Tue, Dec 2, 2025
Volume 34, Issue 1 (1-2024)
JHNM 2024, 34(1): 35-47 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tuğba Yangöz Ş, Korkmaz M. The Pain Characteristics and Caregiver Burden in Patients With Cancer-related Pain and their Associated Factors: A Cross-sectional Study. JHNM 2024; 34 (1) :35-47
URL: http://hnmj.gums.ac.ir/article-1-2269-en.html
URL: http://hnmj.gums.ac.ir/article-1-2269-en.html
1- Assistant Professor, Department of Internal Medicine Nursing, Faculty of Health Sciences, Pamukkale University, Denizli, Turkey. , tugbayangoz@gmail.com
2- Professor, Department of Internal Medicine Nursing, Faculty of Nursing, İnönü University, Malatya, Turkey.
2- Professor, Department of Internal Medicine Nursing, Faculty of Nursing, İnönü University, Malatya, Turkey.
Full-Text [PDF 513 kb]
(462 Downloads)
| Abstract (HTML) (1064 Views)
Full-Text: (383 Views)
Introduction
Pain is one of the most common symptoms of cancer and affects all patient aspects, including physical and mental health, daily life activities, quality of life, family and social relationships, and economic and employment [1-3]. Cancer-related pain encompasses different etiologies, characteristics, and pathological mechanisms. A tumor can pressure on bones, nerves, or other organs in the body, or pain is due to cancer treatment, or a combination of both [1, 2]. One meta-analysis reported that the prevalence of pain was 39.3% in patients after curative treatment, 55% in patients undergoing anticancer therapy, and 66.4% in patients with advanced, metastatic, or terminal disease [4]. Other studies have reported that 20%-50% of cancer patients experience some degree of pain, and 80% of patients with advanced cancer suffer from moderate or severe pain [2, 5, 6].
Pain assessment is a significant step in its management [1]. Pain assessment involves pain intensity, beliefs, and interference [2]. In addition, pain expression is influenced by the pain experiences and beliefs, gender, age, race, and emotional status [7]. Pain beliefs include two dimensions: Organic and psychological [8]. Organic pain beliefs indicate the physiological experience of pain associated with physical harm or threat. Psychological pain beliefs are related to internal feelings and influences [8, 9]. Both of these factors may negatively affect beliefs about pain management. Therefore, assessment of pain beliefs is crucial in pain management. Moreover, a multidisciplinary team approach is needed in the pain beliefs assessment [10].
Cancer-related pain affects patients as well as their caregivers. The caregiver burden of cancer patients has been reported to be 37% to 68% [11-13]. Cancer care is a complex process that includes physical care, symptom management, and emotional support [14]. In this complex process, caregivers adjust their daily lives according to the patient’s conditions, which may cause caregivers physical, psychological, social, and economic problems [15, 16]. All these problems increase the caregiver’s burden. Therefore, a multidisciplinary approach, including caregivers and patients, is crucial in cancer management [17]. Pain management is an interdisciplinary team approach, and the nurses play an important role in this team. Nurses spend more time with patients than other health professionals. Therefore, nurses should have sufficient knowledge and skills in pain mechanisms, assessment, care planning, and management [3, 18]. Nurses should support caregivers psychologically, socially, and spiritually [19].
Several studies have focused on the relationship between depression, anxiety, and cancer pain in patients with cancer [20-22]. However, a few studies have been conducted on the associated factors of pain characteristics of patients with cancer. Many studies assessed associations between demographic variables and pain severity or pain beliefs in patients with cancer without including patients experiencing pain in their studies [23, 24]. Additionally, many studies have evaluated the relationships between demographic variables and caregiver burden in caregivers of patients with cancer [11, 15, 25]. Therefore, we aimed to investigate the factors associated with pain characteristics such as intensity, interference, and beliefs in patients experiencing pain for at least one month due to cancer or cancer treatment and the factors associated with caregiver burden.
Materials and Methods
This cross-sectional study was conducted on 120 patients with cancer and 120 their caregivers in the oncology unit of a publicly-funded hospital in a province in Turkey. The inclusion criteria for patients with cancer were as follows: Having pain for at least one month due to cancer or cancer treatment, being ≥18 years old, being willing to participate, lacking language or communication barriers, having no mental problems or visual or hearing impairment. The inclusion criteria for caregivers were as follows: Being ≥18 years old, willing to participate, lacking language or communication barriers, having mental problems, or visual or hearing impairment. The exclusion criterion for patients with cancer and caregivers was a diagnosis of psychiatric illness in them. In addition, we did not exclude patients with cancer using painkillers.
This study used a convenience sampling method. The sample size was calculated according to Yamane’s sample size method. In the calculation, the population size consisted of 360 patients with cancer who were refered to the hospital where the study was conducted within one year. The precision/error margin level was 0.05 at a confidence level of 95%. According to these variables, the sample size was calculated as 189 patients with cancer-caregiver dyads. However, we reached 120 patients with cancer-their caregiver dyads between November 2011 and June 2012. The reasons included the unwillingness of some patients to participate in the study, no pain for at least one month due to cancer or cancer treatment in some patients, and the allocated timeframe.
The data collection tools included a demographic and clinical/caregiving characteristics form for patients with cancer-related pain and their caregivers, the brief pain inventory (BPI), the pain beliefs questionnaire (PBQ), and the Zarit burden interview scale (ZBI). The patient’s demographic and clinical characteristics form included 11 items: Age, gender, type, duration, stage of cancer, type of cancer treatment, presence of metastasis, the region of metastasis, the area of pain, accompanying symptoms to pain, and kind of pain treatment. The demographic and caregiving characteristics form for caregivers included 11 items: Age, gender, education, employment status, income level, kinship with the patients with cancer, other care recipients, caregiving time, getting support for care, the impact of caregiver on other responsibilities, and responsibilities affecting the caregiver.
The BPI was used to assess pain severity and interference for patients with cancer. It was developed by Cleland and Ryan [26]. It is an 11-item instrument to assess pain intensity and interference. Pain intensity evaluated participants’ least, worst, and mean pain in the last 24 hours and their pain at the time of the survey on a scale of 0 (no pain) to 10 (worst imaginable pain). Pain interference was evaluated in seven areas: General activity, mood, walking ability, normal work, relations with other people, sleep, and enjoyment of life on a scale of 0 (no interference) to 10 (complete interference). The Turkish version of this scale was used in this study [27]. The Cronbach α ranged from 0.90 to 0.98 in our study.
The BPQ was developed by Edwards et al. and used to assess pain beliefs in patients with cancer [28]. It consists of 12 items scored on a Likert scale from 0 (never) to 6 (always) and two sub-dimensions: Organic and psychological beliefs. The high score for each sub-dimension indicates that causal beliefs of pain are psychological or organic. The Turkish version of BPQ was used in this study [29]. The Cronbach α value of each sub-dimension was found to be 0.80 in our study.
The ZBI was used to assess the care burden of caregivers. It was developed by Zarit et al. [30] and consists of 22 items scored on a Likert scale from 0 (never) to 5 (nearly always). The total score ranges from 0 to 88; a higher score indicates a greater burden. Scores are categorized as 0-20 as no care burden, 21-40 as mild, 41-60 as moderate, and 61-88 as severe [30]. The Turkish version of the scale, which İnci and Erdem localized, was used in this study [31]. The Cronbach α was found to be 0.77 in our study.
Data were collected by face-to-face interviews by the researcher and completed in approximately 30 minutes. The obtained data were analyzed with IBM SPSS for Windows version 25 [32]. The descriptive statistics, frequency distributions, and multiple linear regression model were used to analyze the data using the two-tailed P<0.05. The independent t-test, one-way analysis of variance (ANOVA) and Pearson correlation analysis according to testing groups were used to analyze the relationship between demographic and clinical/caregiving characteristics and BPI, PBQ and ZBI scores. The demographic and clinical/caregiver variables that were found to be significant according to these tests were entered into the multiple linear regression model.
Results
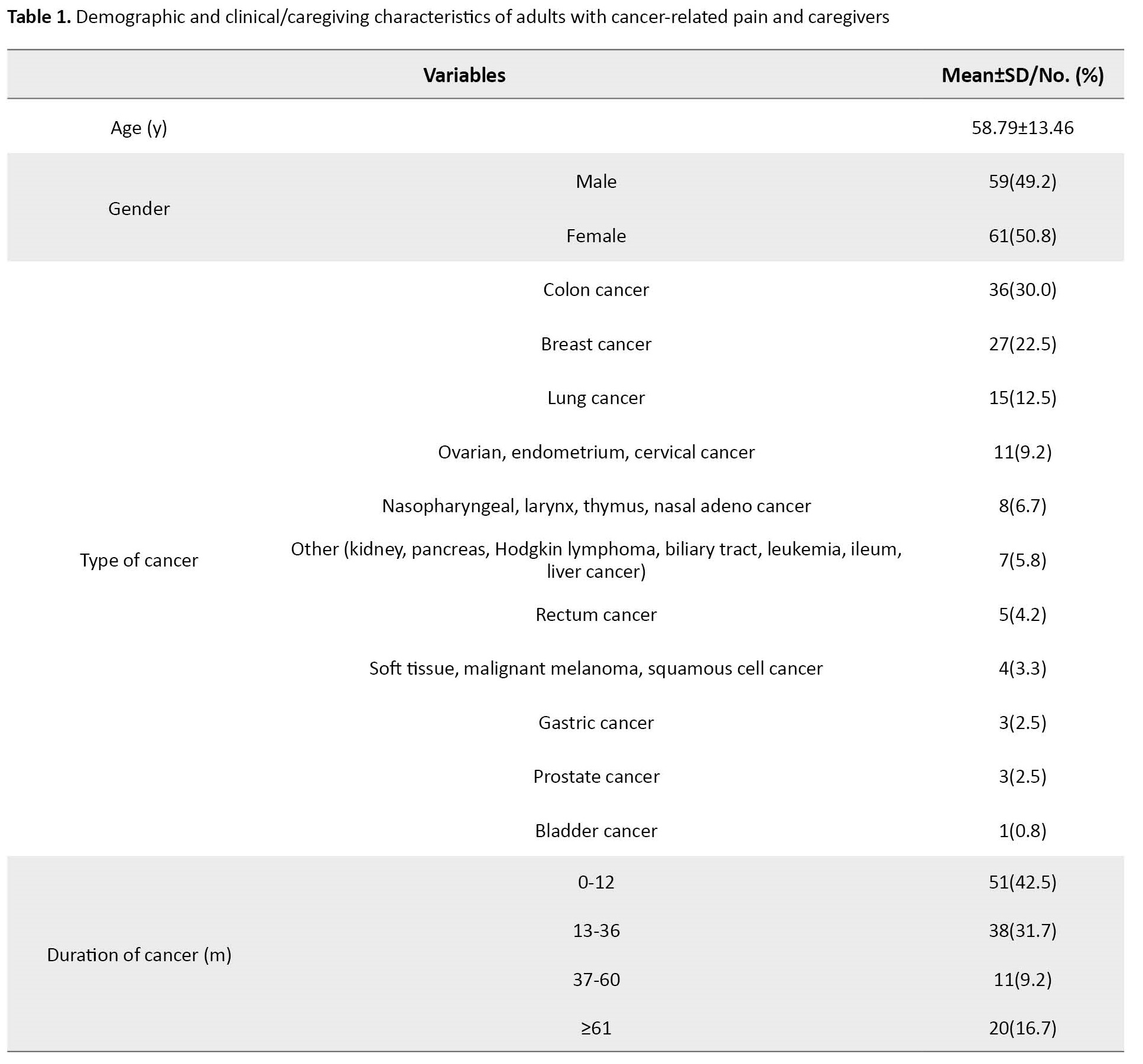
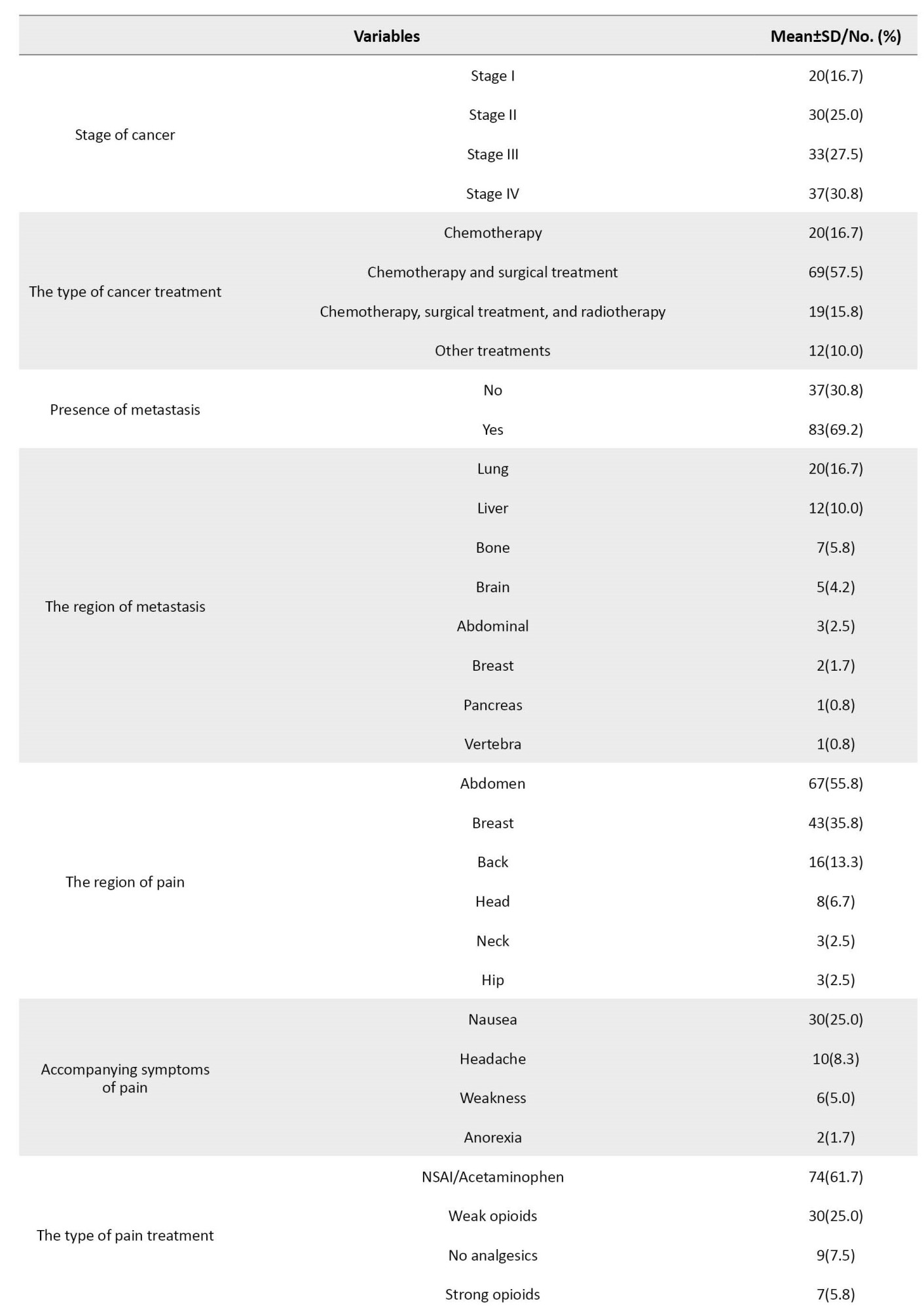
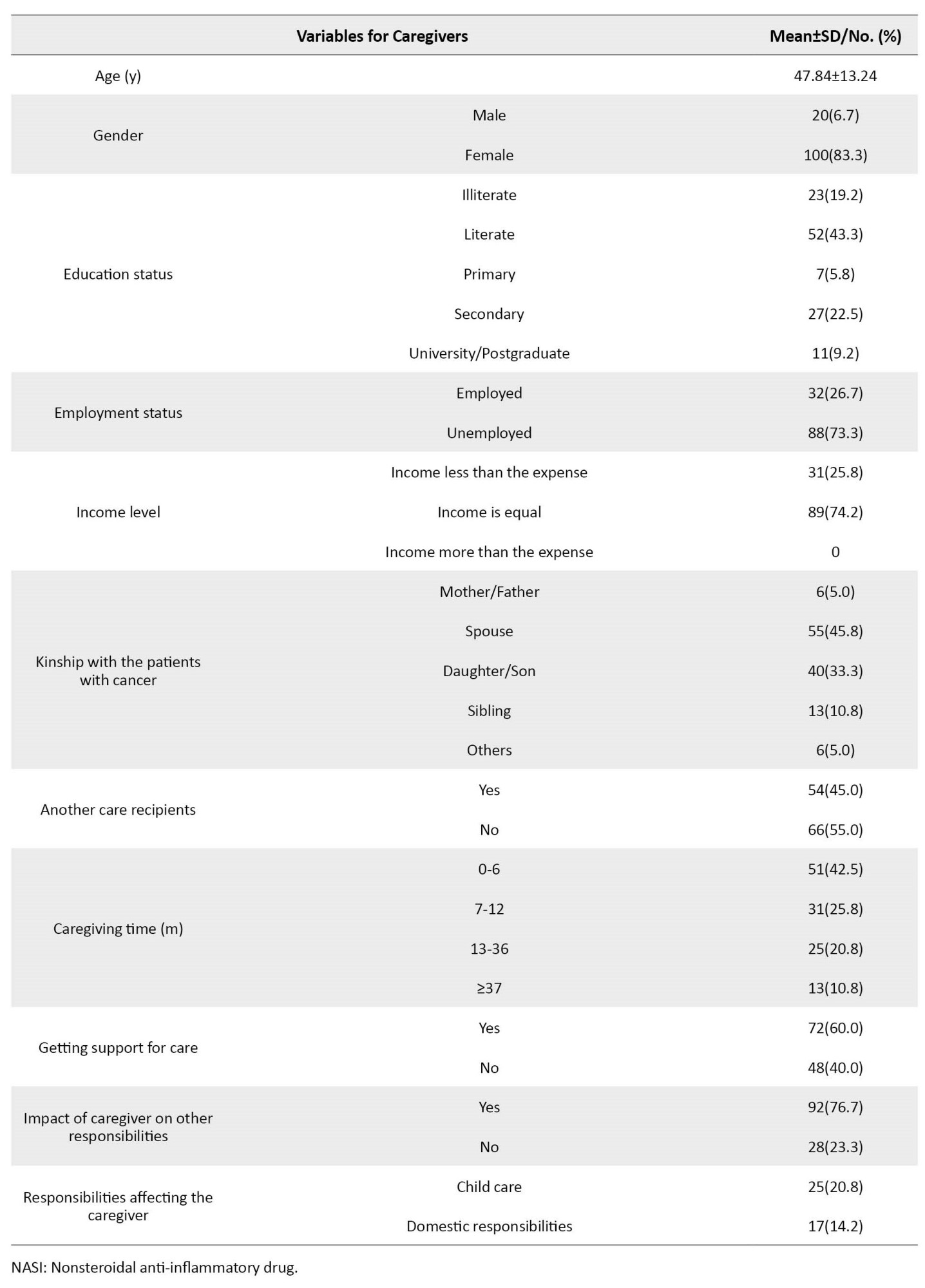
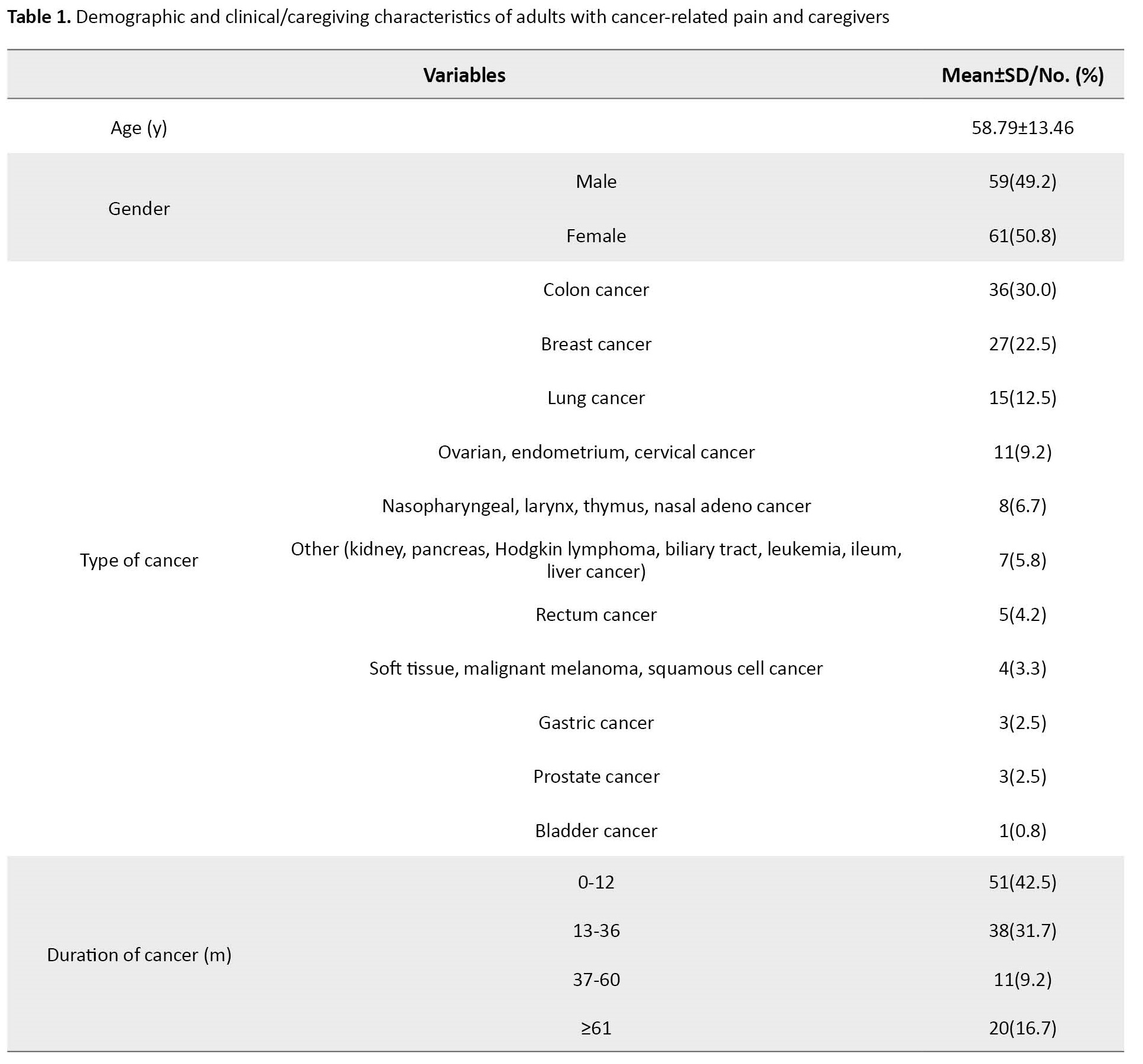
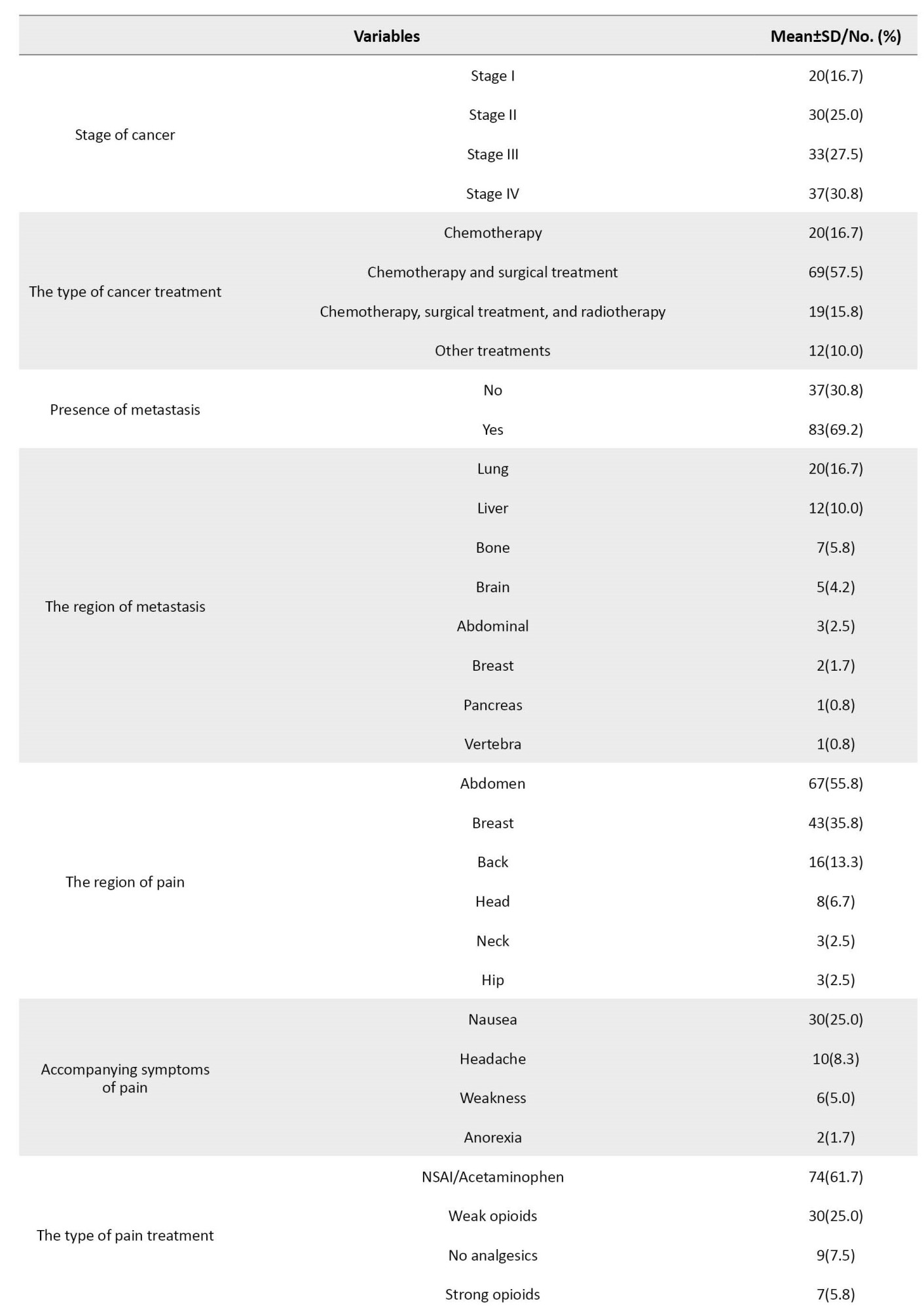
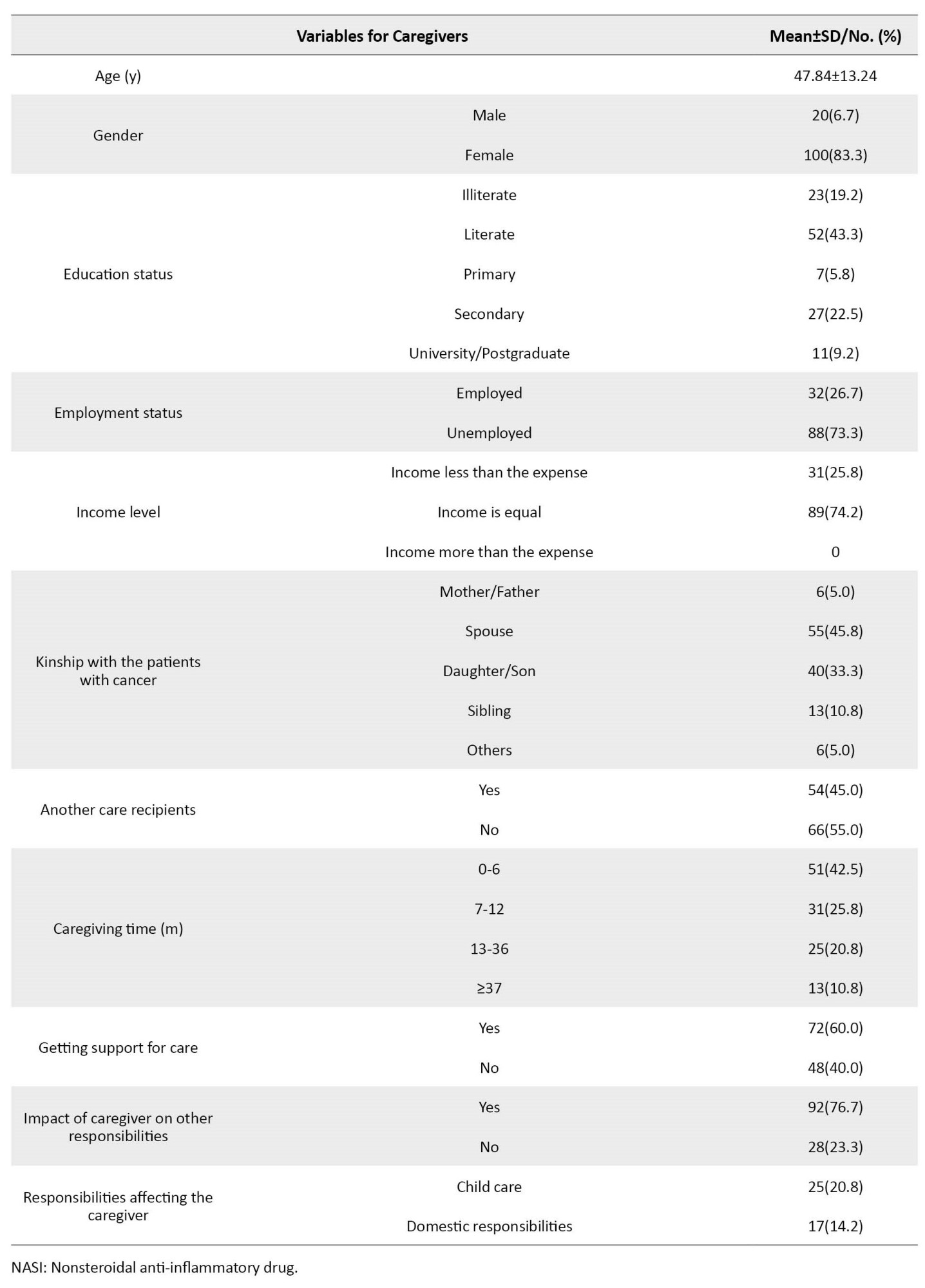
The mean age of the participants was 58.79±13.46 years. Of 120 patients, 61 were female (50.8%), and the most common cancer was colorectal cancer (30%). Abdominal pain was most common in cancer patients (55.8%). The mean age of the caregivers was 47.84±13.24 years. Of 120 caregivers, 100 were female (83.3%), 52 were literate (43.3%), 88 were unemployed (73.3%), and 55 had a spouse relationship with the patient (45.8%). Additionally, 51 caregivers had been caring for 0-6 months (42.5%), and 92 caregivers (76.7%) had their caring interfered with their other responsibilities. These results were shown in Table 1.
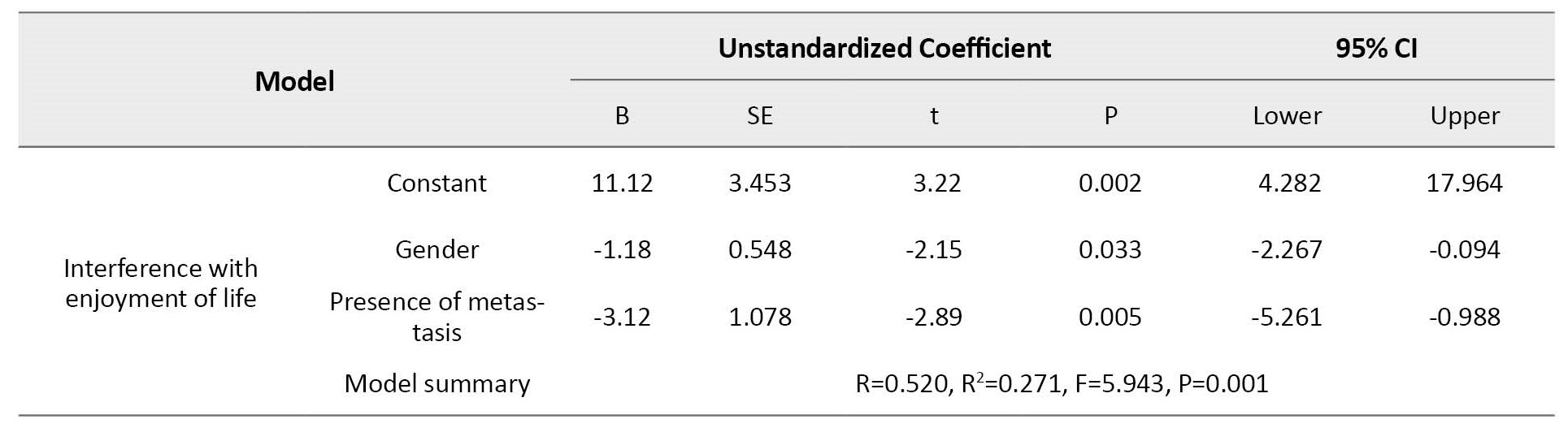
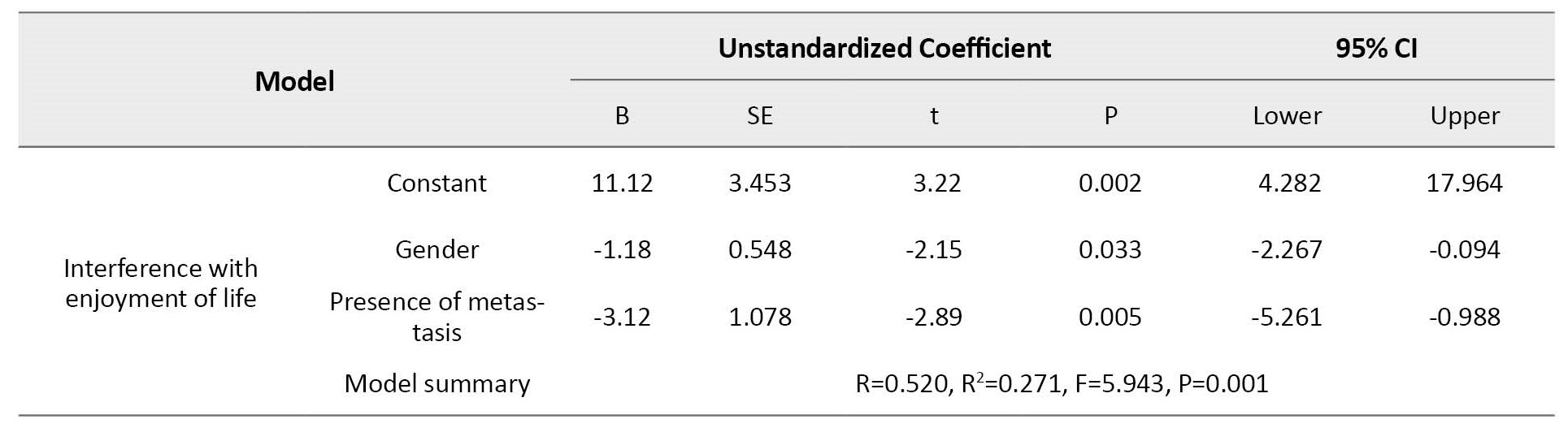
Additionally, the gender (B=-1.16; 95% CI; -2.16, -0.16; P=0.002), presence of metastasis (B=-2.31; 95% CI; -4.26, -0.35; P=0.021) were negatively and duration of cancer (B=0.01; 95% CI; 0.01, 0.03; P=0.042) and the type of pain treatment (B=1.00; 95% CI: 0.32, 1.69; P=0.004) was positively associated with mood. Furthermore, gender (B=-1.32; 95% CI; -2.32, -0.32; P=0.010, B=-1.18; 95% CI; -2.26,-0.09; P=0.033, respectively) and presence of metastasis (B=-1.97; 95% CI; -3.94, -0.006; P=0.049, B=-3.12; 95% CI; -5.26, -0.98; P=0.005, respectively) were negatively related to walking ability and enjoyment of life. The gender (B=-1.34; 95% CI; -2.34,-0.33; P=0.009) were negatively associated with normal walk. The gender was negatively (B=-1.21; 95% CI; -2.20, -0.22; P=0.017), and the type of pain treatment was positively (B=1.20; 95% CI; 0.51, 1.88; P=0.001) associated with relations with other people. The presence of metastasis (B=-3.26; 95% CI; -5.31, -1.21; P=0.002) was negatively associated with sleep (Table 2).
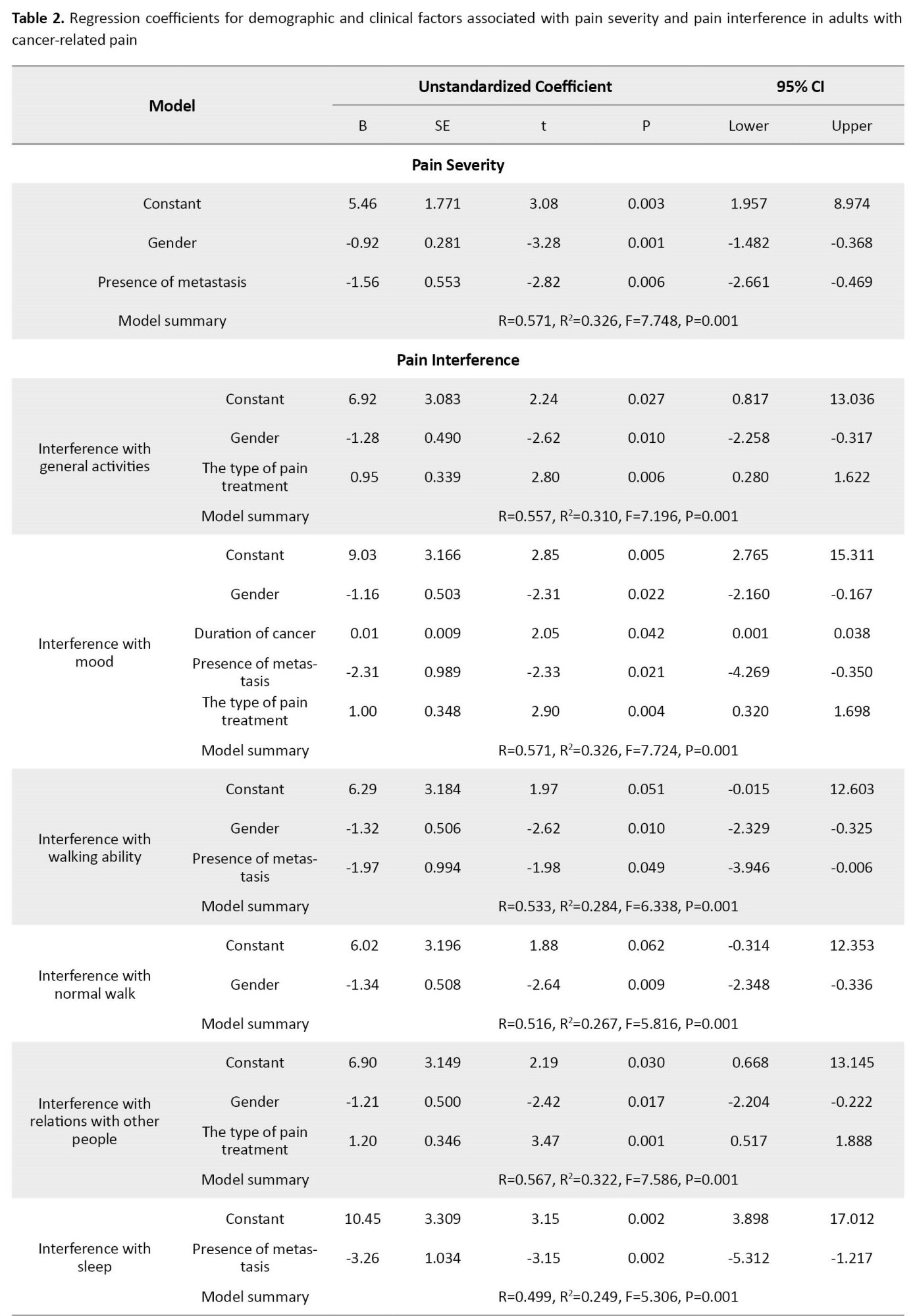
The mean general pain severity was 1.78±1.72. In addition, the mean worst pain score in the last 24 hours was 2.96±2.65; the mean least pain score in the last 24 hours was 0.88±1.40; the mean pain score in the last 24 hours was 1.90±1.79, and the mean current pain score was 1.52±1.74. The gender (B=-0.92, 95% CI; -1.48%, -0.36%, P=0.001) and presence of metastasis (B=-1.56, 95% CI; -2.66%, -0.46%, P=0.006) were negatively associated with pain intensity.
Among pain interference factors, sleep (3.86±3.06) and mood (3.43±3.09) scored higher than others. In addition, 78.8% of patients recovered from their pain with pain treatments or medications. Among the pain interference items, the gender was negatively (B=-1.28, 95% CI; -2.25%, -0.31%, P=0.010), and the type of pain treatment was positively (B=0.95; 95% CI; 0.28%, 1.62%; P=0.006) associated with general activities (Table 2).
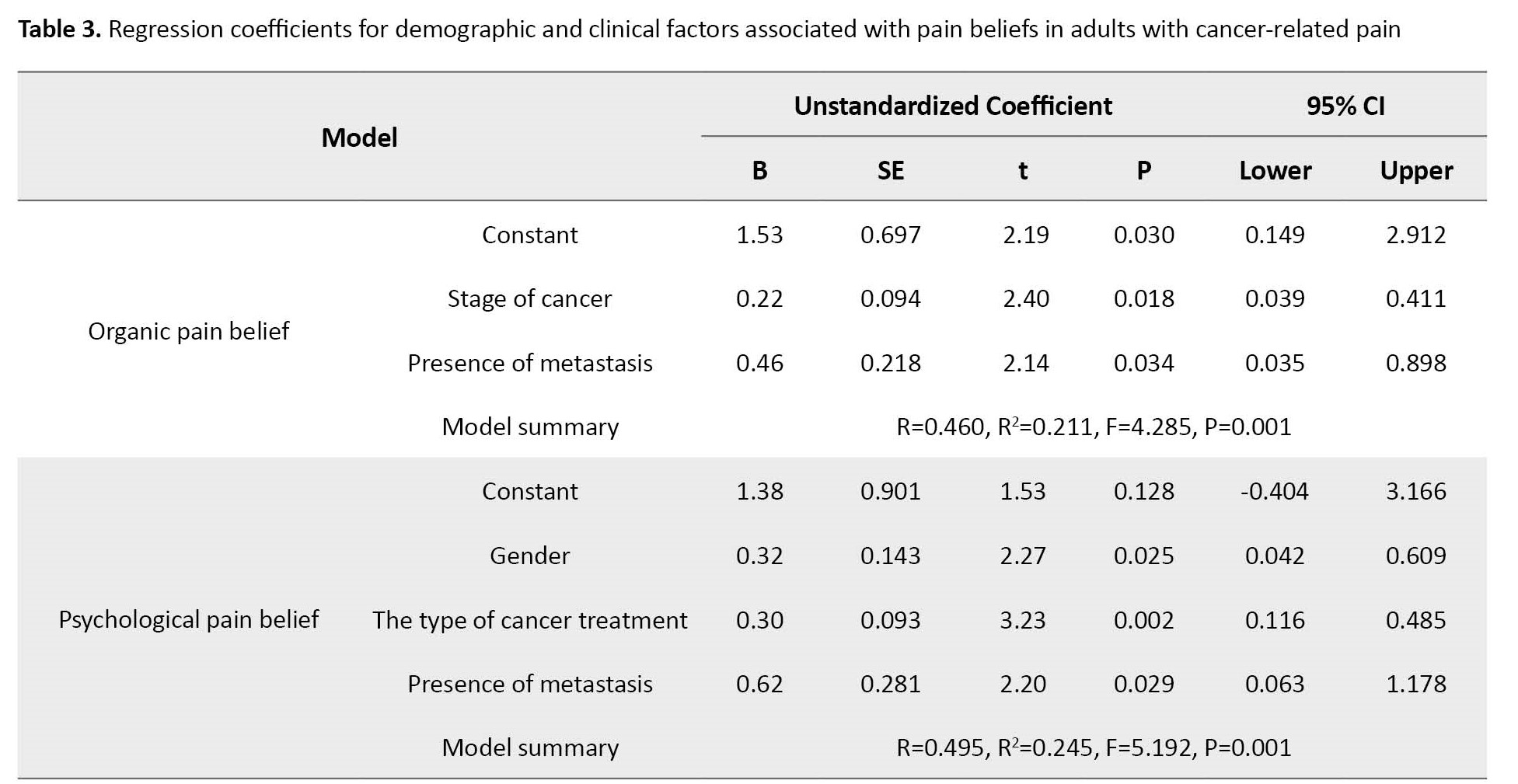
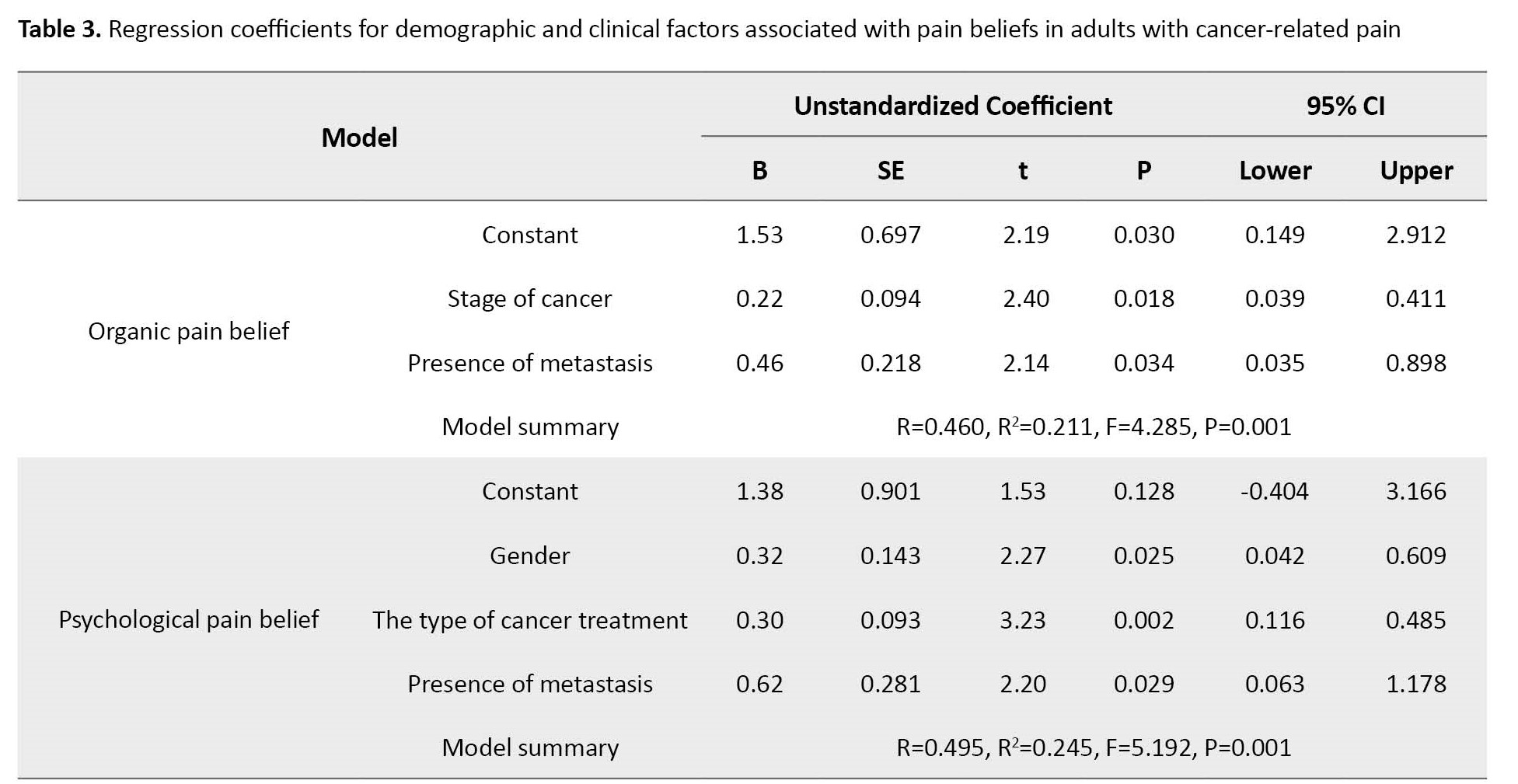
The mean scores of organic and psychological beliefs were 2.86±0.62 and 3.71±0.83, respectively. Stage of cancer (B=0.22, 95% CI; 0.03%, 0.41%, P=0.018) and presence of metastasis (B=0.46, 95% CI; 0.03%, 0.89% P=0.034) were positively associated with organic pain beliefs. Furthermore, gender (B=0.32, 95% CI; 0.04%, 0.60%, P=0.025), type of cancer treatment (B=0.30, 95% CI; 0.11%, 0.48%, P=0.002), and presence of metastasis (B=0.62, 95% CI; 0.06%, 1.17%, P=0.029) were factors positively associated with psychological pain beliefs (Table 3).
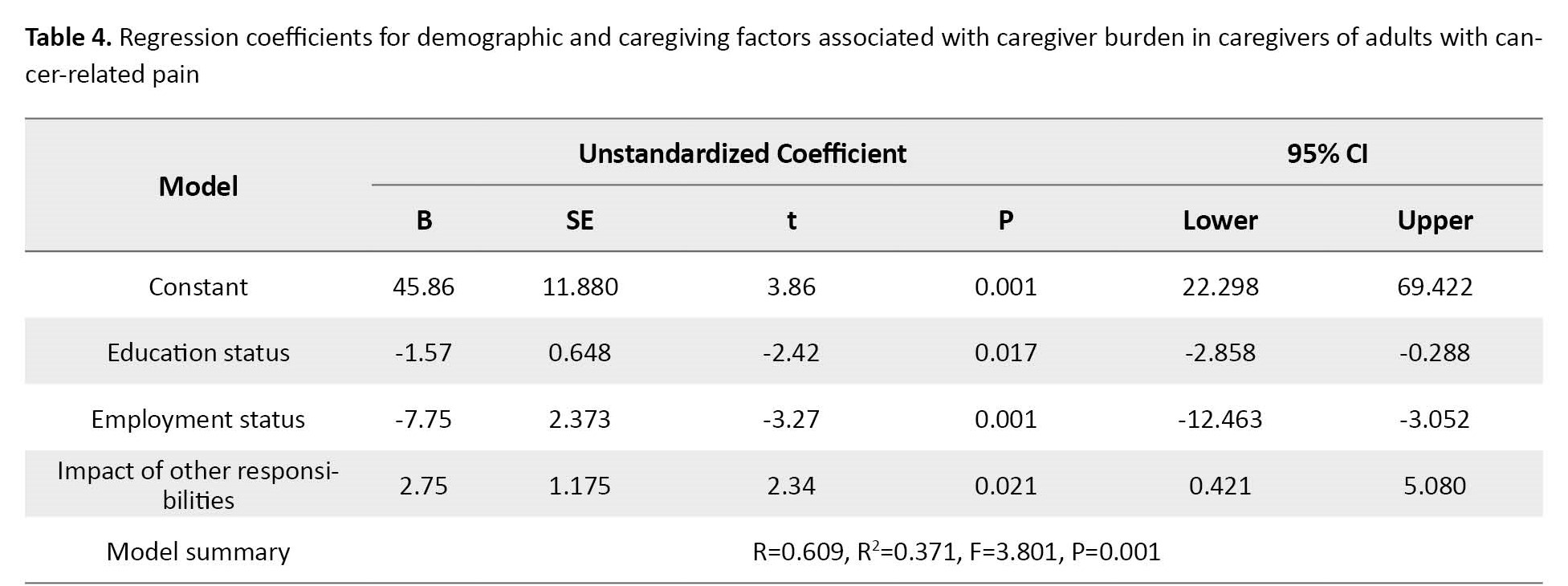
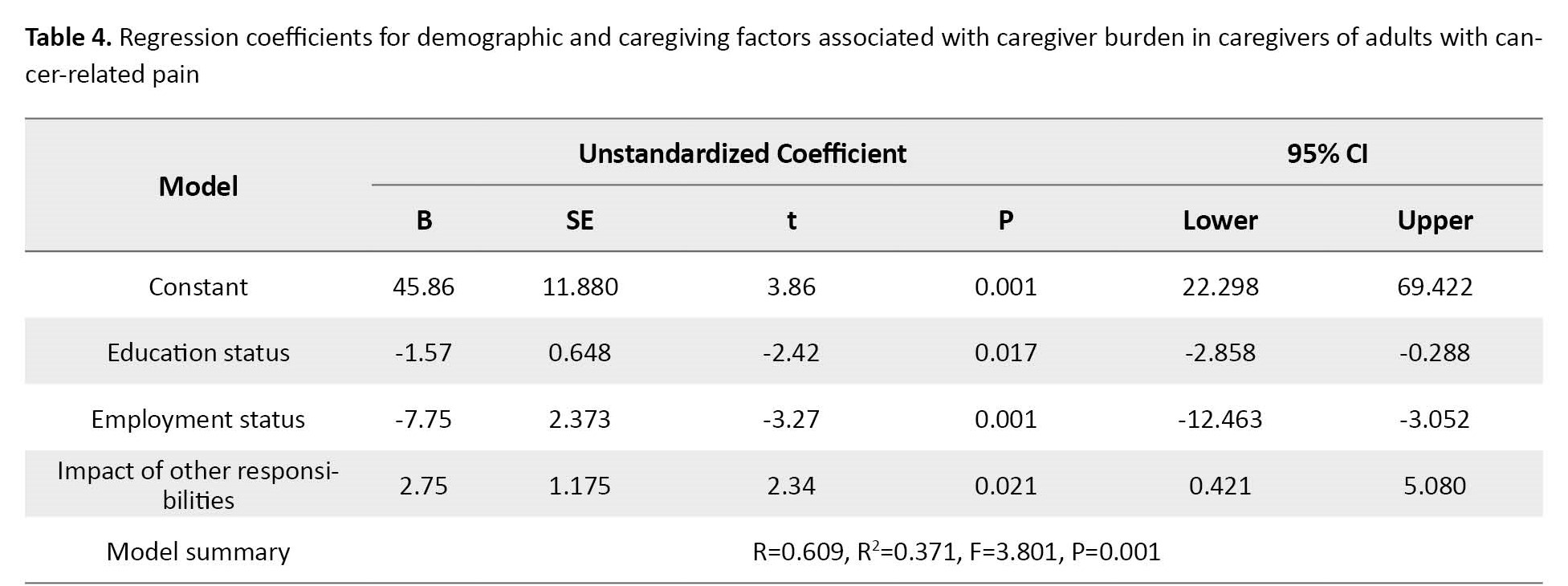
The mean caregiver burden score was 28.19±8.03, and caregivers experienced mild burden. Educational level (B=-1.57, 95% CI; -2.85%, -0.28%, P=0.017) and employment status (B=-7.75, 95% CI; -12.46%, -3.05%, P=0.001), the effect of caregiving on other responsibilities (B=2.75, 95% CI; 0.42%, 5.08%, P=0.021) were associated with caregiver burden (Table 4).
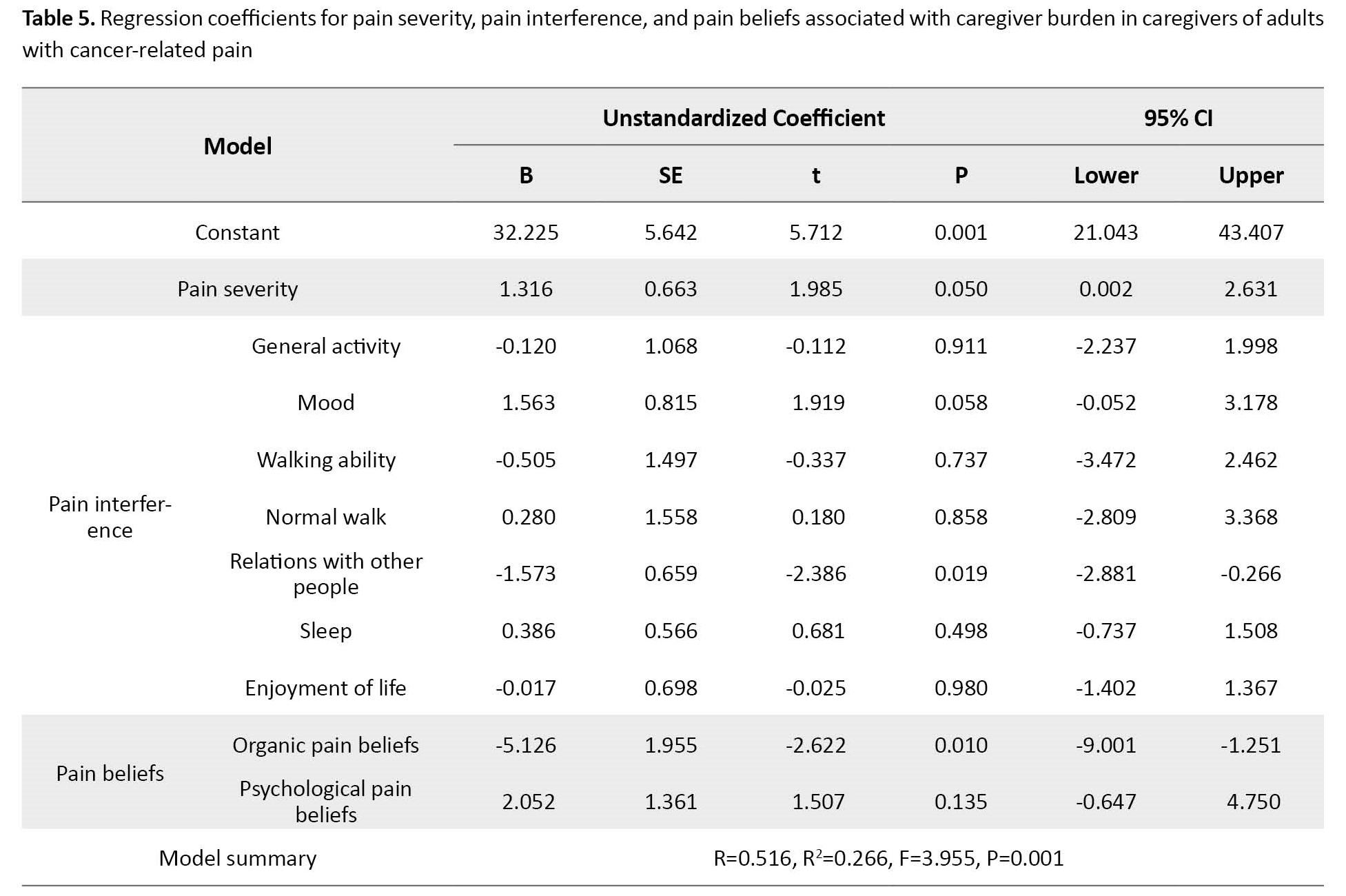
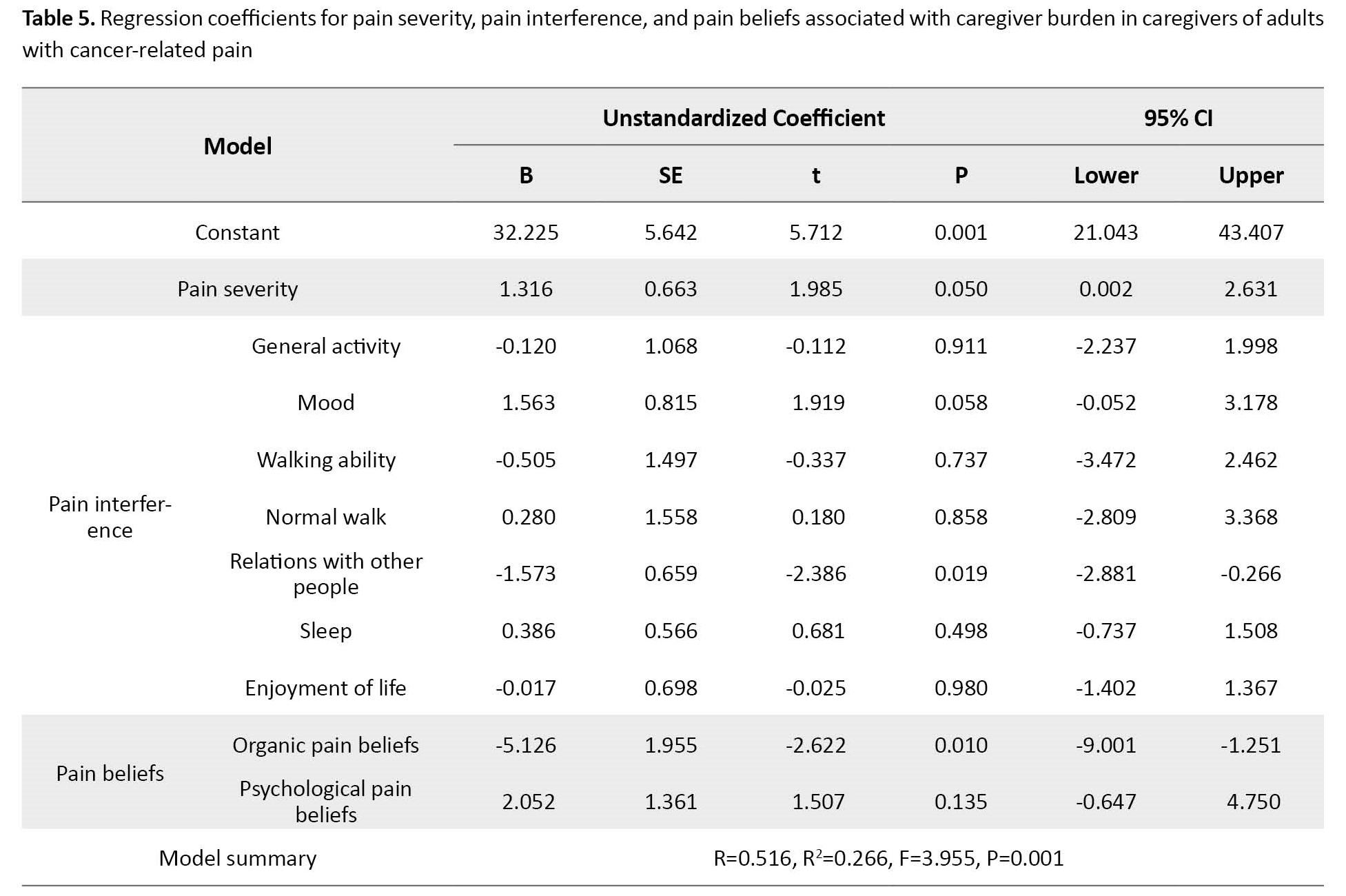
In addition, pain interference sub-dimensions such as relationships with other people (B=-1.57; 95% CI; -2.88, -0.26; P=0.019) were negatively associated with caregiver burden, while pain beliefs sub-dimension such as organic pain beliefs (B=-5.12; 95% CI; -9.00, -1.25; P=0.010) were positively associated (Table 5).
Discussion
This study was conducted to provide evidence on pain characteristics, caregiver burden, and related factors. The results showed a significant relationship between gender and the presence of metastasis and pain intensity. In the literature, many studies have reported gender differences in pain severity that our results were similar to their results [33-35]. In addition, previous studies have shown that metastasis increases pain intensity [16, 36]. Therefore, it is recommended that healthcare professionals consider the effect of gender and the presence of metastasis when assessing pain intensity.
Our study showed that cancer-related pain negatively affected sleep and mood in patients with cancer. Ferreira et al. reported that cancer-related pain negatively affected mood, sleep, and normal walking in breast cancer survivors [37]. Chronic pain affects individuals in all aspects, including activities of daily living, physical and mental health, family, and social life [18]. Pain management guidelines suggest regular and systematic pain assessment is necessary for effective pain management [38]. Therefore, assessing all aspects of pain is very important.
This study revealed that patients’ beliefs about pain were of psychological origin. This finding is similar to previous studies [39, 40]. Additionally, this study showed that the stage of cancer and the presence of metastasis are associated with organic pain beliefs, and gender, stage of cancer, type of cancer treatment, and the presence of metastasis were associated with psychological pain beliefs. Our study showed that the stage of cancer and the presence of metastasis were determinants of both organic and psychological pain beliefs. However, a lack of evidence on the relationship between these variables and pain beliefs suggests the need for further studies.
This study showed that gender was a predictor of psychological pain beliefs, and the mean score of psychological pain beliefs was higher in females. This finding was reported in similar studies [29, 39]. It is stated that psychological factors are more strongly associated with chronic pain in women, possibly because women experience more psychological distress than men, and women respond differently to emotional stimuli than men [41]. This study also reported that the type of cancer treatment was a predictor of psychological pain beliefs. However, no evidence exists of the relationship between these variables and pain beliefs. In the literature, it is reported that patients who undergo cancer treatment experience more pain than patients who do not undergo treatment [42]. Healthcare professionals must assess patients’ pain beliefs and plan pain management strategies according to their pain beliefs.
This study presented that the caregivers of patients with cancer-related pain experienced a mild caregiver burden. In a study conducted by Palacio et al. similar to our results, it was reported that caregiver burden was mild in patients with advanced cancer and cancer-related pain [43]. Apart from this study, there is a lack of evidence in the literature regarding caregiver burden in patients with cancer-related pain. However, it is reported in the literature that caregivers of the general cancer population experience mild to severe burden [15, 44, 45]. Our study showed that educational level, employment status, and the impact of caregiving on other responsibilities were predictors of caregiver burden. Previous studies in the general cancer population have shown that caregiver burden is associated with educational level, similar to our results [14, 45, 46]. Additionally, our study revealed that caregivers who were employed and caregiving interferes with other responsibilities had a high caregiver burden. Previous studies in the general cancer population have shown that caregiver burden is associated with employment status, similar to our results [25, 47]. A study by Danacı and Koç showed that the impact of caregiving on other responsibilities was associated with caregiver burden in the general cancer population [48]. Therefore, further studies are needed to investigate the relationship between these variables and caregiver burden. In addition, health professionals should assess all aspects of caregiver burden and support caregivers.
Our study revealed that relations with other people as a sub-dimension of pain interference were negative, and organic pain beliefs were positive predictors of caregiver burden in patients with cancer-related pain. This finding means that caregivers of patients who were more affected by pain interference with their relationships with other people experienced less caregiver burden. In addition, caregivers of patients who believe that pain is an organic source experience more caregiver burden. However, there is a lack of evidence on the relationship between pain interference in relations with other people, organic pain beliefs, and caregiver burden. Therefore, further studies are needed to investigate the relationship between pain interference, pain beliefs, and caregiver burden. In addition, health professionals should provide more support and help to caregivers of patients who experience more cancer-related pain [19].
Our study has several limitations. First, this single-center study included participants who met the inclusion and exclusion criteria for 8 months. Therefore, the sample size may not be sufficient to evaluate the effect of some variables. Second, pain is a subjective symptom influenced by psychosocial factors. In our study, we determined whether pain was of psychological or organic origin, but we did not evaluate the emotional state of the patients. It is recommended that the emotional dimension of pain be assessed in future studies. Third, we did not exclude patients receiving painkillers or analgesics, which may affect the reliability of our results.
Ethical Considerations
Compliance with ethical guidelines
This study was conducted in accordance with the Helsinki Declaration and received ethical approval from the Research Ethics Committee of the relevant institution (18140/11). Patients with cancer and their caregivers received written and verbal information about the study purpose, procedure, and participants’ role before data collection. Patients with cancer and caregivers were informed that they had the autonomy to participate in or withdraw from the study at any time without any explanation or reason.
Funding
This study was carried out with the support of project number “2903-YL-11” of the Scientific Research Projects Coordination Unit of Süleyman Demirel University.
Authors' contributions
Conceptualization, study design, data analysis, manuscript editing, revision, and final approval: Şefika Tuğba Yangöz and Medet Korkmaz; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all participants and healthcare professionals who made this study possible at the Oncology Unit of Süleyman Demirel University Hospital.
References
Pain is one of the most common symptoms of cancer and affects all patient aspects, including physical and mental health, daily life activities, quality of life, family and social relationships, and economic and employment [1-3]. Cancer-related pain encompasses different etiologies, characteristics, and pathological mechanisms. A tumor can pressure on bones, nerves, or other organs in the body, or pain is due to cancer treatment, or a combination of both [1, 2]. One meta-analysis reported that the prevalence of pain was 39.3% in patients after curative treatment, 55% in patients undergoing anticancer therapy, and 66.4% in patients with advanced, metastatic, or terminal disease [4]. Other studies have reported that 20%-50% of cancer patients experience some degree of pain, and 80% of patients with advanced cancer suffer from moderate or severe pain [2, 5, 6].
Pain assessment is a significant step in its management [1]. Pain assessment involves pain intensity, beliefs, and interference [2]. In addition, pain expression is influenced by the pain experiences and beliefs, gender, age, race, and emotional status [7]. Pain beliefs include two dimensions: Organic and psychological [8]. Organic pain beliefs indicate the physiological experience of pain associated with physical harm or threat. Psychological pain beliefs are related to internal feelings and influences [8, 9]. Both of these factors may negatively affect beliefs about pain management. Therefore, assessment of pain beliefs is crucial in pain management. Moreover, a multidisciplinary team approach is needed in the pain beliefs assessment [10].
Cancer-related pain affects patients as well as their caregivers. The caregiver burden of cancer patients has been reported to be 37% to 68% [11-13]. Cancer care is a complex process that includes physical care, symptom management, and emotional support [14]. In this complex process, caregivers adjust their daily lives according to the patient’s conditions, which may cause caregivers physical, psychological, social, and economic problems [15, 16]. All these problems increase the caregiver’s burden. Therefore, a multidisciplinary approach, including caregivers and patients, is crucial in cancer management [17]. Pain management is an interdisciplinary team approach, and the nurses play an important role in this team. Nurses spend more time with patients than other health professionals. Therefore, nurses should have sufficient knowledge and skills in pain mechanisms, assessment, care planning, and management [3, 18]. Nurses should support caregivers psychologically, socially, and spiritually [19].
Several studies have focused on the relationship between depression, anxiety, and cancer pain in patients with cancer [20-22]. However, a few studies have been conducted on the associated factors of pain characteristics of patients with cancer. Many studies assessed associations between demographic variables and pain severity or pain beliefs in patients with cancer without including patients experiencing pain in their studies [23, 24]. Additionally, many studies have evaluated the relationships between demographic variables and caregiver burden in caregivers of patients with cancer [11, 15, 25]. Therefore, we aimed to investigate the factors associated with pain characteristics such as intensity, interference, and beliefs in patients experiencing pain for at least one month due to cancer or cancer treatment and the factors associated with caregiver burden.
Materials and Methods
This cross-sectional study was conducted on 120 patients with cancer and 120 their caregivers in the oncology unit of a publicly-funded hospital in a province in Turkey. The inclusion criteria for patients with cancer were as follows: Having pain for at least one month due to cancer or cancer treatment, being ≥18 years old, being willing to participate, lacking language or communication barriers, having no mental problems or visual or hearing impairment. The inclusion criteria for caregivers were as follows: Being ≥18 years old, willing to participate, lacking language or communication barriers, having mental problems, or visual or hearing impairment. The exclusion criterion for patients with cancer and caregivers was a diagnosis of psychiatric illness in them. In addition, we did not exclude patients with cancer using painkillers.
This study used a convenience sampling method. The sample size was calculated according to Yamane’s sample size method. In the calculation, the population size consisted of 360 patients with cancer who were refered to the hospital where the study was conducted within one year. The precision/error margin level was 0.05 at a confidence level of 95%. According to these variables, the sample size was calculated as 189 patients with cancer-caregiver dyads. However, we reached 120 patients with cancer-their caregiver dyads between November 2011 and June 2012. The reasons included the unwillingness of some patients to participate in the study, no pain for at least one month due to cancer or cancer treatment in some patients, and the allocated timeframe.
The data collection tools included a demographic and clinical/caregiving characteristics form for patients with cancer-related pain and their caregivers, the brief pain inventory (BPI), the pain beliefs questionnaire (PBQ), and the Zarit burden interview scale (ZBI). The patient’s demographic and clinical characteristics form included 11 items: Age, gender, type, duration, stage of cancer, type of cancer treatment, presence of metastasis, the region of metastasis, the area of pain, accompanying symptoms to pain, and kind of pain treatment. The demographic and caregiving characteristics form for caregivers included 11 items: Age, gender, education, employment status, income level, kinship with the patients with cancer, other care recipients, caregiving time, getting support for care, the impact of caregiver on other responsibilities, and responsibilities affecting the caregiver.
The BPI was used to assess pain severity and interference for patients with cancer. It was developed by Cleland and Ryan [26]. It is an 11-item instrument to assess pain intensity and interference. Pain intensity evaluated participants’ least, worst, and mean pain in the last 24 hours and their pain at the time of the survey on a scale of 0 (no pain) to 10 (worst imaginable pain). Pain interference was evaluated in seven areas: General activity, mood, walking ability, normal work, relations with other people, sleep, and enjoyment of life on a scale of 0 (no interference) to 10 (complete interference). The Turkish version of this scale was used in this study [27]. The Cronbach α ranged from 0.90 to 0.98 in our study.
The BPQ was developed by Edwards et al. and used to assess pain beliefs in patients with cancer [28]. It consists of 12 items scored on a Likert scale from 0 (never) to 6 (always) and two sub-dimensions: Organic and psychological beliefs. The high score for each sub-dimension indicates that causal beliefs of pain are psychological or organic. The Turkish version of BPQ was used in this study [29]. The Cronbach α value of each sub-dimension was found to be 0.80 in our study.
The ZBI was used to assess the care burden of caregivers. It was developed by Zarit et al. [30] and consists of 22 items scored on a Likert scale from 0 (never) to 5 (nearly always). The total score ranges from 0 to 88; a higher score indicates a greater burden. Scores are categorized as 0-20 as no care burden, 21-40 as mild, 41-60 as moderate, and 61-88 as severe [30]. The Turkish version of the scale, which İnci and Erdem localized, was used in this study [31]. The Cronbach α was found to be 0.77 in our study.
Data were collected by face-to-face interviews by the researcher and completed in approximately 30 minutes. The obtained data were analyzed with IBM SPSS for Windows version 25 [32]. The descriptive statistics, frequency distributions, and multiple linear regression model were used to analyze the data using the two-tailed P<0.05. The independent t-test, one-way analysis of variance (ANOVA) and Pearson correlation analysis according to testing groups were used to analyze the relationship between demographic and clinical/caregiving characteristics and BPI, PBQ and ZBI scores. The demographic and clinical/caregiver variables that were found to be significant according to these tests were entered into the multiple linear regression model.
Results
The mean age of the participants was 58.79±13.46 years. Of 120 patients, 61 were female (50.8%), and the most common cancer was colorectal cancer (30%). Abdominal pain was most common in cancer patients (55.8%). The mean age of the caregivers was 47.84±13.24 years. Of 120 caregivers, 100 were female (83.3%), 52 were literate (43.3%), 88 were unemployed (73.3%), and 55 had a spouse relationship with the patient (45.8%). Additionally, 51 caregivers had been caring for 0-6 months (42.5%), and 92 caregivers (76.7%) had their caring interfered with their other responsibilities. These results were shown in Table 1.
Additionally, the gender (B=-1.16; 95% CI; -2.16, -0.16; P=0.002), presence of metastasis (B=-2.31; 95% CI; -4.26, -0.35; P=0.021) were negatively and duration of cancer (B=0.01; 95% CI; 0.01, 0.03; P=0.042) and the type of pain treatment (B=1.00; 95% CI: 0.32, 1.69; P=0.004) was positively associated with mood. Furthermore, gender (B=-1.32; 95% CI; -2.32, -0.32; P=0.010, B=-1.18; 95% CI; -2.26,-0.09; P=0.033, respectively) and presence of metastasis (B=-1.97; 95% CI; -3.94, -0.006; P=0.049, B=-3.12; 95% CI; -5.26, -0.98; P=0.005, respectively) were negatively related to walking ability and enjoyment of life. The gender (B=-1.34; 95% CI; -2.34,-0.33; P=0.009) were negatively associated with normal walk. The gender was negatively (B=-1.21; 95% CI; -2.20, -0.22; P=0.017), and the type of pain treatment was positively (B=1.20; 95% CI; 0.51, 1.88; P=0.001) associated with relations with other people. The presence of metastasis (B=-3.26; 95% CI; -5.31, -1.21; P=0.002) was negatively associated with sleep (Table 2).
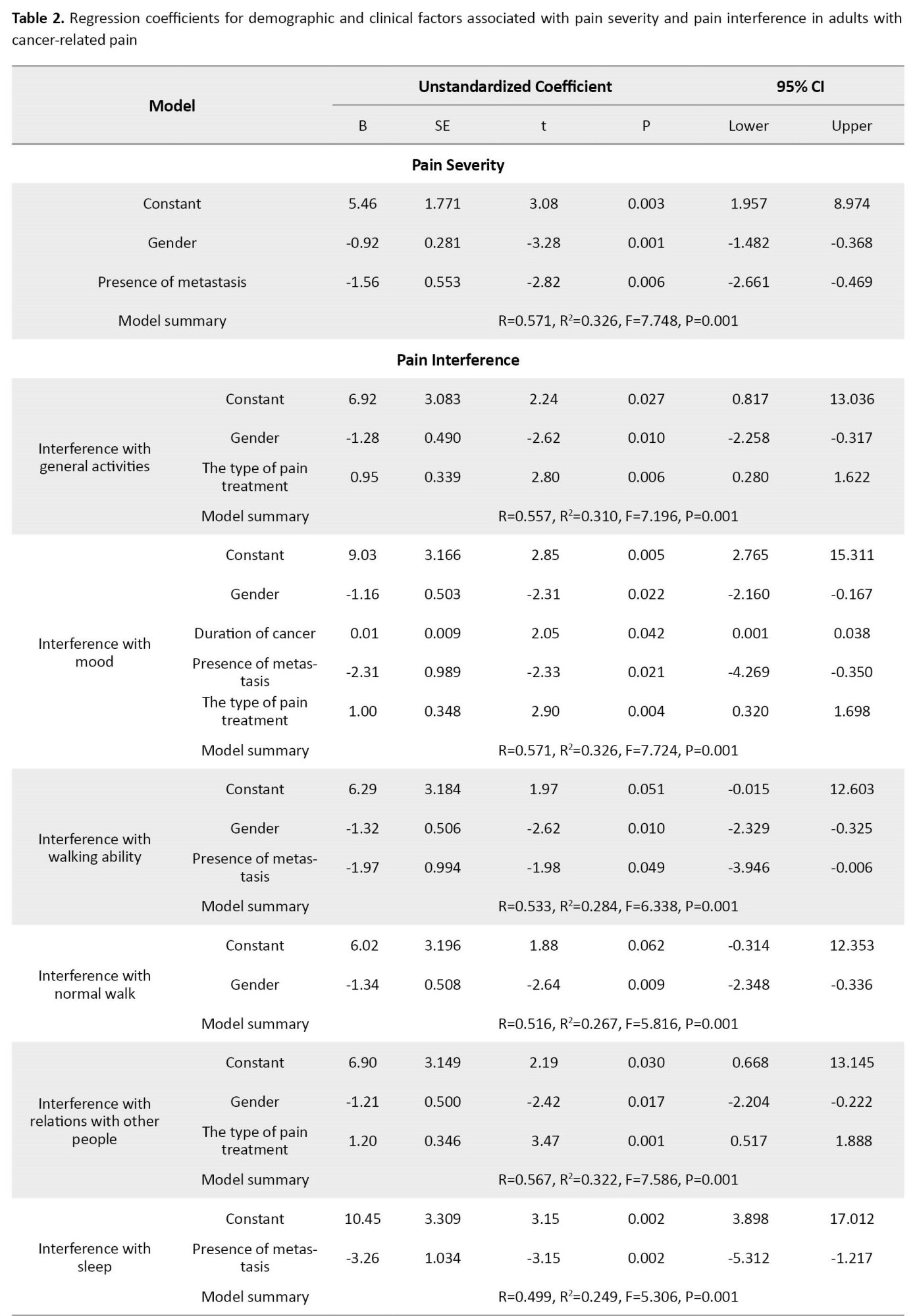
The mean general pain severity was 1.78±1.72. In addition, the mean worst pain score in the last 24 hours was 2.96±2.65; the mean least pain score in the last 24 hours was 0.88±1.40; the mean pain score in the last 24 hours was 1.90±1.79, and the mean current pain score was 1.52±1.74. The gender (B=-0.92, 95% CI; -1.48%, -0.36%, P=0.001) and presence of metastasis (B=-1.56, 95% CI; -2.66%, -0.46%, P=0.006) were negatively associated with pain intensity.
Among pain interference factors, sleep (3.86±3.06) and mood (3.43±3.09) scored higher than others. In addition, 78.8% of patients recovered from their pain with pain treatments or medications. Among the pain interference items, the gender was negatively (B=-1.28, 95% CI; -2.25%, -0.31%, P=0.010), and the type of pain treatment was positively (B=0.95; 95% CI; 0.28%, 1.62%; P=0.006) associated with general activities (Table 2).
The mean scores of organic and psychological beliefs were 2.86±0.62 and 3.71±0.83, respectively. Stage of cancer (B=0.22, 95% CI; 0.03%, 0.41%, P=0.018) and presence of metastasis (B=0.46, 95% CI; 0.03%, 0.89% P=0.034) were positively associated with organic pain beliefs. Furthermore, gender (B=0.32, 95% CI; 0.04%, 0.60%, P=0.025), type of cancer treatment (B=0.30, 95% CI; 0.11%, 0.48%, P=0.002), and presence of metastasis (B=0.62, 95% CI; 0.06%, 1.17%, P=0.029) were factors positively associated with psychological pain beliefs (Table 3).
The mean caregiver burden score was 28.19±8.03, and caregivers experienced mild burden. Educational level (B=-1.57, 95% CI; -2.85%, -0.28%, P=0.017) and employment status (B=-7.75, 95% CI; -12.46%, -3.05%, P=0.001), the effect of caregiving on other responsibilities (B=2.75, 95% CI; 0.42%, 5.08%, P=0.021) were associated with caregiver burden (Table 4).
In addition, pain interference sub-dimensions such as relationships with other people (B=-1.57; 95% CI; -2.88, -0.26; P=0.019) were negatively associated with caregiver burden, while pain beliefs sub-dimension such as organic pain beliefs (B=-5.12; 95% CI; -9.00, -1.25; P=0.010) were positively associated (Table 5).
Discussion
This study was conducted to provide evidence on pain characteristics, caregiver burden, and related factors. The results showed a significant relationship between gender and the presence of metastasis and pain intensity. In the literature, many studies have reported gender differences in pain severity that our results were similar to their results [33-35]. In addition, previous studies have shown that metastasis increases pain intensity [16, 36]. Therefore, it is recommended that healthcare professionals consider the effect of gender and the presence of metastasis when assessing pain intensity.
Our study showed that cancer-related pain negatively affected sleep and mood in patients with cancer. Ferreira et al. reported that cancer-related pain negatively affected mood, sleep, and normal walking in breast cancer survivors [37]. Chronic pain affects individuals in all aspects, including activities of daily living, physical and mental health, family, and social life [18]. Pain management guidelines suggest regular and systematic pain assessment is necessary for effective pain management [38]. Therefore, assessing all aspects of pain is very important.
This study revealed that patients’ beliefs about pain were of psychological origin. This finding is similar to previous studies [39, 40]. Additionally, this study showed that the stage of cancer and the presence of metastasis are associated with organic pain beliefs, and gender, stage of cancer, type of cancer treatment, and the presence of metastasis were associated with psychological pain beliefs. Our study showed that the stage of cancer and the presence of metastasis were determinants of both organic and psychological pain beliefs. However, a lack of evidence on the relationship between these variables and pain beliefs suggests the need for further studies.
This study showed that gender was a predictor of psychological pain beliefs, and the mean score of psychological pain beliefs was higher in females. This finding was reported in similar studies [29, 39]. It is stated that psychological factors are more strongly associated with chronic pain in women, possibly because women experience more psychological distress than men, and women respond differently to emotional stimuli than men [41]. This study also reported that the type of cancer treatment was a predictor of psychological pain beliefs. However, no evidence exists of the relationship between these variables and pain beliefs. In the literature, it is reported that patients who undergo cancer treatment experience more pain than patients who do not undergo treatment [42]. Healthcare professionals must assess patients’ pain beliefs and plan pain management strategies according to their pain beliefs.
This study presented that the caregivers of patients with cancer-related pain experienced a mild caregiver burden. In a study conducted by Palacio et al. similar to our results, it was reported that caregiver burden was mild in patients with advanced cancer and cancer-related pain [43]. Apart from this study, there is a lack of evidence in the literature regarding caregiver burden in patients with cancer-related pain. However, it is reported in the literature that caregivers of the general cancer population experience mild to severe burden [15, 44, 45]. Our study showed that educational level, employment status, and the impact of caregiving on other responsibilities were predictors of caregiver burden. Previous studies in the general cancer population have shown that caregiver burden is associated with educational level, similar to our results [14, 45, 46]. Additionally, our study revealed that caregivers who were employed and caregiving interferes with other responsibilities had a high caregiver burden. Previous studies in the general cancer population have shown that caregiver burden is associated with employment status, similar to our results [25, 47]. A study by Danacı and Koç showed that the impact of caregiving on other responsibilities was associated with caregiver burden in the general cancer population [48]. Therefore, further studies are needed to investigate the relationship between these variables and caregiver burden. In addition, health professionals should assess all aspects of caregiver burden and support caregivers.
Our study revealed that relations with other people as a sub-dimension of pain interference were negative, and organic pain beliefs were positive predictors of caregiver burden in patients with cancer-related pain. This finding means that caregivers of patients who were more affected by pain interference with their relationships with other people experienced less caregiver burden. In addition, caregivers of patients who believe that pain is an organic source experience more caregiver burden. However, there is a lack of evidence on the relationship between pain interference in relations with other people, organic pain beliefs, and caregiver burden. Therefore, further studies are needed to investigate the relationship between pain interference, pain beliefs, and caregiver burden. In addition, health professionals should provide more support and help to caregivers of patients who experience more cancer-related pain [19].
Our study has several limitations. First, this single-center study included participants who met the inclusion and exclusion criteria for 8 months. Therefore, the sample size may not be sufficient to evaluate the effect of some variables. Second, pain is a subjective symptom influenced by psychosocial factors. In our study, we determined whether pain was of psychological or organic origin, but we did not evaluate the emotional state of the patients. It is recommended that the emotional dimension of pain be assessed in future studies. Third, we did not exclude patients receiving painkillers or analgesics, which may affect the reliability of our results.
Ethical Considerations
Compliance with ethical guidelines
This study was conducted in accordance with the Helsinki Declaration and received ethical approval from the Research Ethics Committee of the relevant institution (18140/11). Patients with cancer and their caregivers received written and verbal information about the study purpose, procedure, and participants’ role before data collection. Patients with cancer and caregivers were informed that they had the autonomy to participate in or withdraw from the study at any time without any explanation or reason.
Funding
This study was carried out with the support of project number “2903-YL-11” of the Scientific Research Projects Coordination Unit of Süleyman Demirel University.
Authors' contributions
Conceptualization, study design, data analysis, manuscript editing, revision, and final approval: Şefika Tuğba Yangöz and Medet Korkmaz; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all participants and healthcare professionals who made this study possible at the Oncology Unit of Süleyman Demirel University Hospital.
References
- Caraceni A, Shkodra M. Cancer pain assessment and classification. Cancers (Basel). 2019; 11(4):510. [DOI:10.3390/cancers11040510] [PMID]
- Hamieh NM, Akel R, Anouti B, Traboulsi C, Makki I, Hamieh L, et al. Cancer-related pain: Prevalence, severity and management in a Tertiary Care Center in the Middle East. Asian Pac J Cancer Prev. 2018;19(3):769-75. [DOI:10.22034/APJCP.2018.19.3.769]
- Ahmad I, Ahmed MM, Ahsraf MF, Naeem A, Tasleem A, Ahmed M, et al. Pain management in metastatic bone disease: A literature review. Cureus. 2018; 10(9):1-11. [DOI:10.7759/cureus.3286]
- van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ. Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. J Pain Symptom Manage. 2016; 51(6):1070-1090.e9. [DOI:10.1016/j.jpainsymman.2015.12.340] [PMID]
- Iwase S, Kawaguchi T, Tokoro A, Yamada K, Kanai Y, Matsuda Y, et al. Assessment of cancer-related fatigue, pain, and quality of life in cancer patients at palliative care team referral: A multicenter observational study (JORTC PAL-09). Plos One. 2015; 10(8):e0134022.[DOI:10.1371/journal.pone.0134022] [PMID]
- Tegegn HG, Gebreyohannes EA. Cancer pain management and pain interference with daily functioning among cancer patients in Gondar University Hospital. Pain Res Manag. 2017; 2017:5698640.[DOI:10.1155/2017/5698640] [PMID]
- Liu XK, Xiao SY, Zhou L, Hu M, Liu HM. Different predictors of pain severity across age and gender of a Chinese rural population: A cross-sectional survey. BMJ Open. 2018; 8(7):e020938. [DOI:10.1136/bmjopen-2017-020938] [PMID]
- Tabriz ER, Mohammadi R, Roshandel GR, Talebi R. Pain beliefs and perceptions and their relationship with coping strategies, stress, anxiety, and depression in patients with cancer. Indian J Palliat Care. 2019; 25(1):61-5. [DOI:10.4103%2FIJPC.IJPC_137_18]
- Ister ED, Özdemir L. Pain beliefs and affecting factors of the hematopoietic stem cell transplant patients with hematological cancer. Asian Pacific J Heal Sci. 2018; 5(1):157-61. [DOI:10.21276/apjhs.2018.5.1.35]
- Erol O, Unsar S, Yacan L, Pelin M, Kurt S, Erdogan B. Pain experiences of patients with advanced cancer: A qualitative descriptive study. Eur J Oncol Nurs. 2018; 33:28-34. [DOI:10.1016/j.ejon.2018.01.005] [PMID]
- Gabriel IO, Aluko JO, Okeme MI. Caregiver burden among informal caregivers of women with breast cancer. Biomed J Sci Tech Res. 2019; 15(3):1-9. [DOI:10.26717/bjstr.2019.15.002704]
- Longacre ML, Weber-Raley L, Kent EE. Toward engaging caregivers: Inclusion in care and receipt of information and training among caregivers for cancer patients who have been hospitalized. J Cancer Educ. 2021; 36(3):611-20. [DOI:10.1007/s13187-019-01673-5] [PMID]
- Ramezani A, Azimi Lolaty H, Bastani F, Haghani H. Family caregivers burden and its related factors among Iranian elderly psychiatric patients’ caregivers. Iran J Psychiatry Behav Sci. 2018; 12(2):e9311. [DOI:10.5812/ijpbs.9311]
- Karimi Moghaddam Z, Rostami M, Zeraatchi A, Mohammadi Bytamar J, Saed O, Zenozian S. Caregiving burden, depression, and anxiety among family caregivers of patients with cancer: An investigation of patient and caregiver factors. Front Psychol. 2023; 14:1059605. [DOI:10.3389/fpsyg.2023.1059605] [PMID]
- Unnikrishnan B, Rathi P, Saxena PUP, Aggarwal A, Shekhar S, Bansal S, et al. Psychosocial burden among informal caregivers of adult cancer patients attending a Tertiary Care Cancer Center in Coastal South India. SAGE Open. 2019; 9(3):1-7. [DOI:10.1177/2158244019876287]
- Kokkonen K, Tasmuth T, Lehto JT, Kautiainen H, Elme A, Jääskeläinen AS, et al. Cancer patients’ symptom burden and health-related quality of life (HRQoL) at tertiary cancer center from 2006 to 2013: A cross-sectional study. Anticancer Res. 2019; 39(1):271-7. [DOI:10.21873/anticanres.13107] [PMID]
- Otto AK, Ketcher D, Heyman RE, Vadaparampil ST, Ellington L, Reblin M. Communication between advanced cancer patients and their family caregivers: Relationship with caregiver burden and preparedness for caregiving. Health Commun. 2021; 36(6):714-21. [DOI:10.1080/10410236.2020.1712039] [PMID]
- Cleary JF. Restoring balance to cancer pain management. Cancer. 2020; 126(4):697-700. [DOI:10.1002/cncr.32592] [PMID]
- Johannessen LEF. The commensuration of pain: How nurses transform subjective experience into objective numbers. Soc Sci Med. 2019; 233:38-46. [DOI:10.1016/j.socscimed.2019.05.042] [PMID]
- Alemayehu M, Deyessa N, Medihin G, Fekadu A. A descriptive analysis of depression and pain complaints among patients with cancer in a low income country. PloS One. 2018; 13(3):e0193713.[DOI:10.1371/journal.pone.0193713] [PMID]
- Li XM, Xiao WH, Yang P, Zhao HX. Psychological distress and cancer pain: Results from a controlled cross-sectional survey in China. Sci Rep. 2017; 7:39397. [DOI:10.1038/srep39397] [PMID]
- Wang S, Wang X, Liu X, Zhao C, Duan J. Moderating effects of humanistic care and socioeconomic status on the relationship among pain intensity, psychological factors, and psychological function in adults with cancer pain from a province of China: A cross-sectional study. Front Psychiatry. 2023; 14:928727. [DOI:10.3389/fpsyt.2023.928727] [PMID]
- Hamood R, Hamood H, Merhasin I, Keinan-Boker L. Chronic pain and other symptoms among breast cancer survivors: Prevalence, predictors, and effects on quality of life. Breast Cancer Res Treat. 2018; 167(1):157-69. [DOI:10.1007/s10549-017-4485-0] [PMID]
- Xu X, Ou M, Xie C, Cheng Q, Chen Y. Pain acceptance and its associated factors among cancer patients in mainland China: A cross-sectional study. Pain Res Manag. 2019; 2019:9458683. [DOI:10.1155/2019/9458683] [PMID]
- Hu X, Peng X, Su Y, Huang W. Caregiver burden among Chinese family caregivers of patients with lung cancer: A cross-sectional survey. Eur J Oncol Nurs. 2018; 37:74-80. [DOI:10.1016/j.ejon.2018.11.003] [PMID]
- Cleeland CS, Ryan KM. Pain assessment: Global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994; 23(2):129-38. [PMID]
- Dicle A, Karayurt O, Dirimese E. Validation of the Turkish version of the Brief Pain Inventory in surgery patients. Pain Manag Nurs. 2009; 10(2):107-113.e2. [DOI:10.1016/j.pmn.2008.08.002] [PMID]
- Edwards LC, Pearce SA, Turner-Stokes L, Jones A. The Pain Beliefs Questionnaire: An investigation of beliefs in the causes and consequences of pain. Pain. 1992; 51(3):267-72. [DOI:10.1016/0304-3959(92)90209-t] [PMID]
- Berk H. [The experience of chronic pain and pain beliefs: The Turkish validation study of the pain beliefs questionnaire (Turkish)] [PhD dissertation]. Istanbul: Istanbul University; 2006. [Link]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980; 20(6):649-55. [DOI:10.1093/geront/20.6.649] [PMID]
- İnci F, Erdem M. [Validity and reliability of the burden interview and i̇ts adaptation to Turkish (Turkish)]. J Nursology. 2008; 11(4):85-95. [Link]
- IBM. IBM SPSS statistics: Version 25. New York: IBM; 2016. [Link]
- Alodhayani A, Almutairi KM, Vinluan JM, Alsadhan N, Almigbal TH, Alonazi WB, et al. Gender difference in pain management among adult cancer patients in Saudi Arabia: A cross-sectional assessment. Front Psychol. 2021; 12:628223. [DOI:10.3389/fpsyg.2021.628223] [PMID]
- Komendarek-Kowalska M. [Quality of life of a patient with cancer. Pain and depression-severity of symptoms depending on gender (Polish)]. Palliative Med. 2018; 10(1):30-6. [DOI:10.5114/pm.2018.77204]
- Krok-Schoen JL, Baker TA. Gender differences in personality and cancer-related pain among older cancer patients. J Gend Stud. 2016; 25(5):507-21. [DOI:10.1080/09589236.2015.1041463]
- Raj SX, Thronaes M, Brunelli C, Hjermstad MJ, Klepstad P, Kaasa S. A cross-sectional study on prevalence of pain and breakthrough pain among an unselected group of outpatients in a tertiary cancer clinic. Support Care Cancer. 2014; 22(7):1965-71. [DOI:10.1007/s00520-014-2178-3] [PMID]
- Ferreira VT, Dibai-Filho AV, Kelly de Oliveira A, Gomes CA, Melo ES, Maria de Almeida A. Assessing the impact of pain on the life of breast cancer survivors using the Brief Pain Inventory. J Phys Ther Sci. 2015; 27(5):1361-3. [DOI:10.1589/jpts.27.1361] [PMID]
- Swarm RA, Paice JA, Anghelescu DL, Are M, Bruce JY, Buga S, et al. Adult cancer pain, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019; 17(8):977-1007. [DOI:10.6004/jnccn.2019.0038] [PMID]
- Babadağ B, Alparslan GB, Güleç S. The relationship between pain beliefs and coping with pain of algology patients’. Pain Manag Nurs. 2015; 16(6):910-9. [DOI:10.1016/j.pmn.2015.07.004] [PMID]
- Turk DC, Monarch ES. Biopsychosocial Perspective on Chronic Pain. In: Turk DC, Gatchel RJ, editors. Psychological approaches to pain management: A practitioner’s handbook. New York: The Guilford Press; 2018. [Link]
- Fillingim RB. Sex, gender, and pain. In: Legato MJ, editor. Principles of gender-specific medicine. Massachusetts: Elsevier Academic Press; 2023. [DOI:10.1016/B978-0-323-88534-8.00011-0]
- Makhlouf SM, Pini S, Ahmed S, Bennett MI. Managing pain in people with cancer-a systematic review of the attitudes and knowledge of professionals, patients, caregivers and public. J Cancer Educ. 2020; 35(2):214-40. [DOI:10.1007/s13187-019-01548-9] [PMID]
- Palacio C, Krikorian A, Limonero JT. The influence of psychological factors on the burden of caregivers of patients with advanced cancer: Resiliency and caregiver burden. Palliat Support Care. 2018; 16(3):269-77. [DOI:10.1017/S1478951517000268] [PMID]
- Seo YJ, Park H. Factors influencing caregiver burden in families of hospitalised patients with lung cancer. J Clin Nurs. 2019; 28(9-10):1979-89. [DOI:10.1111/jocn.14812] [PMID]
- Vahidi M, Mahdavi N, Asghari E, Ebrahimi H, Eivazi Ziaei J, Hosseinzadeh M, et al. Other side of breast cancer: Factors associated with caregiver burden. Asian Nurs Res (Korean Soc Nurs Sci). 2016; 10(3):201-6. [DOI:10.1016/j.anr.2016.06.002] [PMID]
- Al-Daken LI, Ahmad MM. Predictors of burden and quality of sleep among family caregivers of patients with cancer. Support Care Cancer. 2018; 26(11):3967-73. [DOI:10.1007/s00520-018-4287-x] [PMID]
- Schrank B, Ebert-Vogel A, Amering M, Masel EK, Neubauer M, Watzke H, et al. Gender differences in caregiver burden and its determinants in family members of terminally ill cancer patients. Psychooncology. 2016; 25(7):808-14.[DOI:10.1002/pon.4005] [PMID]
- Danacı E, Koç Z. Caregiving burden and life satisfaction among caregivers of cancer patients admitted to the emergency department. Clin Nurs Res. 2018; 27(7):800-25. [DOI:10.1177/1054773817708083] [PMID]
Article Type : Research |
Subject:
General
Received: 2022/04/24 | Accepted: 2023/09/13 | Published: 2024/01/1
Received: 2022/04/24 | Accepted: 2023/09/13 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |