Tue, Feb 3, 2026
Volume 35, Issue 2 (3-2025)
JHNM 2025, 35(2): 119-125 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Karbalai F, Jafari F, Bakhtiari S. Evaluating the Urinary Iodine Concentration in Operating Room Personnel After Using Povidone-iodine Hand Scrub. JHNM 2025; 35 (2) :119-125
URL: http://hnmj.gums.ac.ir/article-1-2256-en.html
URL: http://hnmj.gums.ac.ir/article-1-2256-en.html
1- MSc Student of Operating Room, Department of Operating Room, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
2- PhD Student in Nursing, Endocrine and Metabolism Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
3- Assistant Professor, Department of Operating Room, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Isfahan University of Medical Science, Isfahan, Iran. ,baksoheilaa46@gmail.com
2- PhD Student in Nursing, Endocrine and Metabolism Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
3- Assistant Professor, Department of Operating Room, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Isfahan University of Medical Science, Isfahan, Iran. ,
Full-Text [PDF 461 kb]
(282 Downloads)
| Abstract (HTML) (793 Views)
Full-Text: (360 Views)
Introduction
Effective hand scrubbing and disinfection are crucial, particularly before wearing sterile gloves for surgery, as a study found that surgical gloves have perforations in 5.9% of cases [1, 2]. There are two main types of hand sanitizers, including alcoholic and non-alcoholic (povidone-iodine, hexachlorophene, Chlorhexidine gluconate and Hibitane) [3-5]. The materials used for hand sanitizing, particularly in surgical operations, are diverse. Povidone-iodine solution (7.5% betadine) is the most well-known and widely used solution [6]. As a topical antiseptic agent in the form of an iodophor, povidone-iodine reduces the irritating effects of iodine [7]. One of its key characteristics is its high bactericidal activity, which is capable of killing a broad spectrum of microorganisms within 3-5 minutes due to the presence of iodine [8]. However, excessive iodine consumption can lead to poisoning in individuals, with a tolerable intake level of 1100 µg/day for people aged >19 years [9]. The complications and symptoms of iodine poisoning are diverse, ranging from gastrointestinal symptoms (headache, dizziness and nausea) to metabolic and hormonal disorders, including thyroid gland disorders [10, 11].
Despite the limited and negligible side effects of povidone-iodine (7.5% betadine) in case of prolonged use (approximately ≥3 hours), this substance has demonstrated acceptable efficacy [11, 12]. Consequently, it remains a widely used agent in surgical rooms for hand sanitizing [13]. Povidone-iodine exhibits a broad-spectrum antimicrobial effect, displaying high sensitivity against gram-negative and gram-positive bacteria, acidophiles, fungi, amoebic cysts and spores [14-16]. Research has shown that prolonged skin exposure to iodine (≥3 hours) can result in limited absorption [17, 18]. Additionally, the widespread use of amiodarone and iodinated radiological contrast agents has been found to expose the body to high doses of exogenous iodine [7].
The routine use of povidone-iodine solution may be a potential cause of iodine poisoning in operating room personnel, as evidenced by elevated urinary iodine levels [19]. A study revealed that the average urinary iodine level one week after using povidone-iodine for sanitizing was significantly higher than the pre-use period [20]. Furthermore, some studies have suggested that povidone-iodine solution can be absorbed through the skin or mucous membrane due to its high iodine content [17, 18]. However, contradictory results have been reported in other studies [17, 21]. For instance, a study found that the urinary iodine level of operating room personnel in Turkey was at an average level, despite the regular use of povidone-iodine for hand sanitizing, and it did not show elevated levels [21]. This finding highlights the conflicting evidence concerning the skin absorption of iodine from povidone-iodine solutions and its potential impact on the health of operating room personnel [17, 20, 21]. This study aimed to measure the urinary iodine concentration (UIC) in operating room personnel of a hospital in Isfahan, Iran, who used povidone-iodine solution (betadine 7.5%) for hand scrubbing.
Materials and Methods
This is a descriptive-analytical study. A total of 100 operating room personnel (technologists and scrub nurses) were selected from a hospital affiliated to Isfahan University of Medical Sciences in 2022, using a convenience sampling method. The inclusion criteria were consent to participate, no wounds on hand skin up to 5 cm above the elbow, self-report of no skin dermatitis, not receiving iodinated contrast agents during the study, no history of taking certain medications or supplements related to iodine, no history of iodine deficiency or thyroid disorders, no history of thyroidectomy and not following a special diet that includes excessive seafood (≥3 times a week). The exclusion criteria were unwillingness to continue participation, development of skin wounds or scratches during the study, and inconsistent use of povidone-iodine and alcohol solutions for scrubbing. To determine the sample size, the formula for estimating proportions was used [18]. By considering a maximum estimation error of 0.05 at a confidence level of 95% (Z1−α/2=1.96) and a precision (d) of 7.5%, the minimum sample size was calculated to be 100 (50 per group). The study hospital has two operating rooms. We selected 50 personnel from one operating room and assigned them to the povidone-iodine scrub group, while 50 personnel from the second operating room were assigned to the alcohol-based scrub group. The work-related and demographic data were collected using a form surveying age, gender, work experience, educational level, frequency of scrubbing per week, and number of shifts per week. The UIC was measured for both groups using the Sandell-Kolthoff reaction method. This method is popular for its accuracy and sensitivity in measuring urinary iodine, showing reliable results [17, 18].
Before the study, participants were trained on the standard surgical scrub method, which involved scrubbing the four surfaces of each finger, the outside of the fifth finger, the back of the hand, the palm, from the little finger to the thumb, from the wrist to the arm (three times), and up to 5 cm above the elbow [22]. The betadine used during the study was made by a pharmaceutical company that had a contract with the hospital (The participants, the person responsible for measuring the UIC in the laboratory and the researchers did not have information about the name of the company). The betadine was poured into the betadine storage containers in the scrub rooms by the person in charge of operating room equipment. In both groups, scrubbing was performed for one week, three times a day, each for three minutes, using 3-5 mL of povidone-iodine or alcoholic solution. All procedures were carried out under the supervision of the researcher. Participants were instructed to maintain their usual diet and avoid using chemical or herbal medications during this period.
One week after the study, morning urine samples were collected from the participants on a single day. Prior to sampling, comprehensive instructions on urine sampling procedures (initially washing the external urinary tract with water and then collecting mid-stream urine) were provided by the researcher. These instructions were given individually and face-to-face in a private area within the operating rooms. If any confusion arose, further explanations were provided to the participants. Mmidstream urine samples were placed in deionized test tubes with lids shut tightly, placed in cool boxes, maintained at a temperature of 2-8 °C, and transported to the Comprehensive Research Laboratory of Isfahan University of Medical Sciences immediately. The samples were acidified and stored under -20 °C until analysis. The UIC was subsequently measured by the modified Sandell-Kolthoff method using a microplate technique, adhering to the recommendations of the centers for disease control and prevention. The measurement was done by a laboratory expert, and the researcher was responsible for ensuring the accuracy of this measurement. The urine samples were initially dissolved at room temperature and then incubated for 30 minutes with 0.9 M ammonium persulfate at 95 °C using a thermal cycler. After cooling, 50 μL of the processed urine samples were placed into the wells of a microplate. Subsequently, 100 μL of a 0.05 M arsenious acid solution was added to each well and mixed properly. In the final step, 50 μL of a 0.019 M ceric ammonium sulfate solution was added. After a 30-min incubation at 25 °C, absorbance was measured at 405 nm. The UIC was calculated by plotting a standard curve and reported in micrograms per liter (μg/L) [17, 23]. A UIC≤300 μg/L shows normal range, and ˃300 μg/L indicates a potential risk for abnormal thyroid function [17].
Data analysis was performed in SPSS software, version 25 (IBM Corporation, Chicago, IL). The normality of data distribution was assessed using the Shapiro-Wilk test. Quantitative data were presented as Mean±SD or median ±95% interquartile range. The differences between groups were analyzed using the Chi-square test or Mann-Whitney U-test (for non-parametric variables). The significance level was set at 0.05.
Results
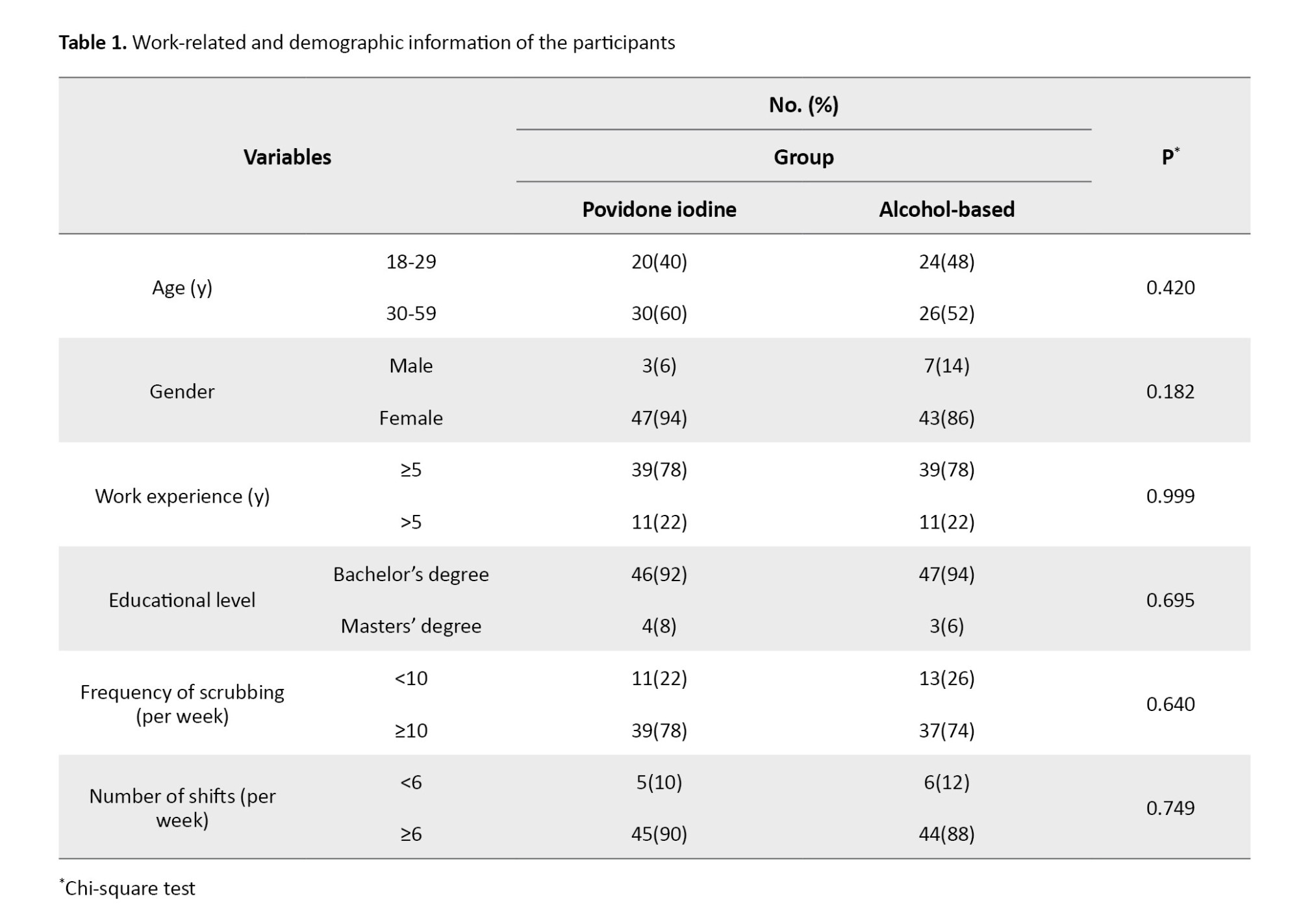
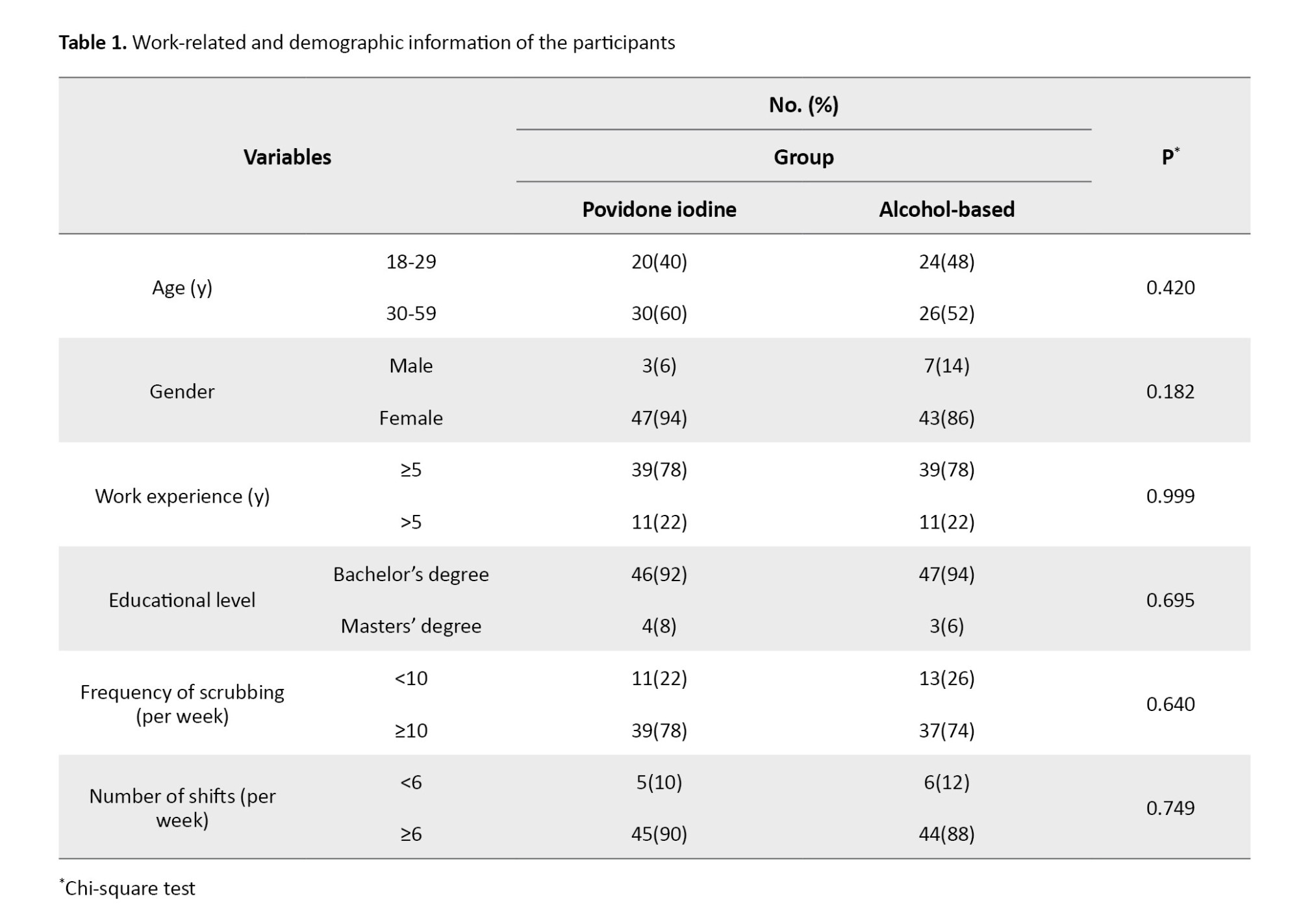
A comparison of the povidone-iodine scrub group with the alcohol-based scrub group revealed no significant differences in terms of age (31.9±6.29 vs 31.7±5.59 years), work experience (3.90±1 vs 4.08±1.69 years), gender (94% vs 86% female), educational level (92% vs 94% with a bachelor’s degree), frequency of scrubbing (78% vs 74% with >6 shifts per week) and shifts per week (Table 1).
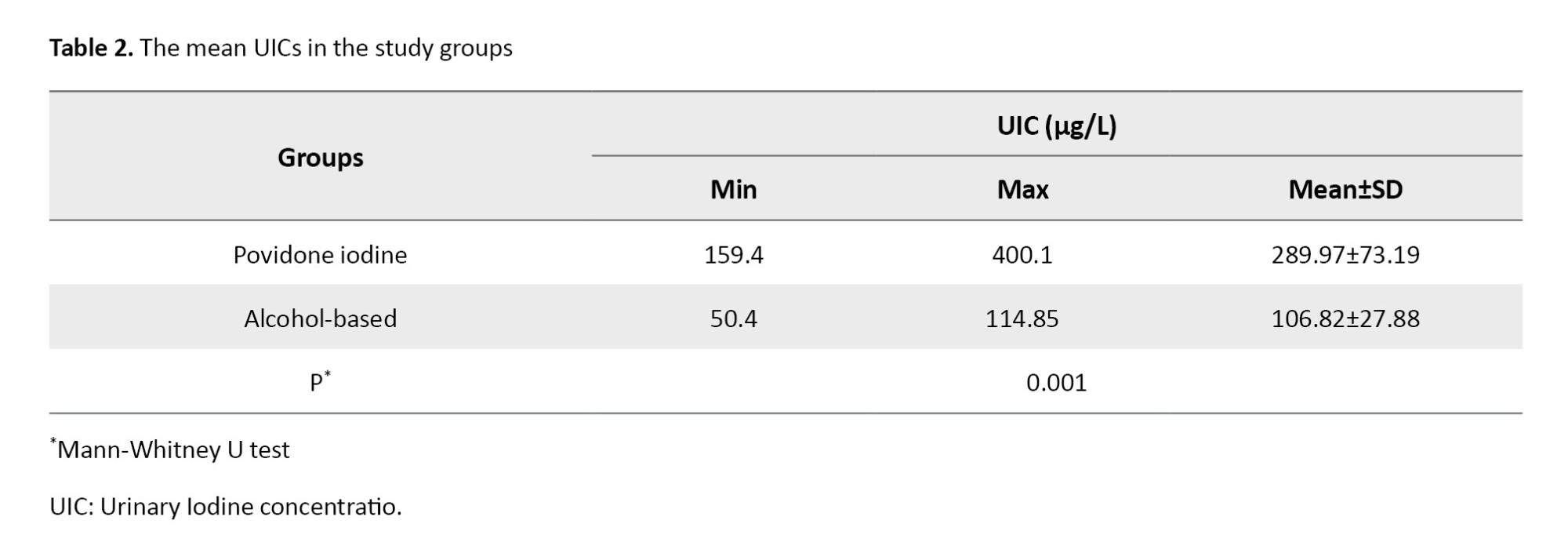
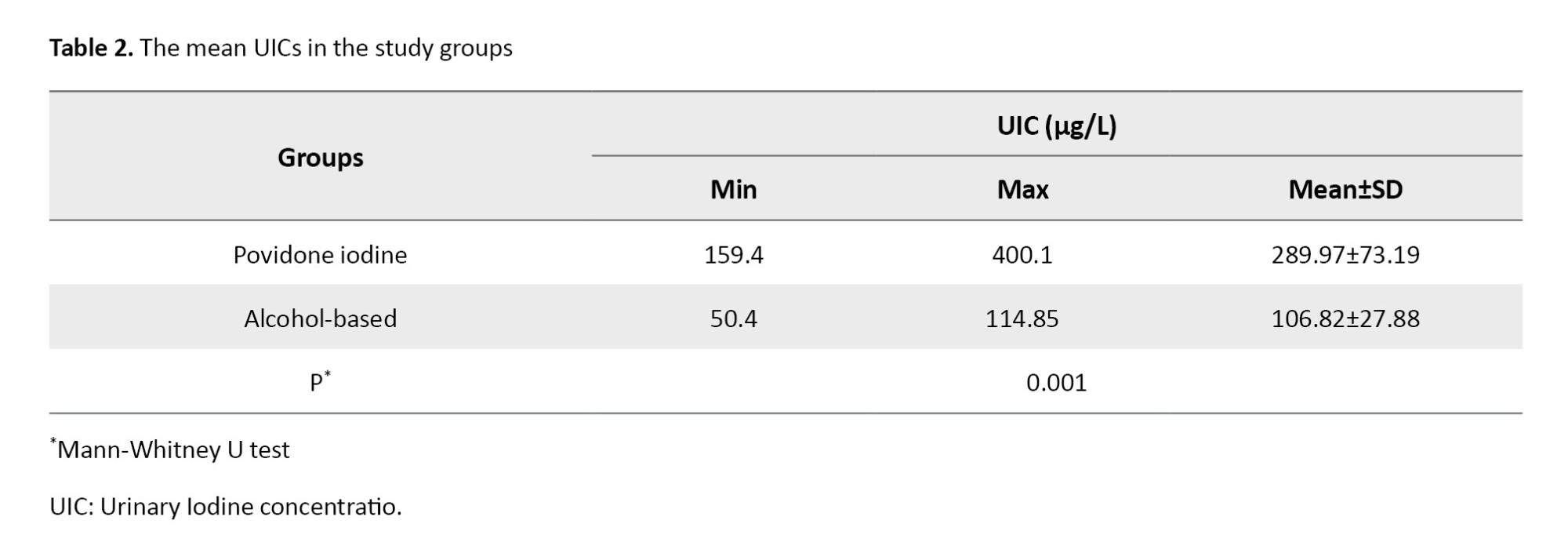
However, the UIC was significantly higher in the povidone-iodine scrub group (289.9±73.19 vs 106.6±27.88 μg/L; P=0.001).These findings were shown in Table2.
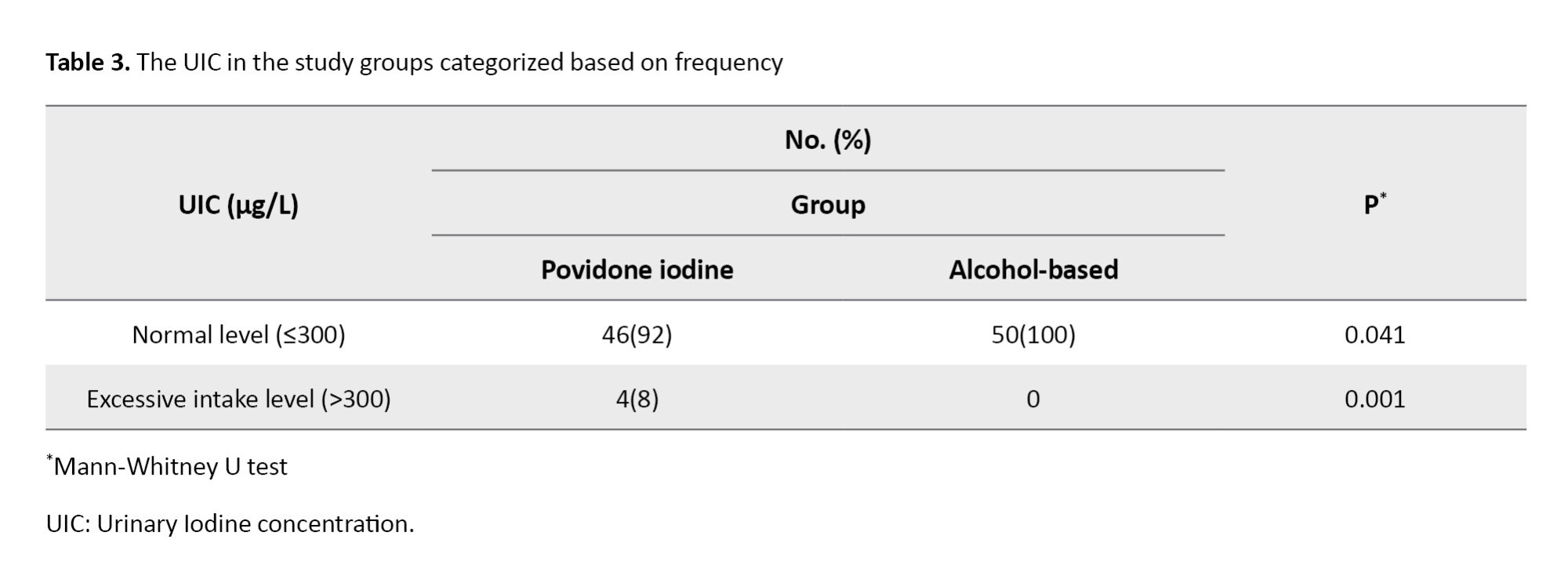
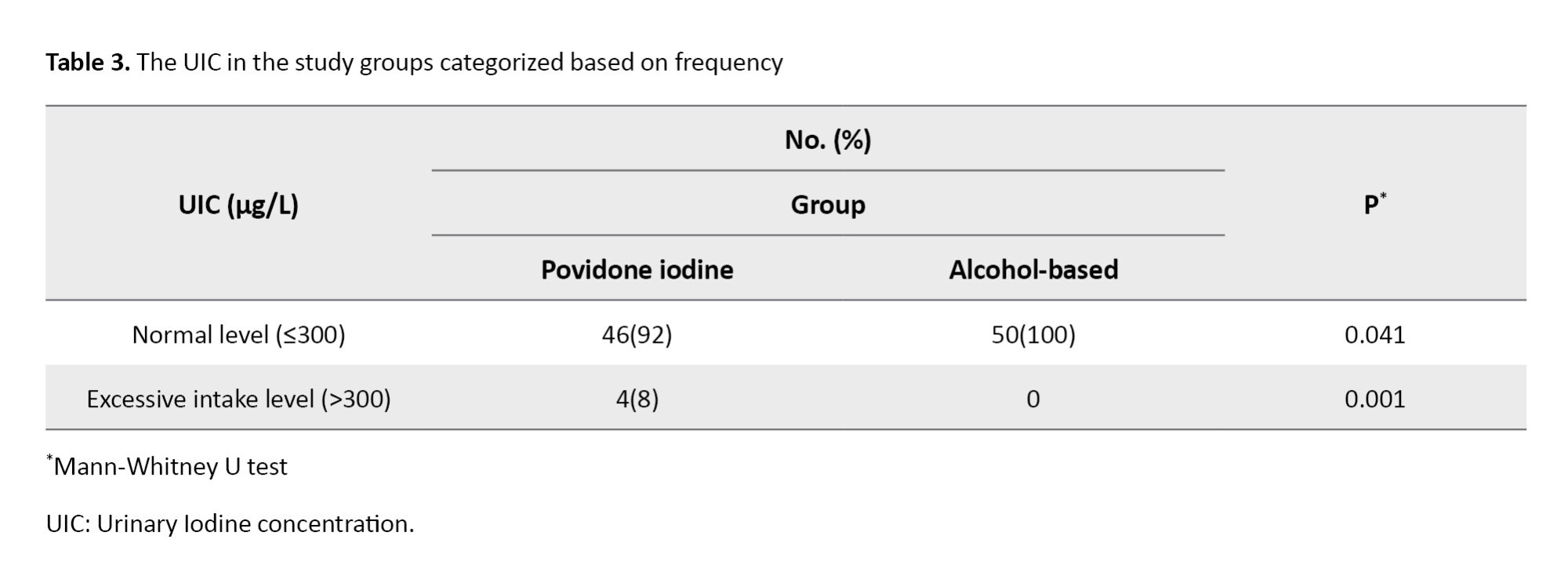
Furthermore, the UIC at a level indicating excessive iodine intake (˃300 µg/L) was significantly higher in the povidone-iodine scrub group compared to the alcohol-based scrub group (8% vs 0%; P=0.001) that was shown in Table 3.
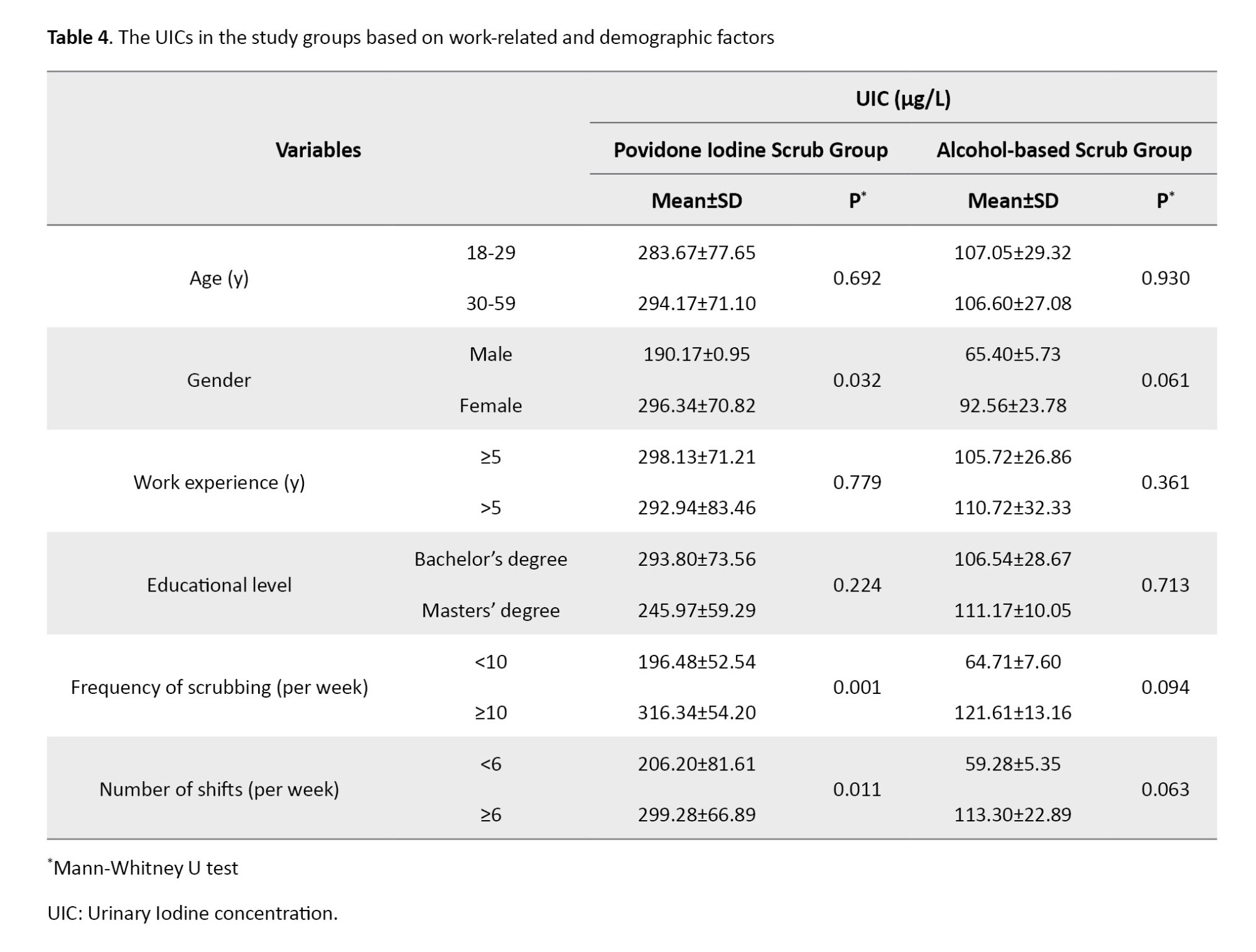
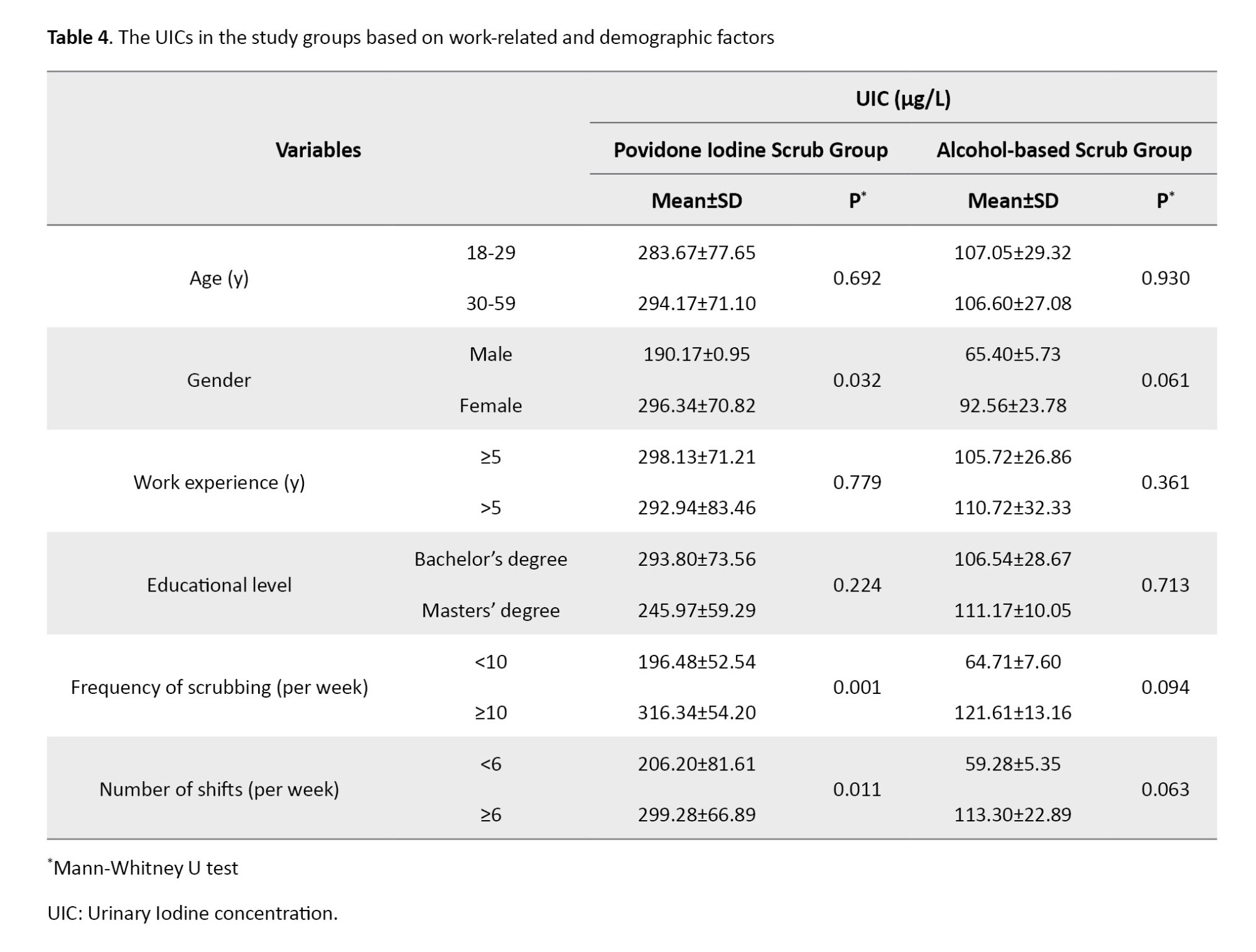
In the povidone-iodine scrub group, the UIC was significantly higher in females (296.3±70.82 vs 190.1±0.95 μg/L; P=0.032), in those who scrubbed ≥10 times per week (316.3± 54.20 vs 196.5±52.54 μg/L; P=0.001), and in those who worked ≥6 shifts per week (299.3±66.9 vs 206.2±81.6 μg/L; P=0.011). However, no significant differences were found in the UIC based on age, work experience, or educational level. In the alcohol-based scrub group, no significant differences were observed in the UIC based on any factors (Table 4).
Discussion
This study demonstrated that, among operating room personnel, the UIC in the povidone-iodine scrub group was significantly higher than in the alcohol-based scrub group. A similar study reported that rinsing the mouth with povidone-iodine increased the serum iodine level by 2-3 times and the UIC by 5 times [20]. Our results are also in line with previous studies, which showed that using hand sanitizers containing iodine increased UIC and suggested that operating room personnel should take necessary measures to control iodine exposure [17, 21]. Our findings differed from these studies; we compared an alcohol-based solution with povidone-iodine, while these two studies only examined povidone-iodine. A laboratory study by Nesvadbova et al. demonstrated that iodine in povidone-iodine solution can be absorbed through skin cells to a significant extent [18]. The authors suggested that frequent professional contact with the povidone-iodine solution as a skin scrub can lead to iodine penetration through the skin. Our study’s findings are in agreement with the results of this study.
Our study revealed that 80.0% of operating room personnel in the povidone-iodine scrub group had extremely high intake levels, indicating iodine poisoning, whereas none of the participants in the control group had excessive intake levels. Idiz et al. in Turkey reported that 7.5% of surgical staff who scrubbed with povidone-iodine had iodine poisoning [17]. Our findings are consistent with their findings. However, Erdoğan et al. in Turkey reported a higher prevalence of excessive intake level (approximately 39%) among operating room staff who scrubbed with povidone-iodine [21], which is nearly five times the prevalence observed in our study. This discrepancy may be due to difference in the follow-up periods; in our study, the UIC was assessed after one week, whereas Erdoğan et al. [21] evaluated it after three months, which may have led to a cumulative increase in UIC.
Our study revealed a significant difference in the UIC based on the frequency of scrubbing in the povidone-iodine scrub group. Those with ≥10 scrubs per week exhibited significantly higher UICs compared to others in this group. Nesvadbova et al. in Italy demonstrated a significant statistical relationship between UIC and the number of povidone-iodine scrubs, where surgical staff performing ≥20 scrubs per week displaying higher UIC than others [18]. Our findings are consistent with their results. In our study, in the povidone-iodine scrub group, those with ≥ 10 shifts per week exhibited significantly higher UIC compared to those with <10 shifts per week. Similar to our findings, Idiz et al. in Turkey reported that operating room staff who worked at least four consecutive shifts per week and used povidone-iodine for hand scrubbing had higher UIC [17]. In contrast, Michalaki et al. in Greece found no significant correlation between UIC and the number of working days among operating room staff using povidone-iodine scrub [24]. This discrepancy may be due to differences in UIC measurement methods and sample sizes among the studies.
This study had some limitations. The UIC was not measured before the study, which can potentially affect the results. The sampling was done by a convenience method, which may lead to selection bias. Other factors, such as dietary habits, were not fully examined which may affect the study results. Also, the generalizability of the results should be done with caution. Further interventional studies are recommended.
Based on the findings, we recommend the operating room personnel to use alternative hand scrubbing solutions, such as alcohol-based solutions. The use of povidone-iodine scrub can increase UIC in operating room personnel, particularly in those at risk of iodine toxicity or with a history of thyroid disorders, such as pregnant women. These individuals may need to consider alternative hand scrubbing solutions or reduce their frequency of povidone-iodine scrub use.
Ethical Considerations
Compliance with ethical guidelines
This study obtained ethical approval from the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran (Code: IR.ARI.MUI.REC.1401.047). Informed written consent was obtained from all participants after describing the study objectives. They were free to leave the study at any time.
Funding
This article was extracted from the master’s thesis of Fateme Karbalai, approved by Isfahan University of Medical Sciences and financially supported by Isfahan University of Medical Sciences, Isfahan, Iran.
Authors' contributions
Conceptualization, study design, review & editing: Fateme Karbalai and Soheila Bakhtiari; Methodology: Soheila Bakhtiari and Farzaneh Jafari; Sampling, writing the original daft: Fateme Karbalai; Data analysis: Fateme Karbalai and Farzaneh Jafari; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research of Isfahan University of Medical Sciences for financial support, and all the operating room staff who participated in this study for their cooperation.
References
Effective hand scrubbing and disinfection are crucial, particularly before wearing sterile gloves for surgery, as a study found that surgical gloves have perforations in 5.9% of cases [1, 2]. There are two main types of hand sanitizers, including alcoholic and non-alcoholic (povidone-iodine, hexachlorophene, Chlorhexidine gluconate and Hibitane) [3-5]. The materials used for hand sanitizing, particularly in surgical operations, are diverse. Povidone-iodine solution (7.5% betadine) is the most well-known and widely used solution [6]. As a topical antiseptic agent in the form of an iodophor, povidone-iodine reduces the irritating effects of iodine [7]. One of its key characteristics is its high bactericidal activity, which is capable of killing a broad spectrum of microorganisms within 3-5 minutes due to the presence of iodine [8]. However, excessive iodine consumption can lead to poisoning in individuals, with a tolerable intake level of 1100 µg/day for people aged >19 years [9]. The complications and symptoms of iodine poisoning are diverse, ranging from gastrointestinal symptoms (headache, dizziness and nausea) to metabolic and hormonal disorders, including thyroid gland disorders [10, 11].
Despite the limited and negligible side effects of povidone-iodine (7.5% betadine) in case of prolonged use (approximately ≥3 hours), this substance has demonstrated acceptable efficacy [11, 12]. Consequently, it remains a widely used agent in surgical rooms for hand sanitizing [13]. Povidone-iodine exhibits a broad-spectrum antimicrobial effect, displaying high sensitivity against gram-negative and gram-positive bacteria, acidophiles, fungi, amoebic cysts and spores [14-16]. Research has shown that prolonged skin exposure to iodine (≥3 hours) can result in limited absorption [17, 18]. Additionally, the widespread use of amiodarone and iodinated radiological contrast agents has been found to expose the body to high doses of exogenous iodine [7].
The routine use of povidone-iodine solution may be a potential cause of iodine poisoning in operating room personnel, as evidenced by elevated urinary iodine levels [19]. A study revealed that the average urinary iodine level one week after using povidone-iodine for sanitizing was significantly higher than the pre-use period [20]. Furthermore, some studies have suggested that povidone-iodine solution can be absorbed through the skin or mucous membrane due to its high iodine content [17, 18]. However, contradictory results have been reported in other studies [17, 21]. For instance, a study found that the urinary iodine level of operating room personnel in Turkey was at an average level, despite the regular use of povidone-iodine for hand sanitizing, and it did not show elevated levels [21]. This finding highlights the conflicting evidence concerning the skin absorption of iodine from povidone-iodine solutions and its potential impact on the health of operating room personnel [17, 20, 21]. This study aimed to measure the urinary iodine concentration (UIC) in operating room personnel of a hospital in Isfahan, Iran, who used povidone-iodine solution (betadine 7.5%) for hand scrubbing.
Materials and Methods
This is a descriptive-analytical study. A total of 100 operating room personnel (technologists and scrub nurses) were selected from a hospital affiliated to Isfahan University of Medical Sciences in 2022, using a convenience sampling method. The inclusion criteria were consent to participate, no wounds on hand skin up to 5 cm above the elbow, self-report of no skin dermatitis, not receiving iodinated contrast agents during the study, no history of taking certain medications or supplements related to iodine, no history of iodine deficiency or thyroid disorders, no history of thyroidectomy and not following a special diet that includes excessive seafood (≥3 times a week). The exclusion criteria were unwillingness to continue participation, development of skin wounds or scratches during the study, and inconsistent use of povidone-iodine and alcohol solutions for scrubbing. To determine the sample size, the formula for estimating proportions was used [18]. By considering a maximum estimation error of 0.05 at a confidence level of 95% (Z1−α/2=1.96) and a precision (d) of 7.5%, the minimum sample size was calculated to be 100 (50 per group). The study hospital has two operating rooms. We selected 50 personnel from one operating room and assigned them to the povidone-iodine scrub group, while 50 personnel from the second operating room were assigned to the alcohol-based scrub group. The work-related and demographic data were collected using a form surveying age, gender, work experience, educational level, frequency of scrubbing per week, and number of shifts per week. The UIC was measured for both groups using the Sandell-Kolthoff reaction method. This method is popular for its accuracy and sensitivity in measuring urinary iodine, showing reliable results [17, 18].
Before the study, participants were trained on the standard surgical scrub method, which involved scrubbing the four surfaces of each finger, the outside of the fifth finger, the back of the hand, the palm, from the little finger to the thumb, from the wrist to the arm (three times), and up to 5 cm above the elbow [22]. The betadine used during the study was made by a pharmaceutical company that had a contract with the hospital (The participants, the person responsible for measuring the UIC in the laboratory and the researchers did not have information about the name of the company). The betadine was poured into the betadine storage containers in the scrub rooms by the person in charge of operating room equipment. In both groups, scrubbing was performed for one week, three times a day, each for three minutes, using 3-5 mL of povidone-iodine or alcoholic solution. All procedures were carried out under the supervision of the researcher. Participants were instructed to maintain their usual diet and avoid using chemical or herbal medications during this period.
One week after the study, morning urine samples were collected from the participants on a single day. Prior to sampling, comprehensive instructions on urine sampling procedures (initially washing the external urinary tract with water and then collecting mid-stream urine) were provided by the researcher. These instructions were given individually and face-to-face in a private area within the operating rooms. If any confusion arose, further explanations were provided to the participants. Mmidstream urine samples were placed in deionized test tubes with lids shut tightly, placed in cool boxes, maintained at a temperature of 2-8 °C, and transported to the Comprehensive Research Laboratory of Isfahan University of Medical Sciences immediately. The samples were acidified and stored under -20 °C until analysis. The UIC was subsequently measured by the modified Sandell-Kolthoff method using a microplate technique, adhering to the recommendations of the centers for disease control and prevention. The measurement was done by a laboratory expert, and the researcher was responsible for ensuring the accuracy of this measurement. The urine samples were initially dissolved at room temperature and then incubated for 30 minutes with 0.9 M ammonium persulfate at 95 °C using a thermal cycler. After cooling, 50 μL of the processed urine samples were placed into the wells of a microplate. Subsequently, 100 μL of a 0.05 M arsenious acid solution was added to each well and mixed properly. In the final step, 50 μL of a 0.019 M ceric ammonium sulfate solution was added. After a 30-min incubation at 25 °C, absorbance was measured at 405 nm. The UIC was calculated by plotting a standard curve and reported in micrograms per liter (μg/L) [17, 23]. A UIC≤300 μg/L shows normal range, and ˃300 μg/L indicates a potential risk for abnormal thyroid function [17].
Data analysis was performed in SPSS software, version 25 (IBM Corporation, Chicago, IL). The normality of data distribution was assessed using the Shapiro-Wilk test. Quantitative data were presented as Mean±SD or median ±95% interquartile range. The differences between groups were analyzed using the Chi-square test or Mann-Whitney U-test (for non-parametric variables). The significance level was set at 0.05.
Results
A comparison of the povidone-iodine scrub group with the alcohol-based scrub group revealed no significant differences in terms of age (31.9±6.29 vs 31.7±5.59 years), work experience (3.90±1 vs 4.08±1.69 years), gender (94% vs 86% female), educational level (92% vs 94% with a bachelor’s degree), frequency of scrubbing (78% vs 74% with >6 shifts per week) and shifts per week (Table 1).
However, the UIC was significantly higher in the povidone-iodine scrub group (289.9±73.19 vs 106.6±27.88 μg/L; P=0.001).These findings were shown in Table2.
Furthermore, the UIC at a level indicating excessive iodine intake (˃300 µg/L) was significantly higher in the povidone-iodine scrub group compared to the alcohol-based scrub group (8% vs 0%; P=0.001) that was shown in Table 3.
In the povidone-iodine scrub group, the UIC was significantly higher in females (296.3±70.82 vs 190.1±0.95 μg/L; P=0.032), in those who scrubbed ≥10 times per week (316.3± 54.20 vs 196.5±52.54 μg/L; P=0.001), and in those who worked ≥6 shifts per week (299.3±66.9 vs 206.2±81.6 μg/L; P=0.011). However, no significant differences were found in the UIC based on age, work experience, or educational level. In the alcohol-based scrub group, no significant differences were observed in the UIC based on any factors (Table 4).
Discussion
This study demonstrated that, among operating room personnel, the UIC in the povidone-iodine scrub group was significantly higher than in the alcohol-based scrub group. A similar study reported that rinsing the mouth with povidone-iodine increased the serum iodine level by 2-3 times and the UIC by 5 times [20]. Our results are also in line with previous studies, which showed that using hand sanitizers containing iodine increased UIC and suggested that operating room personnel should take necessary measures to control iodine exposure [17, 21]. Our findings differed from these studies; we compared an alcohol-based solution with povidone-iodine, while these two studies only examined povidone-iodine. A laboratory study by Nesvadbova et al. demonstrated that iodine in povidone-iodine solution can be absorbed through skin cells to a significant extent [18]. The authors suggested that frequent professional contact with the povidone-iodine solution as a skin scrub can lead to iodine penetration through the skin. Our study’s findings are in agreement with the results of this study.
Our study revealed that 80.0% of operating room personnel in the povidone-iodine scrub group had extremely high intake levels, indicating iodine poisoning, whereas none of the participants in the control group had excessive intake levels. Idiz et al. in Turkey reported that 7.5% of surgical staff who scrubbed with povidone-iodine had iodine poisoning [17]. Our findings are consistent with their findings. However, Erdoğan et al. in Turkey reported a higher prevalence of excessive intake level (approximately 39%) among operating room staff who scrubbed with povidone-iodine [21], which is nearly five times the prevalence observed in our study. This discrepancy may be due to difference in the follow-up periods; in our study, the UIC was assessed after one week, whereas Erdoğan et al. [21] evaluated it after three months, which may have led to a cumulative increase in UIC.
Our study revealed a significant difference in the UIC based on the frequency of scrubbing in the povidone-iodine scrub group. Those with ≥10 scrubs per week exhibited significantly higher UICs compared to others in this group. Nesvadbova et al. in Italy demonstrated a significant statistical relationship between UIC and the number of povidone-iodine scrubs, where surgical staff performing ≥20 scrubs per week displaying higher UIC than others [18]. Our findings are consistent with their results. In our study, in the povidone-iodine scrub group, those with ≥ 10 shifts per week exhibited significantly higher UIC compared to those with <10 shifts per week. Similar to our findings, Idiz et al. in Turkey reported that operating room staff who worked at least four consecutive shifts per week and used povidone-iodine for hand scrubbing had higher UIC [17]. In contrast, Michalaki et al. in Greece found no significant correlation between UIC and the number of working days among operating room staff using povidone-iodine scrub [24]. This discrepancy may be due to differences in UIC measurement methods and sample sizes among the studies.
This study had some limitations. The UIC was not measured before the study, which can potentially affect the results. The sampling was done by a convenience method, which may lead to selection bias. Other factors, such as dietary habits, were not fully examined which may affect the study results. Also, the generalizability of the results should be done with caution. Further interventional studies are recommended.
Based on the findings, we recommend the operating room personnel to use alternative hand scrubbing solutions, such as alcohol-based solutions. The use of povidone-iodine scrub can increase UIC in operating room personnel, particularly in those at risk of iodine toxicity or with a history of thyroid disorders, such as pregnant women. These individuals may need to consider alternative hand scrubbing solutions or reduce their frequency of povidone-iodine scrub use.
Ethical Considerations
Compliance with ethical guidelines
This study obtained ethical approval from the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran (Code: IR.ARI.MUI.REC.1401.047). Informed written consent was obtained from all participants after describing the study objectives. They were free to leave the study at any time.
Funding
This article was extracted from the master’s thesis of Fateme Karbalai, approved by Isfahan University of Medical Sciences and financially supported by Isfahan University of Medical Sciences, Isfahan, Iran.
Authors' contributions
Conceptualization, study design, review & editing: Fateme Karbalai and Soheila Bakhtiari; Methodology: Soheila Bakhtiari and Farzaneh Jafari; Sampling, writing the original daft: Fateme Karbalai; Data analysis: Fateme Karbalai and Farzaneh Jafari; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research of Isfahan University of Medical Sciences for financial support, and all the operating room staff who participated in this study for their cooperation.
References
- Assadian O, Harbarth S, Vos M, Knobloch JK, Asensio A, Widmer AF. Practical recommendations for routine cleaning and disinfection procedures in healthcare institutions: A narrative review. J Hosp Infect. 2021; 113:104-14. [doi:10.1016/j.jhin.2021.03.010]
- Thomson I, Krysa N, McGuire A, Mann S. Recognition of intraoperative surgical glove perforation: A comparison by surgical role and level of training. Can J Surg. 2022; 65(1):E82-8. [DOI:10.1503/cjs.016720] [PMID]
- Saha T, Khadka P, Das SC. Alcohol-based hand sanitizer-composition, proper use and precautions. Germs. 2021; 11(3):408-17. [DOI:10.18683/germs.2021.12782] [PMID]
- Hillier MD. Using effective hand hygiene practice to prevent and control infection. Nurs Stand. 2020; 35(5):45-50. [DOI:10.7748/ns.2020.e11552x] [PMID]
- Lotfinejad N, Peters A, Tartari E, Fankhauser-Rodriguez C, Pires D, Pittet D. Hand hygiene in health care: 20 years of ongoing advances and perspectives. Lancet Infect Dis. 2021; 21(8):e209-21. [DOI:10.1016/S1473-3099(21)00383-2] [PMID]
- Barreto R, Barrois B, Lambert J, Malhotra-Kumar S, Santos-Fernandes V, Monstrey S. Addressing the challenges in antisepsis: Focus on povidone iodine. Int J Antimicrob Agents. 2020; 56(3):106064. [DOI:10.1016/j.ijantimicag.2020.106064] [PMID]
- Kameli A, Raoufian H, Besharati R, Akhlaghi D, Azizi R, Gholami S. [The comparative effects of surgical scrub with alcohol based solutions and povidone-iodine on the growth of the bacterial contamination of hands over time: A randomized crossover study (Persian)]. J North Khorasan Univ Med Sci. 2020; 12(3):56-61. [DOI:10.29252/nkjmd-12039]
- Bashir MH, Hollingsworth A, Thompson JD, Shortridge D, Lake SP, Deeken CR, et al. Antimicrobial performance of two preoperative skin preparation solutions containing iodine and isopropyl alcohol. Am J Infect Control. 2022; 50(7):792-8. [DOI:10.1016/j.ajic.2021.10.031] [PMID]
- Sohn SY, Inoue K, Rhee CM, Leung AM. Risks of iodine excess. Endocr Rev. 2024; 45(6):858-79. [DOI:10.1210/endrev/bnae019] [PMID]
- Wells I, Pharm NK, Ezzet S, Shenas CE, Ray SD. Thyroid hormones, iodine, and iodides, and antithyroid drugs. In: Ray SD, editor. Side effects of drugs annual. Amsterdam: ScienceDirect; 2021. [DOI:/10.1016/bs.seda.2020.07.003]
- Southern AP, Anastasopoulou C, Jwayyed S. Iodine toxicity. StatTreasure Island: Pearls Publishing; 2024. [Link]
- Bai D, Zhou F, Wu L. Comparing the efficacy of chlorhexidine and povidone-iodine in preventing surgical site infections: A systematic review and meta-analysis. Int Wound J. 2023; 21(2):e14463. [DOI:10.1111/iwj.14463] [PMID]
- Wade RG, Burr NE, McCauley G, Bourke G, Efthimiou O. The comparative efficacy of chlorhexidine gluconate and povidone-iodine antiseptics for the prevention of infection in clean surgery: A systematic review and network meta-analysis. Ann Surg. 2021; 274(6):e481-8. [DOI:10.1097/SLA.0000000000004076] [PMID]
- Coles VE, Puri L, Bhandari M, Wood TJ, Burrows LL. The effects of chlorhexidine, povidone-iodine and vancomycin on growth and biofilms of pathogens that cause prosthetic joint infections: An in-vitro model. J Hosp Infect. 2024; 151:99-108. [DOI:10.1016/j.jhin.2024.06.010] [PMID]
- Lepelletier D, Maillard JY, Pozzetto B, Simon A. Povidone Iodine: Properties, mechanisms of action, and role in infection control and staphylococcus aureus decolonization. Antimicrob Agents Chemother. 2020; 64(9):e00682-20. [DOI:10.1128/AAC.00682-20] [PMID]
- Eggers M. Infectious disease management and control with povidone iodine. Infect Dis Ther. 2019; 8(4):581-93. [DOI:10.1007/s40121-019-00260-x] [PMID]
- Idiz C, Altun A, Basaran-Kucukgergin C, Kofoglu Z, Sormaz IC, Yarman S. Effect of iodine-containing antiseptics on urine iodine levels of surgical staff after iodization. Turkish Journal of Biochemistry. 2020; 45(3):277-81. [DOI:10.1515/tjb-2019-0090]
- Nesvadbova M, Crosera M, Maina G, Larese Filon F. Povidone iodine skin absorption: An ex-vivo study. Toxicol Lett. 2015; 235(3):155-60. [DOI:10.1016/j.toxlet.2015.04.004] [PMID]
- Wang D, Huang X, Lv W, Zhou J. The toxicity and antibacterial effects of povidone-iodine irrigation in fracture surgery. Orthop Surg. 2022; 14(9):2286-97. [DOI:10.1111/os.13422] [PMID]
- Gou L, Zhao R, Ren X, Li Y, Ji P. Oral transmucosal absorption of iodine after intraoral preparation with povidone-iodine prior to oral surgeries: A randomized controlled study in 12 male patients. Clin Oral Investig. 2022; 26(1):705-11. [DOI:10.1007/s00784-021-04048-7] [PMID]
- Erdoğan MF, Tatar FA, Unlütürk U, Cin N, Uysal AR. The effect of scrubbing hands with iodine-containing solutions on urinary iodine concentrations of the operating room staff. Thyroid. 2013; 23(3):342-5. [DOI:10.1089/thy.2012.0325] [PMID]
- Phillips N, Hornacky A. Berry & Kohn's operating room technique-e-book. Edinburgh: Elsevier Health Sciences; 2020. [Link]
- Anbardar MH, Afshari A, Ashraf MJ. [Evaluation of urinary iodine by sandell-kolthoff reaction method in urban and rural children referring to the shiraz shahid motahari clinic and village of marvdasht city in 2016 and 2017 (Persian)]. Jundishapur Sci Med J. 2021; 20(3):272-9. [DOI:10.32598/JSMJ.20.3.2046]
- Michalaki M, Pylioti A, Loutas V, Mamali I, Markou KB. Absence of differences in urinary iodine excretion and thyroid function tests in operating room staff members using or not using iodine-containing antiseptic solutions. Thyroid. 2013; 23(12):1659-60. [DOI:10.1089/thy.2013.0218] [PMID]
Article Type : Research |
Subject:
General
Received: 2023/12/18 | Accepted: 2025/03/30 | Published: 2025/04/1
Received: 2023/12/18 | Accepted: 2025/03/30 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |