Sun, Apr 28, 2024
Volume 34, Issue 2 (2-2024)
JHNM 2024, 34(2): 177-188 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Raadabadi M, Khajehminian M R, Nikfard M, Eider M. Factors Affecting the Intention of Healthcare Providers in Responding to Disasters: A Systematic Literature Review. JHNM 2024; 34 (2) :177-188
URL: http://hnmj.gums.ac.ir/article-1-2312-en.html
URL: http://hnmj.gums.ac.ir/article-1-2312-en.html
1- Assistant Professor, Department of Health Services Management, Health Policy and Management Research Center, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Assistant Professor, Department of Health in Disaster and Emergencies, Accident Prevention and Crisis Research Center, School of Public Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran. , khajehaminian@gmail.com
3- PhD Candidate, Department of Health in Disaster and Emergencies, School of Public Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
4- MD, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
2- Assistant Professor, Department of Health in Disaster and Emergencies, Accident Prevention and Crisis Research Center, School of Public Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran. , khajehaminian@gmail.com
3- PhD Candidate, Department of Health in Disaster and Emergencies, School of Public Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
4- MD, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
Keywords: Healthcare provider, Healthcare workers, Healthcare professionals, Human resources, Disasters
Full-Text [PDF 684 kb]
(64 Downloads)
| Abstract (HTML) (191 Views)
Full-Text: (44 Views)
Introduction
According to the United Nations Office for Disaster Risk Reduction (UNDRR), disaster is “ a serious disruption of the functioning of a society leading to widespread human, material, economic, and environmental losses that exceed the capacity of a community to cope using its resources” [1]. Disasters challenge the ability of health systems to meet the needs of society. Damage to infrastructure, staff shortages at all levels, and an increasing need for health services will jeopardize the functioning of health systems [2, 3]. Therefore, healthcare providers (HCPs) must be prepared to manage a surge in the number of patients should a disaster occur [4, 5]. Some disasters may be followed by a lack of workforce and loss of equipment and supplies [6, 7, 8, 9]. In a disaster, HCPs are expected to provide care and treatment for the casualties and the nonemergency patients while concerned about their families [4].
Most people believe that HCPs, firefighters, and relief workers in general who participate in relief operations tend to work in any disaster. In contrast, these people are not always willing to work. Indeed, their intention to work in disaster relief operations is highly dependent on the type of disaster [10, 11]. Evidence also shows that the intention to work varies between 25% and 80% among HCPs in public health emergencies. Factors associated with the nurses’ intention to work in disasters included insufficient knowledge and skills, fear of contracting infectious diseases, overworking, sense of responsibility, perceived self-efficacy, financial compensation, age, gender, knowledge and attitude, and academic degree [12-16].
As an effective measure in the preparedness phase of disaster risk management, identifying the factors related to the intention to participate in disaster relief operations will lead to planning better and coping with such situations. This study used a systematic literature review approach to find the factors affecting the intention of HCPs to work in disaster response.
Materials and Methods
The protocol of this study is registered in PROSPERO (CRD42021234620). To obtain relevant studies from the databases, all original articles examining the intention of HCPs to participate in disaster response operations were enrolled in the study. There were no restrictions on the language of the publications. It is noteworthy that articles on the intention of other relief workers, such as firefighters, to participate in disasters, as well as those in the form of letters to the editor, literature review, short study or brief communication, and conference papers, were excluded.
Scopus, PubMed, and Web of Science (WoS) databases were searched to obtain relevant studies published between 1950 and November 1, 2020. To develop the search strategy, several relevant studies on the intention of HCPs to work in disasters were reviewed to extract the keywords. Regarding the frequent use of”human resource,” all entry terms for this keyword were collected using the MeSH feature. Words were combined using the Boolean search method: AND and the OR operators.
All the retrieved documents using the above syntaxes were imported into EndNote, and duplicates were removed. The articles were screened for titles and abstracts, and the relevant items were selected. Next, the full-text articles were assessed by two authors for eligibility criteria. Any disagreement between the two authors was resolved through group discussion and consensus. In case of disagreement after the group discussion, advice and the opinion of a third party were considered. The references of the included articles were also examined to find possible related articles. Using the Scopus database, key journals in the area of the research title were also reviewed.
After the search was completed, data extraction was provided, and they were imported into Microsoft Excel, version 2010. Each extracted factor affecting the intention of HCPs was entered into Excel, and then the concatenate function was connected to the related article code. All extracted factors were then categorized by thematic analysis, i.e. first, all the affecting factors were listed and then classified into categories and subcategories through a group discussion attended by the research authors and using the data validation feature in Excel. The same factors mentioned in different studies were merged, and a common label was chosen for similar factors. Any uncertainty over labeling and categorizing the factors was discussed with the review team.
Results
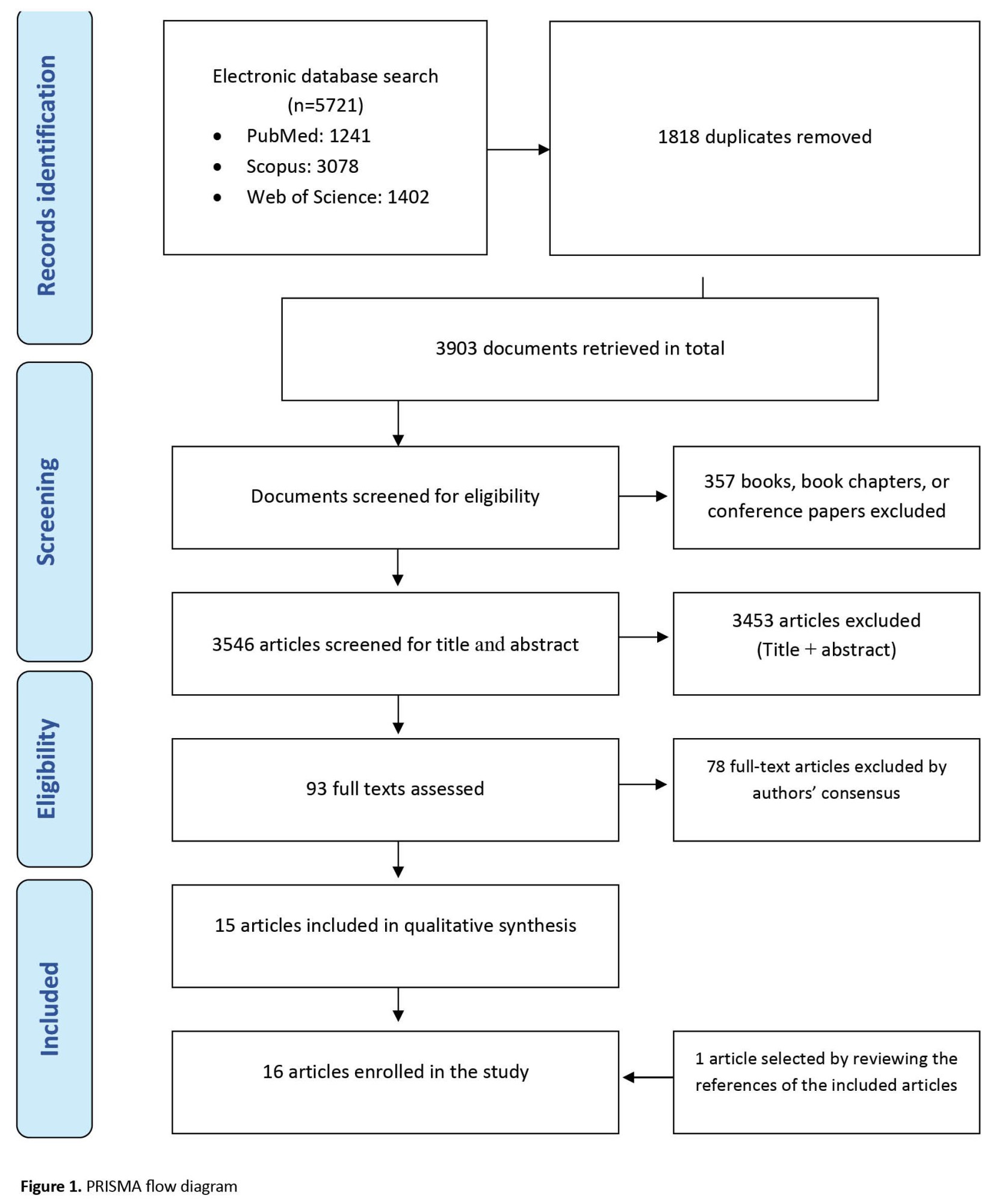
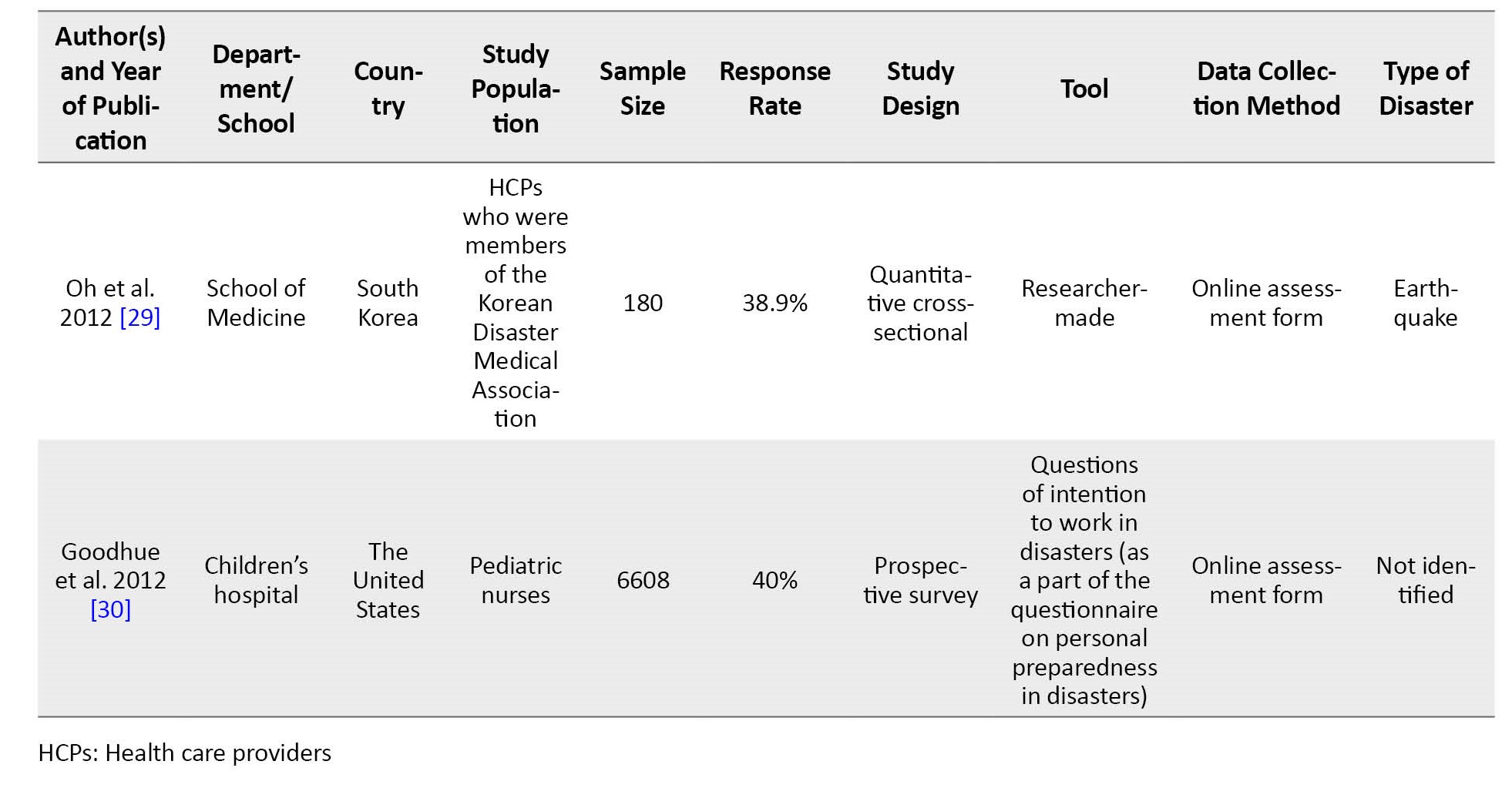
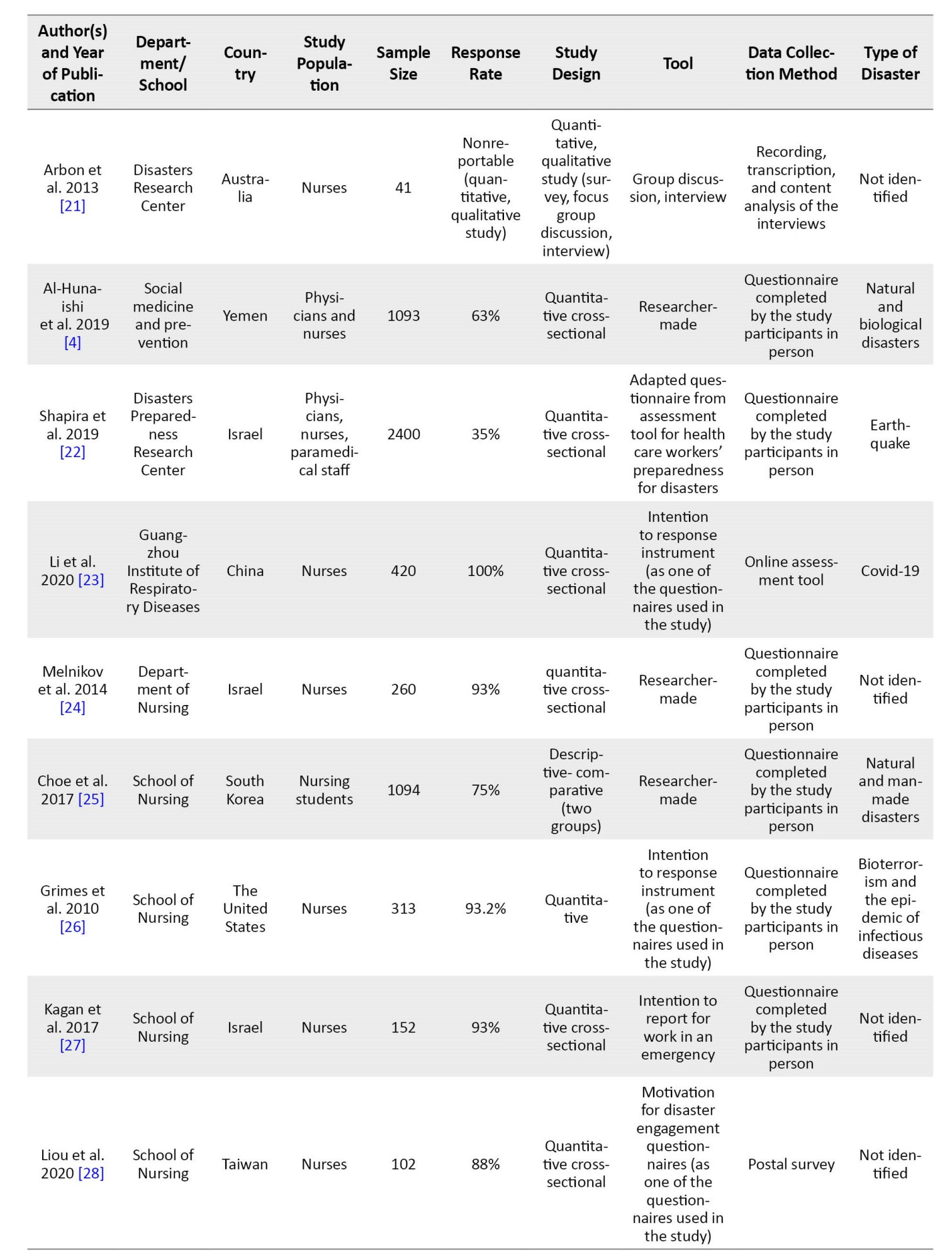
An initial search in Scopus, PubMed, and Web of Science databases yielded 5721 documents, of which 1818 duplicates were removed after being imported into EndNote, version 9 (Figure 1). The 16 enrolled studies in the systematic review were conducted between 2009 and 2020 in Australia (2), South Korea (3), the United States (4), Israel (3), Yemen (1), China (1), Taiwan (1), and Brazil (1). There was one mixed methods study, and the other 15 were performed using quantitative methods. In total, 13 studies specifically examined the intention of nurses to work in disasters, of which one investigated only nursing students and 3 surveyed a combination of nurses, physicians, physicians and or nurses, and emergency medical technicians (Table 1).
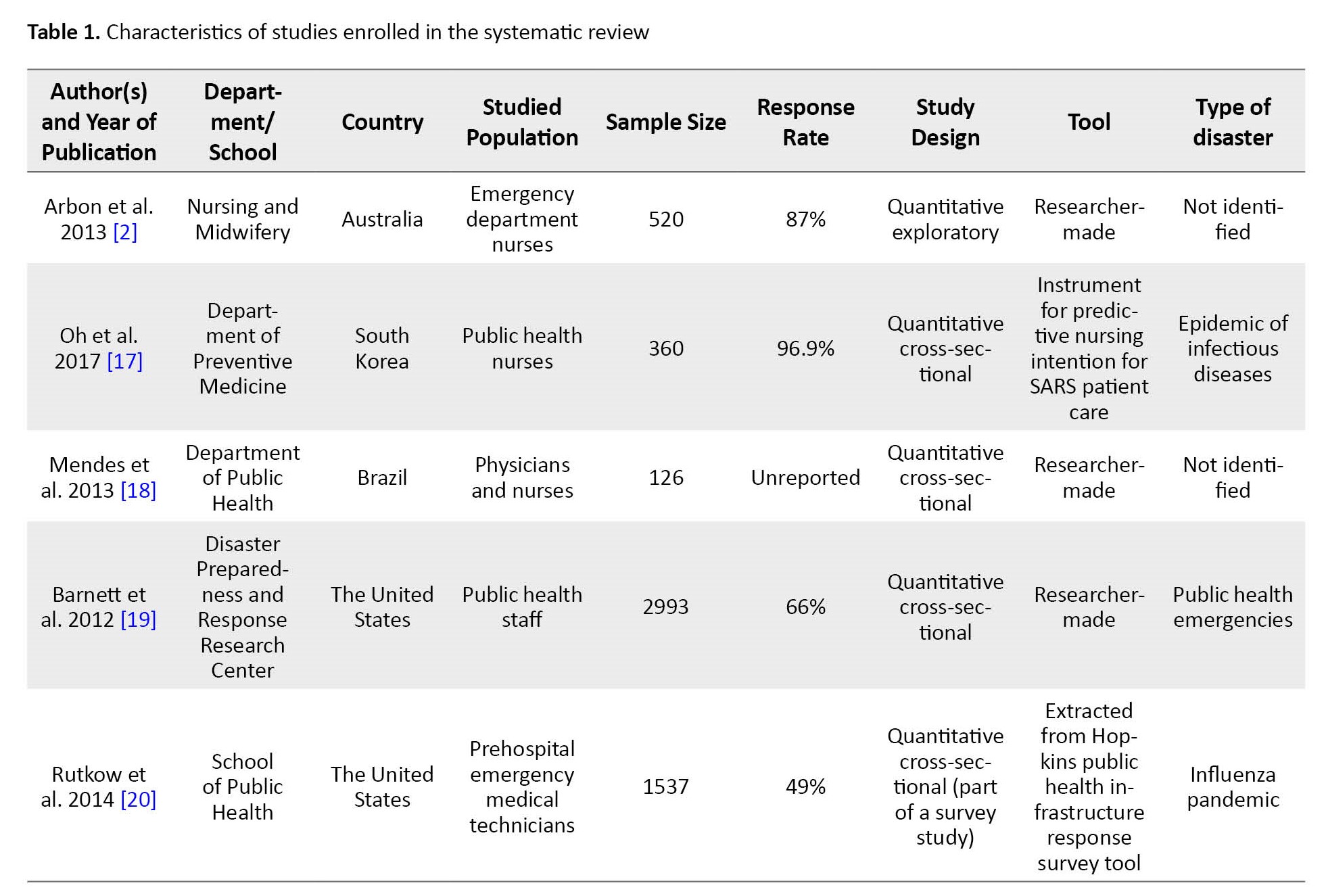
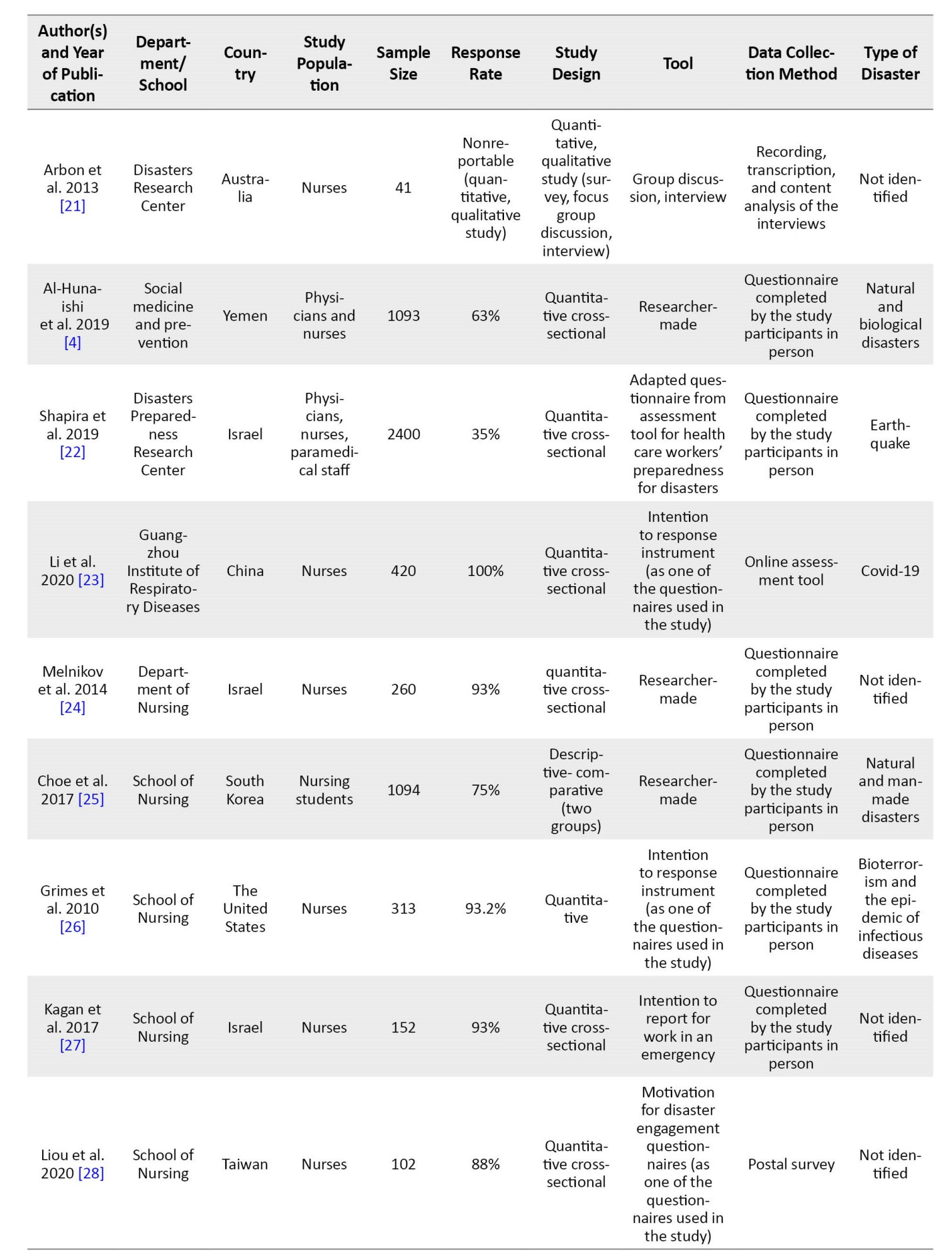
Regarding data collection tools, four studies used specific tools to assess the intention of HCPs in disasters, and the remaining 11 employed researcher-made tools based on the review of previous studies or modification of other non-specific questionnaires of staff intention to work. Only one study approached the issue in a qualitative design using interviews and focus group discussions.
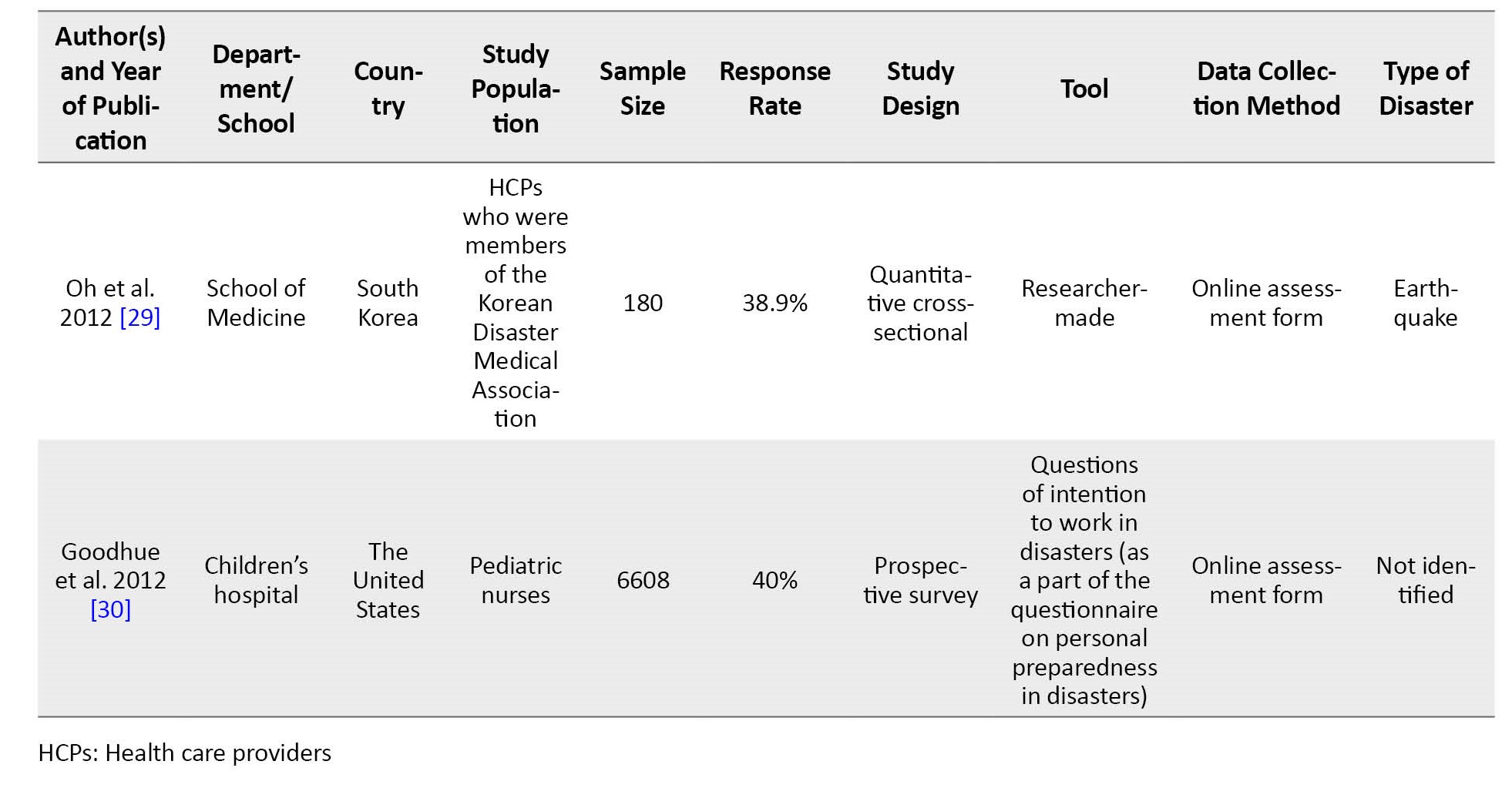
As explained in the study methods, using the concatenate function in Excel, every factor affecting the intention of HCPs was imported into Excel and then connected to the study with the related article code. Next, all extracted factors were categorized by thematic analysis. First, all the affecting factors were listed and then classified through a group discussion attended by the research authors and using the data validation feature in Excel into the following categories and subcategories: Organizational factors (supply management, risk management, organizational environment, organizational climate, managerial support, financial incentives), personal factors (demographic, familial, beliefs and values, health status of HCP, individual experiences, knowledge and education, occupational, self-efficacy), and nature of the disaster (type of disaster, prevention, and treatment). The same factors mentioned in different studies were merged, and a common label was chosen for similar factors. The review team discussed any uncertainty over labeling and categorizing the factors (Table 2).
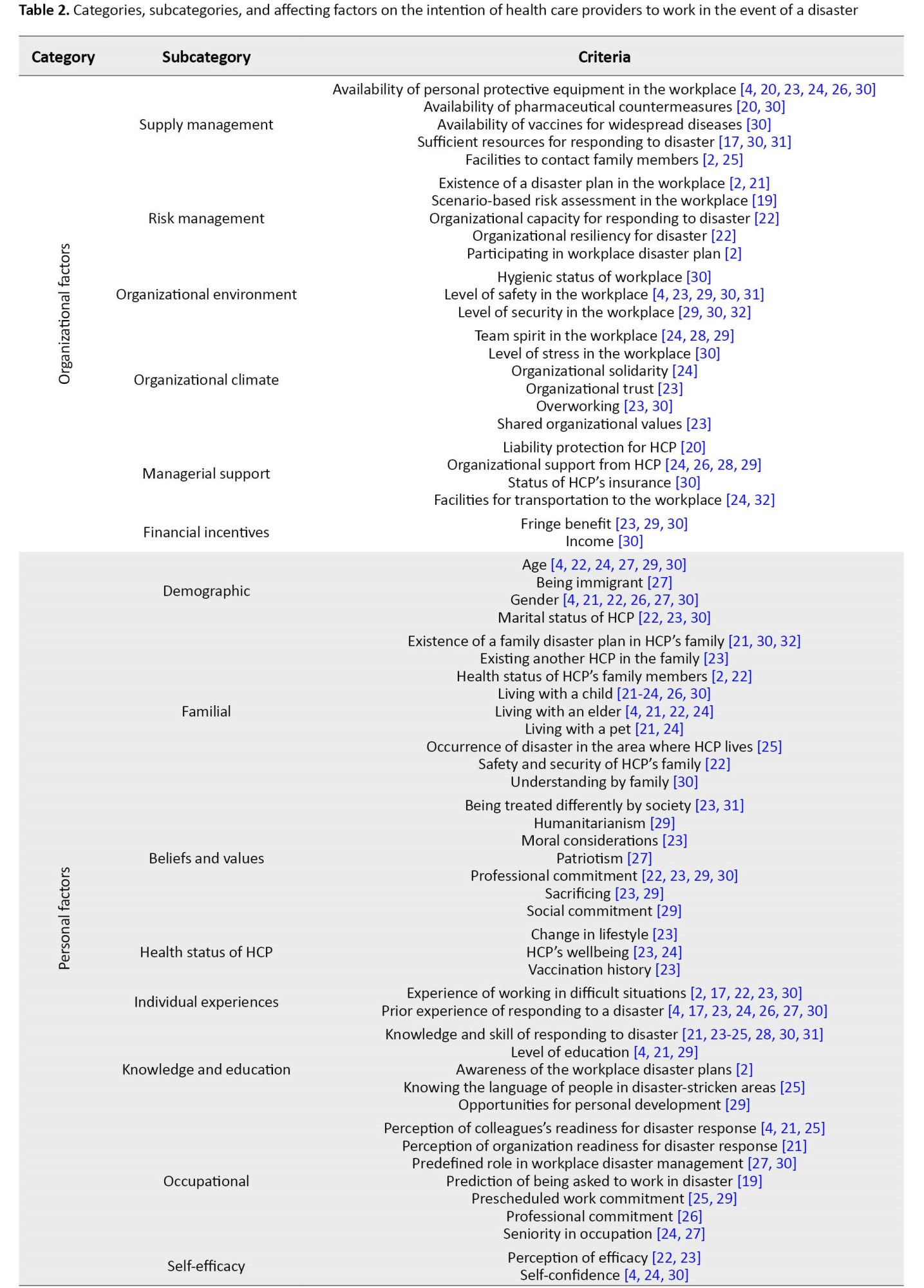
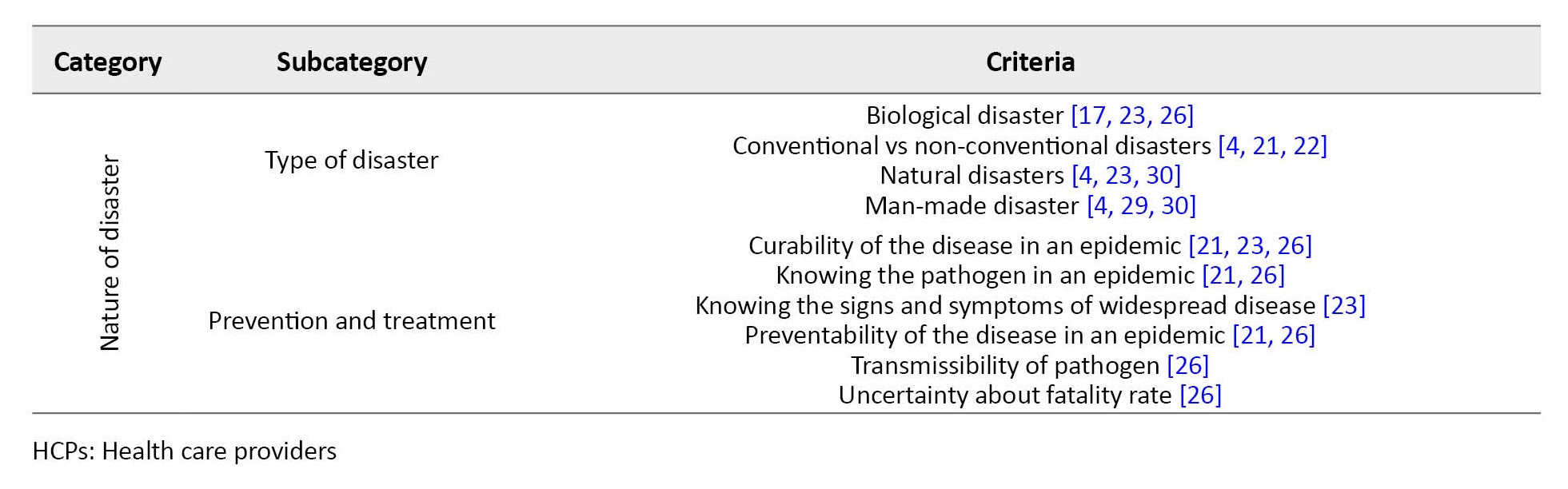
Considering the results of the articles, 75 factors affecting the intention of HCPs were identified and classified into 3 categories and 16 subcategories.
Discussion
In the present study, 13 studies explicitly examined the intention of nurses to participate in disasters, of which one investigated only nursing students, and three surveyed a combination of nurses, physicians, or nurses, physicians, and emergency medical technicians. This finding revealed that health systems had focused on assessing nurses’ intentions as one of the critical health professions. Nurses, as the largest part of the HCPs, are the frontline responders in an emergency or disaster. During disasters, especially in non-conventional ones, nurses experience considerable anxiety [34]. Although caring for irradiated patients in radiological incidents poses the least risk for the HCPs [35-37], such anxiety could have a significant impact on their performance. As a practical solution, training can be used to increase the intention of HCPs in this regard. In most cases, the reluctance of HCPs was due to insufficient knowledge of the nature of disasters [38], leading to delays or refusal to provide care to the patients in disasters, especially chemical, biological, and radiological incidents [38, 39].
In the present study, safety-related issues, categorized into personal and organizational factors, affected the staff’s intention to work during a disaster. Concerns about the safety of family, colleagues, and HCPs were among the most frequent barriers to staff intention to work during disaster [2, 11, 40-45]. HCPs are vulnerable to many occupational hazards and experience a great deal of emotional stress as a result of working in healthcare settings [2, 46]. HCPs are concerned about their safety against illnesses, injuries, and even death, and this issue will ultimately lead to reluctance to work during a disaster [47-50]. The availability of appropriate treatments, prophylaxis, and infection control may increase their willingness to work in such conditions [41, 49, 51, 52]. Lack of trust in employers to provide safe conditions for employees during a disaster could be associated with a decrease in willingness to work [2, 40, 43, 53]. Providing none or contradictory information to HCPs can also cause some degrees of distrust in employers in the health system [2, 54, 55]
In this study, individual factors were demographic, familial, beliefs and values, the health status of HCPs, individual experiences, knowledge and education, occupational, and self-efficacy. Previous experience working in disasters was one of the factors affecting the willingness of HCPs to work during disasters. Nurses with prior disaster experience can play an important role in a crisis and perform triage and life-saving measures [21]. Other studies emphasized the experience of working in difficult situations [2, 17, 22, 23, 30] and prior experience of responding to a disaster [4, 17, 23, 24, 26, 27, 30]. Gaining experience is always beneficial, and by increasing a person’s experience in the natural disaster response team, HCP can be better present in the following events.
A higher level of knowledge and education due to increasing age obtaining more information and improving knowledge about accidents and disasters can increase the level of preparedness of nurses to respond to natural disasters [21, 23-25, 28, 30, 33].
Gender was another important individual factor [4, 21, 22, 26, 27, 30]. A man’s gender is one factor that relates to people’s physical and psychological condition. Since male nurses have more resilience and emotional control, they can perform better in this field. Special needs of female nurses in dealing with disasters can be a challenge that needs attention to reduce their psychological and emotional problems in these situations [56].
Communicating with family members was another influential factor that can improve the willingness of HCPs to be involved in disaster response operations, so one of the barriers was their perceived disability to communicate with their family members while working in such situations [40, 57, 58]. Working long shifts away from family members could cause concern for HCPs, who must be quarantined[40, 57]. Providing various communication methods with family members and friends might increase staff satisfaction and willingness to work in the event of a disaster.
Professional commitment was another important factor that persuaded the staff to work in times of disaster. Evidence suggests a strong sense of professional duty among HCPs worldwide [2, 43, 47, 51, 52, 55]. In some cases, HCPs stated that concerns for their personal or family’s safety might be overlooked in their desire to take on professional responsibilities [2, 40, 43]. Even some studies found the sense of professional duty to be the most influential factor in the intention of the emergency department staff to work during a disaster. However, some evidence predicated that HCPs felt compelled to work during a disaster [42, 47, 52].
The type of disaster was another factor affecting the staff’s intention. HCPs were more inclined to work in case of natural disasters such as earthquakes, floods, and storms, while their willingness to work diminished in non-conventional disasters such as biological, chemical, radiological, and nuclear incidents. A study on the desire of firefighting program students also yielded similar results, where more than 90% of the students were interested in participating in fire incidents and earthquake relief operations. In comparison, about 40% preferred not to be involved in nuclear disasters [59]. Smith et al. depicted that prehospital emergency technicians were more concerned about working in radiological and nuclear incidents [60]. Such a mentality could reduce human resources and disrupt response operations in radiological and nuclear incidents [61].
Epidemic of infectious diseases is another disaster the HCPs were less inclined to get involved in. HCPs experience severe psychological distress during the outbreak of infectious diseases [2, 62]. During the outbreak of MERS (the Middle East respiratory syndrome) as a contagious disease epidemic, evidence shows that more than 90% of HCPs in Saudi Arabia, nearly half of whom were nurses, had a negative attitude towards suspected or infected patients [63]. With the onset of reports on morbidity and mortality of such diseases, the level of anxiety and stress rise among HCPs, as they are likely to be called to the front line to fight against the disease due to a lack of manpower. Furthermore, if HCPs involved in managing the disease become infected or die from the disease, HCPs are more likely to avoid suspected or infected patients [64].
Evidence from previous studies suggested that factors related to the willingness of HCPs to work after public health disasters could be placed into four categories: Personal, professional, organizational, and safety (threat-related) factors; among the personal factors, the findings revealed that women were less willing to work in such situations than men [61, 62]. Concerns about family members, friends, pets, and personal commitments such as caring for a child or older adults were reported as powerful barriers to intention to work in times of disaster [16, 65, 66]. Among the professional factors, evidence indicates that clinical staff are more willing to work than non-clinical staff [65]. Belief in duty to care, knowledge, and a sense of efficiency were described as facilitators of intention to work in the event of a disaster. Organizational factors have not been widely discussed. Apparently, confidence in the employer’s ability to meet the basic needs of the staff (such as food, water, etc.) and other concerns was a key factor in this regard. Findings on safety-related factors depicted a lower tendency to work for disasters, posing a greater personal risk to the practitioners, such as infectious disease epidemics and biological, chemical, and radiological incidents compared to natural and other man-made disasters [16, 65, 67].
In addition to high morbidity and mortality that jeopardize the health of a community, epidemics of infectious diseases are considered a significant threat to the health system and especially the HCPs for being the frontline responders in such situations [12, 68, 69].
Studies have shown that the intention to work during a disaster might be associated with the nature and type of the event, professional needs, individual needs, work environment, atmosphere, knowledge about the incident, and a perception of efficacy [4, 16, 66]. Contrary to the popular belief that HCPs tend to work in any disaster, their intention to work highly depends on the type of disaster, the risk to their health and that of their families, their commitment to the community, professional and financial issues, responsibility, and so on.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences and Health Services.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Study design: Mohammad Reza Khajehminian, Mehdi Raadabadi, and Maryam Nikfard; Search strategy: Mohammad Reza Khajehminian and Mehdi Raadabadi; Databases search: Mehdi Raadabadi, Maryam Nikfard, and Mahnaz Eider; Analysis and interpretation of data: Mohammad Reza Khajehminian, Mehdi Raadabadi, and Maryam Nikfard; Drafting of the manuscript: Mehdi Raadabadi and Mahnaz Eider; Critically revision of the article: Mohammad Reza Khajehminian and Maryam Nikfard; Supervision: Mohammad Reza Khajehminian; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to all scholars who have conducted useful studies in other countries to examine the intention of HCPs to work in times of disaster, and this study is a review of their results. In addition, the authors consider it their duty to appreciate all HCPs who try to promote community health through their professional services.
References
According to the United Nations Office for Disaster Risk Reduction (UNDRR), disaster is “ a serious disruption of the functioning of a society leading to widespread human, material, economic, and environmental losses that exceed the capacity of a community to cope using its resources” [1]. Disasters challenge the ability of health systems to meet the needs of society. Damage to infrastructure, staff shortages at all levels, and an increasing need for health services will jeopardize the functioning of health systems [2, 3]. Therefore, healthcare providers (HCPs) must be prepared to manage a surge in the number of patients should a disaster occur [4, 5]. Some disasters may be followed by a lack of workforce and loss of equipment and supplies [6, 7, 8, 9]. In a disaster, HCPs are expected to provide care and treatment for the casualties and the nonemergency patients while concerned about their families [4].
Most people believe that HCPs, firefighters, and relief workers in general who participate in relief operations tend to work in any disaster. In contrast, these people are not always willing to work. Indeed, their intention to work in disaster relief operations is highly dependent on the type of disaster [10, 11]. Evidence also shows that the intention to work varies between 25% and 80% among HCPs in public health emergencies. Factors associated with the nurses’ intention to work in disasters included insufficient knowledge and skills, fear of contracting infectious diseases, overworking, sense of responsibility, perceived self-efficacy, financial compensation, age, gender, knowledge and attitude, and academic degree [12-16].
As an effective measure in the preparedness phase of disaster risk management, identifying the factors related to the intention to participate in disaster relief operations will lead to planning better and coping with such situations. This study used a systematic literature review approach to find the factors affecting the intention of HCPs to work in disaster response.
Materials and Methods
The protocol of this study is registered in PROSPERO (CRD42021234620). To obtain relevant studies from the databases, all original articles examining the intention of HCPs to participate in disaster response operations were enrolled in the study. There were no restrictions on the language of the publications. It is noteworthy that articles on the intention of other relief workers, such as firefighters, to participate in disasters, as well as those in the form of letters to the editor, literature review, short study or brief communication, and conference papers, were excluded.
Scopus, PubMed, and Web of Science (WoS) databases were searched to obtain relevant studies published between 1950 and November 1, 2020. To develop the search strategy, several relevant studies on the intention of HCPs to work in disasters were reviewed to extract the keywords. Regarding the frequent use of”human resource,” all entry terms for this keyword were collected using the MeSH feature. Words were combined using the Boolean search method: AND and the OR operators.
All the retrieved documents using the above syntaxes were imported into EndNote, and duplicates were removed. The articles were screened for titles and abstracts, and the relevant items were selected. Next, the full-text articles were assessed by two authors for eligibility criteria. Any disagreement between the two authors was resolved through group discussion and consensus. In case of disagreement after the group discussion, advice and the opinion of a third party were considered. The references of the included articles were also examined to find possible related articles. Using the Scopus database, key journals in the area of the research title were also reviewed.
After the search was completed, data extraction was provided, and they were imported into Microsoft Excel, version 2010. Each extracted factor affecting the intention of HCPs was entered into Excel, and then the concatenate function was connected to the related article code. All extracted factors were then categorized by thematic analysis, i.e. first, all the affecting factors were listed and then classified into categories and subcategories through a group discussion attended by the research authors and using the data validation feature in Excel. The same factors mentioned in different studies were merged, and a common label was chosen for similar factors. Any uncertainty over labeling and categorizing the factors was discussed with the review team.
Results
An initial search in Scopus, PubMed, and Web of Science databases yielded 5721 documents, of which 1818 duplicates were removed after being imported into EndNote, version 9 (Figure 1). The 16 enrolled studies in the systematic review were conducted between 2009 and 2020 in Australia (2), South Korea (3), the United States (4), Israel (3), Yemen (1), China (1), Taiwan (1), and Brazil (1). There was one mixed methods study, and the other 15 were performed using quantitative methods. In total, 13 studies specifically examined the intention of nurses to work in disasters, of which one investigated only nursing students and 3 surveyed a combination of nurses, physicians, physicians and or nurses, and emergency medical technicians (Table 1).
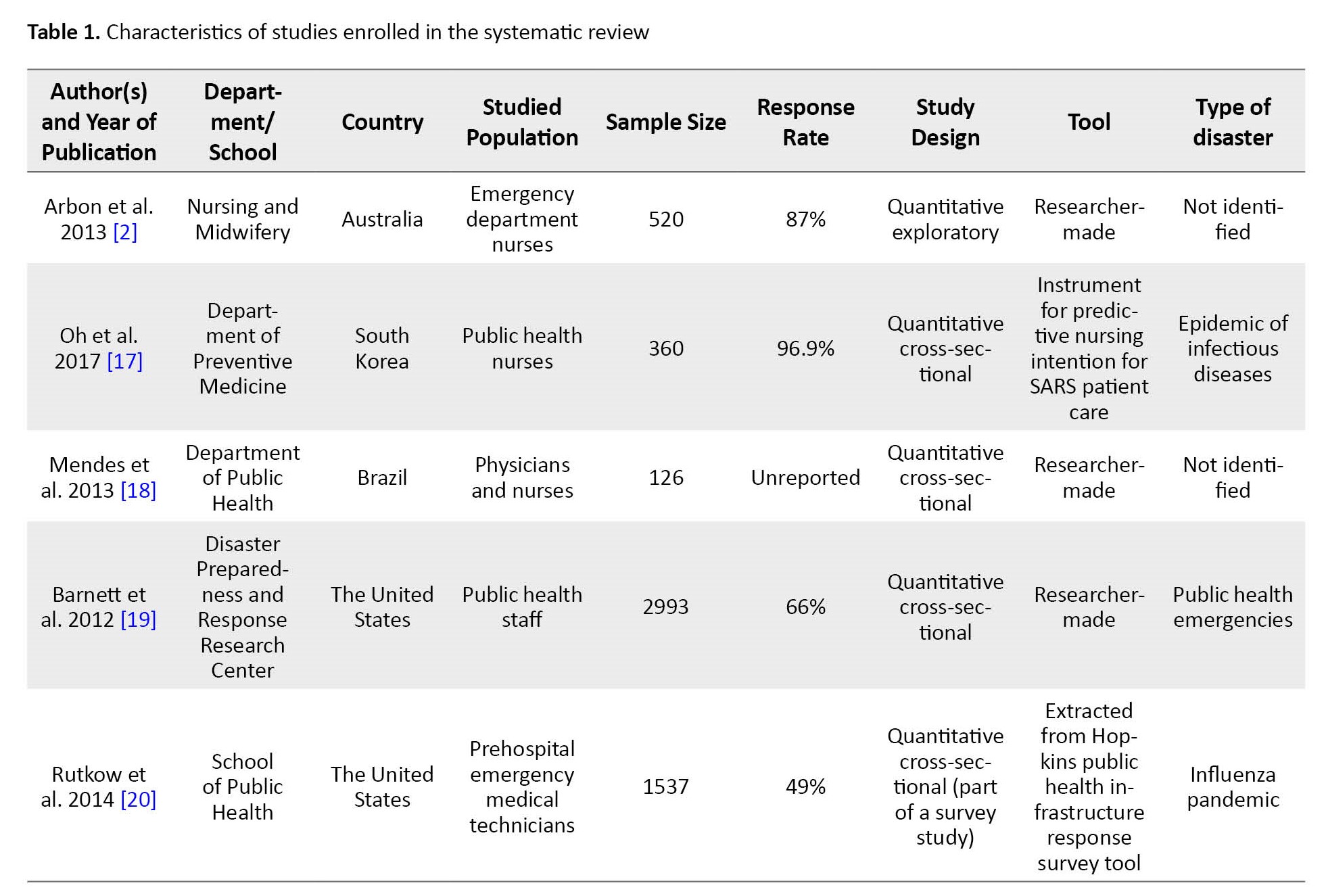
Regarding data collection tools, four studies used specific tools to assess the intention of HCPs in disasters, and the remaining 11 employed researcher-made tools based on the review of previous studies or modification of other non-specific questionnaires of staff intention to work. Only one study approached the issue in a qualitative design using interviews and focus group discussions.
As explained in the study methods, using the concatenate function in Excel, every factor affecting the intention of HCPs was imported into Excel and then connected to the study with the related article code. Next, all extracted factors were categorized by thematic analysis. First, all the affecting factors were listed and then classified through a group discussion attended by the research authors and using the data validation feature in Excel into the following categories and subcategories: Organizational factors (supply management, risk management, organizational environment, organizational climate, managerial support, financial incentives), personal factors (demographic, familial, beliefs and values, health status of HCP, individual experiences, knowledge and education, occupational, self-efficacy), and nature of the disaster (type of disaster, prevention, and treatment). The same factors mentioned in different studies were merged, and a common label was chosen for similar factors. The review team discussed any uncertainty over labeling and categorizing the factors (Table 2).
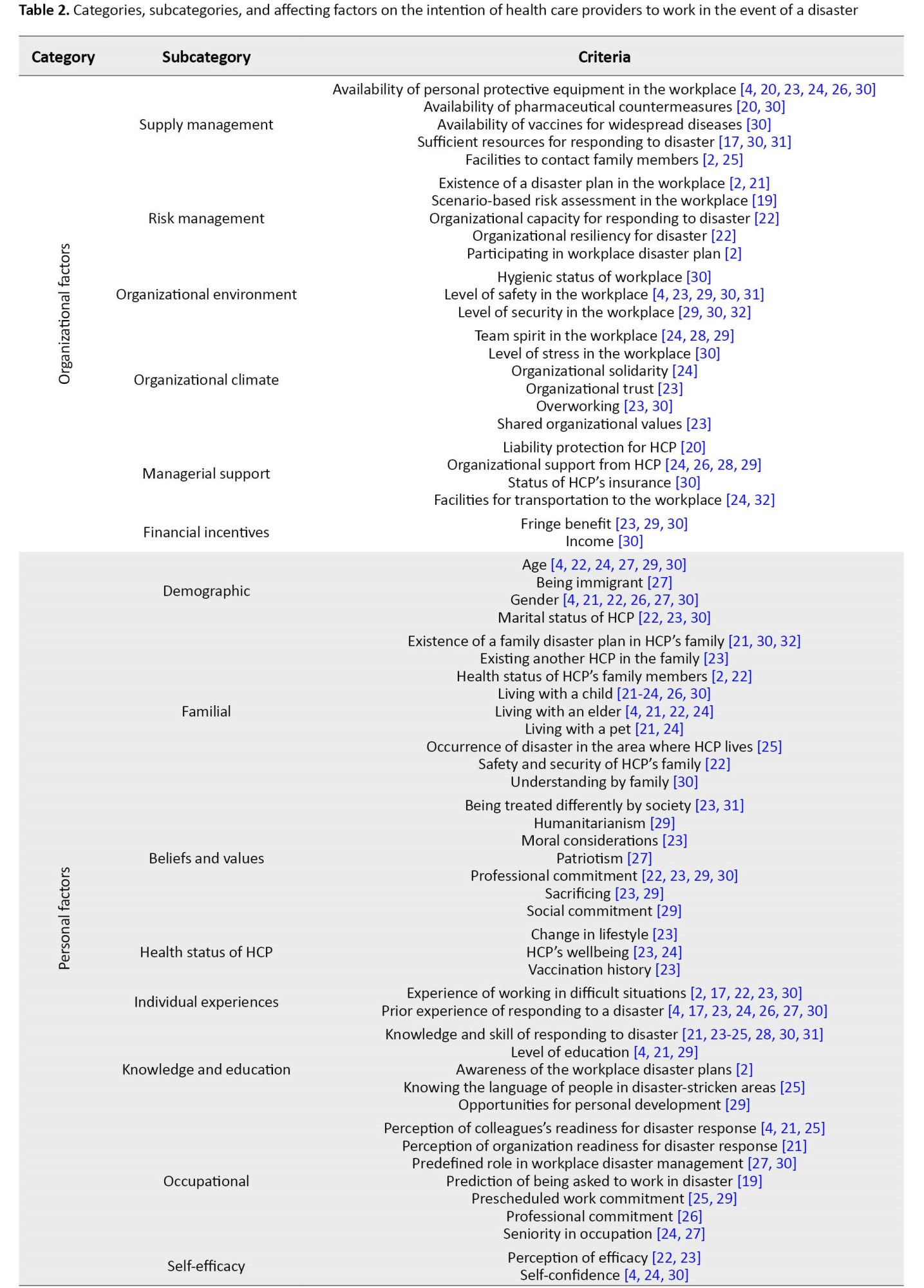
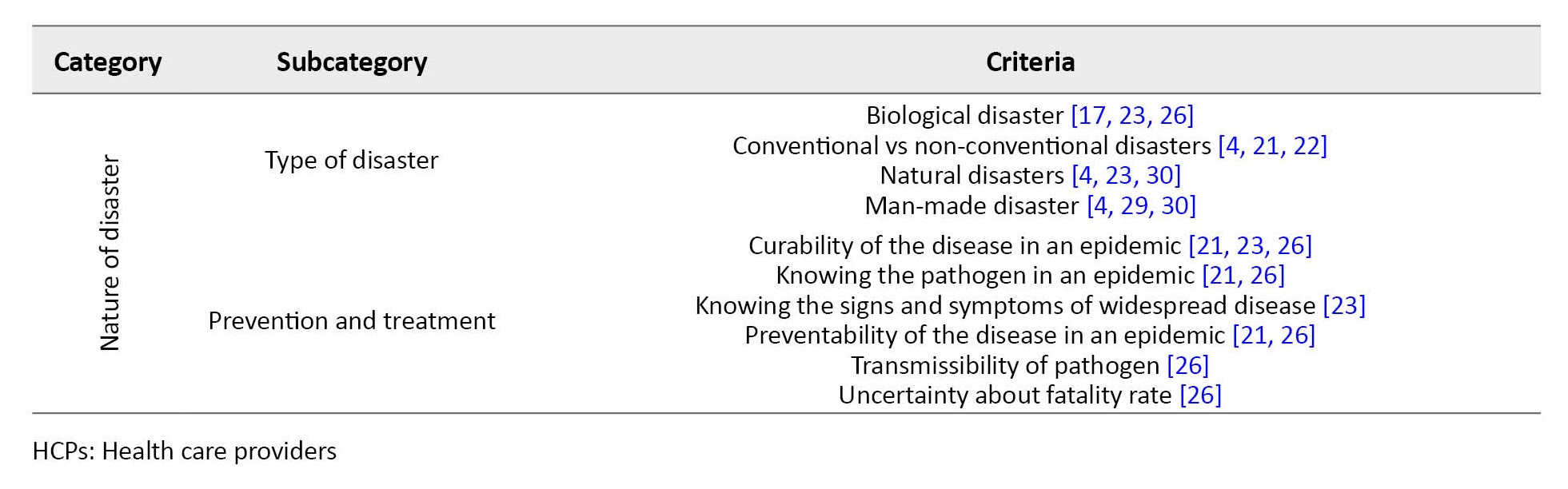
Considering the results of the articles, 75 factors affecting the intention of HCPs were identified and classified into 3 categories and 16 subcategories.
Discussion
In the present study, 13 studies explicitly examined the intention of nurses to participate in disasters, of which one investigated only nursing students, and three surveyed a combination of nurses, physicians, or nurses, physicians, and emergency medical technicians. This finding revealed that health systems had focused on assessing nurses’ intentions as one of the critical health professions. Nurses, as the largest part of the HCPs, are the frontline responders in an emergency or disaster. During disasters, especially in non-conventional ones, nurses experience considerable anxiety [34]. Although caring for irradiated patients in radiological incidents poses the least risk for the HCPs [35-37], such anxiety could have a significant impact on their performance. As a practical solution, training can be used to increase the intention of HCPs in this regard. In most cases, the reluctance of HCPs was due to insufficient knowledge of the nature of disasters [38], leading to delays or refusal to provide care to the patients in disasters, especially chemical, biological, and radiological incidents [38, 39].
In the present study, safety-related issues, categorized into personal and organizational factors, affected the staff’s intention to work during a disaster. Concerns about the safety of family, colleagues, and HCPs were among the most frequent barriers to staff intention to work during disaster [2, 11, 40-45]. HCPs are vulnerable to many occupational hazards and experience a great deal of emotional stress as a result of working in healthcare settings [2, 46]. HCPs are concerned about their safety against illnesses, injuries, and even death, and this issue will ultimately lead to reluctance to work during a disaster [47-50]. The availability of appropriate treatments, prophylaxis, and infection control may increase their willingness to work in such conditions [41, 49, 51, 52]. Lack of trust in employers to provide safe conditions for employees during a disaster could be associated with a decrease in willingness to work [2, 40, 43, 53]. Providing none or contradictory information to HCPs can also cause some degrees of distrust in employers in the health system [2, 54, 55]
In this study, individual factors were demographic, familial, beliefs and values, the health status of HCPs, individual experiences, knowledge and education, occupational, and self-efficacy. Previous experience working in disasters was one of the factors affecting the willingness of HCPs to work during disasters. Nurses with prior disaster experience can play an important role in a crisis and perform triage and life-saving measures [21]. Other studies emphasized the experience of working in difficult situations [2, 17, 22, 23, 30] and prior experience of responding to a disaster [4, 17, 23, 24, 26, 27, 30]. Gaining experience is always beneficial, and by increasing a person’s experience in the natural disaster response team, HCP can be better present in the following events.
A higher level of knowledge and education due to increasing age obtaining more information and improving knowledge about accidents and disasters can increase the level of preparedness of nurses to respond to natural disasters [21, 23-25, 28, 30, 33].
Gender was another important individual factor [4, 21, 22, 26, 27, 30]. A man’s gender is one factor that relates to people’s physical and psychological condition. Since male nurses have more resilience and emotional control, they can perform better in this field. Special needs of female nurses in dealing with disasters can be a challenge that needs attention to reduce their psychological and emotional problems in these situations [56].
Communicating with family members was another influential factor that can improve the willingness of HCPs to be involved in disaster response operations, so one of the barriers was their perceived disability to communicate with their family members while working in such situations [40, 57, 58]. Working long shifts away from family members could cause concern for HCPs, who must be quarantined[40, 57]. Providing various communication methods with family members and friends might increase staff satisfaction and willingness to work in the event of a disaster.
Professional commitment was another important factor that persuaded the staff to work in times of disaster. Evidence suggests a strong sense of professional duty among HCPs worldwide [2, 43, 47, 51, 52, 55]. In some cases, HCPs stated that concerns for their personal or family’s safety might be overlooked in their desire to take on professional responsibilities [2, 40, 43]. Even some studies found the sense of professional duty to be the most influential factor in the intention of the emergency department staff to work during a disaster. However, some evidence predicated that HCPs felt compelled to work during a disaster [42, 47, 52].
The type of disaster was another factor affecting the staff’s intention. HCPs were more inclined to work in case of natural disasters such as earthquakes, floods, and storms, while their willingness to work diminished in non-conventional disasters such as biological, chemical, radiological, and nuclear incidents. A study on the desire of firefighting program students also yielded similar results, where more than 90% of the students were interested in participating in fire incidents and earthquake relief operations. In comparison, about 40% preferred not to be involved in nuclear disasters [59]. Smith et al. depicted that prehospital emergency technicians were more concerned about working in radiological and nuclear incidents [60]. Such a mentality could reduce human resources and disrupt response operations in radiological and nuclear incidents [61].
Epidemic of infectious diseases is another disaster the HCPs were less inclined to get involved in. HCPs experience severe psychological distress during the outbreak of infectious diseases [2, 62]. During the outbreak of MERS (the Middle East respiratory syndrome) as a contagious disease epidemic, evidence shows that more than 90% of HCPs in Saudi Arabia, nearly half of whom were nurses, had a negative attitude towards suspected or infected patients [63]. With the onset of reports on morbidity and mortality of such diseases, the level of anxiety and stress rise among HCPs, as they are likely to be called to the front line to fight against the disease due to a lack of manpower. Furthermore, if HCPs involved in managing the disease become infected or die from the disease, HCPs are more likely to avoid suspected or infected patients [64].
Evidence from previous studies suggested that factors related to the willingness of HCPs to work after public health disasters could be placed into four categories: Personal, professional, organizational, and safety (threat-related) factors; among the personal factors, the findings revealed that women were less willing to work in such situations than men [61, 62]. Concerns about family members, friends, pets, and personal commitments such as caring for a child or older adults were reported as powerful barriers to intention to work in times of disaster [16, 65, 66]. Among the professional factors, evidence indicates that clinical staff are more willing to work than non-clinical staff [65]. Belief in duty to care, knowledge, and a sense of efficiency were described as facilitators of intention to work in the event of a disaster. Organizational factors have not been widely discussed. Apparently, confidence in the employer’s ability to meet the basic needs of the staff (such as food, water, etc.) and other concerns was a key factor in this regard. Findings on safety-related factors depicted a lower tendency to work for disasters, posing a greater personal risk to the practitioners, such as infectious disease epidemics and biological, chemical, and radiological incidents compared to natural and other man-made disasters [16, 65, 67].
In addition to high morbidity and mortality that jeopardize the health of a community, epidemics of infectious diseases are considered a significant threat to the health system and especially the HCPs for being the frontline responders in such situations [12, 68, 69].
Studies have shown that the intention to work during a disaster might be associated with the nature and type of the event, professional needs, individual needs, work environment, atmosphere, knowledge about the incident, and a perception of efficacy [4, 16, 66]. Contrary to the popular belief that HCPs tend to work in any disaster, their intention to work highly depends on the type of disaster, the risk to their health and that of their families, their commitment to the community, professional and financial issues, responsibility, and so on.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences and Health Services.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Study design: Mohammad Reza Khajehminian, Mehdi Raadabadi, and Maryam Nikfard; Search strategy: Mohammad Reza Khajehminian and Mehdi Raadabadi; Databases search: Mehdi Raadabadi, Maryam Nikfard, and Mahnaz Eider; Analysis and interpretation of data: Mohammad Reza Khajehminian, Mehdi Raadabadi, and Maryam Nikfard; Drafting of the manuscript: Mehdi Raadabadi and Mahnaz Eider; Critically revision of the article: Mohammad Reza Khajehminian and Maryam Nikfard; Supervision: Mohammad Reza Khajehminian; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to all scholars who have conducted useful studies in other countries to examine the intention of HCPs to work in times of disaster, and this study is a review of their results. In addition, the authors consider it their duty to appreciate all HCPs who try to promote community health through their professional services.
References
- United Nations International Strategy for Disaster Reduction (UNISDR). 2009 UNISDR terminology on disaster risk reduction. Geneva: UNISDR; 2009. [Link]
- Arbon P, Cusack L, Ranse J, Shaban RZ, Considine J, Kako M, et al. Exploring staff willingness to attend work during a disaster: A study of nurses employed in four Australian emergency departments. Australas Emerg Nurs J. 2013; 16(3):103-9. [DOI:10.1016/j.aenj.2013.05.004] [PMID]
- Below R, Wirtz A, Guha-Sapir D. Disaster category classification and peril terminology for operational purposes. Louvain-la-Neuve: UCL Université catholique de Louvain; 2009. [Link]
- Al-Hunaishi W, Hoe VC, Chinna K. Factors associated with healthcare workers willingness to participate in disasters: A cross-sectional study in Sana'a, Yemen. BMJ Open. 2019; 9(10):e030547. [DOI:10.1136/bmjopen-2019-030547] [PMID]
- Kavukcu N, Altıntaş KH. The challenges of the health care providers in refugee settings: A systematic review. Prehosp Disaster Med. 2019; 34(2):188-96. [DOI:10.1017/S1049023X19000190] [PMID]
- Paturas JL, Smith D, Smith S, Albanese J. Collective response to public health emergencies and large-scale disasters: Putting hospitals at the core of community resilience. J Bus Contin Emer Plan. 2010; 4(3):286-95. [Link] [PMID]
- Timbie JW, Ringel JS, Fox DS, Pillemer F, Waxman DA, Moore M, et al. Systematic review of strategies to manage and allocate scarce resources during mass casualty events. Ann Emerg Med. 2013; 61(6):677-89.e101. [PMID]
- Abolghasem Gorgi H, Jafari M, Shabanikiya H, Seyedin H, Rahimi A, Vafaee-Najar A. Hospital surge capacity in disasters in a developing country: Challenges and strategies. Trauma Monthly. 2017; 22(5):1-5. [DOI:10.5812/traumamon.59238]
- Verelst F, Kuylen E, Beutels P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, March 2020. Euro Surveill. 2020; 25(13):2000323. [DOI:10.2807/1560-7917.ES.2020.25.13.2000323] [PMID]
- Lanzilotti SS, Galanis D, Leoni N, Craig B. Hawaii medical professionals assessment. Hawaii Med J. 2002; 61(8):162-73. [PMID]
- Qureshi K, Gershon RR, Sherman MF, Straub T, Gebbie E, McCollum M, et al. Health care workers' ability and willingness to report to duty during catastrophic disasters. J Urban Health. 2005; 82(3):378-88. [DOI:10.1093/jurban/jti086] [PMID]
- Li J, Li P, Chen J, Ruan L, Zeng Q, Gong Y. Intention to response, emergency preparedness and intention to leave among nurses during COVID-19. Nurs Open. 2020; 7(6):1867-75. [DOI:10.1002/nop2.576] [PMID]
- Maleki L, Pourshaikhian M, Moghadamnia M, Kazemnejad E. Evaluating knowledge and attitude of nurses about disaster preparedness and response phase. Int J Pharmaceutical Research. 2018; 10(1):292-8. [Link]
- Maleki L, Moghadamnia MT, Porshikhian M, Kazemnejad E. Evaluation of the factors predictingnurses’ attitude to phase of preparedness to respond to disasters. Revista Latinoamericana de Hipertensión. 2018; 13(6):538-43. [Link]
- Alwidyan MT, Trainor JE, Bissell RA. Responding to natural disasters vs. disease outbreaks: Do emergency medical service providers have different views? Int J Disaster Risk Reduct. 2020; 44:101440. [DOI:10.1016/j.ijdrr.2019.101440] [PMID]
- Connor SB. When and why health care personnel respond to a disaster: The state of the science. Prehosp Disaster Med. 2014; 29(3):270-4. [DOI:10.1017/S1049023X14000387] [PMID]
- Oh N, Hong N, Ryu DH, Bae SG, Kam S, Kim KY. Exploring nursing intention, stress, and professionalism in response to infectious disease emergencies: The experience of local public hospital nurses during the 2015 MERS Outbreak in South Korea. Asian Nurs Res (Korean Soc Nurs Sci). 2017; 11(3):230-6. [DOI:10.1016/j.anr.2017.08.005] [PMID]
- Mendes Ada C, de Araújo Júnior JL, Furtado BM, Duarte PO, da Silva AL, Miranda GM. [Conditions and motivations for the work of nurses and physicians in high complexity emergency services (Portuguese)] . Rev Bras Enferm. 2013; 66(2):161-6. [DOI:10.1590/S0034-71672013000200002] [PMID]
- Barnett DJ, Thompson CB, Errett NA, Semon NL, Anderson MK, Ferrell JL, et al. Determinants of emergency response willingnes in the local public health workforce by jurisdictional and scenario patterns: A cross-sectional survey. BMC Public Health. 2012; 12:164. [DOI:10.1186/1471-2458-12-164] [PMID]
- Rutkow L, Vernick JS, Gakh M, Siegel J, Thompson CB, Barnett DJ. The public health workforce and willingness to respond to emergencies: A 50-state analysis of potentially influential laws. J Law Med Ethics. 2014; 42(1):64-71. [DOI:10.1111/jlme.12119] [PMID]
- Arbon P, Ranse J, Cusack L, Considine J, Shaban RZ, Woodman RJ, et al. Australasian emergency nurses' willingness to attend work in a disaster: A survey. Australas Emerg Nurs J. 2013; 16(2):52-7. [DOI:10.1016/j.aenj.2013.05.003] [PMID]
- Shapira S, Friger M, Bar-Dayan Y, Aharonson-Daniel L. Healthcare workers' willingness to respond following a disaster: A novel statistical approach toward data analysis. BMC Med Educ. 2019; 19(1):130. [DOI:10.1186/s12909-019-1561-7] [PMID]
- Jeong SA, Kim J. Factors influencing nurses’ intention to care for patients with COVID-19: Focusing on positive psychological capital and nursing professionalism. Plos One. 2022; 17(1):e0262786. [PMID]
- Melnikov S, Itzhaki M, Kagan I. Israeli nurses' intention to report for work in an emergency or disaster. J Nurs Scholarsh. 2014; 46(2):134-42. [DOI:10.1111/jnu.12056] [PMID]
- Choe MA, Kuwano N, Bang KS, Cho MK, Yatsushiro R, Kawata Y. Japanese and Korean nursing students’ motivation for joining disaster relief activities as nurses in the future. J Trauma Nurs. 2017; 24(3):208-18. [DOI:10.1097/JTN.0000000000000291] [PMID]
- Grimes DE, Mendias EP. Nurses' intentions to respond to bioterrorism and other infectious disease emergencies. Nurs Outlook. 2010; 58(1):10-6. [DOI:10.1016/j.outlook.2009.07.002] [PMID]
- Kagan I, Itzhaki M, Melnikov S. Patriotism, organizational commitment and nurses' intention to report for work in emergencies. Int Nurs Rev. 2017; 64(4):468-75. [DOI:10.1111/inr.12395] [PMID]
- Liou SR, Liu HC, Tsai HM, Chu TP, Cheng CY. Relationships between disaster nursing competence, anticipatory disaster stress and motivation for disaster engagement. Int J Disaster Risk Reduct. 2020; 47:101545. [DOI:10.1016/j.ijdrr.2020.101545] [PMID]
- Oh J, Ro YS, Lee JK, Kim MJ, Shin SD, Ahn J, et al. The willingness of and barriers to Korean health care providers participating in a humanitarian assistance field hospital responding to an urgent global health crisis. World Hosp Health Serv. 2014; 50(4):10-6. [PMID]
- Goodhue CJ, Burke RV, Ferrer RR, Chokshi NK, Dorey F, Upperman JS. Willingness to respond in a disaster: A pediatric nurse practitioner national survey. J Pediatr Health Care. 2012; 26(4):e7-20. [DOI:10.1016/j.pedhc.2010.11.003] [PMID]
- Rutkow L, Vernick JS, Thompson CB, Pirrallo RG, Barnett DJ. Emergency preparedness law and willingness to respond in the EMS workforce. Prehosp Disaster Med. 2014; 29(4):358-63. [DOI:10.1017/S1049023X14000788] [PMID]
- Saleh MO, Eshah NF, Rayan AH. Empowerment predicting nurses’ work motivation and occupational mental health. SAGE Open Nurs. 2022; 8:23779608221076811. [DOI:10.1177/23779608221076811]
- Iyama K, Takano Y, Takahashi T, Hasegawa A. Factors associated with the intention to participate in activities during a nuclear disaster situation among firefighters. J Radiat Res. 2020; 61(6):871-5. [DOI:10.1093/jrr/rraa061] [PMID]
- Smith JM, Spano MA. Interim guidelines for hospital response to mass casualties from a radiological incident. Radiation emergencies. Atlanta: Centers for Disease Control and Prevention; 2003. [Link]
- Hogan DE, Burstein JL. Disaster medicine. Philadelphia: Lippincott Williams & Wilkins; 2007. [Link]
- Veenema TG. Disaster nursing and emergency preparedness. Berlin: Springer; 2018. [Link]
- Bushberg JT, Kroger LA, Hartman MB, Leidholdt EM Jr, Miller KL, Derlet R, et al. Nuclear/radiological terrorism: Emergency department management of radiation casualties. J Emerg Med. 2007; 32(1):71-85. [DOI:10.1016/j.jemermed.2006.05.034] [PMID]
- Veenema TG, Karam PA. Radiation: Clinical responses to radiologic incidents and emergencies. Am J Nurs. 2003; 103(5):32-40; quiz 50. [DOI:10.1097/00000446-200305000-00016] [PMID]
- Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors' knowledge of radiation exposure: Questionnaire study. BMJ. 2003; 327(7411):371-2. [DOI:10.1136/bmj.327.7411.371] [PMID]
- Smith E, Morgans A, Qureshi K, Burkle Jr FS, Archer F. Paramedics’ perceptions of risk and willingness to work during disasters. The Australian J Emerg Manag. 2009; 24(3):21-7. [Link]
- Garrett AL, Park YS, Redlener I. Mitigating absenteeism in hospital workers during a pandemic. Disaster Med Public Health Prep. 2009; 3 Suppl 2:S141-7. [DOI:10.1097/DMP.0b013e3181c12959] [PMID]
- Imai H, Matsuishi K, Ito A, Mouri K, Kitamura N, Akimoto K, et al. Factors associated with motivation and hesitation to work among health professionals during a public crisis: A cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Public Health. 2010; 10:672. [DOI:10.1186/1471-2458-10-672] [PMID]
- Seale H, Leask J, Po K, MacIntyre CR. "Will they just pack up and leave?" - Attitudes and intended behaviour of hospital health care workers during an influenza pandemic. BMC Health Serv Res. 2009; 9:30. [DOI:10.1186/1472-6963-9-30] [PMID]
- Chaffee MW. Making the decision to report to work in a disaster: Nurses may have conflicting obligations. Am J Nurs. 2006; 106(9):54-7. [DOI:10.1097/00000446-200609000-00027] [PMID]
- O'Boyle C, Robertson C, Secor-Turner M. Nurses' beliefs about public health emergencies: Fear of abandonment. Am J Infect Control. 2006; 34(6):351-7. [DOI:10.1016/j.ajic.2006.01.012] [PMID]
- Wheeler HH. A review of nurse occupational stress research: 1. Br J Nurs. 1997; 6(11):642-5. [DOI:10.12968/bjon.1997.6.11.642] [PMID]
- Cowden J, Crane L, Lezotte D, Glover J, Nyquist AC. Pre-pandemic planning survey of healthcare workers at a tertiary care children's hospital: Ethical and workforce issues. Influenza Other Respir Viruses. 2010; 4(4):213-22. [DOI:10.1111/j.1750-2659.2010.00145.x] [PMID]
- Damery S, Wilson S, Draper H, Gratus C, Greenfield S, Ives J, et al. Will the NHS continue to function in an influenza pandemic? A survey of healthcare workers in the West Midlands, UK. BMC Public Health. 2009; 9:142. [DOI:10.1186/1471-2458-9-142] [PMID]
- Irvin CB, Cindrich L, Patterson W, Southall A. Survey of hospital healthcare personnel response during a potential avian influenza pandemic: Will they come to work? Prehosp Disaster Med. 2008; 23(4):328-35. [DOI:10.1017/S1049023X00005963] [PMID]
- Martin SD. Nurses' ability and willingness to work during pandemic flu. J Nurs Manag. 2011; 19(1):98-108. [DOI:10.1111/j.1365-2834.2010.01190.x] [PMID]
- Lee S, Kim Y. Predictors of bioterrorism preparedness among clinical nurses: A cross-sectional study. Nurse Educ Today. 2023; 122:105727. [PMID]
- Masterson L, Steffen C, Brin M, Kordick MF, Christos S. Willingness to respond: Of emergency department personnel and their predicted participation in mass casualty terrorist events. J Emerg Med. 2009; 36(1):43-9. [DOI:10.1016/j.annemergmed.2004.07.114] [PMID]
- Tippett VC, Watt K, Raven SG, Kelly HA, Coory M, Archer F, et al. Anticipated behaviors of emergency prehospital medical care providers during an influenza pandemic. Prehosp Disaster Med. 2010; 25(1):20-5. [DOI:10.1017/S1049023X00007603] [PMID]
- Considine J, Shaban RZ, Patrick J, Holzhauser K, Aitken P, Clark M, et al. Pandemic (H1N1) 2009 Influenza in Australia: Absenteeism and redeployment of emergency medicine and nursing staff. Emerg Med Australas. 2011; 23(5):615-23. [DOI:10.1111/j.1742-6723.2011.01461.x] [PMID]
- Healthcare workers' attitudes to working during pandemic influenza: A qualitative study. BMC Public Health. 2009; 9:56. [DOI:10.1186/1471-2458-9-56] [PMID]
- Pourvakhshoori N, Norouzi K, Ahmadi F, Hosseini M, Khankeh H. Challenges of female nurses in disasters: A qualitative study. Health in Emerg Disaster Q. 2016; 2(1):5-12. [DOI:10.18869/nrip.hdq.2.1.5]
- O'Sullivan TL, Amaratunga C, Phillips KP, Corneil W, O'Connor E, Lemyre L, et al. If schools are closed, who will watch our kids? Family caregiving and other sources of role conflict among nurses during large-scale outbreaks. Prehosp Disaster Med. 2009; 24(4):321-5. [DOI:10.1017/S1049023X00007044] [PMID]
- Gershon RR, Magda LA, Qureshi KA, Riley HE, Scanlon E, Carney MT, et al. Factors associated with the ability and willingness of essential workers to report to duty during a pandemic. J Occup Environ Med. 2010; 52(10):995-1003. [DOI:10.1097/JOM.0b013e3181f43872] [PMID]
- Kaya E, Altintas H. Willingness of Firefighting program students to work in Disasters-Turkey. Prehosp Disaster Med. 2018; 33(1):13-22. [DOI:10.1017/S1049023X17007087] [PMID]
- Smith EC, Burkle FM Jr, Archer FL. Fear, familiarity, and the perception of risk: A quantitative analysis of disaster-specific concerns of paramedics. Disaster Med Public Health Prep. 2011; 5(1):46-53. [DOI:10.1001/dmp.10-v4n2-hre10008] [PMID]
- Iyama K, Kakamu T, Yamashita K, Shimada J, Tasaki O, Hasegawa A. Survey about intention to engage in specific disaster activities among disaster medical assistance team members. Prehosp Disaster Med. 2021; 36(6):684-90. [DOI:10.1017/S1049023X21001035] [PMID]
- Chen CS, Wu HY, Yang P, Yen CF. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr Serv. 2005; 56(1):76-9. [DOI:10.1176/appi.ps.56.1.76] [PMID]
- Nour MO, Babilghith AO, Natto HA, Al-Amin FO, Alawneh SM. Knowledge, attitude and practices of healthcare providers towards MERS-CoV infection at Makkah hospitals, KSA. Int Res J Med Sci. 2015; 3(4):103-12. [Link]
- Stone PW, Mooney-Kane C, Larson EL, Horan T, Glance LG, Zwanziger J, et al. Nurse working conditions and patient safety outcomes. Med Care. 2007; 45(6):571-8. [DOI:10.1097/MLR.0b013e3180383667] [PMID]
- Devnani M. Factors associated with the willingness of health care personnel to work during an influenza public health emergency: An integrative review. Prehosp Disaster Med. 2012; 27(6):551-66. [DOI:10.1017/S1049023X12001331] [PMID]
- Chaffee M. Willingness of health care personnel to work in a disaster: An integrative review of the literature. Disaster Med Public Health Prep. 2009; 3(1):42-56. [DOI:10.1097/DMP.0b013e31818e8934] [PMID]
- Charney RL, Rebmann T, Flood RG. Hospital employee willingness to work during earthquakes versus pandemics. J Emerg Med. 2015; 49(5):665-74. [DOI:10.1016/j.jemermed.2015.07.030] [PMID]
- Yonge O, Rosychuk RJ, Bailey TM, Lake R, Marrie TJ. Willingness of university nursing students to volunteer during a pandemic. Public Health Nurs. 2010; 27(2):174-80. [DOI:10.1111/j.1525-1446.2010.00839.x] [PMID]
- Cheong SK, Wong TY, Lee HY, Fong YT, Tan BY, Koh GCh, et al. Concerns and preparedness for an avian influenza pandemic: A comparison between community hospital and tertiary hospital healthcare workers. Ind Health. 2007; 45(5):653-61. [DOI:10.2486/indhealth.45.653] [PMID]
Article Type : Research |
Subject:
General
Received: 2024/02/28 | Accepted: 2024/02/21 | Published: 2024/02/21
Received: 2024/02/28 | Accepted: 2024/02/21 | Published: 2024/02/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |