Sun, Apr 28, 2024
Volume 34, Issue 2 (2-2024)
JHNM 2024, 34(2): 143-150 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Musdalifah Ahmad S, Syam Y, Saleh A. The Role of Complementary Therapy to Reduce Insomnia in Older Adults. JHNM 2024; 34 (2) :143-150
URL: http://hnmj.gums.ac.ir/article-1-2306-en.html
URL: http://hnmj.gums.ac.ir/article-1-2306-en.html
1- Executive Nurse, Department of Medical-Surgical Nursing, Hasanuddin University Teaching Hospital, Makassar, Indonesia. , musdalifah19ahmad@gmail.com
2- Head Lecturer, Department of Fundamental Nursing, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia.
3- Professor, Department of Mental Health Nursing, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia.
2- Head Lecturer, Department of Fundamental Nursing, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia.
3- Professor, Department of Mental Health Nursing, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia.
Full-Text [PDF 551 kb]
(91 Downloads)
| Abstract (HTML) (271 Views)
Full-Text: (64 Views)
Introduction
Based on world population aging, the number of older people is increasing, more than 962 million each year [1, 2]. The Central Bureau of Statistics [3] estimates that the number of elderly aged 60 years and over will continue to increase until 2045 because of demographic transition [4]. This rising trend cannot be separated from the aging process, which causes a decline in health conditions; one of the most common complaints by older adults is sleep disturbances [5, 6]. Insomnia is a symptom in which older adults lack enough sleep, feel tired when they wake up, or frequently wake up at night. It is caused by degenerative processes in older people [7-9], which decreases neurotransmitter function by inhibiting melatonin production as a sleep hormone. This deficiency makes older people awake or experience sleep disturbances [9]. Thus, insomnia results from aging in older adults as a process of decreasing body function.
Insomnia in older adults will cause many health problems and, if left untreated, will impact their quality of life [10]. Thus, effective interventions are needed for dealing with the problem of insomnia in older adults. Complementary therapy is one of the best interventions because it is cheap, has many benefits, and lacks harmful side effects, especially in older adults [10]. Holistically, complementary therapy can stimulate the hypothalamus-pituitary-axis (HPA) mechanism to improve blood circulation, help metabolism work optimally, and relay neurotransmitters throughout the body, thereby reducing reactions to pain, stress, and depression—creating a feeling of relaxation that can make the elderly sleep soundly [12, 13]. Thus, complementary therapy is an appropriate intervention in reducing the problem of sleep disturbances in older adults and improving their quality of sleep.
Although there are many types of complementary therapies, such as massage, music therapy, relaxation techniques, acupuncture, and physical exercises recommended in nursing interventions, the problem of insomnia in older adults is still largely unnoticed [14-16]. In other words, no studies have examined the nature of complementary therapies to alleviate insomnia in older adults, only the quality of his sleep. Therefore, this systematic review examined the complementary therapies commonly used to reduce insomnia in older adults.
Materials and Methods
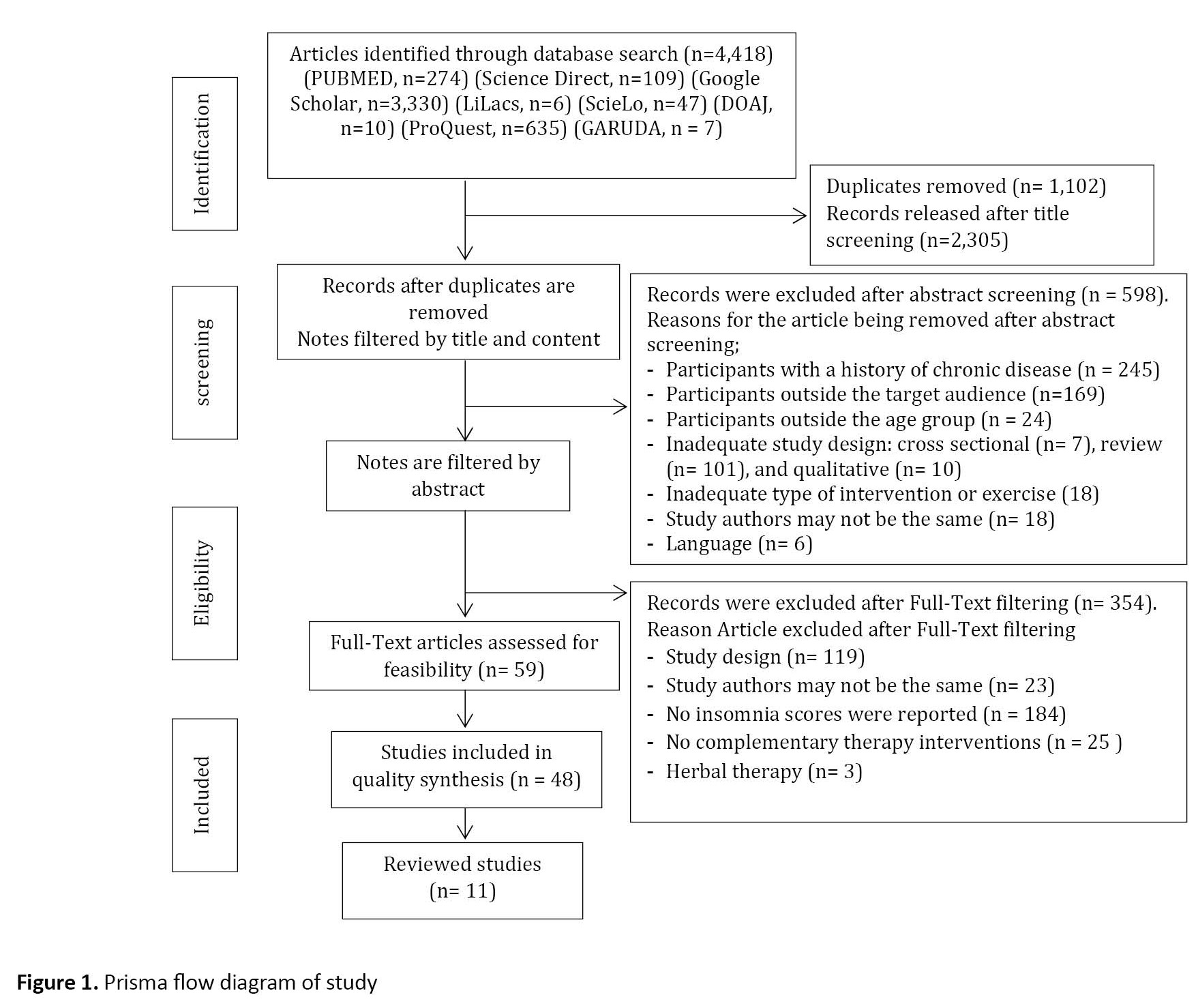
This systematic review was conducted according to PRISMA (the preferred reporting items for systematic reviews and meta-analyses). The study data were collected by searching indexed articles in databases and libraries, including PubMed, Science Direct, Google Scholar, Lilacs, SciELO, DOAJ, ProQuest, and GARUDA. To maximize the search, we hunted for articles discussing complementary therapies published between 2017 and 2022 for six years. Although there were too many studies, no one had explicitly discussed appropriate complementary therapies in dealing with insomnia in older adults. The keywords used to search for resources were selected from the MeSH database with controlled descriptors and selected boolean operators (AND/OR) to broaden the search: “Therapy” AND “insomnia” AND “elderly,” OR “sleep disorder” AND “therapy” AND “elderly.” The studies were eligible for inclusion when they looked at the effects of physical activity programs or, more specifically, exercise programs on the mental health of adults older than 60. To be included in this review, studies must meet the following criteria. First, the study population included older adults living in the community or in residential care centers aged over 60 years. In this review, older adults must be free from pre-existing major chronic diseases, such as cardiovascular disorders, cancer, and mental or psychiatric disorders. Second, the interventions or programs included complementary therapies or more specialized types of therapy (complementary therapies are categorized into five parts: Biological-based practice, mind-body techniques, manipulative and body-based practice, energy therapies, and ancient medical systems) [17]. Third, the study results should include complementary therapies that can ease insomnia in older adults. Fourth, the study design should include intervention studies, randomized controlled trials (RCTs), full-text articles, and research exploring complementary therapies for insomnia in older adults. Cross-sectional, qualitative studies, reviews, meta-analyses, and guidelines were excluded. Three researchers carried out the process of finding and selecting studies independently. The duplicates were removed after loading all notes from different databases in Endnote software, Version 8.1. Irrelevant articles were excluded based on “title” screening. The search strategy is reported in the PRISMA flowchart (Figure 1). Study quality was assessed using the standard EPHPP QAT (effective public health practice project quality assessment tool for quantitative studies) recommended by the Cochrane collaboration [18]. This tool consists of 8 items addressing data bias, study design, confounders, blinding, data collection methods, withdrawals and dropouts, intervention integrity, and analysis. When making judgments about each component, raters should base their opinion on information contained in the study rather than making inferences about what the authors intended. Each item is assessed and put in strong, moderate, and weak categories, each with a different explanation for the assessment and then a rating for all items. The total ratings for this instrument are strong (no weak ratings), moderate (one weak rating), or weak (two or more weak ratings), with both reviewers discussing the ratings [19].
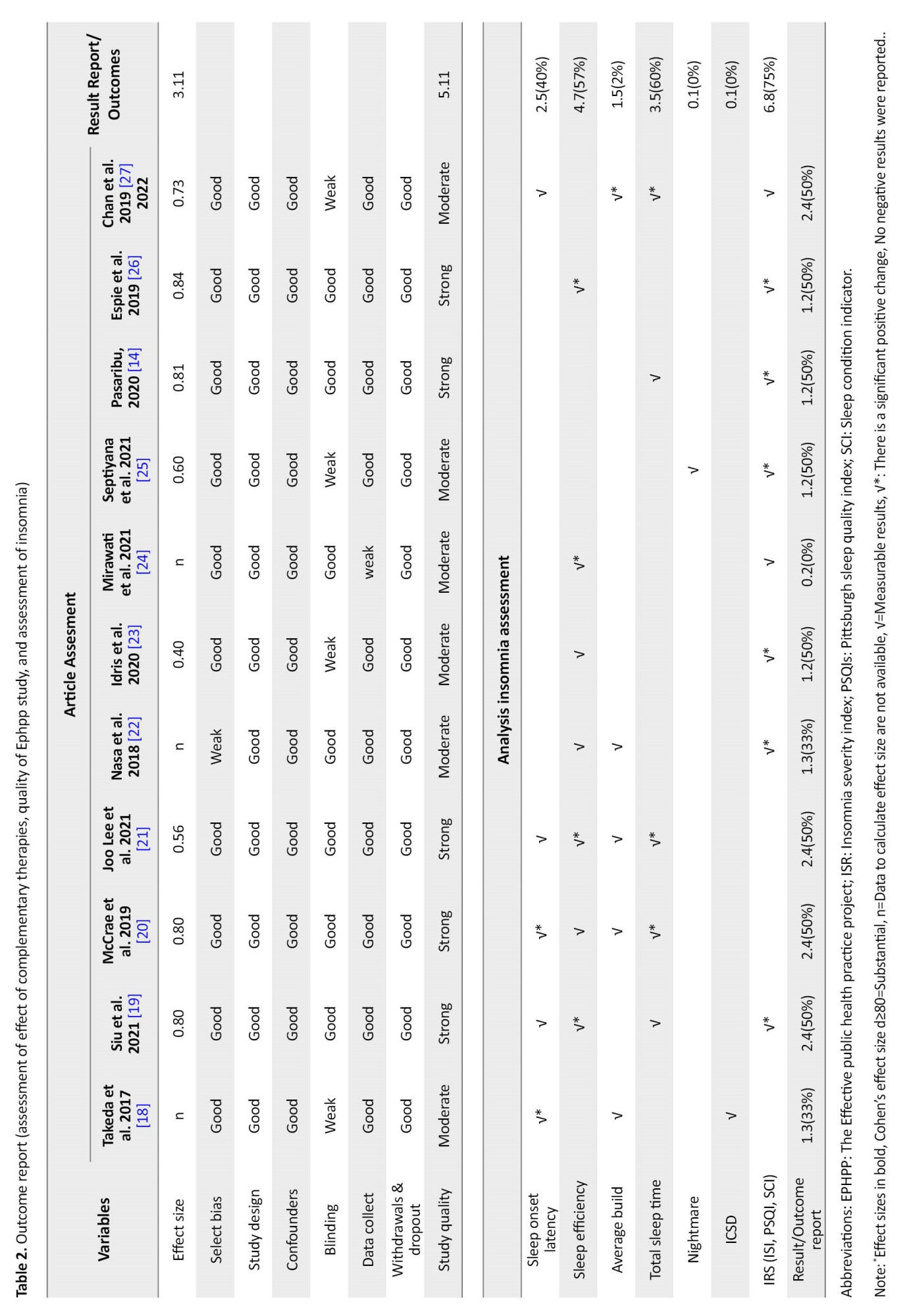
The details of the physical exercise and mental health programs for older adults are reported descriptively. Most of the assessment of insomnia is derived from insomnia instruments. Effect sizes were calculated for all studies that reported relevant data. A Cohen’s d≥0.80 indicates a significant effect size, and a P≤0.05 indicates a strong influence on the intervention.
Results
We analyzed 11 studies with a total sample of 2495 older people when 4418 potential studies were initially identified through an electronic database search. Most articles were excluded in this phase because the study population or design did not meet the eligibility criteria. Also, 598 articles were excluded after screening their “abstracts.” The most frequent reasons for exclusion in this phase were 1) The population did not meet the inclusion criteria, 2) The study design did not meet the inclusion criteria, and 3) No insomnia score. After reading the full text of the remaining 59 articles, they were excluded for the following reasons: 1) Being a cross-sectional study, 2) No peer-reviewed articles, 3) No insomnia score, 4) There was no complementary therapy intervention, and 5) Alluded to herbal therapy. Based on screening moderate and strong quality studies, 11 studies were included in this review. From this study, 6 were of ‘moderate’ quality, and 5 ‘strong’ quality of review (Table 1).
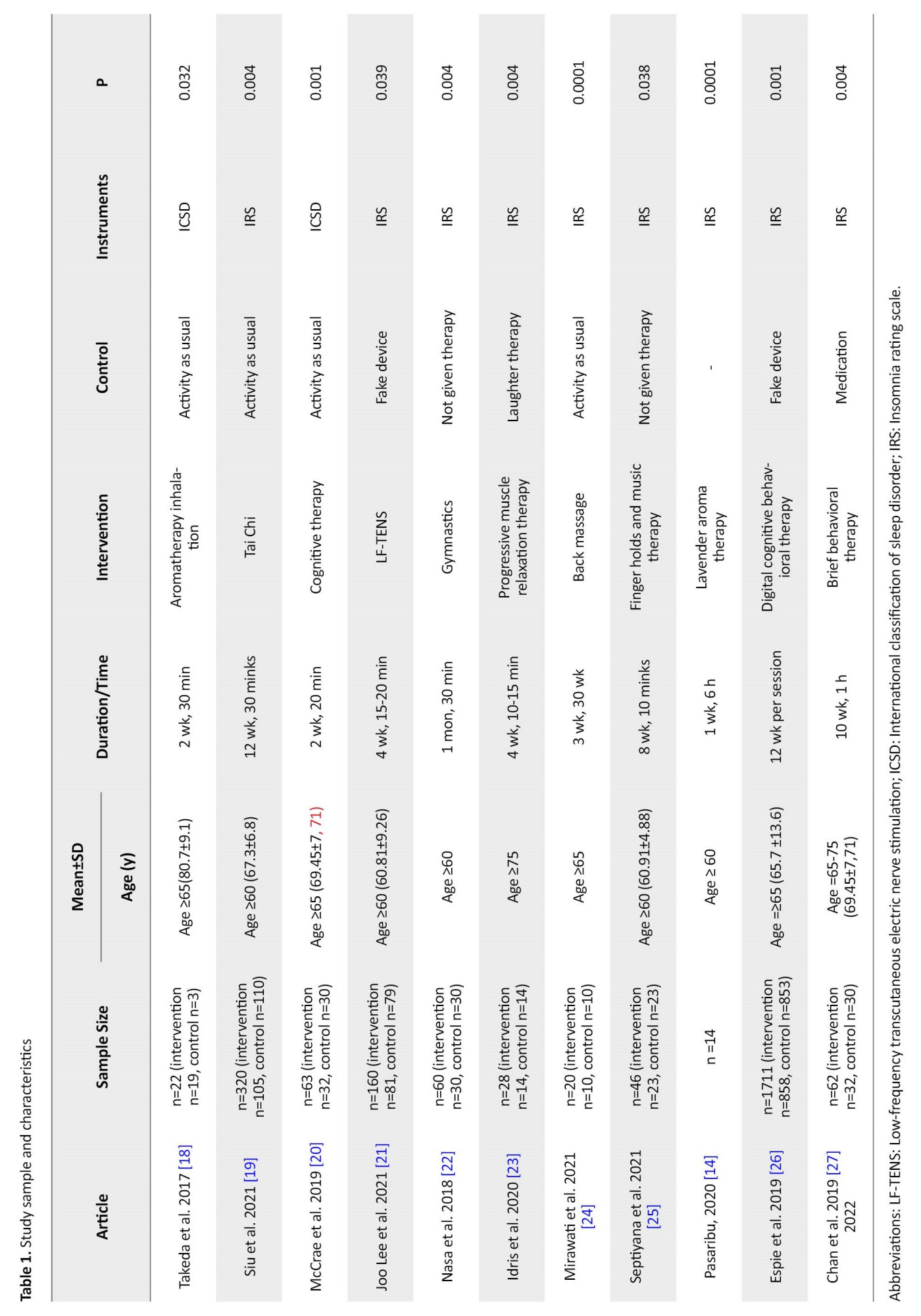
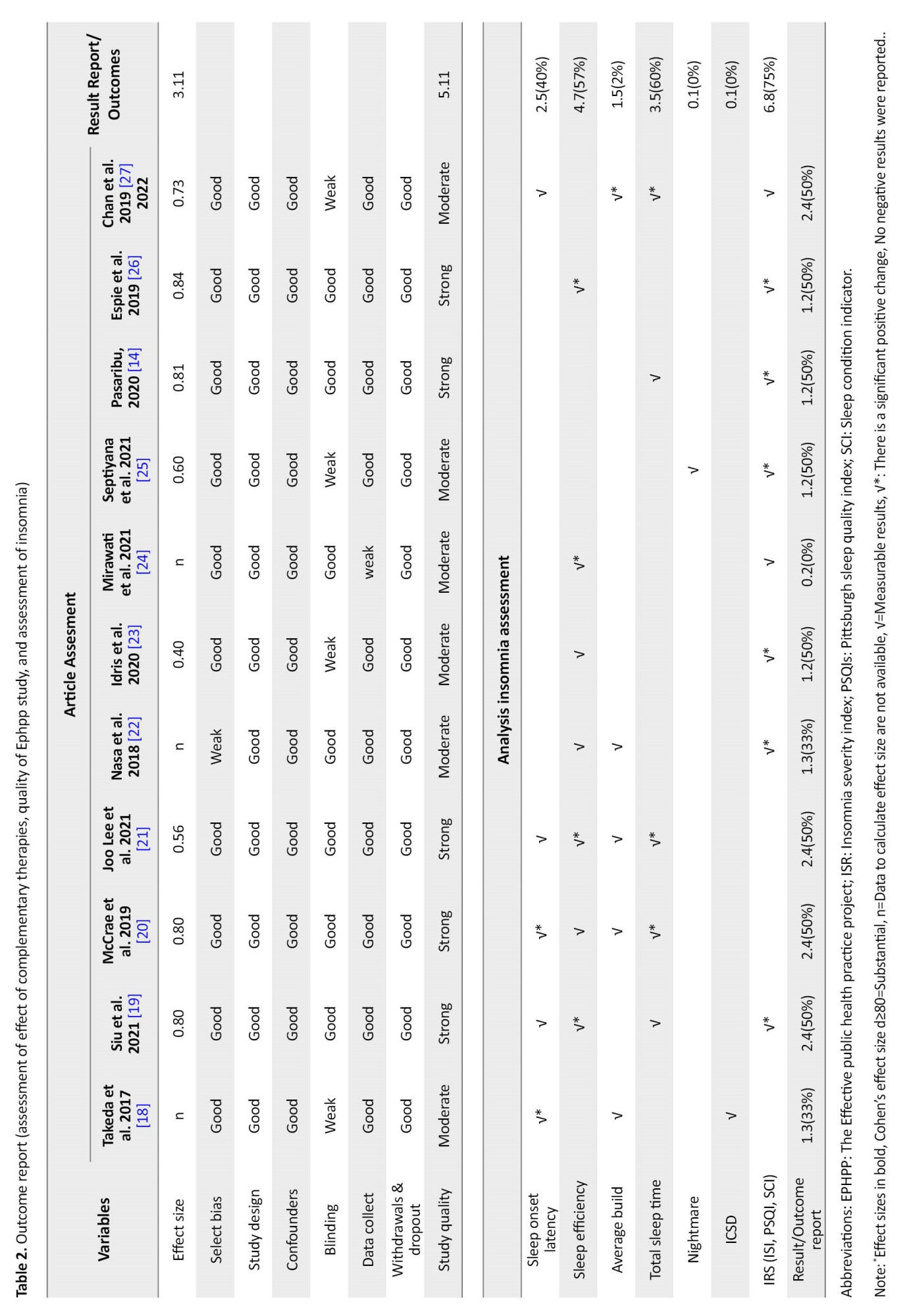
The design of the included studied comprised one pre-test-post-test and ten randomized controlled trials. Studies were conducted in Japan (n=1), China (n=3), the USA (n=2), and Indonesia (n=5). Sample sizes ranged from 12 to 1711 participants. The average age of the study samples ranged from 60 to 80 years. These 11 studies have explored aromatherapy inhalation [19], Tai Chi [20], cognitive therapy [21], low-frequency transcutaneous electric nerve stimulation (LF-TENS) [22], gymnastics [23], progressive muscle relaxation therapy [24], back massage [25], finger hold and music therapy [26], lavender aroma therapy [15], digital cognitive behavioral therapy [27], and brief behavioral therapy (28) with a P<0.05, indicating that all studies showed a positive effect on the elderly insomnia without adverse outcomes. After carrying out complementary therapy, which is shown based on the results of the insomnia questionnaire, namely (international classification of sleep disorder) ICSD and insomnia rating scale, 11 different insomnia digests were reported without significant adverse effects. It was found that there were 5 studies of strong quality [20-27] with 50% significant results on changing insomnia scores, and 6 were of moderate quality [26-28]. From strong quality studies, 5 have high effect sizes on interventions with Cohen’s d values ≥0.80, indicating a strong therapeutic effect on insomnia, and are recommended. These interventions were Tai Chi, cognitive therapy, lavender therapy, and digital cognitive therapy. Without adverse effects, the results of the insomnia score were found to be ≥50% significant positive changes: Sleep efficiency (57%), total sleep time (60%), and insomnia rating scale (IRS) score (75%) (Table 2).
Discussion
This study aimed to systematically review the literature on the complementary therapies commonly used to reduce insomnia in older adults. Eleven studies, including 10 RCTs and one pre-test-post-test study, were entered in this systematic review: 5 of strong and 6 of moderate quality describing the effects of the exercise program. Effect sizes were calculable and considered important out of the 5 studies because they produced significant results. However, although 4 RCTs in this review had a more robust methodological design than the one pretest-posttest study, they did not significantly differ in reported insomnia outcomes or significant effects.
The proportion between the effects of complementary therapy is reported to be higher in the 5 studies of strong quality compared to the 6 studies of moderate quality. This is evidenced by all high-quality studies reporting ≥50% positive results [15-20, 22-27]. In addition, 5 out of 11 high-quality studies reported strong effects of complementary therapies on older adults, while no studies with moderate quality ratings reported effect sizes that exceeded Cohen’s d≥0.80. Thus, more methodologically robust studies are more likely to report more significant effects and larger effect sizes. This finding aligns with research conducted by Hempel et al., which reported that the higher the quality of an article in proving the effectiveness of the intervention used, the greater the influence of the article in determining the size of a subject [29].
Based on the research results, 4 studies of complementary therapy were found to be appropriate in reducing insomnia in older adults, namely Tai Chi, cognitive therapy, lavender aroma, and digital cognitive therapy. They are high-quality studies with significant measurement results of ≥50%. This finding aligns with research conducted by Pitaloka et al. [5], which reports that Tai Chi is a sport encompassing meditation, breathing, and physical movement. Tai Chi increases the release of nor-adrenaline, lowers cortisol levels, and reduces sympathetic nerve activity, which stimulates melatonin release, causing a feeling of sleepiness in older adults. This finding is in accordance with research conducted by Siu et al. [20], who reported that Tai-chi could significantly reduce insomnia in older adults with a P=0.004 and Cohen’s d≥0.80.
In addition, other studies also report that aromatherapy of lavender flowers, which contains linalool, functions as a sedative effect so that when people inhale aromatherapy of lavender flowers, the aroma released will stimulate the neuron receptors of the olfactory nerve located in the olfactory epithelium to transmit the aroma to the bulb via the olfactory nerve. The positive impact of aromatherapy on the quality of sound sleep will be felt more directly (inhalation) because the nose has direct contact with the parts of the brain responsible for stimulating the formation of the effects of aromatherapy [30, 31]. This finding is in line with Pasaribu’s research [15], which states that the aroma of lavender significantly reduces insomnia in older adults.
From the results of this systematic study, it was also found that cognitive therapy, whether done manually or digitally, also positively impacted reducing elderly insomnia scores. According to the research, the cognitive therapy method can change cognitive distortion to produce new, more adaptive behaviors and relaxation skills, as well as an attempt to reduce feelings of anxiety, fear, and pressure that arise in each sufferer before bedtime because of thoughts that he would not be able to fall asleep like the nights before [31]. So, this finding is in line with the research of McCrae et al. and Espie et al., which reported that cognitive therapy significantly reduced insomnia in older adults [21, 27].
This study had some limitations. First, people who provide complementary therapy are nurses and physiotherapists for whom they have a license or training certificate. Second, the interventions used to measure insomnia do not focus on one tool. All of these things can result in a biased result, but the quality can be proven because the article has gone through the process of evaluating the article.
This systematic review shows that complementary therapies positively affect insomnia in older people who are both generally healthy but have experienced a variety of symptoms. Based on the results of this review, complementary therapies that are appropriate and highly recommendable in reducing the problem of elderly insomnia are Tai Chi, cognitive behavior therapy, lavender aroma, and digital cognitive therapy, which reported the highest number of significant effects on elderly insomnia. In addition, studies using the RCT design strengthen the results found to affect insomnia significantly.
Ethical Considerations
Compliance with ethical guidelines
The local Institutional Review Board deemed the study exempt from review, and informed consent was obtained from all individuals included in this study.
Funding
This study did not receive a specific grant from any funding agency, commercial, or non-profit sector.
Authors' Contributions
Conceptualization: Sitti Musdalifah Ahmad; Study design: Sitti Musdalifah Ahmad and Yuliana Syam; Data analysis and the initial draft preparation: All authors; Supervision and final approval: Yuliana Syam and Ariytanti Saleh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Universitas Hasanuddin Teaching Hospital for their support and Andi Masyitha Irwan who inspired them to improve the research.
References
Based on world population aging, the number of older people is increasing, more than 962 million each year [1, 2]. The Central Bureau of Statistics [3] estimates that the number of elderly aged 60 years and over will continue to increase until 2045 because of demographic transition [4]. This rising trend cannot be separated from the aging process, which causes a decline in health conditions; one of the most common complaints by older adults is sleep disturbances [5, 6]. Insomnia is a symptom in which older adults lack enough sleep, feel tired when they wake up, or frequently wake up at night. It is caused by degenerative processes in older people [7-9], which decreases neurotransmitter function by inhibiting melatonin production as a sleep hormone. This deficiency makes older people awake or experience sleep disturbances [9]. Thus, insomnia results from aging in older adults as a process of decreasing body function.
Insomnia in older adults will cause many health problems and, if left untreated, will impact their quality of life [10]. Thus, effective interventions are needed for dealing with the problem of insomnia in older adults. Complementary therapy is one of the best interventions because it is cheap, has many benefits, and lacks harmful side effects, especially in older adults [10]. Holistically, complementary therapy can stimulate the hypothalamus-pituitary-axis (HPA) mechanism to improve blood circulation, help metabolism work optimally, and relay neurotransmitters throughout the body, thereby reducing reactions to pain, stress, and depression—creating a feeling of relaxation that can make the elderly sleep soundly [12, 13]. Thus, complementary therapy is an appropriate intervention in reducing the problem of sleep disturbances in older adults and improving their quality of sleep.
Although there are many types of complementary therapies, such as massage, music therapy, relaxation techniques, acupuncture, and physical exercises recommended in nursing interventions, the problem of insomnia in older adults is still largely unnoticed [14-16]. In other words, no studies have examined the nature of complementary therapies to alleviate insomnia in older adults, only the quality of his sleep. Therefore, this systematic review examined the complementary therapies commonly used to reduce insomnia in older adults.
Materials and Methods
This systematic review was conducted according to PRISMA (the preferred reporting items for systematic reviews and meta-analyses). The study data were collected by searching indexed articles in databases and libraries, including PubMed, Science Direct, Google Scholar, Lilacs, SciELO, DOAJ, ProQuest, and GARUDA. To maximize the search, we hunted for articles discussing complementary therapies published between 2017 and 2022 for six years. Although there were too many studies, no one had explicitly discussed appropriate complementary therapies in dealing with insomnia in older adults. The keywords used to search for resources were selected from the MeSH database with controlled descriptors and selected boolean operators (AND/OR) to broaden the search: “Therapy” AND “insomnia” AND “elderly,” OR “sleep disorder” AND “therapy” AND “elderly.” The studies were eligible for inclusion when they looked at the effects of physical activity programs or, more specifically, exercise programs on the mental health of adults older than 60. To be included in this review, studies must meet the following criteria. First, the study population included older adults living in the community or in residential care centers aged over 60 years. In this review, older adults must be free from pre-existing major chronic diseases, such as cardiovascular disorders, cancer, and mental or psychiatric disorders. Second, the interventions or programs included complementary therapies or more specialized types of therapy (complementary therapies are categorized into five parts: Biological-based practice, mind-body techniques, manipulative and body-based practice, energy therapies, and ancient medical systems) [17]. Third, the study results should include complementary therapies that can ease insomnia in older adults. Fourth, the study design should include intervention studies, randomized controlled trials (RCTs), full-text articles, and research exploring complementary therapies for insomnia in older adults. Cross-sectional, qualitative studies, reviews, meta-analyses, and guidelines were excluded. Three researchers carried out the process of finding and selecting studies independently. The duplicates were removed after loading all notes from different databases in Endnote software, Version 8.1. Irrelevant articles were excluded based on “title” screening. The search strategy is reported in the PRISMA flowchart (Figure 1). Study quality was assessed using the standard EPHPP QAT (effective public health practice project quality assessment tool for quantitative studies) recommended by the Cochrane collaboration [18]. This tool consists of 8 items addressing data bias, study design, confounders, blinding, data collection methods, withdrawals and dropouts, intervention integrity, and analysis. When making judgments about each component, raters should base their opinion on information contained in the study rather than making inferences about what the authors intended. Each item is assessed and put in strong, moderate, and weak categories, each with a different explanation for the assessment and then a rating for all items. The total ratings for this instrument are strong (no weak ratings), moderate (one weak rating), or weak (two or more weak ratings), with both reviewers discussing the ratings [19].
The details of the physical exercise and mental health programs for older adults are reported descriptively. Most of the assessment of insomnia is derived from insomnia instruments. Effect sizes were calculated for all studies that reported relevant data. A Cohen’s d≥0.80 indicates a significant effect size, and a P≤0.05 indicates a strong influence on the intervention.
Results
We analyzed 11 studies with a total sample of 2495 older people when 4418 potential studies were initially identified through an electronic database search. Most articles were excluded in this phase because the study population or design did not meet the eligibility criteria. Also, 598 articles were excluded after screening their “abstracts.” The most frequent reasons for exclusion in this phase were 1) The population did not meet the inclusion criteria, 2) The study design did not meet the inclusion criteria, and 3) No insomnia score. After reading the full text of the remaining 59 articles, they were excluded for the following reasons: 1) Being a cross-sectional study, 2) No peer-reviewed articles, 3) No insomnia score, 4) There was no complementary therapy intervention, and 5) Alluded to herbal therapy. Based on screening moderate and strong quality studies, 11 studies were included in this review. From this study, 6 were of ‘moderate’ quality, and 5 ‘strong’ quality of review (Table 1).
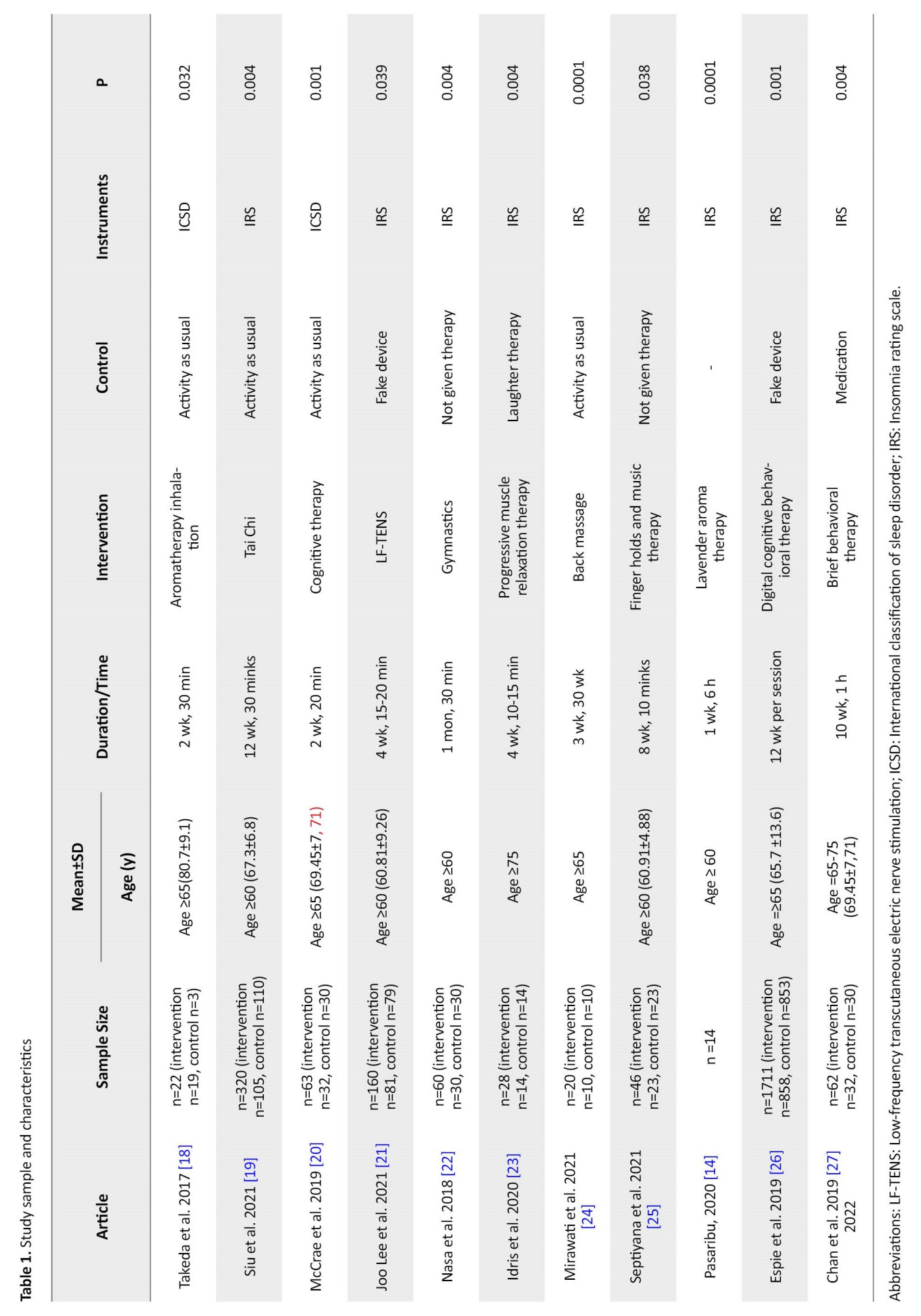
The design of the included studied comprised one pre-test-post-test and ten randomized controlled trials. Studies were conducted in Japan (n=1), China (n=3), the USA (n=2), and Indonesia (n=5). Sample sizes ranged from 12 to 1711 participants. The average age of the study samples ranged from 60 to 80 years. These 11 studies have explored aromatherapy inhalation [19], Tai Chi [20], cognitive therapy [21], low-frequency transcutaneous electric nerve stimulation (LF-TENS) [22], gymnastics [23], progressive muscle relaxation therapy [24], back massage [25], finger hold and music therapy [26], lavender aroma therapy [15], digital cognitive behavioral therapy [27], and brief behavioral therapy (28) with a P<0.05, indicating that all studies showed a positive effect on the elderly insomnia without adverse outcomes. After carrying out complementary therapy, which is shown based on the results of the insomnia questionnaire, namely (international classification of sleep disorder) ICSD and insomnia rating scale, 11 different insomnia digests were reported without significant adverse effects. It was found that there were 5 studies of strong quality [20-27] with 50% significant results on changing insomnia scores, and 6 were of moderate quality [26-28]. From strong quality studies, 5 have high effect sizes on interventions with Cohen’s d values ≥0.80, indicating a strong therapeutic effect on insomnia, and are recommended. These interventions were Tai Chi, cognitive therapy, lavender therapy, and digital cognitive therapy. Without adverse effects, the results of the insomnia score were found to be ≥50% significant positive changes: Sleep efficiency (57%), total sleep time (60%), and insomnia rating scale (IRS) score (75%) (Table 2).
Discussion
This study aimed to systematically review the literature on the complementary therapies commonly used to reduce insomnia in older adults. Eleven studies, including 10 RCTs and one pre-test-post-test study, were entered in this systematic review: 5 of strong and 6 of moderate quality describing the effects of the exercise program. Effect sizes were calculable and considered important out of the 5 studies because they produced significant results. However, although 4 RCTs in this review had a more robust methodological design than the one pretest-posttest study, they did not significantly differ in reported insomnia outcomes or significant effects.
The proportion between the effects of complementary therapy is reported to be higher in the 5 studies of strong quality compared to the 6 studies of moderate quality. This is evidenced by all high-quality studies reporting ≥50% positive results [15-20, 22-27]. In addition, 5 out of 11 high-quality studies reported strong effects of complementary therapies on older adults, while no studies with moderate quality ratings reported effect sizes that exceeded Cohen’s d≥0.80. Thus, more methodologically robust studies are more likely to report more significant effects and larger effect sizes. This finding aligns with research conducted by Hempel et al., which reported that the higher the quality of an article in proving the effectiveness of the intervention used, the greater the influence of the article in determining the size of a subject [29].
Based on the research results, 4 studies of complementary therapy were found to be appropriate in reducing insomnia in older adults, namely Tai Chi, cognitive therapy, lavender aroma, and digital cognitive therapy. They are high-quality studies with significant measurement results of ≥50%. This finding aligns with research conducted by Pitaloka et al. [5], which reports that Tai Chi is a sport encompassing meditation, breathing, and physical movement. Tai Chi increases the release of nor-adrenaline, lowers cortisol levels, and reduces sympathetic nerve activity, which stimulates melatonin release, causing a feeling of sleepiness in older adults. This finding is in accordance with research conducted by Siu et al. [20], who reported that Tai-chi could significantly reduce insomnia in older adults with a P=0.004 and Cohen’s d≥0.80.
In addition, other studies also report that aromatherapy of lavender flowers, which contains linalool, functions as a sedative effect so that when people inhale aromatherapy of lavender flowers, the aroma released will stimulate the neuron receptors of the olfactory nerve located in the olfactory epithelium to transmit the aroma to the bulb via the olfactory nerve. The positive impact of aromatherapy on the quality of sound sleep will be felt more directly (inhalation) because the nose has direct contact with the parts of the brain responsible for stimulating the formation of the effects of aromatherapy [30, 31]. This finding is in line with Pasaribu’s research [15], which states that the aroma of lavender significantly reduces insomnia in older adults.
From the results of this systematic study, it was also found that cognitive therapy, whether done manually or digitally, also positively impacted reducing elderly insomnia scores. According to the research, the cognitive therapy method can change cognitive distortion to produce new, more adaptive behaviors and relaxation skills, as well as an attempt to reduce feelings of anxiety, fear, and pressure that arise in each sufferer before bedtime because of thoughts that he would not be able to fall asleep like the nights before [31]. So, this finding is in line with the research of McCrae et al. and Espie et al., which reported that cognitive therapy significantly reduced insomnia in older adults [21, 27].
This study had some limitations. First, people who provide complementary therapy are nurses and physiotherapists for whom they have a license or training certificate. Second, the interventions used to measure insomnia do not focus on one tool. All of these things can result in a biased result, but the quality can be proven because the article has gone through the process of evaluating the article.
This systematic review shows that complementary therapies positively affect insomnia in older people who are both generally healthy but have experienced a variety of symptoms. Based on the results of this review, complementary therapies that are appropriate and highly recommendable in reducing the problem of elderly insomnia are Tai Chi, cognitive behavior therapy, lavender aroma, and digital cognitive therapy, which reported the highest number of significant effects on elderly insomnia. In addition, studies using the RCT design strengthen the results found to affect insomnia significantly.
Ethical Considerations
Compliance with ethical guidelines
The local Institutional Review Board deemed the study exempt from review, and informed consent was obtained from all individuals included in this study.
Funding
This study did not receive a specific grant from any funding agency, commercial, or non-profit sector.
Authors' Contributions
Conceptualization: Sitti Musdalifah Ahmad; Study design: Sitti Musdalifah Ahmad and Yuliana Syam; Data analysis and the initial draft preparation: All authors; Supervision and final approval: Yuliana Syam and Ariytanti Saleh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Universitas Hasanuddin Teaching Hospital for their support and Andi Masyitha Irwan who inspired them to improve the research.
References
- United Nations. World population ageing. New York: United Nations; 2019
- Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020; 139:6-11. [DOI:10.1016/j.maturitas.2020.05.018] [PMID]
- Bayu D. The proportion of elderly population is expected to continue to increase through 2045 [Internet]. 2022 [Updated December 21, 2022].
- Pitaloka D, Siswi D, Firranda F. Exercise improved sleep quality in the elderly. proceeding 8th International Nursing Conference “Education, Practice and Research Development In Nursing. 2020; 127-31. [Link]
- Gehrman P, Ancoli S. Insomnia in the elderly. Insomnia Diagnosis Treat. 2020; 224-34.
- Patel D, Steinberg J, Patel P. Insomnia in the elderly: A review. J Clin Sleep Med. 2018; 14(6):1017-24. [DOI:10.5664/jcsm.7172] [PMID]
- de Zambotti M, Goldstone A, Colrain IM, Baker FC. Insomnia disorder in adolescence: Diagnosis, impact, and treatment. Sleep Med Rev. 2020; 39:12-24. [DOI:10.1016/j.smrv.2017.06.009] [PMID]
- Dopheide JA. Insomnia overview: Epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy. Am J Manag Care. 2020; 26(4 Suppl):S76-84. [DOI:10.37765/ajmc.2020.42769] [PMID]
- Okamoto R, Mizukami K. [The effective of facial exercises on the mental health in elderly adults (Japanese)]. Nihon Ronen Igakkai Zasshi. 2018; 55(1):74-80. [DOI:10.3143/geriatrics.55.74] [PMID]
- Hamlin AS, Robertson TM. Pain and complementary therapies. Crit Care Nurs Clin North Am. 2017; 29(4):449-60. [DOI:10.1016/j.cnc.2017.08.005] [PMID]
- Haller H, Anheyer D, Cramer H, Dobos G. Complementary therapies for clinical depression: An overview of systematic reviews. BMJ Open. 2019; 9(8):e028527. [DOI:10.1136/bmjopen-2018-028527] [PMID]
- Johnson A, Roberts L, Elkins G. Complementary and alternative medicine for menopause. J Evid Based Integr Med. 2019; 24:2515690X19829380. [DOI:10.1177/2515690X19829380] [PMID]
- Hmwe NTT, Browne G, Mollart L, Allanson V, Chan SW. Acupressure to improve sleep quality of older people in residential aged care: A randomised controlled trial protocol. Trials. 2020; 21(1):360.[DOI:10.1186/s13063-020-04286-2] [PMID]
- Pasaribu M. The effect of lavender aroma complementary therapy on insomnia in the elderly at Joyah Uken Takengon Nursing Home. Sci Midwifery. 2020; 9(1):144-7. [Link]
- Batara GR, Maramis WF, Erikavitri E. Gymnastic frequency and insomnia level in elderly at Bhakti Luhur Nursing Home Tropodo. J Widya Med J. 2019; 1(4):221-7. [Link]
- Verma K, Singh D, Srivastava A. The impact of complementary and alternative medicine on insomnia: A systematic review. Cureus. 2022; 14(8):e28425. [PMID]
- Effective Public Healthcare Panacea Project. Quality assessment tool for quantitative studies [Internet]. 2022 [Updated 2022 Jun 11]. Available from: [Link]
- Takeda A, Watanuki E, Koyama S. Effects of Inhalation aromatherapy on symptoms of sleep disturbance in the elderly with dementia. Evidence-based Complement Altern Med. 2017; 2017:1902807. [DOI:10.1155/2017/1902807] [PMID]
- Siu PM, Yu AP, Tam BT, Chin EC, Yu DS, Chung KF, et al. Effects of Tai Chi or exercise on sleep in older adults with insomnia: A randomized clinical trial. JAMA Netw open. 2021; 4(2):e2037199. [DOI:10.1001/jamanetworkopen.2020.37199] [PMID]
- McCrae CS, Curtis AF, Williams JM, Dautovich ND, McNamara JPH, Stripling A, et al. Efficacy of brief behavioral treatment for insomnia in older adults: Examination of sleep, mood, and cognitive outcomes Sleep Med. 2018; 51:153-66. [DOI:10.1016/j.sleep.2018.05.018] [PMID]
- Joo Lee H, Hong JK, Choi H, Chung S, Yoon IY. Modest therapeutic effects of low-frequency transcutaneous electric nerve stimulation on insomnia among older adults : A 4-week multi-center, randomized controlled study. 2021; 1-24. [Unpublished] [DOI:10.21203/rs.3.rs-363345/v1]
- Nasa FN, Gondodiputro S, Rahmiati L. Relationship between gymnastics exercise and insomnia in elderly. Int J Integr Health Sci. 2018; 6(1):30-45. [DOI:10.15850/ijihs.v6n1.1132]
- Idris DNT, Astarani K, Mahanani S. The comparison between the effectiveness of laughter therapy and progressive muscle relaxation therapy towards insomnia in elderly community at St. Yoseph Kediri Nursing Home. Indian J Public Health. 2020; 11(9):218-25. [DOI:10.37506/ijphrd.v11i9.11012]
- Mirawati D, Izhar J, Oktivani LS, Wahyuni, Putra YW. The effect of back massage on decreasing insomnia in the elderly at the Posyandu Lansia Marsudi Waras Jebres Surakarta. Gaster J Heal Sci. 2021; 19(1):20-30. [Link]
- Septiyana AN, Priyanto S, Priyo P, Ediyono S. The effect of finger hold and music therapy to insomnia in elderly. Proceedings of the 2nd Borobudur International Symposium on Humanities and Social Sciences, BIS-HSS 2020, 18 November 2020, Magelang, Central Java, Indonesia. [DOI:10.4108/eai.18-11-2020.2311643]
- Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, et al. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: A randomized clinical trial. JAMA Psychiatry. 2019; 76(1):21-30.[DOI:10.1001/jamapsychiatry.2018.2745] [PMID]
- Chan WS, Dautovich ND, McNamara JPH, Stripling A, Dzierzewski JM, McCoy K, et al. Sleep discrepancy in a randomized controlled trial of brief behavioral therapy for chronic insomnia in older adults. Behav Sleep Med. 2021; 19(2):221-31. [DOI:10.1080/15402002.2020.1726750] [PMID]
- Brewster GS, Riegel B, Gehrman PR. Insomnia in the older adult. Sleep Med Clin. 2018; 13(1):13-9. [PMID]
- Mindayani S, Yardi FR, Putri AL, Fadilla N. Efektivitas aroma terapi lavender terhadap insomnia pada lansia. J Ris Hesti Medan Akper Kesdam I/BB Medan. 2021; 6(1):63-8. [Link]
- Siagian HS. Pengaruh aromaterapi lavender terhadap penurunan insomnia pada usia lanju. J Pharm Sci Med Res. 2020; 3(1):35-42. [Link]
- Hapsari A, Kurniawan A. Efektivitas cognitive behavior therapy (CBT) untuk meningkatkan kualitas tidur penderita gejala insomnia usia dewasa awal. J Ilmu Kel dan Konsum. 2019; 12(3):223-35. [Link]
Article Type : Research |
Subject:
General
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |