Tue, Feb 3, 2026
Volume 34, Issue 1 (1-2024)
JHNM 2024, 34(1): 48-63 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azami-Aghdash S, Pournaghi-Azar F, Nouri M, Mohseni M, Aghaei M H. Effectiveness of Community-based Interventions in Improving the Oral & Dental Health of the Elderly People: A Systematic Review and Meta-analysis. JHNM 2024; 34 (1) :48-63
URL: http://hnmj.gums.ac.ir/article-1-2257-en.html
URL: http://hnmj.gums.ac.ir/article-1-2257-en.html
Saber Azami-Aghdash1 

 , Fatemeh Pournaghi-Azar2
, Fatemeh Pournaghi-Azar2 

 , Mahdi Nouri3
, Mahdi Nouri3 

 , Mohammad Mohseni4
, Mohammad Mohseni4 

 , Mir Hossein Aghaei *5
, Mir Hossein Aghaei *5 




 , Fatemeh Pournaghi-Azar2
, Fatemeh Pournaghi-Azar2 

 , Mahdi Nouri3
, Mahdi Nouri3 

 , Mohammad Mohseni4
, Mohammad Mohseni4 

 , Mir Hossein Aghaei *5
, Mir Hossein Aghaei *5 


1- Assistant Professor, Department of Health Policy, Research Center for Evidence Based Medicine (RCEBM), Tabriz University of Medical Sciences, Tabriz, Iran.
2- Associate Professor, Department of Restorative Dentistry, Research Center for Evidence Based Medicine (RCEBM), Tabriz University of Medical Sciences, Tabriz, Iran.
3- Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran.
4- Assistant Professor, Department of Health Policy,Social Determinants of Health Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
5- Assistant Professor, Department of Nursing, Institute of Health Education, Ardabil University of Medical Science, Ardabil, Iran. ,mirhosseinaghaei69@yahoo.com
2- Associate Professor, Department of Restorative Dentistry, Research Center for Evidence Based Medicine (RCEBM), Tabriz University of Medical Sciences, Tabriz, Iran.
3- Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran.
4- Assistant Professor, Department of Health Policy,Social Determinants of Health Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
5- Assistant Professor, Department of Nursing, Institute of Health Education, Ardabil University of Medical Science, Ardabil, Iran. ,
Keywords: Oral health, Community-based interventions, Elderly, Dental plaque, Denture plaque, Gingival
Full-Text [PDF 791 kb]
(645 Downloads)
| Abstract (HTML) (1238 Views)
Full-Text: (1001 Views)
Introduction
The evidence has shown the increase in the aged population that may result in the elderly population explosion in the upcoming years [1]. Currently, more than 600 million people in the world are over the age of 60. This number is estimated to reach more than one billion by 2020, and nearly 2 billion by 2050 [2, 3]. Elderly people are considered as vulnerable groups of the society due to being prone to chronic illnesses [4, 5]. One of the most important problems and concerns in the elderly is oral & dental health problems [6, 7]. Despite the increasing advances in the fight against diseases worldwide, the need to observe oral & dental health is felt more than ever [8, 9, 10]. One of the main criteria for community health is the assessment of oral & dental health [11, 12]. Dental caries and periodontal diseases are the most prevalent dental diseases [13-16]. More than 99% of the people suffer from these diseases and more than 50 hours are wasted due to problems caused by them [17].
Reduction in the number of teeth in the elderly negatively affects their ability to chew and choose the type of food they want, and can consequently cause nutritional deficiencies in them [18, 19]. In addition, it can affect their physical appearance, body image, self-confidence, and consequently the psychosocial function and the quality of life [20, 21]. Oral & dental health management is difficult for the elderly due to their illness and medication use [22]. In recent years, many community-based interventions have been designed and carried out based on different social and economic conditions to improve the oral & dental health of the elderly [23, 24]. Given that these interventions were designed and implemented in different ways and reported different results, their systematic review can be useful in designing and implementing more effective interventions. In this regard, this study aims to systematically review the community-based interventions for improving the oral & dental health of the elderly (>60 years).
Materials and Methods
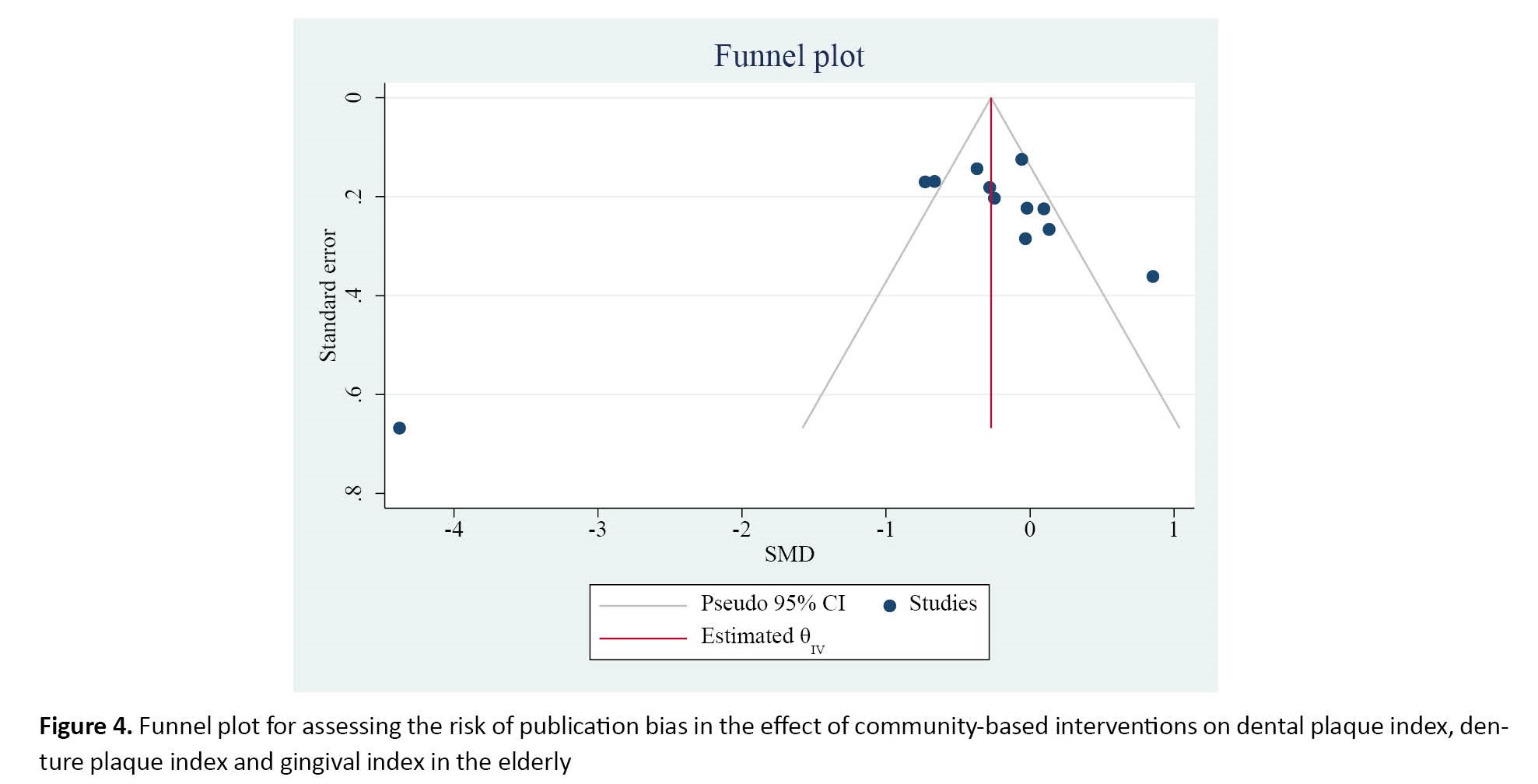
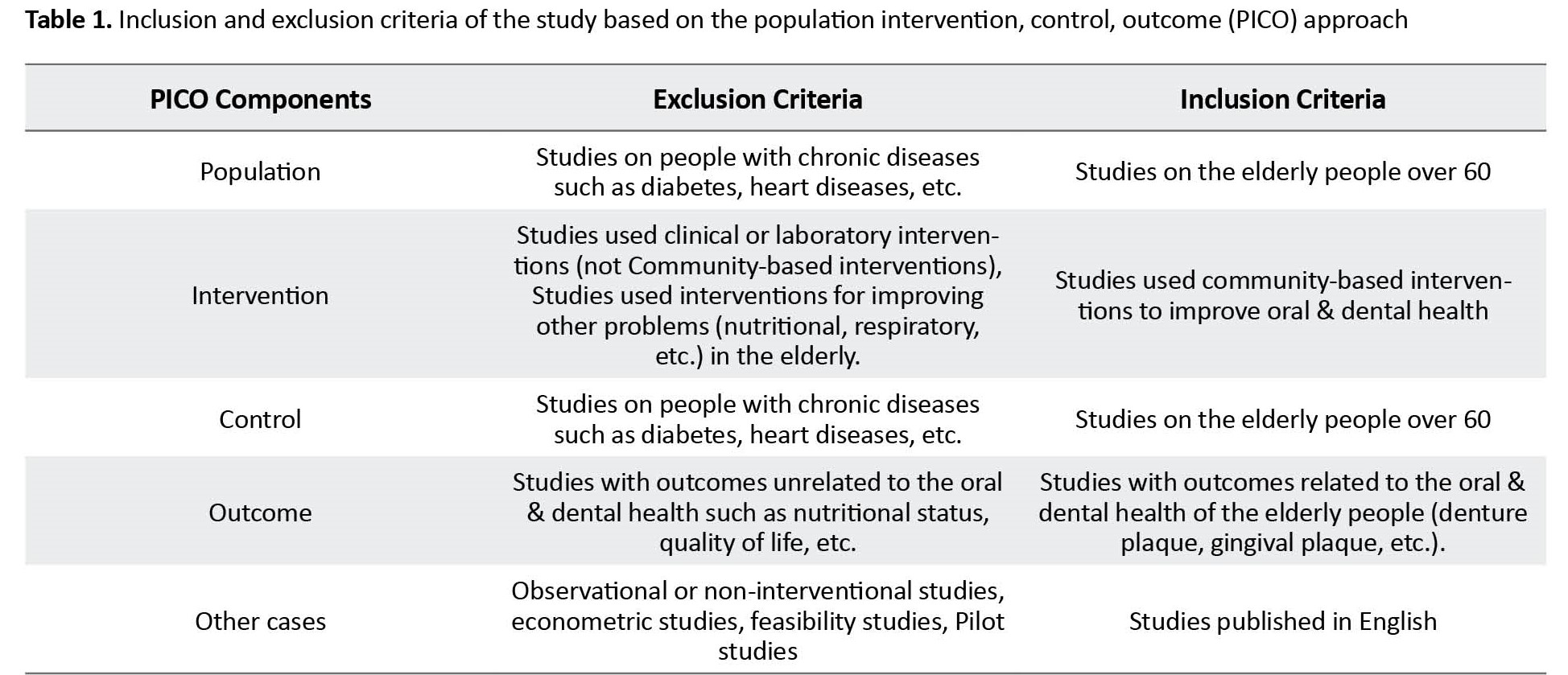
This is a systematic review, conducted in 2023 based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) approach [25]. The required information was collected by searching in PubMed, Scopus, Cochrane Oral Health’s Trials Register, and Web of Science databases using the related keywords based on the medical subject headlines (MeSh) terms. The search strategy was designed by a highly experienced medical librarian. The selected time period for the articles was from January 2000 to March 2023. To identify and cover more published articles, a search in a number of reputable journals found from the Scientific Journal Rankings-SCImago System [26] was also conducted manually. After excluding irrelevant articles, the related articles were selected and their references were examined manually to find more related articles. To examine the grey literature, a search in the databases such as the European Association for Grey Literature Exploitation (EAGLE) and the Healthcare Management Information Consortium (HMIC) was also conducted. Table 1 presents the inclusion and exclusion criteria based on the population, intervention, control, and outcomes (PICO) approach.
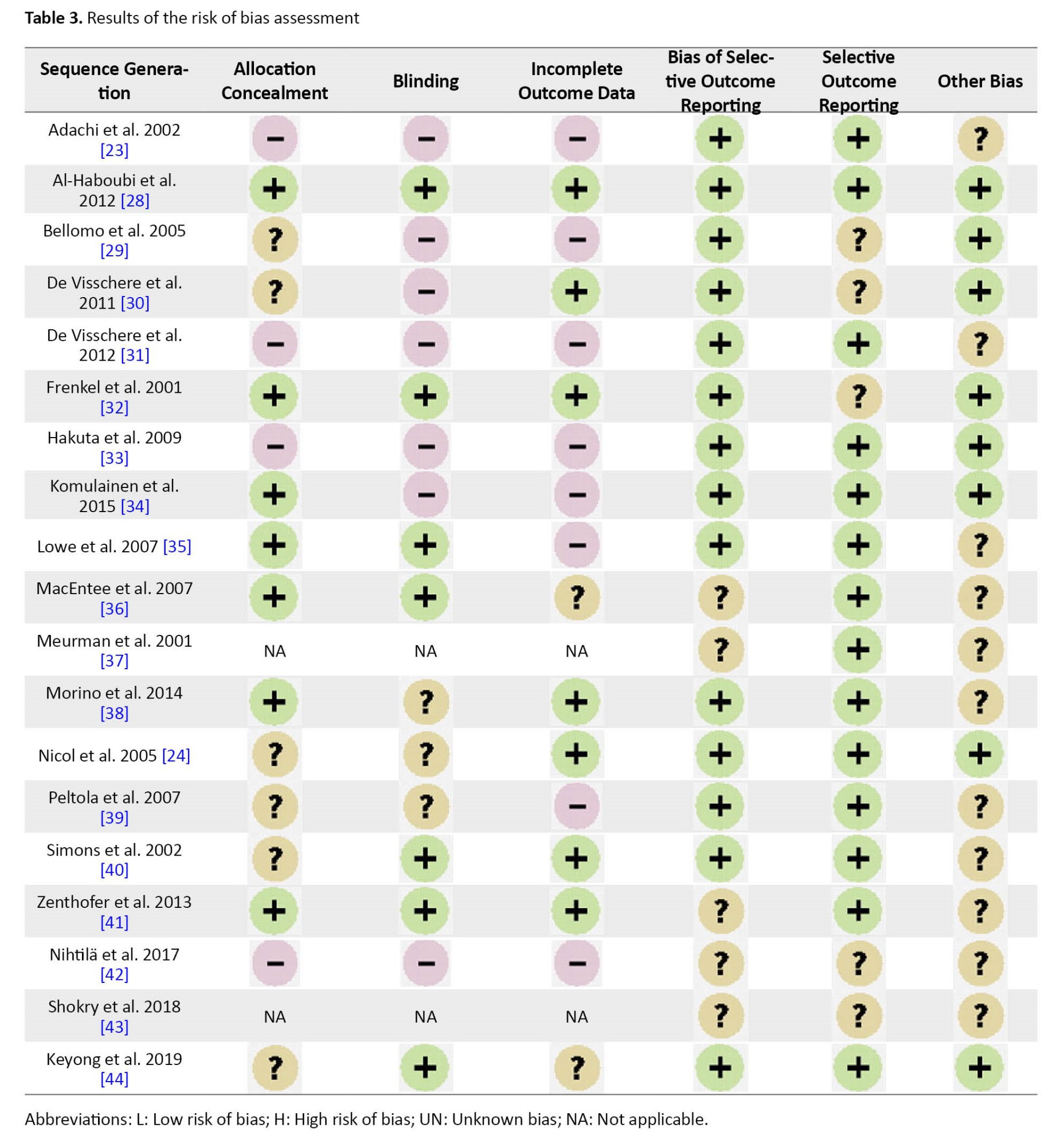
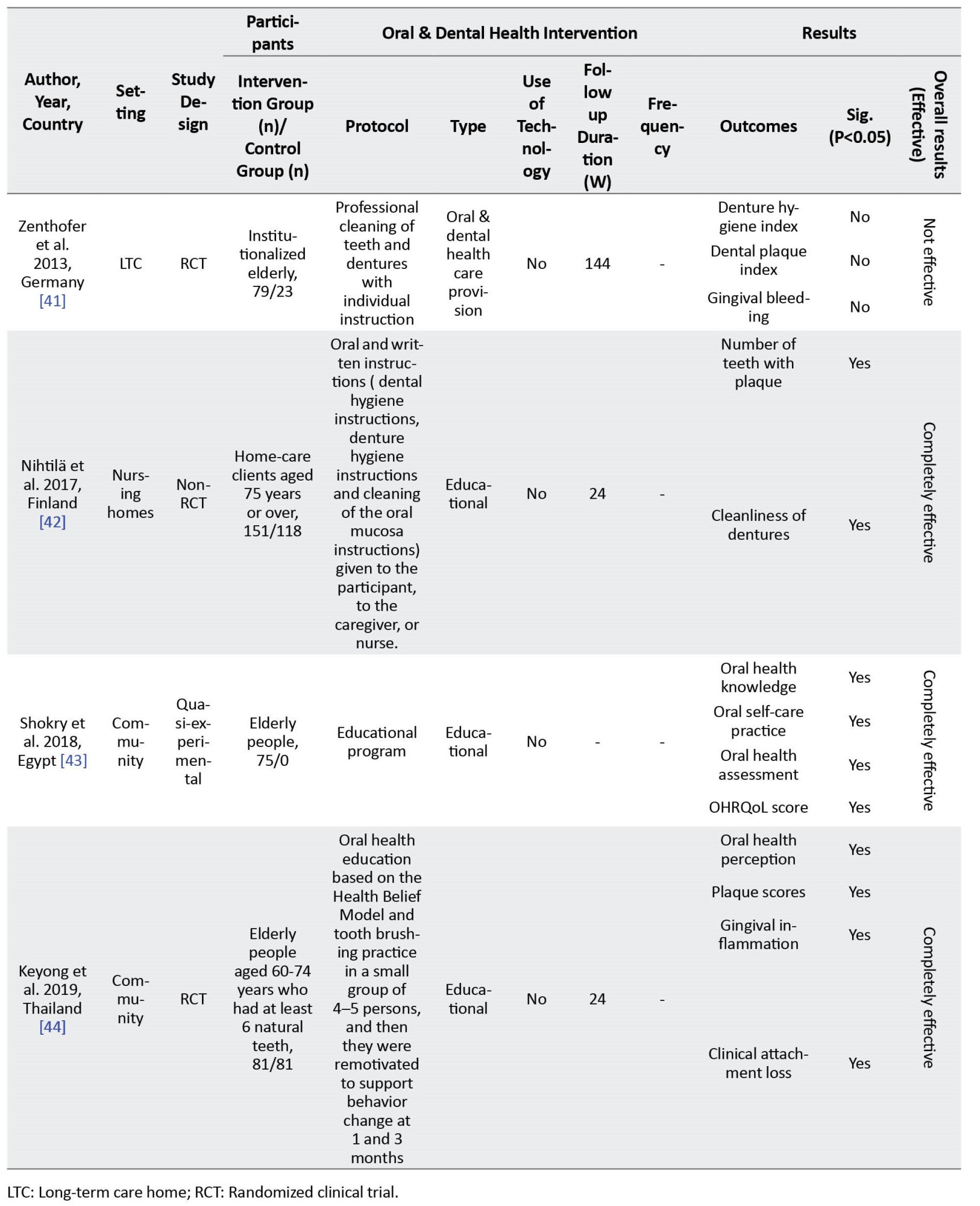
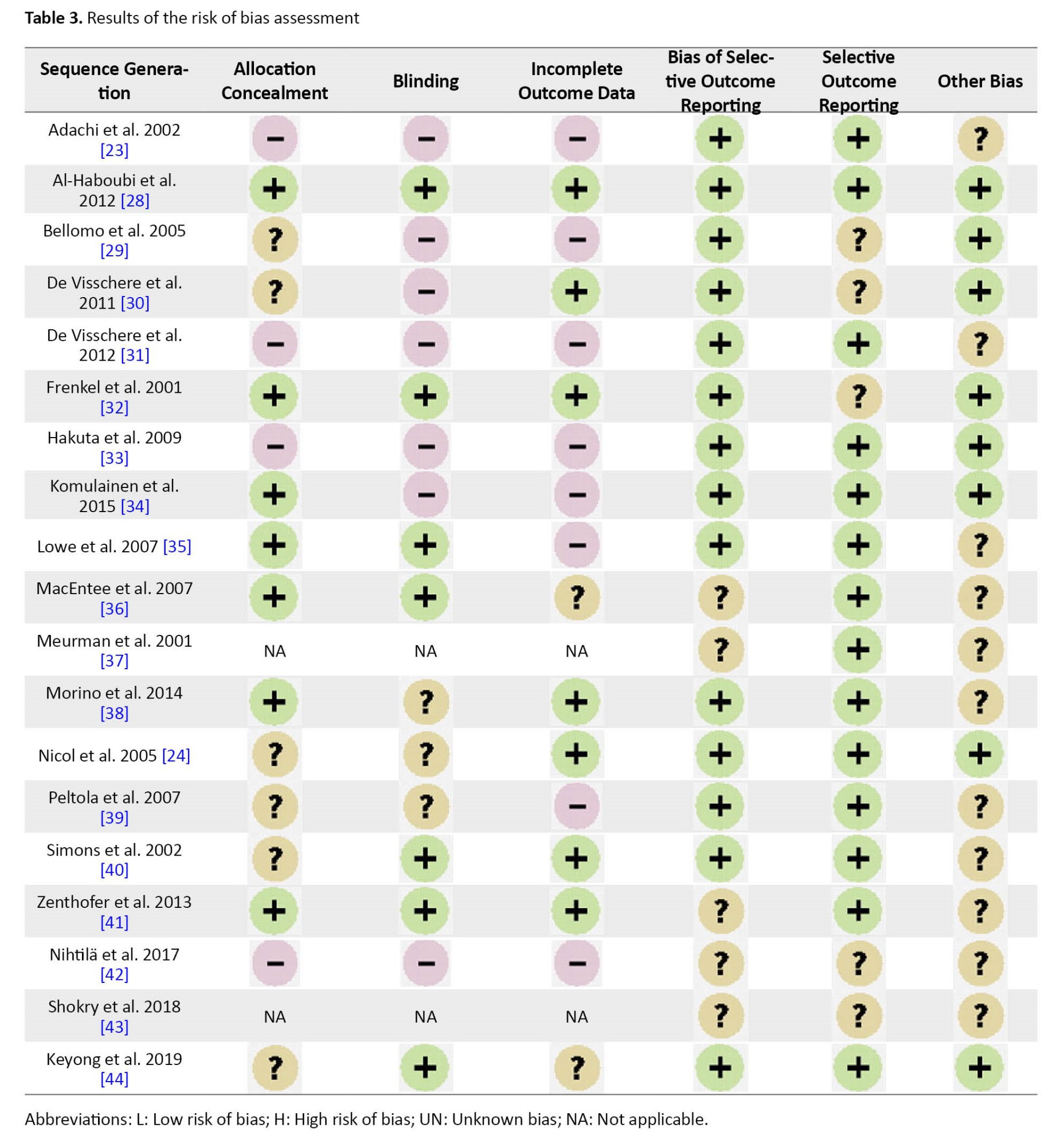
The risk of bias in the included studies was assessed by two authors using the Cochrane checklist [27]. This tool covers six dimensions of bias: Selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Based on the results, the risk of bias is categorized as: Low risk of bias, high risk of bias, and unclear or unknown bias. The disagreement between the two authors were resolved by referring to the third author.
To extract data, two forms (one for the general characteristics of the articles and the other for the information and the results of the interventions) were designed in the Microsoft Word 2016 software. As a trial, these forms were used to collect the data of three papers and, thus, the existing deficiencies in the initial forms were found and resolved. Then, the data was extracted by two authors separately from the selected articles. The data included items as author’s surname, publication year, study country, study area, study design, participants, and sample size.
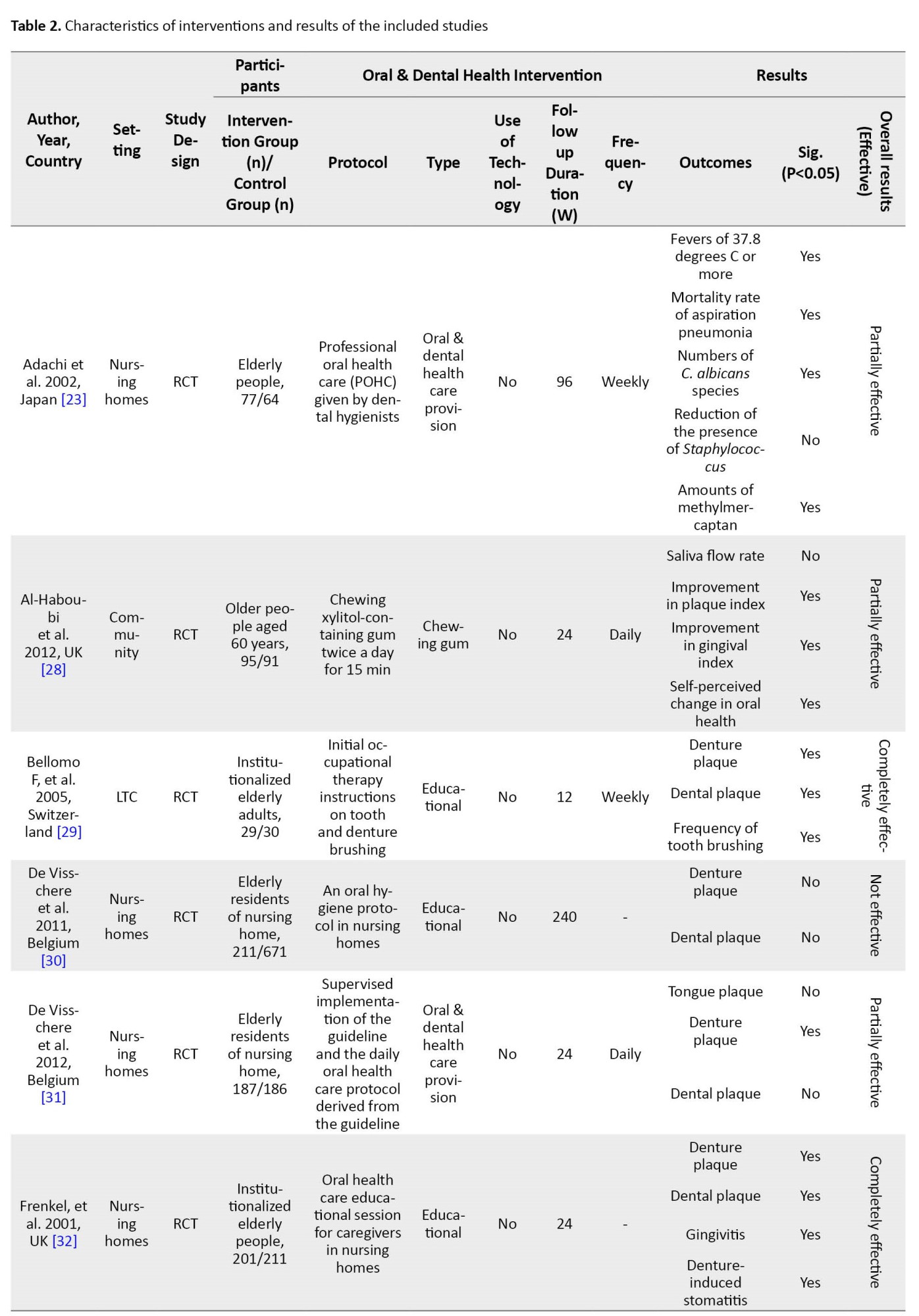
To calculate the mean difference among the indices such as denture plaque and gingival plaque, between the interventions, and between the study groups, a meta-analysis was conducted in StataCorp software, version 16. To report the results, funnel plots were used where the size of each square represents the sample size and the lines represent the confidence interval (95% CI) for each study. To evaluate heterogeneity of the results, Q statistic and I2 index were used. In this study, I2 higher than 50% was determined to be the criterion of heterogeneity. Funnel plot and Egger’s regression test were used at a significance level of 0.01 to measure publication bias. Other collected data were analyzed and reported manually using descriptive statistics (percentage, frequency, mean).
Results
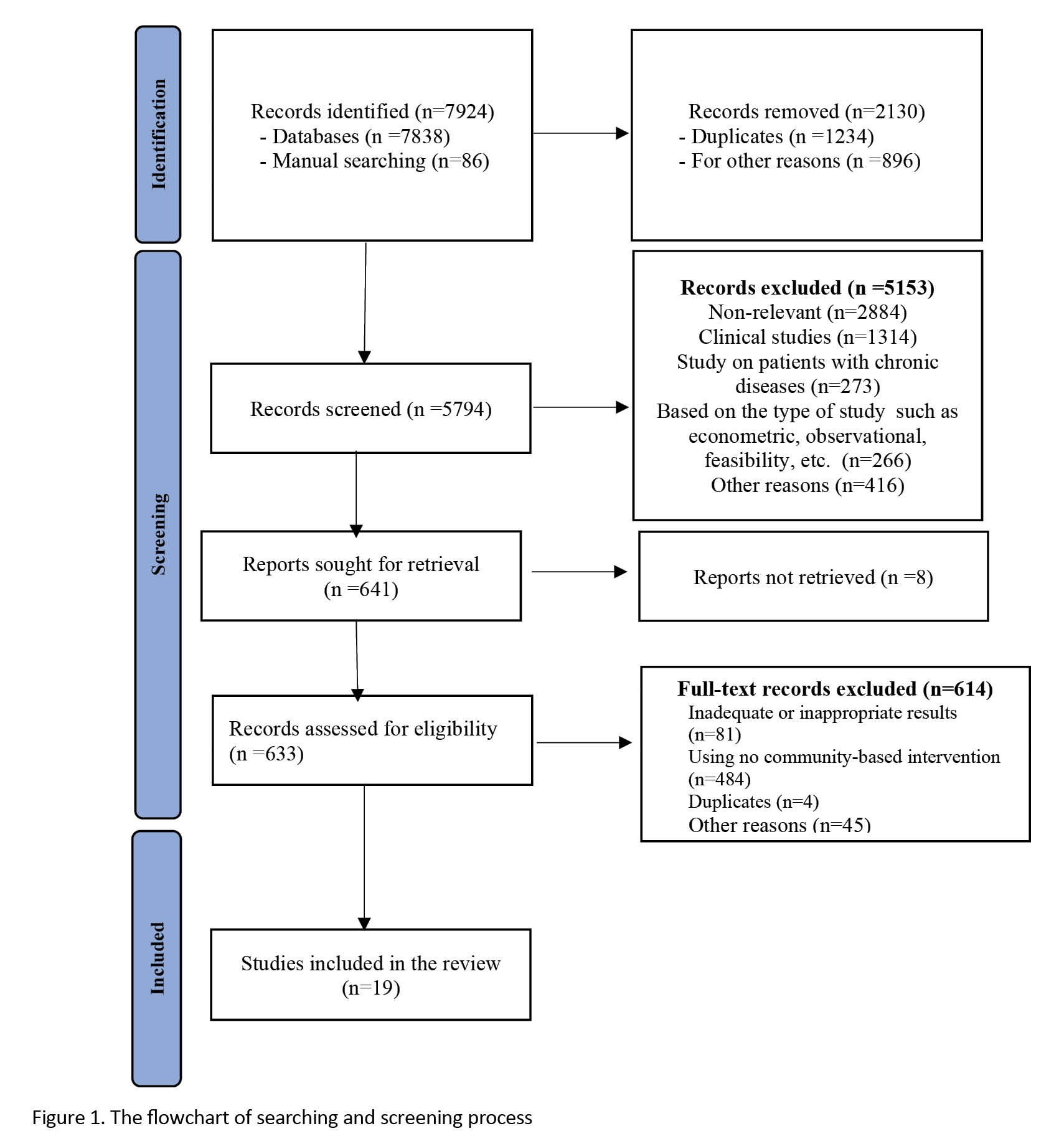
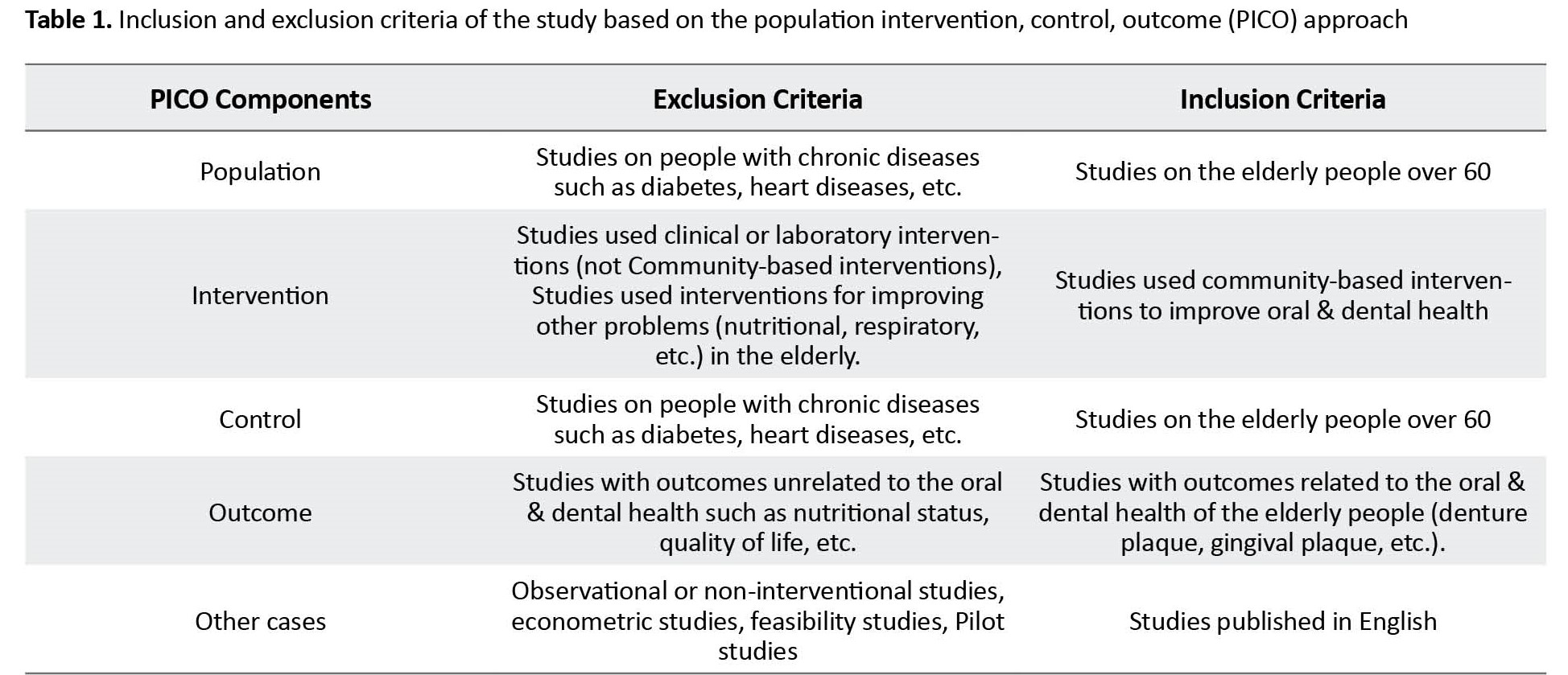
Of 7924 articles found, 2130 were excluded due to being irrelevant. After reading the titles and abstracts, 5794 items were excluded due to not meeting inclusion criteria. After reading the full texts, 614 articles were also excluded. Finally, 19 articles papers were selected for the review (Figure 1). Their information is presented in Table 2.
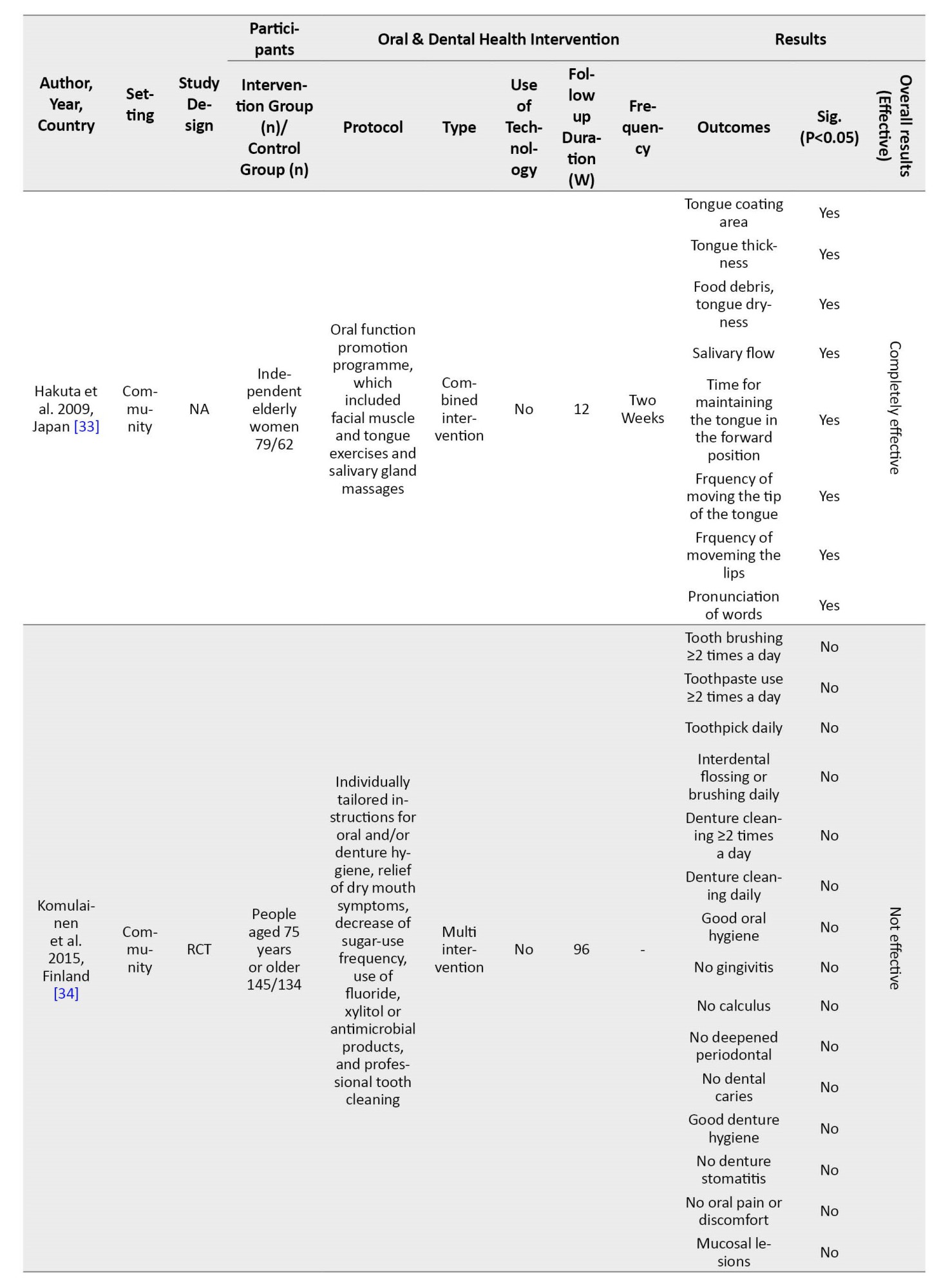
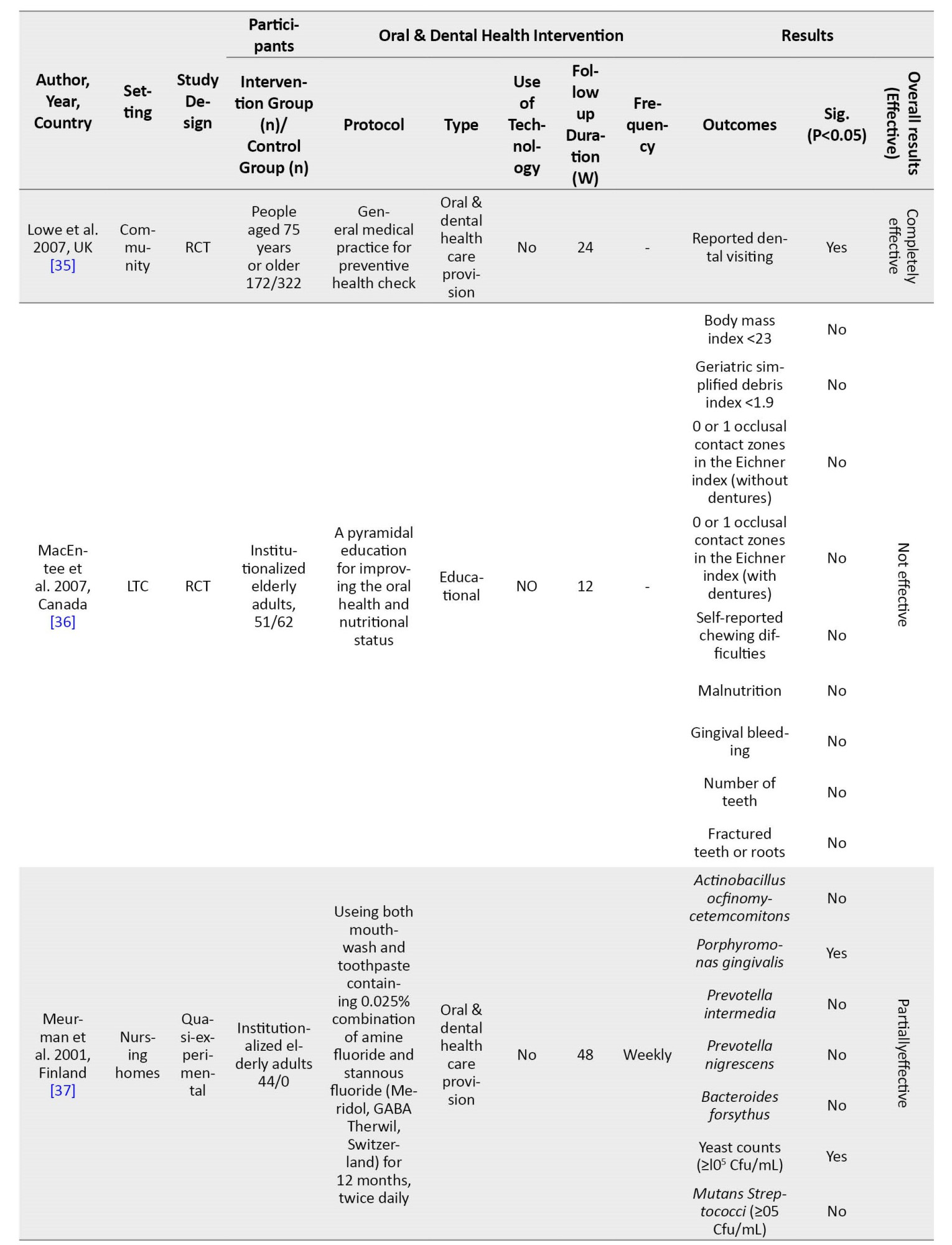
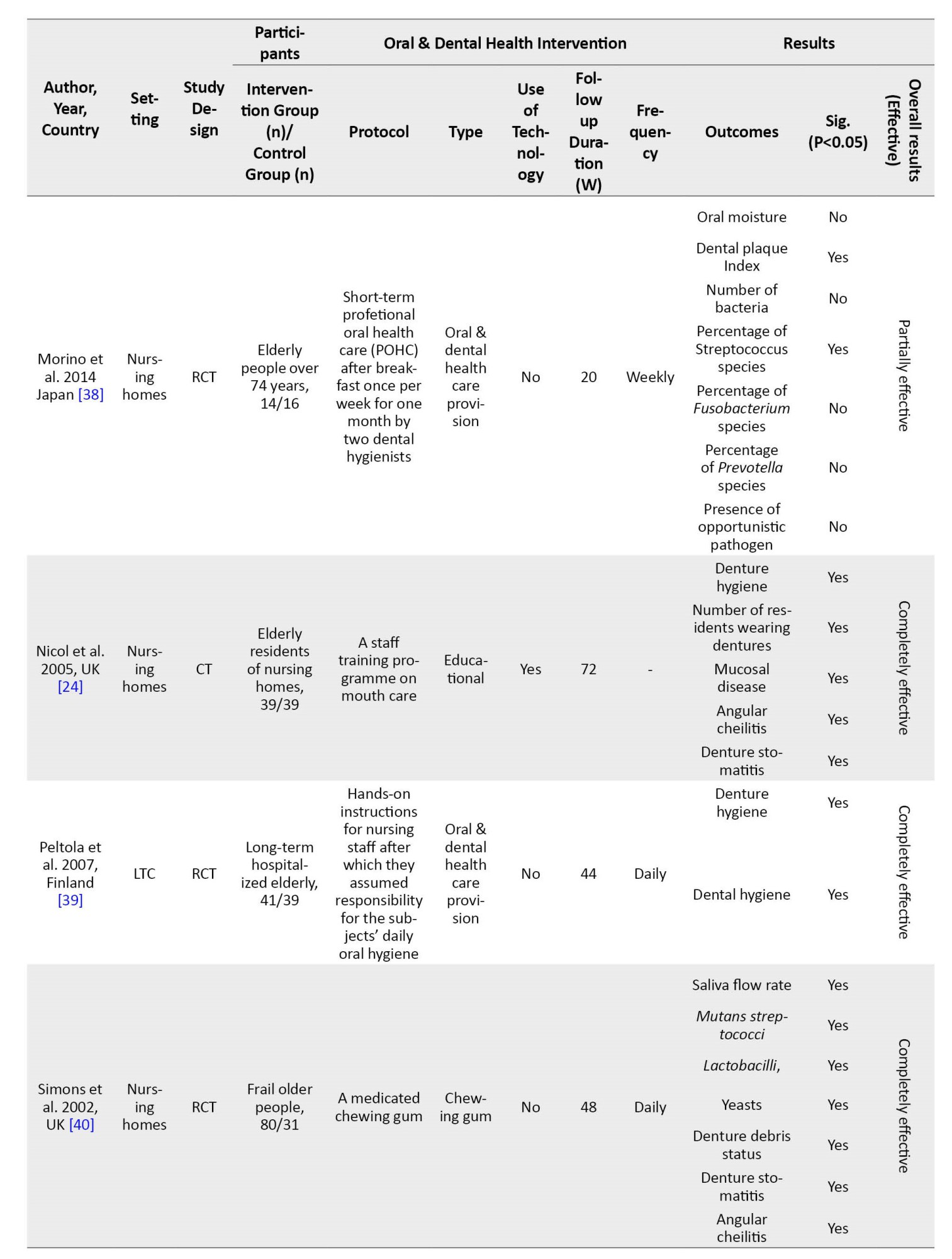
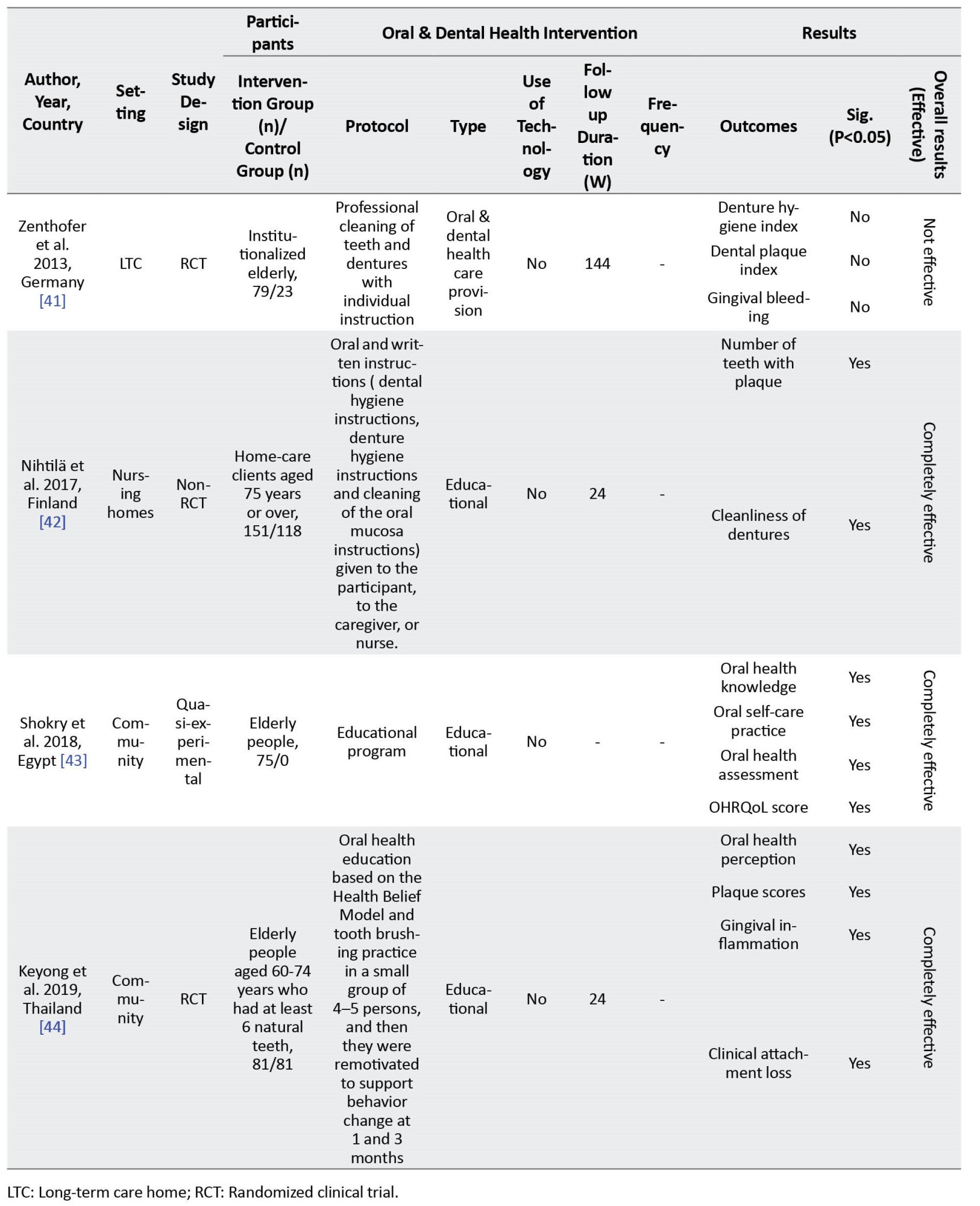
In these studies, there were 1851 samples in the intervention groups and 2255 in the control group.
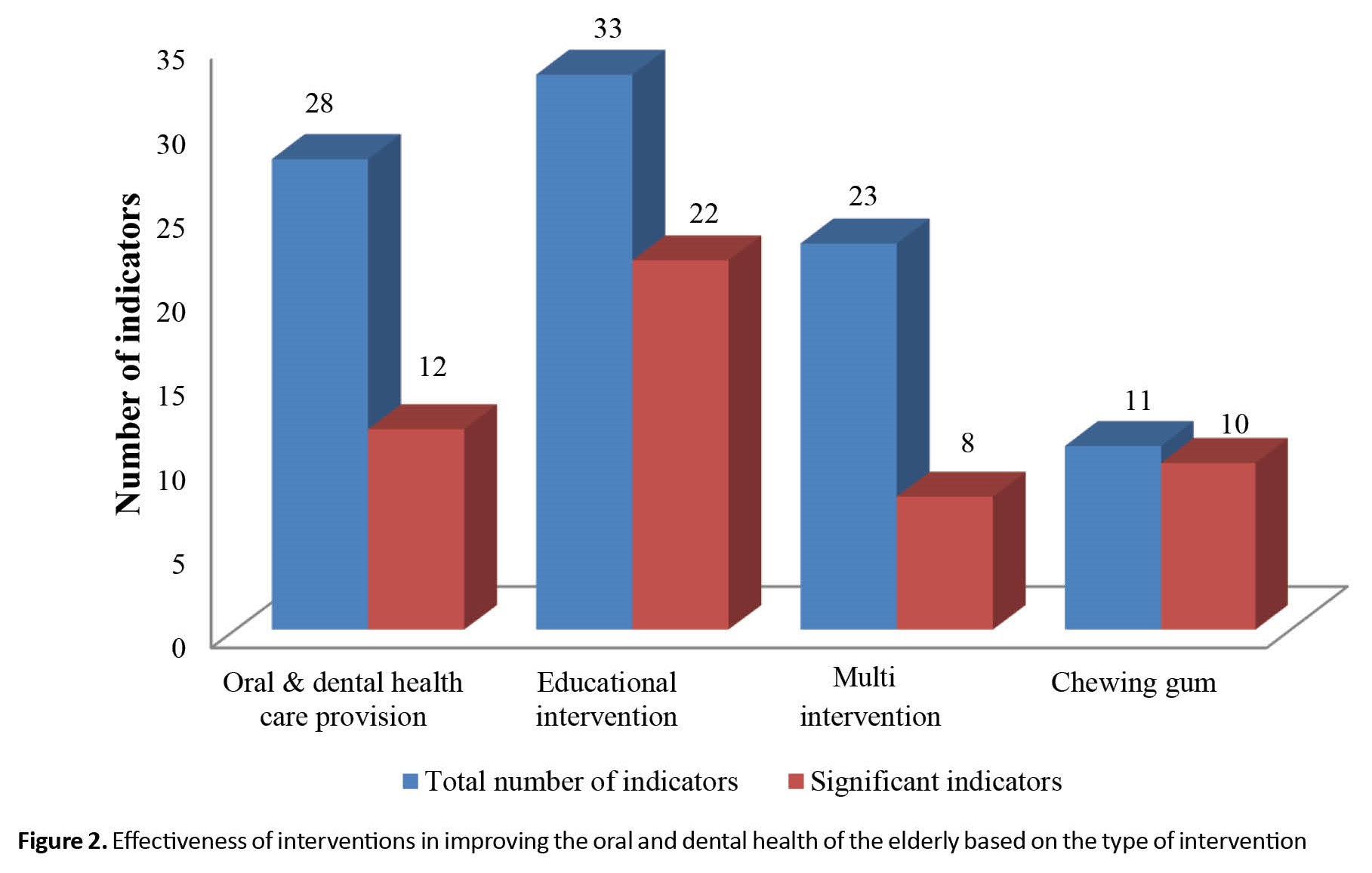
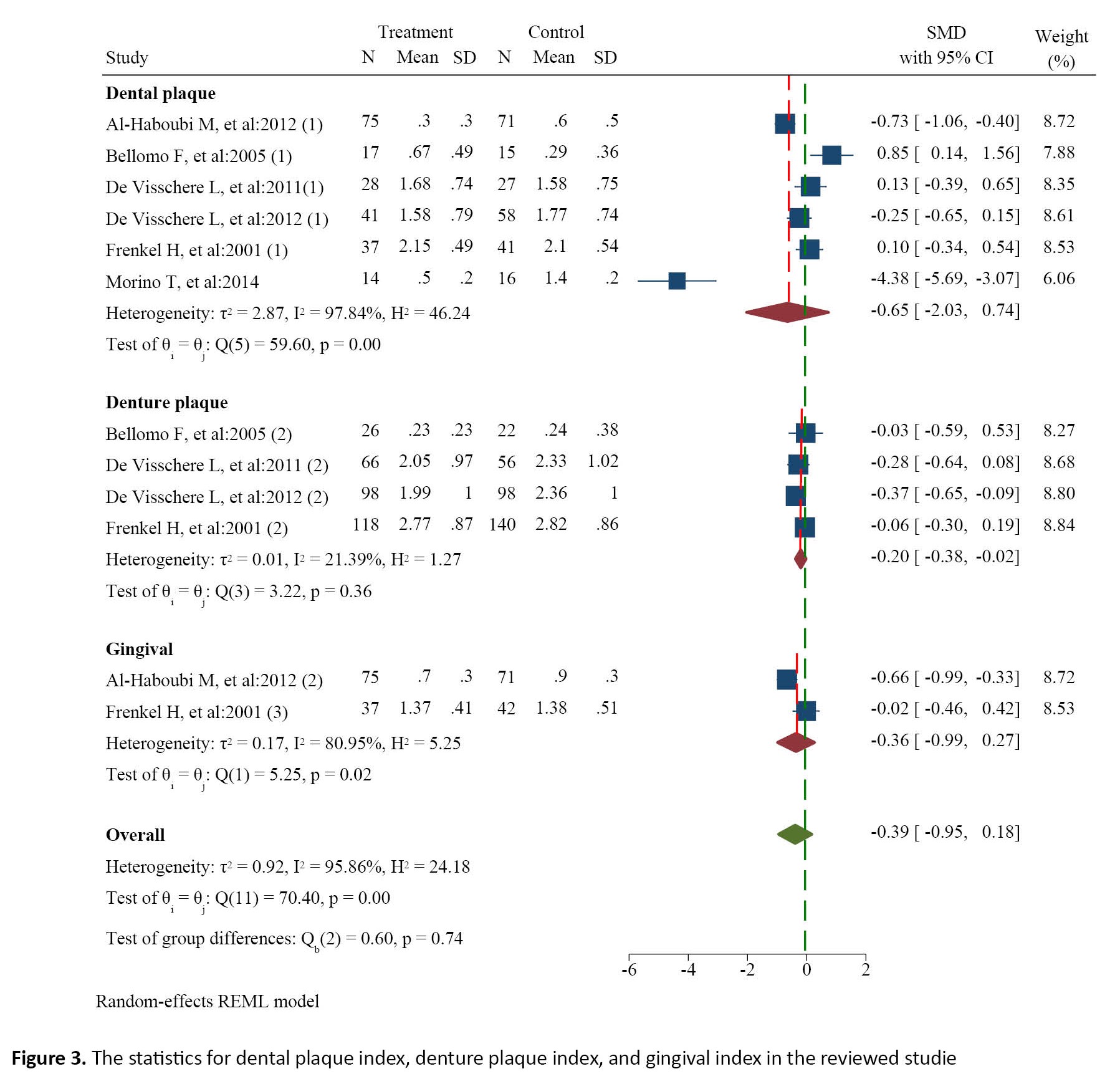
In 19 studies, a total of 95 indicators were measured and reported, of which 53 were reported to be statistically non-significant. Regarding overall effectiveness of the interventions, 10 studies reported them as completely effective (all indicators were statistically significant), 5 studies reported as relatively effective (some indicators were statistically significant) and 4 reported as ineffective (None of the indicators was statistically significant). Regarding the effectiveness based on the type of intervention, the studies showed that chewing gum interventions had the highest effectiveness (90%) and the combined interventions had the lowest effectiveness (34.7%). Furthermore, educational interventions were effective by about 68.0% and the interventions for oral & health care provision were 42.8% effective (Figure 2). Among the indices reported in the studies, the dental plaque index, denture plaque index, and gingival index were reported in different studies. The results of the meta-analysis (Figure 3) showed that the mean difference in the dental plaque index between the intervention and control groups was -0.65 (95% CI; -2.03%, 0.74%; Q=59.6, df=5, P=0.001, I2=97.8%); the mean difference in the denture plaque index was -0.20 (95% CI; -0.38%, -0.02%; Q=3.22, df=3, P=0.36, I2=21.3%) and the mean difference in the gingival index was -0.36 (95% CI; -0.99%, 0.27%; Q=5.2, df=1, P=0.02, I2=80.9%). Based on the mean differences, the difference in the mean scores of denture plaque index and gingival index between the two groups was moderately significant. The results of measuring the risk of publication bias (Figure 4) showed a high risk of bias (z=-2.79, Prob > |z|=0.0053). In assessing the risk of bias in 19 studies, 7 articles had a high risk of bias, 6 articles had a low risk of bias, and 6 has unknown bias (Table 3).
Discussion
The majority of the reviewed studies reported the interventions as completely effective, where chewing gum had the highest effectiveness and the combined interventions had the lowest efficacy. In the studies, the mean difference in the denture plaque index and gingival index was mildly significant between the intervention and control groups. In general, the results of our study indicate that the community-based interventions that have been used to improve the oral & dental health of the elderly do not have a good effectiveness. One of the important reasons can be related to the study areas. As most studies were conducted in nursing homes and long-term care centers, the poor quality of care, psychological problems, and attitudes of the elderly living in these centers can affect the final results [45-47]. Therefore, along with interventions related to oral & dental health in the elderly, it is recommended to pay attention to other concerns of the elderly in these centers. Due to the strong correlation between oral & dental health and other problems in the elderly, it is recommended to conduct multidisciplinary interventions. Also, comprehensive and integrated services with high quality should be provided for the elderly in nursing homes and long-term care centers.
The results of the review showed that chewing gum was the most effective intervention. Various studies in other age groups which examined the effect of chewing gum on the oral & dental hygiene have also shown the high effectiveness of these interventions and have recommended to chew sugar free gums [48-52]. According to these studies, the most important mechanisms of chewing gum can be reduced dental plaque, reduced streptococcus mutans of saliva, reduced production of salivary acid, and increased salivary and mechanical cleansing properties of the chewing gum [53-55].
The results also showed the educational interventions had a moderate effectiveness. Albrecht also did not show the effectiveness of educational interventions [56]. However, most of the educational interventions for lower ages, especially school-based interventions, have been reported to have a relatively good efficacy [57-60]. One of the probable reasons for lower effectiveness of educational interventions for the elderly can be the aging and physiological issues that reduce the learning ability. Educational practices used in the studies can be effective, since most of the educational interventions are usually short-term and traditional, using inefficient methods. One of the educational models that can be recommended in this field is the Health Belief Model. The effectiveness of this educational model in improving oral & dental health has been reported [61-63].
Most of the reviewed studies were conducted in developed countries. It does not mean that no community-based interventions for the oral health of the elderly have been conducted in middle-income and low-income countries; however, it can indicate that, due to their poor performance and reporting, they could not be published. It should be noted that, due to the existing socioeconomic and cultural differences and the different quality of the interventions, their implementation, regardless of the local conditions of each country, will not be effective and will be a waste of resources [64, 65]. Another reason that may explain the high number of studies on the oral health of the elderly in developed countries can be the higher importance of aging in these countries or paying more attention to the health of elderly people [66]. Due to the fact that the aged population in middle-income and lower-income countries is growing, their low attention will increase the burden on health systems of these countries in the near future [67]. Hence, more attention is now being paid to the health of the elderly, especially their oral health [68-70].
A variety of electronical/technological methods (e-mail, internet, designed programs, software) had been used for the oral health of the elderly. The studies using a variety of such technologies have reported a higher efficacy [71, 72]. Recently, the use of technological methods to improve the health of people in other areas has been increased [73-76]. These advancements can be used to design and implement the interventions for the oral health of the elderly. The articles did not have a good status in the risk of bias assessment. The most important problem was related to blinding and allocating individuals to intervention and control groups. Given that most studies had been conducted in nursing homes and long-term care centers, and since the elderly are in contact with each another in these centers, it is likely that the interventions will also have an impact on the control groups, and this can alter the results of the interventions. Therefore, it is recommended that researchers perform interventions in the future studies with more blinding. In this regard, the use of guidelines for conducting interventional studies and reporting their results [77-80] can be effective.
One of the main limitations of the present study was the low generalizability of the results. The main reason is that the reviewed studies were conducted in several high-income countries which limits the generalizability of the results to middle-income and lower-income countries. In addition, due to the high number of oral health indicators and their different method of outcome reporting, meta-analysis was not possible to be done for the most of indicators. Regarding the high costs of dental care and lack of resources in the health system of middle-income and lower-income countries, their health system and people prefer cost-effectiveness interventions. Most of the reviewed studies focused on surrogate endpoints indicators such as saliva flow, bacterial counts, etc. Although these indicators are important, it is recommended that future studies focus more on clinical indicators or clinically significant endpoints such as tooth loss, pain, quality of life, and dentine caries. Also, according to the literature review and to our best knowledge, economic cost-effective studies in the field of oral health of the elderly are limited.
Based on the results of the study, it can be concluded that the community-based interventions for improving the oral & dental health of the elderly do not have a good efficacy. Given the rapid increase in the number of elderly people in the world and their wide oral hygiene problems, there is an increasing need for more effective interventions and planning. Chewing sugar free gums and holding effective and long-term training courses aimed at changing the behavior of the elderly are recommended. In addition, due to the weaknesses in the methodology and outcome reporting in the reviewed studies, it is recommended to use the available guidelines for carrying out the interventions and reporting their outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.REC.1398.674).
Funding
This study was funded by Tabriz University of Medical Sciences.
Authors' contributions
Investigation and drafting the manuscript: Mir Hossein Aghaei, Fatemeh Pournaghi-Azar, and Saber Azami-Aghdash; Data acquisition and data analysis: Fatemeh Pournaghi-Azar, Mohammad Mohseni and Mahdi Nouri; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to the Deputy for Research and Technology of Tabriz University of Medical Sciences.
References
The evidence has shown the increase in the aged population that may result in the elderly population explosion in the upcoming years [1]. Currently, more than 600 million people in the world are over the age of 60. This number is estimated to reach more than one billion by 2020, and nearly 2 billion by 2050 [2, 3]. Elderly people are considered as vulnerable groups of the society due to being prone to chronic illnesses [4, 5]. One of the most important problems and concerns in the elderly is oral & dental health problems [6, 7]. Despite the increasing advances in the fight against diseases worldwide, the need to observe oral & dental health is felt more than ever [8, 9, 10]. One of the main criteria for community health is the assessment of oral & dental health [11, 12]. Dental caries and periodontal diseases are the most prevalent dental diseases [13-16]. More than 99% of the people suffer from these diseases and more than 50 hours are wasted due to problems caused by them [17].
Reduction in the number of teeth in the elderly negatively affects their ability to chew and choose the type of food they want, and can consequently cause nutritional deficiencies in them [18, 19]. In addition, it can affect their physical appearance, body image, self-confidence, and consequently the psychosocial function and the quality of life [20, 21]. Oral & dental health management is difficult for the elderly due to their illness and medication use [22]. In recent years, many community-based interventions have been designed and carried out based on different social and economic conditions to improve the oral & dental health of the elderly [23, 24]. Given that these interventions were designed and implemented in different ways and reported different results, their systematic review can be useful in designing and implementing more effective interventions. In this regard, this study aims to systematically review the community-based interventions for improving the oral & dental health of the elderly (>60 years).
Materials and Methods
This is a systematic review, conducted in 2023 based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) approach [25]. The required information was collected by searching in PubMed, Scopus, Cochrane Oral Health’s Trials Register, and Web of Science databases using the related keywords based on the medical subject headlines (MeSh) terms. The search strategy was designed by a highly experienced medical librarian. The selected time period for the articles was from January 2000 to March 2023. To identify and cover more published articles, a search in a number of reputable journals found from the Scientific Journal Rankings-SCImago System [26] was also conducted manually. After excluding irrelevant articles, the related articles were selected and their references were examined manually to find more related articles. To examine the grey literature, a search in the databases such as the European Association for Grey Literature Exploitation (EAGLE) and the Healthcare Management Information Consortium (HMIC) was also conducted. Table 1 presents the inclusion and exclusion criteria based on the population, intervention, control, and outcomes (PICO) approach.
The risk of bias in the included studies was assessed by two authors using the Cochrane checklist [27]. This tool covers six dimensions of bias: Selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Based on the results, the risk of bias is categorized as: Low risk of bias, high risk of bias, and unclear or unknown bias. The disagreement between the two authors were resolved by referring to the third author.
To extract data, two forms (one for the general characteristics of the articles and the other for the information and the results of the interventions) were designed in the Microsoft Word 2016 software. As a trial, these forms were used to collect the data of three papers and, thus, the existing deficiencies in the initial forms were found and resolved. Then, the data was extracted by two authors separately from the selected articles. The data included items as author’s surname, publication year, study country, study area, study design, participants, and sample size.
To calculate the mean difference among the indices such as denture plaque and gingival plaque, between the interventions, and between the study groups, a meta-analysis was conducted in StataCorp software, version 16. To report the results, funnel plots were used where the size of each square represents the sample size and the lines represent the confidence interval (95% CI) for each study. To evaluate heterogeneity of the results, Q statistic and I2 index were used. In this study, I2 higher than 50% was determined to be the criterion of heterogeneity. Funnel plot and Egger’s regression test were used at a significance level of 0.01 to measure publication bias. Other collected data were analyzed and reported manually using descriptive statistics (percentage, frequency, mean).
Results
Of 7924 articles found, 2130 were excluded due to being irrelevant. After reading the titles and abstracts, 5794 items were excluded due to not meeting inclusion criteria. After reading the full texts, 614 articles were also excluded. Finally, 19 articles papers were selected for the review (Figure 1). Their information is presented in Table 2.
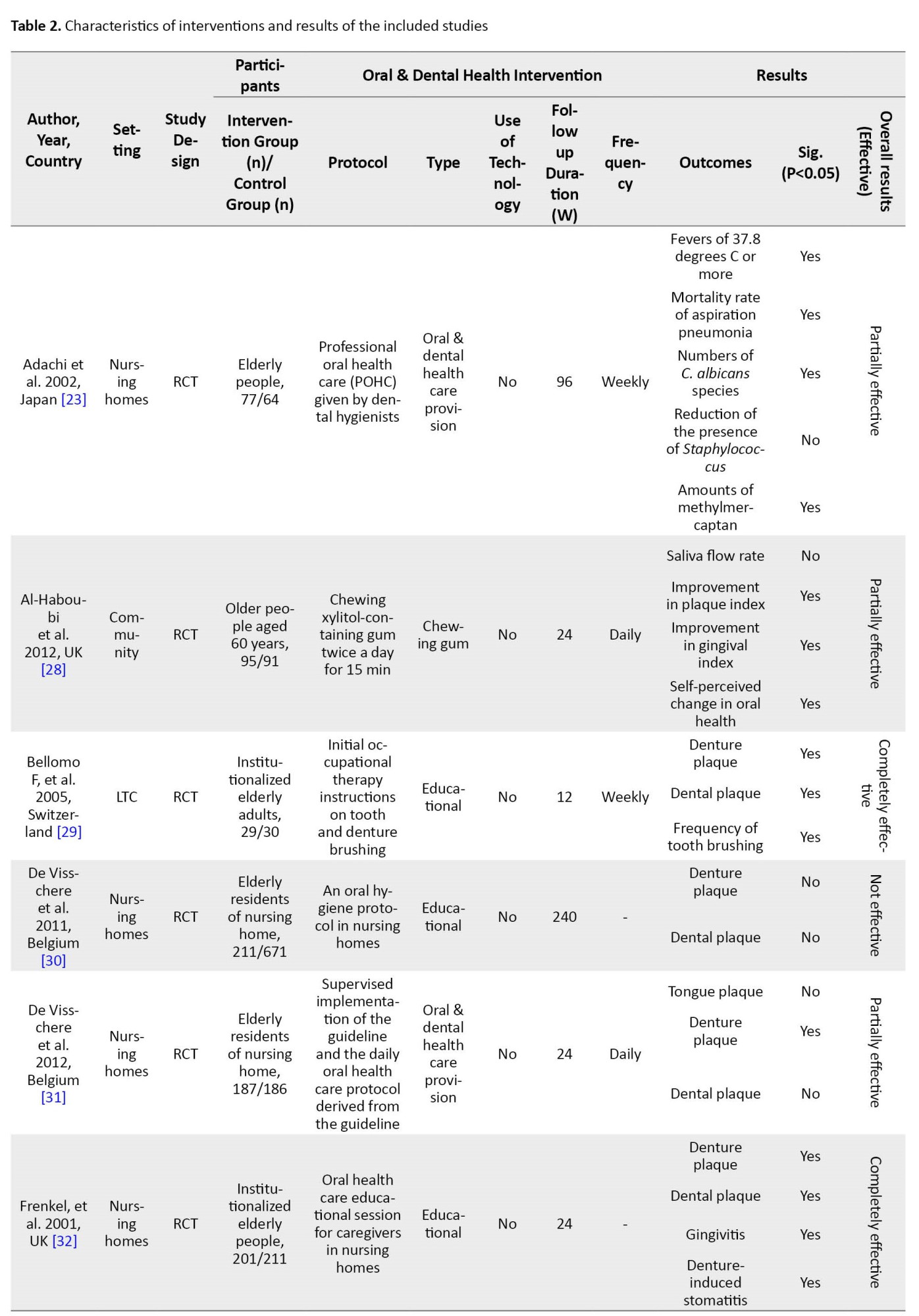
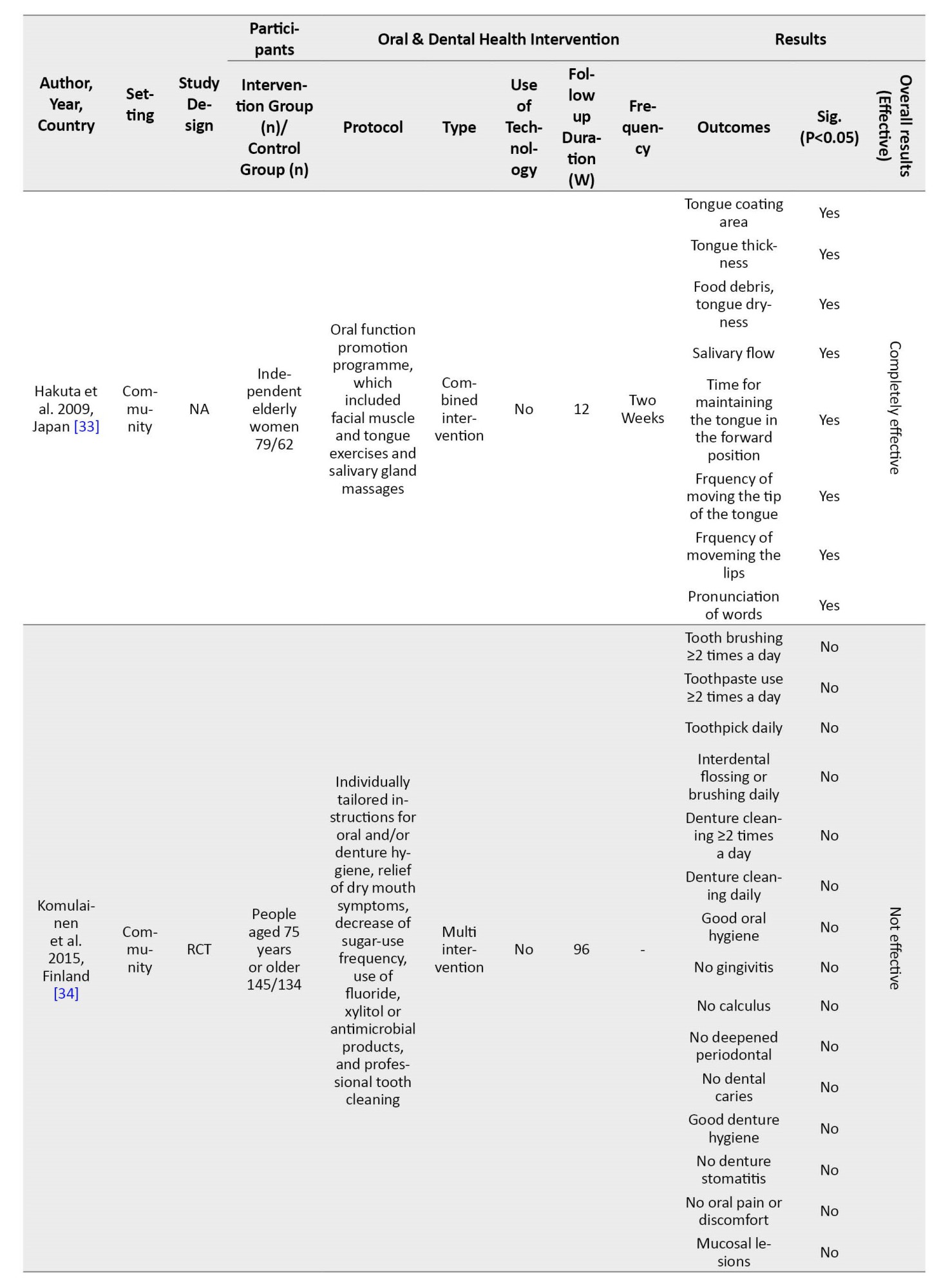
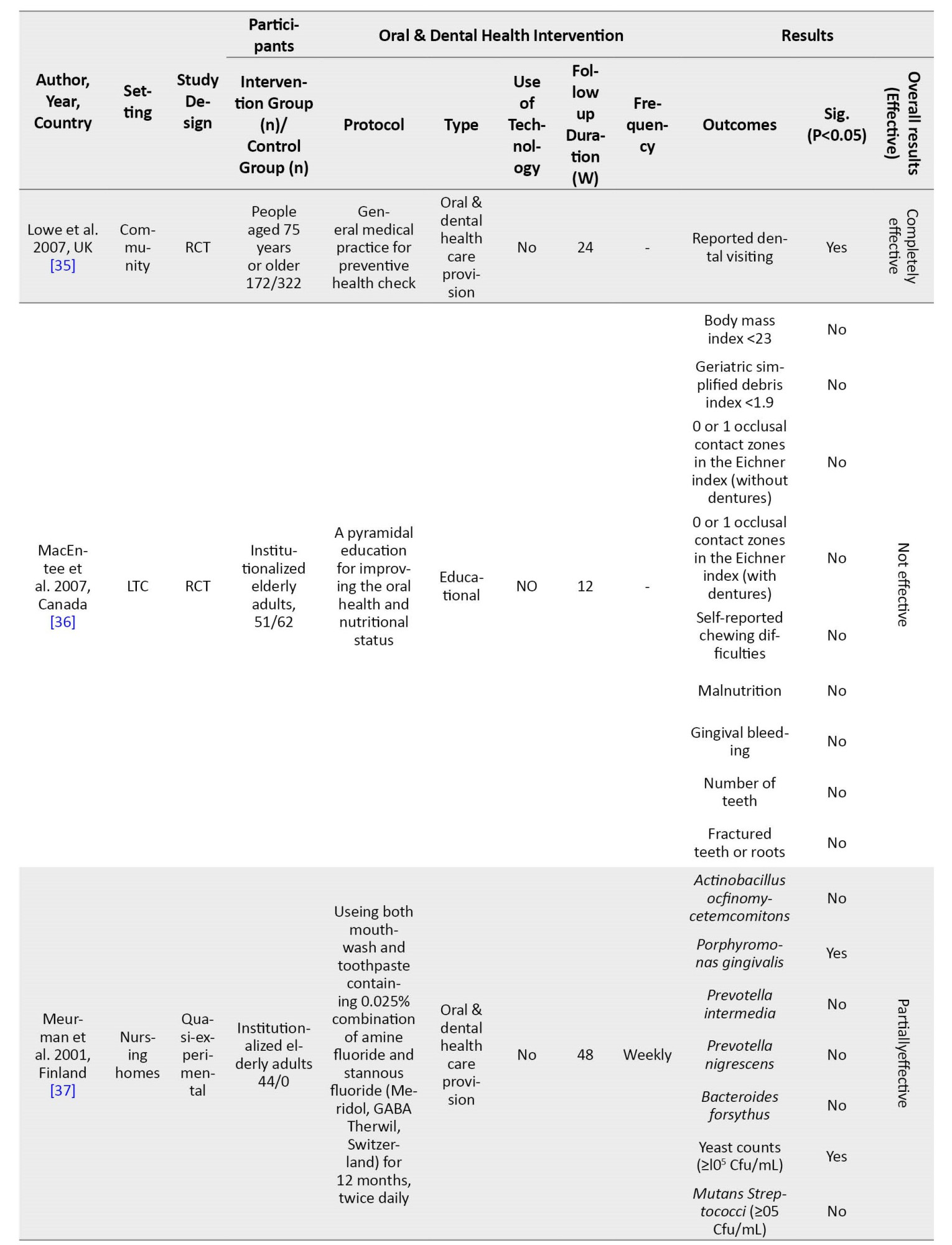
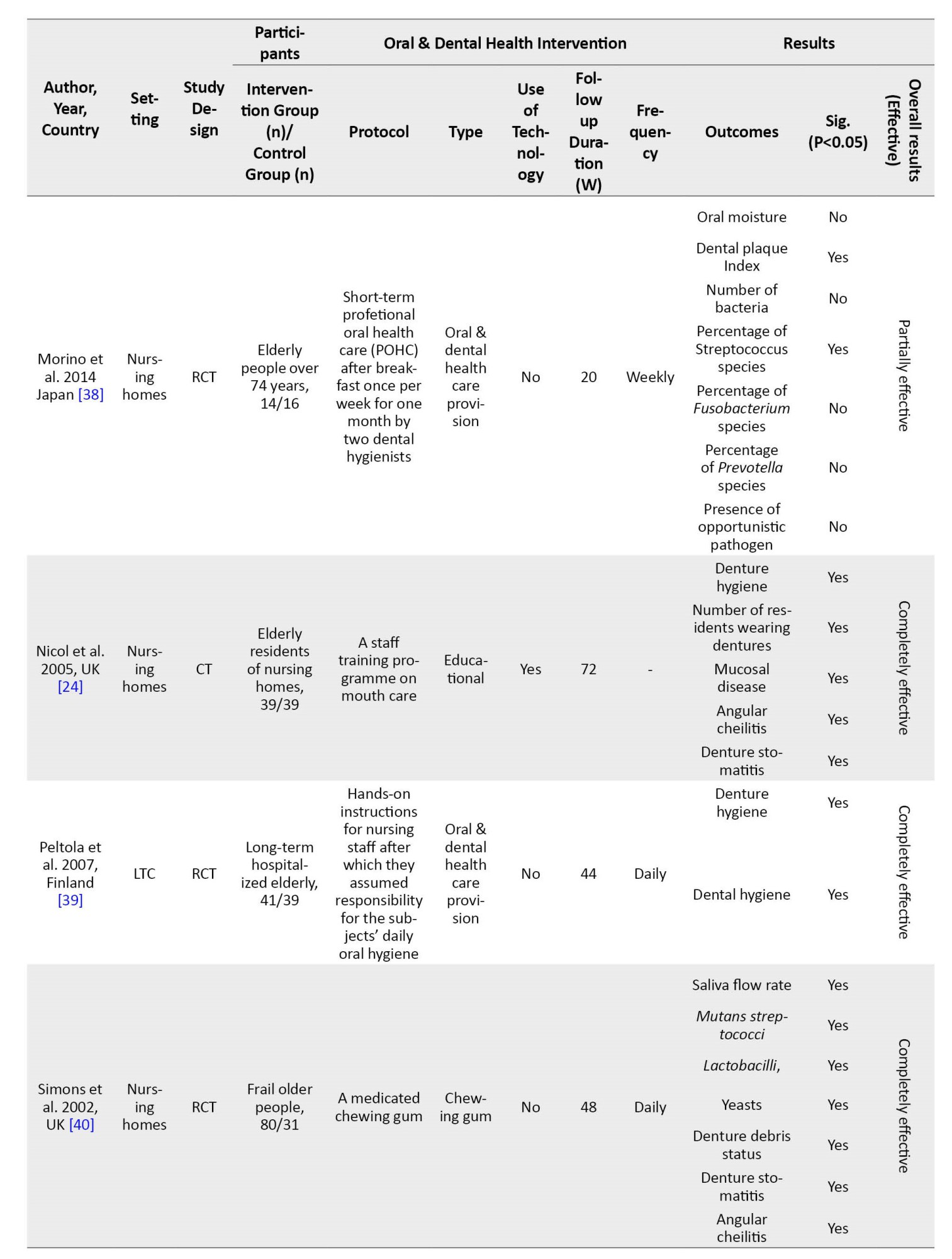
In these studies, there were 1851 samples in the intervention groups and 2255 in the control group.
In 19 studies, a total of 95 indicators were measured and reported, of which 53 were reported to be statistically non-significant. Regarding overall effectiveness of the interventions, 10 studies reported them as completely effective (all indicators were statistically significant), 5 studies reported as relatively effective (some indicators were statistically significant) and 4 reported as ineffective (None of the indicators was statistically significant). Regarding the effectiveness based on the type of intervention, the studies showed that chewing gum interventions had the highest effectiveness (90%) and the combined interventions had the lowest effectiveness (34.7%). Furthermore, educational interventions were effective by about 68.0% and the interventions for oral & health care provision were 42.8% effective (Figure 2). Among the indices reported in the studies, the dental plaque index, denture plaque index, and gingival index were reported in different studies. The results of the meta-analysis (Figure 3) showed that the mean difference in the dental plaque index between the intervention and control groups was -0.65 (95% CI; -2.03%, 0.74%; Q=59.6, df=5, P=0.001, I2=97.8%); the mean difference in the denture plaque index was -0.20 (95% CI; -0.38%, -0.02%; Q=3.22, df=3, P=0.36, I2=21.3%) and the mean difference in the gingival index was -0.36 (95% CI; -0.99%, 0.27%; Q=5.2, df=1, P=0.02, I2=80.9%). Based on the mean differences, the difference in the mean scores of denture plaque index and gingival index between the two groups was moderately significant. The results of measuring the risk of publication bias (Figure 4) showed a high risk of bias (z=-2.79, Prob > |z|=0.0053). In assessing the risk of bias in 19 studies, 7 articles had a high risk of bias, 6 articles had a low risk of bias, and 6 has unknown bias (Table 3).
Discussion
The majority of the reviewed studies reported the interventions as completely effective, where chewing gum had the highest effectiveness and the combined interventions had the lowest efficacy. In the studies, the mean difference in the denture plaque index and gingival index was mildly significant between the intervention and control groups. In general, the results of our study indicate that the community-based interventions that have been used to improve the oral & dental health of the elderly do not have a good effectiveness. One of the important reasons can be related to the study areas. As most studies were conducted in nursing homes and long-term care centers, the poor quality of care, psychological problems, and attitudes of the elderly living in these centers can affect the final results [45-47]. Therefore, along with interventions related to oral & dental health in the elderly, it is recommended to pay attention to other concerns of the elderly in these centers. Due to the strong correlation between oral & dental health and other problems in the elderly, it is recommended to conduct multidisciplinary interventions. Also, comprehensive and integrated services with high quality should be provided for the elderly in nursing homes and long-term care centers.
The results of the review showed that chewing gum was the most effective intervention. Various studies in other age groups which examined the effect of chewing gum on the oral & dental hygiene have also shown the high effectiveness of these interventions and have recommended to chew sugar free gums [48-52]. According to these studies, the most important mechanisms of chewing gum can be reduced dental plaque, reduced streptococcus mutans of saliva, reduced production of salivary acid, and increased salivary and mechanical cleansing properties of the chewing gum [53-55].
The results also showed the educational interventions had a moderate effectiveness. Albrecht also did not show the effectiveness of educational interventions [56]. However, most of the educational interventions for lower ages, especially school-based interventions, have been reported to have a relatively good efficacy [57-60]. One of the probable reasons for lower effectiveness of educational interventions for the elderly can be the aging and physiological issues that reduce the learning ability. Educational practices used in the studies can be effective, since most of the educational interventions are usually short-term and traditional, using inefficient methods. One of the educational models that can be recommended in this field is the Health Belief Model. The effectiveness of this educational model in improving oral & dental health has been reported [61-63].
Most of the reviewed studies were conducted in developed countries. It does not mean that no community-based interventions for the oral health of the elderly have been conducted in middle-income and low-income countries; however, it can indicate that, due to their poor performance and reporting, they could not be published. It should be noted that, due to the existing socioeconomic and cultural differences and the different quality of the interventions, their implementation, regardless of the local conditions of each country, will not be effective and will be a waste of resources [64, 65]. Another reason that may explain the high number of studies on the oral health of the elderly in developed countries can be the higher importance of aging in these countries or paying more attention to the health of elderly people [66]. Due to the fact that the aged population in middle-income and lower-income countries is growing, their low attention will increase the burden on health systems of these countries in the near future [67]. Hence, more attention is now being paid to the health of the elderly, especially their oral health [68-70].
A variety of electronical/technological methods (e-mail, internet, designed programs, software) had been used for the oral health of the elderly. The studies using a variety of such technologies have reported a higher efficacy [71, 72]. Recently, the use of technological methods to improve the health of people in other areas has been increased [73-76]. These advancements can be used to design and implement the interventions for the oral health of the elderly. The articles did not have a good status in the risk of bias assessment. The most important problem was related to blinding and allocating individuals to intervention and control groups. Given that most studies had been conducted in nursing homes and long-term care centers, and since the elderly are in contact with each another in these centers, it is likely that the interventions will also have an impact on the control groups, and this can alter the results of the interventions. Therefore, it is recommended that researchers perform interventions in the future studies with more blinding. In this regard, the use of guidelines for conducting interventional studies and reporting their results [77-80] can be effective.
One of the main limitations of the present study was the low generalizability of the results. The main reason is that the reviewed studies were conducted in several high-income countries which limits the generalizability of the results to middle-income and lower-income countries. In addition, due to the high number of oral health indicators and their different method of outcome reporting, meta-analysis was not possible to be done for the most of indicators. Regarding the high costs of dental care and lack of resources in the health system of middle-income and lower-income countries, their health system and people prefer cost-effectiveness interventions. Most of the reviewed studies focused on surrogate endpoints indicators such as saliva flow, bacterial counts, etc. Although these indicators are important, it is recommended that future studies focus more on clinical indicators or clinically significant endpoints such as tooth loss, pain, quality of life, and dentine caries. Also, according to the literature review and to our best knowledge, economic cost-effective studies in the field of oral health of the elderly are limited.
Based on the results of the study, it can be concluded that the community-based interventions for improving the oral & dental health of the elderly do not have a good efficacy. Given the rapid increase in the number of elderly people in the world and their wide oral hygiene problems, there is an increasing need for more effective interventions and planning. Chewing sugar free gums and holding effective and long-term training courses aimed at changing the behavior of the elderly are recommended. In addition, due to the weaknesses in the methodology and outcome reporting in the reviewed studies, it is recommended to use the available guidelines for carrying out the interventions and reporting their outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.REC.1398.674).
Funding
This study was funded by Tabriz University of Medical Sciences.
Authors' contributions
Investigation and drafting the manuscript: Mir Hossein Aghaei, Fatemeh Pournaghi-Azar, and Saber Azami-Aghdash; Data acquisition and data analysis: Fatemeh Pournaghi-Azar, Mohammad Mohseni and Mahdi Nouri; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to the Deputy for Research and Technology of Tabriz University of Medical Sciences.
References
- Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature. 2008; 451(7179):716-9. [DOI:10.1038/nature06516] [PMID]
- Beard JR, Bloom DE. Towards a comprehensive public health response to population ageing. Lancet. 2015; 385(9968):658-61. [DOI:10.1016/S0140-6736(14)61461-6] [PMID]
- Suzman R, Beard JR, Boerma T, Chatterji S. Health in an ageing world-what do we know? Lancet. 2015; 385(9967):484-6. [DOI:10.1016/S0140-6736(14)61597-X] [PMID]
- Kabeshova A, Launay CP, Gromov VA, Fantino B, Levinoff EJ, Allali G, et al. Falling in the elderly: Do statistical models matter for performance criteria of fall prediction? Results from two large population-based studies. Eur J Intern Med. 2016; 27:48-56. [DOI:10.1016/j.ejim.2015.11.019] [PMID]
- Abolghasem Gorji H, Alikhani M, Mohseni M, Moradi-Joo M, Ziaiifar H, Moosavi A. The prevalence of malnutrition in Iranian elderly: A review article. Iran J Public Health. 2017; 46(12):1603-10. [PMID]
- da Mata C, Cronin M, O'Mahony D, McKenna G, Woods N, Allen PF. Subjective impact of minimally invasive dentistry in the oral health of older patients. Clin Oral Investig. 2015; 19(3):681-7. [DOI:10.1007/s00784-014-1290-6] [PMID]
- Karki AJ, Monaghan N, Morgan M. Oral health status of older people living in care homes in Wales. Br Dent J. 2015; 219(7):331-4. [DOI:10.1038/sj.bdj.2015.756] [PMID]
- Manski R, Moeller J. Barriers to oral health across selected European countries and the USA. Int Dent J. 2017; 67(3):133-8. [DOI:10.1111/idj.12283] [PMID]
- Aminabadi NA, Najafpour E, Erfanparast L, Jamali Z, Pournaghi-Azar F, Tamjid-Shabestari S, et al. Oral health status, dental anxiety, and behavior-management problems in children with oppositional defiant disorder. Eur J Oral Sci. 2016; 124(1):45-51. [DOI:10.1111/eos.12236] [PMID]
- Pournaghi Azar F, Mamizadeh M, Nikniaz Z, Ghojazadeh M, Hajebrahimi S, Salehnia F, et al. Content analysis of advertisements related to oral health in children: A systematic review and meta-analysis. Public Health. 2018; 156:109-16. [DOI:10.1016/j.puhe.2017.12.012] [PMID]
- Baghaie H, Kisely S, Forbes M, Sawyer E, Siskind DJ. A systematic review and meta-analysis of the association between poor oral health and substance abuse. Addiction. 2017; 112(5):765-79.[DOI:10.1111/add.13754] [PMID]
- Lacruz RS, Habelitz S, Wright JT, Paine ML. Dental enamel formation and implications for oral health and disease. Physiol Rev. 2017; 97(3):939-93. [DOI:10.1152/physrev.00030.2016] [PMID]
- Nazar H, Al-Mutawa S, Ariga J, Soparkar P, Mascarenhas AK. Caries prevalence, oral hygiene, and oral health habits of Kuwaiti infants and toddlers. Med Princ Pract. 2014; 23(2):125-8. [DOI:10.1159/000356866] [PMID]
- Mariño R, Albala C, Sanchez H, Cea X, Fuentes A. Prevalence of diseases and conditions which impact on oral health and oral health self-care among older chilean. J Aging Health. 2015; 27(1):3-16. [DOI:10.1177/0898264314533723] [PMID]
- Kobayashi N, Soga Y, Maekawa K, Kanda Y, Kobayashi E, Inoue H, et al. Prevalence of oral health-related conditions that could trigger accidents for patients with moderate-to-severe dementia. Gerodontology. 2017; ;34(1):129-34. [DOI:10.1111/ger.12235] [PMID]
- Azami-Aghdash S, Ghojazadeh M, Pournaghi Azar F, Naghavi-Behzad M, Mahmoudi M, Jamali Z. Fluoride concentration of drinking waters and prevalence of fluorosis in Iran: A systematic review. J Dent Res Dent Clin Dent Prospects. 2013; 7(1):1-7. [PMID]
- Kwan SY, Petersen PE, Pine CM, Borutta A. Health promoting schools: An apportunity for oral health promoting. Bull World Health Organ. 2005; 83(9):677-85. [PMID]
- El Osta N, Hennequin M, Tubert-Jeannin S, Abboud Naaman NB, El Osta L, Geahchan N. The pertinence of oral health indicators in nutritional studies in the elderly. Clin Nutr. 2014; 33(2):316-21.[DOI:10.1016/j.clnu.2013.05.012] [PMID]
- Toniazzo MP, Amorim PS, Muniz FWMG, Weidlich P. Relationship of nutritional status and oral health in elderly: Systematic review with meta-analysis. Clin Nutr. 2018; 37(3):824-30. [DOI:10.1016/j.clnu.2017.03.014] [PMID]
- Bozdemir E, Yilmaz HH, Orhan H. General health and oral health status in elderly dental patients in Isparta, Turkey. East Mediterr Health J. 2016; 22(8):579-85. [DOI:10.26719/2016.22.8.579] [PMID]
- Melo LA, Sousa MM, Medeiros AK, Carreiro AD, Lima KC. Factors associated with negative self-perception of oral health among institutionalized elderly. Cien Saude Colet. 2016; 21(11):3339-46. [DOI:10.1590/1413-812320152111.08802015] [PMID]
- MacEntee MI, Wong ST, Smith A, Beattie BL, Brondani M, Bryant SR, et al. Oral healthcare challenges for older Punjabi-speaking immigrants. Can J Aging. 2014; 33(2):196-207. [DOI:10.1017/S0714980814000087] [PMID]
- Adachi M, Ishihara K, Abe S, Okuda K, Ishikawa T. Effect of professional oral health care on the elderly living in nursing homes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94(2):191-5.[DOI:10.1067/moe.2002.123493] [PMID]
- Nicol R, Petrina Sweeney M, McHugh S, Bagg J. Effectiveness of health care worker training on the oral health of elderly residents of nursing homes. Community Dent Oral Epidemiol. 2005; 33(2):115-24. [DOI:10.1111/j.1600-0528.2004.00212.x] [PMID]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4(1):1.[DOI:10.1186/2046-4053-4-1] [PMID]
- Scimago Journal & Country Rank. SJR : Scientific Journal Rankings - SCImago. 2017 [Updated 2017 November 31]. Availablefrom: [Link]
- Vandamme K, Opdebeeck H, Naert I. Pathways in multidisciplinary oral health care as a tool to improve clinical performance. Int J Prosthodont. 2006; 19(3):227-35. [PMID]
- Al-Haboubi M, Zoitopoulos L, Beighton D, Gallagher JE. The potential benefits of sugar-free chewing gum on the oral health and quality of life of older people living in the community: A randomized controlled trial. Community Dent Oral Epidemiol. 2012; 40(5):415-24. [DOI:10.1111/j.1600-0528.2012.00685.x] [PMID]
- Bellomo F, de Preux F, Chung JP, Julien N, Budtz-Jørgensen E, Müller F. The advantages of occupational therapy in oral hygiene measures for institutionalised elderly adults. Gerodontology. 2005; 22(1):24-31. [DOI:10.1111/j.1741-2358.2004.00047.x] [PMID]
- De Visschere L, de Baat C, Schols JM, Deschepper E, Vanobbergen J. Evaluation of the implementation of an ‘oral hygiene protocol’ in nursing homes: A 5-year longitudinal study. Community Dent Oral Epidemiol. 2011; 39(5):416-25. [DOI:10.1111/j.1600-0528.2011.00610.x] [PMID]
- De Visschere L, Schols J, van der Putten GJ, de Baat C, Vanobbergen J. Effect evaluation of a supervised versus non-supervised implementation of an oral health care guideline in nursing homes: A cluster randomised controlled clinical trial. Gerodontology. 2012; 29(2):e96-106. [DOI:10.1111/j.1741-2358.2010.00418.x] [PMID]
- Frenkel H, Harvey I, Newcombe RG. Improving oral health in institutionalised elderly people by educating caregivers: A randomised controlled trial. Community Dent Oral Epidemiol. 2001; 29(4):289-97. [DOI:10.1034/j.1600-0528.2001.290408.x] [PMID]
- Hakuta C, Mori C, Ueno M, Shinada K, Kawaguchi Y. Evaluation of an oral function promotion programme for the independent elderly in Japan. Gerodontology. 2009; 26(4):250-8. [DOI:10.1111/j.1741-2358.2008.00269.x] [PMID]
- Komulainen K, Ylöstalo P, Syrjälä AM, Ruoppi P, Knuuttila M, Sulkava R, et al. Oral health intervention among community-dwelling older people: A randomised 2-year intervention study. Gerodontology. 2015; 32(1):62-72. [DOI:10.1111/ger.12067] [PMID]
- Lowe C, Blinkhorn AS, Worthington HV, Craven R. Testing the effect of including oral health in general health checks for elderly patients in medical practice--a randomized controlled trial. Community Dent Oral Epidemiol. 2007; 35(1):12-7. [DOI:10.1111/j.1600-0528.2007.00360.x] [PMID]
- MacEntee MI, Wyatt CC, Beattie BL, Paterson B, Levy-Milne R, McCandless L, et al. Provision of mouth-care in long-term care facilities: An educational trial. Community Dent Oral Epidemiol. 2007; 35(1):25-34. [DOI:10.1111/j.1600-0528.2007.00318.x] [PMID]
- Meurman JH, Kari K, Aikäs A, Kallio P. One-year compliance and effects of amine and stannous fluoride on some salivary biochemical constituents and oral microbes in institutionalized elderly. Spec Care Dentist. 2001; 21(1):32-6. [DOI:10.1111/j.1754-4505.2001.tb00221.x] [PMID]
- Morino T, Ookawa K, Haruta N, Hagiwara Y, Seki M. Effects of professional oral health care on elderly: Randomized trial. Int J Dent Hyg. 2014; 12(4):291-7. [DOI:10.1111/idh.12068] [PMID]
- Peltola P, Vehkalahti MM, Simoila R. Effects of 11-month interventions on oral cleanliness among the long-term hospitalised elderly. Gerodontology. 2007; 24(1):14-21. [DOI:10.1111/j.1741-2358.2007.00147.x] [PMID]
- Simons D, Brailsford SR, Kidd EA, Beighton D. The effect of medicated chewing gums on oral health in frail older people: A 1-year clinical trial. J Am Geriatr Soc. 2002; 50(8):1348-53. [DOI:10.1046/j.1532-5415.2002.50355.x] [PMID]
- Zenthöfer A, Dieke R, Dieke A, Wege KC, Rammelsberg P, Hassel AJ. Improving oral hygiene in the long-term care of the elderly--a RCT. Community Dent Oral Epidemiol. 2013; 41(3):261-8. [DOI:10.1111/cdoe.12007] [PMID]
- Nihtilä A, Tuuliainen E, Komulainen K, Autonen-Honkonen K, Nykänen I, Hartikainen S, et al Preventive oral health intervention among old home care clients. Age Ageing. 2017; 46(5):846-51. [DOI:10.1093/ageing/afx020] [PMID]
- Shokry AAE, Adel MR, Rashad AEA. Educational program to improve quality of life among elderly regarding oral health. Future Dent J. 2018; 4(2):211-5. [DOI:10.1016/j.fdj.2018.07.002]
- Keyong E, Thitasomakul S, Tianviwat S. Effectiveness of an oral health promotion program for the elderly in Khiri Mat District, Sukhothai Province: A randomized control trial. J Int Soc Prev Community Dent. 2019; 9(3):225-31. [DOI:10.4103/jispcd.JISPCD_27_19] [PMID]
- MacEntee MI, Kazanjian A, Kozak JF, Hornby K, Thorne S, Kettratad-Pruksapong M. A scoping review and research synthesis on financing and regulating oral care in long-term care facilities. Gerodontology. 2012; 29(2):e41-52. [DOI:10.1111/j.1741-2358.2011.00575.x]
- Mariño R, Minichiello V, Macentee MI. Understanding oral health beliefs and practices among Cantonese-speaking older Australians. Australas J Ageing. 2010; 29(1):21-6. [DOI:10.1111/j.1741-6612.2010.00395.x] [PMID]
- Yao CS, MacEntee MI. Inequity in oral health care for elderly Canadians: Part 1. Oral health status. J Can Dent Assoc. 2013; 79:d114. [PMID]
- Porciani PF, Perra C, Grandini S. Effect on dental stain occurrence by chewing gum containing sodium tripolyphosphate--a double-blind six-week trial. J Clin Dent. 2010; 21(1):4-7. [PMID]
- Hellgren K. Assessment of Krillase chewing gum for the reduction of gingivitis and dental plaque. J Clin Dent. 2009; 20(3):99-102. [PMID]
- Twetman S. Consistent evidence to support the use of xylitol- and sorbitol-containing chewing gum to prevent dental caries. Evid Based Dent. 2009; 10(1):10-1. [DOI:10.1038/sj.ebd.6400626] [PMID]
- Ly KA, Milgrom P, Rothen M. The potential of dental-protective chewing gum in oral health interventions. J Am Dent Assoc. 2008; 139(5):553-63. [DOI:10.14219/jada.archive.2008.0215] [PMID]
- Deshpande A, Jadad AR. The impact of polyol-containing chewing gums on dental caries: A systematic review of original randomized controlled trials and observational studies. J Am Dent Assoc. 2008; 139(12):1602-14. [DOI:10.14219/jada.archive.2008.0102] [PMID]
- Emamieh S, Khaterizadeh Y, Goudarzi H, Ghasemi A, Baghban AA, Torabzadeh H. The effect of two types chewing gum containing casein phosphopeptide-amorphous calcium phosphate and xylitol on salivary Streptococcus mutans. J Conserv Dent. 2015; 18(3):192-5. [DOI:10.4103/0972-0707.157240] [PMID]
- Gueimonde L, Vesterlund S, García-Pola MJ, Gueimonde M, Söderling E, Salminen S. Supplementation of xylitol-containing chewing gum with probiotics: A double blind, randomised pilot study focusing on saliva flow and saliva properties. Food Funct. 2016; 7(3):1601-9. [DOI:10.1039/C5FO01497B] [PMID]
- Kubota C, Kanazawa M, Hama Y, Komagamine Y, Minakuchi S. Association between chewing-stimulated salivary flow under the effects of atropine and mixing ability assessed using a color-changeable chewing gum. J Prosthodont Res. 2017; 61(4):387-92. [DOI:10.1016/j.jpor.2016.12.009] [PMID]
- Albrecht M, Kupfer R, Reissmann DR, Mühlhauser I, Köpke S. Oral health educational interventions for nursing home staff and residents. Cochrane Database Syst Rev. 2016; 9(9):CD010535. [DOI:10.1002/14651858.CD010535.pub2] [PMID]
- Blake H, Dawett B, Leighton P, Rose-Brady L, Deery C. School-based educational intervention to improve children’s oral health-related knowledge. Health Promot Pract. 2015; 16(4):571-82.[DOI:10.1177/1524839914560568] [PMID]
- Haleem A, Siddiqui MI, Khan AA. School-based strategies for oral health education of adolescents--a cluster randomized controlled trial. BMC Oral Health. 2012; 12:54. [DOI:10.1186/1472-6831-12-54] [PMID]
- Hazavehei SM, Shirahmadi S, Taheri M, Noghan N, Rezaei N. Promoting Oral health in 6-12 year-old students: A systematic review. J Educ Community Health. 2015; 1(4):66-84. [DOI:10.20286/jech-010466]
- Gambhir RS, Sohi RK, Nanda T, Sawhney GS, Setia S. Impact of school based oral health education programmes in India: A systematic review. J Clin Diagn Res. 2013; ;7(12):3107-10. [DOI:10.7860/JCDR/2013/6212.3718] [PMID]
- Rahmati-Najarkolaei F, Rahnama P, Gholami Fesharaki M, Behnood V. Predictors of oral health behaviors in female students: An application of the health belief model. Iran Red Crescent Med J. 2016; 18(11):e24747. [DOI:10.5812/ircmj.24747]
- Buglar ME, White KM, Robinson NG. The role of self-efficacy in dental patients’ brushing and flossing: Testing an extended Health Belief Model. Patient Educ Couns. 2010; 78(2):269-72. [DOI:10.1016/j.pec.2009.06.014] [PMID]
- Solhi M, Zadeh DS, Seraj B, Zadeh SF. The application of the health belief model in oral health education. Iran J Public Health. 2010; 39(4):114-9. [PMID]
- Lapão LV. The challenge of benchmarking health systems: Is ICT innovation capacity more systemic than organizational dependent? Isr J Health Policy Res. 2015; 4:43. [DOI:10.1186/s13584-015-0036-5] [PMID]
- Wollum A, Burstein R, Fullman N, Dwyer-Lindgren L, Gakidou E. Benchmarking health system performance across states in Nigeria: A systematic analysis of levels and trends in key maternal and child health interventions and outcomes, 2000-2013. BMC Med. 2015; 13:208. [DOI:10.1186/s12916-015-0438-9] [PMID]
- United Nations. World Population Ageing 2015. New York: United Nations; 2015. [Link]
- Kinsella K, He W. An aging world: 2008. Washington, DC: National Institute on Aging and U.S. Census Bureau; 2009. [Link]
- Garrido Urrutia C, Romo Ormazábal F, Espinoza Santander I, Medics Salvo D. Oral health practices and beliefs among caregivers of the dependent elderly. Gerodontology. 2012; 29(2):e742-7. [DOI:10.1111/j.1741-2358.2011.00553.x] [PMID]
- MacEntee MI, Marino R, Wong S, Kiyak A, Minichiello V, Chi I, et al. Discussions on oral health care among elderly Chinese immigrants in Melbourne and Vancouver. Gerodontology. 2012; 29(2):e822-32. [DOI:10.1111/j.1741-2358.2011.00568.x]
- Nazliel HE, Hersek N, Ozbek M, Karaagaoglu E. Oral health status in a group of the elderly population residing at home. Gerodontology. 2012; 29(2):e761-7. [DOI:10.1111/j.1741-2358.2011.00556.x] [PMID]
- Mohamadkhah F, Shokravi FA, Faghihzadeh S, Ghaffarifar S. The effect of digital media programs on the oral health promotion in the health office: A Quasi-experimental study. Shiraz E Med J. 2013; 14(1):2-12. [Link]
- Vozza I, Guerra F, Marchionne M, Bove E, Corridore D, Ottolenghi L. A multimedia oral health promoting project in primary schools in central Italy. Ann Stomatol (Roma). 2014; 5(3):87-90. [PMID]
- Griffin N, Kehoe M. A questionnaire study to explore the views of people with multiple sclerosis of using smartphone technology for health care purposes. Disabil Rehabil. 2018; 40(12):1434-42. [DOI:10.1080/09638288.2017.1300332] [PMID]
- Rehman H, Kamal AK, Morris PB, Sayani S, Merchant AT, Virani SS. Mobile Health (mHealth) technology for the management of hypertension and hyperlipidemia: Slow start but loads of potential. Curr Atheroscler Rep. 2017; 19(3):12. [DOI:10.1007/s11883-017-0649-y] [PMID]
- Rehman H, Kamal AK, Sayani S, Morris PB, Merchant AT, Virani SS. Using Mobile Health (mHealth) technology in the management of diabetes mellitus, physical inactivity, and smoking. Curr Atheroscler Rep. 2017; 19(4):16. [DOI:10.1007/s11883-017-0650-5] [PMID]
- Sigler BE. Investigating the perceptions of care coordinators on using behavior theory-based mobile health technology with medicaid populations: A grounded theory study. JMIR Mhealth Uhealth. 2017; 5(3):e36. [DOI:10.2196/mhealth.5892] [PMID]
- Boers M. Updated consolidated standards of reporting trials (CONSORT): It just gets better. J Clin Epidemiol. 2010; ;63(8):813-4. [DOI:10.1016/j.jclinepi.2010.01.002] [PMID]
- Liu XT, Zhang X, Wen S, Peng L, Hong Q, Kang D. Impact of the Consolidated Standards of Reporting Trials (CONSORT) checklist on reporting of randomized clinical trials in traditional Chinese medicine. J Evid Based Med. 2015; 8(4):192-208. [DOI:10.1111/jebm.12173] [PMID]
- Turner L, Shamseer L, Altman DG, Weeks L, Peters J, Kober T, et al. Consolidated standards of reporting trials (CONSORT) and the completeness of reporting of randomised controlled trials (RCTs) published in medical journals. Cochrane Database Syst Rev. 2012; 11(11):MR000030. [DOI:10.1002/14651858.MR000030.pub2] [PMID]
- Palys KE, Berger VW. A note on the jadad score as an efficient tool for measuring trial quality. J Gastrointest Surg. 2013; 17(6): p. 1170-1. [DOI:10.1007/s11605-012-2106-0] [PMID]
Article Type : Research |
Subject:
General
Received: 2022/09/5 | Accepted: 2023/05/31 | Published: 2024/01/1
Received: 2022/09/5 | Accepted: 2023/05/31 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |