Sat, Apr 27, 2024
Volume 34, Issue 2 (2-2024)
JHNM 2024, 34(2): 117-124 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ranjbari N, Masoumpoor A, Shirinabadi Farahani A, Mahdizadeh-Shahri M, Nasiri M. The Effect of Modulating Environmental Stimuli on Pain Experience in Premature Infants During Peripherally Inserted Central Catheter-port Implantation. JHNM 2024; 34 (2) :117-124
URL: http://hnmj.gums.ac.ir/article-1-2302-en.html
URL: http://hnmj.gums.ac.ir/article-1-2302-en.html
Narges Ranjbari1 

 , Anahita Masoumpoor *
, Anahita Masoumpoor * 

 2, Azam Shirinabadi Farahani3
2, Azam Shirinabadi Farahani3 

 , Maraym Mahdizadeh-Shahri4
, Maraym Mahdizadeh-Shahri4 

 , Maliheh Nasiri4
, Maliheh Nasiri4 




 , Anahita Masoumpoor *
, Anahita Masoumpoor * 

 2, Azam Shirinabadi Farahani3
2, Azam Shirinabadi Farahani3 

 , Maraym Mahdizadeh-Shahri4
, Maraym Mahdizadeh-Shahri4 

 , Maliheh Nasiri4
, Maliheh Nasiri4 


1- Nursing (MSc), Student Research Committee, School of Nursing & Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Instructor, Department of Pediatric Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran. , anahitakasra@yahoo.com
3- Assistant Professor, Department of Pediatric and Reproductive Health, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Assistant Professor, Department of Basic Sciences, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences. Tehran, Iran.
2- Instructor, Department of Pediatric Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran. , anahitakasra@yahoo.com
3- Assistant Professor, Department of Pediatric and Reproductive Health, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Assistant Professor, Department of Basic Sciences, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences. Tehran, Iran.
Full-Text [PDF 614 kb]
(86 Downloads)
| Abstract (HTML) (290 Views)
Full-Text: (76 Views)
Introduction
Premature birth is the leading cause of hospitalization in neonatal intensive care units (NICUs) [1]. Premature infants experience several painful diagnostic or therapeutic procedures in the NICU, such as intravenous catheterization, venipuncture for blood sampling, gastric nasal tube insertion, endotracheal tube insertion, and peripherally inserted central catheters (PICCs). PICCs are being placed routinely to provide nutrition and medications in NICUs, especially for preterm infants [2-4]. Preterm infants are exposed to frequent painful procedures and agitating stimuli during the many weeks of their stay in the NICU [5]. Noise, pain, and the neonatal intensive care environment can also affect infant neurodevelopment [6]. However, the white noise and lullabies played to premature babies during the blood collection effectively reduced pain [7]. Preterm infants are uniquely vulnerable to early toxic stress exposure and suboptimal neurodevelopmental outcomes while being in the NICUs [8]. Nociceptive signals cause a cascade of physical and behavioral reactions that, alone or in combination, can be observed and used to assess the presence and intensity of pain [9]. The effects of these stresses show up even in the following years of an infant’s life with neurological dysfunctions such as memory, attention, and perception [10, 11]. These infants may need a PICC during a relatively long period of hospitalization to receive total parental nutrition and avoid recurrent venipuncture [10, 12].
PICCs are inserted for various purposes in the NICU, such as administering fluids, blood products, total parental nutrition, and medications [12-14]. To execute PICC better in newborns, it is imperative to use cluster nursing interventions properly and prevent catheter-related bloodstream infection [2, 14, 15]. All treatment policies and strategies should be based on the fact that the infant should never be exposed to relievable pain [16]. A proper interpretation of pain-related behaviors in a preterm infant is crucial. PICC placement is a painful procedure and, like other painful procedures performed on infants, requires non-pharmacological and pharmacological methods to relieve the pain [3]. These methods are helpful, uncomplicated, and cost-effective. Oral sucrose, pacifiers, skin-to-skin contact, containment, and swaddling are the methods most verified in recent years [17, 18].
Pain in the neonate is often challenging to assess but essential to control. Both inadequate pain control and over-utilization of opioids can have long-term consequences, including poor developmental outcomes [19].
Accordingly, adjusting auditory, visual, tactile, olfactory, and taste stimuli in the neonatal care unit is one of the fundamental principles of preterm infant care. The relevant guidelines suggest strategies to control stimuli in the NICU and provide an environment consistent with the normal conditions of neural development [20, 21]. Controlling light and noise levels in the NICU environment is an essential developmental care intervention promoting preterm infants’ development [22]. Preterm infants are vulnerable humans, requiring much care and attention. They may be exposed to irregular noise, light, and odor in the NICUs for several weeks or months. Controlling ambient light and sound are two vital strategies for providing a context that contributes to an infant’s behavioral neurodevelopment. Light and sound are potential sources of harm to the baby. Excessive light can damage the retina, disrupt the circadian rhythm and sleep pattern, and impair the infant’s growth. Physiological changes in response to sounds, such as fluctuations in heart rate, blood pressure, respiration rate, and oxygen saturation, are some of the effects of noise on the baby [20, 23, 24]. Environmental stimuli modification may increase the effectiveness of supportive interventions for premature infants. Accordingly, this study aimed to investigate the impact of reducing environmental stimuli on the pain caused by PICC insertion.
Materials and Methods
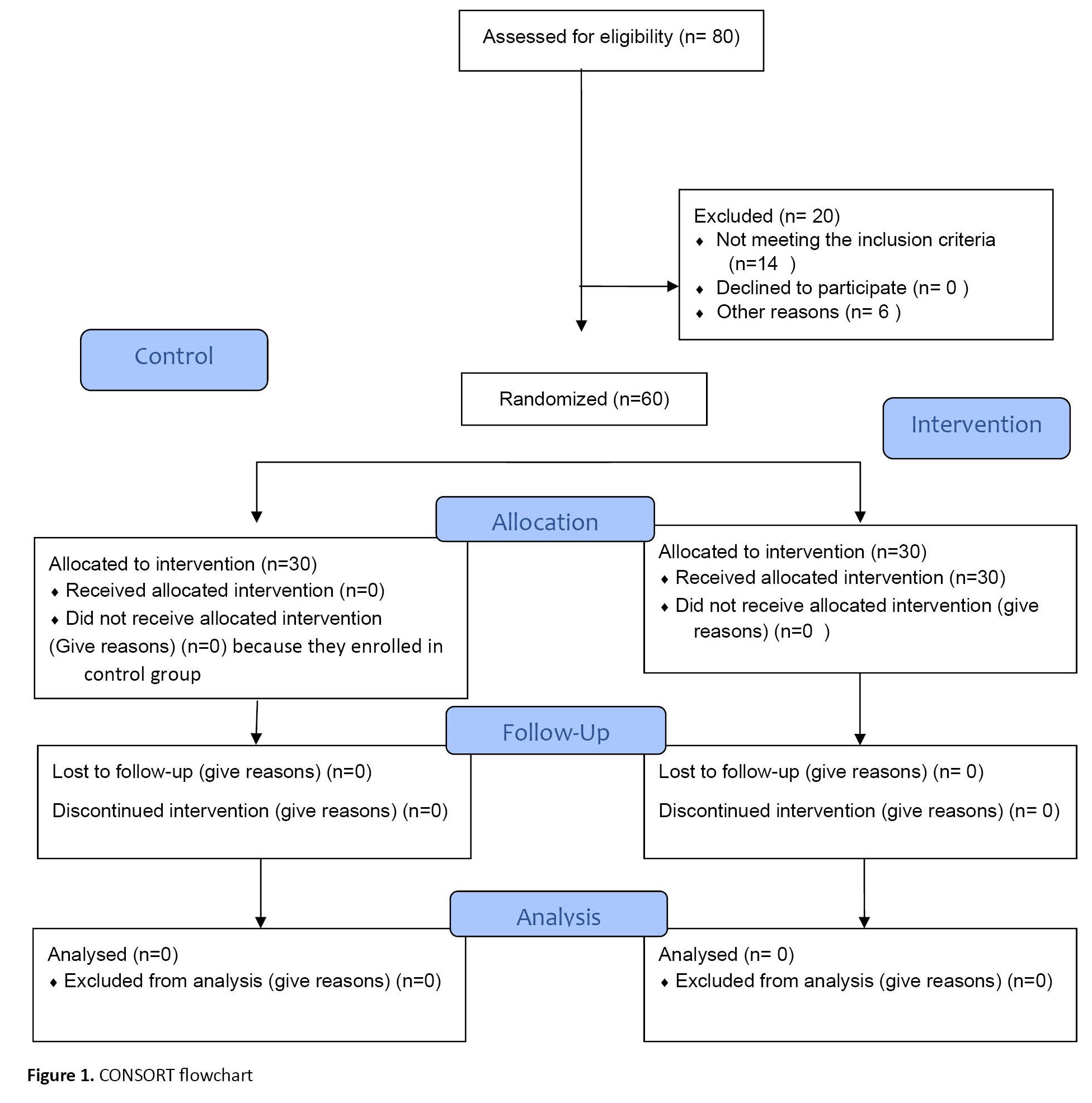
The present study was a controlled randomized clinical trial in the NICUs of the two hospitals affiliated with the Ahvaz Jundishapur University of Medical Sciences (AJUMS) in Ahvaz City, Iran. The total number of infants who were candidates for PICC-port catheter was 80, of whom 14 infants were excluded from the study due to exclusion and 6 due to cardiopulmonary resuscitation problems and death. Sixty infants were thus included in the study (30 in the intervention group and 30 in the control group) that was shown in Figure 1. Even numbers were put in the control and odd numbers in the intervention groups. The inclusion criteria of candidate neonates for PICC insertion were the birth gestational age between 28 to 37 weeks, lack of serious congenital disease based on medical documents, and the vital signs being in the normal range when performing the procedure. The exclusion criteria were changes in the infant’s health status during PICC placement, necessitating supportive care, and failure to insert the catheter.
The study instruments included an infant’s demographic and clinical characteristics questionnaire (including sex, type of delivery, intubation, weight, and current diseases) and the premature infant pain profile (PIPP).
The PIPP assessment tool, developed by Ballantyne et al. [25], objectively assesses preterm infants’ responses to acute pain experienced during procedures. It has seven pain indicators, including behavioral (facial expressions: Brow bulge, eye squeeze, and nasolabial furrow), physiological (heart rate and oxygen saturation), and contextual (gestational age and behavioral state) [26, 27]. Each indicator is scored from 0 to 3. The total score ranges from 0 to 21. A score above 12 indicates moderate to severe pain experienced in the neonate. In this study, two raters scored the Persian PIPP for 10 infants separately, and the inter-rater reliability coefficient was obtained as 0.89. Also, the PIPP content validity was measured through the qualitative content validity method by 10 experts (1 methodologist, 2 instrument developing experts, 5 nurses experienced in NICU, and 2 pain care research experts).
In the intervention group, before performing the procedure, the researcher placed a researcher-made blindfold on the infant’s eyes and an earmuff prepared by a medical equipment center dedicated to covering the infant’s ears. The standard earmuffs used in this study was designed for premature infants, especially those hospitalized in NICU, by Nature company in San Carlos, USA. These earmuffs, laid on infants, external ears, diminish the sound intensity to at least 7 dB and the sound pressure level by 50% so that they do not block infants, necessary hearing stimulation for nervous system development. The Y-shape design of Natus company goggles protects babies from phototherapy light. The phototherapy goggles were cut to a small size to cover just the eyes, not the eyebrows. The phototherapy goggles block lights up to 99.9%. These infants also received routine care, such as non-nutritive sucking and containment. Infants in the control group received only routine care, and the researcher measured their pain.
Four times a week, the researcher attended the ward from 7:30 to 19:30, recorded the vital signs of patients who were candidates for PICC procedure, and was present at the bedside. The child’s pain level has only been investigated during PICC insertion. PICC insertion is done in each department by an expert nurse. During the preparation for implantation, the baby was connected to monitoring, an ear plug was placed on the ears, and a blindfold was worn only on the eyelids. The baby’s eyebrows were exposed to measure the amount of eyebrow bulge. Then, the PICC was implanted, and the baby was monitored by two nurses, one of whom was a researcher, and the other checked the heart rate and arterial blood oxygen saturation on the monitor. The pain during the PICC insertion was measured with the PIPP tool when the baby’s eyelids were covered with a cover, but the facial movements of the raised eyebrows, jumping of the nose edges, frown line, and the line around the lips expressed their pain. The pain level was measured until the end of the PICC insertion, and the results were analyzed after the work was completed. The pain amount during PICC insertion was measured in the control group without using blindfolds and earplugs. The samples were 0 to 28-day-old boys and girls candidates for PICC implantation hospitalized due to prematurity and respiratory distress syndrome. The collected data were analyzed using descriptive statistics (i.e. frequency, mean percentage, and standard deviation) and inferential statistics (independent t-test) in SPSS software, version 16. A P<0.05 was considered significant.
Results
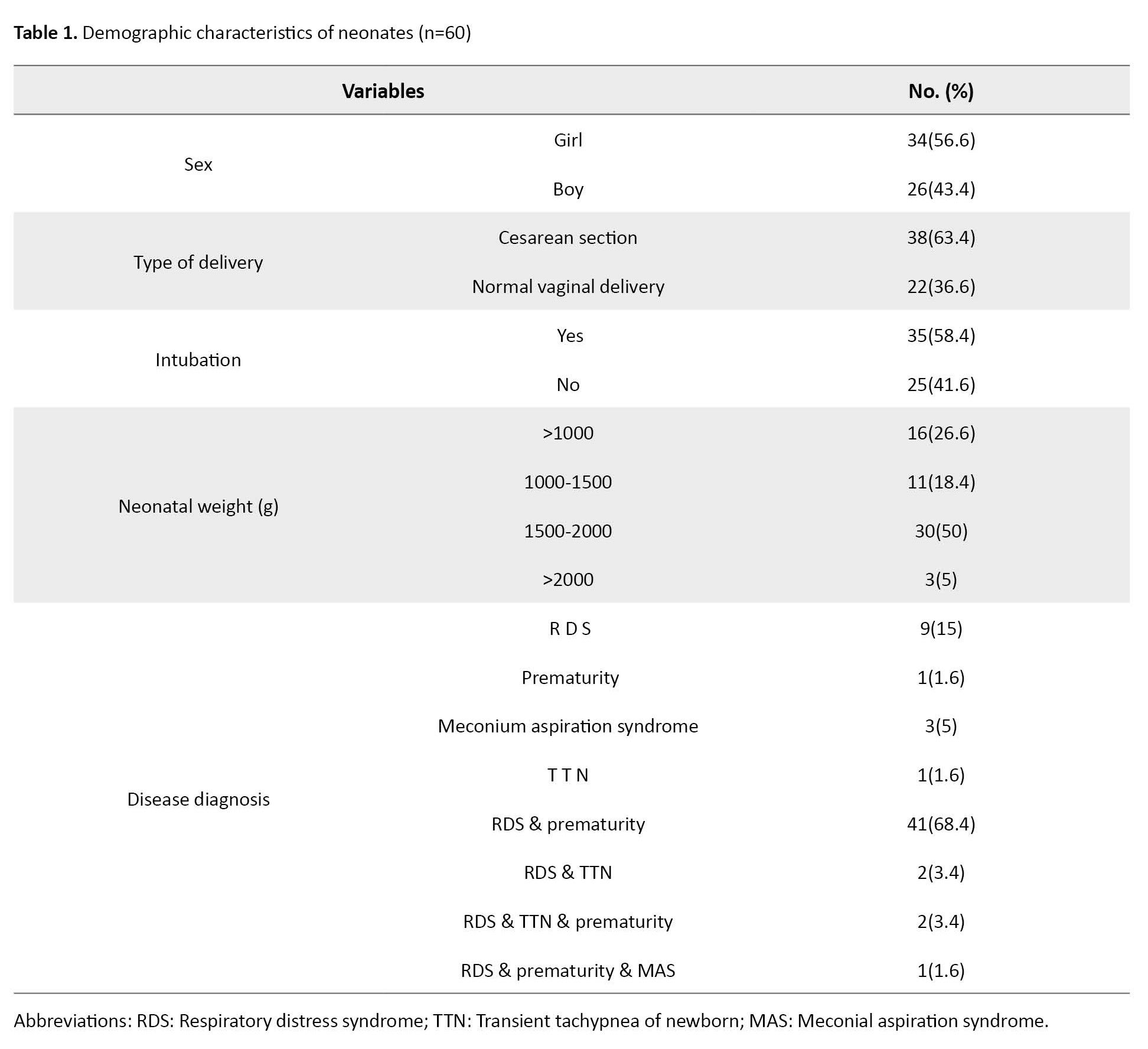
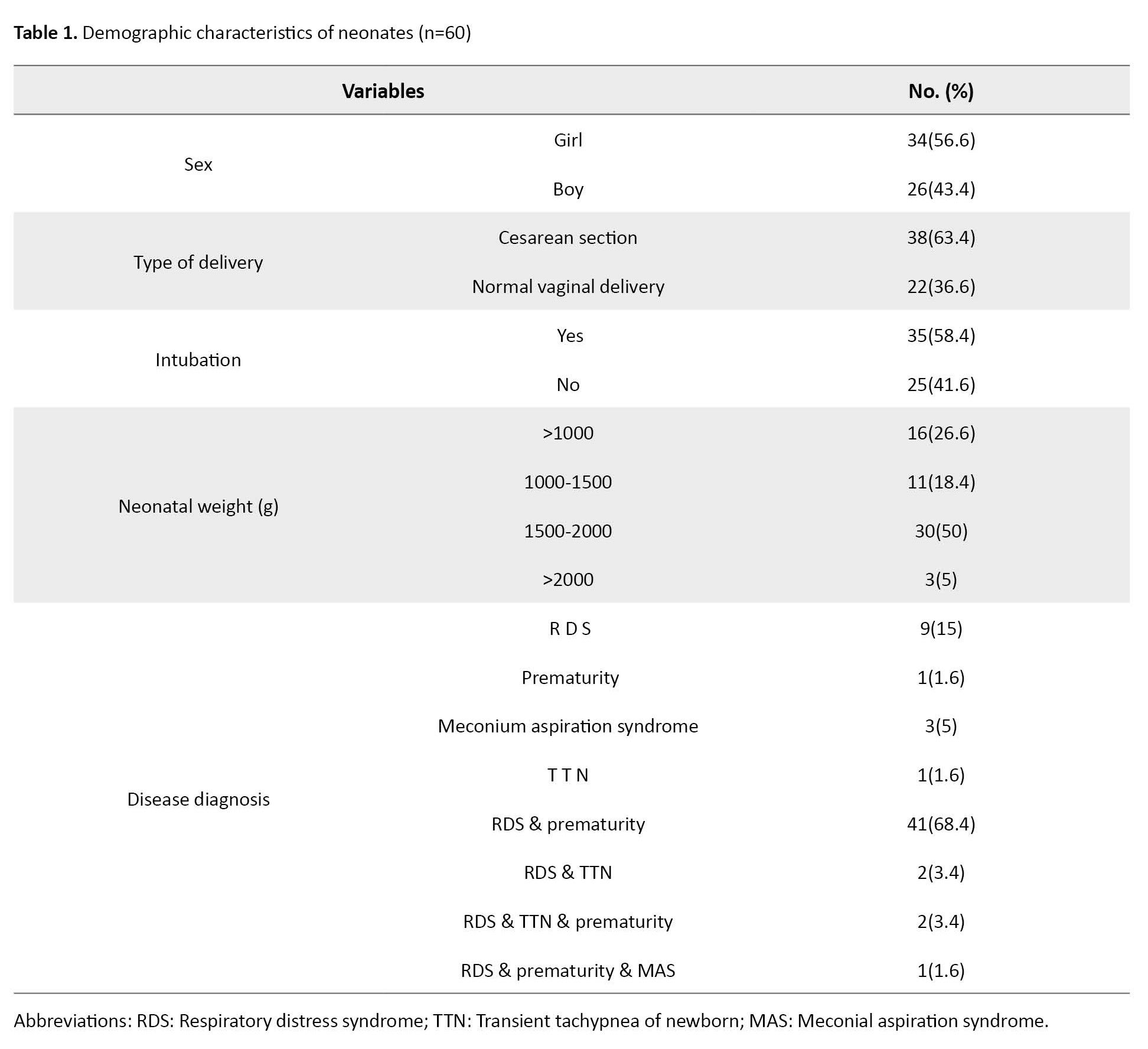
The majority of the studied neonates were female (56.6%), were born through caesarian section, their birth gestational age was between 28 to 31 weeks, their birth weight was between 1501 to 2000 gr, were hospitalized because of prematurity and respiratory distress syndrome, were not intubated, and were the first child of the family (Table 1).
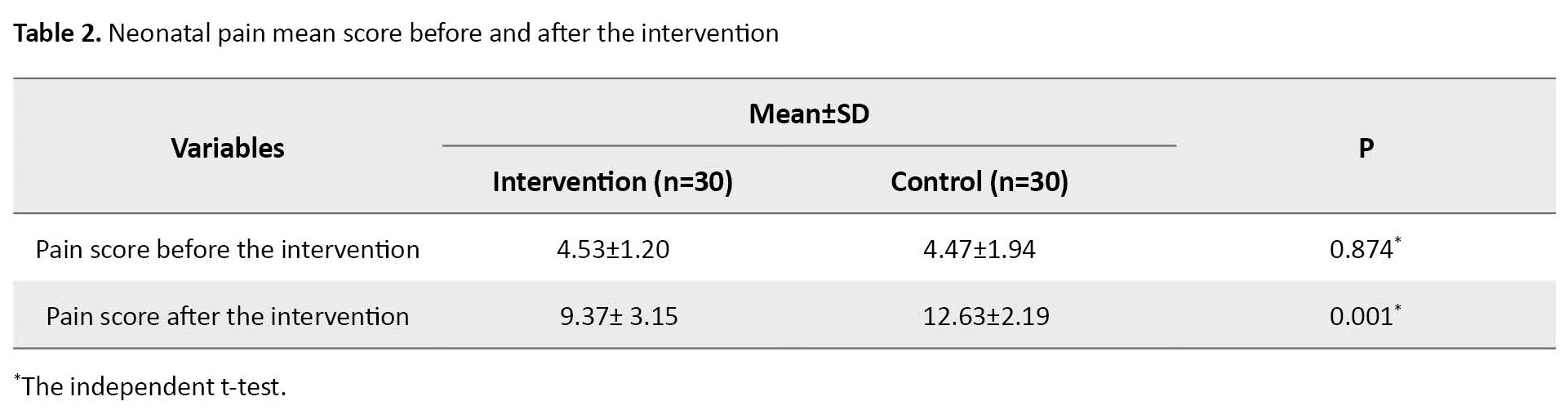
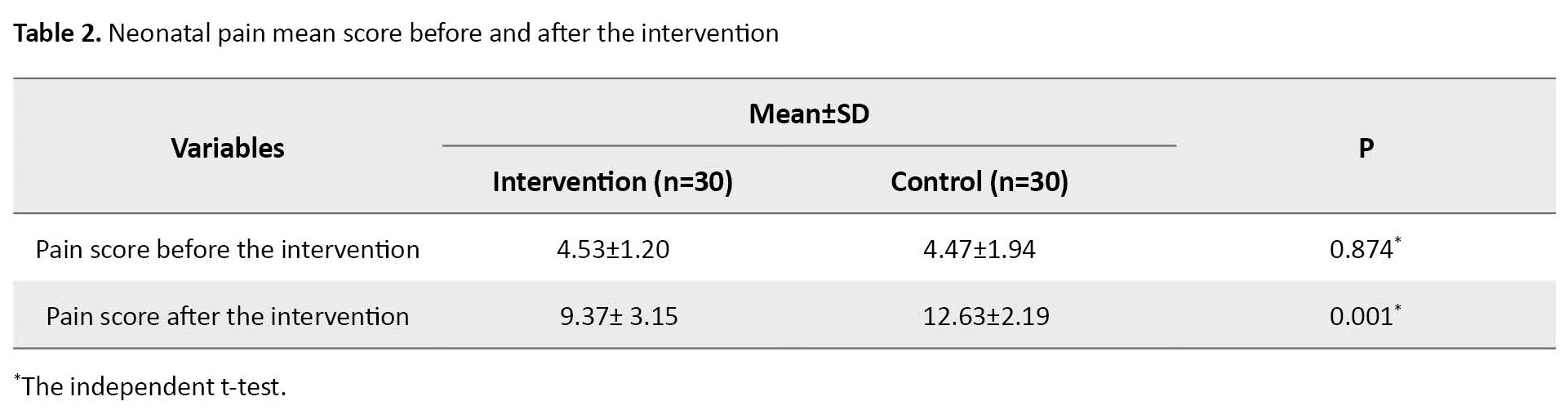
Results of the Kolmogorov-Smirnov test indicated the normal distribution of the PIPP scores; therefore, parametric tests were used in this study. The independent t-test showed no significant difference between the two groups regarding demographic characteristics and the PIPP score. The mean score of PIPP after the intervention was significantly less in the intervention group than in the control group (P=0.001). This result is shown in Table 2.
According to the results of the analysis of covariance, adjusting the environmental stimuli of light and sound was effective on the pain level of the neonate during PICC implantation with an effect size of 0.917.
Discussion
The mean scores before the intervention were 4.48 in the control group and 4.53 in the intervention, indicating the existence of discomfort in neonates even before the beginning of the procedure. In this respect, the results are consistent with other studies. Harrison and McKechnie studied the amount of discomfort during transport on 140 infants using the PIPP. The mean score of the PIPP in premature infants was about 4 to 5, indicating their mild discomfort. Caregiving relationships in the postnatal period are critical to an infant’s development. Preterm infants and their parents face unique challenges in this regard, with infants experiencing separation from their parents, uncomfortable procedures, and increased biological vulnerability. Also, parents face difficulties assuming caregiver roles and increased risk for psychological distress [28]. Received neonates can be exposed to light more than recommended in NICU levels, including extremely bright light [29]. Human cerebellar development occurs late in gestation and is hindered by preterm birth. The fetal development of Purkinje cells, the primary output cells of the cerebellar cortex, is crucial for the structure and function of the cerebellum. However, morphological and electrophysiological features in Purkinje cells at different gestational ages and the effects of the NICU environment on cerebellar development are unexplored [30].
Preterm infants are sensitive to sound peaks and light level variations, with a slightly higher sensitivity to sound peaks. The mechanisms leading to pain behaviors induced by noise and light changes should be evaluated further in the context of preterm infant brain development.
Environmental lighting can affect weight gain and the length of stay in NICUs [31].
Individualized developmental care is an approach to nursing for hospitalized infants. It includes reading the infant’s cues, engaging the parents, and providing a supportive environment [6]. Developmental care practices that mitigate the infant stress experience are promising as modifiable factors that may change the trajectory of neurodevelopmental outcomes in congenital heart disease [32].
In this study, using eye shields and earmuffs during painful procedures significantly reduced pain scores in the intervention group. The results are consistent with some similar studies. According to Mehrnoush et al., conditions caused by neonatal diseases such as respiratory distress and irritability due to central nervous system damage, and neonatal connections such as intravenous catheters, nasogastric tube, nasal continuous positive airway pressure, and routine procedures such as airway suction, and measurement of vital signs, even change position can put the baby in an unpleasant and distressing physical condition [33]. Alemdar et al. showed a significant difference between the mean scores of the neonatal infant pain scale in the intervention and the control groups after intravenous catheter implantation, mainly related to covering the eyes in the intervention groups. They did not find a significant difference between the two groups’ means of neonatal infant pain scale during the procedure [34]. In their other clinical trial, they aimed to investigate the impact of a recorded mother’s voice, breast milk odor, and incubator cover on the pain during peripheral cannulation between the PIPP scores during and after the painful procedure of the two groups [35].
A study that assessed the effect of eye shield versus massage on preterm infants’ pain response during venipuncture showed that in both intervention groups, the PIPP scores were significantly lower compared with the control group [36].
In a randomized clinical trial by Ajam Hassani et al., the researchers used eye shields and earmuffs for the neonates in the intervention group 4 and 2 hours before the oral gastric tube insertion, respectively. The PIPP scores of the intervention group were significantly lower than the control group during and after the procedure [37].
Premature infants are frequently exposed to painful experiences in the NICU due to their relatively lengthy stay and the need for multiple diagnostic and dermatological procedures. In recent decades, much attention has been paid to research on the effectiveness and safety of various pharmacological or non-pharmacological methods on pain caused by procedures performed in neonatal intensive care units [26, 38]. According to the results, modification of light and sound stimuli reduced preterm infants’ pain during PICC implantation.
Comparing the results of this study with similar studies, it is clear that there are still very contradictory results about the effectiveness of reducing environmental stimuli in reducing neonatal pain. The limitation of the present study was its lack of blindness, which affects the generalizability of the results. Educational classes may be helpful and operational. Holding a training class for medical staff, especially nurses, to manage sound and light in the ward and standardize environmental factors such as light and sound in the NICU.
Based on the study, environment modifications are effective, inexpensive, accessible, and safe methods during PICC placement for premature infants in the NICU. Clinical nurses should use this approach to promote neonatal outcomes due to the destructive effect of sound and light on the neural development of the infant and the occurrence of distress symptoms in infants following procedural pain. One of the limitations that prolonged the length of time in this study was that central catheters were not implanted for all infants admitted to the NICU, or some met all the inclusion criteria. However, they were converted in the middle of the way, or sometimes the PICC was inserted when the researcher was not present in the ward, so a long time was spent conducting the study.
Ethical Considerations
Compliance with ethical guidelines
This study was registered at the Iranian Center for Clinical Trials (IRCT) (Code: IRCT640768640768). Also it was approved by the Joint Ethics Committee of Shahid Beheshti University of Medical Sciences (SBMU) (Code: IR.SBMU.PHARMACY.REC.1398.062). The researchers conducted the intervention according to the institutional regulations. Informed consent was obtained from the neonates’ parents after explaining the research objectives and assuring them of the safety of the intervention.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors
Authors' contributions
Conducting research and preparing the first version of the article: Nargess Ranjbari; Designing and supervising the research, participating in writing and editing the article: Anahita Masoumpour; Co-supervising and participating in editing the article: Azam Shirinabadi Farahani; Reviewing and revising the manuscript: Maryam Mahdizadehshahri; Performing expert statistics: Malihe Nasiri; Approve the final version of manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Masoud Dehdashtian and Amir Kamal Hardani for attending NICU in Emam Khomeini and Abouzar hospitals.
References
Premature birth is the leading cause of hospitalization in neonatal intensive care units (NICUs) [1]. Premature infants experience several painful diagnostic or therapeutic procedures in the NICU, such as intravenous catheterization, venipuncture for blood sampling, gastric nasal tube insertion, endotracheal tube insertion, and peripherally inserted central catheters (PICCs). PICCs are being placed routinely to provide nutrition and medications in NICUs, especially for preterm infants [2-4]. Preterm infants are exposed to frequent painful procedures and agitating stimuli during the many weeks of their stay in the NICU [5]. Noise, pain, and the neonatal intensive care environment can also affect infant neurodevelopment [6]. However, the white noise and lullabies played to premature babies during the blood collection effectively reduced pain [7]. Preterm infants are uniquely vulnerable to early toxic stress exposure and suboptimal neurodevelopmental outcomes while being in the NICUs [8]. Nociceptive signals cause a cascade of physical and behavioral reactions that, alone or in combination, can be observed and used to assess the presence and intensity of pain [9]. The effects of these stresses show up even in the following years of an infant’s life with neurological dysfunctions such as memory, attention, and perception [10, 11]. These infants may need a PICC during a relatively long period of hospitalization to receive total parental nutrition and avoid recurrent venipuncture [10, 12].
PICCs are inserted for various purposes in the NICU, such as administering fluids, blood products, total parental nutrition, and medications [12-14]. To execute PICC better in newborns, it is imperative to use cluster nursing interventions properly and prevent catheter-related bloodstream infection [2, 14, 15]. All treatment policies and strategies should be based on the fact that the infant should never be exposed to relievable pain [16]. A proper interpretation of pain-related behaviors in a preterm infant is crucial. PICC placement is a painful procedure and, like other painful procedures performed on infants, requires non-pharmacological and pharmacological methods to relieve the pain [3]. These methods are helpful, uncomplicated, and cost-effective. Oral sucrose, pacifiers, skin-to-skin contact, containment, and swaddling are the methods most verified in recent years [17, 18].
Pain in the neonate is often challenging to assess but essential to control. Both inadequate pain control and over-utilization of opioids can have long-term consequences, including poor developmental outcomes [19].
Accordingly, adjusting auditory, visual, tactile, olfactory, and taste stimuli in the neonatal care unit is one of the fundamental principles of preterm infant care. The relevant guidelines suggest strategies to control stimuli in the NICU and provide an environment consistent with the normal conditions of neural development [20, 21]. Controlling light and noise levels in the NICU environment is an essential developmental care intervention promoting preterm infants’ development [22]. Preterm infants are vulnerable humans, requiring much care and attention. They may be exposed to irregular noise, light, and odor in the NICUs for several weeks or months. Controlling ambient light and sound are two vital strategies for providing a context that contributes to an infant’s behavioral neurodevelopment. Light and sound are potential sources of harm to the baby. Excessive light can damage the retina, disrupt the circadian rhythm and sleep pattern, and impair the infant’s growth. Physiological changes in response to sounds, such as fluctuations in heart rate, blood pressure, respiration rate, and oxygen saturation, are some of the effects of noise on the baby [20, 23, 24]. Environmental stimuli modification may increase the effectiveness of supportive interventions for premature infants. Accordingly, this study aimed to investigate the impact of reducing environmental stimuli on the pain caused by PICC insertion.
Materials and Methods
The present study was a controlled randomized clinical trial in the NICUs of the two hospitals affiliated with the Ahvaz Jundishapur University of Medical Sciences (AJUMS) in Ahvaz City, Iran. The total number of infants who were candidates for PICC-port catheter was 80, of whom 14 infants were excluded from the study due to exclusion and 6 due to cardiopulmonary resuscitation problems and death. Sixty infants were thus included in the study (30 in the intervention group and 30 in the control group) that was shown in Figure 1. Even numbers were put in the control and odd numbers in the intervention groups. The inclusion criteria of candidate neonates for PICC insertion were the birth gestational age between 28 to 37 weeks, lack of serious congenital disease based on medical documents, and the vital signs being in the normal range when performing the procedure. The exclusion criteria were changes in the infant’s health status during PICC placement, necessitating supportive care, and failure to insert the catheter.
The study instruments included an infant’s demographic and clinical characteristics questionnaire (including sex, type of delivery, intubation, weight, and current diseases) and the premature infant pain profile (PIPP).
The PIPP assessment tool, developed by Ballantyne et al. [25], objectively assesses preterm infants’ responses to acute pain experienced during procedures. It has seven pain indicators, including behavioral (facial expressions: Brow bulge, eye squeeze, and nasolabial furrow), physiological (heart rate and oxygen saturation), and contextual (gestational age and behavioral state) [26, 27]. Each indicator is scored from 0 to 3. The total score ranges from 0 to 21. A score above 12 indicates moderate to severe pain experienced in the neonate. In this study, two raters scored the Persian PIPP for 10 infants separately, and the inter-rater reliability coefficient was obtained as 0.89. Also, the PIPP content validity was measured through the qualitative content validity method by 10 experts (1 methodologist, 2 instrument developing experts, 5 nurses experienced in NICU, and 2 pain care research experts).
In the intervention group, before performing the procedure, the researcher placed a researcher-made blindfold on the infant’s eyes and an earmuff prepared by a medical equipment center dedicated to covering the infant’s ears. The standard earmuffs used in this study was designed for premature infants, especially those hospitalized in NICU, by Nature company in San Carlos, USA. These earmuffs, laid on infants, external ears, diminish the sound intensity to at least 7 dB and the sound pressure level by 50% so that they do not block infants, necessary hearing stimulation for nervous system development. The Y-shape design of Natus company goggles protects babies from phototherapy light. The phototherapy goggles were cut to a small size to cover just the eyes, not the eyebrows. The phototherapy goggles block lights up to 99.9%. These infants also received routine care, such as non-nutritive sucking and containment. Infants in the control group received only routine care, and the researcher measured their pain.
Four times a week, the researcher attended the ward from 7:30 to 19:30, recorded the vital signs of patients who were candidates for PICC procedure, and was present at the bedside. The child’s pain level has only been investigated during PICC insertion. PICC insertion is done in each department by an expert nurse. During the preparation for implantation, the baby was connected to monitoring, an ear plug was placed on the ears, and a blindfold was worn only on the eyelids. The baby’s eyebrows were exposed to measure the amount of eyebrow bulge. Then, the PICC was implanted, and the baby was monitored by two nurses, one of whom was a researcher, and the other checked the heart rate and arterial blood oxygen saturation on the monitor. The pain during the PICC insertion was measured with the PIPP tool when the baby’s eyelids were covered with a cover, but the facial movements of the raised eyebrows, jumping of the nose edges, frown line, and the line around the lips expressed their pain. The pain level was measured until the end of the PICC insertion, and the results were analyzed after the work was completed. The pain amount during PICC insertion was measured in the control group without using blindfolds and earplugs. The samples were 0 to 28-day-old boys and girls candidates for PICC implantation hospitalized due to prematurity and respiratory distress syndrome. The collected data were analyzed using descriptive statistics (i.e. frequency, mean percentage, and standard deviation) and inferential statistics (independent t-test) in SPSS software, version 16. A P<0.05 was considered significant.
Results
The majority of the studied neonates were female (56.6%), were born through caesarian section, their birth gestational age was between 28 to 31 weeks, their birth weight was between 1501 to 2000 gr, were hospitalized because of prematurity and respiratory distress syndrome, were not intubated, and were the first child of the family (Table 1).
Results of the Kolmogorov-Smirnov test indicated the normal distribution of the PIPP scores; therefore, parametric tests were used in this study. The independent t-test showed no significant difference between the two groups regarding demographic characteristics and the PIPP score. The mean score of PIPP after the intervention was significantly less in the intervention group than in the control group (P=0.001). This result is shown in Table 2.
According to the results of the analysis of covariance, adjusting the environmental stimuli of light and sound was effective on the pain level of the neonate during PICC implantation with an effect size of 0.917.
Discussion
The mean scores before the intervention were 4.48 in the control group and 4.53 in the intervention, indicating the existence of discomfort in neonates even before the beginning of the procedure. In this respect, the results are consistent with other studies. Harrison and McKechnie studied the amount of discomfort during transport on 140 infants using the PIPP. The mean score of the PIPP in premature infants was about 4 to 5, indicating their mild discomfort. Caregiving relationships in the postnatal period are critical to an infant’s development. Preterm infants and their parents face unique challenges in this regard, with infants experiencing separation from their parents, uncomfortable procedures, and increased biological vulnerability. Also, parents face difficulties assuming caregiver roles and increased risk for psychological distress [28]. Received neonates can be exposed to light more than recommended in NICU levels, including extremely bright light [29]. Human cerebellar development occurs late in gestation and is hindered by preterm birth. The fetal development of Purkinje cells, the primary output cells of the cerebellar cortex, is crucial for the structure and function of the cerebellum. However, morphological and electrophysiological features in Purkinje cells at different gestational ages and the effects of the NICU environment on cerebellar development are unexplored [30].
Preterm infants are sensitive to sound peaks and light level variations, with a slightly higher sensitivity to sound peaks. The mechanisms leading to pain behaviors induced by noise and light changes should be evaluated further in the context of preterm infant brain development.
Environmental lighting can affect weight gain and the length of stay in NICUs [31].
Individualized developmental care is an approach to nursing for hospitalized infants. It includes reading the infant’s cues, engaging the parents, and providing a supportive environment [6]. Developmental care practices that mitigate the infant stress experience are promising as modifiable factors that may change the trajectory of neurodevelopmental outcomes in congenital heart disease [32].
In this study, using eye shields and earmuffs during painful procedures significantly reduced pain scores in the intervention group. The results are consistent with some similar studies. According to Mehrnoush et al., conditions caused by neonatal diseases such as respiratory distress and irritability due to central nervous system damage, and neonatal connections such as intravenous catheters, nasogastric tube, nasal continuous positive airway pressure, and routine procedures such as airway suction, and measurement of vital signs, even change position can put the baby in an unpleasant and distressing physical condition [33]. Alemdar et al. showed a significant difference between the mean scores of the neonatal infant pain scale in the intervention and the control groups after intravenous catheter implantation, mainly related to covering the eyes in the intervention groups. They did not find a significant difference between the two groups’ means of neonatal infant pain scale during the procedure [34]. In their other clinical trial, they aimed to investigate the impact of a recorded mother’s voice, breast milk odor, and incubator cover on the pain during peripheral cannulation between the PIPP scores during and after the painful procedure of the two groups [35].
A study that assessed the effect of eye shield versus massage on preterm infants’ pain response during venipuncture showed that in both intervention groups, the PIPP scores were significantly lower compared with the control group [36].
In a randomized clinical trial by Ajam Hassani et al., the researchers used eye shields and earmuffs for the neonates in the intervention group 4 and 2 hours before the oral gastric tube insertion, respectively. The PIPP scores of the intervention group were significantly lower than the control group during and after the procedure [37].
Premature infants are frequently exposed to painful experiences in the NICU due to their relatively lengthy stay and the need for multiple diagnostic and dermatological procedures. In recent decades, much attention has been paid to research on the effectiveness and safety of various pharmacological or non-pharmacological methods on pain caused by procedures performed in neonatal intensive care units [26, 38]. According to the results, modification of light and sound stimuli reduced preterm infants’ pain during PICC implantation.
Comparing the results of this study with similar studies, it is clear that there are still very contradictory results about the effectiveness of reducing environmental stimuli in reducing neonatal pain. The limitation of the present study was its lack of blindness, which affects the generalizability of the results. Educational classes may be helpful and operational. Holding a training class for medical staff, especially nurses, to manage sound and light in the ward and standardize environmental factors such as light and sound in the NICU.
Based on the study, environment modifications are effective, inexpensive, accessible, and safe methods during PICC placement for premature infants in the NICU. Clinical nurses should use this approach to promote neonatal outcomes due to the destructive effect of sound and light on the neural development of the infant and the occurrence of distress symptoms in infants following procedural pain. One of the limitations that prolonged the length of time in this study was that central catheters were not implanted for all infants admitted to the NICU, or some met all the inclusion criteria. However, they were converted in the middle of the way, or sometimes the PICC was inserted when the researcher was not present in the ward, so a long time was spent conducting the study.
Ethical Considerations
Compliance with ethical guidelines
This study was registered at the Iranian Center for Clinical Trials (IRCT) (Code: IRCT640768640768). Also it was approved by the Joint Ethics Committee of Shahid Beheshti University of Medical Sciences (SBMU) (Code: IR.SBMU.PHARMACY.REC.1398.062). The researchers conducted the intervention according to the institutional regulations. Informed consent was obtained from the neonates’ parents after explaining the research objectives and assuring them of the safety of the intervention.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors
Authors' contributions
Conducting research and preparing the first version of the article: Nargess Ranjbari; Designing and supervising the research, participating in writing and editing the article: Anahita Masoumpour; Co-supervising and participating in editing the article: Azam Shirinabadi Farahani; Reviewing and revising the manuscript: Maryam Mahdizadehshahri; Performing expert statistics: Malihe Nasiri; Approve the final version of manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Masoud Dehdashtian and Amir Kamal Hardani for attending NICU in Emam Khomeini and Abouzar hospitals.
References
- Asghari E, Shirinabadi Farahani A, Nourian M, Bonakchi H, Gholami S. The effects of telenursing on stress in mothers with premature infants. Evid Based Care J. 2021; 10(4):7-16. [Link]
- Maxwell LG, Fraga MV, Malavolta CP. Assessment of pain in the newborn: An update. Clin Perinatol. 2019; 4(46):693-707. [DOI:10.1016/j.clp.2019.08.005] [PMID]
- He L, Chen W, Zhang M, Lin N, Yang W. Outcome of intracavitary electrocardiogram guidance in PICC Tip placement in preterm infants: A single-center experience of 327 cases. Am J Nurs. 2019; 8(4):142-4. [DOI:10.11648/j.ajns.20190804.13]
- Taghinejad F, Nikfarid L, Monfared MN, Hoseini N, Habibi S. Nursing diagnoses of preterm infants in the neonatal intensive care unit: A cross sectional study. J Neonatal Nurs. 2021; 27 (6):451-8. [DOI:10.1016/j.jnn.2021.06.007]
- McPherson C, Miller SP, El-Dib M, Massaro AN, Inder TE. The influence of pain, agitation, and their management on the immature brain. Pediatr Res. 2020; 88(2):168-75. [DOI:10.1038/s41390-019-0744-6] [PMID]
- Cheong JLY, Burnett AC, Treyvaud K, Spittle AJ. Early environment and long-term outcomes of preterm infants. J Neural Transm. 2020; 127(1):1-8. [DOI:10.1007/s00702-019-02121-w] [PMID]
- Döra Ö, Büyük ET. Effect of white noise and lullabies on pain and vital signs in invasive interventions applied to premature babies. Pain Manag Nurs. 2021; 22(6):724-9. [DOI:10.1016/j.pmn.2021.05.005] [PMID]
- Malin jk, Gondwe kw, Fial Av, Moore R, Conley Y, White-Traut R, et al. Scoping review of early toxic stress and epigenetic alterations in the neonatal intensive careunit. Nurs Res. 2023; 72(3):218-28. [DOI:10.1097/NNR.0000000000000652] [PMID]
- Eriksson M, Campbell-Yeo M. Assessment of pain in newborn infants. Semin Fetal Neonatal Med. 2019; 24(4):101003.[DOI:10.1016/j.siny.2019.04.003] [PMID]
- Dix LML, Shepherd K, Polglase GR, Miller SL, Sehgal A, Wong FY. The cerebral hemodynamic response to pain in preterm infants with fetal growth restriction. Front Pediatr. 2020; 8:268. [DOI:10.3389/fped.2020.00268] [PMID]
- Kazemi A, Nikfarid L, Khanali Mojen L, Nasiri M. Obstacles to parentsג interaction with Neonates in Neonatal Intensive Care Units from parentsג and nursesג points of view. Iran J Neonatol. 2019; 10(1):78-85. [DOI:10.22038/IJN.2018.30734.1421]
- Anne RP, Deshabhotla S, Ahmed SW, Ahmed SJ, Reddy N, Farooqui D, et al. A quality improvement initiative to improve management of procedural pain in preterm neonates. Pediatric Anesthesia. 2021; 31(2):221-9. [DOI:10.1111/pan.14075] [PMID]
- Mavis SC, Reis CA, Klinkner DB, Stetson RC, Potter Jr DD, Brumbaugh JE. Extravascular migration of a peripherally inserted central catheter into the retroperitoneum in a preterm infant. J Pediatric Surg Case Rep. 2021; 64:101728. [DOI:10.1016/j.epsc.2020.101728]
- Galen B, Baron S, Young S, Hall A, Berger-Spivack L, Southern W. Reducing peripherally inserted central catheters and midline catheters by training nurses in ultrasound-guided peripheral intravenous catheter placement. BMJ Qual Saf. 2020; 29(3):245-9. [DOI:10.1136/bmjqs-2019-009923] [PMID]
- Hu Y, Ling Y, Ye Y, Zhang L, Xia X, Jiang Q, et al. Analysis of risk factors of PICC-related bloodstream infection in newborns: Implications for nursing care. Eur J Med Res. 2021; 26(1): 80. [DOI:10.1186/s40001-021-00546-2] [PMID]
- De Clifford-Faugère G, Aita M, Le May S. Nurses’ practices regarding procedural pain management of preterm infants. Appl Nurs Res. 2019; 45:52-4. [DOI:10.1016/j.apnr.2018.11.007] [PMID]
- Hatfield LA, Murphy N, Karp K, Polomano RC. A systematic review of behavioral and environmental interventions for procedural pain management in preterm infants. J Pediatr Nurs. 2019; 44:22-30.[DOI:10.1016/j.pedn.2018.10.004] [PMID]
- Schneider J, Duerden EG, Guo T, Ng K, Hagmann P, Bickle Graz M, et al. Procedural pain and oral glucose in preterm neonates: Brain development and sex-specific effects. Pain. 2018; 159(3):515-25. [DOI:10.1097/j.pain.0000000000001123] [PMID]
- Squillaro A, Mahdi EM, Tran N, Lakshmanan A, Kim E, Kelley-Quon LI. Managing procedural pain in the neonate using an opioid-sparing approach. Clin Ther. 2019; 41(9):1701-13. [DOI:10.1016/j.clinthera.2019.07.014] [PMID]
- Farahani E, Nourian M, Ahmadi F, Kazemian M. Comparing the effects of cycled and constant lighting on weight gain and length of stay in neonatal intensive care unit among premature neonates: A two-group randomized controlled clinical trial. Nurs Midwifery Stud. 2018; 7(3):93-9. [Link]
- Nourian M, Nikfarid L, Khavari AM, Barati M, Allahgholipour AR. The impact of an online mindfulness-based stress reduction program on sleep quality of nurses working in covid-19 care units: A Clinical Trial.Holist Nurs Pract. 2021; 35(5):257-63. [DOI:10.1097/HNP.0000000000000466] [PMID]
- Aita M, Stremler R, Feeley N, Nuyt AM, Lavallée A. Acceptability to nurses of reducing NICU light and noise levels during skin-to-skin care: A pilot study. Appl Nurs Res. 2019; 47:29-31. [DOI:10.1016/j.apnr.2019.03.001] [PMID]
- Küçük Alemdar D, İnal S. The effect of individualized developmental care practices in preterm infants. Complement Med Res. 2020; 27(2):97-104. [DOI:10.1159/000504357] [PMID]
- Foladi N, Farahani AS, Nourian M, Faghihzadeh E, Mojen LK, Gholami S, et al. Barriers to the implementation of” newborn individualized developmental care and assessment program” from the perspectives of nurses and physicians. Iran J Neonatolo. 2020; 11(4):14-20. [Link]
- Ballantyne M, Stevens B, McAllister M, Dionne K, Jack A. Validation of the premature infant pain profile in the clinical setting. Clin J Pain. 1999; 15(4):297-303. [DOI:10.1097/00002508-199912000-00006] [PMID]
- Aita M, Goulet C, Oberlander TF, Snider L, Johnston C. A randomized controlled trial of eye shields and earmuffs to reduce pain response of preterm infants. J Neonatal Nurs. 2015; 21(3):93-103. [DOI:10.1016/j.jnn.2014.11.004]
- Basara SG, Calisir H, Sahin S, Bozkurt E. Effect of Using Earmuffs on Physiological Parameters and Stress Levels of Premature Infants: A Randomized Controlled Trial. Iran J Neonatol. 2023; 1(14):54-61.[Link]
- Hartzell G, Shaw RJ, Givrad S. Preterm infant mental health in the neonatal intensive care unit: A review of research on NICU parent-infant interactions and maternal sensitivity. Infant Ment Health J. 2023; 44(6):837-56. [DOI:10.1002/imhj.22086] [PMID]
- Gilmour D, Duong KM, Gilmour IJ, Davies MW. NeoSTRESS: Study of transfer and retrieval environmental stressors upon neonates via a smartphone application-light. Air Med J. 2020; 39(2):97-102. [DOI:10.1016/j.amj.2019.07.015] [PMID]
- Barron T , Kim JH. Preterm birth impedes structural and functional development of cerebellar purkinje cells in the developing baboon cerebellum. Brain Sci. 2020; 10(12):897. [DOI:10.3390/brainsci10120897] [PMID]
- Marchal A, Melchior M, Dufour A, Poisbeau P, Zores C, Kuhn P. Pain behavioural response to acoustic and light environmental changes in very preterm infants. Children (Basel). 2021; 8(12):1081. [Link]
- Miller TA, Lisanti AJ, Witte MK, Elhoff JJ, Mahle WT, Uzark KC, et al. A collaborative learning assessment of developmental care practices for infants in the cardiac intensive care unit. J Pediatr. 2020; 220:93-100. [DOI:10.1016/j.jpeds.2020.01.043] [PMID]
- Mehrnoush N, Ashktorab T, Heidarzadeh M, Momenzadeh S, Khalafi J. Factors influencing neonatal pain management from the perspectives of nurses and physicians in a neonatal intensive care Unit: A qualitative study. Iranian Journal of Pediatrics. 2018; 28(1):e10015. [DOI:10.5812/ijp.10015]
- Alemdar DK, Özdemir FK. Effects of covering the eyes versus playing intrauterine sounds on premature infants’ pain and physiological parameters during venipuncture. J Pediatr Nurse. 2017; 37:e30-6. [PMID]
- Alemdar DK. Effect of recorded maternal voice, breast milk odor, and incubator cover on pain and comfort during peripheral cannulation in preterm infants. Appl Nurs Res. 2018; 40:1-6. [DOI:10.1016/j.apnr.2017.12.001] [PMID]
- Moselhi Mater EA, Mahamud HS, Mohamed MF. Effect of eye shield versus massage on preterm infants’ pain response during venipuncture. Int J Nurs Didactics. 2019; 9(2): 21-7. [Link]
- Sadat Hoseini A S, Ajam Hassani A. [Investigating the effect of earmuffs and eyeshields on pain caused by orogastric tube insertion among infants in neonatal intensive care unit (Persian)]. J Mazandaran Univ Med Sci. 2020; 30(190):152-7. [Link]
- Venkataraman R, Kamaluddeen M, Amin H, Lodha A. Is less noise, light and parental/caregiver stress in the neonatal intensive care unit better for neonates? Indian Pediatr. 2018; 55(1):17-21. [PMID]
Article Type : Research |
Subject:
General
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |