Mon, Dec 29, 2025
Volume 35, Issue 3 (6-2025)
JHNM 2025, 35(3): 168-178 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kabir K, Tourkashvand S, Mehdizadeh Tourzani Z, Yazdkhasti M. Effectiveness of Onosma dichroanthum Boiss Combined Ointment on Episiotomy Healing and Pain in Primiparous Women: A Randomized, Clinical Trial. JHNM 2025; 35 (3) :168-178
URL: http://hnmj.gums.ac.ir/article-1-2336-en.html
URL: http://hnmj.gums.ac.ir/article-1-2336-en.html
1- Associate Professor of Community and Family Medicine, Department of Community and Family Medicine, School of Medicine, Firoozabadi Clinical Research Development Unit, Iran University of Medical Sciences, Tehran, Iran.
2- Instructor, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
3- Instructor, Department of Midwifery and Reproductive Health, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
4- Associate Professor, Department of Midwifery and Reproductive Health, Social Determinants of Health Research Center, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran. ,Mansoyazd@yahoo.com
2- Instructor, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
3- Instructor, Department of Midwifery and Reproductive Health, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
4- Associate Professor, Department of Midwifery and Reproductive Health, Social Determinants of Health Research Center, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran. ,
Full-Text [PDF 694 kb]
(270 Downloads)
| Abstract (HTML) (503 Views)
Full-Text: (161 Views)
Introduction
Episiotomy is performed to facilitate efficient delivery, minimize severe injuries to the vagina and perineum, alleviate pressure on the cervix, and accelerate the delivery process in challenging circumstances [1, 2]. Despite the World Health Organization’s (WHO) recommendation to limit episiotomies in complicated vaginal deliveries, such as breech births, shoulder dystocia, instrumental delivery, fetal distress, and in women with female genital circumcision [2], the rates of episiotomy have remained high in developing countries [3-5]. The prevalence of episiotomy is estimated to be 50% in America, 31% in China, and 41.5% in Iran [4, 6].
The pelvic floor muscles and fascia provide critical support to prevent sagging of pelvic organs, supporting the proper function of the vagina, bladder, uterus, and rectum. Mis-timed episiotomy or incomplete healing can weaken or damage these muscles, resulting in short-term or long-term complications such as urinary incontinence, gas, or stool issues. Therefore, promoting perineal healing is crucial to uphold pelvic floor strength, tissue continuity, and uniformity to avert episiotomy-related complications [7].
Pain or incomplete healing of the episiotomy wound can instill fear in mothers about vaginal delivery and lead to a preference for cesarean sections. This pain and incomplete healing can disrupt a mother’s peace, hinder her enjoyment of childbirth, make her feel inadequate in caring for her baby and performing daily activities, and contribute to diminished sexual performance in the postpartum period [8-10].
The management of postpartum pain resulting from episiotomy and tears can involve various treatments such as using Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), intravenous and epidural narcotics, local anesthetic sprays, as well as other measures like hot or cold-water basins, ultrasonic waves, exercise therapy, massage, acupuncture, distraction, hypnotism, relaxation, and herbal treatment [11, 12]. The use of medicinal plants as remedies and dietary supplements to enhance overall health and medical treatment has garnered considerable attention [12-14]. Herbal medicine, a subset of complementary medicine, has been part of Iran’s long history of using medicinal plants [15, 16]. Various plants in Iran, including frankincense [17], green tea [18], Myrtus communis [19], Pistacia atlantica [20], Aloe vera [21], honey, olive, and curcumin [22], have been utilized to heal episiotomy wounds. Additionally, the root of the Onosma dichroanthum Boiss (ODB) plant, known for its anti-inflammatory and wound-healing properties due to its alkannin/shikonin (A/S) content, has traditionally been used to treat burn wounds [23-28]. Numerous studies have demonstrated the positive effects of ODB, particularly in pain reduction and wound healing for surgical wounds such as those from hemorrhoidectomy. ODB is one of the herbal medicines used in ointments, often combined with olive oil and beeswax for enhanced efficacy. Its properties, including disinfectant, antibacterial, antioxidant, anti-inflammatory, and wound-healing effects, make this herbal medicine native to Iran notable [27-37]. However, there is a lack of studies in Iran investigating the effectiveness of ODB Combined (ODBC) ointment in treating episiotomy wounds. Therefore, this study aims to assess the efficacy of ODBC ointment in healing and managing episiotomy pain intensity in primiparous women.
Materials and Methods
This double-blind, placebo-controlled clinical trial study was conducted on 190 eligible women in a therapeutic education center in Karaj City, Iran, from December 2022 to March 2023. According to Lavaf et al. study [36], the trial was designed to have 190 patients (95 in each group) using G*Power software (USA), considering 90% power, significance level (α) of 0.05, effect size (d) of 0.5, two-sided, allocation ratio (N2/N1) of 1 and 10% loss to follow up. The inclusion criteria were Iranian primiparous women aged 18 to 35 years, with mediolateral episiotomy, gestational age ≥37 weeks, no history of taking psychotropic or narcotic drugs, no alcohol addiction, no instrumental delivery such as forceps or a ventouse suction cup, no vulvovaginal inflammation or infection, no gestational or overt diabetes, without rupture of the membrane for more than 18 hours, and singleton pregnancy. The exclusion criterion was sensitivity to ointment.
For allocation concealment, the medications and placebos were put in sealed opaque envelopes sequentially. Randomized and prepared envelopes were done by someone not involved in sampling and data analysis. In the present study, observers and participants were blinded.
The intervention group received the leading ointment containing ODBC root extract, beeswax, and olive oil. This ointment is produced by Sanable Darou Herbal Pharmaceutical Company under the brand name ODBC with registration number SMMP80102011 and a standard hologram. This ccombined ointment is distributed in official pharmacies all over Iran and is used to heal diabetic foot ulcers.
After getting the approval of the Ethics Committee of Alborz University of Medical Sciences and registering the study on the Iranian Registry of Clinical Trials (IRCT) website, eligible participants entered the study voluntarily after the researcher explained the study’s objectives and obtained their written consent. The researcher completed the demographic and gestational characteristics based on the participants’ medical records. They were assigned to the intervention and control groups based on block randomization using Random Allocation Software (RAS).
In the intervention group, the initial intervention was conducted by a trained midwife, starting 4 hours post-delivery, once every eight hours (three times a day), and continuing until 10 days post-delivery in the Postpartum Department. The procedure involved cleansing the episiotomy wound with physiological saline. Subsequently, the wound was dried using sterile gauze. Following this, ODBC ointment was applied to the episiotomy area using sterile gloves, with a dosage equivalent to the size of an adult’s knuckle (5 mm or 2 g) every 8 hours. Finally, the treated area was covered with sterile gauze. Then, participants used sanitary pads to remove secretions after delivery. In the hospital, participants were taught how to use the ointment after discharge. Because the wound is close to the urethra or anus, mothers were asked to dry the area with a hair dryer after urinating or defecating, use sterile gauze and a new sanitary pad, and continue applying the ointment.
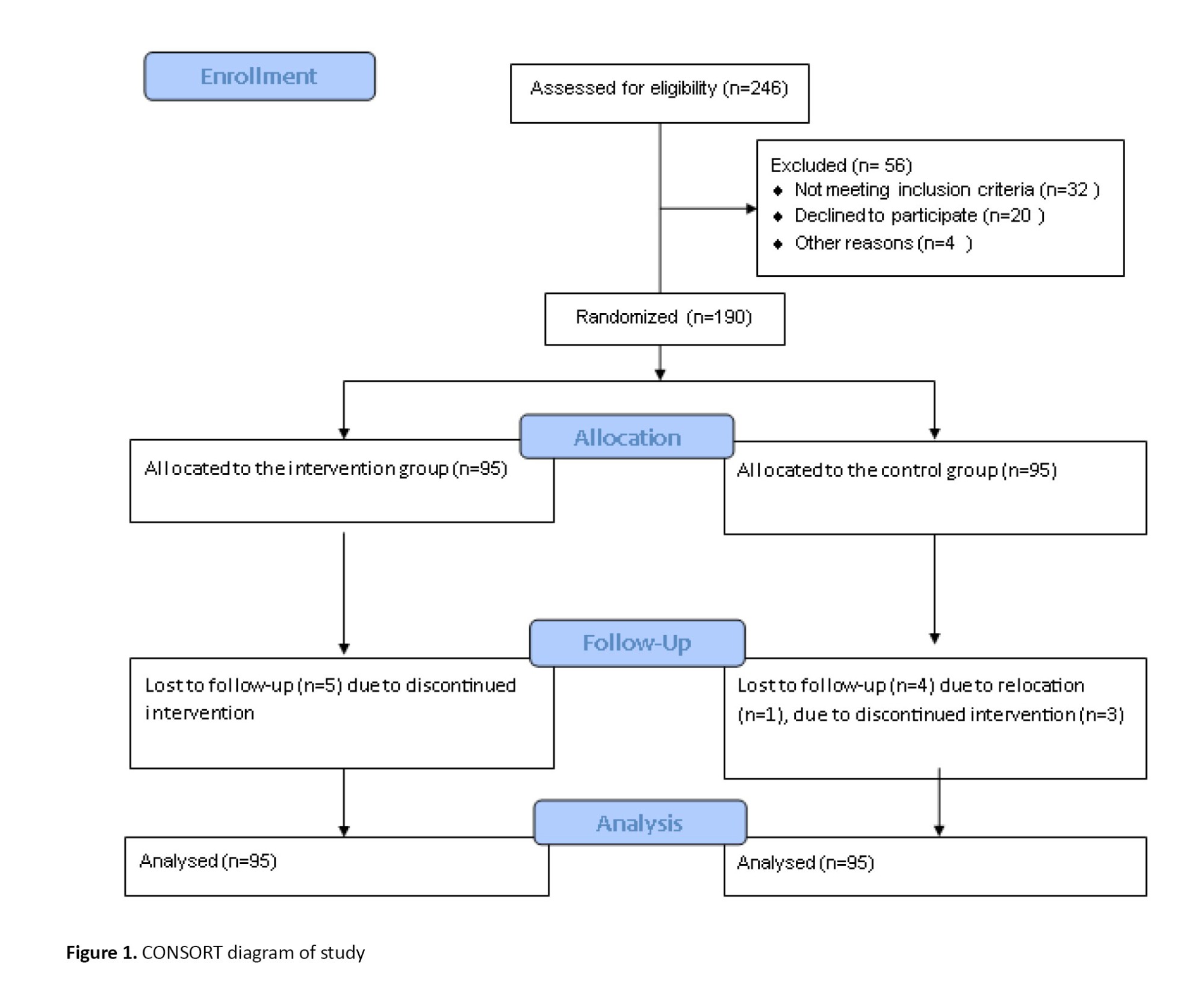
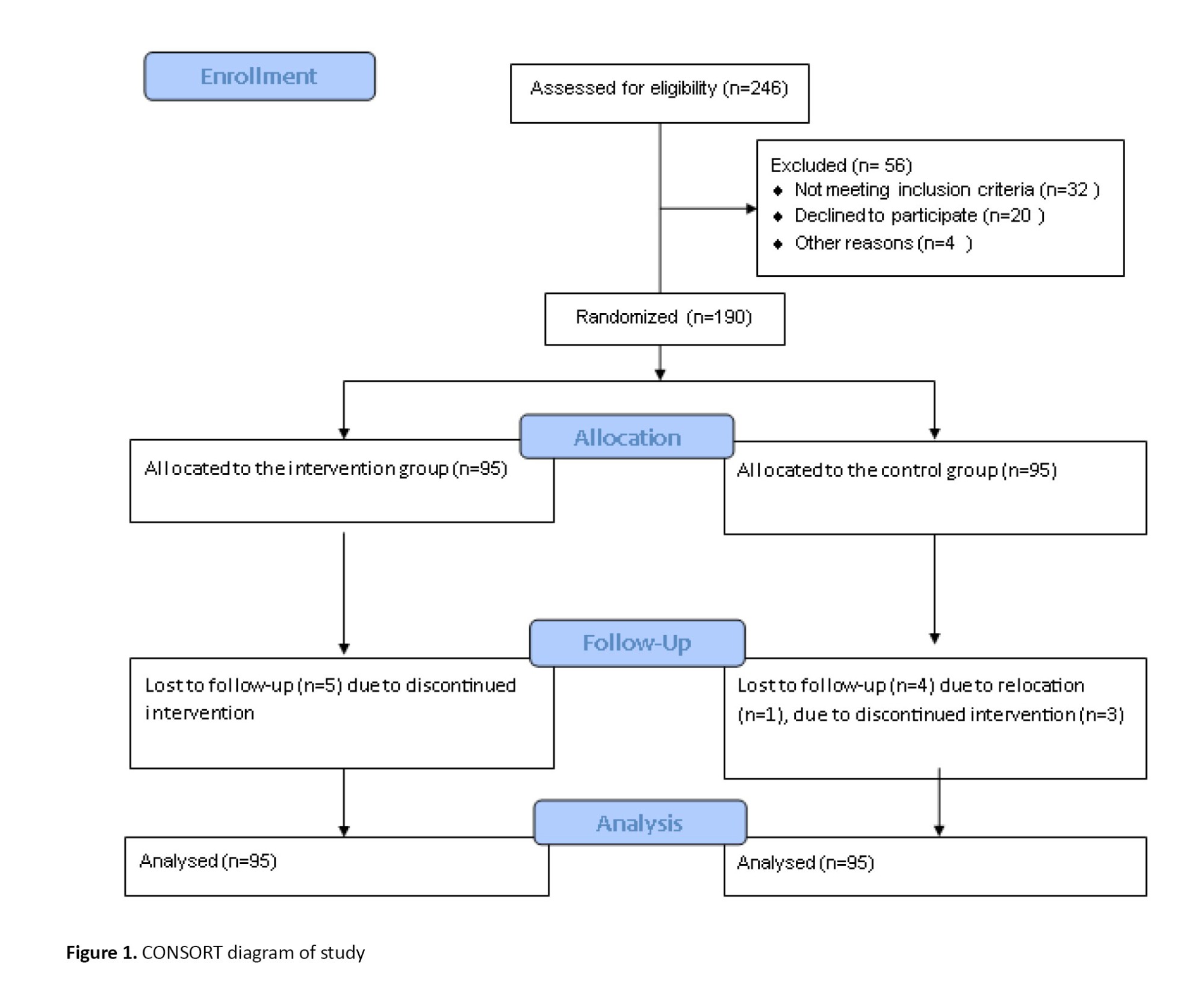
The placebo ointment was prepared by a fellow pharmacist at the Pharmacy Faculty of Alborz University of Medical Sciences. The ointment in the intervention group comprised starch devoid of active ingredients and side effects [36]. It was formulated to possess characteristics such as essence, color, consistency, and weight closely resembling the original ointment. In the control group, placebo ointment was used the same way as in the intervention group. It should be noted that no ointment is routinely used for episiotomy repair. The participants of the two groups were given a checklist to indicate complications or other cases and the frequency of ointment use. The participants were contacted once a day to report their adherence to the use of the ointment or the presence of complications from the use of the ointment and the irregular use of antibiotics or NSAIDs. Five participants in the intervention group and four in the control group lost to follow-up (Figure 1). The participants visited the clinic on the fifth and tenth day after delivery. The intensity of pain and healing was recorded by two observers who were not members of the research team and had received the necessary training (two experienced midwives) in the women’s clinic affiliated in Educational Therapeutic Hospital. The agreement between the two observers was measured by the kappa index (κ=0.8).
Data were collected using demographics, gestational characteristics, and irregular use of antibiotics and NSAIDs during the study and the Redness, Edema, Ecchymosis, Discharge, Approximation (REEDA) checklist and Visual Analog Scale (VAS).
The REEDA scale is a tool that assesses the inflammatory process and tissue healing in the perineal trauma through the evaluation of five items of healing: Redness (hyperemia), edema, ecchymosis, discharge, and approximation of the wound edges (coaptation). For each assessed item, a score ranging from 0 to 3 can be assigned by the health care provider. A higher score indicates a greater level of tissue trauma. The maximum value of 15 means the worst perineum healing outcome [30]. The REEDA scale is a tool for assessing perineal healing primarily developed by Davidson [31]. In Iran, this scale has been confirmed and also its validity and reliability [33]. This scale has been used in many Iranian studies [32, 33]. Episiotomy pain status was assessed using a standardized VAS. This tool measures the pain score from 0 (no pain) to 10 (the most pain amount) [32, 34].
The study data were collected from two groups across 4 time points: Before the intervention (baseline), 4 hours, 5 days, and 10 days after the intervention. In this double-blind study, primiparous mothers and research assistants were blinded to allocating intervention and control group participants. The chi-square test was used for qualitative variables. Statistical results from the quantitative data were presented with Mean±SD. The Kolmogorov-Smirnov test assessed data normality. The Mann-Whitney and Friedman nonparametric tests were used for variables with non-normal distribution. An independent parametric t-test was used for variables with the normal distribution. The significance level was set at less than 0.05. Missing data management was done using Generalized Estimating Equations (GEE) and random assumption. Statistical analyses were done with SPSS software, version 21 (IBM Corporation, USA).
Results
This study analyzed the demographic characteristics and other variables of 190 participants, with 95 participants in each group.
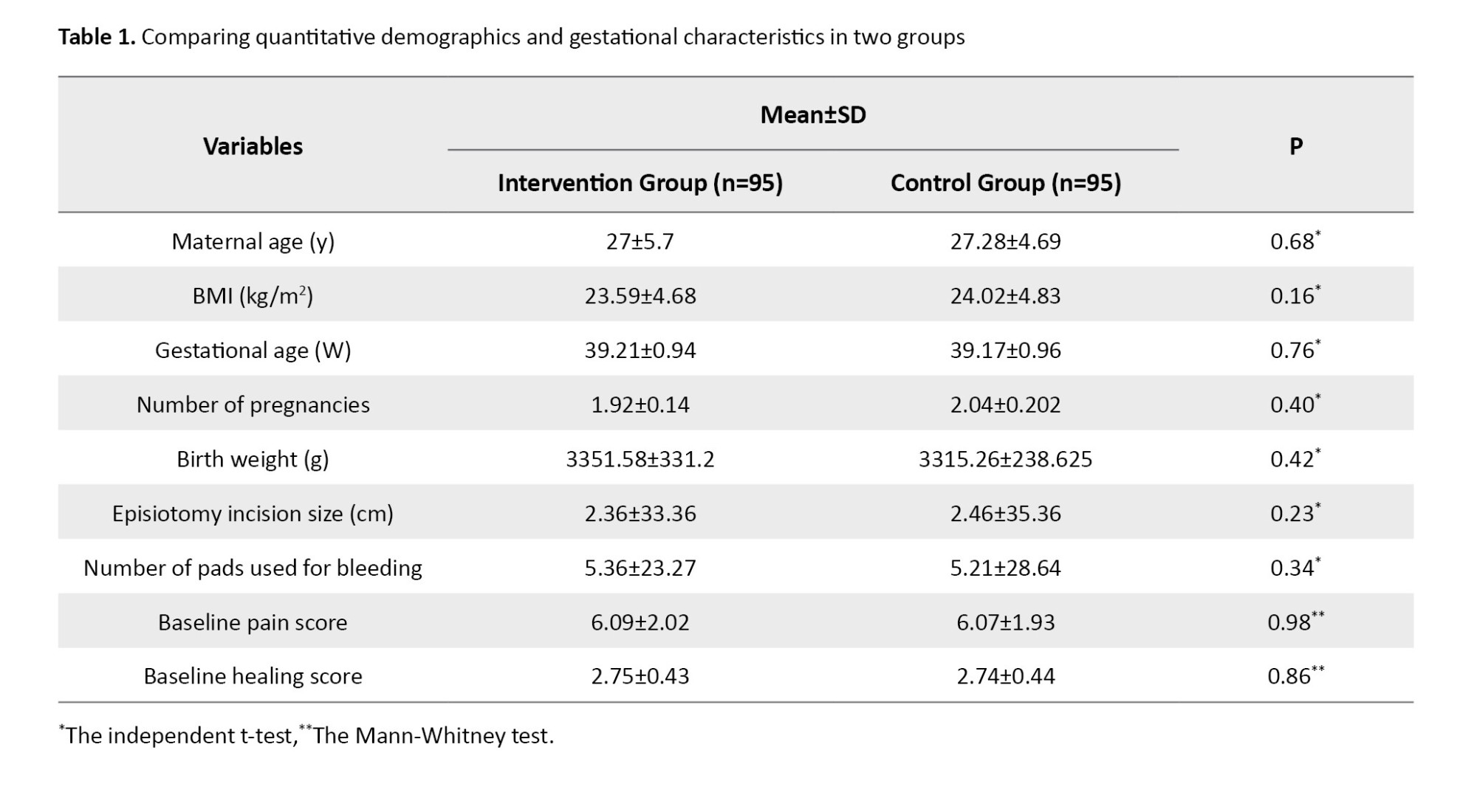
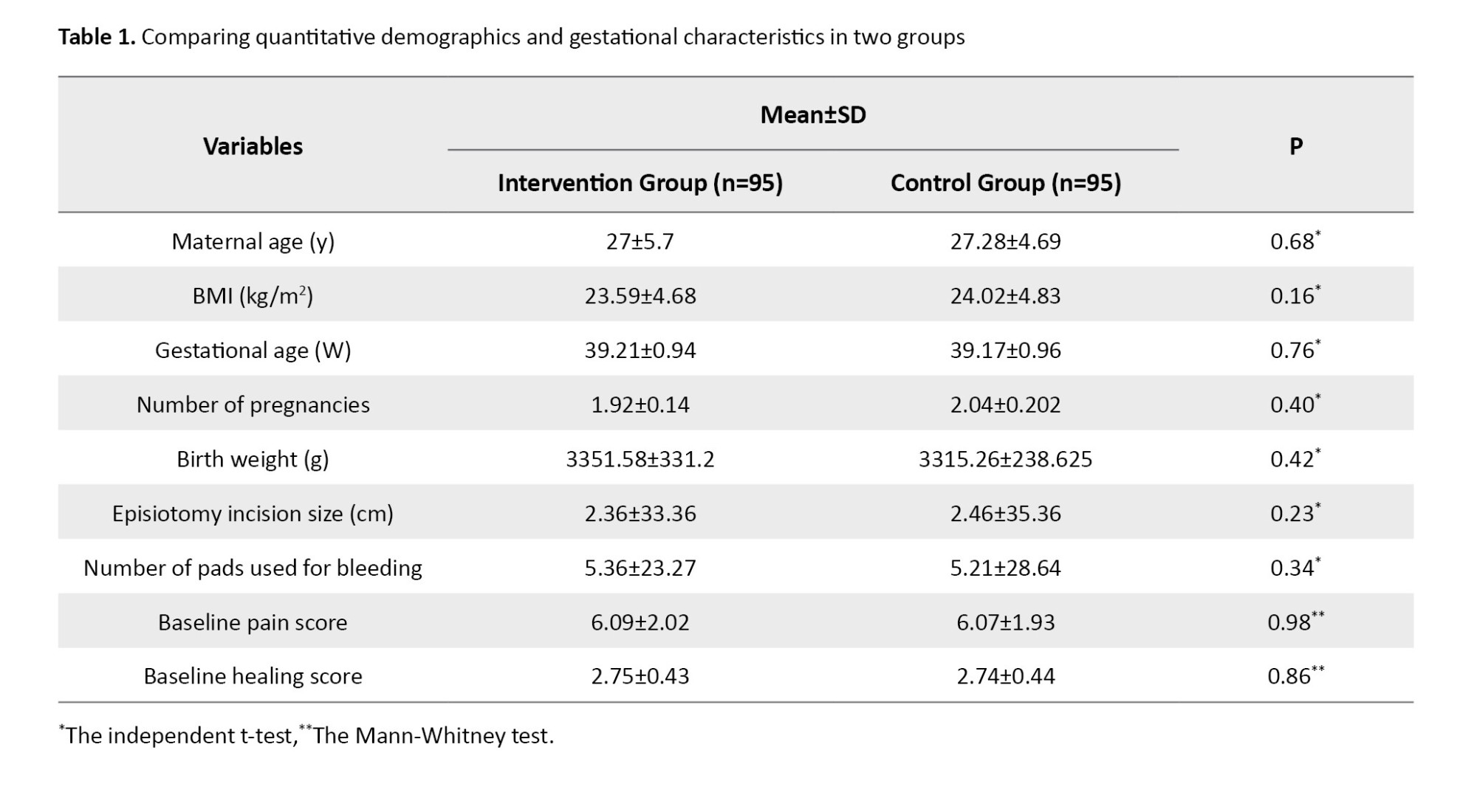
The intervention and control groups were homogeneous regarding maternal age, Body Mass Index (BMI), gestational age, number of pregnancies, birth weight, episiotomy incision size, number of pads used for bleeding, baseline pain, and healing scores. Variables of maternal age, body mass index, gestational age, number of pregnancies, birth weight, episiotomy incision size, and number of pads used for bleeding had normal distribution. Baseline pain and healing scores had a non-normal distribution (Table 1).
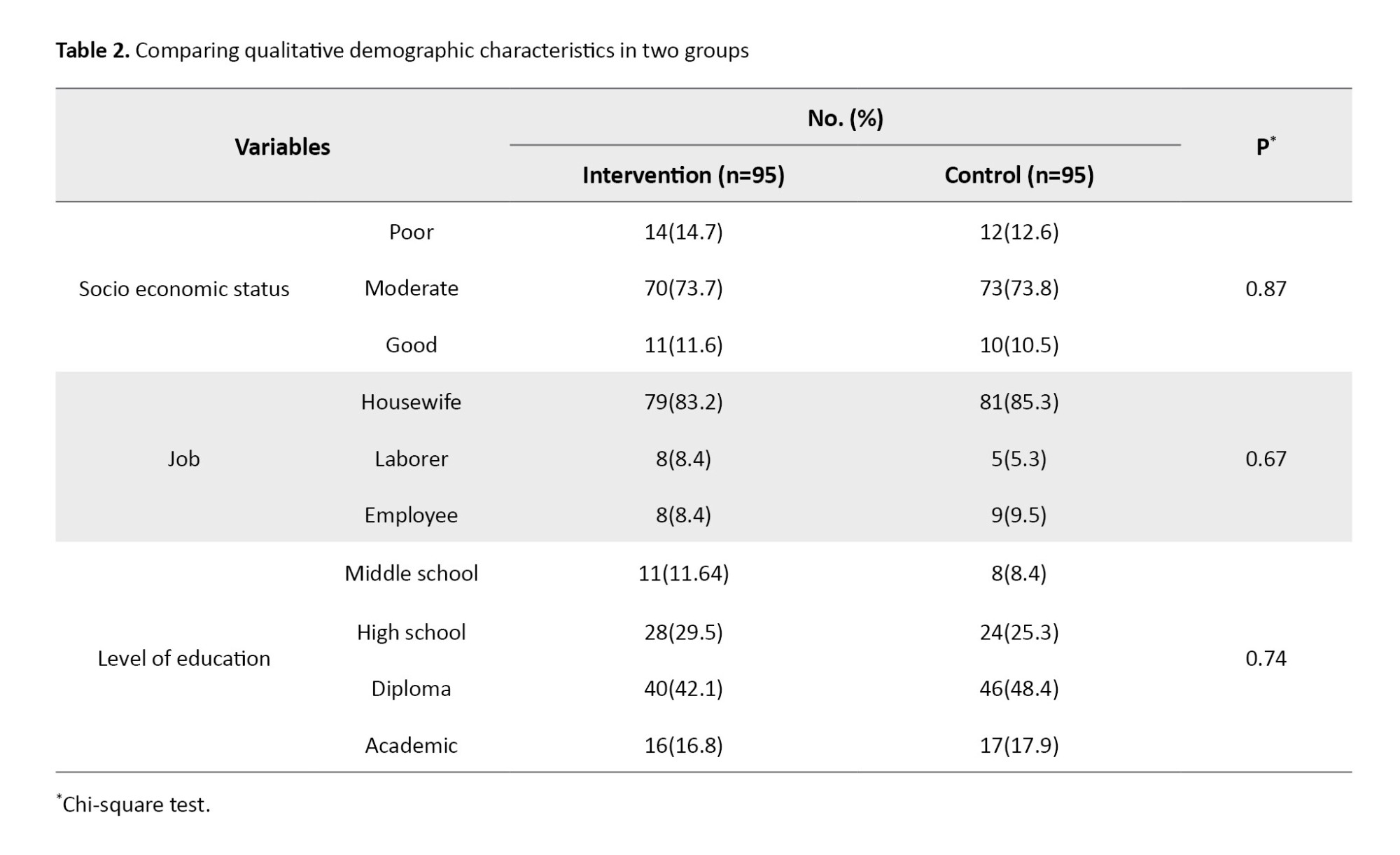
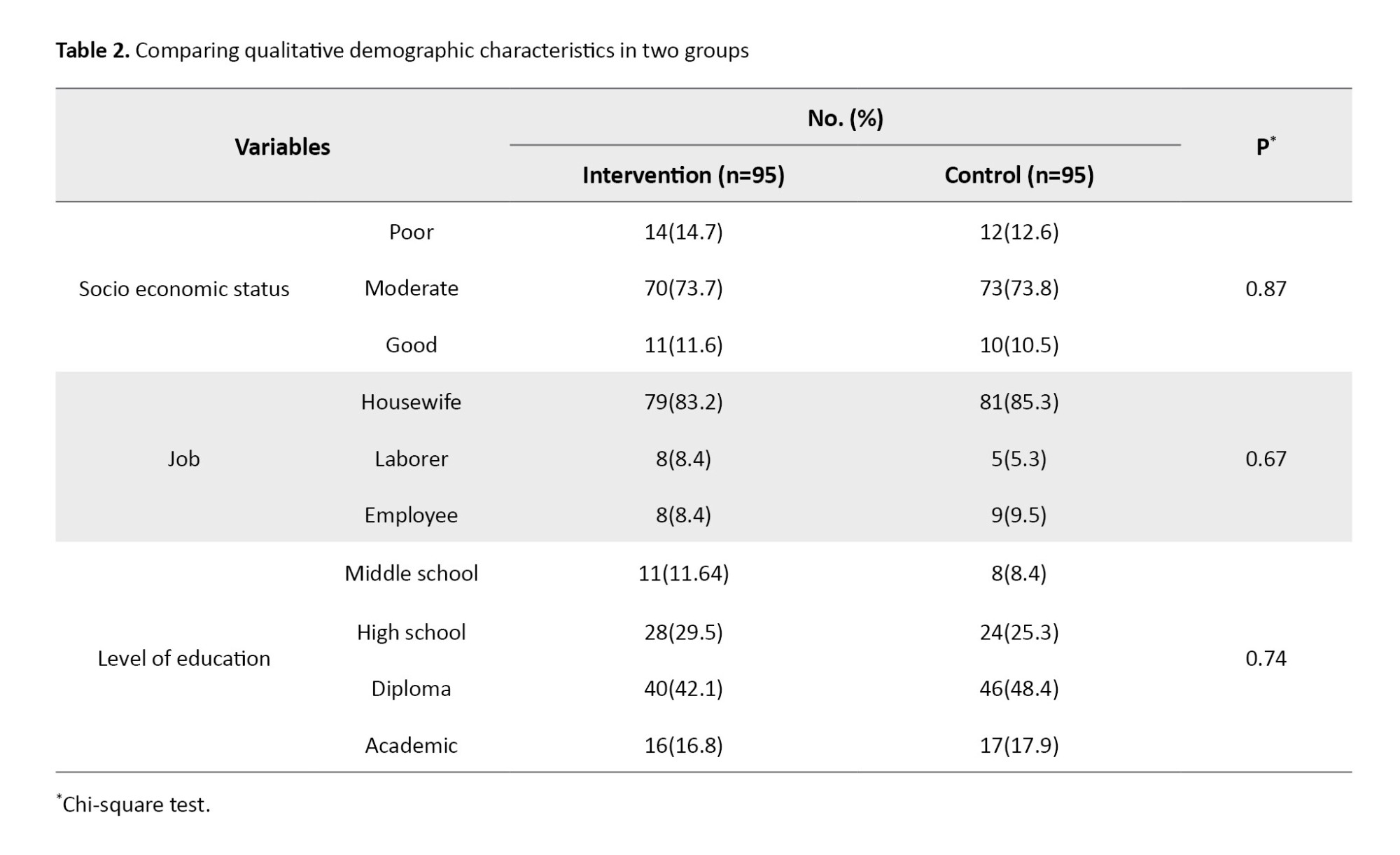
The chi-square test results showed no statistically significant differences between the two groups regarding socioeconomic status, occupation, and education level (Table 2).
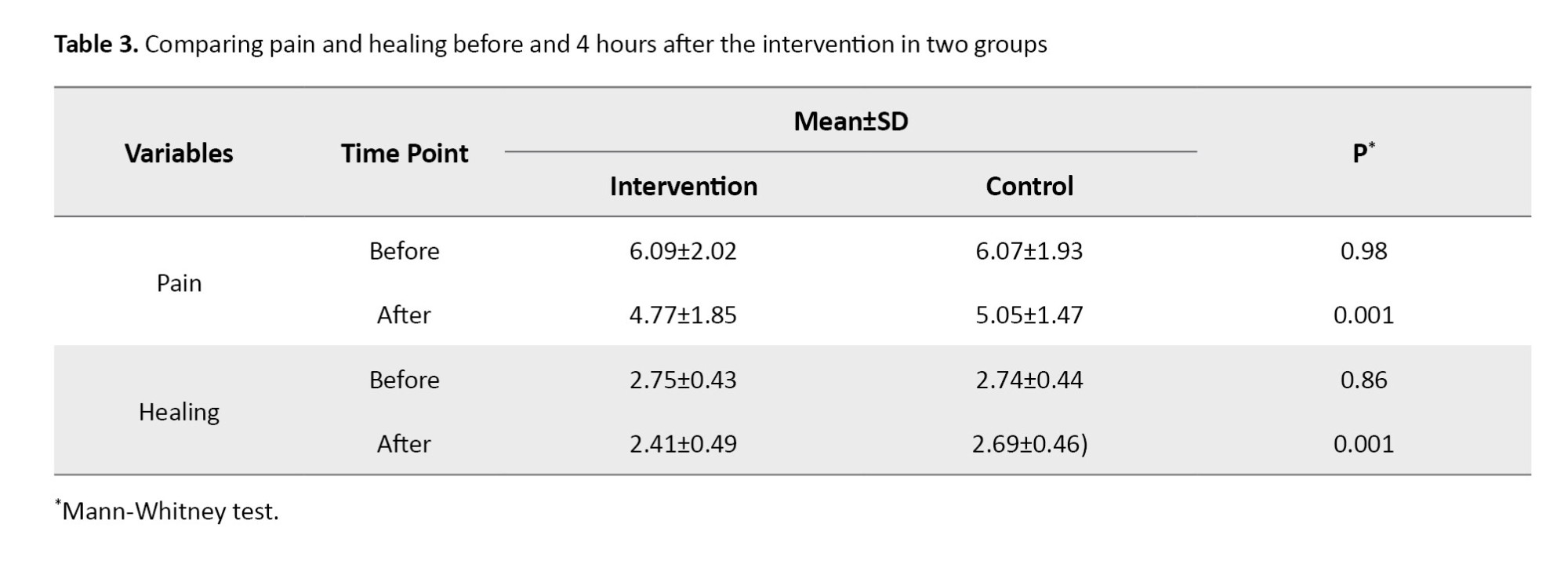
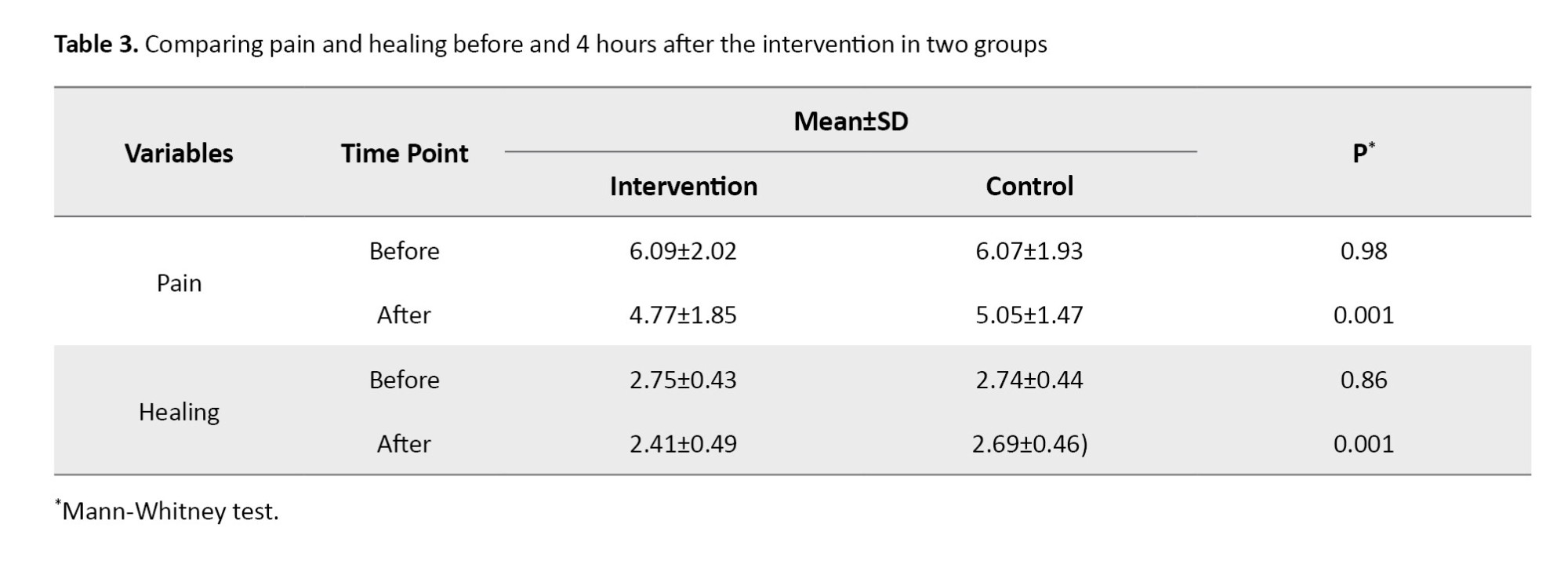
Based on the Mann-Whitney test, there was a statistically significant (P=0.001) difference between the two groups in the score of pain and healing 4 hours after the intervention compared to before the intervention (Table 3).
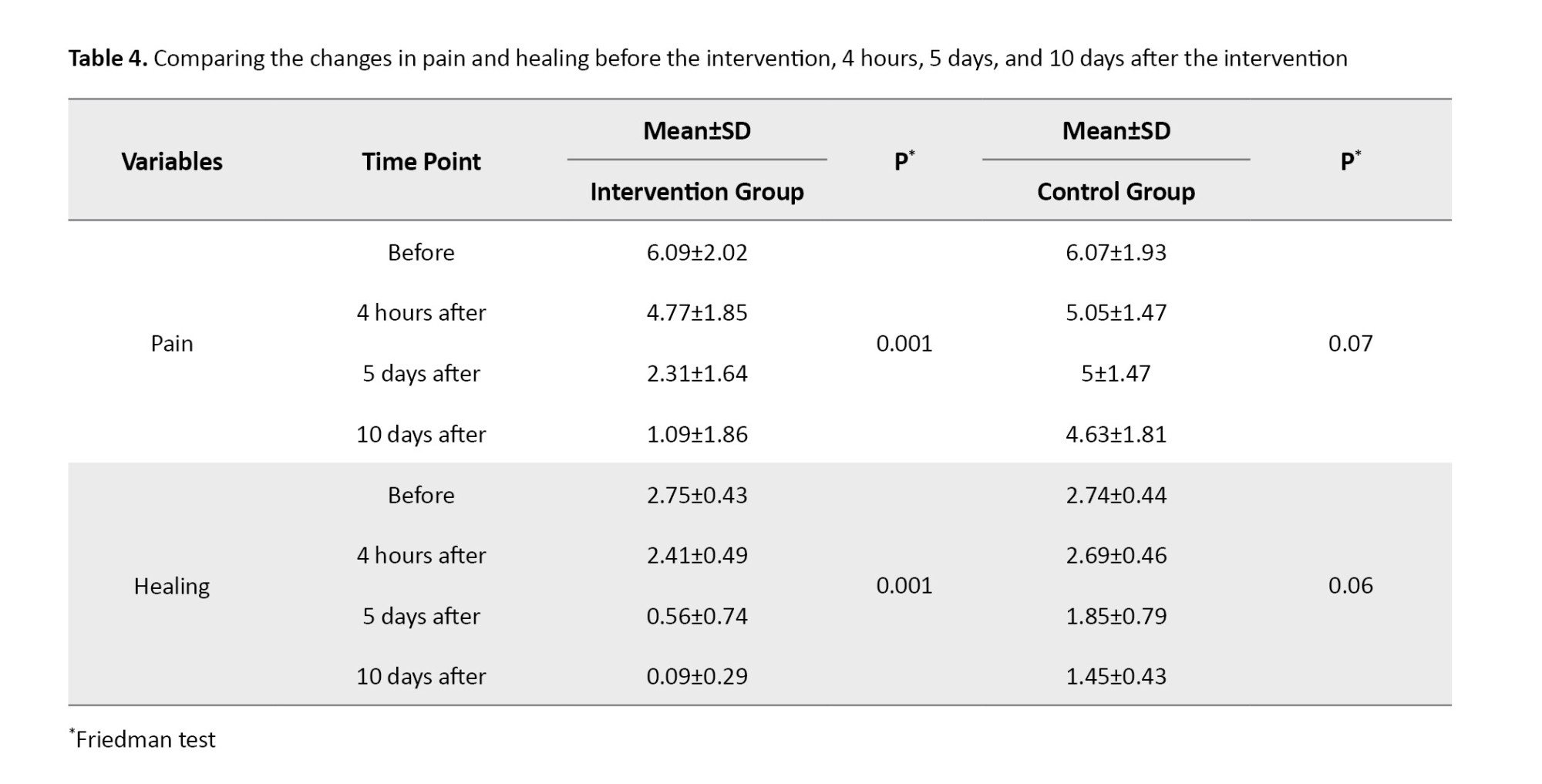
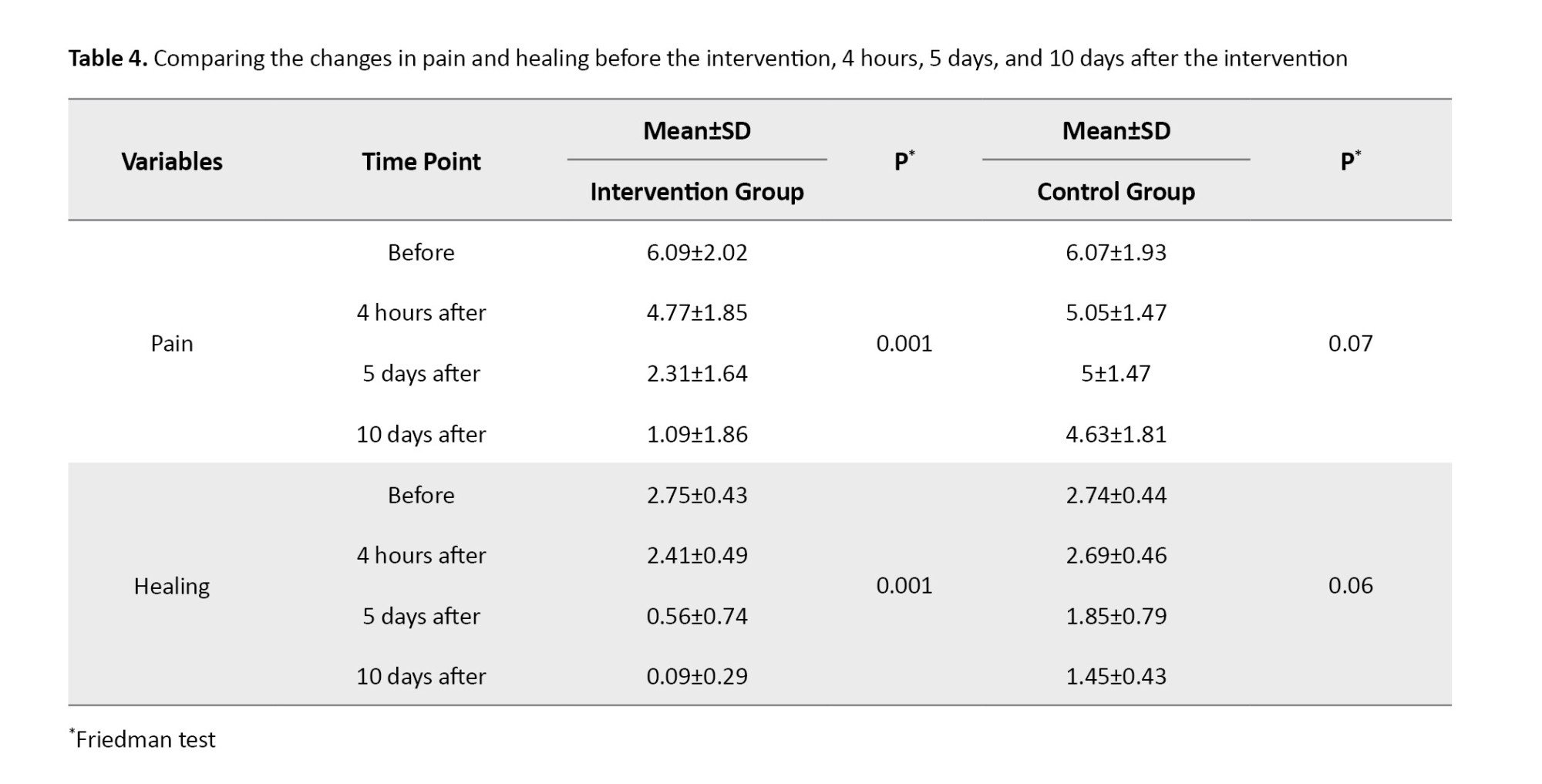
In the intervention group, the results of the Friedman test showed a trend of statistically significant changes in the mean score of pain and healing at 4 time points: Before the intervention, 4 hours, 5 days, and 10 days after the intervention (P=0.001). No statistically significant difference was observed in the control group (Table 4).
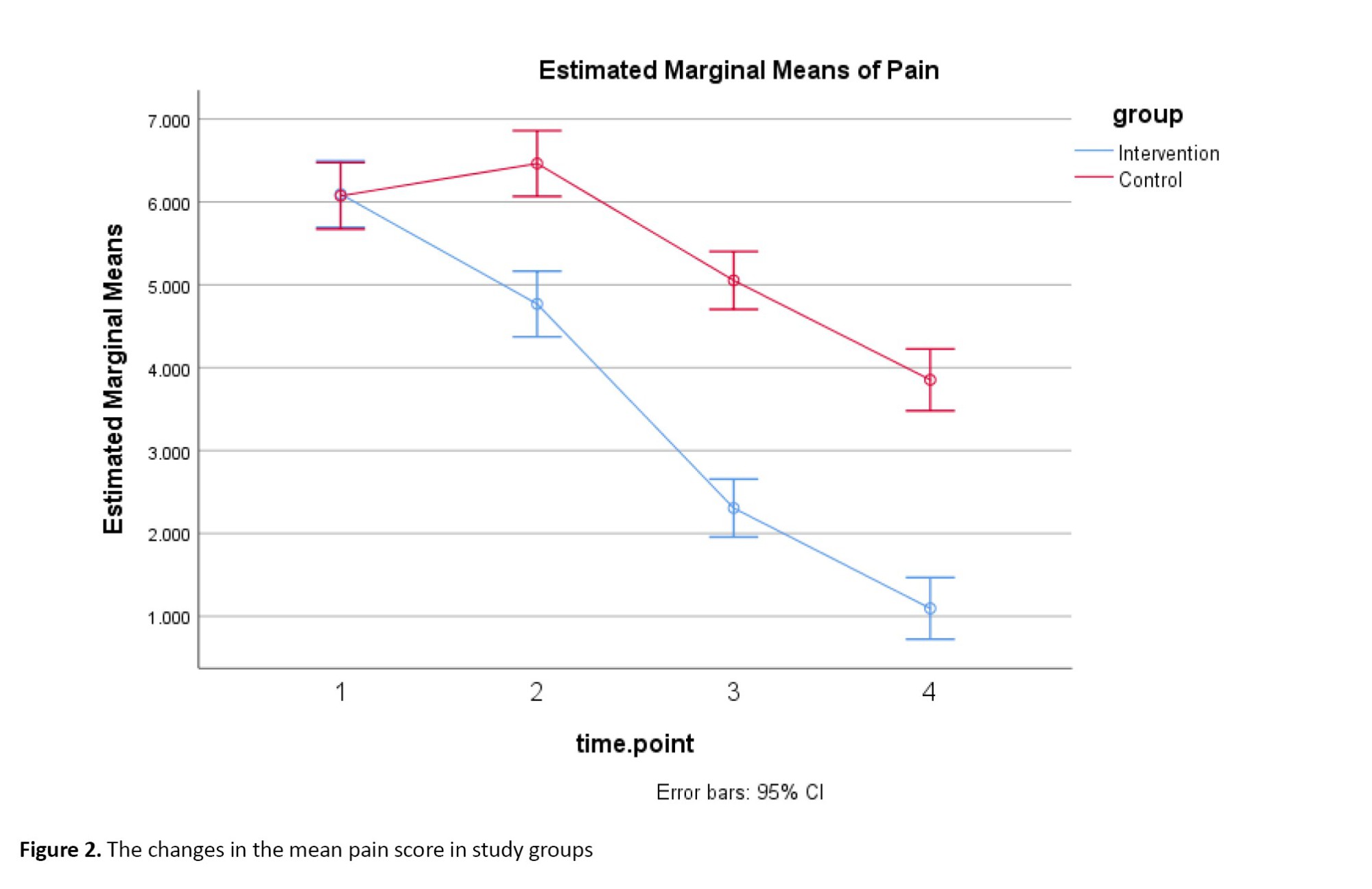
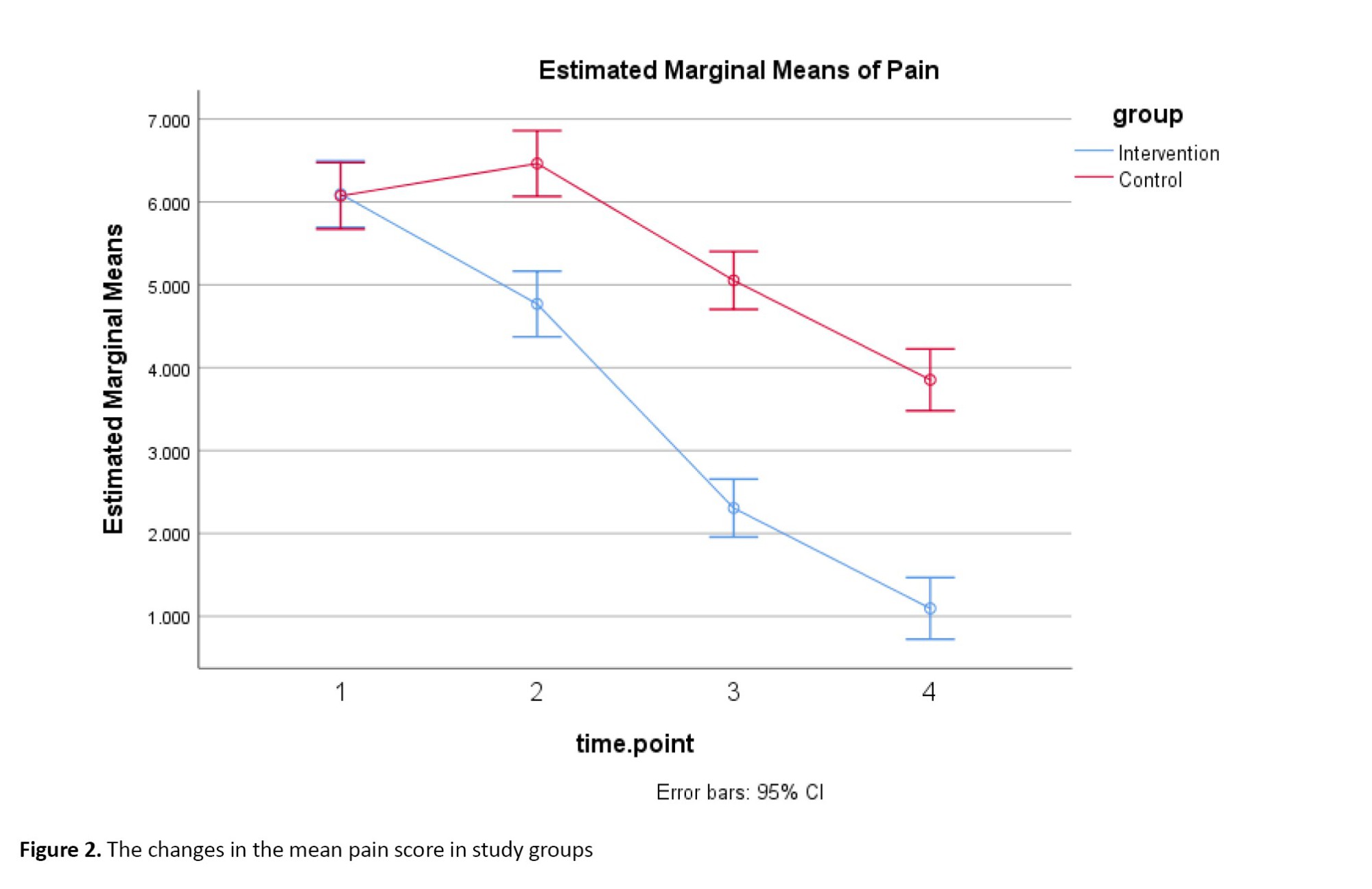
In Figure 2, on the horizontal axis, number 1 represents before the intervention, number 2 represents 4 hours, number 3 represents 5 days after, and number 4 represents 10 days after the intervention and the mean pain scores are on the vertical axis.
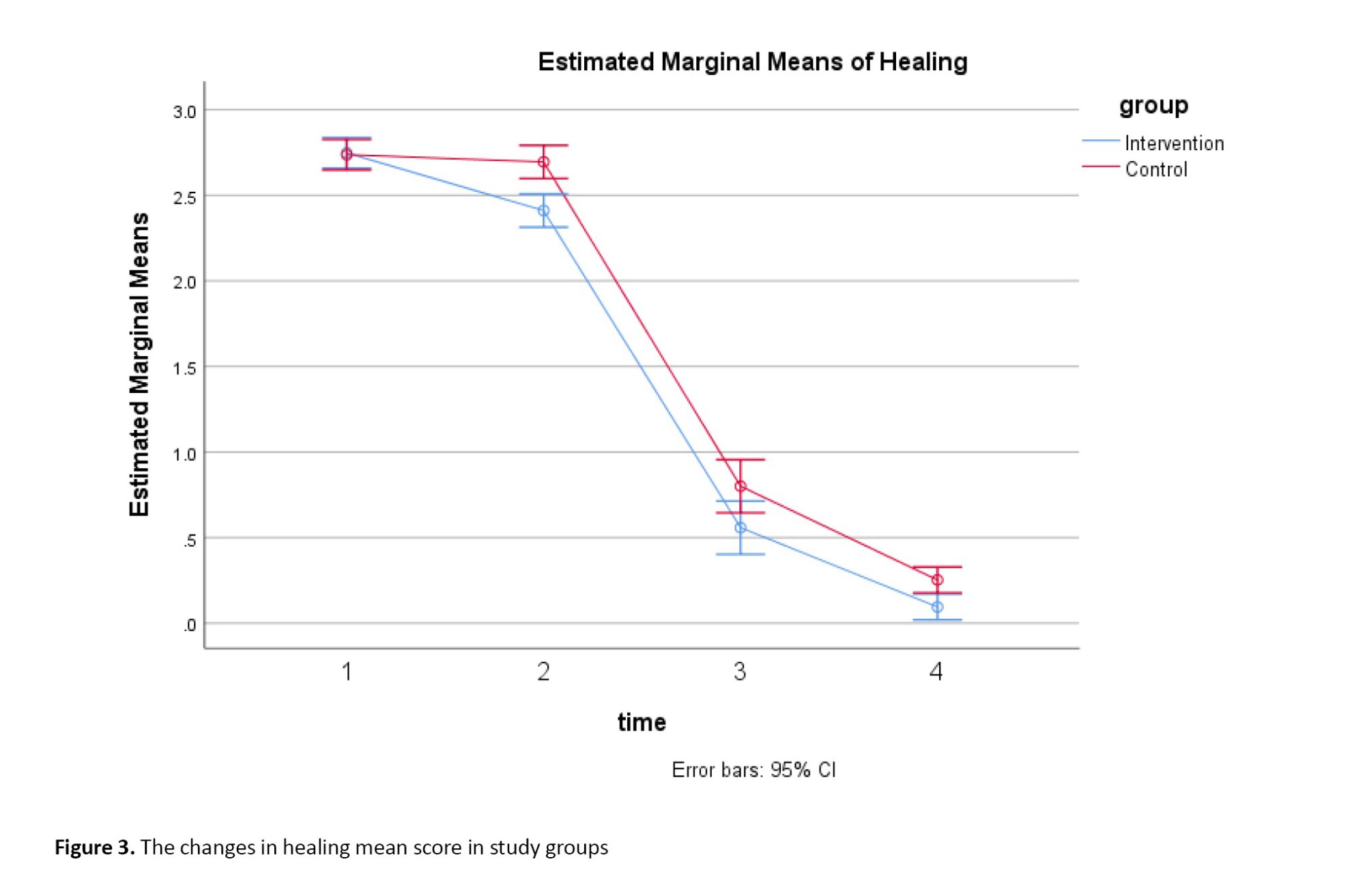
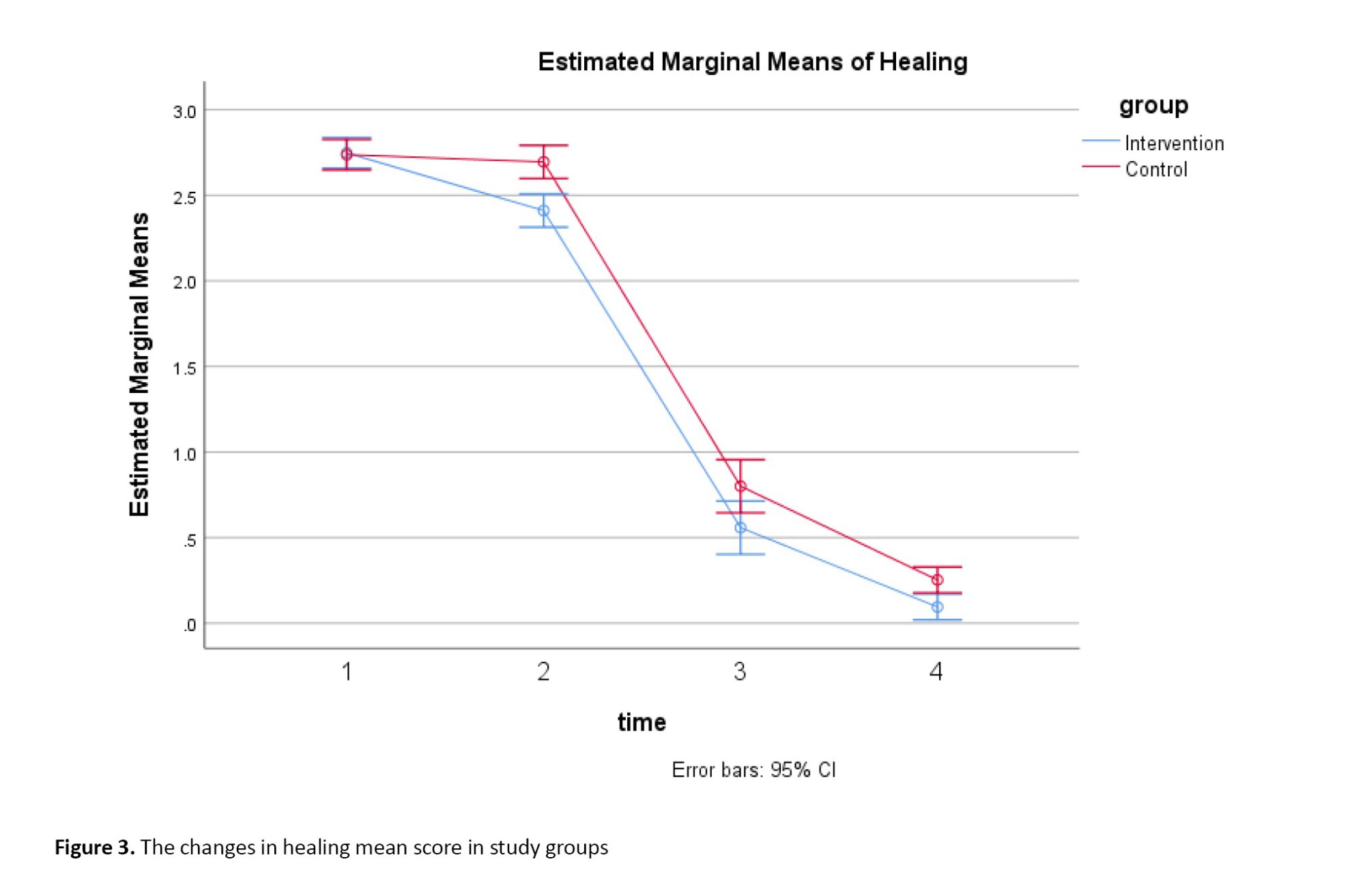
In Figure 3, on the horizontal axis, number 1 represents before the intervention, number 2 represents 4 hours, number 3 represents 5 days after, and number 4 represents 10 days after the intervention and the mean healing scores are on the vertical axis.
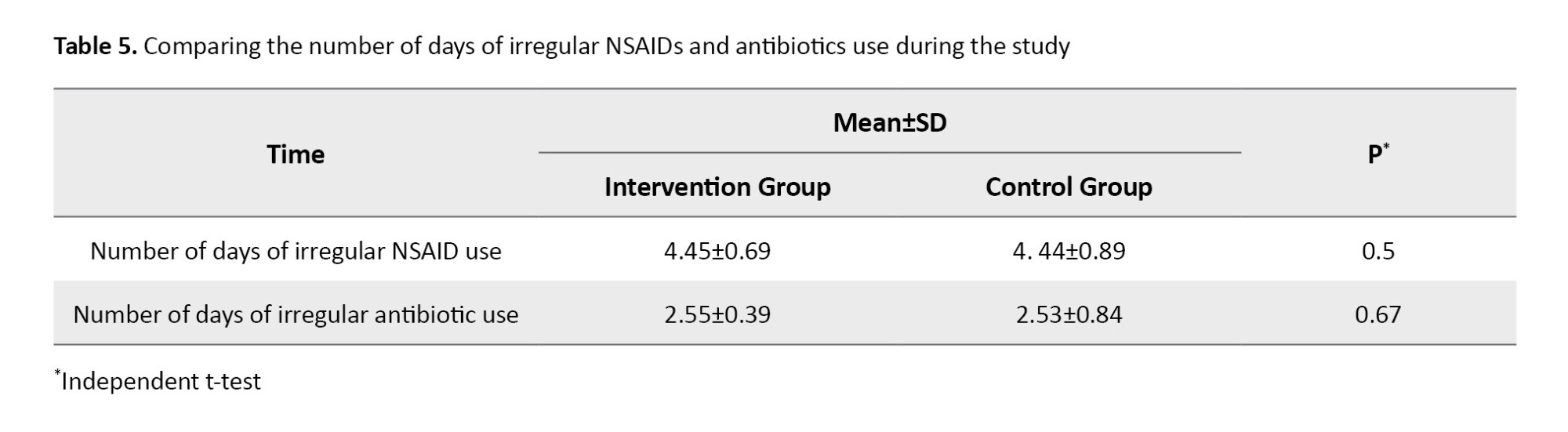
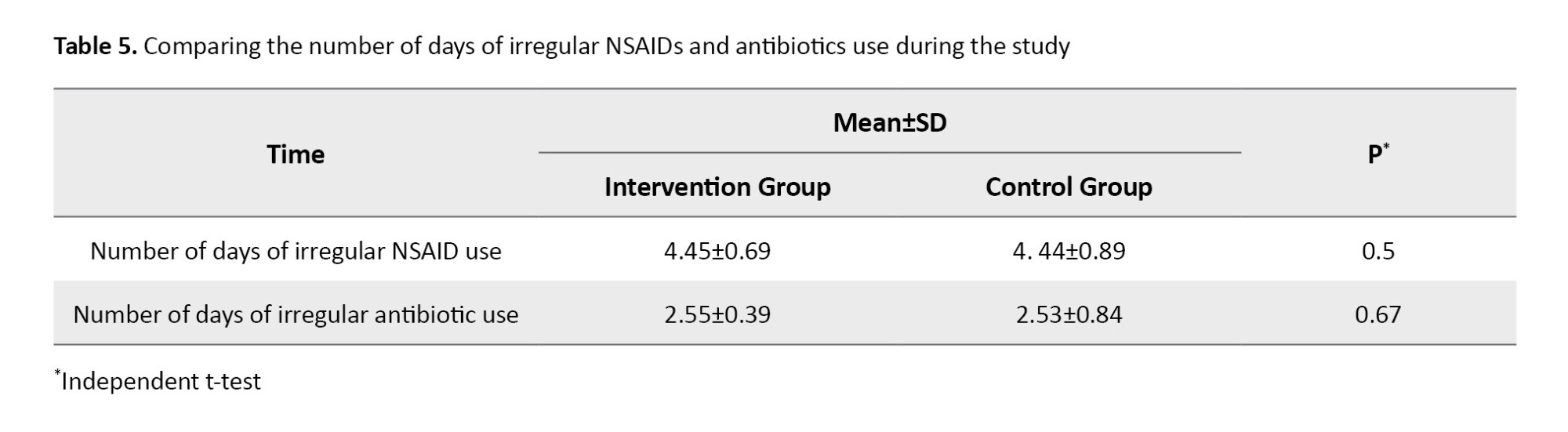
The results of the independent t-test showed that there is no statistically significant difference between the two groups in the mean number of days of NSAIDs and irregular antibiotic use (Table 5).
Discussion
In our study, pain and healing were homogeneous in the two groups before the intervention. Four hours after the intervention, a decrease in pain score and healing was observed in the intervention group. In the intervention group, the trend of changes in pain score and healing significantly differed at four time points: Before the intervention, 4 hours, 5 days, and 10 days after the intervention. The decrease in the mean pain score and enhancement in healing indicate that ODBC has lessened pain intensity and promoted healing within the intervention group. These changes were not observed in the control group.
The evaluation of the effect of quantity and quality of secondary active ingredients in the roots of ODB plant showed that the total amount of flavonoids in the roots is higher than the phenolic compounds, and they practically lack anthocyanins. Its high level of flavonoid as an anti-inflammatory, antioxidant, disinfectant, anti-pathogen, and free radical inhibitor indicates that it can prevent and treat infectious, cardiovascular, and cancer diseases [38, 39]. A study has been conducted in Iran to determine the effect of ODB root on stomach cancer. Since the root of ODB is used as an antiseptic and anti-inflammatory to healing wounds, their purpose was to investigate the cytotoxic and anticancer effects of ODB in laboratory conditions. Three periods (24, 48, and 72 hours) were used to treat gastric cancer and normal fibroblast cell lines L-929. An incubation time of 48 hours with 64 μg/mL showed the best effect on the cancer cell line, while it was safe for the standard cell line. The results showed that ODB root extract has a cytotoxic and safe impact on gastric cancer cell lines and normal cells in 48-hour treatment periods. So, it can be an effective anticancer agent (stomach cancer) [35]. In another study, the anti-inflammatory effect of ODB was investigated using ODB ointment to prevent phlebitis caused by venous catheter placement. Their study showed a decrease in the incidence of phlebitis in the first 12 hours in the intervention group compared to the control group [40, 41]. In our study, the significant difference obtained between the two groups, which shows the improvement of healing and the reduction of pain in the episiotomy area in the intervention group, is attributed to the antimicrobial and anti-inflammatory properties of ODB, which results from the migration of leukocytes to the wound area. It prevents and inhibits inflammatory substances or reduces the mediating factors of inflammation. This effect is similar to Rosemary cream, which is used to heal the episiotomy wound and has improved the process of episiotomy healing during the first 10 days after delivery in the intervention group.
Regarding olive oil as one of the ingredients of this ointment, a study single-blind clinical trial was conducted to investigate the effect of olive oil sitting bath on the healing of perineal wounds after delivery on 60 eligible mothers who had an episiotomy or first or second-grade episiotomy. Data were collected using demographic information, the REEDA tool, and VAS before the intervention, 2 hours later, 5 days, and 10 days after. The results demonstrated the effect of olive oil sitting bath between the two groups 5 days and 10 days after the intervention, but 2 hours after the intervention, no statistically significant difference was found between the two groups [37].
Another component of ODBC ointment was beeswax. There are many studies on the use of honey in healing wounds. The acidic pH of honey, between 3.2 and 4.5, causes the healing of wounds. In addition, the sugar naturally present in honey causes water to be drawn out of the damaged tissues based on the mechanism of the osmotic effect. Therefore, the swelling decreases. It increases lymph flow to heal the wound. Sugar also draws water out of bacterial cells, which can prevent them from multiplying. Healing wounds with honey due to its antibacterial effect so that honey kills the bacteria that normally reside in the wound. Bacteria such as methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococci exist in wounds [36]. In another study, using honey cream or curcumin alone did not reduce the pain intensity, but their combinations (ODB, honey, and curcumin) reduced the pain intensity [22]. In a study where honey was combined with sesame oil and camphor, it positively affected the healing process of pressure ulcers in diabetic people [25]. In another study, ODBC ointment (Sanable Darou) was used with the aim of its effect on wound healing and pain decrease after hemorrhoidectomy. The results demonstrated that pain after hemorrhoidectomy at 4 time points (4, 12, 24 hours, and 7 days) after surgery with ODBC ointment with a dose of 2 g every 8 hours in the intervention group compared to the placebo group has reduced the intensity of pain and burning in the surgical wound. The rapid action of ODBC ointment is attributed to its potent anti-inflammatory properties. Our study observed a decrease in pain and enhancement in healing within the intervention group after 4 hours, at 5 days, and 10 days post-intervention, compared to the placebo group [42]. Our study observed a reduction in pain and improvement in healing within the intervention group at 4 hours, 5 days, and 10 days following the intervention.
In episiotomy or hemorrhoidectomy wounds where the wound is close to the urethra and anus, pain relief reduces constipation and urinary retention. Aloe vera is one of the other plants that have anti-inflammatory effects, such as ODBC. Beta-sitosterol, as one of the components of aloe vera, increases the expression of the vascular endothelial growth factor and its receptor in the wound site, increasing angiogenesis and better healing of damaged tissues. On the other hand, vitamins E and C in Aloe vera affect the wound-healing process by increasing collagen production as an anti-inflammatory [43]. A study utilized Aloe vera to reduce inflammation and alleviate pain following hemorrhoidectomy surgical wounds. The study findings positively impacted wound healing and pain relief within the intervention group [44]. The analgesic effects of ODB are not yet known. In other words, compounds that are effective on pain receptors have not been found at the root of ODB. Hence, the analgesic effects of ODB have a secondary mechanism. Increased tissue perfusion and blood supply reduce pain by accelerating wound healing and healing with anti-inflammatory effects [45].
One of the limitations of our study was assessing participants’ adherence to medication usage, which was addressed by implementing a checklist and conducting follow-up phone calls with the researcher. The large sample and double-blind, placebo-controlled clinical trial design are strengths of our study.
Using an ointment containing ODB root extract, beeswax, and olive oil positively impacted the healing process of the episiotomy wound and effectively reduced pain intensity in that area. Given the significance of minimizing both short-term and long-term complications stemming from incomplete wound healing, along with the absence of adverse effects associated with this treatment, as well as the potential for cost reduction and the growing acceptance of herbal medicine, this approach may be considered as a viable alternative for reducing pain intensity and promoting the wound healing process.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Alborz University of Medical Sciences, Karaj, Iran (Code: ABZUMS.REC.1396.213). The study was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20180110038302N2). Written informed consent was obtained from all the participants.
Funding
This study was sponsored by the Research Deputy Chancellor of Alborz University of Medical Sciences, Karaj, Iran.
Authors' contributions
Study design: Kourosh Kabir and Mansoureh Yazdkhasti; Data analysis: Kourosh Kabir: Data collection: Shekoufee Tourkashvand; Data management: Zahra Mehdizadeh Tourzani; Supervision: Mansoureh Yazdkhasti; writing the original draft Zahra Mehdizadeh Tourzani and Shekoufee Tourkashvand; Review and editing: Kourosh Kabir and Mansoureh Yazdkhasti.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors highly appreciate the Vice President for Research at Alborz University of Medical Sciences, Karaj, Iran, for his support, as well as the study participants and the personnel of the Postpartum Ward, Department of Gynecology, Kamali Educating Hospital, especially Sanable Darou Herbal Pharmaceutical Company who kindly assisted us in conducting this research.
References
Episiotomy is performed to facilitate efficient delivery, minimize severe injuries to the vagina and perineum, alleviate pressure on the cervix, and accelerate the delivery process in challenging circumstances [1, 2]. Despite the World Health Organization’s (WHO) recommendation to limit episiotomies in complicated vaginal deliveries, such as breech births, shoulder dystocia, instrumental delivery, fetal distress, and in women with female genital circumcision [2], the rates of episiotomy have remained high in developing countries [3-5]. The prevalence of episiotomy is estimated to be 50% in America, 31% in China, and 41.5% in Iran [4, 6].
The pelvic floor muscles and fascia provide critical support to prevent sagging of pelvic organs, supporting the proper function of the vagina, bladder, uterus, and rectum. Mis-timed episiotomy or incomplete healing can weaken or damage these muscles, resulting in short-term or long-term complications such as urinary incontinence, gas, or stool issues. Therefore, promoting perineal healing is crucial to uphold pelvic floor strength, tissue continuity, and uniformity to avert episiotomy-related complications [7].
Pain or incomplete healing of the episiotomy wound can instill fear in mothers about vaginal delivery and lead to a preference for cesarean sections. This pain and incomplete healing can disrupt a mother’s peace, hinder her enjoyment of childbirth, make her feel inadequate in caring for her baby and performing daily activities, and contribute to diminished sexual performance in the postpartum period [8-10].
The management of postpartum pain resulting from episiotomy and tears can involve various treatments such as using Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), intravenous and epidural narcotics, local anesthetic sprays, as well as other measures like hot or cold-water basins, ultrasonic waves, exercise therapy, massage, acupuncture, distraction, hypnotism, relaxation, and herbal treatment [11, 12]. The use of medicinal plants as remedies and dietary supplements to enhance overall health and medical treatment has garnered considerable attention [12-14]. Herbal medicine, a subset of complementary medicine, has been part of Iran’s long history of using medicinal plants [15, 16]. Various plants in Iran, including frankincense [17], green tea [18], Myrtus communis [19], Pistacia atlantica [20], Aloe vera [21], honey, olive, and curcumin [22], have been utilized to heal episiotomy wounds. Additionally, the root of the Onosma dichroanthum Boiss (ODB) plant, known for its anti-inflammatory and wound-healing properties due to its alkannin/shikonin (A/S) content, has traditionally been used to treat burn wounds [23-28]. Numerous studies have demonstrated the positive effects of ODB, particularly in pain reduction and wound healing for surgical wounds such as those from hemorrhoidectomy. ODB is one of the herbal medicines used in ointments, often combined with olive oil and beeswax for enhanced efficacy. Its properties, including disinfectant, antibacterial, antioxidant, anti-inflammatory, and wound-healing effects, make this herbal medicine native to Iran notable [27-37]. However, there is a lack of studies in Iran investigating the effectiveness of ODB Combined (ODBC) ointment in treating episiotomy wounds. Therefore, this study aims to assess the efficacy of ODBC ointment in healing and managing episiotomy pain intensity in primiparous women.
Materials and Methods
This double-blind, placebo-controlled clinical trial study was conducted on 190 eligible women in a therapeutic education center in Karaj City, Iran, from December 2022 to March 2023. According to Lavaf et al. study [36], the trial was designed to have 190 patients (95 in each group) using G*Power software (USA), considering 90% power, significance level (α) of 0.05, effect size (d) of 0.5, two-sided, allocation ratio (N2/N1) of 1 and 10% loss to follow up. The inclusion criteria were Iranian primiparous women aged 18 to 35 years, with mediolateral episiotomy, gestational age ≥37 weeks, no history of taking psychotropic or narcotic drugs, no alcohol addiction, no instrumental delivery such as forceps or a ventouse suction cup, no vulvovaginal inflammation or infection, no gestational or overt diabetes, without rupture of the membrane for more than 18 hours, and singleton pregnancy. The exclusion criterion was sensitivity to ointment.
For allocation concealment, the medications and placebos were put in sealed opaque envelopes sequentially. Randomized and prepared envelopes were done by someone not involved in sampling and data analysis. In the present study, observers and participants were blinded.
The intervention group received the leading ointment containing ODBC root extract, beeswax, and olive oil. This ointment is produced by Sanable Darou Herbal Pharmaceutical Company under the brand name ODBC with registration number SMMP80102011 and a standard hologram. This ccombined ointment is distributed in official pharmacies all over Iran and is used to heal diabetic foot ulcers.
After getting the approval of the Ethics Committee of Alborz University of Medical Sciences and registering the study on the Iranian Registry of Clinical Trials (IRCT) website, eligible participants entered the study voluntarily after the researcher explained the study’s objectives and obtained their written consent. The researcher completed the demographic and gestational characteristics based on the participants’ medical records. They were assigned to the intervention and control groups based on block randomization using Random Allocation Software (RAS).
In the intervention group, the initial intervention was conducted by a trained midwife, starting 4 hours post-delivery, once every eight hours (three times a day), and continuing until 10 days post-delivery in the Postpartum Department. The procedure involved cleansing the episiotomy wound with physiological saline. Subsequently, the wound was dried using sterile gauze. Following this, ODBC ointment was applied to the episiotomy area using sterile gloves, with a dosage equivalent to the size of an adult’s knuckle (5 mm or 2 g) every 8 hours. Finally, the treated area was covered with sterile gauze. Then, participants used sanitary pads to remove secretions after delivery. In the hospital, participants were taught how to use the ointment after discharge. Because the wound is close to the urethra or anus, mothers were asked to dry the area with a hair dryer after urinating or defecating, use sterile gauze and a new sanitary pad, and continue applying the ointment.
The placebo ointment was prepared by a fellow pharmacist at the Pharmacy Faculty of Alborz University of Medical Sciences. The ointment in the intervention group comprised starch devoid of active ingredients and side effects [36]. It was formulated to possess characteristics such as essence, color, consistency, and weight closely resembling the original ointment. In the control group, placebo ointment was used the same way as in the intervention group. It should be noted that no ointment is routinely used for episiotomy repair. The participants of the two groups were given a checklist to indicate complications or other cases and the frequency of ointment use. The participants were contacted once a day to report their adherence to the use of the ointment or the presence of complications from the use of the ointment and the irregular use of antibiotics or NSAIDs. Five participants in the intervention group and four in the control group lost to follow-up (Figure 1). The participants visited the clinic on the fifth and tenth day after delivery. The intensity of pain and healing was recorded by two observers who were not members of the research team and had received the necessary training (two experienced midwives) in the women’s clinic affiliated in Educational Therapeutic Hospital. The agreement between the two observers was measured by the kappa index (κ=0.8).
Data were collected using demographics, gestational characteristics, and irregular use of antibiotics and NSAIDs during the study and the Redness, Edema, Ecchymosis, Discharge, Approximation (REEDA) checklist and Visual Analog Scale (VAS).
The REEDA scale is a tool that assesses the inflammatory process and tissue healing in the perineal trauma through the evaluation of five items of healing: Redness (hyperemia), edema, ecchymosis, discharge, and approximation of the wound edges (coaptation). For each assessed item, a score ranging from 0 to 3 can be assigned by the health care provider. A higher score indicates a greater level of tissue trauma. The maximum value of 15 means the worst perineum healing outcome [30]. The REEDA scale is a tool for assessing perineal healing primarily developed by Davidson [31]. In Iran, this scale has been confirmed and also its validity and reliability [33]. This scale has been used in many Iranian studies [32, 33]. Episiotomy pain status was assessed using a standardized VAS. This tool measures the pain score from 0 (no pain) to 10 (the most pain amount) [32, 34].
The study data were collected from two groups across 4 time points: Before the intervention (baseline), 4 hours, 5 days, and 10 days after the intervention. In this double-blind study, primiparous mothers and research assistants were blinded to allocating intervention and control group participants. The chi-square test was used for qualitative variables. Statistical results from the quantitative data were presented with Mean±SD. The Kolmogorov-Smirnov test assessed data normality. The Mann-Whitney and Friedman nonparametric tests were used for variables with non-normal distribution. An independent parametric t-test was used for variables with the normal distribution. The significance level was set at less than 0.05. Missing data management was done using Generalized Estimating Equations (GEE) and random assumption. Statistical analyses were done with SPSS software, version 21 (IBM Corporation, USA).
Results
This study analyzed the demographic characteristics and other variables of 190 participants, with 95 participants in each group.
The intervention and control groups were homogeneous regarding maternal age, Body Mass Index (BMI), gestational age, number of pregnancies, birth weight, episiotomy incision size, number of pads used for bleeding, baseline pain, and healing scores. Variables of maternal age, body mass index, gestational age, number of pregnancies, birth weight, episiotomy incision size, and number of pads used for bleeding had normal distribution. Baseline pain and healing scores had a non-normal distribution (Table 1).
The chi-square test results showed no statistically significant differences between the two groups regarding socioeconomic status, occupation, and education level (Table 2).
Based on the Mann-Whitney test, there was a statistically significant (P=0.001) difference between the two groups in the score of pain and healing 4 hours after the intervention compared to before the intervention (Table 3).
In the intervention group, the results of the Friedman test showed a trend of statistically significant changes in the mean score of pain and healing at 4 time points: Before the intervention, 4 hours, 5 days, and 10 days after the intervention (P=0.001). No statistically significant difference was observed in the control group (Table 4).
In Figure 2, on the horizontal axis, number 1 represents before the intervention, number 2 represents 4 hours, number 3 represents 5 days after, and number 4 represents 10 days after the intervention and the mean pain scores are on the vertical axis.
In Figure 3, on the horizontal axis, number 1 represents before the intervention, number 2 represents 4 hours, number 3 represents 5 days after, and number 4 represents 10 days after the intervention and the mean healing scores are on the vertical axis.
The results of the independent t-test showed that there is no statistically significant difference between the two groups in the mean number of days of NSAIDs and irregular antibiotic use (Table 5).
Discussion
In our study, pain and healing were homogeneous in the two groups before the intervention. Four hours after the intervention, a decrease in pain score and healing was observed in the intervention group. In the intervention group, the trend of changes in pain score and healing significantly differed at four time points: Before the intervention, 4 hours, 5 days, and 10 days after the intervention. The decrease in the mean pain score and enhancement in healing indicate that ODBC has lessened pain intensity and promoted healing within the intervention group. These changes were not observed in the control group.
The evaluation of the effect of quantity and quality of secondary active ingredients in the roots of ODB plant showed that the total amount of flavonoids in the roots is higher than the phenolic compounds, and they practically lack anthocyanins. Its high level of flavonoid as an anti-inflammatory, antioxidant, disinfectant, anti-pathogen, and free radical inhibitor indicates that it can prevent and treat infectious, cardiovascular, and cancer diseases [38, 39]. A study has been conducted in Iran to determine the effect of ODB root on stomach cancer. Since the root of ODB is used as an antiseptic and anti-inflammatory to healing wounds, their purpose was to investigate the cytotoxic and anticancer effects of ODB in laboratory conditions. Three periods (24, 48, and 72 hours) were used to treat gastric cancer and normal fibroblast cell lines L-929. An incubation time of 48 hours with 64 μg/mL showed the best effect on the cancer cell line, while it was safe for the standard cell line. The results showed that ODB root extract has a cytotoxic and safe impact on gastric cancer cell lines and normal cells in 48-hour treatment periods. So, it can be an effective anticancer agent (stomach cancer) [35]. In another study, the anti-inflammatory effect of ODB was investigated using ODB ointment to prevent phlebitis caused by venous catheter placement. Their study showed a decrease in the incidence of phlebitis in the first 12 hours in the intervention group compared to the control group [40, 41]. In our study, the significant difference obtained between the two groups, which shows the improvement of healing and the reduction of pain in the episiotomy area in the intervention group, is attributed to the antimicrobial and anti-inflammatory properties of ODB, which results from the migration of leukocytes to the wound area. It prevents and inhibits inflammatory substances or reduces the mediating factors of inflammation. This effect is similar to Rosemary cream, which is used to heal the episiotomy wound and has improved the process of episiotomy healing during the first 10 days after delivery in the intervention group.
Regarding olive oil as one of the ingredients of this ointment, a study single-blind clinical trial was conducted to investigate the effect of olive oil sitting bath on the healing of perineal wounds after delivery on 60 eligible mothers who had an episiotomy or first or second-grade episiotomy. Data were collected using demographic information, the REEDA tool, and VAS before the intervention, 2 hours later, 5 days, and 10 days after. The results demonstrated the effect of olive oil sitting bath between the two groups 5 days and 10 days after the intervention, but 2 hours after the intervention, no statistically significant difference was found between the two groups [37].
Another component of ODBC ointment was beeswax. There are many studies on the use of honey in healing wounds. The acidic pH of honey, between 3.2 and 4.5, causes the healing of wounds. In addition, the sugar naturally present in honey causes water to be drawn out of the damaged tissues based on the mechanism of the osmotic effect. Therefore, the swelling decreases. It increases lymph flow to heal the wound. Sugar also draws water out of bacterial cells, which can prevent them from multiplying. Healing wounds with honey due to its antibacterial effect so that honey kills the bacteria that normally reside in the wound. Bacteria such as methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococci exist in wounds [36]. In another study, using honey cream or curcumin alone did not reduce the pain intensity, but their combinations (ODB, honey, and curcumin) reduced the pain intensity [22]. In a study where honey was combined with sesame oil and camphor, it positively affected the healing process of pressure ulcers in diabetic people [25]. In another study, ODBC ointment (Sanable Darou) was used with the aim of its effect on wound healing and pain decrease after hemorrhoidectomy. The results demonstrated that pain after hemorrhoidectomy at 4 time points (4, 12, 24 hours, and 7 days) after surgery with ODBC ointment with a dose of 2 g every 8 hours in the intervention group compared to the placebo group has reduced the intensity of pain and burning in the surgical wound. The rapid action of ODBC ointment is attributed to its potent anti-inflammatory properties. Our study observed a decrease in pain and enhancement in healing within the intervention group after 4 hours, at 5 days, and 10 days post-intervention, compared to the placebo group [42]. Our study observed a reduction in pain and improvement in healing within the intervention group at 4 hours, 5 days, and 10 days following the intervention.
In episiotomy or hemorrhoidectomy wounds where the wound is close to the urethra and anus, pain relief reduces constipation and urinary retention. Aloe vera is one of the other plants that have anti-inflammatory effects, such as ODBC. Beta-sitosterol, as one of the components of aloe vera, increases the expression of the vascular endothelial growth factor and its receptor in the wound site, increasing angiogenesis and better healing of damaged tissues. On the other hand, vitamins E and C in Aloe vera affect the wound-healing process by increasing collagen production as an anti-inflammatory [43]. A study utilized Aloe vera to reduce inflammation and alleviate pain following hemorrhoidectomy surgical wounds. The study findings positively impacted wound healing and pain relief within the intervention group [44]. The analgesic effects of ODB are not yet known. In other words, compounds that are effective on pain receptors have not been found at the root of ODB. Hence, the analgesic effects of ODB have a secondary mechanism. Increased tissue perfusion and blood supply reduce pain by accelerating wound healing and healing with anti-inflammatory effects [45].
One of the limitations of our study was assessing participants’ adherence to medication usage, which was addressed by implementing a checklist and conducting follow-up phone calls with the researcher. The large sample and double-blind, placebo-controlled clinical trial design are strengths of our study.
Using an ointment containing ODB root extract, beeswax, and olive oil positively impacted the healing process of the episiotomy wound and effectively reduced pain intensity in that area. Given the significance of minimizing both short-term and long-term complications stemming from incomplete wound healing, along with the absence of adverse effects associated with this treatment, as well as the potential for cost reduction and the growing acceptance of herbal medicine, this approach may be considered as a viable alternative for reducing pain intensity and promoting the wound healing process.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Alborz University of Medical Sciences, Karaj, Iran (Code: ABZUMS.REC.1396.213). The study was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20180110038302N2). Written informed consent was obtained from all the participants.
Funding
This study was sponsored by the Research Deputy Chancellor of Alborz University of Medical Sciences, Karaj, Iran.
Authors' contributions
Study design: Kourosh Kabir and Mansoureh Yazdkhasti; Data analysis: Kourosh Kabir: Data collection: Shekoufee Tourkashvand; Data management: Zahra Mehdizadeh Tourzani; Supervision: Mansoureh Yazdkhasti; writing the original draft Zahra Mehdizadeh Tourzani and Shekoufee Tourkashvand; Review and editing: Kourosh Kabir and Mansoureh Yazdkhasti.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors highly appreciate the Vice President for Research at Alborz University of Medical Sciences, Karaj, Iran, for his support, as well as the study participants and the personnel of the Postpartum Ward, Department of Gynecology, Kamali Educating Hospital, especially Sanable Darou Herbal Pharmaceutical Company who kindly assisted us in conducting this research.
References
- Ghulmiyyah L, Sinno S, Mirza F, Finianos E, Nassar AH. Episiotomy: History, present and future - a review. J Matern Fetal Neonatal Med. 2022; 35(7):1386-91. [DOI:10.1080/14767058.2020.1755647] [PMID]
- Navi Nezhad M, Abedian Z, Asili J, Esmaeili H, Vatanchi A. [Effect of alpha ointment (fundermol) on episiotomy wound healing in primiparous women (Persian)]. Iran J Obstet Gynecol Infertil. 2017; 20(4):58-65. [DOI:10.22038/ijogi.2017.8983]
- Yang J, Bai H. Knowledge, attitude and experience of episiotomy practice among obstetricians and midwives: A cross-sectional study from China. BMJ Open. 2021; 11(4):e043596. [DOI:10.1136/bmjopen-2020-043596] [PMID]
- Rasouli M, Keramat A, Khosravi A, Mohabatpour Z. Prevalence and factors associated with episiotomy in Shahroud City, northeast of Iran. Int J Womens Health Reprod Sci. 2016; 4(3):125-9. [DOI:10.15296/ijwhr.2016.29]
- Lam KW, Wong HS, Pun TC. The practice of episiotomy in public hospitals in Hong Kong. Hong Kong Med J. 2006; 12(2):94-8. [PMID]
- Akhlaghi F, Sabeti Baygi Z, Miri M, Najaf Najafi M. Effect of perineal massage on the rate of episiotomy. J Family Reprod Health. 2019; 13(3):160-6. [PMID]
- Carter AG, Creedy DK, Sidebotham M. Critical thinking skills in midwifery practice: Development of a self-assessment tool for students. Midwifery. 2017; 50:184-92. [DOI:10.1016/j.midw.2017.04.010] [PMID]
- Adama O, Natacha LB, Smaila O, Alexis SY, Francoise MT, Charlemagne OM, et al. Episiotomy: Epidemiological aspects, indications and prognosis in the Bogodogo Health District. Open J Obstet Gynecol. 2018; 8(13):1354. [DOI:10.4236/ojog.2018.813137]
- Esmaeili A, Parsaei P, Nazer M, Bakhtiari R, Mirbehresi H, Safian Boldaji H. Phytotherapy in burn wound healing: A review of native Iranian Medicinal Plants. J Chem Health Risks. 2023; 13(1):17-29. [Link]
- Konlan KD, Afaya A, Mensah E, Suuk AN, Kombat DI. Non-pharmacological interventions of pain management used during labour; an exploratory descriptive qualitative study of puerperal women in Adidome Government Hospital of the Volta Region, Ghana. Reprod Health. 2021; 18(1):86. [DOI:10.1186/s12978-021-01141-8] [PMID]
- Ijaz SA, Qasim R. Comparison of Rectal diclofenac verses oral mefenamic acid in terms of mean pain score after Episiotomy. Pak J Med Health Sci. 2021; 15:610-2. [Link]
- Kalahroudi MA, Sadat Z, Saberi F. [The efficacy of 2% lidocaine gel versus diclofenac suppository in pain reliving after episiotomy (Persian)]. Koomesh. 2024; 10(4):301-6. [Link]
- Babu SN, Noor A. Bioactive constituents of the genus Aloe and their potential therapeutic and pharmacological applications: A review. J Appl Pharm Sci. 2020; 10(11):133-45. [Link]
- Yahya S, Mehrban Z. [The effect of tea herb cream on wound healing satisfaction and episiotomy pain intensity in primiparous women (double-blind clinical trial) (Persian)]. Iran J Obstet Gynecol Infertil. 2023; 26(2):46-55. [Link]
- Roper JC, Amber N, Wan OYK, Sultan AH, Thakar R. Review of available national guidelines for obstetric anal sphincter injury. Int Urogynecol J. 2020; 31(11):2247-59. [DOI:10.1007/s00192-020-04464-5] [PMID]
- Shirbeigi L, Dalfardi B, Abolhassanzadeh Z, Nejatbakhsh F. Dementia etiologies and remedies in traditional Persian Medicine; A review of medicinal plants and phytochemistry. Curr Drug Metab. 2018; 19(5):414-23. [DOI:10.2174/1389200218666170810170124] [PMID]
- Laki E, Torkzahrani S, Mojab F, Heydari A, Soltani Kermanshahi M. [The effect frankincense ointment on pain intensity and episiotomy wound healing in primiparous women (Persian)]. Iran J Obstet Gynecol Infertil. 2019; 22(2):42-51. [DOI:10.22038/ijogi.2019.13201]
- Shahrahmani H, Kariman N, Jannesari S, Rafieian-Kopaei M, Mirzaei M, Shahrahmani N. The effect of camellia sinensis ointment on perineal wound healing in primiparous women. J Babol Univ Med Sci. 2018; 20(5):7-15. [Link]
- Mirzaee F, Jannesari S, Kariman N, Mojab F, Nasiri M. [The effect of Myrtus communis cream on wound healing and severity of episiotomy pain: Double-blind clinical trial (Persian)]. Iran J Obstet Gynecol Infertil. 2019; 22(8):52-61. [DOI:10.22038/ijogi.2019.13920]
- Moudi Z, Edozahi M, Emami SA, Asili J, Pour MS. Effects of mastic oleoresin on wound healing and episiotomy pain: A mixed methods study. J Ethnopharmacol. 2018; 214:225-31. [DOI:10.1016/j.jep.2017.12.028] [PMID]
- Nazari S, Ezati Arasteh F, Nazari S, Shobeiri F, Shayan A, Parsa P. [Persian)]. Effect of Aloe Vera gel on perineal pain and wound healing after episiotomy among primiparous women: A randomized clinical trial. Iran J Obstet Gynecol Infertil. 2019; 21(11):44-51. [DOI:10.22038/ijogi.2019.12325]
- Nikpour M, Delavar MA, Khafri S, Ghanbarpour A, Moghadamnia AA, Esmaeilzadeh S, et al. The use of honey and curcumin for episiotomy pain relief and wound healing: A three-group double-blind randomized clinical trial. Nurs Midwifery Stud. 2019; 8(2):64-9. [Link]
- Mazandarani M, Moghaddam Z, Zolfaghari MR, Ghaemi EA, Bayat H. Effects of solvent type on phenolics and flavonoids content and antioxidant activities in Onosma dichroanthum Boiss. J Med Plants Res. 2012; 6(28):4481-8. [Link]
- Moghaddam PZ, Zolfaghari MR, Ghaemi EA, Mazandarani M, Mansourian AR, Taheri SA. Negative performance of root extract of Onosma dichroanthum Boiss. on the burn wound healing in an animal model. Arch Clin Microbiol. 2011; 2(5). [Link]
- Aliasl J, Barikbin B, Khoshzaban F, Naseri M, Sedaghat R, Kamalinejad M, et al. Effect of Arnebia euchroma ointment on post-laser wound healing in rats. J Cosmet Laser Ther. 2015; 17(1):41-5. [DOI:10.3109/14764172.2014.968583] [PMID]
- Jabbar AA, Abdullah FO, Hassan AO, Galali Y, Hassan RR, Rashid EQ, et al. Ethnobotanical, phytochemistry, and pharmacological activity of onosma (boraginaceae): An updated review. Molecules. 2022; 27(24):8687. [DOI:10.3390/molecules27248687] [PMID]
- Mohebbi A, Azadi F, Hashemi MM, Askari FS, Razzaghi N. Havachoobe (Onosma dichroanthum Boiss) Root Extract Decreases the Hepatitis B Virus Surface Antigen Secretion in the PLC/PRF/5 Cell Line. Intervirology. 2020; 1-5. [DOI:10.1159/000512140] [PMID]
- Kaur K, Sharma R, Singh A, Attri S, Arora S, Kaur S, et al. Pharmacological and analytical aspects of alkannin/shikonin and their derivatives: An update from 2008 to 2022. Chin Herb Med. 2022; 14(4):511-27. [DOI:10.1016/j.chmed.2022.08.001] [PMID]
- Chierici A, Frontali A. Post-hemorrhoidectomy pain management: The latest news. Rev Recent Clin Trials. 2021; 16(1):32-8. [DOI:10.2174/1574887115666200406122009] [PMID]
- Alvarenga MB, Francisco AA, de Oliveira SM, da Silva FM, Shimoda GT, Damiani LP. Episiotomy healing assessment: Redness, Oedema, Ecchymosis, Discharge, Approximation (REEDA) scale reliability. Rev Lat Am Enfermagem. 2015; 23(1):162-8. [DOI:10.1590/0104-1169.3633.2538] [PMID]
- Davidson N. REEDA: evaluating postpartum healing. J Nurse Midwifery. 1974; 19(2):6-8. [PMID]
- Izadpanah A, Soorgi S, Geraminejad N, Hosseini M. Effect of grape seed extract ointment on cesarean section wound healing: A double-blind, randomized, controlled clinical trial. Complement Ther Clin Pract. 2019; 35:323-8. [DOI:10.1016/j.ctcp.2019.03.011] [PMID]
- Faraji A, Aghdaki M, Hessami K, Hosseinkhani A, Roozmeh S, Asadi N, et al. Episiotomy wound healing by Commiphora myrrha (Nees) Engl. and Boswellia carteri Birdw. in primiparous women: A randomized controlled trial. J Ethnopharmacol. 2021; 264:113396. [DOI:10.1016/j.jep.2020.113396] [PMID]
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017; 389(10070):736-747. [DOI:10.1016/S0140-6736(16)30970-9] [PMID]
- Hashemi MM, Marjani M, Poursharifi N, Marjani A. Effects of Onosma dichroanthum Boiss. root extract on AGS human gastric cancer cell-line. J Basic Clin Physiol Pharmacol. 2021; 33(4):487-92. [DOI:10.1515/jbcpp-2020-0323] [PMID]
- Lavaf M, Simbar M, Mojab F, Alavi Majd H, Samimi M. Comparison of honey and phenytoin (PHT) cream effects on intensity of pain and episiotomy wound healing in nulliparous women. J Complement Integr Med. 2017; 15(1). [DOI:10.1515/jcim-2016-0139] [PMID]
- Behmanesh F, AghaMohammadi A, ZeynalZadeh M, Khafri S. [Effects of olive oil sitz bath on improvement of perineal injury after delivery (Persian)]. Koomesh. 2013; 14(3):e152581. [Link]
- Mohammadi Tofigh A, Hayatollah G, Ayazi K, Hosseinian MA, Nemati Honar B, Safdari F. [Treatment of pressure ulcer in diabetic patients using honey, sesame and campher ointment (Persian)]. ResMed. 2014; 38(3):131-8. [Link]
- Shourab NJ, Irani M, Mirzaei K, Sadeghi T, Mazloum SR, Jamali J. Comparing prenatal and postnatal social support of women with wanted and unwanted pregnancies referring to the health centers of Mashhad, Iran. J Midwifery Reprod Health. 2022; 10(1):3128-34. [DOI:10.22038/jmrh.2021.56256.1682]
- Varaei Sh,Ghafoorzadeh Sh, Kamalnegjad M, Yeganinejad M, Kazemi F, Ebrahim S, et al. [Effect of Arnebia Euchroma poultice on the prevention of peripheral intravenous catheter-related phlebitis: A randomized clinical trial (Persian)]. Hayat. 2018; 24(1):59-70. [Link]
- Hadizadeh-Talasaz F, Mardani F, Bahri N, Rakhshandeh H, Khajavian N, Taghieh M. Effect of rosemary cream on episiotomy wound healing in primiparous women: A randomized clinical trial. BMC Complement Med Ther. 2022; 22(1):226. [DOI:10.1186/s12906-022-03675-1] [PMID]
- Memarbashi E, Nasiri E, Etezadpour M, Hosseinimehr SJ. [Effect of Arnebia euchroma ointment on pain and burning after hemorrhoidectomy: A randomized clinical trial (Persian)]. J Mazandaran Univ Med Sci. 2021; 31(202):38-48. [Link]
- Poylin V, Quinn J, Messer K, Nagle D. Gabapentin significantly decreases posthemorrhoidectomy pain: A prospective study. Int J Colorectal Dis. 2014; 29(12):1565-9. [DOI:10.1007/s00384-014-2018-4] [PMID]
- Ahmed E. Efficacy of aloe vera cream versus transcutanos electrical nervestimulation on post hemmorrhoidectomy pain. International Journal of Medical Science and Public Health. 2013; 2(2):229-35. [DOI:10.5455/ijmsph.2013.2.221-226]
- Xiong H, Huang TY, Chang YL, Su WT. Achyranthes bidentate extracts protect the IL-1β-induced osteoarthritis of SW1353 chondrocytes. J Biosci Bioeng. 2023; 136(6):462-70. [DOI:10.1016/j.jbiosc.2023.09.008] [PMID]
Article Type : Research |
Subject:
Special
Received: 2024/04/13 | Accepted: 2025/02/23 | Published: 2025/06/10
Received: 2024/04/13 | Accepted: 2025/02/23 | Published: 2025/06/10
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |