Wed, Feb 4, 2026
Volume 35, Issue 2 (3-2025)
JHNM 2025, 35(2): 126-132 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hassan Abid G, Kafaei-Atrian M, Sayadi L, Asghari-Jafarabadi M. Treatment Adherence and the Related Factors in Patients With Myocardial Infarction. JHNM 2025; 35 (2) :126-132
URL: http://hnmj.gums.ac.ir/article-1-2335-en.html
URL: http://hnmj.gums.ac.ir/article-1-2335-en.html
1- Master of Science in Nursing, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
2- Assistant Professor, Department of Midwifery, Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran.
3- Associate Professor, Department of Medical Surgical Nursing, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran. ,sayadi00@gmail.com
4- Associate Professor, Biostatistics Unit, Department of Public Health and Preventive Medicine, Faculty of Medicine Nursing and Health Sciences, Monash University, Melbourne, Australia.
2- Assistant Professor, Department of Midwifery, Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran.
3- Associate Professor, Department of Medical Surgical Nursing, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran. ,
4- Associate Professor, Biostatistics Unit, Department of Public Health and Preventive Medicine, Faculty of Medicine Nursing and Health Sciences, Monash University, Melbourne, Australia.
Full-Text [PDF 464 kb]
(288 Downloads)
| Abstract (HTML) (677 Views)
Full-Text: (299 Views)
Introduction
Myocardial Infarction (MI) or “heart attack” is caused by a reduction or complete cessation of blood flow to a part of the myocardium [1]. It is one of the most common heart diseases and the most common cause of death worldwide, accounting for 35% of deaths in the world. This disease has significant complications for the patients and puts a huge cost burden on the patients and the health system [2]. The prevalence of MI in Iraq has been reported to be high. It is one of the first causes of death in Iraq [3].
Treatment adherence refers to the degree to which an individual’s behavior complies with health or treatment recommendations [4] or the instructions of the medical team [5], which can result in decreased complications [6]. The results of a study conducted in Poland in 2018 on assessing the level of treatment adherence in patients with MI treated with percutaneous coronary intervention showed that 59 patients had high adherence (26.7%) and 52 patients had low adherence (23.5%) [7]. Several factors contribute to poor treatment adherence, including socioeconomic factors, treatment-related factors, patient-related factors, disease-related factors, health system factors, and factors related to the healthcare team [8-10].
Training of healthcare providers and the follow-up of patients can increase the level of adherence to treatment in MI patients. It is essential to control the MI and prevent its complications [11]. Considering that heart diseases are the leading cause of mortality worldwide [12], treatment adherence is needed to confirm the validity and generalizability of the results of clinical trials regarding these diseases [13]. The present study aims to determine treatment adherence and related factors among patients with MI at selected hospitals in Hilla, Iraq.
Materials and Methods
This is a cross-sectional study, conducted from September 1 to December 30, 2021. The study population consists of all patients over 18 years of age diagnosed with MI by a cardiologist and had a history of hospitalization due to MI admitted to three teaching hospitals in Hilla city, located in Babylon province of Iraq. The inclusion criteria were the diagnosis of MI for at least six months, no self-reported history of mental illness, congenital abnormality in the heart muscle, or other chronic diseases affecting heart disease. The sample size was calculated based on a study conducted in Iran on the correlation between treatment adherence and health-related quality of life in patients with hypertension (r=-0.25) [14], and considering α=0.05, z(1-α/2)=1.96 and β=0.10 (Z1-β=1.28). In this regard, the sample size was obtained as 132. After multiplying by 2 (as the effect of the sampling plan), the final sample size was 264. A convenience sampling method was used to select participants.
The data collection tools included a demographic form and the coronary artery disease treatment adherence scale (CADTAS). Demographic form surveyed age, sex, marital status, educational level, occupation, number of children, age at the onset of diagnosis, duration of the disease, history of heart attack, number of heart attacks, history of coronary artery reconstruction, underlying diseases, duration of medication use, number of used medications. The CADTAS has 35 items and the dimensions of dietary adherence (items 1-13), healthy lifestyle adherence (items 14-20), medication adherence (items 21-31) and exercise adherence (items 32-35). The items are rated as 1 (never), 2 (rarely), 3 (sometimes), 4 (often) and 5 (always). The total score of the dietary adherence dimension is 13-65; healthy lifestyle adherence, 7-35; medication adherence, 11-55; and adherence to exercise, 4-20. The total score of the questionnaire ranges from 35 to 175, with a high score indicating better adherence to treatment regimen. The CADTAS was developed by Dehghan Nayeri et al. [15]. It is a valid and reliable tool that can be used in different clinical settings. The reliability of the CADTAS in our study, using Cronbach’s alpha, was 0.79. It was tested on 25 participants, who were included in the final sample size. After explaining the study objectives to the participants and obtaining their informed consent to participate in the study, the questionnaires were completed through interviews. The researcher asked the questions and the answers were marked.
Data for qualitative and quantitative variables were presented as frequency (percentage) and Mean±SD, respectively. The normality of the data distribution was assessed and confirmed based on the values of skewness (within ±1.5) and kurtosis (within ±2). The correlation between the continuous variables was estimated using the Pearson correlation test. Independent t-test and analysis of variance (ANOVA) were also used for data analysis. A multivariable general linear model (GLM) was used to assess the relationship between the total CADTAS score and demographic factors. In addition, Wilk’s lambda statistic was calculated for the variables in the GLM. All analyses were conducted in SPSS software, version 16 (SPSS Inc., IL, Chicago, USA), considering P<0.05 as statistically significant.
Results
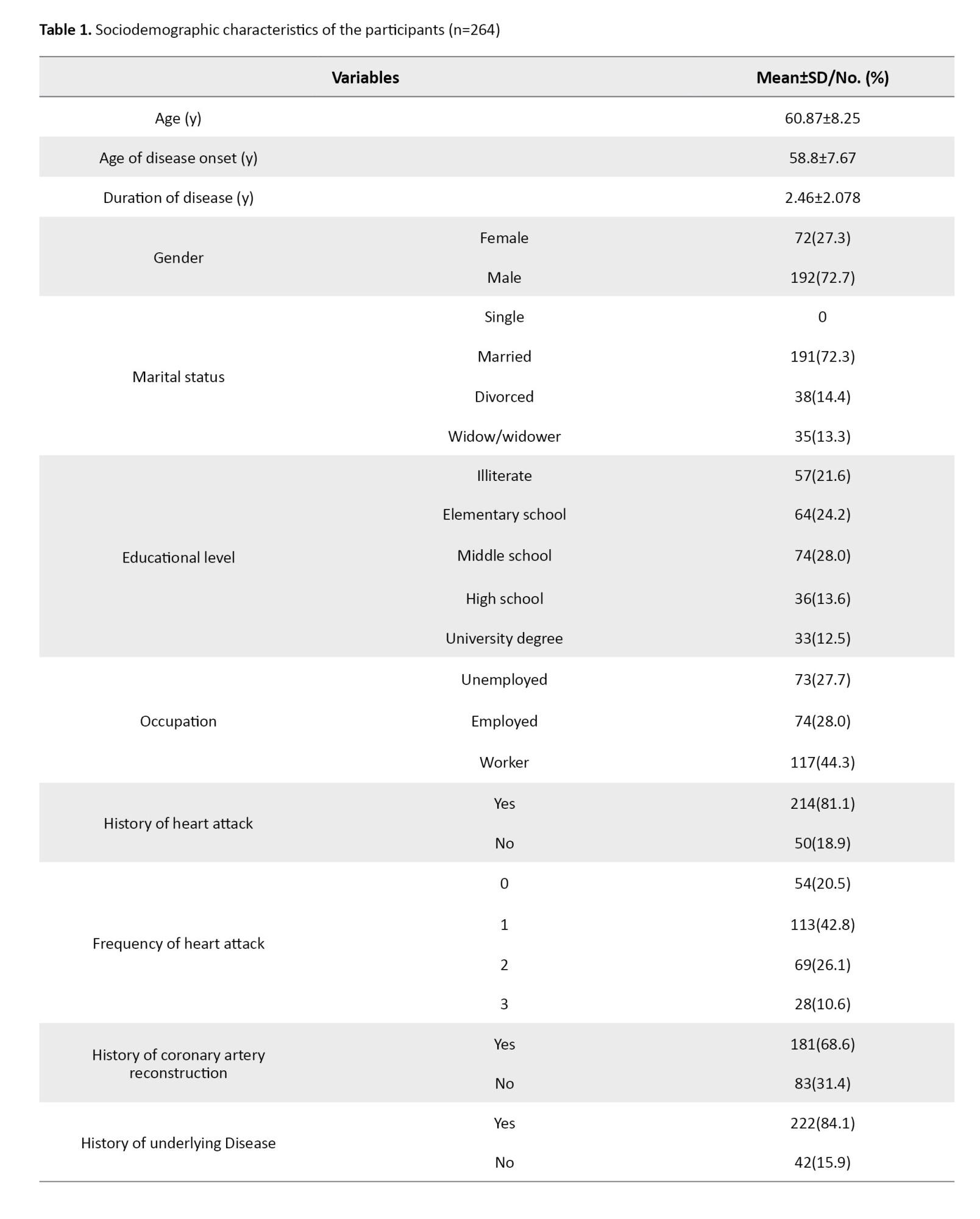
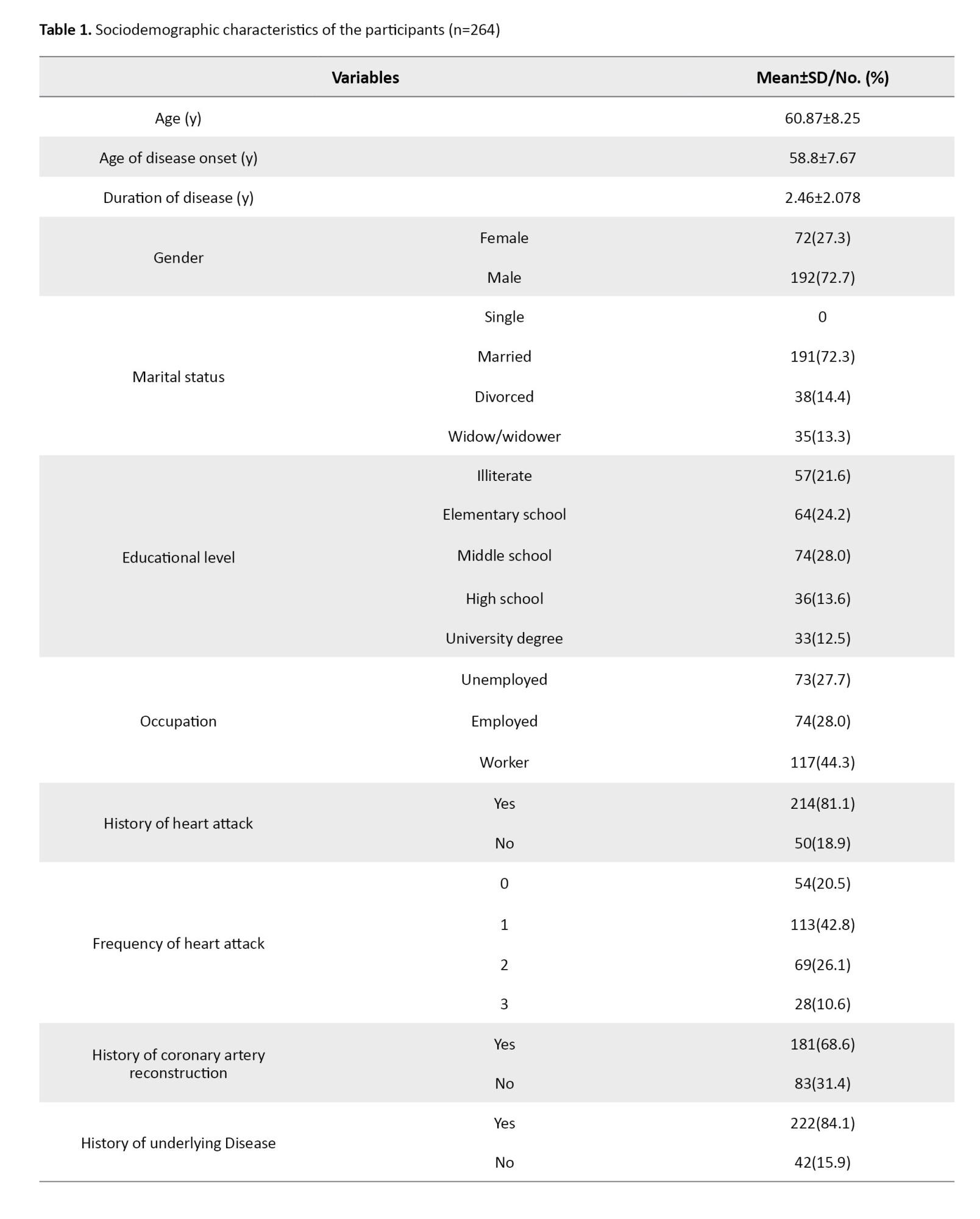
Most of the participants were male, married and workers with a middle school education. Their mean duration of disease was 2.46±2.078 years. Most of them had a history of heart attack (n=214, 81.1%), a history of coronary artery reconstruction (n=181, 68.6%), and a history of underlying diseases (n=222, 84.1%).These results showed in Table 1.
Their mean age at the onset of diagnosis was 58.80±7.67 years and their mean CADTAS score was 92.28±8.01, ranged 35-175. Table 2 shows the scores for the dimensions of CADTAS. The mean dietary adherence score was 35.74±2.87 (out of 65); the healthy lifestyle adherence score was 16.77±3.85 (out of 35); the medication adherence score was 28.38±3.34 (out of 55) and the exercise adherence score was 11.40±2.16 (out of 20).
The CADTAS score had a significant and negative relationship with age (r=-0.225, P=0.001) and age at the onset of diagnosis (r=-0.239, P=0.001), but it had no significant relationships with the duration of disease or the duration of medication use. Also, there were significant differences in the CADTAS score in terms of occupation (P=0.001), history of heart attack (P=0.026) and history of underlying disease (P=0.009). The difference was not significant in terms of marital status.
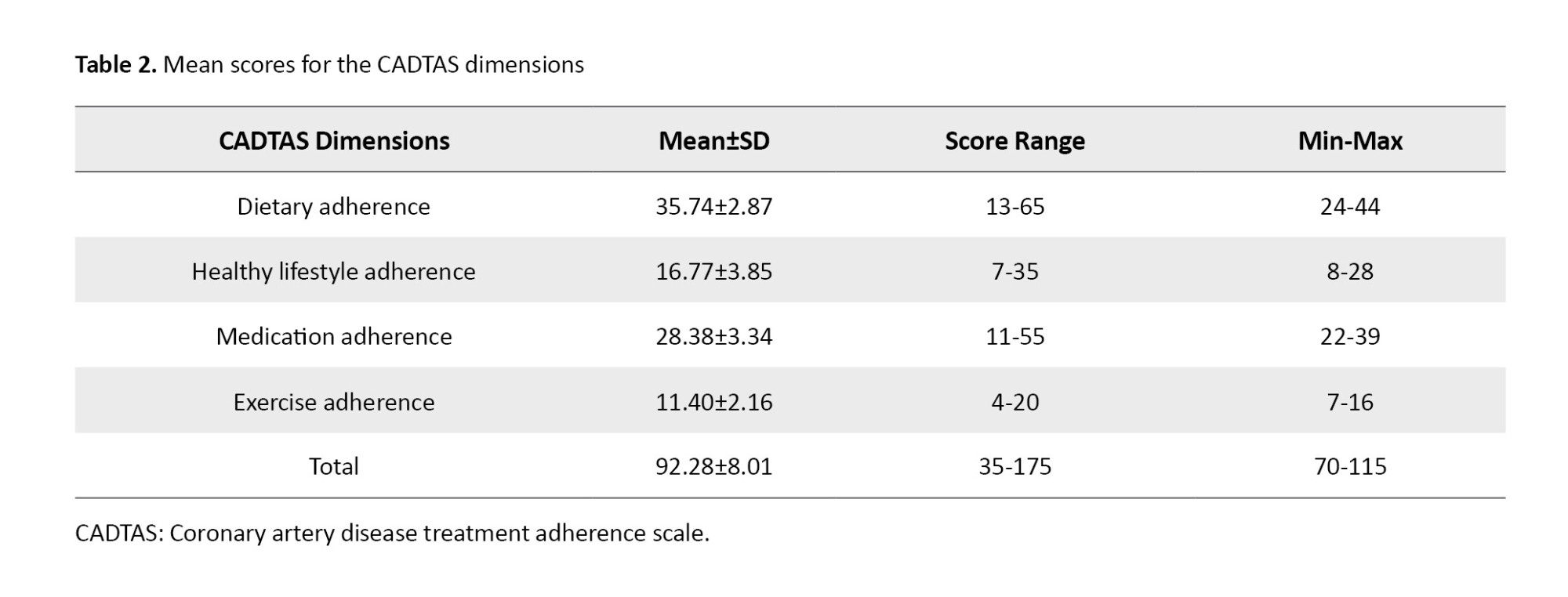
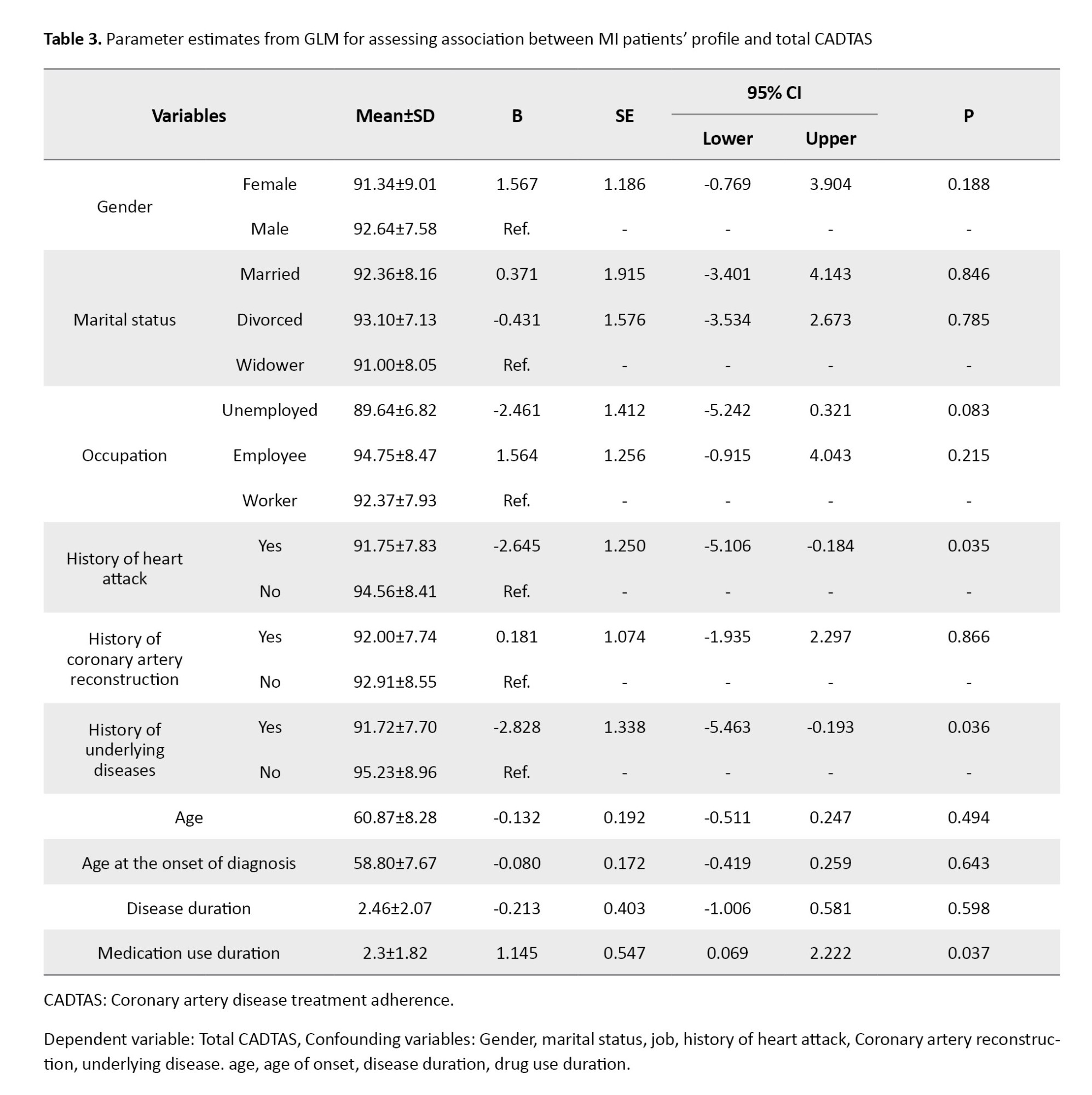
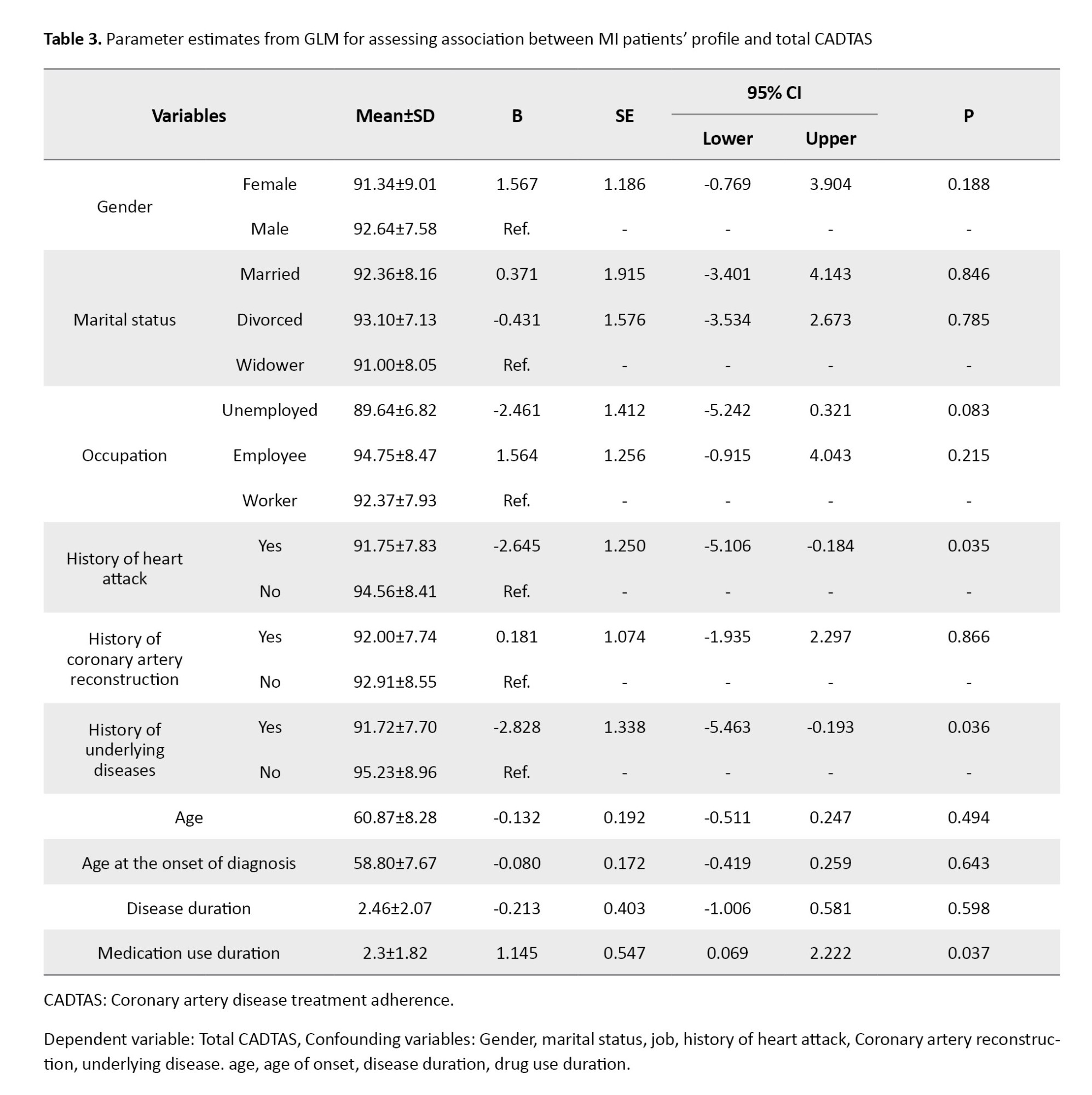
Table 3 shows the results of GLM for finding the demographic characteristics that can predict the total CADTAS score. Gender, marital status, occupation, history of heart attack, history of coronary artery reconstruction, history of underlying diseases, age, age at the onset of diagnosis, disease duration, and medication use duration were entered into the model as binary. The results showed a significant and negative association between a history of heart attack (B=-2.645, 95% CI, -5.106, -0.184, P=0.035) and underlying diseases (B=-2.828, 95%CI, -5.463, -0.193, P=0.036) and the CADTAS score. Also, the medication use duration was positively and significantly associated with the CADTAS score (B=1.145, 95% CI, 0.069, 2.222, P=0.037).
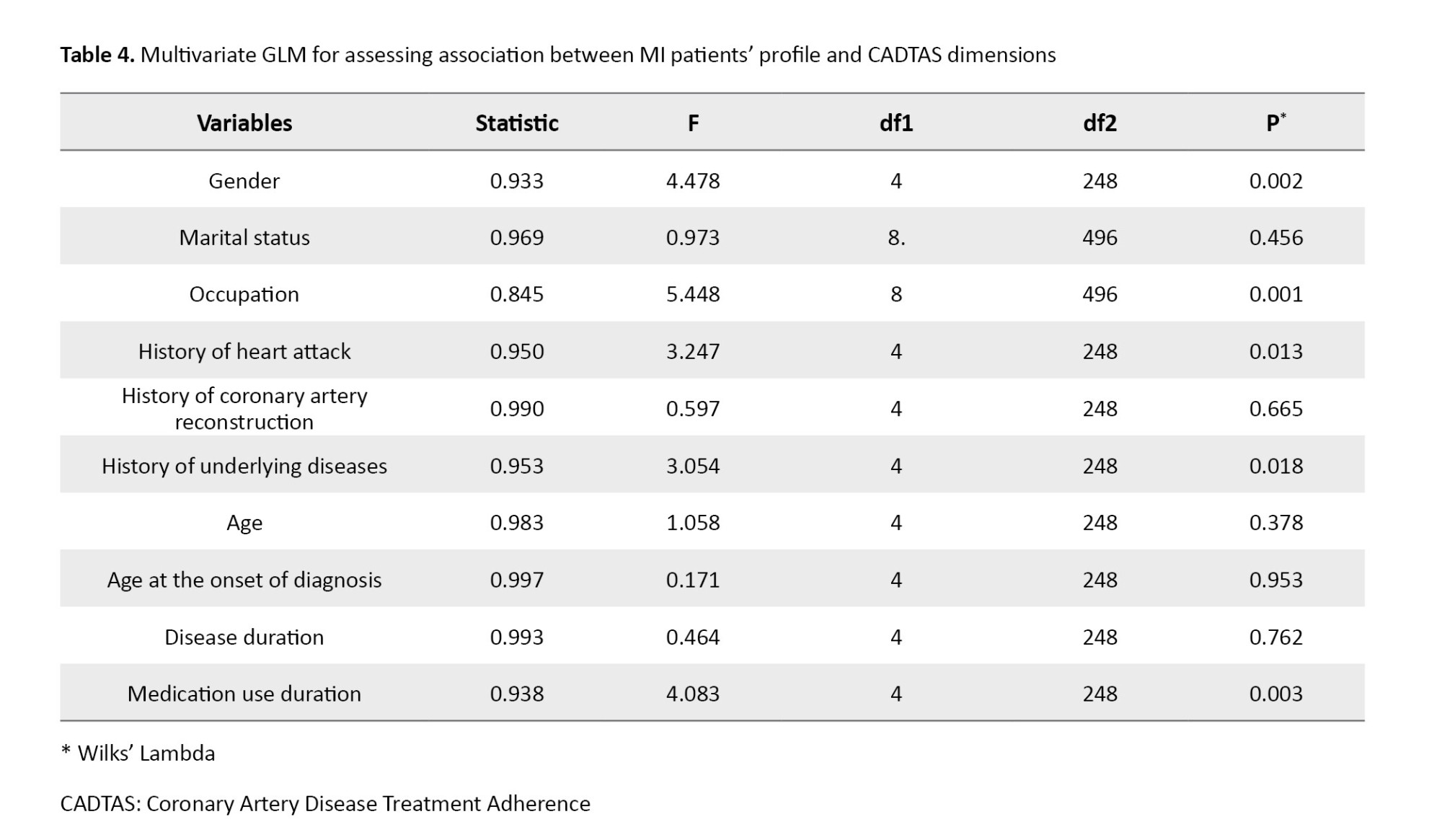
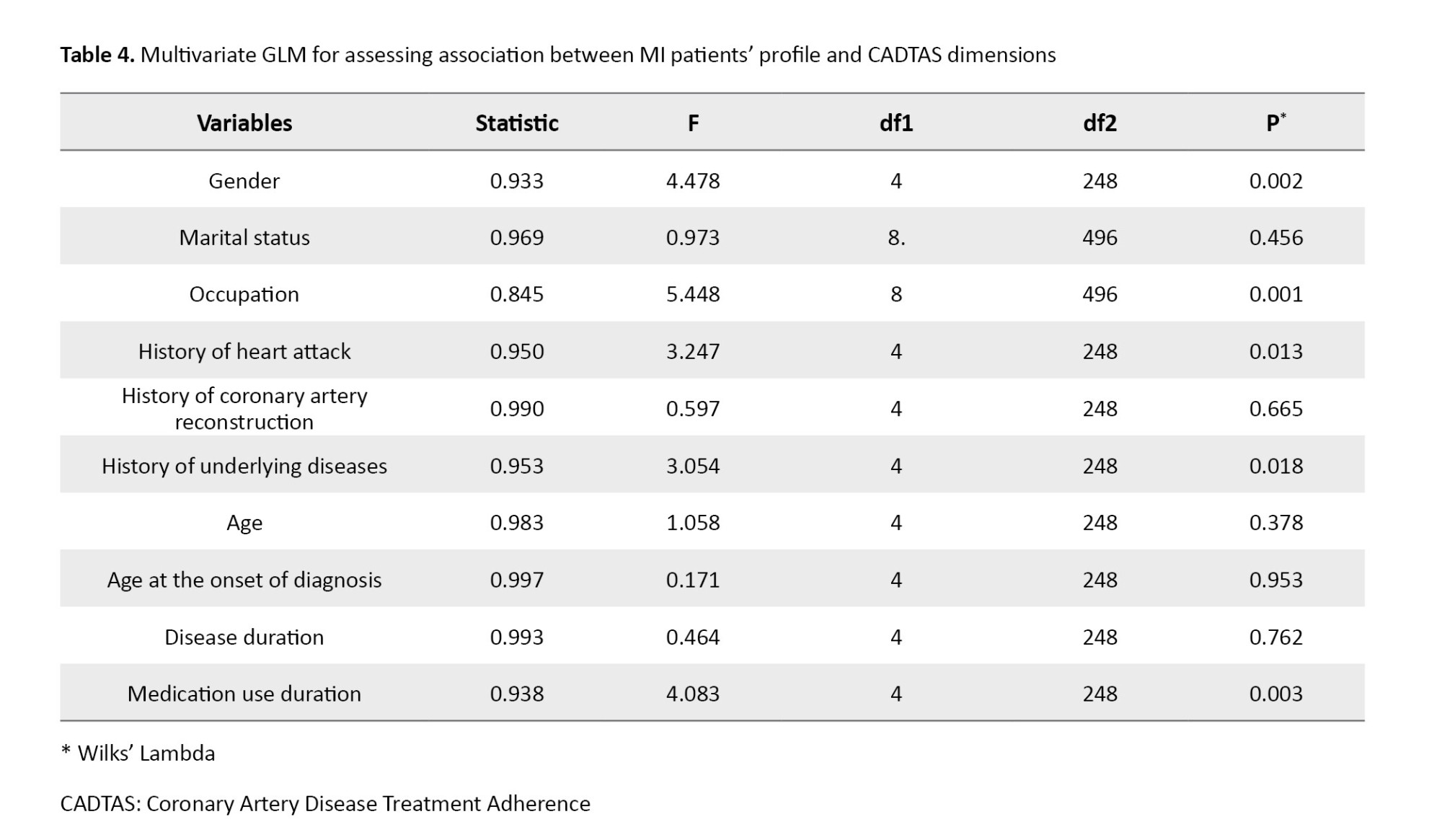
Also, the results showed a significant difference in the total CADTAS score in terms of gender (Wilks’ Lambda =0.933, P=0.002), occupation (Wilks’ Lambda =0.845, P=0.001), history of heart attack (Wilks’ Lambda =0.950, P=0.013), history of underlying diseases (Wilks’ Lambda=0.953, P=0.018), and medication use duration (Wilks’ Lambda=0.938, P=0.003) in the Table 4.
Discussion
The results indicated that the treatment adherence score of patients was 92.28±8.01 ( achieve ranged 70-115). In a study in Brazil, the overall treatment adherence of patients with MI was also moderate [16]. Other studies have reported different levels of treatment adherence. For example, in a study in Poland, adherence to treatment in 25% of MI patients was high [7]. A study conducted in Italy showed that only half of the MI patients had good adherence [17].
Among the study variables, only age and age at the onset of diagnosis had a significant negative relationship with treatment adherence in patients. Treatment adherence was higher in younger patients and in those with the disease onset at younger ages. In addition, there was a significant difference in treatment adherence of patients based on occupation, where unemployed patients had lower treatment adherence compared to the workers and employed patients. It can be said that with increasing age and unemployment, people’s connections with scientific resources and medical centers decrease. Unemployed people may have obstacles due to economic problems. If these patients are connected with their peers who have been under treatment, better results may be achieved. Numerous studies have also shown that adherence to treatment decreases with increasing age [18-20]. A study also reported treatment adherence decreased with an increase in the disease duration [21]. A study showed that the female gender, younger age, new drug prescription, low education level and low-income level were the predictors of non-adherence to treatment [22]. However, a study reported that the disease duration had no effect on treatment adherence [19]. In a study on the effects of medication adherence in hypertensive patients, it was shown that the level of education and occupation had an effect on medication adherence [20]. The reason for this discrepancy can be due to factors such as the difference in the age of participants or other demographic differences.
Overall, the results of this study showed that the mean score obtained by the study samples was higher than the mean score of the tool used to determine the level of compliance. It is essential that nurses educate and follow up these patients and their families to adhere to treatment (healthy lifestyle, medication, healthy diet, and exercise). If adherence to medications increases, it can reduce the negative consequences of MI and thus reduce treatment and household costs. Therefore, it is necessary for the health care system in Iraq to consider this issue and apply strategies to increase the treatment adherence of patients with MI. This study was conducted only in one city in Iraq (Hilla); therefore, the results cannot be generalized to all patients with MI in Iraq. Another limitation was that it was not possible to determine medication adherence objectively by counting medications, measuring serum levels of drugs, or monitoring patients’ diet and exercise. Hence, we used a questionnaire and patients’ self-reports.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.FNM.REC.1400.093). Informed consent was obtained from the participants.
Funding
This article was extracted from a Master’s thesis of Ghasem Hassan Abid, approved from Tehran University of Medical Sciences, Tehran, Iran. The research was financially supported by Tehran University of Medical Sciences, Tehran, Iran (Grant No.: 1401-1-100-57736).
Authors' contributions
Conceptualization and study design: Ghasem Hassan Abid, Mahboobeh Kafaei-Atrian and Leila Sayadi; Writing the original draft and data collection: Ghasem Hassan Abid and Leila Sayadi; Statistical analysis: Mohammad Asghari-Jafarabadi and Leila Sayadi; Review & editing: Mahboobeh Kafaei-Atrian; Final approval: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in the study.
References
Myocardial Infarction (MI) or “heart attack” is caused by a reduction or complete cessation of blood flow to a part of the myocardium [1]. It is one of the most common heart diseases and the most common cause of death worldwide, accounting for 35% of deaths in the world. This disease has significant complications for the patients and puts a huge cost burden on the patients and the health system [2]. The prevalence of MI in Iraq has been reported to be high. It is one of the first causes of death in Iraq [3].
Treatment adherence refers to the degree to which an individual’s behavior complies with health or treatment recommendations [4] or the instructions of the medical team [5], which can result in decreased complications [6]. The results of a study conducted in Poland in 2018 on assessing the level of treatment adherence in patients with MI treated with percutaneous coronary intervention showed that 59 patients had high adherence (26.7%) and 52 patients had low adherence (23.5%) [7]. Several factors contribute to poor treatment adherence, including socioeconomic factors, treatment-related factors, patient-related factors, disease-related factors, health system factors, and factors related to the healthcare team [8-10].
Training of healthcare providers and the follow-up of patients can increase the level of adherence to treatment in MI patients. It is essential to control the MI and prevent its complications [11]. Considering that heart diseases are the leading cause of mortality worldwide [12], treatment adherence is needed to confirm the validity and generalizability of the results of clinical trials regarding these diseases [13]. The present study aims to determine treatment adherence and related factors among patients with MI at selected hospitals in Hilla, Iraq.
Materials and Methods
This is a cross-sectional study, conducted from September 1 to December 30, 2021. The study population consists of all patients over 18 years of age diagnosed with MI by a cardiologist and had a history of hospitalization due to MI admitted to three teaching hospitals in Hilla city, located in Babylon province of Iraq. The inclusion criteria were the diagnosis of MI for at least six months, no self-reported history of mental illness, congenital abnormality in the heart muscle, or other chronic diseases affecting heart disease. The sample size was calculated based on a study conducted in Iran on the correlation between treatment adherence and health-related quality of life in patients with hypertension (r=-0.25) [14], and considering α=0.05, z(1-α/2)=1.96 and β=0.10 (Z1-β=1.28). In this regard, the sample size was obtained as 132. After multiplying by 2 (as the effect of the sampling plan), the final sample size was 264. A convenience sampling method was used to select participants.
The data collection tools included a demographic form and the coronary artery disease treatment adherence scale (CADTAS). Demographic form surveyed age, sex, marital status, educational level, occupation, number of children, age at the onset of diagnosis, duration of the disease, history of heart attack, number of heart attacks, history of coronary artery reconstruction, underlying diseases, duration of medication use, number of used medications. The CADTAS has 35 items and the dimensions of dietary adherence (items 1-13), healthy lifestyle adherence (items 14-20), medication adherence (items 21-31) and exercise adherence (items 32-35). The items are rated as 1 (never), 2 (rarely), 3 (sometimes), 4 (often) and 5 (always). The total score of the dietary adherence dimension is 13-65; healthy lifestyle adherence, 7-35; medication adherence, 11-55; and adherence to exercise, 4-20. The total score of the questionnaire ranges from 35 to 175, with a high score indicating better adherence to treatment regimen. The CADTAS was developed by Dehghan Nayeri et al. [15]. It is a valid and reliable tool that can be used in different clinical settings. The reliability of the CADTAS in our study, using Cronbach’s alpha, was 0.79. It was tested on 25 participants, who were included in the final sample size. After explaining the study objectives to the participants and obtaining their informed consent to participate in the study, the questionnaires were completed through interviews. The researcher asked the questions and the answers were marked.
Data for qualitative and quantitative variables were presented as frequency (percentage) and Mean±SD, respectively. The normality of the data distribution was assessed and confirmed based on the values of skewness (within ±1.5) and kurtosis (within ±2). The correlation between the continuous variables was estimated using the Pearson correlation test. Independent t-test and analysis of variance (ANOVA) were also used for data analysis. A multivariable general linear model (GLM) was used to assess the relationship between the total CADTAS score and demographic factors. In addition, Wilk’s lambda statistic was calculated for the variables in the GLM. All analyses were conducted in SPSS software, version 16 (SPSS Inc., IL, Chicago, USA), considering P<0.05 as statistically significant.
Results
Most of the participants were male, married and workers with a middle school education. Their mean duration of disease was 2.46±2.078 years. Most of them had a history of heart attack (n=214, 81.1%), a history of coronary artery reconstruction (n=181, 68.6%), and a history of underlying diseases (n=222, 84.1%).These results showed in Table 1.
Their mean age at the onset of diagnosis was 58.80±7.67 years and their mean CADTAS score was 92.28±8.01, ranged 35-175. Table 2 shows the scores for the dimensions of CADTAS. The mean dietary adherence score was 35.74±2.87 (out of 65); the healthy lifestyle adherence score was 16.77±3.85 (out of 35); the medication adherence score was 28.38±3.34 (out of 55) and the exercise adherence score was 11.40±2.16 (out of 20).
The CADTAS score had a significant and negative relationship with age (r=-0.225, P=0.001) and age at the onset of diagnosis (r=-0.239, P=0.001), but it had no significant relationships with the duration of disease or the duration of medication use. Also, there were significant differences in the CADTAS score in terms of occupation (P=0.001), history of heart attack (P=0.026) and history of underlying disease (P=0.009). The difference was not significant in terms of marital status.
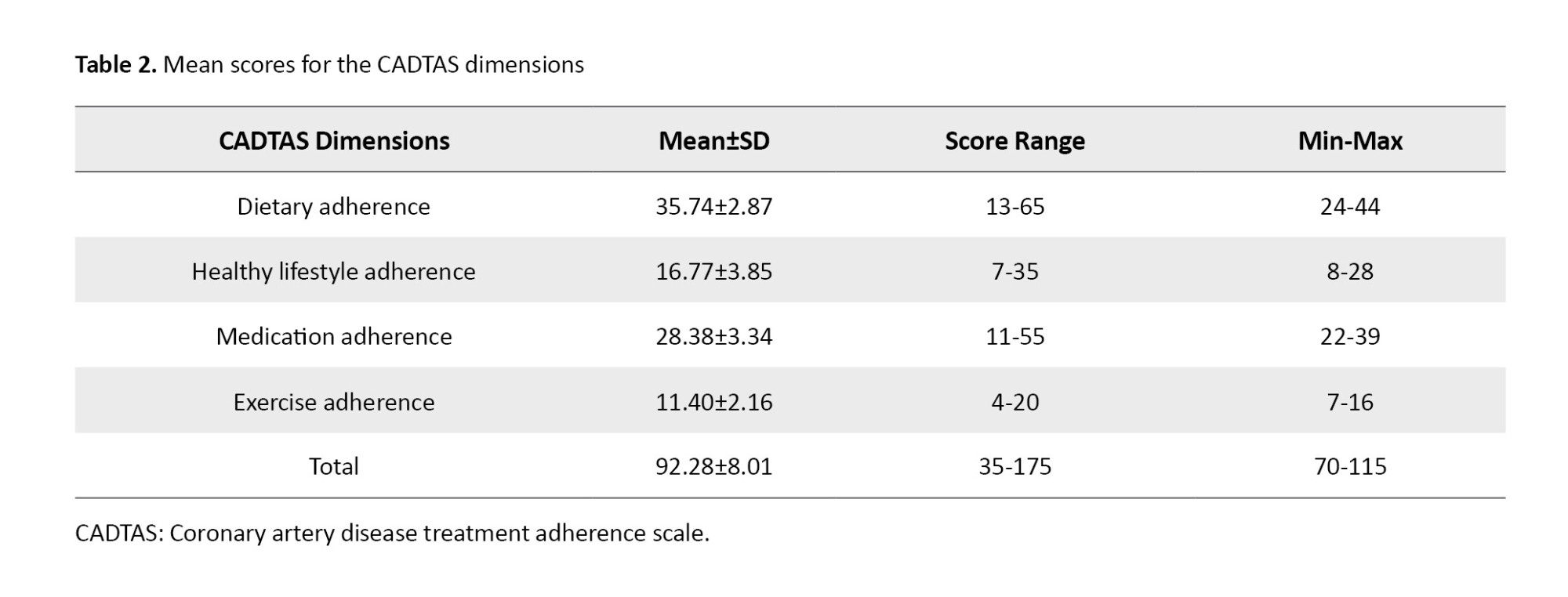
Table 3 shows the results of GLM for finding the demographic characteristics that can predict the total CADTAS score. Gender, marital status, occupation, history of heart attack, history of coronary artery reconstruction, history of underlying diseases, age, age at the onset of diagnosis, disease duration, and medication use duration were entered into the model as binary. The results showed a significant and negative association between a history of heart attack (B=-2.645, 95% CI, -5.106, -0.184, P=0.035) and underlying diseases (B=-2.828, 95%CI, -5.463, -0.193, P=0.036) and the CADTAS score. Also, the medication use duration was positively and significantly associated with the CADTAS score (B=1.145, 95% CI, 0.069, 2.222, P=0.037).
Also, the results showed a significant difference in the total CADTAS score in terms of gender (Wilks’ Lambda =0.933, P=0.002), occupation (Wilks’ Lambda =0.845, P=0.001), history of heart attack (Wilks’ Lambda =0.950, P=0.013), history of underlying diseases (Wilks’ Lambda=0.953, P=0.018), and medication use duration (Wilks’ Lambda=0.938, P=0.003) in the Table 4.
Discussion
The results indicated that the treatment adherence score of patients was 92.28±8.01 ( achieve ranged 70-115). In a study in Brazil, the overall treatment adherence of patients with MI was also moderate [16]. Other studies have reported different levels of treatment adherence. For example, in a study in Poland, adherence to treatment in 25% of MI patients was high [7]. A study conducted in Italy showed that only half of the MI patients had good adherence [17].
Among the study variables, only age and age at the onset of diagnosis had a significant negative relationship with treatment adherence in patients. Treatment adherence was higher in younger patients and in those with the disease onset at younger ages. In addition, there was a significant difference in treatment adherence of patients based on occupation, where unemployed patients had lower treatment adherence compared to the workers and employed patients. It can be said that with increasing age and unemployment, people’s connections with scientific resources and medical centers decrease. Unemployed people may have obstacles due to economic problems. If these patients are connected with their peers who have been under treatment, better results may be achieved. Numerous studies have also shown that adherence to treatment decreases with increasing age [18-20]. A study also reported treatment adherence decreased with an increase in the disease duration [21]. A study showed that the female gender, younger age, new drug prescription, low education level and low-income level were the predictors of non-adherence to treatment [22]. However, a study reported that the disease duration had no effect on treatment adherence [19]. In a study on the effects of medication adherence in hypertensive patients, it was shown that the level of education and occupation had an effect on medication adherence [20]. The reason for this discrepancy can be due to factors such as the difference in the age of participants or other demographic differences.
Overall, the results of this study showed that the mean score obtained by the study samples was higher than the mean score of the tool used to determine the level of compliance. It is essential that nurses educate and follow up these patients and their families to adhere to treatment (healthy lifestyle, medication, healthy diet, and exercise). If adherence to medications increases, it can reduce the negative consequences of MI and thus reduce treatment and household costs. Therefore, it is necessary for the health care system in Iraq to consider this issue and apply strategies to increase the treatment adherence of patients with MI. This study was conducted only in one city in Iraq (Hilla); therefore, the results cannot be generalized to all patients with MI in Iraq. Another limitation was that it was not possible to determine medication adherence objectively by counting medications, measuring serum levels of drugs, or monitoring patients’ diet and exercise. Hence, we used a questionnaire and patients’ self-reports.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.FNM.REC.1400.093). Informed consent was obtained from the participants.
Funding
This article was extracted from a Master’s thesis of Ghasem Hassan Abid, approved from Tehran University of Medical Sciences, Tehran, Iran. The research was financially supported by Tehran University of Medical Sciences, Tehran, Iran (Grant No.: 1401-1-100-57736).
Authors' contributions
Conceptualization and study design: Ghasem Hassan Abid, Mahboobeh Kafaei-Atrian and Leila Sayadi; Writing the original draft and data collection: Ghasem Hassan Abid and Leila Sayadi; Statistical analysis: Mohammad Asghari-Jafarabadi and Leila Sayadi; Review & editing: Mahboobeh Kafaei-Atrian; Final approval: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in the study.
References
- Ojha N, Dhamoon AS, Chapagain R. Myocardial Infarction (Nursing). StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. [PMID]
- Mohseni J, Kazemi T, Maleki MH, Beydokhti H. A systematic review on the prevalence of acute myocardial infarction in Iran. Heart Views. 2017; 18(4):125-32. [DOI:10.4103/HEARTVIEWS.HEARTVIEWS_71_17] [PMID]
- Mohammad AM, Rashad HH, Habeeb QS, Rashad BH, Saeed SY. Demographic, clinical and angiographic profile of coronary artery disease in kurdistan region of Iraq. Am J Cardiovasc Dis. 2021; 11(1):39-45. [PMID]
- WHO. Adherence to long term therapies: Evidence for action. Geneva: World Health Organization; 2003. [Link]
- Ghosh A, Suhas S, Solanki C, Dave M, Tharayil HM, Damodharan D, et al. From compliance to adherence: Changing views, changing concepts. Indian J Psychiatry. 2017; 59(3):399-400. [DOI:10.4103/psychiatry.IndianJPsychiatry_281_17] [PMID]
- Gregoriano C, Dieterle T, Breitenstein AL, Dürr S, Baum A, Giezendanner S, et al. Does a tailored intervention to promote adherence in patients with chronic lung disease affect exacerbations? A randomized controlled trial. Respir Res. 2019; 20(1):273. [DOI:10.1186/s12931-019-1219-3] [PMID]
- Kosobucka A, Michalski P, Pietrzykowski Ł, Kasprzak M, Obońska K, Fabiszak T, et al. Adherence to treatment assessed with the Adherence in Chronic Diseases Scale in patients after myocardial infarction. Patient Prefer Adherence. 2018; 12:333-40. [DOI:10.2147/PPA.S150435] [PMID]
- Lam WY, Fresco P. Medication adherence measures: An overview. Biomed Res Int. 2015; 2015:217047. [DOI:10.1155/2015/217047] [PMID]
- Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011; 86(4):304-14. [DOI:10.4065/mcp.2010.0575] [PMID]
- Yoon S, Kwan YH, Yap WL, Lim ZY, Phang JK, Loo YX, et al. Factors influencing medication adherence in multi-ethnic Asian patients with chronic diseases in Singapore: A qualitative study. Front Pharmacol. 2023; 14:1124297. [DOI:10.3389/fphar.2023.1124297] [PMID]
- Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics—2022 update: A report from the American Heart Association. Circulation. 2022; 145(8):e153-639. DOI:10.1161/CIR.0000000000001052] [PMID]
- Bermon A, Uribe AF, Pérez-Rivero PF, Prieto-Merino D, Saaibi JF, Silva FA, et al. Efficacy and safety of text messages targeting adherence to cardiovascular medications in secondary prevention: TXT2HEART Colombia randomized controlled trial. JMIR Mhealth Uhealth. 2021; 9(7):e25548. [DOI:10.2196/25548] [PMID]
- Glasser SP, Vitolins M, Rocco MV, Still CH, Cofield SS, Haley WE, et al. Is medication adherence predictive of cardiovascular outcomes and blood pressure control? The systolic blood pressure intervention trial (SPRINT). Am J Hypertens. 2022; 35(2):182-91. [DOI:10.1093/ajh/hpab145] [PMID]
- Masror Roudsari D, Dabiri Golchin M, Parsa yekta Z, Haghani H. [Relationship between adherence to therapeutic regimen and health related quality of life in hypertensive patients (Persian)]. Iran J Nurs. 2013; 26(85):44-54. [Link]
- Dehghan Nayeri N, Yadegary MA, Seylani K, Navab E. Development and Psychometric Evaluation of Coronary Artery Disease Treatment Adherence Scale. Cardiol Ther. 2019; 8(1):103-15.[DOI:10.1007/s40119-019-0135-4] [PMID]
- Rojas-Reyes J, Flórez-Flórez ML. Adherence to treatment and quality of life in people with acute myocardial infarction. Aquichan. 2016; 16(3):328-39. [DOI:10.5294/aqui.2016.5216.5293.5295]
- Monaldi B, Bologna G, Costa GG, D'Agostino C, Ferrante F, Filice M, et al. Adherence to statin treatment following a myocardial infarction: An Italian population-based survey. Clinicoecon Outcomes Res. 2015; 7:273-80. [DOI:10.2147/CEOR.S70936] [PMID]
- Eindhoven DC, Hilt AD, Zwaan TC, Schalij MJ, Borleffs CJW. Age and gender differences in medical adherence after myocardial infarction: Women do not receive optimal treatment- The Netherlands claims database. Eur J Prev Cardiol. 2018; 25(2):181-9. [DOI:10.1177/2047487317744363] [PMID]
- Gast A, Mathes T. Medication adherence influencing factors-an (updated) overview of systematic reviews. Syst Rev. 2019; 8(1):112.[DOI:10.1186/s13643-019-1014-8] [PMID]
- Karakurt P, Kaşikçi M. Factors affecting medication adherence in patients with hypertension. J Vasc Nurs. 2012; 30(4):118-26.[DOI:10.1016/j.jvn.2012.1004.1002] [PMID]
- Mailani F, Bakri SO. The duration of hemodialysis treatment and the adherence of chronic kidney disease patients in fluid intake limitation: A relationship. Indonesian J Nurs Sci. 2020; 1(1):43-8. [DOI:10.32734/ijns.v2i1.4188]
- Venditti V, Bleve E, Morano S, Filardi T. Gender-related factors in medication adherence for metabolic and cardiovascular health. Metabolites. 2023; 13(10):1087. [DOI:10.3390/metabo13101087] [PMID]
Article Type : Research |
Subject:
General
Received: 2024/04/10 | Accepted: 2025/03/30 | Published: 2025/04/1
Received: 2024/04/10 | Accepted: 2025/03/30 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |