Wed, Feb 4, 2026
Volume 34, Issue 1 (1-2024)
JHNM 2024, 34(1): 82-91 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tartibzadeh G, Feizollahzadeh H, Shabanloei R. Effect of Self-care Education Using Face-to-face Method and Pamphlets on Epilepsy Risk Awareness of Patients With Epilepsy and their Family Caregivers. JHNM 2024; 34 (1) :82-91
URL: http://hnmj.gums.ac.ir/article-1-2260-en.html
URL: http://hnmj.gums.ac.ir/article-1-2260-en.html
1- Emergency Nursing student in MSc, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran.
2- Associate Professor, Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran. ,feizollahzadehh@tbzmed.ac.ir
3- Associate Professor, Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran.
2- Associate Professor, Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran. ,
3- Associate Professor, Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran.
Full-Text [PDF 449 kb]
(560 Downloads)
| Abstract (HTML) (1205 Views)
Full-Text: (593 Views)
Introduction
Epilepsy is a chronic disorder that affects about 50 million people worldwide [1]. Epileptic seizures are unpredictable and often debilitating, affecting patients’ quality of life throughout their lives [2, 3]. After a seizure, especially if it is frequent and uncontrolled, a variety of physical injuries can occur, ranging from minor injuries to sudden death [4, 5]. Effective epilepsy management, including raising awareness and improving patients’ self-care skills, can protect them from possible injuries and prevent unnecessary restrictions to improve their quality of life [6, 7]. According to Orem’s self-care theory, people can take care of themselves and the care should focus on strengthening self-care ability in patients or family members, especially family caregivers [8]. Patients with epilepsy should learn various skills to protect themselves. They need regular care and education [9, 10].
Although many studies have been conducted on different aspects of epilepsy care [11], there is scant research on the epilepsy risk awareness (ERA) of patients, and we found no studies in this field in Iran. However, some studies have examined the general knowledge of patients and families about epilepsy, and the results have shown that patients and families do not have enough knowledge of the different aspects of epilepsy care [12, 13] and that comprehensive and effective training is needed. Eze et al. reported that many school teachers have poor knowledge and practice related to epilepsy and have negative attitudes towards patients with epilepsy. After an educational intervention, their knowledge, attitudes, and practice related to epilepsy were improved [14]. To meet the educational needs of patients, nurses play a main role in the care and education of patients and their families [15]. It is better to use the most effective educational strategies, such as the standard face-to-face method [16]. However, due to various factors such as the lack of resources, staff, and time [17-19], it can be challenging to assess risk factors and provide necessary training with the desired quality to the patients and family caregivers. Therefore, to overcome these challenges, it is necessary to use other effective, cost-effective and flexible educational strategies, such as the pamphlets. Accordingly, this study aims to investigate the effect of self-care training on the ERA of patients with epilepsy and their family caregivers in Tabriz, Iran using two methods, face-to-face training and pamphlets. In this regard, the objectives of this study include:
1) Comparing the ERA of patients with epilepsy before and after training in the intervention and pamphlet groups;
2) Comparing the ERA of the family caregivers of patients with epilepsy before and after training in the intervention and pamphlet groups.
Materials and Methods
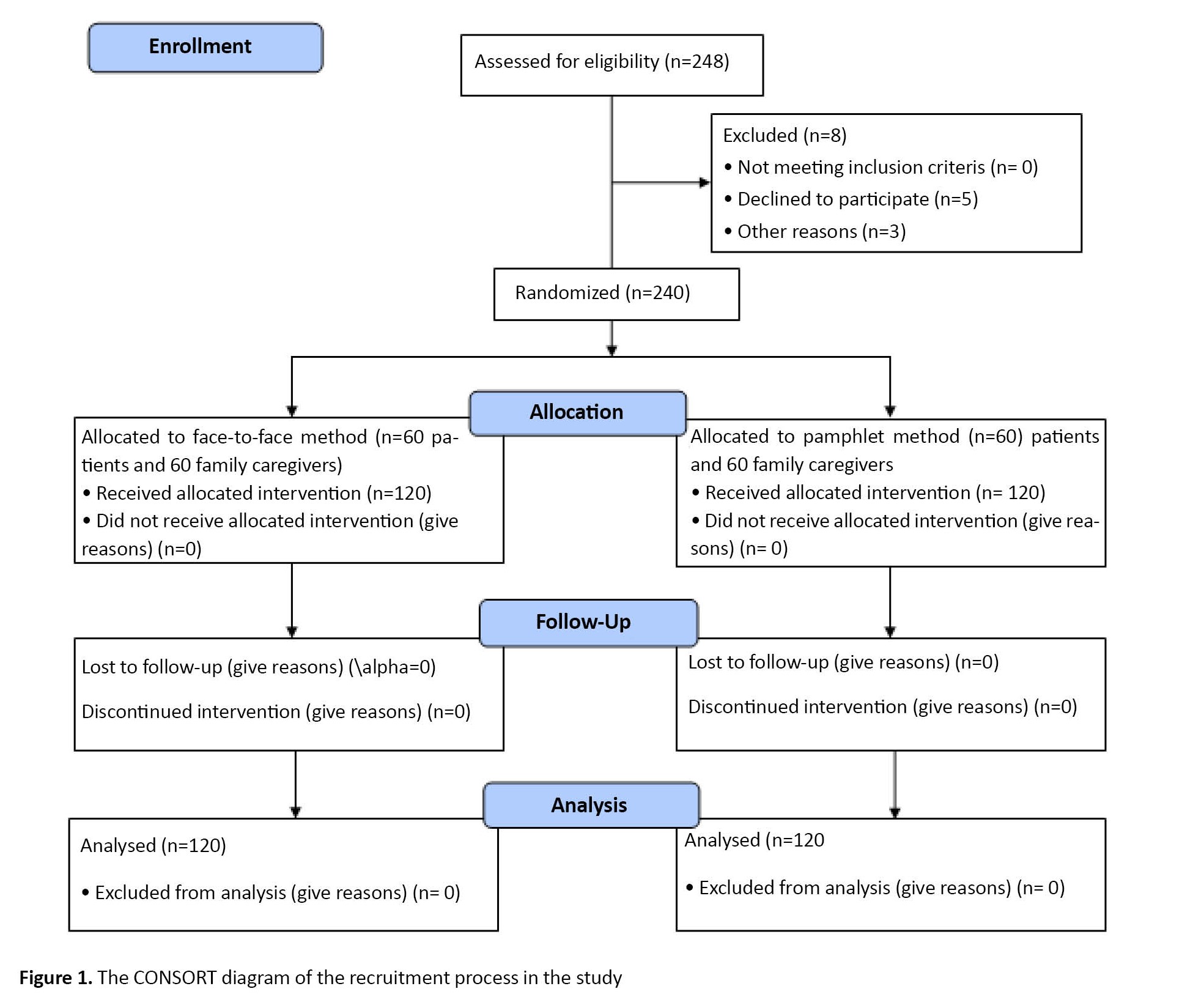
In this quasi-experimental study, the study population consists of patients with epilepsy and their family caregivers referred to the neurological clinic of a hospital affiliated to Tabriz University of Medical Sciences. To determine the sample size, a pilot study was conducted on 30 patients with epilepsy (mean ERA score=81.9±7.3) and their family caregivers (mean ERA score=83.7±9.2). Considering a 95% confidence level and a statistical power of 80%, the required sample size for each group was determined 54 for patients and 56 for caregivers. Considering a 10% sample dropout, 124 patients (62 in each group) and 124 caregivers (62 in each group) were selected for the study. Of these, three were excluded due to lack of consent and five were excluded for lack of interest (Figure 1). The samples were selected by a convenience sampling method. Opaque, numbered, and sealed envelopes were used for allocation concealment. Inclusion criteria were ability to communicate and answer the questions, age ≥15 years, no drug addiction based on medical records, and a confirmed diagnosis of epilepsy based on a history of seizures and EEG results according to a neurologist. Exclusion criteria for both groups were absence due to death or travel, withdrawal, unwillingness to continue participation, and not responding to ≥10% of the questions. The sampling was carried for 3 months from December 2021 to March 2022.
The primary outcome variable was ERA in patients with epilepsy and their family caregivers. The third edition of the ERA scale for patients and its modified version for family caregivers were used to collect data. The first part of the scales surveys demographic characteristics such as age (years), gender (female, male), marital status (single, married, divorced, widowed), occupation (employed, unemployed), ethnicity (Persian, Turkish, Kurdish), patient’s history of seizures (year), educational level (elementary school, high school, high school diploma, academic), history of using anticonvulsants, and relationship with caregiver (spouse, father, mother, child, and other). The second part of the two ERA scales for patients and family caregivers had 40 items measuring ERA in four areas, including the characteristics of epilepsy (18 items), personal safety (10 items), physical wellbeing (6 items), and mental wellbeing (6 items). The items are rated on a four-point scale as yes (3 points), sometimes (2 points), no (1 point) and not applicable (0 points). The total score ranges from 0 to 120, with higher scores indicating more active participation, more safety, and lower risk level. The time required to complete each questionnaire was 7-10 minutes [6]. In the present study, the ERA scale was first translated into Persian by a professional translator and then translated back to English by another professional translator. The translators and researchers evaluated all versions of the scale, and the final Persian version of the ERA scale for patients was developed and approved by consensus. After small modification of some items, an ERA scale for family caregivers was also developed. For determining the content and face validity of the scale, the Persian version was sent to 15 professors of the Faculty of Nursing and Midwifery and their suggestions were implemented. The reliability of the scale was assessed using the Cronbach’s α coefficient in a pilot study with 30 patients with epilepsy (α=0.86) and family caregivers (α=0.88). For data collection, the researcher first visited the patients with epilepsy and family caregivers in the outpatient neurological clinic of a teaching hospital in the morning and evening shifts. After explaining the study objectives to them and obtaining their written informed consent, the questionnaire was completed through the interview with the participants (response rate=100%). Due to ethical considerations, all patients received routine medical and nursing care throughout the study.
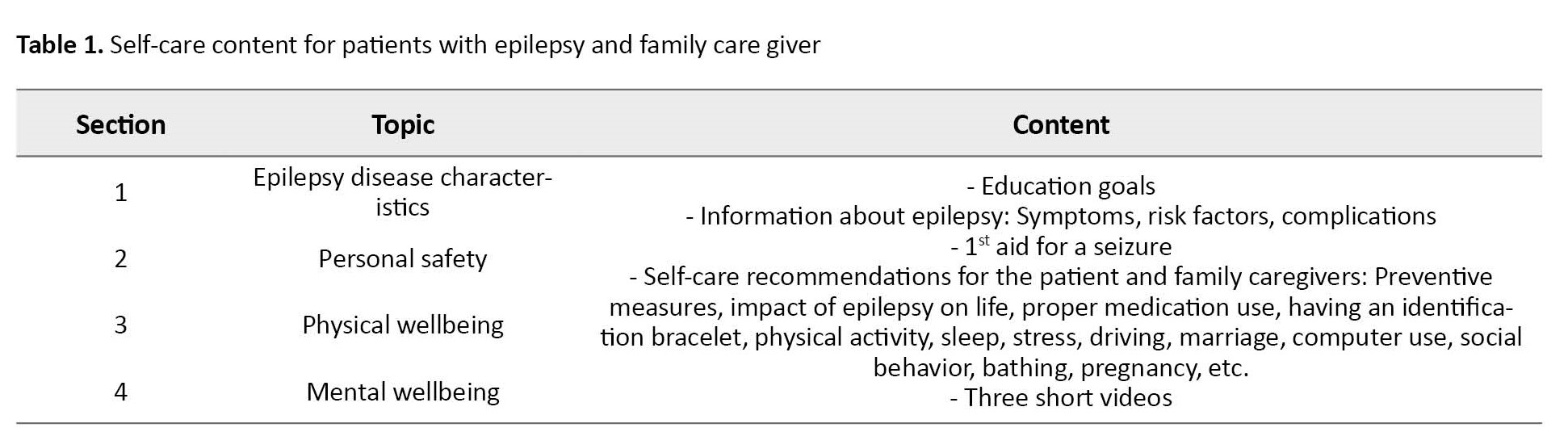
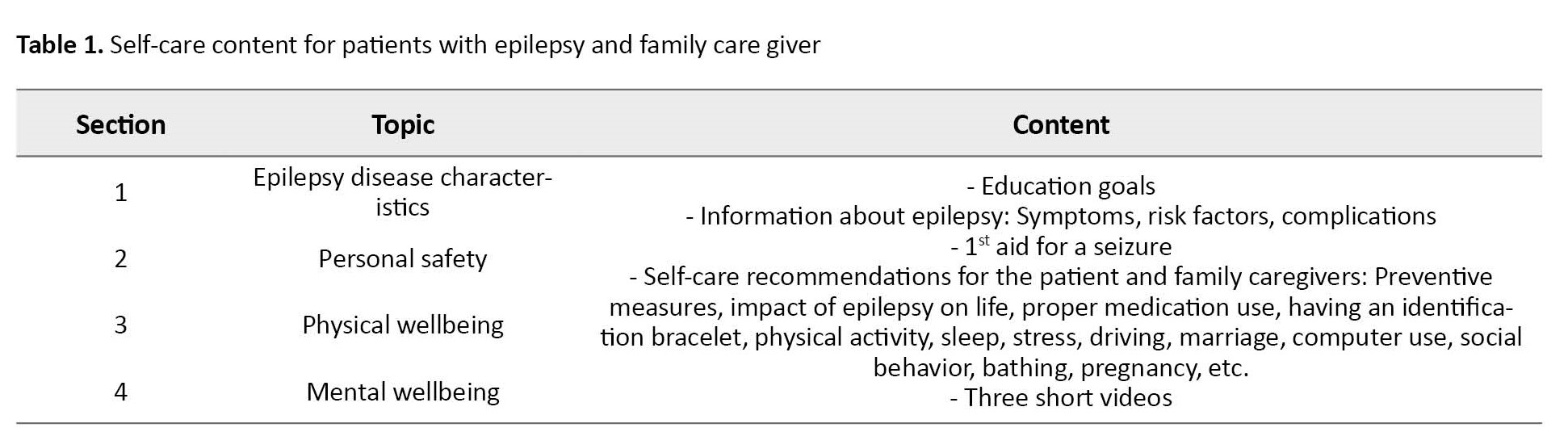
After extensive review of literature, ERA-based self-care training content for patients with epilepsy and family caregivers was prepared in four sections (Table 1).
To simplify and facilitate learning, the content was prepared with simple sentences, using large fonts, colored images, and three short videos. Its validity was confirmed by five professors and one neurologist. After the pre-test assessments, the intervention group received the ERA-based self-care training by face-to-face method. The training sessions were carried out in paired groups (patient and his/her family caregiver) in a designated room in the clinic 60 minutes. During the training, there was a question & answer session. The participants could ask their questions and receive feedback. The pamphlet group received the self-care education using pamphlets. Except for the videos, the content was the same as in the intervention group. A telephone number was provided to the participants in both groups to follow up and answer the questions. One week after the first visit, the researcher called the patients and their family caregivers and answered any questions they have. To prevent a possible exchange of information between the two groups, the training and the tests were carried out separately for them. The patients, family caregivers, and nurses were unaware of the allocation and the research details. One month after the first visit, both groups were asked to fill out the ERA questionnaire again. For ethical considerations, participants in the pamphlet group also received the ERA-based self-care training by face-to-face method and the intervention group received the ERA-based self-care education pamphlets at the end of the post-test phase.
Collected data were analyzed in SPSS software, version 21 (SPSS Inc., Chicago, IL, USA) using descriptive statistics, paired t-test, independent t-test, Fisher’s exact test, chi-square test, and analysis of covariance (ANCOVA). The results of the Kolmogorov-Smirnov test indicated the normality of the data distribution. P<0.05 was considered as statistically significance.
Results
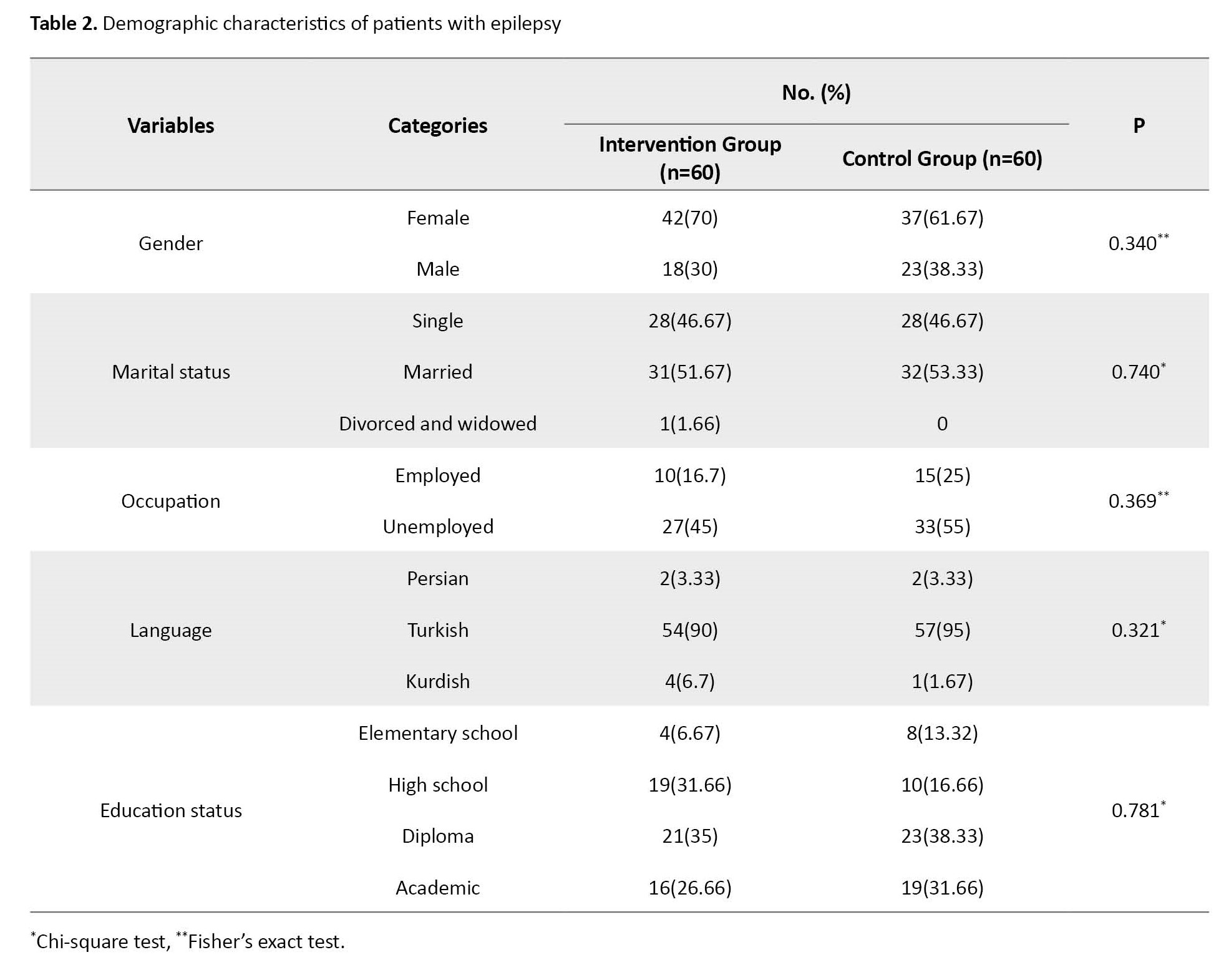
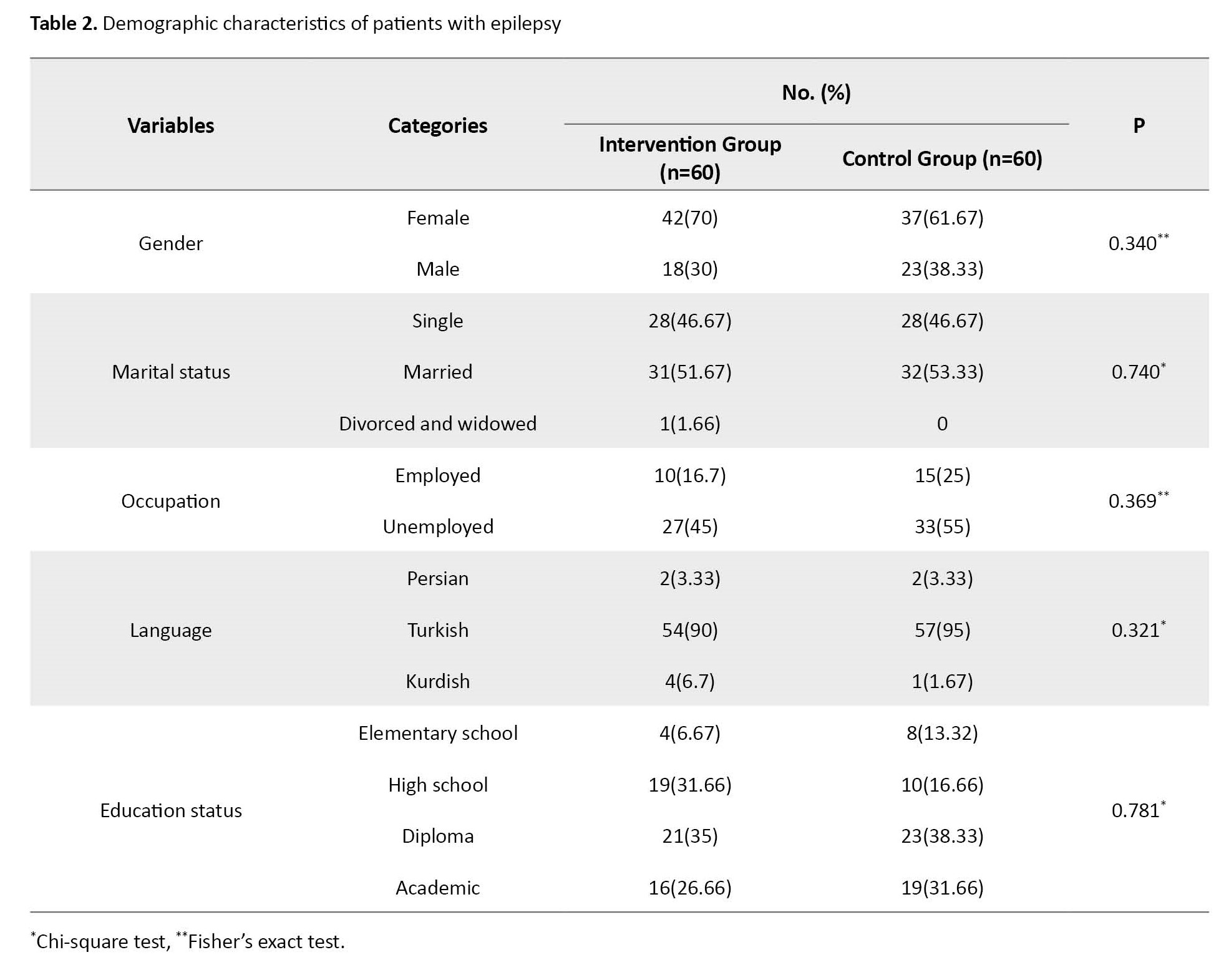
The mean age of the patients was 28.07±10.87 years in the intervention group and 30.28±10.64 years in the pamphlet group. Table 2 shows other demographic characteristics of the patients.
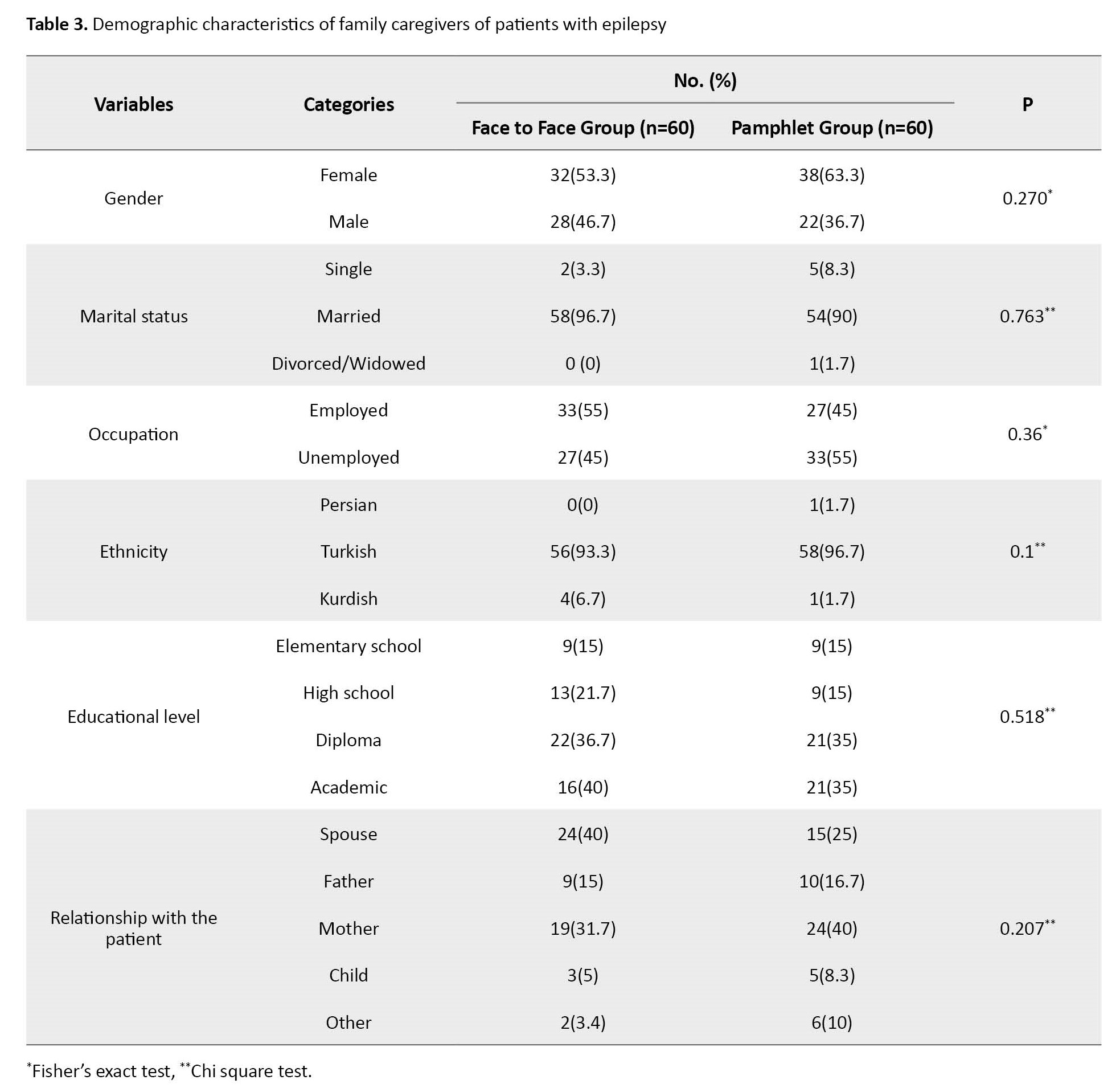
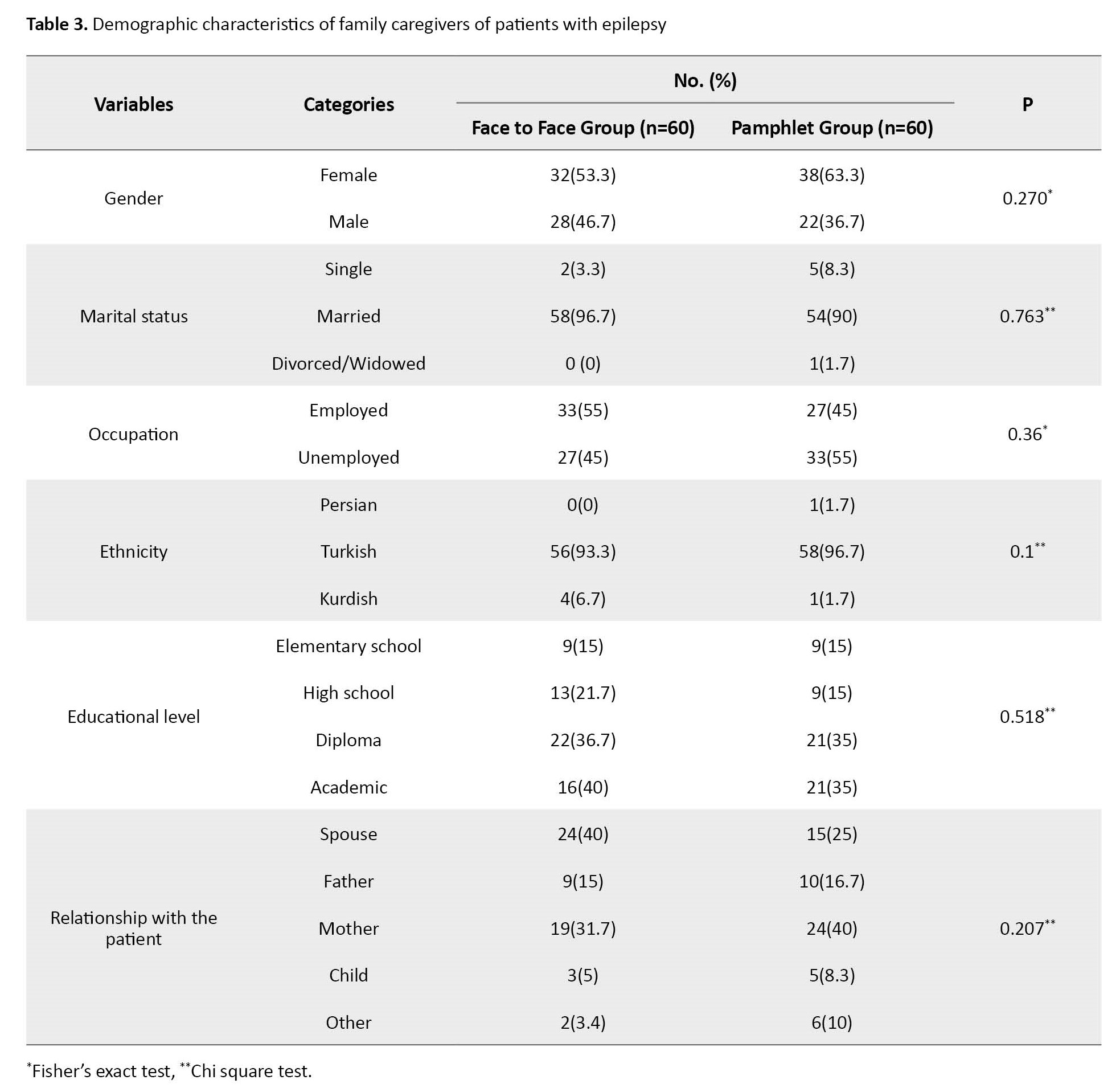
The mean age of family caregivers was 40.75±9.52 years in the intervention group and 42.32±10.70 years in the pamphlet group. The independent t-test results indicated that the difference in age between groups was not statistically significant. Table 3 shows other demographic characteristics of family caregivers.
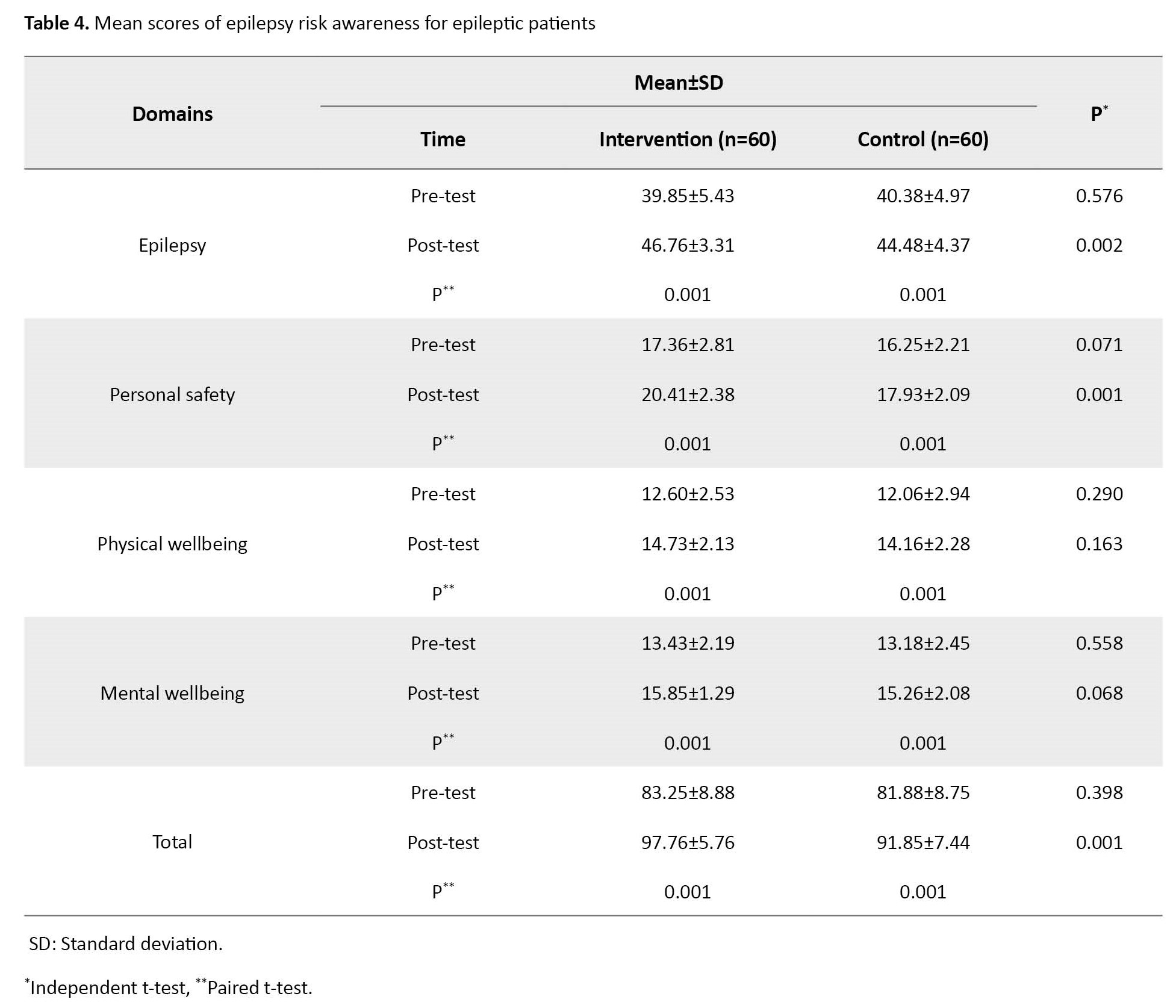
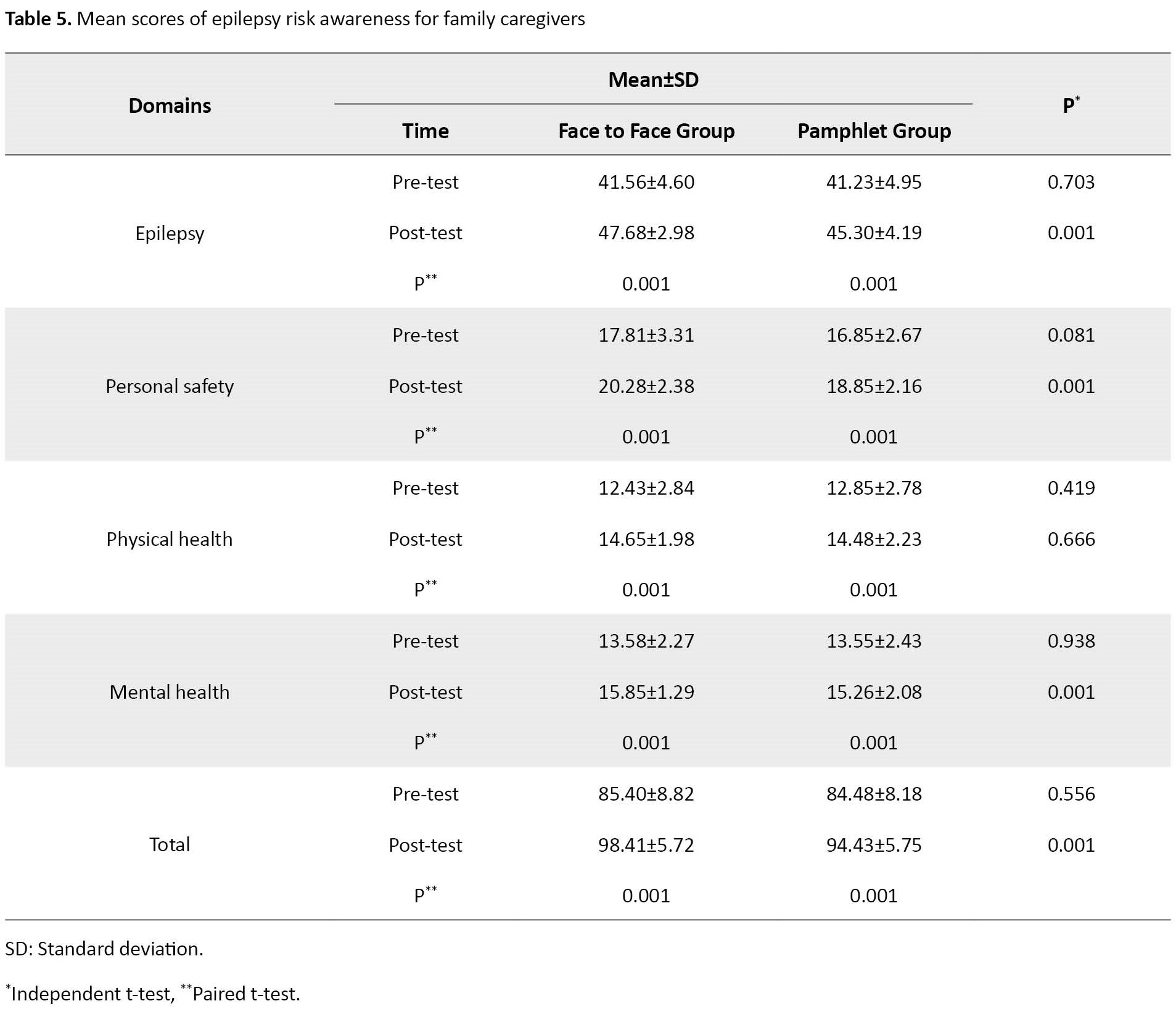
The mean ERA scores for patients and family caregivers are presented in Table 4 and Table 5 , respectively. The ANCOVA was used to compare the post-test ERA scores between two groups, after controlling the pre-test scores.
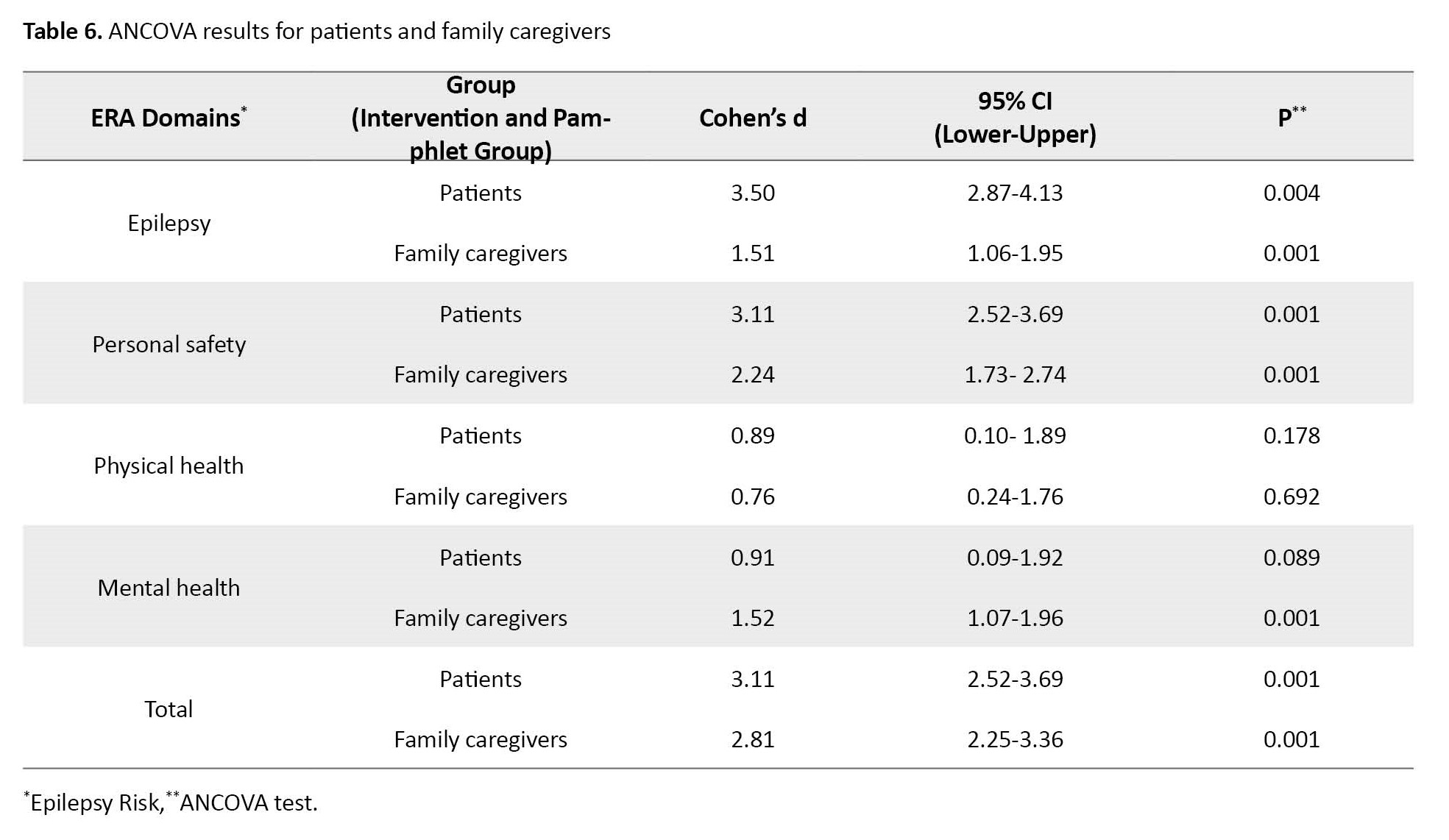
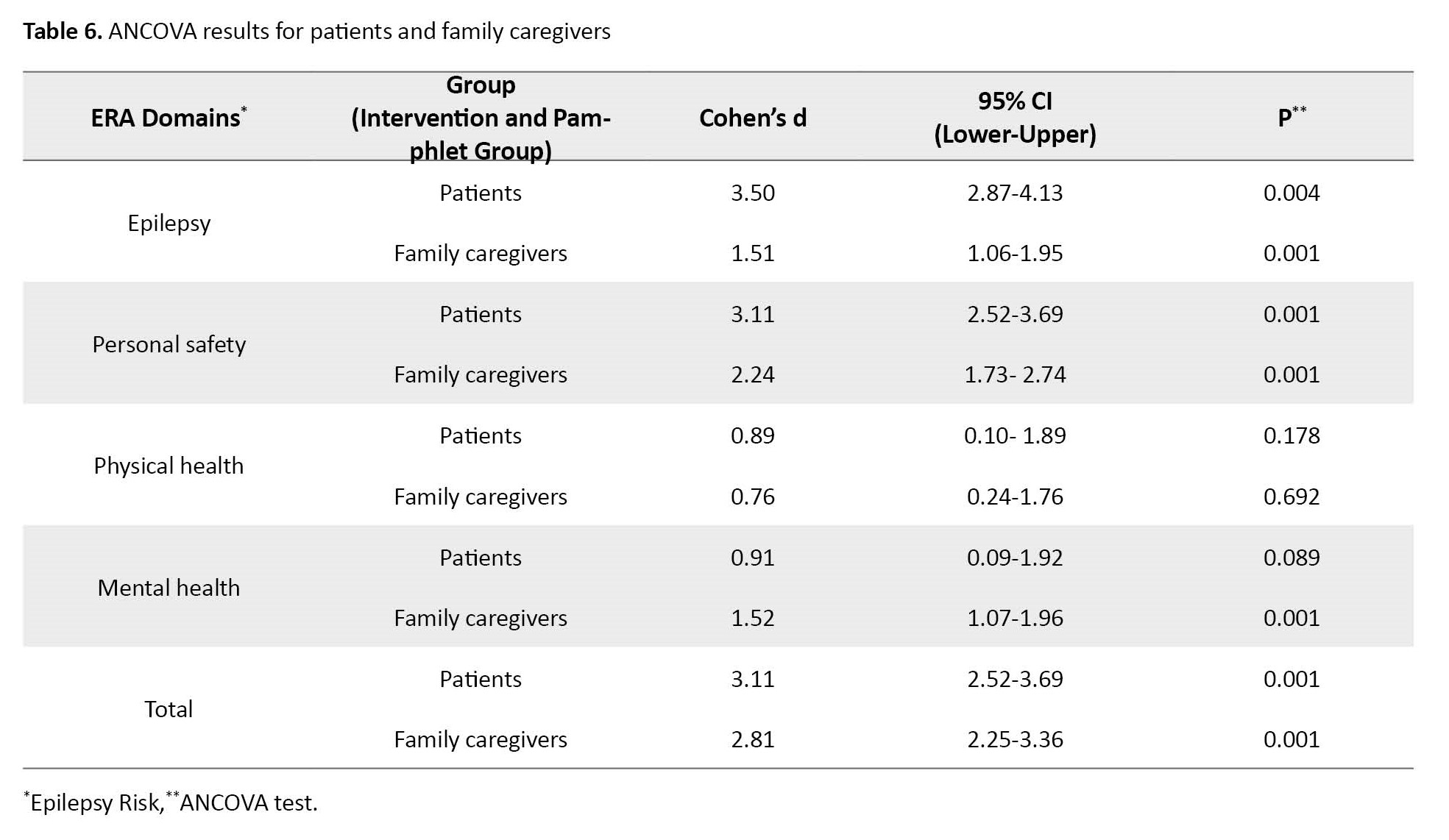
The results showed a significant increase in the domains of ERA in the intervention and pamphlet groups of patients and family caregivers after education. The mean post-test ERA scores in the intervention group of patients and caregivers were significantly higher than in the pamphlet group (Cohen’s d for patients=3.11, P=0.001; Cohen’s d for family caregivers=2.81, P=0.001) the rest of information is presented in Table 6.
Discussion
The results of the present study showed that self-care education about ERA by face-to-face method resulted in a significant increase in all domains of ERA in patients with epilepsy and family caregivers. In patients with epilepsy, only two domains of ERA (characteristics of epilepsy and personal safety) were significantly different between the two intervention and pamphlet groups in the post-test phase. The difference in the domains of physical and mental health was not significant between the two groups after education. In the family caregivers, the results showed that, after education, the score of ERA were significant between the intervention and pamphlet groups in all domains exception for physical wellbeing. In other words, the face-to-face method improved ERA of patients and their family caregivers in some cases better than the pamphlet use. Therefore, the self-care training programs based on the ERA for patients with epilepsy and their family caregivers are better in the face-to-face method. Effective education can improve self-care and quality of life of patients. A study used discussion sessions about health issues between nurses and patients or their families a patient education strategy [20]. The face-to-face education should be performed by an experienced nurse along with proper follow-up. In this way, patients can be protected against the possible risks of epilepsy and their lifestyle can be improved.
Based on the results of the present study, the ERA of patients with epilepsy and family caregivers were significantly improved in all domains in the pamphlet group. Therefore, in the absence of available resources, including lack of time, lack of human resources, or financial problems, nurses can use pamphlets to provide self-care education for patients with epilepsy and their family caregivers to improve their ERA. It should be performed by an experienced nurse along with proper follow-up and responsiveness.
In ERA-based self-care education for patients with epilepsy and their family caregivers, the potential risks, educational needs, and the cases requiring intervention should be identified. After evaluating different strategies for patient education, Zirwas et al. found that due to various factors such as time and patient motivation, a single strategy is not always the most effective way to educate patients. They suggested that a combination of pedagogical strategies should be used for optimal learning [20]. Results of a systematic review study identified five themes that categorize facilitators and barriers to the successful implementation of epilepsy self-management programs, including relevance, personalization, intervention components, clinicians, and technology considerations. Their results indicated that involving patients with epilepsy and their caregivers in program development and then tailoring the educational content during the intervention can help ensure that the content is relevant to intervention participants. Their results also indicated that the clinician’s role in providing self-management training is important [21].
In the present study, most of patients with epilepsy and their family caregivers did not have enough knowledge of the side effects of antiepileptic drugs and the prevention of epilepsy risk factors before education. After the education, their information and awareness improved. Results of a study by Hu et al. showed that self-management training can reduce seizure frequency, improve quality of life, increase antiepileptic drug use, and reduce seizure-related accidental injuries in patients with epilepsy who are aware of seizure precursors or precipitating factors [22]. In the study by Yadegari et al., one month after the educational intervention in patients with epilepsy, the mean scores of medications self-management were significantly improved [23]. Hagemann et al. provided an educational program for the parents of children with epilepsy in Germany and Austria. Their results showed that the educational program was effective and helped parents to manage their children’s epilepsy and reduce the anxiety associated with epilepsy [24]. Pascual et al. conducted a public education intervention with educational pamphlets and videos aimed at reducing the cost of epilepsy management. Four months after the educational intervention, the number of visits to the emergency department for patients with epilepsy decreased significantly. This finding supports patient and family education as a valuable strategy in reducing emergency room visits, which can reduce healthcare costs [25].
As one of the limitations of the present study, it should be taken into account that ERA is a subjective and multi-domain concept and is influenced in various ways by personal, social, and environmental factors. Although an appropriate instrument was used for measurement in this study, there was a possibility of response bias. In the present study, the education was provided in the evening shift. The difference in the shift can affect the results. In addition, only patients and family caregivers with an appropriate cognitive level were included in this study. There are different types of epilepsy; the training on safety precautions should be tailored to the epilepsy type and treatment relevant. Therefore, the necessary considerations should be made when generalizing these results to all epilepsy types.
In conclusion, the ERA-based self-care education using both face-to-face method and pamphlets can significantly increase the ERA and its four domains (characteristics of epilepsy, personal safety, physical wellbeing, and mental wellbeing) in patients with epilepsy and their family caregivers, where the face-to-face method is more effective than the pamphlet use. Depending on the existing conditions and available resources, nurses can use the face-to-face method or education pamphlets to facilitate the learning process of patients with epilepsy and family caregivers and improve their quality of life.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.REC.1400.840). Before the study, the patients and family caregivers were informed about the study objectives and their rights to leave the study at any time. Then, a written informed consent was obtained from them.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, design, data collection, data analysis, data interpretation, and draft preparation: Hossein Feizollahzadeh and Golzar Tartibzadeh; Data analysis, data interpretation and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the patients and their families for their cooperation.
References
Epilepsy is a chronic disorder that affects about 50 million people worldwide [1]. Epileptic seizures are unpredictable and often debilitating, affecting patients’ quality of life throughout their lives [2, 3]. After a seizure, especially if it is frequent and uncontrolled, a variety of physical injuries can occur, ranging from minor injuries to sudden death [4, 5]. Effective epilepsy management, including raising awareness and improving patients’ self-care skills, can protect them from possible injuries and prevent unnecessary restrictions to improve their quality of life [6, 7]. According to Orem’s self-care theory, people can take care of themselves and the care should focus on strengthening self-care ability in patients or family members, especially family caregivers [8]. Patients with epilepsy should learn various skills to protect themselves. They need regular care and education [9, 10].
Although many studies have been conducted on different aspects of epilepsy care [11], there is scant research on the epilepsy risk awareness (ERA) of patients, and we found no studies in this field in Iran. However, some studies have examined the general knowledge of patients and families about epilepsy, and the results have shown that patients and families do not have enough knowledge of the different aspects of epilepsy care [12, 13] and that comprehensive and effective training is needed. Eze et al. reported that many school teachers have poor knowledge and practice related to epilepsy and have negative attitudes towards patients with epilepsy. After an educational intervention, their knowledge, attitudes, and practice related to epilepsy were improved [14]. To meet the educational needs of patients, nurses play a main role in the care and education of patients and their families [15]. It is better to use the most effective educational strategies, such as the standard face-to-face method [16]. However, due to various factors such as the lack of resources, staff, and time [17-19], it can be challenging to assess risk factors and provide necessary training with the desired quality to the patients and family caregivers. Therefore, to overcome these challenges, it is necessary to use other effective, cost-effective and flexible educational strategies, such as the pamphlets. Accordingly, this study aims to investigate the effect of self-care training on the ERA of patients with epilepsy and their family caregivers in Tabriz, Iran using two methods, face-to-face training and pamphlets. In this regard, the objectives of this study include:
1) Comparing the ERA of patients with epilepsy before and after training in the intervention and pamphlet groups;
2) Comparing the ERA of the family caregivers of patients with epilepsy before and after training in the intervention and pamphlet groups.
Materials and Methods
In this quasi-experimental study, the study population consists of patients with epilepsy and their family caregivers referred to the neurological clinic of a hospital affiliated to Tabriz University of Medical Sciences. To determine the sample size, a pilot study was conducted on 30 patients with epilepsy (mean ERA score=81.9±7.3) and their family caregivers (mean ERA score=83.7±9.2). Considering a 95% confidence level and a statistical power of 80%, the required sample size for each group was determined 54 for patients and 56 for caregivers. Considering a 10% sample dropout, 124 patients (62 in each group) and 124 caregivers (62 in each group) were selected for the study. Of these, three were excluded due to lack of consent and five were excluded for lack of interest (Figure 1). The samples were selected by a convenience sampling method. Opaque, numbered, and sealed envelopes were used for allocation concealment. Inclusion criteria were ability to communicate and answer the questions, age ≥15 years, no drug addiction based on medical records, and a confirmed diagnosis of epilepsy based on a history of seizures and EEG results according to a neurologist. Exclusion criteria for both groups were absence due to death or travel, withdrawal, unwillingness to continue participation, and not responding to ≥10% of the questions. The sampling was carried for 3 months from December 2021 to March 2022.
The primary outcome variable was ERA in patients with epilepsy and their family caregivers. The third edition of the ERA scale for patients and its modified version for family caregivers were used to collect data. The first part of the scales surveys demographic characteristics such as age (years), gender (female, male), marital status (single, married, divorced, widowed), occupation (employed, unemployed), ethnicity (Persian, Turkish, Kurdish), patient’s history of seizures (year), educational level (elementary school, high school, high school diploma, academic), history of using anticonvulsants, and relationship with caregiver (spouse, father, mother, child, and other). The second part of the two ERA scales for patients and family caregivers had 40 items measuring ERA in four areas, including the characteristics of epilepsy (18 items), personal safety (10 items), physical wellbeing (6 items), and mental wellbeing (6 items). The items are rated on a four-point scale as yes (3 points), sometimes (2 points), no (1 point) and not applicable (0 points). The total score ranges from 0 to 120, with higher scores indicating more active participation, more safety, and lower risk level. The time required to complete each questionnaire was 7-10 minutes [6]. In the present study, the ERA scale was first translated into Persian by a professional translator and then translated back to English by another professional translator. The translators and researchers evaluated all versions of the scale, and the final Persian version of the ERA scale for patients was developed and approved by consensus. After small modification of some items, an ERA scale for family caregivers was also developed. For determining the content and face validity of the scale, the Persian version was sent to 15 professors of the Faculty of Nursing and Midwifery and their suggestions were implemented. The reliability of the scale was assessed using the Cronbach’s α coefficient in a pilot study with 30 patients with epilepsy (α=0.86) and family caregivers (α=0.88). For data collection, the researcher first visited the patients with epilepsy and family caregivers in the outpatient neurological clinic of a teaching hospital in the morning and evening shifts. After explaining the study objectives to them and obtaining their written informed consent, the questionnaire was completed through the interview with the participants (response rate=100%). Due to ethical considerations, all patients received routine medical and nursing care throughout the study.
After extensive review of literature, ERA-based self-care training content for patients with epilepsy and family caregivers was prepared in four sections (Table 1).
To simplify and facilitate learning, the content was prepared with simple sentences, using large fonts, colored images, and three short videos. Its validity was confirmed by five professors and one neurologist. After the pre-test assessments, the intervention group received the ERA-based self-care training by face-to-face method. The training sessions were carried out in paired groups (patient and his/her family caregiver) in a designated room in the clinic 60 minutes. During the training, there was a question & answer session. The participants could ask their questions and receive feedback. The pamphlet group received the self-care education using pamphlets. Except for the videos, the content was the same as in the intervention group. A telephone number was provided to the participants in both groups to follow up and answer the questions. One week after the first visit, the researcher called the patients and their family caregivers and answered any questions they have. To prevent a possible exchange of information between the two groups, the training and the tests were carried out separately for them. The patients, family caregivers, and nurses were unaware of the allocation and the research details. One month after the first visit, both groups were asked to fill out the ERA questionnaire again. For ethical considerations, participants in the pamphlet group also received the ERA-based self-care training by face-to-face method and the intervention group received the ERA-based self-care education pamphlets at the end of the post-test phase.
Collected data were analyzed in SPSS software, version 21 (SPSS Inc., Chicago, IL, USA) using descriptive statistics, paired t-test, independent t-test, Fisher’s exact test, chi-square test, and analysis of covariance (ANCOVA). The results of the Kolmogorov-Smirnov test indicated the normality of the data distribution. P<0.05 was considered as statistically significance.
Results
The mean age of the patients was 28.07±10.87 years in the intervention group and 30.28±10.64 years in the pamphlet group. Table 2 shows other demographic characteristics of the patients.
The mean age of family caregivers was 40.75±9.52 years in the intervention group and 42.32±10.70 years in the pamphlet group. The independent t-test results indicated that the difference in age between groups was not statistically significant. Table 3 shows other demographic characteristics of family caregivers.
The mean ERA scores for patients and family caregivers are presented in Table 4 and Table 5 , respectively. The ANCOVA was used to compare the post-test ERA scores between two groups, after controlling the pre-test scores.
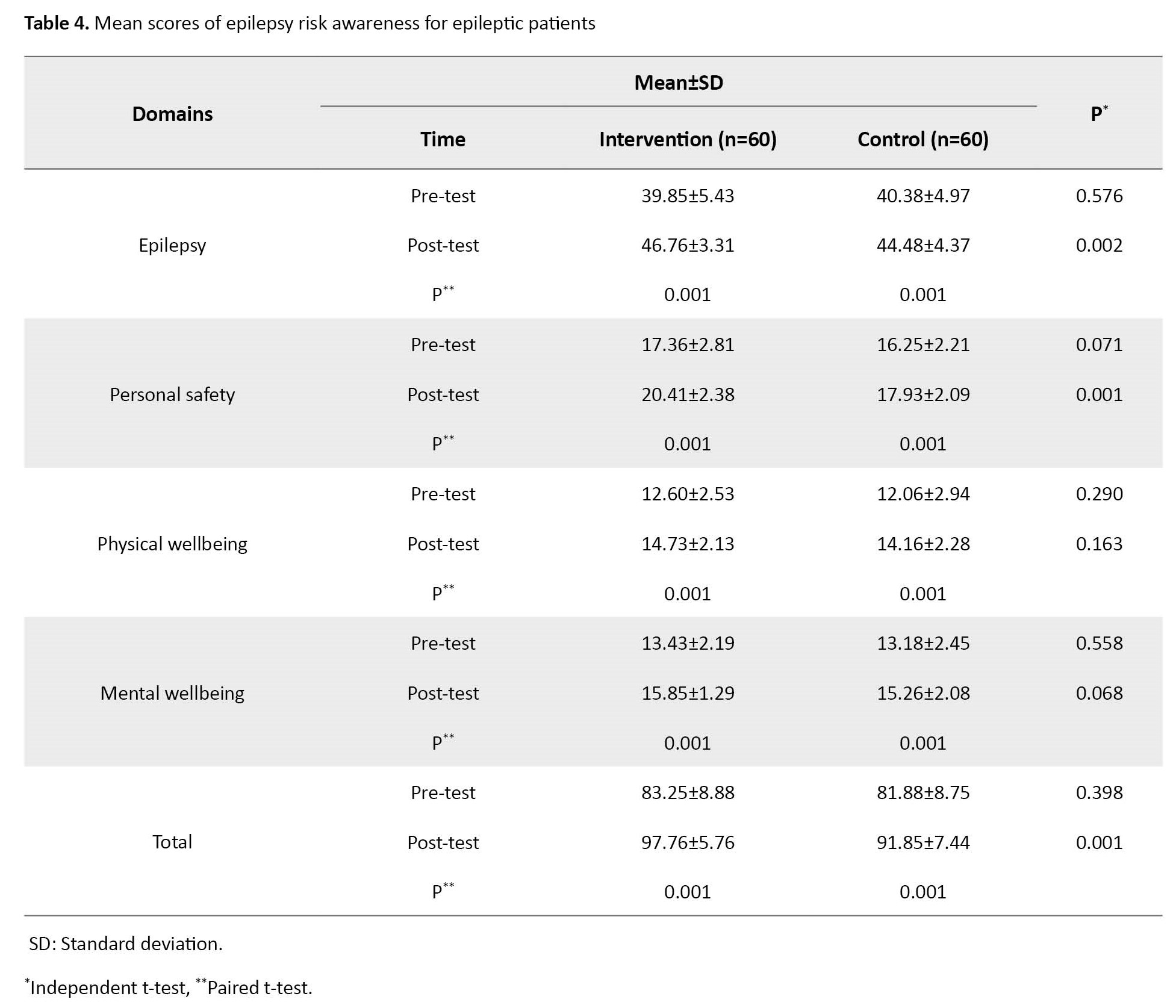
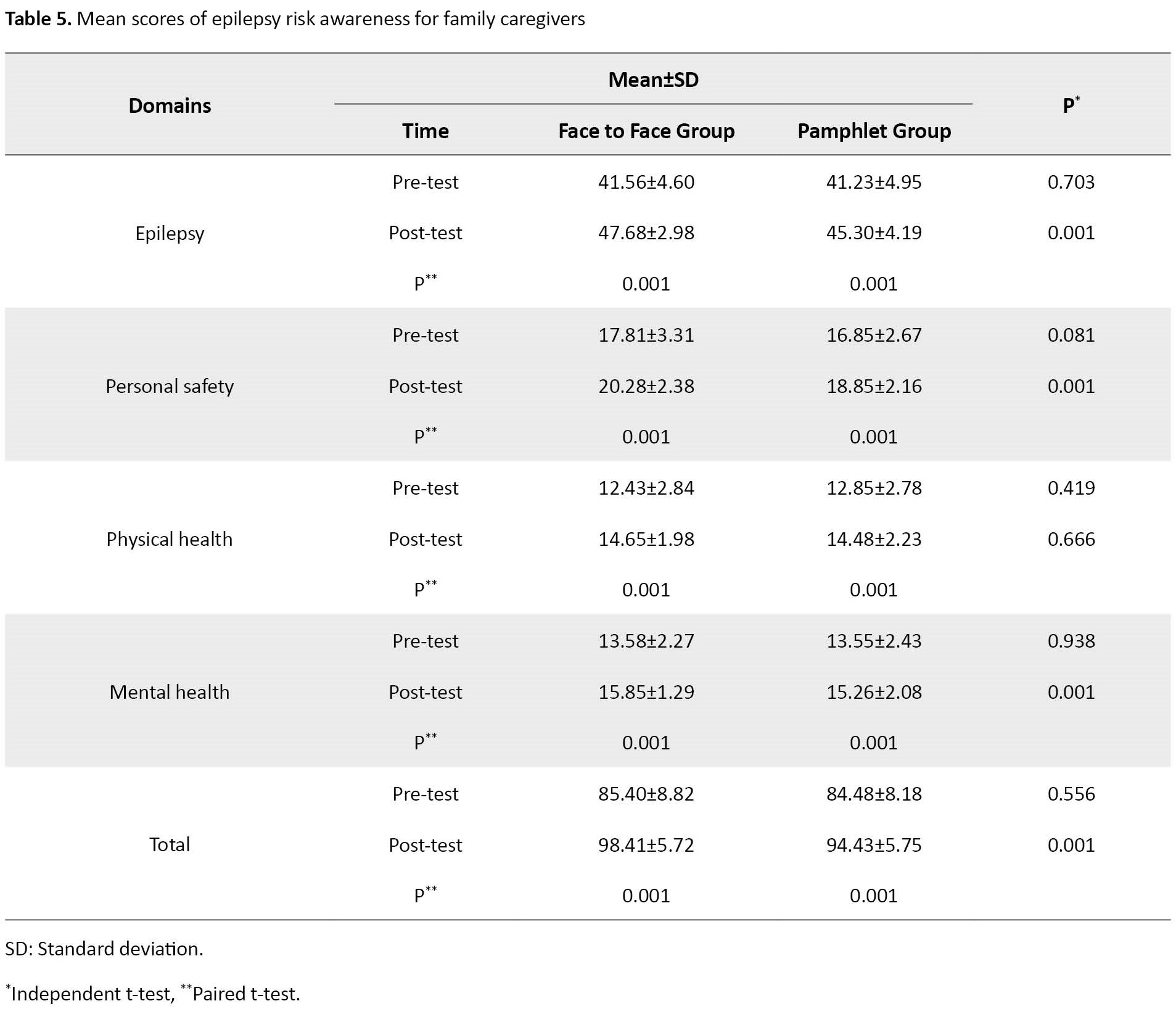
The results showed a significant increase in the domains of ERA in the intervention and pamphlet groups of patients and family caregivers after education. The mean post-test ERA scores in the intervention group of patients and caregivers were significantly higher than in the pamphlet group (Cohen’s d for patients=3.11, P=0.001; Cohen’s d for family caregivers=2.81, P=0.001) the rest of information is presented in Table 6.
Discussion
The results of the present study showed that self-care education about ERA by face-to-face method resulted in a significant increase in all domains of ERA in patients with epilepsy and family caregivers. In patients with epilepsy, only two domains of ERA (characteristics of epilepsy and personal safety) were significantly different between the two intervention and pamphlet groups in the post-test phase. The difference in the domains of physical and mental health was not significant between the two groups after education. In the family caregivers, the results showed that, after education, the score of ERA were significant between the intervention and pamphlet groups in all domains exception for physical wellbeing. In other words, the face-to-face method improved ERA of patients and their family caregivers in some cases better than the pamphlet use. Therefore, the self-care training programs based on the ERA for patients with epilepsy and their family caregivers are better in the face-to-face method. Effective education can improve self-care and quality of life of patients. A study used discussion sessions about health issues between nurses and patients or their families a patient education strategy [20]. The face-to-face education should be performed by an experienced nurse along with proper follow-up. In this way, patients can be protected against the possible risks of epilepsy and their lifestyle can be improved.
Based on the results of the present study, the ERA of patients with epilepsy and family caregivers were significantly improved in all domains in the pamphlet group. Therefore, in the absence of available resources, including lack of time, lack of human resources, or financial problems, nurses can use pamphlets to provide self-care education for patients with epilepsy and their family caregivers to improve their ERA. It should be performed by an experienced nurse along with proper follow-up and responsiveness.
In ERA-based self-care education for patients with epilepsy and their family caregivers, the potential risks, educational needs, and the cases requiring intervention should be identified. After evaluating different strategies for patient education, Zirwas et al. found that due to various factors such as time and patient motivation, a single strategy is not always the most effective way to educate patients. They suggested that a combination of pedagogical strategies should be used for optimal learning [20]. Results of a systematic review study identified five themes that categorize facilitators and barriers to the successful implementation of epilepsy self-management programs, including relevance, personalization, intervention components, clinicians, and technology considerations. Their results indicated that involving patients with epilepsy and their caregivers in program development and then tailoring the educational content during the intervention can help ensure that the content is relevant to intervention participants. Their results also indicated that the clinician’s role in providing self-management training is important [21].
In the present study, most of patients with epilepsy and their family caregivers did not have enough knowledge of the side effects of antiepileptic drugs and the prevention of epilepsy risk factors before education. After the education, their information and awareness improved. Results of a study by Hu et al. showed that self-management training can reduce seizure frequency, improve quality of life, increase antiepileptic drug use, and reduce seizure-related accidental injuries in patients with epilepsy who are aware of seizure precursors or precipitating factors [22]. In the study by Yadegari et al., one month after the educational intervention in patients with epilepsy, the mean scores of medications self-management were significantly improved [23]. Hagemann et al. provided an educational program for the parents of children with epilepsy in Germany and Austria. Their results showed that the educational program was effective and helped parents to manage their children’s epilepsy and reduce the anxiety associated with epilepsy [24]. Pascual et al. conducted a public education intervention with educational pamphlets and videos aimed at reducing the cost of epilepsy management. Four months after the educational intervention, the number of visits to the emergency department for patients with epilepsy decreased significantly. This finding supports patient and family education as a valuable strategy in reducing emergency room visits, which can reduce healthcare costs [25].
As one of the limitations of the present study, it should be taken into account that ERA is a subjective and multi-domain concept and is influenced in various ways by personal, social, and environmental factors. Although an appropriate instrument was used for measurement in this study, there was a possibility of response bias. In the present study, the education was provided in the evening shift. The difference in the shift can affect the results. In addition, only patients and family caregivers with an appropriate cognitive level were included in this study. There are different types of epilepsy; the training on safety precautions should be tailored to the epilepsy type and treatment relevant. Therefore, the necessary considerations should be made when generalizing these results to all epilepsy types.
In conclusion, the ERA-based self-care education using both face-to-face method and pamphlets can significantly increase the ERA and its four domains (characteristics of epilepsy, personal safety, physical wellbeing, and mental wellbeing) in patients with epilepsy and their family caregivers, where the face-to-face method is more effective than the pamphlet use. Depending on the existing conditions and available resources, nurses can use the face-to-face method or education pamphlets to facilitate the learning process of patients with epilepsy and family caregivers and improve their quality of life.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.REC.1400.840). Before the study, the patients and family caregivers were informed about the study objectives and their rights to leave the study at any time. Then, a written informed consent was obtained from them.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, design, data collection, data analysis, data interpretation, and draft preparation: Hossein Feizollahzadeh and Golzar Tartibzadeh; Data analysis, data interpretation and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the patients and their families for their cooperation.
References
- Perucca P, Bahlo M, Berkovic SF. The genetics of epilepsy. Annu Rev Genomics Hum Genet. 2020; 21:205-30. [DOI:10.1146/annurev-genom-120219-074937] [PMID]
- Bilgiç A, Işık Ü, Sivri Çolak R, Derin H, Çaksen H. Psychiatric symptoms and health-related quality of life in children with epilepsy and their mothers. Epilepsy Behav. 2018; 80:114-21. [DOI:10.1016/j.yebeh.2017.12.031] [PMID]
- Wo SW, Ong LC, Low WY, Lai PSM. Exploring the needs and challenges of parents and their children in childhood epilepsy care: A qualitative study. Epilepsy Behav. 2018; 88:268-76. [DOI:10.1016/j.yebeh.2018.09.018] [PMID]
- Lam NN, Duc NM, Nam L. Epilepsy related burn injuries in developing country: An experience in National Burn Hospital. Burns Open. 2019; 3(3):99-102. [DOI:10.1016/j.burnso.2019.05.003]
- Tartibzadeh G, Feizollahzadeh H, Shabanloei R, Mwamba B. Epilepsy risk awareness and background factors in patients with epilepsy and family caregivers. Epilepsy Res. 2023; 193, 107146. [DOI:10.1016/j.eplepsyres.2023.107146] [PMID]
- Ison R, Kisan V, Cole C, Angus-Leppan H. The ERA(ERA) Scale: A new era for holistic risk assessment in epilepsy. Front Neurol. 2020; 11:465. [DOI:10.3389/fneur.2020.00465] [PMID]
- Kanner AM. Management of psychiatric and neurological comorbidities in epilepsy. Nat Rev Neurol. 2016; 12(2):106-16. [DOI:10.1038/nrneurol.2015.243] [PMID]
- Younas A. A foundational analysis of dorothea orem’s self-care theory and evaluation of its significance for nursing practice and research. Creat Nurs. 2017; 23(1):13-23. [DOI:10.1891/1078-4535.23.1.13] [PMID]
- Hamerle M, Ghaeni L, Kowski A, Weissinger F, Holtkamp M. Alcohol use and alcohol-related seizures in patients with epilepsy. Front Neurol. 2018; 9:401. [DOI:10.3389/fneur.2018.00401] [PMID]
- Adem K, Kassew T, Birhanu A, Abate A. Sleep quality and associated factors among peoples with epilepsy who have a follow-up at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia, 2019: An institutional based cross-sectional study.Psychiatry J. 2020; 2020:1402712. [DOI:10.1155/2020/1402712] [PMID]
- Jones LA, Thomas RH. Sudden death in epilepsy: Insights from the last 25 years. Seizure. 2017; 44:232-6. [DOI:10.1016/j.seizure.2016.10.002] [PMID]
- Henok A, Lamaro T. Knowledge about and attitude towards epilepsy among Menit Community, Southwest Ethiopia. Ethiop J Health Sci. 2017; 27(1):47-58. [DOI:10.4314/ejhs.v27i1.7] [PMID]
- Kangevari MA, Kolahi AA, Farsar AR, Kermaniranjbar S. Public awareness, attitudes, and first-aid measures on epilepsy in Tehran. Iran J Child Neurol 2019; 13(1):91-106. [DOI:10.22037/ijcn.v13i1.21025 ]
- Eze CN, Ebuehi OM, Brigo F, Otte WM, Igwe SC. Effect of health education on trainee teachers’ knowledge, attitudes, and first aid management of epilepsy: An interventional study. Seizure. 2015; 33:46-53. [DOI:10.1016/j.seizure.2015.10.014] [PMID]
- Buelow J, Miller W, Fishman J. Development of an epilepsy nursing communication tool: Improving the quality of interactions between nurses and patients with seizures.J Neurosci Nurs. 2018; 50(2):74-80. [DOI:10.1097/JNN.0000000000000353] [PMID]
- Martin-Khan M, Varghese P, Wootton R, Gray L. Successes and failures in assessing cognitive function in older adults using video consultation. J Telemed Telecare. 2007; 13(3_suppl):60-2. [DOI:10.1258/135763307783247211]
- Hamid S, Malik AU, Kamran I, Ramzan M. Job satisfaction among nurses working in the private and public sectors: A qualitative study in tertiary care hospitals in Pakistan. J Multidiscip Healthc. 2013; 7:25-35. [DOI:10.2147/JMDH.S55077] [PMID]
- Shamsi A, Peyravi H. Nursing shortage, a different challenge in Iran: A systematic review. Med J Islam Repub Iran. 2020; 34:8. [DOI:10.47176/mjiri.34.8] [PMID]
- Chen CS, Chan SW, Chan MF, Yap SF, Wang W, Kowitlawakul Y. Nurses’ perceptions of psychosocial care and barriers to its provision: A qualitative study. J Nurs Res. 2017; 25(6):411-8. [DOI:10.1097/JNR.0000000000000185] [PMID]
- Zirwas MJ, Holder JL. Patient education strategies in dermatology: Part 2: Methods. J Clin Aesthet Dermatol. 2009; 2(12):28-34. [PMID]
- Lewinski AA, Shapiro A, Gierisch JM, Goldstein KM, Blalock DV, Luedke MW, et al. Barriers and facilitators to implementation of epilepsy self-management programs: A systematic review using qualitative evidence synthesis methods. Syst Rev. 2020; 9(1):92. [DOI:10.1186/s13643-020-01322-9] [PMID]
- Hu M, Zhang C, Xiao X, Guo J, Sun H. Effect of intensive self-management education on seizure frequency and quality of life in epilepsy patients with prodromes or precipitating factors. Seizure. 2020; 78:38-42. [DOI:10.1016/j.seizure.2020.03.003] [PMID]
- Yadegary MA, Dehghan-Naeyeri N, Ali-asgharpoor M, Naseh L. [The effect of educational program on drugs self-management in patient with epilepsy-A randomized clinical trial (Persian)]. J Clin Nurs Midwifery. 2013; 2(3):86-94. [Link]
- Hagemann A, Pfäfflin M, Nussbeck FW, May TW. The efficacy of an educational program for parents of children with epilepsy (FAMOSES): Results of a controlled multicenter evaluation study. Epilepsy Behav. 2016; 64(Pt A):143-51. [DOI:10.1016/j.yebeh.2016.09.027] [PMID]
- Pascual FT, Hoang K, Hollen C, Swearingen R, Hakimi AS, King JA, et al. Outpatient education reduces emergency room use by patients with epilepsy. Epilepsy Behav. 2015; 42:3-6. [DOI:10.1016/j.yebeh.2014.10.024] [PMID]
Article Type : Research |
Subject:
General
Received: 2023/01/13 | Accepted: 2023/05/22 | Published: 2024/01/1
Received: 2023/01/13 | Accepted: 2023/05/22 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |