Tue, Feb 3, 2026
Volume 35, Issue 2 (3-2025)
JHNM 2025, 35(2): 141-148 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezvani F, Abbasi Dolatabadi Z, Esmaeili M, Maroufizadeh S, Garakyaraghi M, Mazaheri M. Factors Associated With the 30-day Readmission Rate in Patients With Heart Failure. JHNM 2025; 35 (2) :141-148
URL: http://hnmj.gums.ac.ir/article-1-2330-en.html
URL: http://hnmj.gums.ac.ir/article-1-2330-en.html
Fereshteh Rezvani1 

 , Zahra Abbasi Dolatabadi2
, Zahra Abbasi Dolatabadi2 

 , Maryam Esmaeili *3
, Maryam Esmaeili *3 

 , Saman Maroufizadeh4
, Saman Maroufizadeh4 

 , Mohammad Garakyaraghi5
, Mohammad Garakyaraghi5 

 , Monir Mazaheri6
, Monir Mazaheri6 




 , Zahra Abbasi Dolatabadi2
, Zahra Abbasi Dolatabadi2 

 , Maryam Esmaeili *3
, Maryam Esmaeili *3 

 , Saman Maroufizadeh4
, Saman Maroufizadeh4 

 , Mohammad Garakyaraghi5
, Mohammad Garakyaraghi5 

 , Monir Mazaheri6
, Monir Mazaheri6 


1- Critical care nursing, Department of Critical Care, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
2- Associate Professor, Department of of Medical Surgical and Nursing and Midwifery Care, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
3- Professor, Department of Critical Care, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran. ,mesmaeilie77@gmail.com
4- Assistant Professor, Department of Biostatistics, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
5- Professor, Department of Cardiology, School of Medicine, Heart Failure Research Center, Cardiovascular Research Institute, Chamran Hospital, Isfahan University of Medical Sciences, Isfahan, Iran.
6- Professor, Department of Health Sciences, Sophiahemmet University, Stockholm, Sweden.
2- Associate Professor, Department of of Medical Surgical and Nursing and Midwifery Care, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
3- Professor, Department of Critical Care, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran. ,
4- Assistant Professor, Department of Biostatistics, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
5- Professor, Department of Cardiology, School of Medicine, Heart Failure Research Center, Cardiovascular Research Institute, Chamran Hospital, Isfahan University of Medical Sciences, Isfahan, Iran.
6- Professor, Department of Health Sciences, Sophiahemmet University, Stockholm, Sweden.
Full-Text [PDF 480 kb]
(485 Downloads)
| Abstract (HTML) (767 Views)
Full-Text: (289 Views)
Introduction
In Iran, cardiovascular diseases, with a prevalence of 22% among people aged ≥30 years, are one of the main causes of death. The most common cardiovascular disease is heart failure (HF). The prevalence of HF in Iran is 8%, which is higher than in other countries in Asia and the world. Also, the one-year mortality rate of this disease in Iran is estimated at 32% [1-3]. As the prevalence of HF increases, the hospitalization and mortality rates also increase [4]. Current treatments for patients with HF can improve the quality and prolongation of life in these patients, but rarely reverse the progression of the disease. Readmission to hospital, debilitating symptoms, and poor quality of life are common in patients with HF [5]. The Hospital readmission reduction program of the patient protection and affordable act defines readmission as “admission to an acute care hospital within 30 days of discharge from the same or another acute care hospital” [6]. There is an increasing need to improve the perception of the medical team, especially nurses, about hospital readmission after discharge due to the increase in the hospital readmission rate over the past few decades [7, 8].
HF is associated with some cardiac and non-cardiac complications that predispose patients to hospital readmission. Although significant progress has been made in treating patients with HF, the average hospital readmission rate is still constant; approximately one in four HF patients is readmitted to the hospital within 30 days after discharge [9]. In addition to the cost burden, readmission can cause problems such as waste of time and absenteeism, contributing to poor quality of patient care [10]. The 30-day readmission rate is a good indicator in patients with HF. It shows the severity of the disease and the importance of careful evaluation and management in inpatient and outpatient service providers [11]. A study showed that 17-35% of hospital readmissions were due to the worsening of HF and 53-62% were due to non-cardiac reasons [12]. The various reasons for readmission highlight the importance of comprehensive care to prevent secondary complications [13].
It is necessary to identify the effective factors to reduce the cost burden on the health system and make appropriate planning to reduce the readmission rate in patients with HF. Although several studies have been conducted to identify factors associated with hospital readmission of HF patients, there are still high readmission rates in these patients. The effective factors vary according to the study design and population [14]. This study aims to identify the factors associated with the 30-day readmission rate in patients with HF in Isfahan, Iran.
Materials and Methods
This is a retrospective single-center study. The medical records of patients with HF (n=312) admitted to a hospital affiliated to Isfahan University of Medical Sciences in Isfahan, Iran, within the 6 months were examined from April 1 to September 22, 2019. Then, they were followed up for 6 months after admission regarding 30-day readmission and non-readmission rates to the same hospital. The inclusion criteria were being admitted to the study hospital during the first 6 months of 2019 due to HF, having a definitive diagnosis of HF and age >18 years. A history of heart transplantation, being in the later stages of life and in need of palliative care, discharge with personal consent during the initial admission, readmission to another medical center or hospital, having an implantable defibrillator, death during the treatment process and hospitalization for less than 24 hours were the exclusion criteria. The sample size was determined to be 312 due to the use of logistic regression analysis for detecting the effective factors, based on the researcher’s estimation of the frequency of readmissions to the study hospital, and by considering 10 samples for each independent variable,
A researcher-made form was used to collect data, which was designed after the literature review. The form included the following parts: Demographic information (age, sex, marital status, history of smoking, history of substance use, occupation), clinical information, body mass index (BMI), vital signs, laboratory tests, history of drug use, ejection fraction, history of HF, comorbidities (hypertension, diabetes, ischemic heart disease, hyperlipidemia, chronic kidney disease, chronic lung disease, atrial fibrillation, anemia, cardiovascular diseases, arthritis, respiratory disorder), routine drug treatments, and discharge information (length of hospital stay, vital signs, sodium level, creatinine level). The data collection tool’s content validity was evaluated and confirmed by a panel of experts, including cardiac nurses and cardiologists.
After collection, quantitative data were presented as Mean±SD and the qualitative data were presented as “frequency (percentage)”. Independent t-test, chi-square test, and logistic regression analysis were used to analyze the data. Data were analyzed in SPSS software, version 16 software and the significance level was set at 0.05.
Results
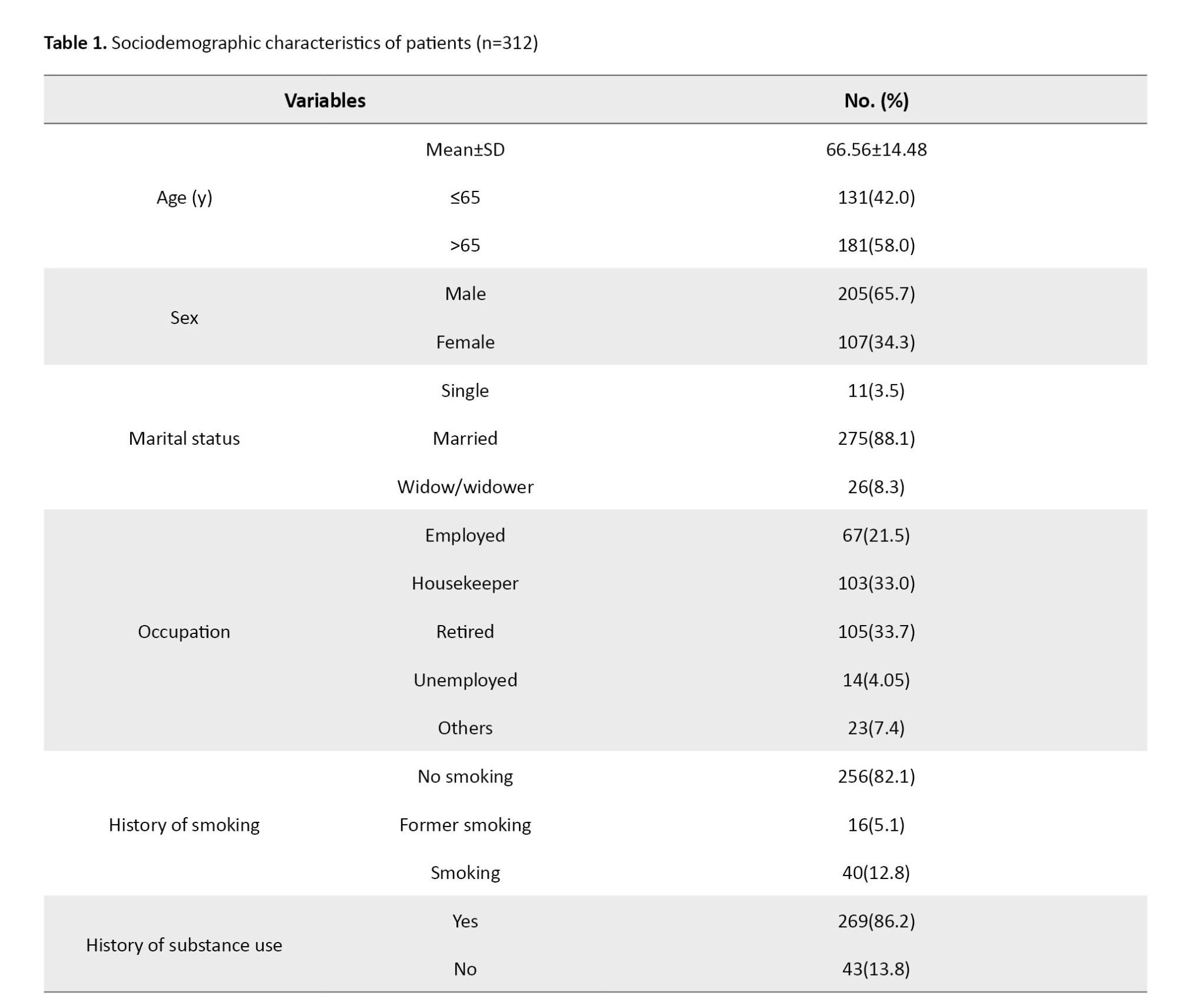
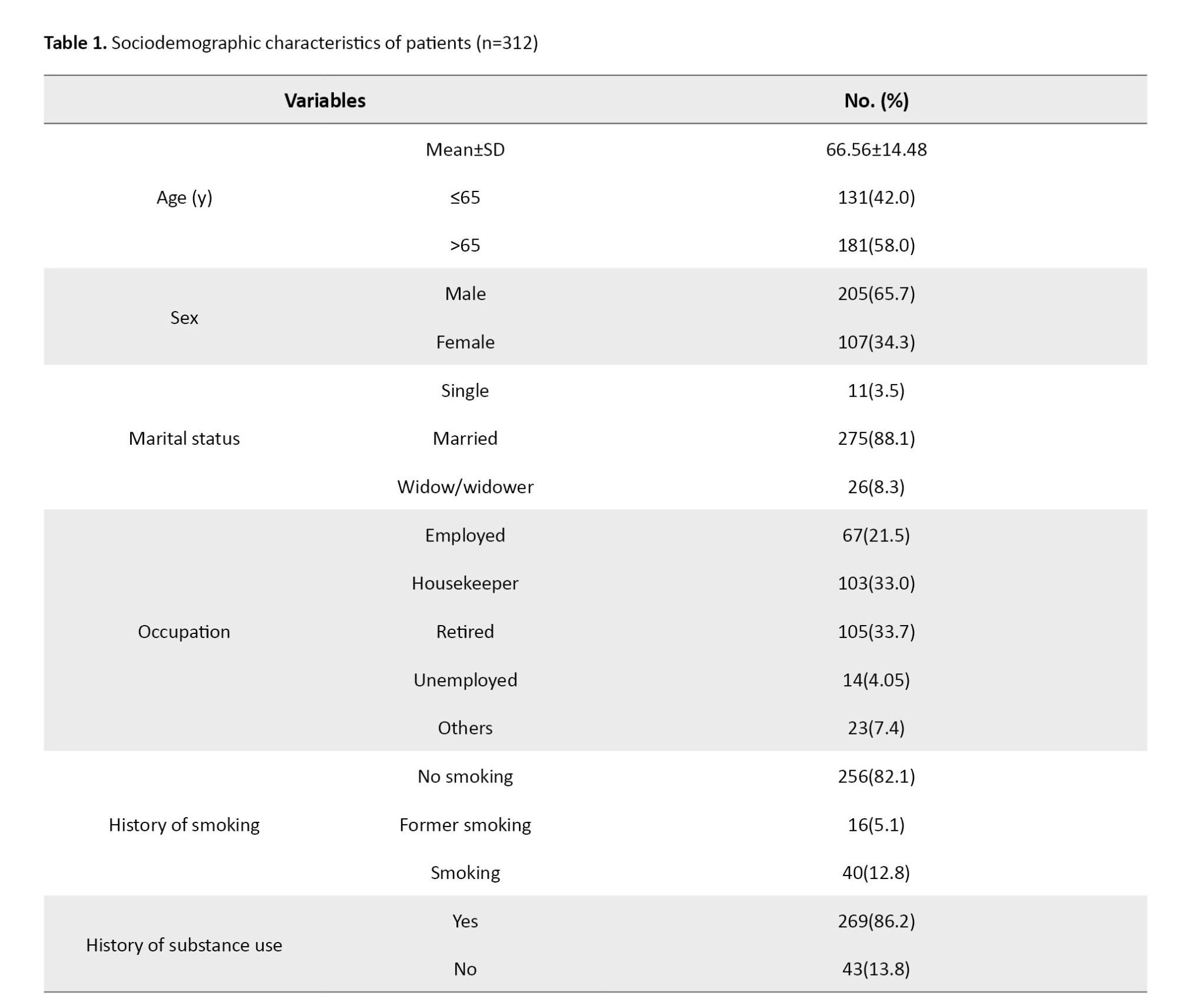
The mean age of patients was 66.56±14.48 years. Of the 312 patients, 181(58%) were over 65. Other demographic characteristics are given in Table 1. The mean BMI of patients was 26.11±4.70 kg/m2 and the oxygen saturation level in 55.1% of patients was normal (95-100%).
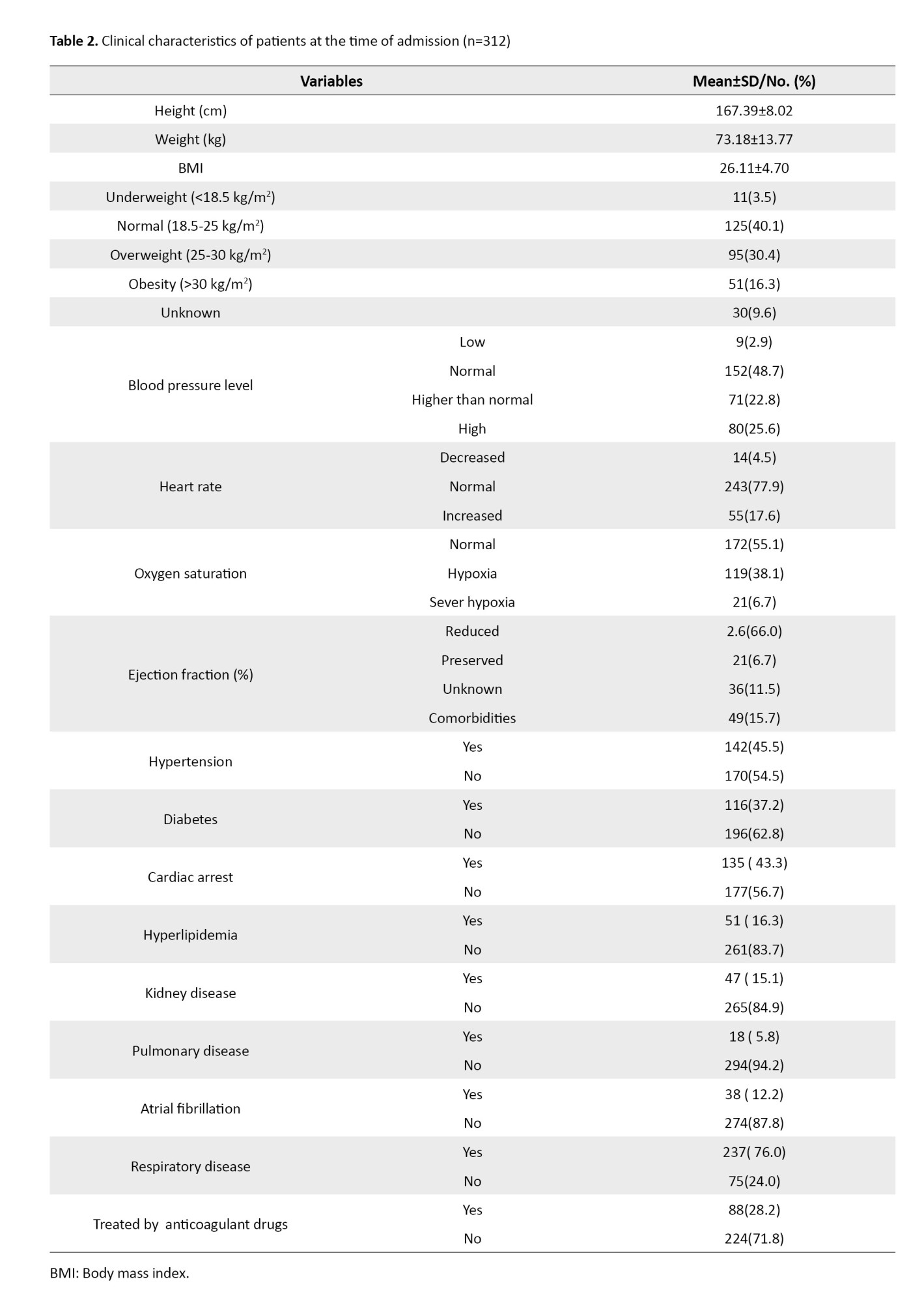
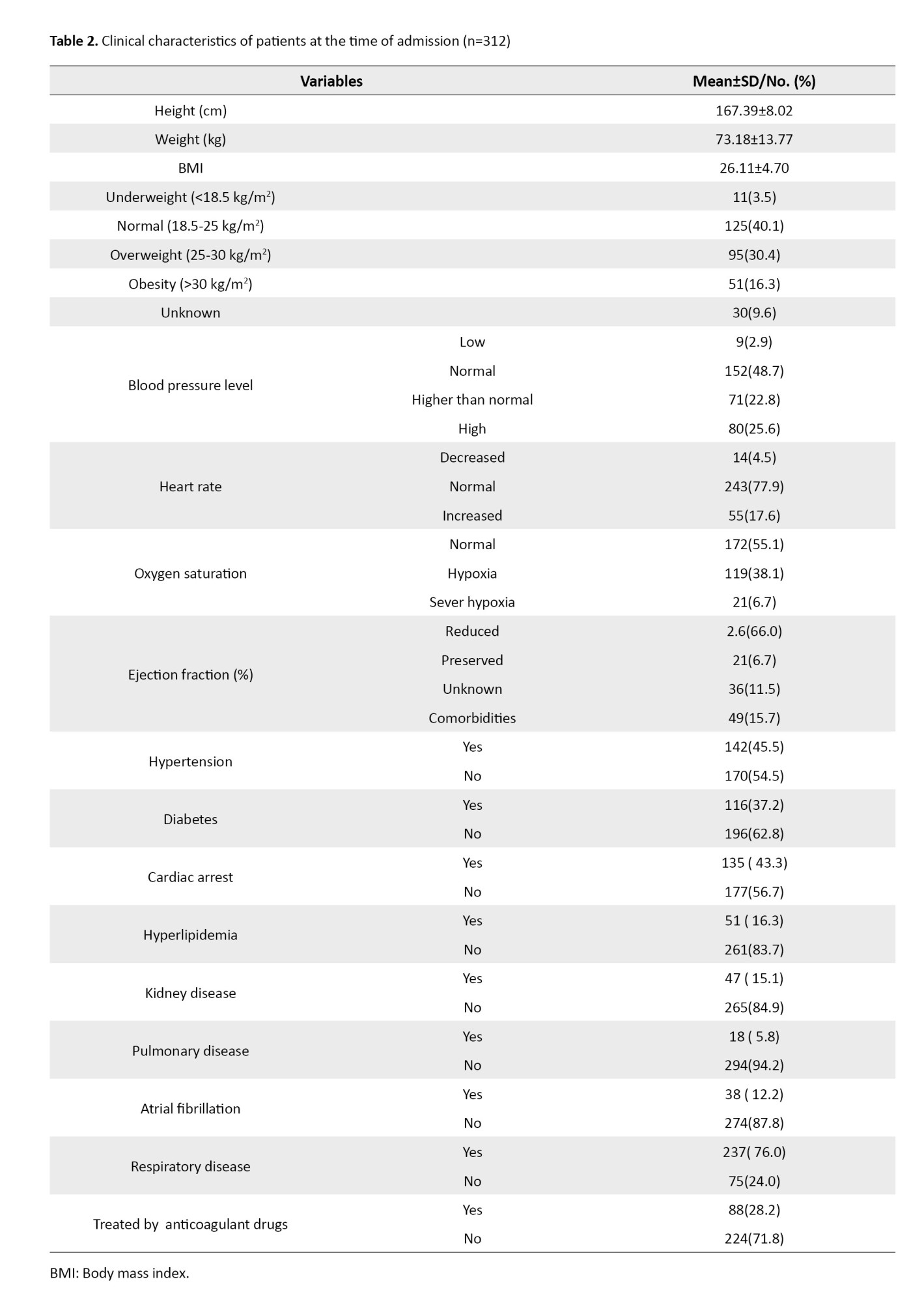
The most common routine drug treatment was the use of diuretics (63.5%) and the least common treatment was the use of angiotensin-converting-enzyme (ACE) inhibitors (11.5%). The length of hospital stay in 156 patients (49.8%) was 2-5 days, and the sodium level of 112 patients (35.8%) was low, while the creatinine level of 156 patients (49.8%) was high. Other clinical characteristics are shown in Table 2.
The 30-day readmission rate was 7.4% in overall (23 out of 312) and the rate of over 30-day readmission was 17% (53 out of 312). The readmission rate in men (8.8%) was higher than in women (4.7%), but the difference was not statistically significant based on the chi-square test results. The readmission rate in unemployed patients (21.4%) was higher than in patients with other occupations (0.9-3.9%), but the difference was not statistically significant, either. Moreover, no statistically significant difference was observed in terms of age, marital status, smoking, and drug use. The readmission rate in patients with atrial fibrillation (8.8%) was higher than in patients with no atrial fibrillation (4.7%), but the difference was not statistically significant. There was a significant difference in the 30-day readmission rate based on diuretic drug treatment (P=0.015). The readmission rate in patients treated with anticoagulants (28.2%) was higher than in patients not treated with anticoagulants (71.8%), but the difference was not statistically significant. No statistically significant difference was found based on other drug treatments, either. In examining the difference in the 30-day readmission rate based on discharge conditions, the results showed a statistically significant difference based on the mean systolic blood pressure (P=0.001) and diastolic blood pressure (P=0.024) based on the t student test results.
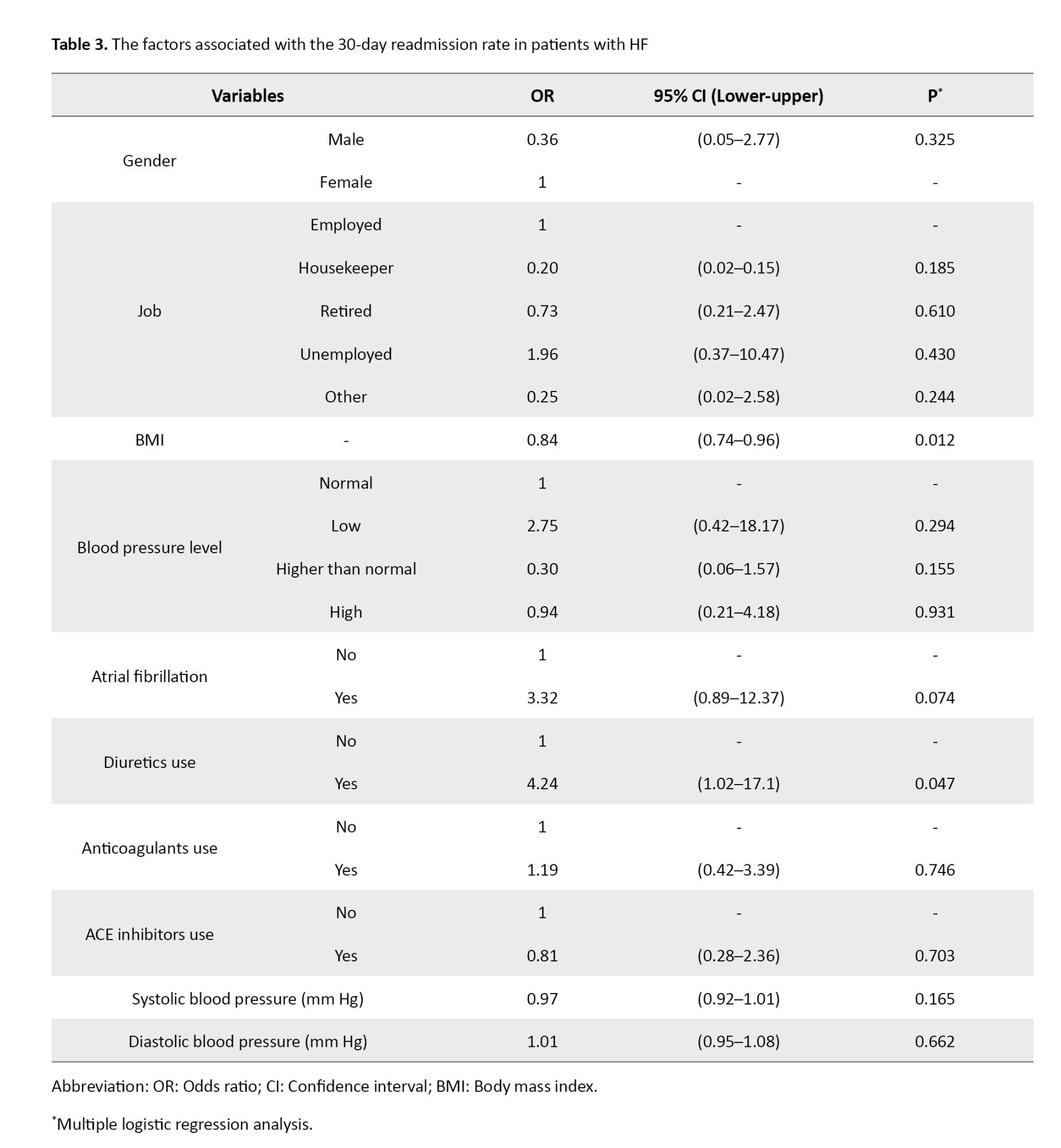
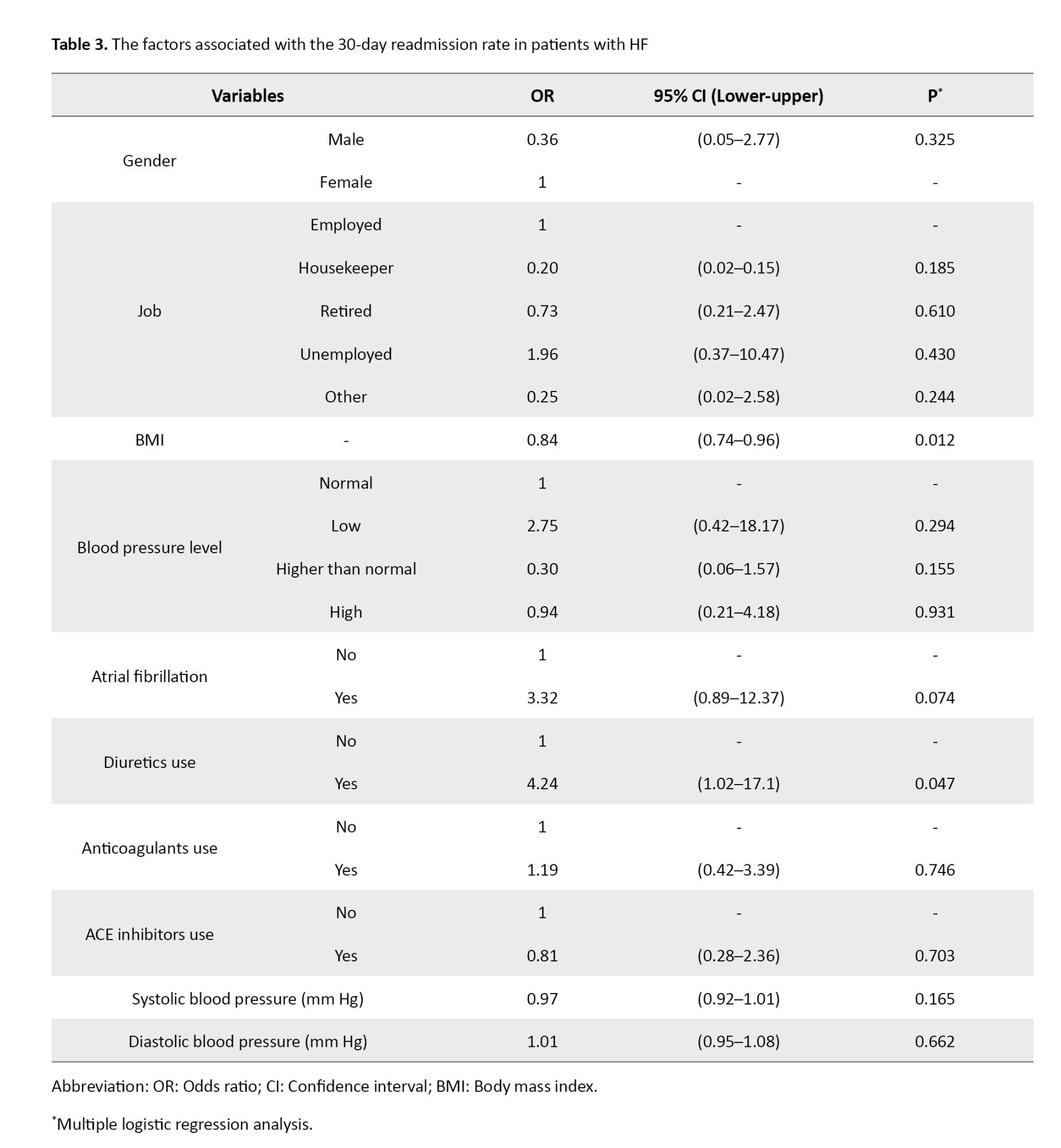
Based on the results of logistic regression analysis, as BMI increased, the likelihood of 30-day readmission significantly decreased (OR=0.84, 95% CI, 0.74, 0.96, P=0.001) and the likelihood of readmission in patients who received diuretics was 4.24 times higher than in those who did not receive diuretics (OR=4.24, 95% CI, 1.02, 17.1, P=0.047). Additionally, the likelihood of readmission in patients with atrial fibrillation was 3.32 times higher than in other patients (OR=3.32, 95% CI, 1.37, 12.12, P=0.074), although this difference was borderline significant. No other variables showed a statistically significant association with the 30-day readmission rate (Table 3).
Discussion
The purpose of this study was to investigate the factors affecting the 30-day readmission of hospitalized patients with HF in Isfahan, Iran. Findings showed that the rate of 30-day readmission increased with a decrease in BMI and the use of diuretics. The readmission rate in men, unemployed patients, patients with atrial fibrillation, and users of anticoagulants was higher than in other patients, but they had no statistically significant association with the 30-day readmission rate. However, it was clinically significant in the present study.
Khan et al. investigated the trend of 30-day and 90-day readmission rates in HF patients and showed that 18.2% and 31.2% of patients were readmitted within 30 and 90 days, respectively [15]. Deek et al. investigated the readmission rate of HF patients in Lebanon within 30, 60, and 90 days of hospital discharge and examined the factors associated with the readmission rate. They concluded that, of 187 patients, 15% were readmitted within 30 days, 22.2% within 60 days, and 27.8% within 90 days [16]. In this study the 30-day readmission rate was 7.4% in overall and the rate of over 30-day readmission was 17% .
In the present study, it was found that with the increase in BMI, the 30-day readmission rate decreased significantly. However, it is necessary to follow up and investigate this issue in further studies. In a study conducted in Japan [17] on identifying the factors associated with the 30-day readmission rate in patients with HF, the results also revealed that a higher BMI was associated with a reduction in the readmission rate in patients. In our study, atrial fibrillation had no statistically significant with the 30-day readmission rate. A study conducted in the United States [18] showed that early readmission was associated with atrial fibrillation at discharge. Another study showed that the readmission rate in HF patients with atrial fibrillation increased significantly and suggested that, to reduce it, patients should maintain a controlled sinus rhythm or manage their atrial fibrillation [19]. Fung et al. demonstrated that atrial fibrillation was an important predictor of death and readmission in 238 HF patients with a normal ejection fraction, and the group with atrial fibrillation had a higher admission rate than patients in sinus rhythm [20]. This may heighten the physical vulnerability of patients with atrial fibrillation, underscoring the critical need for more stringent therapeutic adherence to prevent hospital readmissions. Such an approach is essential to improve patient outcomes and reduce the risk of recurrent hospitalizations in this population.
According to the results, the 30-day readmission rate in patients who received diuretics or anticoagulants was higher than in patients who did not receive diuretics or anticoagulants, but the association was not statistically significant. Conversely, Barsuk et al. [21] reported that the use of diuretics during hospital discharge was associated with adverse consequences such as increased readmission in Japanese patients with HF. Hernandez et al. also reported a contradictory result. In their study, it was shown that the use of diuretic protocol for hospitalized patients with HF decreased the fluid load of patients, which is characterized by weight loss, and it led to a decreased rate of 30-day readmission without increasing the mortality rate [22]. While diuretics are widely recognized as a cornerstone in the pharmacological management of HF, the findings of this study emphasize the critical importance of therapeutic adherence, self-management, and self-care in preventing disease exacerbation and mitigating life-threatening complications. The existence of different findings in studies regarding the use of diuretics indicates the need for further studies in this area. Tsimploulis et al. reported that the initiation of anticoagulant therapy at discharge was associated with a reduction in 30-day and 1-year mortality rates of older patients with HF and atrial fibrillation, but it was not associated with a reduction in readmission [23].
In our study, the mean systolic and diastolic blood pressures of patients with readmission within 30 days were significantly lower than in patients without readmission. Muzzarelli et al. [24] in a study consistent with the present study showed that in older patients hospitalized due to HF and preserved ejection fraction were associated with a higher risk of mortality and readmission. Their results showed that lower systolic blood pressure is a predictor of 30-day readmission [24]. This result is in line with the result reported by Fuchida et al. [25].
In conclusion, the increase in the 30-day readmission rate of hospitalized HF patients in Isfahan is associated with their decreased BMI and use of diuretics. Although other study factors were not statistically significant, it is important to pay attention to them due to their clinical significance. This study examined the readmission of HF patients to a hospital in one city in Iran. Therefore, we should be cautious about the generalizability of the results to all HF patients in Iran. The small sample size was another limitation. It was not possible to select more samples due to time constraints and the low rate of readmission.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.FNM.REC.1399.120). All ethical principles were considered.
Funding
This article was extracted from the master’s thesis of Fereshteh Rezvani, at Tehran University of Medical Sciences, Tehran, Iran. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Data collection and writing the original draft: Maryam Esmaeili and Freshteh Rezvani; Data and statistical analysis: Saman Maroufizadeh; Conceptualization, supervision, review and editing: Mohammad Garakyaraghi, Zahra Abbasi Dolatabadi, Monir Mazaheri and Maryam Esmaeili.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
References
In Iran, cardiovascular diseases, with a prevalence of 22% among people aged ≥30 years, are one of the main causes of death. The most common cardiovascular disease is heart failure (HF). The prevalence of HF in Iran is 8%, which is higher than in other countries in Asia and the world. Also, the one-year mortality rate of this disease in Iran is estimated at 32% [1-3]. As the prevalence of HF increases, the hospitalization and mortality rates also increase [4]. Current treatments for patients with HF can improve the quality and prolongation of life in these patients, but rarely reverse the progression of the disease. Readmission to hospital, debilitating symptoms, and poor quality of life are common in patients with HF [5]. The Hospital readmission reduction program of the patient protection and affordable act defines readmission as “admission to an acute care hospital within 30 days of discharge from the same or another acute care hospital” [6]. There is an increasing need to improve the perception of the medical team, especially nurses, about hospital readmission after discharge due to the increase in the hospital readmission rate over the past few decades [7, 8].
HF is associated with some cardiac and non-cardiac complications that predispose patients to hospital readmission. Although significant progress has been made in treating patients with HF, the average hospital readmission rate is still constant; approximately one in four HF patients is readmitted to the hospital within 30 days after discharge [9]. In addition to the cost burden, readmission can cause problems such as waste of time and absenteeism, contributing to poor quality of patient care [10]. The 30-day readmission rate is a good indicator in patients with HF. It shows the severity of the disease and the importance of careful evaluation and management in inpatient and outpatient service providers [11]. A study showed that 17-35% of hospital readmissions were due to the worsening of HF and 53-62% were due to non-cardiac reasons [12]. The various reasons for readmission highlight the importance of comprehensive care to prevent secondary complications [13].
It is necessary to identify the effective factors to reduce the cost burden on the health system and make appropriate planning to reduce the readmission rate in patients with HF. Although several studies have been conducted to identify factors associated with hospital readmission of HF patients, there are still high readmission rates in these patients. The effective factors vary according to the study design and population [14]. This study aims to identify the factors associated with the 30-day readmission rate in patients with HF in Isfahan, Iran.
Materials and Methods
This is a retrospective single-center study. The medical records of patients with HF (n=312) admitted to a hospital affiliated to Isfahan University of Medical Sciences in Isfahan, Iran, within the 6 months were examined from April 1 to September 22, 2019. Then, they were followed up for 6 months after admission regarding 30-day readmission and non-readmission rates to the same hospital. The inclusion criteria were being admitted to the study hospital during the first 6 months of 2019 due to HF, having a definitive diagnosis of HF and age >18 years. A history of heart transplantation, being in the later stages of life and in need of palliative care, discharge with personal consent during the initial admission, readmission to another medical center or hospital, having an implantable defibrillator, death during the treatment process and hospitalization for less than 24 hours were the exclusion criteria. The sample size was determined to be 312 due to the use of logistic regression analysis for detecting the effective factors, based on the researcher’s estimation of the frequency of readmissions to the study hospital, and by considering 10 samples for each independent variable,
A researcher-made form was used to collect data, which was designed after the literature review. The form included the following parts: Demographic information (age, sex, marital status, history of smoking, history of substance use, occupation), clinical information, body mass index (BMI), vital signs, laboratory tests, history of drug use, ejection fraction, history of HF, comorbidities (hypertension, diabetes, ischemic heart disease, hyperlipidemia, chronic kidney disease, chronic lung disease, atrial fibrillation, anemia, cardiovascular diseases, arthritis, respiratory disorder), routine drug treatments, and discharge information (length of hospital stay, vital signs, sodium level, creatinine level). The data collection tool’s content validity was evaluated and confirmed by a panel of experts, including cardiac nurses and cardiologists.
After collection, quantitative data were presented as Mean±SD and the qualitative data were presented as “frequency (percentage)”. Independent t-test, chi-square test, and logistic regression analysis were used to analyze the data. Data were analyzed in SPSS software, version 16 software and the significance level was set at 0.05.
Results
The mean age of patients was 66.56±14.48 years. Of the 312 patients, 181(58%) were over 65. Other demographic characteristics are given in Table 1. The mean BMI of patients was 26.11±4.70 kg/m2 and the oxygen saturation level in 55.1% of patients was normal (95-100%).
The most common routine drug treatment was the use of diuretics (63.5%) and the least common treatment was the use of angiotensin-converting-enzyme (ACE) inhibitors (11.5%). The length of hospital stay in 156 patients (49.8%) was 2-5 days, and the sodium level of 112 patients (35.8%) was low, while the creatinine level of 156 patients (49.8%) was high. Other clinical characteristics are shown in Table 2.
The 30-day readmission rate was 7.4% in overall (23 out of 312) and the rate of over 30-day readmission was 17% (53 out of 312). The readmission rate in men (8.8%) was higher than in women (4.7%), but the difference was not statistically significant based on the chi-square test results. The readmission rate in unemployed patients (21.4%) was higher than in patients with other occupations (0.9-3.9%), but the difference was not statistically significant, either. Moreover, no statistically significant difference was observed in terms of age, marital status, smoking, and drug use. The readmission rate in patients with atrial fibrillation (8.8%) was higher than in patients with no atrial fibrillation (4.7%), but the difference was not statistically significant. There was a significant difference in the 30-day readmission rate based on diuretic drug treatment (P=0.015). The readmission rate in patients treated with anticoagulants (28.2%) was higher than in patients not treated with anticoagulants (71.8%), but the difference was not statistically significant. No statistically significant difference was found based on other drug treatments, either. In examining the difference in the 30-day readmission rate based on discharge conditions, the results showed a statistically significant difference based on the mean systolic blood pressure (P=0.001) and diastolic blood pressure (P=0.024) based on the t student test results.
Based on the results of logistic regression analysis, as BMI increased, the likelihood of 30-day readmission significantly decreased (OR=0.84, 95% CI, 0.74, 0.96, P=0.001) and the likelihood of readmission in patients who received diuretics was 4.24 times higher than in those who did not receive diuretics (OR=4.24, 95% CI, 1.02, 17.1, P=0.047). Additionally, the likelihood of readmission in patients with atrial fibrillation was 3.32 times higher than in other patients (OR=3.32, 95% CI, 1.37, 12.12, P=0.074), although this difference was borderline significant. No other variables showed a statistically significant association with the 30-day readmission rate (Table 3).
Discussion
The purpose of this study was to investigate the factors affecting the 30-day readmission of hospitalized patients with HF in Isfahan, Iran. Findings showed that the rate of 30-day readmission increased with a decrease in BMI and the use of diuretics. The readmission rate in men, unemployed patients, patients with atrial fibrillation, and users of anticoagulants was higher than in other patients, but they had no statistically significant association with the 30-day readmission rate. However, it was clinically significant in the present study.
Khan et al. investigated the trend of 30-day and 90-day readmission rates in HF patients and showed that 18.2% and 31.2% of patients were readmitted within 30 and 90 days, respectively [15]. Deek et al. investigated the readmission rate of HF patients in Lebanon within 30, 60, and 90 days of hospital discharge and examined the factors associated with the readmission rate. They concluded that, of 187 patients, 15% were readmitted within 30 days, 22.2% within 60 days, and 27.8% within 90 days [16]. In this study the 30-day readmission rate was 7.4% in overall and the rate of over 30-day readmission was 17% .
In the present study, it was found that with the increase in BMI, the 30-day readmission rate decreased significantly. However, it is necessary to follow up and investigate this issue in further studies. In a study conducted in Japan [17] on identifying the factors associated with the 30-day readmission rate in patients with HF, the results also revealed that a higher BMI was associated with a reduction in the readmission rate in patients. In our study, atrial fibrillation had no statistically significant with the 30-day readmission rate. A study conducted in the United States [18] showed that early readmission was associated with atrial fibrillation at discharge. Another study showed that the readmission rate in HF patients with atrial fibrillation increased significantly and suggested that, to reduce it, patients should maintain a controlled sinus rhythm or manage their atrial fibrillation [19]. Fung et al. demonstrated that atrial fibrillation was an important predictor of death and readmission in 238 HF patients with a normal ejection fraction, and the group with atrial fibrillation had a higher admission rate than patients in sinus rhythm [20]. This may heighten the physical vulnerability of patients with atrial fibrillation, underscoring the critical need for more stringent therapeutic adherence to prevent hospital readmissions. Such an approach is essential to improve patient outcomes and reduce the risk of recurrent hospitalizations in this population.
According to the results, the 30-day readmission rate in patients who received diuretics or anticoagulants was higher than in patients who did not receive diuretics or anticoagulants, but the association was not statistically significant. Conversely, Barsuk et al. [21] reported that the use of diuretics during hospital discharge was associated with adverse consequences such as increased readmission in Japanese patients with HF. Hernandez et al. also reported a contradictory result. In their study, it was shown that the use of diuretic protocol for hospitalized patients with HF decreased the fluid load of patients, which is characterized by weight loss, and it led to a decreased rate of 30-day readmission without increasing the mortality rate [22]. While diuretics are widely recognized as a cornerstone in the pharmacological management of HF, the findings of this study emphasize the critical importance of therapeutic adherence, self-management, and self-care in preventing disease exacerbation and mitigating life-threatening complications. The existence of different findings in studies regarding the use of diuretics indicates the need for further studies in this area. Tsimploulis et al. reported that the initiation of anticoagulant therapy at discharge was associated with a reduction in 30-day and 1-year mortality rates of older patients with HF and atrial fibrillation, but it was not associated with a reduction in readmission [23].
In our study, the mean systolic and diastolic blood pressures of patients with readmission within 30 days were significantly lower than in patients without readmission. Muzzarelli et al. [24] in a study consistent with the present study showed that in older patients hospitalized due to HF and preserved ejection fraction were associated with a higher risk of mortality and readmission. Their results showed that lower systolic blood pressure is a predictor of 30-day readmission [24]. This result is in line with the result reported by Fuchida et al. [25].
In conclusion, the increase in the 30-day readmission rate of hospitalized HF patients in Isfahan is associated with their decreased BMI and use of diuretics. Although other study factors were not statistically significant, it is important to pay attention to them due to their clinical significance. This study examined the readmission of HF patients to a hospital in one city in Iran. Therefore, we should be cautious about the generalizability of the results to all HF patients in Iran. The small sample size was another limitation. It was not possible to select more samples due to time constraints and the low rate of readmission.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.FNM.REC.1399.120). All ethical principles were considered.
Funding
This article was extracted from the master’s thesis of Fereshteh Rezvani, at Tehran University of Medical Sciences, Tehran, Iran. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Data collection and writing the original draft: Maryam Esmaeili and Freshteh Rezvani; Data and statistical analysis: Saman Maroufizadeh; Conceptualization, supervision, review and editing: Mohammad Garakyaraghi, Zahra Abbasi Dolatabadi, Monir Mazaheri and Maryam Esmaeili.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
References
- Sarrafzadegan N, Mohammmadifard N. Cardiovascular disease in Iran in the last 40 years: prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Arch Iran Med. 2019; 22(4):204-10. [PMID]
- WHO. Cardiovascular diseases. Geveva: World Health Organization; 2024. [Link]
- Martin SS, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. 2024 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2024; 149(8):e347-913. [DOI:10.1161/CIR.0000000000001209]
- Naderi N, Chenaghlou M, Mirtajaddini M, Norouzi Z, Mohammadi N, Amin A, et al. Predictors of readmission in hospitalized heart failure patients. J Cardiovasc Thorac Res. 2022; 14(1):11-7. [DOI:10.34172/jcvtr.2022.08] [PMID]
- Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review. Patient Educ Couns. 2018; 101(3):363-74. [DOI:10.1016/j.pec.2017.10.002] [PMID]
- Long JR. Using financial education to reduce heart failure readmissions [PhD dissertation]. Phoenix: Grand Canyon University; 2018. [Link]
- Tersalvi G, Gasperetti A, Schiavone M, Dauw J, Gobbi C, Denora M, et al. Acute heart failure in elderly patients: A review of invasive and non-invasive management. J Geriatr Cardiol. 2021; 18(7):560-76. [PMID]
- Sherer AP, Crane PB, Abel WM, Efird J. Predicting heart failure readmissions. J Cardiovasc Nurs. 2016; 31(2):114-20. [DOI:10.1097/JCN.0000000000000225] [PMID]
- Diamond J, DeVore AD. New strategies to prevent rehospitalizations for heart failure. Curr Treat Options Cardiovasc Med. 2022; 24(12):199-212. [DOI:10.1007/s11936-022-00969-y] [PMID]
- Cilla F, Sabione I, D'Amelio P. Risk factors for early hospital readmission in geriatric patients: a systematic review. Int J Environ Res Public Health. 2023; 20(3):1674. [DOI:10.3390/ijerph20031674] [PMID]
- Al Sattouf A, Farahat R, Khatri AA. Effectiveness of transitional care interventions for heart failure patients: A systematic review with meta-analysis. Cureus. 2022; 14(9):e29726. [DOI:10.7759/cureus.29726]
- Wan Ahmad WA, Abdul Ghapar AK, Zainal Abidin HA, Karthikesan D, Ross NT, S K Abdul Kader MA, et al. Characteristics of patients admitted with heart failure: Insights from the first Malaysian Heart Failure Registry. ESC Heart Fail. 2024; 11(2):727-36. [DOI:10.1002/ehf2.14608] [PMID]
- Agarwal MA, Fonarow GC, Ziaeian B. National trends in heart failure hospitalizations and readmissions from 2010 to 2017. JAMA Cardiol. 2021; 6(8):952-6. [DOI:10.1001/jamacardio.2020.7472] [PMID]
- Ahmed A, Ullah W, Hussain I, Roomi S, Sattar Y, Ahmed F, et al. Atrial fibrillation: A leading cause of heart failure-related hospitalizations; a dual epidemic. Am J Cardiovasc Dis. 2019; 9(5):109-15. [PMID]
- Khan MS, Sreenivasan J, Lateef N, Abougergi MS, Greene SJ, Ahmad T, et al. Trends in 30-and 90-day readmission rates for heart failure. Circ Heart Fail. 2021; 14(4):e008335. [DOI:10.1161/CIRCHEARTFAILURE.121.008335] [PMID]
- Deeka H, Skouri H, Noureddine S. Readmission rates and related factors in heart failure patients: A study in Lebanon. Collegian. 2016; 23(1):61-8. [DOI:10.1016/j.colegn.2014.11.001] [PMID]
- Aizawa H, Imai S, Fushimi K. Factors associated with 30-day readmission of patients with heart failure from a Japanese administrative database. BMC Cardiovasc Disord. 2015; 15:134. [DOI:10.1186/s12872-015-0127-9] [PMID]
- Carlson B, Hoyt H, Gillespie K, Kunath J, Lewis D, Bratzke LC. Predictors of heart failure readmission in a high-risk primarily Hispanic population in a rural setting. J Cardiovasc Nurs. 2019; 34(3):267-74. [DOI:10.1097/JCN.0000000000000567] [PMID]
- Kaneko H, Suzuki S, Goto M, Arita T, Yuzawa Y, Yagi N, et al. Incidence and predictors of rehospitalization of acute heart failure patients. Int Heart J. 2015; 56(2):219-25. [DOI:10.1536/ihj.14-290] [PMID]
- Fung JW, Sanderson JE, Yip GW, Zhang Q, Yu CM. Impact of atrial fibrillation in heart failure with normal ejection fraction: a clinical and echocardiographic study. J Card Fail. 2007; 13(8):649-55. [DOI:10.1016/j.cardfail.2007.04.014] [PMID]
- Barsuk JH, Gordon RA, Cohen ER, Cotts WG, Malkenson D, Yancy CW, et al. A diuretic protocol increases volume removal and reduces readmissions among hospitalized patients with acute decompensated heart failure. Congest Heart Fail. 2013; 19(2):53-60. [DOI:10.1111/chf.12020] [PMID]
- Hernandez AF, Liang L, Fonarow GC, Hammill BG, Hammill SC, Heidenreich PA, et al. Associations between anticoagulation therapy and risks of mortality and readmission among patients with heart failure and atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2014; 7(5):670-9. [DOI:10.1161/CIRCOUTCOMES.113.000632] [PMID]
- Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic blood pressure and outcomes in patients with heart failure with preserved ejection fraction. JAMA Cardiol. 2018; 3(4):288-97. [DOI:10.1001/jamacardio.2017.5365] [PMID]
- Muzzarelli S, Leibundgut G, Maeder MT, Rickli H, Handschin R, Gutmann M, et al. Predictors of early readmission or death in elderly patients with heart failure. Am Heart J. 2010; 160(2):308-14. [DOI:10.1111/j.1532-5415.1990.tb03450.x] [PMID]
- Fuchida A, Suzuki S, Motoki H, Kanzaki Y, Maruyama T, Hashizume N, et al. Prognostic significance of diastolic blood pressure in patients with heart failure with preserved ejection fraction. Heart Vessels. 2021; 36(8):1159-65. [DOI:10.1007/s00380-021-01788-0] [PMID]
Article Type : Research |
Subject:
Special
Received: 2024/03/31 | Accepted: 2024/10/30 | Published: 2025/04/1
Received: 2024/03/31 | Accepted: 2024/10/30 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |