Wed, Jan 28, 2026
Volume 36, Issue 1 (1-2026)
JHNM 2026, 36(1): 72-81 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zokaei F, Kamalinejad M, Farid M, Pirak A, Yazdkhasti M. Effect of Green Ocimum Basilicum Leaf Extract Capsule on the Quality of Life of Postmenopausal Women: A Randomized, Placebo-Controlled, Clinical Trial. JHNM 2026; 36 (1) :72-81
URL: http://hnmj.gums.ac.ir/article-1-2251-en.html
URL: http://hnmj.gums.ac.ir/article-1-2251-en.html
1- Instructor, Department of Midwifery, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
2- Associate Professor, Department of Pharmacy, School of Pharmacy, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Associate Professor, Department of Community Medicine and Epidemiology, School of Medicine, Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran.
4- Assistant Professor, Department of Midwifery, School of Nursing and Midwifery, Iranshahr University of Medical Sciences, Iranshahr, Iran.
5- Associate Professor, Department of Midwifery and Reproductive Health, Social Determinants of Health Research Center, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran. ,Mansoyazd@yahoo.com
2- Associate Professor, Department of Pharmacy, School of Pharmacy, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Associate Professor, Department of Community Medicine and Epidemiology, School of Medicine, Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran.
4- Assistant Professor, Department of Midwifery, School of Nursing and Midwifery, Iranshahr University of Medical Sciences, Iranshahr, Iran.
5- Associate Professor, Department of Midwifery and Reproductive Health, Social Determinants of Health Research Center, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran. ,
Full-Text [PDF 644 kb]
(52 Downloads)
| Abstract (HTML) (138 Views)
Full-Text: (3 Views)
Introduction
Menopause causes various changes in women’s physical, psychosocial, and sexual functioning that can significantly affect their Quality of Life (QOL) across different physical, psychosocial, and sexual aspects [1]. Symptoms of menopause and sociodemographic factors influence the QOL of postmenopausal women [1, 2]. Each year, half a million women is added to the middle-aged population of women. The average age of menopause is 51 years in the world, and 47.8 years in Iran. In 2022, about 5 million menopausal women were living in Iran [2, 3]. The most common symptoms of menopause include vasomotor symptoms. Most menopausal women complain of hot flashes, joint and bone pain, depression, and decreased sexual desire [3].
There is a wide range of therapeutic methods to control menopause symptoms, including Hormone Replacement Therapy (HRT), acupressure, various herbal compounds, acupuncture, massage therapy, and lifestyle changes, including exercise (yoga) and a healthy diet [4]. Decision-making regarding the treatment of menopausal symptoms is inherently complex and has increased over the past decade [5]. This complexity, in addition to the existing challenges in HRT and the uncertainty about the effects of other methods, such as Complementary and Alternative Medicine (CAM), may be due to the different nature of decision-making regarding the treatment of menopausal symptoms compared to other health fields. Since menopausal symptoms are common in all women, there is no single treatment for all symptoms, and even treating one symptom may aggravate other symptoms [6]. Reported hot flashes in postmenopausal women vary between different countries. In women from European and North American countries, the rate of hot flashes is 70-80%, while it is 14-25% in Japanese, Chinese, and Southeast Asian women. This difference is due to many factors. One possible factor is the presence of phytoestrogen-containing plants in the food [7, 8]. Phytoestrogens are plant compounds with estrogenic activity [9]. These plants have a special place in improving or treating menopause symptoms. Many plants, such as black cohosh, Panax ginseng, Glycine max, Trifolium pratense, Vitex agnus-castus [10], Trigonella foenum-graecum [11], Passiflora incarnata [12], and Salvia officinalis extract [13] are among this group. Their use has been shown to reduce menopausal symptoms [14].
One medicinal plant commonly used to alleviate menopausal symptoms is sweet basil (Ocimum basilicum L.), a member of the Lamiaceae family [15]. It is the only species of this family that is cultivated in Iran [8]. The green leaves of this plant are traditionally used for various medicinal purposes such as improving memory, reducing anxiety and depression, relieving bone and joint pain, and promoting a sense of well-being. The Green O. basilicum Leaf Extract (GOBLE) capsules contain phytoestrogens, such as flavonoids and coumarins, which mimic estrogen and bind to estrogen receptors, making it beneficial for postmenopausal women experiencing hormonal decline. These compounds may help alleviate menopausal symptoms, including hot flashes and mood swings, by exerting weak estrogenic effects. Additionally, the antioxidants in green basil combat oxidative stress and inflammation, supporting overall hormonal health and reducing the risk of chronic conditions. The phytoestrogens in green basil may play a significant role in improving the QOL in postmenopausal women [15, 16]. Given the global trend and increasing interest in CAM and herbal medicines [17, 18], as well as the importance of QOL studies on menopausal women, this study aimed to evaluate the impact of GOBLE capsules on the QOL of menopausal women in Iran.
Materials and Methods
This is a double-blind, randomized clinical trial involving 80 women at a teaching hospital affiliated with Alborz University of Medical Sciences in Karaj, Iran, from November 2019 to May 2022. The sample size was estimated according to Taavoni et al.’s study on the effect of Lemon Balm supplementation on menopausal symptoms [19]. The sample size was calculated (n=80) using G*Power software, version 3.1, by considering α=0.05, Effect size (d)=0.72, test power (1-β) =0.90, and a 5% sample dropout rate. Inclusion criteria were a natural menopause (absence of menstruation in the last 12 months) and experiencing menopausal symptoms, being married, not having menopause due to chemotherapy or radiation therapy, not using HRT or herbal phytoestrogens, not consuming alcohol, tobacco, or drugs; no sensitivity to the plants from the Lamiaceae family or other phytoestrogen-contaning plants, and no history of unknown vaginal bleeding, diabetes, or hypertension. Exclusion criteria were unwillingness to continue participation in the research or failure to take medication regularly. For allocation concealment, the capsules and placebos were sequentially placed in sealed, opaque envelopes. The code for eligible participants to enter the study was the same as the code on the capsules’ labels.
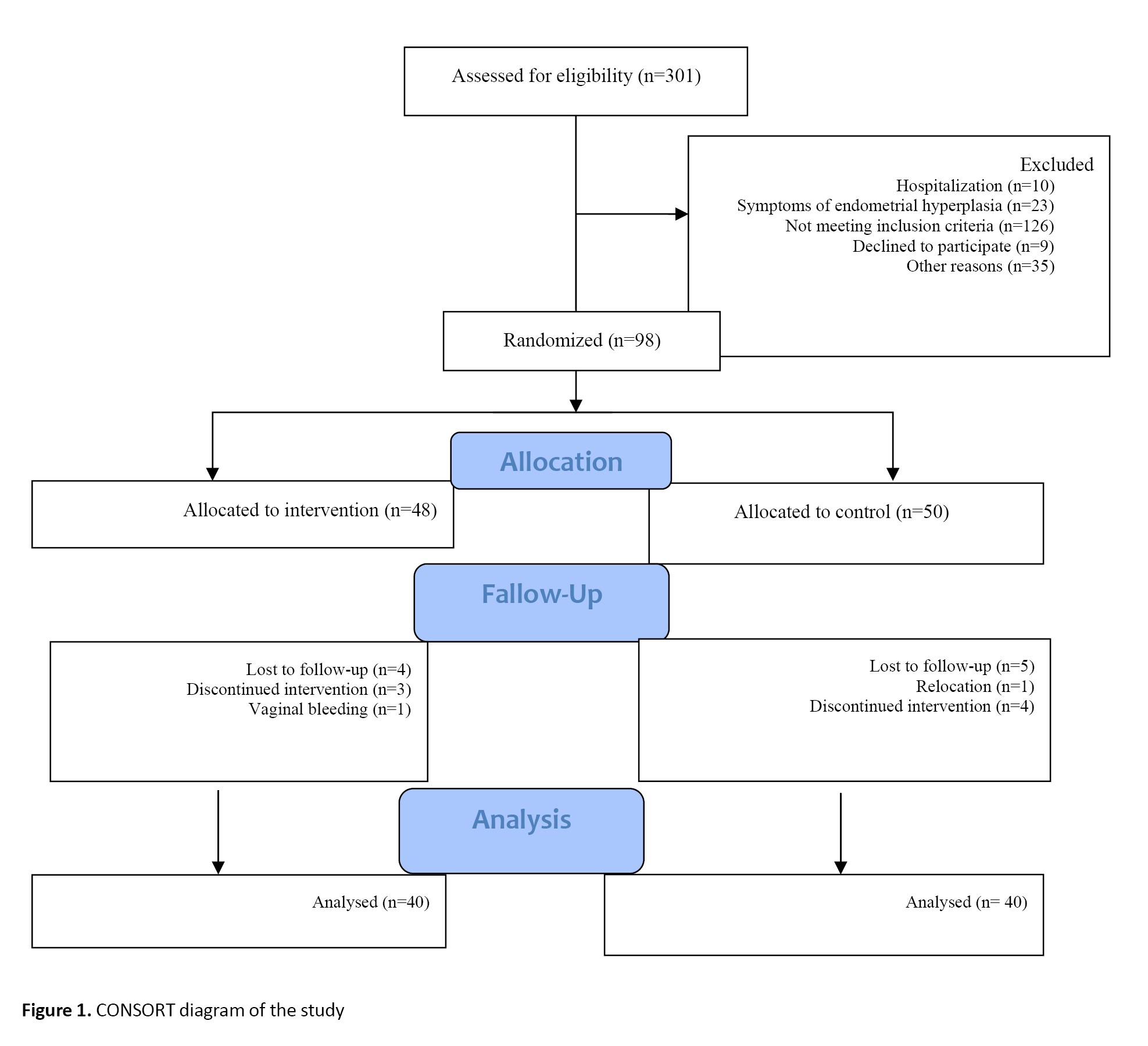
First, a list of menopausal women reporting menopausal symptoms was prepared from the patient files by referring to the gynecology department’s medical records. Next, we contacted the women by phone, explained the study objectives, and invited them to attend the relevant center at the scheduled time (Figure 1).
Menopause causes various changes in women’s physical, psychosocial, and sexual functioning that can significantly affect their Quality of Life (QOL) across different physical, psychosocial, and sexual aspects [1]. Symptoms of menopause and sociodemographic factors influence the QOL of postmenopausal women [1, 2]. Each year, half a million women is added to the middle-aged population of women. The average age of menopause is 51 years in the world, and 47.8 years in Iran. In 2022, about 5 million menopausal women were living in Iran [2, 3]. The most common symptoms of menopause include vasomotor symptoms. Most menopausal women complain of hot flashes, joint and bone pain, depression, and decreased sexual desire [3].
There is a wide range of therapeutic methods to control menopause symptoms, including Hormone Replacement Therapy (HRT), acupressure, various herbal compounds, acupuncture, massage therapy, and lifestyle changes, including exercise (yoga) and a healthy diet [4]. Decision-making regarding the treatment of menopausal symptoms is inherently complex and has increased over the past decade [5]. This complexity, in addition to the existing challenges in HRT and the uncertainty about the effects of other methods, such as Complementary and Alternative Medicine (CAM), may be due to the different nature of decision-making regarding the treatment of menopausal symptoms compared to other health fields. Since menopausal symptoms are common in all women, there is no single treatment for all symptoms, and even treating one symptom may aggravate other symptoms [6]. Reported hot flashes in postmenopausal women vary between different countries. In women from European and North American countries, the rate of hot flashes is 70-80%, while it is 14-25% in Japanese, Chinese, and Southeast Asian women. This difference is due to many factors. One possible factor is the presence of phytoestrogen-containing plants in the food [7, 8]. Phytoestrogens are plant compounds with estrogenic activity [9]. These plants have a special place in improving or treating menopause symptoms. Many plants, such as black cohosh, Panax ginseng, Glycine max, Trifolium pratense, Vitex agnus-castus [10], Trigonella foenum-graecum [11], Passiflora incarnata [12], and Salvia officinalis extract [13] are among this group. Their use has been shown to reduce menopausal symptoms [14].
One medicinal plant commonly used to alleviate menopausal symptoms is sweet basil (Ocimum basilicum L.), a member of the Lamiaceae family [15]. It is the only species of this family that is cultivated in Iran [8]. The green leaves of this plant are traditionally used for various medicinal purposes such as improving memory, reducing anxiety and depression, relieving bone and joint pain, and promoting a sense of well-being. The Green O. basilicum Leaf Extract (GOBLE) capsules contain phytoestrogens, such as flavonoids and coumarins, which mimic estrogen and bind to estrogen receptors, making it beneficial for postmenopausal women experiencing hormonal decline. These compounds may help alleviate menopausal symptoms, including hot flashes and mood swings, by exerting weak estrogenic effects. Additionally, the antioxidants in green basil combat oxidative stress and inflammation, supporting overall hormonal health and reducing the risk of chronic conditions. The phytoestrogens in green basil may play a significant role in improving the QOL in postmenopausal women [15, 16]. Given the global trend and increasing interest in CAM and herbal medicines [17, 18], as well as the importance of QOL studies on menopausal women, this study aimed to evaluate the impact of GOBLE capsules on the QOL of menopausal women in Iran.
Materials and Methods
This is a double-blind, randomized clinical trial involving 80 women at a teaching hospital affiliated with Alborz University of Medical Sciences in Karaj, Iran, from November 2019 to May 2022. The sample size was estimated according to Taavoni et al.’s study on the effect of Lemon Balm supplementation on menopausal symptoms [19]. The sample size was calculated (n=80) using G*Power software, version 3.1, by considering α=0.05, Effect size (d)=0.72, test power (1-β) =0.90, and a 5% sample dropout rate. Inclusion criteria were a natural menopause (absence of menstruation in the last 12 months) and experiencing menopausal symptoms, being married, not having menopause due to chemotherapy or radiation therapy, not using HRT or herbal phytoestrogens, not consuming alcohol, tobacco, or drugs; no sensitivity to the plants from the Lamiaceae family or other phytoestrogen-contaning plants, and no history of unknown vaginal bleeding, diabetes, or hypertension. Exclusion criteria were unwillingness to continue participation in the research or failure to take medication regularly. For allocation concealment, the capsules and placebos were sequentially placed in sealed, opaque envelopes. The code for eligible participants to enter the study was the same as the code on the capsules’ labels.
First, a list of menopausal women reporting menopausal symptoms was prepared from the patient files by referring to the gynecology department’s medical records. Next, we contacted the women by phone, explained the study objectives, and invited them to attend the relevant center at the scheduled time (Figure 1).
Then, their written consent was obtained. The participants were randomly assigned to two intervention (n=40) and control (n=40) groups using random sampling by quadruple random blocks. The first participant was randomly assigned to either the intervention or the control group via simple random sampling, using a lottery or a random number generator. Then, we defined a block size of 4 (each block consisting of 2 participants in the intervention group and 2 in the control group). Next, we created randomized sequences for each block of four. This method ensured that, at the end of each block, both groups had an equal number of participants, effectively preventing significant imbalances that could affect the study’s outcomes. The process was repeated for subsequent blocks until all participants were assigned, with each new block following the same randomized order. Blinding was ensured by having an expert (the second author) prepare and label the capsules and manage group allocation. Neither the participants nor the first author who administered the intervention and collected outcome data were aware of the group assignments. This approach ensured a double-blind design, minimizing potential bias.
The sociodemographic form collected information on participants’ characteristics, including age, Body Mass Index (BMI), occupation, educational level, age at menopause, and the number of living or deceased children. The Menopause-specific Quality of Life (MENQOL) questionnaire was used to measure the impact of menopausal symptoms on the QOL. It has 29 items covering vasomotor (3 items), psychosocial (7 items), physical (16 items), and sexual (3 items) domains of symptoms. The total scores for the four dimensions are 3-24, 7-56, 16-128, and 3-24, respectively. The total score for the overall scale ranges from 29 to 232, with higher scores indicating a lower QOL [20]. The Persian version of this questionnaire was validated in our other study [21]. The test re-test reliability, as measured by the intraclass correlation coefficient, was 0.84 for the overall MENQOL, 0.80 for the vasomotor domain, 0.79 for the psychosocial domain, 0.82 for the physical domain, and 0.83 for the sexual domain.
For the intervention group, 250 mg of GOBLE capsules (green basil leaf powder) was prescribed to be taken for 8 consecutive weeks, twice a day, every 12 hours, with breakfast and dinner. The capsules were prepared in Iran under the supervision of a professor of pharmacognosy (Mohammad Kamalinejad). The green basil leaves were collected from the Qasemabad Farm in Karaj, Iran. They were confirmed and registered in the Herbarium of the Faculty of Pharmacy, Shahid Beheshti University of Medical Sciences (No.: SBMU-1084 A). To prepare the GOBLE capsules, the fresh green basil leaves were first dried in the laboratory at 25 ͦC. Then, 100 g of dry leaves were added to 1000 cc of ethanol-water solvent (50% each) in a dish and macerated for 48 hours in the laboratory. Next, the extract was filtered, concentrated, dried in a bain-marie bath (freezing bath), ground in a mill, and placed in 250 mg capsules. For the control group, placebo capsules were used. The capsules were made of 250 mg corn starch, dipped in edible green color, and filled with green basil essential oil with the same color, smell, weight, and packaging as the original capsule used in the intervention group. The placebo was also prepared in the same pharmaceutical laboratory under the supervision of an expert in pharmacognosy (Mohammad Kamalinejad). The researcher monitored patients’ adherence to medication usage by providing them with a checklist.
Data were collected via self-reporting before the intervention and one and two months after the intervention. Statistical analysis was conducted in SPSS software, version 23. Chi-square and Fisher’s exact tests were used to analyze the qualitative variables. The quantitative data were presented as Mean±SD. The normality of the data was assessed based on the Skewness and Kurtosis values. Nonparametric tests such as the Mann-Whitney U test, the Wilcoxon test, and Friedman’s test were used for variables with abnormal distributions, while parametric tests, including the independent t-test, the paired t-test, and the repeated measures ANOVA, were used for variables with normal distributions. The significance level was set at 0.05.
Results
In this study four participants in the intervention group and 5 participants in the control group were lost to follow-up and finally the participants included 80 women (40 in each group). The majority of women were in the age range of 47-51 years (51.4% in the intervention group and 43.6% in the control group). The age at menopause for the majority of women in both groups was in the range of 48-52 years (55% in the intervention group and 59% in the control group). The intervention and control groups were homogeneous with respect to age, age at menopause, BMI, number of living or deceased children, education level, and occupation before the intervention (Table 1).

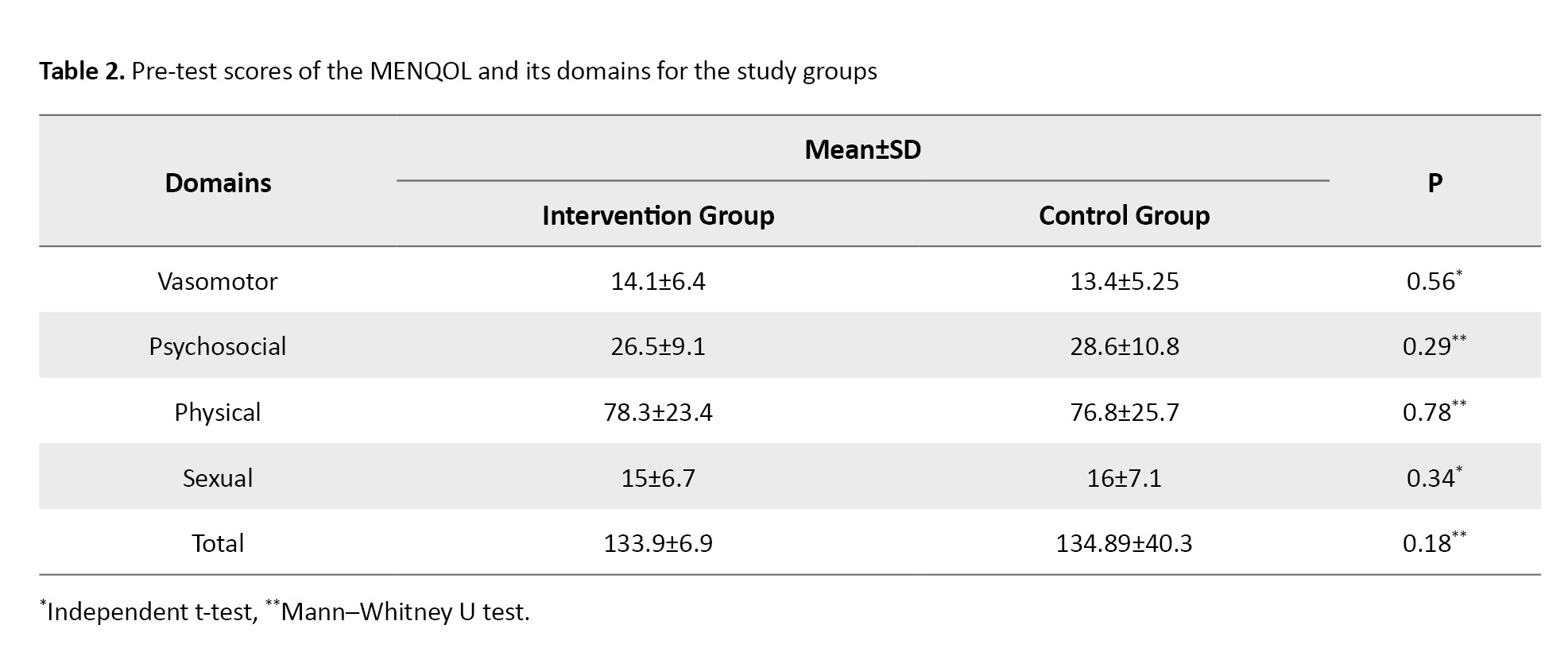
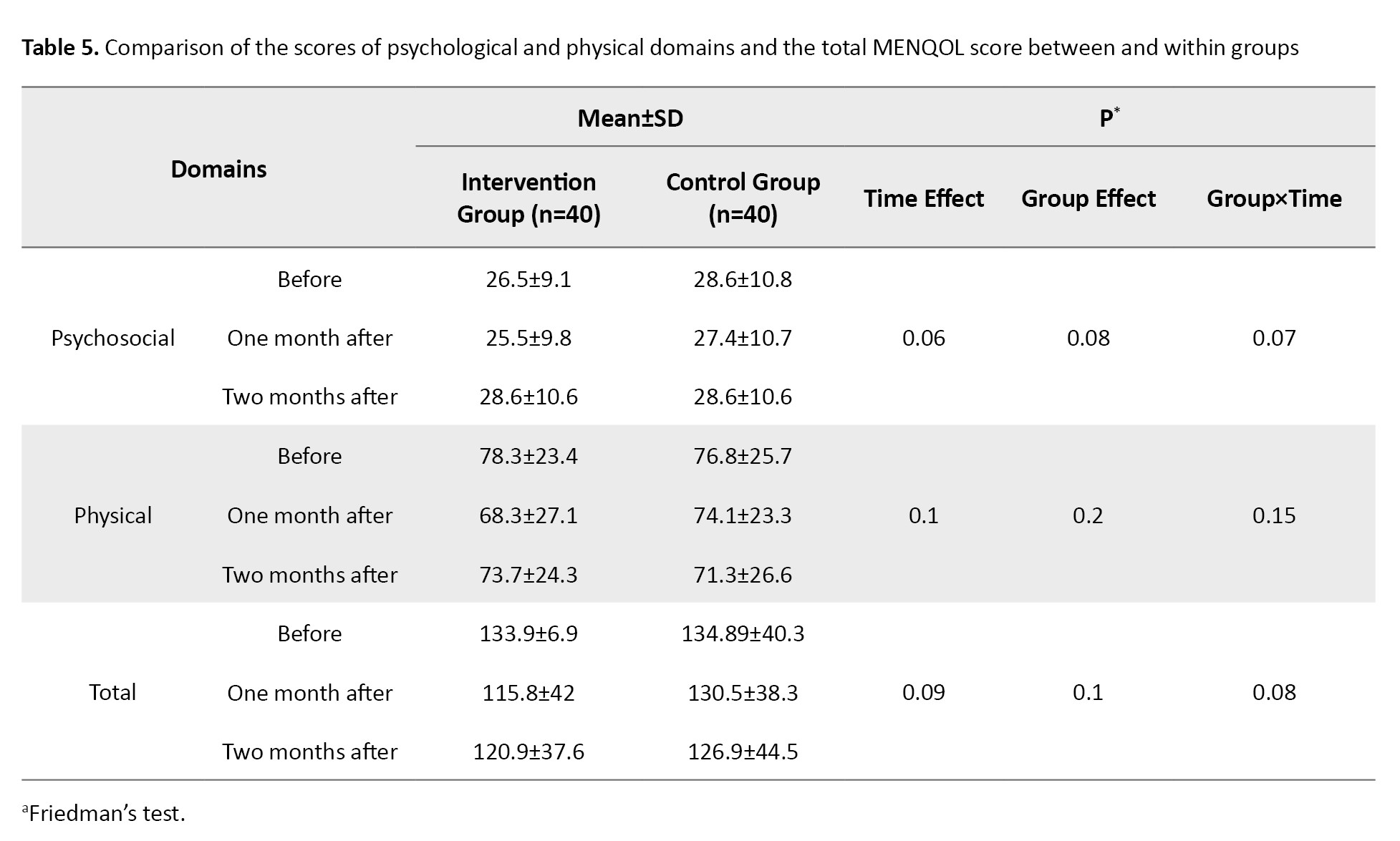
Baseline MENQOL scores were not significantly different between the two groups before the intervention (Table 2).
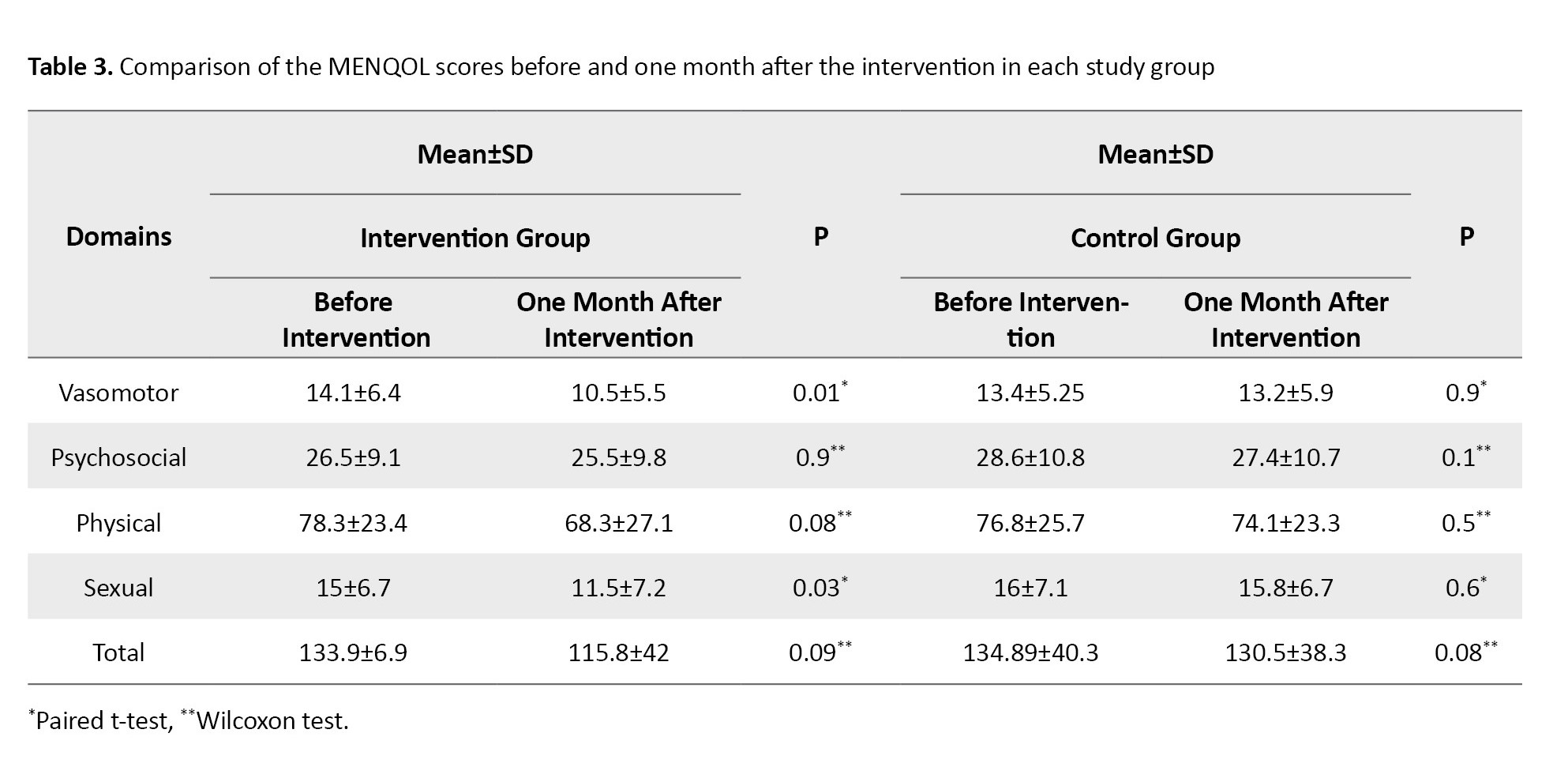
The results of the paired t-test for the intervention group showed that before and one month after the intervention, there was a statistically significant reduction in vasomotor (P=0.01) and sexual (P=0.03) dimensions, but not in psychosocial and physical dimensions and total score based on the results of the Wilcoxon test. In the control group, no statistically significant difference was found one month after the intervention in MENQOL total score or domain scores (Table 3).
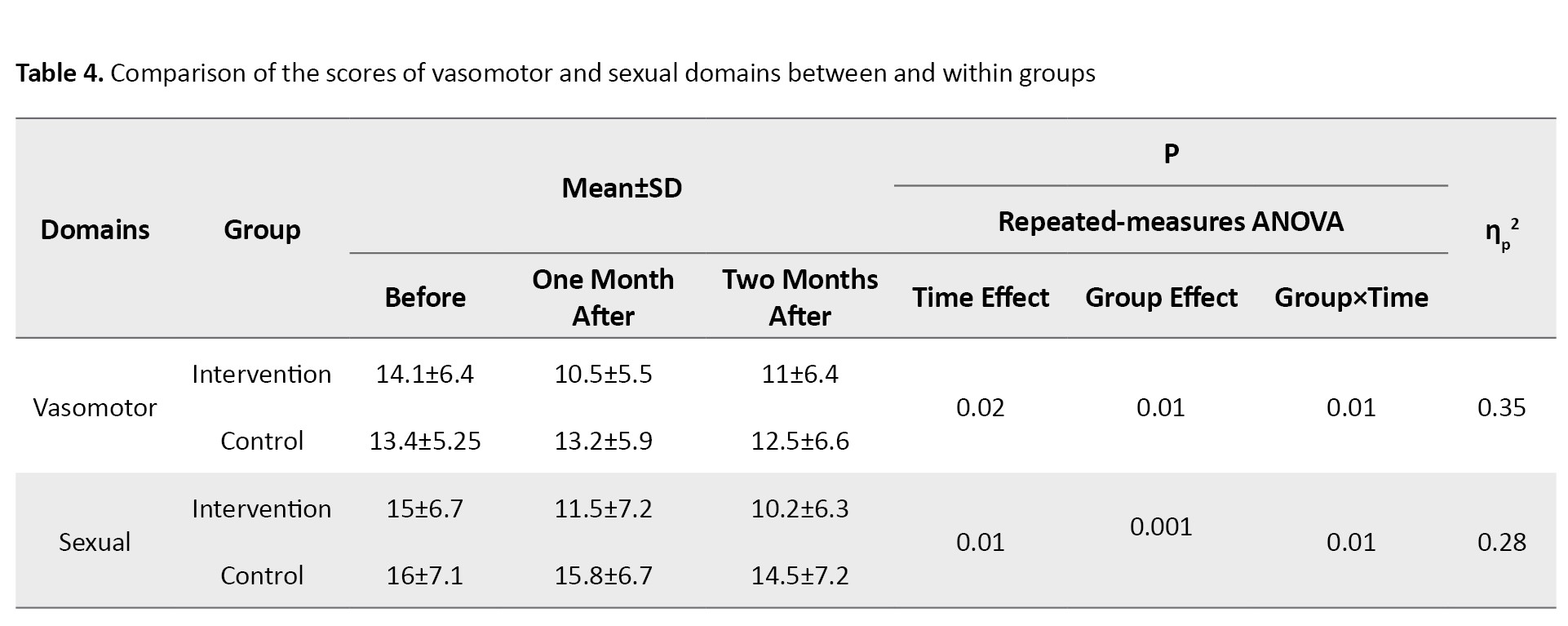
Changes in the scores of the vasomotor and sexual dimensions two months after were measured using a repeated-measures ANOVA. In the vasomotor domain, the group effect (P=0.01), the time effect (P=0.02), and the interaction effect of time and group (P=0.01) were significant with a partial eta-squared (ηp2) value of 0.35. In the sexual domain, the group effect (P=0.001), the time effect (P=0.01), and the interaction effect of time and group (P=0.01) were also significant, with a ηp2 score of 0.28 (Table 4).
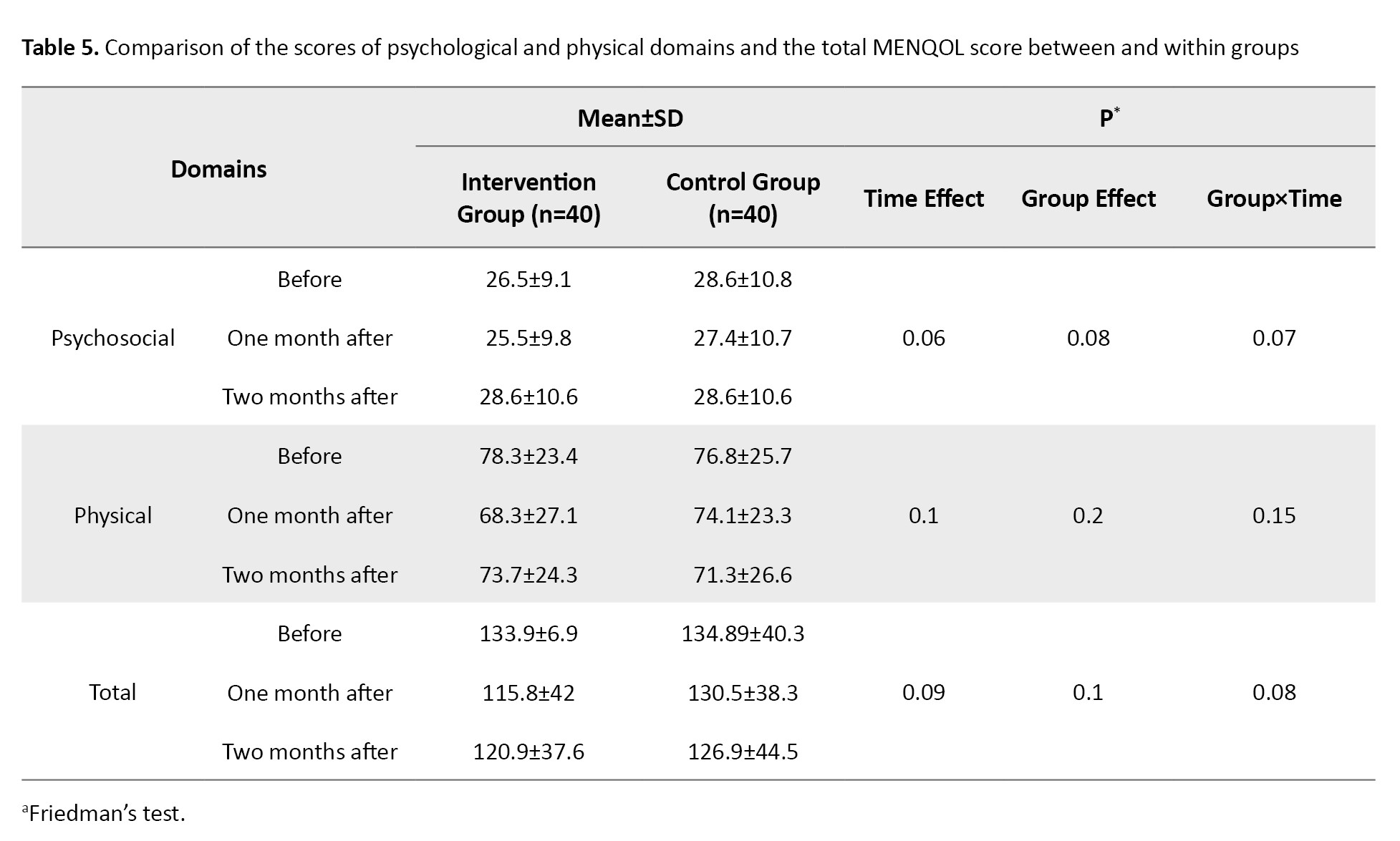
Changes in the scores of psychosocial and physical dimensions and total MENQOL score two months after were measured using Friedman’s test, whose results showed no statistically significant difference in either the intervention group or the control group (Table 5).
Discussion
Some demographic/obstetric factors have been reported to affect the QOL of postmenopausal women [2]. Therefore, in this study, the effects of factors such as age, age at menopause, BMI, number of children (living or deceased), educational level, and occupation were measured in postmenopausal women. Also, the impact of vasomotor, psychosocial, physical, and sexual domains of menopausal symptoms on their QOL was assessed in two groups of intervention (received GOBLE capsules) and placebo. Based on the results, the intervention group showed a significant reduction only in the vasomotor and sexual domains after intervention.
Hot flash is the most common complaint in postmenopausal women. The hot flashes due to hypoestrogenism are related to the sudden deprivation of estrogen, which causes changes in brain mediators and instability of the thermoregulation center [22]. Studies on the effects of some plants containing phytoestrogens on menopausal symptoms have indicated that these plants can reduce menopausal symptoms [11, 23-25]. Green basil is rich in phytoestrogens, such as flavonoids and coumarins, which can bind to estrogen receptors and partially mimic estrogen. This activity may alleviate menopausal symptoms like hot flashes and mood swings. Its antioxidant properties further reduce oxidative stress and inflammation, supporting hormonal balance, metabolic health, and overall well-being in postmenopausal women [15, 16].
Hakimi et al. showed reduced hot flashes in the intervention group that received fenugreek seed [26]. Nahidi et al. showed reduced hot flashes in the intervention group that received Licorice root extract [27]. A comparison of the effects of S. officinalis (100 mg thrice a day) and black cohosh (6.5 mg once a day) on vasomotor symptoms revealed that black cohosh significantly reduced symptoms by the third week, while S. officinalis was effective from the second to the eighth week [28]. A study on the effects of standardized alcoholic extract of T. pratense (Kolubara) showed reduced hot flashes and improvement in other vasomotor symptoms [29]. A systematic review confirmed that various phytoestrogenic plants effectively reduce the severity and frequency of hot flashes in postmenopausal women [30]. However, one study reported no significant effect, suggesting that the type of herbal product, dosage, duration, and timing with meals influence efficacy [31]. Taking phytoestrogens with carbohydrates increases their absorption [29]. Sweat basil reduces vasomotor symptoms via binding to mineralocorticoid receptors and inhibiting beta-hydroxysteroid dehydrogenase [32]. Reduced vasomotor symptoms can enhance sexual function by improving sleep and reducing night sweats [33]. In our study, administration of GOBLE capsules also reduced the sexual symptoms of menopause. Other studies reported benefits of Ginkgo biloba, while G. max, T. pratense, Korean red ginseng, and flaxseed did not affect sexual performance [34, 35]. In another study, Dracocephalum reduced vasomotor, psychosocial, physical, and sexual symptoms of menopause [19]. Menopause can cause depression and isolation. Sweat basil contains monoterpenes, flavonoids, rosmarinic acid, and phenolic compounds, which affect GABA receptors and may improve mood [36-38].
In our study, GOBLE capsule administration had no significant effect on psychosocial or physical symptoms of menopause. Similar Lamiaceae plants, such as Dracocephalum, have shown a positive impact on depression, sleep, anxiety, and stress in clinical studies [39]. Phytoestrogens may preserve bone health, but their efficacy and optimal doses remain uncertain [40]. They are mainly used to prevent osteoporosis [41]. Comparisons with hormonal drugs suggest that both can have beneficial or adverse effects, but further research and regulatory approval are needed for herbal therapies [42]. In our study, the GOBLE capsule administration had no positive effect on the physical symptoms of menopause. This result may be related to the fact that osteoporosis treatment requires a longer course. The use of phytoestrogens often affects the prevention of osteoporosis rather than having therapeutic effects [43]. One limitation of our study was that assessing participants’ adherence to medication was challenging, which we addressed by using a checklist and conducting follow-up phone calls.
In conclusion, GOBLE capsule administration can reduce the effects of vasomotor and sexual symptoms of menopause on the QOL of Iranian postmenopausal women, but has no positive impact on psychosocial or physical symptoms or the overall symptoms. Therefore, this product may help alleviate hot flashes, sweating, and night sweats (vasomotor symptoms) and improve sexual desire, vaginal dryness, and sexual activity of postmenopausal women. Further research with a larger sample size and a longer duration is recommended to assess the effectiveness of GOBLE capsules on physical and psychological symptoms of menopause.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Alborz University of Medical Sciences, Karaj, Iran (Code: IR.ABZUMS.REC.1400.026) and was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20180110038302N7). Written informed consent was obtained from all the participants.
Funding
This study was funded by the Alborz University of Medical Sciences, Karaj, Iran.
Authors' contributions
Conceptualization and study design: Fateme Zokaei and Mansoureh Yazdkhasti; Preparation of GOBLE capsules and experiments: Mohammad Kamalinejad; Data analysis and interpretation: Malihe Farid; Sampling and writing the initial draft: Arezoo Pirak; Reagents preparation, resources, review and editnig: Mansoureh Yazdkhasti; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants and the staff of Kamali Hospital in Alborz Province, Iran.
The sociodemographic form collected information on participants’ characteristics, including age, Body Mass Index (BMI), occupation, educational level, age at menopause, and the number of living or deceased children. The Menopause-specific Quality of Life (MENQOL) questionnaire was used to measure the impact of menopausal symptoms on the QOL. It has 29 items covering vasomotor (3 items), psychosocial (7 items), physical (16 items), and sexual (3 items) domains of symptoms. The total scores for the four dimensions are 3-24, 7-56, 16-128, and 3-24, respectively. The total score for the overall scale ranges from 29 to 232, with higher scores indicating a lower QOL [20]. The Persian version of this questionnaire was validated in our other study [21]. The test re-test reliability, as measured by the intraclass correlation coefficient, was 0.84 for the overall MENQOL, 0.80 for the vasomotor domain, 0.79 for the psychosocial domain, 0.82 for the physical domain, and 0.83 for the sexual domain.
For the intervention group, 250 mg of GOBLE capsules (green basil leaf powder) was prescribed to be taken for 8 consecutive weeks, twice a day, every 12 hours, with breakfast and dinner. The capsules were prepared in Iran under the supervision of a professor of pharmacognosy (Mohammad Kamalinejad). The green basil leaves were collected from the Qasemabad Farm in Karaj, Iran. They were confirmed and registered in the Herbarium of the Faculty of Pharmacy, Shahid Beheshti University of Medical Sciences (No.: SBMU-1084 A). To prepare the GOBLE capsules, the fresh green basil leaves were first dried in the laboratory at 25 ͦC. Then, 100 g of dry leaves were added to 1000 cc of ethanol-water solvent (50% each) in a dish and macerated for 48 hours in the laboratory. Next, the extract was filtered, concentrated, dried in a bain-marie bath (freezing bath), ground in a mill, and placed in 250 mg capsules. For the control group, placebo capsules were used. The capsules were made of 250 mg corn starch, dipped in edible green color, and filled with green basil essential oil with the same color, smell, weight, and packaging as the original capsule used in the intervention group. The placebo was also prepared in the same pharmaceutical laboratory under the supervision of an expert in pharmacognosy (Mohammad Kamalinejad). The researcher monitored patients’ adherence to medication usage by providing them with a checklist.
Data were collected via self-reporting before the intervention and one and two months after the intervention. Statistical analysis was conducted in SPSS software, version 23. Chi-square and Fisher’s exact tests were used to analyze the qualitative variables. The quantitative data were presented as Mean±SD. The normality of the data was assessed based on the Skewness and Kurtosis values. Nonparametric tests such as the Mann-Whitney U test, the Wilcoxon test, and Friedman’s test were used for variables with abnormal distributions, while parametric tests, including the independent t-test, the paired t-test, and the repeated measures ANOVA, were used for variables with normal distributions. The significance level was set at 0.05.
Results
In this study four participants in the intervention group and 5 participants in the control group were lost to follow-up and finally the participants included 80 women (40 in each group). The majority of women were in the age range of 47-51 years (51.4% in the intervention group and 43.6% in the control group). The age at menopause for the majority of women in both groups was in the range of 48-52 years (55% in the intervention group and 59% in the control group). The intervention and control groups were homogeneous with respect to age, age at menopause, BMI, number of living or deceased children, education level, and occupation before the intervention (Table 1).

Baseline MENQOL scores were not significantly different between the two groups before the intervention (Table 2).
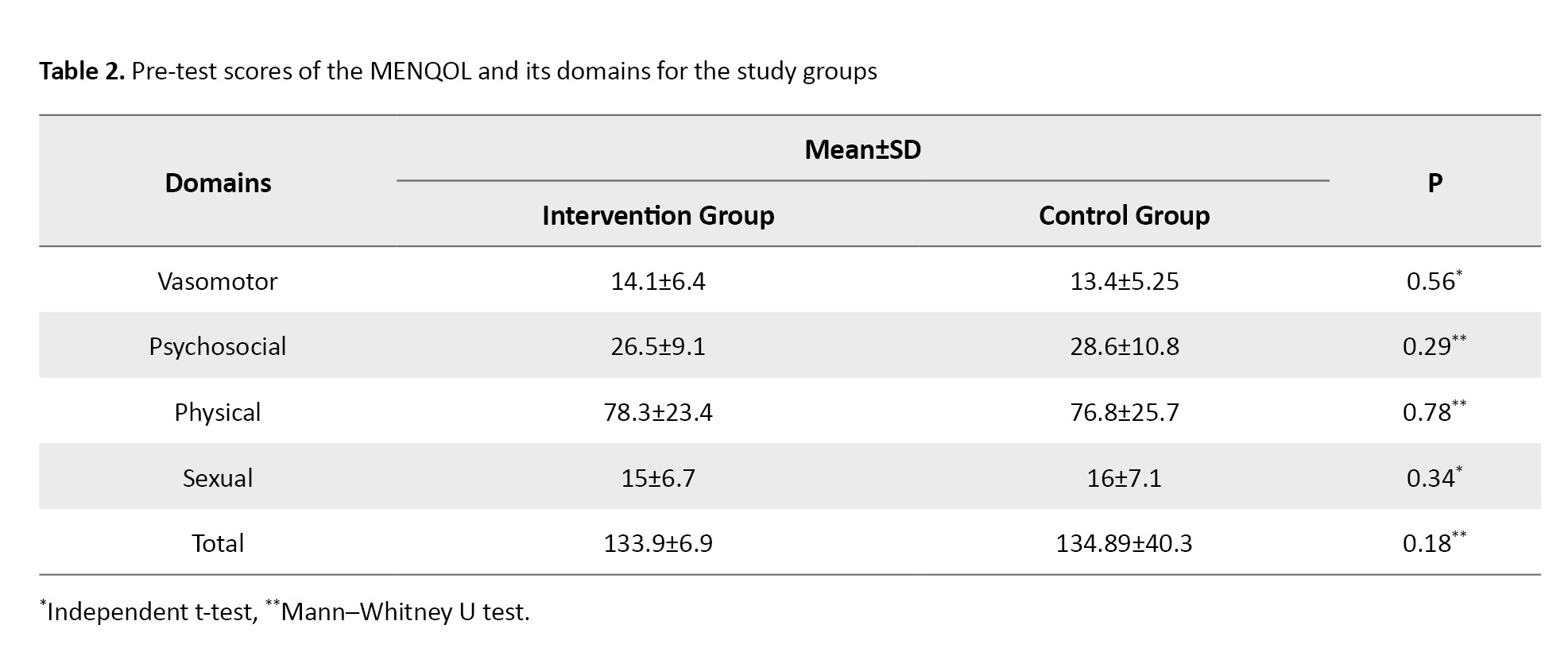
The results of the paired t-test for the intervention group showed that before and one month after the intervention, there was a statistically significant reduction in vasomotor (P=0.01) and sexual (P=0.03) dimensions, but not in psychosocial and physical dimensions and total score based on the results of the Wilcoxon test. In the control group, no statistically significant difference was found one month after the intervention in MENQOL total score or domain scores (Table 3).
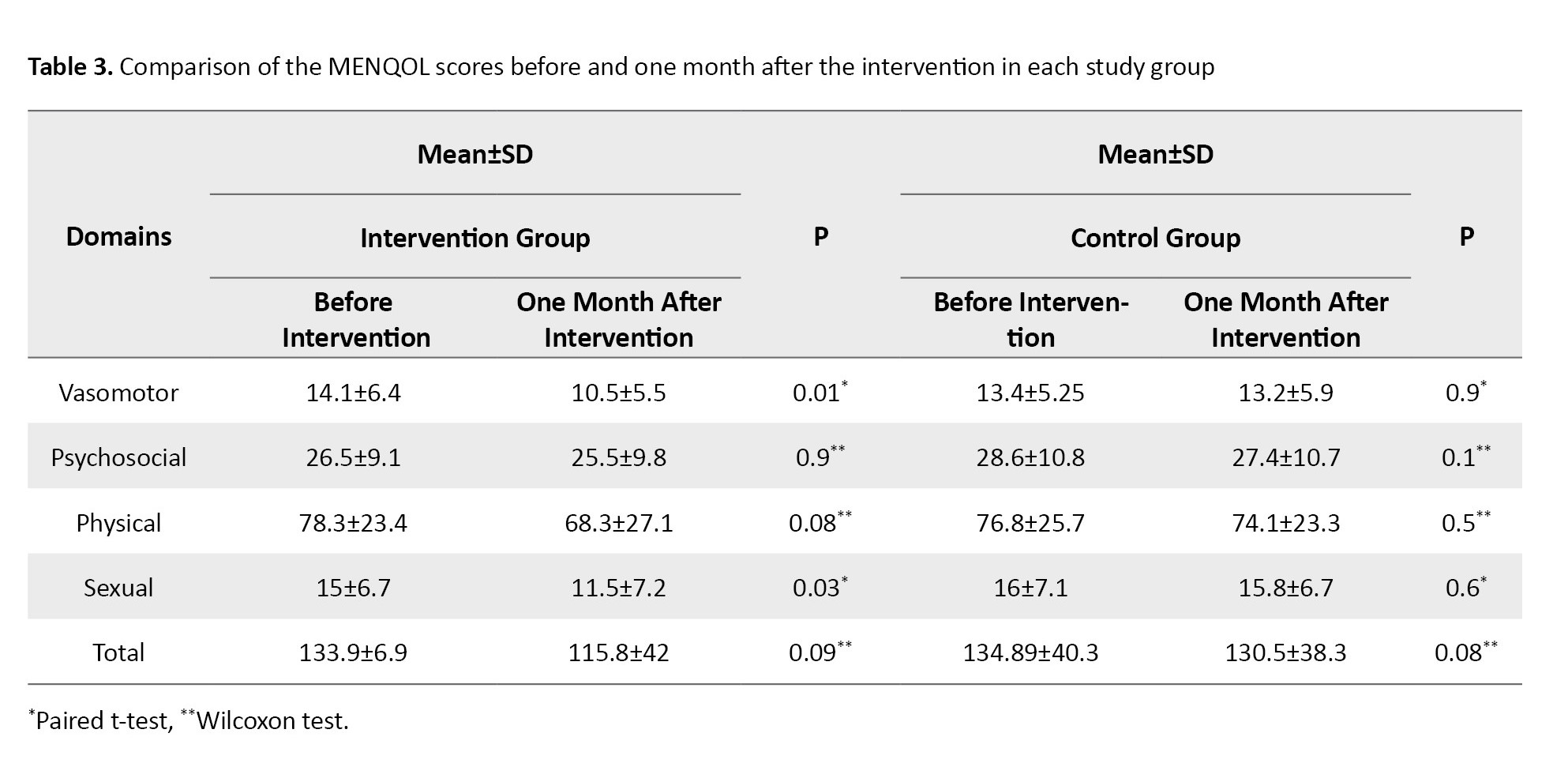
Changes in the scores of the vasomotor and sexual dimensions two months after were measured using a repeated-measures ANOVA. In the vasomotor domain, the group effect (P=0.01), the time effect (P=0.02), and the interaction effect of time and group (P=0.01) were significant with a partial eta-squared (ηp2) value of 0.35. In the sexual domain, the group effect (P=0.001), the time effect (P=0.01), and the interaction effect of time and group (P=0.01) were also significant, with a ηp2 score of 0.28 (Table 4).
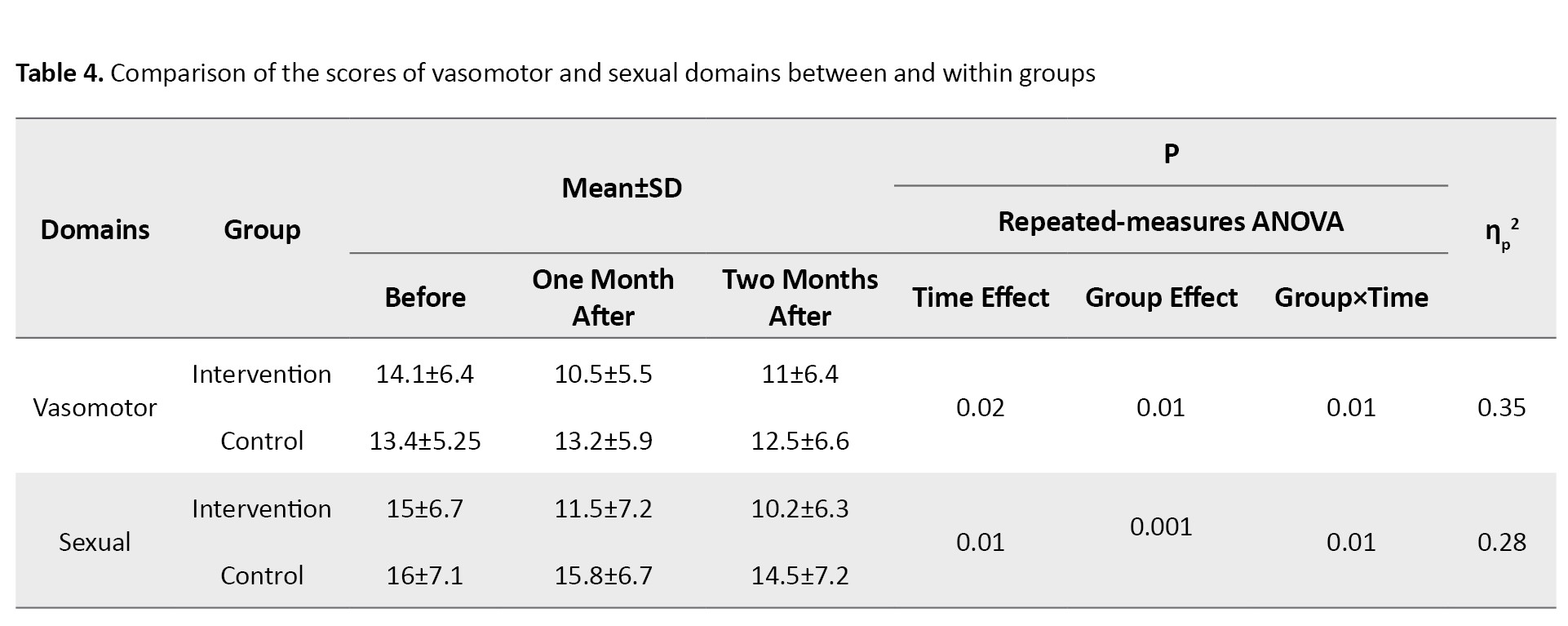
Changes in the scores of psychosocial and physical dimensions and total MENQOL score two months after were measured using Friedman’s test, whose results showed no statistically significant difference in either the intervention group or the control group (Table 5).
Discussion
Some demographic/obstetric factors have been reported to affect the QOL of postmenopausal women [2]. Therefore, in this study, the effects of factors such as age, age at menopause, BMI, number of children (living or deceased), educational level, and occupation were measured in postmenopausal women. Also, the impact of vasomotor, psychosocial, physical, and sexual domains of menopausal symptoms on their QOL was assessed in two groups of intervention (received GOBLE capsules) and placebo. Based on the results, the intervention group showed a significant reduction only in the vasomotor and sexual domains after intervention.
Hot flash is the most common complaint in postmenopausal women. The hot flashes due to hypoestrogenism are related to the sudden deprivation of estrogen, which causes changes in brain mediators and instability of the thermoregulation center [22]. Studies on the effects of some plants containing phytoestrogens on menopausal symptoms have indicated that these plants can reduce menopausal symptoms [11, 23-25]. Green basil is rich in phytoestrogens, such as flavonoids and coumarins, which can bind to estrogen receptors and partially mimic estrogen. This activity may alleviate menopausal symptoms like hot flashes and mood swings. Its antioxidant properties further reduce oxidative stress and inflammation, supporting hormonal balance, metabolic health, and overall well-being in postmenopausal women [15, 16].
Hakimi et al. showed reduced hot flashes in the intervention group that received fenugreek seed [26]. Nahidi et al. showed reduced hot flashes in the intervention group that received Licorice root extract [27]. A comparison of the effects of S. officinalis (100 mg thrice a day) and black cohosh (6.5 mg once a day) on vasomotor symptoms revealed that black cohosh significantly reduced symptoms by the third week, while S. officinalis was effective from the second to the eighth week [28]. A study on the effects of standardized alcoholic extract of T. pratense (Kolubara) showed reduced hot flashes and improvement in other vasomotor symptoms [29]. A systematic review confirmed that various phytoestrogenic plants effectively reduce the severity and frequency of hot flashes in postmenopausal women [30]. However, one study reported no significant effect, suggesting that the type of herbal product, dosage, duration, and timing with meals influence efficacy [31]. Taking phytoestrogens with carbohydrates increases their absorption [29]. Sweat basil reduces vasomotor symptoms via binding to mineralocorticoid receptors and inhibiting beta-hydroxysteroid dehydrogenase [32]. Reduced vasomotor symptoms can enhance sexual function by improving sleep and reducing night sweats [33]. In our study, administration of GOBLE capsules also reduced the sexual symptoms of menopause. Other studies reported benefits of Ginkgo biloba, while G. max, T. pratense, Korean red ginseng, and flaxseed did not affect sexual performance [34, 35]. In another study, Dracocephalum reduced vasomotor, psychosocial, physical, and sexual symptoms of menopause [19]. Menopause can cause depression and isolation. Sweat basil contains monoterpenes, flavonoids, rosmarinic acid, and phenolic compounds, which affect GABA receptors and may improve mood [36-38].
In our study, GOBLE capsule administration had no significant effect on psychosocial or physical symptoms of menopause. Similar Lamiaceae plants, such as Dracocephalum, have shown a positive impact on depression, sleep, anxiety, and stress in clinical studies [39]. Phytoestrogens may preserve bone health, but their efficacy and optimal doses remain uncertain [40]. They are mainly used to prevent osteoporosis [41]. Comparisons with hormonal drugs suggest that both can have beneficial or adverse effects, but further research and regulatory approval are needed for herbal therapies [42]. In our study, the GOBLE capsule administration had no positive effect on the physical symptoms of menopause. This result may be related to the fact that osteoporosis treatment requires a longer course. The use of phytoestrogens often affects the prevention of osteoporosis rather than having therapeutic effects [43]. One limitation of our study was that assessing participants’ adherence to medication was challenging, which we addressed by using a checklist and conducting follow-up phone calls.
In conclusion, GOBLE capsule administration can reduce the effects of vasomotor and sexual symptoms of menopause on the QOL of Iranian postmenopausal women, but has no positive impact on psychosocial or physical symptoms or the overall symptoms. Therefore, this product may help alleviate hot flashes, sweating, and night sweats (vasomotor symptoms) and improve sexual desire, vaginal dryness, and sexual activity of postmenopausal women. Further research with a larger sample size and a longer duration is recommended to assess the effectiveness of GOBLE capsules on physical and psychological symptoms of menopause.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Alborz University of Medical Sciences, Karaj, Iran (Code: IR.ABZUMS.REC.1400.026) and was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20180110038302N7). Written informed consent was obtained from all the participants.
Funding
This study was funded by the Alborz University of Medical Sciences, Karaj, Iran.
Authors' contributions
Conceptualization and study design: Fateme Zokaei and Mansoureh Yazdkhasti; Preparation of GOBLE capsules and experiments: Mohammad Kamalinejad; Data analysis and interpretation: Malihe Farid; Sampling and writing the initial draft: Arezoo Pirak; Reagents preparation, resources, review and editnig: Mansoureh Yazdkhasti; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants and the staff of Kamali Hospital in Alborz Province, Iran.
References
- De Franciscis P, Colacurci N, Riemma G, Conte A, Pittana E, Guida M, et al. A Nutraceutical Approach to menopausal complaints. Medicina (Kaunas). 2019; 55(9):544. [DOI:10.3390/medicina55090544] [PMID]
- Hoggard TM, Jeray KJ. Osteoporosis management in the United States. OTA Int. 2022; 5(3S):e184. [DOI:10.1097/OI9.0000000000000184] [PMID]
- Yazdkhasti M, Negarandeh R, Behboodi Moghadam Z. An empowerment model of Iranian women for the management of menopause: A grounded theory study. Int J Qual Stud Health Well-being. 2019; 14(1):1665958. [DOI:10.1080/17482631.2019.1665958] [PMID]
- Ye L, Knox B, Hickey M. Management of menopause symptoms and quality of life during the menopause transition. Endocrinol Metab Clin North Am. 2022; 51(4):817-36. [DOI:10.1016/j.ecl.2022.04.006] [PMID]
- Khodadad Kashi S, Mirzazadeh ZS, Saatchian V. A systematic review and meta-analysis of resistance training on quality of life, depression, muscle strength, and functional exercise capacity in older adults aged 60 years or more. Biol Res Nurs. 2023; 25(1):88-106. [DOI:10.1177/10998004221120945] [PMID]
- Essa RM, Mahmoud NM. Factors associated with the severity of menopausal symptoms among menopausal women. J Nurs Health Sci. 2018; 7(2):29-40. [Link]
- Pajalić Z, Raboteg-Šarić Z. Determinants of menopause-related symptoms in women during the transition to menopause and the postmenopausal period-a systematic literature review. J Health Sci. 2020; 10(1):1-33. [DOI:10.17532/jhsci.2020.885]
- Hodis HN, Mack WJ. Menopausal hormone replacement therapy and reduction of all-cause mortality and cardiovascular disease: It is about time and timing. Cancer J. 2022; 28(3):208-23.[DOI:10.1097/PPO.0000000000000591] [PMID]
- Dolitsky SN, Cordeiro Mitchell CN, Stadler SS, Segars JH. Efficacy of progestin-only treatment for the management of menopausal symptoms: A systematic review. Menopause. 2020; 28(2):217-24. [DOI:10.1097/GME.0000000000001676] [PMID]
- van Die MD, Burger HG, Bone KM, Cohen MM, Teede HJ. Hypericum perforatum with Vitex agnus-castus in menopausal symptoms: A randomized, controlled trial. Menopause. 2009; 16(1):156-63. [DOI:10.1097/gme.0b013e31817fa9e0] [PMID]
- Steels E, Steele M, Harold M, Coulson S. Efficacy of a proprietary Trigonella foenum-graecum L. de-husked seed extract in reducing menopausal symptoms in otherwise healthy women: A double-blind, randomized, placebo-controlled study. Phytother Res. 2017; 31(9):1316-22. [DOI:10.1002/ptr.5856] [PMID]
- Jiao M, Liu X, Ren Y, Wang Y, Cheng L, Liang Y, et al. Comparison of herbal medicines used for women’s menstruation diseases in different areas of the world. Front Pharmacol. 2022; 12:751207. [DOI:10.3389/fphar.2021.751207] [PMID]
- Zeidabadi A, Yazdanpanahi Z, Dabbaghmanesh MH, Sasani MR, Emamghoreishi M, Akbarzadeh M, et al. The effect of Salvia officinalis extract on symptoms of flushing, night sweat, sleep disorders, and score of forgetfulness in postmenopausal women. J Family Med Prim Care. 2020; 9(2):1086-92. [DOI:10.4103/jfmpc.jfmpc_913_19] [PMID]
- Newton KM, Reed SD, LaCroix AZ, Grothaus LC, Ehrlich K, Guiltinan J. Treatment of vasomotor symptoms of menopause with black cohosh, multibotanicals, soy, hormone therapy, or placebo: A randomized trial. Obstet Gynecol Surv. 2007; 62(4):249-50. [DOI:10.1097/01.ogx.0000259156.08271.b4]
- Javanmardi J, Khalighi A, Kashi A, Bais HP, Vivanco JM. Chemical characterization of basil (Ocimum basilicum L.) found in local accessions and used in traditional medicines in Iran. J Agric Food Chem. 2002; 50(21):5878-83. [DOI:10.1021/jf020487q] [PMID]
- Tangpao T, Charoimek N, Teerakitchotikan P, Leksawasdi N, Jantanasakulwong K, Rachtanapun P, et al. Volatile organic compounds from basil essential oils: plant taxonomy, biological activities, and their applications in tropical fruit productions. Horticulturae. 2022; 8(2):144. [DOI:10.3390/horticulturae8020144]
- Albertazzi P, Pansini F, Bonaccorsi G, Zanotti L, Forini E, De Aloysio D. The effect of dietary soy supplementation on hot flushes. Obstet Gynecol. 1998; 91(1):6-11. [DOI:10.1016/S0029-7844(97)00597-8] [PMID]
- Fjær EL, Landet ER, McNamara CL, Eikemo TA. The use of complementary and alternative medicine (CAM) in Europe. BMC Complement Med Ther. 2020; 20(1):108. [DOI:10.1186/s12906-020-02903-w] [PMID]
- Taavoni S, Nazem Ekbatani N, Izadjoo M, Haghani H. [Effect of Lemon Balm supplementation on menopausal symptoms (Persian)]. Complement Med J. 2016; 5(4):13-16. [Link]
- Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire: Development and psychometric properties. Maturitas. 1996; 24(3):161-75.[DOI:10.1016/S0378-5122(96)82006-8] [PMID]
- Yazdkhasti M, Keshavarz M, Merghati-khoee E, Hosseini AF. [The effect of structured educational program by support group on menopause women’s quality of life (Persian)]. Iran J Med Educ.2012; 11(8):986-94. [Link]
- Khan SJ, Kapoor E, Faubion SS, Kling JM. Vasomotor symptoms during menopause: A practical guide on current treatments and future perspectives. Int J Womens Health. 2023; 15:273-87. [DOI:10.2147/IJWH.S365808] [PMID]
- Moore TR, Franks RB, Fox C. Review of efficacy of complementary and alternative medicine treatments for menopausal symptoms. J Midwifery Womens Health. 2017; 62(3):286-97. [DOI:10.1111/jmwh.12628] [PMID]
- Kanadys W, Baranska A, Jedrych M, Religioni U, Janiszewska M. Effects of red clover (Trifolium pratense) isoflavones on the lipid profile of perimenopausal and postmenopausal women-A systematic review and meta-analysis. Maturitas. 2020; 132:7-16.[DOI:10.1016/j.maturitas.2019.11.001] [PMID]
- Portella CF, Silva ID, Simões RS, Ghelman R, Baracat EC, Júnior JM, et al. An overview of systematic reviews of medicinal plants and herbal formulations for the treatment of climacteric symptoms. J Herbal Med. 2024; 29:100863. [DOI:10.1016/j.hermed.2024.100863]
- Hakimi S, Mohammad Alizadeh S, Delazar A, Abbasalizadeh F, Bamdad Mogaddam R, Siiahi M, et al. [Probable effects of fenugreek seed on hot flash in menopausal women (Persian)]. J Med Plants. 2006; 5(19):9-14. [Link]
- Nahidi F ZE, Mojab F, Alavi Majd H. [The effect of Licorice root extract on hot flashes in menopause (Persian)]. Pejouhandeh. 2011;16(1):7-11. [Link]
- Moradi M, Ghavami V, Niazi A, Seraj Shirvan F, Rasa S. The effect of salvia officinalis on hot flashes in postmenopausal women: A systematic review and meta-analysis. Int J Community Based Nurs Midwifery. 2023; 11(3):169-78. [PMID]
- Salehi K, Ehsanpour S, Zolfaghari B, Salehi Z, Honarjoo MJ. [The effects of red clover on hot flushes in post-menopausal women (Persian)]. Hormozgan Medical Journal. 2014; 17(6):521-9. [Link]
- Ghazanfarpour M, Sadeghi R, Abdolahian S, Latifnejad Roudsari R. The efficacy of Iranian herbal medicines in alleviating hot flashes: A systematic review. Int J Reprod Biomed. 2016; 14(3):155-66. [PMID]
- van de Weijer PH, Barentsen R. Isoflavones from red clover (Promensil®) significantly reduce menopausal hot flush symptoms compared with placebo. Maturitas. 2002; 42(3):187-93. [DOI:10.1016/S0378-5122(02)00080-4] [PMID]
- Zeidabadi A, Emamghoreishi M, Tayebi N, Akbarzadeh M. Effect of Vitex Agnus-Castus extract on hot flushes, night sweats, sleep disorders and some other symptoms in postmenopausal women: A clinical trial study. Aust J Herbal Naturopathic Med. 2022; 34(4):148-54. [Link]
- Ozcan H, Çolak P, Oturgan B, Gülsever E. Complementary and alternative treatment methods for menopausal hot flashes used in Turkey. Afr Health Sci. 2019; 19(4):3001-8. [DOI:10.4314/ahs.v19i4.21] [PMID]
- Amiri Pebdani M, Taavoni S, Haghani H. The effect of herbal supplement of ginkgo biloba on attitudes toward menopausal women to sexual relations. Nurs Midwifery J. 2013; 11(3):10-16. [Link]
- Najaf Najafi M, Ghazanfarpour MJC. Effect of phytoestrogens on sexual function in menopausal women: A systematic review and meta-analysis. Climacteric. 2018; 21(5):437-45. [DOI:10.1080/13697137.2018.1472566] [PMID]
- Karimi FZ, Hosseini H, Mazlom SR, Rakhshandeh H. The effect of oral capsules containing Ocimum basilicum leaf extract on menopausal symptoms in women: A triple-blind randomized clinical trial. Eur J Med Res. 2024; 29(1):367. [DOI:10.1186/s40001-024-01965-7] [PMID]
- Gradinariu V, Cioanca O, Hritcu L, Trifan A, Gille E, Hancianu M. Comparative efficacy of Ocimum sanctum L. and Ocimum basilicum L. essential oils against amyloid beta (1-42)-induced anxiety and depression in laboratory rats. Phytochem Rev. 2015; 14:567-75. [DOI:10.1007/s11101-014-9389-6]
- Sahib SE. Study the analgesic and sedative effect of Ocimum basilicum alcoholic extract in male rats. Diyala Agricultural Sciences Journal. 2014; 6(1):9–22. [Link]
- Heidari M, Soltanpour A, Naseri M, Kazemnezhad J. [The effect of Lemon Balm (Melissa Officinalis) on depression in patients after coronary artery bypass graft (Persian)]. Cardiovasc Nurs J. 2015; 4(2):36-43. [Link]
- Rietjens IM, Louisse J, Beekmann K. The potential health effects of dietary phytoestrogens. Br J Pharmacol. 2017; 174(11):1263-80. [DOI:10.1111/bph.13622] [PMID]
- Arjmandi BH. The role of phytoestrogens in the prevention and treatment of osteoporosis in ovarian hormone deficiency. J Am Coll Nutr. 2001; 20(5 Suppl):398S-402S; discussion 417S-420S. [DOI:10.1080/07315724.2001.10719175] [PMID]
- Al-Anazi AF, Qureshi VF, Javaid K, Qureshi S. Preventive effects of phytoestrogens against postmenopausal osteoporosis as compared to the available therapeutic choices: An overview. J Nat Sci Biol Med. 2011; 2(2):154-63. [DOI:10.4103/0976-9668.92322] [PMID]
- Tu KN, Lie JD, Wan CKV, Cameron M, Austel AG, Nguyen JK, et al. Osteoporosis: A review of treatment options. P T. 2018; 43(2):92-104. [PMID]
Article Type : Research |
Subject:
General
Received: 2023/12/7 | Accepted: 2025/02/23 | Published: 2026/01/11
Received: 2023/12/7 | Accepted: 2025/02/23 | Published: 2026/01/11
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |