Tue, Feb 3, 2026
Volume 34, Issue 3 (6-2024)
JHNM 2024, 34(3): 201-210 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bastani F, Haghani H, Maleki M. Evaluation of Drug Adherence in Older Adults With Polypharmac. JHNM 2024; 34 (3) :201-210
URL: http://hnmj.gums.ac.ir/article-1-2368-en.html
URL: http://hnmj.gums.ac.ir/article-1-2368-en.html
1- Professor, Department of Community Health Nursing and Geriatric Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. , bastani.f@iums.ac.ir
2- Assistant Professor, Department of Biostatistics, School of Health, Iran University of Medical Sciences, Tehran, Iran.
3- MSc in Geriatric Nursing, Department of Community Health Nursing and Geriatric Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Assistant Professor, Department of Biostatistics, School of Health, Iran University of Medical Sciences, Tehran, Iran.
3- MSc in Geriatric Nursing, Department of Community Health Nursing and Geriatric Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 538 kb]
(824 Downloads)
| Abstract (HTML) (1428 Views)
Full-Text: (859 Views)
Introduction
Older adults are the largest consumers of medication due to an age-associated increase in chronic conditions. Thus, multiple medication use (i.e. polypharmacy) is a common consequence of providing healthcare to older adults. Polypharmacy among older adults is a significant issue, which refers to the simultaneous use of five or more drugs [1]. By reviewing the statistics and information available in the field of the elderly population, we repeatedly come across studies that report the progressive aging of the population worldwide. The growth of the elderly population in societies poses a new challenge to the organizations in charge of their health [2]. The issue of nonadherence in healthcare systems is important because it is responsible for over 20% of hospital admissions due to preventable adverse events, leading to unnecessary costs with a major economic impact [1, 3]. The results of studies show that the prevalence of polypharmacy increases with age. The medication treatment will be effective if individuals use it accurately and regularly [4-6]. The number of home-dwelling older people who need drug treatment is increasing as the population ages. Potentially inappropriate medications are drugs that should be avoided whenever possible in older adults because of their poor benefit-risk ratio in old age [7]. One of the important issues in this group is polypharmacy, which is defined as the simultaneous use of several drugs. The research on polypharmacy reveals adverse effects of this issue, the increase in the hospitalization rate of older people, the decline in health status, the rise in health costs for older people as well as the health system, and many other things that can probably cause health issues and overshadowing treatment, including medication adherence [8].
Both polypharmacy and potentially inappropriate medications have widely been studied in the scientific literature, but primarily in an overall context in older populations [9, 10, 11]. Based on what was discussed, polypharmacy and medication adherence concepts are considered essential and influential phenomena, especially in Geriatrics. Considering the importance of polypharmacy and medication adherence, we decided to search in this field, as the issue of medication adherence in older people with polypharmacy has been relatively neglected, and there is limited information in this field. This study focused on older adults with polypharmacy and aimed to identify their drug adherence.
Materials and Methods
This cross-sectional descriptive-analytical study was conducted on elderly patients with polypharmacy referred to selected educational-therapeutic centers of Iran University of Medical Sciences in Tehran City, Iran. The inclusion criteria were as follows: Age 60 or older, taking 5 or more drugs, not having cognitive impairment according to the abbreviated mental test (AMT) tool (obtaining a score of at least 7 out of 10), and ability to communicate in Persian language. Considering the medication adherence rate in older people with polypharmacy at the confidence level of 95% and accurate estimation of 0.5 scores based on the range of the score (0-28) of the related questionnaire, the sample size was estimated to be at least 250. This study used a continuous sampling method (stratified with proportional allocation) to take 50 samples (older adults) from each of the five large hospitals in Tehran, Iran.
In this study, the data collection tool was a demographic and clinical form questionnaire, the AMT and the adherence in chronic diseases scale (ACDS) to measure medication adherence. AMT short cognitive test [12] is a shortened form of cognitive test with 10 questions; this form has 10 points and scoring 6 or less is a sign of cognitive impairment. Foroughan et al. determined the validity and reliability of this questionnaire in the Persian version [13].
The ACDS is a 7-item questionnaire. Each question is associated with 5 predefined propositions of answers. The questions relate to patients’ behavior determining adherence (items 1-5) or situations and opinions, which may influence adherence (items 6, 7). This scale is supposed to reflect real-life adherence to pharmacological treatment and explain mechanisms determining patients’ adherence. Each item has 5 options to answer, so the options are named from ‘a’ to ‘e,’ and the order is scored from 0 to 4. A total score <20 means low adherence, 20 to 26 is moderate and a score ≥27 is considered high compliance. The lowest score in this tool is 0 and the highest score is 28. In a previous Iranian study, the reliability was carried out in Persian using the Cronbach α, equal to 0.92 [14]. In this study, we used the internal similarity coefficient method to determine the internal reliability of the questions (a Cronbach α of 0.83 was obtained). The questionnaire was completed by 20 older patients with polypharmacy who met the inclusion criteria. In this study, the variable of perceived health status in the demographic information reflects people’s overall perception of their health, including physical and psychological dimensions. Typically ascertained through health interview surveys, respondents were asked questions such as “How is your health in general? Is it very good, good, fair, poor and very poor?” using the horizontal 10-cm visual analog scale (VAS) [15].
After approving the proposal and obtaining permission from the ethics committee of the Iran University of Medical Sciences, the target population comprised all older adults with polypharmacy. After scoring the questionnaire, specifying the data and completing the answers to the questionnaires, the information related to each item was entered in the SPSS software, version 20. The data analysis was done in two sections: Descriptive statistics and inferential statistics. The descriptive statistics section used frequency distribution tables, numerical indices and percentage, Mean±SD. The inferential statistics section used the independent t-test and analysis of variance (ANOVA) and the Pearson correlation coefficient. The significance level of the test was set at P<0.05.
Results
The data-gathering instrument was provided to 250 people, but 243 participants responded to all items of the questionnaires. The findings show that the largest percentage of the participants were young seniors (53%) with a mean age 69.38±6.6, were male (54.7%), had a low level of education of being illiterate or with primary education (68.4%), were urbanite (93%), married (72.5%), were living with family members (91.8%) as well as possession of high level of health perception (45.5%) with only 0-3 underlying diseases (84.9%) These results were shown in Table 1.
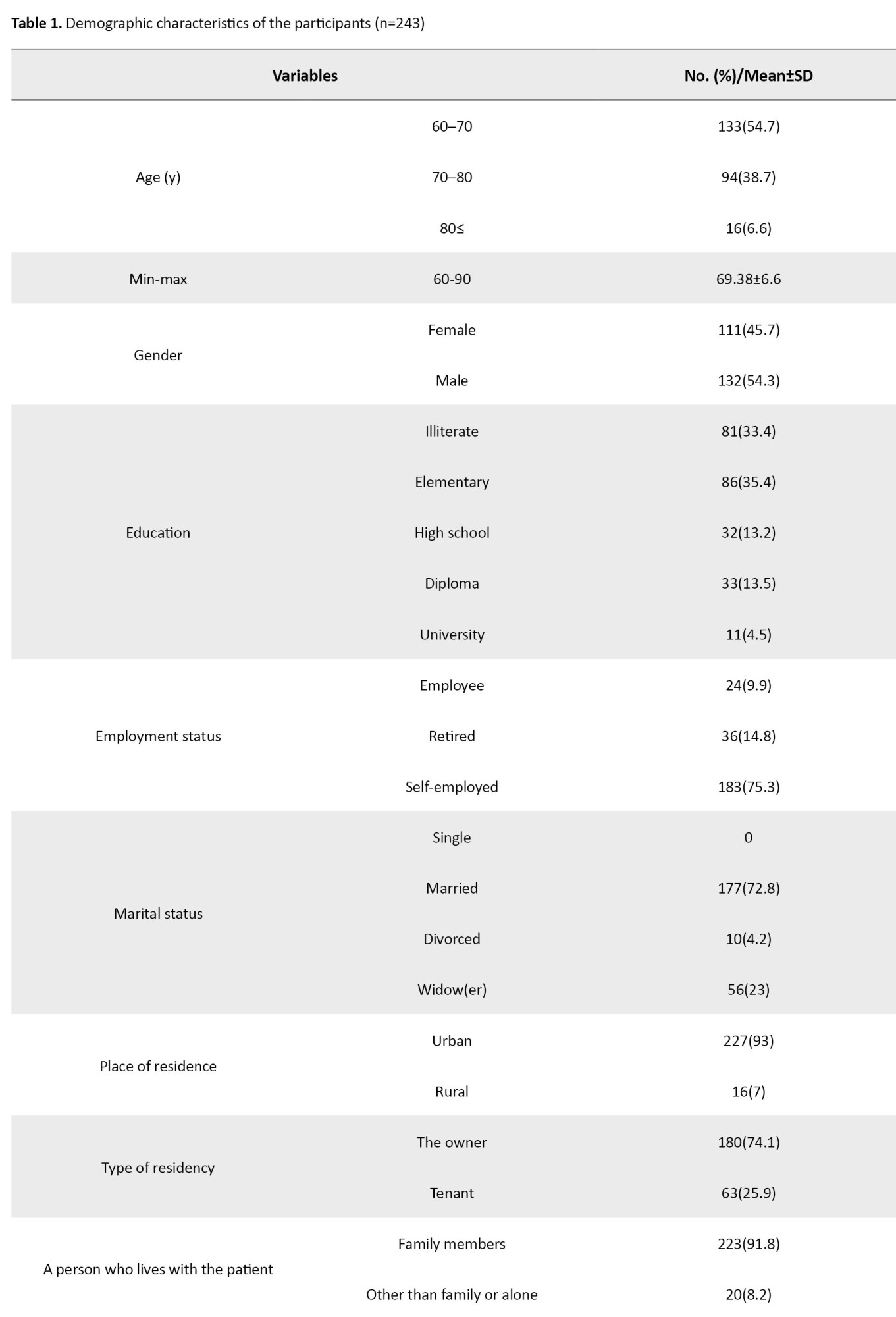
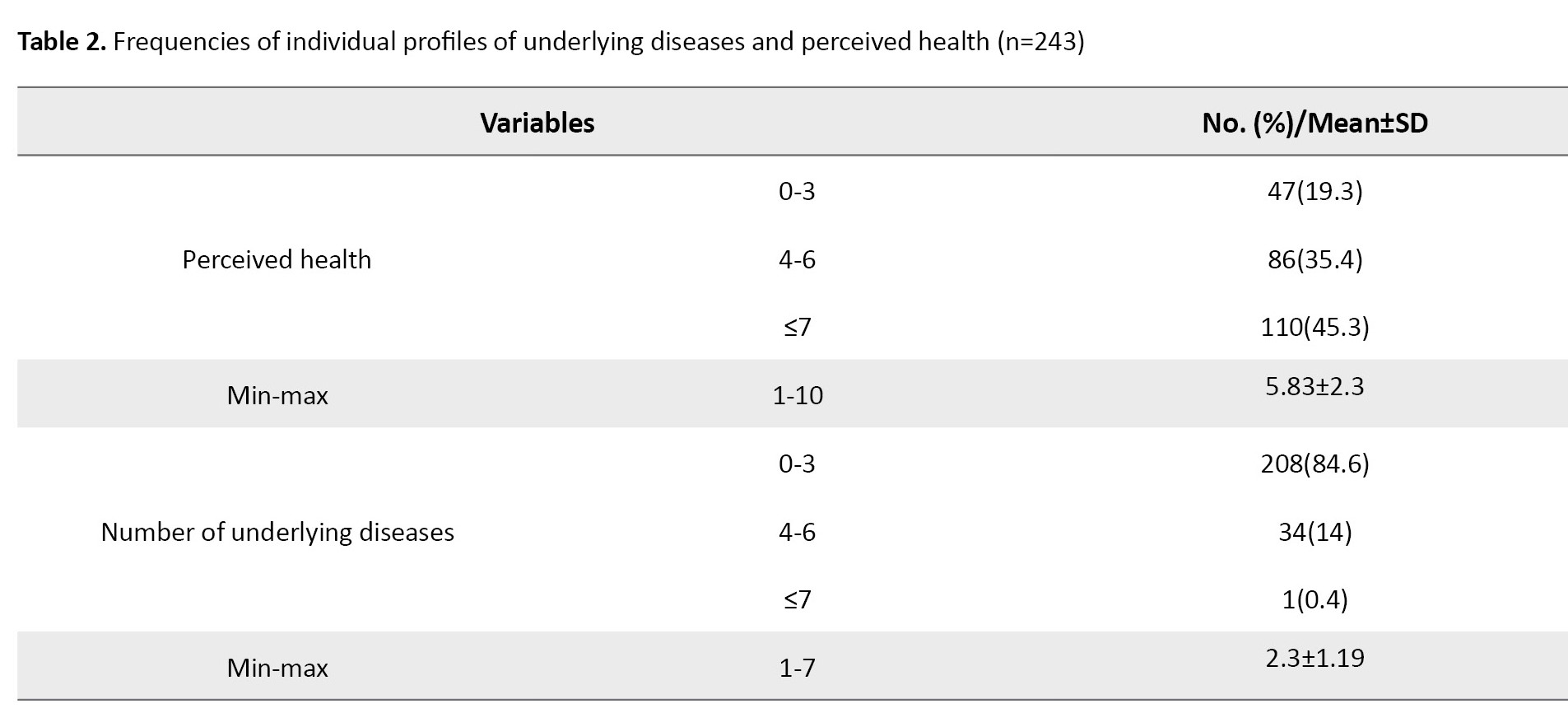
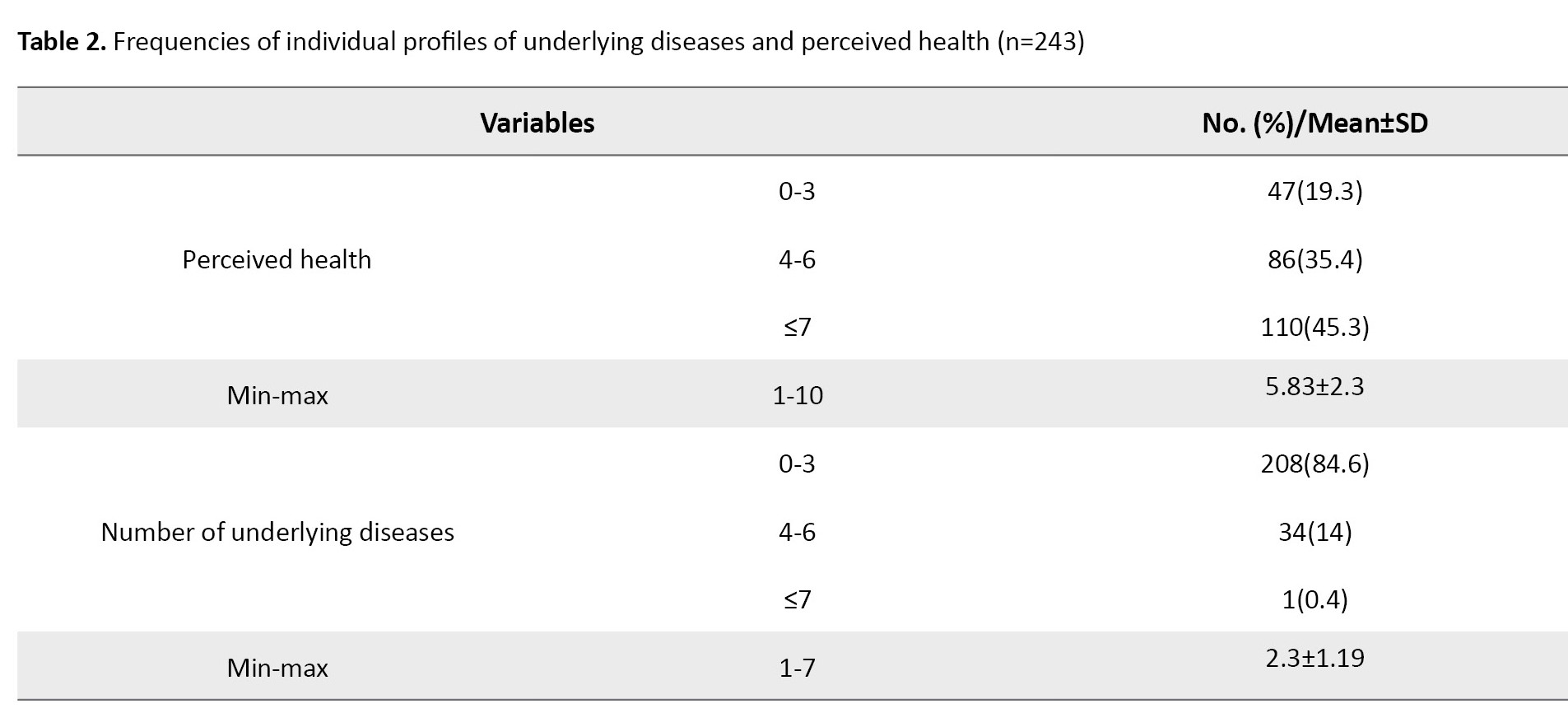
Table 2 presents the clinical health and disease data to analyze the state of drug adherence in the elderly participants.
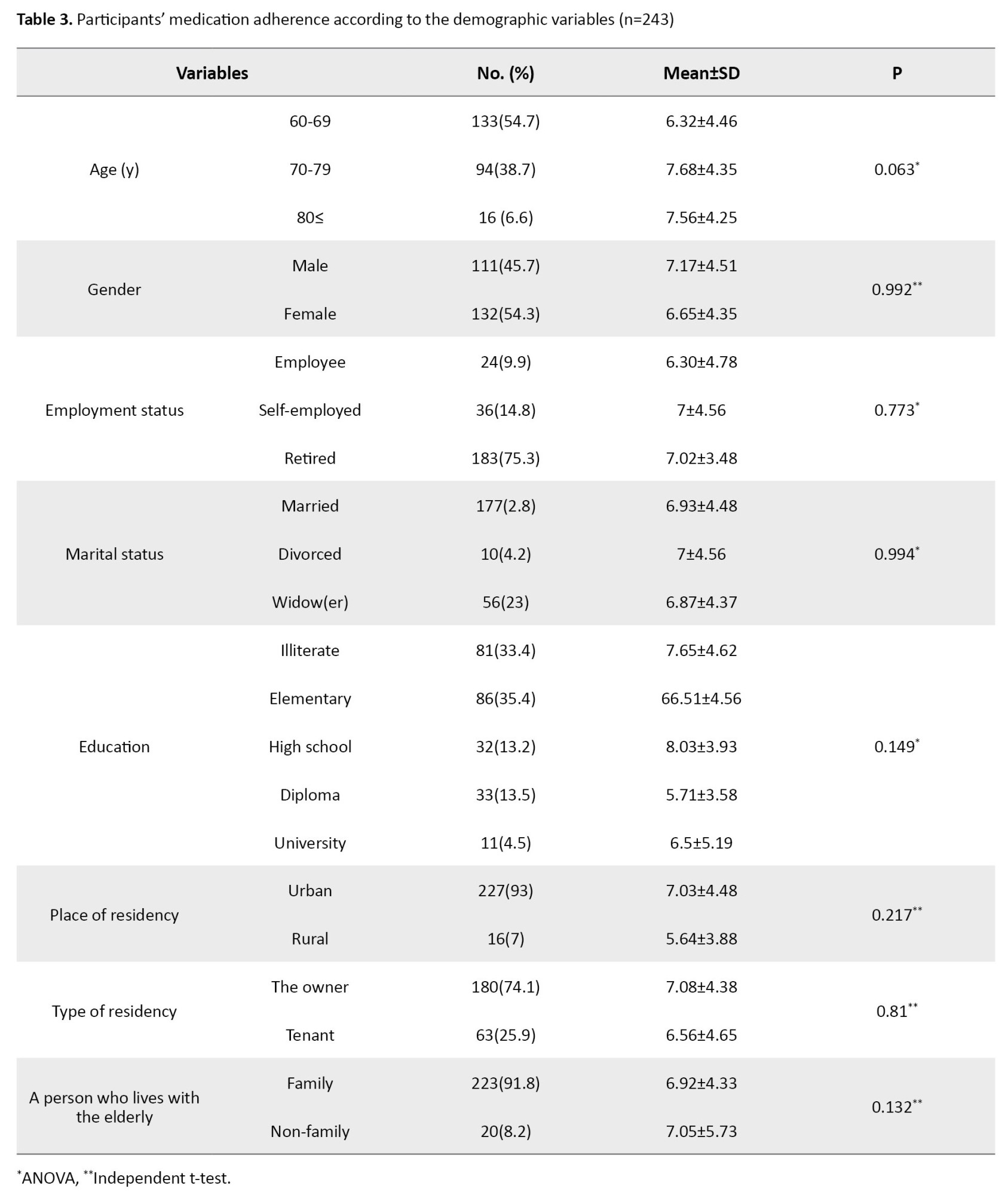
Based on the data among the 243 respondents to the medication adherence questionnaire, the minimum score obtained was 7, the maximum score was 28, and the Mean±SD was 21.06±4.44. There were no statistically significant relationships between the study’s main variable of medication adherence and demographic characteristics.
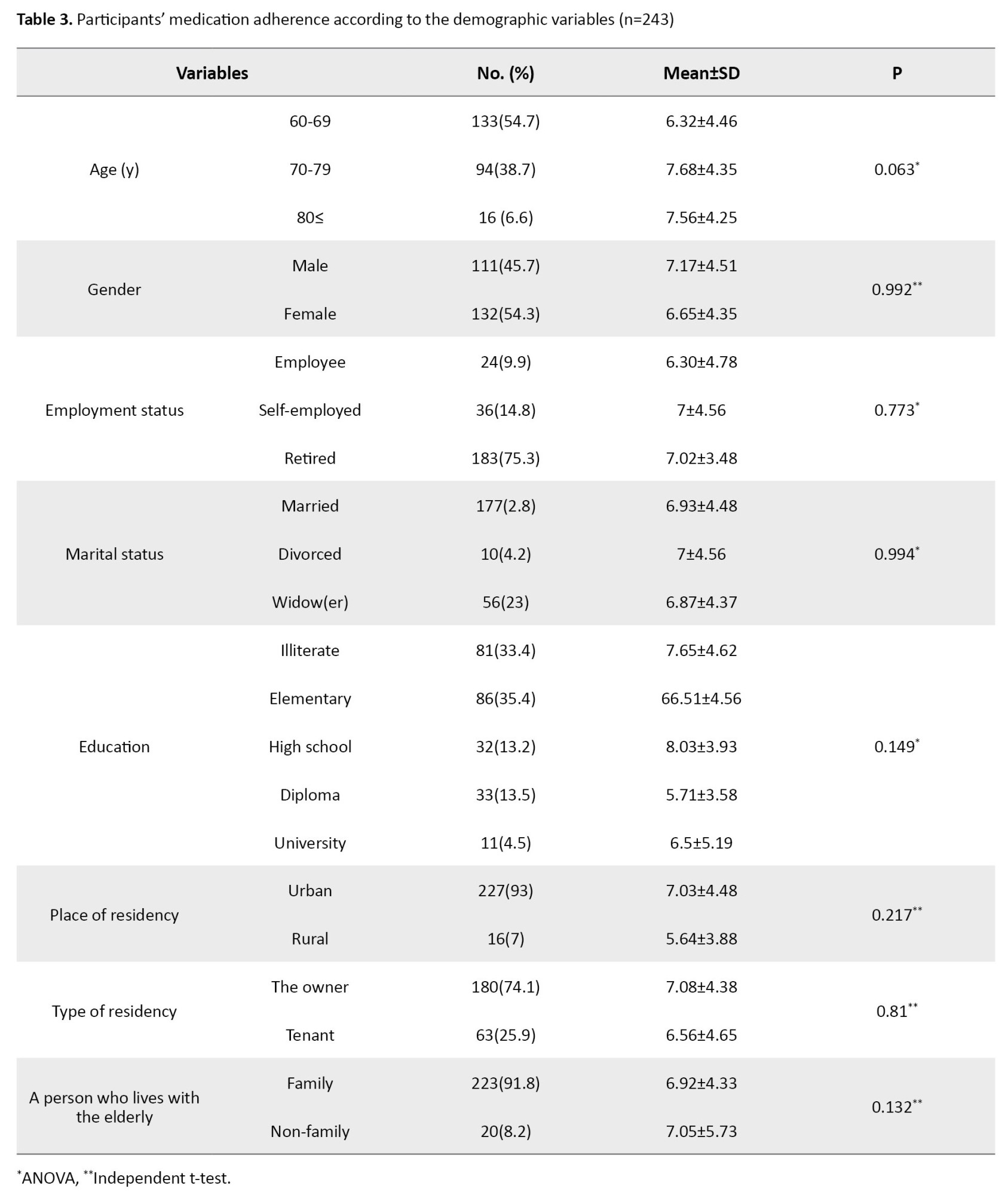
As shown in Table 3, none of the demographic variables have a statistically significant relationship with medication adherence.
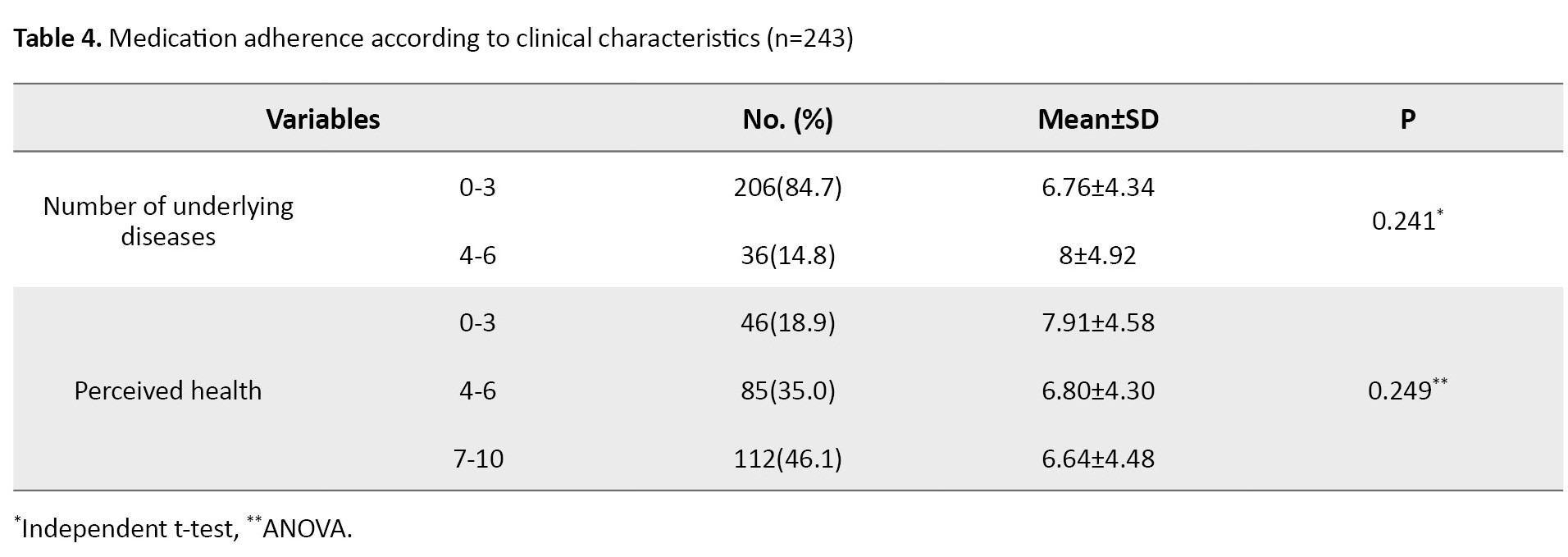
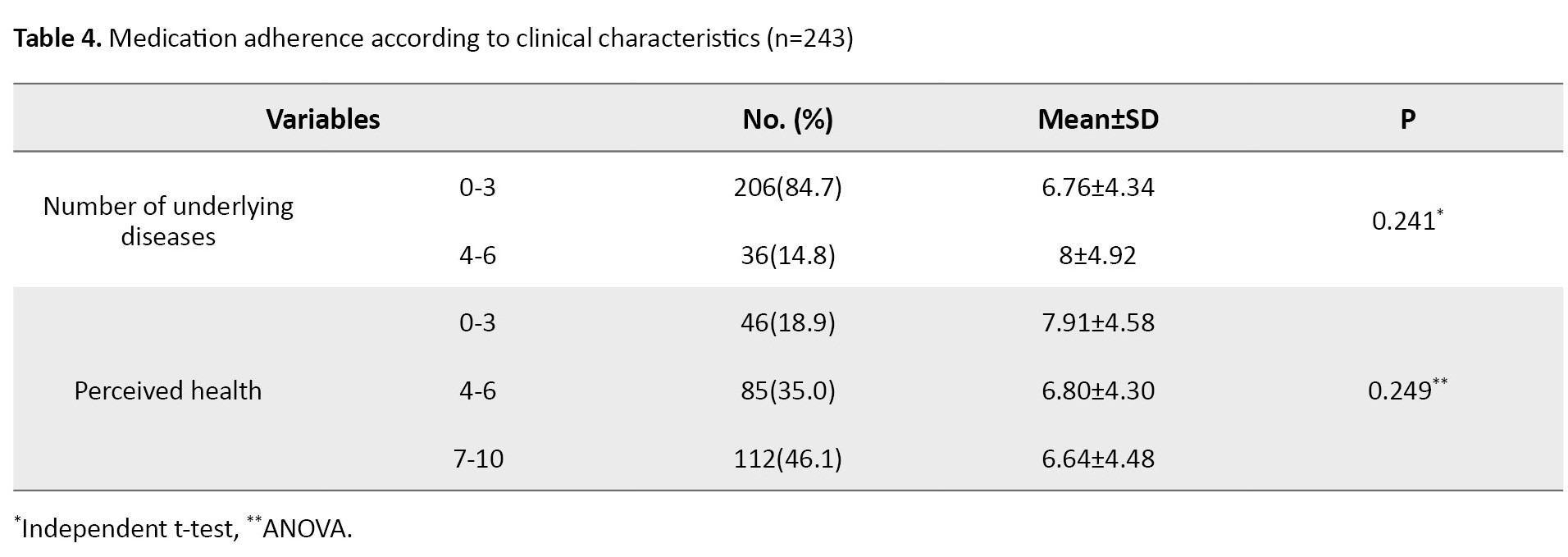
In addition, about 45.5% of the study participants had a high score of perceived health, and 84.9% had 0-3 underlying chronic diseases. Also, there was no statistical relationship between perceived health and personal characteristics. Moreover, there was no significant relationship between the number of underlying diseases of the older adults and demographic variables. The Pearson correlation test results showed a direct weak correlation between age and the main variables of “medication adherence” and “number of underlying diseases” (r=0.029, P=0.001 and r=0.031, P=0.001, respectively). Based on the ACDS scale, getting a score between 20 and 26 is considered medium drug adherence, with a mean 21.06±4.44 among 243 respondents. Similarly, the results of Table 4 present no significant relationship between the number of underlying diseases and the perception of the participants’ health with medication adherence.
In this study, we descriptively calculated the response frequency of the participants to the questions of the data-gathering instrument of ACDS. Regarding question No. 6, “Does your physician inquire about medication-related problems that you might experience?” 35.1% answered ‘No’ and got a 0 score. This negative reply of the participants “as a remarkable answer” did not exist in the answers to other questions.
Discussion
This study aimed to assess medication adherence status among older adults with polypharmacy living in Tehran City, Iran. This study was conducted among community-dwelling older adults. It was the first study investigating medication adherence as a major health challenge in Iran. According to the findings among the respondents to the medication adherence questionnaire and in line with the main aim of the research to assess the medication adherence of older people with polypharmacy, a percentage of the older adults showed a lack of optimal adherence to prescribed medicines. This finding is a major public health issue related to multimorbidity, poor control of chronic diseases, such as diabetes, hypertension, and dyslipidemia, and a subsequent decrease in the patient’s quality of life. Nonadherence contributes to adverse drug events, unplanned hospitalization, and increased emergency visits, especially in older individuals [16, 17]. According to the results of Melali et al., the medication adherence level among the users in older adults was low. They reported that low adherence could be due to medication side effects, psychological problems related to age, memory disorders, and chronic and debilitating diseases [18]. However, in our study, the AMT scale regarding the participants’ mental status showed no memory disorder in the elderly participants.
The study findings also showed no significant relationships between demographic/clinical characteristics and medication adherence. This finding may be due to the low sample size and the fact that medication adherence is a complex multi-factor behavior [19, 20]. According to the findings in line with the sub-objectives of the research, demographic variables including “gender,” “marital status,” “employment,” “level of education,” “the person with whom the elderly lives,” “place of residence,” “housing ownership,” as well as “perception of one’s health” had no statistically significant relationship with the drug adherence. In this regard, a quantitative study related to doctor-patient communication and the role of cognitive factors in non-compliance reported that none of the common demographic factors such as age, marital status, living alone, sex, race, income, occupation, number of dependents, intelligence, level of education or type of personality have been consistently related to medication nonadherence [21]. Another study on polypharmacy reported that low levels of drug adherence were associated with living in predominantly urbanized regions [22], which is almost consistent with our findings. Also, the positive association between health conditions (i.e. poor perceived health and increased number of chronic diseases) and polypharmacy in older adults has been reported in a systematic review about polypharmacy and pattern of medication use in community-dwelling older adults [23].
In addition, there is a direct correlation between medication adherence and increasing age and also between medication adherence and the number of underlying diseases [24-27]. Some researchers believed that in the elderly community, the role of sociodemographic factors such as age, education, living with family and not being alone was statistically significant in explaining polypharmacy and treatment adherence [28-30]. According to the World Health Organization (WHO), multiple factors contribute to poor medication adherence, normally classified into five categories: Socioeconomic factors, therapy-related factors, patient-related factors, condition-related factors and health system/health care team-related factors [31].
A systematic review examining the factors related to medication adherence and polypharmacy reported a significant relationship between medication adherence and the variable of age groups in older people [32].
Along with the study results, in the form of seven questions of the ACDS questionnaire, the greatest score of the study participants was reported as a non-follow-up by a physisian or drug prescriber.
In this context, side effects and poor communication between the user and the prescriber of the drug are frequently known factors in reducing patient drug adherence [33]. It was found that pharmacist-delivered education could improve treatment adherence [34].
Several studies have focused on medication adherence in diseases such as diabetes mellitus or hypertension. They all highlighted medication nonadherence as contributing to poorer control of the chronic disease. We included elderly patients with polypharmacy and any chronic diseases, making our results more generalizable to other diseases [35-38].
However, some limitations to the present study need to be considered. First, it is a cross-sectional descriptive study, whereby claims about the directionality of the causal relationship between the variables cannot be verified. Second, the subjects were recruited from a few health centers in Tehran, Iran, rather than to be multicenter. Third, we used non-probability sampling, which can lead to underrepresenting particular groups within the sample. Finally, the information was derived from self-reported data that can potentially lead to recall bias by the respondents, which should be considered while interpreting the results.
In summary, our findings show that older people with polypharmacy participating in this study have demonstrated moderate medication adherence, and there is a direct relationship between medication adherence of older people with polypharmacy and their age. The results revealed that the overall drug adherence in older people with polypharmacy who were referred to the medical education centers of Iran University of Medical Sciences was not optimum. In assessing the participants’ responses to the medication adherence questionnaire items, one of the remarkable answers was the lack of follow-up medication regimens by drug prescribers. It is necessary to emphasize healthcare professionals involved in patients’ medication use and follow-up drug adherence. Based on this study’s results, comprehensive educational interventions should be designed to improve older adults’ medication adherence with polypharmacy. In addition, future studies should focus on predictive correlational and or experimental design, how to enhance the elderly’ treatment adherence, and the possible facilitators and barriers to this problem.
Taking medicine as prescribed or medication adherence is important for controlling chronic diseases, treating temporary conditions, and overall long-term health and well-being. The study findings indicate medium medication adherence among the subjects, which is not optimum. Based on the study findings, a significant percentage of the participants believed that a personal connection with a healthcare provider or pharmacist to follow up on drug use is an important part of medication adherence. However, it should be noted that some study findings cast doubt about the need for multiple medications in older people due to dementia or not transmitting symptoms well, and this is another challenge, along with not observing the correctness of its use [39, 40]. Improving prescribing for older adults is a priority for all healthcare systems and optimizing drug prescriptions for older people is essential. A multidisciplinary team of healthcare professionals, including pharmacists, should be involved in medication use. This measure appears helpful and advisable for optimum drug adherence. Because patient education and counseling are the key to improving medication adherence, pharmacists-led medication education and counseling by healthcare professionals are necessary for drug adherence in older adults with polypharmacy.
Prospective and longitudinal studies are recommended to observe the causal relationships and confirm the findings of the current cross-sectional study. More research is needed to delineate further the consequences associated with drug use in elderly patients with polypharmacy. Considering that the present research is conducted in a hospital environment with inpatient participants who have been treated and hospitalized, conducting research outside the treatment environment and in a larger area through home healthcare visits with older people is appropriate.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1399.978). Informed consent was obtained from all participants, and they were assured of the confidentiality of their information.
Funding
This article was extracted from the master's thesis of Mahdi Maleki, approved by Research Vice-Chancellor of Iran University of Medical Sciences.
Authors' contributions
Data collection and writing the original draft: Mahdi Maleki; Data analysis and statistical analysis: Hamid Haghani; Conceptualization, supervision, review and editing: Farideh Bastani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all samples for participating and contributing to the study.
References
Older adults are the largest consumers of medication due to an age-associated increase in chronic conditions. Thus, multiple medication use (i.e. polypharmacy) is a common consequence of providing healthcare to older adults. Polypharmacy among older adults is a significant issue, which refers to the simultaneous use of five or more drugs [1]. By reviewing the statistics and information available in the field of the elderly population, we repeatedly come across studies that report the progressive aging of the population worldwide. The growth of the elderly population in societies poses a new challenge to the organizations in charge of their health [2]. The issue of nonadherence in healthcare systems is important because it is responsible for over 20% of hospital admissions due to preventable adverse events, leading to unnecessary costs with a major economic impact [1, 3]. The results of studies show that the prevalence of polypharmacy increases with age. The medication treatment will be effective if individuals use it accurately and regularly [4-6]. The number of home-dwelling older people who need drug treatment is increasing as the population ages. Potentially inappropriate medications are drugs that should be avoided whenever possible in older adults because of their poor benefit-risk ratio in old age [7]. One of the important issues in this group is polypharmacy, which is defined as the simultaneous use of several drugs. The research on polypharmacy reveals adverse effects of this issue, the increase in the hospitalization rate of older people, the decline in health status, the rise in health costs for older people as well as the health system, and many other things that can probably cause health issues and overshadowing treatment, including medication adherence [8].
Both polypharmacy and potentially inappropriate medications have widely been studied in the scientific literature, but primarily in an overall context in older populations [9, 10, 11]. Based on what was discussed, polypharmacy and medication adherence concepts are considered essential and influential phenomena, especially in Geriatrics. Considering the importance of polypharmacy and medication adherence, we decided to search in this field, as the issue of medication adherence in older people with polypharmacy has been relatively neglected, and there is limited information in this field. This study focused on older adults with polypharmacy and aimed to identify their drug adherence.
Materials and Methods
This cross-sectional descriptive-analytical study was conducted on elderly patients with polypharmacy referred to selected educational-therapeutic centers of Iran University of Medical Sciences in Tehran City, Iran. The inclusion criteria were as follows: Age 60 or older, taking 5 or more drugs, not having cognitive impairment according to the abbreviated mental test (AMT) tool (obtaining a score of at least 7 out of 10), and ability to communicate in Persian language. Considering the medication adherence rate in older people with polypharmacy at the confidence level of 95% and accurate estimation of 0.5 scores based on the range of the score (0-28) of the related questionnaire, the sample size was estimated to be at least 250. This study used a continuous sampling method (stratified with proportional allocation) to take 50 samples (older adults) from each of the five large hospitals in Tehran, Iran.
In this study, the data collection tool was a demographic and clinical form questionnaire, the AMT and the adherence in chronic diseases scale (ACDS) to measure medication adherence. AMT short cognitive test [12] is a shortened form of cognitive test with 10 questions; this form has 10 points and scoring 6 or less is a sign of cognitive impairment. Foroughan et al. determined the validity and reliability of this questionnaire in the Persian version [13].
The ACDS is a 7-item questionnaire. Each question is associated with 5 predefined propositions of answers. The questions relate to patients’ behavior determining adherence (items 1-5) or situations and opinions, which may influence adherence (items 6, 7). This scale is supposed to reflect real-life adherence to pharmacological treatment and explain mechanisms determining patients’ adherence. Each item has 5 options to answer, so the options are named from ‘a’ to ‘e,’ and the order is scored from 0 to 4. A total score <20 means low adherence, 20 to 26 is moderate and a score ≥27 is considered high compliance. The lowest score in this tool is 0 and the highest score is 28. In a previous Iranian study, the reliability was carried out in Persian using the Cronbach α, equal to 0.92 [14]. In this study, we used the internal similarity coefficient method to determine the internal reliability of the questions (a Cronbach α of 0.83 was obtained). The questionnaire was completed by 20 older patients with polypharmacy who met the inclusion criteria. In this study, the variable of perceived health status in the demographic information reflects people’s overall perception of their health, including physical and psychological dimensions. Typically ascertained through health interview surveys, respondents were asked questions such as “How is your health in general? Is it very good, good, fair, poor and very poor?” using the horizontal 10-cm visual analog scale (VAS) [15].
After approving the proposal and obtaining permission from the ethics committee of the Iran University of Medical Sciences, the target population comprised all older adults with polypharmacy. After scoring the questionnaire, specifying the data and completing the answers to the questionnaires, the information related to each item was entered in the SPSS software, version 20. The data analysis was done in two sections: Descriptive statistics and inferential statistics. The descriptive statistics section used frequency distribution tables, numerical indices and percentage, Mean±SD. The inferential statistics section used the independent t-test and analysis of variance (ANOVA) and the Pearson correlation coefficient. The significance level of the test was set at P<0.05.
Results
The data-gathering instrument was provided to 250 people, but 243 participants responded to all items of the questionnaires. The findings show that the largest percentage of the participants were young seniors (53%) with a mean age 69.38±6.6, were male (54.7%), had a low level of education of being illiterate or with primary education (68.4%), were urbanite (93%), married (72.5%), were living with family members (91.8%) as well as possession of high level of health perception (45.5%) with only 0-3 underlying diseases (84.9%) These results were shown in Table 1.
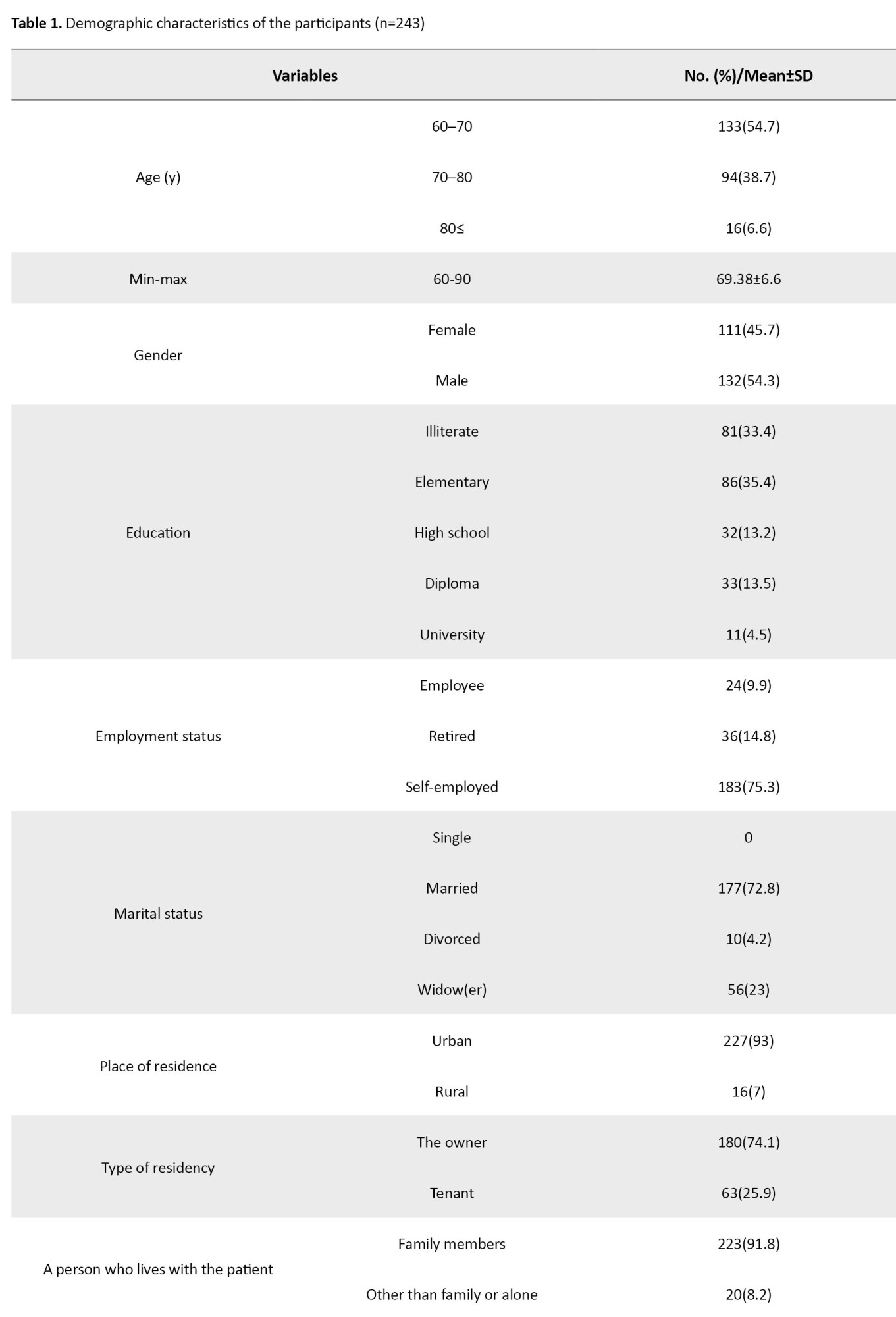
Table 2 presents the clinical health and disease data to analyze the state of drug adherence in the elderly participants.
Based on the data among the 243 respondents to the medication adherence questionnaire, the minimum score obtained was 7, the maximum score was 28, and the Mean±SD was 21.06±4.44. There were no statistically significant relationships between the study’s main variable of medication adherence and demographic characteristics.
As shown in Table 3, none of the demographic variables have a statistically significant relationship with medication adherence.
In addition, about 45.5% of the study participants had a high score of perceived health, and 84.9% had 0-3 underlying chronic diseases. Also, there was no statistical relationship between perceived health and personal characteristics. Moreover, there was no significant relationship between the number of underlying diseases of the older adults and demographic variables. The Pearson correlation test results showed a direct weak correlation between age and the main variables of “medication adherence” and “number of underlying diseases” (r=0.029, P=0.001 and r=0.031, P=0.001, respectively). Based on the ACDS scale, getting a score between 20 and 26 is considered medium drug adherence, with a mean 21.06±4.44 among 243 respondents. Similarly, the results of Table 4 present no significant relationship between the number of underlying diseases and the perception of the participants’ health with medication adherence.
In this study, we descriptively calculated the response frequency of the participants to the questions of the data-gathering instrument of ACDS. Regarding question No. 6, “Does your physician inquire about medication-related problems that you might experience?” 35.1% answered ‘No’ and got a 0 score. This negative reply of the participants “as a remarkable answer” did not exist in the answers to other questions.
Discussion
This study aimed to assess medication adherence status among older adults with polypharmacy living in Tehran City, Iran. This study was conducted among community-dwelling older adults. It was the first study investigating medication adherence as a major health challenge in Iran. According to the findings among the respondents to the medication adherence questionnaire and in line with the main aim of the research to assess the medication adherence of older people with polypharmacy, a percentage of the older adults showed a lack of optimal adherence to prescribed medicines. This finding is a major public health issue related to multimorbidity, poor control of chronic diseases, such as diabetes, hypertension, and dyslipidemia, and a subsequent decrease in the patient’s quality of life. Nonadherence contributes to adverse drug events, unplanned hospitalization, and increased emergency visits, especially in older individuals [16, 17]. According to the results of Melali et al., the medication adherence level among the users in older adults was low. They reported that low adherence could be due to medication side effects, psychological problems related to age, memory disorders, and chronic and debilitating diseases [18]. However, in our study, the AMT scale regarding the participants’ mental status showed no memory disorder in the elderly participants.
The study findings also showed no significant relationships between demographic/clinical characteristics and medication adherence. This finding may be due to the low sample size and the fact that medication adherence is a complex multi-factor behavior [19, 20]. According to the findings in line with the sub-objectives of the research, demographic variables including “gender,” “marital status,” “employment,” “level of education,” “the person with whom the elderly lives,” “place of residence,” “housing ownership,” as well as “perception of one’s health” had no statistically significant relationship with the drug adherence. In this regard, a quantitative study related to doctor-patient communication and the role of cognitive factors in non-compliance reported that none of the common demographic factors such as age, marital status, living alone, sex, race, income, occupation, number of dependents, intelligence, level of education or type of personality have been consistently related to medication nonadherence [21]. Another study on polypharmacy reported that low levels of drug adherence were associated with living in predominantly urbanized regions [22], which is almost consistent with our findings. Also, the positive association between health conditions (i.e. poor perceived health and increased number of chronic diseases) and polypharmacy in older adults has been reported in a systematic review about polypharmacy and pattern of medication use in community-dwelling older adults [23].
In addition, there is a direct correlation between medication adherence and increasing age and also between medication adherence and the number of underlying diseases [24-27]. Some researchers believed that in the elderly community, the role of sociodemographic factors such as age, education, living with family and not being alone was statistically significant in explaining polypharmacy and treatment adherence [28-30]. According to the World Health Organization (WHO), multiple factors contribute to poor medication adherence, normally classified into five categories: Socioeconomic factors, therapy-related factors, patient-related factors, condition-related factors and health system/health care team-related factors [31].
A systematic review examining the factors related to medication adherence and polypharmacy reported a significant relationship between medication adherence and the variable of age groups in older people [32].
Along with the study results, in the form of seven questions of the ACDS questionnaire, the greatest score of the study participants was reported as a non-follow-up by a physisian or drug prescriber.
In this context, side effects and poor communication between the user and the prescriber of the drug are frequently known factors in reducing patient drug adherence [33]. It was found that pharmacist-delivered education could improve treatment adherence [34].
Several studies have focused on medication adherence in diseases such as diabetes mellitus or hypertension. They all highlighted medication nonadherence as contributing to poorer control of the chronic disease. We included elderly patients with polypharmacy and any chronic diseases, making our results more generalizable to other diseases [35-38].
However, some limitations to the present study need to be considered. First, it is a cross-sectional descriptive study, whereby claims about the directionality of the causal relationship between the variables cannot be verified. Second, the subjects were recruited from a few health centers in Tehran, Iran, rather than to be multicenter. Third, we used non-probability sampling, which can lead to underrepresenting particular groups within the sample. Finally, the information was derived from self-reported data that can potentially lead to recall bias by the respondents, which should be considered while interpreting the results.
In summary, our findings show that older people with polypharmacy participating in this study have demonstrated moderate medication adherence, and there is a direct relationship between medication adherence of older people with polypharmacy and their age. The results revealed that the overall drug adherence in older people with polypharmacy who were referred to the medical education centers of Iran University of Medical Sciences was not optimum. In assessing the participants’ responses to the medication adherence questionnaire items, one of the remarkable answers was the lack of follow-up medication regimens by drug prescribers. It is necessary to emphasize healthcare professionals involved in patients’ medication use and follow-up drug adherence. Based on this study’s results, comprehensive educational interventions should be designed to improve older adults’ medication adherence with polypharmacy. In addition, future studies should focus on predictive correlational and or experimental design, how to enhance the elderly’ treatment adherence, and the possible facilitators and barriers to this problem.
Taking medicine as prescribed or medication adherence is important for controlling chronic diseases, treating temporary conditions, and overall long-term health and well-being. The study findings indicate medium medication adherence among the subjects, which is not optimum. Based on the study findings, a significant percentage of the participants believed that a personal connection with a healthcare provider or pharmacist to follow up on drug use is an important part of medication adherence. However, it should be noted that some study findings cast doubt about the need for multiple medications in older people due to dementia or not transmitting symptoms well, and this is another challenge, along with not observing the correctness of its use [39, 40]. Improving prescribing for older adults is a priority for all healthcare systems and optimizing drug prescriptions for older people is essential. A multidisciplinary team of healthcare professionals, including pharmacists, should be involved in medication use. This measure appears helpful and advisable for optimum drug adherence. Because patient education and counseling are the key to improving medication adherence, pharmacists-led medication education and counseling by healthcare professionals are necessary for drug adherence in older adults with polypharmacy.
Prospective and longitudinal studies are recommended to observe the causal relationships and confirm the findings of the current cross-sectional study. More research is needed to delineate further the consequences associated with drug use in elderly patients with polypharmacy. Considering that the present research is conducted in a hospital environment with inpatient participants who have been treated and hospitalized, conducting research outside the treatment environment and in a larger area through home healthcare visits with older people is appropriate.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1399.978). Informed consent was obtained from all participants, and they were assured of the confidentiality of their information.
Funding
This article was extracted from the master's thesis of Mahdi Maleki, approved by Research Vice-Chancellor of Iran University of Medical Sciences.
Authors' contributions
Data collection and writing the original draft: Mahdi Maleki; Data analysis and statistical analysis: Hamid Haghani; Conceptualization, supervision, review and editing: Farideh Bastani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all samples for participating and contributing to the study.
References
- Lavrador M, Cabral AC, Castel-Branco M, Figueiredo IV, Fernandez-Llimos F. Polypharmacy and medication adherence. In: Oliveria PJ, Malv JO. Aging: From fundamentals biology to social impact. Cambridge: Academic Press; 2023. [DOI:10.1016/B978-0-12-823761-8.00014-8]
- Ueno H, Ishikawa H, Kato M, Okuhara TG, Okada H, Kiuchi H. Factors related to self-care drug treatment and medication adherence of elderly people in Japan. Public Health Pract (Oxf), 2021; 2:100106. [PMID] [PMCID]
- AL Shidhani A, Al Salmani A, AL Saidi Y, Al Shehhi M, Al Khanjari H, AL Aamri M, et al. Polypharmacy and medication compliance among patients with type 2 diabetes in Oman: A cross-sectional study. Arch Pharm Pract. 2022; 13(3):48-53. [DOI:10.51847/zimW7hb8OD]
- Shareinia H, Sadeghmoghadam L, Mokhtarzadeh MR, Zahrayi SM, Jafari N, Noori R. Relationship between polypharmacy and medication adherence in the hypertensive elderly patients. Dis Diagn. 2020; 9(4):153-7. [Link]
- Nimee F, Steier J, Papandreou G, Skouroliakou M. A comprehensive medication review of a polypharmacy patient population: A cross-sectional observational study. Explor Res Clin Soc Pharm. 2022; 6:100144. [DOI:10.1016/j.rcsop.2022.100144]
- Ramey OL, Silva Almodóvar A, Nahata MC. Medication adherence in Medicare-enrolled older adults with asthma before and during the coronavirus disease 2019 pandemic. Ann Allergy Asthma Immunol. 2022; 128(5):561−7. [PMID] [PMCID]
- World Health Organization. Noncommunicable diseases country profiles 2018. Geneva: World Health Organization; 2018. [Link]
- Zheng H, Long Y, Wood R. Moran D, Zhang Z, Meg J, et al. Ageing society in developed countries challenges carbon mitigation. Nat Clim Chang. 2022; 12:241-8. [Link]
- Jørring Pallesen AV, Kristiansen M, Westendorp RGJ, Mortensen LH. Polypharmacy occurrence and the related risk of premature death among older adults in Denmark: A nationwide register-based cohort study. PLoS One. 2022; 17(2):e0264332.[PMID] [PMCID]
- Pazan F, Wehling M. Polypharmacy in older adults: A narrative review of definitions, epidemiology and consequences. Eur Geriatr Med. 2021; 12(3):443-52. [DOI:10.1007/s41999-021-00479-3] [PMID] [PMCID]
- Jungo KT, Streit S, Lauffenburger JC. Patient factors associated with new prescribing of potentially inappropriate medications in multimorbid US older adults using multiple medications. BMC Geriatr. 2021; 21(1):163. [DOI:10.1186/s12877-021-02089-x] [PMID] [PMCID]
- Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing, 1972; 1(4):233-8. [PMID]
- Foroughan M, Wahlund L, Jafari Z, Rahgozar M, Farahani IG, Rashidi V. Validity and reliability of Abbreviated Mental Test Score (AMTS) among older Iranian. Psychogeriatrics. 2017; 17(6):460-5. [DOI:10.1111/psyg.12276] [PMID]
- Pouresmaeel Niyazi M, Farshbaf Mani Sefat F, Khademi A, Meshgi S. [The relationship of treatment adherence with illness perception, self-compassion and perceived social support: The mediatory role of life expectancy among patients with cardiovascular diseases (Persian)]. Shenakht J Psychol Psychiatry. 2022; 9(2):92-105.[DOI:10.32598/shenakht.9.2.92]
- Åström M, Thet Lwin ZM, Teni FS, Burström K, Berg J. Use of the visual analogue scale for health state valuation: A scoping review. Qual Life Res. 2023; 32(10):2719-29. [PMID] [PMCID]
- World Health Organization. The World Health Report 2002: Reducing risks, promoting healthy life. World Health Organization: Geneva; 2002. [Link]
- Lavsa SM, Holzworth A, Ansani NT. Selection of a validated scale for measuring medication adherence. J Am Pharm Ass. 2011; 51(1):90-4. [DOI:10.1331/JAPhA.2011.09154] [PMID]
- Melali F, Hoseini H, Moeini M. [Medication adherence among elderly with hypertension: Johnson Model-based Program (Persian)]. Salmand. 2023; 18(1):104-17. [DOI:10.32598/sija.2022.3393.1]
- Zangiabadi A, Shah Esmaili A, Ahmady Tabatabaei SV, Movahed E, Shankestani H. Factors regarding adherence to medication in patients with hypertension based on health belief model in the South of Kerman, Iran, in 2019. J Community Health Res. 2022; 11(2):82 -90. [DOI:10.18502/jchr.v11i2.9995]
- Maffoni M, Traversoni S, Costa E, Midão L, Kardas P, Kurczewska-Michalak M, et al. Medication adherence in the older adults with chronic multimorbidity: A systematic review of qualitative studies on patient’s experience. Eur Geriatr Med. 2020; 11(3):369-81.[DOI:10.1007/s41999-020-00313-2] [PMID]
- Ley P. Doctor-patient communication: Some quantitative estimates of the role of cognitive factors in non-compliance. J Hypertens Suppl. 1985; 3(1):S51-5. [PMID]
- Midão L, Giardini A, Menditto E, Kardas P, Costa E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr. 2018; 78:213-20. [DOI:10.1016/j.archger.2018.06.018] [PMID]
- Hsu HF, Chen KM, Belcastro F, Chen YF. Polypharmacy and pattern of medication use in community-dwelling older adults: A systematic review. J Clin Nurs. 2021; 30(7-8):918-28. [DOI:10.1111/jocn.15595] [PMID]
- Smaje A, Weston-Clark M, Raj R, Orlu M, Davis D, Rawle M. Factors associated with medication adherence in older patients: A systematic review. Aging Med (Milton). 2018; 1(3):254-66. [DOI:10.1002/agm2.12045] [PMID] [PMCID]
- Kim SJ, Kwon OD, Han EB, Lee CM, Oh SW, Joh HK, et al. Impact of number of medications and age on adherence to antihypertensive medications: A nationwide population-based study. Medicine (Baltimore). 2019; 98(49):e17825. [DOI:10.1097/MD.0000000000017825] [PMID] [PMCID]
- Burnier M, Polychronopoulou E, Wuerzner G. Hypertension and drug adherence in the elderly. Front Cardiovasc Med. 2020; 7:49. [DOI:10.3389/fcvm.2020.00049] [PMID] [PMCID]
- Yao S, Lix L, Teare G, Evans C, Blackburn D. The impact of age and sex concordance between patients and physicians on medication adherence: A population-based study. Patient Prefer Adherence. 2022; 16:169-78. [PMID] [PMCID]
- Menditto E, Cahir C, Aza-Pascual-Salcedo M, Bruzzese D, Poblador-Plou B, Malo S, et al. Adherence to chronic medication in older populations: Application of a common protocol among three European cohorts. Patient Prefer Adherence. 2018; 12:1975-87. [DOI:10.2147/PPA.S164819] [PMID] [PMCID]
- Castioni J, Marques-Vidal P, Abolhassani N, Vollenweider P, Waeber G. Prevalence and determinants of polypharmacy in Switzerland: Data from the CoLaus study. BMC Health Serv Res. 2017; 17(1):840. [DOI:10.1186/s12913-017-2793-z] [PMID] [PMCID]
- Morin L, Johnell K, Laroche ML, Fastbom J, Wastesson JW. The epidemiology of poly- Pharmacy in older adults: Register-based prospective cohort study. Clin Epidemiol. 2018; 10:289-98. [DOI:10.2147/CLEP.S153458] [PMID] [PMCID]
- World Health Organization. Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization; 2003. [Link]
- Yeam CT, Chia S, Tan HCC, Kwan YH, Fong W, Seng JJB. A systematic review of factors affecting medication adherence among patients with osteoporosis. Osteoporos Int. 2018; 29(12):2623-37. [DOI:10.1007/s00198-018-4759-3] [PMID]
- Abbas H, Kurdi M, de Vries F, van Onzenoort HAW, Driessen JHM, Watfa M, et al. Factors associated with antihypertensive medication nonadherence: A cross-sectional study among Lebanese Hypertensive Adults. Patient Prefer Adherence. 2020; 14:663-73.[DOI: 10.2147/PPA.S238751] [PMID] [PMCID]
- Contreras-Vergara A, Sifuentes-Franco S, Haack S, Graciano-Machuca O, Rodriguez-Carrizalez AD, López-Contreras AK, et al. Impact of pharmaceutical education on medication adherence and its clinical efficacy in patients with type 2 diabetes and systemic arterial hypertension. Patient Prefer Adherence. 2022; 16:1999-2007.[DOI:10.2147/PPA.S370323] [PMID] [PMCID]
- Kassahun T, Gesesew H, Mwanri L, Eshetie T. Diabetes related knowledge, self-care behaviours and adherence to medications among diabetic patients in Southwest Ethiopia: A cross-sectional survey. BMC Endocr Disord. 2016; 16(1):28. [DOI:10.1186/s12902-016-0114-x] [PMID] [PMCID]
- Mekonnen HS, Gebrie MH, Eyasu KH, Gelagay AA. Drug adherence for antihypertensive medications and its determinants among adult hypertensive patients attending in chronic clinics of referral hospitals in Northwest Ethiopia. BMC Pharmacol Toxicol. 2017; 18(1):27. [PMID] [PMCID]
- Abebaw M, Messele A, Hailu M, Zewdu F. Adherence and associated factors towards antidiabetic medication among type II diabetic patients on follow-up at university of Gondar hospital, Northwest Ethiopia. Adv Nurs. 2016. [DOI:10.1155/2016/8579157]
- Kassahun A, Gashe F, Mulisa E, Rike WA. Nonadherence and factors affecting adherence of diabetic patients to anti-diabetic medication in Assela General Hospital, Oromia Region, Ethiopia. J Pharm Bioallied Sci. 2016; 8(2):124-9. [DOI:10.4103/0975-7406.171696] [PMID] [PMCID]
- Drusch S, Zureik M, Herr M. Potentially inappropriate medications and polypharmacy in the older population: A nationwide cross-sectional study in France in 2019. Therapies. 2023; 78(5):575-84. [DOI:10.1016/j.therap.2023.02.001] [PMID]
- Rochon PA, Petrovic M, Cherubini A, Onder G, O'Mahony D, Sternberg SA, et al. Polypharmacy, inappropriate prescribing, and deprescribing in older people: Through a sex and gender lens. Lancet Healthy Longev. 2021; 2(5):e290-300. [DOI:10.1016/S2666-7568(21)00054-4] [PMID]
Article Type : Research |
Subject:
General
Received: 2022/08/27 | Accepted: 2024/02/3 | Published: 2024/07/1
Received: 2022/08/27 | Accepted: 2024/02/3 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |