Tue, Feb 3, 2026
Volume 34, Issue 1 (1-2024)
JHNM 2024, 34(1): 13-20 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yousefi-Ghalehroodkhani F, Rouhani-Tonekaboni N, Shakiba M, Mehrabian F, Kazemi-Aski S. Assessing Natural Childbirth Intention Based on the Theory of Planned Behavior and Social Support in Pregnant Women in Northern Iran. JHNM 2024; 34 (1) :13-20
URL: http://hnmj.gums.ac.ir/article-1-2249-en.html
URL: http://hnmj.gums.ac.ir/article-1-2249-en.html
Fatemeh Yousefi-Ghalehroodkhani1 

 , Nooshin Rouhani-Tonekaboni *2
, Nooshin Rouhani-Tonekaboni *2 

 , Maryam Shakiba3
, Maryam Shakiba3 

 , Fardin Mehrabian4
, Fardin Mehrabian4 

 , Soudabeh Kazemi-Aski5
, Soudabeh Kazemi-Aski5 




 , Nooshin Rouhani-Tonekaboni *2
, Nooshin Rouhani-Tonekaboni *2 

 , Maryam Shakiba3
, Maryam Shakiba3 

 , Fardin Mehrabian4
, Fardin Mehrabian4 

 , Soudabeh Kazemi-Aski5
, Soudabeh Kazemi-Aski5 


1- Health Education (MSc), Department of Health Education and Promotion, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
2- Assistant Professor, Department of Health Education and Promotion, Research Center of Health and Environment, School of Health, Guilan University of Medical Sciences, Rasht, Iran. ,rouhani.phd@gmail.com
3- Associate Professor, Cardiovascular Diseases Research Center, Department of Epidemiology and Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Professor, Department of Health Education and Promotion, Research Center of Health and Environment, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
5- Associate Professor, Reproductive Health Research Center, Department of Obstetrics and Gynecology, Al-Zahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Assistant Professor, Department of Health Education and Promotion, Research Center of Health and Environment, School of Health, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Associate Professor, Cardiovascular Diseases Research Center, Department of Epidemiology and Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Professor, Department of Health Education and Promotion, Research Center of Health and Environment, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
5- Associate Professor, Reproductive Health Research Center, Department of Obstetrics and Gynecology, Al-Zahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
Keywords: Cesarean section, Natural childbirth, Pregnant women, Social support, Theory of planned behavior
Full-Text [PDF 475 kb]
(638 Downloads)
| Abstract (HTML) (1613 Views)
Full-Text: (777 Views)
Introduction
Natural vaginal childbirth is the most challenging physiological and psychological event in the life of women [1]. Cesarean section (CS), avoided for its alarming mortality rate over a little more than a century ago, is now the mode of delivery for one in three women in the United States [2] and up to four in five women in some other areas in the world [3]. CS has many complications for the mother and the child. Three known postpartum complications of CS include postpartum hemorrhage (PPH), surgical site infection (SSI), and venous thromboembolism (VTE). These complications contribute to maternal morbidity and mortality, increased healthcare costs, and prolonged hospital stays [4, 5, 6]. CS is now the most common surgery performed in the United States, with over 1 million women delivered by CS every year. The CS rate rose from 5% in 1970 to 31.9% in 2016 [7]. According to a meta-analysis research conducted using 41 studies from 1999-2016, the prevalence of CS was 48% in Iran and 52% in Guilan Province. In this study, the main causes of the prevalence of CS included higher education of mothers, previous history of CS, and physician advice [8]. In 1985, as part of a multidisciplinary report on appropriate technologies for childbirth, the Word Health Organization (WHO) concluded that there is no justification for any geographic region to have a CS rate of more than 10-15% [9]. According to the evidence, continuous and systematic educational interventions by health staff can have a significant impact on encouraging pregnant mothers to perform natural childbirth and reduce CS rate [10].
Health education and health-promoting models provide a framework for healthcare educators to use it to predict behaviors and subsequently design and implement educational interventions [11]. It has been empirically proven that if the provision of healthcare services is not sufficiently accompanied by health education, it will not be beneficial. In health education, higher and appropriate theoretical support along with providing basic health needs can cause the health education programs to be more effective. In this regard, the use of educational theories appropriate to the study society and the expected results can be very useful [12]. The theory of planned behavior (TPB) is a useful model for predicting health behaviors, designing educational interventions, and promoting health [13]. This theory is free to enter more variables to improve the predictive power [14]. According to the TPB, when people have enough time to think about what they want to do, the best predictor of their behavior will be their intention, which is determined by three factors, including their attitude, subjective norms, and perceived behavioral control. Attitude is a favorable or unfavorable assessment of a behavior that has been formed through past experiences. Subjective norms refer to the perceived social pressures from others for a person to behave in a certain manner. Perceived behavioral control refers to how much a person feels s/he is able to enact the behavior. Some studies have used TPB to predict childbirth intention and have reported its high predictive power [15, 16, 17]. Social support during pregnancy can promote better birth outcomes [18]. Studies have shown that some dimensions of social support, including informational and emotional support, are related to choosing the type of delivery [19]. Despite the provisions of training on natural childbirth preparation in health centers and the recommendations of the Ministry of Health and Medical Education about reducing CS, the change in the CS rate has not been significant in the last ten years in Guilan Province; therefore, effective educational interventions, especially in the frame of health education and health-promotion models are needed in this area. In Ghafari et al.’s study [20], all TPB constructs, including the attitude towards choosing natural childbirth had a significant relationship with choosing natural childbirth, such that after telephone follow-up, 71.15% of the women had natural birth. In Sohaili et al.’s study [17], subjective norms and perceived behavioral controls showed a significant relationship with the choice of the delivery method.
Therefore, by examining the psychological and social factors of the natural childbirth intention, the present study aims to determine the predictors of natural childbirth intention based on the TPB and investigate the perceived social support in pregnant women referred to selected hospitals in Rasht, Guilan Province, Iran.
Material and Methods
This is an analytic cross-sectional study. The study population consists of all pregnant women referred to the perinatal clinics in four hospitals in Rasht city in 2020. Inclusion criteria were being literate, Full consciousness, gestational age 1-9 months, age 15-45 years, no high-risk pregnancy, and indication for inforced CS by physician. Exclusion criteria were contraindications for natural childbirth according to the physician and return of incomplete questionnaire. Based on the results of Abdolkarimi et al. [21] and considering the natural childbirth intention (as a dependent variable) of 69%, 8% accuracy, 5% error, a dropout rate of 10%, and inclusion of 5 samples for each 46 items of the questionnaire, final sample size was determined 374, 124 samples in three groups of trimesters one, two and three.
Sampling was done by systematic random sampling method proportional to the population size. Sampling was performed in hospitals with prenatal clinics. In this regard, 180 samples were selected from teaching hospitals, 88 form public hospitals, 37 from private hospitals, and 48 from military hospitals. In private hospitals, because of the prevalence of COVID-19 pandemic and the low number of referred pregnant women, the convenience sampling method was used.
The data collection tool was a three-part questionnaire adapted from other studies [22, 23, 24]. The first part surveys demographic information of the pregnant women and their husbands (13 item). The second part included items related to the constructs of the TPB (2 items for intention, 15 items for attitude, 12 items for subjective norms, 9 items for perceived behavioral control). The items are scored on a 5-point Likert scale (1=strongly disagree to 5=strongly agree). The third part measures perceived social support with 8 items rated on a 5-point Likert scale (1=not at all to 5=extremely). This section was adapted from Otogara et al.’s study [23, 24]. The first part surveys demographic information of the pregnant women and their husbands (13 item). The second part included items related to the const]. Content validity was confirmed using the opinions of a panel of experts (five experts in health education and promotion, one gynecologist, one reproductive health specialist, and two epidemiologists). The content validity ratio (CVR) and content validity index (CVI) for the constructs of intention were obtained 1 and 1; for attitude, 0.95 and 0.97; for perceived behavioral control, 0.84 and 0.91; for subjective norms, 0.86 and 1; and for social support, 0.85 and 0.91, respectively which were acceptable (>0.7). For assessing the reliability, a pilot study was performed on 20 pregnant women. Cronbach’s α coefficient was obtained 0.97 for intention, 0.92 for attitude, 0.89 for subjective norms, 0.91 for perceived behavioral control, and 0.72 for social support.
Gestational age, previous childbirth experience, and participation in childbirth preparation programs were considered as confounding variables. The collected data were analyzed in SPSS software, version 21. Data were described using Mean±SD indices for quantitative variables and frequency and percentage for qualitative variables. Analysis of variance (ANOVA) and t-test were used to investigate the difference in natural childbirth intentions based on demographic variables. Pearson correlation test was used to examine the correlation between each of the subscales with natural childbirth intention. Multiple linear regression analysis (forward method) was used to determine the predictors of natural childbirth intention.
Results
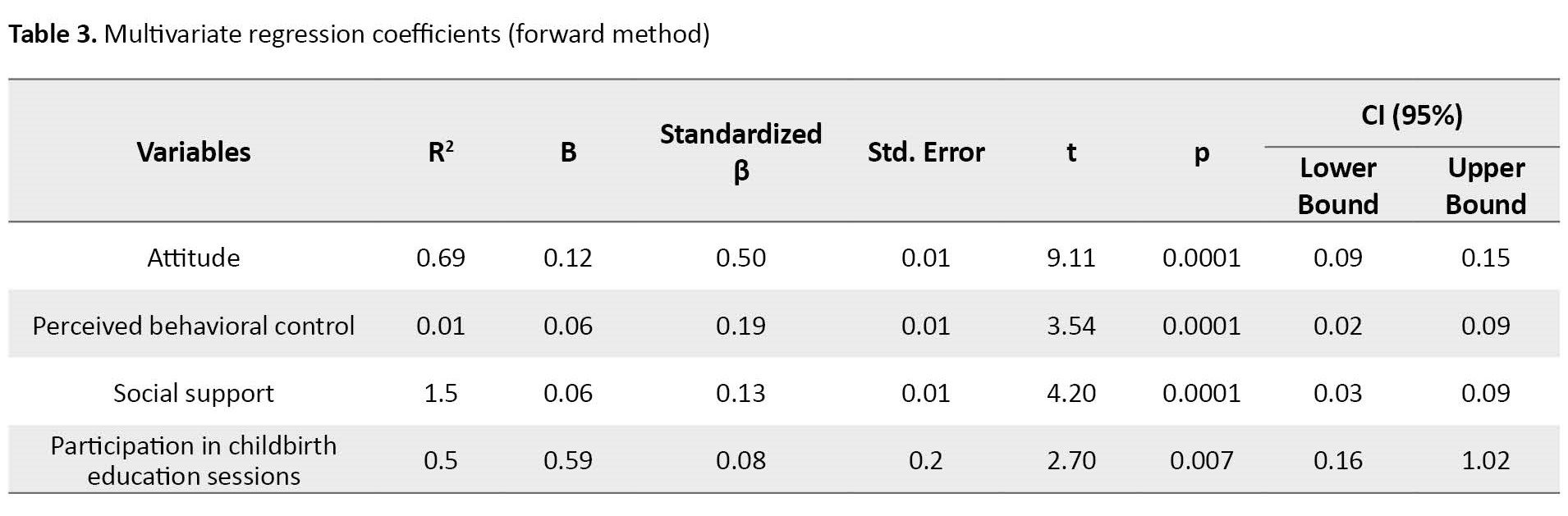
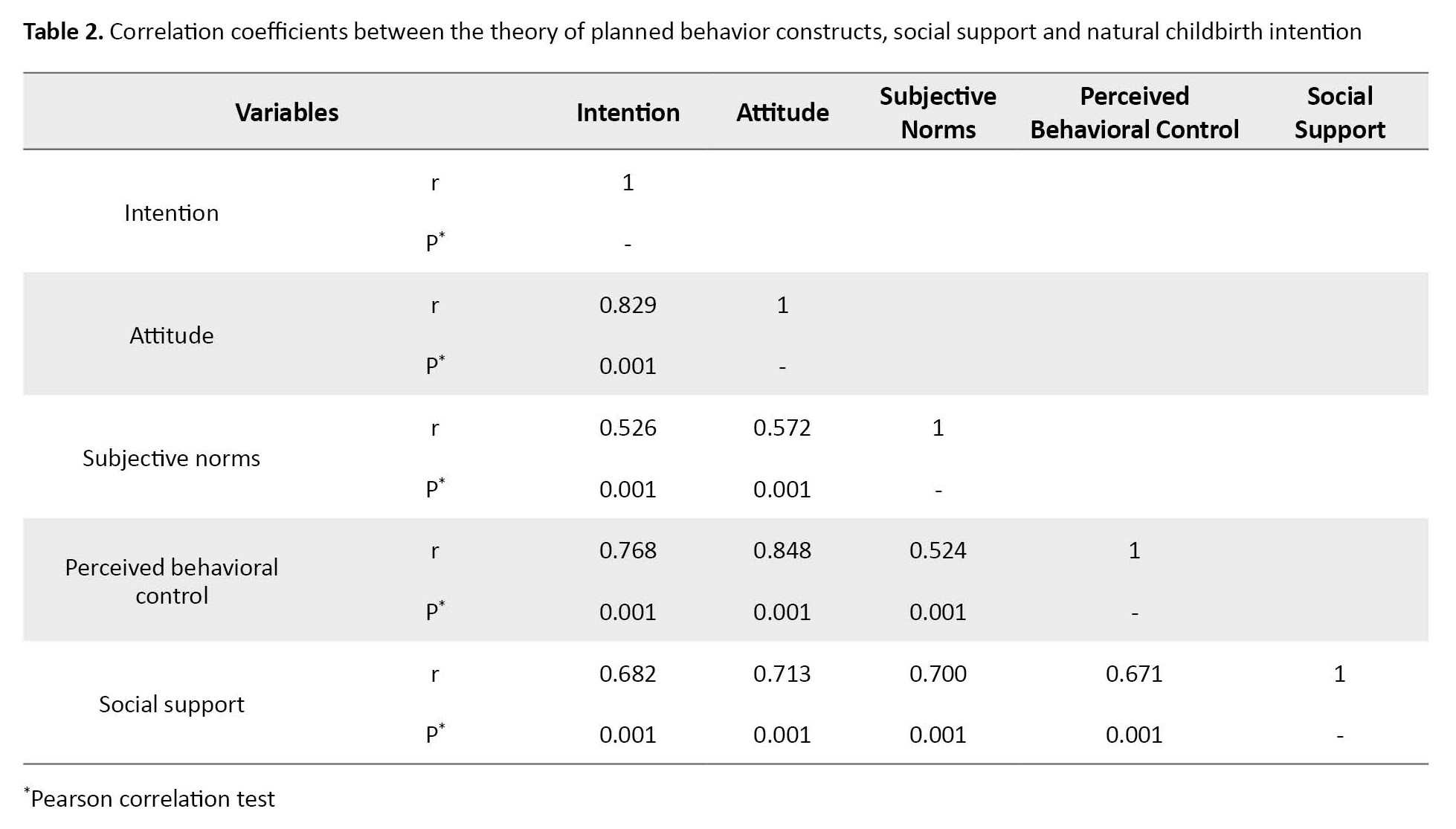
Out of 374 samples with inclusion criteria, 21 people did not agree to participate in the research and total of 353 women participated in this study. Their characteristics are presented in Table 1.
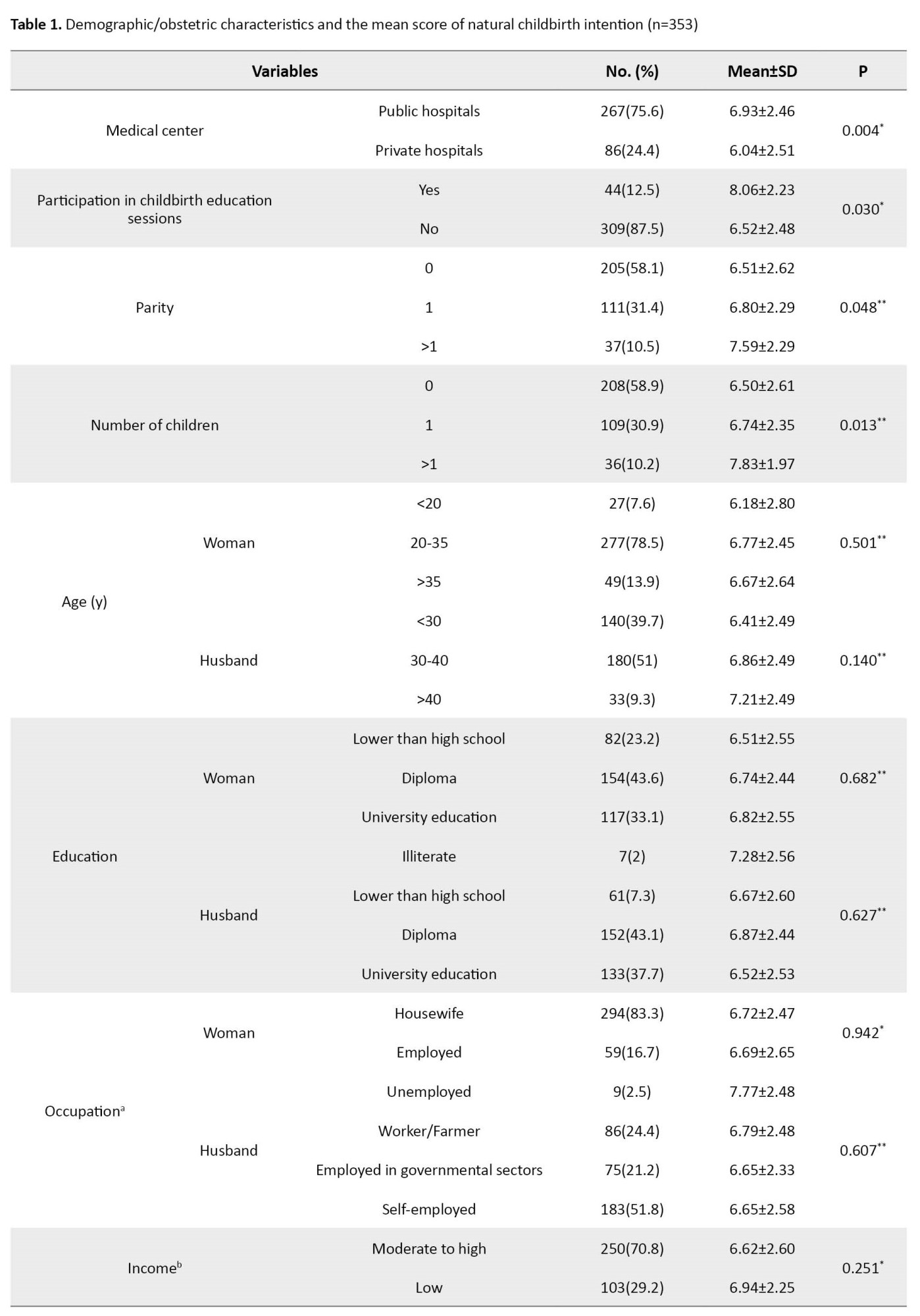
The mean score of natural childbirth intention was not significantly different according to age, educational level, occupation of pregnant women and their husbands, place of residence, income, previous childbirth experience, number of pregnancies, and gestational age.
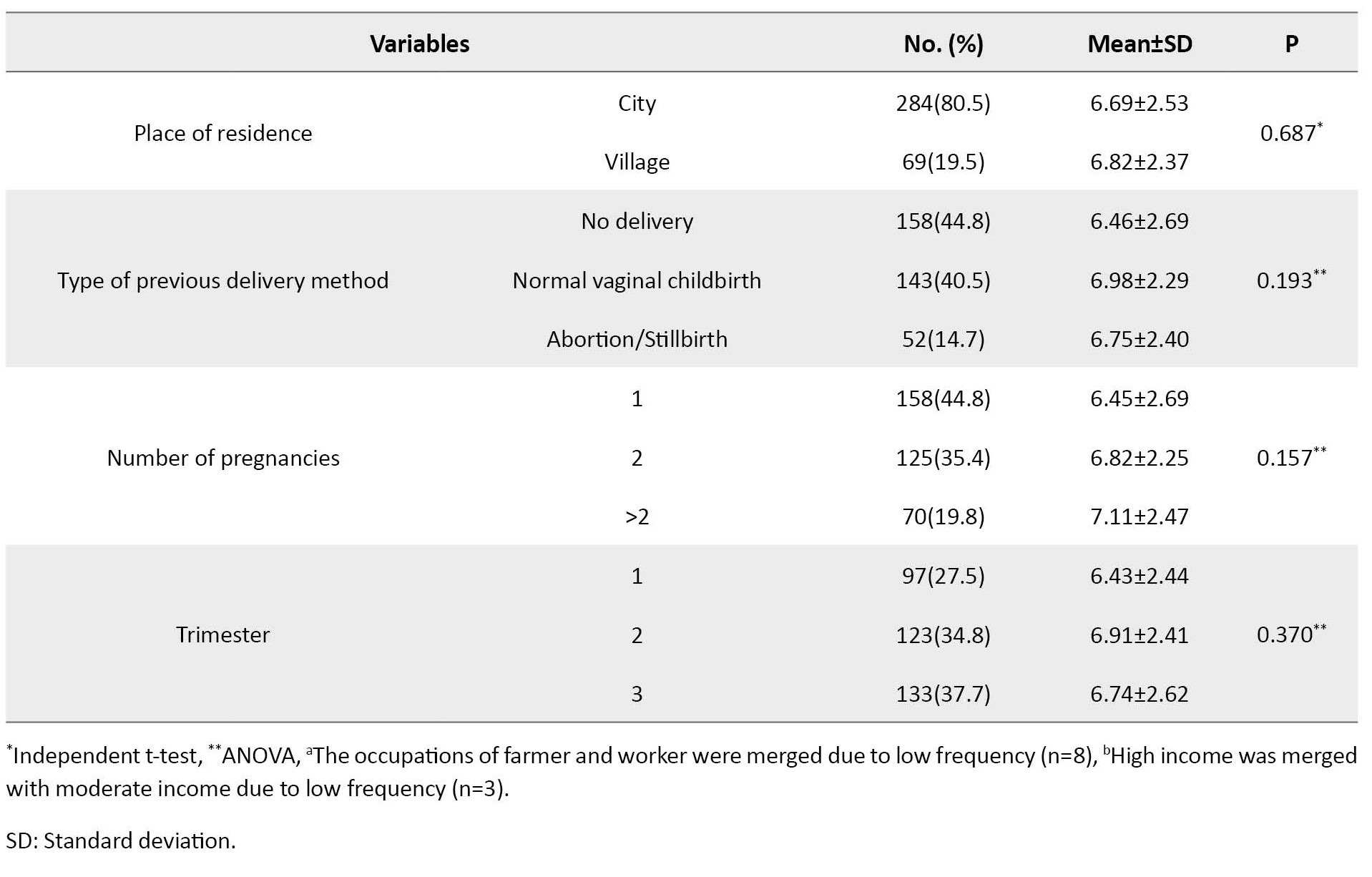
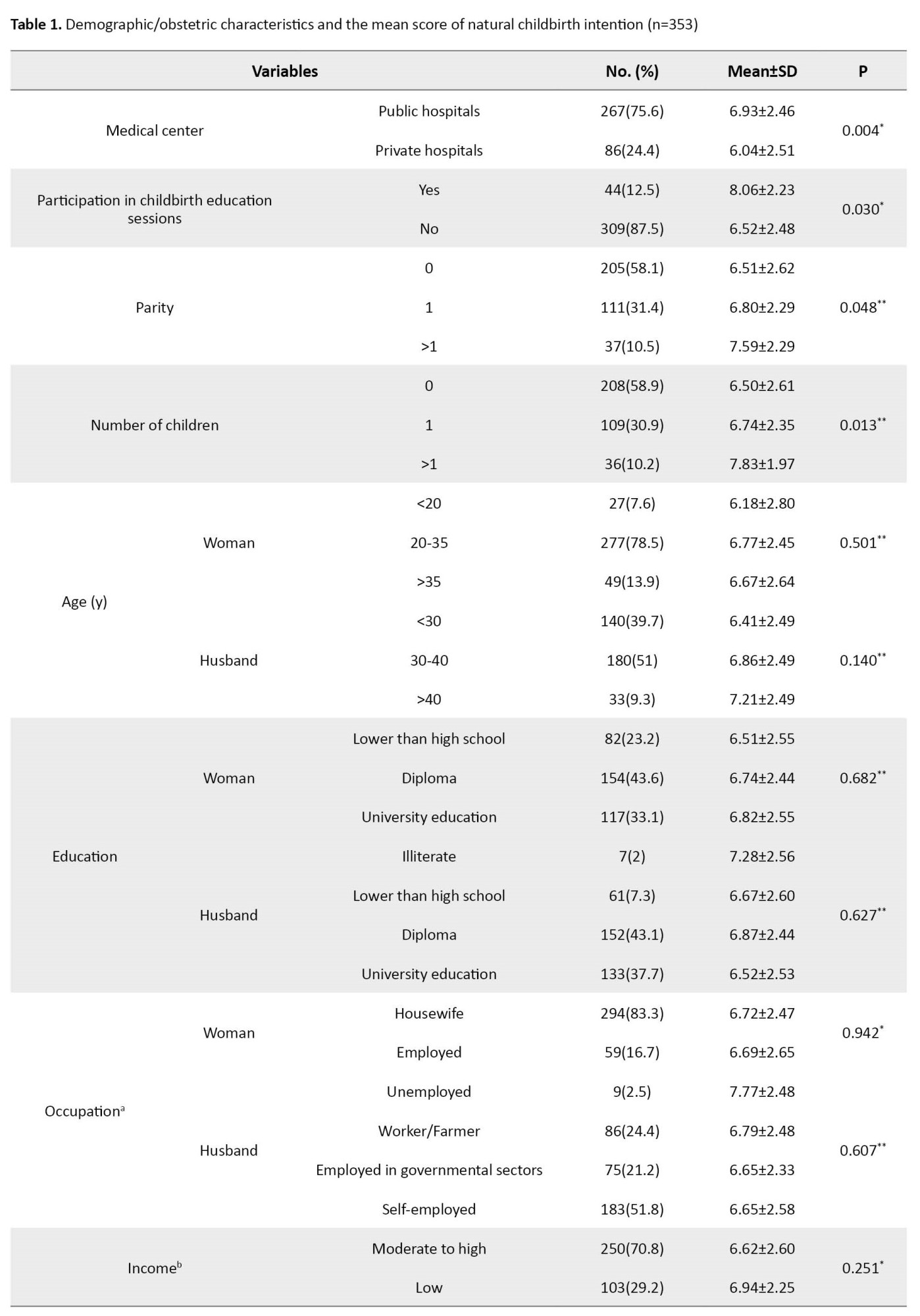
The mean score of the intention score was 6.71±2.50, out of 10. In this regard, 58.8% intended to give birth naturally. There was a strong and very strong positive correlation between natural childbirth intention and all TPB constructs and social support. The highest correlation was observed between intention and attitude (r=0.829, P=0.001). Correlation coefficients between natural childbirth intention and other constructs of TPB and social support were reported in Table 2.
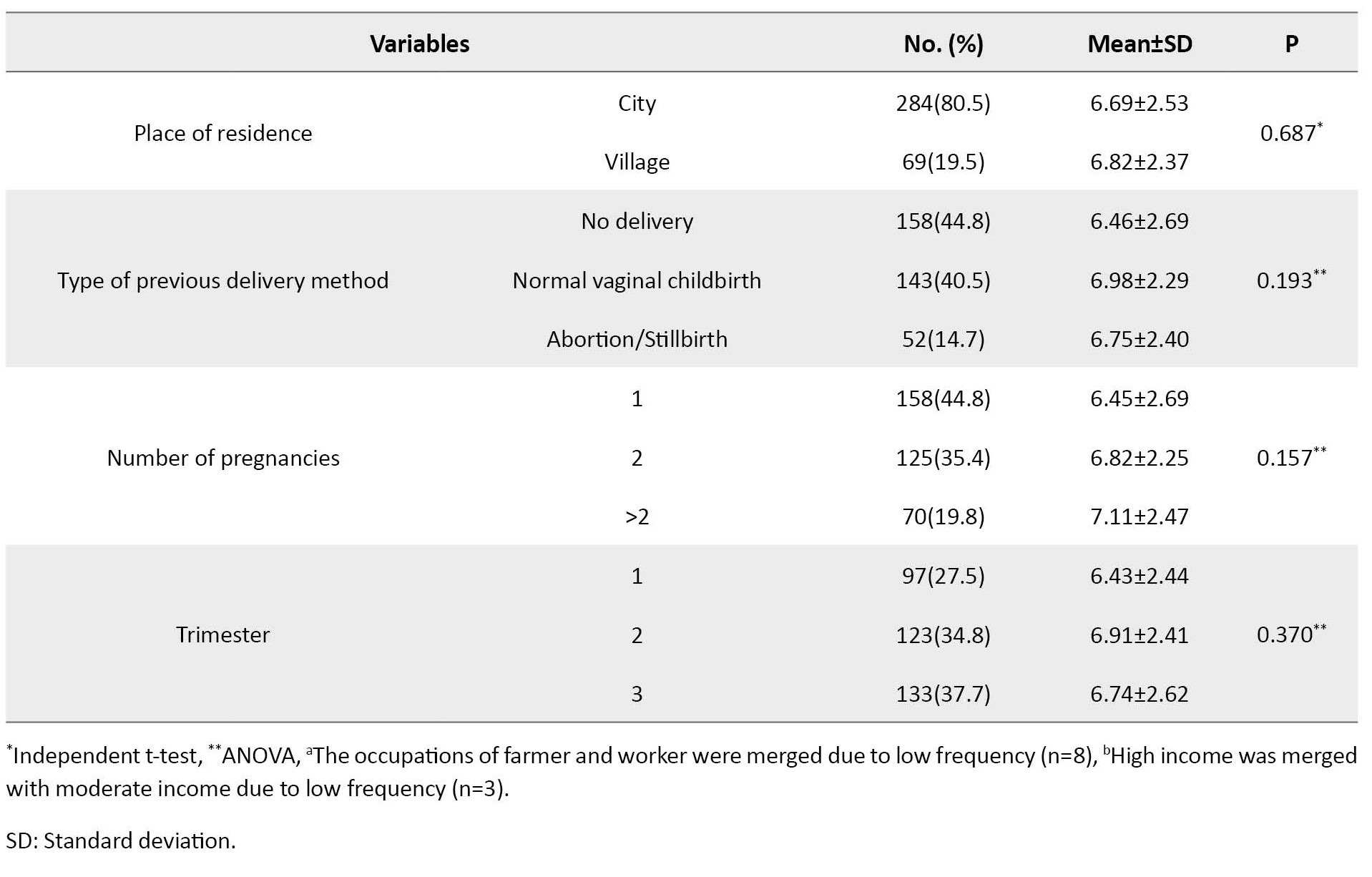
In the regression model, the coefficient of determination (R2) was obtained 72%. This means that attitude, perceived behavioral control, social support and participation in childbirth education classes together were able to predict 72% of variance in natural childbirth intention. Based on the results in Table 3, attitude alone was able to explain the variance in natural childbirth intention by 69% (β=0.12, 95% CI; 0.09%, 0.15%, P=0.0001) and one unit increase in the attitude mean score can increase the mean score of natural childbirth intention by 0.12.
Moreover, one unit increase in the mean score of each perceived behavioral control and social support variables can increase the mean score of natural childbirth intention by 0.06. Social support added 1.5% to the predictive power of the TPB model. One unit increase in the score of participation in educational sessions can increase the mean score of natural childbirth intention by 0.59. Based on beta coefficient value, the attitude variable was the best predictor of the natural childbirth intention.
Discussion
The purpose of the present study was to determine the predictors of natural childbirth intention based on the TPB and social support among pregnant women in northern Iran. More than half of the women intended to have a natural birth. This result is consistent with the result of other studies [15, 17, 25]. The mean score of natural childbirth intention in the study by Abdolkarimi et al. [21] was more than in the present study. In their study, the study population included pregnant women referred to rural health centers in Urmia, Iran. In the rural population, due to the tendency of people to traditional behaviors as well as economic problems and lower income, the probability of choosing natural childbirth is higher than in the urban population.
In the present study, the natural childbirth intention had a statistically significant relationship with parity, the number of children, participation in childbirth preparation sessions, the type of medical centers (public hospitals/private hospitals). There was no statistically significant relationship between the natural childbirth intention and educational level, occupation of pregnant women and their husbands, place of residence, income, previous childbirth experience, number of pregnancies. These results are not consistent with the results of other studies in Guilan Province [21, 25] and the study by Nouri Zadeh et al [26]. In Abdolkarimi et al.’s study [21], with increasing gestational age, the natural childbirth intention reduced and the CS intention increased. In the study by Moeini et al [25], a statistically significant relationship was observed between the choice of delivery method and the number of pregnancies, maternal age, income, and education. In the study by Nouri Zadeh et al [26], the level of education had also a significant relationship with selection of delivery method. Reasons for these discrepancies can be the difference in the study area or study populations.
In the present study, all constructs of TPB and social support had a direct correlation with the intention to have natural childbirth. This indicates that the attitudes, perceived behavioral control, subjective norms and social support in pregnant women are related to their intention to have natural childbirth, and this is probably due to high education and health literacy related to natural childbirth in women, although it does not ultimately lead to the choice of natural childbirth. In the present study, the natural childbirth intention had the highest correlation with attitudes. This finding is against the results of other studies [16, 17]. In Soheili et al.’s study [17], the intention had the highest correlation with the construct of subjective norms. The mean age of the participants in their study was 23.7 years. Due to the young age of the participants, it seems that they are more influenced by the pressure of significant others to choose natural childbirth. Another reason for discrepancy is that their study was conducted in the west of Iran, which can be attributed to cultural differences and climate. In the study by Ghasemi et al. [16], the intention had the highest correlation with the perceived behavioral control. Their study was conducted in the south of Iran. Due to the tendency of people towards natural childbirth in southern cities of Iran, it seems that people are more confident in their ability to have a natural childbirth. No study was found in other countries on the natural childbirth intention based on the TPB to compare the results.
Based on the multivariate regression model, the constructs of TPB without subjective norms were able to explain 72% of variance in natural childbirth intention. The best predictor of natural childbirth intention was attitude. This result is consistent with the result of some studies [20, 23], while is against the results of other studies [15, 17, 21], where the best TPB construct for explaining the variance in choosing the type of delivery method was subjective norms. The reason for the discrepancy is probably the differences in climate, demographic characteristics, cultural differences, and the level of literacy in samples. In the study by Rahmati Najarkolaei [15], most of the participants had a university education, while in our study, most of women had a high school diploma.
In the present study, social support increased the predictive power of TPB by 1.5%, which is consistent with the results of Otogara et al. where it was 3% [23]. The result suggests that pregnant women rely on their learning, experiences, thoughts, inner feelings, and their attitudes to choose their type of delivery, rather than being influenced by support from friends, family, or even the doctor. Promoting women’s awareness of the benefits of natural childbirth and training of midwives and nurses for providing a high standard prenatal and postnatal care for women can improve natural childbirth intention and eliminate misconceptions about this method.
This study had some limitations including the difficulty recruiting samples and short length of sampling phase due to the Covid-19 pandemic, and the use of a self-report questionnaire to collect information. The condition of pregnant women may affect their responses. Since attitude of women explained 96% of changes in natural childbirth intention in the present study, it seems to be useful to design educational TPB-based interventions with emphasis on attitudes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.367).
Funding
This study was funded by the Guilan University of Medical Sciences.
Authors' contributions
Conceptualization, data analysis, and writing: Nooshin Rouhani-Tonekaboni, Maryam Shakiba and Fatemeh Yousefi-Ghalehroodkhani; Editing & review: Fardin Mehrabian and Soodabeh Kazemi; Data collection: Fatemeh Yousefi- Ghalehroodghani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research and Technology of Guilan University of Medical Sciences and all pregnant women who participated in present study for their support and cooperation.
References
Natural vaginal childbirth is the most challenging physiological and psychological event in the life of women [1]. Cesarean section (CS), avoided for its alarming mortality rate over a little more than a century ago, is now the mode of delivery for one in three women in the United States [2] and up to four in five women in some other areas in the world [3]. CS has many complications for the mother and the child. Three known postpartum complications of CS include postpartum hemorrhage (PPH), surgical site infection (SSI), and venous thromboembolism (VTE). These complications contribute to maternal morbidity and mortality, increased healthcare costs, and prolonged hospital stays [4, 5, 6]. CS is now the most common surgery performed in the United States, with over 1 million women delivered by CS every year. The CS rate rose from 5% in 1970 to 31.9% in 2016 [7]. According to a meta-analysis research conducted using 41 studies from 1999-2016, the prevalence of CS was 48% in Iran and 52% in Guilan Province. In this study, the main causes of the prevalence of CS included higher education of mothers, previous history of CS, and physician advice [8]. In 1985, as part of a multidisciplinary report on appropriate technologies for childbirth, the Word Health Organization (WHO) concluded that there is no justification for any geographic region to have a CS rate of more than 10-15% [9]. According to the evidence, continuous and systematic educational interventions by health staff can have a significant impact on encouraging pregnant mothers to perform natural childbirth and reduce CS rate [10].
Health education and health-promoting models provide a framework for healthcare educators to use it to predict behaviors and subsequently design and implement educational interventions [11]. It has been empirically proven that if the provision of healthcare services is not sufficiently accompanied by health education, it will not be beneficial. In health education, higher and appropriate theoretical support along with providing basic health needs can cause the health education programs to be more effective. In this regard, the use of educational theories appropriate to the study society and the expected results can be very useful [12]. The theory of planned behavior (TPB) is a useful model for predicting health behaviors, designing educational interventions, and promoting health [13]. This theory is free to enter more variables to improve the predictive power [14]. According to the TPB, when people have enough time to think about what they want to do, the best predictor of their behavior will be their intention, which is determined by three factors, including their attitude, subjective norms, and perceived behavioral control. Attitude is a favorable or unfavorable assessment of a behavior that has been formed through past experiences. Subjective norms refer to the perceived social pressures from others for a person to behave in a certain manner. Perceived behavioral control refers to how much a person feels s/he is able to enact the behavior. Some studies have used TPB to predict childbirth intention and have reported its high predictive power [15, 16, 17]. Social support during pregnancy can promote better birth outcomes [18]. Studies have shown that some dimensions of social support, including informational and emotional support, are related to choosing the type of delivery [19]. Despite the provisions of training on natural childbirth preparation in health centers and the recommendations of the Ministry of Health and Medical Education about reducing CS, the change in the CS rate has not been significant in the last ten years in Guilan Province; therefore, effective educational interventions, especially in the frame of health education and health-promotion models are needed in this area. In Ghafari et al.’s study [20], all TPB constructs, including the attitude towards choosing natural childbirth had a significant relationship with choosing natural childbirth, such that after telephone follow-up, 71.15% of the women had natural birth. In Sohaili et al.’s study [17], subjective norms and perceived behavioral controls showed a significant relationship with the choice of the delivery method.
Therefore, by examining the psychological and social factors of the natural childbirth intention, the present study aims to determine the predictors of natural childbirth intention based on the TPB and investigate the perceived social support in pregnant women referred to selected hospitals in Rasht, Guilan Province, Iran.
Material and Methods
This is an analytic cross-sectional study. The study population consists of all pregnant women referred to the perinatal clinics in four hospitals in Rasht city in 2020. Inclusion criteria were being literate, Full consciousness, gestational age 1-9 months, age 15-45 years, no high-risk pregnancy, and indication for inforced CS by physician. Exclusion criteria were contraindications for natural childbirth according to the physician and return of incomplete questionnaire. Based on the results of Abdolkarimi et al. [21] and considering the natural childbirth intention (as a dependent variable) of 69%, 8% accuracy, 5% error, a dropout rate of 10%, and inclusion of 5 samples for each 46 items of the questionnaire, final sample size was determined 374, 124 samples in three groups of trimesters one, two and three.
Sampling was done by systematic random sampling method proportional to the population size. Sampling was performed in hospitals with prenatal clinics. In this regard, 180 samples were selected from teaching hospitals, 88 form public hospitals, 37 from private hospitals, and 48 from military hospitals. In private hospitals, because of the prevalence of COVID-19 pandemic and the low number of referred pregnant women, the convenience sampling method was used.
The data collection tool was a three-part questionnaire adapted from other studies [22, 23, 24]. The first part surveys demographic information of the pregnant women and their husbands (13 item). The second part included items related to the constructs of the TPB (2 items for intention, 15 items for attitude, 12 items for subjective norms, 9 items for perceived behavioral control). The items are scored on a 5-point Likert scale (1=strongly disagree to 5=strongly agree). The third part measures perceived social support with 8 items rated on a 5-point Likert scale (1=not at all to 5=extremely). This section was adapted from Otogara et al.’s study [23, 24]. The first part surveys demographic information of the pregnant women and their husbands (13 item). The second part included items related to the const]. Content validity was confirmed using the opinions of a panel of experts (five experts in health education and promotion, one gynecologist, one reproductive health specialist, and two epidemiologists). The content validity ratio (CVR) and content validity index (CVI) for the constructs of intention were obtained 1 and 1; for attitude, 0.95 and 0.97; for perceived behavioral control, 0.84 and 0.91; for subjective norms, 0.86 and 1; and for social support, 0.85 and 0.91, respectively which were acceptable (>0.7). For assessing the reliability, a pilot study was performed on 20 pregnant women. Cronbach’s α coefficient was obtained 0.97 for intention, 0.92 for attitude, 0.89 for subjective norms, 0.91 for perceived behavioral control, and 0.72 for social support.
Gestational age, previous childbirth experience, and participation in childbirth preparation programs were considered as confounding variables. The collected data were analyzed in SPSS software, version 21. Data were described using Mean±SD indices for quantitative variables and frequency and percentage for qualitative variables. Analysis of variance (ANOVA) and t-test were used to investigate the difference in natural childbirth intentions based on demographic variables. Pearson correlation test was used to examine the correlation between each of the subscales with natural childbirth intention. Multiple linear regression analysis (forward method) was used to determine the predictors of natural childbirth intention.
Results
Out of 374 samples with inclusion criteria, 21 people did not agree to participate in the research and total of 353 women participated in this study. Their characteristics are presented in Table 1.
The mean score of natural childbirth intention was not significantly different according to age, educational level, occupation of pregnant women and their husbands, place of residence, income, previous childbirth experience, number of pregnancies, and gestational age.
The mean score of the intention score was 6.71±2.50, out of 10. In this regard, 58.8% intended to give birth naturally. There was a strong and very strong positive correlation between natural childbirth intention and all TPB constructs and social support. The highest correlation was observed between intention and attitude (r=0.829, P=0.001). Correlation coefficients between natural childbirth intention and other constructs of TPB and social support were reported in Table 2.
In the regression model, the coefficient of determination (R2) was obtained 72%. This means that attitude, perceived behavioral control, social support and participation in childbirth education classes together were able to predict 72% of variance in natural childbirth intention. Based on the results in Table 3, attitude alone was able to explain the variance in natural childbirth intention by 69% (β=0.12, 95% CI; 0.09%, 0.15%, P=0.0001) and one unit increase in the attitude mean score can increase the mean score of natural childbirth intention by 0.12.
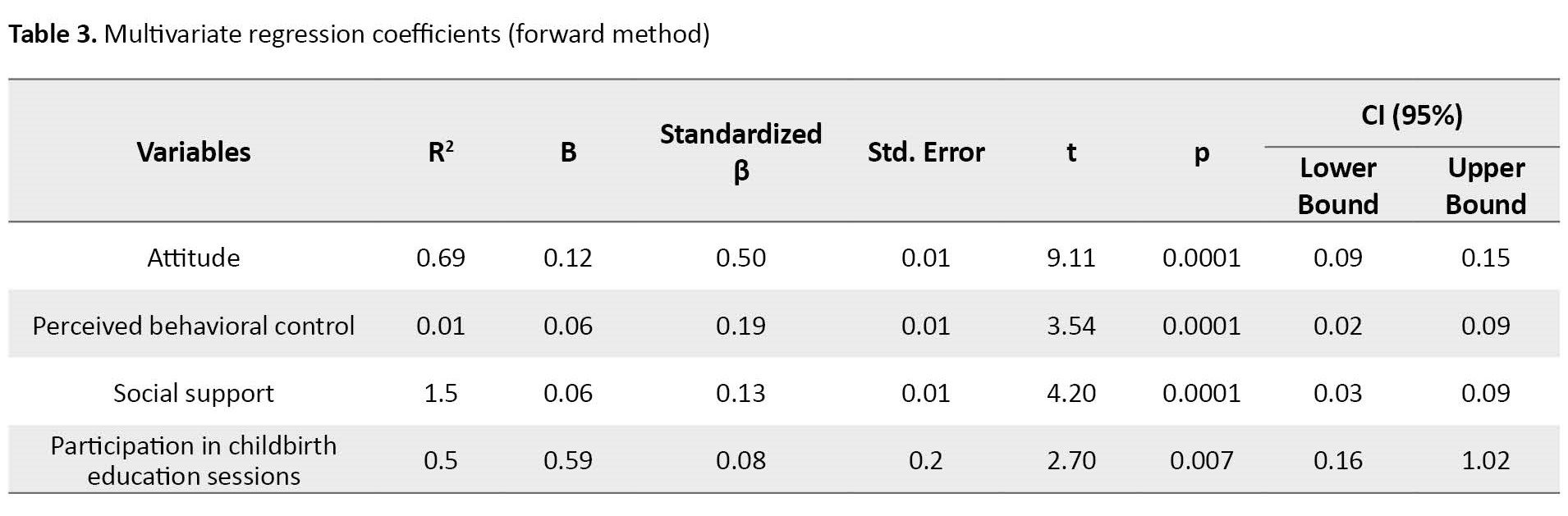
Moreover, one unit increase in the mean score of each perceived behavioral control and social support variables can increase the mean score of natural childbirth intention by 0.06. Social support added 1.5% to the predictive power of the TPB model. One unit increase in the score of participation in educational sessions can increase the mean score of natural childbirth intention by 0.59. Based on beta coefficient value, the attitude variable was the best predictor of the natural childbirth intention.
Discussion
The purpose of the present study was to determine the predictors of natural childbirth intention based on the TPB and social support among pregnant women in northern Iran. More than half of the women intended to have a natural birth. This result is consistent with the result of other studies [15, 17, 25]. The mean score of natural childbirth intention in the study by Abdolkarimi et al. [21] was more than in the present study. In their study, the study population included pregnant women referred to rural health centers in Urmia, Iran. In the rural population, due to the tendency of people to traditional behaviors as well as economic problems and lower income, the probability of choosing natural childbirth is higher than in the urban population.
In the present study, the natural childbirth intention had a statistically significant relationship with parity, the number of children, participation in childbirth preparation sessions, the type of medical centers (public hospitals/private hospitals). There was no statistically significant relationship between the natural childbirth intention and educational level, occupation of pregnant women and their husbands, place of residence, income, previous childbirth experience, number of pregnancies. These results are not consistent with the results of other studies in Guilan Province [21, 25] and the study by Nouri Zadeh et al [26]. In Abdolkarimi et al.’s study [21], with increasing gestational age, the natural childbirth intention reduced and the CS intention increased. In the study by Moeini et al [25], a statistically significant relationship was observed between the choice of delivery method and the number of pregnancies, maternal age, income, and education. In the study by Nouri Zadeh et al [26], the level of education had also a significant relationship with selection of delivery method. Reasons for these discrepancies can be the difference in the study area or study populations.
In the present study, all constructs of TPB and social support had a direct correlation with the intention to have natural childbirth. This indicates that the attitudes, perceived behavioral control, subjective norms and social support in pregnant women are related to their intention to have natural childbirth, and this is probably due to high education and health literacy related to natural childbirth in women, although it does not ultimately lead to the choice of natural childbirth. In the present study, the natural childbirth intention had the highest correlation with attitudes. This finding is against the results of other studies [16, 17]. In Soheili et al.’s study [17], the intention had the highest correlation with the construct of subjective norms. The mean age of the participants in their study was 23.7 years. Due to the young age of the participants, it seems that they are more influenced by the pressure of significant others to choose natural childbirth. Another reason for discrepancy is that their study was conducted in the west of Iran, which can be attributed to cultural differences and climate. In the study by Ghasemi et al. [16], the intention had the highest correlation with the perceived behavioral control. Their study was conducted in the south of Iran. Due to the tendency of people towards natural childbirth in southern cities of Iran, it seems that people are more confident in their ability to have a natural childbirth. No study was found in other countries on the natural childbirth intention based on the TPB to compare the results.
Based on the multivariate regression model, the constructs of TPB without subjective norms were able to explain 72% of variance in natural childbirth intention. The best predictor of natural childbirth intention was attitude. This result is consistent with the result of some studies [20, 23], while is against the results of other studies [15, 17, 21], where the best TPB construct for explaining the variance in choosing the type of delivery method was subjective norms. The reason for the discrepancy is probably the differences in climate, demographic characteristics, cultural differences, and the level of literacy in samples. In the study by Rahmati Najarkolaei [15], most of the participants had a university education, while in our study, most of women had a high school diploma.
In the present study, social support increased the predictive power of TPB by 1.5%, which is consistent with the results of Otogara et al. where it was 3% [23]. The result suggests that pregnant women rely on their learning, experiences, thoughts, inner feelings, and their attitudes to choose their type of delivery, rather than being influenced by support from friends, family, or even the doctor. Promoting women’s awareness of the benefits of natural childbirth and training of midwives and nurses for providing a high standard prenatal and postnatal care for women can improve natural childbirth intention and eliminate misconceptions about this method.
This study had some limitations including the difficulty recruiting samples and short length of sampling phase due to the Covid-19 pandemic, and the use of a self-report questionnaire to collect information. The condition of pregnant women may affect their responses. Since attitude of women explained 96% of changes in natural childbirth intention in the present study, it seems to be useful to design educational TPB-based interventions with emphasis on attitudes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.367).
Funding
This study was funded by the Guilan University of Medical Sciences.
Authors' contributions
Conceptualization, data analysis, and writing: Nooshin Rouhani-Tonekaboni, Maryam Shakiba and Fatemeh Yousefi-Ghalehroodkhani; Editing & review: Fardin Mehrabian and Soodabeh Kazemi; Data collection: Fatemeh Yousefi- Ghalehroodghani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Deputy for Research and Technology of Guilan University of Medical Sciences and all pregnant women who participated in present study for their support and cooperation.
References
- Khamehchian M, Adib-Hajbaghery M, HeydariKhayat N, Rezaei M, Sabery M. Primiparous women’s experiences of normal vaginal delivery in Iran: A qualitative study.BMC Pregnancy Childbirth. 2020; 20(1):259. [DOI:10.1186/s12884-020-02954-4] [PMID]
- Martin JA, Hamilton BE, Osterman M, Driscoll AK. Births: Final data for 2018. Natl Vital Stat Rep. 2019; 68(13):35-9. [Link]
- Nakamura-Pereira M, do Carmo Leal M, Esteves-Pereira AP, Domingues RM, Torres JA, Dias MA, et al. Use of Robson classification to assess cesarean section rate in Brazil: The role of source of payment for childbirth. Reprod Health. 2016; 13(Suppl 3):128.[DOI:10.1186/s12978-016-0228-7] [PMID]
- Butwick AJ, Ramachandran B, Hegde P, Riley ET, El-Sayed YY, Nelson LM. Risk factors for severe postpartum hemorrhage after cesarean delivery: Case-control studies. Anesth Analg. 2017; 125(2):523-32.[DOI:10.1213/ANE.0000000000001962] [PMID]
- D’Alton ME, Main EK, Menard MK, Levy BS. The national partnership for maternal safety. Obstet Gynecol. 2014; 123(5):973-7. [DOI:10.1097/AOG.0000000000000219] [PMID]
- Haidar ZA, Hoseini Nasab S, Moussa HN, Sibai BM, Blackwell SC. Caesarean delivery surgical site infection: What are expected rates and potentially modifiable risk factors? J Obstet Gynaecol Can. 2018; 40(6):684-9. [DOI:10.1016/j.jogc.2017.09.020] [PMID]
- No Author. ACOG Practice Bulletin No. 205: Vaginal birth after cesarean delivery. Obstet Gynecol. 2019; 133(2):e110-27. [DOI:10.1097/AOG.0000000000003078] [PMID]
- Rafiei M, Saei Ghare M, Akbari M, Kiani F, Sayehmiri F, Sayehmiri K, et al. Prevalence, causes, and complications of cesarean delivery in Iran: A systematic review and meta-analysis. Int J Reprod Biomed. 2018; 16(4):221-34. [PMID]
- No Author. Appropriate technology for birth. Lancet. 1985; 2(8452):436-7 [DOI:10.1016/S0140-6736(85)92750-3]
- Rabiepoor S, Alipoor P, Mesgarzadeh M, Shirzadeh E. [The effect of childbirth preparation training classes on attitude of women towards the delivey method (Persian)]. Nurs Midwifery J. 2017; 15(8):567-74. [Link]
- Saffari M, Shojaeizade D. [Principles and foundations of health promotion and education (Persian)]. Tehran: Samat; 2021.
- Tavasoli M, Heidar nia MA, Ghofranipour F. [Investigating the effect of education in reducing elective cesarean section in pregnant women (Persian)]. Tolooebehdasht. 2003; 2:39.
- Keshavarz Z, Ghazanfarian A, Simbar M, Shakeri N. [Effect of educational intervention based on theory of planned behavior (TPB) in selecting mode of delivery (Persian)]. Iran J Obstet Gynecol Infertil. 2016; 19(27):1-7. [DOI:10.22038/IJOGI.2016.7846]
- Ajzen I. The theory of planned behavior. Organ Behav HumDecis Processes. 1991; 50(2):179-211. [DOI:10.1016/0749-5978(91)90020-T]
- Rahmati Najarkolaei F, Eshraghi T, Dopeykar N, Zamani O. [Determinants of delivery type selection by using theory of planned behaviors (TPB) (Persian)]. Nurs Midwifery J. 2014; 12 (4):305-13. [Link]
- Ghasemi S, Nazari M, Vafaei H, Fararouei M. The impact of educational intervention based on the theory of planned behavior in choosing delivery mode in primigravida pregnant women. Int J Women's Health Reprod Sci. 2017; 5(1):47-54. [DOI:10.15296/ijwhr.2017.09]
- Soheili B, Mirzaei A, Sayemiri K, Ghazanfari Z. Predicting the behavioral intention of pregnant women’s choice of delivery method based on the theory of planned behavior: A cross-sectional study. J Basic Res Med Sci. 2017; 4(1):37-44. [DOI:10.18869/acadpub.jbrms.4.1.37]
- Dosar RZ, Meran NM. Impact of a social support for pregnant women upon their pregnancy outcomes at Maternity Hospitals in Baghdad City. Ann Romanian Soc Cell Biol. 2021; 25(6):14429-33. [Link]
- Moosavi A, Sheikhlou SG, Sheikhlou SG, Abdolahi K, Yaminifar L, Maktabi M. Influencing factors in choosing delivery method: Iranian primiparous women’s perspective. Electron Physician. 2017; 9(4):4150-4. [DOI:10.19082/4150] [PMID]
- Ghaffari M, Afshari A, Rakhshanderou S, Armoon B. Using theory of planned behavior for prediction of delivery mode among pregnant women: A theory-based cross-sectional research. Int J Adolesc Med Health. 2017; 32(2):/j/ijamh.2020.32.issue-2/ijamh-2017-0106/ijamh-2017-0106.xml. [DOI:10.1515/ijamh-2017-0106] [PMID]
- Abdolkarimi M, Zareipour M, Mahmoodi H, Rezaie Moradali M, Movahed E, Alinejad M. [Prediction of delivery type based on the theory of planned behaviors (Persian)]. Nurs J Vulnerable. 2016; 3(2):47-58. [Link]
- Besharati F, Hazavehei SMM, Moeini B, Moghimbeigi A. [Effect of educational interventions based on theory of planned behavior (TPB) in selecting delivery mode among pregnant women referred to Rasht health centers (Persian)]. Zanjan J Med Sci Health Serv. 2011; 19(77):94-106. [Link]
- Otogara M, Karimi-Shahanjarini A, Hazavehei SMM, Poorolajal J, Radnia N, Tabib MS. The effects of social support on pregnant women’s choice of delivery method: Application of an Expanded Theory of Planned Behavior. Crescent J Med Biol Sci. 2018; 5(3):181-8. [Link]
- Tai CY. Development of an investigator-designed questionnaire concerning childbirth delivery options based on the theory of planned behavior [PhD dissertation]. Florida: University of South Florida; 2013. [Link]
- Moeini B, Besharati F, Hazavehei SMM, Moghimbeigi A. [Women’s attitudes toward elective delivery mode based on the theory of planned behavior (Persian)]. J Guilan Uni Med Sci. 2011; 20(79):68-76. [Link]
- Nouri Zadeh R, Mohammadpour Asl A, Kazempour R, Bakhtari Aghdam F. [Selection of mode of delivery and its related factors in pregnant women in Marand (Persian)]. J Urmia Nurs Midwifery. 2009; 7(1):50-7. [Link]
Article Type : Research |
Subject:
Special
Received: 2022/07/6 | Accepted: 2023/05/31 | Published: 2024/01/1
Received: 2022/07/6 | Accepted: 2023/05/31 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |