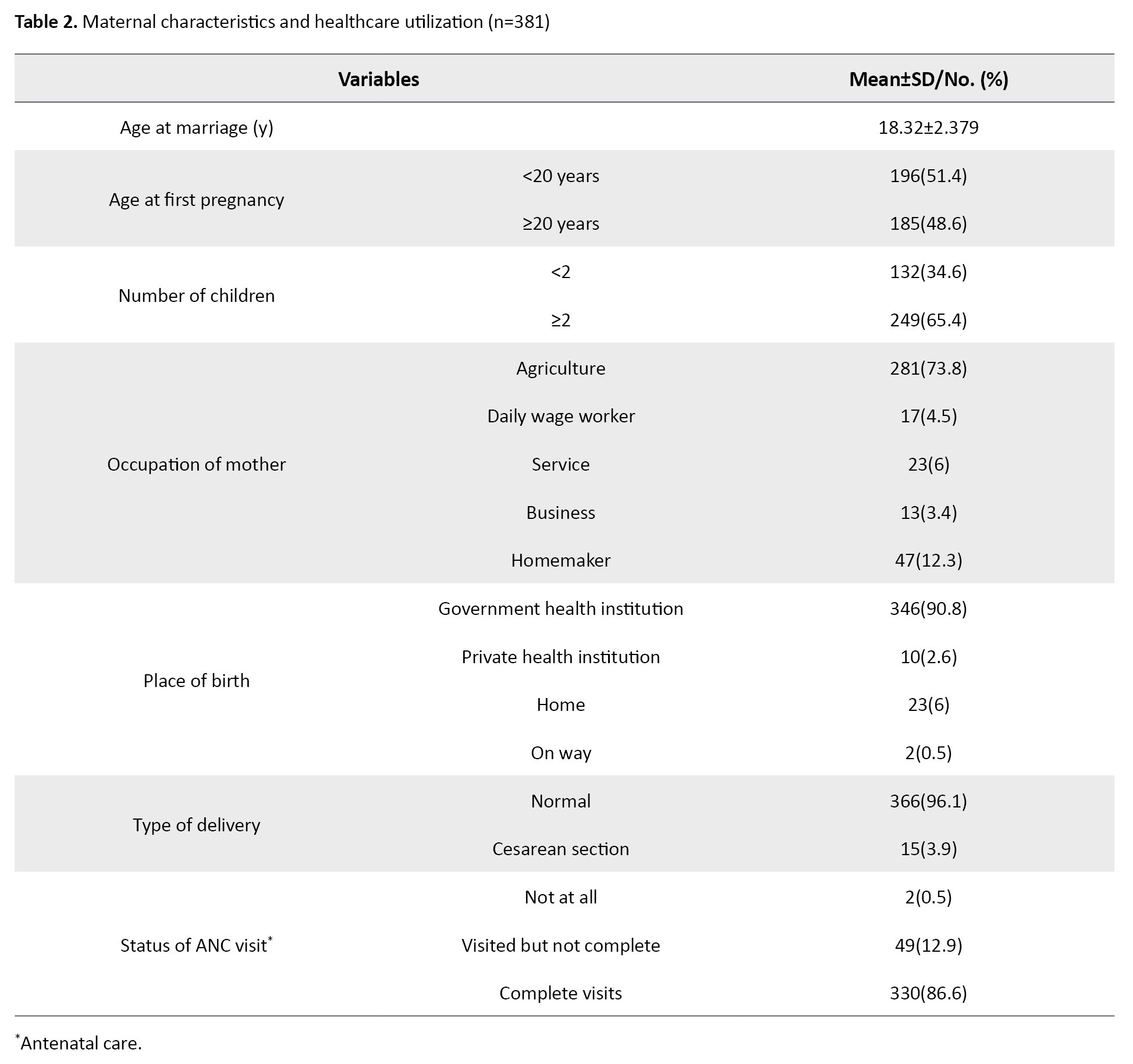
The mean age at which the mothers got married was 18.32±2.38 years. A significant portion of the mothers (51.4%) became pregnant for the first time before age 20. The majority of the mothers (73.8%) were engaged in agriculture. Furthermore, a high percentage of mothers (90.8%) gave birth to their most recent child at a government health institution. Regarding mode of delivery, nearly all mothers (96.1%) had a spontaneous vaginal delivery. Approximately 86.6% of the mothers had attended all the recommended antenatal care (ANC) visits. These results are presented in Table 2.
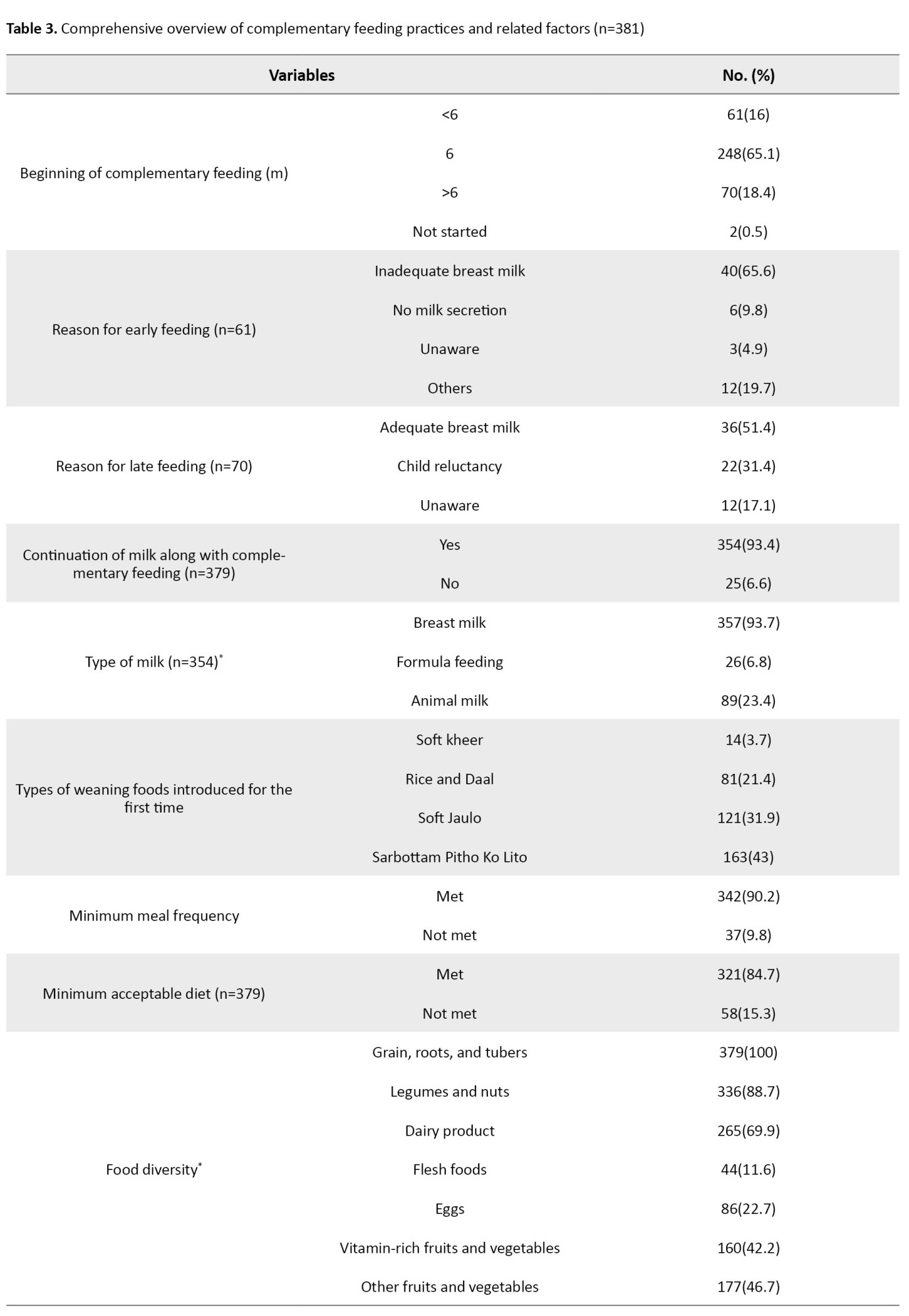
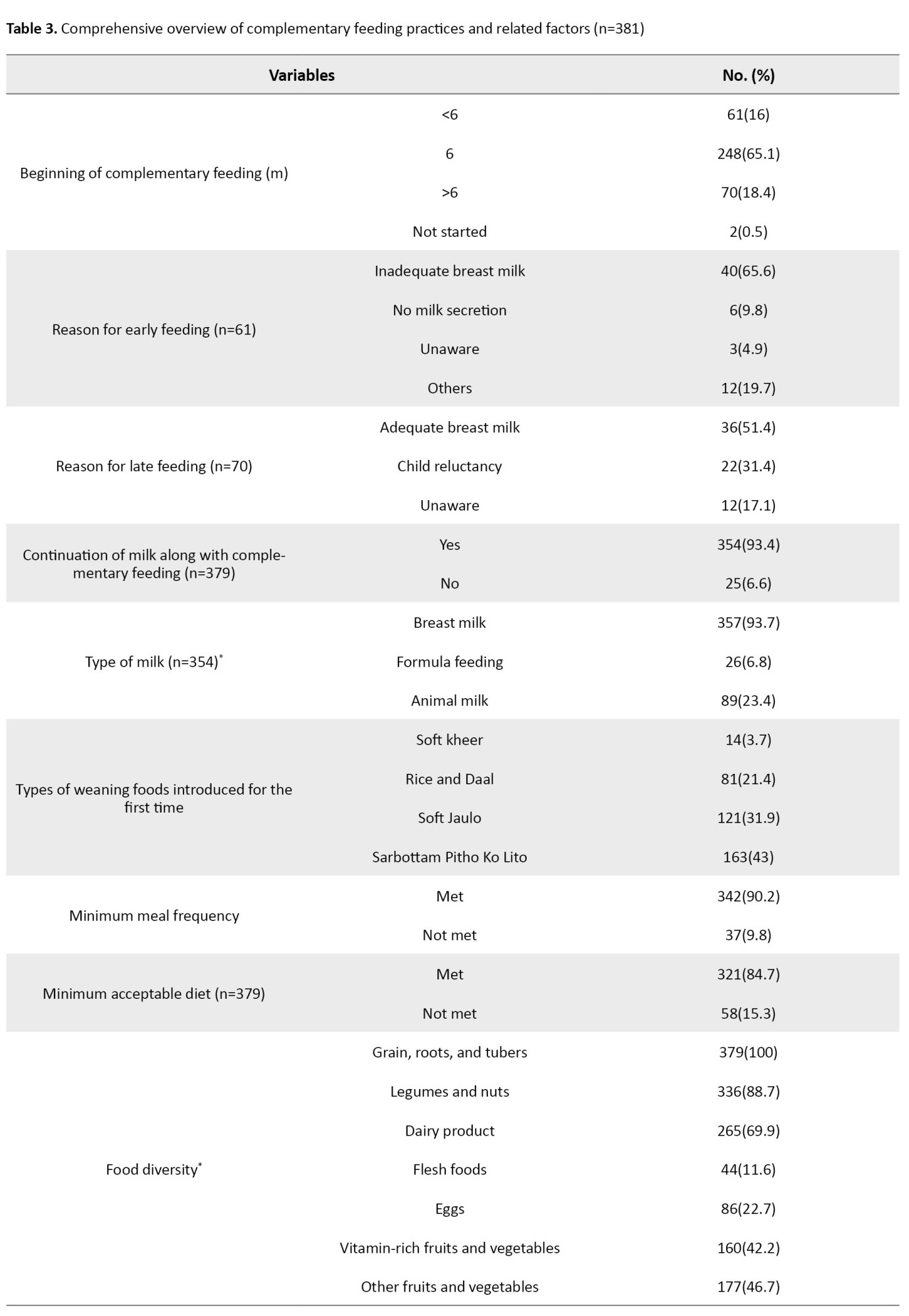
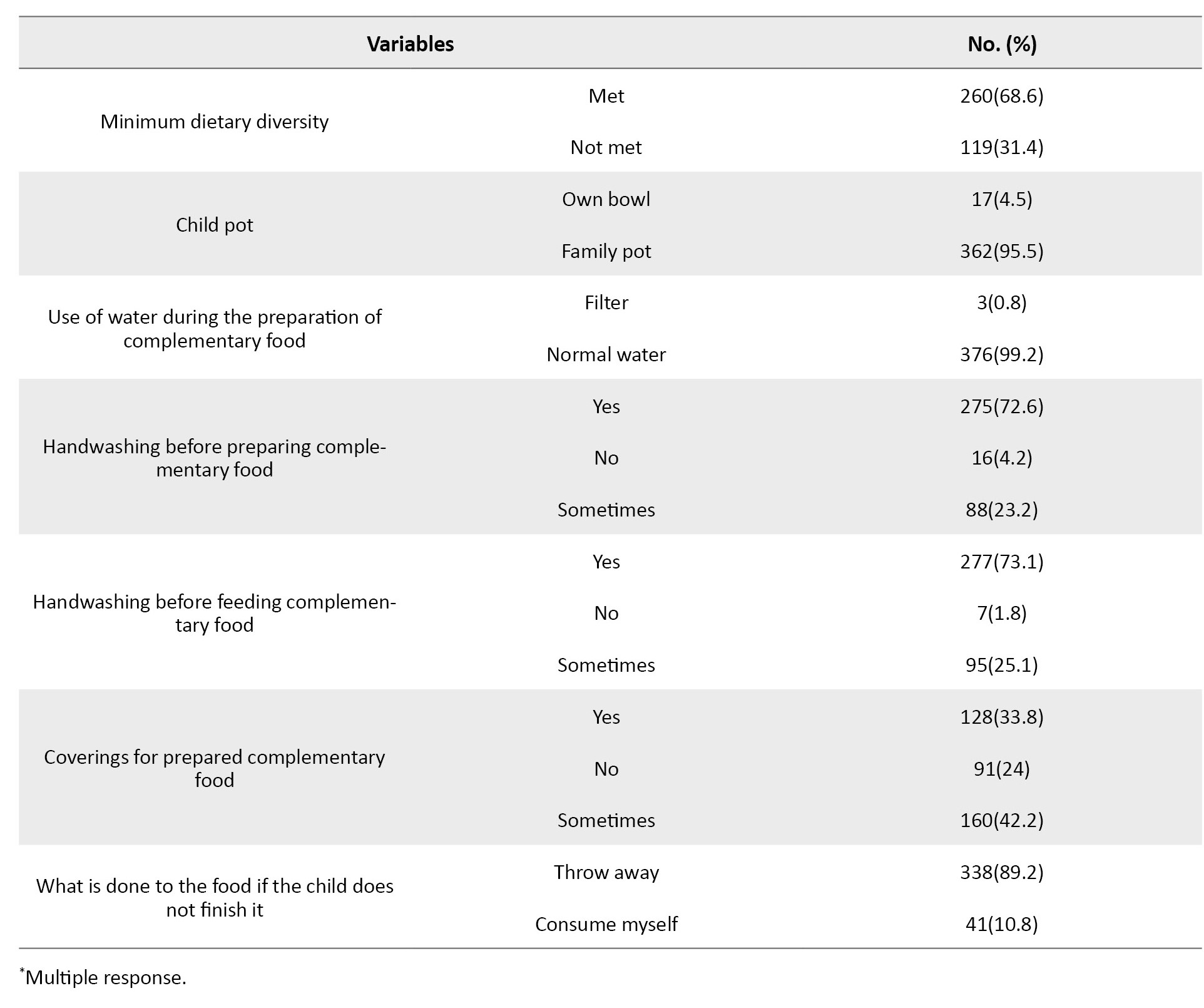
Out of the participants, the majority (65.1%) initiated complementary feeding at 6 months. However, many respondents started late (18.4%), and 16% began early. Among those who initiated early, the primary reason cited by the majority (65.6%) was inadequate breast milk. On the other hand, for those who started late, the main reason the majority gave (51.4%) was adequate breast milk supply.
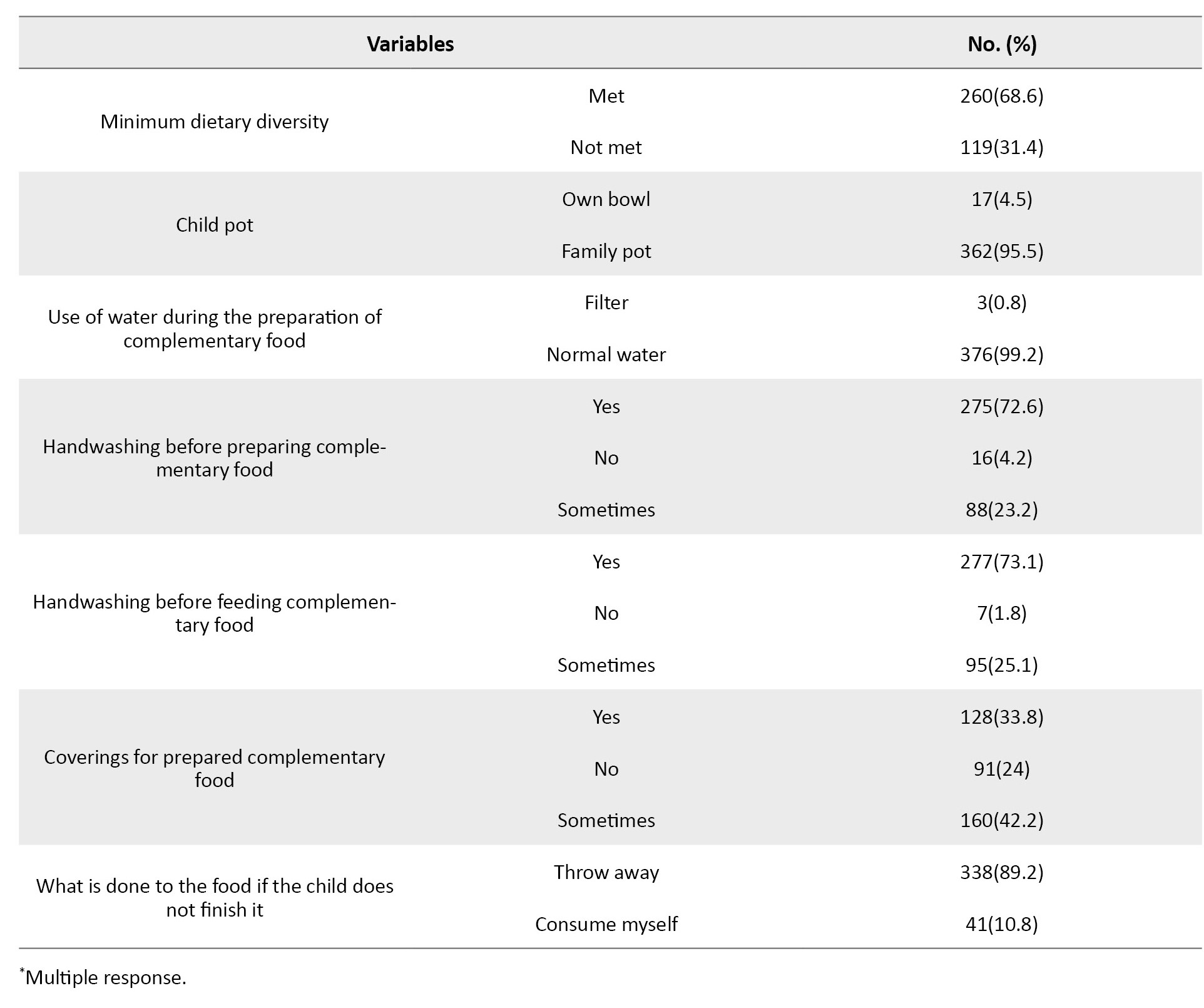
Regarding the types of weaning foods introduced, 43% of respondents reported using “Sarbottam Pitho” (Lito). Furthermore, a significant percentage of respondents (93.4%) continued providing milk and complementary feeding. In terms of meeting recommended feeding standards, the majority of respondents achieved minimum dietary diversity (68.6%), minimum meal frequency (90.2%), and minimum acceptable diet (84.7%). These results are presented in Table 3.
Out of the mothers who participated in our study, only 38.6% followed appropriate complementary feeding practices, and 61.4% were identified as having inappropriate feeding practices based on WHO guidelines.
In the bivariate analyses, only variables significantly associated with complementary feeding practices (both appropriate and inappropriate) were incorporated into their respective models. Both models exhibited a satisfactory fit, as indicated by the omnibus tests of model coefficients (P=0.001) and the Hosmer and Lemeshow Test (P=0.957), with a Nagelkerke pseudo-R2 of 0.14.
In the multivariate analysis (Table 4), the odds of appropriate complementary feeding practices were significantly higher among mothers whose children were aged 12-24 months, with a pronounced considerable increase of more than two times (adjusted odds ratio [aOR]=2.2, 95% CI; 1.4, 3.5, P=0.001).
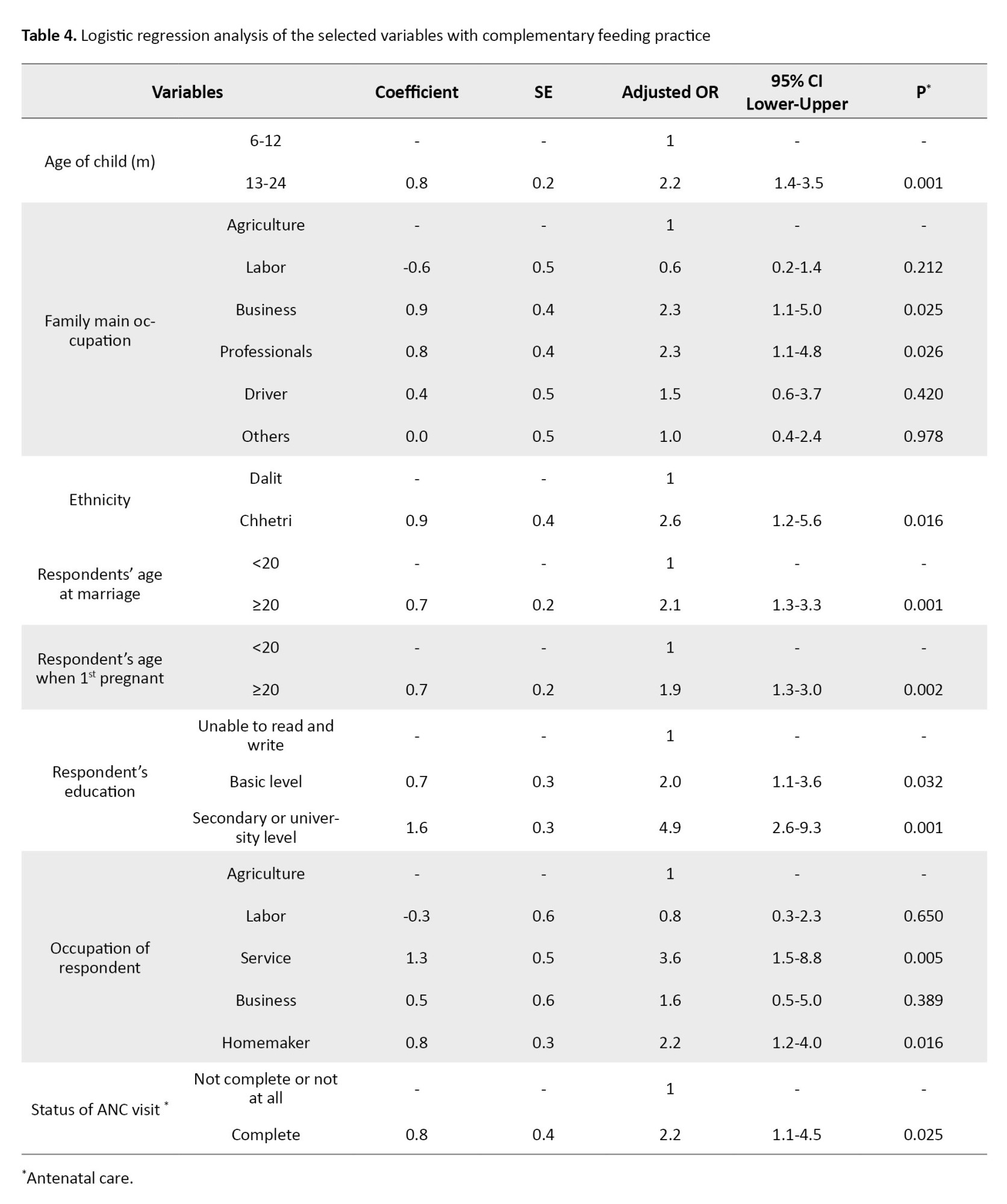
Additionally, higher odds were observed among mothers whose family’s primary income source was a business (aOR=2.3, 95% CI; 1.1, 5.0, P=0.025) or those in professional occupations (aOR=2.3, 95% CI; 1.1, 4.8, P=0.026). Other factors associated with increased odds of appropriate complementary feeding practices included being of Chhetri ethnicity (aOR=2.6, 95% CI; 1.2, 5.6, P=0.016), being ≥20 years at marriage (aOR=2.1, 95% CI; 1.3, 3.3; P=0.001), being ≥20 years at first pregnancy (aOR=1.9, 95% CI; 1.3, 3.0, P=0.002), having basic level education (aOR=2.0, 95% CI; 1.1, 3.6, P=0.032), or possessing secondary or university level education (aOR=4.9, 95% CI; 2.6, 9.3, P=0.001).
Furthermore, higher odds of appropriate complementary feeding practices were associated with mothers who were homemakers (aOR=2.2, 95% CI; 1.2, 4.0, P=0.016), engaged in service occupations (aOR=3.6, 95% CI; 1.5, 8.8, P=0.005), and had a history of complete ANC visits (aOR=2.2, 95% CI; 1.1, 4.5, P=0.025).
Discussion
After 6 months, breast milk alone is insufficient for an infant’s nutritional needs. Introducing appropriate complementary foods alongside continued breastfeeding until age 2 or older is crucial to prevent undernourishment during the transition from exclusive breastfeeding. Our study aims to identify the ferequency of appropriate complementary feeding and its associated factors among mothers of 6 to 24-month-old children in rural areas in Nepal.
Our study found that many mothers initiated complementary feeding at the recommended 6-month mark. However, this percentage differed from findings reported elsewhere, highlighting regional variations in practices. For instance, a study conducted in Coastal South India [13] reported a higher percentage of mothers initiating feeding on time, while a study in Bhaktapur district, Nepal [4], revealed a lower rate. These discrepancies could be attributed to cultural beliefs about breastfeeding duration, access to information about complementary feeding practices, or socioeconomic factors influencing food availability. Further research exploring these factors across diverse regions of Nepal would be valuable in understanding the underlying reasons behind these variations.
A significant proportion of children in our study met the minimum meal frequency (MMF) criteria. This result contrasts with studies in Ethiopia [14, 15], India [16], and Pakistan [17], where lower percentages have been reported. These disparities might be due to study setting variations and sociocultural factors influencing child feeding routines. It is possible that rural Nepali communities traditionally practice frequent feeding throughout the day, which aligns well with MMF recommendations. Yet, further research is required to understand how cultural norms impact these practices and their effect on children’s nutrient intake.
In this study, a high percentage of mothers met the MMF criteria, which contrasts with findings from studies in Lumbini Province, Nepal [12], Ethiopia [14], and India [18], where lower percentages were reported. These differences underscore the influence of regional factors on feeding practices. Recent public health initiatives promoting balanced diets for children might have contributed to these improvements. Alternatively, rural Nepal’s specific food availability and cultural preferences might contribute to a more diverse diet than other regions. Further research, including dietary assessments, is needed to understand children’s diets and identify nutritional gaps.
The percentage of mothers meeting the minimum dietary diversity criteria was slightly lower than the national survey results [19] but consistent with a study conducted in the western hilly region of Nepal [10]. Studies conducted in Lebanon [20] and Ethiopia [14] showed lower percentages than our research. This finding highlights the influence of regional dietary patterns. Notably, all mothers in our study provided food from the grains, tubers, and roots group, reflecting cultural preferences in Nepal, as observed in other studies conducted within the country [4]. However, the results from the studies conducted in Northwest Ethiopia [15] and Iseyin, Nigeria [21] showed lower percentages in the consumption of grains, roots, and tubers than in our study. This difference could be attributed to variations in cultural practices, dietary preferences, and the availability of food resources. Grains, tubers, and roots are more commonly consumed in the Nepalese community due to cultural preferences and traditional dishes, which might explain the higher consumption in our study compared to the others.
Our findings suggest that mothers with children between 12-24 months are more likely to practice appropriate feeding practices, consistent with previous research [21]. Additionally, maternal education level and complete ANC follow-up status emerged as positive indicators for proper complementary feeding practice, aligning with findings from studies in Ethiopia [14, 22, 23]. Mothers with higher education might better understand appropriate complementary feeding practices due to increased access to information. Similarly, mothers who complete their ANC visits likely receive guidance from healthcare professionals on infant feeding practices.
This cross-sectional study was conducted in a rural area, limiting its generalizability to the broader population. The use of purposive sampling introduces potential selection bias. Future studies with larger and more diverse samples are needed to validate our findings. We recommend assessing mothers’ knowledge of complementary feeding practices in future research, as inadequate education contributes to malnutrition.
Our study highlighted that early marriage and pregnancy among respondents are prevalent despite being illegal according to Nepalese laws. While many respondents adhered to recommended dietary frequencies and continued breastfeeding alongside complementary feeding, a significant proportion demonstrated inappropriate practices as per WHO guidelines.
The study underscores the importance of maternal education on timely complementary feeding introduction to meet children’s nutritional needs. Addressing inadequate breast milk production through education is crucial. Discouraging animal milk feeding and promoting diverse food groups, particularly meat, for balanced nutrition is essential. Attention to proper food preparation and safety practices is necessary. Efforts to prevent child marriage, delay early pregnancy, improve education access, and promote ANC visits are vital. These factors significantly influence complementary feeding practices.
Despite limitations, our findings contribute to maternal and child health knowledge, serving as a basis for targeted interventions to enhance feeding practices and child nutrition.
Ethical Considerations
Compliance with ethical guidelines
Before conducting the study, we obtained permission from the relevant authority of the selected Municipality. Additionally, the research protocol received ethical approval from the Institutional Review Committee of Yeti Health Science Academy (YHSA) (Code: 079/70). The study’s objective was transparently communicated to each participant, and informed consent was obtained from all participants before conducting interviews. We ensured that participants had the right to refuse participation and that their decision to decline involvement was fully respected.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Study design and statistical analysis: Rajesh Karki; Data collection and initial draft preparation: Shreeya Joshi; Review and editing: Rajesh Karki and Maheshor Kaphle; Final approval; All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank Surendra Bahadur Bohara and Kailash Bahadur, Ward Chairpersons of Wards No. 2 and No. 3, for granting us data collection permission. Our gratitude extends to FCHVs Tipuri Bohara, Sushila Bohara, and Ujeli B.K. for their invaluable assistance during data collection. The authors acknowledge the ethical clearance provided by the Institutional Review Committee of Yeti Health Science Academy, and appreciate the participants for their time and insights, which enrich our study.
References
The first six months are crucial for infant development, and the World Health Organization (WHO) recommends exclusive breastfeeding during this period. However, as breastfeeding alone may become insufficient afterward, the introduction of complementary feeding is advised [1]. Effective breastfeeding and complementary feeding practices play a vital role in reducing under-five mortality. Research shows that growth faltering can start at 3 months and persist for 2 years. Despite optimal breastfeeding, children may be at risk of stunting if they lack adequate dietary intake, variety, and meal frequency after 6 months of age [2].
This critical period extends from 6 to 18-24 months and significantly impacts the global prevalence of malnutrition in children under five years [3]. Complementary feeding, as defined by WHO and the United Nations Children’s Fund (UNICEF), involves the introduction of solid, semi-solid, or other foods alongside breastfeeding [4].
The initial 1000 days of life are crucial for long-term health and development, especially from 6 to 24 months, which is particularly sensitive. During this phase, complementary feeding plays an increasingly vital role, emphasizing the importance of consuming nutritious foods [5]. According to WHO, introducing complementary foods in a timely manner can save the lives of over 820000 children every year. In 2008, WHO designed various measures to assess the effectiveness of infant and young child feeding (IYCF) practices. However, these measurements reveal that many children in low- and middle-income countries frequently lack adequate complementary feeding [6, 7].
Nepal actively addresses malnutrition through policies and programs, yet it has remained a significant public health issue. High rates of underweight children (19%) and alarming anemia prevalence (43% in under-five, 65% in the 6-23 months age group) persist [8]. One primary cause of malnutrition is inadequate or limited maternal knowledge regarding what, when, and how to feed a child, rather than food unavailability [9]. Additional factors include maternal education, nutritional counseling, food security, number of children, maternal health services, decision-making power, poverty, lack of access to clean water and sanitation, poor hygiene practices, and inadequate care and feeding practices [8, 10]. Complementary feeding practices in Nepal have made limited progress over the past 15 years, with an average yearly growth rate of only 1% to 2% [11]. Regular assessments of infant and young child feeding practices are crucial for evidence-based decision-making to combat undernourishment [12]. Therefore, this study aims to identify the prevalence of complementary feeding practices and associated factors among mothers with children aged 6-24 months. To our knowledge, this is the first study conducted on complementary feeding practices in this rural area. Analyzing the current prevalence of complementary feeding practices and uncovering the factors can provide baseline information for the concerned municipalities to develop effective public health intervention programs.
Materials and Methods
A community-based cross-sectional study was conducted in Surma Rural Municipality, Sudurpashchim Province (Far-West Province), Nepal, in 2023. Mothers with children aged between 6 and 24 months were recruited from the study area. The sample size was calculated considering a 95% confidence interval (CI), a proportion of timely initiation of complementary feeding estimated at 53% based on previous research [10], and a desired margin of error of 5%. This calculation resulted in a sample size of 384. A total of 381 mothers from the selected sample actively participated, achieving a response rate of 99.2%.
Only eligible mothers permanently residing in Surma Municipality with children aged 6-24 months, who were available during data collection and willing to participate, were included. Individuals who did not provide consent and family members other than mothers were excluded from the study.
Study participants were selected using purposive sampling due to the challenges of tracing respondents’ houses within limited time and resources. Before their selection, the female community health volunteers (FCHVs) were contacted and informed about the study’s objectives. The FCHVs provided a list of households with mothers having children between 6-24 months. Subsequently, each household, including the mothers of the children, was visited as per the provided list. Assistance from the FCHVs was sought to locate the homes. When the mothers were unavailable during the initial data collection, a second visit to the same household was attempted. However, if the mothers were still absent during the second attempt, they were excluded from the study.
Face-to-face interviews were conducted by trained researchers using the Nepali language from March 27th to April 7th, 2023. After conducting an extensive literature review, a researcher-made questionnaire was used to assess the information on the sociodemographic characteristics of the mother and child and maternal factors. The practice of complementary feeding was evaluated using the WHO guidelines [6]. The questionnaire included 17 questions covering initiation time, additional breastfeeding, meal frequency, dietary diversity, and hygiene practices. To determine the quantity of food and evaluate the minimum acceptable diet, a 250-mL cup was provided to mothers, allowing them to indicate the amount of food they fed to their children. The nutritional status of children was measured using the mid-upper arm circumference (MUAC) tape.
To ensure the validity of the instrument, three experts in public health and nutrition participated in the validation process and evaluated the questionnaire based on criteria such as clarity, relevance, appropriateness, and cultural sensitivity. Additionally, a pilot study was conducted among 40 respondents at Jaya Prithvi Municipality to enhance the reliability of the questionnaire. We evaluated the participants’ understanding of the questionnaire during the pilot study. We assessed if the questions were clear, easy to answer, and understandable. Also, we checked for redundancy and identified any questions that might be confusing or unnecessary. Based on this feedback, we refined the questionnaire to improve its clarity, ease of use, and overall flow. This condition allowed us to assess the consistency and stability of the questionnaire’s results. Based on the feedback and data collected during the pilot study, necessary modifications were made to improve the instrument’s reliability.
Children aged 6-24 months who were introduced to solid or semi-solid food precisely at 6 months of age, fed at the required frequency, given the appropriate quantity of food for their age, and provided with at least 4 out of the 7 food categories outlined in the WHO feeding practice guidelines were considered to have appropriate complementary feeding practices [6]. Data coding and entering to software was done after data collection. Descriptive statistics were employed for categorical variables. The Pearson’s chi-square test assessed the association between independent variables and the practice of complementary feeding (appropriate and inappropriate). The most prevalent predictors for complementary feeding practices were determined using multivariate logistic regression analysis, incorporating variables that demonstrated a significant association at the bivariate level. All statistical significance was determined at a significance level of P<0.05. All analyses were performed using IBM SPSS statistics software, version 26.
Results
The sociodemographic characteristics of mothers are presented in Table 1.
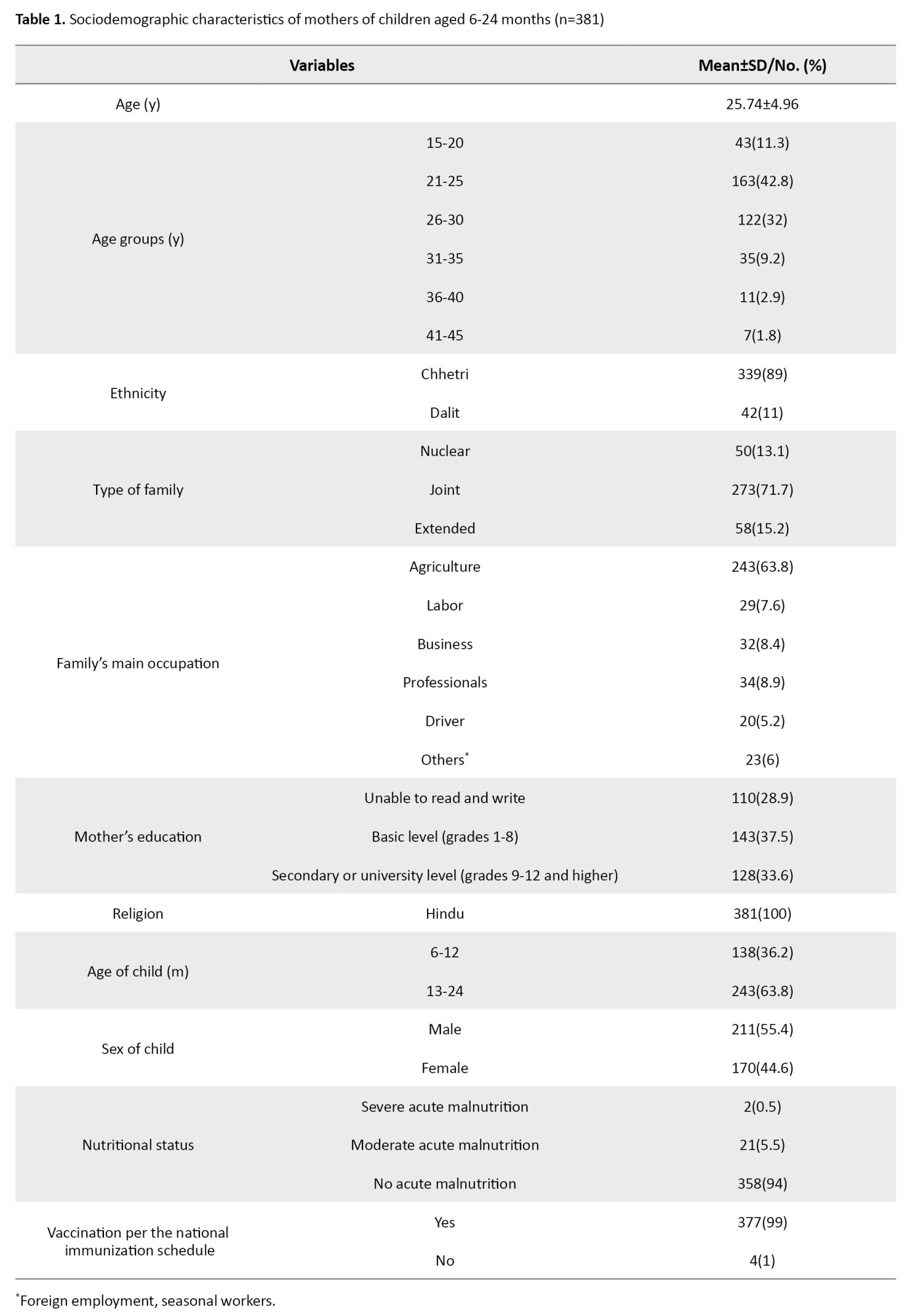
Among the 381 respondents, the majority (42.8%) belonged to the age group of 21-25 years, with a mean age of 25.74±4.96 years. The ethnicity of most respondents was Chhetri (89%), and all participants identified as Hindus. In addition, a significant number of respondents (71.7%) lived in joint families, with agriculture being the primary source of income for the majority (63.8%). Moreover, a majority of the respondents (37.5%) had received only basic level education.
Regarding the children, the majority (63.8%) fell within the age range of 13-24 months, and 55.4% were male. Notably, 94% of the children showed no signs of acute malnutrition, and 99% of the children had received vaccinations in accordance with the national immunization schedule.
The mean age at which the mothers got married was 18.32±2.38 years. A significant portion of the mothers (51.4%) became pregnant for the first time before age 20. The majority of the mothers (73.8%) were engaged in agriculture. Furthermore, a high percentage of mothers (90.8%) gave birth to their most recent child at a government health institution. Regarding mode of delivery, nearly all mothers (96.1%) had a spontaneous vaginal delivery. Approximately 86.6% of the mothers had attended all the recommended antenatal care (ANC) visits. These results are presented in Table 2.
Out of the participants, the majority (65.1%) initiated complementary feeding at 6 months. However, many respondents started late (18.4%), and 16% began early. Among those who initiated early, the primary reason cited by the majority (65.6%) was inadequate breast milk. On the other hand, for those who started late, the main reason the majority gave (51.4%) was adequate breast milk supply.
Regarding the types of weaning foods introduced, 43% of respondents reported using “Sarbottam Pitho” (Lito). Furthermore, a significant percentage of respondents (93.4%) continued providing milk and complementary feeding. In terms of meeting recommended feeding standards, the majority of respondents achieved minimum dietary diversity (68.6%), minimum meal frequency (90.2%), and minimum acceptable diet (84.7%). These results are presented in Table 3.
Out of the mothers who participated in our study, only 38.6% followed appropriate complementary feeding practices, and 61.4% were identified as having inappropriate feeding practices based on WHO guidelines.
In the bivariate analyses, only variables significantly associated with complementary feeding practices (both appropriate and inappropriate) were incorporated into their respective models. Both models exhibited a satisfactory fit, as indicated by the omnibus tests of model coefficients (P=0.001) and the Hosmer and Lemeshow Test (P=0.957), with a Nagelkerke pseudo-R2 of 0.14.
In the multivariate analysis (Table 4), the odds of appropriate complementary feeding practices were significantly higher among mothers whose children were aged 12-24 months, with a pronounced considerable increase of more than two times (adjusted odds ratio [aOR]=2.2, 95% CI; 1.4, 3.5, P=0.001).
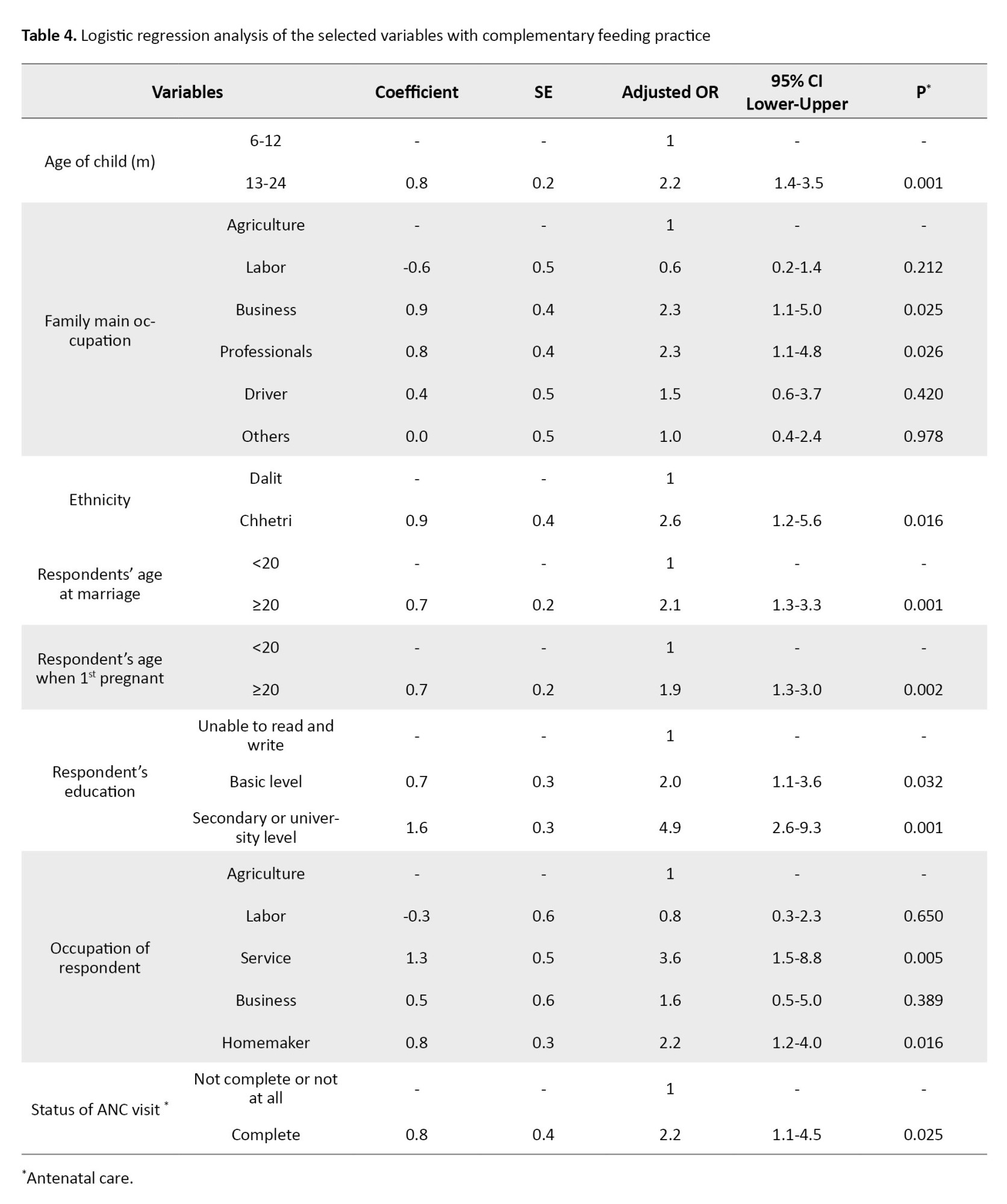
Additionally, higher odds were observed among mothers whose family’s primary income source was a business (aOR=2.3, 95% CI; 1.1, 5.0, P=0.025) or those in professional occupations (aOR=2.3, 95% CI; 1.1, 4.8, P=0.026). Other factors associated with increased odds of appropriate complementary feeding practices included being of Chhetri ethnicity (aOR=2.6, 95% CI; 1.2, 5.6, P=0.016), being ≥20 years at marriage (aOR=2.1, 95% CI; 1.3, 3.3; P=0.001), being ≥20 years at first pregnancy (aOR=1.9, 95% CI; 1.3, 3.0, P=0.002), having basic level education (aOR=2.0, 95% CI; 1.1, 3.6, P=0.032), or possessing secondary or university level education (aOR=4.9, 95% CI; 2.6, 9.3, P=0.001).
Furthermore, higher odds of appropriate complementary feeding practices were associated with mothers who were homemakers (aOR=2.2, 95% CI; 1.2, 4.0, P=0.016), engaged in service occupations (aOR=3.6, 95% CI; 1.5, 8.8, P=0.005), and had a history of complete ANC visits (aOR=2.2, 95% CI; 1.1, 4.5, P=0.025).
Discussion
After 6 months, breast milk alone is insufficient for an infant’s nutritional needs. Introducing appropriate complementary foods alongside continued breastfeeding until age 2 or older is crucial to prevent undernourishment during the transition from exclusive breastfeeding. Our study aims to identify the ferequency of appropriate complementary feeding and its associated factors among mothers of 6 to 24-month-old children in rural areas in Nepal.
Our study found that many mothers initiated complementary feeding at the recommended 6-month mark. However, this percentage differed from findings reported elsewhere, highlighting regional variations in practices. For instance, a study conducted in Coastal South India [13] reported a higher percentage of mothers initiating feeding on time, while a study in Bhaktapur district, Nepal [4], revealed a lower rate. These discrepancies could be attributed to cultural beliefs about breastfeeding duration, access to information about complementary feeding practices, or socioeconomic factors influencing food availability. Further research exploring these factors across diverse regions of Nepal would be valuable in understanding the underlying reasons behind these variations.
A significant proportion of children in our study met the minimum meal frequency (MMF) criteria. This result contrasts with studies in Ethiopia [14, 15], India [16], and Pakistan [17], where lower percentages have been reported. These disparities might be due to study setting variations and sociocultural factors influencing child feeding routines. It is possible that rural Nepali communities traditionally practice frequent feeding throughout the day, which aligns well with MMF recommendations. Yet, further research is required to understand how cultural norms impact these practices and their effect on children’s nutrient intake.
In this study, a high percentage of mothers met the MMF criteria, which contrasts with findings from studies in Lumbini Province, Nepal [12], Ethiopia [14], and India [18], where lower percentages were reported. These differences underscore the influence of regional factors on feeding practices. Recent public health initiatives promoting balanced diets for children might have contributed to these improvements. Alternatively, rural Nepal’s specific food availability and cultural preferences might contribute to a more diverse diet than other regions. Further research, including dietary assessments, is needed to understand children’s diets and identify nutritional gaps.
The percentage of mothers meeting the minimum dietary diversity criteria was slightly lower than the national survey results [19] but consistent with a study conducted in the western hilly region of Nepal [10]. Studies conducted in Lebanon [20] and Ethiopia [14] showed lower percentages than our research. This finding highlights the influence of regional dietary patterns. Notably, all mothers in our study provided food from the grains, tubers, and roots group, reflecting cultural preferences in Nepal, as observed in other studies conducted within the country [4]. However, the results from the studies conducted in Northwest Ethiopia [15] and Iseyin, Nigeria [21] showed lower percentages in the consumption of grains, roots, and tubers than in our study. This difference could be attributed to variations in cultural practices, dietary preferences, and the availability of food resources. Grains, tubers, and roots are more commonly consumed in the Nepalese community due to cultural preferences and traditional dishes, which might explain the higher consumption in our study compared to the others.
Our findings suggest that mothers with children between 12-24 months are more likely to practice appropriate feeding practices, consistent with previous research [21]. Additionally, maternal education level and complete ANC follow-up status emerged as positive indicators for proper complementary feeding practice, aligning with findings from studies in Ethiopia [14, 22, 23]. Mothers with higher education might better understand appropriate complementary feeding practices due to increased access to information. Similarly, mothers who complete their ANC visits likely receive guidance from healthcare professionals on infant feeding practices.
This cross-sectional study was conducted in a rural area, limiting its generalizability to the broader population. The use of purposive sampling introduces potential selection bias. Future studies with larger and more diverse samples are needed to validate our findings. We recommend assessing mothers’ knowledge of complementary feeding practices in future research, as inadequate education contributes to malnutrition.
Our study highlighted that early marriage and pregnancy among respondents are prevalent despite being illegal according to Nepalese laws. While many respondents adhered to recommended dietary frequencies and continued breastfeeding alongside complementary feeding, a significant proportion demonstrated inappropriate practices as per WHO guidelines.
The study underscores the importance of maternal education on timely complementary feeding introduction to meet children’s nutritional needs. Addressing inadequate breast milk production through education is crucial. Discouraging animal milk feeding and promoting diverse food groups, particularly meat, for balanced nutrition is essential. Attention to proper food preparation and safety practices is necessary. Efforts to prevent child marriage, delay early pregnancy, improve education access, and promote ANC visits are vital. These factors significantly influence complementary feeding practices.
Despite limitations, our findings contribute to maternal and child health knowledge, serving as a basis for targeted interventions to enhance feeding practices and child nutrition.
Ethical Considerations
Compliance with ethical guidelines
Before conducting the study, we obtained permission from the relevant authority of the selected Municipality. Additionally, the research protocol received ethical approval from the Institutional Review Committee of Yeti Health Science Academy (YHSA) (Code: 079/70). The study’s objective was transparently communicated to each participant, and informed consent was obtained from all participants before conducting interviews. We ensured that participants had the right to refuse participation and that their decision to decline involvement was fully respected.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Study design and statistical analysis: Rajesh Karki; Data collection and initial draft preparation: Shreeya Joshi; Review and editing: Rajesh Karki and Maheshor Kaphle; Final approval; All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank Surendra Bahadur Bohara and Kailash Bahadur, Ward Chairpersons of Wards No. 2 and No. 3, for granting us data collection permission. Our gratitude extends to FCHVs Tipuri Bohara, Sushila Bohara, and Ujeli B.K. for their invaluable assistance during data collection. The authors acknowledge the ethical clearance provided by the Institutional Review Committee of Yeti Health Science Academy, and appreciate the participants for their time and insights, which enrich our study.
References
- Al-Samarrai MAM, Al-Rawi RA, Yaseen SM, Jadoo SAA. Knowledge, attitude, and practice of mothers about complementary feeding for infants aged 6-12 months in Anbar Province, Iraq. J Ideas Health. 2020; 3(1):125-9. [DOI:10.47108/jidhealth.Vol3.Iss1.17]
- Chhabra P, Gupta A, Thakur N. Complementary feeding practices and nutritional status of children (6-23 months) in an urban resettlement colony of East Delhi. Indian J Community Med. 2021; 46(3):528-32. [DOI:10.4103/ijcm.IJCM_1046_20] [PMID] [PMCID]
- Deuja V. Complementary feeding practices among mothers having 6-24 months children in Pokhari VDC of Doti District [MA thesis]. Kathmandu: Tribhuvan University; 2017. [Link]
- Ulak N, Kc D, Tiwari K. Complementary feeding practices and it’s associated factors among mothers in selected urban area of Nepal. Asp Biomed Clin Case Rep. 2020; 3(1):6-14. [DOI:10.36502/2020/ASJBCCR.6176]
- Sirkka O, Abrahamse-Berkeveld M, van der Beek EM. Complementary feeding practices among young children in China, India, and Indonesia: A narrative review. Curr Dev Nutr. 2022; 6(6):nzac092. [DOI:10.1093/cdn/nzac092] [PMID] [PMCID]
- World Health Organization. Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. Geneva: World Health Organization; 2009. [Link]
- Esan DT, Adegbilero-Iwari OE, Hussaini A, Adetunji AJ. Complementary feeding pattern and its determinants among mothers in selected primary health centers in the urban metropolis of Ekiti State, Nigeria. Sci Rep. 2022; 12(1):6252. [DOI:10.1038/s41598-022-10308-7] [PMID] [PMCID]
- Ministry of Health and Population (Nepal). Annual report (2021/2022). Kathmandu: Ministry of Health and Population ;2023. [Link]
- Mutuku JN, Ochola S, Osero J. Maternal knowledge and complementary feeding practices and their relationship with nutritional status among children 6-23 months old in pastoral community of marsabit county, kenya: A cross-sectional study. Curr Res Nutr Food Sci. 2020; 8(3):862-76. [DOI:10.12944/CRNFSJ.8.3.17]
- Adhikari N, Acharya K, Upadhya DP, Pathak S, Pokharel S, Pradhan PMS. Infant and young child feeding practices and its associated factors among mothers of under two years children in a western hilly region of Nepal. PLoS One. 2021; 16(12):e0261301. [DOI:10.1371/journal.pone.0261301] [PMID] [PMCID]
- Na M, Aguayo VM, Arimond M, Dahal P, Lamichhane B, Pokharel R, et al. Trends and predictors of appropriate complementary feeding practices in Nepal: An analysis of national household survey data collected between 2001 and 2014. Matern Child Nutr. 2018; 14 Suppl 4(Suppl 4):e12564. [DOI:10.1111/mcn.12564] [PMID] [PMCID]
- Gautam KP, Adhikari M, Khatri RB, Devkota MD. Determinants of infant and young child feeding practices in Rupandehi, Nepal. BMC Res Notes. 2016; 9:135. [DOI:10.1186/s13104-016-1956-z] [PMID] [PMCID]
- Rao S, Swathi P, Unnikrishnan B, Hegde A. Study of complementary feeding practices among mothers of children aged six months to two years-A study from coastal south India. Australas Med J. 2011; 4(5):252-7. [DOI:10.4066/AMJ.2011.607] [PMID] [PMCID]
- Ahmed JA, Sadeta KK, Lenbo KH. Magnitude and factors associated with appropriate complementary feeding practice among mothers of children 6-23 months age in Shashemene town, Oromia-Ethiopia: Community based cross sectional study. Plos One. 2022; 17(3):e0265716. [DOI:10.1371/journal.pone.0265716] [PMID] [PMCID]
- Yeshaneh A, Zebene M, Gashu M, Abebe H, Abate H. Complementary feeding practice and associated factors among internally displaced mothers of children aged 6-23 months in Amhara region, Northwest Ethiopia: A cross-sectional study. BMC Pediatr. 2021; 21(1):583. [DOI:10.1186/s12887-021-03050-y] [PMID] [PMCID]
- Jain S, Bhan BD, Bhatt GC. Complementary feeding practices and their determinants among children 6-23 months of age in an outpatient hospital setting in Central India: A cross-sectional study. J Family Med Prim Care. 2020; 9(2):1187-90. [DOI:10.4103/jfmpc.jfmpc_958_19] [PMID] [PMCID]
- Ali M, Arif M, Shah AA. Complementary feeding practices and associated factors among children aged 6-23 months in Pakistan. PLoS One. 2021; 16(2):e0247602. [DOI:10.1371/journal.pone.0247602] [PMID] [PMCID]
- Dhami MV, Ogbo FA, Osuagwu UL, Agho KE. Prevalence and factors associated with complementary feeding practices among children aged 6-23 months in India: A regional analysis.BMC Public Health. 2019; 19(1):1034. [DOI:10.1186/s12889-019-7360-6] [PMID] [PMCID]
- Ministry of Health and Population. Demographic and Health Survey 2022: Key indicators report. Nepal: Ministry of Health and Population; 2022. [Link]
- Naja F, Hwalla N, Chokor FAZ, Zgheib R, Nasreddine L. Infant and young child feeding practices in Lebanon: A cross-sectional national study. Public Health Nutr. 2023; 26(1):143-59. [DOI:10.1017/S1368980022000842] [PMID] [PMCID]
- Ariyo O, Aderibigbe OR, Ojo TJ, Sturm B, Hensel O. Determinants of appropriate complementary feeding practices among women with children aged 6-23 months in Iseyin, Nigeria. Sci Afr. 2021; 13:e00848. [DOI:10.1016/j.sciaf.2021.e00848]
- Shagaro SS, Mulugeta BT, Kale TD. Complementary feeding practices and associated factors among mothers of children aged 6-23 months in Ethiopia: Secondary data analysis of Ethiopian mini demographic and health survey 2019. Arch Public Health. 2021; 79(1):205. [DOI:10.1186/s13690-021-00725-x] [PMID] [PMCID]
- Gebretsadik MT, Adugna DT, Aliyu AD, Belachew T. Optimal complementary feeding practices of children aged 6-23 months in three agro-ecological rural districts of Jimma zones of southwest Ethiopia. J Nutr Sci. 2023; 12:e40. [DOI:10.1017/jns.2023.26] [PMID] [PMCID]
Article Type : Research |
Subject:
General
Received: 2023/08/29 | Accepted: 2024/02/18 | Published: 2024/07/1
Received: 2023/08/29 | Accepted: 2024/02/18 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |