Wed, Jan 28, 2026
Volume 36, Issue 1 (1-2026)
JHNM 2026, 36(1): 9-16 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Soltani Nejad Z, Salmani Mood M, Zia T, Sabeghi H. Relationship Between Nurse Managers’ Communication Skills and Nurses’ Caring Behaviors. JHNM 2026; 36 (1) :9-16
URL: http://hnmj.gums.ac.ir/article-1-2317-en.html
URL: http://hnmj.gums.ac.ir/article-1-2317-en.html
1- Nursing (MSN), Student Research Committee, Birjand University of Medical Sciences, Birjand, Iran.
2- PhD candidate in Nursing, Instructor, School of Nursing and Midwifery, Birjand University of Medical sciences, Birjand, Iran.
3- Nursing (MSN), Iranmehr Hospital, Birjand University of Medical Sciences, Birjand, Iran.
4- Assistant Professor, Department of Nursing, Geriatric Health Research Center, School of Nursing and Midwifery, Birjand University of Medical Sciences, Birjand, Iran. ,hakimeh.sabeghi@gmail.com
2- PhD candidate in Nursing, Instructor, School of Nursing and Midwifery, Birjand University of Medical sciences, Birjand, Iran.
3- Nursing (MSN), Iranmehr Hospital, Birjand University of Medical Sciences, Birjand, Iran.
4- Assistant Professor, Department of Nursing, Geriatric Health Research Center, School of Nursing and Midwifery, Birjand University of Medical Sciences, Birjand, Iran. ,
Full-Text [PDF 506 kb]
(58 Downloads)
| Abstract (HTML) (120 Views)
Full-Text: (6 Views)
Introduction
The nursing practice is a core element of patient care [1]. The theoretical principles of nursing are rooted in an understanding of care and caregiving behaviors [2]. Patient care is synonymous with nursing care [3]. Given the significant impact of quality nursing care on patients’ well-being and overall health, caring behaviors are an important element of nursing practice [2]. Caring behavior is not only a reflection of nurses’ professional competence but also a defining and distinctive feature of the nursing profession [4, 5]. Caring behavior has two components: Physical and psychosocial. Physical caring behaviors include performing daily tasks, diagnostic interventions, treatments, procedures, education, and problem-solving, all aimed at achieving desired outcomes and physical improvement. On the other hand, psychosocial caring behaviors involve building trust, accepting the patient’s emotions, being transparent and honest, fostering a sense of hope in patients, establishing effective communication with patients, and providing emotional support to patients [6].
According to a study conducted in Taiwan, although the majority of patients are satisfied with the caring behaviors of nurses, there is still a need to enhance the quality of nursing care, particularly in addressing ethical issues such as respect and effective communication with patients [7]. The studies conducted in Iran in this field have reported conflicting results. A study focusing on nurses working in intensive care units found that, while nurses had higher scores in the physical and technical aspects of care (e.g. ensuring patient safety and administering medications), their scores were lower in the psychosocial aspect. This is concerning due to the importance of addressing patients’ psychosocial needs [8]. A cross-sectional study in Iran found that nurses placed greater emphasis on technical and routine care than on social and emotional aspects. However, this approach was insufficient to meet all patients’ needs [3]. Salimi et al. reported that Iranian nurses gave equal attention to both the physical and psychological aspects of care [9].
Various factors associated with the development and reinforcement of caring behaviors in nurses, including care competence, sense of duty, work experience, religious beliefs, and supervision of nursing care behaviors [10]. Factors such as work shift delivery process [4] and training programs for nurses also contribute to nurturing caring behaviors [6]. Inadequate organizational support and nurse dissatisfaction are intra-organizational factors that indirectly affect the provision of proper nursing care [3]. A study conducted in Indonesia found that nursing management not only contributed to nurses’ personal and professional satisfaction but also played a significant role in shaping their caring behaviors [4]. Nurse managers have a wide range of tasks, including identifying the training needs of nurses [11]. However, the primary and most crucial task of a nurse manager for achieving caring goals is to establish an effective intra-organizational communication with nurses [12]. Garon highlighted the significant role of nurse managers in cultivating a culture of communication among nurses, which directly correlates with improved patient care [13].
Recognizing the significance of delivering high-quality nursing care to patients and acknowledging the potential impact of nurse managers’ communication skills on nurses’ caring behaviors, and given the conflicting findings in the existing studies regarding the level of communication skills, quality of nursing care, and the limited research conducted in Iran, this study aimed to explore the relationship between the communication skills of nurse managers and the quality of caring behaviors in nurses.
Materials and Methods
This is a descriptive-analytical study with a cross-sectional design that was conducted in teaching hospitals affiliated with Birjand University of Medical Sciences in 2023. The nurse managers of these hospitals were selected using a census sampling method, while the nurses were selected using a non-random convenience sampling method. In this regard, 44 nurse managers (including supervisors, matrons, and head nurses) with at least two years of work experience in managerial positions were selected. Also, 209 nurses with at least 2 years of experience in providing direct patient care from various departments were selected for the study. The sample size of nurses was determined using the formula of correlation considering the Standard Deviation (SD) of nursing caring behavior (0.64) in Hosseinzadeh et al.’s study [2], 95% Confidence Interval (CI), and 5% margin of error. All nursing managers of the educational and treatment center where the research was conducted (n=44), participated in the study.
The recorded sociodemographic characteristics included: Age, sex, marital status, work experience, and education level. The Nurse Leader Communication Behaviors (NLCA) scale, developed by Hopkinson et al. in 2020 [14], was used to collect data on nurse managers’ communication skills from both managers’ and nurses’ perspectives. The questionnaire was first translated into Persian using the back-translation method, and its face validity and content validity were evaluated and confirmed (Content Validity Index [CVI] >0.79). It had high internal consistency (Cronbach’s α=0.85). It consisted of 35 items and 8 subscales, including comprehensibility, method of communication, listening, feedback delivery, empathy, non-verbal communication, meta-linguistic communication, and participation. Each item is rated on a five-point Likert scale, ranging from 0 (never) to 4 (always). The total score ranges from 0 to 140, with higher scores indicating better communication skills. The 42-item Caring Behavior Inventory (CBI-42), developed by Wolf et al. in 1998 [15], was used to assess the quality of caring behaviors from the perspective of both managers and nurses. The CBI-42 has five subscales, including respectful deference to others, assurance of human presence, positive connectedness, professional knowledge and skills, and attentiveness to others’ experiences. Each item is rated on a six-point rating scale from 1 (never) to 6 (always). The total score ranges from 42 to 252. Previous studies have reported its favorable validity (face and content) [16, 17]. To assess the reliability of this tool in our study, Cronbach’s α was calculated and obtained at 0.83.
Data were collected over two months. They were analyzed in SPSS software, version 26. Descriptive statistics (Mean±SD, and frequency) were used to describe demographic and main study variables. Also, inferential statistics including Pearson’s correlation test, stepwise linear regression analysis, chi-square test, Fisher’s exact test, and independent t-test were applied to analyze the collected data. Since the significance levels of demographic variables in the univariate regression model were not less than 0.1, none of them entered the multivariate regression model. Significance level was set at 0.05.
Results
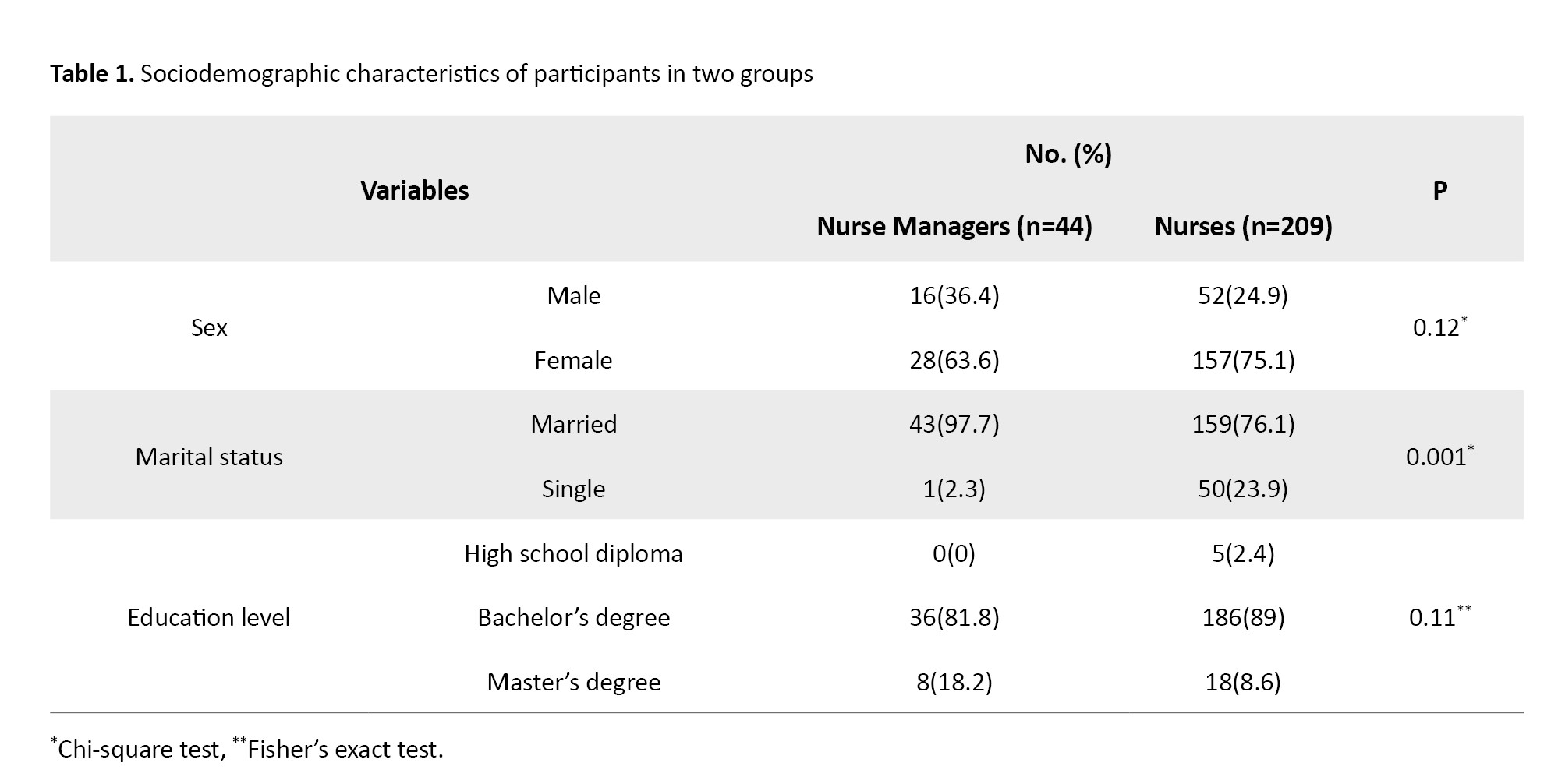
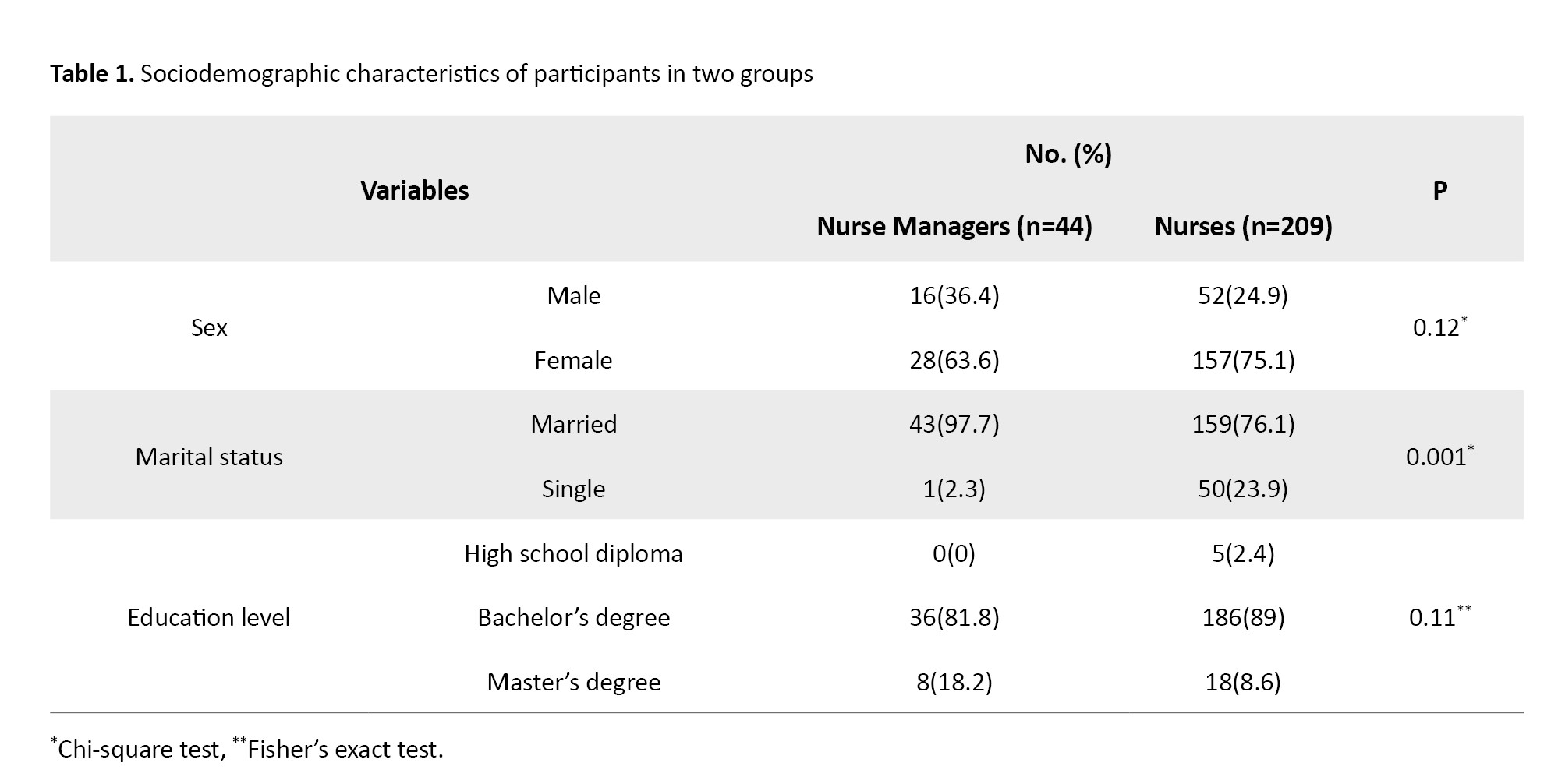
The participants included 44 nurse managers and 209 nurses working in teaching hospitals in Birjand. The mean age of nurse managers and nurses was 44.64±6.00 and 34.22±7.72 years, and their mean work experience was 20.36±7.72 and 10.06±7.72 years, respectively. Table 1 presents the sociodemographic characteristics of both groups.
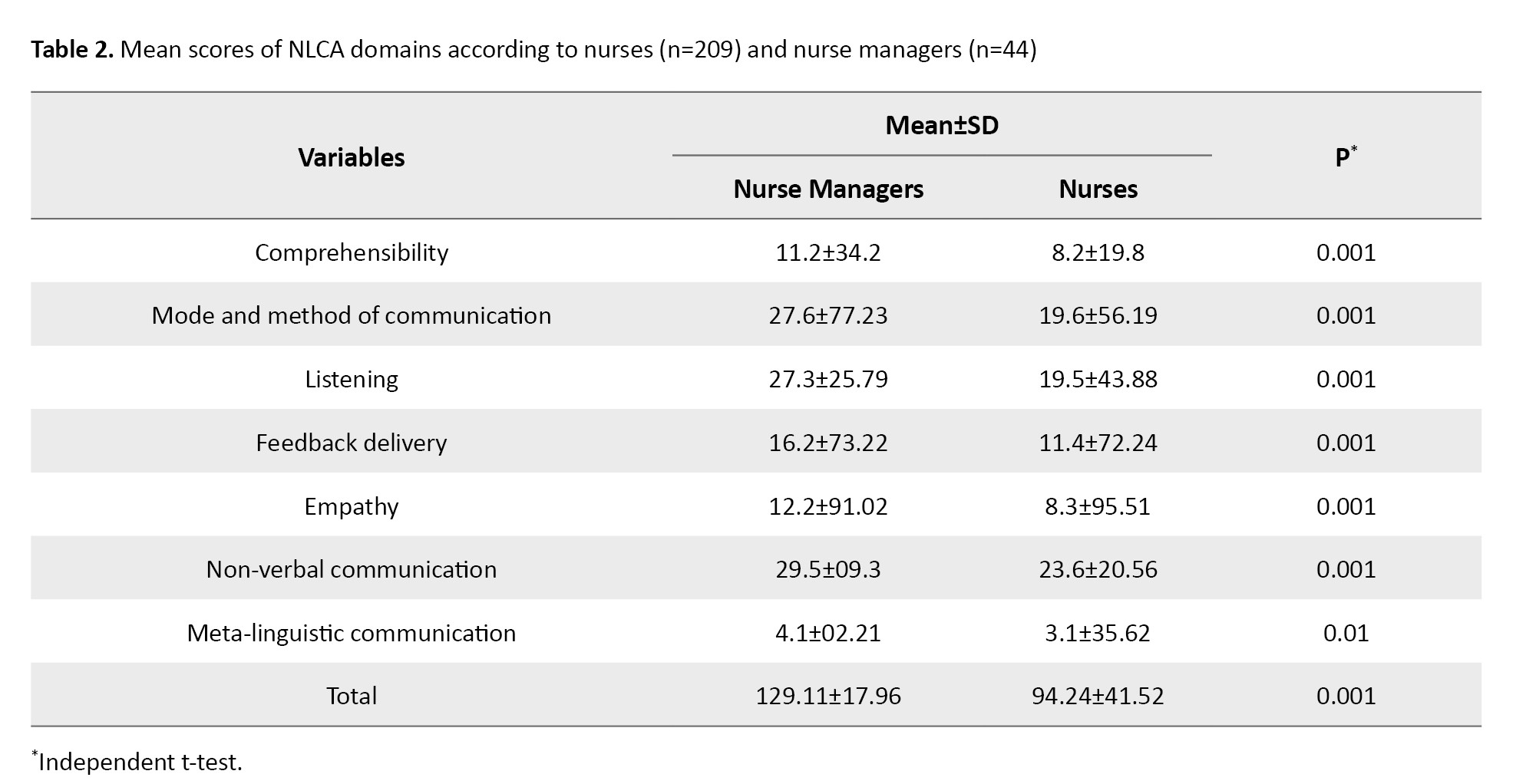
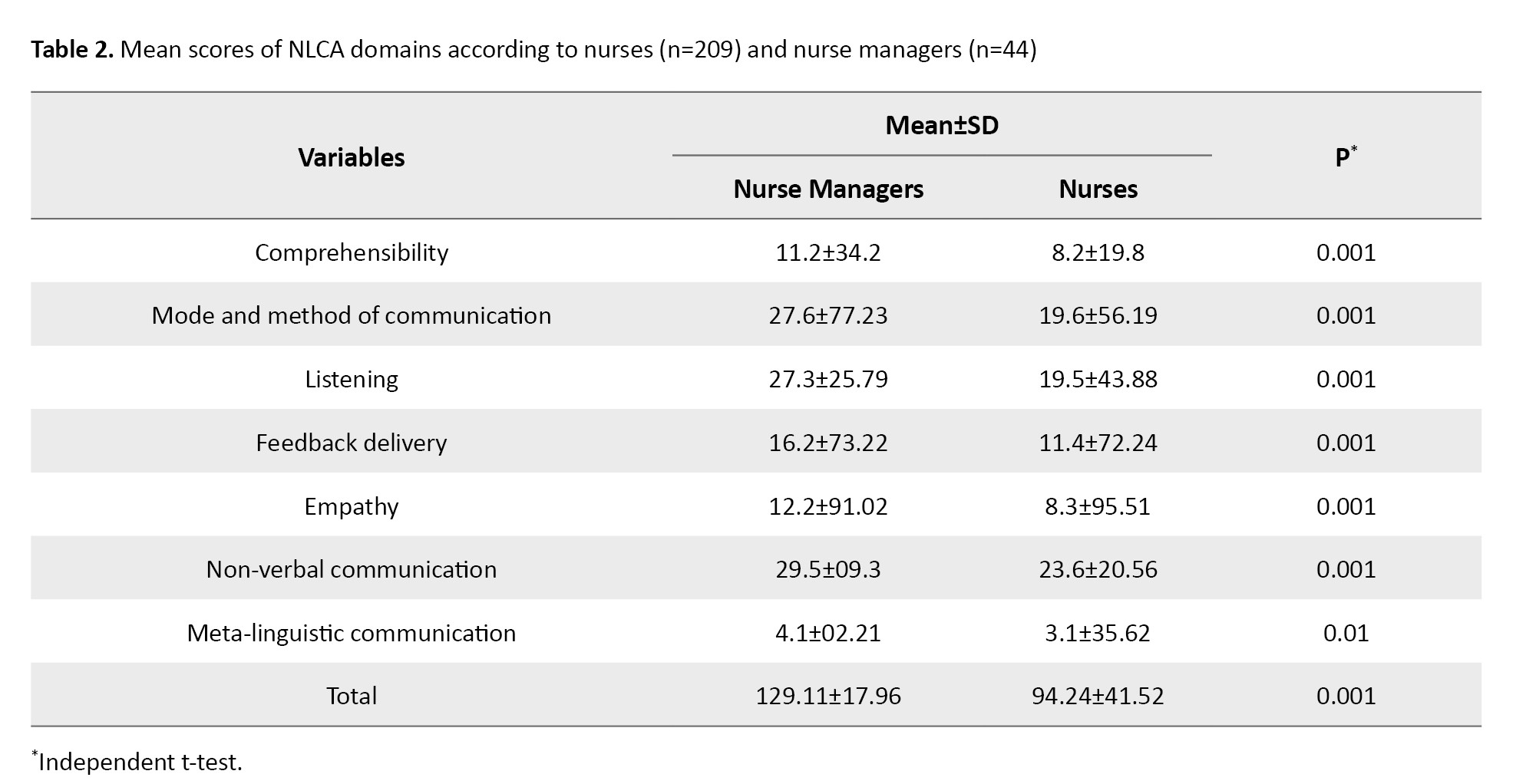
The mean total NLCA score based on the nurse managers’ perspectives was 129.11±17.96, while the score based on the nurses’ perspectives was 94.24±41.52. This difference in scores was statistically significant (P=0.001). The results for the NLCA domains are shown in Table 2.
According to the nurses’ reports, the mean total CBI-42 score was 181.42±18.34, which was significantly (P=0.01) higher than the score reported by nurse managers (172.23±23.64).
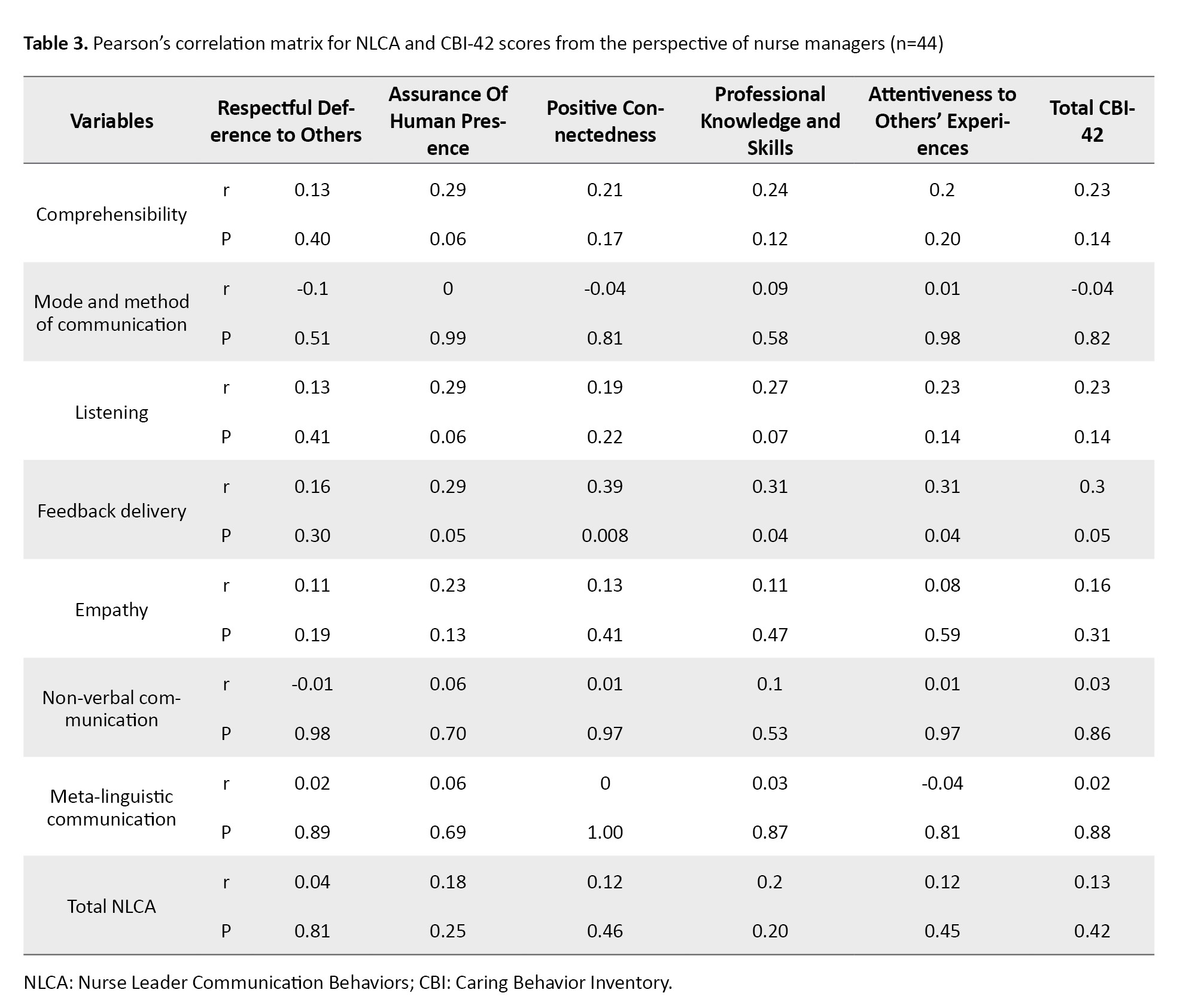
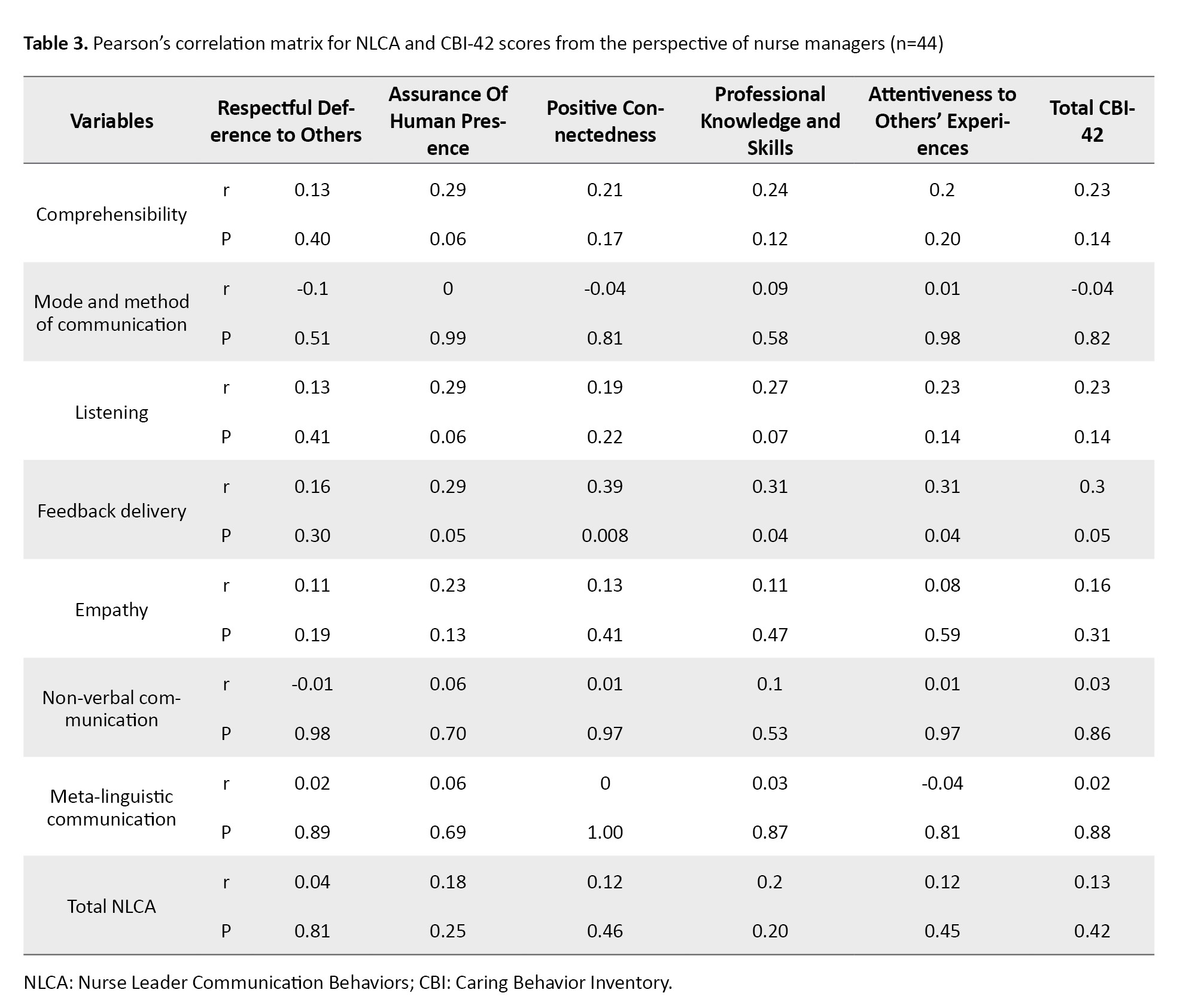
The results of Pearson’s correlation test indicated no significant relationship between the total NLCA and CBI-42 scores according to nurse managers and nurses. According to nurse managers, there was a positive and significant relationship between the feedback delivery domain of NLCA and the total CBI-42 score (r=0.30, P=0.05). No significant relationships were found for other domains of NLCA. The feedback delivery domain of NLCA had a positive relationship with professional knowledge and skills (r=0.31, P=0.04), attentiveness to others’ experiences (r=0.31, P=0.04) and positive connectedness (r=0.39, P=0.008) domains of CBI-42, from the perspective of nurse managers (Table 3).
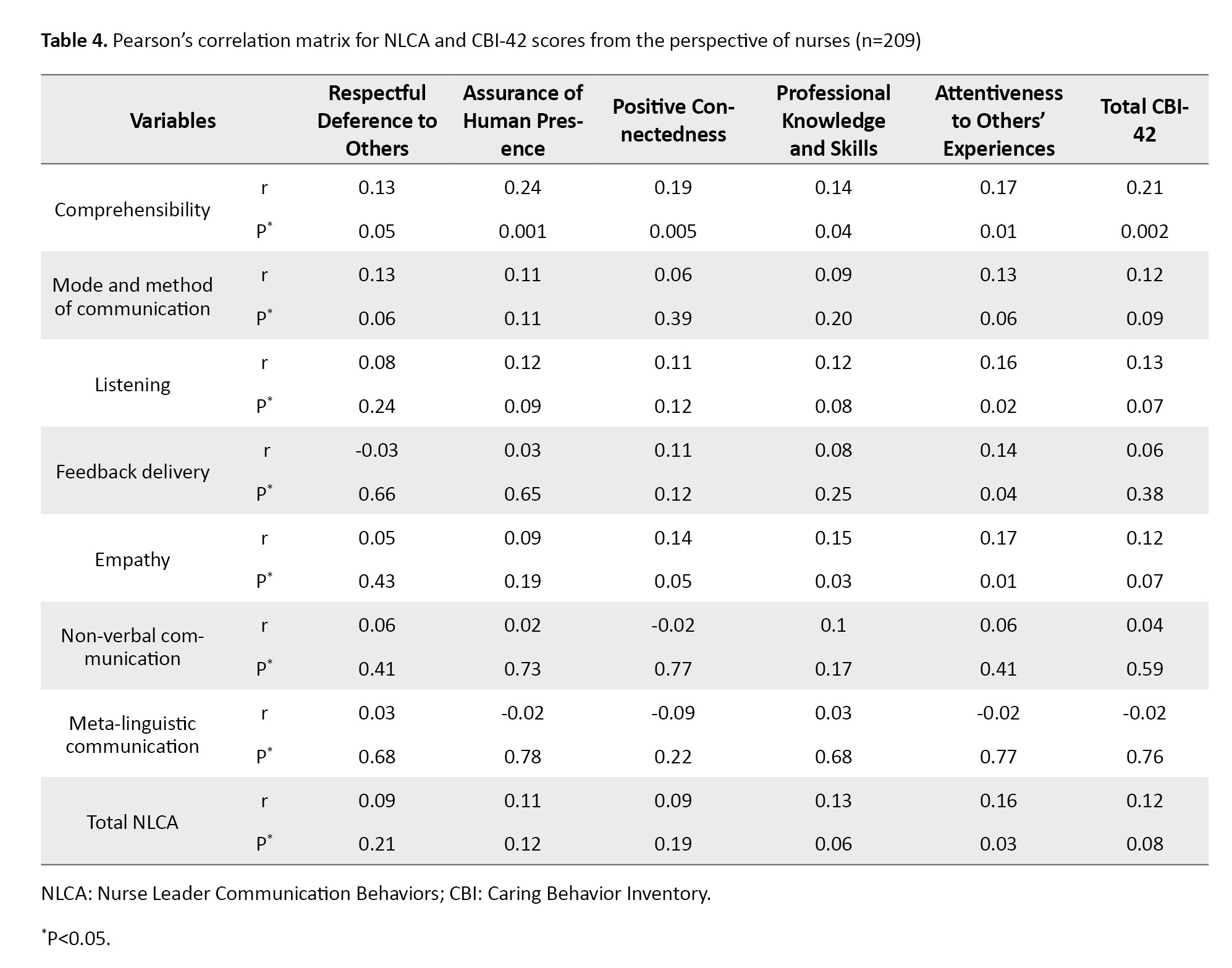
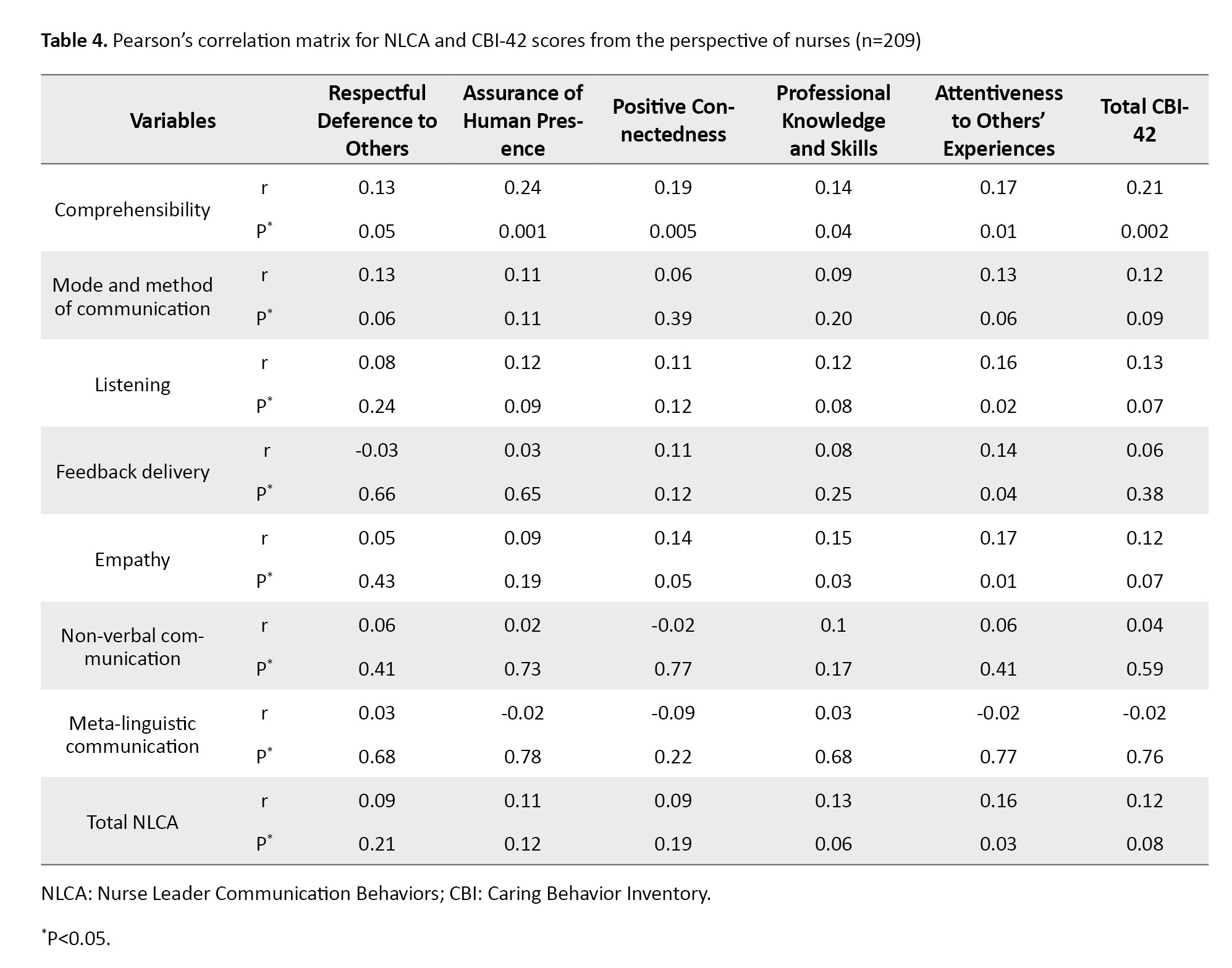
Based on the results of Pearson’s correlation test, according to nurses’ perspectives, there was a positive and significant relationship between the comprehensibility domain of NLCA and total CBI-42 score (r=0.21, P=0.002). Additionally, the attentiveness to others’ experiences domain of CBI-42 had a positive and significant relationship with the listening (r=0.16, P=0.02), feedback delivery (r=0.14, P=0.04), and empathy (r=0.17, P=0.01) domains of NLCA. The professional knowledge and skills domain of CBI-42 had a positive and significant relationship empathy domain of NLCA (r=0.15, P=0.03). No significant relationship was found between the total NLCA score and its other components, and the total CBI-42 score (Table 4).
In order to determine which NLCA domains can predict the CBI-42 score according to nurses, a multiple regression analysis was used. According to Table 5, the regression model significantly predicted 3% of the variance in the CBI-42 score.
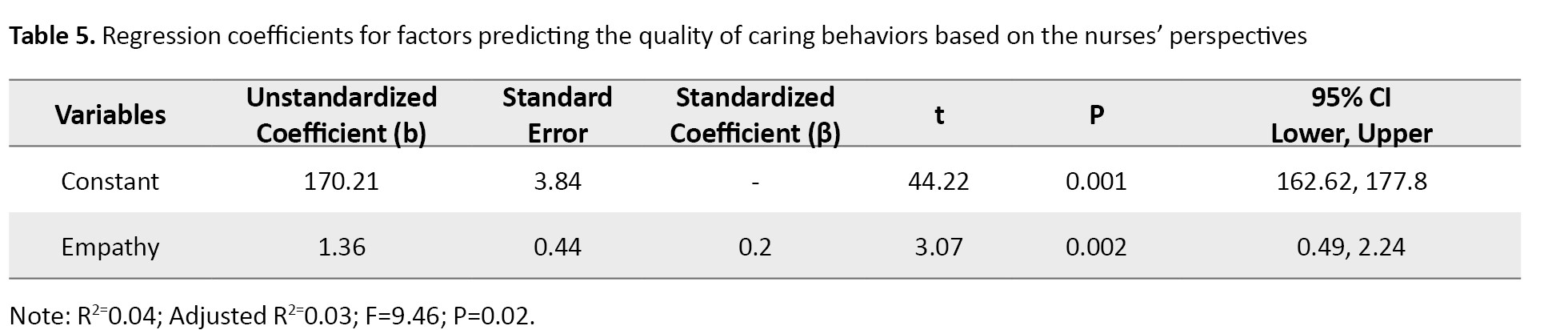
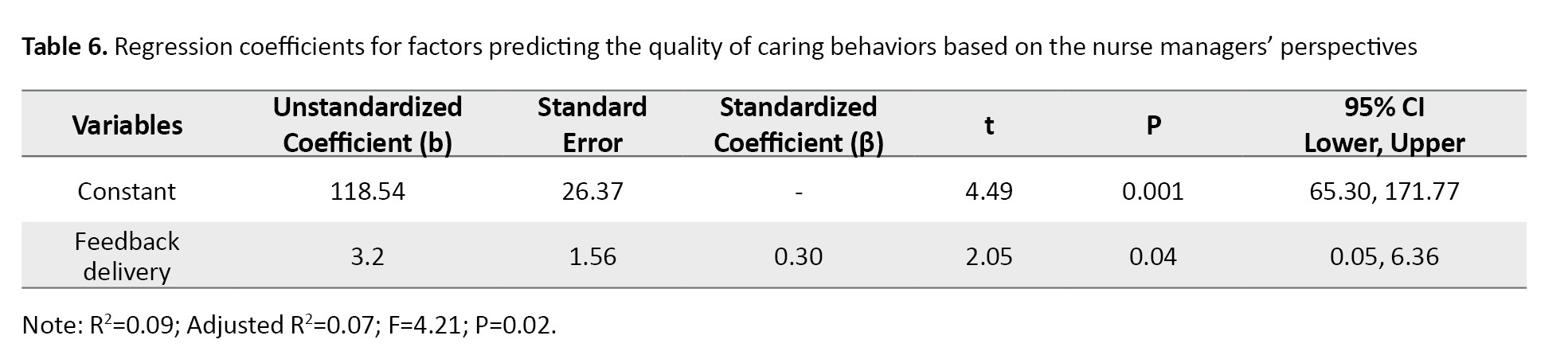
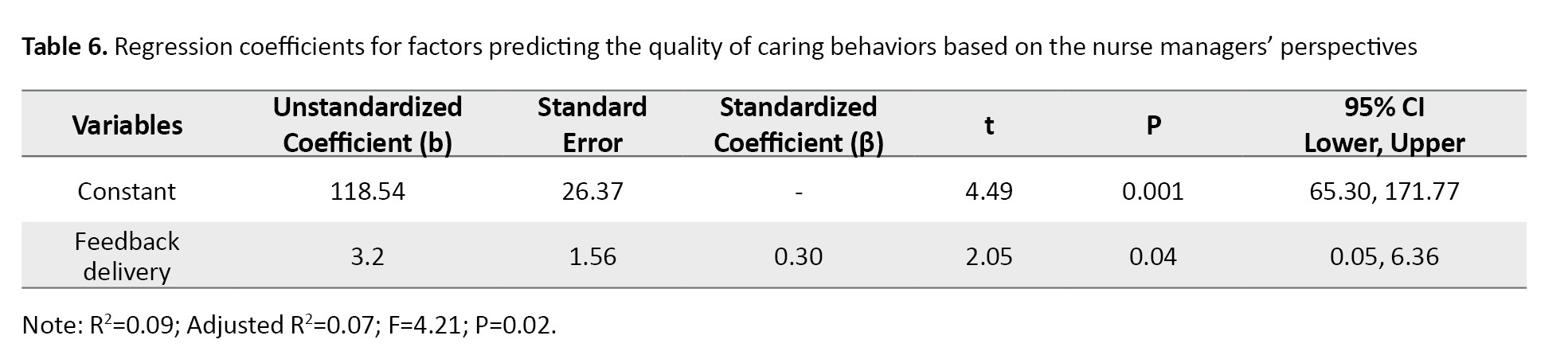
Only the empathy domain could predict the CBI-42 score based on the perspective of nurses (β=0.2, 95% CI; 0.49%, 2.24%, P=0.002). Also, according to the perspective of nurse managers, only the feedback delivery domain could predict the CBI-42 score (β=0.3, 95% CI; 0.05%, 6.36%, P=0.04). This regression model accounted for 7% of the variance in the CBI-42 score (R²=0.07). These results were shown in Table 6.
Discussion
The purpose of this study was to investigate the relationship between the communication skills of nurse managers and the quality of caring behaviors in nurses, according to the perspectives of nurses and nurse managers. The findings indicated that the quality of caring behavior in nurses working in the study hospitals was higher than the average level. This is against the results of some studies [3, 8, 18], which suggested that nurses tended to prioritize technical routine care over emotional-social care. This discrepancy can be due to the use of different measurement tools to assess the communication skills of nurse managers, or due to the difference in the study duration/time. Given the importance of nurses’ caring behaviors (with physical and psychological aspects) in enhancing professional competence, it is recommended that further studies be conducted in this area.
Although the caring behaviors of nurses were perceived as favorable by both nurse managers and nurses, there was a statistically significant difference in the scores given by nurses and nurse managers. This difference is consistent with the findings of Tohidi et al. [19], suggesting that individuals often assess themselves more favorably and want to maintain a positive self-image. However, this can hinder improvements in conditions and personal and professional growth. The results revealed that the mean score of caring behaviors given by female nurses was significantly higher than that given by male nurses. However, the score of caring behaviors showed no significant difference between male and female nurse managers. These findings are consistent with those of Tarbiyat Nazloo and Salimi [18], but are against the findings of Hosseinzadeh et al., which suggested that gender was the least important factor influencing caring behaviors [2]. This discrepancy may be due to cultural differences in different regions of Iran where studies were conducted. The study revealed that both nurse managers and nurses perceived nurse managers’ communication skills as above average. This finding is consistent with the results of other studies [12, 20] but in disagreement with those of other studies [21, 22], which reported moderate communication skills among nurse managers. It is possible that different study settings contributed to this discrepancy. Given the vital role of nurse managers in fostering a healthy work environment in hospitals, it is crucial to prioritize the maintenance or improvement of their communication skills.
Based on the results, according to nurse managers’ perspectives, there was a positive and significant relationship between feedback delivery (as a domain of communication skills) and all components of caring behaviors, except for the component of respectful deference to others. Other domains of nurse managers’ communication skills and nurses’ caring behaviors showed no significant relationship. These results are not consistent with the findings of Ahanchian and Monideri, who highlighted the managers’ recognition of the effectiveness of proper communication with human resources in facilitating the achievement of organizational goals [23]. Providing appropriate feedback is an important principle in behavior modification; therefore, to achieve quality caring behavior in nurses, it seems necessary to receive feedback from nursing managers.
According to the perspective of nurses in this study, several significant relationships were found between the components of communication skills and caring behaviors. These findings are somewhat consistent with the results of Rouse and Al-Maqbali, which emphasized that nurse managers should maintain positive and constructive relationships with nurses, providing feedback privately and respectfully, as embarrassing nurses in front of colleagues can have a negative impact on nursing care [24]. According to the perspective of nurses and nurse managers, no significant relationship was found between the total scores of communication skills and caring behaviors. This finding is not consistent with the results of Jankelová and Joniaková, who reported the direct effect of nurse managers’ communication skills and leadership style on nurses’ job satisfaction [25]. Given the impact of nurses’ caring behaviors on patients’ physical and mental well-being, it is necessary to enhance the quality of nursing care. Putra et al. [4] suggested that improving components such as listening and feedback delivery can be beneficial in this regard.
This study had some limitations. The questionnaires were distributed only in teaching hospitals in Birjand city. Future studies should also include nurses and nurse managers from non-teaching and private hospitals in other cities of Iran. Since there is a positive and significant relationship between specific components of nurses’ caring behaviors and nurse managers’ communication skills, and given the crucial role of nurses’ caring quality in enhancing patient outcomes and expediting the treatment course, hospital officials are strongly advised to take appropriate measures to improve nurse managers’ communication skills.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Birjand University of Medical Sciences, Birjand, Iran (Code: IR.BUMS.REC.1402.152). Before the study, the participants were informed about the study objectives and the confidentiality of their information, and they were free to leave the research at any time.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Conceptualization, study design, data interpretation, and final approval: All authors; Data collection: Zahra Soltani Nejad, Toktam Zia, and Maryam Salmani Mood; Data analysis and writing: Zahra Soltani Nejad and Hakimeh Sabeghi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants for their cooperation in this study.
The nursing practice is a core element of patient care [1]. The theoretical principles of nursing are rooted in an understanding of care and caregiving behaviors [2]. Patient care is synonymous with nursing care [3]. Given the significant impact of quality nursing care on patients’ well-being and overall health, caring behaviors are an important element of nursing practice [2]. Caring behavior is not only a reflection of nurses’ professional competence but also a defining and distinctive feature of the nursing profession [4, 5]. Caring behavior has two components: Physical and psychosocial. Physical caring behaviors include performing daily tasks, diagnostic interventions, treatments, procedures, education, and problem-solving, all aimed at achieving desired outcomes and physical improvement. On the other hand, psychosocial caring behaviors involve building trust, accepting the patient’s emotions, being transparent and honest, fostering a sense of hope in patients, establishing effective communication with patients, and providing emotional support to patients [6].
According to a study conducted in Taiwan, although the majority of patients are satisfied with the caring behaviors of nurses, there is still a need to enhance the quality of nursing care, particularly in addressing ethical issues such as respect and effective communication with patients [7]. The studies conducted in Iran in this field have reported conflicting results. A study focusing on nurses working in intensive care units found that, while nurses had higher scores in the physical and technical aspects of care (e.g. ensuring patient safety and administering medications), their scores were lower in the psychosocial aspect. This is concerning due to the importance of addressing patients’ psychosocial needs [8]. A cross-sectional study in Iran found that nurses placed greater emphasis on technical and routine care than on social and emotional aspects. However, this approach was insufficient to meet all patients’ needs [3]. Salimi et al. reported that Iranian nurses gave equal attention to both the physical and psychological aspects of care [9].
Various factors associated with the development and reinforcement of caring behaviors in nurses, including care competence, sense of duty, work experience, religious beliefs, and supervision of nursing care behaviors [10]. Factors such as work shift delivery process [4] and training programs for nurses also contribute to nurturing caring behaviors [6]. Inadequate organizational support and nurse dissatisfaction are intra-organizational factors that indirectly affect the provision of proper nursing care [3]. A study conducted in Indonesia found that nursing management not only contributed to nurses’ personal and professional satisfaction but also played a significant role in shaping their caring behaviors [4]. Nurse managers have a wide range of tasks, including identifying the training needs of nurses [11]. However, the primary and most crucial task of a nurse manager for achieving caring goals is to establish an effective intra-organizational communication with nurses [12]. Garon highlighted the significant role of nurse managers in cultivating a culture of communication among nurses, which directly correlates with improved patient care [13].
Recognizing the significance of delivering high-quality nursing care to patients and acknowledging the potential impact of nurse managers’ communication skills on nurses’ caring behaviors, and given the conflicting findings in the existing studies regarding the level of communication skills, quality of nursing care, and the limited research conducted in Iran, this study aimed to explore the relationship between the communication skills of nurse managers and the quality of caring behaviors in nurses.
Materials and Methods
This is a descriptive-analytical study with a cross-sectional design that was conducted in teaching hospitals affiliated with Birjand University of Medical Sciences in 2023. The nurse managers of these hospitals were selected using a census sampling method, while the nurses were selected using a non-random convenience sampling method. In this regard, 44 nurse managers (including supervisors, matrons, and head nurses) with at least two years of work experience in managerial positions were selected. Also, 209 nurses with at least 2 years of experience in providing direct patient care from various departments were selected for the study. The sample size of nurses was determined using the formula of correlation considering the Standard Deviation (SD) of nursing caring behavior (0.64) in Hosseinzadeh et al.’s study [2], 95% Confidence Interval (CI), and 5% margin of error. All nursing managers of the educational and treatment center where the research was conducted (n=44), participated in the study.
The recorded sociodemographic characteristics included: Age, sex, marital status, work experience, and education level. The Nurse Leader Communication Behaviors (NLCA) scale, developed by Hopkinson et al. in 2020 [14], was used to collect data on nurse managers’ communication skills from both managers’ and nurses’ perspectives. The questionnaire was first translated into Persian using the back-translation method, and its face validity and content validity were evaluated and confirmed (Content Validity Index [CVI] >0.79). It had high internal consistency (Cronbach’s α=0.85). It consisted of 35 items and 8 subscales, including comprehensibility, method of communication, listening, feedback delivery, empathy, non-verbal communication, meta-linguistic communication, and participation. Each item is rated on a five-point Likert scale, ranging from 0 (never) to 4 (always). The total score ranges from 0 to 140, with higher scores indicating better communication skills. The 42-item Caring Behavior Inventory (CBI-42), developed by Wolf et al. in 1998 [15], was used to assess the quality of caring behaviors from the perspective of both managers and nurses. The CBI-42 has five subscales, including respectful deference to others, assurance of human presence, positive connectedness, professional knowledge and skills, and attentiveness to others’ experiences. Each item is rated on a six-point rating scale from 1 (never) to 6 (always). The total score ranges from 42 to 252. Previous studies have reported its favorable validity (face and content) [16, 17]. To assess the reliability of this tool in our study, Cronbach’s α was calculated and obtained at 0.83.
Data were collected over two months. They were analyzed in SPSS software, version 26. Descriptive statistics (Mean±SD, and frequency) were used to describe demographic and main study variables. Also, inferential statistics including Pearson’s correlation test, stepwise linear regression analysis, chi-square test, Fisher’s exact test, and independent t-test were applied to analyze the collected data. Since the significance levels of demographic variables in the univariate regression model were not less than 0.1, none of them entered the multivariate regression model. Significance level was set at 0.05.
Results
The participants included 44 nurse managers and 209 nurses working in teaching hospitals in Birjand. The mean age of nurse managers and nurses was 44.64±6.00 and 34.22±7.72 years, and their mean work experience was 20.36±7.72 and 10.06±7.72 years, respectively. Table 1 presents the sociodemographic characteristics of both groups.
The mean total NLCA score based on the nurse managers’ perspectives was 129.11±17.96, while the score based on the nurses’ perspectives was 94.24±41.52. This difference in scores was statistically significant (P=0.001). The results for the NLCA domains are shown in Table 2.
According to the nurses’ reports, the mean total CBI-42 score was 181.42±18.34, which was significantly (P=0.01) higher than the score reported by nurse managers (172.23±23.64).
The results of Pearson’s correlation test indicated no significant relationship between the total NLCA and CBI-42 scores according to nurse managers and nurses. According to nurse managers, there was a positive and significant relationship between the feedback delivery domain of NLCA and the total CBI-42 score (r=0.30, P=0.05). No significant relationships were found for other domains of NLCA. The feedback delivery domain of NLCA had a positive relationship with professional knowledge and skills (r=0.31, P=0.04), attentiveness to others’ experiences (r=0.31, P=0.04) and positive connectedness (r=0.39, P=0.008) domains of CBI-42, from the perspective of nurse managers (Table 3).
Based on the results of Pearson’s correlation test, according to nurses’ perspectives, there was a positive and significant relationship between the comprehensibility domain of NLCA and total CBI-42 score (r=0.21, P=0.002). Additionally, the attentiveness to others’ experiences domain of CBI-42 had a positive and significant relationship with the listening (r=0.16, P=0.02), feedback delivery (r=0.14, P=0.04), and empathy (r=0.17, P=0.01) domains of NLCA. The professional knowledge and skills domain of CBI-42 had a positive and significant relationship empathy domain of NLCA (r=0.15, P=0.03). No significant relationship was found between the total NLCA score and its other components, and the total CBI-42 score (Table 4).
In order to determine which NLCA domains can predict the CBI-42 score according to nurses, a multiple regression analysis was used. According to Table 5, the regression model significantly predicted 3% of the variance in the CBI-42 score.
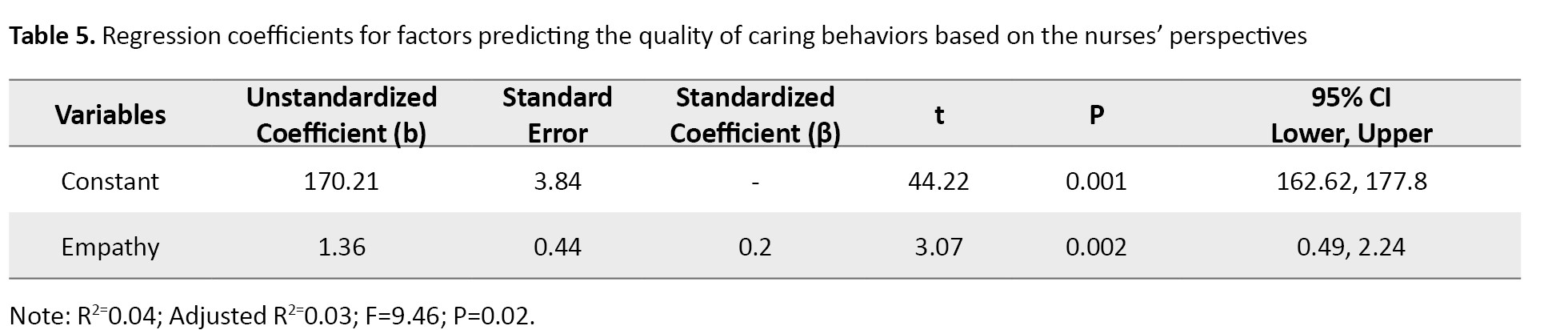
Only the empathy domain could predict the CBI-42 score based on the perspective of nurses (β=0.2, 95% CI; 0.49%, 2.24%, P=0.002). Also, according to the perspective of nurse managers, only the feedback delivery domain could predict the CBI-42 score (β=0.3, 95% CI; 0.05%, 6.36%, P=0.04). This regression model accounted for 7% of the variance in the CBI-42 score (R²=0.07). These results were shown in Table 6.
Discussion
The purpose of this study was to investigate the relationship between the communication skills of nurse managers and the quality of caring behaviors in nurses, according to the perspectives of nurses and nurse managers. The findings indicated that the quality of caring behavior in nurses working in the study hospitals was higher than the average level. This is against the results of some studies [3, 8, 18], which suggested that nurses tended to prioritize technical routine care over emotional-social care. This discrepancy can be due to the use of different measurement tools to assess the communication skills of nurse managers, or due to the difference in the study duration/time. Given the importance of nurses’ caring behaviors (with physical and psychological aspects) in enhancing professional competence, it is recommended that further studies be conducted in this area.
Although the caring behaviors of nurses were perceived as favorable by both nurse managers and nurses, there was a statistically significant difference in the scores given by nurses and nurse managers. This difference is consistent with the findings of Tohidi et al. [19], suggesting that individuals often assess themselves more favorably and want to maintain a positive self-image. However, this can hinder improvements in conditions and personal and professional growth. The results revealed that the mean score of caring behaviors given by female nurses was significantly higher than that given by male nurses. However, the score of caring behaviors showed no significant difference between male and female nurse managers. These findings are consistent with those of Tarbiyat Nazloo and Salimi [18], but are against the findings of Hosseinzadeh et al., which suggested that gender was the least important factor influencing caring behaviors [2]. This discrepancy may be due to cultural differences in different regions of Iran where studies were conducted. The study revealed that both nurse managers and nurses perceived nurse managers’ communication skills as above average. This finding is consistent with the results of other studies [12, 20] but in disagreement with those of other studies [21, 22], which reported moderate communication skills among nurse managers. It is possible that different study settings contributed to this discrepancy. Given the vital role of nurse managers in fostering a healthy work environment in hospitals, it is crucial to prioritize the maintenance or improvement of their communication skills.
Based on the results, according to nurse managers’ perspectives, there was a positive and significant relationship between feedback delivery (as a domain of communication skills) and all components of caring behaviors, except for the component of respectful deference to others. Other domains of nurse managers’ communication skills and nurses’ caring behaviors showed no significant relationship. These results are not consistent with the findings of Ahanchian and Monideri, who highlighted the managers’ recognition of the effectiveness of proper communication with human resources in facilitating the achievement of organizational goals [23]. Providing appropriate feedback is an important principle in behavior modification; therefore, to achieve quality caring behavior in nurses, it seems necessary to receive feedback from nursing managers.
According to the perspective of nurses in this study, several significant relationships were found between the components of communication skills and caring behaviors. These findings are somewhat consistent with the results of Rouse and Al-Maqbali, which emphasized that nurse managers should maintain positive and constructive relationships with nurses, providing feedback privately and respectfully, as embarrassing nurses in front of colleagues can have a negative impact on nursing care [24]. According to the perspective of nurses and nurse managers, no significant relationship was found between the total scores of communication skills and caring behaviors. This finding is not consistent with the results of Jankelová and Joniaková, who reported the direct effect of nurse managers’ communication skills and leadership style on nurses’ job satisfaction [25]. Given the impact of nurses’ caring behaviors on patients’ physical and mental well-being, it is necessary to enhance the quality of nursing care. Putra et al. [4] suggested that improving components such as listening and feedback delivery can be beneficial in this regard.
This study had some limitations. The questionnaires were distributed only in teaching hospitals in Birjand city. Future studies should also include nurses and nurse managers from non-teaching and private hospitals in other cities of Iran. Since there is a positive and significant relationship between specific components of nurses’ caring behaviors and nurse managers’ communication skills, and given the crucial role of nurses’ caring quality in enhancing patient outcomes and expediting the treatment course, hospital officials are strongly advised to take appropriate measures to improve nurse managers’ communication skills.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Birjand University of Medical Sciences, Birjand, Iran (Code: IR.BUMS.REC.1402.152). Before the study, the participants were informed about the study objectives and the confidentiality of their information, and they were free to leave the research at any time.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Conceptualization, study design, data interpretation, and final approval: All authors; Data collection: Zahra Soltani Nejad, Toktam Zia, and Maryam Salmani Mood; Data analysis and writing: Zahra Soltani Nejad and Hakimeh Sabeghi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants for their cooperation in this study.
References
- Ghafouri R, Nasiri M, Atashzadeh-Shoorideh F, Tayyar-Iravanlou F, Rahmaty Z. Translation and validation of caring behaviors inventory among nurses in Iran. Plos One. 2021; 16(7):e0254317. [DOI:10.1371/journal.pone.0254317] [PMID]
- Hosseinzadeh H, Mohammadi M, Shamshiri M. [The study of caring behaviors and its determinant factors from the perspective of nurses in educational hospitals of Ardabil (Persian)]. J Health Care. 2019; 21(3):203-11. [DOI:10.29252/jhc.21.3.203]
- Baljani E, Azimi N, Hosseinloo A. [A survey on nurses’ perception of the importance of caring behaviors and factors affecting its provision (Persian)]. Evid Based Care J. 2012; 2(1):13-21. [DOI:10.22038/ebcj.2012.377]
- Putra KR, Andayani T, Ningrum EH. Job satisfaction and caring behavior among nurses in a military hospital: A cross-sectional study. J Public Health Res. 2021; 10(2):2212. [DOI:10.4081/jphr.2021.2212] [PMID]
- Lee H, Seo K. Mediating effect of compassion competence on the relationship between caring behaviors and quality of nursing services in South Korea. Healthcare (Basel, Switzerland). 2022; 10(5):964.[DOI:10.3390/healthcare10050964] [PMID]
- Gheybi M, Zeinali A. [The role of meta-memory and positive meta-cognitions and meta-emotions in predicting caring behavior of nurses (Persian)]. J Nurs Educ. 2021; 10(4):19-21. [Link]
- Kuo FH, Huang HM, Sun FK, Lin WJ. [Interpersonal communication competence and conflict handling styles of nurses in intensive care units (Chinese)]. Hu Li Za Zhi. 2019; 66(2):67-76. [DOI:10.6224/JN.201904_66(2).00] [PMID]
- Asgari Z, Pahlavanzadeh S, Alimohammadi N, Alijanpour S. [Quality of holistic nursing care from critical care nurses’ point of view (Persian)]. Criti Care Nurs. 2019; 12(1):9-14. [Link]
- Salimi S, Azimpour A, Fesharaki M, Mohammadzadeh SH. [Nurses’ perception of importance of caring behaviors and its determinant factors (Persian)]. Nurs Midwifery J. 2012; 10(1):1-12. [Link]
- De Los Santos JAA, Labrague LJ. Job engagement and satisfaction are associated with nurse caring behaviours: A cross-sectional study.J Nurs Manag. 2021; 29(7):2234-42. [DOI:10.1111/jonm.13384] [PMID]
- Abbassi M, Hajibabaee F. [Communication competencies of nursing managers: A review study (Persian)]. Iran J Nurs Res. 2021; 16 (5):10-18. [Link]
- Amraei M, Valizadi H, Haghighizadeh MH, Faraji-Khiavi F. The relationship between managers communication skills and organizational performance of nurses in educational hospitals. Depiction Health. 2022; 13(1):83-96. [DOI:10.34172/doh.2022.07]
- Garon M. Speaking up, being heard: Registered nurses’ perceptions of workplace communication. J Nurs Manag. 2012. 20(3):361-71. [DOI:10.1111/j.1365-2834.2011.01296.x] [PMID]
- Hopkinson SG, Glaser D, Napier C, Trego LL. Developing an instrument to assess empowering nurse leader communication behaviours. J Nurs Manag. 2021; 29(7):2037-46. [DOI:10.1111/jonm.13340] [PMID]
- Wolf ZR, Colahan M, Costello A. Relationship between nurse caring and patient satisfaction. Medsurg Nurs. 1998; 7(2):99-105. [PMID]
- Rafii F, Oskouie F, Peravi H, Haghani H. [A comparative study of the effectiveness of the clinical practice of fundamental nursing through role-play versus traditional method on caring behaviors of sophomore-level nursing students (Persian)]. Iran J Nurs. 2009; 22(60):42-52. [Link]
- Hajinezhad MS, Rafii F, Jafarjalal E, Haghani H. [relationship between nurse caring behaviors from patients’ perspectives & their satisfaction (Persian)]. Iran J Nurs. 2007; 20(49):73-83. [Link]
- Tarbiyat Nazloo S, Salimi S. [Predictors of nursing care behaviors in critical care units (Persian)]. Nurs Midwifery J. 2019; 17 (5):371-8. [Link]
- Tohidi S, Norozi H, Karimi Moonaghi H, behnamvoshani H. [Correlation between nurses’ self-assessment scores with the scores observed in the performance of their teaching competency in patient education (Persian)]. Nurs Midwifery J. 2015; 13(7):588-95. [Link]
- Acefzadeh S, Fatehi F, Mohamadi M. [The relationship between Head-nurses’ communication skills and demographic characteristics in educational hospoitals of Sanandaj: A cross sectional study (Persian)]. Zanko J Med Sci. 2018; 18(59):48-56. [Link]
- Eghtedar S, Soheili A, Nemati S. [The communication skills of nursing managers and their associations with nurses’ job satiafaction and anxiety (Persian)]. Nurs Midwifery J. 2023; 21 9):708-17. [DOI:10.61186/unmf.21.9.708]
- Tabibi SJ, Nasiripoor A, Zahiri Abyaneh Z. [Relationship between managers communication skill and staff motivation in Modarres Hospital of Tehran (Persian)]. J Hosp. 2013; 12(2):73-80. [Link]
- Ahanchian M, Monideri R. [Relationship between communication skills and organizational health (Persian)]. J Exec Manage. 2004; 4(12):41-60. [Link]
- Rouse RA, Al-Maqbali M. Identifying nurse managers’ essential communication skills: An analysis of nurses’ perceptions in Oman. J Nurs Manag. 2014; 22(2):192-200. [DOI:10.1111/jonm.12222] [PMID]
- Jankelová N, Joniaková Z. Communication skills and transformational leadership style of first-line nurse managers in relation to job satisfaction of nurses and moderators of this relationship. Healthcare (Basel, Switzerland). 2021;9(3):346. [DOI:10.3390/healthcare9030346] [PMID]
Article Type : Research |
Subject:
Special
Received: 2024/03/2 | Accepted: 2025/05/13 | Published: 2026/01/11
Received: 2024/03/2 | Accepted: 2025/05/13 | Published: 2026/01/11
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






