Fri, Jul 12, 2024
Volume 34, Issue 3 (6-2024)
JHNM 2024, 34(3): 229-236 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseininezhad M, Saadat S, Pourramzani A, Zhaleparvar M, Jafroudi M, Sheikholeslami F. Mediating Role of Self-efficacy in the Relationship of Social Support and Resilience in Nurses During the COVID-19 Pandemic: A Cross-sectional Study. JHNM 2024; 34 (3) :229-236
URL: http://hnmj.gums.ac.ir/article-1-2371-en.html
URL: http://hnmj.gums.ac.ir/article-1-2371-en.html
Mozaffar Hosseininezhad1 

 , Sajjad Saadat *
, Sajjad Saadat * 

 2, Ali Pourramzani3
2, Ali Pourramzani3 

 , Maryam Zhaleparvar4
, Maryam Zhaleparvar4 

 , Maryam Jafroudi5
, Maryam Jafroudi5 

 , Farzaneh Sheikholeslami6
, Farzaneh Sheikholeslami6 




 , Sajjad Saadat *
, Sajjad Saadat * 

 2, Ali Pourramzani3
2, Ali Pourramzani3 

 , Maryam Zhaleparvar4
, Maryam Zhaleparvar4 

 , Maryam Jafroudi5
, Maryam Jafroudi5 

 , Farzaneh Sheikholeslami6
, Farzaneh Sheikholeslami6 


1- Associate Professor, Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- PhD in Psychology, Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,sajjadsaadat69@gmail.com
3- Assistant Professor, Department of Psychiatry, Kavosh Behavioural, Cognitive and Addiction Sciences Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- M.D, Clinical Research Development Unit of Poursina Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
5- M.A. in General Psychology, School of Literature and Humanities, University of Guilan, Rasht, Iran.
6- Instructor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- PhD in Psychology, Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Assistant Professor, Department of Psychiatry, Kavosh Behavioural, Cognitive and Addiction Sciences Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- M.D, Clinical Research Development Unit of Poursina Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
5- M.A. in General Psychology, School of Literature and Humanities, University of Guilan, Rasht, Iran.
6- Instructor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 771 kb]
(36 Downloads)
| Abstract (HTML) (167 Views)
Full-Text: (18 Views)
Introduction
COVID-19 was first identified in China in December 2019 and spread to numerous countries worldwide [1, 2]. The disease has increased the workload and the hazard of infection for all health caregivers, including nurses [3]. It created a significant rise in nurses’ anxiety and stress levels [4], led to intense workload [5], anxiety man-agement, patient fear, and a stressful work environment [6]. These conditions threaten the nurses’ health, well-being, and quality of services [7, 8].
Psychological resilience is a dynamic process [9] that is dominant in increasing personal strength in stressful conditions, developing productive coping strategies, and accommodating changing circumstances [10]. In this regard, a study conducted in the first weeks after the diagnosis of the epidemic in China showed that nurses had encountered various psychological problems such as anxiety, stress, and major depression [11]. Due to the con-stant exposure of nurses to human suffering and unfavorable work environments, resilience is essential for nurses to maintain mental health [12, 13], perceive denotation in their incidents, and lessen their responses to stressors in the workplace [14]. In this regard, some researchers have shown that nurses with a higher level of resilience, as a vital element in a changing healthcare system [15], can respond better to stressful situations. Resilience is essential as an effective coping mechanism [16], which is affected by several personal, managerial, and social components [17].
Psychological, caring, and supportive resources are provided as social support by social networks, including significant others, family, and friends. They are influential in increasing nurses’ resilience [18-20]. The foremost task of social support is to act as a moderator by decreasing or balancing the psychological damage brought by life-menacing occasions and the ongoing challenges of life [21]. In addition, it is important to meet people’s basic social needs, have equal love, compassion, and group belonging, and find financial, psychological, and emotional peace in stressful circumstances [22]. Social support can play an influential role in self-efficacy [23]. Self-efficacy is considered an essential characteristic of a successful professional nurse [24, 25] and helps be flex-ible in high-risk situations and have a stable mental state [26]. Self-efficacy can improve people’s resilience, rely more on their knowledge and expertise, and increase their desire to work and willingness to care for patients with infectious diseases [27-29].
During the COVID-19 pandemic, nurses were at the front line of the fight and were under much pressure [30]. As a result, nurses must be armed with the required physical and psychological arsenal to main-tain continuity of care [11]. Paying attention to these issues can pave the way for effective interven-tions and improve the psychological status of nurses during and after the epidemic. Although many studies have been conducted on the medical aspects of COVID-19, only a handful have focused on nurses’ social support and self-efficacy during the epidemic and its psychological outcomes. Conse-quently, the present research was conducted to determine the relationship between perceived social support and self-efficacy in predicting nurses’ psychological resilience during COVID-19.
Materials and Methods
This cross-sectional study was conducted on nurses in educational and medical centers of Rasht City, Iran, dur-ing October and November 2021. To determine the sample size, we considered the type I error of 0.05 and the study power of 0.8. According to a pilot implementation of the Connor-Davidson resilience scale in 30 nurses and the researcher’s expectation, the effect size was considered 0.04 (less than the mean score), and the number of independent and mediator variables was 4. So, a sample size of 210 was determined. Accounting for a 10% drop, 231 nurses were entered into the study. They were selected by simple random sampling based on the list of nurses at the main hospitalization centers for patients with COVID-19. Informed consent to partic-ipate in the study, work experience of at least one year, and receiving the COVID-19 vaccine were the inclusion criteria. However, failure to complete at least 10% of the questions in each questionnaire was considered the exclusion criterion.
The multidimensional scale of perceived social support was used to measure the perceived social support. Zimet et al. designed this 12-item scale to measure perceived social support. This scale has three subscales of support for the family, friends, and significant others. It evaluates the level of perceived social support on the 7-point Likert scale from strongly disagree (point 1) to strongly agree (point 7). The minimum and maximum scores are 12 and 84 [31]. The Persian version of this tool was used in this study [32].
The general self-efficacy scale (GSE) was used to measure the self-efficacy. This scale has 10 questions scored on a 4-point scale from strongly disagreeing with (point 1) to strongly agreeing with (point 4). The minimum score of the subject in this test is 10, and the maximum is 40, and the higher the score of the person, the higher the level of perceived self-efficacy beliefs in the person [33]. The Persian version of the GSE was used in this study [34 ].
The Connor-Davidson resilience scale (CD-RISC) was used to measure resilience. Connor and Davidson devel-oped this scale, which applies to people 15 years and older. It has 25 items scored from 0 (completely incorrect) to 4 (always correct). The minimum and maximum scores of the subject on this scale are 0 and 100, respectively [35] and The Persian version of the CD-RISC was used in this study [36].
Demographic and occupational data were collected with a researcher-made questionnaire of age, sex, work-ing unit, marital status, employment history, work experience, career position, and education level.
Moreover, owing to the COVID-19 pandemic, sampling was done using an online survey form. The research tools were uploaded to the Porsline system, and the link was provided to the nurses through the hospital supervisor. IBM SPSS software, version 24, and Amos software, version 24 were used for data analysis. Also, the mean and standard deviation were calcu-lated for quantitative variables. Qualitative variables were reported based on frequency and percentage. Skew-ness and kurtosis were calculated to assess the normal distribution of the main variables (social support, self-efficacy, and resilience). The Pearson correlation coefficient test was used to investigate the linear relationship between the study variables. To evaluate the fit of the proposed model, the chi-square test (X2), degrees of freedom (df), goodness of fit index (GFI), Tucker-Lewis Index (TLI), comparative fit index (CFI), and root mean square error of approximation (RMSEA) were reported. Bootstrap test was used to investigate the role of self-efficacy in the middle of social support and resilience and to assess the direct effects of variables. The findings were reported following the STROBE (strengthening the reporting of observational studies in epidemiology) guidelines [37].
Results
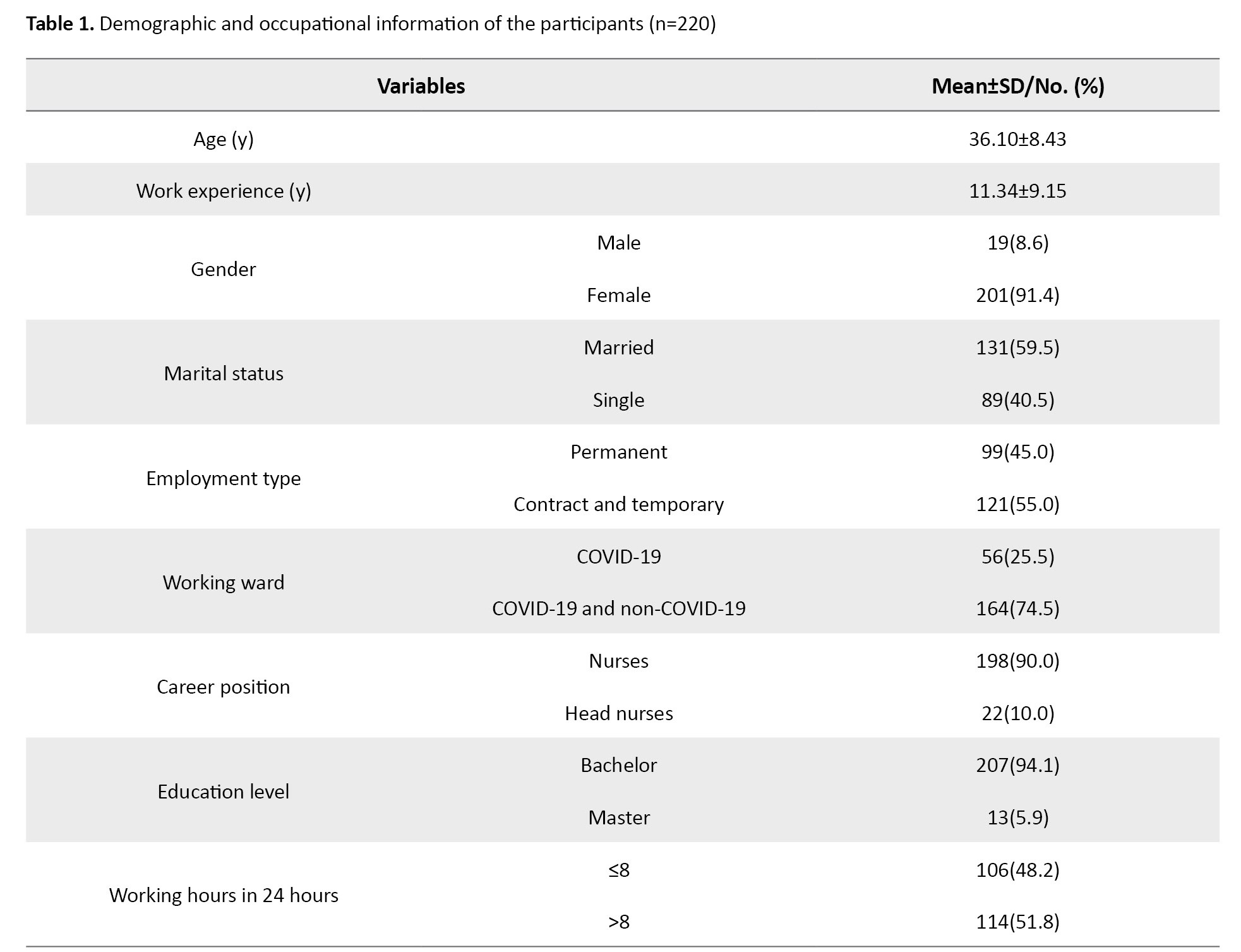
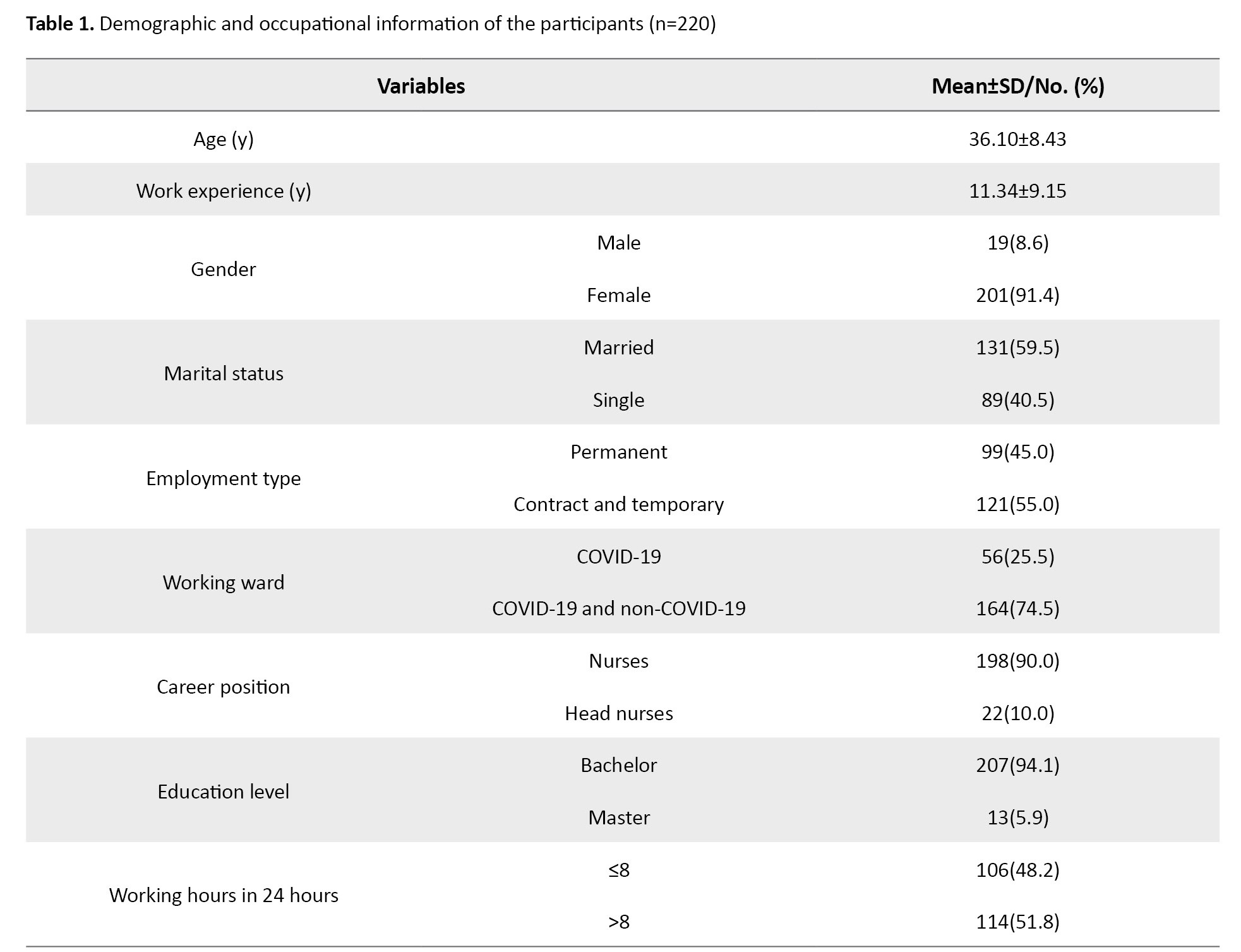
A total of 220 nurses answered the questionnaires completely (participation rate: 95.23%). Their demographic and occupational information is presented in Table 1.
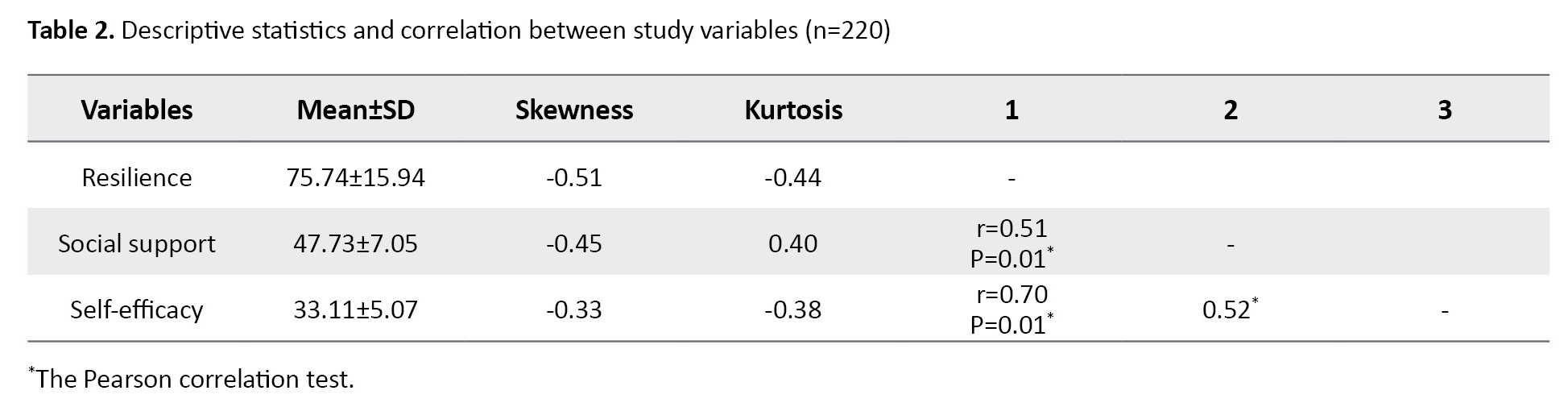
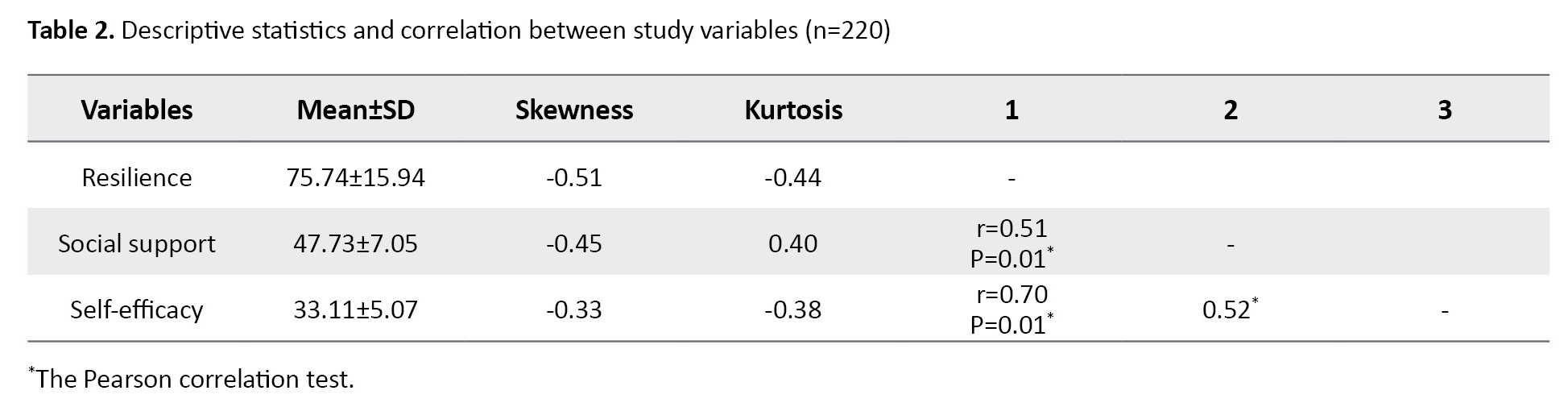
The results showed that resilience, social support, and self-efficacy are in the normal distribution. Moreover, the mean values of resilience, social support, and self-efficacy were 75.74±15.94, 47.33±7.05, and 33.11±5.07, respectively.
The Pearson correlation coefficient test results showed that social support (r=0.51, P=0.01) and self-efficacy (r=0.70, P=0.01) were positively and significantly related to resilience. A positive and significant relationship existed between self-efficacy and social support (r=0.52, P=0.05).
Table 2 presents that the variance inflation factor (VIF) for the social support and self-efficacy variables was 1.386, and the tolerance was 0.721, so there is no multiple collinearity relationship between the variables.
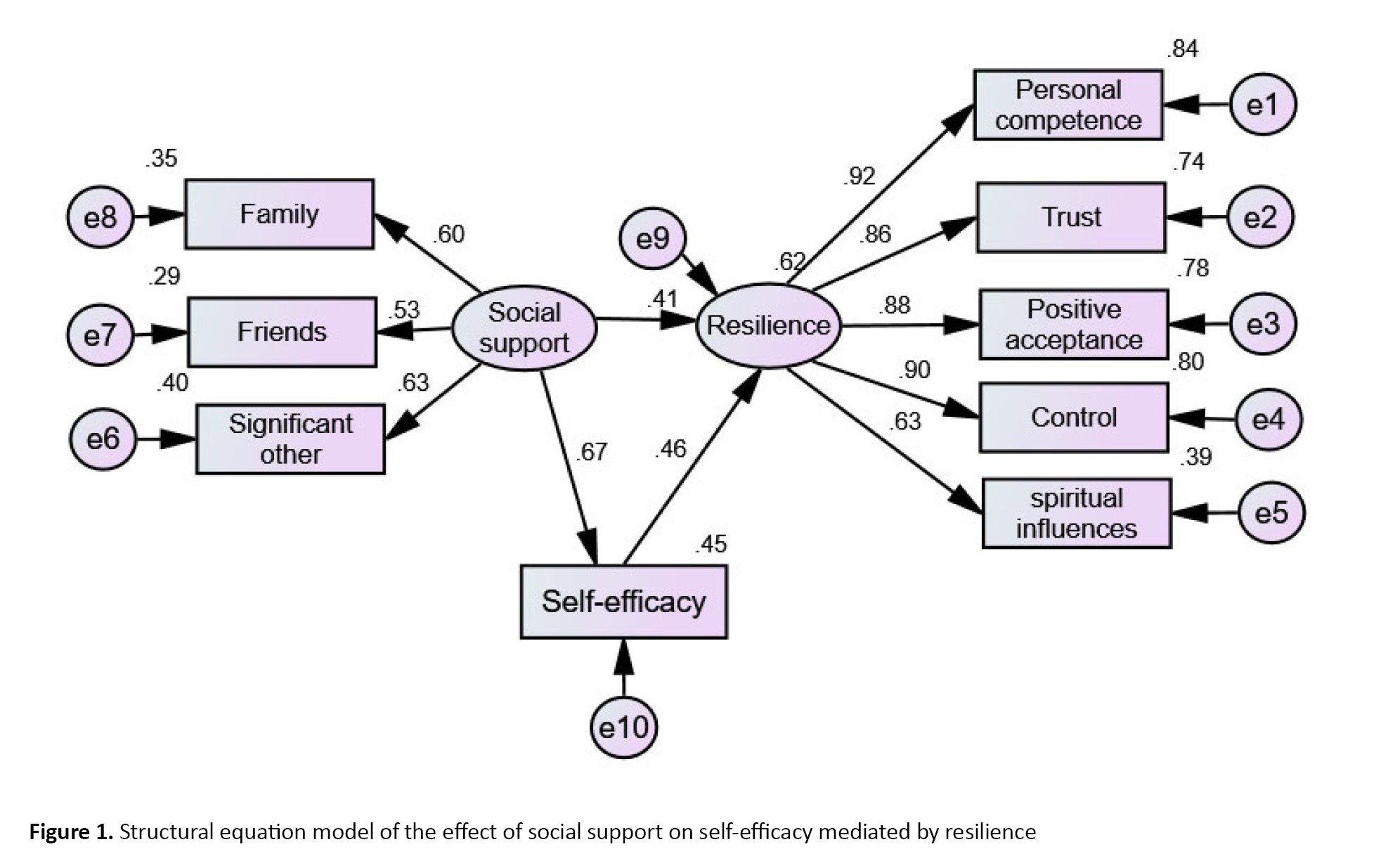
Durbin–Watson statistic was also calculated to be 1.98, which is between 1.50 and 2.50, indicating a lack of autocorrelations. Figure 1 shows the structural equation model of the effect of social support on self-efficacy by mediated resilience and reveals the social support effect on nurses’ resilience both directly and through the mediation of self-efficacy and predicts a total of 62% of the variance of resilience. The results show that the fit indices consisted of ꭕ2/df=1.60, CFI=0.98, GFI=0.96; TLI=0.98; RMSEA=0.05 showing their good condition, and the proposed model fits (Table 3).

Bootstrap test was used to investigate the direct and indirect effects of variables in the proposed model (Table 4).
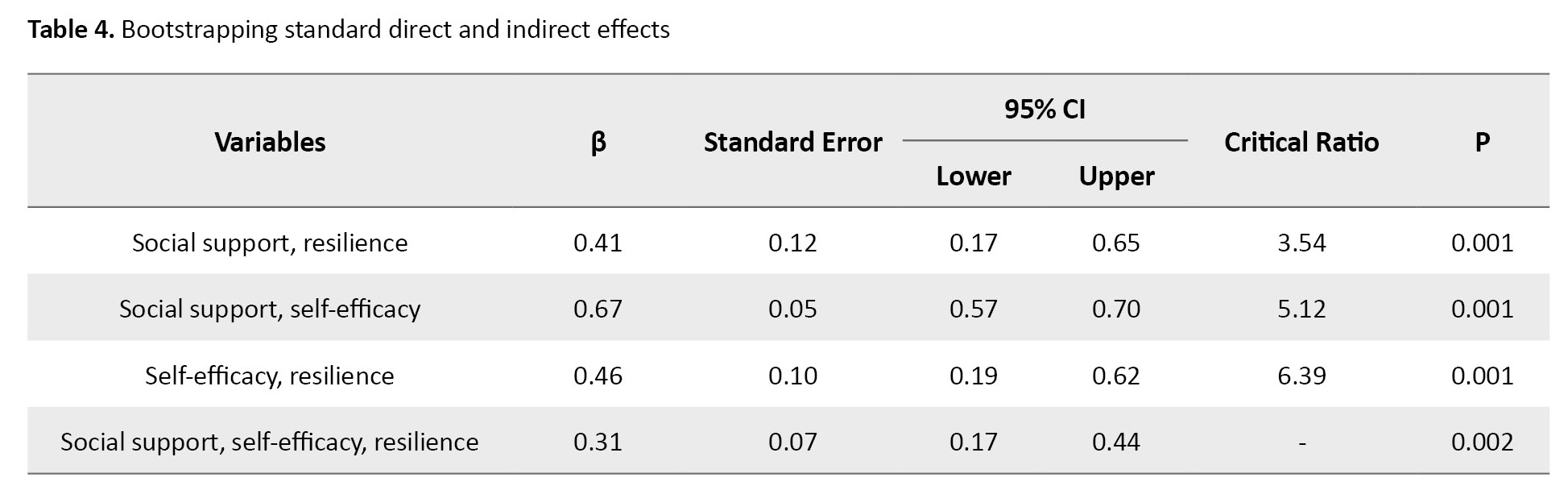
Bootstrap results showed that the direct impact of social support (β=0.41, P=0.001) and self-efficacy (β=0.46, P=0.001) on resilience was significant. The direct effect of social support on self-efficacy (β=0.67, P=0.001) was also significant. The results also showed that the accompanying consequence of social support on resilience with the conciliating role of self-efficacy was significant (β=0.31, P=0.001). It should be noted that no adjustment has been made through modification indexes. With the total effect size (β=0.72, P=0.001), the variance accounted for (VAF) was calculated as 43%, indicating the partial mediating role of self-efficacy in the relationship between perceived social support and resilience in nurses (Table 4).
Discussion
The results showed that self-efficacy significantly mediates the relationship between social support and productivity. These results are compatible with previous studies showing that high social support is related to higher levels of self-efficacy [23]. Another study showed that the negative effect of perceived stress on the quality of life can be mediated by social support and self-efficacy variables [38]. Although our findings are compatible with previous studies, this study further confirms the relative mediating effects of self-efficacy in the association between resilience and social support in Iranian nurses during the COVID-19 epidemic.
Research evidence shows that support in the workplace can empower personnel, increase self-efficacy, and develop professional performance [18, 39, 40]. It leads to greater apprehension, encouragement, courageousness, respect, and a sense of professional success [41], increased motivation, improved performance, and work attitude [42-44]. Social support from colleagues can inhibit stress and reduce psychological problems. Therefore, executing strategies that assist social support can notably enhance nurses’ self-efficacy [45]. In this study, it was shown that self-efficacy mediates the relationship between resilience and social support. Particularly, social support directly or through the mediating effects of self-efficacy affects resilience. The finding showed why self-efficacy is a connection between social support and resilience. Understanding high social support may expand self-efficacy and boost resilience. Bandura reported that support relationships improved individual self-efficacy [24]. Research has shown that support programs for nurses can play a crucial role in their self-efficacy [46] and enhance the quality of nursing care [47]. Therefore, social support is vital to boost the resilience of nurses, protect them, and promote behaviors that improve stress regulation [48].
In the explanation, it can be argued that people who receive greater social support benefit more from the verbal encouragement of those around them. They experience more efficiency in life crises and overcome problems because, in Bandura’s interpretation, one of the most effective ways to grow self-efficacy is to receive verbal encouragement from those around them [24]. In contrast, self-efficacy is essential in resilience [18, 49, 50] and human endeavors. In other words, highly self-efficient nurses will be more likely to survive after exposure to failure. When a low self-efficacy nurse experiences problems, it will experience stress and anxiety that can interfere with other functions and even reduce self-efficacy. However, individuals with high self-efficacy are assured of their capacity to overcome difficult situations [51]. They are optimistic about the future, and this positive expectation of their future will help them against obstacles. Most people committed to achieving goals are better at dealing with problems, and instead of magnifying them, they make them natural and sometimes even think of problems as challenge that can make them stronger [50].
Although our results have provided evidence of the mediation of self-efficacy in the relation between resilience and social support of Iranian nurses during the COVID-19 pandemic, this research is accompanied by limitations.
First, this study was done in two hospitals, and future research could use wider sampling at the national level to increase the generalization of the results. This study was carried out within the framework of a correlational project, so our suggestion to future researchers is to conduct experimental and longitudinal research to achieve causality. In this study, we used self-report questionnaires that can be answered with social bias and lack actual answers. It is also recommended that exploration interviews be used to understand better the variables of self-efficacy and social support, which requires qualitative and even hybrid research design. Due to the COVID-19 epidemic and observing social distance, we collected the desired data online. Our suggestion is to collect data face-to-face.
This study gave a detailed understanding of how self-efficacy and social support improve nurses’ resilience. This paper has identified paths to improve the resilience of nurses through social support and self-efficacy. Accordingly, it would be suggested that medical education managers and planners provide the necessary training and therapeutic programs for nurses’ psychological empowerment during COVID-19 and afterward.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.363). All participants signed the informed consent form.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design, data analysis, interpretation, review, editing and final approval: All authors. Sampling and writing the initial draft: Sajjad Saadat and Maryam Jafroudi; Recruiting the participants: Sajjad Saadat and Maryam Zhaleparvar.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the nurses who completed the questionnaires and the Clinical Research Development Unit of Poursina Hospital, Guilan University of Medical Sciences.
References
COVID-19 was first identified in China in December 2019 and spread to numerous countries worldwide [1, 2]. The disease has increased the workload and the hazard of infection for all health caregivers, including nurses [3]. It created a significant rise in nurses’ anxiety and stress levels [4], led to intense workload [5], anxiety man-agement, patient fear, and a stressful work environment [6]. These conditions threaten the nurses’ health, well-being, and quality of services [7, 8].
Psychological resilience is a dynamic process [9] that is dominant in increasing personal strength in stressful conditions, developing productive coping strategies, and accommodating changing circumstances [10]. In this regard, a study conducted in the first weeks after the diagnosis of the epidemic in China showed that nurses had encountered various psychological problems such as anxiety, stress, and major depression [11]. Due to the con-stant exposure of nurses to human suffering and unfavorable work environments, resilience is essential for nurses to maintain mental health [12, 13], perceive denotation in their incidents, and lessen their responses to stressors in the workplace [14]. In this regard, some researchers have shown that nurses with a higher level of resilience, as a vital element in a changing healthcare system [15], can respond better to stressful situations. Resilience is essential as an effective coping mechanism [16], which is affected by several personal, managerial, and social components [17].
Psychological, caring, and supportive resources are provided as social support by social networks, including significant others, family, and friends. They are influential in increasing nurses’ resilience [18-20]. The foremost task of social support is to act as a moderator by decreasing or balancing the psychological damage brought by life-menacing occasions and the ongoing challenges of life [21]. In addition, it is important to meet people’s basic social needs, have equal love, compassion, and group belonging, and find financial, psychological, and emotional peace in stressful circumstances [22]. Social support can play an influential role in self-efficacy [23]. Self-efficacy is considered an essential characteristic of a successful professional nurse [24, 25] and helps be flex-ible in high-risk situations and have a stable mental state [26]. Self-efficacy can improve people’s resilience, rely more on their knowledge and expertise, and increase their desire to work and willingness to care for patients with infectious diseases [27-29].
During the COVID-19 pandemic, nurses were at the front line of the fight and were under much pressure [30]. As a result, nurses must be armed with the required physical and psychological arsenal to main-tain continuity of care [11]. Paying attention to these issues can pave the way for effective interven-tions and improve the psychological status of nurses during and after the epidemic. Although many studies have been conducted on the medical aspects of COVID-19, only a handful have focused on nurses’ social support and self-efficacy during the epidemic and its psychological outcomes. Conse-quently, the present research was conducted to determine the relationship between perceived social support and self-efficacy in predicting nurses’ psychological resilience during COVID-19.
Materials and Methods
This cross-sectional study was conducted on nurses in educational and medical centers of Rasht City, Iran, dur-ing October and November 2021. To determine the sample size, we considered the type I error of 0.05 and the study power of 0.8. According to a pilot implementation of the Connor-Davidson resilience scale in 30 nurses and the researcher’s expectation, the effect size was considered 0.04 (less than the mean score), and the number of independent and mediator variables was 4. So, a sample size of 210 was determined. Accounting for a 10% drop, 231 nurses were entered into the study. They were selected by simple random sampling based on the list of nurses at the main hospitalization centers for patients with COVID-19. Informed consent to partic-ipate in the study, work experience of at least one year, and receiving the COVID-19 vaccine were the inclusion criteria. However, failure to complete at least 10% of the questions in each questionnaire was considered the exclusion criterion.
The multidimensional scale of perceived social support was used to measure the perceived social support. Zimet et al. designed this 12-item scale to measure perceived social support. This scale has three subscales of support for the family, friends, and significant others. It evaluates the level of perceived social support on the 7-point Likert scale from strongly disagree (point 1) to strongly agree (point 7). The minimum and maximum scores are 12 and 84 [31]. The Persian version of this tool was used in this study [32].
The general self-efficacy scale (GSE) was used to measure the self-efficacy. This scale has 10 questions scored on a 4-point scale from strongly disagreeing with (point 1) to strongly agreeing with (point 4). The minimum score of the subject in this test is 10, and the maximum is 40, and the higher the score of the person, the higher the level of perceived self-efficacy beliefs in the person [33]. The Persian version of the GSE was used in this study [34 ].
The Connor-Davidson resilience scale (CD-RISC) was used to measure resilience. Connor and Davidson devel-oped this scale, which applies to people 15 years and older. It has 25 items scored from 0 (completely incorrect) to 4 (always correct). The minimum and maximum scores of the subject on this scale are 0 and 100, respectively [35] and The Persian version of the CD-RISC was used in this study [36].
Demographic and occupational data were collected with a researcher-made questionnaire of age, sex, work-ing unit, marital status, employment history, work experience, career position, and education level.
Moreover, owing to the COVID-19 pandemic, sampling was done using an online survey form. The research tools were uploaded to the Porsline system, and the link was provided to the nurses through the hospital supervisor. IBM SPSS software, version 24, and Amos software, version 24 were used for data analysis. Also, the mean and standard deviation were calcu-lated for quantitative variables. Qualitative variables were reported based on frequency and percentage. Skew-ness and kurtosis were calculated to assess the normal distribution of the main variables (social support, self-efficacy, and resilience). The Pearson correlation coefficient test was used to investigate the linear relationship between the study variables. To evaluate the fit of the proposed model, the chi-square test (X2), degrees of freedom (df), goodness of fit index (GFI), Tucker-Lewis Index (TLI), comparative fit index (CFI), and root mean square error of approximation (RMSEA) were reported. Bootstrap test was used to investigate the role of self-efficacy in the middle of social support and resilience and to assess the direct effects of variables. The findings were reported following the STROBE (strengthening the reporting of observational studies in epidemiology) guidelines [37].
Results
A total of 220 nurses answered the questionnaires completely (participation rate: 95.23%). Their demographic and occupational information is presented in Table 1.
The results showed that resilience, social support, and self-efficacy are in the normal distribution. Moreover, the mean values of resilience, social support, and self-efficacy were 75.74±15.94, 47.33±7.05, and 33.11±5.07, respectively.
The Pearson correlation coefficient test results showed that social support (r=0.51, P=0.01) and self-efficacy (r=0.70, P=0.01) were positively and significantly related to resilience. A positive and significant relationship existed between self-efficacy and social support (r=0.52, P=0.05).
Table 2 presents that the variance inflation factor (VIF) for the social support and self-efficacy variables was 1.386, and the tolerance was 0.721, so there is no multiple collinearity relationship between the variables.
Durbin–Watson statistic was also calculated to be 1.98, which is between 1.50 and 2.50, indicating a lack of autocorrelations. Figure 1 shows the structural equation model of the effect of social support on self-efficacy by mediated resilience and reveals the social support effect on nurses’ resilience both directly and through the mediation of self-efficacy and predicts a total of 62% of the variance of resilience. The results show that the fit indices consisted of ꭕ2/df=1.60, CFI=0.98, GFI=0.96; TLI=0.98; RMSEA=0.05 showing their good condition, and the proposed model fits (Table 3).

Bootstrap test was used to investigate the direct and indirect effects of variables in the proposed model (Table 4).
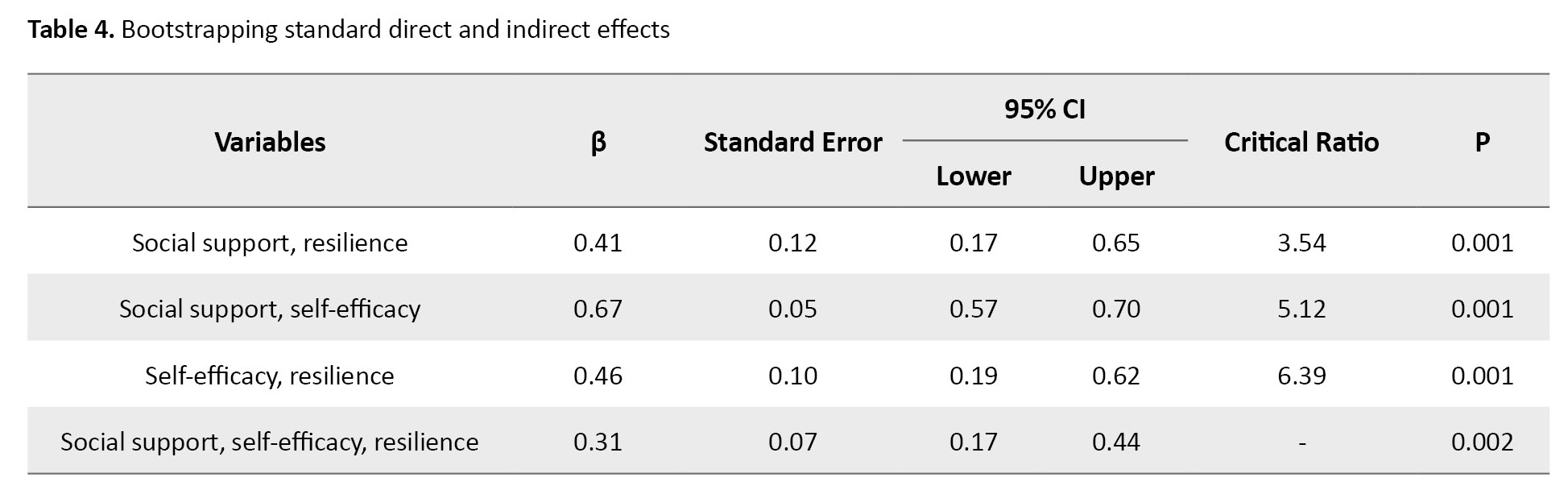
Bootstrap results showed that the direct impact of social support (β=0.41, P=0.001) and self-efficacy (β=0.46, P=0.001) on resilience was significant. The direct effect of social support on self-efficacy (β=0.67, P=0.001) was also significant. The results also showed that the accompanying consequence of social support on resilience with the conciliating role of self-efficacy was significant (β=0.31, P=0.001). It should be noted that no adjustment has been made through modification indexes. With the total effect size (β=0.72, P=0.001), the variance accounted for (VAF) was calculated as 43%, indicating the partial mediating role of self-efficacy in the relationship between perceived social support and resilience in nurses (Table 4).
Discussion
The results showed that self-efficacy significantly mediates the relationship between social support and productivity. These results are compatible with previous studies showing that high social support is related to higher levels of self-efficacy [23]. Another study showed that the negative effect of perceived stress on the quality of life can be mediated by social support and self-efficacy variables [38]. Although our findings are compatible with previous studies, this study further confirms the relative mediating effects of self-efficacy in the association between resilience and social support in Iranian nurses during the COVID-19 epidemic.
Research evidence shows that support in the workplace can empower personnel, increase self-efficacy, and develop professional performance [18, 39, 40]. It leads to greater apprehension, encouragement, courageousness, respect, and a sense of professional success [41], increased motivation, improved performance, and work attitude [42-44]. Social support from colleagues can inhibit stress and reduce psychological problems. Therefore, executing strategies that assist social support can notably enhance nurses’ self-efficacy [45]. In this study, it was shown that self-efficacy mediates the relationship between resilience and social support. Particularly, social support directly or through the mediating effects of self-efficacy affects resilience. The finding showed why self-efficacy is a connection between social support and resilience. Understanding high social support may expand self-efficacy and boost resilience. Bandura reported that support relationships improved individual self-efficacy [24]. Research has shown that support programs for nurses can play a crucial role in their self-efficacy [46] and enhance the quality of nursing care [47]. Therefore, social support is vital to boost the resilience of nurses, protect them, and promote behaviors that improve stress regulation [48].
In the explanation, it can be argued that people who receive greater social support benefit more from the verbal encouragement of those around them. They experience more efficiency in life crises and overcome problems because, in Bandura’s interpretation, one of the most effective ways to grow self-efficacy is to receive verbal encouragement from those around them [24]. In contrast, self-efficacy is essential in resilience [18, 49, 50] and human endeavors. In other words, highly self-efficient nurses will be more likely to survive after exposure to failure. When a low self-efficacy nurse experiences problems, it will experience stress and anxiety that can interfere with other functions and even reduce self-efficacy. However, individuals with high self-efficacy are assured of their capacity to overcome difficult situations [51]. They are optimistic about the future, and this positive expectation of their future will help them against obstacles. Most people committed to achieving goals are better at dealing with problems, and instead of magnifying them, they make them natural and sometimes even think of problems as challenge that can make them stronger [50].
Although our results have provided evidence of the mediation of self-efficacy in the relation between resilience and social support of Iranian nurses during the COVID-19 pandemic, this research is accompanied by limitations.
First, this study was done in two hospitals, and future research could use wider sampling at the national level to increase the generalization of the results. This study was carried out within the framework of a correlational project, so our suggestion to future researchers is to conduct experimental and longitudinal research to achieve causality. In this study, we used self-report questionnaires that can be answered with social bias and lack actual answers. It is also recommended that exploration interviews be used to understand better the variables of self-efficacy and social support, which requires qualitative and even hybrid research design. Due to the COVID-19 epidemic and observing social distance, we collected the desired data online. Our suggestion is to collect data face-to-face.
This study gave a detailed understanding of how self-efficacy and social support improve nurses’ resilience. This paper has identified paths to improve the resilience of nurses through social support and self-efficacy. Accordingly, it would be suggested that medical education managers and planners provide the necessary training and therapeutic programs for nurses’ psychological empowerment during COVID-19 and afterward.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.363). All participants signed the informed consent form.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design, data analysis, interpretation, review, editing and final approval: All authors. Sampling and writing the initial draft: Sajjad Saadat and Maryam Jafroudi; Recruiting the participants: Sajjad Saadat and Maryam Zhaleparvar.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the nurses who completed the questionnaires and the Clinical Research Development Unit of Poursina Hospital, Guilan University of Medical Sciences.
References
- Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health-The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020; 91:264-6. [DOI:10.1016/j.ijid.2020.01.009] [PMID] [PMCID]
- Jiloha RC. COVID-19 and mental health. Epidemiol Int. 2020; 5(1):7-9. [Link]
- World Health Organization. State of the world's nursing 2020: Investing in education, jobs and leadership. Geneva: WHO; 2020. [Link]
- World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. Geneva: WHO; 2020. [Link]
- No Author. Essential case management practices amidst the novel coronavirus disease 2019 (COVID-19) crisis: Part 1: Tele-Case management, surge capacity, discharge planning, and transitions of care. Prof Case Manag. 2020; 25(5):E15-6. [DOI:10.1097/NCM.0000000000000463] [PMID]
- Deng D, Naslund JA. Psychological impact of COVID-19 pandemic on frontline health workers in low-and middle-income countries. Harva Public Health Rev. 2020; 26. [DOI:10.54111/0001/Z1]
- Neto MLR, Almeida HG, Esmeraldo JD, Nobre CB, Pinheiro WR, de Oliveira CRT, et al. When health professionals look death in the eye: The mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res. 2020; 288:112972. [DOI:10.1016/j.psychres.2020.112972] [PMID] [PMCID]
- Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: Qualitative analysis of survey responses. Int J Environ Res Public Health. 2020; 17(21):8126. [DOI:10.3390/ijerph17218126] [PMID] [PMCID]
- Johnston MC, Porteous T, Crilly MA, Burton CD, Elliott A, Iversen L, et al. Physical disease and resilient outcomes: A systematic review of resilience definitions and study methods. Psychosomatics. 2015; 56(2):168-80. [DOI:10.1016/j.psym.2014.10.005] [PMID] [PMCID]
- Öksüz E, Demiralp M, Mersin S, Tüzer H, Aksu M, Sarıkoc G. Resilience in nurses in terms of perceived social support, job satisfaction and certain variables. J Nurs Manag. 2019; 27(2):423-32. [DOI:10.1111/jonm.12703] [PMID]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020; 17(5):1729. [DOI:10.3390/ijerph17051729] [PMID] [PMCID]
- Hegney DG, Rees CS, Osseiran-Moisson R, Breen L, Eley R, Windsor C, et al. Perceptions of nursing workloads and contributing factors, and their impact on implicit care rationing: A Queensland, Australia study. J Nurs Manag. 2019; 27(2):371-80. [DOI:10.1111/jonm.12693] [PMID]
- Jo S, Kurt S, Bennett JA, Mayer K, Pituch KA, Simpson V, et al. Nurses’ resilience in the face of coronavirus (COVID-19): An international view. Nurs Health Sci. 2021; 23(3):646-57. [DOI:10.1111/nhs.12863] [PMID] [PMCID]
- McAllister M, Lowe JB. Preparing for practice: Becoming resilient. In: McAllister M, Lowe JB, editors. The resilient nurse: Empowering your practice. New York: Springer Publishing Company; 2011. [Link]
- Arrogante O, Pérez-García AM, Aparicio-Zaldívar EG. [Personal resources relevant to psychological well-being in nursing (Spanish)]. Enferm Intensiva. 2016; 27(1):22-30. [DOI:10.1016/j.enfi.2015.07.002] [PMID]
- Morse JM, Kent-Marvick J, Barry LA, Harvey J, Okang EN, Rudd EA, et al. Developing the resilience framework for nursing and healthcare. Glob Qual Nurs Res. 2021; 8:23333936211005475. [PMID]
- McCann CM, Beddoe E, McCormick K, Huggard P, Kedge S, Adamson C, et al. Resilience in the health professions: A review of recent literature. Int J Wellbeing. 2013; 3(1):60-81. [DOI:10.5502/ijw.v3i1.4]
- Wang L, Tao H, Bowers BJ, Brown R, Zhang Y. Influence of social support and self-efficacy on resilience of early career registered nurses. West J Nurs Res. 2018; 40(5):648-64. [DOI:10.1177/0193945916685712] [PMID]
- Kılınç T, Sis Çelik A. Relationship between the social support and psychological resilience levels perceived by nurses during the COVID-19 pandemic: A study from Turkey. Perspect Psychiatr Care. 2021; 57(3):1000-8. [DOI:10.1111/ppc.12648] [PMID]
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988; 52(1):30-41. [DOI:10.1207/s15327752jpa5201_2]
- Prati G, Pietrantoni L. The relation of perceived and received social support to mental health among first responders: A meta-analytic review. J Community Psychol. 2010; 38(3):403-17. [DOI:10.1002/jcop.20371]
- Wu F, Ren Z, Wang Q, He M, Xiong W, Ma G, et al. The relationship between job stress and job burnout: The mediating effects of perceived social support and job satisfaction. Psychol Health Med. 2021; 26(2):204-11. [DOI:10.1080/13548506.2020.1778750] [PMID]
- Stetz TA, Stetz MC, Bliese PD. The importance of self-efficacy in the moderating effects of social support on stressor-strain relationships. Work Stress. 2006; 20(1):49-59. [DOI:10.1080/02678370600624039]
- Bandura A. Perceived self-efficacy in cognitive development and functioning. Educ Psychol. 1993; 28(2):117-48. [DOI:10.1207/s15326985ep2802_3]
- Boudreaux S, Broussard L. School nurses’ perceived barriers and perceptual influences when implementing AED programs. J Sch Nurs. 2020; 36(3):187-92. [DOI:10.1177/1059840518805822] [PMID]
- Chen X, Zhang Y, Xu X, Wang W, Yan H, Li S, et al. Mediating roles of anxiety, self-efficacy, and sleep quality on the relationship between patient-reported physician empathy and inflammatory markers in ulcerative colitis patients. Med Sci Monit. 2019; 25:7889-97. [DOI:10.12659/msm.917552] [PMID] [PMCID]
- O'Neill E, Clarke P, Fido D, Vione KC. The role of future time perspective, body awareness, and social connectedness in the relationship between self-efficacy and resilience. Int J Ment Health Addiction. 2022; 20:1171–81. [Link]
- Aoyagi Y, Beck CR, Dingwall R, Nguyen-Van-Tam JS. Healthcare workers’ willingness to work during an influenza pandemic: A systematic review and meta-analysis. Influenza Other Respir Viruses. 2015; 9(3):120-30. [DOI:10.1111/irv.12310] [PMID] [PMCID]
- Lee J, Kang SJ. Factors influencing nurses’ intention to care for patients with emerging infectious diseases: Application of the theory of planned behavior. Nurs Health Sci. 2020; 22(1):82-90.[DOI:10.1111/nhs.12652] [PMID]
- Chow SC, Shao J, Wang H, Lokhnygina Y. Sample size calculations in clinical research. New York: Chapman and Hall/CRC; 2017. [DOI:10.1201/9781315183084]
- Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990; 55(3-4):610-7. [DOI:10.1207/s15327752jpa5201_2]
- Bagherian-Sararoudi R, Hajian A, Ehsan HB, Sarafraz MR, Zimet GD. Psychometric properties of the Persian version of the multidimensional scale of perceived social support in Iran. Int J Prev Med. 2013; 4(11):1277-81. [Link]
- Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: A user’s portfolio. Causal and control beliefs. Windsor, UK: NFER-NELSON; 1995. [Link]
- Farnia V, Asadi R, Abdoli N, Radmehr F, Alikhani M, Khodamoradi M, et al. Psychometric properties of the Persian version of General Self-Efficacy Scale (GSES) among substance abusers the year 2019-2020 in Kermanshah city. Clin Epidemiol Glob Health. 2020; 8(3):949-53. [DOI:10.1016/j.cegh.2020.03.002]
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003; 18(2):76-82. [PMID]
- Ahangarzadeh Rezaei S. [Psychometric properties of the Persian version of “Conner-Davision Resilience Scale” in Adolescents with Cancer (Persian)]. Nurs Midwifery J. 2015; 13(9):739-47. [Link]
- Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Epidemiology. 2007; 18(6):805-35. [DOI:10.1097/EDE.0b013e3181577511] [PMID]
- Long Q, Guo J, Zhong Q, Jiang S, Wiley J, Chen JL. General self-efficacy and social support as mediators of the association between perceived stress and quality of life among rural women with previous gestational diabetes mellitus. J Clin Nurs. 2021; 30(7-8):1026-36. [DOI:10.1111/jocn.15648] [PMID]
- Welsh D. Self-efficacy measurement and enhancement strategies for medical-surgical clinical nurses. Medsurg Nurs. 2014; 23(6):371-7. [PMID]
- Conner M. Self-efficacy, stress, and social support in retention of student registered nurse anesthetists. AANA J. 2015; 83(2):133-8. [PMID]
- Glozah FN. Exploring Ghanaian adolescents’ meaning of health and wellbeing: A psychosocial perspective. I Int J Qual Stud Health Well-being. 2015; 10:26370. [DOI:10.3402/qhw.v10.26370] [PMID] [PMCID]
- Papadopoulou C, Kotronoulas G, Schneider A, Miller MI, McBride J, Polly Z, et al. Patient-reported self-efficacy, anxiety, and health-related quality of life during chemotherapy: Results from a longitudinal study. Oncol Nurs Forum. 2017; 44(1):127-36.[DOI:10.1188/17.onf.127-136] [PMID]
- Molero Jurado MDM, Pérez-Fuentes MDC, Oropesa Ruiz NF, Simón Márquez MDM, Gázquez Linares JJ. Self-efficacy and emotional intelligence as predictors of perceived stress in nursing professionals. Medicina. 2019; 55(6):237. [DOI:10.3390/medicina55060237] [PMID] [PMCID]
- Holland B, Gosselin K, Mulcahy A. The effect of autogenic training on self-efficacy, anxiety, and performance on nursing student simulation. Nurs Educ Perspect. 2017; 38(2):87-89.[DOI:10.1097/01.NEP.0000000000000110] [PMID]
- Hall DS. The relationship between supervisor support and registered nurse outcomes in nursing care units. Nurs Adm Q. 2007; 31(1):68-80. [DOI:10.1097/00006216-200701000-00015] [PMID]
- Jnah AJ, Robinson CB. Mentoring and self-efficacy: Implications for the neonatal nurse practitioner workforce. Adv Neonatal Care. 2015; 15(5):E3-11. [DOI:10.1097/anc.0000000000000227] [PMID]
- Kim EY, Chang SO. Exploring nurse perceptions and experiences of resilience: A meta-synthesis study. BMC Nurs. 2022; 21(1):26.[DOI:10.1186/s12912-021-00803-z] [PMID] [PMCID]
- Sippel LM, Pietrzak RH, Charney DS, Mayes LC, Southwick SM. How does social support enhance resilience in the trauma-exposed individual? Ecol Soc. 2015; 20(4). [DOI:10.5751/ES-07832-200410]
- Taylor H, Reyes H. Self-efficacy and resilience in baccalaureate nursing students. Int J Nurs Educ Scholarsh. 2012; 9:Article 2 [DOI:10.1515/1548-923X.2218] [PMID]
- Lau R, Willetts G, Hood K, Cross W. Development of self-efficacy of newly graduated registered nurses in an aged care program. Australas J Ageing. 2015; 34(4):224-8. [DOI:10.1111/ajag.12156] [PMID]
- Pragholapati A. Self-efficacy of nurses during the pandemic Covid-19. Diunduh Dari Academia. edu. 2020. [Link]
Article Type : Research |
Subject:
General
Received: 2023/01/12 | Accepted: 2024/03/9 | Published: 2024/07/1
Received: 2023/01/12 | Accepted: 2024/03/9 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |