Sat, Apr 27, 2024
Volume 34, Issue 2 (2-2024)
JHNM 2024, 34(2): 133-142 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Naghdipour Mirsadeghi M, Rafiei Sorouri Z, Mansour Ghanaie M, Hosseinzadeh F, Farzadi S, Biazar G et al . Not-prescribed Use of Herbal Products and Supplements Among Pregnant Women. JHNM 2024; 34 (2) :133-142
URL: http://hnmj.gums.ac.ir/article-1-2305-en.html
URL: http://hnmj.gums.ac.ir/article-1-2305-en.html
Misa Naghdipour Mirsadeghi1 

 , Zahra Rafiei Sorouri1
, Zahra Rafiei Sorouri1 

 , Mandana Mansour Ghanaie2
, Mandana Mansour Ghanaie2 

 , Fatemeh Hosseinzadeh1
, Fatemeh Hosseinzadeh1 

 , Sara Farzadi1
, Sara Farzadi1 

 , Gelareh Biazar *
, Gelareh Biazar * 

 3, Seyed Mohamadreza Tabatabaei Taher4
3, Seyed Mohamadreza Tabatabaei Taher4 




 , Zahra Rafiei Sorouri1
, Zahra Rafiei Sorouri1 

 , Mandana Mansour Ghanaie2
, Mandana Mansour Ghanaie2 

 , Fatemeh Hosseinzadeh1
, Fatemeh Hosseinzadeh1 

 , Sara Farzadi1
, Sara Farzadi1 

 , Gelareh Biazar *
, Gelareh Biazar * 

 3, Seyed Mohamadreza Tabatabaei Taher4
3, Seyed Mohamadreza Tabatabaei Taher4 


1- Assistant Professor, Reproductive Health Research Center, Department of Obstetrics & Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Associate Professor, Reproductive Health Research Center, Department of Obstetrics and Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
3- Associate Professor, Anesthesiology Research Center, Department of Anesthesiology, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran. , gelarehbiazar1386@gmail.com
4- MD Student of Medicine, Student Research Committee, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Associate Professor, Reproductive Health Research Center, Department of Obstetrics and Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
3- Associate Professor, Anesthesiology Research Center, Department of Anesthesiology, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran. , gelarehbiazar1386@gmail.com
4- MD Student of Medicine, Student Research Committee, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 518 kb]
(82 Downloads)
| Abstract (HTML) (154 Views)
Full-Text: (35 Views)
Introduction
Not-prescribed use (NPU) of complementary supplements and herbal medicine during pregnancy has been increasing over the past two decades. Studies have demonstrated that the prevalence of herbal use during pregnancy ranges from 1% to 60% in different societies [1]. Several studies have shown that middle-aged white people with higher levels of education and better economic status tend to use supplementations more than others [2]. Regarding supplements during pregnancy, the use of the necessary and recommended ones by physicians, such as acid folic, is essential, while NPU of them could be harmful [3, 4, 5]. Today, herbal and complementary supplements with different properties, especially for pregnant women, are readily available at local herb markets and pharmacies and sold at a lower cost. Some factors justify their higher use among pregnant women; pregnancy is associated with several complications such as nausea and vomiting, constipation, and fatigue that sometimes are not sufficiently treated by conventional medical treatments. In addition, pregnant women prefer to relieve their symptoms with these natural components, which are presumed safer compared to industrial drugs [6, 7, 8]. However, due to the passage of active ingredients of the herbs through the placental barrier and reaching the fetus, the safety of herbal products during pregnancy is debatable [9]. According to a recent systematic review, the use of herbal medicinal products during pregnancy should be avoided until strong evidence of safety is available [10]. NPU of herbal products or supplements during pregnancy is also a challenge for anesthesiologists. Some pregnant women are candidates for cesarean section due to obstetrics indications, and some should receive general anesthesia in certain conditions despite several disadvantages of regional anesthesia [11, 12].
In this regard, dietary supplements, vitamins, or herbs could significantly interfere with the anesthetic drugs. Hemodynamic fluctuations, nausea and vomiting, altered drug metabolism, intraoperative arrhythmias, hypoglycemia, allergic reactions, increased bleeding, increased sedative effects of anesthetics, and cardiovascular instability may occur. Therefore, it is necessary to discontinue them at a certain time before operation [13]. In general, if the type of supplementation or herbs is unknown, it is recommended to stop them at least two weeks before delivery [14]. The consumption status of herbs and supplements is affected by the regions, ethnic backgrounds, cultures, and demographics [15]. Therefore, a better understanding of the conditions in each area seems vital to help improve mother-infant health programs and policies. The frequency of consumption of herbal products was investigated [16], which was valuable in this field. However, it had many defects, and the main problem was the non-prescribed consumption of the herbs, and the status of receiving supplements was not investigated. Therefore, this study aimed to examine the pattern of arbitrary consumption of herbal products and supplements among pregnant women.
Materials and Methods
This analytical cross-sectional study was conducted on pregnant women who were referred to an academic center affiliated with Guilan University of Medical Sciences (GUMS) for vaginal or cesarean delivery in 2022. The center performs 3500 to 4000 deliveries annually. According to the inclusion criteria, 682 mothers entered this study.
The inclusion criteria were women with term pregnancy admitted to an academic referral center in Rasht City for delivery, living in Guilan Province, being able to communicate, and having a stable hemodynamic status. The exclusion criteria were women who did not give informed consent for any reason and referal pregnant women as they might have different traditions in the consumption of herbal components or supplements.
A researcher-made questionnaire containing questions about maternal demographic data (age, education, residency, and occupational status) and the maternal pattern of herbs and supplements used during pregnancy was used. The questionnaire items were presented to 10 Obstetrics and Anesthesiology Department faculty members, and they confirmed its validity. The reliability of the questionnaire was not assessed due to the type of questions. All questions were answered by “yes” or “no.” At the beginning of the interview, enough information about the study was provided to all 682 eligible mothers, and an herbal compound was described as any remedy product from herbs to prevent or cure illness or achieve better health [10]. Then, their written consent was obtained. A medical student filled out the questionnaire through a direct interview on the day after delivery.
The face-to-face interview was chosen because it would provide more comprehensive and reliable information than a self-administered questionnaire.
The collected data were entered into and analyzed using the SPSS software, version 21. Percentages and frequencies were used to express different variables. The chi-square and Mann-Whitney U tests were performed to analyze the data. Multivariate logistic regression analysis determined factors associated with herbal products and supplemental use. Odds ratio (OR) with a 95% confidence interval (CI) were also calculated. A P<0.05 was considered statistically significant.
Results
A total of 710 women were interviewed, with a response rate of 96.3% (28 refused to participate). The data from 682 participants, with a mean age of 28.01±5.33 (18-42) years, were analyzed. A total of 488 women (71.6%) were less or equal to 30 years old, 498(73%) lived in urban areas, 508(74.5%) were homemakers, 444(65.1%) had under diploma or diploma grades, 292(42.8%) were gravid one and 251(36.8%) gravid two. Also, 49 participants (7.2%) reported no consumption of herbal products or supplements, and 121(17.7%) used both herbal products and supplements during pregnancy. In addition, 614(90%) took supplements and 140(20.5%) used herbal products during pregnancy. About 93.6% used herbal products without healthcare professionals’ supervision (Table 1).
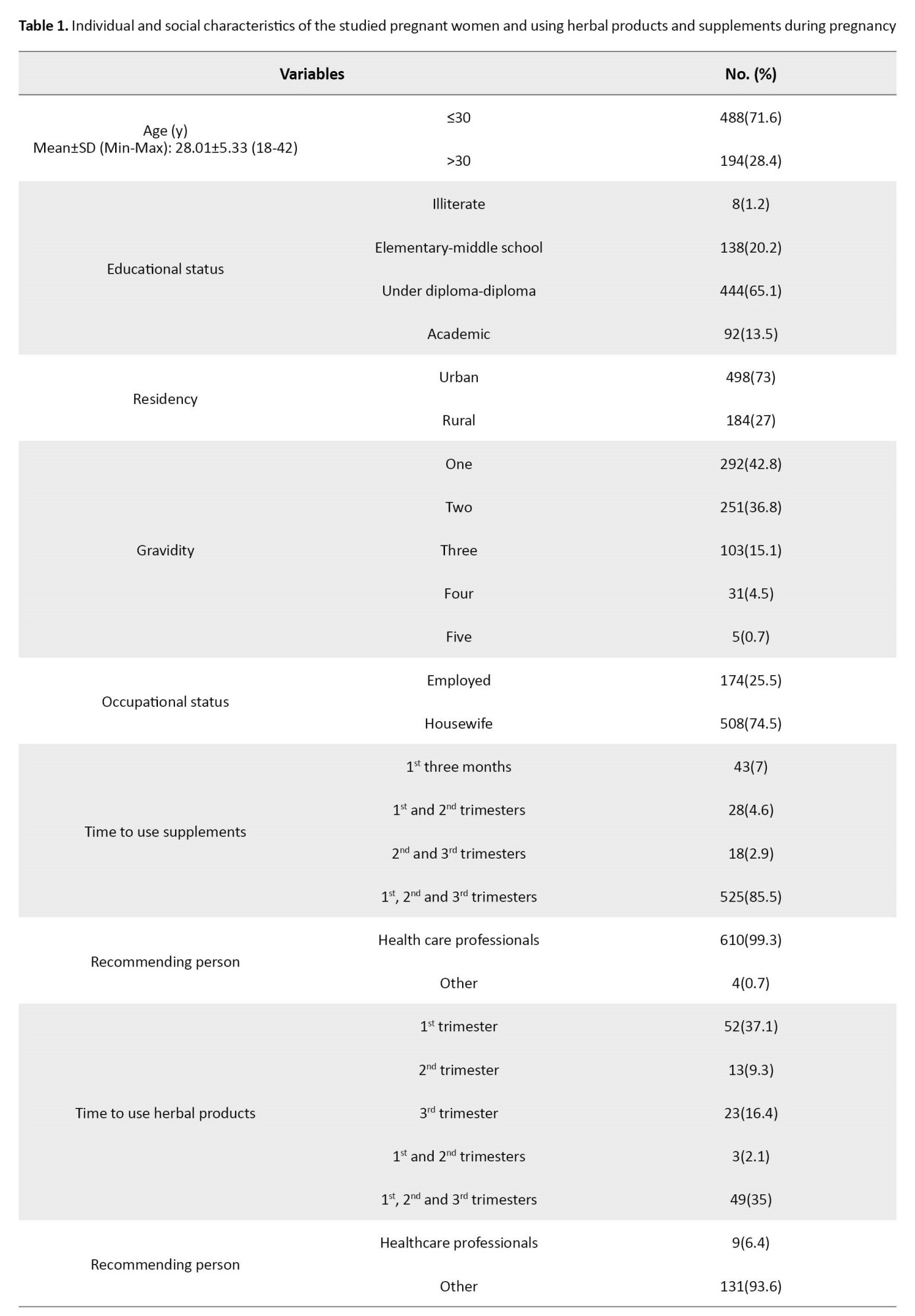
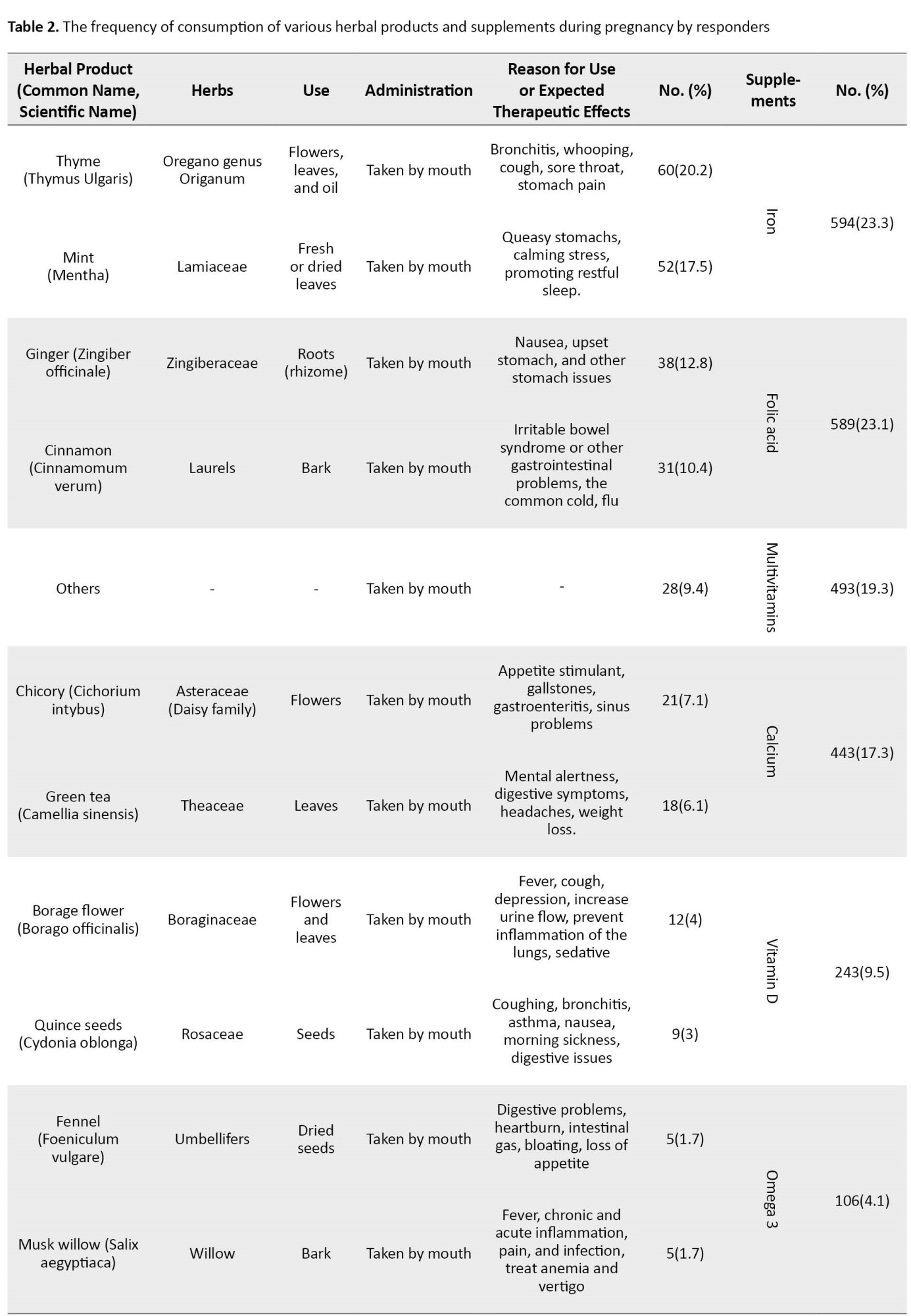
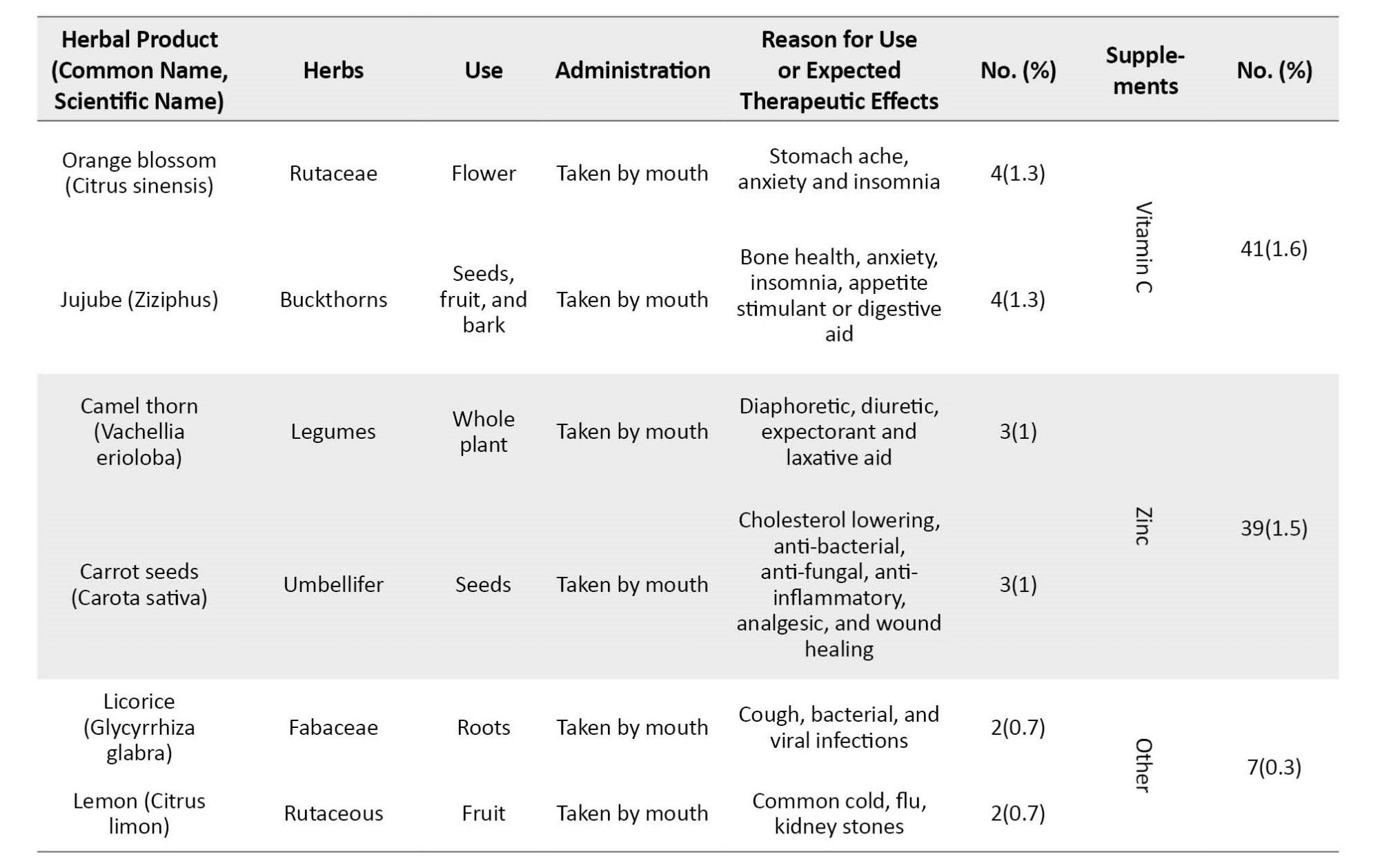
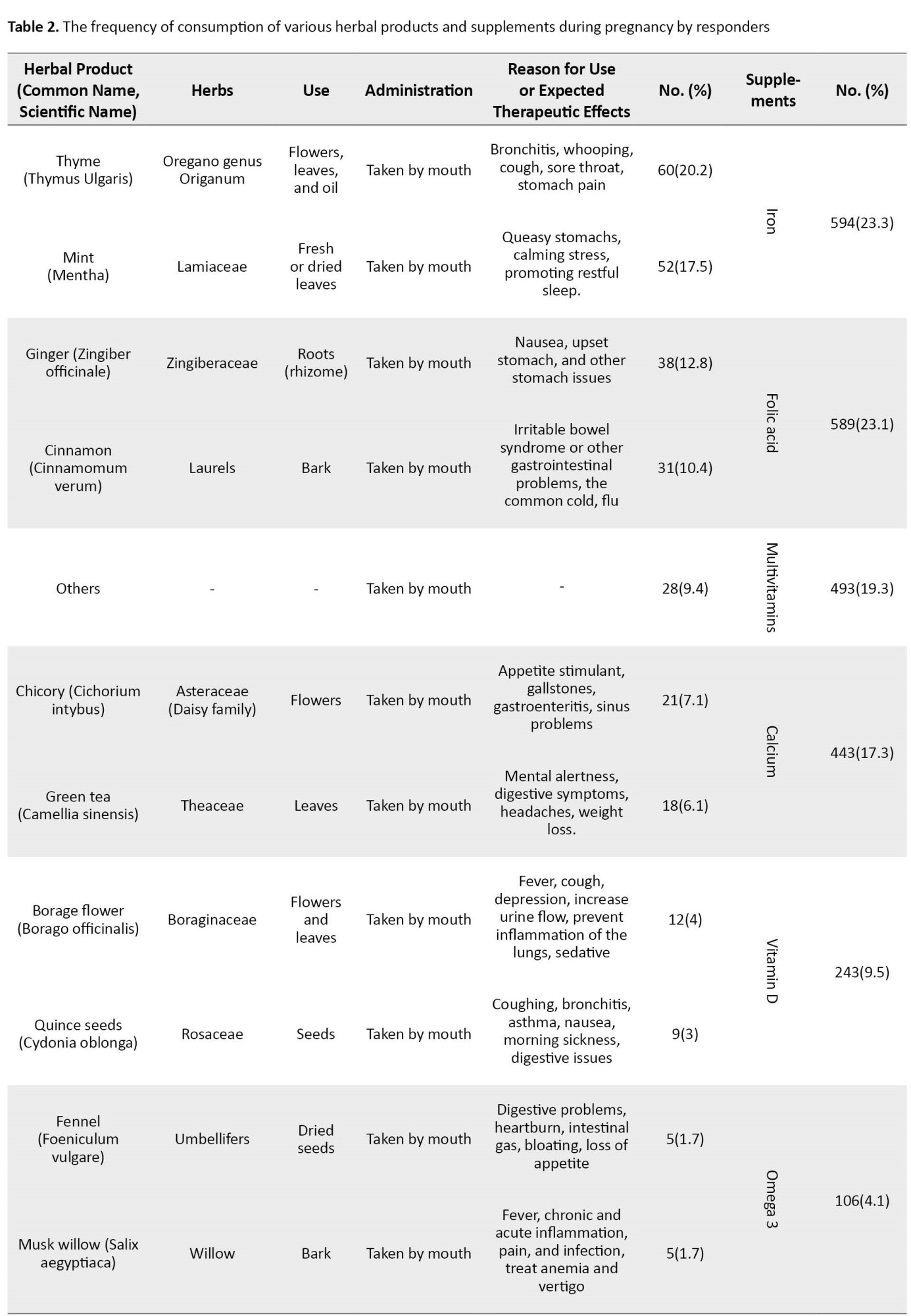
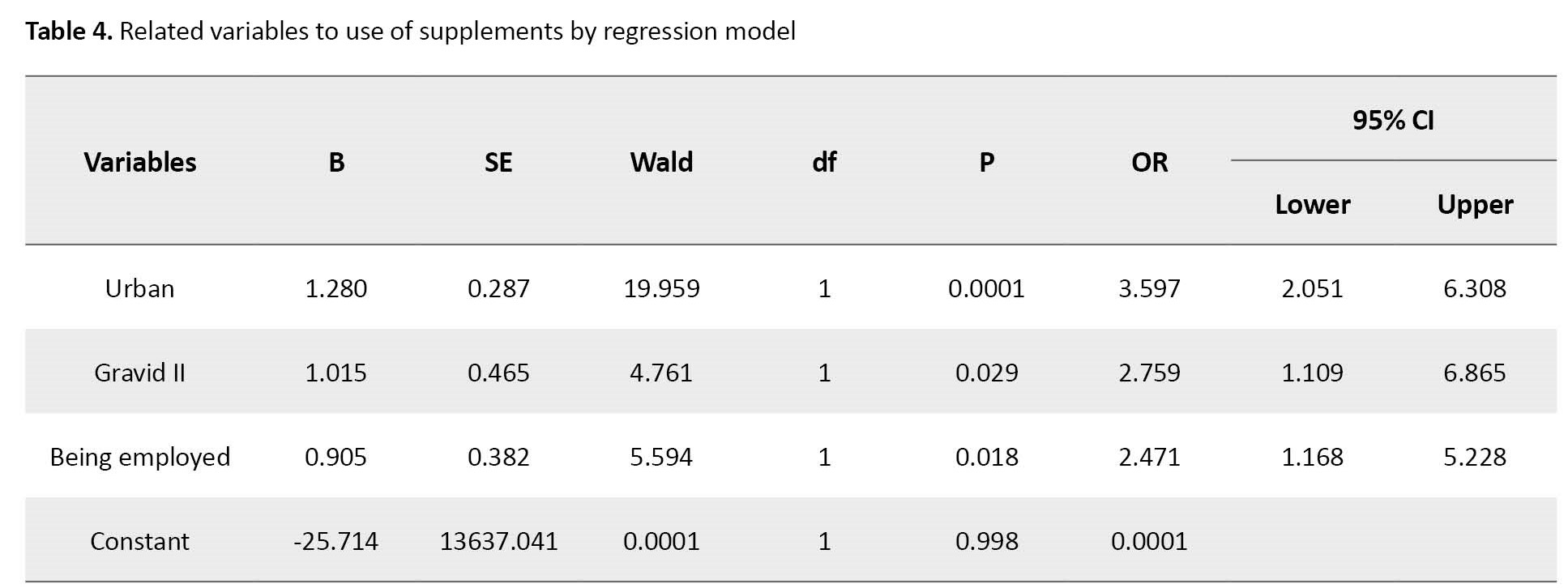
Iron (23.3%) and folic acid (23.1%) were the most frequent ones in supplements, and thyme (20.2%) and mint (17.5%) were the most taken herbs among pregnant women (Table 2).
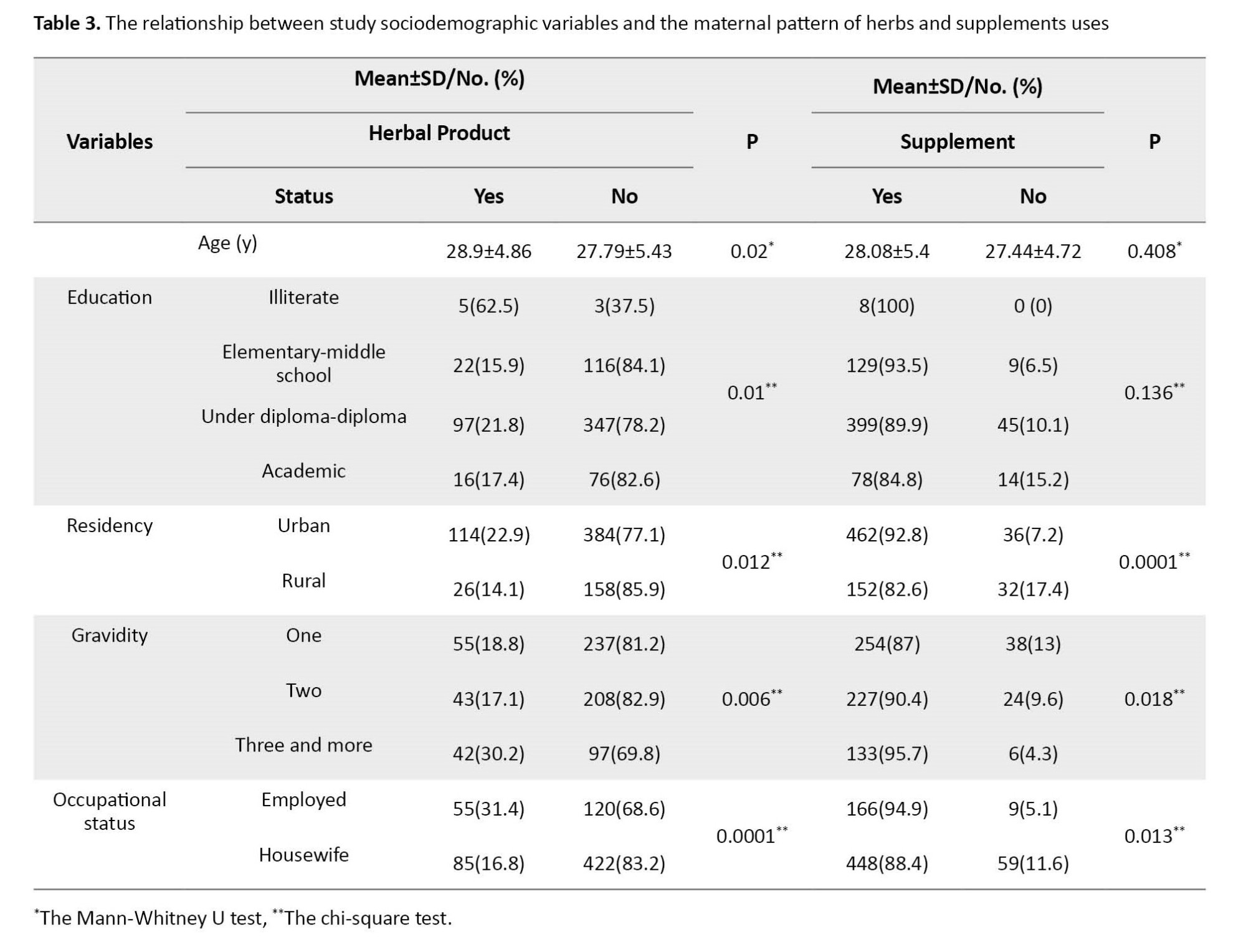
Residency, gravidity, and occupation status had a significant relationship with using supplements and herbal products (P). Also, age (P=0.02) and education (P=0.01) had relationships with herbal product consumption (Table 3).
Logistic regression analyses (Table 4) found that living in urban areas increases the probability of using supplements during pregnancy by 3.59 times compared to rural residents (OR=3.59, 95% CI; 2.05%, 6.3%, P=0.0001).
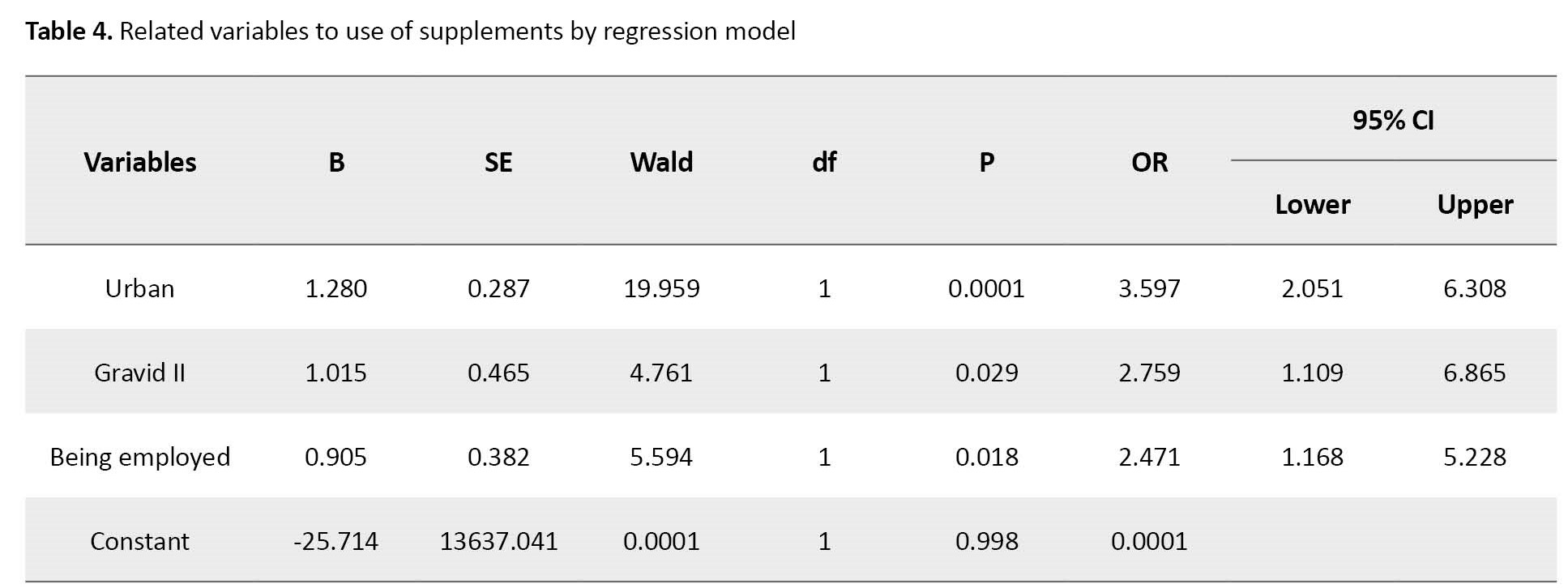
It was also found that women with gravid II were 2.7 times more likely to use supplements during pregnancy than women with gravid I (OR=2.75, 95% CI; 1.1%, 6.86%, P=0.029), and being employed increases 2.47 times the probability of taking supplements during pregnancy (OR=2.47, 95% CI; 1.16%, 5.22%, P=0.018). In terms of herbal use, it was found that urbanization increases the probability of consuming herbal products during pregnancy by 1.91 times compared to rural residents (OR=1.91, 95% CI; 1.6%, 3.14%, P=0.01).
Moreover, Table 5 presents the logistic regression model for variables related to herbal products.
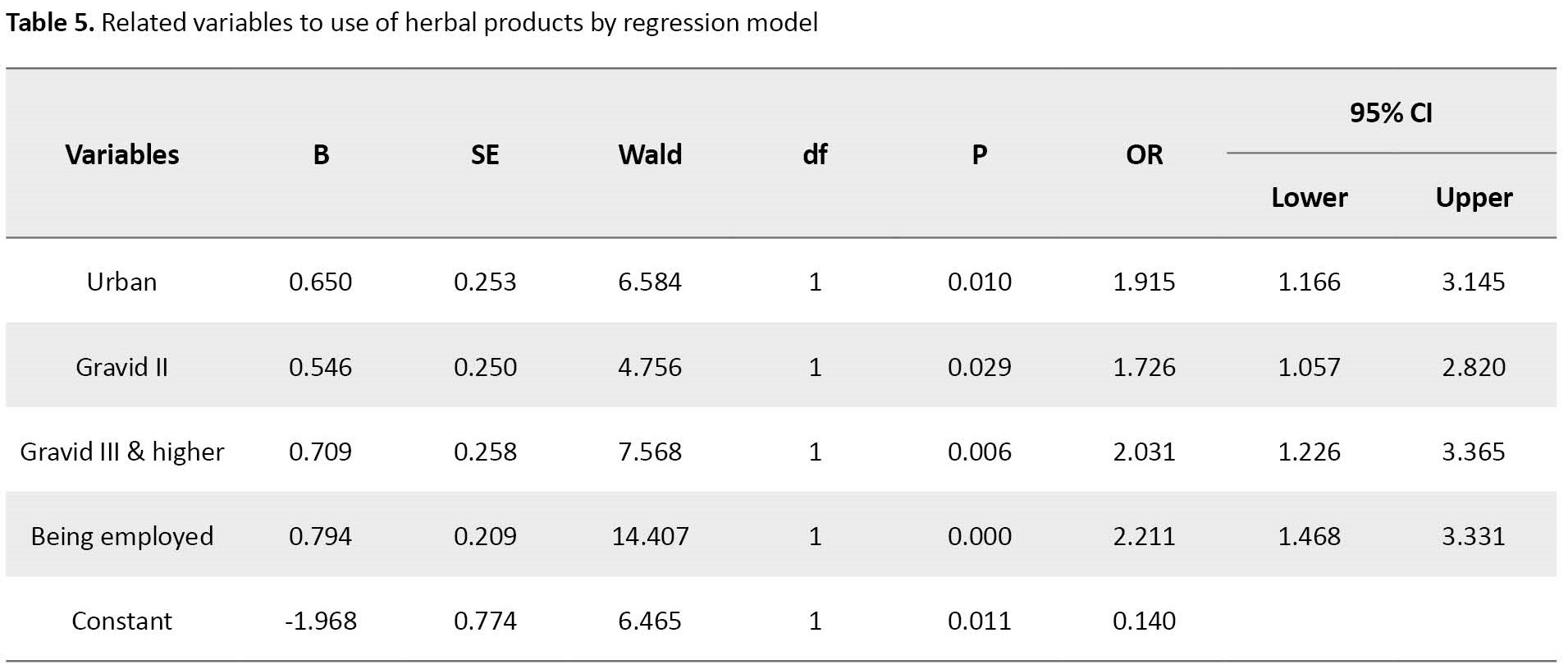
The results showed that gravid II women were 1.72 times more likely to consume herbal products during pregnancy than gravid I women (OR=1.72 95% CI; 1.05-2.82, P=0.029) and gravidity III were 2.03 times more likely to consume herbal products than women with gravid I (OR=2.03, 95% CI; 1.22%, 3.36%, P=0.006). Furthermore, being employed increases 2.21 times the probability of consuming herbal products during pregnancy compared to non-employed women (OR=2.21, 95% CI; 1.46%, 3.33%, P=0.0001).
Discussion
Non-prescribed and unreported use of herbs and supplements is a huge concern for anesthesiologists as they may cause serious drug interactions [17-19]. This geographical and ethnic study was conducted to estimate the frequency of use and the micronutrient contribution of dietary supplements among pregnant women. Many studies report that consumption of herbal products during pregnancy in Iran ranges from 19.2% to 71.3% [19-22], while this study shows that the frequency of consumption of herbal substances is 20.5%.
Thyme and mint were the most commonly used herbs in our study, while in other populations, topical almond oil [2], ginger [23], and ginseng [24] were the most popular ones. Regarding supplementations, this study revealed that 10% of the women do not take complementary medicine.
Jun et al. investigated the prevalence of the consumption of dietary supplements among pregnant women in the United States. They reported that 77% of pregnant women used at least one dietary supplement, while half of them used supplements as recommended by physicians. Among pregnant women, those aged 20 to 34 in the first trimester of pregnancy and a lower-income family were less likely to take supplements. Most pregnant women took supplements that contributed nutrients in higher doses than the recommended allowable doses. On the other hand, inadequate intake of necessary nutrition components was of concern among pregnant women not taking supplements. They suggested a potential need for healthcare providers to discuss the importance of the correct supplement use at recommended doses during prenatal visits [25].
Despite that, most cases had physicians’ orders, as some are essential during pregnancy. Particular attention should be paid to this small percentage, and the reason for not taking supplements such as folate and iron should be searched for. It should be noted that the problem is worldwide spread, and studies reported that it is nearly universal and polypharmacy is common [25, 26].
Regarding the consumption pattern of herbal products, it was revealed that more than half of the women took them in the first trimester. It was also found that younger ages, higher levels of education, urbanization, and occupation were significantly related to higher herb consumption. Most women use supplements during the whole pregnancy, and urbanization and occupation have a significant relationship with using more supplements.
In the study by Facchinetti et al. in Italy, half of the subjects reported using herbal products once at least during pregnancy, and more than one-quarter had a regular daily intake of herbal compounds [2]. Sattari et al. reported that 44.9% of the women took herbal products during pregnancy without a physician’s advice. Also, 39.8% believed these components could be used safely with no caution [27]. Soleimani et al. reported that only 19.2% of their samples used herbal medicines during pregnancy, but most were not supervised by a physician [22]. A study by Karimian in Kashan City in the center of Iran showed that more than 50% of the studied pregnant women used medicinal herbs. They found that subjective norms were the main predictor of herbal usage [20]. In Yazdi et al. study in one of the southern provinces of Iran, it was demonstrated that about half of women used herbal therapy and other self-medicated complementary alternative medicine [19]. Different cultures, beliefs, and ethics could justify the reason for the discordance among studies. In addition, the method of data collection was not the same. A direct interview after or before delivery will yield more reliable results than other methods, such as national registries or questioning times after childbirth. Indeed, the way and timing of the interview affect the quality and precision of the gathered information. Vegetation of different areas, availability of medicinal supplements and herbal products according to the rules, and strictness in pharmaceutical systems are also influential factors.
This study assessed the prevalence of NPU of both herbal products and supplements during pregnancy in an academic referral hospital. However, excluding the private sector should be considered as the limitation of the survey. Furthermore, the possibility of forgetting and being unable to accurately recall the consumption pattern, especially in the case of herbs, should be accepted as another research limitation.
Our suggestion for future studies is to evaluate the relationship between NPU of herbs and supplements and pregnancy outcomes and fetus abnormalities by considering influential factors such as genetics, parenteral social and economic status, and other environmental factors [28].
This study concludes that herbal use during pregnancy is almost popular but worrisome because healthcare professionals do not recommend their usage. In contrast, supplements are based on health care professionals’ advice. The main concern relates to pregnant women not using supplements and, consequently, having inadequate intakes of folate and iron. Healthcare providers should pay enough attention and discuss NPU herbal products and necessary supplementation during pregnancy.
Ethical Considerations
Compliance with ethical guidelines
The Guilan University of Medical Sciences Research Ethics Committee approved the study protocol and registered it (Code: IR.GUMS.REC.1400.498).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Gelareh Biazar and Misa Naghdipour Mirsadeghi; Data analysis and data interpretation: Zahra Rafiei Sorouri and Seyed Mohamadreza Tabatabaei Taher; Drafting of the manuscript: Fatemeh Hosseinzadeh and Sara Farzadi; Statistical analysis: Mandana Mansour Ghanaie; Critical revision of the manuscript for important intellectual content: Gelareh Biazar, Fatemeh Hosseinzadeh, and Mandana Mansour Ghanaie; Final approval: All authors.
Conflict of interest
The authors declared no conflict of study.
Acknowledgments
The research team would like to thank the Anesthesiology Research Center of Guilan University of Medical Sciences personnel, Mohadese Ahmadi and Mahin Tayefeh Ashrafie, for their collaboration in this study.
References
Not-prescribed use (NPU) of complementary supplements and herbal medicine during pregnancy has been increasing over the past two decades. Studies have demonstrated that the prevalence of herbal use during pregnancy ranges from 1% to 60% in different societies [1]. Several studies have shown that middle-aged white people with higher levels of education and better economic status tend to use supplementations more than others [2]. Regarding supplements during pregnancy, the use of the necessary and recommended ones by physicians, such as acid folic, is essential, while NPU of them could be harmful [3, 4, 5]. Today, herbal and complementary supplements with different properties, especially for pregnant women, are readily available at local herb markets and pharmacies and sold at a lower cost. Some factors justify their higher use among pregnant women; pregnancy is associated with several complications such as nausea and vomiting, constipation, and fatigue that sometimes are not sufficiently treated by conventional medical treatments. In addition, pregnant women prefer to relieve their symptoms with these natural components, which are presumed safer compared to industrial drugs [6, 7, 8]. However, due to the passage of active ingredients of the herbs through the placental barrier and reaching the fetus, the safety of herbal products during pregnancy is debatable [9]. According to a recent systematic review, the use of herbal medicinal products during pregnancy should be avoided until strong evidence of safety is available [10]. NPU of herbal products or supplements during pregnancy is also a challenge for anesthesiologists. Some pregnant women are candidates for cesarean section due to obstetrics indications, and some should receive general anesthesia in certain conditions despite several disadvantages of regional anesthesia [11, 12].
In this regard, dietary supplements, vitamins, or herbs could significantly interfere with the anesthetic drugs. Hemodynamic fluctuations, nausea and vomiting, altered drug metabolism, intraoperative arrhythmias, hypoglycemia, allergic reactions, increased bleeding, increased sedative effects of anesthetics, and cardiovascular instability may occur. Therefore, it is necessary to discontinue them at a certain time before operation [13]. In general, if the type of supplementation or herbs is unknown, it is recommended to stop them at least two weeks before delivery [14]. The consumption status of herbs and supplements is affected by the regions, ethnic backgrounds, cultures, and demographics [15]. Therefore, a better understanding of the conditions in each area seems vital to help improve mother-infant health programs and policies. The frequency of consumption of herbal products was investigated [16], which was valuable in this field. However, it had many defects, and the main problem was the non-prescribed consumption of the herbs, and the status of receiving supplements was not investigated. Therefore, this study aimed to examine the pattern of arbitrary consumption of herbal products and supplements among pregnant women.
Materials and Methods
This analytical cross-sectional study was conducted on pregnant women who were referred to an academic center affiliated with Guilan University of Medical Sciences (GUMS) for vaginal or cesarean delivery in 2022. The center performs 3500 to 4000 deliveries annually. According to the inclusion criteria, 682 mothers entered this study.
The inclusion criteria were women with term pregnancy admitted to an academic referral center in Rasht City for delivery, living in Guilan Province, being able to communicate, and having a stable hemodynamic status. The exclusion criteria were women who did not give informed consent for any reason and referal pregnant women as they might have different traditions in the consumption of herbal components or supplements.
A researcher-made questionnaire containing questions about maternal demographic data (age, education, residency, and occupational status) and the maternal pattern of herbs and supplements used during pregnancy was used. The questionnaire items were presented to 10 Obstetrics and Anesthesiology Department faculty members, and they confirmed its validity. The reliability of the questionnaire was not assessed due to the type of questions. All questions were answered by “yes” or “no.” At the beginning of the interview, enough information about the study was provided to all 682 eligible mothers, and an herbal compound was described as any remedy product from herbs to prevent or cure illness or achieve better health [10]. Then, their written consent was obtained. A medical student filled out the questionnaire through a direct interview on the day after delivery.
The face-to-face interview was chosen because it would provide more comprehensive and reliable information than a self-administered questionnaire.
The collected data were entered into and analyzed using the SPSS software, version 21. Percentages and frequencies were used to express different variables. The chi-square and Mann-Whitney U tests were performed to analyze the data. Multivariate logistic regression analysis determined factors associated with herbal products and supplemental use. Odds ratio (OR) with a 95% confidence interval (CI) were also calculated. A P<0.05 was considered statistically significant.
Results
A total of 710 women were interviewed, with a response rate of 96.3% (28 refused to participate). The data from 682 participants, with a mean age of 28.01±5.33 (18-42) years, were analyzed. A total of 488 women (71.6%) were less or equal to 30 years old, 498(73%) lived in urban areas, 508(74.5%) were homemakers, 444(65.1%) had under diploma or diploma grades, 292(42.8%) were gravid one and 251(36.8%) gravid two. Also, 49 participants (7.2%) reported no consumption of herbal products or supplements, and 121(17.7%) used both herbal products and supplements during pregnancy. In addition, 614(90%) took supplements and 140(20.5%) used herbal products during pregnancy. About 93.6% used herbal products without healthcare professionals’ supervision (Table 1).
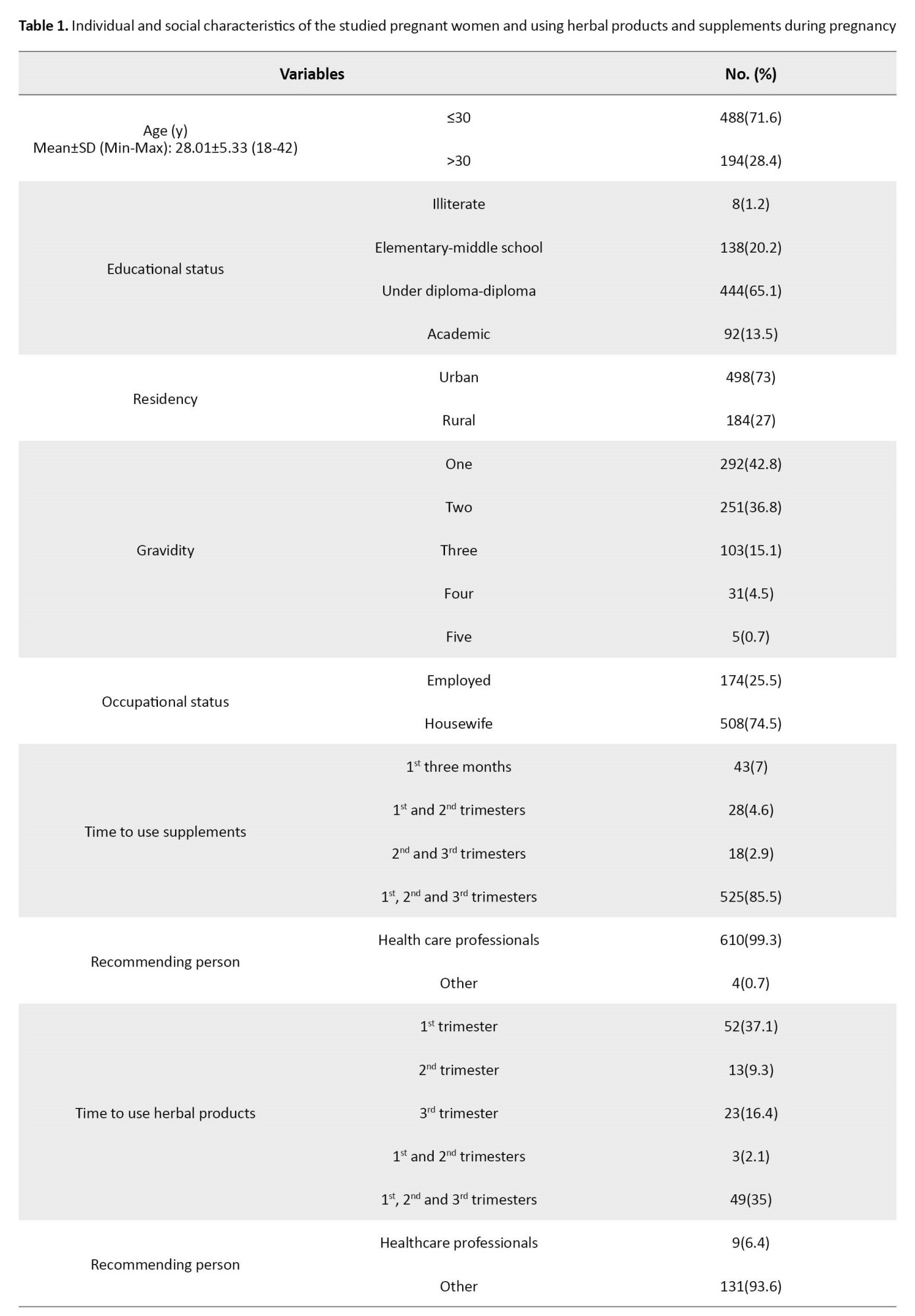
Iron (23.3%) and folic acid (23.1%) were the most frequent ones in supplements, and thyme (20.2%) and mint (17.5%) were the most taken herbs among pregnant women (Table 2).
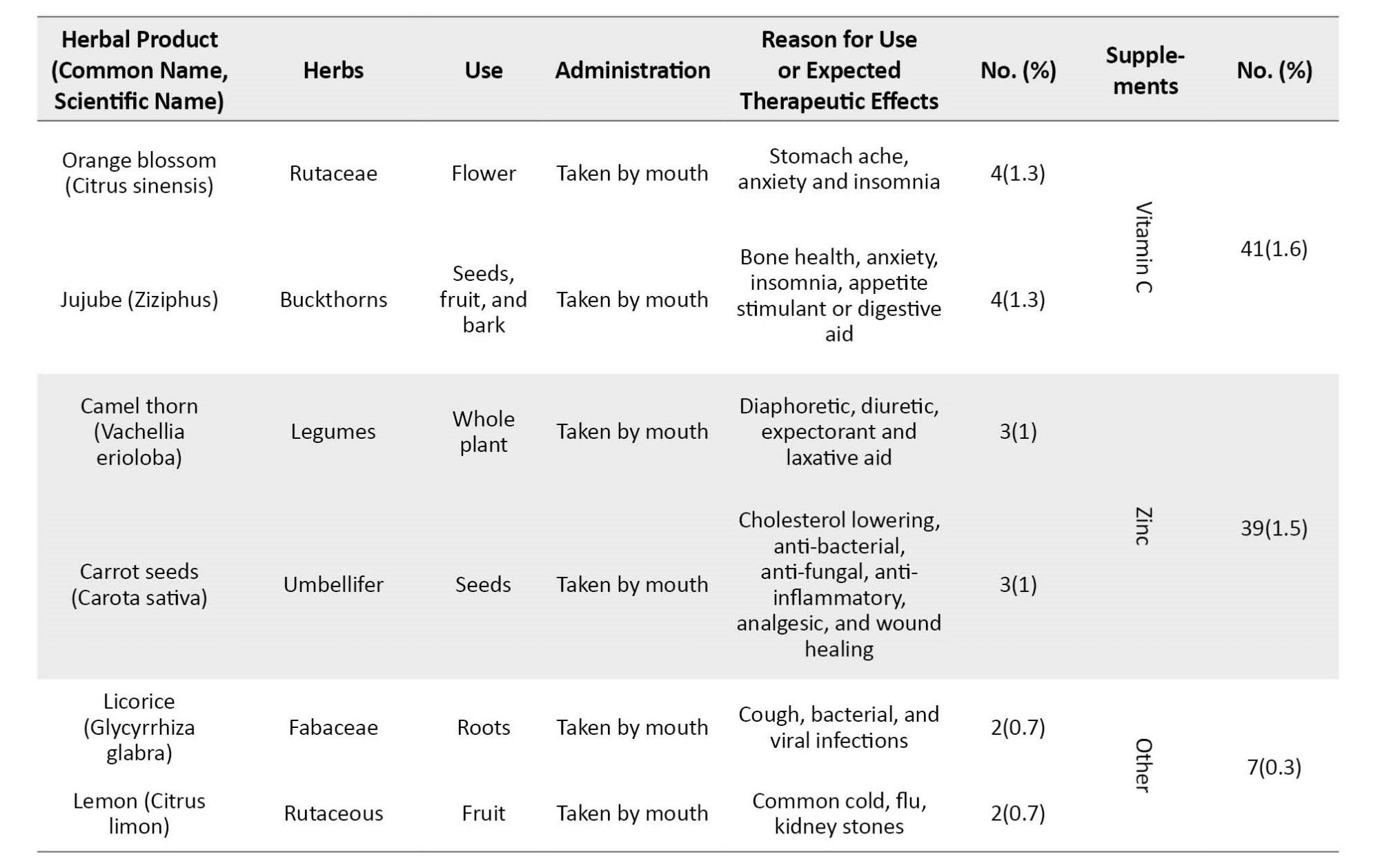
Residency, gravidity, and occupation status had a significant relationship with using supplements and herbal products (P). Also, age (P=0.02) and education (P=0.01) had relationships with herbal product consumption (Table 3).
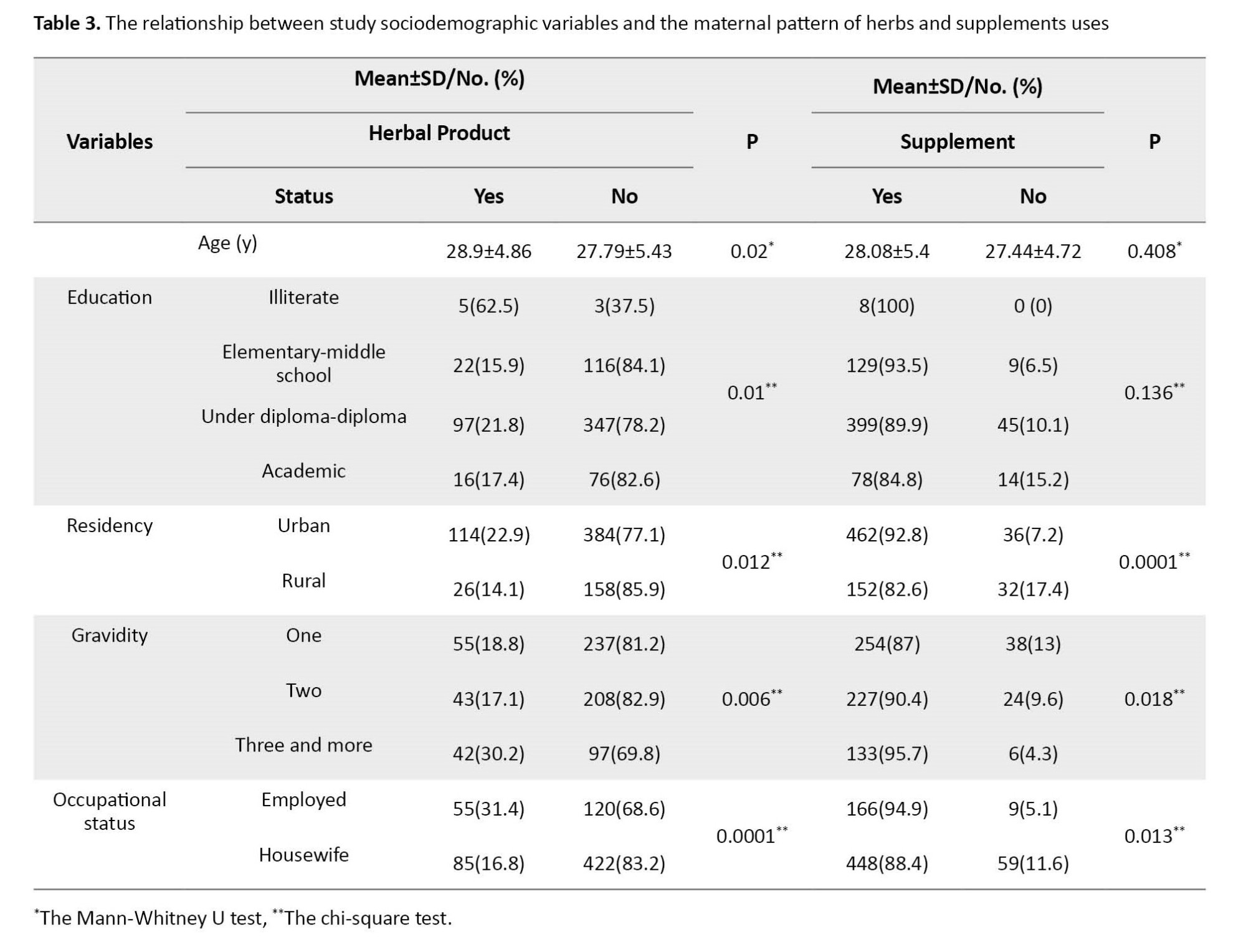
Logistic regression analyses (Table 4) found that living in urban areas increases the probability of using supplements during pregnancy by 3.59 times compared to rural residents (OR=3.59, 95% CI; 2.05%, 6.3%, P=0.0001).
It was also found that women with gravid II were 2.7 times more likely to use supplements during pregnancy than women with gravid I (OR=2.75, 95% CI; 1.1%, 6.86%, P=0.029), and being employed increases 2.47 times the probability of taking supplements during pregnancy (OR=2.47, 95% CI; 1.16%, 5.22%, P=0.018). In terms of herbal use, it was found that urbanization increases the probability of consuming herbal products during pregnancy by 1.91 times compared to rural residents (OR=1.91, 95% CI; 1.6%, 3.14%, P=0.01).
Moreover, Table 5 presents the logistic regression model for variables related to herbal products.
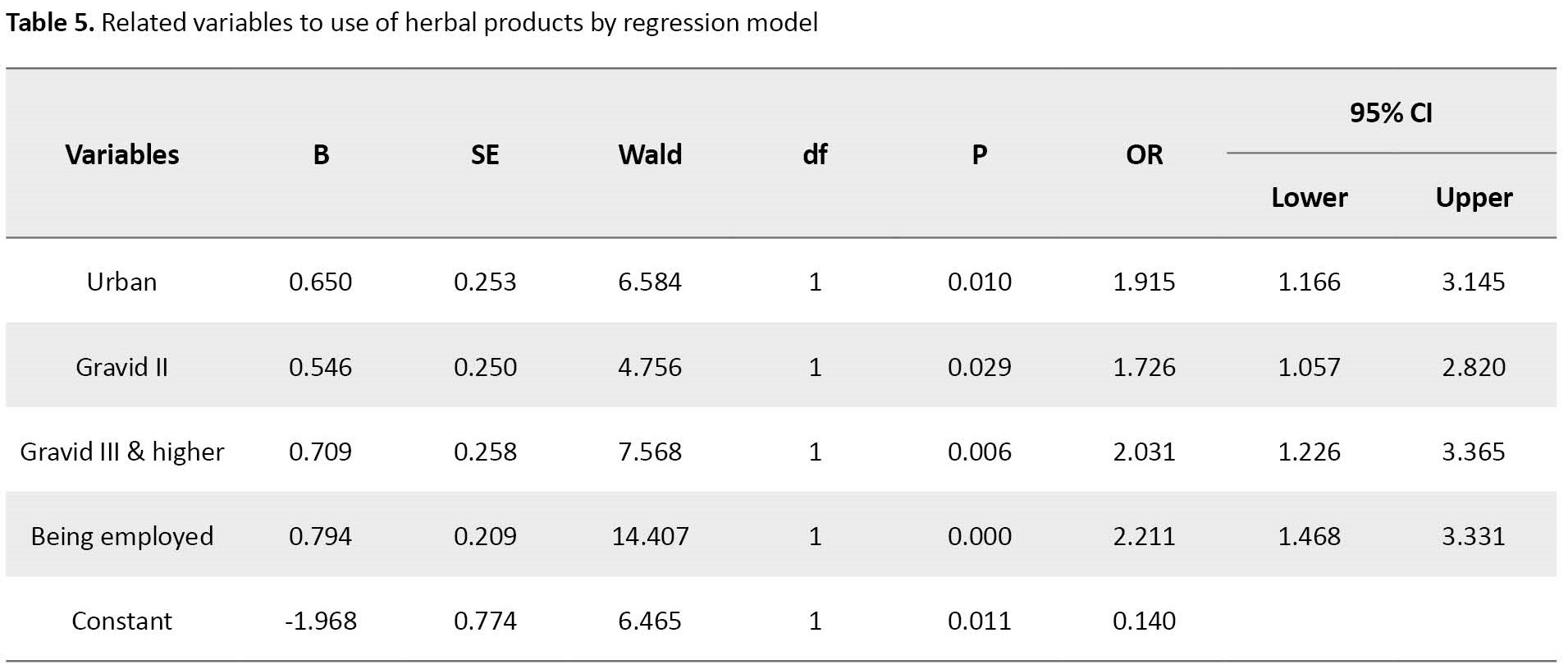
The results showed that gravid II women were 1.72 times more likely to consume herbal products during pregnancy than gravid I women (OR=1.72 95% CI; 1.05-2.82, P=0.029) and gravidity III were 2.03 times more likely to consume herbal products than women with gravid I (OR=2.03, 95% CI; 1.22%, 3.36%, P=0.006). Furthermore, being employed increases 2.21 times the probability of consuming herbal products during pregnancy compared to non-employed women (OR=2.21, 95% CI; 1.46%, 3.33%, P=0.0001).
Discussion
Non-prescribed and unreported use of herbs and supplements is a huge concern for anesthesiologists as they may cause serious drug interactions [17-19]. This geographical and ethnic study was conducted to estimate the frequency of use and the micronutrient contribution of dietary supplements among pregnant women. Many studies report that consumption of herbal products during pregnancy in Iran ranges from 19.2% to 71.3% [19-22], while this study shows that the frequency of consumption of herbal substances is 20.5%.
Thyme and mint were the most commonly used herbs in our study, while in other populations, topical almond oil [2], ginger [23], and ginseng [24] were the most popular ones. Regarding supplementations, this study revealed that 10% of the women do not take complementary medicine.
Jun et al. investigated the prevalence of the consumption of dietary supplements among pregnant women in the United States. They reported that 77% of pregnant women used at least one dietary supplement, while half of them used supplements as recommended by physicians. Among pregnant women, those aged 20 to 34 in the first trimester of pregnancy and a lower-income family were less likely to take supplements. Most pregnant women took supplements that contributed nutrients in higher doses than the recommended allowable doses. On the other hand, inadequate intake of necessary nutrition components was of concern among pregnant women not taking supplements. They suggested a potential need for healthcare providers to discuss the importance of the correct supplement use at recommended doses during prenatal visits [25].
Despite that, most cases had physicians’ orders, as some are essential during pregnancy. Particular attention should be paid to this small percentage, and the reason for not taking supplements such as folate and iron should be searched for. It should be noted that the problem is worldwide spread, and studies reported that it is nearly universal and polypharmacy is common [25, 26].
Regarding the consumption pattern of herbal products, it was revealed that more than half of the women took them in the first trimester. It was also found that younger ages, higher levels of education, urbanization, and occupation were significantly related to higher herb consumption. Most women use supplements during the whole pregnancy, and urbanization and occupation have a significant relationship with using more supplements.
In the study by Facchinetti et al. in Italy, half of the subjects reported using herbal products once at least during pregnancy, and more than one-quarter had a regular daily intake of herbal compounds [2]. Sattari et al. reported that 44.9% of the women took herbal products during pregnancy without a physician’s advice. Also, 39.8% believed these components could be used safely with no caution [27]. Soleimani et al. reported that only 19.2% of their samples used herbal medicines during pregnancy, but most were not supervised by a physician [22]. A study by Karimian in Kashan City in the center of Iran showed that more than 50% of the studied pregnant women used medicinal herbs. They found that subjective norms were the main predictor of herbal usage [20]. In Yazdi et al. study in one of the southern provinces of Iran, it was demonstrated that about half of women used herbal therapy and other self-medicated complementary alternative medicine [19]. Different cultures, beliefs, and ethics could justify the reason for the discordance among studies. In addition, the method of data collection was not the same. A direct interview after or before delivery will yield more reliable results than other methods, such as national registries or questioning times after childbirth. Indeed, the way and timing of the interview affect the quality and precision of the gathered information. Vegetation of different areas, availability of medicinal supplements and herbal products according to the rules, and strictness in pharmaceutical systems are also influential factors.
This study assessed the prevalence of NPU of both herbal products and supplements during pregnancy in an academic referral hospital. However, excluding the private sector should be considered as the limitation of the survey. Furthermore, the possibility of forgetting and being unable to accurately recall the consumption pattern, especially in the case of herbs, should be accepted as another research limitation.
Our suggestion for future studies is to evaluate the relationship between NPU of herbs and supplements and pregnancy outcomes and fetus abnormalities by considering influential factors such as genetics, parenteral social and economic status, and other environmental factors [28].
This study concludes that herbal use during pregnancy is almost popular but worrisome because healthcare professionals do not recommend their usage. In contrast, supplements are based on health care professionals’ advice. The main concern relates to pregnant women not using supplements and, consequently, having inadequate intakes of folate and iron. Healthcare providers should pay enough attention and discuss NPU herbal products and necessary supplementation during pregnancy.
Ethical Considerations
Compliance with ethical guidelines
The Guilan University of Medical Sciences Research Ethics Committee approved the study protocol and registered it (Code: IR.GUMS.REC.1400.498).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Gelareh Biazar and Misa Naghdipour Mirsadeghi; Data analysis and data interpretation: Zahra Rafiei Sorouri and Seyed Mohamadreza Tabatabaei Taher; Drafting of the manuscript: Fatemeh Hosseinzadeh and Sara Farzadi; Statistical analysis: Mandana Mansour Ghanaie; Critical revision of the manuscript for important intellectual content: Gelareh Biazar, Fatemeh Hosseinzadeh, and Mandana Mansour Ghanaie; Final approval: All authors.
Conflict of interest
The authors declared no conflict of study.
Acknowledgments
The research team would like to thank the Anesthesiology Research Center of Guilan University of Medical Sciences personnel, Mohadese Ahmadi and Mahin Tayefeh Ashrafie, for their collaboration in this study.
References
- Balarastaghi S, Delirrad M, Jafari A, Majidi M, Sadeghi M, Zare-Zardini H, et al. Potential benefits versus hazards of herbal therapy during pregnancy; A systematic review of available literature. Phytother Res. 2022; 36(2):824-41. [DOI:10.1002/ptr.7363] [PMID]
- Facchinetti F, Pedrielli G, Benoni G, Joppi M, Verlato G, Dante G, et al. Herbal supplements in pregnancy: Unexpected results from a multicentre study. Hum Reprod. 2012; 27(11):3161-7.[DOI:10.1093/humrep/des303] [PMID]
- Yan Y, Xie C, Di S, Wang Z, Wu M, Li Y, et al. Supplemental folic acid and/or multivitamins in pregnancy is associated with a decreased risk of childhood and adolescent nasopharyngeal carcinoma. J Dev Orig Health Dis. 2022; 13(5):550-5. [Link]
- Gallo S, McDermid JM, Al-Nimr RI, Hakeem R, Moreschi JM, Pari-Keener M, et al. Vitamin D supplementation during pregnancy: An evidence analysis center systematic review and meta-analysis. J Acad Nutr Diet. 2020; 120(5):898-24. e4. [DOI:10.1016/j.jand.2019.07.002] [PMID]
- Trabace L, Tucci P, Ciuffreda L, Matteo M, Fortunato F, Campolongo P, et al. “Natural” relief of pregnancy-related symptoms and neonatal outcomes: Above all do no harm. J Ethnopharmacol. 2015; 174:396-402. [DOI:10.1016/j.jep.2015.08.046] [PMID]
- Eid AM, Jaradat N. Public knowledge, attitude, and practice on herbal remedies used during pregnancy and lactation in West Bank Palestine. Front Pharmacol. 2020; 11:46. [DOI:10.3389/fphar.2020.00046] [PMID]
- Vitalone A, Allkanjari O, Federico D, Marina G, Aleandri V. The use of herbal products during pregnancy: Which is the risk perception? Am Phytomed Clin Ther. 2021; 9(1):1-8. [Link]
- Bruno LO, Simoes RS, de Jesus Simoes M, Girão MJBC, Grundmann O. Pregnancy and herbal medicines: An unnecessary risk for women’s health-A narrative review. Phytother Res. 2018; 32(5):796-810. [PMID]
- Bernstein N, Akram M, Yaniv-Bachrach Z, Daniyal M. Is it safe to consume traditional medicinal plants during pregnancy? Phytother Res. 2021; 35(4):1908-24. [DOI:10.1002/ptr.6935] [PMID]
- Muñoz Balbontín Y, Stewart D, Shetty A, Fitton CA, McLay JS. Herbal medicinal product use during pregnancy and the postnatal period: A systematic review. Obstet Gynecol. 2019; 133(5):920-32. [DOI:10.1097/AOG.0000000000003217] [PMID]
- Sedighnejad A, Soltanipour S, Saberi A, Kousha M, Bidabadi E, Biazar G, et al. Risk of attention deficit hyper activity disorder after early exposure to general anesthesia; A case control study. Iran J Pediatr. 2020; 30(3):e99976. [Link]
- Biazar G, Farzi F, Nabi BN, Atrkarroushan Z, Chaibakhsh Y, Lima SR. General anesthesia-related neurotoxicity: Status of pediatric surgeries at an academic hospital in the North of Iran. J Compr Pediatr. 2019; 10(4):e92316. [DOI:10.5812/compreped.92316]
- Woodbury A, Soong SN, Fishman D, García PS. Complementary and alternative medicine therapies for the anesthesiologist and pain practitioner: A narrative review. Can J Anaesth. 2016; 63(1):69-85. [DOI:10.1007/s12630-015-0506-9] [PMID]
- Wong A, Townley SA. Herbal medicines and anaesthesia. Contin Educ Anaesth Crit Care Pain. 2011; 11(1):14-7. [DOI:10.1093/bjaceaccp/mkq046]
- Addis GT, Workneh BD, Kahissay MH. Herbal medicines use and associated factors among pregnant women in Debre Tabor town, north West Ethiopia: A mixed method approach. BMC Complement Med Ther. 2021; 21(1):268. [DOI:10.1186/s12906-021-03439-3] [PMID]
- Biazar G, Nabi BN, Sedighinejad A, Moghadam AD, Farzi F, Atrkarroushan Z, et al. Herbal products use during pregnancy in north of Iran. Int J Women’s Health Reprod Sci. 2019; 7(1):134–7. [Link]
- McLay JS, Izzati N, Pallivalapila AR, Shetty A, Pande B, Rore C, et al. Pregnancy, prescription medicines and the potential risk of herb-drug interactions: A cross-sectional survey. BMC Complement Altern Med. 2017; 17(1):543. [DOI:10.1186/s12906-017-2052-1] [PMID]
- Willetts KE, Ekangaki A, Eden JA. Effect of a ginger extract on pregnancy-induced nausea: A randomised controlled trial. Aust N Z J Obstet Gynaecol. 2003; 43(2):139-44. [DOI:10.1046/j.0004-8666.2003.00039.x] [PMID]
- Yazdi N, Salehi A, Vojoud M, Sharifi MH, Hoseinkhani A. Use of complementary and alternative medicine in pregnant women: A cross-sectional survey in the south of Iran. J Integr Med. 2019; 17(6):392-5. [DOI:10.1016/j.joim.2019.09.003] [PMID]
- Karimian Z, Sadat Z, Afshar B, Hasani M, Araban M, Kafaei-Atrian M. Predictors of self-medication with herbal remedies during pregnancy based on the theory of planned behavior in Kashan, Iran. BMC Complement Med Ther. 2021; 21(1):211. [DOI:10.1186/s12906-021-03353-8] [PMID]
- Saber M, Khanjani N, Zamanian M, Safinejad H, Shahinfar S, Borhani M. Use of medicinal plants and synthetic medicines by pregnant women in Kerman, Iran. Arch Iran Med. 2019; 22(7):390-3. [PMID]
- Soleymani S, Makvandi S. [Rate of herbal medicines use during pregnancy and some related factors in women of Ahvaz, Iran: 2017 (Persian)]. Iran J Obstet Gynecol Infertil. 2018; 21(5):80-6. [DOI:10.22038/IJOGI.2018.11388]
- Louik C, Gardiner P, Kelley K, Mitchell AA. Use of herbal treatments in pregnancy. Am J Obstet Gynecol. 2010; 202(5):439.e1-439.e10. [DOI:10.1016/j.ajog.2010.01.055] [PMID]
- Holst L, Wright D, Haavik S, Nordeng H. Safety and efficacy of herbal remedies in obstetrics-review and clinical implications. Midwifery. 2011; 27(1):80-6. [DOI:10.1016/j.midw.2009.05.010] [PMID]
- Jun S, Gahche JJ, Potischman N, Dwyer JT, Guenther PM, Sauder KA, et al. Dietary supplement use and its micronutrient contribution during pregnancy and lactation in the United States. Obstet Gynecol. 2020; 135(3):623-33. [DOI:10.1097/AOG.0000000000003657] [PMID]
- Haas DM, Marsh DJ, Dang DT, Parker CB, Wing DA, Simhan HN, et al. Prescription and other medication use in pregnancy. Obstet Gynecol. 2018; 131(5):789-98. [PMID]
- Sattari M, Dilmaghanizadeh M, Hamishehkar H, Mashayekhi SO. Self-reported use and attitudes regarding herbal medicine safety during pregnancy in Iran. Jundishapur J Nat Pharm Prod. 2012; 7(2):45-9. [DOI:10.17795/jjnpp-3416] [PMID]
- Zamawe C, King C, Jennings HM, Fottrell E. Associations between the use of herbal medicines and adverse pregnancy outcomes in rural Malawi: A secondary analysis of randomised controlled trial data. BMC Complement Altern Med. 2018; 18(1):166. [PMID]
Article Type : Research |
Subject:
General
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |