Sat, Apr 27, 2024
Volume 34, Issue 2 (2-2024)
JHNM 2024, 34(2): 189-199 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rokni Shirazi F, Moghadamnia M T, Javadi-Pashaki N, Kazemnezhad Leili E, Ghasemzade M. Effect of Adding Continuous Positive Airway Pressure via Mask on Respiratory Indices During Cardiac Rehabilitation After Coronary Artery Bypass Grafting. JHNM 2024; 34 (2) :189-199
URL: http://hnmj.gums.ac.ir/article-1-2301-en.html
URL: http://hnmj.gums.ac.ir/article-1-2301-en.html
Fatemeh Rokni Shirazi1 

 , Mohammad Taghi Moghadamnia *
, Mohammad Taghi Moghadamnia * 

 2, Nazila Javadi-Pashaki3
2, Nazila Javadi-Pashaki3 

 , Ehsan Kazemnezhad Leili4
, Ehsan Kazemnezhad Leili4 

 , Mehrzad Ghasemzade5
, Mehrzad Ghasemzade5 



 , Mohammad Taghi Moghadamnia *
, Mohammad Taghi Moghadamnia * 

 2, Nazila Javadi-Pashaki3
2, Nazila Javadi-Pashaki3 

 , Ehsan Kazemnezhad Leili4
, Ehsan Kazemnezhad Leili4 

 , Mehrzad Ghasemzade5
, Mehrzad Ghasemzade5 

1- Nursing (MsN), Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Associate Professor, Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. , moghadamnia@gums.ac.ir
3- Associate Professor, Social Determinants of Health Research Center (SDHRC), Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatistics, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
5- Anesthesiologist, Ghaem International Hospital, Rasht, Iran.
2- Associate Professor, Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. , moghadamnia@gums.ac.ir
3- Associate Professor, Social Determinants of Health Research Center (SDHRC), Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatistics, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
5- Anesthesiologist, Ghaem International Hospital, Rasht, Iran.
Keywords: Coronary artery bypasses graft (CABG), Atelectasis, Incentive spirometry, Continuous positive airway pressure
Full-Text [PDF 573 kb]
(102 Downloads)
| Abstract (HTML) (211 Views)
Full-Text: (49 Views)
Introduction
Coronary artery disease (CAD) is the most prevalent cardiovascular disease [1, 2] and the leading cause of mortality worldwide, with up to 17.3 million deaths every year [3]. According to official data provided by the Ministry of Health and Medical Education in Iran, 33% to 38% of deaths are due to CAD, especially acute myocardial infarction [4]. The mortality rate is controlled or prevented by appropriate treatments [5]. Coronary artery bypass graft (CABG) is the choice of treatment for these patients, which may cause complications [6].
Pulmonary complications are among the most important complications that postpone recovery [7, 8]. Atelectasis is one of the serious pulmonary complications after CABG that usually occurs in the lower lobe of the lungs close to the heart [9]. The incidence of atelectasis has been reported to be 95%-100% in all patients undergoing CABG on the first and second postoperative days [10]. Several rehabilitation strategies have been applied to minimize or prevent postoperative pulmonary complications [8].
Chest physiotherapy, concentrating on deep breathing and encouraging coughing, can treat postoperative atelectasis. Regular incentive spirometry (IS) is used to maintain airway patency and prevent or reverse alveolar atelectasis. However, several publications have not revealed any evidence that IS therapy can prevent pulmonary complications after cardiac surgery. A new meta-analysis conducted by Sullivan et al. reveals that IS alone has little effect in reducing mortality from postoperative pulmonary complications and length of hospital stay [10]. Evidence-based studies show no benefit for IS in preventing postoperative pulmonary complications [9, 10, 11]. Noncompliance of most patients with cardiac rehabilitation programs, especially IS (due to time-consuming, postoperative fatigue, and the probability of staff supervision deficiency because of a high number of patients and additional workload), has encouraged researchers to adopt new methods in the cardiac rehabilitation process. Another method of atelectasis prevention is using noninvasive positive pressure ventilation mode, especially continuous positive airway pressure (CPAP) [12].
Studies show no evidence of a reduction in pulmonary complaints after using IS after cardiac surgery. The use of CPAP during inhalation and exhalation periods in the cardiac rehabilitation program of hospitalized patients after CABG has improved the relevant clinical results. Continuous positive airway pressure increases walking time and ventilatory performance and improves respiratory pattern [8]. Since atelectasis is an essential pulmonary complication after cardiac surgery, resulting in pneumonia and acute respiratory failure [8, 13, 14], using a method that can help reduce the severity of these complications after cardiac surgery can help the patient recover faster and the medical service delivery systems to save costs. Therefore, this study evaluated the effect of adding CPAP to the cardiac rehabilitation program after CABG on exercise and respiratory parameters in admitted patients.
Materials and Methods
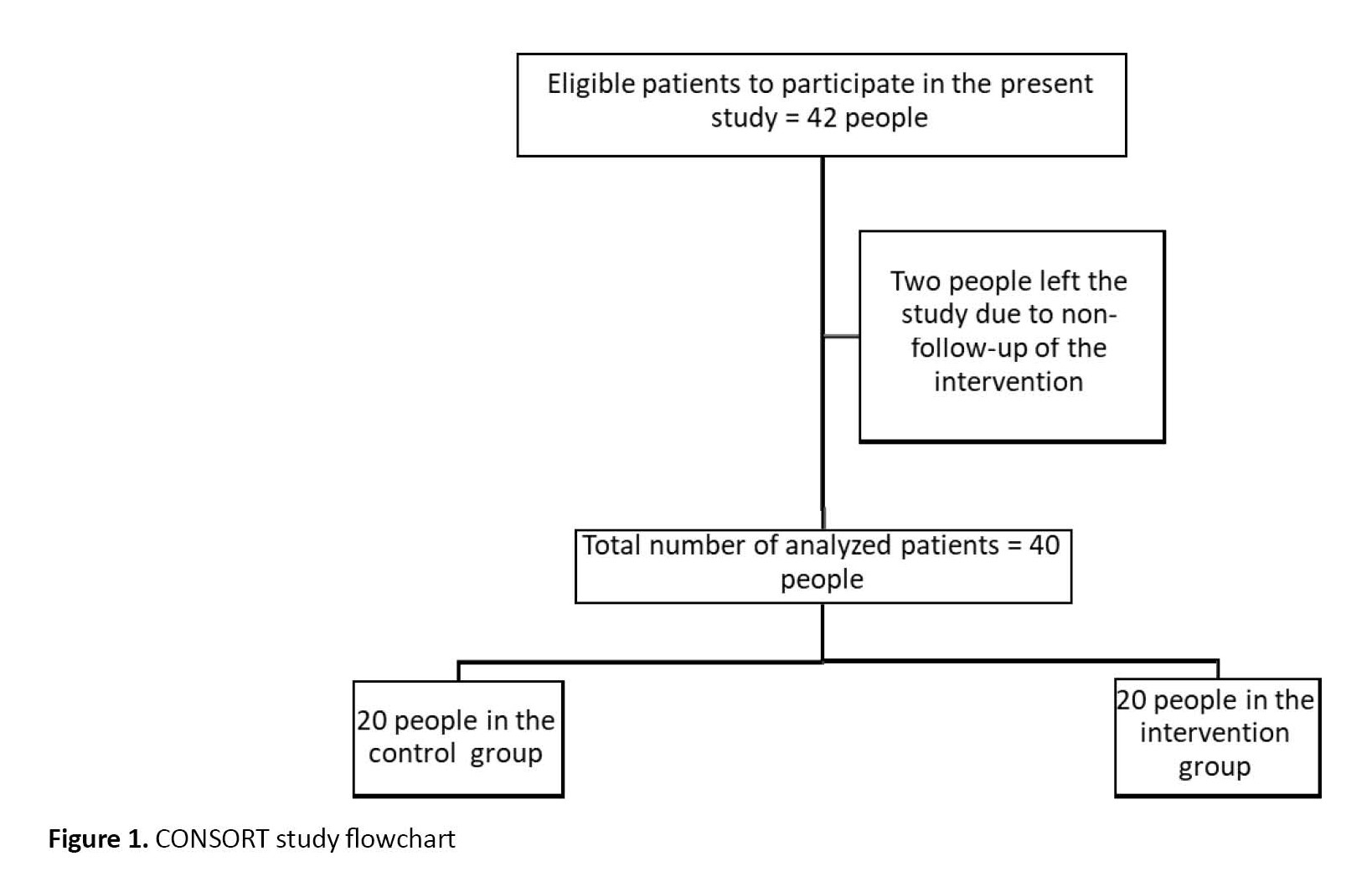
The current study is a randomized controlled trial performed on 40 patients undergoing CABG in one of the educational and remedial centers, Guilan University of Medical Sciences, Guilan Province, Iran, from September to November 2018 for 50 consecutive days. The sample size was estimated as 20 people in each group with 95% confidence and 10% type II error based on the results of Pantoni et al.’s study (Mean±SD were 90.2±2.8 and 92.8±2.3 in the control and intervention groups, respectively) and using the oxygen saturation index of the peripheral blood in the two-domain test [8]. Samples were entered into this study based on the inclusion criteria. First, they were randomly allocated by flipping the coin to determine intervention or control, and then, with four block randomizations, defined the sequences of the intervention (20 patients) and control (20 patients) groups.
The inclusion criteria were elective CABG with cardiopulmonary bypass, sternotomy incision and use of saphenous vein, internal mamillary artery or radial vein graft, ability to perform an exercise, no previous cardiac surgery, non-use of intra-aortic balloon pump, no permanent pacemaker, no valvular heart disease, and no chronic obstructive pulmonary disease (COPD) history based on the medical record (Figure 1). In this study, all information was obtained from the registered medical records of the patients and the researcher’s observations, which consisted of three general sections. The first part included demographic information: Age, gender, and body mass index (BMI). The second part involved extraction of non-spirometry results consisting of dyspnea-using modified Borg scale 10 for dyspnea score (16), leg effort-using rate of perceived exertion (RPE) scale, walking time, SpO2 before walking, and SpO2 after walking from the first to the third day of study that measured with calibrated pulse oximeter accurate model. This research divides the Borg scale into two sections: Modified CR-10 and RPE. Modified CR-10 is used to assess the degree of dyspnea, rated from 0 to 10. Zero means nothing at all, 0.5=extremely slight, 1=very slight, 2=slight, 3=moderate, 4=somewhat severe, 5=severe, 7=very severe, 9=extremely severe (almost maximal). RPE is used to measure the perceived exertion during a patient’s activity, which is rated from 6 to 20. Six means no exertion at all (no muscle fatigue, breathlessness, or difficulty in breathing), 7=extremely light (very, very light), 9=very light (like walking slowly for a short while and very easy to talk), 11=light (like alight exercise at patient own pace), 12=moderate, 13=somewhat hard (fairly strenuous and breathless and not so easy to talk), 15=hard ( heavy and strenuous and upper limit for fitness training as when running or walking fast, 17=very hard (very strenuous and patient is very tired and breathless, very difficult to talk), 19=extremely hard (the most strenuous effort that patient has ever experienced, 20=maximal exertion (maximal heaviness). There are not explanation for items 6, 8 in CR – 10 and for items 8, 14, 16 in RPE inn original version of scale [16]. These two sections are illustrated as two separate checklists. It is noticeable that the researcher recorded the total time of physical activity and the amounts of SpO2 right before and after physical activity. The third part contained extracting spirometry results using a computed spirometry test consisting of tidal volume (VT), respiratory rate (RR), minute ventilation (VE), forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FVC/FEV1, and peak expiratory flow (PEF) on the fourth day of study. One person did all spirometry tests for all samples. The walking time was recorded based on the researcher’s observation.
Patients in the control group received routine IS, and patients in the intervention group received CPAP mask with controlled pressure set 3-5 cm H2O besides IS as prescriptive cardiac rehabilitation for three days (8). Two masks (made by Vygon Co., France) were used in this study. The masks were disinfected with ethylene oxide gas after use for each patient. At the time of this intervention, the samples of the intervention and control groups were separated from each other in two different rooms to prevent sensitivity to the change in the routine method. In our research environment, patients undergoing CABG were admitted to open heart ICU for two days after surgery. Then, on the third day after surgery, the patient is transferred to an open-heart ward and monitored for four more days. After studying the patient’s medical record and reviewing the inclusion criteria, the researcher provided a complete description of the study process, the non-use of any invasive procedure, and the confidentiality of personal information. Then, agreement consent was signed, and the researcher completed the questionnaire.
In the cardiac rehabilitation program, 48 hours after the operation, the patients in the control group received a routine program, including using IS and deep breathing exercises for half an hour before starting to walk. In addition to receiving routine IS for 30 minutes, patients in the intervention group were used to apply continuous positive airway pressure with balanced airway pressure in the inhalation and exhalation periods of 4-6 cm H2O according to the patient’s tolerance. Then, two hours after applying continuous positive airway pressure with balanced airway pressure during inhalation and exhalation periods, active physical exercises in the form of walking for 5 to 10 minutes on the first day (depending on the patient’s tolerance), 10 to 15 minutes on the second day, and 15 minutes and more on the third day, were done. The control group also had the same amount of activity due to the possibility of the patient’s intolerance to this mask; the researcher was present throughout the intervention.
The findings of this study were analyzed by SPSS software, version 16 after coding. Before analyzing data, the Shapiro-Wilks test was used to determine the normal distribution of data. Non-spirometry variables were analyzed using descriptive statistics such as Mean±SD, time effect, group effect, and interaction between group and time using repeated measure analysis of variance. The spirometry variables were analyzed using descriptive statistics such as mean, standard deviation, first and third quartile. Finally, repeated measures analysis of covariance, t-test, Mann-Whitney test, and multivariate analysis of covariance were used to analyze the relationship and significance of dependent and independent variables in non-spirometry and spirometry parameters as multivariate. The statistical tests were considered significant when P˂0.05.
Results
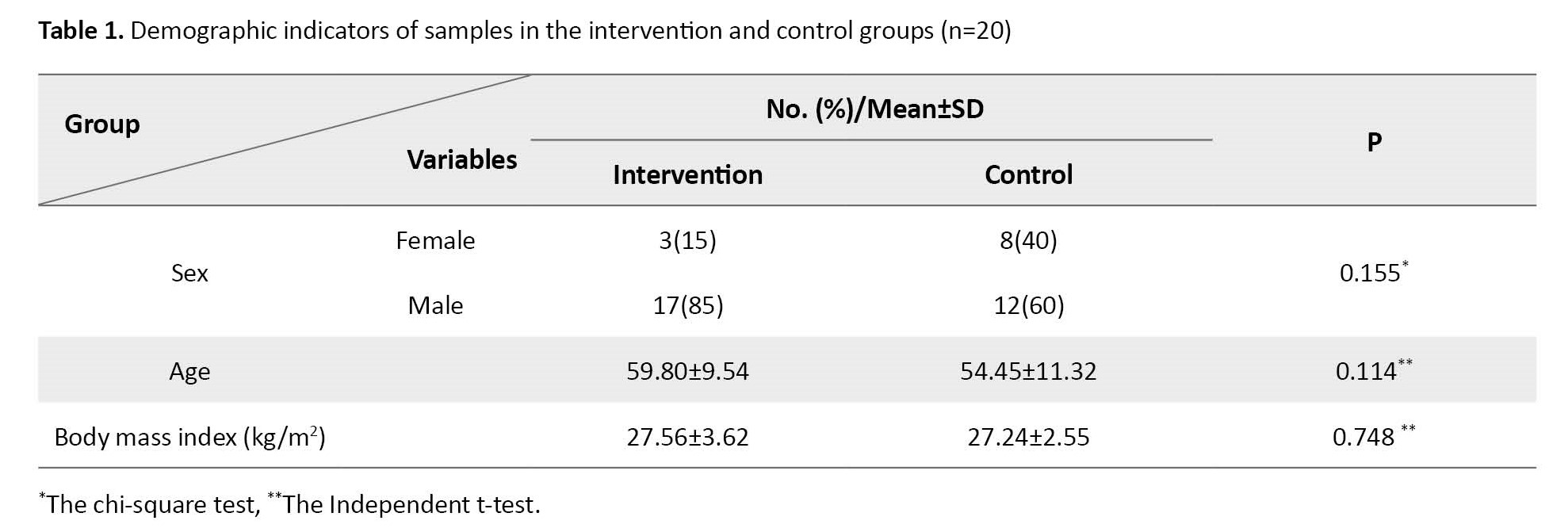
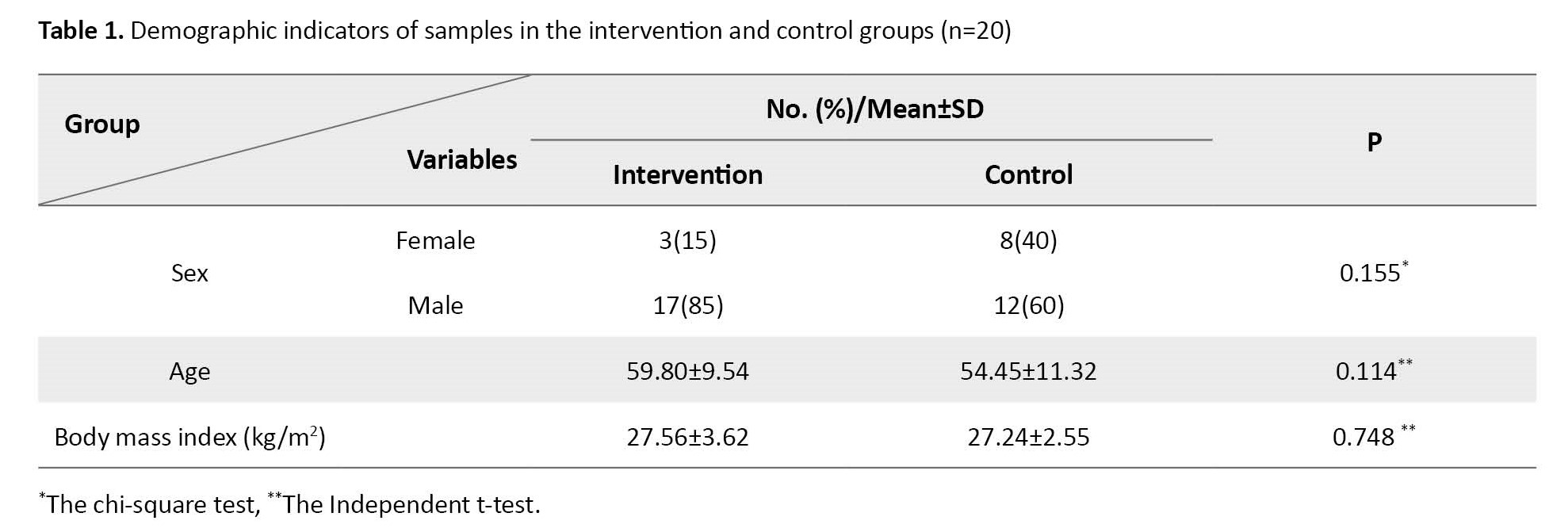
There were 17 men and 3 women in the intervention group and 12 men and 8 women in the control group. Their mean age was 59.80±9.54 years in the intervention and 54.45±11.32 years in the control group. Their mean BMI was 27.24±2.55 kg/m2 in the intervention group and 27.56±3.62 kg/m2 in the control group. The statistical test showed that age, gender, and BMI had a normal distribution. No significant differences were observed between groups regarding gender, age, and BMI (Table 1).
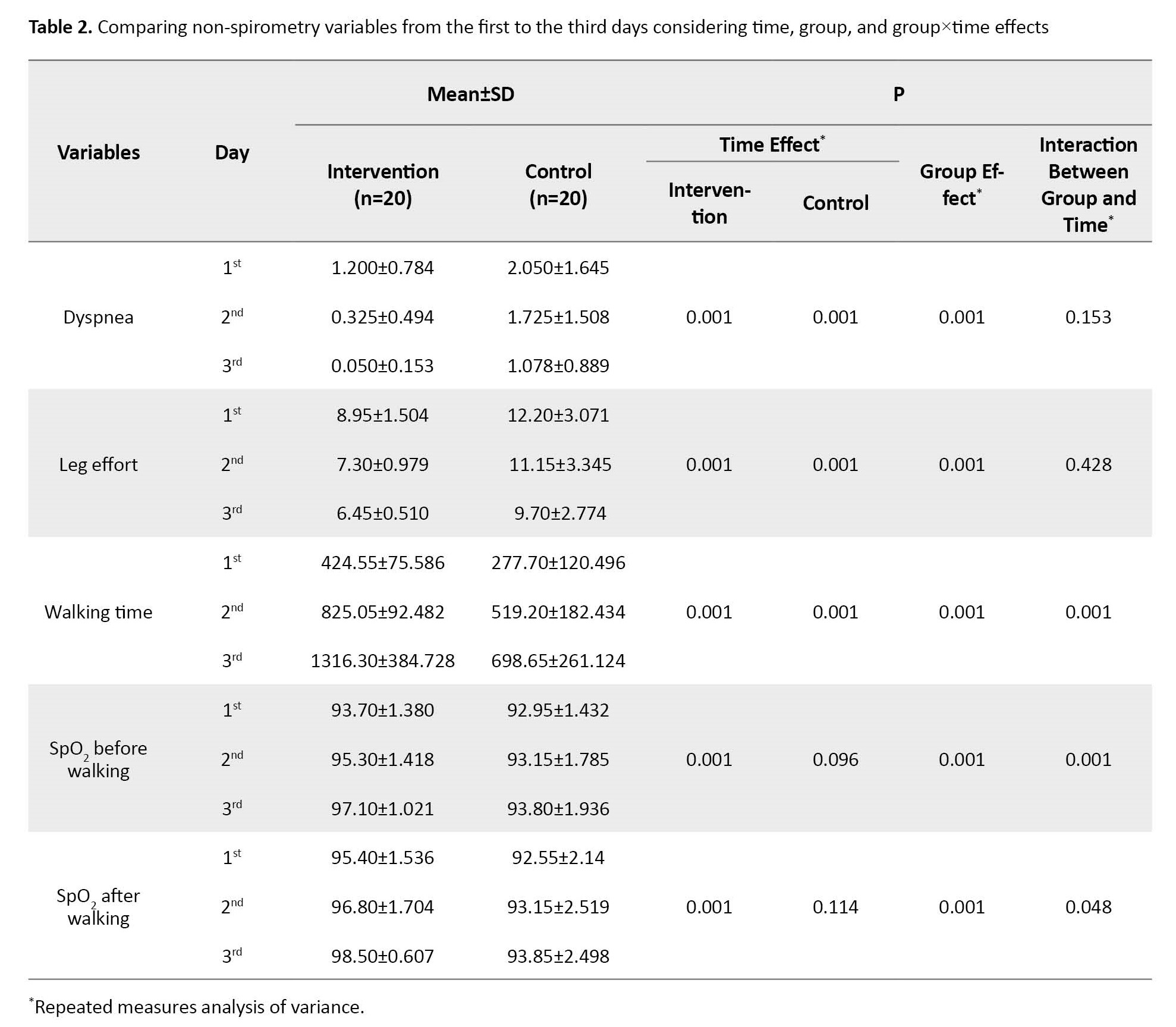
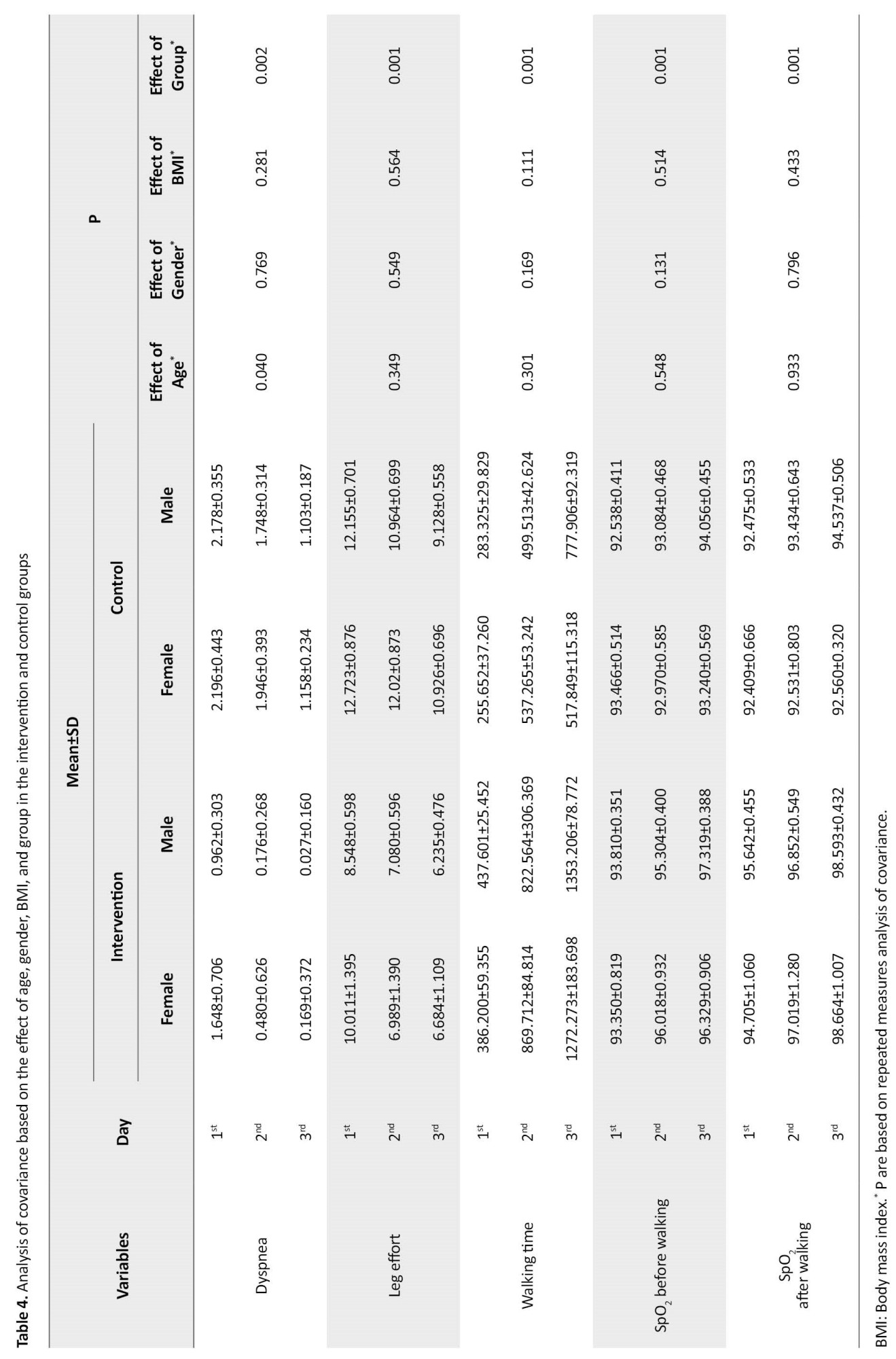
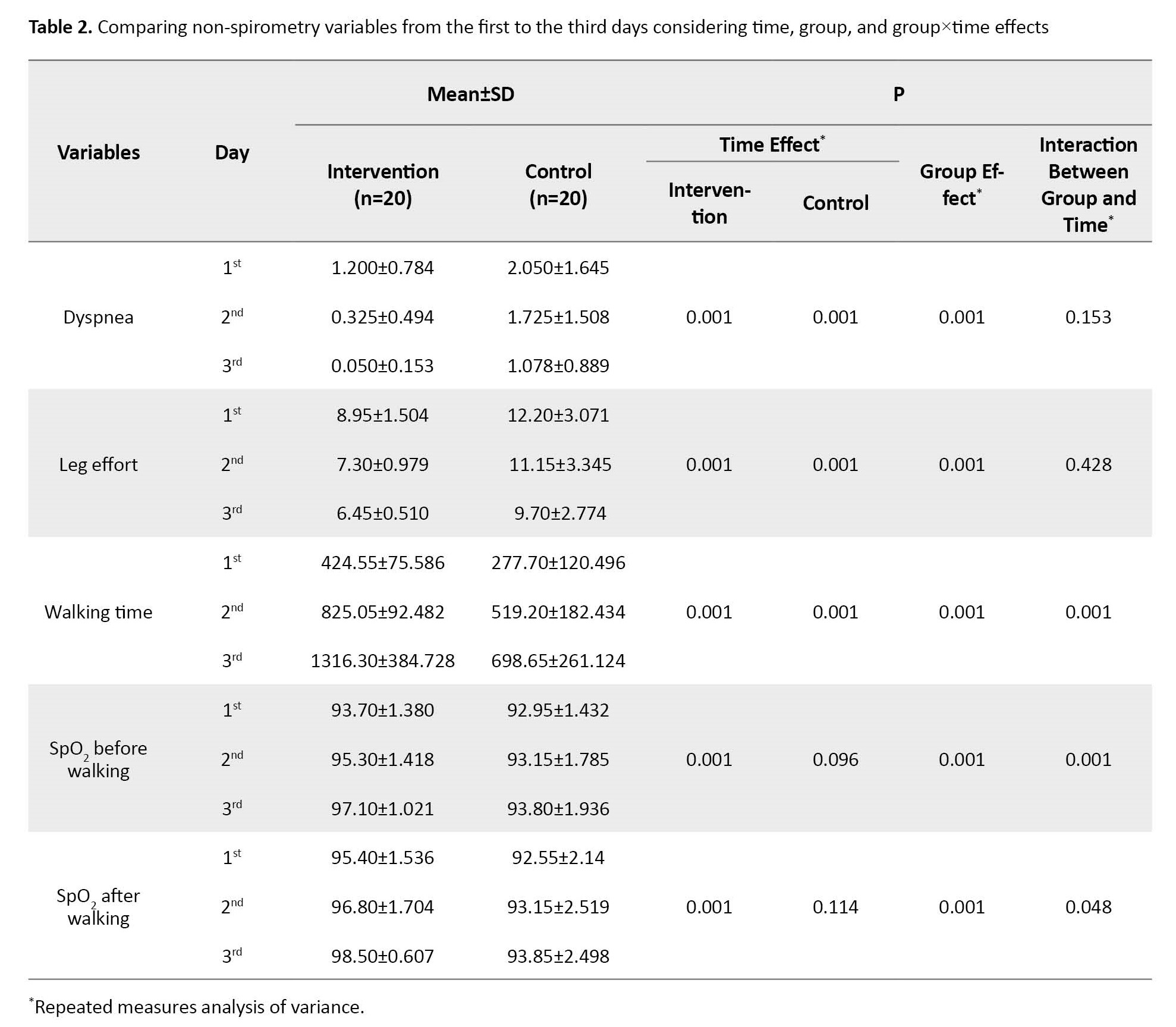
The two groups’ spirometry and non-spirometry variables were different, presenting lower values for dyspnea and leg effort and higher values for walking time and SpO2 before and after walking in the intervention group. Dyspnea and leg effort had similar decreasing trends during three days, and walking time increased in the intervention group. SpO2 before and after walking had increasing trends in the intervention group but fixed in the control group. Although the group effect was statistically significant in all non-spirometry variables, interactions between group and time were insignificant in dyspnea and leg effort variables (Table 2).
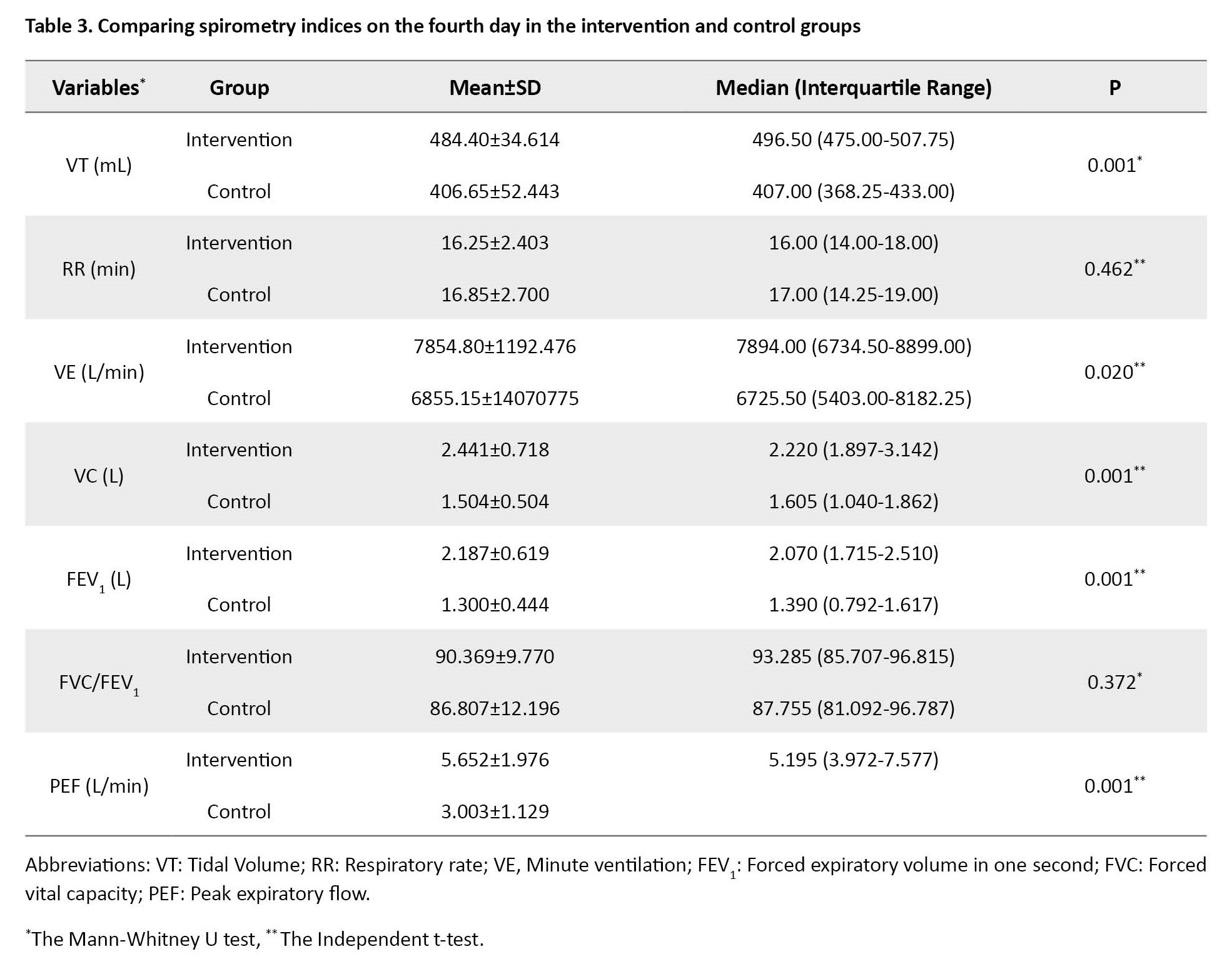
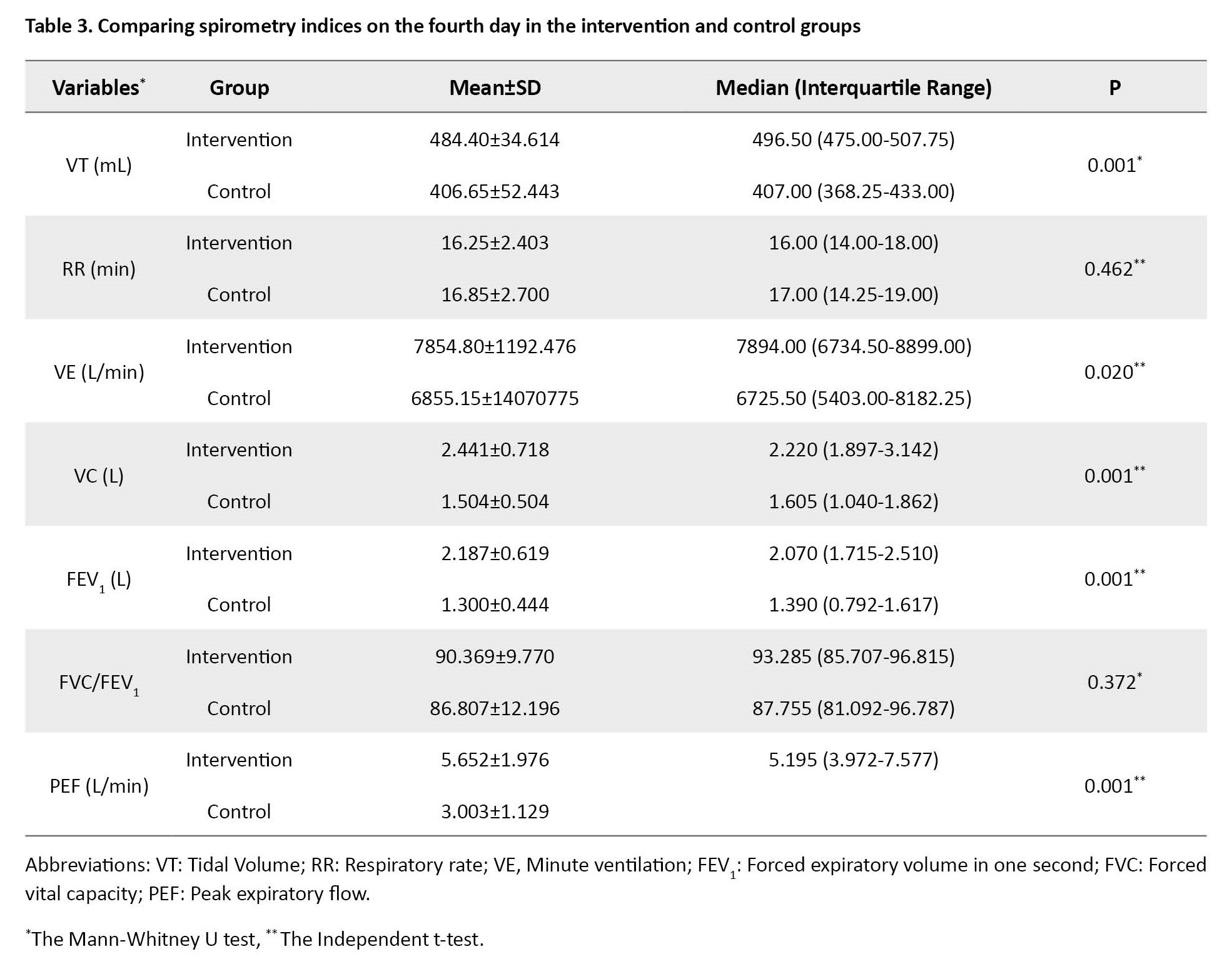
Comparison of means and standard deviations of spirometry parameters on the fourth day in the intervention and control groups indicated that values like VT, VE, FVC, FEV1, and PEF in the intervention group were higher than in the control group. Significant statistical differences were seen between groups in VT (P=0.001), VE (P=0.020), FVC (P=0.001), FEV1 (P=0.001), and PEF (P=0.001), but none in RR and FVC/FEV1 (Table 3).
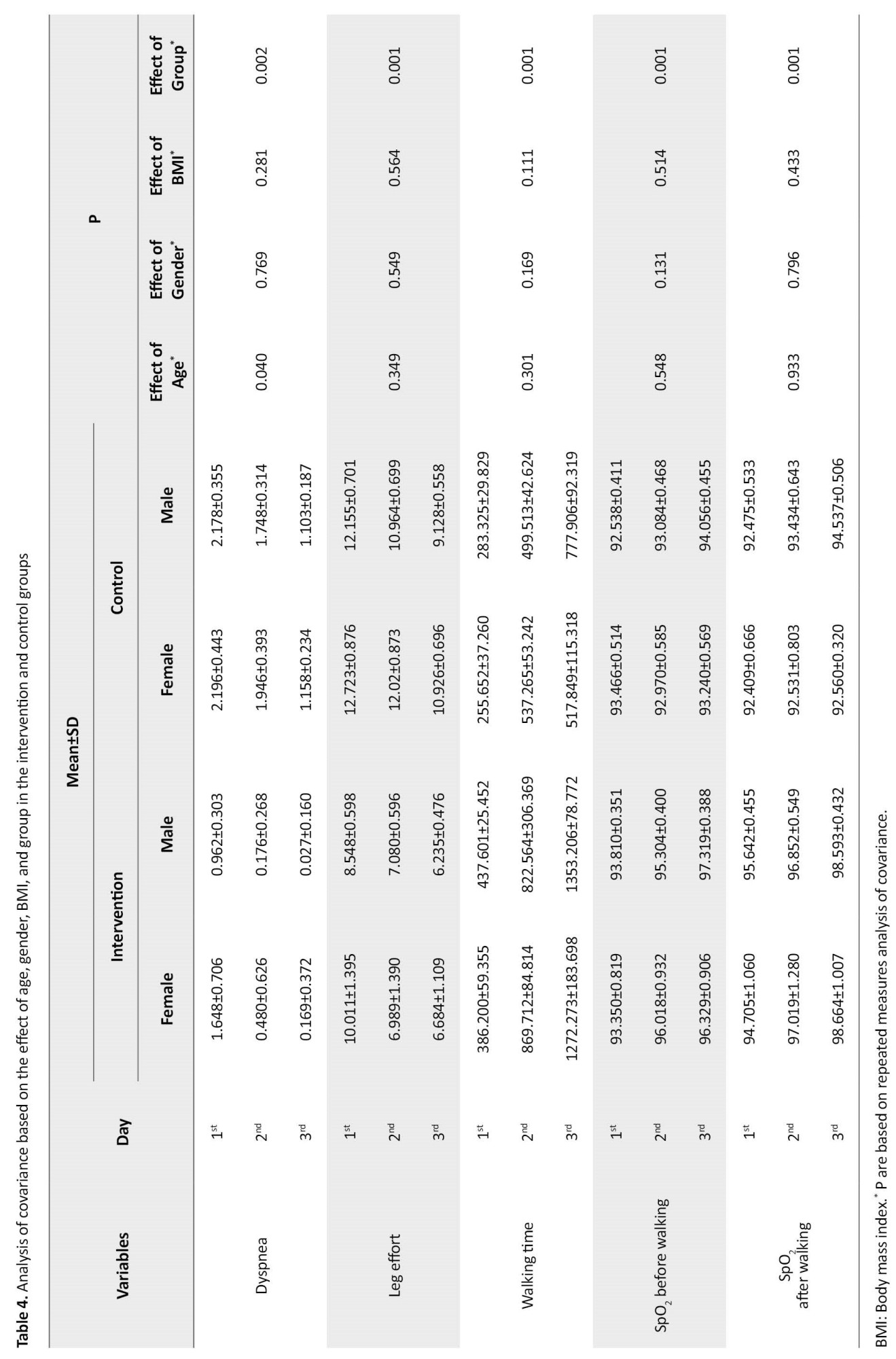
The study showed that non-spirometry variables were higher in the intervention group. The effect of age was significant just in dyspnea. Gender and BMI did not affect any non-spirometry variables. In addition, all non-spirometry parameters affected the group (Table 4).
A comparison of the two groups showed that the mean values of all spirometry parameters in the intervention group were higher than those in the control group. Regarding the relationship between dependent variables in spirometry parameters and independent variables in both groups simultaneously and controlling the additional and continuous effect of independent variables demonstrated that age significantly affected VT (P=0.001), FVC (P=0.001), and FEV1 (P=0.001), and impact of gender was significant just in FVC (P=0.017). Also, BMI was significantly effective in FVC (P=0.004) and PEF (P=0.008). Besides, the effect of group in the intervention group was significantly different from the control group in VT (P=0.001), VE (P=0.006), FVC (P=0.001), and FEV1(P=0.001). These results were shown in Table 5.
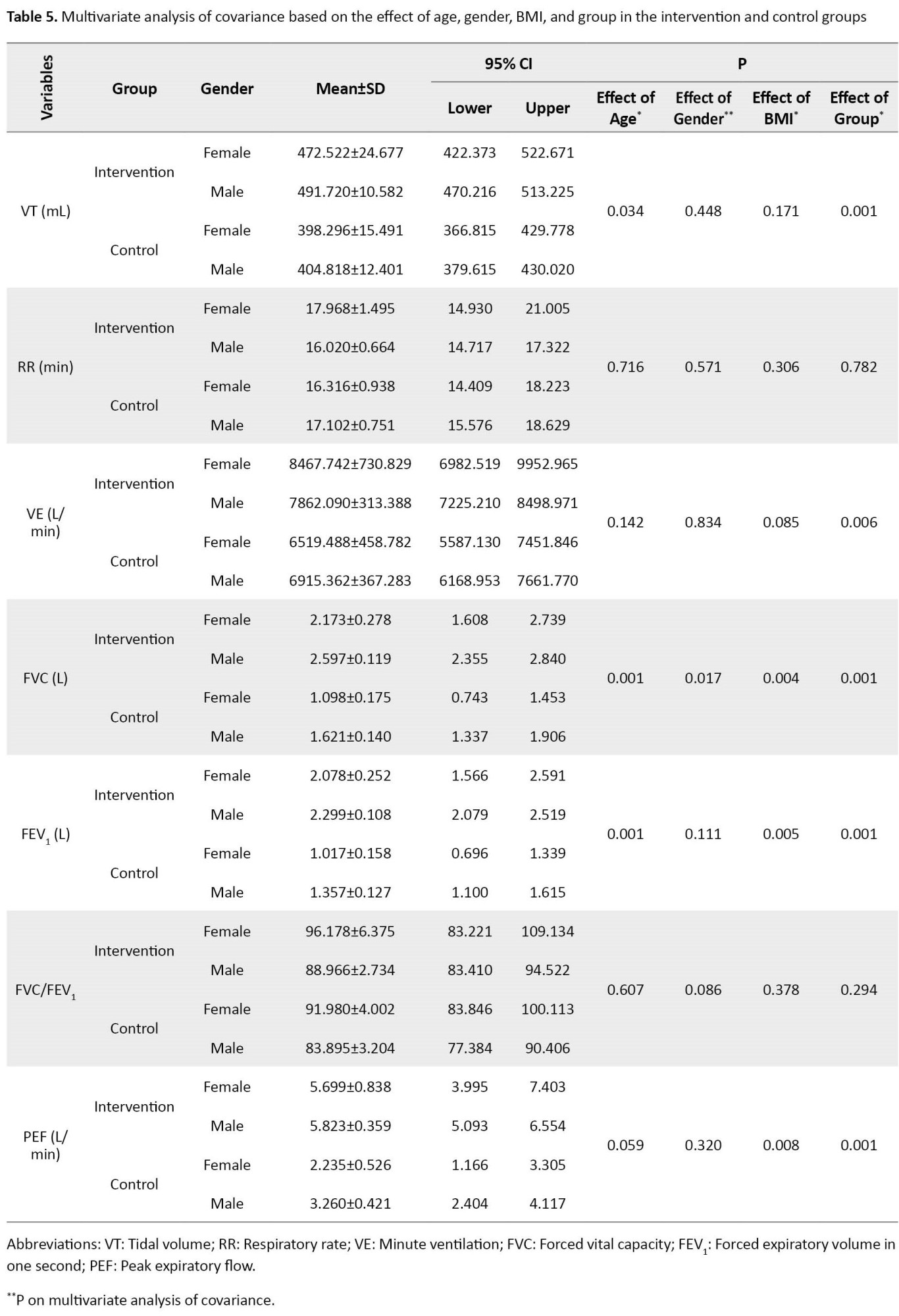
Comparing mean values of spirometry parameters on the fourth day of study considering age, gender, and BMI effectiveness indicated that all spirometry variables were higher in the intervention group except FVC/FEV1.
Discussion
The current study’s findings indicate that using CPAP and routine cardiac rehabilitation positively improves non-spirometry and spirometry parameters. This study showed a significant difference in dyspnea between the two groups on the days under investigation. So, all these days, the amount of dyspnea in the intervention group was always lower than in the control group. In a study conducted by Kamisaka et al. to determine the effect of ventilation aids on reducing dyspnea while walking, especially in patients with cardiac and pulmonary dysfunction after cardiovascular surgery in Japan, the rate of dyspnea after using the ventilation aids, there was a significant difference compared to the previous session [14].
Also, the findings showed that the leg effort was significantly different between the two groups. So, all these days, the leg effort in the intervention group was lower than in the control group. In this regard, research by Ferreira et al. to determine the effect of IS and CPAP during exhalation simultaneously in preventing pulmonary complications showed that the amount of leg effort by the patient during the 6-minute walking test in the control group was significantly more than that in the intervention group [5].
On the fourth day of the study, VT, VE, FVC, FEV1, and PEF as spirometry variables were higher in the intervention group. In addition, dyspnea was just influenced by age and group. Besides, the group influenced the other non-spirometry parameters, too. Also, VT was influenced by age and group, and VE was just affected by group, but no independent variables influenced RR.
In this regard, the study by Kamisaka et al. using ventilatory assistant gadgets in patients with cardiopulmonary dysfunctions after CABG showed a significant difference in the dyspnea group compared before using ventilatory assistant gadgets [14]. Additionally, Ferreira et al. proved that using CPAP and IS together significantly reduced dyspnea score and perceived effort sensation [5]. Previously, Pantoni et al. indicated that walking time was significantly different between groups by 43.4 s. Although Olper et al. although this study showed that CPAP increased lung capacity [8], Al-Mutairi did not report a significant difference between the IS group and 4-h CPAP. Of course, 2-h CPAP was statistically significant [9]. On the other hand, when using noninvasive ventilation, Preisig et al. did not mention any significant difference between the intervention and control groups [16]. In this context, we demonstrated that CPAP and IS reduce dyspnea and leg effort. The findings of our study showed that the walking time and SpO2 improved after the intervention. A possible mechanism for the results of the present study may be related to CPAP decreasing the physiologic work of breathing, thereby unloading the respiratory musculature and reducing the likelihood of fatigue. It may have decreased the presence of hypoxia during walking and potentially contributed to the observed improvement in walking time.
Using plethysmography during walking, Pantoni et al. showed significant differences in VT and VE between the two groups [8]. Also, Al-Mutairi et al. demonstrated no significant difference in RR among all study groups [9]. Age, BMI, and group variables did not affect FVC and FEV1, but gender influenced FVC. Contrary to the results obtained in this study, Bittencourt et al., in a randomized controlled trial, proved that no difference was seen between the two groups in amounts of FVC and FEV1 before and after cardiac rehabilitation [17]. Perhaps different research communities and the duration of rehabilitation programs caused this variation in the results of the two studies. Additionally, Guimarães et al. demonstrated no significant difference in FVC and FEV1 between the two groups in the 1st, 2nd, and 24th hours after the operation [18]. A low sample size and different research communities led to these diversities among the above two studies. Therefore, FVC/FEV1 was not influenced by any independent variables, including age, gender, BMI, and group, but PEF was affected by BMI and group. On the other hand, Ferriera et al. indicated no significant differences in FVC, FEV1, and PEF variables in two control and intervention groups before and 18 months after the operation periods [5]. Probably, different methods applied in their study and measuring these variables before and after intervention yielded different results.
Findings of this study indicate that values of VT, FVC, FEV1, and PEF were statistically significant between the two groups, while RR, VE, and FVC/FEV1 were not. It seems that because of adequate ventilation in the intervention group and prevention of pulmonary endothelial dysfunction and due to the increase of alveolar stability, atelectasis is prevented, and oxygenation is improved. However, appropriate pulmonary muscles and diaphragm function were effective. They caused significant differences in spirometry parameters in the two studied groups. Since most of the spirometry parameters such as VT, VE, FVC, FEV1, and PEF were influenced by the group significantly and due to the researcher’s intervention, applying a ventilator assistant instrument featuring CPAP along with routine cardiac rehabilitation, it seems that increased pulmonary capacity is associated with this respiratory assistant procedure. It appears that in the intervention group, due to the proper establishment of ventilation, pulmonary endothelial dysfunction is prevented, and by increasing the stability of the alveoli, the amount of atelectasis decreases and improves oxygenation. In addition, the proper functioning of the lung and diaphragm muscles is also effective in improving the patient’s respiratory condition [19, 20, 21].
Placing a bulky mask of CPAP on the face of patients can cause anxiety, and this change can affect physiological parameters, including cardiovascular and respiratory function.
The study shows that adding a ventilation assistant gadget featuring CPAP to IS in cardiac rehabilitation programs improves the exercise and respiratory parameters after CABG, which can be considered in patients undergoing cardiac surgery. Usage of CPAP may cause alveolar re-opening and increase oxygenation, leading to non-spirometry and spirometry parameters (i.e. VT, VE, FVC, FEV1, and PEF) improvement after CABG. Therefore, it is recommended that a ventilatory assistant instrument featuring CPAP as a simple and modern tool to improve exercise and respiratory parameters should be applied. It can also be suggested to policymakers for rehabilitation programs after coronary artery bypass surgery.
Ethical Considerations
Compliance with ethical guidelines
This study was supported by the Deputy of Research and Technology and the Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1397.007) and Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20101019004971N5).
Funding
This study was funded by Guilan University of Medical Sciences.
Authors' contributions
Prepare the initial proposal, collect data, and write the manuscript: Fatemeh Roknishirazi; Technical consultant in the research process: Nazila Javadi-Pashaki; Statistical analysis: Ehsan Kazemnejad Lili; Clinical consultant in the research field: Mehrzad Ghasemzade; Corresponding author. Research supervisor and last version manuscript approval: Mohammad Taghi Moghadamnia; Approved the final version of manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the Deputy for Research of Guilan University of Medical Sciences and the patients hospitalized in the Heart surgery Department of Dr Heshmat Rasht Medical Training Center.
References
Coronary artery disease (CAD) is the most prevalent cardiovascular disease [1, 2] and the leading cause of mortality worldwide, with up to 17.3 million deaths every year [3]. According to official data provided by the Ministry of Health and Medical Education in Iran, 33% to 38% of deaths are due to CAD, especially acute myocardial infarction [4]. The mortality rate is controlled or prevented by appropriate treatments [5]. Coronary artery bypass graft (CABG) is the choice of treatment for these patients, which may cause complications [6].
Pulmonary complications are among the most important complications that postpone recovery [7, 8]. Atelectasis is one of the serious pulmonary complications after CABG that usually occurs in the lower lobe of the lungs close to the heart [9]. The incidence of atelectasis has been reported to be 95%-100% in all patients undergoing CABG on the first and second postoperative days [10]. Several rehabilitation strategies have been applied to minimize or prevent postoperative pulmonary complications [8].
Chest physiotherapy, concentrating on deep breathing and encouraging coughing, can treat postoperative atelectasis. Regular incentive spirometry (IS) is used to maintain airway patency and prevent or reverse alveolar atelectasis. However, several publications have not revealed any evidence that IS therapy can prevent pulmonary complications after cardiac surgery. A new meta-analysis conducted by Sullivan et al. reveals that IS alone has little effect in reducing mortality from postoperative pulmonary complications and length of hospital stay [10]. Evidence-based studies show no benefit for IS in preventing postoperative pulmonary complications [9, 10, 11]. Noncompliance of most patients with cardiac rehabilitation programs, especially IS (due to time-consuming, postoperative fatigue, and the probability of staff supervision deficiency because of a high number of patients and additional workload), has encouraged researchers to adopt new methods in the cardiac rehabilitation process. Another method of atelectasis prevention is using noninvasive positive pressure ventilation mode, especially continuous positive airway pressure (CPAP) [12].
Studies show no evidence of a reduction in pulmonary complaints after using IS after cardiac surgery. The use of CPAP during inhalation and exhalation periods in the cardiac rehabilitation program of hospitalized patients after CABG has improved the relevant clinical results. Continuous positive airway pressure increases walking time and ventilatory performance and improves respiratory pattern [8]. Since atelectasis is an essential pulmonary complication after cardiac surgery, resulting in pneumonia and acute respiratory failure [8, 13, 14], using a method that can help reduce the severity of these complications after cardiac surgery can help the patient recover faster and the medical service delivery systems to save costs. Therefore, this study evaluated the effect of adding CPAP to the cardiac rehabilitation program after CABG on exercise and respiratory parameters in admitted patients.
Materials and Methods
The current study is a randomized controlled trial performed on 40 patients undergoing CABG in one of the educational and remedial centers, Guilan University of Medical Sciences, Guilan Province, Iran, from September to November 2018 for 50 consecutive days. The sample size was estimated as 20 people in each group with 95% confidence and 10% type II error based on the results of Pantoni et al.’s study (Mean±SD were 90.2±2.8 and 92.8±2.3 in the control and intervention groups, respectively) and using the oxygen saturation index of the peripheral blood in the two-domain test [8]. Samples were entered into this study based on the inclusion criteria. First, they were randomly allocated by flipping the coin to determine intervention or control, and then, with four block randomizations, defined the sequences of the intervention (20 patients) and control (20 patients) groups.
The inclusion criteria were elective CABG with cardiopulmonary bypass, sternotomy incision and use of saphenous vein, internal mamillary artery or radial vein graft, ability to perform an exercise, no previous cardiac surgery, non-use of intra-aortic balloon pump, no permanent pacemaker, no valvular heart disease, and no chronic obstructive pulmonary disease (COPD) history based on the medical record (Figure 1). In this study, all information was obtained from the registered medical records of the patients and the researcher’s observations, which consisted of three general sections. The first part included demographic information: Age, gender, and body mass index (BMI). The second part involved extraction of non-spirometry results consisting of dyspnea-using modified Borg scale 10 for dyspnea score (16), leg effort-using rate of perceived exertion (RPE) scale, walking time, SpO2 before walking, and SpO2 after walking from the first to the third day of study that measured with calibrated pulse oximeter accurate model. This research divides the Borg scale into two sections: Modified CR-10 and RPE. Modified CR-10 is used to assess the degree of dyspnea, rated from 0 to 10. Zero means nothing at all, 0.5=extremely slight, 1=very slight, 2=slight, 3=moderate, 4=somewhat severe, 5=severe, 7=very severe, 9=extremely severe (almost maximal). RPE is used to measure the perceived exertion during a patient’s activity, which is rated from 6 to 20. Six means no exertion at all (no muscle fatigue, breathlessness, or difficulty in breathing), 7=extremely light (very, very light), 9=very light (like walking slowly for a short while and very easy to talk), 11=light (like alight exercise at patient own pace), 12=moderate, 13=somewhat hard (fairly strenuous and breathless and not so easy to talk), 15=hard ( heavy and strenuous and upper limit for fitness training as when running or walking fast, 17=very hard (very strenuous and patient is very tired and breathless, very difficult to talk), 19=extremely hard (the most strenuous effort that patient has ever experienced, 20=maximal exertion (maximal heaviness). There are not explanation for items 6, 8 in CR – 10 and for items 8, 14, 16 in RPE inn original version of scale [16]. These two sections are illustrated as two separate checklists. It is noticeable that the researcher recorded the total time of physical activity and the amounts of SpO2 right before and after physical activity. The third part contained extracting spirometry results using a computed spirometry test consisting of tidal volume (VT), respiratory rate (RR), minute ventilation (VE), forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FVC/FEV1, and peak expiratory flow (PEF) on the fourth day of study. One person did all spirometry tests for all samples. The walking time was recorded based on the researcher’s observation.
Patients in the control group received routine IS, and patients in the intervention group received CPAP mask with controlled pressure set 3-5 cm H2O besides IS as prescriptive cardiac rehabilitation for three days (8). Two masks (made by Vygon Co., France) were used in this study. The masks were disinfected with ethylene oxide gas after use for each patient. At the time of this intervention, the samples of the intervention and control groups were separated from each other in two different rooms to prevent sensitivity to the change in the routine method. In our research environment, patients undergoing CABG were admitted to open heart ICU for two days after surgery. Then, on the third day after surgery, the patient is transferred to an open-heart ward and monitored for four more days. After studying the patient’s medical record and reviewing the inclusion criteria, the researcher provided a complete description of the study process, the non-use of any invasive procedure, and the confidentiality of personal information. Then, agreement consent was signed, and the researcher completed the questionnaire.
In the cardiac rehabilitation program, 48 hours after the operation, the patients in the control group received a routine program, including using IS and deep breathing exercises for half an hour before starting to walk. In addition to receiving routine IS for 30 minutes, patients in the intervention group were used to apply continuous positive airway pressure with balanced airway pressure in the inhalation and exhalation periods of 4-6 cm H2O according to the patient’s tolerance. Then, two hours after applying continuous positive airway pressure with balanced airway pressure during inhalation and exhalation periods, active physical exercises in the form of walking for 5 to 10 minutes on the first day (depending on the patient’s tolerance), 10 to 15 minutes on the second day, and 15 minutes and more on the third day, were done. The control group also had the same amount of activity due to the possibility of the patient’s intolerance to this mask; the researcher was present throughout the intervention.
The findings of this study were analyzed by SPSS software, version 16 after coding. Before analyzing data, the Shapiro-Wilks test was used to determine the normal distribution of data. Non-spirometry variables were analyzed using descriptive statistics such as Mean±SD, time effect, group effect, and interaction between group and time using repeated measure analysis of variance. The spirometry variables were analyzed using descriptive statistics such as mean, standard deviation, first and third quartile. Finally, repeated measures analysis of covariance, t-test, Mann-Whitney test, and multivariate analysis of covariance were used to analyze the relationship and significance of dependent and independent variables in non-spirometry and spirometry parameters as multivariate. The statistical tests were considered significant when P˂0.05.
Results
There were 17 men and 3 women in the intervention group and 12 men and 8 women in the control group. Their mean age was 59.80±9.54 years in the intervention and 54.45±11.32 years in the control group. Their mean BMI was 27.24±2.55 kg/m2 in the intervention group and 27.56±3.62 kg/m2 in the control group. The statistical test showed that age, gender, and BMI had a normal distribution. No significant differences were observed between groups regarding gender, age, and BMI (Table 1).
The two groups’ spirometry and non-spirometry variables were different, presenting lower values for dyspnea and leg effort and higher values for walking time and SpO2 before and after walking in the intervention group. Dyspnea and leg effort had similar decreasing trends during three days, and walking time increased in the intervention group. SpO2 before and after walking had increasing trends in the intervention group but fixed in the control group. Although the group effect was statistically significant in all non-spirometry variables, interactions between group and time were insignificant in dyspnea and leg effort variables (Table 2).
Comparison of means and standard deviations of spirometry parameters on the fourth day in the intervention and control groups indicated that values like VT, VE, FVC, FEV1, and PEF in the intervention group were higher than in the control group. Significant statistical differences were seen between groups in VT (P=0.001), VE (P=0.020), FVC (P=0.001), FEV1 (P=0.001), and PEF (P=0.001), but none in RR and FVC/FEV1 (Table 3).
The study showed that non-spirometry variables were higher in the intervention group. The effect of age was significant just in dyspnea. Gender and BMI did not affect any non-spirometry variables. In addition, all non-spirometry parameters affected the group (Table 4).
A comparison of the two groups showed that the mean values of all spirometry parameters in the intervention group were higher than those in the control group. Regarding the relationship between dependent variables in spirometry parameters and independent variables in both groups simultaneously and controlling the additional and continuous effect of independent variables demonstrated that age significantly affected VT (P=0.001), FVC (P=0.001), and FEV1 (P=0.001), and impact of gender was significant just in FVC (P=0.017). Also, BMI was significantly effective in FVC (P=0.004) and PEF (P=0.008). Besides, the effect of group in the intervention group was significantly different from the control group in VT (P=0.001), VE (P=0.006), FVC (P=0.001), and FEV1(P=0.001). These results were shown in Table 5.
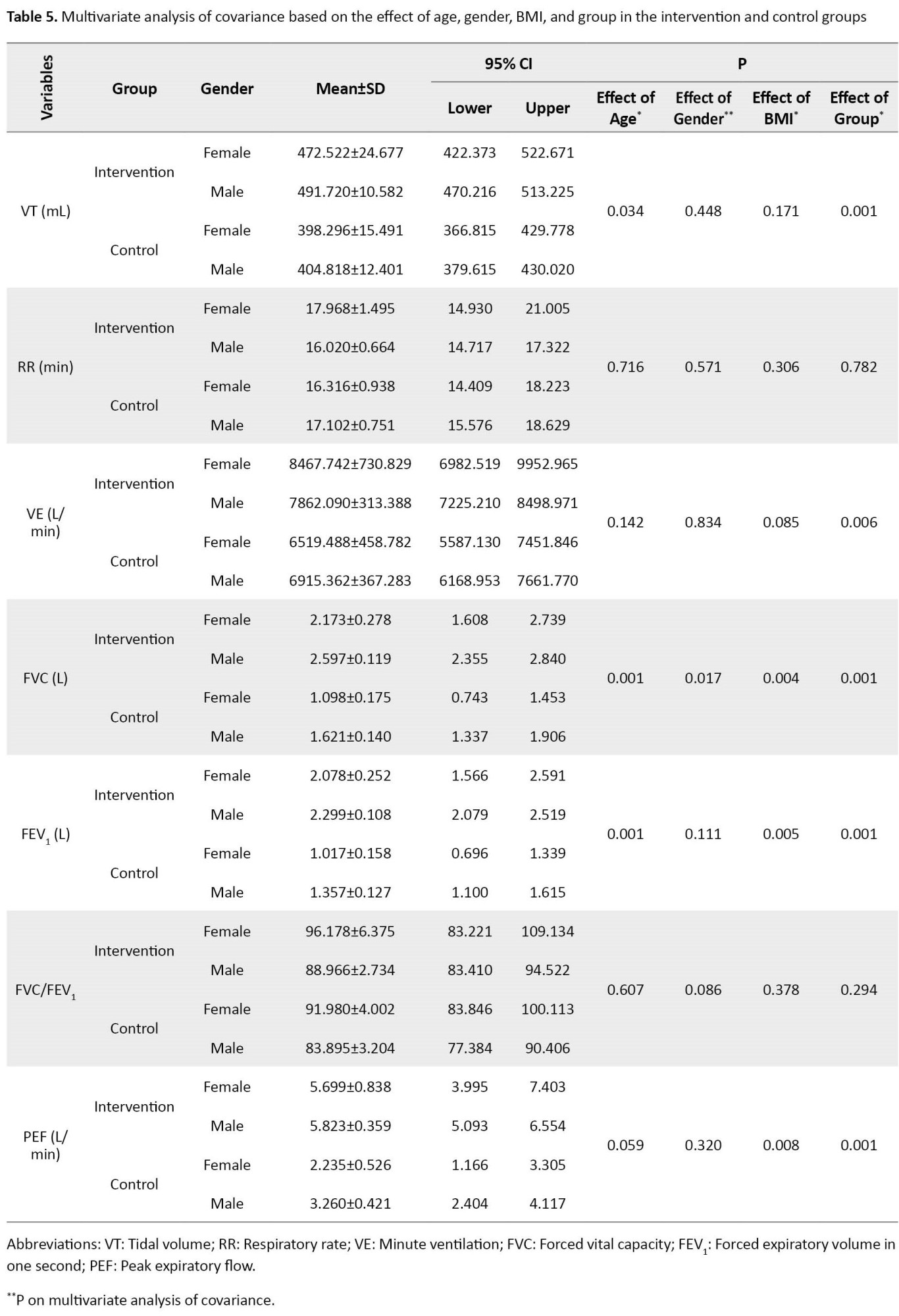
Comparing mean values of spirometry parameters on the fourth day of study considering age, gender, and BMI effectiveness indicated that all spirometry variables were higher in the intervention group except FVC/FEV1.
Discussion
The current study’s findings indicate that using CPAP and routine cardiac rehabilitation positively improves non-spirometry and spirometry parameters. This study showed a significant difference in dyspnea between the two groups on the days under investigation. So, all these days, the amount of dyspnea in the intervention group was always lower than in the control group. In a study conducted by Kamisaka et al. to determine the effect of ventilation aids on reducing dyspnea while walking, especially in patients with cardiac and pulmonary dysfunction after cardiovascular surgery in Japan, the rate of dyspnea after using the ventilation aids, there was a significant difference compared to the previous session [14].
Also, the findings showed that the leg effort was significantly different between the two groups. So, all these days, the leg effort in the intervention group was lower than in the control group. In this regard, research by Ferreira et al. to determine the effect of IS and CPAP during exhalation simultaneously in preventing pulmonary complications showed that the amount of leg effort by the patient during the 6-minute walking test in the control group was significantly more than that in the intervention group [5].
On the fourth day of the study, VT, VE, FVC, FEV1, and PEF as spirometry variables were higher in the intervention group. In addition, dyspnea was just influenced by age and group. Besides, the group influenced the other non-spirometry parameters, too. Also, VT was influenced by age and group, and VE was just affected by group, but no independent variables influenced RR.
In this regard, the study by Kamisaka et al. using ventilatory assistant gadgets in patients with cardiopulmonary dysfunctions after CABG showed a significant difference in the dyspnea group compared before using ventilatory assistant gadgets [14]. Additionally, Ferreira et al. proved that using CPAP and IS together significantly reduced dyspnea score and perceived effort sensation [5]. Previously, Pantoni et al. indicated that walking time was significantly different between groups by 43.4 s. Although Olper et al. although this study showed that CPAP increased lung capacity [8], Al-Mutairi did not report a significant difference between the IS group and 4-h CPAP. Of course, 2-h CPAP was statistically significant [9]. On the other hand, when using noninvasive ventilation, Preisig et al. did not mention any significant difference between the intervention and control groups [16]. In this context, we demonstrated that CPAP and IS reduce dyspnea and leg effort. The findings of our study showed that the walking time and SpO2 improved after the intervention. A possible mechanism for the results of the present study may be related to CPAP decreasing the physiologic work of breathing, thereby unloading the respiratory musculature and reducing the likelihood of fatigue. It may have decreased the presence of hypoxia during walking and potentially contributed to the observed improvement in walking time.
Using plethysmography during walking, Pantoni et al. showed significant differences in VT and VE between the two groups [8]. Also, Al-Mutairi et al. demonstrated no significant difference in RR among all study groups [9]. Age, BMI, and group variables did not affect FVC and FEV1, but gender influenced FVC. Contrary to the results obtained in this study, Bittencourt et al., in a randomized controlled trial, proved that no difference was seen between the two groups in amounts of FVC and FEV1 before and after cardiac rehabilitation [17]. Perhaps different research communities and the duration of rehabilitation programs caused this variation in the results of the two studies. Additionally, Guimarães et al. demonstrated no significant difference in FVC and FEV1 between the two groups in the 1st, 2nd, and 24th hours after the operation [18]. A low sample size and different research communities led to these diversities among the above two studies. Therefore, FVC/FEV1 was not influenced by any independent variables, including age, gender, BMI, and group, but PEF was affected by BMI and group. On the other hand, Ferriera et al. indicated no significant differences in FVC, FEV1, and PEF variables in two control and intervention groups before and 18 months after the operation periods [5]. Probably, different methods applied in their study and measuring these variables before and after intervention yielded different results.
Findings of this study indicate that values of VT, FVC, FEV1, and PEF were statistically significant between the two groups, while RR, VE, and FVC/FEV1 were not. It seems that because of adequate ventilation in the intervention group and prevention of pulmonary endothelial dysfunction and due to the increase of alveolar stability, atelectasis is prevented, and oxygenation is improved. However, appropriate pulmonary muscles and diaphragm function were effective. They caused significant differences in spirometry parameters in the two studied groups. Since most of the spirometry parameters such as VT, VE, FVC, FEV1, and PEF were influenced by the group significantly and due to the researcher’s intervention, applying a ventilator assistant instrument featuring CPAP along with routine cardiac rehabilitation, it seems that increased pulmonary capacity is associated with this respiratory assistant procedure. It appears that in the intervention group, due to the proper establishment of ventilation, pulmonary endothelial dysfunction is prevented, and by increasing the stability of the alveoli, the amount of atelectasis decreases and improves oxygenation. In addition, the proper functioning of the lung and diaphragm muscles is also effective in improving the patient’s respiratory condition [19, 20, 21].
Placing a bulky mask of CPAP on the face of patients can cause anxiety, and this change can affect physiological parameters, including cardiovascular and respiratory function.
The study shows that adding a ventilation assistant gadget featuring CPAP to IS in cardiac rehabilitation programs improves the exercise and respiratory parameters after CABG, which can be considered in patients undergoing cardiac surgery. Usage of CPAP may cause alveolar re-opening and increase oxygenation, leading to non-spirometry and spirometry parameters (i.e. VT, VE, FVC, FEV1, and PEF) improvement after CABG. Therefore, it is recommended that a ventilatory assistant instrument featuring CPAP as a simple and modern tool to improve exercise and respiratory parameters should be applied. It can also be suggested to policymakers for rehabilitation programs after coronary artery bypass surgery.
Ethical Considerations
Compliance with ethical guidelines
This study was supported by the Deputy of Research and Technology and the Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1397.007) and Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20101019004971N5).
Funding
This study was funded by Guilan University of Medical Sciences.
Authors' contributions
Prepare the initial proposal, collect data, and write the manuscript: Fatemeh Roknishirazi; Technical consultant in the research process: Nazila Javadi-Pashaki; Statistical analysis: Ehsan Kazemnejad Lili; Clinical consultant in the research field: Mehrzad Ghasemzade; Corresponding author. Research supervisor and last version manuscript approval: Mohammad Taghi Moghadamnia; Approved the final version of manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the Deputy for Research of Guilan University of Medical Sciences and the patients hospitalized in the Heart surgery Department of Dr Heshmat Rasht Medical Training Center.
References
- Hinkle JL, Cheever KH. Brunner and suddarth’s textbook of medical - surgical nursing. Punjab: Wolters kluwer india Pvt Ltd; 2018.
- Pourshaikhian M, Moghadamnia MT, Yekaninejad MS, Ghanbari A, Rashti AS, Afraz Kamachli S. The effects of meteorological variables on ambulance attendance for cardiovascular diseases in Rasht, Iran. J Therm Biol. 2019; 83:150-6. [DOI:10.1016/j.jtherbio.2019.05.002] [PMID]
- Kachur S, Chongthammakun V, Lavie CJ, DeSchutter A, Arena R, Milani RV, et al. Impact of cardiac rehabilitation and exercise training programs in coronary heart disease. Prog Cardiovasc Dis. 2017; 60(1):103-14. [DOI:10.1016/j.pcad.2017.07.002] [PMID]
- Ghiasmand M, Moghadamnia MT, Pourshaikhian M, Kazemnejad Lili E. Acute triggers of myocardial infarction: A case-crossover study. Egypt Heart J. 2017; 69(4):223-8. [DOI:10.1016/j.ehj.2017.03.003] [PMID]
- Ferreira GM, Haeffner MP, Barreto SS, Dall'Ago P. Incentive spirometry with expiratory positive airway pressure brings benefits after myocardial revascularization. Arq Bras Cardiol. 2010; 94(2):230-5. [DOI:10.1590/s0066-782x2010000200017] [PMID]
- Andersen DK, Brunicardi CF. Schwartz’s principles of surgery. New York: Mc GrawHill; 2015.
- Paryad E. [Nursing care in open heart Intensive Care Unit (Persian)]. Rasht: Guilan University of Medical Sciences; 2012.
- Pantoni CB, Di Thommazo-Luporini L, Mendes RG, Caruso FC, Mezzalira D, Arena R, et al. Continuous positive airway pressure during exercise improves walking time in patients undergoing inpatient cardiac rehabilitation after coronary artery bypass graft surgery: A randomized controlled trial. J Cardiopulm Rehabil Prev. 2016; 36(1):20-7. [DOI:10.1097/HCR.0000000000000144] [PMID]
- Al-Mutairi FH, Fallows SJ, Abukhudair WA, Islam BB, Morris MM. Difference between continuous positive airway pressure via mask therapy and incentive spirometry to treat or prevent post-surgical atelectasis. Saudi Med J. 2012; 33(11):1190-5. [PMID]
- Sullivan KA, Churchill IF, Hylton DA, Hanna WC. Use of incentive spirometry in adults following cardiac, thoracic, and upper abdominal surgery to prevent postoperative pulmonary complications: A systematic review and meta-analysis. Respiration. 2021; 100(11):1114-27. [DOI:10.1159/000517012] [PMID]
- Odor PM, Bampoe S, Gilhooly D, Creagh-Brown B, Moonesinghe SR. Perioperative interventions for prevention of postoperative pulmonary complications: Systematic review and meta-analysis. BMJ. 2020; 368:m540. [DOI:10.1136/bmj.m540] [PMID]
- Sadahiro M. Cardiopulmonary rehabilitation using adaptive servo-ventilation after cardiac surgery. Circ J. 2015; 79(6):1204-5. [DOI:10.1253/circj.CJ-15-0407] [PMID]
- Cordeiro ALL, Gruska CA, Ysla P, Queiroz A, Nogueira SCO, Leite MC, et al. Effect of different levels of peep on oxygenation during noninvasive ventilation in patients submitted to CABG surgery: Randomized clinical trial. Braz J Cardiovasc Surg. 2017; 32(4):295-300. [DOI:10.21470/1678-9741-2016-0038] [PMID]
- Kamisaka K, Sakui D, Hagiwara Y, Kamiya K, Adachi T, Iida J, et al. Mechanical ventilatory assistance may reduce dyspnea during walking especially in patients with impaired cardiopulmonary function early after cardiovascular surgery. J Cardiol. 2016; 67(6):560-6. [DOI:10.1016/j.jjcc.2015.08.003] [PMID]
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982; 14(5):377-81. [PMID]
- Verlaine Balzan L, Vinícius Lovatto A, Fernando Nataniel V, Eraldo de Azevedo L, Laura Jurema S, et al. Ventilação não Invasiva após Cirurgia Cardiovascular: Um En- saio Clínico Randomizado / Non-invasive ventilation after cardiovascular surgery: A randomized clinical trial. Revista da Associação Médica Brasileira. 2014; 27(1):43-52. [Link]
- Portal Regional da BVS. VHL Regional Portal: Information and Knowledge for Health. Available from: [Link]
- Bittencourt HS, Cruz CG, David BC, Rodrigues E Jr, Abade CM, Junior RA, et al. Addition of noninvasive ventilatory support to combined aerobic and resistance training improves dyspnea and quality of life in heart failure patients: A randomized controlled trial. Clin Rehabil. 2017; 31(11):1508-15. [DOI:10.1177/0269215517704269] [PMID]
- Guimarães J, Pinho D, Nunes CS, Cavaleiro CS, Machado HS. Effect of Boussignac continuous positive airway pressure ventilation on PaO2 and PaO2/FIO2 ratio immediately after extubation in morbidly obese patients undergoing bariatric surgery: A randomized controlled trial. J Clin Anesth. 2016; 34:562-70. [DOI:10.1016/j.jclinane.2016.06.024] [PMID]
- Bolukçu A, İlhan S, Topçu AC, Günay R, Kayacıoğlu İ. Causes of dyspnea after cardiac surgery. Turk Thorac J. 2018; 19(4):165-9. [DOI:10.5152/TurkThoracJ.2018.17084] [PMID]
- Treschan TA, Schaefer M, Kemper J, Bastin B, Kienbaum P, Pannen B, et al. Ventilation with high versus low peep levels during general anaesthesia for open abdominal surgery does not affect postoperative spirometry. Eur J Anaesthesiol. 2017; 34(8):534-43. [DOI:10.1097/EJA.0000000000000626] [PMID]
Article Type : Research |
Subject:
General
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Received: 2024/02/24 | Accepted: 2024/02/21 | Published: 2024/02/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |