Sun, Apr 28, 2024
Volume 34, Issue 2 (2-2024)
JHNM 2024, 34(2): 125-132 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zare O, Ebadi A, Ozgoli G, Kariman N. Psychometric Properties of the Persian Version of the Evidence-based Practice Implementation Questionnaire in Nurses. JHNM 2024; 34 (2) :125-132
URL: http://hnmj.gums.ac.ir/article-1-2304-en.html
URL: http://hnmj.gums.ac.ir/article-1-2304-en.html
1- Department of Midwifery, Comprehensive Health Research Center, Babol Branch, Islamic Azad University, Babol, Iran. , mahyazare@yahoo.com
2- Professor, Behavioral Sciences Research Center, School of Nursing, Life Style Institute, Baqiyatallah University of Medical Sciences, Tehran, Iran.
3- Associate Professor, Department of Midwifery and Reproductive Health, Midwifery and Reproductive Health Research Center, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Professor, Behavioral Sciences Research Center, School of Nursing, Life Style Institute, Baqiyatallah University of Medical Sciences, Tehran, Iran.
3- Associate Professor, Department of Midwifery and Reproductive Health, Midwifery and Reproductive Health Research Center, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 547 kb]
(89 Downloads)
| Abstract (HTML) (240 Views)
Full-Text: (47 Views)
Introduction
Evidence-based practice (EBP) in nursing is a framework for clinical practice that integrates the best available scientific evidence with nurse expertise and patient preferences to make healthcare decisions for individual patients. Nurses are the largest group of healthcare providers who play an essential role in ensuring better services to promote healthcare. Nurses must provide high-quality, safe, effective, fast, and patient-centered care. Knowledge of research and evidence-based care is integral to nursing practice [1-3].
This approach has been proposed to provide the best services for patients. The healthcare system is facing the challenge of providing consistent and high-quality services. If EBP is implemented and used properly in healthcare centers, it will help improve overall patient care [4].
Ongoing advances in medical science show that the effectiveness of nurses’ knowledge and the life span of information is short, and previously learned content is becoming increasingly obsolete. However, these problems can be overcome through EBP, which helps healthcare providers make sound decisions and eliminating outdated knowledge’s effects. EBP opens a window to modernity and helps healthcare providers enjoy a secure practice [5].
EBP is one of the main needs of health systems of the 21 th century [6]. For the quality of nursing care to be continuously improved, new research-based scientific evidence must be regularly used in clinical practice [7]. Most healthcare professionals have a positive attitude toward EBP but lack enough knowledge and skills to implement it [8]. In Asian countries, including Saudi Arabia, the implementation rate of EBP is 14% [9], and in Oman, attitude 4.07±1.34, knowledge 3.99±1.26, the lowest mean 3.84±1.41 related to the implementation of EBP was reported [10]. In Iran, the implementation of EBP is low [11]. The EBP implementation (EBP-I) scale can be used to evaluate the effectiveness of organizational strategies to increase healthcare professionals’ trust in EBP and support its use and implementation [12].
There are three valid and reliable scales to measure the critical concepts in the ARCC (advancing research and clinical practice through close collaboration) model: 1) The organizational culture and readiness scale for widespread EBP system integration, 2) The EBP beliefs scale, and 3) The EBP implementation scale. These three scales have been widely used in research and evidence-based quality improvement projects [13]. Many healthcare centers use EBP-I as a key tool to provide better and safer healthcare. A literature review reveals that the baseline assessments of EBP-I in the daily practice of healthcare providers were designed by Melnyk et al., and its psychometric properties were assessed in 2008 [13, 14]. However, EBP has not been psychometrically tested in Iran. There is scant research on the implementation of EBP in the healthcare community. EBP implementation (EBP-I) requires tools to assess the status quo and the effectiveness of interventions [15]. Due to the importance of EBP and the lack of appropriate measurement tools, this study assessed the psychometric properties of the Persian version of the EBP-I questionnaire in nurses.
Materials and Methods
This research is a methodological and cross-sectional descriptive analytical study conducted in the cities of Mazandaran Province in northern Iran from February to April 2022. The sample size was estimated based on the number of items in the tool. The minimum sample size required for exploratory analysis is 3 to 10 samples per item [16]; thus, we needed 220 participants.
We employed the multi-stage cluster sampling method to choose the study samples. Initially, a list of all cities in Mazandaran Province was prepared, from which 4 cities were randomly selected. Then, 3 hospitals from each city were randomly selected, and 5 wards or more were randomly selected from each hospital. With a probability of 20% dropout, a sample of 220 people was finally selected, and the study data were collected. The inclusion criteria were being a clinical nurse and being willing to complete the questionnaire. Because 20 questionnaires were incomplete and were excluded, 200 completed questionnaires were analyzed.
Demographic questionnaires and the Persian version of EBP-I were used in this study. The demographic questionnaire consisted of personal information (age, gender, level of education and work experience). The Persian version of the EBP-I questionnaire consists of 18 items scored on a 5-point Likert scale so that the options of 0, 1-3, 4-5, 6-7, and 8≤ were assigned a score of 0 to 4, respectively. The total score for this scale ranges from 0 to 72, with higher scores indicating greater implementation of this scale in clinical practice.
After obtaining permission from the original designer, the questionnaire was translated from English to Persian by an English-language expert and then back-translated into English using the forward-backward procedure according to guidelines [17]. Finally, the research team compared the Persian and English versions and prepared the final Persian version. Also, the original designer approved the English back-translation.
To evaluate the face and content validity of the tool, 10 experts specialized in Nursing and the EBP field in the Department of Nursing, Shahid Beheshti University of Medical Sciences, were selected and asked to read the questionnaire carefully and comment on the quality of the questionnaire items in terms of the difficulty, relevance, and clarity of the questions. After modifications based on their opinions, the content validity index (CVI) was calculated. The relevancy of each of the 18 items was rated by experts based on a 4-point Likert scale as (1 irrelevant, 2 somewhat relevant, 3 relevant, and 4 completely relevant). To calculate the CVI score for each item, the number of experts who gave each item a score of 3 and 4 was divided by their total number. A CVI score above 0.79 is considered appropriate, while one ranging from 0.70 to 0.79 must be reconsidered and revised. Items with a score below 0.70 were removed [18].
Data were analyzed using SPSS software, version 18 and LISREL software version 8.8. The reliability of the questionnaire was assessed using the Cronbach α coefficient to determine the internal consistency of the EBP-I questionnaire. A Cronbach α coefficient of 0.7 to 0.9 indicates good reliability [19]. The test re-test method was used to determine the repeatability of the EBP-I questionnaire. The interval between two tests is suggested from two weeks to one month [20]. For this purpose, 30 nurses completed the EBP-I questionnaire twice at a two-week interval.
To evaluate the scale’s construct validity, exploratory factor analysis (EFA) was used to extract the latent factors. At this stage, latent factors were extracted, and the Kaiser-Meyer-Olkin (KMO) index and Bartlett’s test were calculated. KMO values ranging from 0.70 to 0.80 and 0.80 to 0.90 were considered good and excellent, respectively [21].
Latent factors were extracted with maximum likelihood using Promax rotation and Scree diagrams. The minimum factor load was considered 0.3 [22]. Usually, the sample size used for Confirmatory Factor Analysis (CFA) is not less than 200 people [16], so 200 new samples of hospital nurses were selected by multi-stage random sampling with the same inclusion criteria. CFA was performed on 200 questionnaires. At this stage, the goodness-of-fit indexes from this analysis are reported. These are extracted factors with CFA, consisting of root mean squares error of approximation (RMSEA), normed fit index (NFI), comparative fit index (CFI), parsimony normed fit index (PNFI), incremental fit index (IFI), and adjusted goodness of fit index (AGFI). These were used to evaluate the fitness of the model.
Results
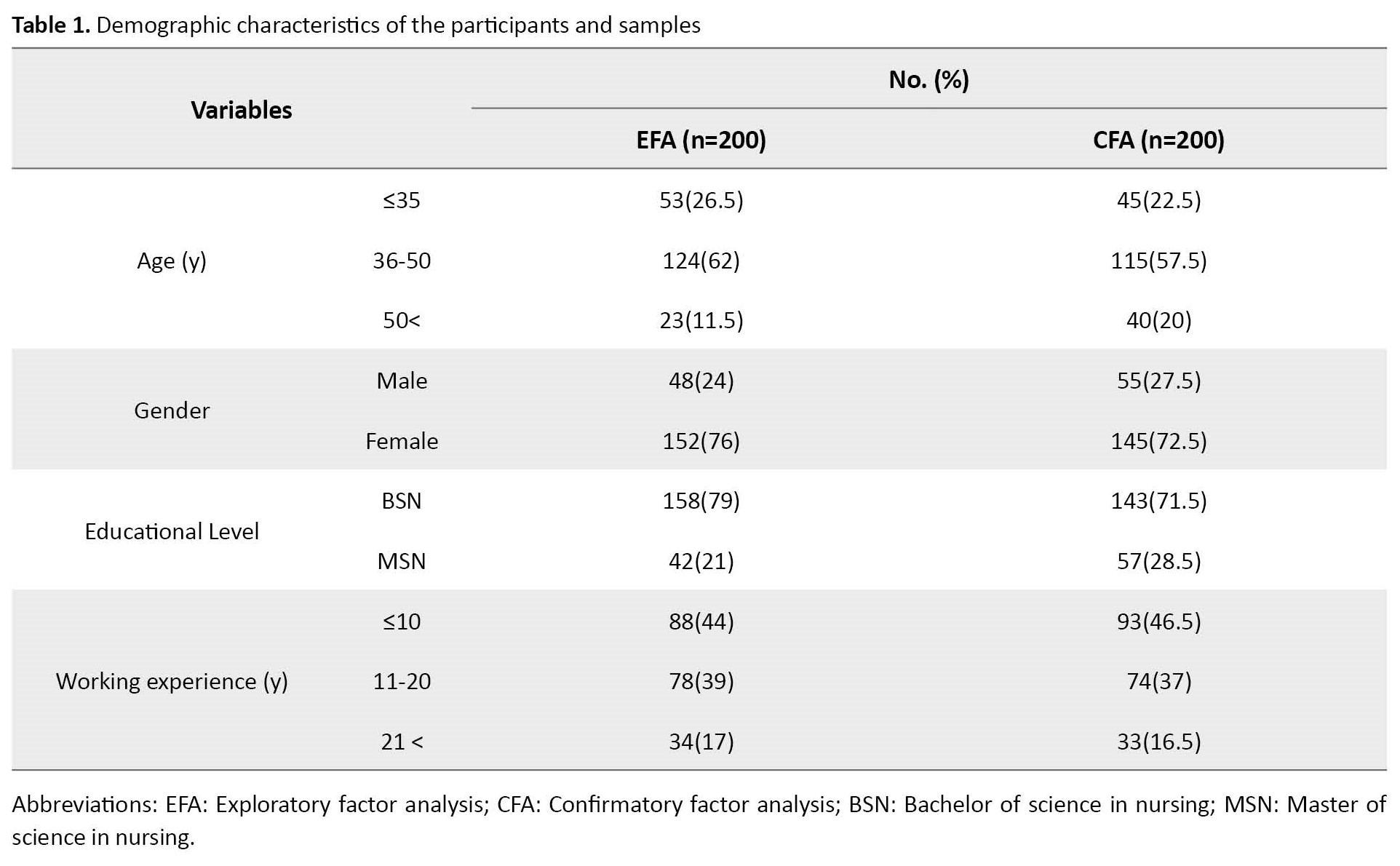
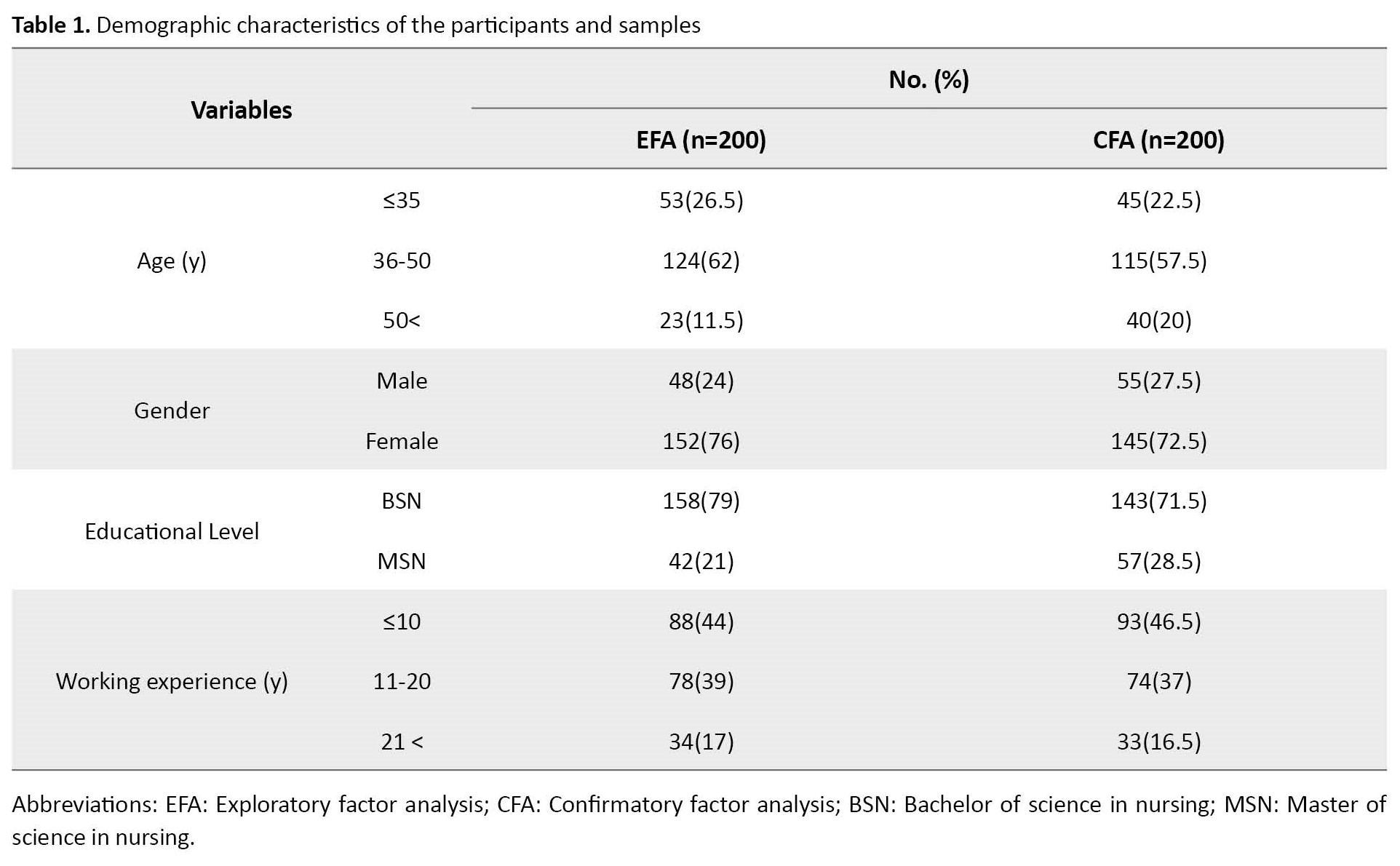
The participants in EFA and CFA were nurses, including 48 and 55 men and 152 and 145 women with a Mean±SD age of 42.64±7.58 and 41.75±5.65 years with an age range of 36 to 50 years, respectively. Most nurses in EFA and CFA (44% and 46.5%) had up to 10 years and less work experience and had a Bachelor’s degree (79% and 71.5%), respectively. Table 1 presents the demographic characteristics of the two selected samples.
The scale’s qualitative face and content validity was confirmed after reviewing the opinions of highly qualified nurses and experts about it. The CVI results indicated that all items had a CVI score higher than 0.79 and were considered appropriate. All items scored 1 in the 3 criteria of relevancy, simplicity, and clarity, and only 5 items (6, 10, 11, 13, and 18) scored 0.8 in the criteria of clarity. In total, 18 items were maintained in the research instrument based on the coefficient of impact (>1.5), content validity ratio (>0.62), and content validity index (>0.7).
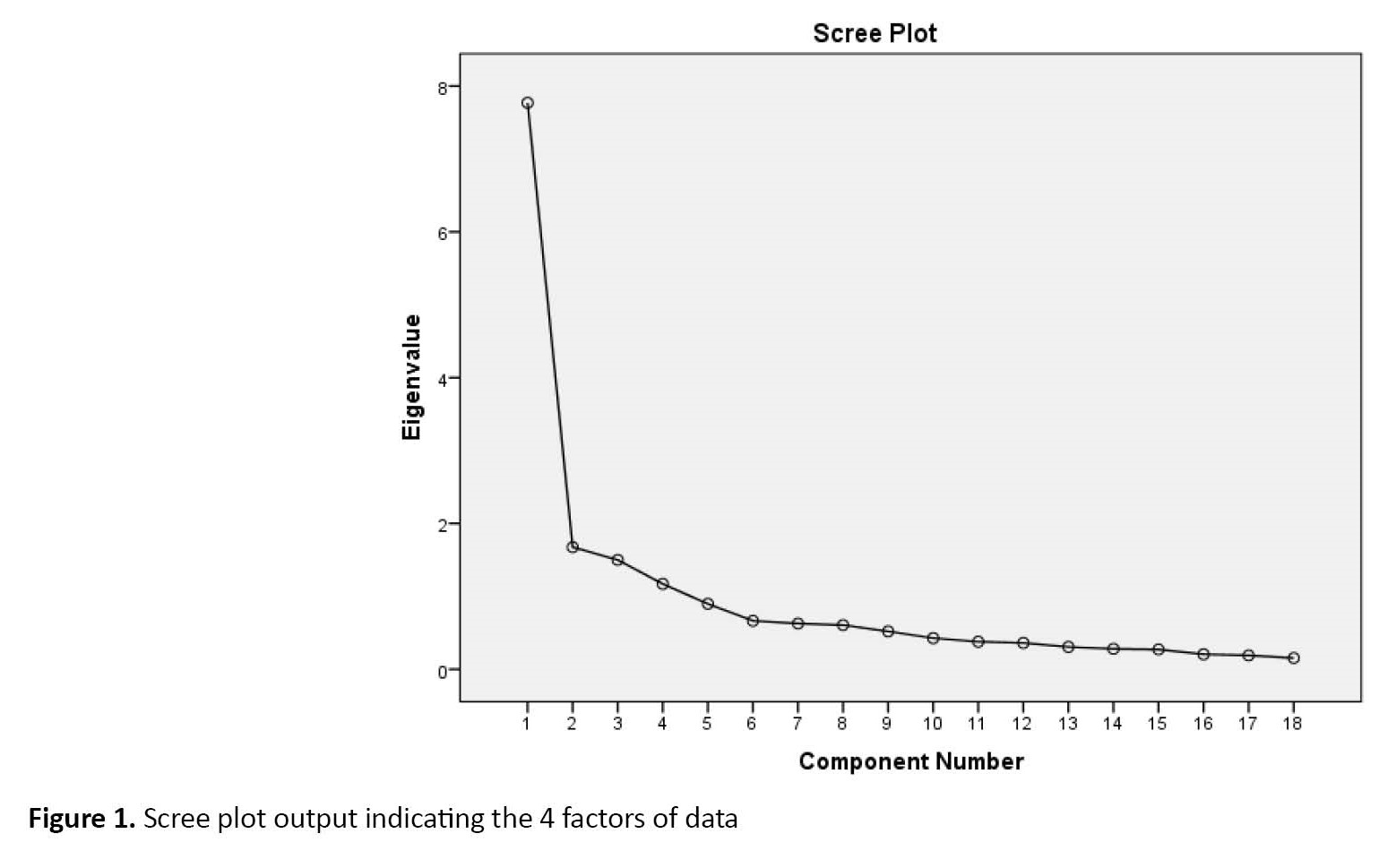
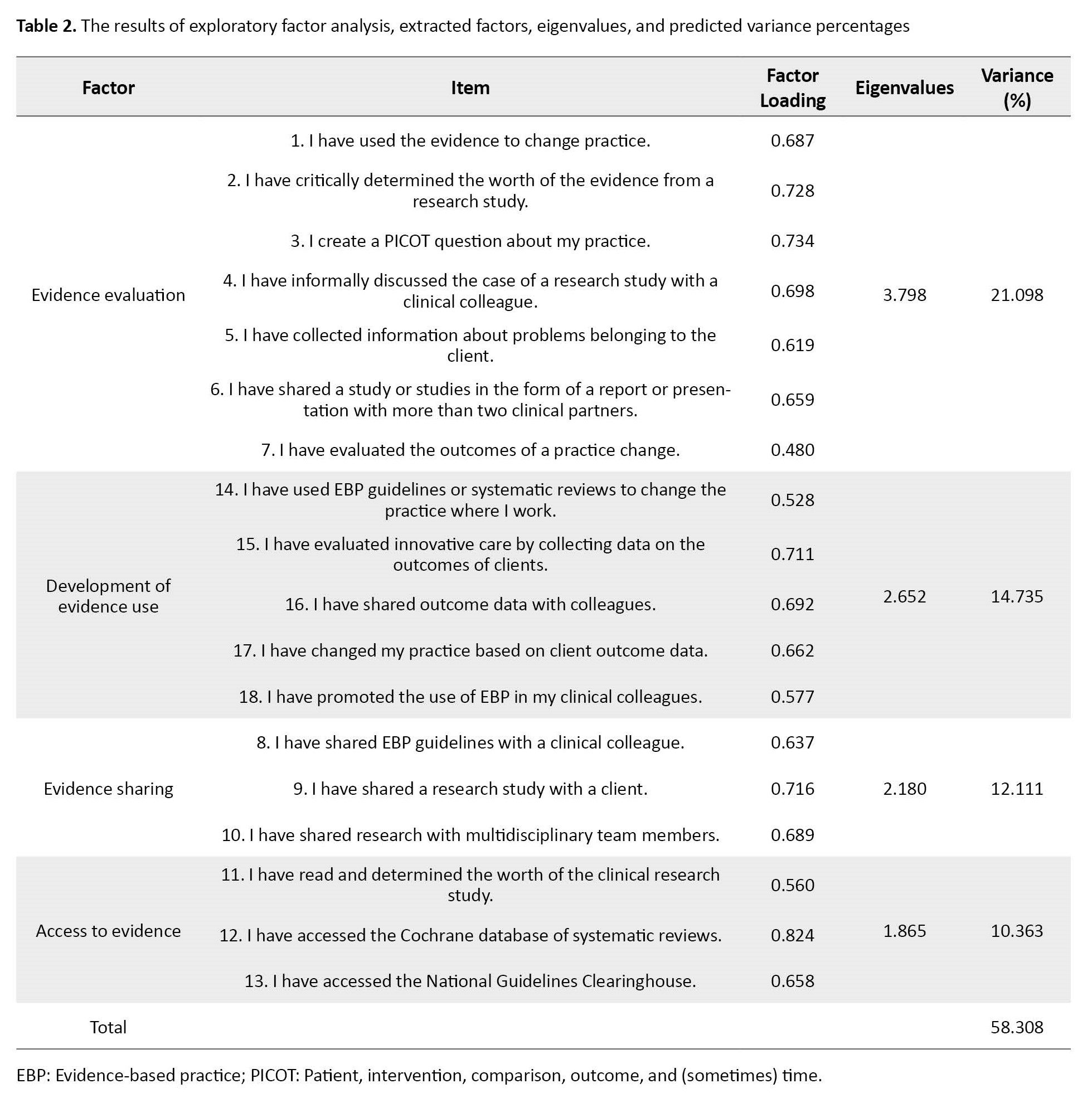
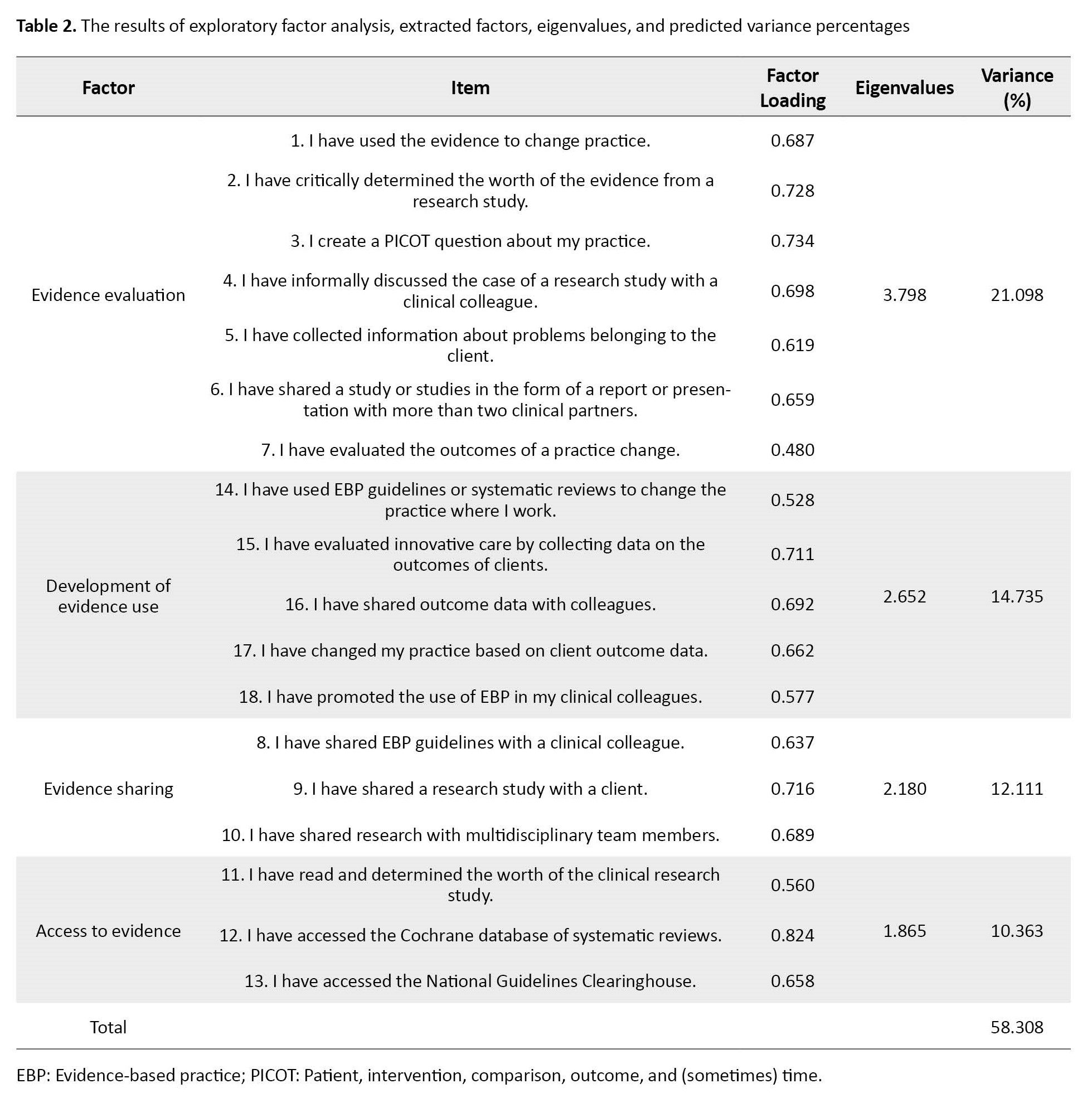
In performing EFA, KMO showed the adequacy of sampling (KMO=0.87). The Bartlett’s test of sphericity was statistically significant (χ2=2063.645, df=153, P=0.001). Based on EFA, four factors of evidence evaluation (items 1, 2, 3, 4, 5, 6, 7), development of evidence use (14, 15, 16, 17, and 18), evidence sharing (items 8, 9, and 10), and evidence access (items 11, 12, and 13) obtained eigenvalues of 3.798, 2.652, 2.180, and 1.865, respectively (Table 2).
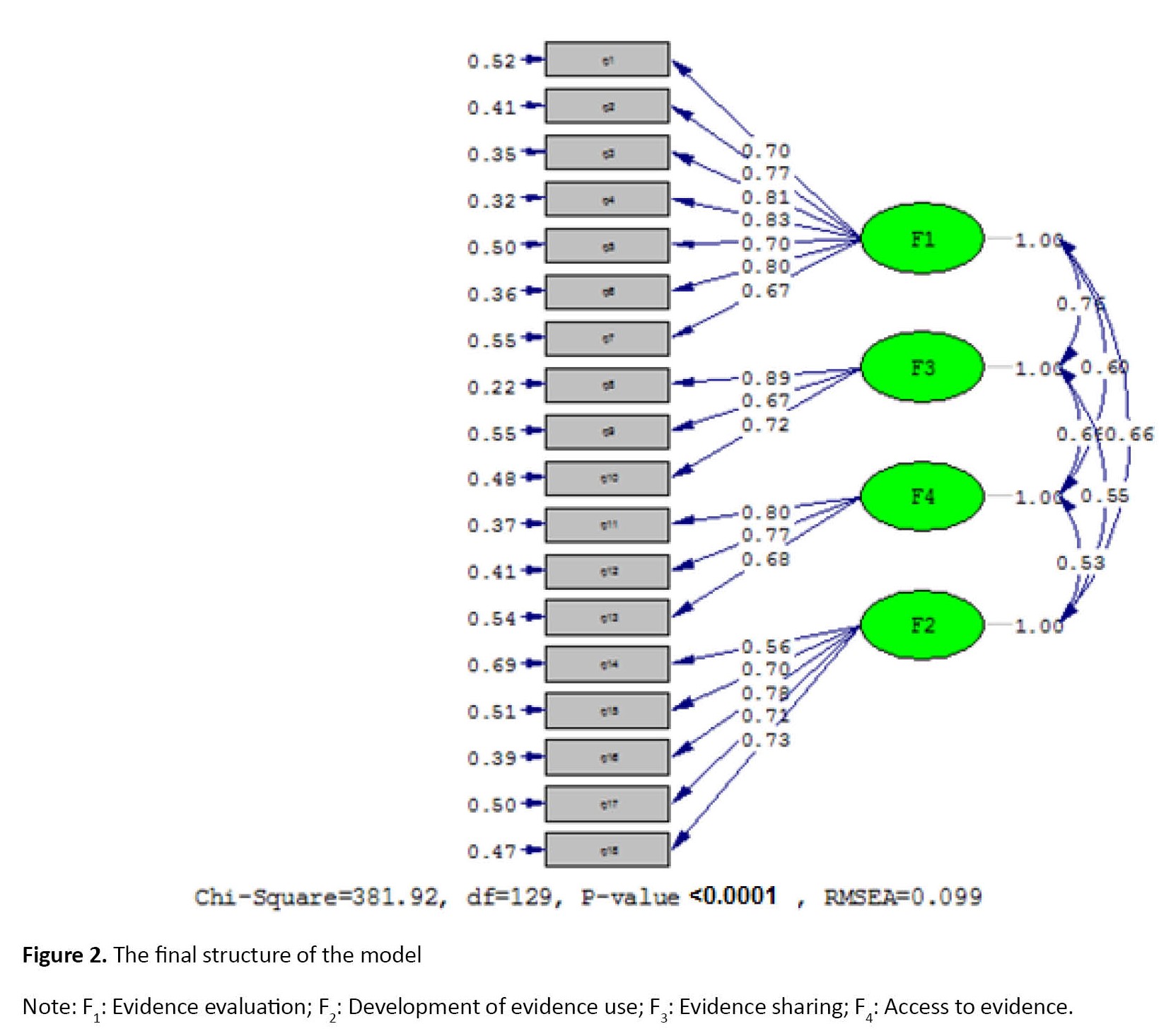
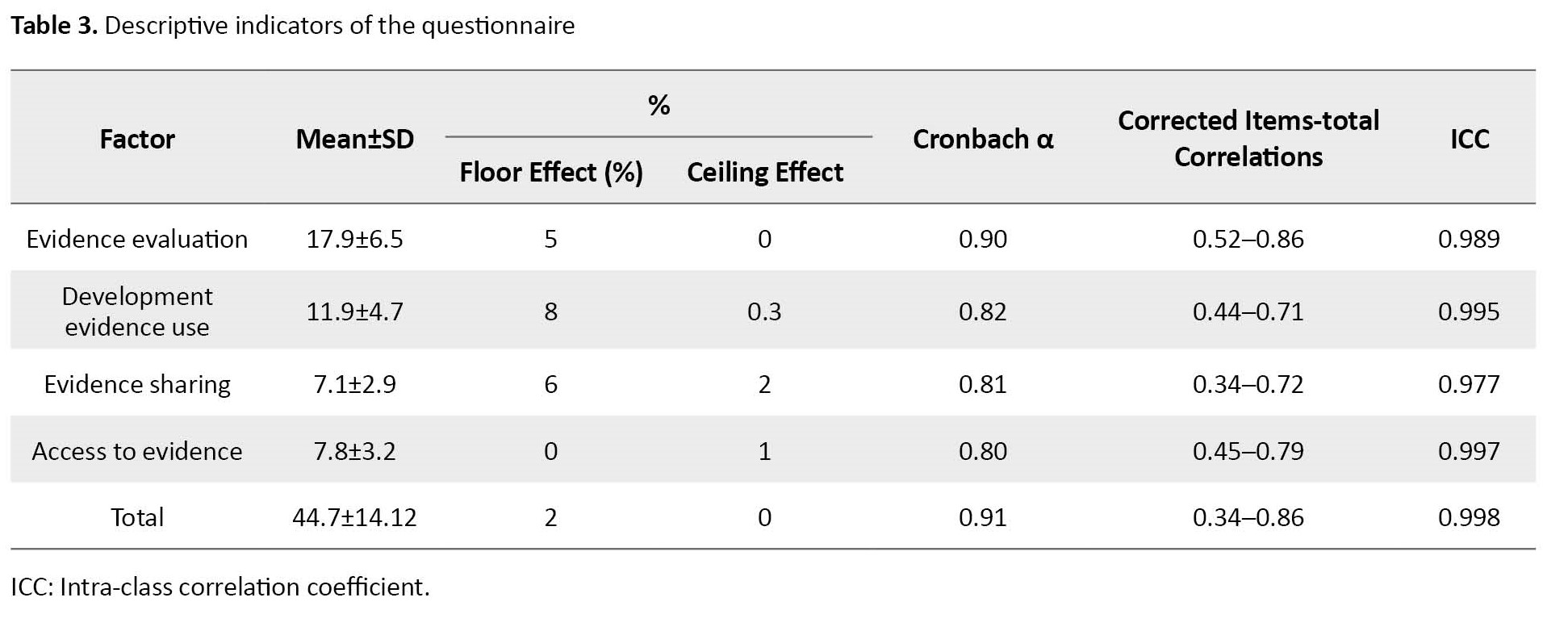
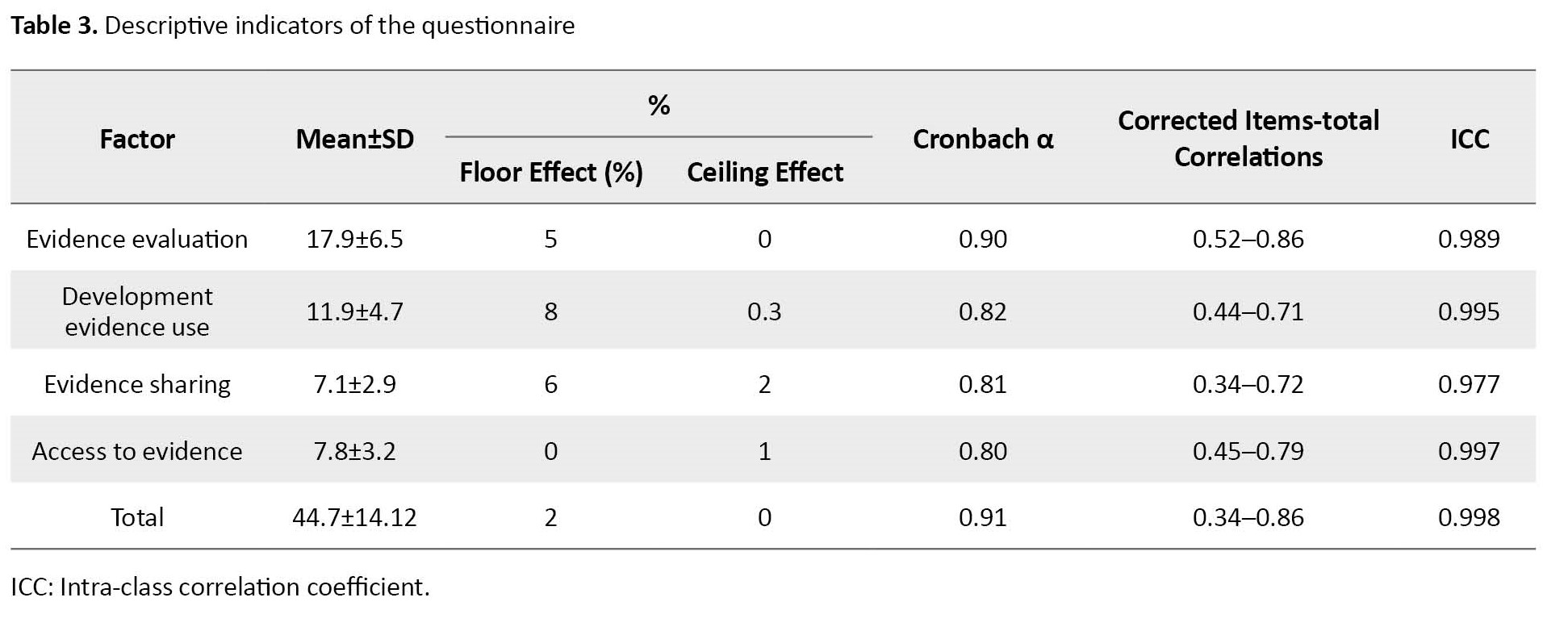
These four factors extracted based on eigenvalues and scree plot (Figure 1) could predict 58.308% of the total variances in the scale. The questionnaires were redistributed among 200 nurses, and CFA was performed on 200 returned questionnaires. First, the chi-square goodness of fit test was performed (χ2=381.92, df=129, χ2/df=2.96, P=0.001) to evaluate the model fit. Other indices such as RMSEA, NFI, CFI, PNFI, IFI, and AGFI confirmed the fit value for the final model (RMSEA=0.099, CFI=0.94, NFI=0.92, PNFI=0.77, IFI=0.94, AGFI=0.82). The results showed that CFA based on a 4-factor model obtained from EFA is relatively well-fitted with the obtained data (Figure 2). The Cronbach α determined the scale’s reliability, which was calculated to be 0.91. The reliability of “evidence evaluation,” “development of evidence use,” “evidence sharing,” and “evidence access” was obtained as 0.90, 0.82, 0.81, and 0.80, respectively, by calculating the Cronbach α coefficients. In addition, this questionnaire had excellent test re-test reliability and the intra-class correlation coefficient (ICC), whose values were reported to be 0.996 with a Confidence Interval (CI) of 0.991 to 0.998 and P=0.001. Also, its re-test reliability was equal to 0.85 (Table 3).
Discussion
This methodological study assessed the psychometric properties of the Persian version of the EBP-1 scale in nurses, which showed good psychometric properties. Its Cronbach α was found to be 0.92. However, the Cronbach α coefficients for the original scale of Melnyk et al. [14] and the French version of Verloo et al. [12] were 0.96 and 0.95, respectively. Also, the Cronbach α value for the Czech and Slovak version of the EBP-I scale exceeded 0.90 [23]. In addition, the Cronbach α value for the German version of the EBP-I scale was 0.87 [24].
The construct validity of the EBP-I scale showed a significant inconsistency among 4 factors with high values in this study. Using factor analysis, the structure of the four factors was determined as follows: “Evidence evaluation,” “development of evidence use,” “evidence sharing,” and “evidence access.” However, in the German version, a single construct in EBP implementation was measured in 5 dimensions; use of EBP, scientific research and analysis, sharing of evidence knowledge, sharing and use of evidence-based guidelines, and practice change process) [24], which our study was almost aligned with it. Of course, the item “generated a PICO question about my clinical practice” was not correlated with other items and was deleted in the German-language version. Therefore, the principal component analysis evaluated the underlying structure of the 17 items in the German-language translation of the EBP-I scale. However, Melnyk et al. [14] reported that the main EBP-I scale is a 1-factor structure scale, and Verloo’s study [12] reported a 2-factor structure in the French version of this scale. This inconsistency between the present study and the above studies can be explained by the fact that it is necessary to reduce the items (remove the redundant ones) in cases where the factor load of the items is high, and the Cronbach α value is more than 0.95 [25]. In addition, the low variance between items on the EBP-I scale causes a floor effect [12].
Since the statistical population of the present study consisted of only clinical nurses working in hospitals, care should be exercised to generalize the results to other samples. In the studies of Melnyk [14] and Verloo [12], in addition to nurses from Bachelor to doctorate, diploma nurses and qualified health service providers participated; in Zeleníková’s study [23], the research samples were nursing students. Because participation in the study was voluntary, most participants might not already hold a positive perception of EBP. Also, the participants had self-evaluated their knowledge of EBP, and these items could potentially impact the results of the present study.
However, no Persian questionnaire has yet evaluated EBP implementation in nurses, and the existence of such a reliable tool can be beneficial in future studies. In addition, the number of items in this questionnaire is low. It is well established that excessive survey length can increase respondent burden, reduce the quality of data collected, and increase non-response bias [13]. Using the EBP-I scale, nurses who need training are identified, which can play an important role in improving the practical knowledge of nurses and patient-centered care.
According to the results of this study, the Persian version of the EBP-I scale has acceptable reliability and validity. In addition, the number of items in this questionnaire is low. Therefore, it can be used to measure EBP implementation in Iranian nurses and identify groups of nurses who need special interventions for EBP.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Babol Branch, Islamic Azad University (Code: IR.IAU.BABOL.REC.1401.001). All participants signed the informed consent form.
Funding
This study was financially supported by the Islamic Azad University, Babol Branch (Grand No.: 1560012150003).
Authors' contributions
Conceptualization and data interpretation: Abbas Ebadi and Ommolbanin Zare; Data collection: Ommolbanin Zare; Data analysis: Abbas Ebadi; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the Research Deputy of Babol Branch, Azad University for funding this research project.
References
Evidence-based practice (EBP) in nursing is a framework for clinical practice that integrates the best available scientific evidence with nurse expertise and patient preferences to make healthcare decisions for individual patients. Nurses are the largest group of healthcare providers who play an essential role in ensuring better services to promote healthcare. Nurses must provide high-quality, safe, effective, fast, and patient-centered care. Knowledge of research and evidence-based care is integral to nursing practice [1-3].
This approach has been proposed to provide the best services for patients. The healthcare system is facing the challenge of providing consistent and high-quality services. If EBP is implemented and used properly in healthcare centers, it will help improve overall patient care [4].
Ongoing advances in medical science show that the effectiveness of nurses’ knowledge and the life span of information is short, and previously learned content is becoming increasingly obsolete. However, these problems can be overcome through EBP, which helps healthcare providers make sound decisions and eliminating outdated knowledge’s effects. EBP opens a window to modernity and helps healthcare providers enjoy a secure practice [5].
EBP is one of the main needs of health systems of the 21 th century [6]. For the quality of nursing care to be continuously improved, new research-based scientific evidence must be regularly used in clinical practice [7]. Most healthcare professionals have a positive attitude toward EBP but lack enough knowledge and skills to implement it [8]. In Asian countries, including Saudi Arabia, the implementation rate of EBP is 14% [9], and in Oman, attitude 4.07±1.34, knowledge 3.99±1.26, the lowest mean 3.84±1.41 related to the implementation of EBP was reported [10]. In Iran, the implementation of EBP is low [11]. The EBP implementation (EBP-I) scale can be used to evaluate the effectiveness of organizational strategies to increase healthcare professionals’ trust in EBP and support its use and implementation [12].
There are three valid and reliable scales to measure the critical concepts in the ARCC (advancing research and clinical practice through close collaboration) model: 1) The organizational culture and readiness scale for widespread EBP system integration, 2) The EBP beliefs scale, and 3) The EBP implementation scale. These three scales have been widely used in research and evidence-based quality improvement projects [13]. Many healthcare centers use EBP-I as a key tool to provide better and safer healthcare. A literature review reveals that the baseline assessments of EBP-I in the daily practice of healthcare providers were designed by Melnyk et al., and its psychometric properties were assessed in 2008 [13, 14]. However, EBP has not been psychometrically tested in Iran. There is scant research on the implementation of EBP in the healthcare community. EBP implementation (EBP-I) requires tools to assess the status quo and the effectiveness of interventions [15]. Due to the importance of EBP and the lack of appropriate measurement tools, this study assessed the psychometric properties of the Persian version of the EBP-I questionnaire in nurses.
Materials and Methods
This research is a methodological and cross-sectional descriptive analytical study conducted in the cities of Mazandaran Province in northern Iran from February to April 2022. The sample size was estimated based on the number of items in the tool. The minimum sample size required for exploratory analysis is 3 to 10 samples per item [16]; thus, we needed 220 participants.
We employed the multi-stage cluster sampling method to choose the study samples. Initially, a list of all cities in Mazandaran Province was prepared, from which 4 cities were randomly selected. Then, 3 hospitals from each city were randomly selected, and 5 wards or more were randomly selected from each hospital. With a probability of 20% dropout, a sample of 220 people was finally selected, and the study data were collected. The inclusion criteria were being a clinical nurse and being willing to complete the questionnaire. Because 20 questionnaires were incomplete and were excluded, 200 completed questionnaires were analyzed.
Demographic questionnaires and the Persian version of EBP-I were used in this study. The demographic questionnaire consisted of personal information (age, gender, level of education and work experience). The Persian version of the EBP-I questionnaire consists of 18 items scored on a 5-point Likert scale so that the options of 0, 1-3, 4-5, 6-7, and 8≤ were assigned a score of 0 to 4, respectively. The total score for this scale ranges from 0 to 72, with higher scores indicating greater implementation of this scale in clinical practice.
After obtaining permission from the original designer, the questionnaire was translated from English to Persian by an English-language expert and then back-translated into English using the forward-backward procedure according to guidelines [17]. Finally, the research team compared the Persian and English versions and prepared the final Persian version. Also, the original designer approved the English back-translation.
To evaluate the face and content validity of the tool, 10 experts specialized in Nursing and the EBP field in the Department of Nursing, Shahid Beheshti University of Medical Sciences, were selected and asked to read the questionnaire carefully and comment on the quality of the questionnaire items in terms of the difficulty, relevance, and clarity of the questions. After modifications based on their opinions, the content validity index (CVI) was calculated. The relevancy of each of the 18 items was rated by experts based on a 4-point Likert scale as (1 irrelevant, 2 somewhat relevant, 3 relevant, and 4 completely relevant). To calculate the CVI score for each item, the number of experts who gave each item a score of 3 and 4 was divided by their total number. A CVI score above 0.79 is considered appropriate, while one ranging from 0.70 to 0.79 must be reconsidered and revised. Items with a score below 0.70 were removed [18].
Data were analyzed using SPSS software, version 18 and LISREL software version 8.8. The reliability of the questionnaire was assessed using the Cronbach α coefficient to determine the internal consistency of the EBP-I questionnaire. A Cronbach α coefficient of 0.7 to 0.9 indicates good reliability [19]. The test re-test method was used to determine the repeatability of the EBP-I questionnaire. The interval between two tests is suggested from two weeks to one month [20]. For this purpose, 30 nurses completed the EBP-I questionnaire twice at a two-week interval.
To evaluate the scale’s construct validity, exploratory factor analysis (EFA) was used to extract the latent factors. At this stage, latent factors were extracted, and the Kaiser-Meyer-Olkin (KMO) index and Bartlett’s test were calculated. KMO values ranging from 0.70 to 0.80 and 0.80 to 0.90 were considered good and excellent, respectively [21].
Latent factors were extracted with maximum likelihood using Promax rotation and Scree diagrams. The minimum factor load was considered 0.3 [22]. Usually, the sample size used for Confirmatory Factor Analysis (CFA) is not less than 200 people [16], so 200 new samples of hospital nurses were selected by multi-stage random sampling with the same inclusion criteria. CFA was performed on 200 questionnaires. At this stage, the goodness-of-fit indexes from this analysis are reported. These are extracted factors with CFA, consisting of root mean squares error of approximation (RMSEA), normed fit index (NFI), comparative fit index (CFI), parsimony normed fit index (PNFI), incremental fit index (IFI), and adjusted goodness of fit index (AGFI). These were used to evaluate the fitness of the model.
Results
The participants in EFA and CFA were nurses, including 48 and 55 men and 152 and 145 women with a Mean±SD age of 42.64±7.58 and 41.75±5.65 years with an age range of 36 to 50 years, respectively. Most nurses in EFA and CFA (44% and 46.5%) had up to 10 years and less work experience and had a Bachelor’s degree (79% and 71.5%), respectively. Table 1 presents the demographic characteristics of the two selected samples.
The scale’s qualitative face and content validity was confirmed after reviewing the opinions of highly qualified nurses and experts about it. The CVI results indicated that all items had a CVI score higher than 0.79 and were considered appropriate. All items scored 1 in the 3 criteria of relevancy, simplicity, and clarity, and only 5 items (6, 10, 11, 13, and 18) scored 0.8 in the criteria of clarity. In total, 18 items were maintained in the research instrument based on the coefficient of impact (>1.5), content validity ratio (>0.62), and content validity index (>0.7).
In performing EFA, KMO showed the adequacy of sampling (KMO=0.87). The Bartlett’s test of sphericity was statistically significant (χ2=2063.645, df=153, P=0.001). Based on EFA, four factors of evidence evaluation (items 1, 2, 3, 4, 5, 6, 7), development of evidence use (14, 15, 16, 17, and 18), evidence sharing (items 8, 9, and 10), and evidence access (items 11, 12, and 13) obtained eigenvalues of 3.798, 2.652, 2.180, and 1.865, respectively (Table 2).
These four factors extracted based on eigenvalues and scree plot (Figure 1) could predict 58.308% of the total variances in the scale. The questionnaires were redistributed among 200 nurses, and CFA was performed on 200 returned questionnaires. First, the chi-square goodness of fit test was performed (χ2=381.92, df=129, χ2/df=2.96, P=0.001) to evaluate the model fit. Other indices such as RMSEA, NFI, CFI, PNFI, IFI, and AGFI confirmed the fit value for the final model (RMSEA=0.099, CFI=0.94, NFI=0.92, PNFI=0.77, IFI=0.94, AGFI=0.82). The results showed that CFA based on a 4-factor model obtained from EFA is relatively well-fitted with the obtained data (Figure 2). The Cronbach α determined the scale’s reliability, which was calculated to be 0.91. The reliability of “evidence evaluation,” “development of evidence use,” “evidence sharing,” and “evidence access” was obtained as 0.90, 0.82, 0.81, and 0.80, respectively, by calculating the Cronbach α coefficients. In addition, this questionnaire had excellent test re-test reliability and the intra-class correlation coefficient (ICC), whose values were reported to be 0.996 with a Confidence Interval (CI) of 0.991 to 0.998 and P=0.001. Also, its re-test reliability was equal to 0.85 (Table 3).
Discussion
This methodological study assessed the psychometric properties of the Persian version of the EBP-1 scale in nurses, which showed good psychometric properties. Its Cronbach α was found to be 0.92. However, the Cronbach α coefficients for the original scale of Melnyk et al. [14] and the French version of Verloo et al. [12] were 0.96 and 0.95, respectively. Also, the Cronbach α value for the Czech and Slovak version of the EBP-I scale exceeded 0.90 [23]. In addition, the Cronbach α value for the German version of the EBP-I scale was 0.87 [24].
The construct validity of the EBP-I scale showed a significant inconsistency among 4 factors with high values in this study. Using factor analysis, the structure of the four factors was determined as follows: “Evidence evaluation,” “development of evidence use,” “evidence sharing,” and “evidence access.” However, in the German version, a single construct in EBP implementation was measured in 5 dimensions; use of EBP, scientific research and analysis, sharing of evidence knowledge, sharing and use of evidence-based guidelines, and practice change process) [24], which our study was almost aligned with it. Of course, the item “generated a PICO question about my clinical practice” was not correlated with other items and was deleted in the German-language version. Therefore, the principal component analysis evaluated the underlying structure of the 17 items in the German-language translation of the EBP-I scale. However, Melnyk et al. [14] reported that the main EBP-I scale is a 1-factor structure scale, and Verloo’s study [12] reported a 2-factor structure in the French version of this scale. This inconsistency between the present study and the above studies can be explained by the fact that it is necessary to reduce the items (remove the redundant ones) in cases where the factor load of the items is high, and the Cronbach α value is more than 0.95 [25]. In addition, the low variance between items on the EBP-I scale causes a floor effect [12].
Since the statistical population of the present study consisted of only clinical nurses working in hospitals, care should be exercised to generalize the results to other samples. In the studies of Melnyk [14] and Verloo [12], in addition to nurses from Bachelor to doctorate, diploma nurses and qualified health service providers participated; in Zeleníková’s study [23], the research samples were nursing students. Because participation in the study was voluntary, most participants might not already hold a positive perception of EBP. Also, the participants had self-evaluated their knowledge of EBP, and these items could potentially impact the results of the present study.
However, no Persian questionnaire has yet evaluated EBP implementation in nurses, and the existence of such a reliable tool can be beneficial in future studies. In addition, the number of items in this questionnaire is low. It is well established that excessive survey length can increase respondent burden, reduce the quality of data collected, and increase non-response bias [13]. Using the EBP-I scale, nurses who need training are identified, which can play an important role in improving the practical knowledge of nurses and patient-centered care.
According to the results of this study, the Persian version of the EBP-I scale has acceptable reliability and validity. In addition, the number of items in this questionnaire is low. Therefore, it can be used to measure EBP implementation in Iranian nurses and identify groups of nurses who need special interventions for EBP.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Babol Branch, Islamic Azad University (Code: IR.IAU.BABOL.REC.1401.001). All participants signed the informed consent form.
Funding
This study was financially supported by the Islamic Azad University, Babol Branch (Grand No.: 1560012150003).
Authors' contributions
Conceptualization and data interpretation: Abbas Ebadi and Ommolbanin Zare; Data collection: Ommolbanin Zare; Data analysis: Abbas Ebadi; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the Research Deputy of Babol Branch, Azad University for funding this research project.
References
- Al-Lenjawi B, Kunjavara J, Hassan N, Mannethodi K, Martinez E, Joy GV, et al. Evidence-based practice among critical care nurse’s/midwives in Qatar. Open J Nurs. 2022; 12(1):42-59. [DOI:10.4236/ojn.2022.121004]
- Shayan SJ, Kiwanuka F, Nakaye Z. Barriers associated with evidence-based practice among nurses in low-and middle-income countries: A systematic review. Worldviews Evid Based Nurs. 2019; 16(1):12-20. [DOI:10.1111/wvn.12337] [PMID]
- Wakibi S. The evidence available to teach evidence-based nursing practice by nurse educators [Doctoral dissertation]. Saskatchewan: University of Saskatchewan; 2019. [Link]
- Alatawi M, Aljuhani E, Alsufiany F, Aleid K, Rawah R, Aljanabi S, et al. Barriers of implementing evidence-based practice in nursing profession: A literature review. Am J Nurs Sci. 2020; 9(1):35-42.[DOI:10.11648/j.ajns.20200901.16]
- Mohammadi MM, Poursaberi R, Salahshoor MR. Evaluating the adoption of evidence-based practice using Rogers’s diffusion of innovation theory: A model testing study. Health Promot Perspect. 2018; 8(1):25-32. [DOI:10.15171/hpp.2018.03] [PMID]
- Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormack B. What counts as evidence in evidence-based practice? J Adv Nurs. 2004; 47(1):81-90. [DOI:10.1111/j.1365-2648.2004.03068.x] [PMID]
- Flodgren G, Rojas-Reyes MX, Cole N, Foxcroft DR. Effectiveness of organisational infrastructures to promote evidence-based nursing practice. Cochrane Database Syst Rev. 2012; 2012(2):CD002212. [PMID]
- Weng YH, Kuo KN, Yang CY, Lo HL, Chen C, Chiu YW. Implementation of evidence-based practice across medical, nursing, pharmacological and allied healthcare professionals: A questionnaire survey in nationwide hospital settings. Implement Sci. 2013; 8:112. [DOI:10.1186/1748-5908-8-112] [PMID]
- Abuhasheesh M, AbuRuz M. Knowledge, attitude and practice of nurses towards evidence-based practice at Al-Medina, KSA. Jordan Med J. 2017; 51(2):47-56. [Link]
- AbuRuz ME, Hayeah HA, Al-Dweik G, Al-Akash HY. Knowledge, attitudes, and practice about evidence-based practice: A Jordanian study. Health Sci J. 2017; 11:2. [Link]
- Valizadeh L, Zamanzadeh V, Babaei N, Avazeh M. [Challenges and strategies for implementing evidence-based practice in nursing: A systematic review (Persian)]. Res Med Educ. 2020; 12(3):55-67. [Link]
- Verloo H, Desmedt M, Morin D. Adaptation and validation of the Evidence-Based Practice Belief and Implementation scales for French-speaking Swiss nurses and allied healthcare providers. J Clin Nurs. 2017; 26(17-18):2735-43. [DOI:10.1111/jocn.13786] [PMID]
- Melnyk BM, Hsieh AP, Gallagher-Ford L, Thomas B, Guo J, Tan A, et al. Psychometric Properties of the Short Versions of the EBP Beliefs Scale, the EBP Implementation Scale, and the EBP Organizational Culture and Readiness Scale. Worldviews Evid Based Nurs. 2021; 18(4):243-50. [DOI:10.1111/wvn.12525] [PMID]
- Melnyk BM, Fineout-Overholt E, Mays MZ. The evidence-based practice beliefs and implementation scales: Psychometric properties of two new instruments. Worldviews Evid Based Nurs. 2008; 5(4):208-16. [DOI:10.1111/j.1741-6787.2008.00126.x] [PMID]
- Pereira F, Pellaux V, Verloo H. Beliefs and implementation of evidence-based practice among community health nurses: A cross-sectional descriptive study J Clin Nurs. 2018; 27(9-10):2052-61. [DOI:10.1111/jocn.14348] [PMID]
- Plichta SB, Kelvin EA, Munro's statistical methods for health care research. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2013. [Link]
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000; 25(24):3186-91. [DOI:10.1097/00007632-200012150-00014] [PMID]
- Polit DF, Beck CT. Essentials of nursing research: Appraising evidence for nursing practice. Philadelphia: Lippincott Williams & Wilkins; 2010. [Link]
- DeVellis RF. Scale Development: Theory and applications. Thousand Oaks, CA: Sage; 2017. [Link]
- Grove SK, Gray JR. Understanding nursing research building: An evidence-based practice. Amsterdam: Elsevier Health Sciences; 2022. [Link]
- Nia HS, Ebadi A, Lehto RH, Mousavi B, Peyrovi H, Chan YH. Reliability and validity of the persian version of templer death anxiety scale-extended in veterans of Iran-Iraq warfare. Iran J Psychiatry Behav Sci. 2014; 8(4):29-37. [PMID]
- Çokluk Bökeoğlu Ö, Koçak D. Using Horn's parallel analysis method in exploratory factor analysis for determining the number of factors. Educ Sci Theory Pract. 2016; 16(2):537-51. [Link]
- Zeleníková R, Gurková E, Žiaková K, Tomagová M, Jarošová D, Fineout-Overholt E. Psychometric properties of the Slovak and Czech versions of the evidence-based practice beliefs and implementation scales. Worldviews Evid Based Nurs. 2016; 13(2):139-52.[DOI:10.1111/wvn.12128] [PMID]
- Kerwien-Jacquier E, Verloo H, Pereira F, Peter KA. Adaptation and validation of the evidence-based practice beliefs and implementation scales into German. Nurs Open. 2020; 7(6):1997-2008.[DOI:10.1002/nop2.593] [PMID]
- Streiner DL, Norman GR, Cairney J. Health measurement scales: A practical guide to their development and use. Oxford: Oxford University Press, USA; 2015. [DOI:10.1093/med/9780199685219.001.0001]
Article Type : Research |
Subject:
General
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |