Tue, Dec 2, 2025
Volume 35, Issue 1 (1-2025)
JHNM 2025, 35(1): 62-70 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shahmohammadi D, Mousavizadeh S N, Ilkhani M, Nasiri M, Sattari M. Effect of a Nursing Care Program Based on King’s Theory of Goal Attainment on the Self-efficacy of Diabetic Patients. JHNM 2025; 35 (1) :62-70
URL: http://hnmj.gums.ac.ir/article-1-2270-en.html
URL: http://hnmj.gums.ac.ir/article-1-2270-en.html
Delshad Shahmohammadi1 

 , Seyedeh Narjes Mousavizadeh *2
, Seyedeh Narjes Mousavizadeh *2 

 , Mahnaz Ilkhani3
, Mahnaz Ilkhani3 

 , Malihe Nasiri4
, Malihe Nasiri4 
 , Mahtab Sattari5
, Mahtab Sattari5 




 , Seyedeh Narjes Mousavizadeh *2
, Seyedeh Narjes Mousavizadeh *2 

 , Mahnaz Ilkhani3
, Mahnaz Ilkhani3 

 , Malihe Nasiri4
, Malihe Nasiri4 
 , Mahtab Sattari5
, Mahtab Sattari5 


1- Nursing (MsN), Student Research Committee, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Assistant Professor, Department of Psychiatric Nursing and Management, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,n.mousavi@sbmu.ac.ir
3- Associate Professor, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Assistant Professor, Department of Basic Sciences, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
5- PhD Candidate of Reproductive Health, Student Research Committee, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Assistant Professor, Department of Psychiatric Nursing and Management, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,
3- Associate Professor, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Assistant Professor, Department of Basic Sciences, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
5- PhD Candidate of Reproductive Health, Student Research Committee, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 647 kb]
(746 Downloads)
| Abstract (HTML) (924 Views)
Full-Text: (1422 Views)
Introduction
Diabetes is one of the most common and serious metabolic diseases and also one of the major health concerns in the world [1, 2]. According to the statistics of the World Health Organization (WHO), people in Asia and the Middle East are at higher risk for diabetes, and 80% of diabetic patients live in developing countries [3]. According to the WHO report, the overall prevalence of diabetes in Iran in 2020 was 10.3%, where obesity (24.9%), lack of physical activity (31.9%), and overweight (60.5%) were the main risk factors for diabetes [4]. This disease is not curable but can be managed [5]. Successful prevention and management of diabetes complications require preventive and therapeutic measures. This is possible if the patient actively participates in the treatment process and follows the physicians’ recommendations, or has self-efficacy [6, 7].
Patient-centered approach (focuses on patient empowerment) and community-centered approach (moves care from the hospital into the community) are two attractive approaches to health [8, 9]. Both approaches seek to empower patients to adopt self-care behaviors by providing them with the support and care they need outside of clinical settings such as hospitals and clinics [10]. Imogene King’s theory of goal attainment is one of the most important nursing models as it comprehensively and deeply addresses patient participation and interaction in the treatment process [11]. This model proposes three interacting systems: Personal, interpersonal, and social [12]. The personal system includes patients, nurses, and their understanding [11]. In patients with chronic diseases, the disease complications change the perception of life. The personal system focuses on helping them adapt to these changes [13]. The interpersonal system, the most important concept of the theory, consists of the concepts of communication, interaction, stress, and role [11]. Considering the considerable effects of chronic diseases on stress and the role of the patient, appropriate communication between the patient and the physician and their active interactions in this process are necessary for the patient’s physical and psychological health [14]. The social system includes the decision-making process [11]. This process is critical in treating and caring for patients with chronic diseases such as diabetes [13]. Therefore, the theory of goal attainment facilitates patient-centered and family-centered care by providing a framework for establishing a mutual and therapeutic relationship between nurses and patients based on their mutual understanding [15]. Based on this theory, the nurse systematically and thoroughly examines the patient using interviews, observations, and examinations and then determines the goals (the patient’s problems) after reaching an agreement with the patient. The nurse and the patient then try to achieve the goals through interactions [16, 17].
King’s theory of goal attainment is an effective approach to nursing practice in various situations [18, 19], because it reduces the risk of poor communication, lowers stress during care, establishes more targeted nurse-patient relationships, facilitates patients’ adaptation to hospital discharge and nursing care plans [20, 21], and hence gives the patients a chance to better know their bodies and its functioning in terms of time and place [22]. Many studies in different countries have used the concepts of the goal attainment theory in nursing, but it has been neglected in Iranian studies [16, 17, 21, 23 ]. In addition, given the importance of evidence-based practice in providing care for patients with chronic conditions, and considering the fact that few studies have examined the application of King’s theory of goal attainment in promoting self-efficacy of diabetic patients, this study aims to investigate the effect of applying King’s theory of goal attainment on self-efficacy in patients with type 2 diabetes in Iran.
Material and Methods
This quasi-experimental study was conducted on 60 eligible patients with type 2 diabetes admitted to the endocrinology departments of two hospitals affiliated with Shahid Beheshti University of Medical Sciences in Tehran, Iran, who were selected using a convenience sampling method. After signing an informed consent form, they were randomly assigned to the intervention and control groups (30 per group) using a table of random numbers. In this table, even numbers were considered for the intervention group and odd numbers were considered for the control group. To prevent data leakage between the two groups, the single-blinding method was used, and the patients did not know which group they were in.
In this study, the required sample size was determined at a confidence interval of 95% (error rate of 5%), a test power of 95%, and an effect size of 1 using the formula of comparison of two means and based on the study of Feghhi et al. [24] who put 24 people in the control group and 24 people in the intervention group. In this regard, the sample size was calculated as 30 per group.
The inclusion criteria were the diagnosis of type 2 diabetes (in the past year by a physician), Persian speaking, ability to interact with the researcher, adherence to the treatment plan, and having no mental disability (e.g. mental or cognitive disorders that could prevent the patients from participating in the decision-making process). The exclusion criteria were participation in non-routine educational programs or similar studies during the current study and inability to continue participation in the study for any reason. If a patient could not participate in all intervention sessions, the sessions were rescheduled or performed intensively for them; otherwise, s/he would be excluded from the study. Sampling was done in the morning and evening shifts (at least three days per week).
The data were collected using a sociodemographic/clinical form, the diabetes management self-efficacy scale (DMSES), and the goal attainment scaling (GAS). The sociodemographic/clinical form surveyed age, gender, marital status, educational level, economic status, duration of diabetes, and family history of diabetes. The DMSES is a 20-item instrument with four subscales: Diet and nutrition (9 items), medication and leg examination (3 items), physical activity (3 items), and medical care (5 items). The items are scored on an 11-point Likert scale ranging from 1 (not at all confident) to 10 (totally confident). The total score ranges from 20 to 200, with higher scores indicating greater self-efficacy. The DMSES was used because it has been translated and psychometrically evaluated in Iran by the Mohammadi-Nejad et al. study [23]. In our study, the internal consistency of this scale was investigated by randomly distributing the questionnaire among 30 diabetic patients (who were not among the participants) and a Cronbach’s α of 0.89 was obtained. The GAS was designed in 1998 by the King international nursing group based on King’s theory of goal attainment and has been used in other studies [16, 25]. The GAS lists each patient’s care goals based on three systems (personal, interpersonal, and social), specifies the expected outcomes for each patient based on their conditions and priorities, and measures how well a patient attains a specific goal. The items are scored on a five-point Likert scale from -2 to +2: Achievement of much less than expected goal (-2), achievement of somewhat less than expected goal (-1), achievement of a goal (0), achievement of somewhat more than expected goal (1), and achievement of much more than expected goal (2). We translated the GAS into Persian and then back-translated it into English after obtaining permission from the scale developer. In the next step, a panel of experts (15 professors from Shahid-Beheshti University of Medical Sciences) determined the “relevance”, “unambiguity”, and “simplicity” of the items by rating them on a Likert scale. After confirming the content validity of the Persian version, its test-rested reliability was confirmed with an intraclass correlation coefficient of 0.93. The DMSES was completed before intervention, two weeks after, and two months after by the researcher (at a time appropriate for the patients) by the face-to-face method or through the phone (if the patients were discharged from the hospital).
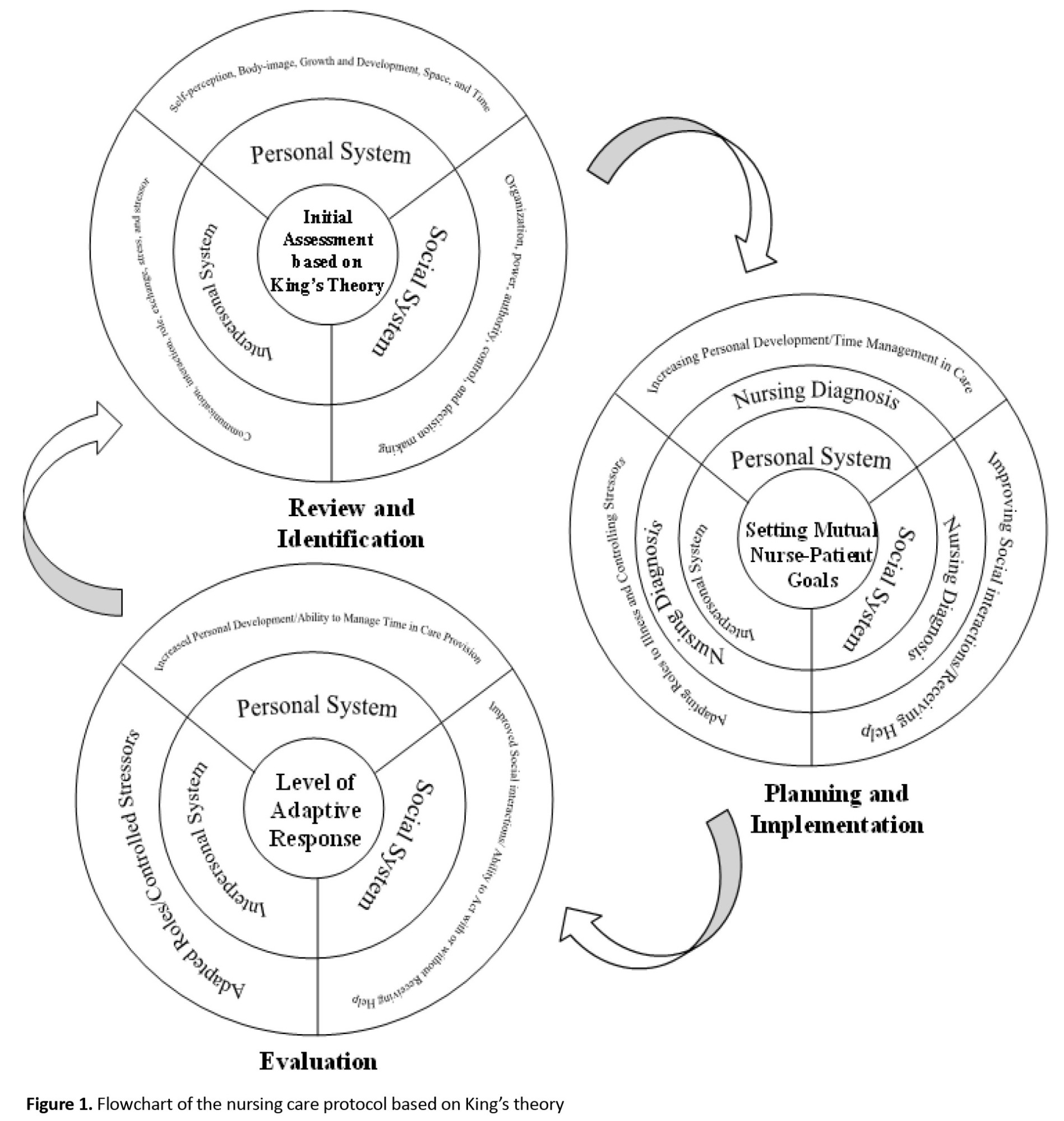
The control group received routine care and training in the ward. In addition to the routine nursing care and training, the intervention group participated in a nursing care program developed based on King’s theory of goal attainment. The priorities of the patient’s care needs based on King’s three interactive systems were first examined by the GAS. Mutual goal setting was achieved after implementing a nursing care protocol for each patient separately. Three main mutual goals or criteria were determined to measure each patient’s problems. The “personal,” “interpersonal,” and “social” systems included the criteria of “increasing personal development and time management in care,” “adapting roles and controlling stressors,” and “improving social interactions and receiving help,” respectively. After setting goals, the nursing care program was implemented for ten consecutive days, where the patients were taught how to adapt their roles to the disease and were asked to practice the methods. The duration of the intervention was ten days, according to Vincent’s study [27]. The training was conducted once a day, each session for 20 minutes individually and face to face in the hospital or through the phone for the patients at home. Patients were also given educational booklets. Figure 1 shows a flowchart of the nursing care protocol developed based on King’s theory of goal attainment to help diabetic patients with major personal, interpersonal, and social problems to improve their adaptive response [27]. The SPSS software, version 20 was used for data analysis. Chi-square test was used to compare the two groups in terms of sociodemographic/clinical characteristics. Also, independent t-test, paired t-test, and repeated measures ANOVA were used to compare the DMSES score. Before conducting ANOVA, the Box’s M test, Mauchly’s sphericity test, Levene’s test, and Kolmogorov-Smirnov test were performed to examine the assumptions of the equality of variance-covariance matrices, sphericity, homogeneity of the variances, and normality of the data distribution. The results of the Box’s M test showed that the variance-covariance matrices were not homogeneous. In the Mauchly’s sphericity test, the estimated epsilon (ε) and P were 0.75 and 0.05, respectively; thus, the assumption of sphericity was rejected. Therefore, the Greenhouse-Geisser test was used to correct this violation.
Results
Most of the participants were in the age range of 51-60 (40% in the intervention group and 46.7% in the control group). In addition, the majority of them were female (70% in the intervention group and 66.7% in the control group), married (63.3% in the intervention group and 80% in the control group), with moderate socioeconomic status (60% in the intervention group and 53.3% in the control group) and illiterate (30%). Using the chi-square test was showed there was no significant difference in terms of individual and social variables. Moreover, most patients had been diagnosed with diabetes 5-10 years ago (26.7% in the intervention group and 70% in the control group) and had a family history of diabetes (83% in the intervention group and 67% in the control group).
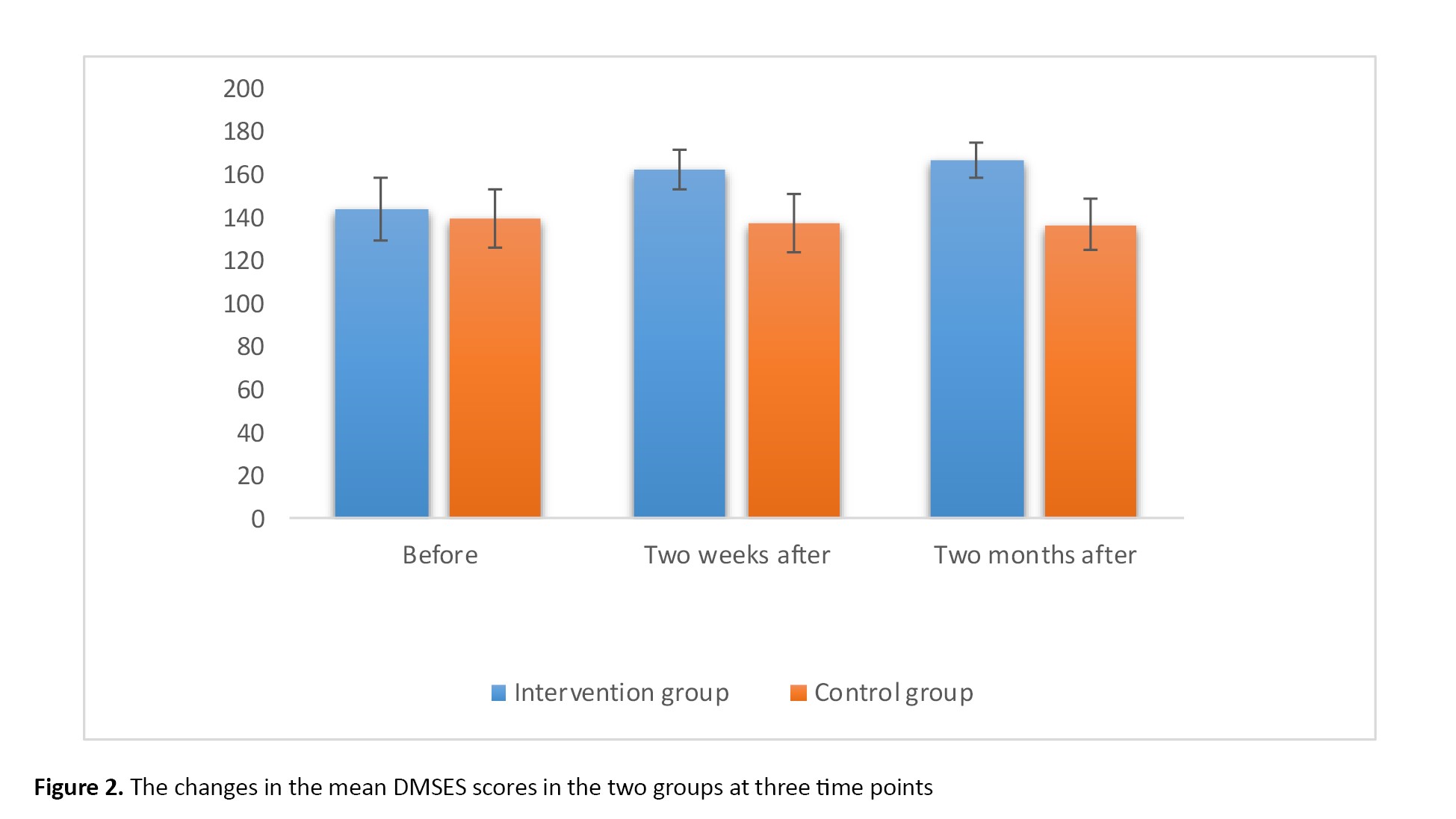
The mean DMSES score in the intervention group increased from 144.1±14.13 to 162.26±8.97 two weeks after the intervention. In the control group, the mean DMSES score was 139.63±13.46 before the intervention, and did not change significantly after the intervention. Two months after the intervention, the mean DMSES score of the intervention group (166.50±8.16) was higher than that of the control group. It was also higher than the mean post-test score (two weeks after the intervention), suggesting that the nursing care program increased the self-efficacy of patients over time (Table 1).
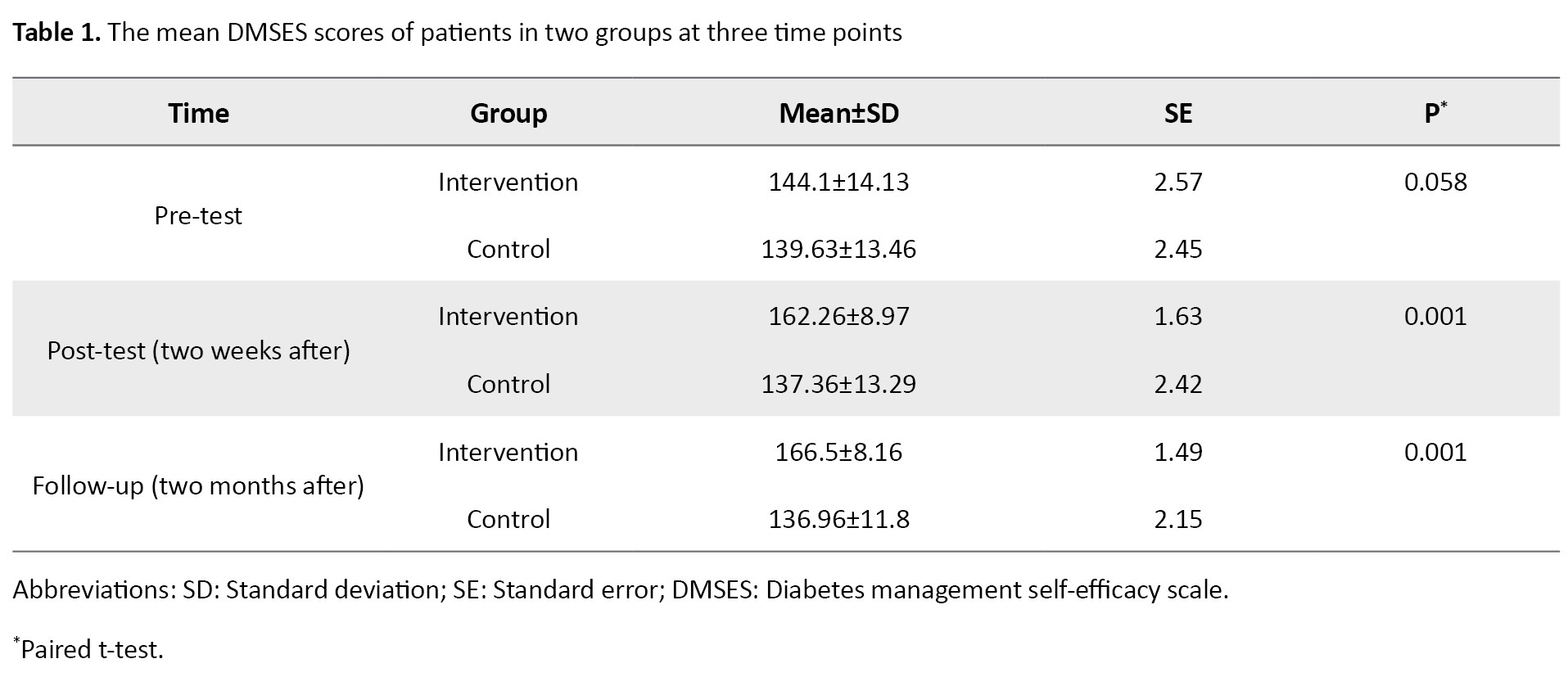
Figure 2 compares the mean DMSES scores of the two groups before, two weeks after, and two months after the intervention. Results showed no significant difference between the two groups in the DMSES score before the intervention. However, significant differences were observed between them two weeks after (P=0.001) and two months after (P=0.001) the intervention (Table 2).
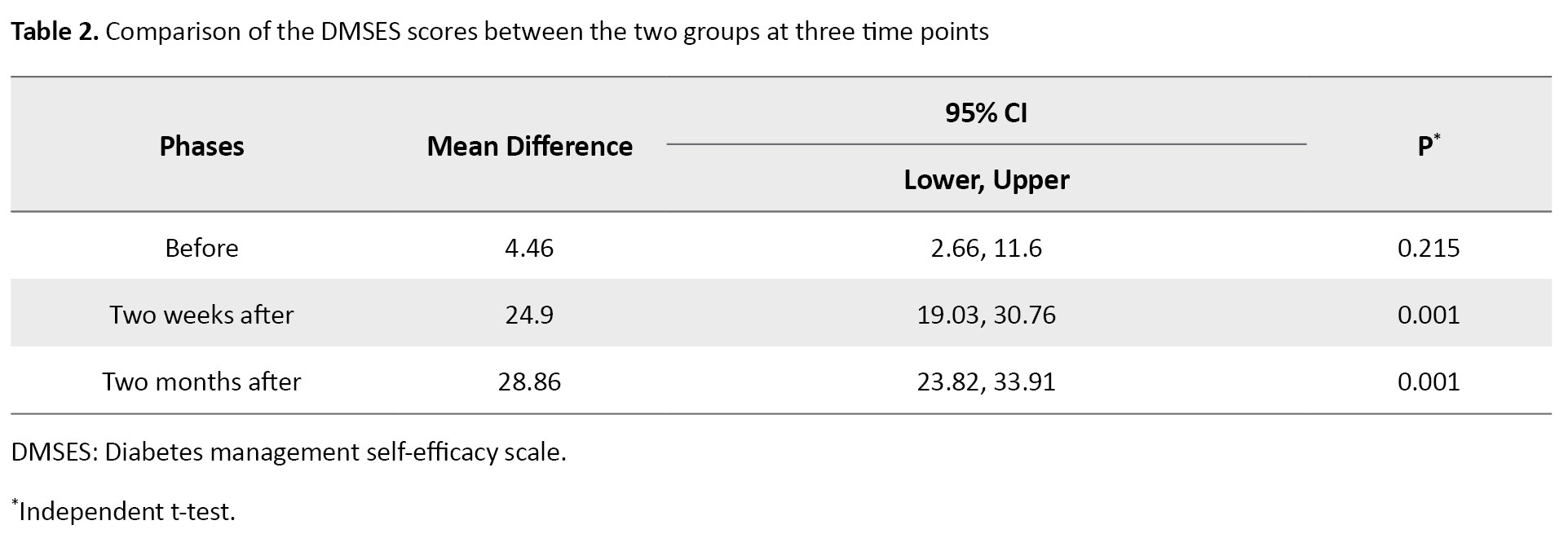
Table 3 shows the results for the pairwise comparison of three assessment phases using the paired t-test.
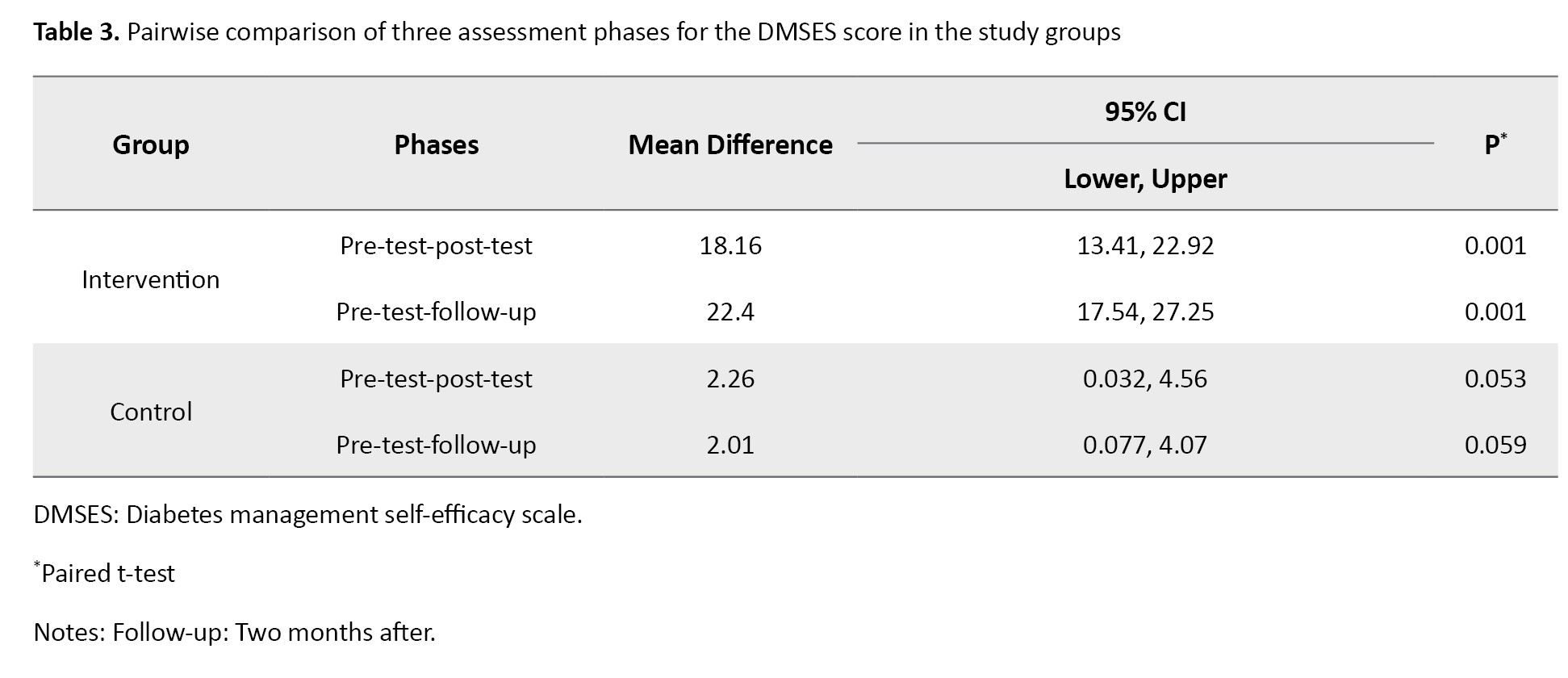
There were a significant difference in the mean DMSES score in the intervention group between pre-test and post-test (P=0.001), and between pre-test and follow-up (P=0.001) phases.
The repeated measures ANOVA was used to further examine the interaction effects of time (measurement phase) and group on the DMSES score. As shown in Table 4, the results showed that the effect of time and the interaction effect of time and group were significant (P=0.001).
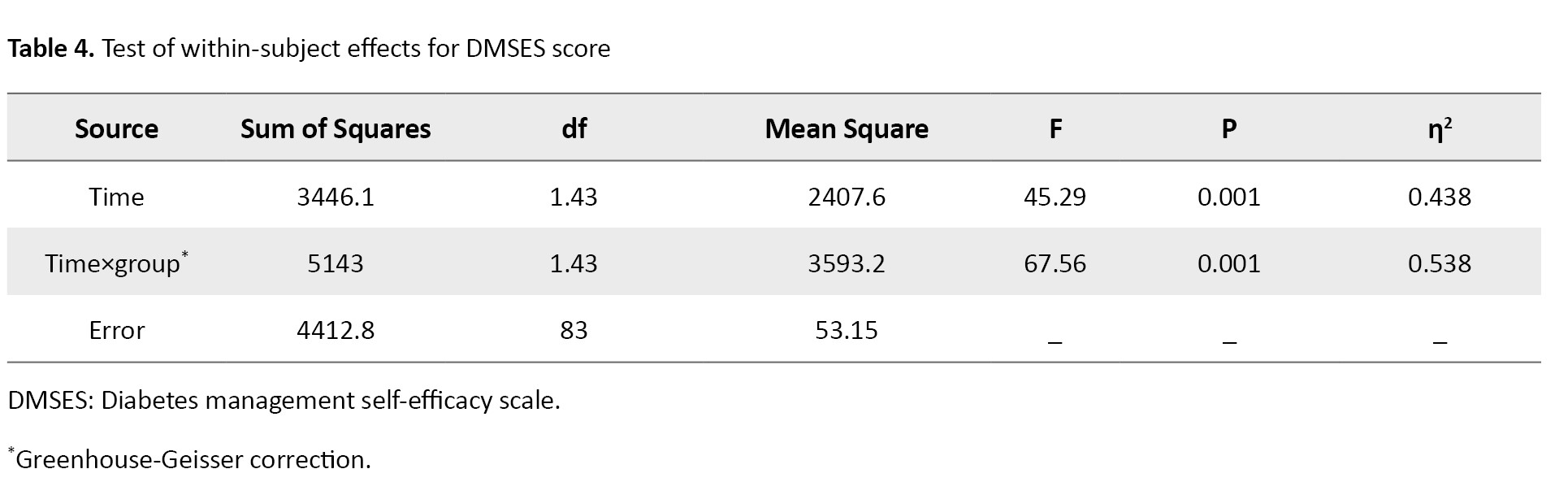
In other words, the improvements in DMSES score were significant two weeks and two months after the intervention in the intervention group compared to the control group.
Discussion
This study used King’s theory of goal attainment to determine three main nurse-patient interaction systems (personal, interpersonal, and social) for improving the self-efficacy of patients with type 2 diabetes. The personal, interpersonal, and social systems included the goals of “increasing personal development and time management in care,” “adapting roles to disease and controlling stressors,” and “improving social interactions and receiving help,” respectively. A systematic review of studies on the effectiveness of nursing interventions based on King’s theory has shown that 40% of studies have used the theory in educational fields and 60% in the clinical field. The review study suggested that King’s proposed systems and theory can provide a valuable approach for nurses facing complex health care situations in the hospitals [26]. The results of the present study are consistent with this study and confirm that King’s goal attainment theory is a suitable model to guide professional nursing care which supports patients, respects their rights (social system), emphasizes their health rights (individual system) and ensures participation in health care practices (interpersonal system).
The results of this study indicated that the nursing care program based on the goal attainment theory significantly increased the self-efficacy (DMSES score) in the intervention group compared to the control group, and after intervention (two weeks after) compared to the pre-intervention phase. In addition, the self-efficacy in the intervention group increased significantly two months after the intervention (follow-up) compared to the pre-intervention phase.
In a case study, Vincent used King’s theory in providing care to a client with self-image problem, and suggested that the implementation of the nursing interventions based on King’s model increased the level of adaptive response in the client [27]. Another study observed significant adherence to the defined goals among diabetic patients after intervention [16]. These two studies concluded that King’s theory can be well integrated into the family health strategy (FHS) program to achieve the expected goals. Bezerra et al. investigated nurses’ perceptions of King’s theory and observed that the conceptual model of interactive open systems developed based on King’s theory provided adequate explanations about primary health care in hypertensive patients [28]. It seems that routine methods, which are not mainly patient-centered, are used in the care of patients in the current health system. This affects the quality of care, especially in chronic diseases where the patient’s compliance with the treatment is poor, and the patient leaves the treatment after a while, and the symptoms re-occur. Therefore, using patient-centered and interactive methods can be a solution to this problem.
In our study, two months after the application of King’s theory in a nursing program, the mean DMSES score in the intervention group was significantly higher than the scores of pre-test and post-test (two weeks after the intervention). This is along to the findings of a study in Iran where the behavior changes of diabetic patients were assessed before and four months after the intervention, and a significant increase in the mean self-efficacy score was reported [29]. However, application of a new intervention may not lead to positive outcomes. In a feasibility study, regular follow-up was done for 6 months by making frequent calls and insisting on regular visits for examination [30].
In King’s nursing theory, the direct interaction between the nurse and the patient is emphasized, which indicates patients’ participation in care plans. In this way, diabetic patients can receive information from the nurse and choose options according to their conditions. Therefore, the care program is designed and implemented based on the selected priorities of the patient, which can lead to more acceptance of and compliance with the care program in diabetic patients [31-33]. Nursing theories, although they provide very useful theoretical and practical frameworks in care, their effects on solving health system problems, quality of care, patient satisfaction, and reduction of health costs are still unknown, and the use of care models based on the interaction between the nurse and the patient has been neglected.
One of the limitations of this study was the low cooperation of the patients in the study because of the long intervention period. In this regard, the researchers tried to motivate them throughout the study by explaining the possible benefits of the study for the patients or by considering incentives for them. Based on the results, it can be concluded that a systematic care program based on King’s theory can help diabetic patients identify their problems in the three human systems and find ways to achieve mutual nurse-patient goals. In addition, it can improve the self-efficacy of diabetic patients two weeks and two months after the intervention. Therefore, future studies are recommended to investigate the effect of this nursing care program on other patients to identify and solve their problems and challenges and pave the way for the application of nursing theories in routine clinical practice.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the School of Pharmacy and Nursing, and the School of Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran (Code: IR.SBMU.PHARMACY.REC.1401.103).
Funding
This study was funded by Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Authors' contributions
Conceptualization, investigation, and methodology: Seyedeh Narjes Mousavizadeh, Delshad Shahmohammadi, and Mahnaz Ilkhani; Formal analysis: Seyedeh Narjes Mousavizadeh and Delshad Shahmohammadi; Supervision: Seyedeh Narjes Mousavizadeh; Visualization, review and editing: Seyedeh Narjes Mousavizadeh, Delshad Shahmohammadi, and Mahtab Sattari; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the participants for their cooperation in this research, and the Deputy for Research of Shahid Beheshti University of Medical Sciences, Tehran, Iran for the financial support of this study.
References
Diabetes is one of the most common and serious metabolic diseases and also one of the major health concerns in the world [1, 2]. According to the statistics of the World Health Organization (WHO), people in Asia and the Middle East are at higher risk for diabetes, and 80% of diabetic patients live in developing countries [3]. According to the WHO report, the overall prevalence of diabetes in Iran in 2020 was 10.3%, where obesity (24.9%), lack of physical activity (31.9%), and overweight (60.5%) were the main risk factors for diabetes [4]. This disease is not curable but can be managed [5]. Successful prevention and management of diabetes complications require preventive and therapeutic measures. This is possible if the patient actively participates in the treatment process and follows the physicians’ recommendations, or has self-efficacy [6, 7].
Patient-centered approach (focuses on patient empowerment) and community-centered approach (moves care from the hospital into the community) are two attractive approaches to health [8, 9]. Both approaches seek to empower patients to adopt self-care behaviors by providing them with the support and care they need outside of clinical settings such as hospitals and clinics [10]. Imogene King’s theory of goal attainment is one of the most important nursing models as it comprehensively and deeply addresses patient participation and interaction in the treatment process [11]. This model proposes three interacting systems: Personal, interpersonal, and social [12]. The personal system includes patients, nurses, and their understanding [11]. In patients with chronic diseases, the disease complications change the perception of life. The personal system focuses on helping them adapt to these changes [13]. The interpersonal system, the most important concept of the theory, consists of the concepts of communication, interaction, stress, and role [11]. Considering the considerable effects of chronic diseases on stress and the role of the patient, appropriate communication between the patient and the physician and their active interactions in this process are necessary for the patient’s physical and psychological health [14]. The social system includes the decision-making process [11]. This process is critical in treating and caring for patients with chronic diseases such as diabetes [13]. Therefore, the theory of goal attainment facilitates patient-centered and family-centered care by providing a framework for establishing a mutual and therapeutic relationship between nurses and patients based on their mutual understanding [15]. Based on this theory, the nurse systematically and thoroughly examines the patient using interviews, observations, and examinations and then determines the goals (the patient’s problems) after reaching an agreement with the patient. The nurse and the patient then try to achieve the goals through interactions [16, 17].
King’s theory of goal attainment is an effective approach to nursing practice in various situations [18, 19], because it reduces the risk of poor communication, lowers stress during care, establishes more targeted nurse-patient relationships, facilitates patients’ adaptation to hospital discharge and nursing care plans [20, 21], and hence gives the patients a chance to better know their bodies and its functioning in terms of time and place [22]. Many studies in different countries have used the concepts of the goal attainment theory in nursing, but it has been neglected in Iranian studies [16, 17, 21, 23 ]. In addition, given the importance of evidence-based practice in providing care for patients with chronic conditions, and considering the fact that few studies have examined the application of King’s theory of goal attainment in promoting self-efficacy of diabetic patients, this study aims to investigate the effect of applying King’s theory of goal attainment on self-efficacy in patients with type 2 diabetes in Iran.
Material and Methods
This quasi-experimental study was conducted on 60 eligible patients with type 2 diabetes admitted to the endocrinology departments of two hospitals affiliated with Shahid Beheshti University of Medical Sciences in Tehran, Iran, who were selected using a convenience sampling method. After signing an informed consent form, they were randomly assigned to the intervention and control groups (30 per group) using a table of random numbers. In this table, even numbers were considered for the intervention group and odd numbers were considered for the control group. To prevent data leakage between the two groups, the single-blinding method was used, and the patients did not know which group they were in.
In this study, the required sample size was determined at a confidence interval of 95% (error rate of 5%), a test power of 95%, and an effect size of 1 using the formula of comparison of two means and based on the study of Feghhi et al. [24] who put 24 people in the control group and 24 people in the intervention group. In this regard, the sample size was calculated as 30 per group.
The inclusion criteria were the diagnosis of type 2 diabetes (in the past year by a physician), Persian speaking, ability to interact with the researcher, adherence to the treatment plan, and having no mental disability (e.g. mental or cognitive disorders that could prevent the patients from participating in the decision-making process). The exclusion criteria were participation in non-routine educational programs or similar studies during the current study and inability to continue participation in the study for any reason. If a patient could not participate in all intervention sessions, the sessions were rescheduled or performed intensively for them; otherwise, s/he would be excluded from the study. Sampling was done in the morning and evening shifts (at least three days per week).
The data were collected using a sociodemographic/clinical form, the diabetes management self-efficacy scale (DMSES), and the goal attainment scaling (GAS). The sociodemographic/clinical form surveyed age, gender, marital status, educational level, economic status, duration of diabetes, and family history of diabetes. The DMSES is a 20-item instrument with four subscales: Diet and nutrition (9 items), medication and leg examination (3 items), physical activity (3 items), and medical care (5 items). The items are scored on an 11-point Likert scale ranging from 1 (not at all confident) to 10 (totally confident). The total score ranges from 20 to 200, with higher scores indicating greater self-efficacy. The DMSES was used because it has been translated and psychometrically evaluated in Iran by the Mohammadi-Nejad et al. study [23]. In our study, the internal consistency of this scale was investigated by randomly distributing the questionnaire among 30 diabetic patients (who were not among the participants) and a Cronbach’s α of 0.89 was obtained. The GAS was designed in 1998 by the King international nursing group based on King’s theory of goal attainment and has been used in other studies [16, 25]. The GAS lists each patient’s care goals based on three systems (personal, interpersonal, and social), specifies the expected outcomes for each patient based on their conditions and priorities, and measures how well a patient attains a specific goal. The items are scored on a five-point Likert scale from -2 to +2: Achievement of much less than expected goal (-2), achievement of somewhat less than expected goal (-1), achievement of a goal (0), achievement of somewhat more than expected goal (1), and achievement of much more than expected goal (2). We translated the GAS into Persian and then back-translated it into English after obtaining permission from the scale developer. In the next step, a panel of experts (15 professors from Shahid-Beheshti University of Medical Sciences) determined the “relevance”, “unambiguity”, and “simplicity” of the items by rating them on a Likert scale. After confirming the content validity of the Persian version, its test-rested reliability was confirmed with an intraclass correlation coefficient of 0.93. The DMSES was completed before intervention, two weeks after, and two months after by the researcher (at a time appropriate for the patients) by the face-to-face method or through the phone (if the patients were discharged from the hospital).
The control group received routine care and training in the ward. In addition to the routine nursing care and training, the intervention group participated in a nursing care program developed based on King’s theory of goal attainment. The priorities of the patient’s care needs based on King’s three interactive systems were first examined by the GAS. Mutual goal setting was achieved after implementing a nursing care protocol for each patient separately. Three main mutual goals or criteria were determined to measure each patient’s problems. The “personal,” “interpersonal,” and “social” systems included the criteria of “increasing personal development and time management in care,” “adapting roles and controlling stressors,” and “improving social interactions and receiving help,” respectively. After setting goals, the nursing care program was implemented for ten consecutive days, where the patients were taught how to adapt their roles to the disease and were asked to practice the methods. The duration of the intervention was ten days, according to Vincent’s study [27]. The training was conducted once a day, each session for 20 minutes individually and face to face in the hospital or through the phone for the patients at home. Patients were also given educational booklets. Figure 1 shows a flowchart of the nursing care protocol developed based on King’s theory of goal attainment to help diabetic patients with major personal, interpersonal, and social problems to improve their adaptive response [27]. The SPSS software, version 20 was used for data analysis. Chi-square test was used to compare the two groups in terms of sociodemographic/clinical characteristics. Also, independent t-test, paired t-test, and repeated measures ANOVA were used to compare the DMSES score. Before conducting ANOVA, the Box’s M test, Mauchly’s sphericity test, Levene’s test, and Kolmogorov-Smirnov test were performed to examine the assumptions of the equality of variance-covariance matrices, sphericity, homogeneity of the variances, and normality of the data distribution. The results of the Box’s M test showed that the variance-covariance matrices were not homogeneous. In the Mauchly’s sphericity test, the estimated epsilon (ε) and P were 0.75 and 0.05, respectively; thus, the assumption of sphericity was rejected. Therefore, the Greenhouse-Geisser test was used to correct this violation.
Results
Most of the participants were in the age range of 51-60 (40% in the intervention group and 46.7% in the control group). In addition, the majority of them were female (70% in the intervention group and 66.7% in the control group), married (63.3% in the intervention group and 80% in the control group), with moderate socioeconomic status (60% in the intervention group and 53.3% in the control group) and illiterate (30%). Using the chi-square test was showed there was no significant difference in terms of individual and social variables. Moreover, most patients had been diagnosed with diabetes 5-10 years ago (26.7% in the intervention group and 70% in the control group) and had a family history of diabetes (83% in the intervention group and 67% in the control group).
The mean DMSES score in the intervention group increased from 144.1±14.13 to 162.26±8.97 two weeks after the intervention. In the control group, the mean DMSES score was 139.63±13.46 before the intervention, and did not change significantly after the intervention. Two months after the intervention, the mean DMSES score of the intervention group (166.50±8.16) was higher than that of the control group. It was also higher than the mean post-test score (two weeks after the intervention), suggesting that the nursing care program increased the self-efficacy of patients over time (Table 1).
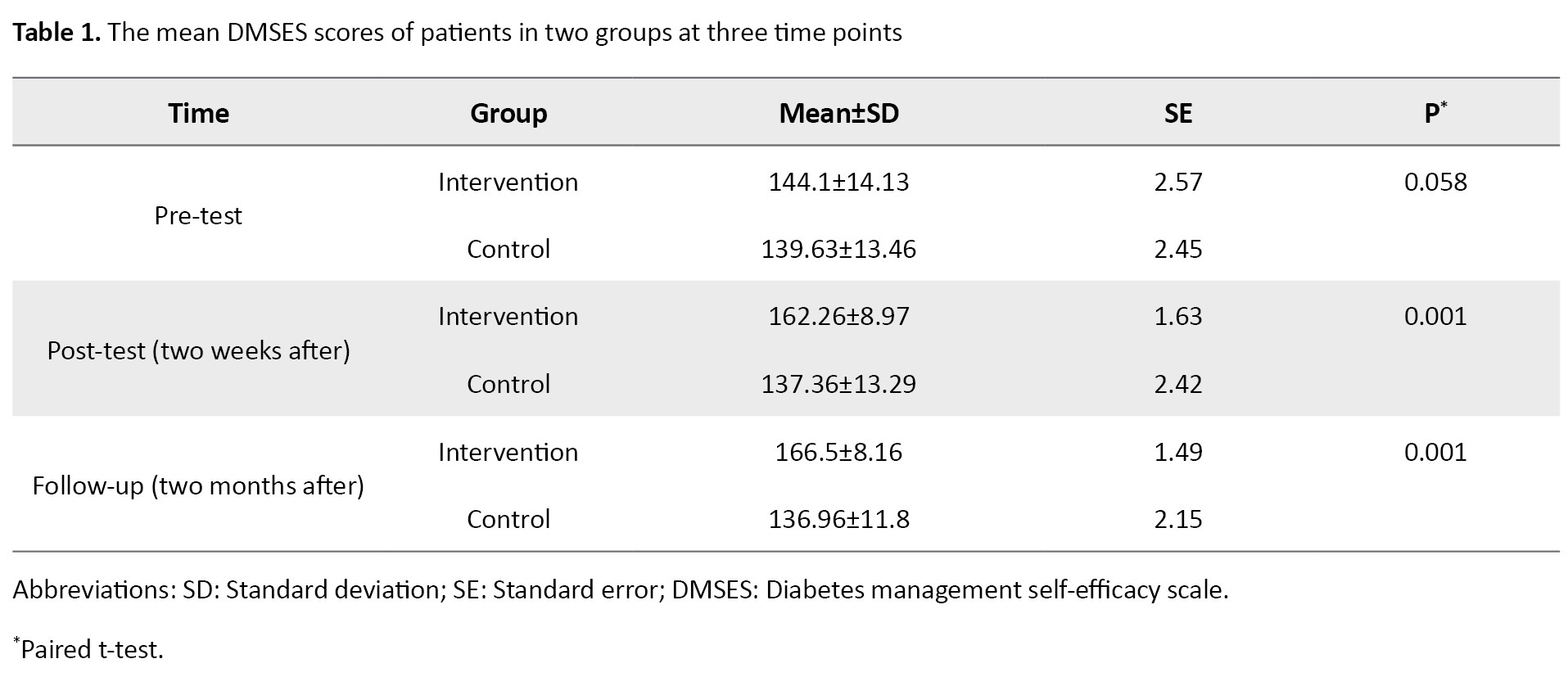
Figure 2 compares the mean DMSES scores of the two groups before, two weeks after, and two months after the intervention. Results showed no significant difference between the two groups in the DMSES score before the intervention. However, significant differences were observed between them two weeks after (P=0.001) and two months after (P=0.001) the intervention (Table 2).
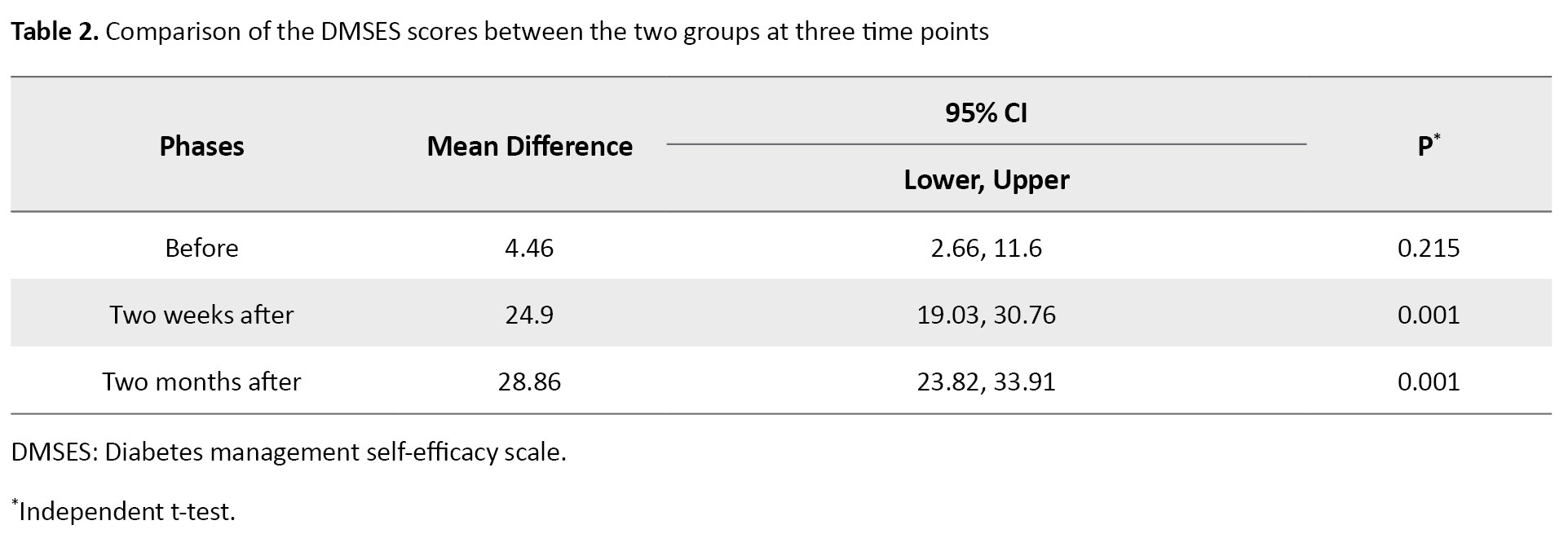
Table 3 shows the results for the pairwise comparison of three assessment phases using the paired t-test.
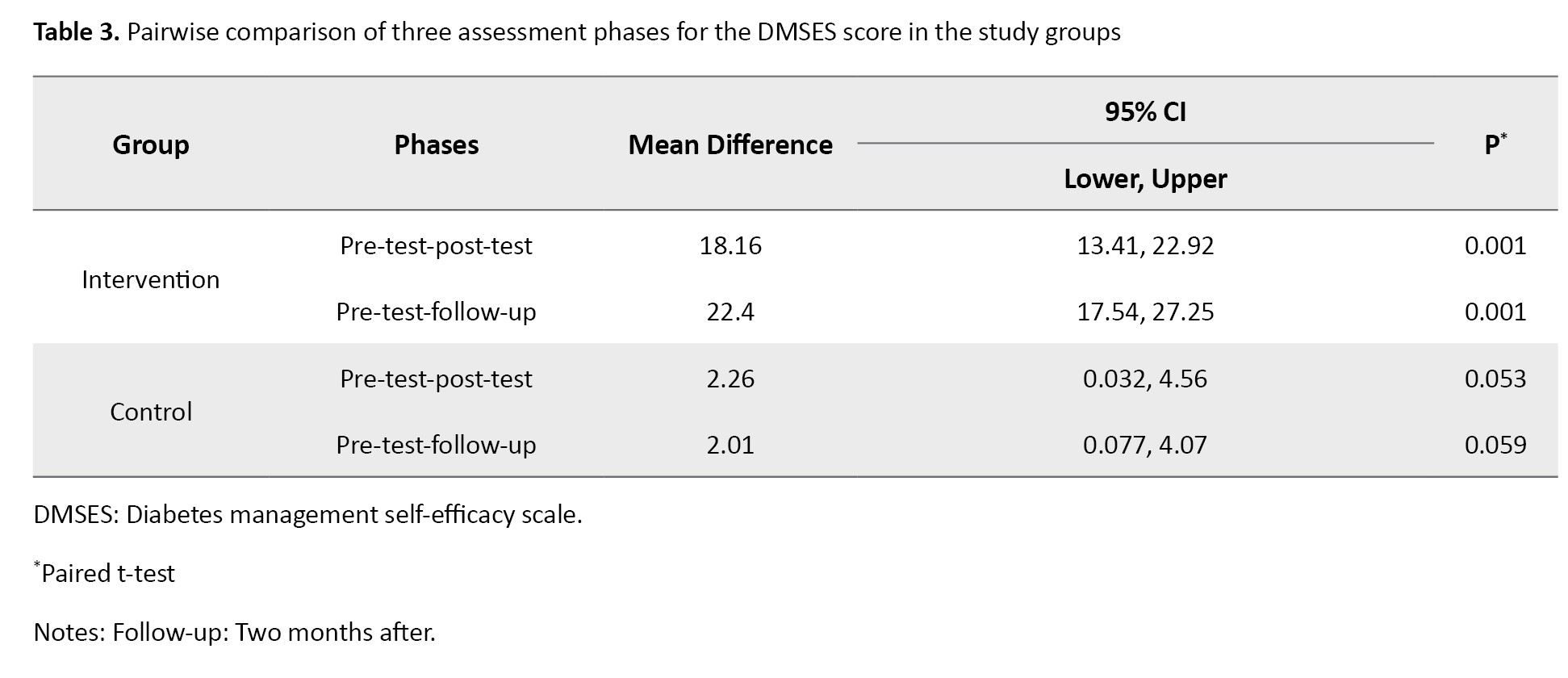
There were a significant difference in the mean DMSES score in the intervention group between pre-test and post-test (P=0.001), and between pre-test and follow-up (P=0.001) phases.
The repeated measures ANOVA was used to further examine the interaction effects of time (measurement phase) and group on the DMSES score. As shown in Table 4, the results showed that the effect of time and the interaction effect of time and group were significant (P=0.001).
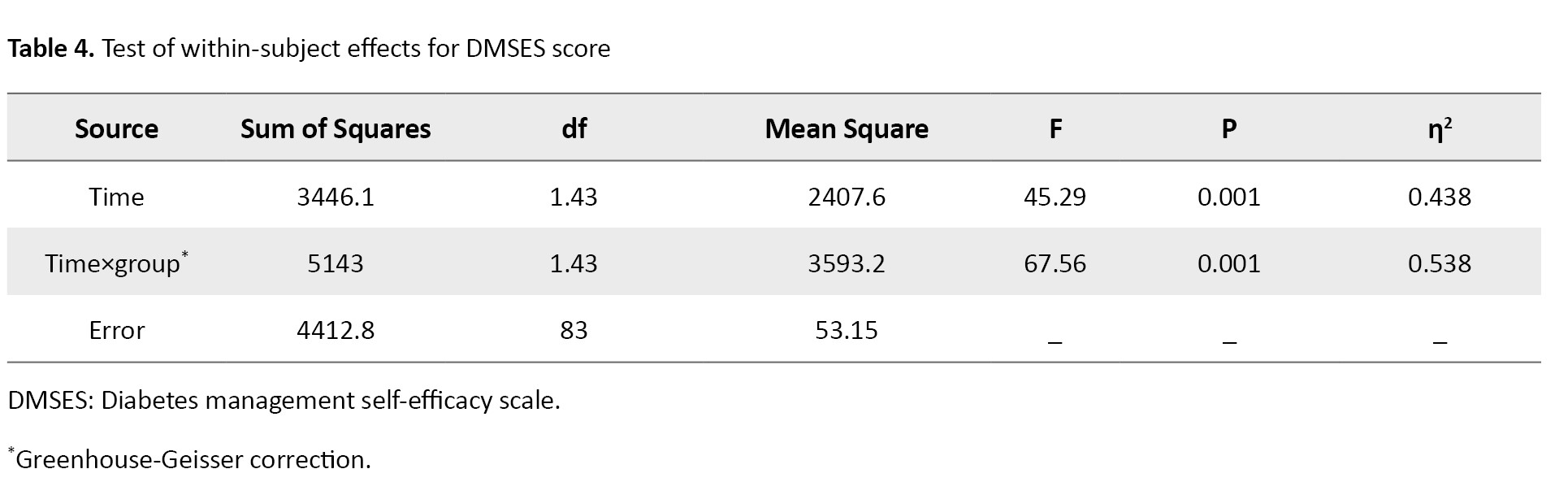
In other words, the improvements in DMSES score were significant two weeks and two months after the intervention in the intervention group compared to the control group.
Discussion
This study used King’s theory of goal attainment to determine three main nurse-patient interaction systems (personal, interpersonal, and social) for improving the self-efficacy of patients with type 2 diabetes. The personal, interpersonal, and social systems included the goals of “increasing personal development and time management in care,” “adapting roles to disease and controlling stressors,” and “improving social interactions and receiving help,” respectively. A systematic review of studies on the effectiveness of nursing interventions based on King’s theory has shown that 40% of studies have used the theory in educational fields and 60% in the clinical field. The review study suggested that King’s proposed systems and theory can provide a valuable approach for nurses facing complex health care situations in the hospitals [26]. The results of the present study are consistent with this study and confirm that King’s goal attainment theory is a suitable model to guide professional nursing care which supports patients, respects their rights (social system), emphasizes their health rights (individual system) and ensures participation in health care practices (interpersonal system).
The results of this study indicated that the nursing care program based on the goal attainment theory significantly increased the self-efficacy (DMSES score) in the intervention group compared to the control group, and after intervention (two weeks after) compared to the pre-intervention phase. In addition, the self-efficacy in the intervention group increased significantly two months after the intervention (follow-up) compared to the pre-intervention phase.
In a case study, Vincent used King’s theory in providing care to a client with self-image problem, and suggested that the implementation of the nursing interventions based on King’s model increased the level of adaptive response in the client [27]. Another study observed significant adherence to the defined goals among diabetic patients after intervention [16]. These two studies concluded that King’s theory can be well integrated into the family health strategy (FHS) program to achieve the expected goals. Bezerra et al. investigated nurses’ perceptions of King’s theory and observed that the conceptual model of interactive open systems developed based on King’s theory provided adequate explanations about primary health care in hypertensive patients [28]. It seems that routine methods, which are not mainly patient-centered, are used in the care of patients in the current health system. This affects the quality of care, especially in chronic diseases where the patient’s compliance with the treatment is poor, and the patient leaves the treatment after a while, and the symptoms re-occur. Therefore, using patient-centered and interactive methods can be a solution to this problem.
In our study, two months after the application of King’s theory in a nursing program, the mean DMSES score in the intervention group was significantly higher than the scores of pre-test and post-test (two weeks after the intervention). This is along to the findings of a study in Iran where the behavior changes of diabetic patients were assessed before and four months after the intervention, and a significant increase in the mean self-efficacy score was reported [29]. However, application of a new intervention may not lead to positive outcomes. In a feasibility study, regular follow-up was done for 6 months by making frequent calls and insisting on regular visits for examination [30].
In King’s nursing theory, the direct interaction between the nurse and the patient is emphasized, which indicates patients’ participation in care plans. In this way, diabetic patients can receive information from the nurse and choose options according to their conditions. Therefore, the care program is designed and implemented based on the selected priorities of the patient, which can lead to more acceptance of and compliance with the care program in diabetic patients [31-33]. Nursing theories, although they provide very useful theoretical and practical frameworks in care, their effects on solving health system problems, quality of care, patient satisfaction, and reduction of health costs are still unknown, and the use of care models based on the interaction between the nurse and the patient has been neglected.
One of the limitations of this study was the low cooperation of the patients in the study because of the long intervention period. In this regard, the researchers tried to motivate them throughout the study by explaining the possible benefits of the study for the patients or by considering incentives for them. Based on the results, it can be concluded that a systematic care program based on King’s theory can help diabetic patients identify their problems in the three human systems and find ways to achieve mutual nurse-patient goals. In addition, it can improve the self-efficacy of diabetic patients two weeks and two months after the intervention. Therefore, future studies are recommended to investigate the effect of this nursing care program on other patients to identify and solve their problems and challenges and pave the way for the application of nursing theories in routine clinical practice.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the School of Pharmacy and Nursing, and the School of Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran (Code: IR.SBMU.PHARMACY.REC.1401.103).
Funding
This study was funded by Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Authors' contributions
Conceptualization, investigation, and methodology: Seyedeh Narjes Mousavizadeh, Delshad Shahmohammadi, and Mahnaz Ilkhani; Formal analysis: Seyedeh Narjes Mousavizadeh and Delshad Shahmohammadi; Supervision: Seyedeh Narjes Mousavizadeh; Visualization, review and editing: Seyedeh Narjes Mousavizadeh, Delshad Shahmohammadi, and Mahtab Sattari; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the participants for their cooperation in this research, and the Deputy for Research of Shahid Beheshti University of Medical Sciences, Tehran, Iran for the financial support of this study.
References
- Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, et al. Pathophysiology of type 2 diabetes mellitus. Int J Mol Sci. 2020; 21(17):6275. [DOI:10.3390/ijms21176275] [PMID]
- Lau LH, Lew J, Borschmann K, Thijs V, Ekinci EI. Prevalence of diabetes and its effects on stroke outcomes: A meta-analysis and literature review. J Diabetes Investig. 2019 ; 10(3):780-92. [DOI:10.1111/jdi.12932] [PMID]
- World Health Organization. Diabetes. Genewa: WHO; 2022. [Link]
- Hazar N, Jokar M, Namavari N, Hosseini S, Rahmanian V. An updated systematic review and Meta-analysis of the prevalence of type 2 diabetes in Iran, 1996–2023. Frontiers in Public Health. 2024; 12:1322072. [DOI: 10.3389/fpubh.2024.1322072] [PMID]
- Sasson C, Eckel R, Alger H, Bozkurt B, Carson A, Daviglus M, et al. American heart association diabetes and cardiometabolic health summit: Summary and recommendations. J Am Heart Assoc. 2018; 7(15):e009271. [DOI:10.1161/JAHA.118.009271] [PMID]
- Braunwald E. Diabetes, heart failure, and renal dysfunction: The vicious circles. Prog Cardiovasc Dis. 2019; 62(4):298-302. [DOI:10.1016/j.pcad.2019.07.003] [PMID]
- Pivari F, Mingione A, Brasacchio C, Soldati L. Curcumin and type 2 diabetes mellitus: Prevention and treatment. Nutrients. 2019; 11(8):1837. [DOI:10.3390/nu11081837] [PMID]
- Dehvan F, Baghi V, Lotfi A, Ghanei Gheshlagh R. [Medication adherence inhibitors and facilitators in type 2 diabetic patients: An integrative review (Persian)]. Sci J Nurs Midwifery Paramed Fac. 2017; 3(1):1-17. [DOI:10.29252/sjnmp.3.1.1]
- Eller LS, Lev EL, Yuan C, Watkins AV. Describing self-care self-efficacy: Definition, measurement, outcomes, and implications. Int J Nurs Knowl. 2018; 29(1):38-48. [DOI:10.1111/2047-3095.12143] [PMID]
- Tharek Z, Ramli AS, Whitford DL, Ismail Z, Mohd Zulkifli M, Ahmad Sharoni SK, et al. Relationship between self-efficacy, self-care behaviour and glycaemic control among patients with type 2 diabetes mellitus in the Malaysian primary care setting. BMC Fam Pract. 2018; 19(1):39. [DOI:10.1186/s12875-018-0725-6] [PMID]
- Alligood MR. Introduction to nursing theory: Its history and significance. In: Alligood MR. Nursing theorists and their work. Munich: Elsevier Health Sciences; 2021. [Link]
- Fawcett J, DeSanto-Madeya S. Contemporary nursing knowledge: Analysis and evaluation of nursing models and theories. Pennsylvania: Fa Davis; 2012. [Link]
- Shahraki vahed A, Asadi Bidmeshki E, shahraki H. [Determine self-care assessmet with educational needs diabetic patients (Persian)]. J Diabetes Nurs. 2014; 2(2):29-41. [Link]
- Moradi M, Nasiri M, Jahanshahi M, Hajiahmadi M. The effects of a self-management program based on the 5 A’s model on self-efficacy among older men with hypertension. Nurs Midwifery stud. 2019; 8(1):21-7. [Link]
- Smith MC. Nursing theories and nursing practice. Philadelphia: FA Davis; 2019. [Link]
- Araújo ESS, Silva LFD, Moreira TMM, Almeida PC, Freitas MC, Guedes MVC. Nursing care to patients with diabetes based on King’s Theory. Rev Bras Enferm. 2018; 71(3):1092-8.[DOI:10.1590/0034-7167-2016-0268] [PMID]
- Rouhi Balasi L, Elahi N, Beiranvand S, Tavakoli P, Rouhi Balasi R. The effectiveness of nursing interventions based on King’s Theory: A systematic review. Adv Nurs Midwifery. 2021; 29(3): 41-7. [Link]
- Ladee C, Lagampan S, Pichayapinyo P, Mayurasakorn K, Lagampan C. Effect of a goal attainment nursing program on self-management and blood pressure control in high-risk hypertensive patients in a primary care unit. Siriraj Med J. 2020; 72(2):140-50. [Link]
- Mousavizadeh SN. The experiences of nursing students using virtual education during the Covid-19 pandemic. J Med Life. 2022; 15(9):1090-5. [DOI:10.25122/jml-2021-0315] [PMID]
- Bhandari S, Jacob J. A study to assess the effectiveness of a structured teaching programme on knowledge and attitude regarding nursing profession among Pre University Course Students of Selected Colleges Bengaluru. Int J Health Sci Res (IJHSR). 2016; 6(12):127-36. [Link]
- Hojjatoleslami S, Cheraghi F, Borzou S R, Payamani F, Khatiban M. [Nursing process of a client with acute coronary syndrome based on King’s Goal Attainment Model: A case study (Persian)]. J Nurs Educ. 2021; 10(1):55-67. [Link]
- Park BM. Development and effect of a fall prevention program based on King’s theory of goal attainment in long-term care hospitals: An experimental study. Healthcare (Basel). 2021; 9(6):715. [DOI:10.3390/healthcare9060715] [PMID]
- Mohamadinejad F, Pedram Razi S, Aliasgharpour M, Tabari F, Kazemnejad A. [Effect of patient education program on self-efficacy in patients with diabetes (Persian)]. Iran J Nurs Res. 2015; 10(1):35-41. [Link]
- Feghhi H, Saadatjoo S, Dastjerdi R, Kalantari S, Alidousti M. [The effect of a training program based on Roy’s adaptation model on psychosocial adaptation in patients with type II diabetes in Birjand, Iran (Persian)]. J Diabetes Nurs. 2016; 4(2):8-24. [Link]
- Marson SM, Wei G, Wasserman D. A reliability analysis of goal attainment scaling (GAS) weights. Am J Eval. 2009; 30(2):203-16. [DOI:10.1177/1098214009334676]
- Balasi LR, Elahi N, Beiranvand S, Tavakoli P, Balasi RR. The Effectiveness of Nursing interventions based on King’s theory: A Systematic review. Advances in Nursing & Midwifery. 2020; 29(3):41-7. [Link]
- Vincent M. King’s theory in the care of client with self-image problem. Nurs Sci Q. 2015; 15(4): 311-7. [Link]
- Bezerra STF, Guedes MVC, Silva LFD. Perception of nursing in Primary Health Care about patients with hypertension: Does King explain? Rev Bras Enferm. 2020; 73(suppl 6):e20190676.[DOI:10.1590/0034-7167-2019-0676] [PMID]
- De Santa. Application of king's theory on nursing care outcome among diabetic clients: Report of pilot study. Pharma Innovation. 2018; 1(1):267-9. [Link]
- Aghamolaei T, Eftekhar H, Mohammad K. [Application of health belief model to behavior change of diabetic patients (Persian)]. Payesh. 2005; 4 (4). [Link]
- Shujaeizade D, Tal A, Sharifi Rad Gh, Alhani F. The effect of an educational program based on the empowerment model on improving self-care behaviors of patients with type 2 diabetes in Isfahan city. Razi Journal of Medical Sciences.2013; 107(20):31-18. [Link]
- Mardani Hamooleh M, Ebrahimi E, Mostaghasi M, Taghavi Larijani T. [Relationship between organizational justice and job stress among hospital personnel (Persian)]. Iran J Med Ethics Hist Med. 2013; 6 (3):64-71. [Link]
- Tol A, Mohebbi B, Sadeghi R, Yaseri M, Akbari Abdolabadi M, Dadrast F, et al. [Assessing the related factors to self-efficacy predictors among patients with type 2 diabetes (Persian)]. Iran J Diabetes Metab. 2017; 16(1):39-48. [Link]
Article Type : Research |
Subject:
General
Received: 2023/12/26 | Accepted: 2024/06/24 | Published: 2025/01/12
Received: 2023/12/26 | Accepted: 2024/06/24 | Published: 2025/01/12
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |