Tue, Feb 3, 2026
Volume 35, Issue 2 (3-2025)
JHNM 2025, 35(2): 133-140 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aram M, Rezaie-Chamani S, Bostani Khalesi Z, Maroufizadeh S. Effect of Mobile-based Breastfeeding Education on Breastfeeding Experience of Mothers: A Quasi-Experimental Study. JHNM 2025; 35 (2) :133-140
URL: http://hnmj.gums.ac.ir/article-1-2341-en.html
URL: http://hnmj.gums.ac.ir/article-1-2341-en.html
1- Midwifery (MSc), Department of Reproductive Health, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,sedigherezaie65@yahoo.com
3- Associate Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Associate Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 593 kb]
(390 Downloads)
| Abstract (HTML) (739 Views)
Full-Text: (345 Views)
Introduction
Breastfeeding has proven benefits for the health of mothers and babies [1]. One of the goals of the World Health Organization (WHO) is to reach 70% exclusive breastfeeding at 6 months by 2030 [2]. Currently, the exclusive breastfeeding rate is 44% globally and 49% in Iran [3, 4]. One of the factors affecting the early discontinuation of breastfeeding is the negative breastfeeding experience caused by factors such as breast-related problems, breastfeeding difficulties, infant-related difficulties and social concerns [5]. Breastfeeding difficulties are common among mothers. However, the severity of these difficulties may vary [6]. It can lead to negative consequences such as early cessation of breastfeeding, reduced frequency and duration of breastfeeding, decreased breastfeeding self-efficacy, and increased risk of postpartum anxiety and depression [7, 8].
Based on previous studies, the increase of knowledge and skills of mothers in solving breastfeeding difficulties through education can help them deal with the negative breastfeeding experience and its consequences [9, 10]. Traditional teaching methods can be challenging due to various barriers, such as mothers’ lack of physical and mental preparation, limited opportunities to learn due to short hospital stays, busy schedules of health workers, the need to attend training at specific times and places and limited access to educational materials. These barriers can make it difficult for mothers to receive adequate and effective education [11, 12]. Health professionals use mobile health (mHealth) services to remove learning barriers, provide medical and health services, manage and monitor patients, make clinical decisions, and educate patients [13, 14]. The WHO has recommended using mobile applications for education as a comprehensive educational method for the health system [15]. Mobile applications eliminate time and place limitations in education, reduce costs, make education accessible to everyone, and facilitate understanding of educational content [16, 17]. Despite the actions of the Iranian Ministry of Health and Medical Education to promote the exclusive breastfeeding rate, it is still less than the desired level [3]. This study aimed to determine the effect of mobile-based breastfeeding education on the breastfeeding experience of nursing mothers in north of Iran.
Material and Methods
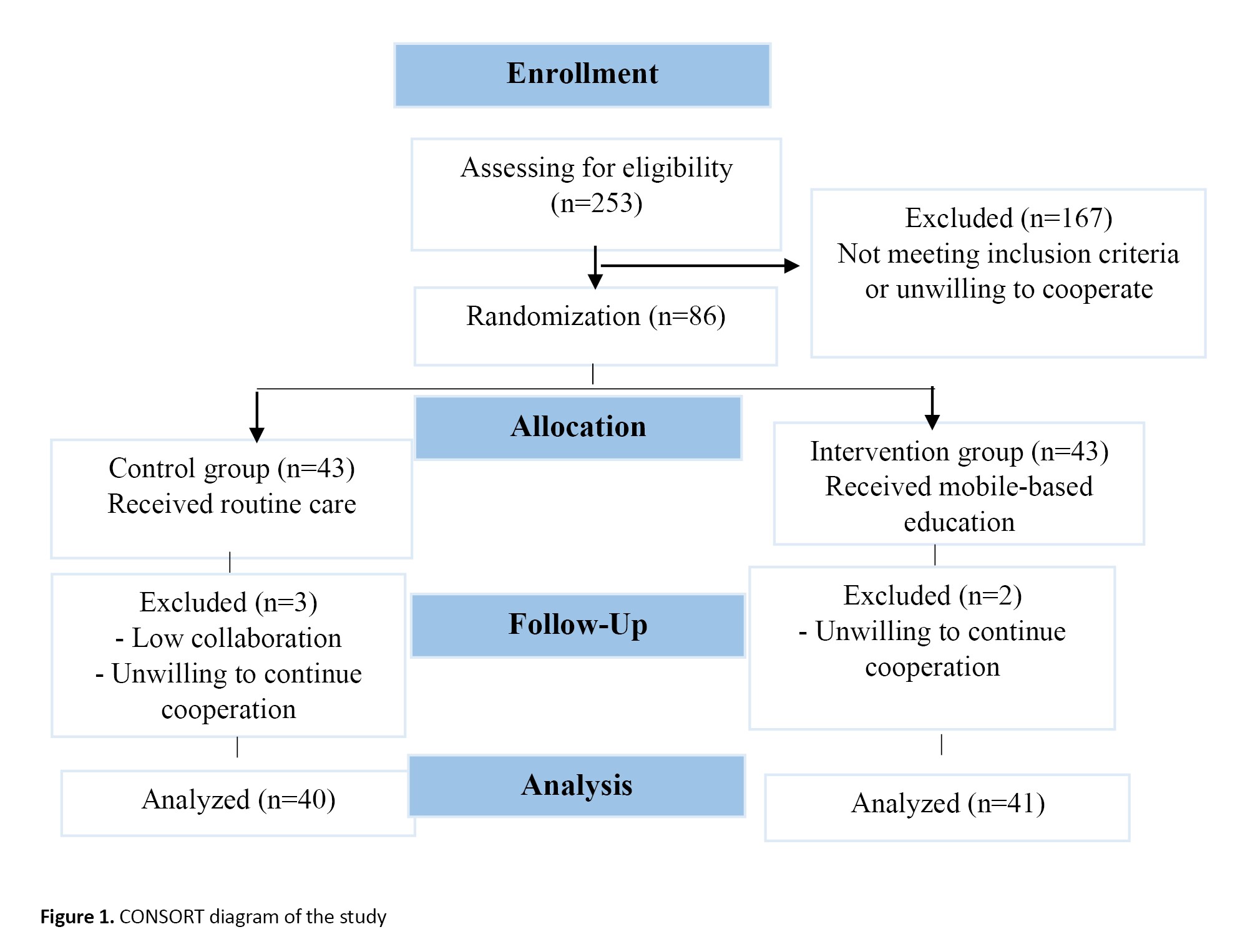
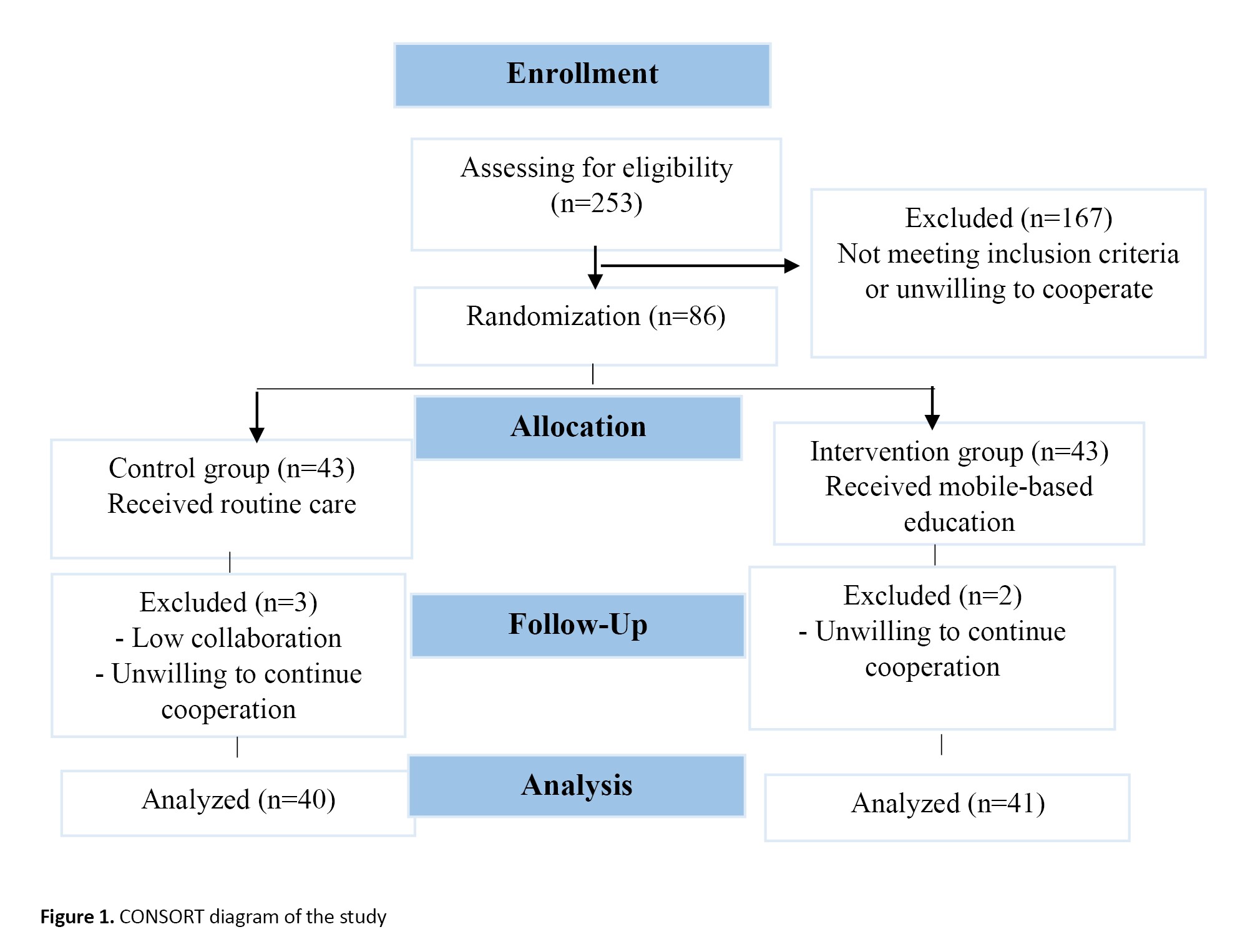
This is a quasi-experimental study. The participants were 81 nursing mothers referred to comprehensive health centers in Rasht, Iran, who were selected using a multi-stage cluster random sampling method from 8 centers (two centers from each region). The inclusion criteria were 3-5 days after giving birth, the ability to read and write, being primiparous, practicing either exclusive breastfeeding or mixed feeding (combination of breastfeeding and bottle feeding), no medical contraindications for breastfeeding such as HIV and human T-cell lymphotropic virus infections, no active tuberculosis, no breast herpes, no galactosemia and phenylketonuria in newborns, and no use of illegal drugs during breastfeeding (based on the health records), having a mobile phone with an Android system, ability to install mobile applications, having healthy and full-term infants, and singleton birth. Exclusion criteria were prescription of infant formula by a physician, unwillingness to continue participation in the study and not using the mobile application at least once a week. The sample size was determined as 34 per group by considering α=0.05, β=0.2, test power=0.8 and an effect size (d)=0.7 according to the expectations of practical difference. By considering a 20% possible sample dropout, it increased to 43 per group (total sample size=86). The participants were allocated to two groups of control and intervention using the block randomization method. A random sequence generation software was employed to facilitate the randomization [18]. In this study, 253 women met the inclusion criteria that 167 of whom did not meet the inclusion criteria or did not participate in the study despite meeting the inclusion criteria. In the block randomization process, 86 units were evenly classified into 11 blocks of 6 units and five blocks of 4 units, resulting in 43 samples in the intervention group and 43 in the control group. In the end, 3 samples from the control group were excluded from the study due to low collaboration and unwilling to continue cooperation and 2 samples from the intervention group were excluded due to unwilling to continue cooperation. Figure 1 shows the flowchart of sampling and allocation processes.
The instruments used in this study included: A demographic form surveying the age and educational level of mothers and their spouses, mothers’ occupation, monthly family income, and delivery type; the breastfeeding experience scale (BES) with 30 items and two parts. The first part, with 18 items, assesses breastfeeding difficulties and their severity in the early postpartum period (45-60 days) using a five-point Likert scale from 1 (not at all) to 5 (unbearable). The total score of this domain ranges from 18 to 90, with a higher total score indicating higher breastfeeding difficulties. The first domain included five groups of common breastfeeding difficulties: breast concerns, mechanic concerns, process concerns, milk insufficiency concerns, and social concerns. The second part measures the information about continuing or stopping breastfeeding, the time and reasons for stopping, and the daily consumption of formula milk or other substituted milk [19]. In this study, the valid and reliable Persian version of the BES was used [5].
We first explained the study objectives and methods to the participants and ensured the confidentiality of their information. Then, they signed an informed consent form to participate in the study. The women in the control and intervention groups completed the demographic form and the BES 3-5 days after delivery. For the intervention group, the researcher installed the breastfeeding mobile application on the mothers’ mobile phones and explained how to use it. This group received the educational intervention alongside standard breastfeeding care. When completing the second part of the BES, a 24-hour reminder recommended by WHO was used to minimize recall bias [20]. The control group received standard breastfeeding care only without any additional intervention. According to a similar study [21], each mother in the intervention group received the educational program for 8 weeks. The content of the educational application was prepared with the cooperation of seven reproductive health experts and one software engineer and based on the “breastfeeding mothers guide” of the Iranian Ministry of Health and Medical Education. The topics included the importance of breastfeeding, risks of formula feeding, different breastfeeding situations, how to assess breastfeeding adequacy, breast milk pumping and hand expression, breast milk storage and reuse and how to manage common breast and breastfeeding problems. During the 8-week intervention, mothers were advised to read different educational materials of the application twice a week, and text messages containing the benefits of breastfeeding were sent to them [22]. To minimize the possible access of the control group to the educational application, the application was installed and explanations were provided in a separate room for the intervention group. The researcher provided their mobile phone number to mothers in both groups to answer their possible questions. After 8 weeks of education, both groups completed the BES again after two months when the mothers visited the centers for vaccination. After the end of the study, educational application was provided to the control group. Data collection was done from July to November 2022.
An independent t-test was used to compare the quantitative variables, while chi-square test (or Fisher’s exact test) was employed for qualitative variables. The Shapiro-Wilks test was used to evaluate the normality of data distribution for the total BES score before and after the educational intervention. The mean pre-test score of the BES was compared between the two groups using an independent t-test. The mean post-test score of the BES was compared using ANCOVA. If the data distribution was abnormal, the Mann-Whitney U test was used to compare univariate analyses, and the Kruskal-Wallis test and the Wilcoxon test were used for within-group comparisons. The data were analyzed in SPSS software version 16 and the significance level was set at 0.05.
Results
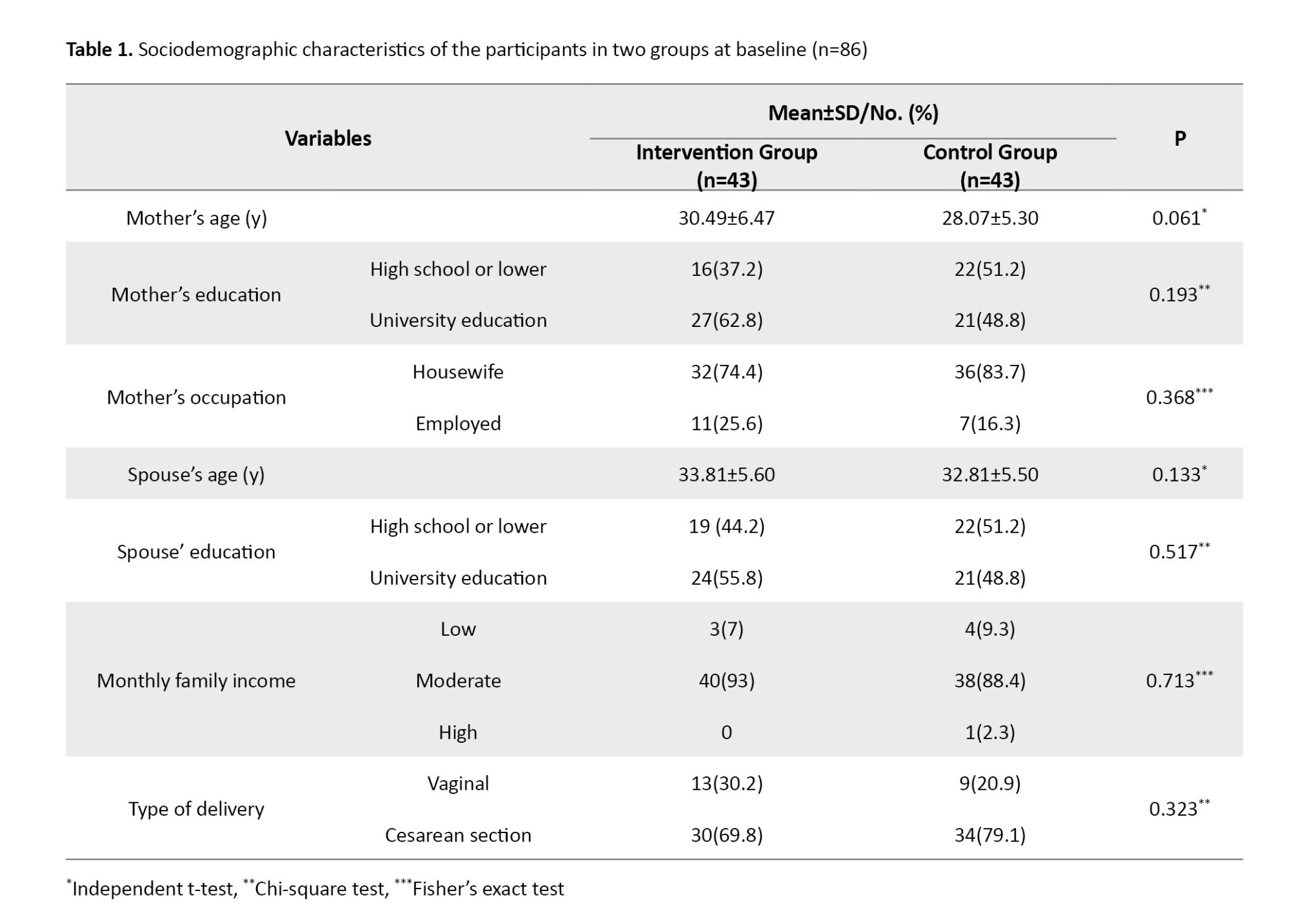
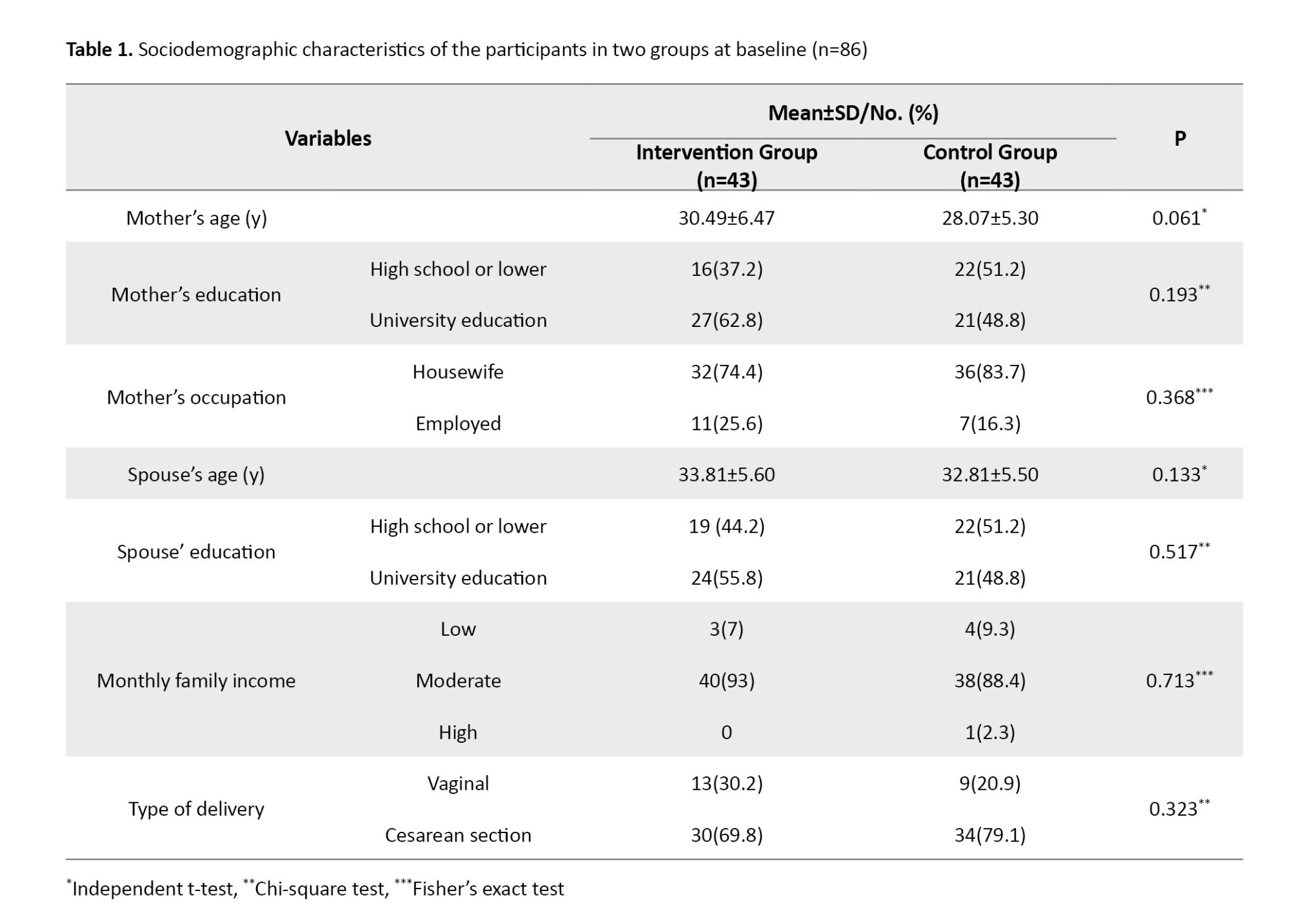
The mean age of mothers and their spouses was 29.55±6.56 and 32.93±5.44, respectively. It was found that 55.8% of mothers and 52.3% of spouses had a university education. Also, 79.1% of mothers were housewives, 90.7% had a moderate monthly income level, and 74.4% had given birth by a cesarean section. There was no significant difference in demographic data and type of delivery between the two groups (Table 1).
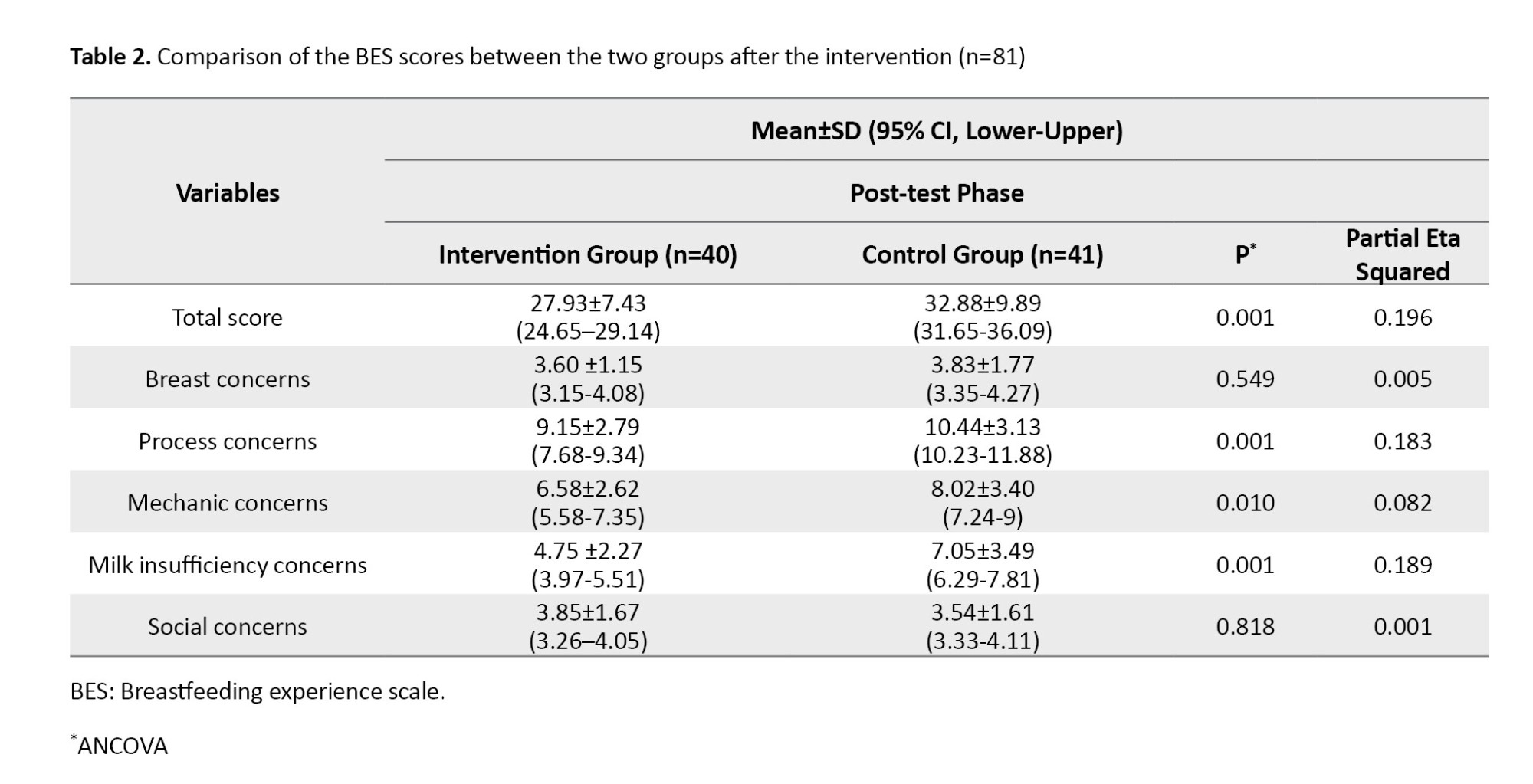
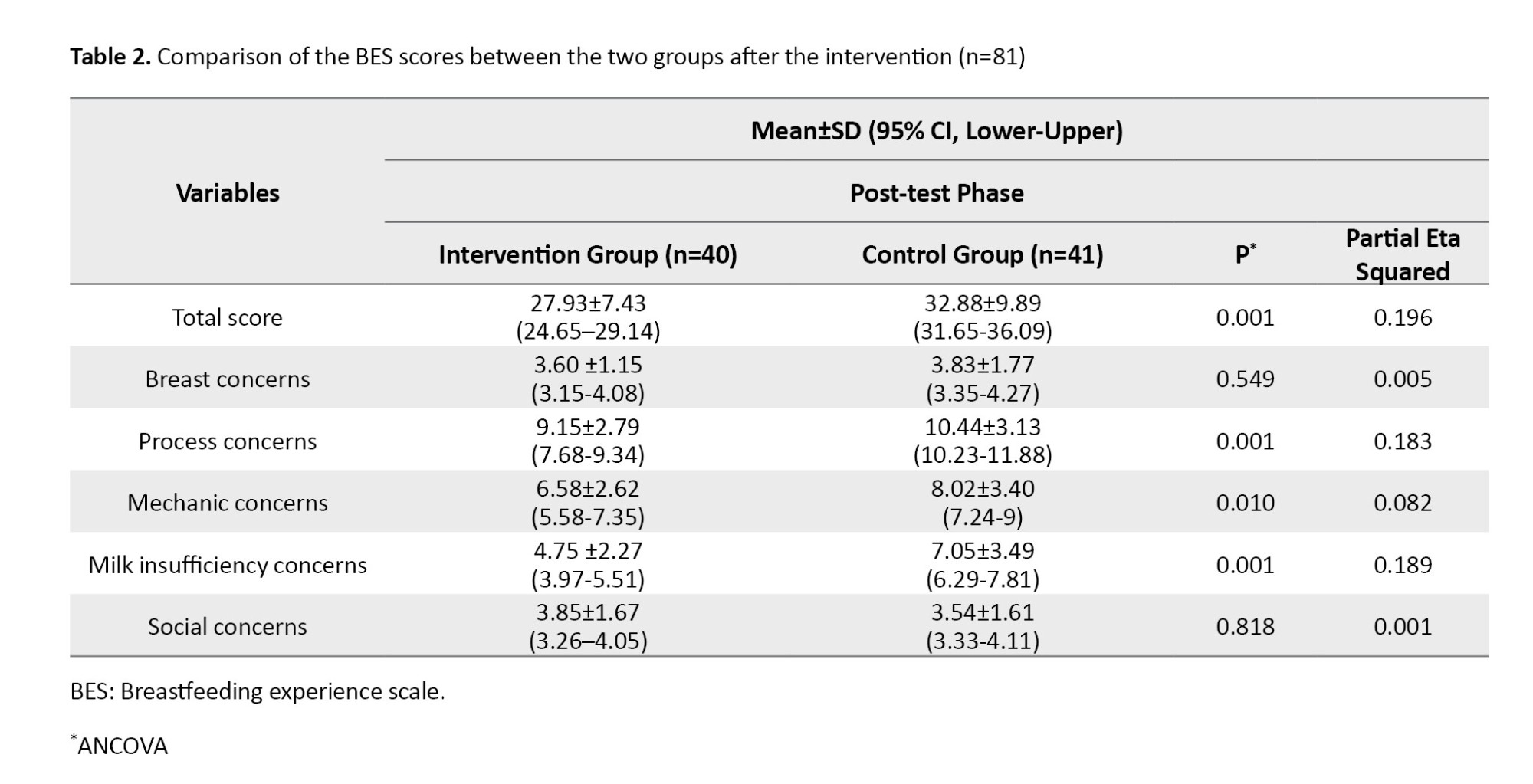
The mean total score of the BES before the intervention was 38.51±7.08 and 35.63±8.91 in the intervention and control groups, respectively. The independent t-test and Mann-Whitney U test results showed no significant difference between the two groups in total BES score and the BES domains of breast concerns, process concerns, mechanic concerns, milk insufficiency concerns, or social concerns before the intervention. After the intervention, mechanic concerns (P=0.01, Eta squared=0.082), process concerns (P=0.001, Eta Squared=0.183), milk insufficiency concerns (P=0.001, Eta Squared=0.189) and total BES score (P=0.001, Eta Squared=0.196) were significantly lower in the intervention group than in the control group . However, breast concerns and social concerns were not significantly different between the two groups after the intervention (Table 2).
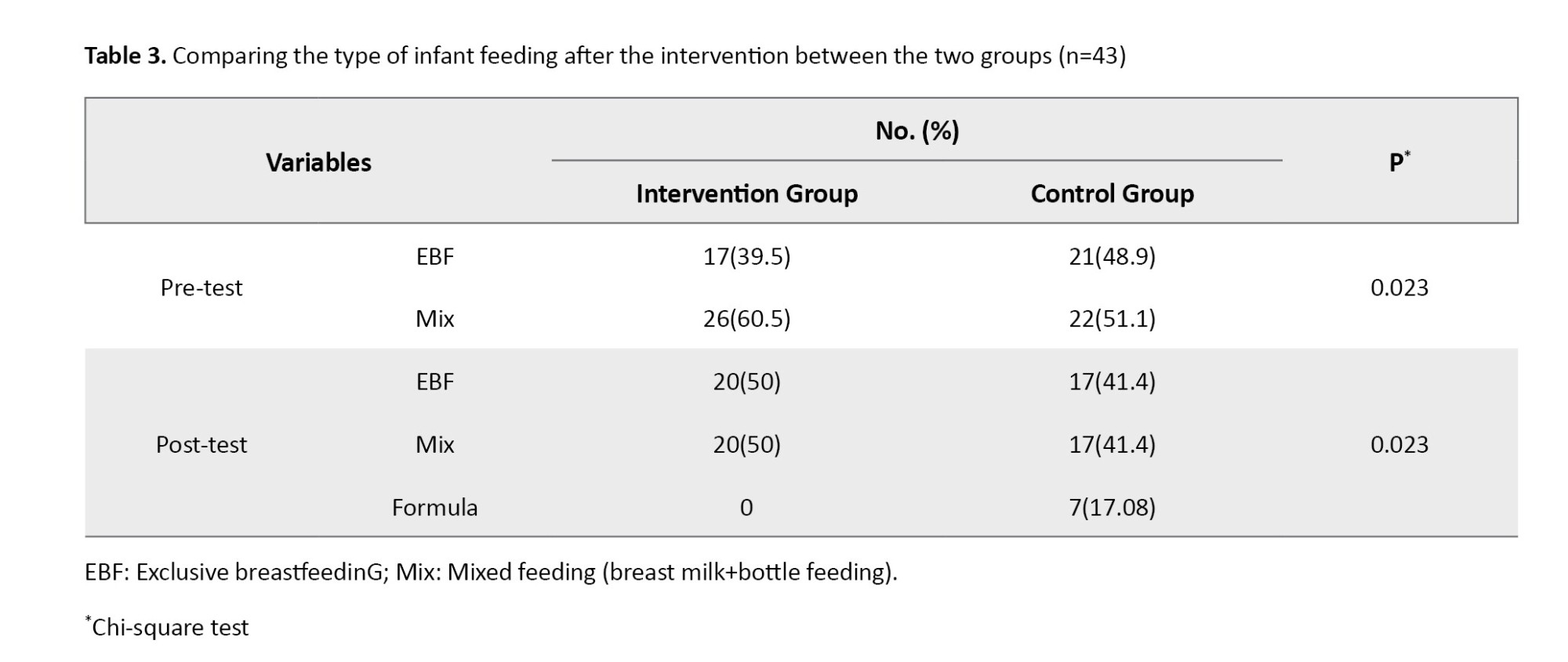
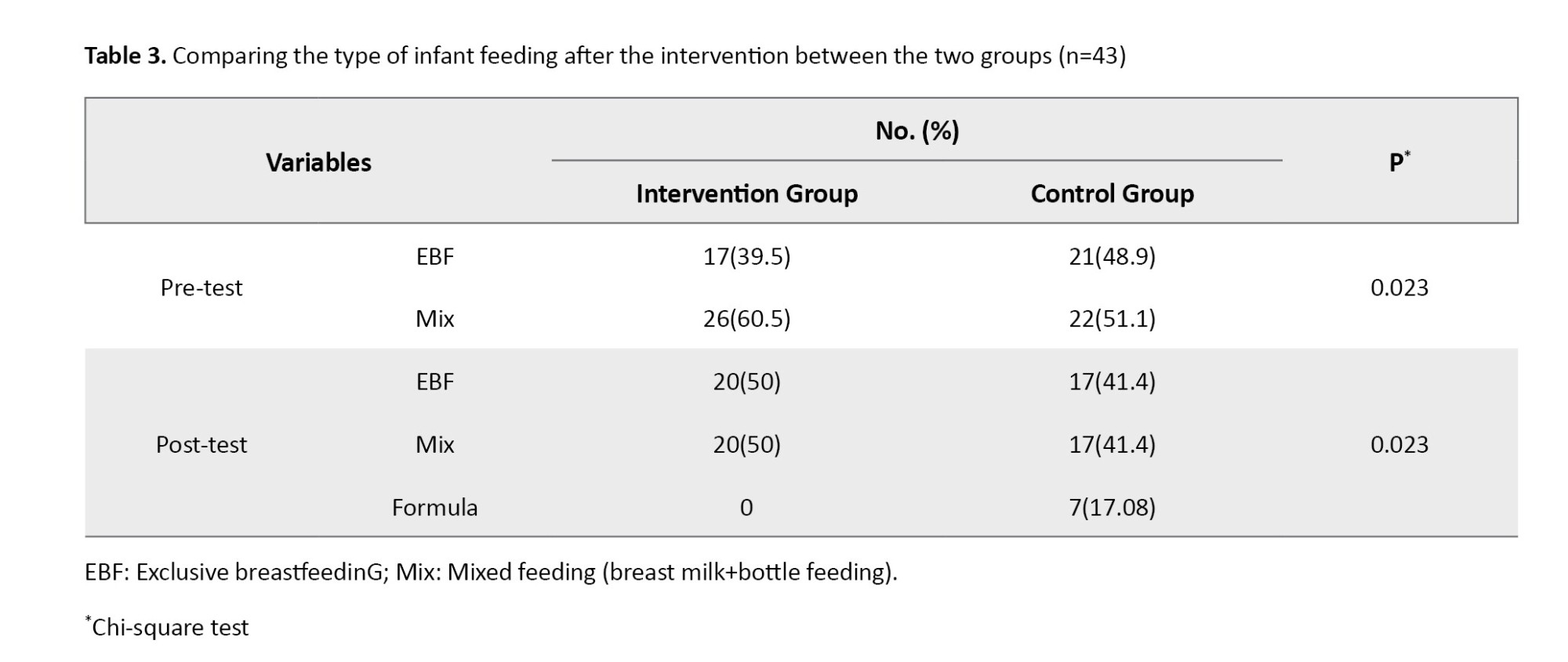
Exclusive breastfeeding rate in the intervention group increased from 39.5% to 50% after the intervention, while the control group experienced a decrease from 48.9% to 41.4%. Also, in the control group, 17.08% of mothers completely stopped breastfeeding, where the most common reasons included insufficient milk concerns, inadequate weight gains of the baby, and the baby’s difficulty with latching on. In the control group, 17.08% of mothers completely ceased breastfeeding, where the most common reasons included insufficient milk concerns, inadequate weight gain in the baby, the baby’s difficulties with latching on, the baby’s difficulties with sucking, and difficulty with positioning the baby during breastfeeding. On average, mothers stopped breastfeeding in 40-50 days. A significant difference in the type of infant feeding (P=0.023) was observed after the intervention between the two groups (Table 3).
In comparing the changes in daily use of formula milk for infants in mothers who had mixed feeding at the start of the study, the mothers in the intervention group reported a 28.4% decrease after the education, while those in the control group had a 27.5% increase in their daily use of formula milk.
Discussion
The present study investigated the effects of mobile-based breastfeeding education on the breastfeeding experience of Iranian nursing mothers. The results showed that the breastfeeding experience of women in the intervention group improved significantly compared to the control group. Breastfeeding problems and the use of formula milk in the intervention group decreased, and their exclusive breastfeeding rate increased compared to that of the control group. These results are consistent with the findings of systematic review studies, which suggested that mobile-based education can help alleviate the difficulties with breastfeeding [23, 24]. The results are against the findings of Eksioglu et al. and Lewkowitz et al. [25, 26], which may be due to differences in educational content and the characteristics of participants. Providing regular text messages about the benefits of breastfeeding twice a week in the present study seems to be effective in increasing mothers’ motivation to continue exclusive breastfeeding.
In the present study, breast concerns decreased after education in the intervention group, but this decrease was not statistically significant compared to the control group. This finding is in contrast with the results of Eksioglu et al. and Crasta et al. [25, 27], which can be due to the difference in the method and duration of education. It seems that the combination of mHealth and face-to-face education can effectively reduce breast concerns in north Iranian mothers. The timing of education may also affect the outcomes. The present study provided education only after delivery due to time limitations, whereas in other studies, the integration of prenatal and postnatal education with a greater emphasis on prenatal education showed effectiveness in reducing breastfeeding difficulties and promoting exclusive breastfeeding [9، 14].
In our study, the mothers’ concern about insufficient milk to meet the baby’s nutritional needs and the baby’s inappropriate weight gain seems to be mainly due to the baby’s high crying and the mother’s misunderstanding of the baby’s nutritional and behavioral patterns. Ensuring the adequacy of breastfeeding, increasing the mother’s awareness, and reassuring the mother of breastfeeding adequacy can strengthen their understanding of milk sufficiency and provide them with a positive breastfeeding experience. The intervention group in the present study experienced significantly fewer breastfeeding difficulties related to breast engorgement and reported less worry about insufficient milk than the control group. These findings are consistent with the results of some related studies [28-31]. In the current study, breastfeeding-related social concerns did not significantly decrease after education. This is consistent with the results of some related studies which suggested that addressing social concerns requires measures beyond individual education, such as the formation of breastfeeding support groups including peers, family members, and the healthcare system [32, 33].
Overall, mobile-based breastfeeding education improved the breastfeeding experience of nursing mothers. It could reduce their breastfeeding difficulties and increase the exclusive breastfeeding rate. The study had limitations. Despite the recommendation to the women in the intervention group to read the educational content in the application at least once a week, some of them had a lack of cooperation, and the researcher had to send an SMS reminder weekly. During the study, to minimize communication between the intervention and control groups, we tried to explain the application to the intervention group in a separate room. Also, it is possible that, despite the recommendations to women to only use the installed application, they have used other methods to gain knowledge and improve their breastfeeding experience.
In conclusion, mobile-based breastfeeding education has a positive effect on improving the breastfeeding experience of women in north of Iran. Using a mobile application for breastfeeding education can encourage mothers to give exclusive breastfeeding, increase their awareness of self-management methods in case of having breastfeeding problems, and improve their empowerment. Integrating mobile-based education with face-to-face education starting from late pregnancy is recommended for future studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.164). The procedures in this study are in accordance with the ethical guidelines.
Funding
This study was financially supported by Guilan University of Medical Sciences.
Authors' contributions
Study design: Sedighe Rezaie-Chamani; Data collection: Sedighe Rezaie-Chamani and Mona Aram; Statistical analyses: Saman Maroufizadeh; Writing the original draft: Mona Aram, Sedighe Rezaie Chamani and Zahra Bostani Khalesi; Review, editing and final approval: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the staff of comprehensive health centers in Rasht city and the mothers who participated in this study for their cooperation.
References
Breastfeeding has proven benefits for the health of mothers and babies [1]. One of the goals of the World Health Organization (WHO) is to reach 70% exclusive breastfeeding at 6 months by 2030 [2]. Currently, the exclusive breastfeeding rate is 44% globally and 49% in Iran [3, 4]. One of the factors affecting the early discontinuation of breastfeeding is the negative breastfeeding experience caused by factors such as breast-related problems, breastfeeding difficulties, infant-related difficulties and social concerns [5]. Breastfeeding difficulties are common among mothers. However, the severity of these difficulties may vary [6]. It can lead to negative consequences such as early cessation of breastfeeding, reduced frequency and duration of breastfeeding, decreased breastfeeding self-efficacy, and increased risk of postpartum anxiety and depression [7, 8].
Based on previous studies, the increase of knowledge and skills of mothers in solving breastfeeding difficulties through education can help them deal with the negative breastfeeding experience and its consequences [9, 10]. Traditional teaching methods can be challenging due to various barriers, such as mothers’ lack of physical and mental preparation, limited opportunities to learn due to short hospital stays, busy schedules of health workers, the need to attend training at specific times and places and limited access to educational materials. These barriers can make it difficult for mothers to receive adequate and effective education [11, 12]. Health professionals use mobile health (mHealth) services to remove learning barriers, provide medical and health services, manage and monitor patients, make clinical decisions, and educate patients [13, 14]. The WHO has recommended using mobile applications for education as a comprehensive educational method for the health system [15]. Mobile applications eliminate time and place limitations in education, reduce costs, make education accessible to everyone, and facilitate understanding of educational content [16, 17]. Despite the actions of the Iranian Ministry of Health and Medical Education to promote the exclusive breastfeeding rate, it is still less than the desired level [3]. This study aimed to determine the effect of mobile-based breastfeeding education on the breastfeeding experience of nursing mothers in north of Iran.
Material and Methods
This is a quasi-experimental study. The participants were 81 nursing mothers referred to comprehensive health centers in Rasht, Iran, who were selected using a multi-stage cluster random sampling method from 8 centers (two centers from each region). The inclusion criteria were 3-5 days after giving birth, the ability to read and write, being primiparous, practicing either exclusive breastfeeding or mixed feeding (combination of breastfeeding and bottle feeding), no medical contraindications for breastfeeding such as HIV and human T-cell lymphotropic virus infections, no active tuberculosis, no breast herpes, no galactosemia and phenylketonuria in newborns, and no use of illegal drugs during breastfeeding (based on the health records), having a mobile phone with an Android system, ability to install mobile applications, having healthy and full-term infants, and singleton birth. Exclusion criteria were prescription of infant formula by a physician, unwillingness to continue participation in the study and not using the mobile application at least once a week. The sample size was determined as 34 per group by considering α=0.05, β=0.2, test power=0.8 and an effect size (d)=0.7 according to the expectations of practical difference. By considering a 20% possible sample dropout, it increased to 43 per group (total sample size=86). The participants were allocated to two groups of control and intervention using the block randomization method. A random sequence generation software was employed to facilitate the randomization [18]. In this study, 253 women met the inclusion criteria that 167 of whom did not meet the inclusion criteria or did not participate in the study despite meeting the inclusion criteria. In the block randomization process, 86 units were evenly classified into 11 blocks of 6 units and five blocks of 4 units, resulting in 43 samples in the intervention group and 43 in the control group. In the end, 3 samples from the control group were excluded from the study due to low collaboration and unwilling to continue cooperation and 2 samples from the intervention group were excluded due to unwilling to continue cooperation. Figure 1 shows the flowchart of sampling and allocation processes.
The instruments used in this study included: A demographic form surveying the age and educational level of mothers and their spouses, mothers’ occupation, monthly family income, and delivery type; the breastfeeding experience scale (BES) with 30 items and two parts. The first part, with 18 items, assesses breastfeeding difficulties and their severity in the early postpartum period (45-60 days) using a five-point Likert scale from 1 (not at all) to 5 (unbearable). The total score of this domain ranges from 18 to 90, with a higher total score indicating higher breastfeeding difficulties. The first domain included five groups of common breastfeeding difficulties: breast concerns, mechanic concerns, process concerns, milk insufficiency concerns, and social concerns. The second part measures the information about continuing or stopping breastfeeding, the time and reasons for stopping, and the daily consumption of formula milk or other substituted milk [19]. In this study, the valid and reliable Persian version of the BES was used [5].
We first explained the study objectives and methods to the participants and ensured the confidentiality of their information. Then, they signed an informed consent form to participate in the study. The women in the control and intervention groups completed the demographic form and the BES 3-5 days after delivery. For the intervention group, the researcher installed the breastfeeding mobile application on the mothers’ mobile phones and explained how to use it. This group received the educational intervention alongside standard breastfeeding care. When completing the second part of the BES, a 24-hour reminder recommended by WHO was used to minimize recall bias [20]. The control group received standard breastfeeding care only without any additional intervention. According to a similar study [21], each mother in the intervention group received the educational program for 8 weeks. The content of the educational application was prepared with the cooperation of seven reproductive health experts and one software engineer and based on the “breastfeeding mothers guide” of the Iranian Ministry of Health and Medical Education. The topics included the importance of breastfeeding, risks of formula feeding, different breastfeeding situations, how to assess breastfeeding adequacy, breast milk pumping and hand expression, breast milk storage and reuse and how to manage common breast and breastfeeding problems. During the 8-week intervention, mothers were advised to read different educational materials of the application twice a week, and text messages containing the benefits of breastfeeding were sent to them [22]. To minimize the possible access of the control group to the educational application, the application was installed and explanations were provided in a separate room for the intervention group. The researcher provided their mobile phone number to mothers in both groups to answer their possible questions. After 8 weeks of education, both groups completed the BES again after two months when the mothers visited the centers for vaccination. After the end of the study, educational application was provided to the control group. Data collection was done from July to November 2022.
An independent t-test was used to compare the quantitative variables, while chi-square test (or Fisher’s exact test) was employed for qualitative variables. The Shapiro-Wilks test was used to evaluate the normality of data distribution for the total BES score before and after the educational intervention. The mean pre-test score of the BES was compared between the two groups using an independent t-test. The mean post-test score of the BES was compared using ANCOVA. If the data distribution was abnormal, the Mann-Whitney U test was used to compare univariate analyses, and the Kruskal-Wallis test and the Wilcoxon test were used for within-group comparisons. The data were analyzed in SPSS software version 16 and the significance level was set at 0.05.
Results
The mean age of mothers and their spouses was 29.55±6.56 and 32.93±5.44, respectively. It was found that 55.8% of mothers and 52.3% of spouses had a university education. Also, 79.1% of mothers were housewives, 90.7% had a moderate monthly income level, and 74.4% had given birth by a cesarean section. There was no significant difference in demographic data and type of delivery between the two groups (Table 1).
The mean total score of the BES before the intervention was 38.51±7.08 and 35.63±8.91 in the intervention and control groups, respectively. The independent t-test and Mann-Whitney U test results showed no significant difference between the two groups in total BES score and the BES domains of breast concerns, process concerns, mechanic concerns, milk insufficiency concerns, or social concerns before the intervention. After the intervention, mechanic concerns (P=0.01, Eta squared=0.082), process concerns (P=0.001, Eta Squared=0.183), milk insufficiency concerns (P=0.001, Eta Squared=0.189) and total BES score (P=0.001, Eta Squared=0.196) were significantly lower in the intervention group than in the control group . However, breast concerns and social concerns were not significantly different between the two groups after the intervention (Table 2).
Exclusive breastfeeding rate in the intervention group increased from 39.5% to 50% after the intervention, while the control group experienced a decrease from 48.9% to 41.4%. Also, in the control group, 17.08% of mothers completely stopped breastfeeding, where the most common reasons included insufficient milk concerns, inadequate weight gains of the baby, and the baby’s difficulty with latching on. In the control group, 17.08% of mothers completely ceased breastfeeding, where the most common reasons included insufficient milk concerns, inadequate weight gain in the baby, the baby’s difficulties with latching on, the baby’s difficulties with sucking, and difficulty with positioning the baby during breastfeeding. On average, mothers stopped breastfeeding in 40-50 days. A significant difference in the type of infant feeding (P=0.023) was observed after the intervention between the two groups (Table 3).
In comparing the changes in daily use of formula milk for infants in mothers who had mixed feeding at the start of the study, the mothers in the intervention group reported a 28.4% decrease after the education, while those in the control group had a 27.5% increase in their daily use of formula milk.
Discussion
The present study investigated the effects of mobile-based breastfeeding education on the breastfeeding experience of Iranian nursing mothers. The results showed that the breastfeeding experience of women in the intervention group improved significantly compared to the control group. Breastfeeding problems and the use of formula milk in the intervention group decreased, and their exclusive breastfeeding rate increased compared to that of the control group. These results are consistent with the findings of systematic review studies, which suggested that mobile-based education can help alleviate the difficulties with breastfeeding [23, 24]. The results are against the findings of Eksioglu et al. and Lewkowitz et al. [25, 26], which may be due to differences in educational content and the characteristics of participants. Providing regular text messages about the benefits of breastfeeding twice a week in the present study seems to be effective in increasing mothers’ motivation to continue exclusive breastfeeding.
In the present study, breast concerns decreased after education in the intervention group, but this decrease was not statistically significant compared to the control group. This finding is in contrast with the results of Eksioglu et al. and Crasta et al. [25, 27], which can be due to the difference in the method and duration of education. It seems that the combination of mHealth and face-to-face education can effectively reduce breast concerns in north Iranian mothers. The timing of education may also affect the outcomes. The present study provided education only after delivery due to time limitations, whereas in other studies, the integration of prenatal and postnatal education with a greater emphasis on prenatal education showed effectiveness in reducing breastfeeding difficulties and promoting exclusive breastfeeding [9، 14].
In our study, the mothers’ concern about insufficient milk to meet the baby’s nutritional needs and the baby’s inappropriate weight gain seems to be mainly due to the baby’s high crying and the mother’s misunderstanding of the baby’s nutritional and behavioral patterns. Ensuring the adequacy of breastfeeding, increasing the mother’s awareness, and reassuring the mother of breastfeeding adequacy can strengthen their understanding of milk sufficiency and provide them with a positive breastfeeding experience. The intervention group in the present study experienced significantly fewer breastfeeding difficulties related to breast engorgement and reported less worry about insufficient milk than the control group. These findings are consistent with the results of some related studies [28-31]. In the current study, breastfeeding-related social concerns did not significantly decrease after education. This is consistent with the results of some related studies which suggested that addressing social concerns requires measures beyond individual education, such as the formation of breastfeeding support groups including peers, family members, and the healthcare system [32, 33].
Overall, mobile-based breastfeeding education improved the breastfeeding experience of nursing mothers. It could reduce their breastfeeding difficulties and increase the exclusive breastfeeding rate. The study had limitations. Despite the recommendation to the women in the intervention group to read the educational content in the application at least once a week, some of them had a lack of cooperation, and the researcher had to send an SMS reminder weekly. During the study, to minimize communication between the intervention and control groups, we tried to explain the application to the intervention group in a separate room. Also, it is possible that, despite the recommendations to women to only use the installed application, they have used other methods to gain knowledge and improve their breastfeeding experience.
In conclusion, mobile-based breastfeeding education has a positive effect on improving the breastfeeding experience of women in north of Iran. Using a mobile application for breastfeeding education can encourage mothers to give exclusive breastfeeding, increase their awareness of self-management methods in case of having breastfeeding problems, and improve their empowerment. Integrating mobile-based education with face-to-face education starting from late pregnancy is recommended for future studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.164). The procedures in this study are in accordance with the ethical guidelines.
Funding
This study was financially supported by Guilan University of Medical Sciences.
Authors' contributions
Study design: Sedighe Rezaie-Chamani; Data collection: Sedighe Rezaie-Chamani and Mona Aram; Statistical analyses: Saman Maroufizadeh; Writing the original draft: Mona Aram, Sedighe Rezaie Chamani and Zahra Bostani Khalesi; Review, editing and final approval: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the staff of comprehensive health centers in Rasht city and the mothers who participated in this study for their cooperation.
References
- Giannì ML, Lanzani M, Consales A, Bestetti G, Colombo L, Bettinelli ME, et al. Exploring the emotional breastfeeding experience of first-time mothers: implications for healthcare support. Front Pediatr. 2020; 8:199. [DOI:10.3389/fped.2020.00199] [PMID]
- WHO, UNICEF. The extension of the 2025 maternal, infant and young child nutrition targets to 2030. Geneva: World Health Organization; 2019. [Link]
- Baba Ahmadi A, Pajohideh ZS, Mohammadi S. [Elements of exclusive breastfeeding and related factors in Iran: A systematic review and meta analysis (Persian)]. Iran J Obstet Gynecol Infertil. 2021; 24(5):103-15. [doi:10.22038/ijogi.2021.18576]
- WHO. Global breastfeeding scorecard 2021: Protecting breastfeeding through bold national actions during the COVID 19 pandemic and beyond. Geneva: World Health Organization; 2021. [Link]
- Mortazavi F, Mousavi SA, Chaman R, Khosravi A. Validation of the breastfeeding experience scale in a sample of Iranian mothers. Int J Pediatr. 2014; 2014:608657. [DOI:10.1155/2014/608657] [PMID]
- Xiao X, Loke AY, Zhu SN, Gong L, Shi HM, Ngai FW. "The sweet and the bitter": Mothers' experiences of breastfeeding in the early postpartum period: A qualitative exploratory study in China. Int Breastfeed J. 2020; 15(1):12. [DOI:10.1186/s13006-020-00256-1] [PMID]
- Mahmoodi Z, Dolatian M, Jalal M, Mirabzadeh A. A path analysis of the effects of mental health and socio-personal factors on breastfeeding problems in infants aged less than six months. Evidence Based Care. 2018; 7(4):38-45. [doi:10.22038/ebcj.2017.26740.1620]
- Nilsson IMS, Kronborg H, Rahbek K, Strandberg-Larsen K. The significance of early breastfeeding experiences on breastfeeding self-efficacy one week postpartum. Matern Child Nutr. 2020; 16(3):e12986. [DOI:10.1111/mcn.12986] [PMID]
- Karaçam Z, Sağlık M. Breastfeeding problems and interventions performed on problems: Systematic review based on studies made in Turkey. Turk Pediatri Ars. 2018; 53(3):134-48. [DOI:10.5152/TurkPediatriArs.2018.6350] [PMID]
- Shafaei FS, Mirghafourvand M, Havizari S. The effect of prenatal counseling on breastfeeding self-efficacy and frequency of breastfeeding problems in mothers with previous unsuccessful breastfeeding: A randomized controlled clinical trial. BMC Womens Health. 2020; 20(1):94. [DOI:10.1186/s12905-020-00947-1] [PMID]
- Feenstra MM, Jørgine Kirkeby M, Thygesen M, Danbjørg DB, Kronborg H. Early breastfeeding problems: A mixed method study of mothers' experiences. Sex Reprod Healthc. 2018; 16:167-74.[DOI:10.1016/j.srhc.2018.04.003] [PMID]
- Shahbazi Sighildeh S, Parvanehvar S, Tayibi Z. [Description of mothers’ experiences of receiving breastfeeding education (Persian)]. J Qual Res Health Sci. 2016; 6(3):310-24. [Link]
- Koçak V, Ege E, İyisoy MS. The development of the postpartum mobile support application and the effect of the application on mothers' anxiety and depression symptoms. Arch Psychiatr Nurs. 2021; 35(5):441-9. [DOI:10.1016/j.apnu.2021.06.009] [PMID]
- Meedya S, Win K, Yeatman H, Fahy K, Walton K, Burgess L, et al. Developing and testing a mobile application for breastfeeding support: The Milky Way application. Women Birth. 2021; 34(2):e196-203. [DOI:10.1016/j.wombi.2020.02.006] [PMID]
- WHO. mHealth: New horizons for health through mobile technologies. Geneva: World Health Organization; 2011. [Link]
- Farzandipour M, Farkhian A, Nabovati E, Mir Ali K, Anvari Tafti S, Rajabi Moghadam H. [Smartphone-based application for training outpatient cardiac rehabilitation: Design and usability evaluation (Persian)]. Koomesh. 2020; 22(4):686-95. [Link]
- Wheaton N, Lenehan J, Amir LH. Evaluation of a breastfeeding app in rural Australia: prospective cohort study. J Hum Lact. 2018; 34(4):711-20. [DOI:10.1177/0890334418794181] [PMID]
- Sealed Envelope. Randomisation and online databases for clinical trials [Internet]. Available from: [Link]
- Wambach KA. Breastfeeding intention and outcome: A test of the theory of planned behavior. Res Nurs Health. 1997; 20(1):51-9. [PMID]
- WHO. Indicators for assessing breast feeding practices. Geneva: World Health Organization; 1991. [Link]
- Wambach KA. Maternal fatigue in breastfeeding primiparae during the first nine weeks postpartum. J Hum Lact. 1998; 14(3):219-29. [DOI:10.1177/089033449801400311] [PMID]
- Barkati SH, Saadvandia S, Alaei S, Farivar M, Homayounfar N, Motlagh ME. [Guidance for mothers for feeding with breastfeeding answering the common questions of mothers (Persian)]. Qom: Andisheh Mandegar; 2016. [Link]
- Almohanna AA, Win KT, Meedya S. Effectiveness of internet-based electronic technology interventions on breastfeeding outcomes: Systematic review. J Med Internet Res. 2020; 22(5):e17361.[DOI:10.2196/17361] [PMID]
- Qian J, Wu T, Lv M, Fang Z, Chen M, Zeng Z, et al. The value of mobile health in improving breastfeeding outcomes among perinatal or postpartum women: Systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2021; 9(7):e26098. [DOI:10.2196/26098] [PMID]
- Eksioglu A, Yesil Y, Demir Gungor D, Ceber Turfan E. The effects of different breastfeeding training techniques for primiparous mothers before discharge on the incidence of cracked nipples. Breastfeed Med. 2017; 12:311-5. [DOI:10.1089/bfm.2016.0150] [PMID]
- Lewkowitz AK, López JD, Werner EF, Ranney ML, Macones GA, Rouse DJ, et al. Effect of a novel smartphone application on breastfeeding rates among low-income, first-time mothers intending to exclusively breastfeed: Secondary analysis of a randomized controlled trial. Breastfeed Med. 2021; 16(1):59-67. [DOI:10.1089/bfm.2020.0240] [PMID]
- Crasta S, D'Souza P, Frank RW. Effectiveness of awareness programme regarding breastfeeding techniques on the prevention of nipple soreness amongst primipara mothers in a selected hospital at Mangaluru, Karnataka. Indian J Contin Nurs Educ. 2022; 23(1):49-53. [DOI:10.4103/ijcn.ijcn_10_21]
- Abuidhail J, Odeh A, Ibrewish T, Alqam B, Alajrab IA. Evaluation of postnatal education on breastfeeding technique of Jordanian mothers. Br J Midwifery. 2017; 25(11):715-22. [DOI:10.12968/bjom.2017.25.11.715]
- Huda MH, Chipojola R, Lin YM, Lee GT, Shyu ML, Kuo SY. The influence of breastfeeding educational interventions on breast engorgement and exclusive breastfeeding: A systematic review and meta-analysis. J Hum Lact. 2022; 38(1):156-70.[DOI:10.1177/08903344211029279] [PMID]
- Prasitwattanaseree P, Sinsuksai N, Prasopkittikun T, Viwatwongkasem C. Effectiveness of breastfeeding skills training and support program among first time mothers: A randomized control trial. Pacific Rim Int J Nurs Res. 2019; 23(3):258-70. [Link]
- Varghese B, Patwa A. Effectiveness of hospital based teaching programme on knowledge regarding home management for breast engorgement among postnatal mothers. Int J Res Rev. 2020; 7(6):486-93. [Link]
- Beggs B, Koshy L, Neiterman E. Women's perceptions and experiences of breastfeeding: A scoping review of the literature. BMC Public Health. 2021; 21(1):2169. [DOI:10.1186/s12889-021-12216-3] [PMID]
- Bookhart LH, Joyner AB, Lee K, Worrell N, Jamieson DJ, Young MF. Moving beyond breastfeeding initiation: A qualitative study unpacking factors that influence infant feeding at hospital discharge among urban, socioeconomically disadvantaged women. J Acad Nutr Diet. 2021; 121(9):1704-20. [DOI:10.1016/j.jand.2021.02.005] [PMID]
Article Type : Research |
Subject:
Special
Received: 2024/04/19 | Accepted: 2025/02/3 | Published: 2025/04/1
Received: 2024/04/19 | Accepted: 2025/02/3 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |