Fri, Jan 30, 2026
Volume 34, Issue 4 (9-2024)
JHNM 2024, 34(4): 365-375 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghashghaee N, Rezasoltani P, Nazari M, Kazemnezhad Leyli E. Comparison of Pregnancy-related Concerns, Perceived Social Support, and Anxiety Between Pregnant Mothers With and Without Participation in Antenatal Education Classes. JHNM 2024; 34 (4) :365-375
URL: http://hnmj.gums.ac.ir/article-1-2359-en.html
URL: http://hnmj.gums.ac.ir/article-1-2359-en.html
1- Midwifery (MSc), Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Assistant Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,rezasoltani@gums.ac.ir
3- Assistant Professor, Department of Midwifery, Zeyinab (P.B.U.H) School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
2- Assistant Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Assistant Professor, Department of Midwifery, Zeyinab (P.B.U.H) School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 494 kb]
(378 Downloads)
| Abstract (HTML) (963 Views)
Full-Text: (416 Views)
Introduction
During pregnancy, mothers may experience worries related to childbirth, child health, and their maternal role, which are considered anxiety symptoms during this stage of life [1, 2]. Additionally, a pregnant woman experiences a significant transformation in her physical state, such as weight gain [3, 4]. The challenges that pregnant women encounter can be divided into three domains: Concerns about childbirth and child health, concerns about weight/body image, and concerns about emotions/relationships [2, 5]. Pregnancy-related worries and concerns, along with fear of the future, are natural and somewhat inappropriate reactions to uncertainty and lived experience of personal relationships, individual roles, and daily affairs in various social situations [1, 6]. Pregnancy-related worries and concerns have been observed globally, with rates varying from 6.8% to about 60% [7-9]. Many factors are associated with pregnancy-related concerns, including age, occupation, income level, educational level, place of residence, number of pregnancies, history of stillbirth, history of abortion, history of childbirth, number of prenatal care visits, and perceived social support [10, 11]. The relationship between perceived social support and pregnancy-related concerns is of great importance [12].
Mothers’ concerns during pregnancy may accompany with adverse maternal and child health outcomes [9, 13]. Promoting the mothers’ awareness of pregnancy and childbirth events and their understanding of the impact of pregnancy-related concerns on maternal and fetal health can help them adapt to the physical and emotional changes during pregnancy which, in turn, can prepare them for having pleasant motherhood and childbirth experience and facilitate a stronger mother-baby bond [14, 15]. In this regard, one of the programs offered by the health care systems is the provision of free antenatal education classes (AEC), whose goal is to familiarize the parents with pregnancy knowledge and prepare them for childbirth and the postpartum period while ensuring a pleasant experience [16, 17]. In Iran, mother-friendly hospitals have offered the AEC interventions since 2008, conducted by trained midwives. The classes cover a wide range of topics, including the anatomical/physiological changes during pregnancy, nutrition, mental health, the spouse role, communication with the fetus, warning signs, labor planning, childbirth types and processes, postpartum care and breastfeeding, correction of pregnancy-related issues, musculoskeletal and breathing exercises, and relaxation techniques [16, 18].
Some studies have examined the efficacy of the AEC in reducing pregnancy-related concerns and have reported conflicting results [14, 18-20]. Najafi et al. found that the tendency to normal vaginal delivery among primigravida mothers significantly increased from 85.3% to 89.2% after attending the AEC courses [18]. Uslu Yuvaci et al. also observed that such classes may significantly reduce worries about childbirth; however, they did not affect concerns about the type of delivery [20]. This study aimed to compare the pregnancy-related concerns, perceived social support, and anxiety between pregnant mothers with and without participating in the AECs.
Materials and Methods
This is a comparative-analytical study that was conducted at a hospital belonged to the Iranian Social Welfare Organization and a governmental teaching hospital in Rasht, Iran, from August 2020 to May 2021. The sample size was determined 160 (80 per group) using the mean score of pregnancy-related concerns (45.96±5.59) reported in a previous study [2] and by considering 95% confidence level, a test power of 80%, a clinical difference of 50% of standard deviation, and a sample drop rate of 10%. The inclusion criteria were a singleton pregnancy, 20 weeks of gestational age, no history of chronic diseases and complications during the previous pregnancies, no history of stillbirth or abortion, not taking neuro-psychiatric drugs, no history of known diseases or abnormalities in the fetus, having a wanted pregnancy according to the couples, tendency to voluntarily attend the study, being familiar with the Persian language, and being literate enough to read and write. Exclusion criteria were any complications during the pregnancy, unwillingness to participate in any training sessions, and lack of cooperation during the study.
A total of 160 eligible pregnant mothers were recruited using a consecutive sampling method through individual interviews, 80 were put in the intervention group and 80 in the control group. The pregnant mothers in the intervention group were selected from among 89 mothers referred to one clinic of the Social Welfare Organization and received the AEC intervention during the given period. In this groups, seven mothers were excluded due to not meeting the inclusion criteria and two had gestational diabetes. The pregnant mothers in the control group were selected from among 101 mothers visited the prenatal clinic of a teaching hospital to receive routine prenatal care during the given period. In this group, 13 mothers were excluded due to not meeting the inclusion criteria, six had gestational diabetes, and two had gestational hypertension.
The instrument used in this study was a four-part questionnaire. The first part surveys the participants’ demographic and obstetric characteristics including age, educational level, occupation, spouse education, spouse occupation, income status, place of residence, housing situation, number of pregnancies, number of childbirths, type of previous delivery, number of children, previous childbirth experience, gender of the fetus, source of gained information related to pregnancy and childbirth, and number of prenatal care visits during the current pregnancy.
The second part was the prenatal distress questionnaire (PDQ). This measure was originally developed by Alderdice [5] and the psychometric evaluation of its Persian version has been conducted in Iran [2]. It has 12 items and three subscales: Concerns about birth and the baby (5 items), concerns about weight/body image (3 items), and concerns about emotions and relationships (4 items). The items are rated on a five-point Likert scale from 0 (not at all) to 4 (always). The total score ranges from 0 to 48, with higher scores indicating higher concerns.
The third part was the multidimensional scale of perceived social support (MSPSS), developed by Zimet et al. [21]. In this study, its Persian version was used [22]. The questionnaire has 12 items and three subscales: Support from family (4 items), support from friends (4 items), and support from a significant other (4 items). The items are rated on a five-point Likert scale from 1 (completely disagree) to 5 (completely agree). The total score ranges from 12 to 60. The higher score indicates a higher perceived social support. The fourth section was Spielberger’s state-trait anxiety inventory (STAI), which consists of 40 items (20 for state anxiety and 20 for trait anxiety) scored on a four-point scale from 1 to 4, having a total score of 20-80 [23]. This measure was localized by Mahram for Iranian samples [24]. We used items related to trait anxiety, rated as 1 (almost never), 2 (sometimes), 3 (often), and 4 (almost always), with higher scores indicating higher anxiety.
Upon entering the study at the 20th week of gestation, the demographic form, PDQ, MSPSS, and STAI were completed for both groups through face-to-face interviews. The PDQ was then completed again at the 37th week of gestation. While the classes were being held in the clinic a a part of a national program at eight face-to-face sessions from the 20th to 37th weeks of gestation, the timely and regular attendance of the intervention group was monitored by the researcher. Despite the COVID-19 pandemic at the time of the study, a trained midwife individually conducted the courses, considering the health protocols.
Descriptive statistics and Kolmogorov-Smirnov test, Independent t-test, chi-square and Fisher’s exact tests, Man-Whitney U test, and Wilcoxon signed-rank test were used for data analysis, followed by multivariate analysis of covariance (MANCOVA), analysis of covariance (ANCOVA), and multiple linear regression analysis using the general linear model (GLM). The obtained data were analyzed in SPSS software, version 26 (IBM Inc. USA). The significance level was set at 0.05.
Results
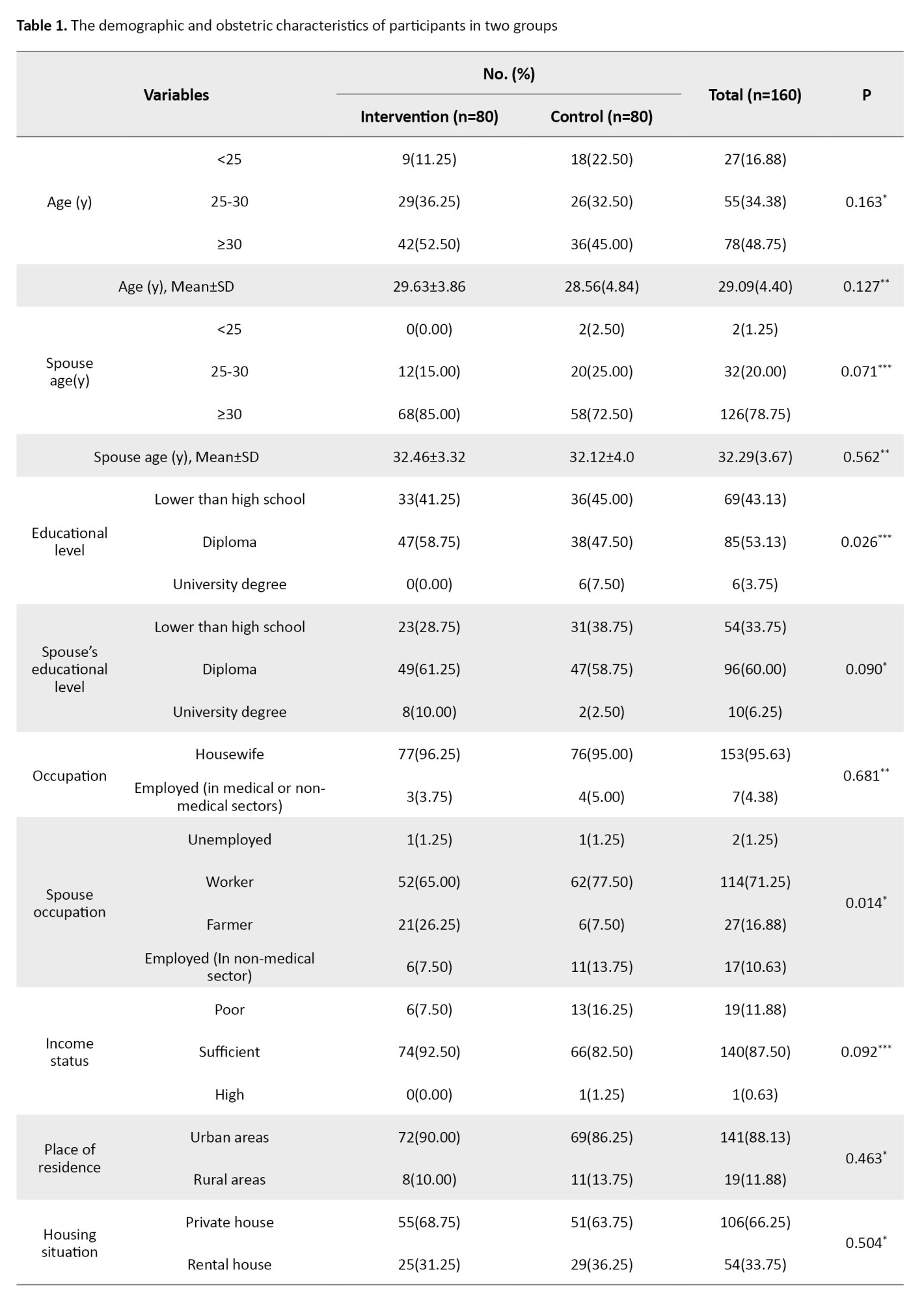
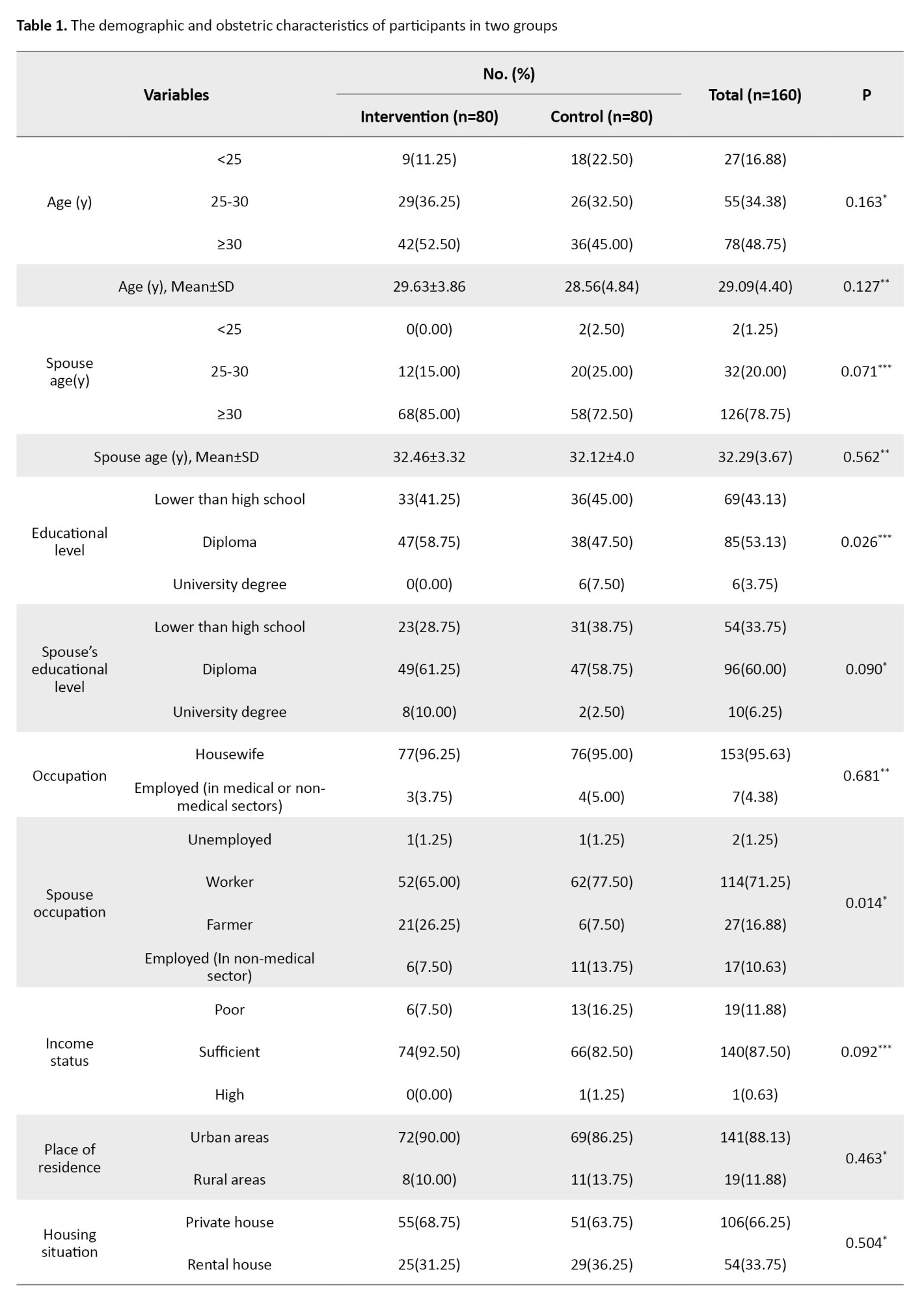
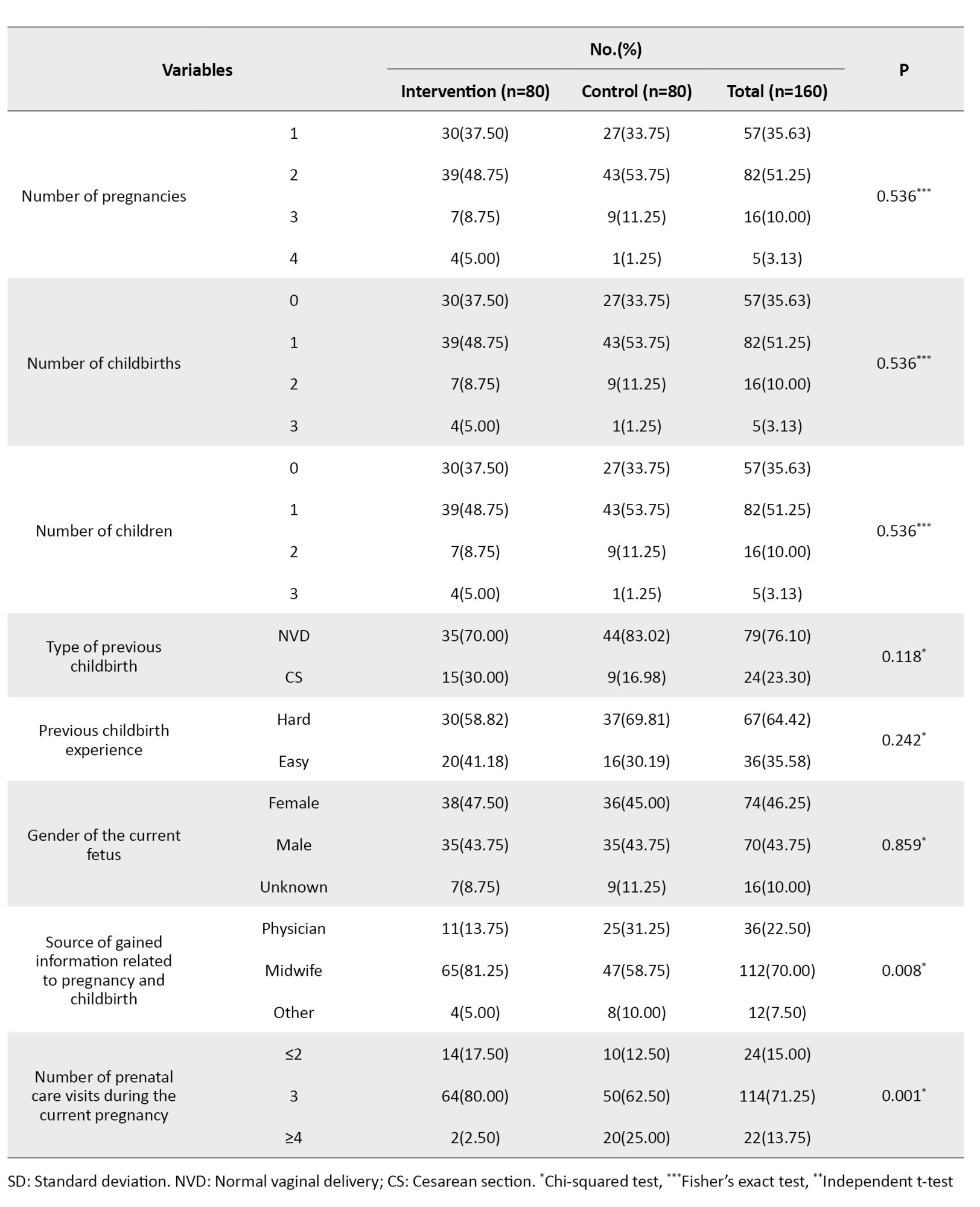
The participants’ demographic and obstetric characteristics are shown in Table 1.
According to the Mann-Whitney U test results, the two groups were not significantly different regarding the total and subscale scores of PDQ in the 20th week of gestation. Moreover, the total scores of MSPSS and friends support in the 20th week of gestation were significantly higher in the intervention group compared to the control group (P=0.044 and 0.046, respectively), according to the Mann-Whitney U test results. The two groups were not statistically different regarding family support and trait anxiety scores.
According to the Man-Whitney U test, in the 37th week of gestation, the median or interquartile range (IQR) of the total score of PDQ significantly reduced in the intervention group, compared to the control group (P=0.001). In addition, the intervention group showed significant decrease in PDQ domains of concerns about birth and the baby (P=0.045), weight/body image (P=0.001), and emotions and relationships (P=0.001).
In the within-group comparison, the Wilcoxon test results revealed the median of the total score of PDQ reduced significantly in the intervention group after attending the ACE course (P=0.001). Furthermore, in this group, the median of PDQ domains of concerns about birth and the baby (P=0.001), and concerns about emotions and relationships (P=0.001) significantly reduced after the end of course. However, the concerns about weight/body image in the intervention group showed no significant difference after the end of course. Similarly, the control group showed a significant decrease in the median of the total score of PDQ (P=0.001), and in its two domains of concerns about birth and the baby (P=0.006) and concerns about emotions and relationships (P=0.006).
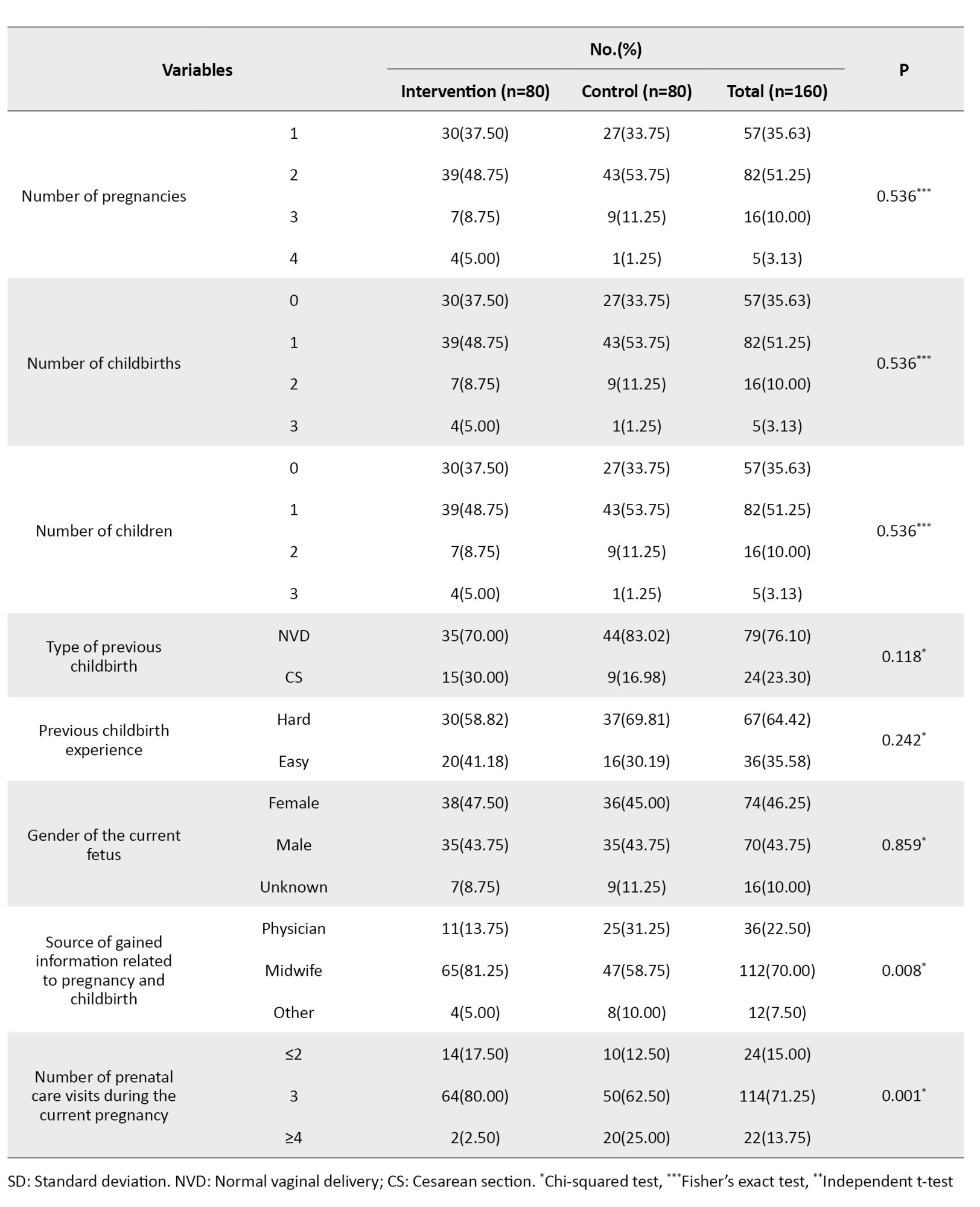
Table 2 compares the two study groups regarding pregnancy-related concerns in the 20th and 37th weeks of gestation after controlling covariates, using MANCOVA.
Participation in the ACE courses resulted in a significant decrease in concerns about birth and the baby (η2=0.036, P=0.018), weight/body image (η2=0.147, P=0.001), and emotions and relationships (η2=0.095, P=0.001) in the 37th week of gestation. As can be seen, participation in the ACE course had more effect on reducing pregnancy-related concerns about weight/body image compared to other concerns in the 37th week of gestation. The pregnancy-related concerns about birth and the baby were significantly different between the 20th and 37th weeks of gestation (η2=0.028, P=0.04). In addition, perceived social support from significant others was significantly related to pregnancy-related concerns about emotions and relationships in the 37th week of gestation (η2=0.041, P=0.012).
According to the ANCOVA results shown in Table 3, pregnancy-related concerns in the 37th week of gestation significantly different in terms of group (η2=0.142, P<0.001).
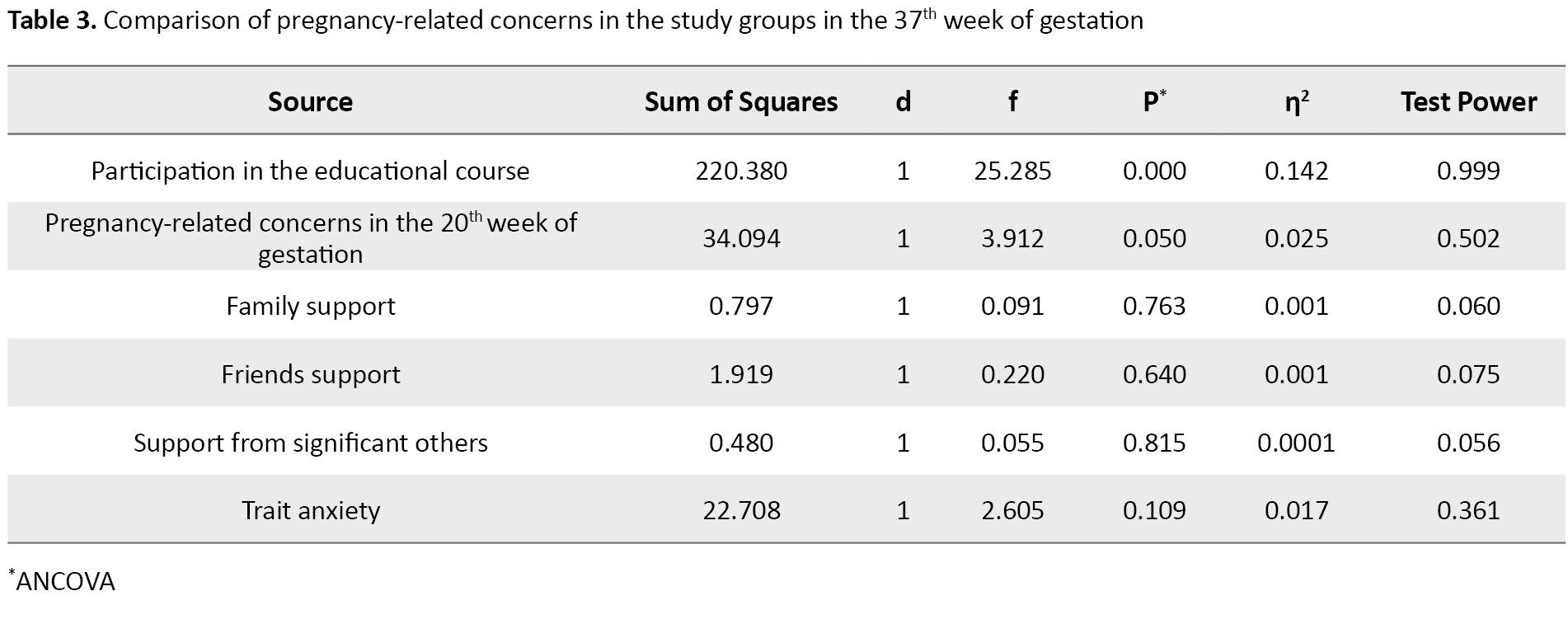
Table 4 shows the results of multiple linear regression analysis using the GLM method.
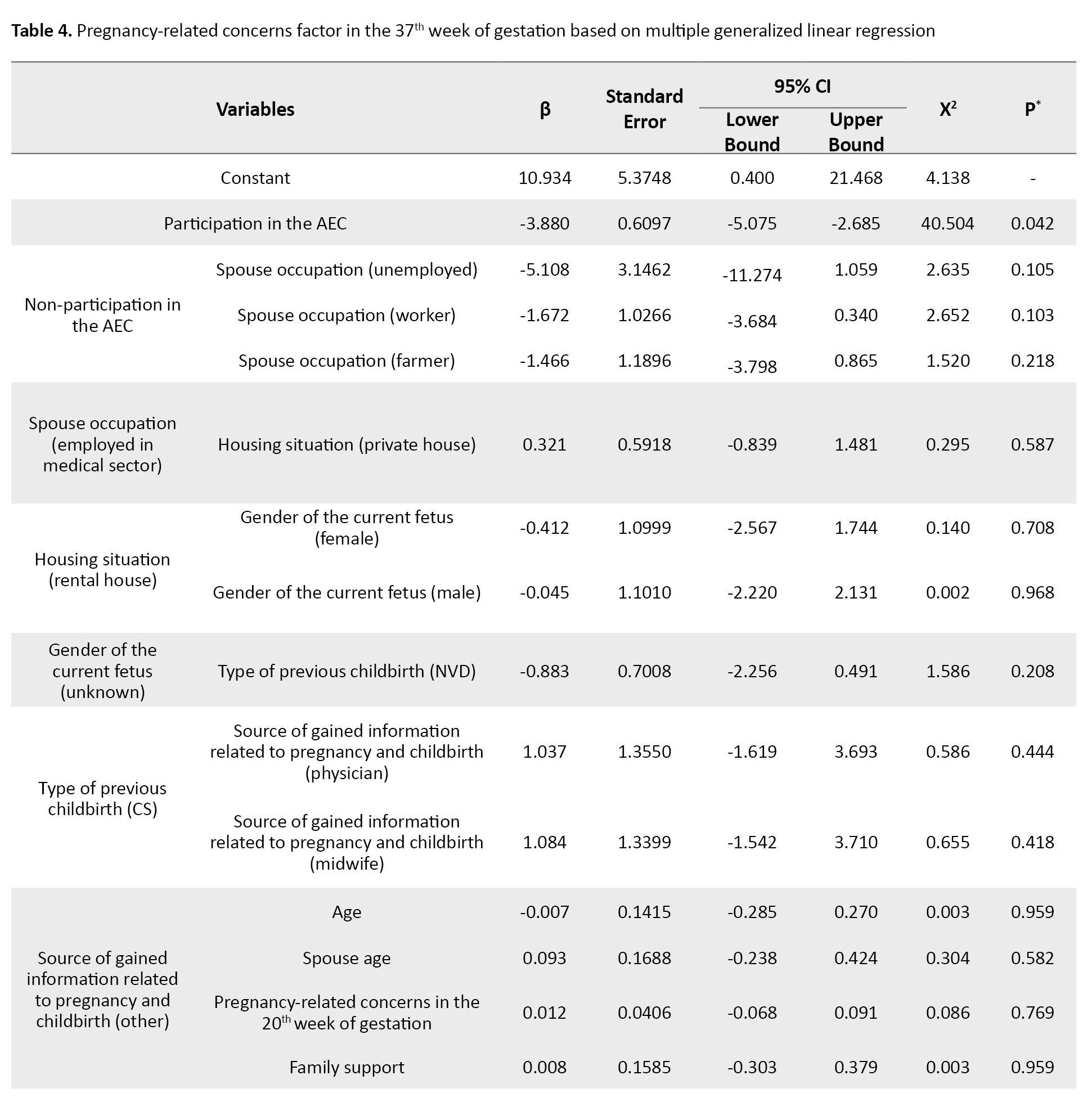
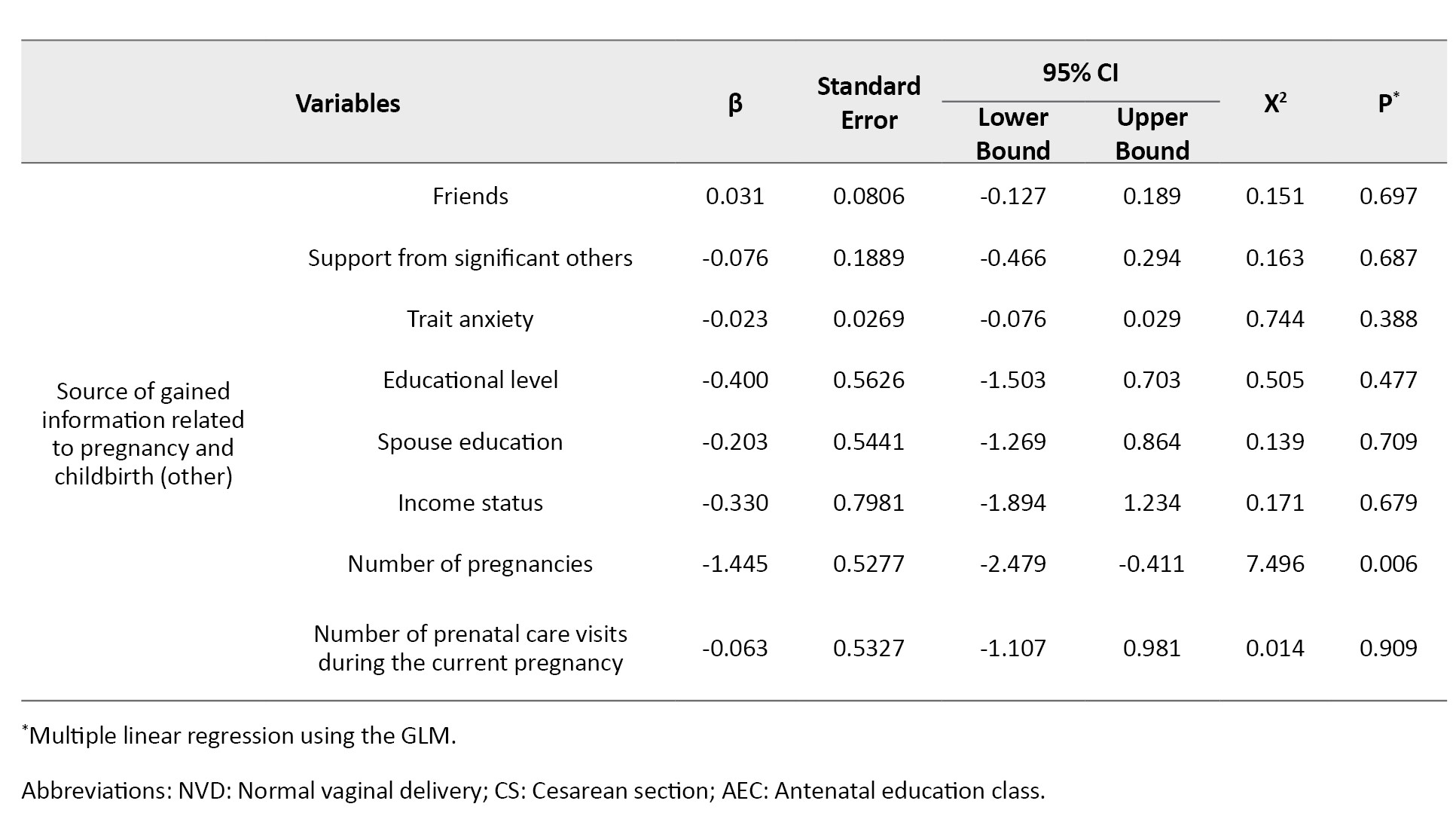
Accordingly, the participation in the educational course (β=-3.88, 95% CI; -5.075%, -2.685%, P=0.042) and the number of pregnancies (β=-1.44, 95% CI; -2.479%, -0.411%, P=0.006) were significant predictors of pregnancy-related concerns in the 37th week of gestation.
Discussion
The present study compared pregnancy-related concerns of the two groups of Iranian pregnant mothers with and without participation in the AEC interventions, using the PDQ. As expected, the intervention group had lower scores in the 37th week of gestation, indicating fewer pregnancy-related concerns after the AEC course. Uslu Yuvaci et al. found that the antepartum education significantly reduced concerns about childbirth in Turkish primigravida pregnant women; however, it could not reduce concerns about the type of delivery [20]. Similarly, we observed a significant decrease after attending the classes in the pregnancy-related concerns about birth and the baby, which included worries about childbirth and labor pain. Another study showed that problem-focused counseling could reduce pregnancy-related concerns about maternal and fetal health, childbirth, and family relationships; however, it could not help reduce the concerns about economic affairs [25]. A cohort study in Iran demonstrated that the fear of childbirth experienced during the third semester of gestation significantly declined among the participants of the AEC course. Consequently, this group showed higher tendency towards vaginal delivery [18]. We also found that attending the AEC intervention could reduce pregnancy-related concerns about birth and the baby. This indicates that the course could alleviate the mothers’ worries about childbirth and labor pain. Serçekuş et al. found no association difference in pregnant mothers’ fear of childbirth after antenatal education [19]. Conversely, we found a reduction in concerns about birth and the baby, including the fear of childbirth, after the educational course. Therefore, it seems necessary to conduct further research on the association between pregnancy-related concerns, fear of childbirth, and the selection of delivery type. On the other hand, it is important to consider the quality of antenatal education [26]. Another study in Turkey showed that providing education to pregnant mothers could enhanced their pregnancy acceptance and reduced their fear of childbirth [27]. This is consistent with our study regarding the fear of childbirth which is related to the concerns about birth and the baby. However, the mentioned study revealed an enhanced acceptance of pregnancy (related to concerns about birth and the baby) among those received education.
This study showed that the number of pregnancy was a predictor of pregnancy-related concerns. This is consistent with the results of Hassanzadeh et al. [28]. Additionally, our finding regarding the association of participation in the educational course during pregnancy and the reduction of concerns about birth and the baby, including fear of childbirth, is consistent with them. In the present study both groups of pregnant women with and without participating in the AEC intervention showed a notable decrease in concerns about childbirth and the baby and concerns about emotions and relationships from the 20th week to the 37th week. However, the concerns about weight/body image did not show any significant change in any groups over time.
This study had some limitations. First, the AEC was provided during the COVID-19 pandemic in a clinic using face-to-face method that can affect these classes. Another limitation was that the findings cannot be generalized to all pregnant women in the country. Accordingly, studies conducted in other cities and health centers using larger sample sizes are recommended to verify the results.
The pregnant mothers participated in the AEC courses experience fewer pregnancy-related concerns compared to the pregnant mothers with receiving the education. This suggest that AEC courses can provide an effective solution to address the pregnancy-related concerns, including concerns about birth and the baby, weight/body image, and emotions and relationships in pregnant mothers. Therefore, healthcare providers should encourage pregnant mothers to attend the AEC courses for having acceptable maternal and child health outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1399.232). The participants received information regarding the study objectives and were assured of the confidentiality of their participation and their right to leave the study at any time. All participants signed a written informed consent form.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Design: Najme Ghashghaee, Parvaneh Rezasoltani, and Mojgan Nazari; Data collection and analysis: Najme Ghashghaee, Parvaneh Rezasoltani, and Ehsan Kazemnezhad Leili. Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Vice Chancellor for Research and Technology of Guilan University of Medical Sciences, the staff at health centers, and all pregnant mothers who attended this study for their cooperation. We also thank Nazila Didevar, MSc in midwifery, for her assistance in this study.
References
During pregnancy, mothers may experience worries related to childbirth, child health, and their maternal role, which are considered anxiety symptoms during this stage of life [1, 2]. Additionally, a pregnant woman experiences a significant transformation in her physical state, such as weight gain [3, 4]. The challenges that pregnant women encounter can be divided into three domains: Concerns about childbirth and child health, concerns about weight/body image, and concerns about emotions/relationships [2, 5]. Pregnancy-related worries and concerns, along with fear of the future, are natural and somewhat inappropriate reactions to uncertainty and lived experience of personal relationships, individual roles, and daily affairs in various social situations [1, 6]. Pregnancy-related worries and concerns have been observed globally, with rates varying from 6.8% to about 60% [7-9]. Many factors are associated with pregnancy-related concerns, including age, occupation, income level, educational level, place of residence, number of pregnancies, history of stillbirth, history of abortion, history of childbirth, number of prenatal care visits, and perceived social support [10, 11]. The relationship between perceived social support and pregnancy-related concerns is of great importance [12].
Mothers’ concerns during pregnancy may accompany with adverse maternal and child health outcomes [9, 13]. Promoting the mothers’ awareness of pregnancy and childbirth events and their understanding of the impact of pregnancy-related concerns on maternal and fetal health can help them adapt to the physical and emotional changes during pregnancy which, in turn, can prepare them for having pleasant motherhood and childbirth experience and facilitate a stronger mother-baby bond [14, 15]. In this regard, one of the programs offered by the health care systems is the provision of free antenatal education classes (AEC), whose goal is to familiarize the parents with pregnancy knowledge and prepare them for childbirth and the postpartum period while ensuring a pleasant experience [16, 17]. In Iran, mother-friendly hospitals have offered the AEC interventions since 2008, conducted by trained midwives. The classes cover a wide range of topics, including the anatomical/physiological changes during pregnancy, nutrition, mental health, the spouse role, communication with the fetus, warning signs, labor planning, childbirth types and processes, postpartum care and breastfeeding, correction of pregnancy-related issues, musculoskeletal and breathing exercises, and relaxation techniques [16, 18].
Some studies have examined the efficacy of the AEC in reducing pregnancy-related concerns and have reported conflicting results [14, 18-20]. Najafi et al. found that the tendency to normal vaginal delivery among primigravida mothers significantly increased from 85.3% to 89.2% after attending the AEC courses [18]. Uslu Yuvaci et al. also observed that such classes may significantly reduce worries about childbirth; however, they did not affect concerns about the type of delivery [20]. This study aimed to compare the pregnancy-related concerns, perceived social support, and anxiety between pregnant mothers with and without participating in the AECs.
Materials and Methods
This is a comparative-analytical study that was conducted at a hospital belonged to the Iranian Social Welfare Organization and a governmental teaching hospital in Rasht, Iran, from August 2020 to May 2021. The sample size was determined 160 (80 per group) using the mean score of pregnancy-related concerns (45.96±5.59) reported in a previous study [2] and by considering 95% confidence level, a test power of 80%, a clinical difference of 50% of standard deviation, and a sample drop rate of 10%. The inclusion criteria were a singleton pregnancy, 20 weeks of gestational age, no history of chronic diseases and complications during the previous pregnancies, no history of stillbirth or abortion, not taking neuro-psychiatric drugs, no history of known diseases or abnormalities in the fetus, having a wanted pregnancy according to the couples, tendency to voluntarily attend the study, being familiar with the Persian language, and being literate enough to read and write. Exclusion criteria were any complications during the pregnancy, unwillingness to participate in any training sessions, and lack of cooperation during the study.
A total of 160 eligible pregnant mothers were recruited using a consecutive sampling method through individual interviews, 80 were put in the intervention group and 80 in the control group. The pregnant mothers in the intervention group were selected from among 89 mothers referred to one clinic of the Social Welfare Organization and received the AEC intervention during the given period. In this groups, seven mothers were excluded due to not meeting the inclusion criteria and two had gestational diabetes. The pregnant mothers in the control group were selected from among 101 mothers visited the prenatal clinic of a teaching hospital to receive routine prenatal care during the given period. In this group, 13 mothers were excluded due to not meeting the inclusion criteria, six had gestational diabetes, and two had gestational hypertension.
The instrument used in this study was a four-part questionnaire. The first part surveys the participants’ demographic and obstetric characteristics including age, educational level, occupation, spouse education, spouse occupation, income status, place of residence, housing situation, number of pregnancies, number of childbirths, type of previous delivery, number of children, previous childbirth experience, gender of the fetus, source of gained information related to pregnancy and childbirth, and number of prenatal care visits during the current pregnancy.
The second part was the prenatal distress questionnaire (PDQ). This measure was originally developed by Alderdice [5] and the psychometric evaluation of its Persian version has been conducted in Iran [2]. It has 12 items and three subscales: Concerns about birth and the baby (5 items), concerns about weight/body image (3 items), and concerns about emotions and relationships (4 items). The items are rated on a five-point Likert scale from 0 (not at all) to 4 (always). The total score ranges from 0 to 48, with higher scores indicating higher concerns.
The third part was the multidimensional scale of perceived social support (MSPSS), developed by Zimet et al. [21]. In this study, its Persian version was used [22]. The questionnaire has 12 items and three subscales: Support from family (4 items), support from friends (4 items), and support from a significant other (4 items). The items are rated on a five-point Likert scale from 1 (completely disagree) to 5 (completely agree). The total score ranges from 12 to 60. The higher score indicates a higher perceived social support. The fourth section was Spielberger’s state-trait anxiety inventory (STAI), which consists of 40 items (20 for state anxiety and 20 for trait anxiety) scored on a four-point scale from 1 to 4, having a total score of 20-80 [23]. This measure was localized by Mahram for Iranian samples [24]. We used items related to trait anxiety, rated as 1 (almost never), 2 (sometimes), 3 (often), and 4 (almost always), with higher scores indicating higher anxiety.
Upon entering the study at the 20th week of gestation, the demographic form, PDQ, MSPSS, and STAI were completed for both groups through face-to-face interviews. The PDQ was then completed again at the 37th week of gestation. While the classes were being held in the clinic a a part of a national program at eight face-to-face sessions from the 20th to 37th weeks of gestation, the timely and regular attendance of the intervention group was monitored by the researcher. Despite the COVID-19 pandemic at the time of the study, a trained midwife individually conducted the courses, considering the health protocols.
Descriptive statistics and Kolmogorov-Smirnov test, Independent t-test, chi-square and Fisher’s exact tests, Man-Whitney U test, and Wilcoxon signed-rank test were used for data analysis, followed by multivariate analysis of covariance (MANCOVA), analysis of covariance (ANCOVA), and multiple linear regression analysis using the general linear model (GLM). The obtained data were analyzed in SPSS software, version 26 (IBM Inc. USA). The significance level was set at 0.05.
Results
The participants’ demographic and obstetric characteristics are shown in Table 1.
According to the Mann-Whitney U test results, the two groups were not significantly different regarding the total and subscale scores of PDQ in the 20th week of gestation. Moreover, the total scores of MSPSS and friends support in the 20th week of gestation were significantly higher in the intervention group compared to the control group (P=0.044 and 0.046, respectively), according to the Mann-Whitney U test results. The two groups were not statistically different regarding family support and trait anxiety scores.
According to the Man-Whitney U test, in the 37th week of gestation, the median or interquartile range (IQR) of the total score of PDQ significantly reduced in the intervention group, compared to the control group (P=0.001). In addition, the intervention group showed significant decrease in PDQ domains of concerns about birth and the baby (P=0.045), weight/body image (P=0.001), and emotions and relationships (P=0.001).
In the within-group comparison, the Wilcoxon test results revealed the median of the total score of PDQ reduced significantly in the intervention group after attending the ACE course (P=0.001). Furthermore, in this group, the median of PDQ domains of concerns about birth and the baby (P=0.001), and concerns about emotions and relationships (P=0.001) significantly reduced after the end of course. However, the concerns about weight/body image in the intervention group showed no significant difference after the end of course. Similarly, the control group showed a significant decrease in the median of the total score of PDQ (P=0.001), and in its two domains of concerns about birth and the baby (P=0.006) and concerns about emotions and relationships (P=0.006).
Table 2 compares the two study groups regarding pregnancy-related concerns in the 20th and 37th weeks of gestation after controlling covariates, using MANCOVA.
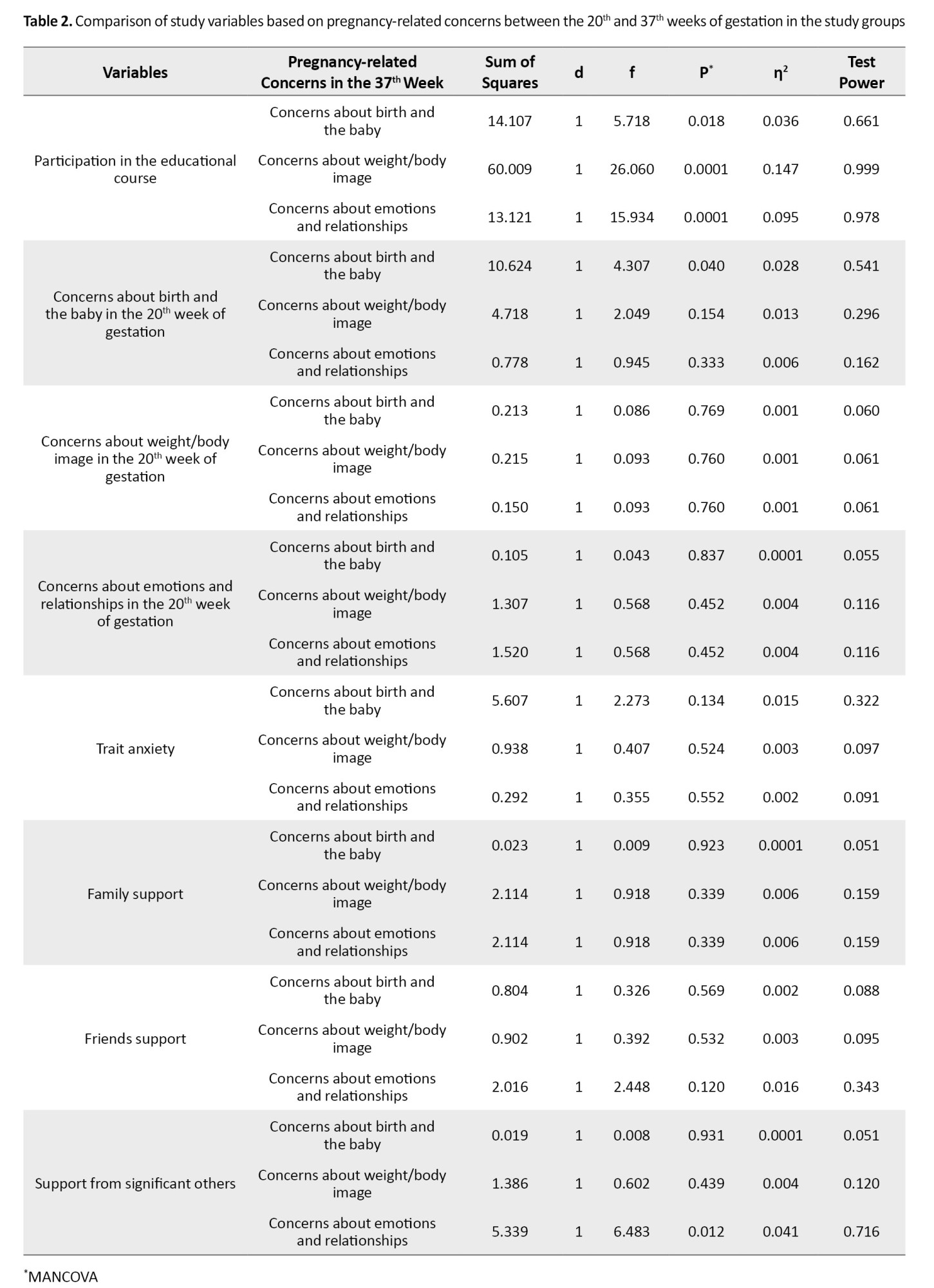
Participation in the ACE courses resulted in a significant decrease in concerns about birth and the baby (η2=0.036, P=0.018), weight/body image (η2=0.147, P=0.001), and emotions and relationships (η2=0.095, P=0.001) in the 37th week of gestation. As can be seen, participation in the ACE course had more effect on reducing pregnancy-related concerns about weight/body image compared to other concerns in the 37th week of gestation. The pregnancy-related concerns about birth and the baby were significantly different between the 20th and 37th weeks of gestation (η2=0.028, P=0.04). In addition, perceived social support from significant others was significantly related to pregnancy-related concerns about emotions and relationships in the 37th week of gestation (η2=0.041, P=0.012).
According to the ANCOVA results shown in Table 3, pregnancy-related concerns in the 37th week of gestation significantly different in terms of group (η2=0.142, P<0.001).
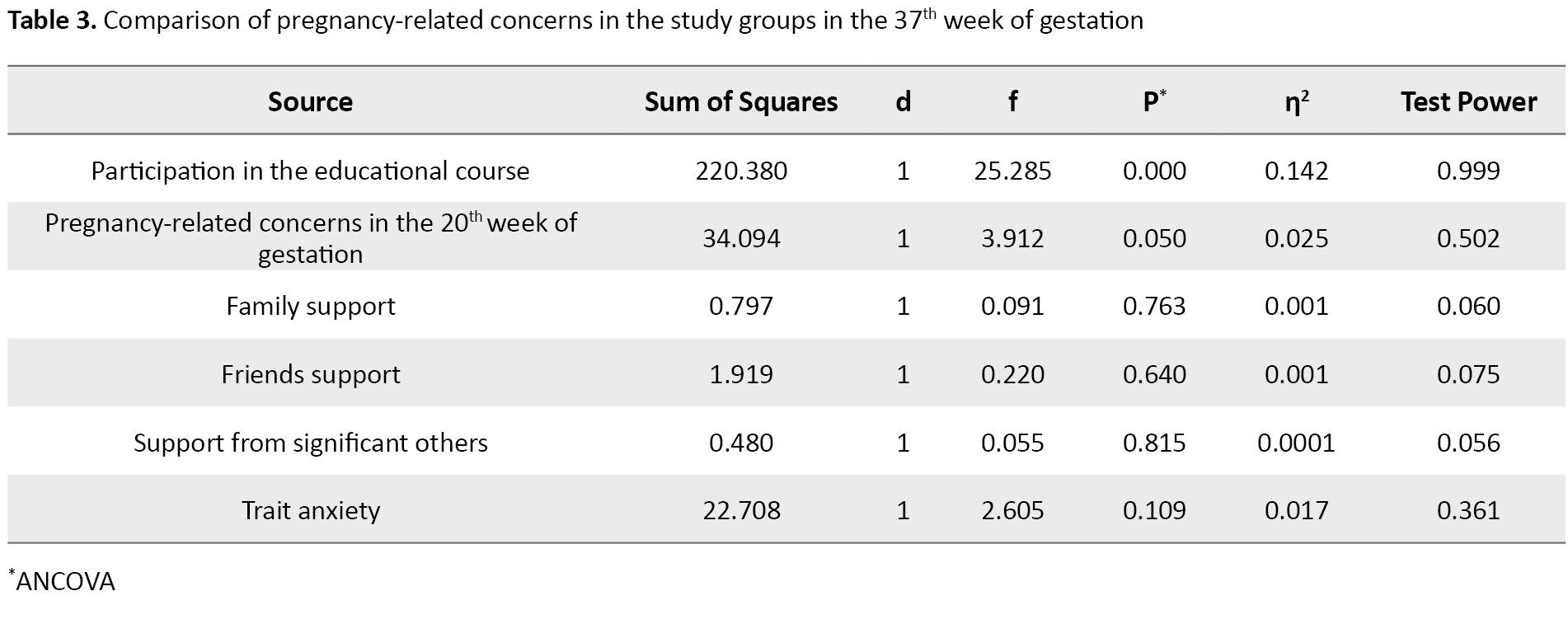
Table 4 shows the results of multiple linear regression analysis using the GLM method.
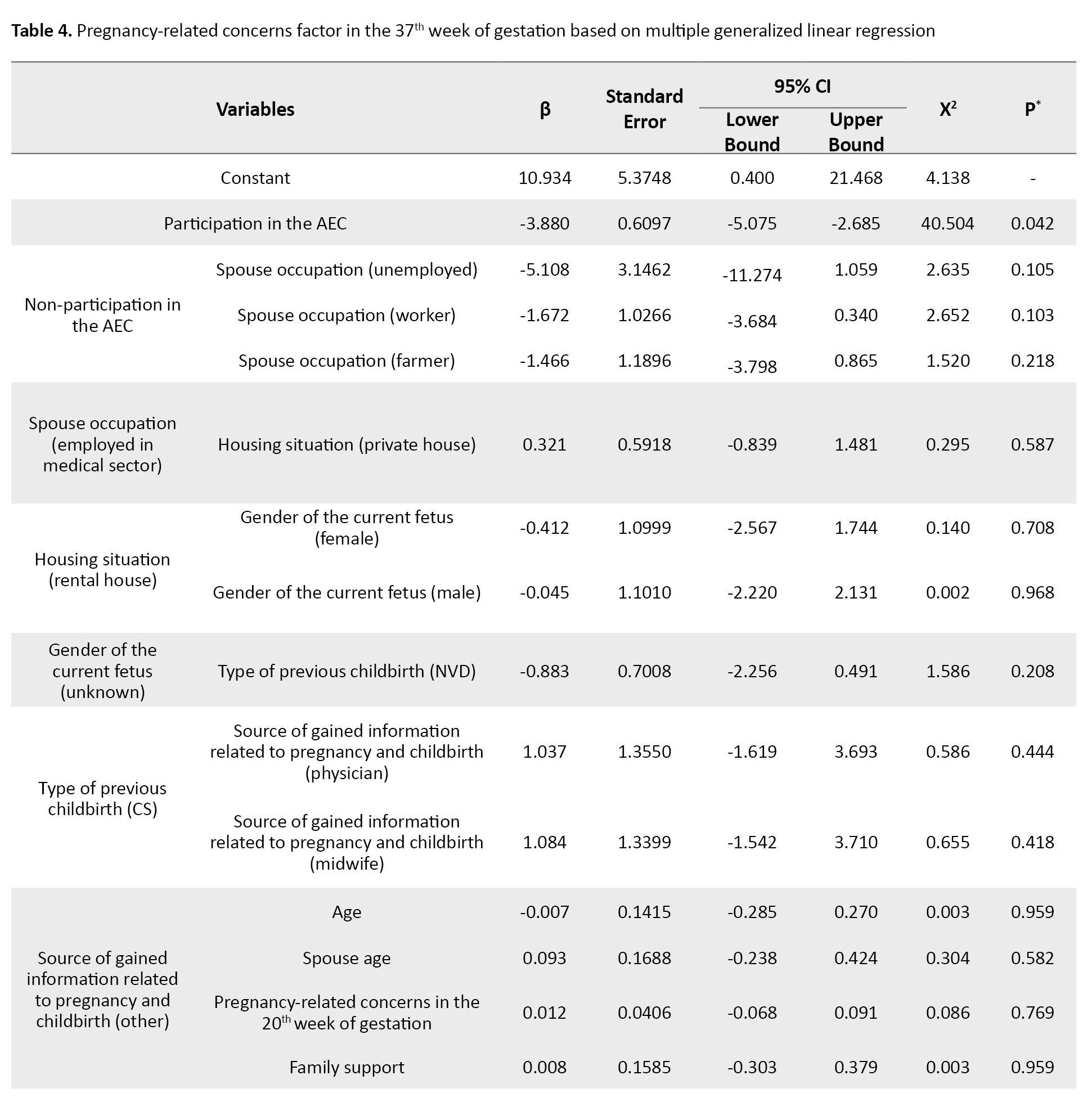
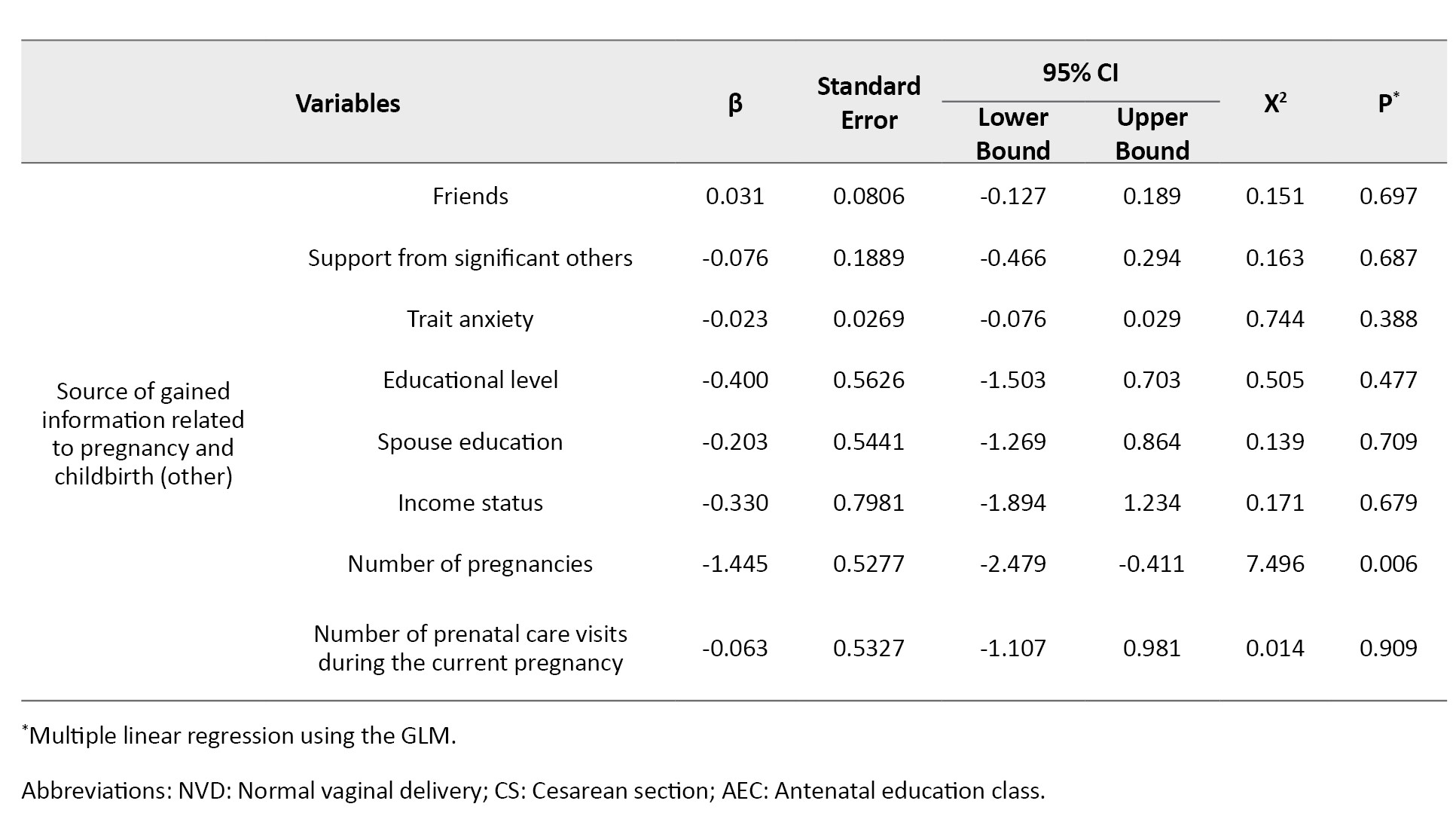
Accordingly, the participation in the educational course (β=-3.88, 95% CI; -5.075%, -2.685%, P=0.042) and the number of pregnancies (β=-1.44, 95% CI; -2.479%, -0.411%, P=0.006) were significant predictors of pregnancy-related concerns in the 37th week of gestation.
Discussion
The present study compared pregnancy-related concerns of the two groups of Iranian pregnant mothers with and without participation in the AEC interventions, using the PDQ. As expected, the intervention group had lower scores in the 37th week of gestation, indicating fewer pregnancy-related concerns after the AEC course. Uslu Yuvaci et al. found that the antepartum education significantly reduced concerns about childbirth in Turkish primigravida pregnant women; however, it could not reduce concerns about the type of delivery [20]. Similarly, we observed a significant decrease after attending the classes in the pregnancy-related concerns about birth and the baby, which included worries about childbirth and labor pain. Another study showed that problem-focused counseling could reduce pregnancy-related concerns about maternal and fetal health, childbirth, and family relationships; however, it could not help reduce the concerns about economic affairs [25]. A cohort study in Iran demonstrated that the fear of childbirth experienced during the third semester of gestation significantly declined among the participants of the AEC course. Consequently, this group showed higher tendency towards vaginal delivery [18]. We also found that attending the AEC intervention could reduce pregnancy-related concerns about birth and the baby. This indicates that the course could alleviate the mothers’ worries about childbirth and labor pain. Serçekuş et al. found no association difference in pregnant mothers’ fear of childbirth after antenatal education [19]. Conversely, we found a reduction in concerns about birth and the baby, including the fear of childbirth, after the educational course. Therefore, it seems necessary to conduct further research on the association between pregnancy-related concerns, fear of childbirth, and the selection of delivery type. On the other hand, it is important to consider the quality of antenatal education [26]. Another study in Turkey showed that providing education to pregnant mothers could enhanced their pregnancy acceptance and reduced their fear of childbirth [27]. This is consistent with our study regarding the fear of childbirth which is related to the concerns about birth and the baby. However, the mentioned study revealed an enhanced acceptance of pregnancy (related to concerns about birth and the baby) among those received education.
This study showed that the number of pregnancy was a predictor of pregnancy-related concerns. This is consistent with the results of Hassanzadeh et al. [28]. Additionally, our finding regarding the association of participation in the educational course during pregnancy and the reduction of concerns about birth and the baby, including fear of childbirth, is consistent with them. In the present study both groups of pregnant women with and without participating in the AEC intervention showed a notable decrease in concerns about childbirth and the baby and concerns about emotions and relationships from the 20th week to the 37th week. However, the concerns about weight/body image did not show any significant change in any groups over time.
This study had some limitations. First, the AEC was provided during the COVID-19 pandemic in a clinic using face-to-face method that can affect these classes. Another limitation was that the findings cannot be generalized to all pregnant women in the country. Accordingly, studies conducted in other cities and health centers using larger sample sizes are recommended to verify the results.
The pregnant mothers participated in the AEC courses experience fewer pregnancy-related concerns compared to the pregnant mothers with receiving the education. This suggest that AEC courses can provide an effective solution to address the pregnancy-related concerns, including concerns about birth and the baby, weight/body image, and emotions and relationships in pregnant mothers. Therefore, healthcare providers should encourage pregnant mothers to attend the AEC courses for having acceptable maternal and child health outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1399.232). The participants received information regarding the study objectives and were assured of the confidentiality of their participation and their right to leave the study at any time. All participants signed a written informed consent form.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Design: Najme Ghashghaee, Parvaneh Rezasoltani, and Mojgan Nazari; Data collection and analysis: Najme Ghashghaee, Parvaneh Rezasoltani, and Ehsan Kazemnezhad Leili. Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Vice Chancellor for Research and Technology of Guilan University of Medical Sciences, the staff at health centers, and all pregnant mothers who attended this study for their cooperation. We also thank Nazila Didevar, MSc in midwifery, for her assistance in this study.
References
- Newman MG, Llera SJ, Erickson TM, Przeworski A, Castonguay LG. Worry and generalized anxiety disorder: A review and theoretical synthesis of evidence on nature, etiology, mechanisms, and treatment. Annu Rev Clin Psychol. 2013; 9:275-97. [DOI:10.1146/annurev-clinpsy-050212-185544] [PMID]
- Yousefi R. [Psychometric properties of Persian version of prenatal distress questionnaire (PDQ) (Persian)]. Nurs Midwifery J. 2015; 13(3):215-25. [Link]
- Crossland AE, Munns L, Kirk E, Preston CEJ. Comparing body image dissatisfaction between pregnant women and non-pregnant women: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2023; 23(1):709. [DOI:10.1186/s12884-023-05930-w] [PMID]
- Escañuela Sánchez T, Meaney S, O'Connor C, Linehan L, O'Donoghue K, Byrne M, et al. Facilitators and barriers influencing weight management behaviours during pregnancy: A meta-synthesis of qualitative research. BMC Pregnancy Childbirth. 2022; 22(1):682. [DOI:10.1186/s12884-022-04929-z] [PMID]
- Alderdice F, Lynn F. Factor structure of the Prenatal Distress Questionnaire. Midwifery. 2011; 27(4):553-9. [DOI:10.1016/j.midw.2010.05.003] [PMID]
- Brunton R, Simpson N, Dryer R. Pregnancy-related anxiety, perceived parental self-efficacy and the influence of parity and age. Int J Environ Res Public Health. 2020; 17(18):6709. [DOI:10.3390/ijerph17186709] [PMID]
- Gourounti K, Anagnostopoulos F, Lykeridou K. Coping strategies as psychological risk factor for antenatal anxiety, worries, and depression among Greek women. Arch Womens Ment Health. 2013; 16(5):353-61. [DOI:10.1007/s00737-013-0338-y] [PMID]
- Malakouti J, Mirghafourvand M, Salehi Pour Mehr H, Shamsaei F, Safari Komeil M. [Maternal worries and their relationship with coping strategies in pregnant women referring to health centers in Hamadan (Persian)]. J Hayat. 2018; 24(1):35-47. [Link]
- Akinsulore A, Temidayo AM, Oloniniyi IO, Olalekan BO, Yetunde OB. Pregnancy-related anxiety symptoms and associated factors amongst pregnant women attending a tertiary hospital in south-west Nigeria. S Afr J Psychiatr. 2021; 27:1616. [DOI:10.4102/sajpsychiatry.v27i0.1616]
- Chen J, Huang J, Ooi S, Lin L, Chen C, Liu Y, et al. Effect of flexible patterns of health education on enhancing the compliance of pregnant women from Tibet, China. Medicine (Baltimore). 2020; 99(1):e18447. [DOI:10.1097/MD.0000000000018447]
- Kabukcu C, Sert C, Gunes C, Akyol HH, Tipirdamaz M. Predictors of prenatal distress and fear of childbirth among nulliparous and parous women. Niger J Clin Pract. 2019; 22(12):1635-43. [DOI:10.4103/njcp.njcp_613_18]
- Bedaso A, Adams J, Peng W, Sibbritt D. The relationship between social support and mental health problems during pregnancy: A systematic review and meta-analysis. Reprod Health. 2021; 18(1):162. [DOI:10.1186/s12978-021-01209-5]
- Mortazavi F, Akaberi A. Worries of pregnant women: Testing the Farsi Cambridge worry scale. Scientifica (Cairo). 2016; 2016:5791560. [DOI:10.1155/2016/5791560] [PMID]
- Gandomi N, Sharifzadeh G, Torshizi M, Norozi E. The effect of educational intervention based on self-efficacy theory on pregnancy anxiety and childbirth outcomes among Iranian primiparous women. J Educ Health Promot. 2022; 11(1):14. [DOI:10.4103/jehp.jehp_1548_20]
- Kashiha M, Hosseini J, Samadaee Gelehkolaee K. Mothers’ perceptions about childbirth preparation classes: A qualitative study. Int J Community Based Nurs Midwifery. 2023; 11(4):278-86. [PMID]
- Hadjigeorgiou E, Frangou M, Koliandri Y, Christofi MD, Middleton N. Description of the culture of childbirth and parenting classes in Cyprus: An ethnographic approach. Eur J Midwifery. 2024; 8. [DOI:10.18332/ejm/186665] [PMID]
- Moghasemi S, Vedadhir A, Simbar M. Models for providing midwifery care and its challenges in the context of Iran. J Holistic NursMidwifery. 2018; 28(1):64-74. [DOI:10.18869/acadpub.hnmj.28.1.64]
- Najafi F, Abouzari-Gazafroodi K, Jafarzadeh-Kenarsari F, Rahnama P, Gholami Chaboki B. [Relationship between attendance at childbirth preparation classes and fear of childbirth and type of delivery (Persian)]. Hayat. 2016; 21(4):30-40.
- Serçekuş P, Mete S. Turkish women’s perceptions of antenatal education. Int Nurs Rev. 2010; 57(3):395-401. [DOI:10.1111/j.1466-7657.2009.00799.x]
- Uslu Yuvaci H, Cinar N, Yalnizoglu Caka S, Topal S, Peksen S, Saglam N, et al. Effects of antepartum education on worries about labor and mode of delivery. J Psychosom Obstet Gynecol. 2021; 42(3):228-34. [DOI:10.1080/0167482X.2020.1725465]
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional scale of perceived social support. J Pers Assess. 1988; 52(1):30-41. [DOI:10.1207/s15327752jpa5201_2]
- Rajabi G. [The study of psychometric properties of the multidimensional scale perceived social support (Persian)]. Int J Behav Sci. 2012; 5(4):357-64. [Link]
- Spielberger CD. Manual for the State-Trait-Anxiety Inventory: STAI (form Y). Palo Alto, CA: Consulting Psychologists Press; 1983. [Link]
- Mahram B. Standardization of Spielberger’s test anxiety inventory in Mashhad [MA thesis]. Mashad: Ferdousi University; 1993. [Link]
- Karrabi R, Farjamfar M, Mortazavi F, Nazari A M, Goli S. [The effect of solution-focused group counseling on pregnant women’s worries: A randomized clinical trial (Persian)]. J Hayat. 2019; 25(1):81-94. [Link]
- Anis W, Amalia RB, Dewi ER. Do mothers who meet the minimum standard of antenatal visits have better knowledge? A study from Indonesia. J Educ Health Promot. 2022; 11(1):134. [DOI:10.4103/jehp.jehp_671_21]
- Karabulut Ö, Coşkuner Potur D, Doğan Merih Y, Cebeci Mutlu S, Demirci N. Does antenatal education reduce fear of childbirth? Int Nurs Rev. 2016; 63(1):60-7. [DOI:10.1111/inr.12223]
- Hasanzadeh R, Abbas-Alizadeh F, Meedya S, Mohammad-Alizadeh-Charandabi S, Mirghafourvand M. Assessment of childbirth preparation classes: A parallel convergent mixed study. Reprod Health. 2019; 16:160. [DOI:10.1186/s12978-019-0826-2]
Article Type : Research |
Subject:
Special
Received: 2024/05/16 | Accepted: 2024/06/11 | Published: 2024/10/1
Received: 2024/05/16 | Accepted: 2024/06/11 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |