Fri, Nov 21, 2025
Volume 35, Issue 4 (9-2025)
JHNM 2025, 35(4): 259-269 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abbaszadeh F, Khakbazan Z, Damghanian M, Zareiyan A, Jaafarpour M, Rasoulzadeh Bidgoli M. Development and Psychometric Evaluation of Maternity Care Quality in Maternity Units Scale (MCQ-MUS). JHNM 2025; 35 (4) :259-269
URL: http://hnmj.gums.ac.ir/article-1-2316-en.html
URL: http://hnmj.gums.ac.ir/article-1-2316-en.html
Development and Psychometric Evaluation of Maternity Care Quality in Maternity Units Scale (MCQ-MUS)
Fatemeh Abbaszadeh1 
 , Zohreh Khakbazan2
, Zohreh Khakbazan2 
 , Maryam Damghanian *3
, Maryam Damghanian *3 
 , Armin Zareiyan4
, Armin Zareiyan4 
 , Molouk Jaafarpour5
, Molouk Jaafarpour5 
 , Mahboobeh Rasoulzadeh Bidgoli1
, Mahboobeh Rasoulzadeh Bidgoli1 


 , Zohreh Khakbazan2
, Zohreh Khakbazan2 
 , Maryam Damghanian *3
, Maryam Damghanian *3 
 , Armin Zareiyan4
, Armin Zareiyan4 
 , Molouk Jaafarpour5
, Molouk Jaafarpour5 
 , Mahboobeh Rasoulzadeh Bidgoli1
, Mahboobeh Rasoulzadeh Bidgoli1 

1- Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran.
2- Nursing and Midwifery Care Research Center, Tehran University of Medical Sciences, Tehran, Iran.
3- Nursing and Midwifery Care Research Center, Tehran University of Medical Sciences, Tehran, Iran. ,maryamdamghanian@gmail.com
4- Associate Professor, Department of Public Health Nursing, Nursing Faculty, Aja University of Medical Sciences, Tehran, Iran.
5- Assistant Professor, Department of Midwifery, School of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
2- Nursing and Midwifery Care Research Center, Tehran University of Medical Sciences, Tehran, Iran.
3- Nursing and Midwifery Care Research Center, Tehran University of Medical Sciences, Tehran, Iran. ,
4- Associate Professor, Department of Public Health Nursing, Nursing Faculty, Aja University of Medical Sciences, Tehran, Iran.
5- Assistant Professor, Department of Midwifery, School of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
Full-Text [PDF 556 kb]
(117 Downloads)
| Abstract (HTML) (253 Views)
References
Full-Text: (84 Views)
Introduction
Care quality refers to “the degree to which healthcare services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” [1]. Care quality can also be defined in a three-dimensional format, in which the relationships among structure, process, and outcomes are based on the notion that a good structure should promote a good process and a good process should promote good outcomes [2]. Maternity Care Quality (MCQ) has a significant impact on childbirth outcomes and can help reduce maternal and perinatal mortality rates, ultimately contributing to the achievement of the sustainable development goals [3, 4]. Nonetheless, according to the World Health Organization (WHO), despite the improved accessibility of maternity care services worldwide, the MCQ has not improved proportionately [5]. There is no clear definition for the concept of MCQ, and there are limited studies in this field. The MCQ is beyond the administration of medications and monitoring of women during labor; it is the emotional presence of healthcare providers for the women to comfort them through providing guidance, support, and counseling [6]. Respectful Maternity Care (RMC) is a key approach for MCQ improvement [7].
For MCQ improvement, an assessment is first needed, which helps assess the quality of care plans, the process of their implementation, and their success rate. MCQ assessment requires standardized instruments. To our knowledge, there is no comprehensive tool to evaluate the MCQ in the maternity units. There is an instrument for MCQ assessment called the GRIlle d’Observation des Soins (GRIOS), which was developed based on available guidelines in Senegal and in accordance with the guidelines of the International Federation of Gynecology and Obstetrics (FIGO) [5]. This instrument has 12 criteria to assess the process of intrapartum care and does not include items related to the structural aspects of MCQ such as access to resources. Moreover, the development of this instrument, based on the guidelines of a local area and a federation, limits its generalizability to other cultural contexts. A study identified and suggested 30 quality indicators for care assessment in birth centers in the Netherlands [8], which are context-specific and cannot be easily generalized to other contexts. Additionally, these indicators are specific to birth centers, as such centers for childbirth are not available in Iran.
It seems that in Iran, there is no comprehensive and standard tool based on a tool design process framework to evaluate the MCQ. Instruments used for MCQ assessment in Iran have addressed some aspects of MCQ. For example, one study only included items on the process component of the MCQ [9], while another study included the items related to the structure and process components of the MCQ [10]. Other studies also used instruments which addressed only some aspects of MCQ such as midwives’ knowledge and practice concerning respectful RMC [11] and midwives’ relationships with women in maternity units [12]. The lack of a comprehensive instrument for MCQ assessment in Iran underscores the need to design a culturally adapted tool for this purpose. Therefore, the present study aims to develop and evaluate the psychometric properties of the MCQ in Maternity Units Scale (MCQ-MUS).
Materials and Methods
This study with an exploratory sequential mixed methods design was conducted from February 2019 to September 2021, based on the classical test theory and in two phases. In the first phase of the study, the MCQ-MUS was developed through a hybrid concept analysis. Since the concept of care quality has been defined and its importance has been proven in existing studies, and its relationship with maternal care has been determined [13-15], we intended to reach a higher level of its expansion and evolution through the concept analysis and break the concepts into their components and rebuild them so that their features and dimensions are well defined as completely as possible [16] and provide a clear definition of the concept. The hybrid model integrates deductive methods (a literature review) and inductive methods (a qualitative study) to provide more detailed data and clearer explanations about the concepts and, hence, is preferred over other concept analysis approaches [17]. It consists of three main stages: theoretical, fieldwork, and final analysis. In the theoretical stage, an integrative review study was conducted based on Whittemore and Knafl’s approach [18], which provides a framework for the comprehensive assessment of complex concepts or theories and allows for the inclusion of studies with different methodologies in the review [19]. The steps of this phase included specifying the review purpose, searching the literature, evaluating data, analyzing data, and presenting the results. The first step provides a comprehensive definition for the concept of MCQ in maternity units through determining its attributes, antecedents, and consequences. In the second step, online databases such as Medline, as well as the websites of healthcare and midwifery care organizations such as the WHO and the international confederation of midwives, were searched to retrieve articles published until July 6, 2019 because we started our search from this date and there have been many changes in the method of maternal care during childbirth due to the development of mother-friendly hospitals and the practice of physiological childbirth. Finally, 21 qualitative studies, 12 review studies, one mixed-methods study, one cross-sectional study, and two guidelines were retrieved and their quality was appraised using the mixed appraisal tool (for qualitative and quantitative studies), the appraisal of guidelines research and evaluation (for guidelines), and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (for review studies). Conventional content analysis was used to determine the attributes, antecedents, and consequences of the concept of MCQ in maternity units. The results of this integrative review have been reported in our previous study [20]. In the fieldwork stage of the hybrid concept analysis, a descriptive qualitative study was conducted. Participants were four midwives, two faculty members of the midwifery department, three obstetricians and their assistants, two policy makers, and six postpartum women, who were purposively selected from the Kashan University of Medical Sciences and public and private hospitals in Kashan, Iran. Data were collected through in-depth semi-structured interviews held in participants’ preferred places. Each interview took 25–60 minutes. Data were analyzed in MAXQDA software, version 18 using Graneheim and Lundman’s conventional content analysis method [21]. The results of this qualitative study have been reported in our previous study [22]. In the final stage of the hybrid concept analysis, the codes and categories generated in the first and second phases were compared and combined, and the different dimensions of the concept of MCQ in maternity units were determined and used to generate the items of MCQ-MUS.
In the second phase of the study, the psychometric properties, including face validity, content validity, construct validity, and reliability, were assessed. Qualitative and quantitative methods were used to assess face validity. In the qualitative assessment, ten midwives from maternity units were interviewed about the difficulty, suitability, and clarity of the items. Based on their comments, revisions were made. In the quantitative assessment, ten midwives from maternity units were invited to rate the comprehensibility of the items on a five-point scale from 1 (“low comprehensibility”) to 5 (“high comprehensibility”). Then, the item impact score was calculated based on their rating. Items with impact scores >1.5 were considered appropriate [23].
Content validity of MCQ-MUS was also assessed using qualitative and quantitative methods. For qualitative assessment, 10 midwifery instructors experienced in maternity care were invited to give written feedback on the wording, grammar, allocation, and scoring of the items. The items were then revised based on their comments. For quantitative assessment, the Content Validity Ratio (CVR) and Content Validity Index (CVI) were calculated. Accordingly, 15 experts in maternity care were asked to rate each item on a three-point scale: 2=essentia, 1=useful but not essential, and 0=unessential. Then CVR was calculated using the Equation 1:
1. CVR=(ne-(N/2)/(N/2)
where N was the total number of experts and ne was the number of experts who rated an item as “essential”. The minimum acceptable CVR is 0.49 when the number of experts is 15 [24]. Moreover, experts were asked to rate item relevance on a four-point scale: 4=completely relevant, 3=relevant, 2= somewhat relevant, and 1= irrelevant. Then, CVI was calculated by dividing the number of experts rated an item 3 or 4 by the total number of experts. The minimum acceptable CVI value is 0.78 [25]. The average scale-level CVI (S-CVI/Ave) was also calculated by averaging the item CVI values. An S-CVI/Ave value >0.80 is considered acceptable, and a value >0.90 is considered excellent [26]. Modified kappa was also calculated for each item to reduce the probability of chance agreement. This statistic reflects inter-rater agreement and is interpreted as: Excellent (>0.74), good (0.60–0.74), or weak (<0.6) [27].
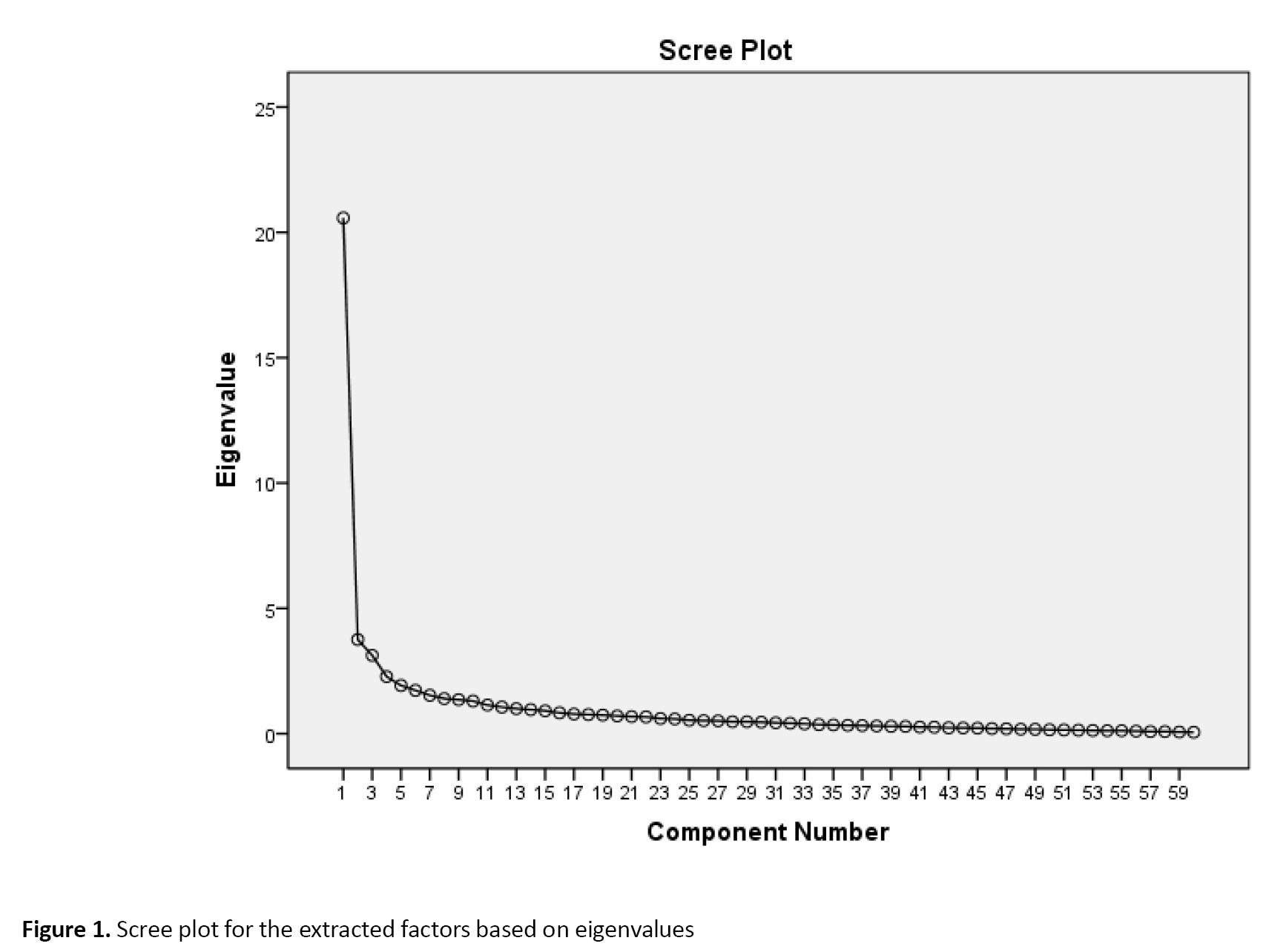
For assessment of construct validity, the Exploratory Factor Analysis (EFA) was performed. Accordingly, 220 midwives with a work experience of more than two years and a bachelor’s degree or higher were selected from hospitals affiliated to Tehran and Kashan medical universities. The Keyser-Meyer-Olkin (KMO) and the Bartlett’s tests were conducted to test sampling adequacy and factor analysis appropriateness, and the number of factors was determined based on eigenvalues and scree plot. The minimum factor loading value was set at 0.3, and eigenvalues less than one were omitted [28]. Principal Axis Factoring (PAF) with Promax rotation was used in factor analysis. Data normality and outliers were assessed using skewness (±3) and kurtosis (±7) [29].
For the assessment of internal consistency and test-retest reliability, 30 midwives from maternity units completed MCQ-MUS at two time points with an interval of two weeks and their test data were used to calculate Cronbach’s α for internal consistency and their test-retest data were used to calculate Intraclass Correlation Coefficient (ICC) for test/re-test reliability using the two-way mixed model. ICC values more than 0.80 were considered acceptable. Moreover, Standard Error of Measurement (SEM) was calculated as Equation 2:
2. SEM =Sd√1-ICC
where SD was the standard deviation.
Results
In the first phase, based on the results of the theoretical [22] and fieldwork [20] stages of the hybrid concept analysis, definitions and concepts were integrated and, finally, the concept of MCQ in maternity units was defined as “a complex and multidimensional concept which refers to the process of providing care to the parturient during the childbirth process by a morally and scientifically competent midwife based on professional standards and mental/emotional/informational/instrumental support in order to empower the parturient and improve her self-efficacy in maternity unit under appropriate physical conditions and using adequate equipment, which maintains maternal and neonatal health and leads to a positive childbirth experience and is influenced by internal and external motivation, attention to the parturient expectations, physical/psychological preparation of the parturient during pregnancy, and efficient managerial support”. This definition revealed that the four dimensions of the concept encompassed effective interaction, maternal empowerment, professional care, and appropriate human and physical resources. Based on this definition and the results of the hybrid concept analysis, a primary item pool with 150 items was created. Items were compared, revised, and combined. Finally, an initial draft of MCQ-MUS with 88 items was developed.
In assessing face validity, the impact scores of all items were found to be in the range of 2.6-5, i.e. more than the minimum acceptable value of 1.5, and hence, none of the items was omitted. In the qualitative face validity assessment, five items were revised due to poor comprehensibility. In assessing content validity, four items were revised, nine overlapping items were combined, three items were omitted, one new item was added, and the allocation of two items was changed based on experts’ comments. During the quantitative content validity assessment of the 77-item draft, six items with CVR values <0.49 were omitted. The remaining items had acceptable CVI values of 0.88–1. The S-CVI/Ave was 0.94, and the modified kappa value of the items was in the range of 0.72–1.
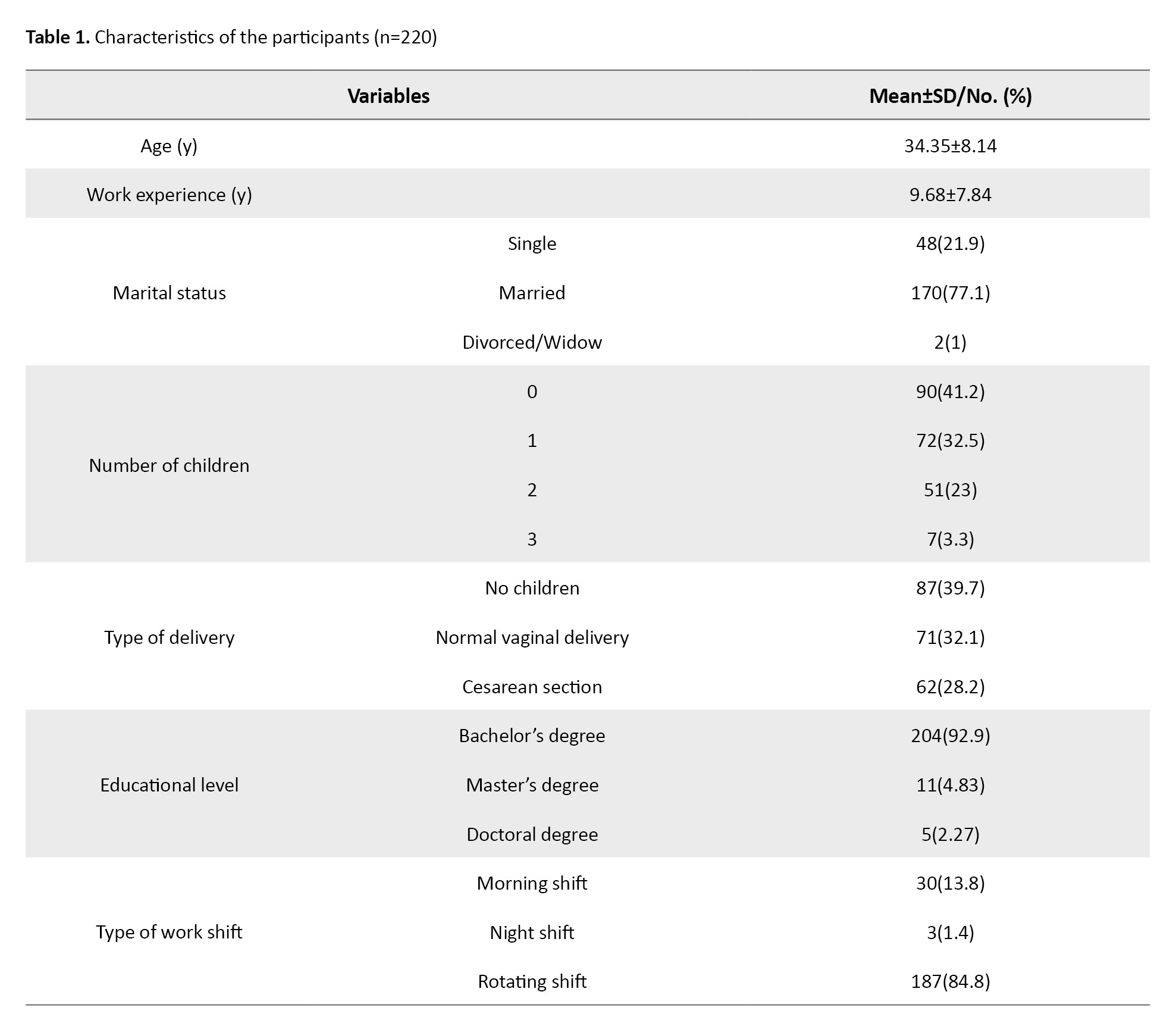
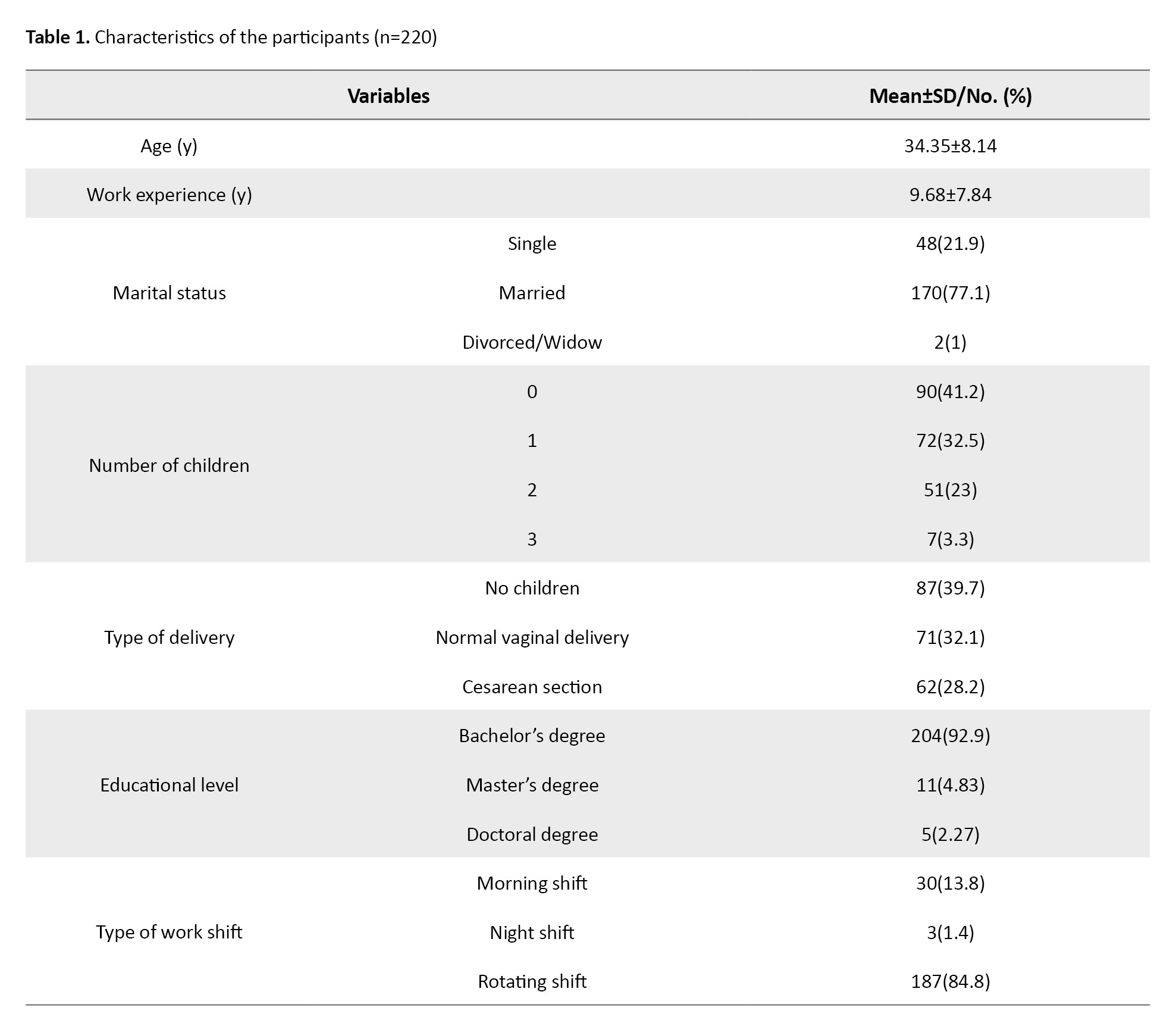
Participants who were selected for assessment of construct validity were 220 midwives with a mean age of 34.35±8.14 years and a mean work experience of 9.68±7.84 years. Most participants had a bachelor’s degree and rotating work shifts (Table 1).
The KMO value was obtained as 0.922, and the Bartlett’s test was significant (P=0.001), confirming sampling adequacy (Table 2).

The scree plot showed a five-factor structure for MCQ-MUS (Figure 1).
Care quality refers to “the degree to which healthcare services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” [1]. Care quality can also be defined in a three-dimensional format, in which the relationships among structure, process, and outcomes are based on the notion that a good structure should promote a good process and a good process should promote good outcomes [2]. Maternity Care Quality (MCQ) has a significant impact on childbirth outcomes and can help reduce maternal and perinatal mortality rates, ultimately contributing to the achievement of the sustainable development goals [3, 4]. Nonetheless, according to the World Health Organization (WHO), despite the improved accessibility of maternity care services worldwide, the MCQ has not improved proportionately [5]. There is no clear definition for the concept of MCQ, and there are limited studies in this field. The MCQ is beyond the administration of medications and monitoring of women during labor; it is the emotional presence of healthcare providers for the women to comfort them through providing guidance, support, and counseling [6]. Respectful Maternity Care (RMC) is a key approach for MCQ improvement [7].
For MCQ improvement, an assessment is first needed, which helps assess the quality of care plans, the process of their implementation, and their success rate. MCQ assessment requires standardized instruments. To our knowledge, there is no comprehensive tool to evaluate the MCQ in the maternity units. There is an instrument for MCQ assessment called the GRIlle d’Observation des Soins (GRIOS), which was developed based on available guidelines in Senegal and in accordance with the guidelines of the International Federation of Gynecology and Obstetrics (FIGO) [5]. This instrument has 12 criteria to assess the process of intrapartum care and does not include items related to the structural aspects of MCQ such as access to resources. Moreover, the development of this instrument, based on the guidelines of a local area and a federation, limits its generalizability to other cultural contexts. A study identified and suggested 30 quality indicators for care assessment in birth centers in the Netherlands [8], which are context-specific and cannot be easily generalized to other contexts. Additionally, these indicators are specific to birth centers, as such centers for childbirth are not available in Iran.
It seems that in Iran, there is no comprehensive and standard tool based on a tool design process framework to evaluate the MCQ. Instruments used for MCQ assessment in Iran have addressed some aspects of MCQ. For example, one study only included items on the process component of the MCQ [9], while another study included the items related to the structure and process components of the MCQ [10]. Other studies also used instruments which addressed only some aspects of MCQ such as midwives’ knowledge and practice concerning respectful RMC [11] and midwives’ relationships with women in maternity units [12]. The lack of a comprehensive instrument for MCQ assessment in Iran underscores the need to design a culturally adapted tool for this purpose. Therefore, the present study aims to develop and evaluate the psychometric properties of the MCQ in Maternity Units Scale (MCQ-MUS).
Materials and Methods
This study with an exploratory sequential mixed methods design was conducted from February 2019 to September 2021, based on the classical test theory and in two phases. In the first phase of the study, the MCQ-MUS was developed through a hybrid concept analysis. Since the concept of care quality has been defined and its importance has been proven in existing studies, and its relationship with maternal care has been determined [13-15], we intended to reach a higher level of its expansion and evolution through the concept analysis and break the concepts into their components and rebuild them so that their features and dimensions are well defined as completely as possible [16] and provide a clear definition of the concept. The hybrid model integrates deductive methods (a literature review) and inductive methods (a qualitative study) to provide more detailed data and clearer explanations about the concepts and, hence, is preferred over other concept analysis approaches [17]. It consists of three main stages: theoretical, fieldwork, and final analysis. In the theoretical stage, an integrative review study was conducted based on Whittemore and Knafl’s approach [18], which provides a framework for the comprehensive assessment of complex concepts or theories and allows for the inclusion of studies with different methodologies in the review [19]. The steps of this phase included specifying the review purpose, searching the literature, evaluating data, analyzing data, and presenting the results. The first step provides a comprehensive definition for the concept of MCQ in maternity units through determining its attributes, antecedents, and consequences. In the second step, online databases such as Medline, as well as the websites of healthcare and midwifery care organizations such as the WHO and the international confederation of midwives, were searched to retrieve articles published until July 6, 2019 because we started our search from this date and there have been many changes in the method of maternal care during childbirth due to the development of mother-friendly hospitals and the practice of physiological childbirth. Finally, 21 qualitative studies, 12 review studies, one mixed-methods study, one cross-sectional study, and two guidelines were retrieved and their quality was appraised using the mixed appraisal tool (for qualitative and quantitative studies), the appraisal of guidelines research and evaluation (for guidelines), and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (for review studies). Conventional content analysis was used to determine the attributes, antecedents, and consequences of the concept of MCQ in maternity units. The results of this integrative review have been reported in our previous study [20]. In the fieldwork stage of the hybrid concept analysis, a descriptive qualitative study was conducted. Participants were four midwives, two faculty members of the midwifery department, three obstetricians and their assistants, two policy makers, and six postpartum women, who were purposively selected from the Kashan University of Medical Sciences and public and private hospitals in Kashan, Iran. Data were collected through in-depth semi-structured interviews held in participants’ preferred places. Each interview took 25–60 minutes. Data were analyzed in MAXQDA software, version 18 using Graneheim and Lundman’s conventional content analysis method [21]. The results of this qualitative study have been reported in our previous study [22]. In the final stage of the hybrid concept analysis, the codes and categories generated in the first and second phases were compared and combined, and the different dimensions of the concept of MCQ in maternity units were determined and used to generate the items of MCQ-MUS.
In the second phase of the study, the psychometric properties, including face validity, content validity, construct validity, and reliability, were assessed. Qualitative and quantitative methods were used to assess face validity. In the qualitative assessment, ten midwives from maternity units were interviewed about the difficulty, suitability, and clarity of the items. Based on their comments, revisions were made. In the quantitative assessment, ten midwives from maternity units were invited to rate the comprehensibility of the items on a five-point scale from 1 (“low comprehensibility”) to 5 (“high comprehensibility”). Then, the item impact score was calculated based on their rating. Items with impact scores >1.5 were considered appropriate [23].
Content validity of MCQ-MUS was also assessed using qualitative and quantitative methods. For qualitative assessment, 10 midwifery instructors experienced in maternity care were invited to give written feedback on the wording, grammar, allocation, and scoring of the items. The items were then revised based on their comments. For quantitative assessment, the Content Validity Ratio (CVR) and Content Validity Index (CVI) were calculated. Accordingly, 15 experts in maternity care were asked to rate each item on a three-point scale: 2=essentia, 1=useful but not essential, and 0=unessential. Then CVR was calculated using the Equation 1:
1. CVR=(ne-(N/2)/(N/2)
where N was the total number of experts and ne was the number of experts who rated an item as “essential”. The minimum acceptable CVR is 0.49 when the number of experts is 15 [24]. Moreover, experts were asked to rate item relevance on a four-point scale: 4=completely relevant, 3=relevant, 2= somewhat relevant, and 1= irrelevant. Then, CVI was calculated by dividing the number of experts rated an item 3 or 4 by the total number of experts. The minimum acceptable CVI value is 0.78 [25]. The average scale-level CVI (S-CVI/Ave) was also calculated by averaging the item CVI values. An S-CVI/Ave value >0.80 is considered acceptable, and a value >0.90 is considered excellent [26]. Modified kappa was also calculated for each item to reduce the probability of chance agreement. This statistic reflects inter-rater agreement and is interpreted as: Excellent (>0.74), good (0.60–0.74), or weak (<0.6) [27].
For assessment of construct validity, the Exploratory Factor Analysis (EFA) was performed. Accordingly, 220 midwives with a work experience of more than two years and a bachelor’s degree or higher were selected from hospitals affiliated to Tehran and Kashan medical universities. The Keyser-Meyer-Olkin (KMO) and the Bartlett’s tests were conducted to test sampling adequacy and factor analysis appropriateness, and the number of factors was determined based on eigenvalues and scree plot. The minimum factor loading value was set at 0.3, and eigenvalues less than one were omitted [28]. Principal Axis Factoring (PAF) with Promax rotation was used in factor analysis. Data normality and outliers were assessed using skewness (±3) and kurtosis (±7) [29].
For the assessment of internal consistency and test-retest reliability, 30 midwives from maternity units completed MCQ-MUS at two time points with an interval of two weeks and their test data were used to calculate Cronbach’s α for internal consistency and their test-retest data were used to calculate Intraclass Correlation Coefficient (ICC) for test/re-test reliability using the two-way mixed model. ICC values more than 0.80 were considered acceptable. Moreover, Standard Error of Measurement (SEM) was calculated as Equation 2:
2. SEM =Sd√1-ICC
where SD was the standard deviation.
Results
In the first phase, based on the results of the theoretical [22] and fieldwork [20] stages of the hybrid concept analysis, definitions and concepts were integrated and, finally, the concept of MCQ in maternity units was defined as “a complex and multidimensional concept which refers to the process of providing care to the parturient during the childbirth process by a morally and scientifically competent midwife based on professional standards and mental/emotional/informational/instrumental support in order to empower the parturient and improve her self-efficacy in maternity unit under appropriate physical conditions and using adequate equipment, which maintains maternal and neonatal health and leads to a positive childbirth experience and is influenced by internal and external motivation, attention to the parturient expectations, physical/psychological preparation of the parturient during pregnancy, and efficient managerial support”. This definition revealed that the four dimensions of the concept encompassed effective interaction, maternal empowerment, professional care, and appropriate human and physical resources. Based on this definition and the results of the hybrid concept analysis, a primary item pool with 150 items was created. Items were compared, revised, and combined. Finally, an initial draft of MCQ-MUS with 88 items was developed.
In assessing face validity, the impact scores of all items were found to be in the range of 2.6-5, i.e. more than the minimum acceptable value of 1.5, and hence, none of the items was omitted. In the qualitative face validity assessment, five items were revised due to poor comprehensibility. In assessing content validity, four items were revised, nine overlapping items were combined, three items were omitted, one new item was added, and the allocation of two items was changed based on experts’ comments. During the quantitative content validity assessment of the 77-item draft, six items with CVR values <0.49 were omitted. The remaining items had acceptable CVI values of 0.88–1. The S-CVI/Ave was 0.94, and the modified kappa value of the items was in the range of 0.72–1.
Participants who were selected for assessment of construct validity were 220 midwives with a mean age of 34.35±8.14 years and a mean work experience of 9.68±7.84 years. Most participants had a bachelor’s degree and rotating work shifts (Table 1).
The KMO value was obtained as 0.922, and the Bartlett’s test was significant (P=0.001), confirming sampling adequacy (Table 2).

The scree plot showed a five-factor structure for MCQ-MUS (Figure 1).
However, different 4– and 8-factor structures were tested through different rotations. Finally, PAF and Promax rotation revealed the four-factor structure as the best structure for MCQ-MUS. The extracted four factors comprised 39 items and accounted for 49.61% of the total variance (Table 3).
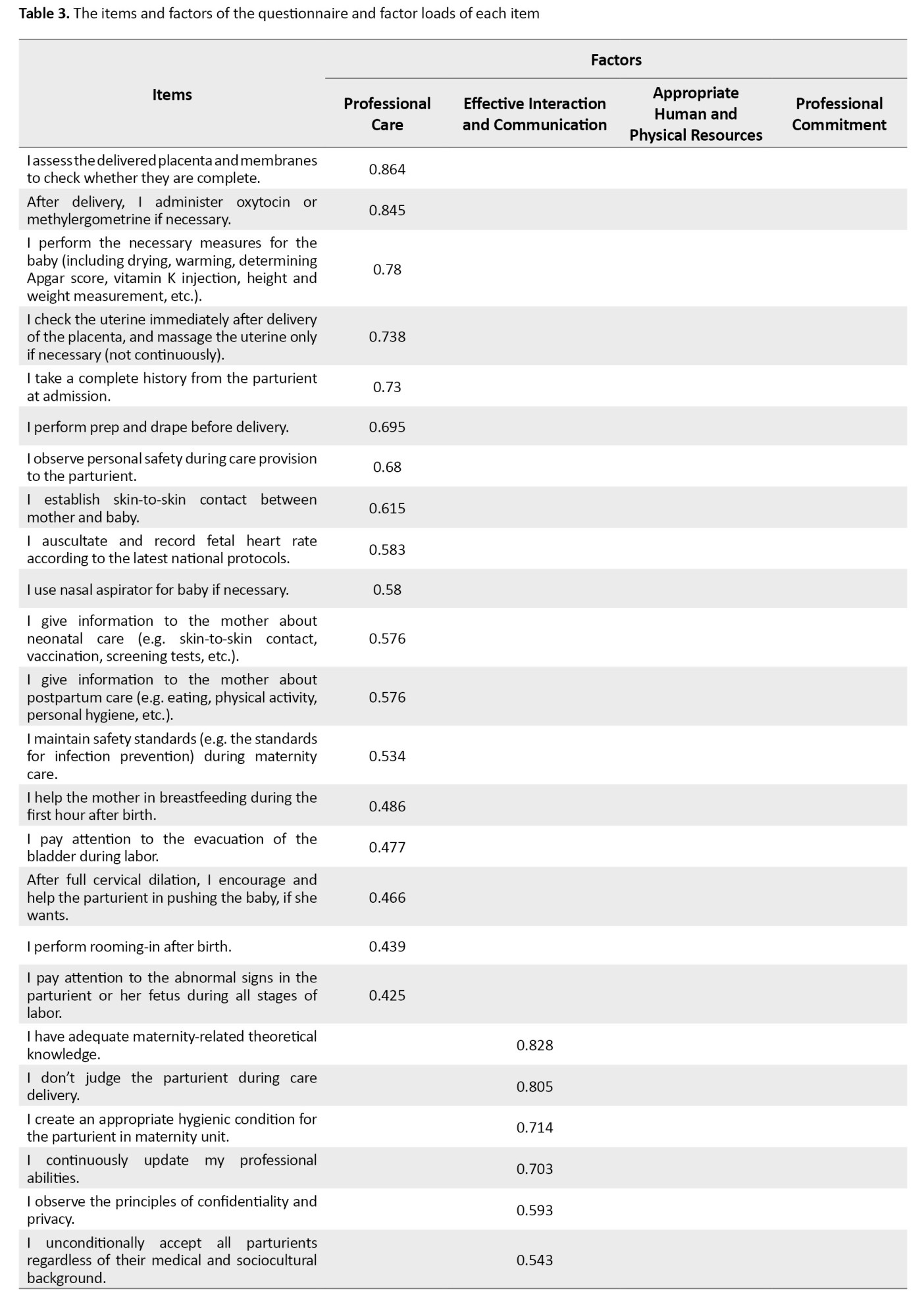
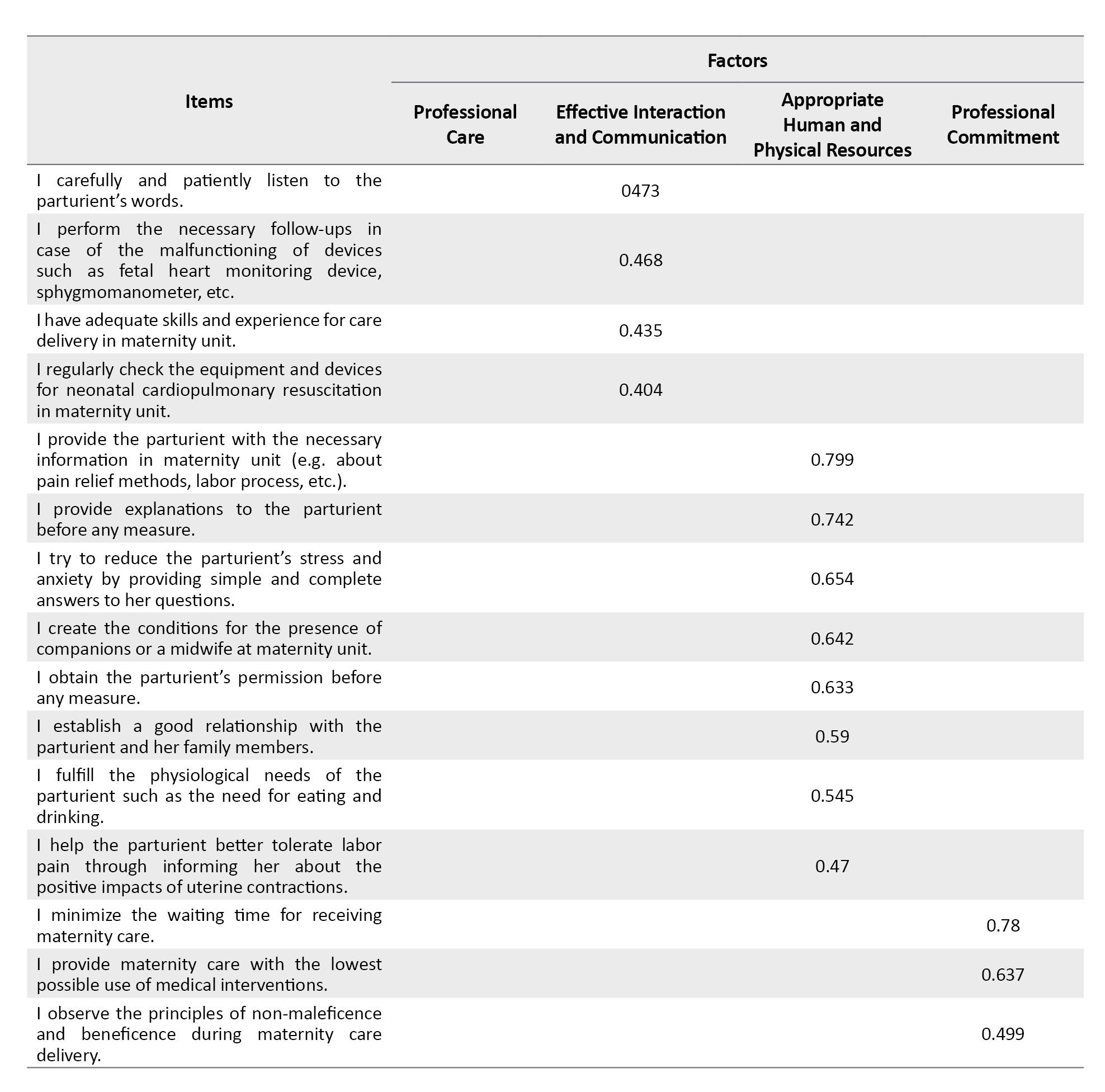
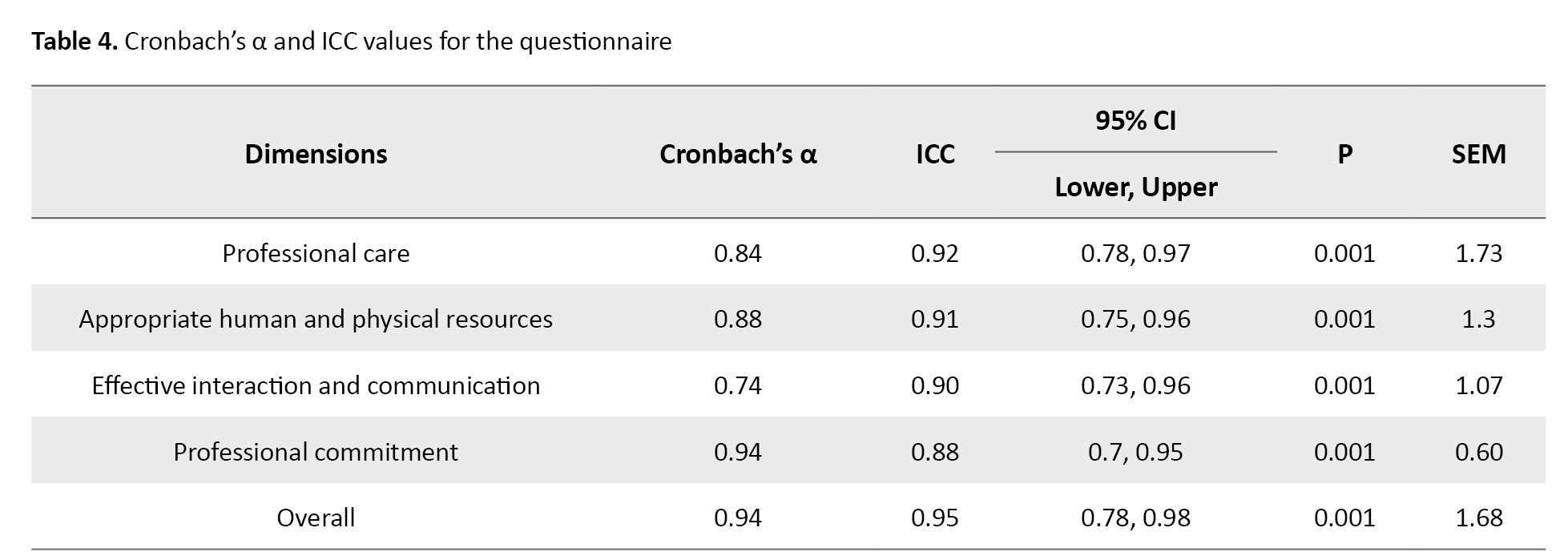
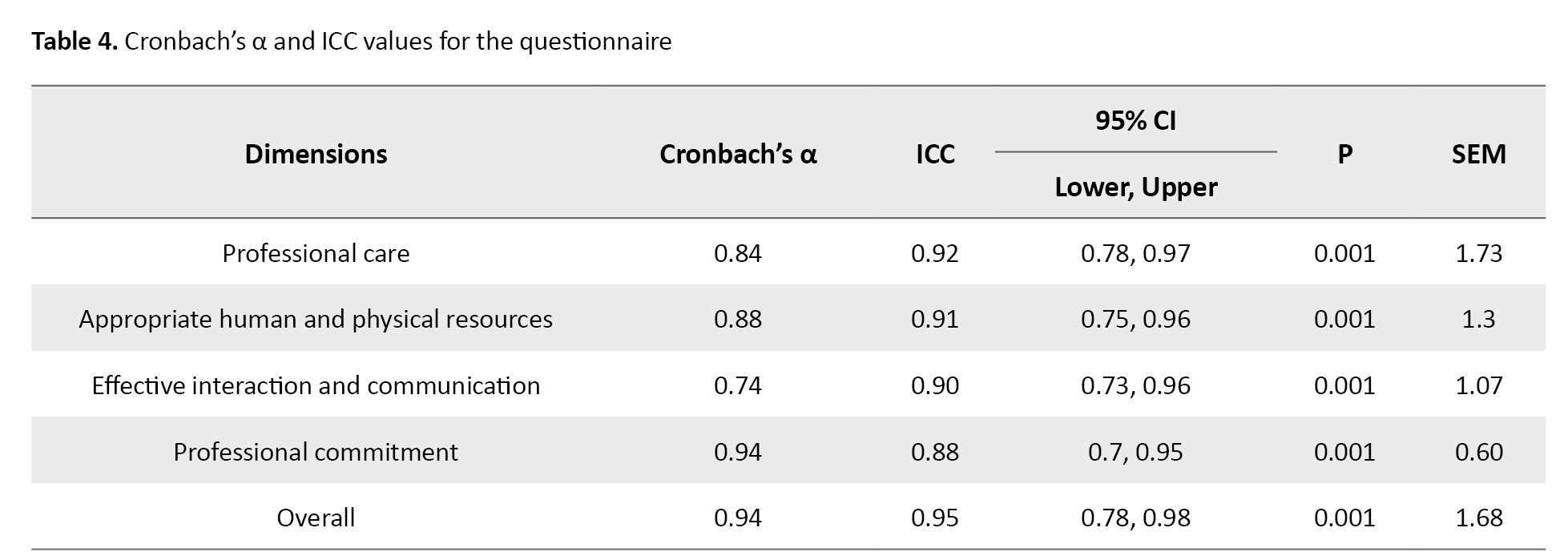
The factors were labeled as professional care (18 items), appropriate human and physical resources (10 items), effective interaction and communication (8 items), and professional commitment (3 items). These factors explained 37.41%, 5.65%, 3.72%, and 2.84% of the variance, respectively. The Cronbach’s α values of the four factors were 0.741–0.940, the ICC of the scale was 0.950 (95% CI; 0.781%, 0.984%), and the SEM of the scale was 1.68 (Table 4).
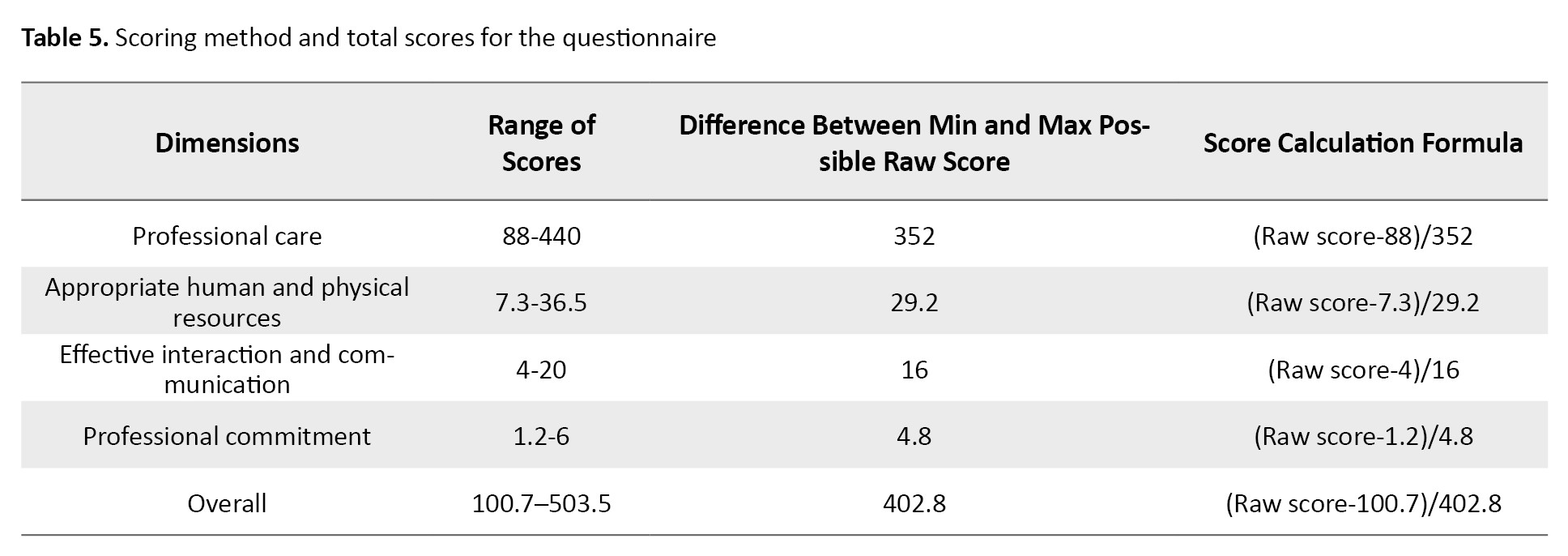
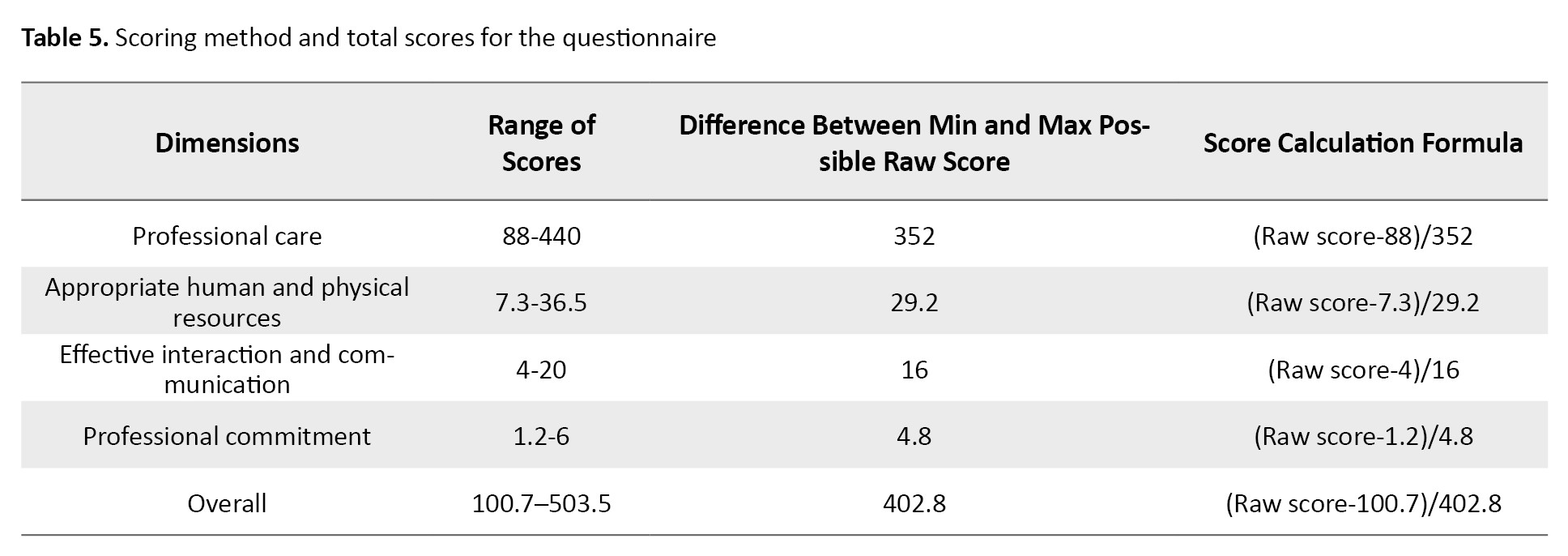
For scoring, the weight of each item was primarily determined using the percent of the variance explained and factor loading values. Then, its raw score in the range of 1–5 was multiplied by its weight. The total score of each factor was determined by summing the scores of all items, and the total score of the scale was determined by summing the scores of all factors. The possible total score of the scale was in the range of 100.7–503.5, with higher scores showing higher MCQ (Table 5).
Discussion
In this study, we developed a scale to measure the MCQ in maternity units named “MCQ-MUS” and evaluated its psychometric properties. It had 39 items and four factors, namely professional care, appropriate human and physical resources, effective interaction and communication, and professional commitment. The main features of this questionnaire are the inclusion of all aspects of MCQ in maternity units and the development based on the experiences of midwives and maternity care experts. Faye et al. developed the GRIOS based on local guidelines and protocols in Senegal and the guidelines of the FIGO and, hence, is not generalizable to Iranian culture [5]. Simbar et al. used an instrument to assess the quality of midwifery care, which included many items related to professional care and clinical measures, although the instrument was developed based on the protocols of the WHO for the management of normal vaginal delivery [10], while the MCQ-MUS was developed through a hybrid concept analysis and has a small number of items. Therefore, it is easy to understand and answer the items, takes less time, and the collected data may be more reliable. Tripathi et al. also developed a measure to assess the quality of facility-based labor and delivery care, which had five main dimensions, namely technical quality, interpersonal care, screening and monitoring, infection prevention/control, and avoidance of harmful/non-indicated practices. However, that instrument was developed based on the opinions of maternal and neonatal care experts in Sub-Saharan Africa; hence, it may not be generalizable to Iranian culture [30].
The first dimension of MCQ-MUS was professional care with 18 items. Professional care includes all care measures necessary for women in maternity units such as diagnosis, treatment, preventive measures, and patient education. MCQ in maternity units should be assessed through assessing the processes of perinatal and postnatal care [2]. Moridi et al. developed the Midwives’ Knowledge and Practice Scale on RMC which had a care dimension measuring the importance of providing evidence-based care and information [11]. The second dimension of MCQ-MUS was appropriate human and physical resources with 10 items. The highest factor loading value in this dimension was related to the item “I have adequate maternity-related theoretical knowledge”, denoting the importance of maternity-related knowledge. In this dimension, the items “I don’t judge the parturient during care delivery”, “I observe the principles of confidentiality and privacy”, and “I unconditionally accept all parturients regardless of their medical and sociocultural background” imply the necessity of adherence to ethical principles. The item “I carefully and patiently listen to parturient’s words” also highlights the importance of communication skills in maternity units. In line with this finding, Butler et al. in a qualitative study, also reported communication skills as a key aspect of professionalism among healthcare providers in maternity units [31]. Sengane reported constant presence of midwife during labor, adequate interpersonal communication skills, and establishment of effective communication with clients as the key aspects of midwifery care [32]. The item “I create an appropriate hygienic condition for the parturient in maternity unit” also had a high factor loading value in the second dimension. Availability of a hygienic environment, observance of the principles of hygiene and cleanliness [33-35], and careful attention to the hygiene of the labor room [36] are among the important components of a good maternity unit. Observance of hygiene and availability of clean bathrooms contributed to maternal satisfaction in western Kenya [37]. Simbar et al. also included items on physical structure, environmental hygiene, and equipment in their instrument for the assessment of midwifery care quality [10]. Shakibazadeh et al. also reported the significant impact of physical environment on care quality in health facilities [7].
The third dimension of MCQ-MUS was effective interaction and communication. Effective communication with the parturient and her family during labor is the cornerstone of quality care delivery. Good and trust-based relationships and continuous effective support during labor and childbirth stop the fear-pain cycle, improve calmness, reduce catecholamine release, relieve pain, and thereby, strengthen uterine contractions, facilitate the progress of physiologic delivery, and minimize labor duration [38]. Studies on the development and psychometric evaluation of RMC instruments also highlighted the importance of midwife-parturient relationships [11, 39-42]. The item “I provide the parturient with the necessary education and information in maternity unit” had highest factor loading. Providing timely education to the parturient facilitates effective communication and interaction between midwife and parturient [43], calms the parturient, and turns childbirth into a positive experience [44]. The scale for women’s perception of RMC developed by Ayoubi et al. also had items related to access to information, maintenance of maternal dignity, informed consent, participatory care, providing comfort, and avoidance of mistreatment [39].
Professional commitment was the last dimension of MCQ-MUS. Professional commitment refers to inner satisfaction with the assigned tasks and close adherence to them without any need for supervision. Professional commitment is a strong belief in professional values and their acceptance that motivates people to promote their profession and maintain professionalism. It includes components such as professional concerns and preoccupations, honesty, loyalty, conscientiousness, beliefs, morality, inner satisfaction, professional development, and professional involvement [45].
One strength of MCQ-MUS is its comprehensiveness and coverage of the two MCQ elements of process and structure. However, its limitation is that it is appropriate for MCQ assessment among women with low-risk pregnancies. Additionally, the number of participants in the psychometric assessment was low, and all of them were from a single city in Iran. Therefore, the development of instruments for MCQ assessment among women with high-risk pregnancies is recommended. Moreover, further studies are recommended to assess the factor structure of MCQ-MUS using confirmatory factor analysis or to evaluate its psychometric properties in other languages. It can be concluded that the 39-item MCQ-MUS with the four dimensions of professional care, appropriate human and physical resources, effective interaction and communication, and professional commitment is a valid and reliable instrument. Therefore, it can be used for MCQ assessment in maternity units.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.FNM.REC.1398.053). Informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Funding
This study was extracted from the PhD dissertation of Fatemeh Abbaszadeh, approved by Tehran University of Medical Sciences and financially supported by Tehran University of Medical Sciences, Tehran, Iran (Grant No.: 9611151005).
Authors' contributions
Study design and recruitment of samples: Maryam Damghanian, Fatemeh Abbaszadeh and Zohreh Khakbazan; Conceptualization, resources, original draft preparation: Maryam Damghanian and Fatemeh Abbaszadeh; Critical revision: Zohreh Khakbazan; Methodology and data analysis: Armin Zareiyan; Data interpretation: Molouk Jaafarpour, Mahboobeh Rasoulzadeh Bidgoli, and Fatemeh Abbaszadeh; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Vice-Chancellor for Research of Tehran University of Medical Sciences, Tehran, Iran, for funding this project, and all participants for their cooperation in this study.
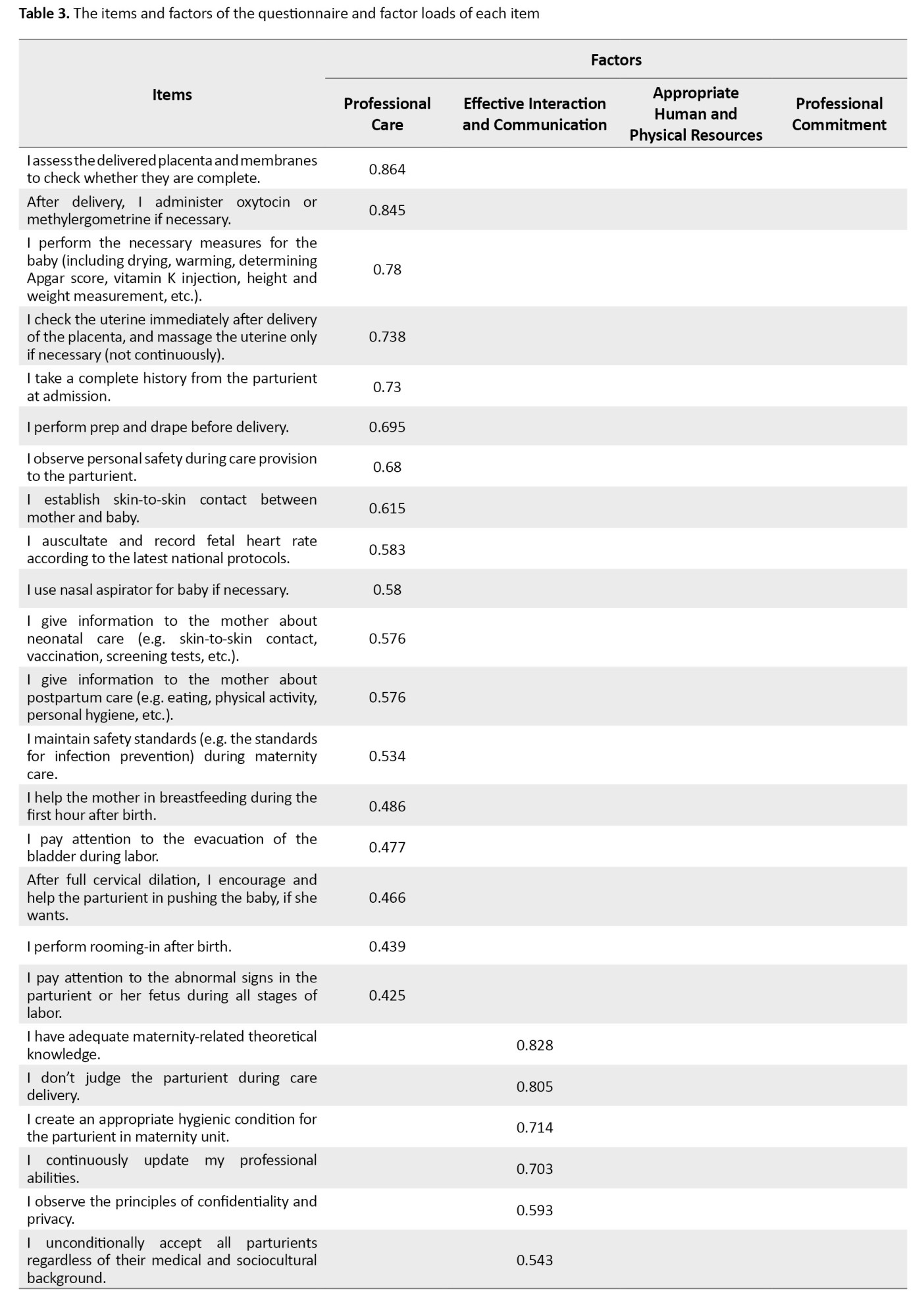
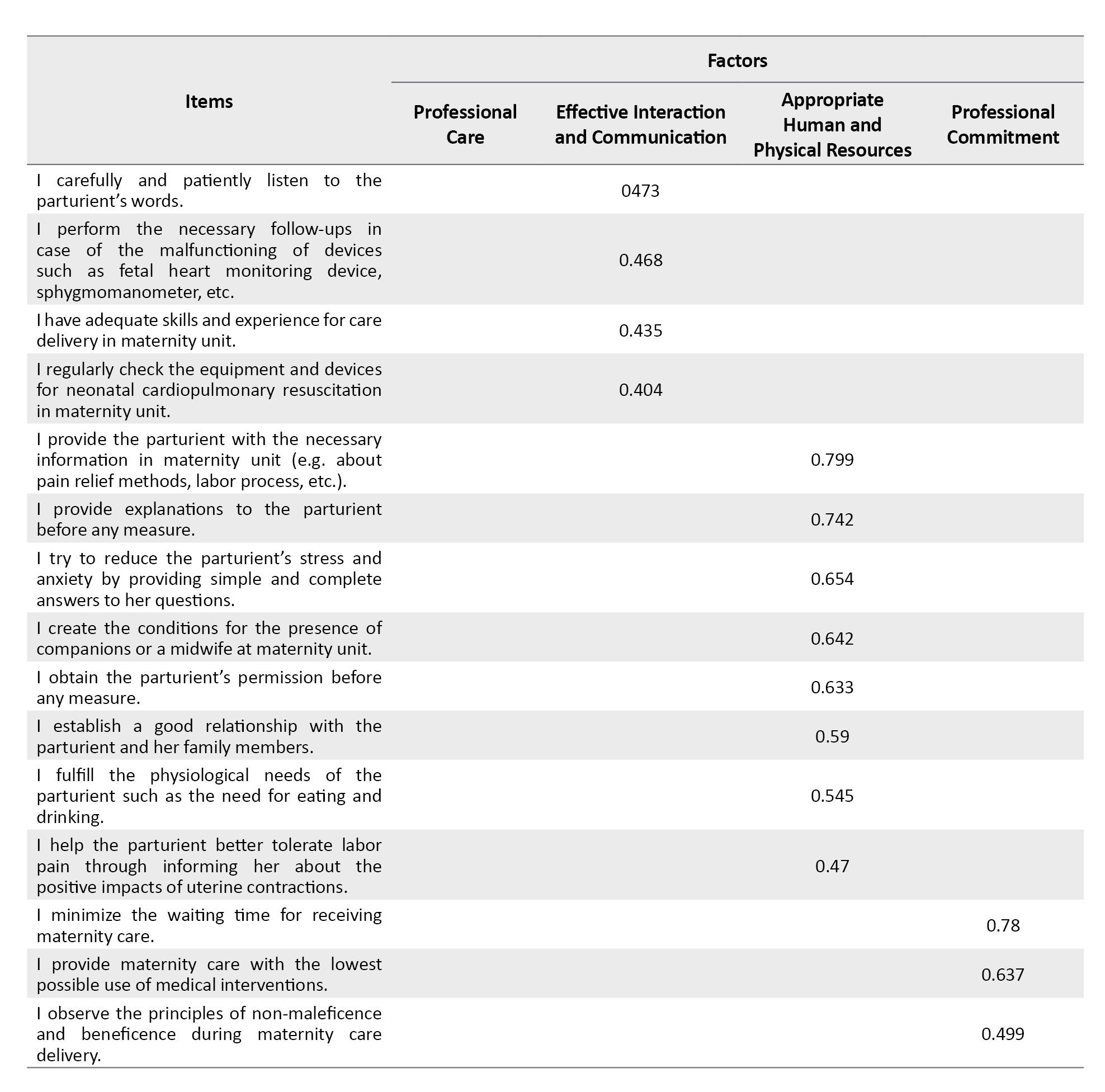
The factors were labeled as professional care (18 items), appropriate human and physical resources (10 items), effective interaction and communication (8 items), and professional commitment (3 items). These factors explained 37.41%, 5.65%, 3.72%, and 2.84% of the variance, respectively. The Cronbach’s α values of the four factors were 0.741–0.940, the ICC of the scale was 0.950 (95% CI; 0.781%, 0.984%), and the SEM of the scale was 1.68 (Table 4).
For scoring, the weight of each item was primarily determined using the percent of the variance explained and factor loading values. Then, its raw score in the range of 1–5 was multiplied by its weight. The total score of each factor was determined by summing the scores of all items, and the total score of the scale was determined by summing the scores of all factors. The possible total score of the scale was in the range of 100.7–503.5, with higher scores showing higher MCQ (Table 5).
Discussion
In this study, we developed a scale to measure the MCQ in maternity units named “MCQ-MUS” and evaluated its psychometric properties. It had 39 items and four factors, namely professional care, appropriate human and physical resources, effective interaction and communication, and professional commitment. The main features of this questionnaire are the inclusion of all aspects of MCQ in maternity units and the development based on the experiences of midwives and maternity care experts. Faye et al. developed the GRIOS based on local guidelines and protocols in Senegal and the guidelines of the FIGO and, hence, is not generalizable to Iranian culture [5]. Simbar et al. used an instrument to assess the quality of midwifery care, which included many items related to professional care and clinical measures, although the instrument was developed based on the protocols of the WHO for the management of normal vaginal delivery [10], while the MCQ-MUS was developed through a hybrid concept analysis and has a small number of items. Therefore, it is easy to understand and answer the items, takes less time, and the collected data may be more reliable. Tripathi et al. also developed a measure to assess the quality of facility-based labor and delivery care, which had five main dimensions, namely technical quality, interpersonal care, screening and monitoring, infection prevention/control, and avoidance of harmful/non-indicated practices. However, that instrument was developed based on the opinions of maternal and neonatal care experts in Sub-Saharan Africa; hence, it may not be generalizable to Iranian culture [30].
The first dimension of MCQ-MUS was professional care with 18 items. Professional care includes all care measures necessary for women in maternity units such as diagnosis, treatment, preventive measures, and patient education. MCQ in maternity units should be assessed through assessing the processes of perinatal and postnatal care [2]. Moridi et al. developed the Midwives’ Knowledge and Practice Scale on RMC which had a care dimension measuring the importance of providing evidence-based care and information [11]. The second dimension of MCQ-MUS was appropriate human and physical resources with 10 items. The highest factor loading value in this dimension was related to the item “I have adequate maternity-related theoretical knowledge”, denoting the importance of maternity-related knowledge. In this dimension, the items “I don’t judge the parturient during care delivery”, “I observe the principles of confidentiality and privacy”, and “I unconditionally accept all parturients regardless of their medical and sociocultural background” imply the necessity of adherence to ethical principles. The item “I carefully and patiently listen to parturient’s words” also highlights the importance of communication skills in maternity units. In line with this finding, Butler et al. in a qualitative study, also reported communication skills as a key aspect of professionalism among healthcare providers in maternity units [31]. Sengane reported constant presence of midwife during labor, adequate interpersonal communication skills, and establishment of effective communication with clients as the key aspects of midwifery care [32]. The item “I create an appropriate hygienic condition for the parturient in maternity unit” also had a high factor loading value in the second dimension. Availability of a hygienic environment, observance of the principles of hygiene and cleanliness [33-35], and careful attention to the hygiene of the labor room [36] are among the important components of a good maternity unit. Observance of hygiene and availability of clean bathrooms contributed to maternal satisfaction in western Kenya [37]. Simbar et al. also included items on physical structure, environmental hygiene, and equipment in their instrument for the assessment of midwifery care quality [10]. Shakibazadeh et al. also reported the significant impact of physical environment on care quality in health facilities [7].
The third dimension of MCQ-MUS was effective interaction and communication. Effective communication with the parturient and her family during labor is the cornerstone of quality care delivery. Good and trust-based relationships and continuous effective support during labor and childbirth stop the fear-pain cycle, improve calmness, reduce catecholamine release, relieve pain, and thereby, strengthen uterine contractions, facilitate the progress of physiologic delivery, and minimize labor duration [38]. Studies on the development and psychometric evaluation of RMC instruments also highlighted the importance of midwife-parturient relationships [11, 39-42]. The item “I provide the parturient with the necessary education and information in maternity unit” had highest factor loading. Providing timely education to the parturient facilitates effective communication and interaction between midwife and parturient [43], calms the parturient, and turns childbirth into a positive experience [44]. The scale for women’s perception of RMC developed by Ayoubi et al. also had items related to access to information, maintenance of maternal dignity, informed consent, participatory care, providing comfort, and avoidance of mistreatment [39].
Professional commitment was the last dimension of MCQ-MUS. Professional commitment refers to inner satisfaction with the assigned tasks and close adherence to them without any need for supervision. Professional commitment is a strong belief in professional values and their acceptance that motivates people to promote their profession and maintain professionalism. It includes components such as professional concerns and preoccupations, honesty, loyalty, conscientiousness, beliefs, morality, inner satisfaction, professional development, and professional involvement [45].
One strength of MCQ-MUS is its comprehensiveness and coverage of the two MCQ elements of process and structure. However, its limitation is that it is appropriate for MCQ assessment among women with low-risk pregnancies. Additionally, the number of participants in the psychometric assessment was low, and all of them were from a single city in Iran. Therefore, the development of instruments for MCQ assessment among women with high-risk pregnancies is recommended. Moreover, further studies are recommended to assess the factor structure of MCQ-MUS using confirmatory factor analysis or to evaluate its psychometric properties in other languages. It can be concluded that the 39-item MCQ-MUS with the four dimensions of professional care, appropriate human and physical resources, effective interaction and communication, and professional commitment is a valid and reliable instrument. Therefore, it can be used for MCQ assessment in maternity units.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.FNM.REC.1398.053). Informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Funding
This study was extracted from the PhD dissertation of Fatemeh Abbaszadeh, approved by Tehran University of Medical Sciences and financially supported by Tehran University of Medical Sciences, Tehran, Iran (Grant No.: 9611151005).
Authors' contributions
Study design and recruitment of samples: Maryam Damghanian, Fatemeh Abbaszadeh and Zohreh Khakbazan; Conceptualization, resources, original draft preparation: Maryam Damghanian and Fatemeh Abbaszadeh; Critical revision: Zohreh Khakbazan; Methodology and data analysis: Armin Zareiyan; Data interpretation: Molouk Jaafarpour, Mahboobeh Rasoulzadeh Bidgoli, and Fatemeh Abbaszadeh; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Vice-Chancellor for Research of Tehran University of Medical Sciences, Tehran, Iran, for funding this project, and all participants for their cooperation in this study.
References
- Caroselli M. Quality care: Prescription for injecting quality into healthcare systems. Boca Raton: CRC Press; 1997. [Link]
- Donabedian A. The quality of care. How can it be assessed? JAMA. 1988; 260(12):1743-8. [DOI:10.1001/jama.260.12.1743] [PMID]
- United Nations. Transforming our world: The 2030 agenda for sustainable development [Internet]. 2015 [Updated 25 September 2015]. Available from: [Link]
- United Nations. What are sustainable development goals. New York: United Nations; 2015. [Link]
- Faye A, Dumont A, Ndiaye P, Fournier P. Development of an instrument to evaluate intrapartum care quality in Senegal: Evaluation quality care. Int J Qual Health Care. 2014; 26(2):184-9. [DOI:10.1093/intqhc/mzu018] [PMID]
- Bohren MA, Titiloye MA, Kyaddondo D, Hunter EC, Oladapo OT, Tunçalp Ö, et al. Defining quality of care during childbirth from the perspectives of Nigerian and Ugandan women: A qualitative study. Int J Gynaecol Obstet. 2017; 139(Suppl 1):4-16. [DOI:0.1002/ijgo.12378] [PMID]
- Shakibazadeh E, Namadian M, Bohren MA, Vogel JP, Rashidian A, Nogueira Pileggi V, et al. Respectful care during childbirth in health facilities globally: A qualitative evidence synthesis. BJOG. 2018; 125(8):932-42. [DOI:10.1111/1471-0528.15015] [PMID]
- Boesveld IC, Hermus MAA, de Graaf HJ, Hitzert M, van der Pal-de Bruin KM, de Vries RG, et al. Developing quality indicators for assessing quality of birth centre care: A mixed- methods study. BMC Pregnancy Childbirth. 2017; 17(1):259. [DOI:10.1186/s12884-017-1439-9] [PMID]
- Araban M, Karimy M, Tavousi M, Shamsi M, Niakan Kalhori S, Khazaiyan S, et al. Quality of midwifery care provided to women admitted for delivery in selected hospitals of Yazd. Adv Nurs Midwifery. 2013; 23(81):19-26. [DOI:10.22037/anm.v23i81.5893]
- Simbar M, Ghafari F, Zahrani ST, Majd HA. Assessment of quality of midwifery care in labour and delivery wards of selected Kordestan Medical Science University hospitals. Int J Health Care Qual Assur. 2009; 22(3):266-77. [DOI:10.1108/09526860910953539] [PMID]
- Moridi M, Pazandeh F, Hajian S, Potrata B. Development and psychometric properties of midwives' knowledge and practice scale on respectful maternity care (MKP-RMC). Plos One. 2020; 15(11):e0241219. [DOI:10.1371/journal.pone.0241219] [PMID]
- Attarha M, Keshavarz Z, Bakhtiari M, Jamilian M, Zayeri F. Development and psychometric tests of midwife-mother relationship scale (MMRS) in delivery room. Glob J Health Sci. 2017; 9(2):184. [DOI:10.5539/gjhs.v9n2p184]
- van der Goes DN, Edwardson N, Rayamajhee V, Hollis C, Hunter D. An iron triangle ROI model for health care. Clinicoecon Outcomes Res. 2019; 11:335-48. [DOI:10.2147/CEOR.S130623] [PMID]
- WHO. Standards for improving quality of maternal and newborn care in health facilities [Internet]. 2016 [Updated 4 July 2016]. Available from: [Link]
- WHO. Quality of care [Internet]. 2020 [Updated 2025 September 27]. Available from: [Link]
- Smith S, Mِrelius E. Principle-based concept analysis methodology using a phased approach with quality criteria. International Journal of Qualitative Methods. 2021; 20. [DOI:10.1177/160940692110579]
- Rafii F, Sajadi Hezaveh M, Seyed Fatemi N, Rezaei M. [Concept analysis of social support of new graduate nurses in the workplace: a hybrid model (Persian)]. Iran J Nurs. 2014; 26(86):71-89. [Link]
- Whittemore R, Knafl K. The integrative review: Updated methodology. J Adv Nurs. 2005; 52(5):546-53. [DOI:10.1111/j.1365-2648.2005.03621.x] [PMID]
- Ganong LH. Integrative reviews of nursing research. Res Nurs Health. 1987; 10(1):1-11. [DOI:10.1002/nur.4770100103] [PMID]
- Khakbazan Z, Damghanian M, Zareiyan A, Abbaszadeh F. Explaining the concept and dimensions of midwifery care quality in maternity ward: A Qualitative Study. J Complement Med Res. 2020;11(4):247-54. [DOI:10.5455/jcmr.2020.11.04.32]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004; 24(2):105-12. [DOI:10.1016/j.nedt.2003.10.001] [PMID]
- Khakbazan Z, Damghanian M, Zareiyan A, Abbaszadeh F. The concept of maternal care quality for women with low-risk pregnancy in the maternity ward: An integrative review. Nurs Midwifery Stud. 2022; 11(1):1-10. [DOI:.4103/nms.nms_2_21]
- Polit D, Beck CT. Nursing research-principles and methods, Chapter 17. Philadelphia: Lippincott Williams & Wilkins; 1999. [Link]
- Polit-O’Hara D, Yang FM. Measurement and the measurement of change: A primer for the health professions. Alphen aan den Rijn: Wolters Kluwer; 2016. [Link]
- Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007; 30(4):459-67. [DOI:10.1002/nur.20199] [PMID]
- Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006; 29(5):489-97. [DOI:10.1002/nur.20147] [PMID]
- Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. Philadelphia: Lippincott Williams & Wilkins; 2008. [Link]
- Friedberg MW, Landon M. Measuring quality in hospitals in the United States [Internet]. 2018 [Updated 2024 April 10]. Available from: [Link]
- Esposito Vinzi V, Chin WW, Henseler J, Wang H. Handbook of partial least squares: Concepts, methods and applications. New York: Springer; 2010. [DOI:10.1007/978-3-540-32827-8]
- Tripathi V, Stanton C, Strobino D, Bartlett L. Development and validation of an index to measure the quality of facility-based labor and delivery care processes in Sub-Saharan Africa. Plos One. 2015; 10(6):e0129491. [DOI:10.1371/journal.pone.0129491] [PMID]
- Butler MM, Fraser DM, Murphy RJ. What are the essential competencies required of a midwife at the point of registration? Midwifery. 2008; 24(3):260-9. [DOI:10.1016/j.midw.2006.10.010] [PMID]
- Sengane M. Mothers’ expectations of midwives’ care during labour in a public hospital in Gauteng. Curationis. 2013;36(1):E1-9. [DOI:10.4102/curationis.v36i1.320] [PMID]
- Afaya A, Yakong VN, Afaya RA, Salia SM, Adatara P, Kuug AK, et al. A Qualitative study on women's experiences of intrapartum nursing care at tamale teaching hospital (TTH), Ghana. J Caring Sci. 2017; 6(4):303-14. [DOI:10.15171/jcs.2017.029] [PMID]
- Kyaddondo D, Mugerwa K, Byamugisha J, Oladapo OT, Bohren MA. Expectations and needs of Ugandan women for improved quality of childbirth care in health facilities: A qualitative study. Int J Gynaecol Obstet. 2017; 139(Suppl 1):38-46. [DOI:10.1002/ijgo.12405] [PMID]
- Srivastava A, Avan BI, Rajbangshi P, Bhattacharyya S. Determinants of women's satisfaction with maternal health care: A review of literature from developing countries. BMC Pregnancy Childbirth. 2015; 15:97. [DOI:10.1186/s12884-015-0525-0] [PMID]
- Ndirima Z, Neuhann F, Beiersmann C. Listening to their voices: Understanding rural women's perceptions of good delivery care at the Mibilizi District Hospital in Rwanda. BMC Womens Health. 2018; 18(1):38. [DOI:10.1186/s12905-018-0530-3] [PMID]
- Afulani PA, Kirumbi L, Lyndon A. What makes or mars the facility-based childbirth experience: Thematic analysis of women's childbirth experiences in western Kenya. Reprod Health. 2017; 14(1):180. [DOI:10.1186/s12978-017-0446-7] [PMID]
- Dahlberg U, Aune I. The woman's birth experience---the effect of interpersonal relationships and continuity of care. Midwifery. 2013; 29(4):407-15. [DOI:10.1016/j.midw.2012.09.006] [PMID]
- Ayoubi S, Pazandeh F, Simbar M, Moridi M, Zare E, Potrata B. A questionnaire to assess women's perception of respectful maternity care (WP-RMC): Development and psychometric properties. Midwifery. 2020; 80:102573. [DOI:10.1016/j.midw.2019] [PMID]
- Sheferaw ED, Bazant E, Gibson H, Fenta HB, Ayalew F, Belay TB, et al. Respectful maternity care in Ethiopian public health facilities. Reprod Health. 2017; 14(1):60. [DOI:10.1186/s12978-017-0323-4] [PMID]
- Sheferaw ED, Mengesha TZ, Wase SB. Development of a tool to measure women's perception of respectful maternity care in public health facilities. BMC Pregnancy Childbirth. 2016; 16:67. [DOI:10.1186/s12884-016-0848-5] [PMID]
- Taavoni S, Goldani Z, Rostami Gooran N, Haghani H. Development and assessment of respectful maternity care questionnaire in Iran. Int J Community Based Nurs Midwifery. 2018; 6(4):334-49. [Link]
- Mohale H, Sweet L, Graham K. Maternity health care: The experiences of Sub-Saharan African women in Sub-Saharan Africa and Australia. Women Birth. 2017; 30(4):298-307. [DOI:10.1016/j.wombi.2016.11.011] [PMID]
- Dahlberg U, Persen J, Skogås AK, Selboe ST, Torvik HM, Aune I. How can midwives promote a normal birth and a positive birth experience? The experience of first-time Norwegian mothers. Sex Reprod Healthc. 2016; 7:2-7. [DOI:10.1016/j.srhc.2015.08.001] [PMID]
- Lin CJ, Wang HC, Li TC, Huang LC. Reliability and validity of nurses’ job satisfaction scale and nurses’ professional commitment. Mid-Taiwan J Med. 2007; 12(2):65-75. [Link]
Article Type : Research |
Subject:
Special
Received: 2024/03/2 | Accepted: 2025/08/5 | Published: 2025/09/8
Received: 2024/03/2 | Accepted: 2025/08/5 | Published: 2025/09/8
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |