Mon, Dec 1, 2025
Volume 34, Issue 3 (6-2024)
JHNM 2024, 34(3): 254-261 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mirzaei-Alavijeh M, Amini M, Hosseini S N, Khashij S, Jalilian F. Cervical Cancer Screening Uptake Inequality. JHNM 2024; 34 (3) :254-261
URL: http://hnmj.gums.ac.ir/article-1-2374-en.html
URL: http://hnmj.gums.ac.ir/article-1-2374-en.html
Mehdi Mirzaei-Alavijeh1 

 , Mahin Amini2
, Mahin Amini2 

 , Seyyed Nasrollah Hosseini3
, Seyyed Nasrollah Hosseini3 

 , Shima Khashij4
, Shima Khashij4 

 , Farzad Jalilian *5
, Farzad Jalilian *5 




 , Mahin Amini2
, Mahin Amini2 

 , Seyyed Nasrollah Hosseini3
, Seyyed Nasrollah Hosseini3 

 , Shima Khashij4
, Shima Khashij4 

 , Farzad Jalilian *5
, Farzad Jalilian *5 


1- Associate Professor, Social Development and Health Promotion Research Center, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
2- MSc in Epidemiology, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
3- Assistant Professor, Ministry of Health and Medical Sciences, Tehran, Iran.
4- MSc in Natural Resources Engineering, Social Development and Health Promotion Research Center, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
5- Associate Professor, Social Development and Health Promotion Research Center, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran. ,f_jalilian@yahoo.com
2- MSc in Epidemiology, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
3- Assistant Professor, Ministry of Health and Medical Sciences, Tehran, Iran.
4- MSc in Natural Resources Engineering, Social Development and Health Promotion Research Center, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
5- Associate Professor, Social Development and Health Promotion Research Center, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran. ,
Full-Text [PDF 531 kb]
(256 Downloads)
| Abstract (HTML) (963 Views)
Full-Text: (391 Views)
Introduction
Cervical cancer is the fourth most frequent cancer in women and the third most common cancer in 146 countries, affecting women younger than 45 years old. Furthermore, more than half a million women are diagnosed with cervical cancer annually; cervical cancer resulted in the deaths of 311000 women worldwide in 2018, of which approximately 90% occurred in low- and middle-income countries [1]. Since the introduction of screening programs in high-income countries, the mortality rates of cervical cancer have dropped by more than half over the past 30 years, but it has not changed or increased in low-income countries [2, 3].
There are two very effective prevention strategies for cervical cancer: Human papillomavirus (HPV) vaccination and cervical screening with initial HPV testing followed by the treatment of precancerous lesions. Although the vaccination can prevent 70%-90% of cervical cancer, it cannot prevent cancer if the vaccine is injected in the precancerous phase [4]. Cervical screening is accessible and affordable, and more importantly, it is an effective method for early detection of cervical cancer, especially in developing countries [5]. Results have shown that regular pap smear (PS) test can help early treatment and thus reduce the incidence of cervical cancer in women aged 30-70 years old, especially in the range of 45-55 years old. Therefore, the widespread use of cervical cytology screening in developed countries has significantly reduced cervical cancer and its mortality [6, 7]. Inadequate resources for screening, insufficient education of women about the importance of screening, low socioeconomic status (SES), and low level of education are the most critical factors influencing PS test uptake in women [8, 9, 10, 11].
Due to the importance of cervical cancer health issues and the existence of preventive strategies, screening should be done regularly to reduce the burden of the disease [12]. Performing PS test for early detection of cervical cancer is a practical, inexpensive, necessary, and available method that can significantly reduce the burden of cervical cancer [13]. Therefore, this study aimed to investigate the inequality in cervical cancer screening uptake in women in 2019.
Materials and Methods
This cross-sectional research was conducted from July to September 2019 among 774 women aged 30-75 years living in Kermanshah City, Iran. Samples were selected through multi-stage cluster sampling. First, Kermanshah was divided into 8 areas according to the municipal areas. Then, each area was divided into 10 blocks, and 2 blocks were randomly selected, and eligible households were included in the study from these blocks. Data collection was completed using a written questionnaire and holding interviews. For this study, it was determined that a sample size of 751 individuals was needed. This calculation was based on considering a 4% margin of error, a 50% prevalence rate, and a 25% allowance for dropped samples. Ultimately, data was gathered from 774 participants.
The questionnaire consisted of three parts. In the first part, demographic information was collected. The second section assessed socioeconomic status of the participants. In the third part, participants PS uptakes were assessed.
In section one, age, level of education, marital status, family size, and positive family history of cervical cancer were collected as demographic variables.
In section two, as the main variable of household economic status was calculated using principal component analysis (PCA) and considering participants’ economic and social variables. Socioeconomic status information related to durable goods and social determinants included ownership of cars, refrigerators, televisions, freezers, washing machines, vacuum cleaners, cell phones, bicycles, laptops smear, etc. and the number of rooms in an apartment. Moreover, annual domestic and international travel was questioned. This questionnaire has been used in studies measuring inequality in Iran [14-17].
In section three, to assess whether participants had PS test uptake in the past, they answered the questions “Have you ever had PS test uptake for cervical cancer screening?” and “Have you regularly undergone PS test for cervical cancer screening?”
Four trained public health experts conducted interviews and gathered data for this study. The data were collected by visiting the participants in their homes.
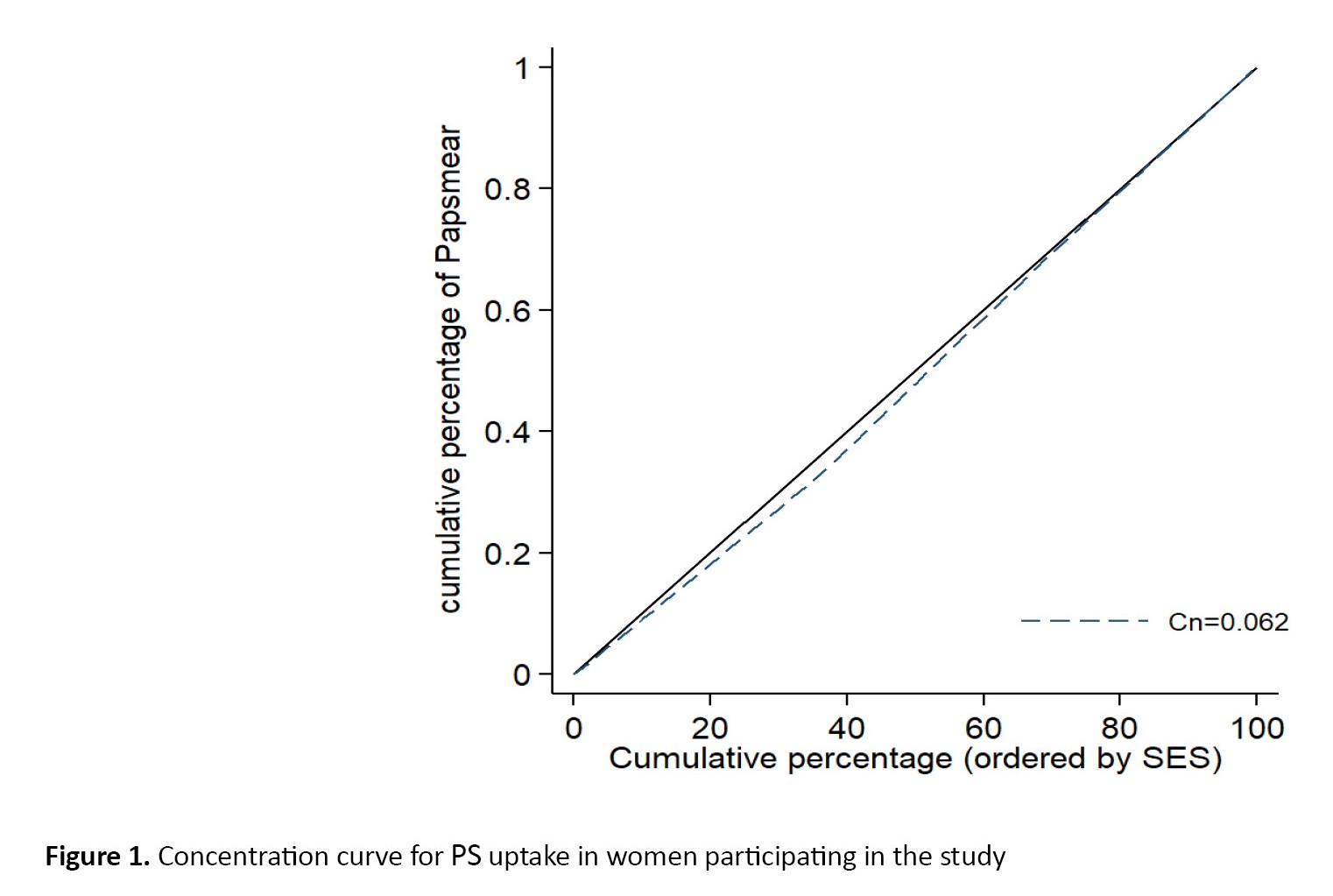
The concentration index (Cn) is defined using a concentration curve. Cn is twice the area between the concentration curve and the isopleth line (45° line). If there is no socioeconomic inequality, Cn will be zero. In this convention, the index takes a negative value if the curve lies above the equivalence line, indicating a disproportionate concentration of the health variable among the poor. It takes a positive value if it lies below the equivalence line [18]. Cn is determined using the Equation 1.
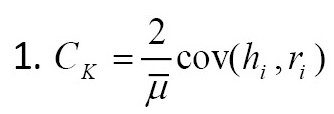
, where is the mean health variable in the entire population and ri each Pearson’s rank in the socioeconomic quintile. ri=1/N for the poorest person and ri=N/N for the richest. hi is the health variable for the person i. According to Equation 1, for binary dependent variables, the Cn may not fall in the -1 to +1 range, in which case the normalized Cn in Equation 2 should be used [19].

In descriptive analysis, numbers and percentages have been used for all nominal and sequential qualitative variables. Logistic regression was used to identify predictors of regular PS test uptake, and model 1 (crude analysis) was used for this analysis. Variables with P>0.25 were excluded from the adjusted model, whereas variables with P<0.25 were included in model 2 (adjusted analysis). It is worth mentioning that widowed women may have different property arrangements than married women. Married women are considered the reference group for the analysis. In this study, a significance level of 5% has been considered for the 95% confidence interval (CI) to confirm the statistical significance of the relationship PS. Data were analyzed using STATA software, version 14 including the chi-square test, t-test, logistic regression, and compensation statistical tests.
Results
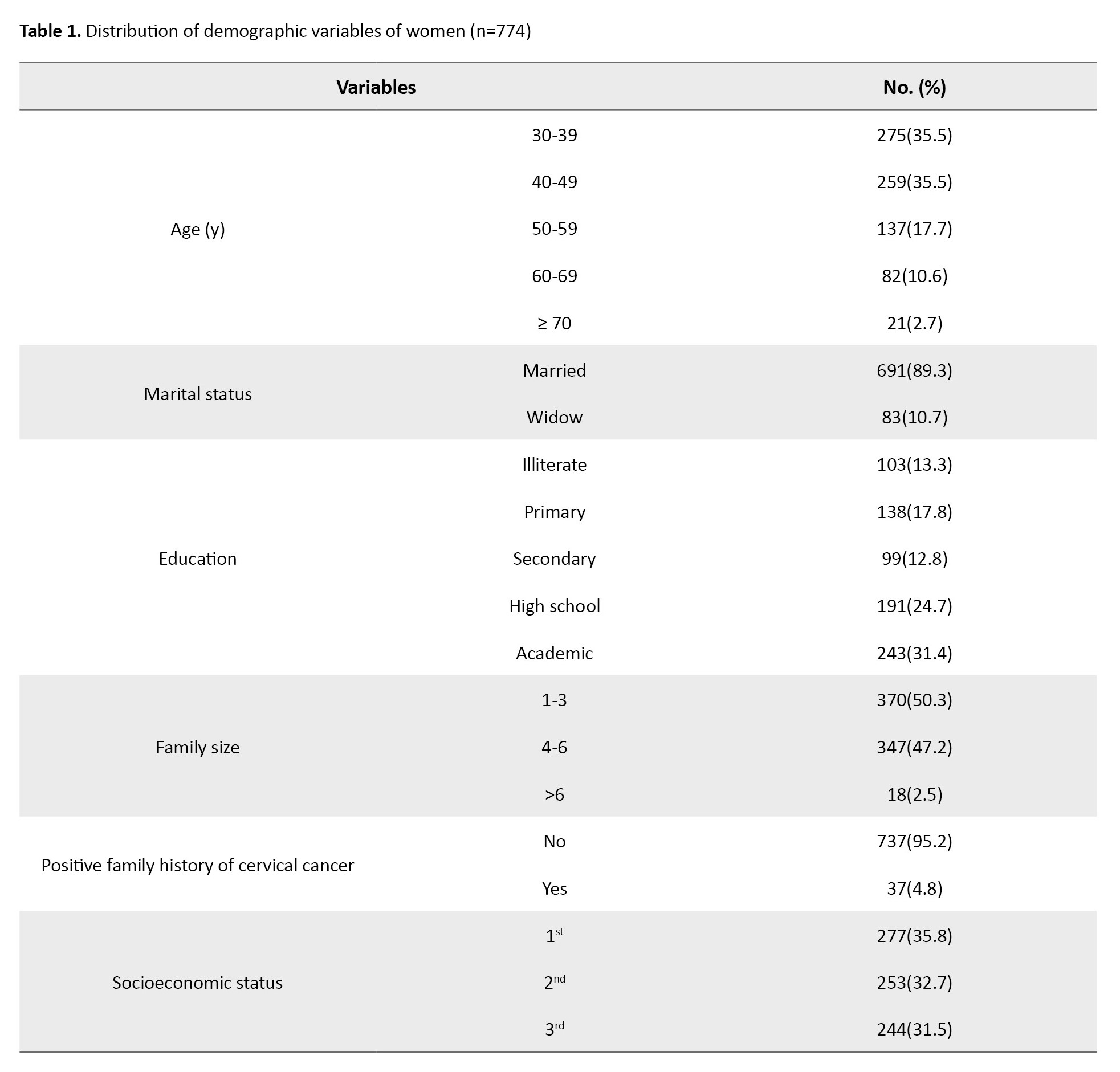
The mean age of participants was 45.42±10.66 years. A total of 450 women (58.1%) had a history of PS test uptake. In addition, 205 women (26.5%) have a regular PS test uptake. Details of the participants’ demographic characteristics are shown in Table 1.
The mean age of women with regular PS test uptake was 44.19±8.89 years. Initially, a logistic regression was conducted to analyze the data, and variables that were not statistically significant (family size and socioeconomic states) were removed from the model. The participants’ education level (OR=1.181, 95% CI; 1.022, 1.364, P=0.024) and a positive family history of cervical cancer (OR=3.591, 95% CI; 1.811, 7.120, P=0.001) had significant impacts on their regular PS test uptake (Table 2).
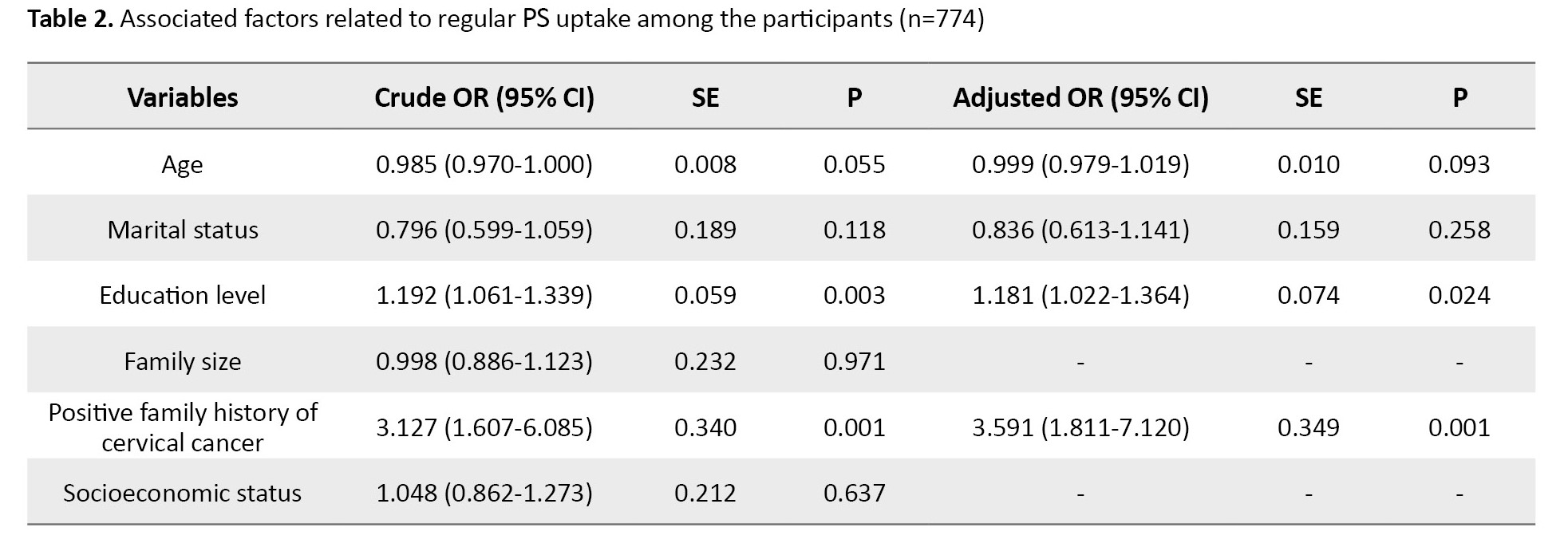
Table 3 indicates that women in the rich category had a notably lower average age.
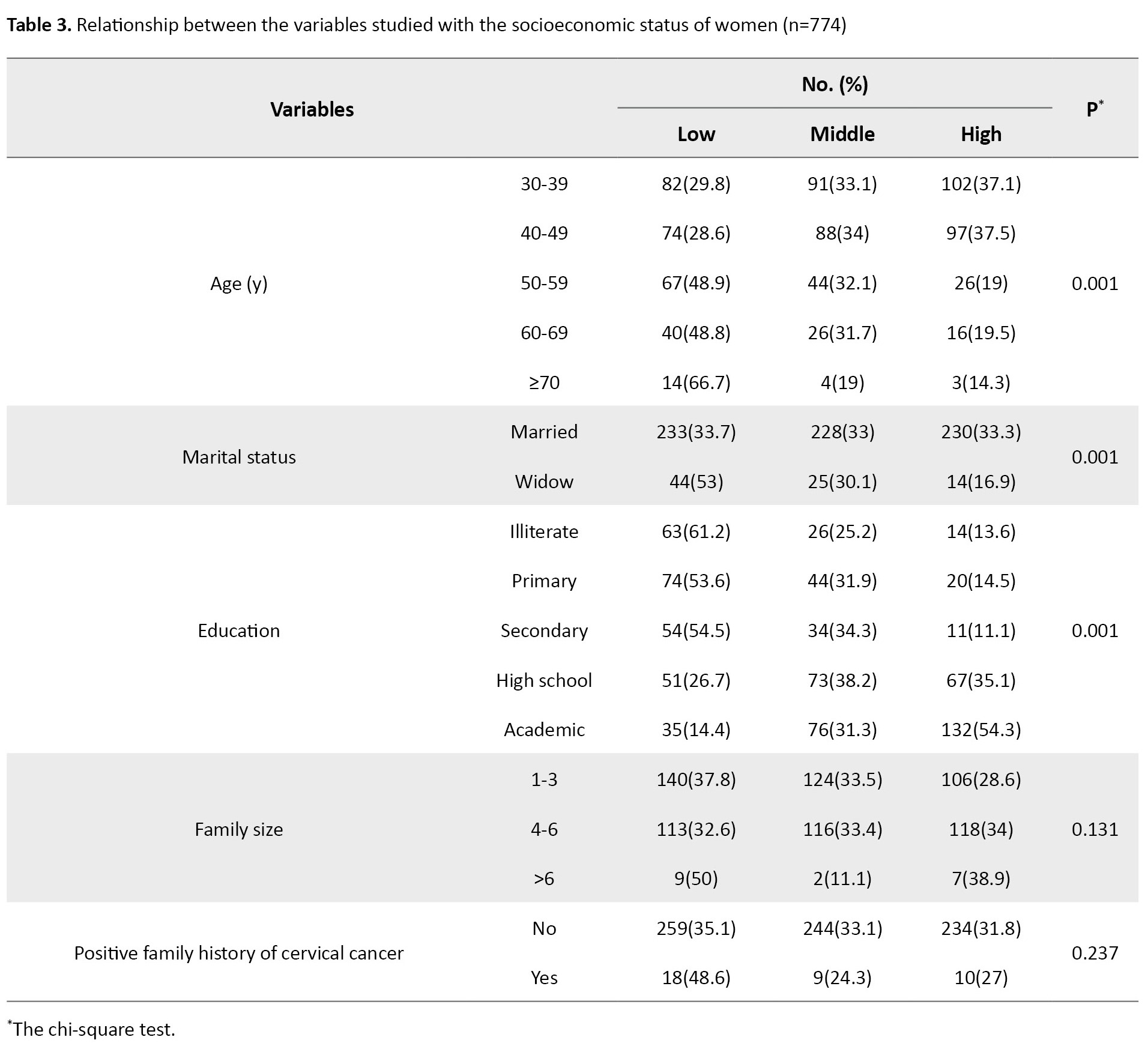
Specifically, the mean age for poor, middle, and rich women was 48.23, 44.80, and 42.86, respectively, with a statistically significant difference. Moreover, when considering socioeconomic status, a higher proportion of married women were observed to belong to the rich group. Additionally, 54.3% of educated women were found in the rich category. It was determined that education level had a significant association with SES. Family size and positive family history of cervical cancer did not show a significant relationship with SES.
The concentration index for PS test uptake in the women was 0.062, which indicates the concentration of PS in the high socioeconomic status of the participants. Still, due to the low value of the index and the lack of statistical significance, it can be concluded that PS test uptake independently with SES has no significant relationship (Figure 1).
Discussion
This study aimed to determine the inequality of cervical cancer screening uptake. Although the numerical value of the concentration index in this study was positive, it was not significant. Given the cheapness and availability of this screening test in Iran, this result is not far-fetched.
It is important to note that a large number of women aged 60 and above were either illiterate or had only completed primary education. However, the research revealed that education was crucial in determining whether women underwent regular PS tests. Additionally, there was a significant connection between education and SES, with educated women generally having better SES. A study examining the barriers to PS uptake in low- and middle-income countries discovered that in Latin American countries, women with low SES had significantly lower rates of PS test uptake. However, age lacked a significant impact on uptake [20]. Moreover, our finding was in line with a study conducted in Brazil by Açucena Vieira Alves et al., which found that a higher level of education positively correlated to cervical cancer screening [21]. Furthermore, Ahmed et al., in a study among female university students in a multiethnic institution, indicated that the increase in PS test uptake was associated with increased knowledge about cervical cancer PS risk factors [22]. These results may highlight the role of information and communication inequality in addressing health disparities, which are important determinants. Compared to illiterate women, educated individuals prioritize their health more [23]. Our findings highlight the education to encourage women, especially older and less educated women, to undergo regular cervical cancer screening. Measures to improve education, especially among older women, are extremely difficult or even impossible. Instead, addressing inequities and communication gaps may be more effective in increasing the uptake of preventive services. Educating society about the benefits of cancer screening and more active health educators in Iranian health centers as the first line of health care would be beneficial. This approach could make a significant contribution to promoting better health outcomes.
In our study, we found women with a family history of cervical cancer had the highest rate of screening. This finding suggests that these women felt concerned about their health and were motivated to get screened to learn about their condition. Therefore, educating all women in the community about the significance of screening is crucial. Numerous studies conducted in Iran have indicated that having a family history of cancer plays a significant role in determining whether individuals undergo cancer screening [24-26]. This group appears to be more sensitive or perceive a greater risk than others. Using fear appeal strategies [26] to promote PS test uptake may be beneficial.
This study had several limitations. First, data collection was based on the questionnaire, which is usually prone to recall bias. When analyzing the results, it is essential to consider the bias. Second, due to the nature of the dependent variable, it was better to ask about the age of marriage, the number of pregnancies, and the method of contraception. Third, some important variables, such as the frequency of PS test uptake, were not examined; only the history of PS test uptake and its regular use were assessed. Finally, the current study was conducted among women in Kermanshah in the west of Iran; therefore, the generalizability of our findings is limited. However, the present study demonstrates the factors influencing the PS uptake for cervical cancer screening and may help plan for further in-depth research before developing health promotion programs.
Ethical Considerations
Compliance with ethical guidelines
The Research Ethics Committee of Kermanshah University of Medical Sciences, approved the study protocol (Code: IR.KUMS.REC.1398.301). Details of the study were provided to participants, including how the study was being performed, the confidentiality of information, and the purpose of the study before participation.
Funding
This study was funded by Kermanshah University of Medical Sciences (Code: 980441).
Authors' contributions
Study design, conceptualization and data interpretation: Mehdi Mirzaei-Alavijeh and Farzad Jalilian; Data analysis: Mahin Amini; Initial draft preparation: Shima Khashij; Review and editing: Seyyed Nasrollah Hosseini; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the women who participated in this study. In addition, the authors would like to thank the Research Deputy at Kermanshah University of Medical Sciences.
References
Cervical cancer is the fourth most frequent cancer in women and the third most common cancer in 146 countries, affecting women younger than 45 years old. Furthermore, more than half a million women are diagnosed with cervical cancer annually; cervical cancer resulted in the deaths of 311000 women worldwide in 2018, of which approximately 90% occurred in low- and middle-income countries [1]. Since the introduction of screening programs in high-income countries, the mortality rates of cervical cancer have dropped by more than half over the past 30 years, but it has not changed or increased in low-income countries [2, 3].
There are two very effective prevention strategies for cervical cancer: Human papillomavirus (HPV) vaccination and cervical screening with initial HPV testing followed by the treatment of precancerous lesions. Although the vaccination can prevent 70%-90% of cervical cancer, it cannot prevent cancer if the vaccine is injected in the precancerous phase [4]. Cervical screening is accessible and affordable, and more importantly, it is an effective method for early detection of cervical cancer, especially in developing countries [5]. Results have shown that regular pap smear (PS) test can help early treatment and thus reduce the incidence of cervical cancer in women aged 30-70 years old, especially in the range of 45-55 years old. Therefore, the widespread use of cervical cytology screening in developed countries has significantly reduced cervical cancer and its mortality [6, 7]. Inadequate resources for screening, insufficient education of women about the importance of screening, low socioeconomic status (SES), and low level of education are the most critical factors influencing PS test uptake in women [8, 9, 10, 11].
Due to the importance of cervical cancer health issues and the existence of preventive strategies, screening should be done regularly to reduce the burden of the disease [12]. Performing PS test for early detection of cervical cancer is a practical, inexpensive, necessary, and available method that can significantly reduce the burden of cervical cancer [13]. Therefore, this study aimed to investigate the inequality in cervical cancer screening uptake in women in 2019.
Materials and Methods
This cross-sectional research was conducted from July to September 2019 among 774 women aged 30-75 years living in Kermanshah City, Iran. Samples were selected through multi-stage cluster sampling. First, Kermanshah was divided into 8 areas according to the municipal areas. Then, each area was divided into 10 blocks, and 2 blocks were randomly selected, and eligible households were included in the study from these blocks. Data collection was completed using a written questionnaire and holding interviews. For this study, it was determined that a sample size of 751 individuals was needed. This calculation was based on considering a 4% margin of error, a 50% prevalence rate, and a 25% allowance for dropped samples. Ultimately, data was gathered from 774 participants.
The questionnaire consisted of three parts. In the first part, demographic information was collected. The second section assessed socioeconomic status of the participants. In the third part, participants PS uptakes were assessed.
In section one, age, level of education, marital status, family size, and positive family history of cervical cancer were collected as demographic variables.
In section two, as the main variable of household economic status was calculated using principal component analysis (PCA) and considering participants’ economic and social variables. Socioeconomic status information related to durable goods and social determinants included ownership of cars, refrigerators, televisions, freezers, washing machines, vacuum cleaners, cell phones, bicycles, laptops smear, etc. and the number of rooms in an apartment. Moreover, annual domestic and international travel was questioned. This questionnaire has been used in studies measuring inequality in Iran [14-17].
In section three, to assess whether participants had PS test uptake in the past, they answered the questions “Have you ever had PS test uptake for cervical cancer screening?” and “Have you regularly undergone PS test for cervical cancer screening?”
Four trained public health experts conducted interviews and gathered data for this study. The data were collected by visiting the participants in their homes.
The concentration index (Cn) is defined using a concentration curve. Cn is twice the area between the concentration curve and the isopleth line (45° line). If there is no socioeconomic inequality, Cn will be zero. In this convention, the index takes a negative value if the curve lies above the equivalence line, indicating a disproportionate concentration of the health variable among the poor. It takes a positive value if it lies below the equivalence line [18]. Cn is determined using the Equation 1.
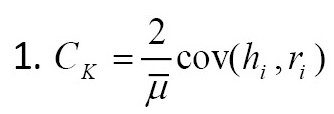
, where is the mean health variable in the entire population and ri each Pearson’s rank in the socioeconomic quintile. ri=1/N for the poorest person and ri=N/N for the richest. hi is the health variable for the person i. According to Equation 1, for binary dependent variables, the Cn may not fall in the -1 to +1 range, in which case the normalized Cn in Equation 2 should be used [19].

In descriptive analysis, numbers and percentages have been used for all nominal and sequential qualitative variables. Logistic regression was used to identify predictors of regular PS test uptake, and model 1 (crude analysis) was used for this analysis. Variables with P>0.25 were excluded from the adjusted model, whereas variables with P<0.25 were included in model 2 (adjusted analysis). It is worth mentioning that widowed women may have different property arrangements than married women. Married women are considered the reference group for the analysis. In this study, a significance level of 5% has been considered for the 95% confidence interval (CI) to confirm the statistical significance of the relationship PS. Data were analyzed using STATA software, version 14 including the chi-square test, t-test, logistic regression, and compensation statistical tests.
Results
The mean age of participants was 45.42±10.66 years. A total of 450 women (58.1%) had a history of PS test uptake. In addition, 205 women (26.5%) have a regular PS test uptake. Details of the participants’ demographic characteristics are shown in Table 1.
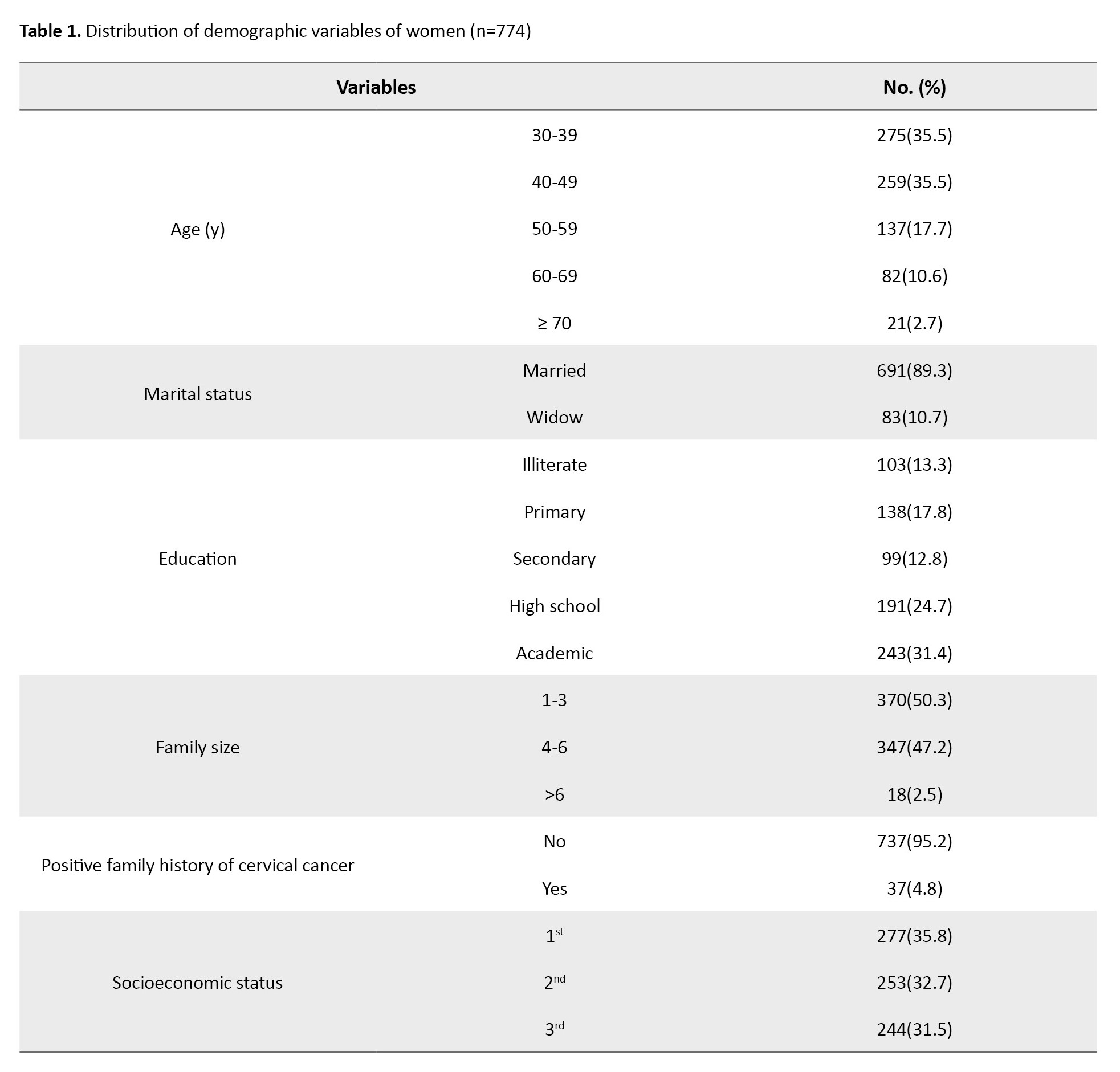
The mean age of women with regular PS test uptake was 44.19±8.89 years. Initially, a logistic regression was conducted to analyze the data, and variables that were not statistically significant (family size and socioeconomic states) were removed from the model. The participants’ education level (OR=1.181, 95% CI; 1.022, 1.364, P=0.024) and a positive family history of cervical cancer (OR=3.591, 95% CI; 1.811, 7.120, P=0.001) had significant impacts on their regular PS test uptake (Table 2).
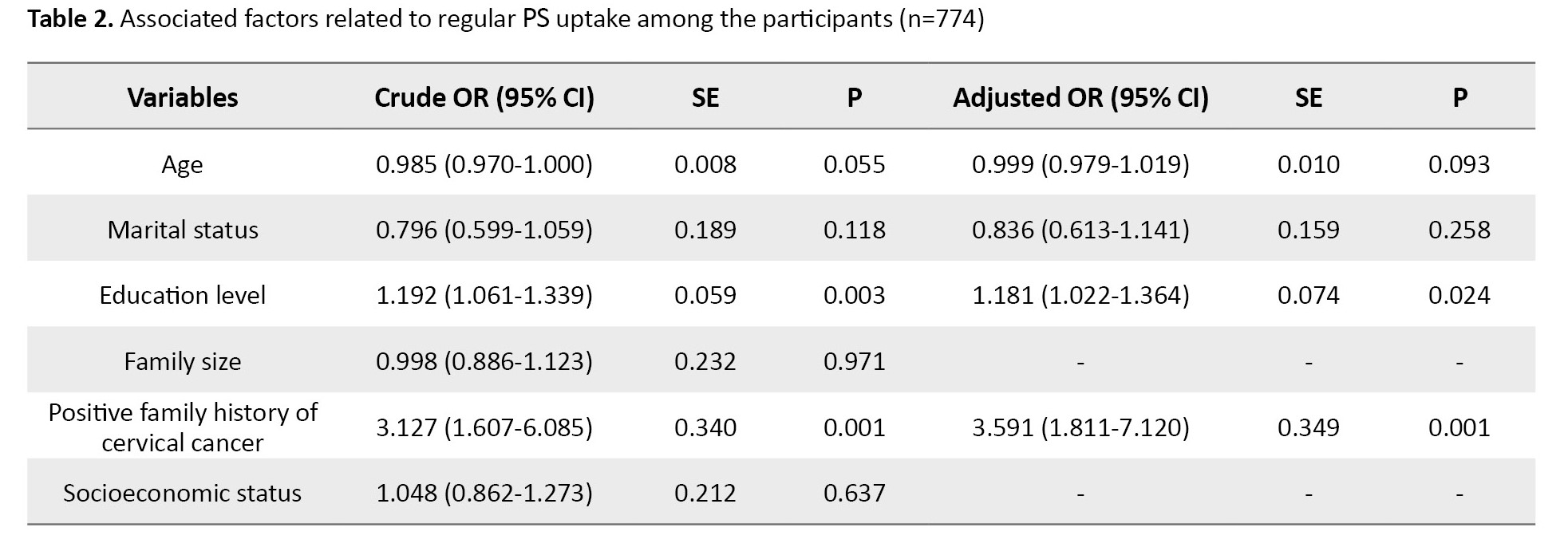
Table 3 indicates that women in the rich category had a notably lower average age.
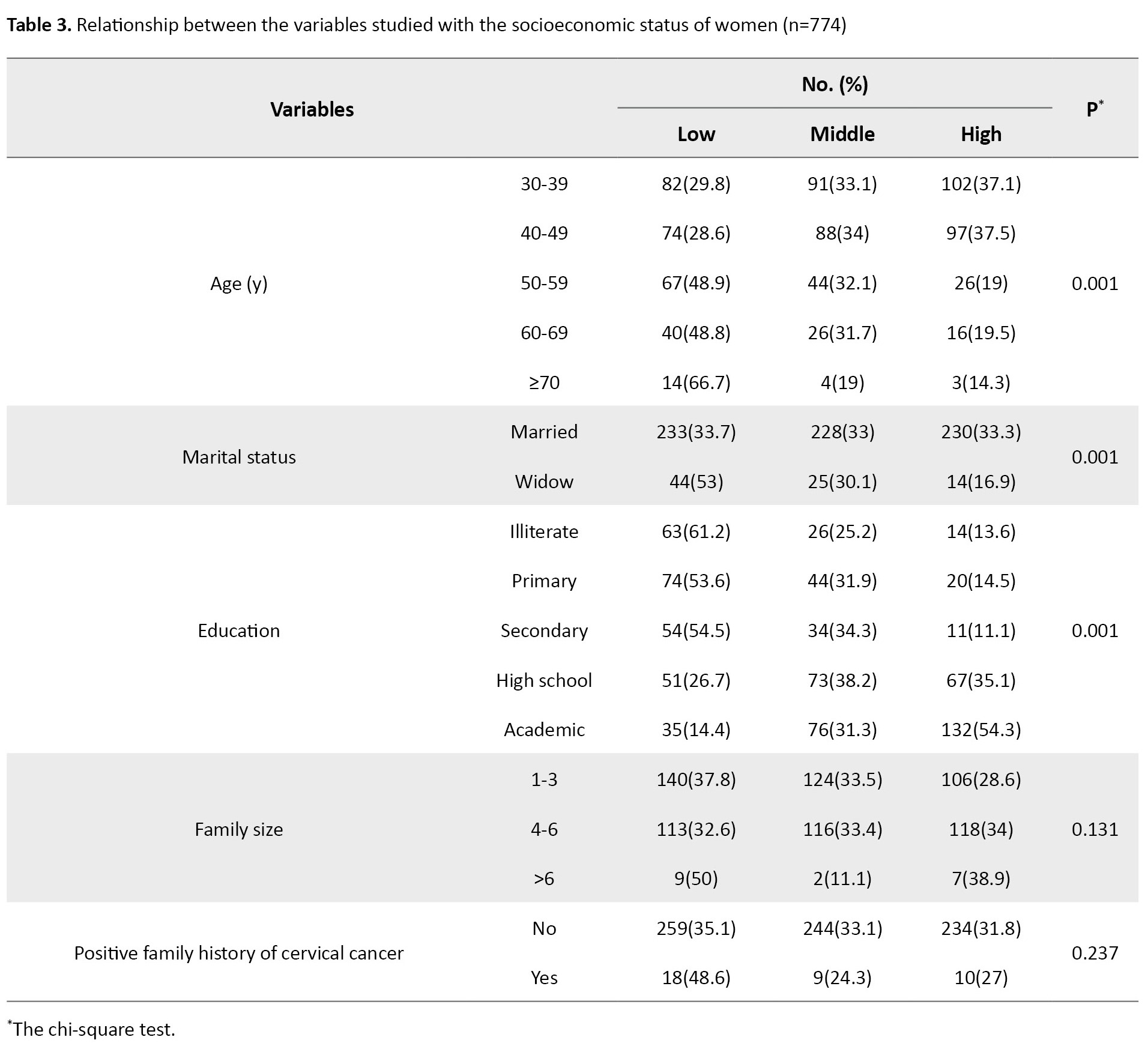
Specifically, the mean age for poor, middle, and rich women was 48.23, 44.80, and 42.86, respectively, with a statistically significant difference. Moreover, when considering socioeconomic status, a higher proportion of married women were observed to belong to the rich group. Additionally, 54.3% of educated women were found in the rich category. It was determined that education level had a significant association with SES. Family size and positive family history of cervical cancer did not show a significant relationship with SES.
The concentration index for PS test uptake in the women was 0.062, which indicates the concentration of PS in the high socioeconomic status of the participants. Still, due to the low value of the index and the lack of statistical significance, it can be concluded that PS test uptake independently with SES has no significant relationship (Figure 1).
Discussion
This study aimed to determine the inequality of cervical cancer screening uptake. Although the numerical value of the concentration index in this study was positive, it was not significant. Given the cheapness and availability of this screening test in Iran, this result is not far-fetched.
It is important to note that a large number of women aged 60 and above were either illiterate or had only completed primary education. However, the research revealed that education was crucial in determining whether women underwent regular PS tests. Additionally, there was a significant connection between education and SES, with educated women generally having better SES. A study examining the barriers to PS uptake in low- and middle-income countries discovered that in Latin American countries, women with low SES had significantly lower rates of PS test uptake. However, age lacked a significant impact on uptake [20]. Moreover, our finding was in line with a study conducted in Brazil by Açucena Vieira Alves et al., which found that a higher level of education positively correlated to cervical cancer screening [21]. Furthermore, Ahmed et al., in a study among female university students in a multiethnic institution, indicated that the increase in PS test uptake was associated with increased knowledge about cervical cancer PS risk factors [22]. These results may highlight the role of information and communication inequality in addressing health disparities, which are important determinants. Compared to illiterate women, educated individuals prioritize their health more [23]. Our findings highlight the education to encourage women, especially older and less educated women, to undergo regular cervical cancer screening. Measures to improve education, especially among older women, are extremely difficult or even impossible. Instead, addressing inequities and communication gaps may be more effective in increasing the uptake of preventive services. Educating society about the benefits of cancer screening and more active health educators in Iranian health centers as the first line of health care would be beneficial. This approach could make a significant contribution to promoting better health outcomes.
In our study, we found women with a family history of cervical cancer had the highest rate of screening. This finding suggests that these women felt concerned about their health and were motivated to get screened to learn about their condition. Therefore, educating all women in the community about the significance of screening is crucial. Numerous studies conducted in Iran have indicated that having a family history of cancer plays a significant role in determining whether individuals undergo cancer screening [24-26]. This group appears to be more sensitive or perceive a greater risk than others. Using fear appeal strategies [26] to promote PS test uptake may be beneficial.
This study had several limitations. First, data collection was based on the questionnaire, which is usually prone to recall bias. When analyzing the results, it is essential to consider the bias. Second, due to the nature of the dependent variable, it was better to ask about the age of marriage, the number of pregnancies, and the method of contraception. Third, some important variables, such as the frequency of PS test uptake, were not examined; only the history of PS test uptake and its regular use were assessed. Finally, the current study was conducted among women in Kermanshah in the west of Iran; therefore, the generalizability of our findings is limited. However, the present study demonstrates the factors influencing the PS uptake for cervical cancer screening and may help plan for further in-depth research before developing health promotion programs.
Ethical Considerations
Compliance with ethical guidelines
The Research Ethics Committee of Kermanshah University of Medical Sciences, approved the study protocol (Code: IR.KUMS.REC.1398.301). Details of the study were provided to participants, including how the study was being performed, the confidentiality of information, and the purpose of the study before participation.
Funding
This study was funded by Kermanshah University of Medical Sciences (Code: 980441).
Authors' contributions
Study design, conceptualization and data interpretation: Mehdi Mirzaei-Alavijeh and Farzad Jalilian; Data analysis: Mahin Amini; Initial draft preparation: Shima Khashij; Review and editing: Seyyed Nasrollah Hosseini; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the women who participated in this study. In addition, the authors would like to thank the Research Deputy at Kermanshah University of Medical Sciences.
References
- Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob Health. 2020; 8(2):e191-203. [DOI:10.1016/S2214-109X(19)30482-6] [PMID]
- Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. Lancet. 2019; 393(10167):169-82. [DOI:10.1016/S0140-6736(18)32470-X] [PMID]
- Vale DB, Teixeira JC, Bragança JF, Derchain S, Sarian LO, Zeferino LC. Elimination of cervical cancer in low-and middle-income countries: Inequality of access and fragile healthcare systems. Int J Gynaecol Obstet. 2021; 152(1):7-11. [DOI:10.1002/ijgo.13458] [PMID]
- Simms KT, Steinberg J, Caruana M, Smith MA, Lew JB, Soerjomataram I, et al. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020-99: A modelling study. Lancet Oncol. 2019; 20(3):394-407. [DOI:10.1016/S1470-2045(18)30836-2] [PMID]
- Siseho KN, Omoruyi BE, Okeleye BI, Okudoh VI, Amukugo HJ, Aboua YG. Women’s perception of cervical cancer pap smear screening. Nurs Open. 2022; 9(3):1715-22. [DOI:10.1002/nop2.1196] [PMID] [PMCID]
- Sinha R, Kumar P, Singh G, Saha R. Opportunistic cervical cancer screening by Papanicolaou stain Pap smear among women: A pilot study at urban health training centre of All India Institute of Medical Sciences, Patna, Bihar, India. Int J Reprod Contracept Obstet Gynecol. 2020; 9(7):2714-21. [Link]
- Basu P, Mittal S, Bhadra Vale D, Chami Kharaji Y. Secondary prevention of cervical cancer. Best Pract Res Clin Obstet Gynaecol. 2018; 47:73-85. [DOI:10.1016/j.bpobgyn.2017.08.012] [PMID]
- Pimple SA, Mishra GA. Global strategies for cervical cancer prevention and screening. Minerva Ginecol. 2019; 71(4):313-20. [DOI:10.23736/S0026-4784.19.04397-1]
- Campos NG, Tsu V, Jeronimo J, Regan C, Resch S, Clark A, et al. Health impact of delayed implementation of cervical cancer screening programs in India: A modeling analysis. Int J Cancer. 2019; 144(4):687-96. [DOI:10.1002/ijc.31823] [PMID] [PMCID]
- Suurna M, Orumaa M, Ringmets I, Pärna K. Inequalities in reported use of cervical screening in Estonia: Results from cross-sectional studies in 2004-2020. BMC Womens Health. 2022; 22(1):545. [DOI:10.1186/s12905-022-02123-z] [PMID] [PMCID]
- Brooks SE, Davis EC, Farley JH. Disparities in pap smear screening follow up: A catalyst for collective action vs. collective despair. Gynecol Oncol. 2021; 160(2):361-3. [DOI:10.1016/j.ygyno.2021.01.004] [PMID]
- Dsouza JP, Broucke SVD, Pattanshetty S, Dhoore W. A comparison of behavioural models explaining cervical cancer screening uptake. BMC Women’s Health. 2022; 22(1):235. [DOI:10.1186/s12905-022-01801-2] [PMID] [PMCID]
- da Silva DCB, Garnelo L, Herkrath FJ. Barriers to access the Pap smear test for cervical cancer screening in rural riverside populations covered by a fluvial primary healthcare team in the Amazon. Int J Environ Res Public Health. 2022; 19(7):4193. [DOI:10.3390/ijerph19074193] [PMID] [PMCID]
- Moradinazar M, Najafi F, Jalilian F, Pasdar Y, Hamzeh B, Shakiba E, et al. Prevalence of drug use, alcohol consumption, cigarette smoking and measure of socioeconomic-related inequalities of drug use among Iranian people: Findings from a national survey. Subst Abuse Treat Prev Policy. 2020; 15(1):39. [DOI:10.1186/s13011-020-00279-1] [PMID] [PMCID]
- Mirzaei-Alavijeh M, Jerome-D Emilia B, Najafi F, Moradinazar M, Pirouzeh R, et al. Inequality in mammography uptake: Results from recruitment phase of first cohort study among Iranian Kurdish population. Glob Health Res Policy. 2022; 7(1):43.[DOI:10.1186/s41256-022-00277-9] [PMID] [PMCID]
- Jalilian F, Jerome-D'Emilia B, Najafi F, Pasdar Y, Karami Matin B, Amini M, et al. Socioeconomic Status and clinical breast examination screening uptake: Findings from the First Cohort Study among iranian kurdish women. Asian Pac J Cancer Prev. 2022; 23(5):1555-64. [DOI:10.31557/APJCP.2022.23.5.1555] [PMID] [PMCID]
- Mirzaei-Alavijeh M, Amini M, Keshavarzi A, Jalilian F. Inequality in breast cancer screening tests uptake among women in Western Iran. Iran J Breast Dis. 2022; 15(4):89-104. [DOI:10.30699/ijbd.15.4.89]
- O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: A guide to techniques and their implementation. Washington: World Bank; 2008. [DOI:10.1596/978-0-8213-6933-3]
- Wagstaff A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005; 14(4):429-32. [DOI:10.1002/hec.953] [PMID]
- Liebermann EJ, VanDevanter N, Hammer MJ, Fu MR. Social and cultural barriers to women’s participation in Pap smear screening programs in low-and middle-income Latin American and Caribbean countries: An integrative review. J Transcult Nurs. 2018; 29(6):591-602. [DOI:10.1177/1043659618755424] [PMID]
- Açucena Vieira Alves S, Schiaveto de Souza A, Weller M, Pires Batiston A. Differential impact of education level, occupation and marital status on performance of the Papanicolaou test among women from various regions in Brazil. Asian Pac J Cancer Prev. 2019; 20(4):1037-44. [DOI:10.31557/APJCP.2019.20.4.1037] [PMID] [PMCID]
- Ahmed NU, Rojas P, Degarege A. Knowledge of cervical cancer and adherence to Pap smear screening test among female university students in a multiethnic institution, USA. J Natl Med Assoc. 2020; 112(3):300-7. [DOI:10.1016/j.jnma.2020.03.007] [PMID]
- Krishnakumar S, Govindarajulu Y, Vishwanath U, Nagasubramanian VR, Palani T. Impact of patient education on KAP, medication adherence and therapeutic outcomes of metformin versus insulin therapy in patients with gestational diabetes: A Hospital based pilot study in South India. Diabetes Metab Syndr. 2020; 14(5):1379-83. [DOI:10.1016/j.dsx.2020.07.026] [PMID]
- Mirzaei-Alavijeh M, Ghorbani P, Jalilian F. Socio-cognitive determinants of the mammography screening uptake among Iranian women. Asian Pac J Cancer Prev. 2018; 19(5):1351-5. [PMID]
- Mirzaei-Alavijeh M, Schaafsma D, Karami-Matin B, Jalilian F. Socio-cognitive determinants of colorectal cancer screening uptake: An application of intervention mapping approach. Med J Islam Repub Iran. 2019; 33:80. [DOI:10.47176/mjiri.33.80] [PMID] [PMCID]
- Tannenbaum MB, Hepler J, Zimmerman RS, Saul L, Jacobs S, Wilson K, et al. Appealing to fear: A meta-analysis of fear appeal effectiveness and theories. Psychol Bull. 2015; 141(6):1178-204. [DOI:10.1037/a0039729] [PMID] [PMCID]
Article Type : Research |
Subject:
General
Received: 2023/02/19 | Accepted: 2023/12/30 | Published: 2024/07/1
Received: 2023/02/19 | Accepted: 2023/12/30 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |