Tue, Feb 3, 2026
Volume 35, Issue 2 (3-2025)
JHNM 2025, 35(2): 109-118 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bhatt L, Ghimire P, Khadka A, Raj Joshi M, Gurung T, Gurung L. Quality of Life of Postmenopausal Women Residing in Lalitpur District, Nepal. JHNM 2025; 35 (2) :109-118
URL: http://hnmj.gums.ac.ir/article-1-2238-en.html
URL: http://hnmj.gums.ac.ir/article-1-2238-en.html
1- Hospital Nursing Inspector, Department of Surgery, Seti Provincial Hospital, Kailali, Nepal.
2- Public Health Inspector, Health Section, Chandragiri Municipality, Kathmandu, Nepal. ,prakash.ghimire707@gmail.com
3- Nursing Officer, Department of Emergency, Kanti Children’s Hospital, Kathmandu, Nepal.
4- Public Health Inspector, Sudurpaschim Provincial Health Directorate, Doti, Nepal.
5- Bachelor in Public Health, School of Public Health, Chitwan Medical College, Bharatpur, Nepal.
6- Public Health Inspector, Health Section, Byas Municipality, Tanahu, Nepal.
2- Public Health Inspector, Health Section, Chandragiri Municipality, Kathmandu, Nepal. ,
3- Nursing Officer, Department of Emergency, Kanti Children’s Hospital, Kathmandu, Nepal.
4- Public Health Inspector, Sudurpaschim Provincial Health Directorate, Doti, Nepal.
5- Bachelor in Public Health, School of Public Health, Chitwan Medical College, Bharatpur, Nepal.
6- Public Health Inspector, Health Section, Byas Municipality, Tanahu, Nepal.
Full-Text [PDF 507 kb]
(356 Downloads)
| Abstract (HTML) (827 Views)
Full-Text: (275 Views)
Introduction
Menopause is an event in women’s lives accounting for decreased reproductive hormone levels, particularly at the age of 45-55 years [1-3]. Inadequacy of these hormones results in the experience of vasomotor, somatic, psychological, and sexual symptoms that could hinder the quality of life (QoL) of post-menopausal women [4]. It has been estimated that the number of postmenopausal women aged ≥50 worldwide will reach more than 1 billion by 2025 [5]. In developing countries, due to not giving proper attention to the health of menopausal women, these women are suffering from various menopause-related health problems and are at risk for osteoporosis and cardiovascular diseases [6]. The type, severity, and duration of menopausal symptoms are varied in women. The most prevalent symptom in Egyptian women was reported to be low back pain (86%) [3]. Asian women were found to experience mostly somatic symptoms followed by vasomotor, sexual, and psychological symptoms [7]. In Nepal, the majority of postmenopausal women had a feeling of tiredness followed by a decline in stamina, decreased physical strength and lack of energy [8].
Previous studies have indicated the prevalence of menopausal complaints in postmenopausal women and its association with their QoL [9]. Menopausal symptoms have a substantial influence on women’s work, social activities, sexual fulfilment, quality of sleep, temperament, and concentration [10]. Some studies found that older age, marital status, health-seeking behaviours, physical inactivity, hand working, lesser economic status, educational level, occupation and number of children were predictors of QoL in postmenopausal women [3, 8, 11]. In Nepal, the patriarchal dominance and the ignorance of menopausal symptoms have made women have poor QoL after menopause. There are limited community-based studies on the QoL of postmenopausal women in Kathmandu Valley, Nepal. Therefore, to fill this research gap, this study aimed to assess the QoL of postmenopausal women in the Lalitpur District, Nepal. This study can be helpful for identifying Nepali postmenopausal women’s healthcare requirements for having an ideal QoL.
Material and Methods
This is a community-based analytical study with a cross-sectional design that was conducted on postmenopausal women aged 45-60 years residing in Mahalaxmi municipality, Lalitpur district located in the central part of Nepal in August 2022. Using the Cochran formula [12], the required sample size was obtained as 215 after considering a 10% sample dropout rate. Samples were selected using a systematic random sampling technique. The total population size of women aged 45-60 years was obtained from the records of the ward office. Then, the sampling interval (kth) was calculated by dividing the total population by the sample size. The first sample was randomly selected followed by consecutive sampling at every kth interval until reaching the required sample size. The inclusion criteria were age 45-60 years, a history of menopause for at least one year, willingness to participate in the study, no history of hysterectomy, being on hormone therapy, and no history of diabetes mellitus, thyroid disorders, hypertension, and cardiac disease based on women’s health records.
The instrument used in this study had two parts. The first part included questions related to sociodemographic characteristics, and the second part was the Menopause-specific QoL (MENQOL) questionnaire, which included items measuring the QoL of postmenopausal women. In this study, the Nepali version of this tool was used, which was translated using the forward-backward translation method and with the help of experts. The MENQOL has also been previously used in a study in Nepal [13]. The MENQOL is a valid tool developed by Hilditch and Lewis [14]. It assesses the impact of menopausal symptoms experienced in the past 30 days. It consists of 29 items and four domains of vasomotor symptoms (3 items), psychosocial symptoms (7 items), physical symptoms (16 items) and sexual symptoms (3 items). The scoring for each domain is identical. Each item is scored from 0 (not bothersome) to 6 (extremely bothersome). The total score is obtained by summing up the four domains’ overall scores. The higher total score indicates a lower QoL. Menopausal symptoms’ severity was categorized as mild (score 2-4), moderate (score 5-6), and severe (score 7-8). The QoL level was classified asgood (scores≤ Mean-1 SD), moderate (scores between Mean-1 SD and Mean+1 SD), and poor (scores ≥ Mean+1 SD) based on the mean and standard deviation of the MENQOL total score [15]. In our study, internal consistency of the MENQOL was tested on 22 samples and a Cronbach’s α of 0.87 was obtained.
Data analysis was done in the SPSS software, version 20. Descriptive statistics such as frequency, percentage, mean, median, and standard deviation were used to describe the data. Inferential statistics, including the chi-square test, was used to examine the difference in QoL based on the sociodemographic variables.
Results
A total of 215 postmenopausal women were included in the study (100% response rate). More than one-third of them (41.9%) had age 55-60 years. The mean age of the women was 54.51±3.83 years. The majority of them (87.4%) were married. Almost two-thirds (74%) were living in a joint family. Most of the women (66%) had no formal or informal education and were illiterate. Also, 48.4% of the participants had 1-2 children. More than half of the participants (52%) had their menarche after the age of 15 (Table 1). The occupation of about half of them (45.58%) was agriculture. Also, the majority (54.4%) had their menopause for ≤5 years.

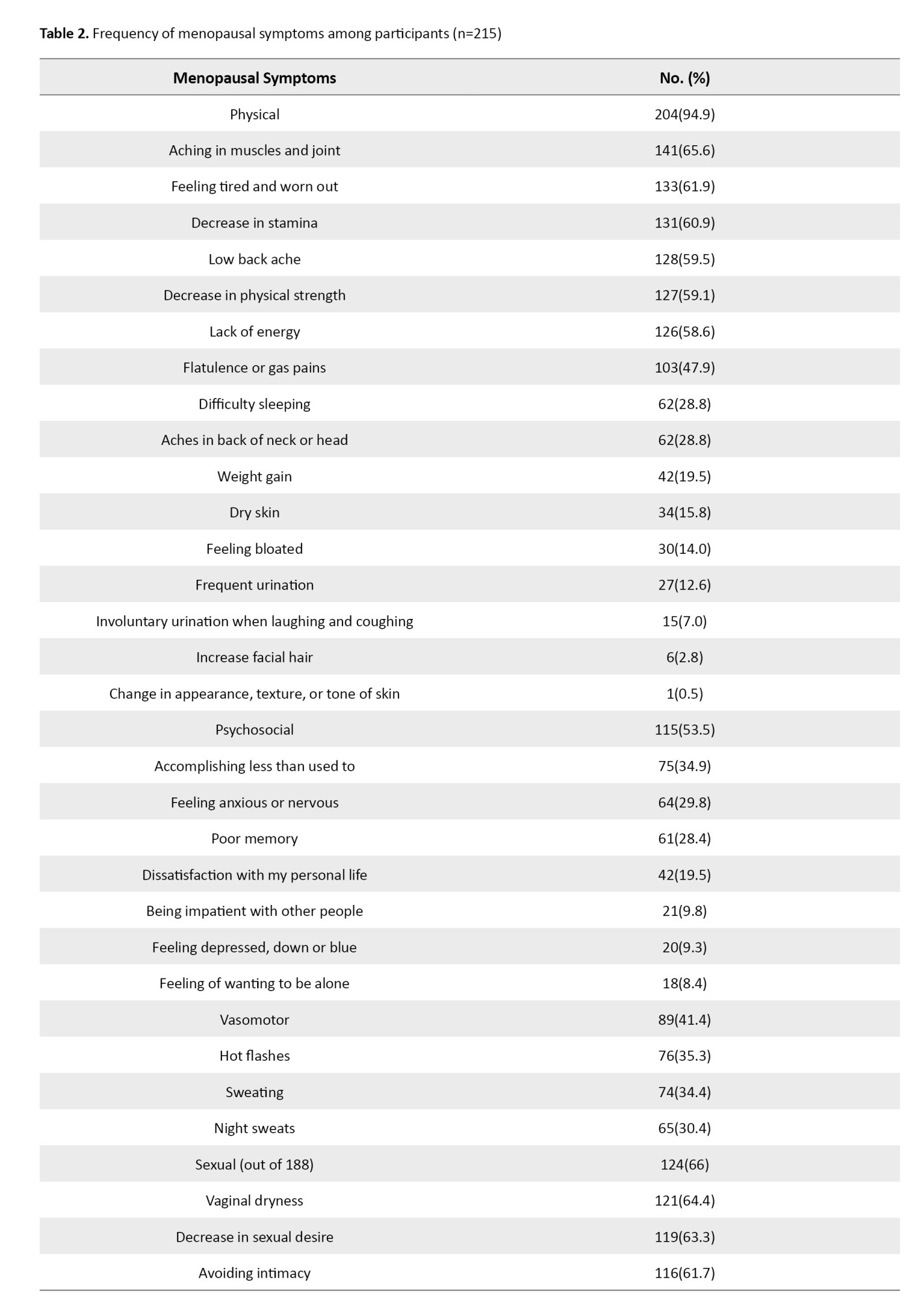
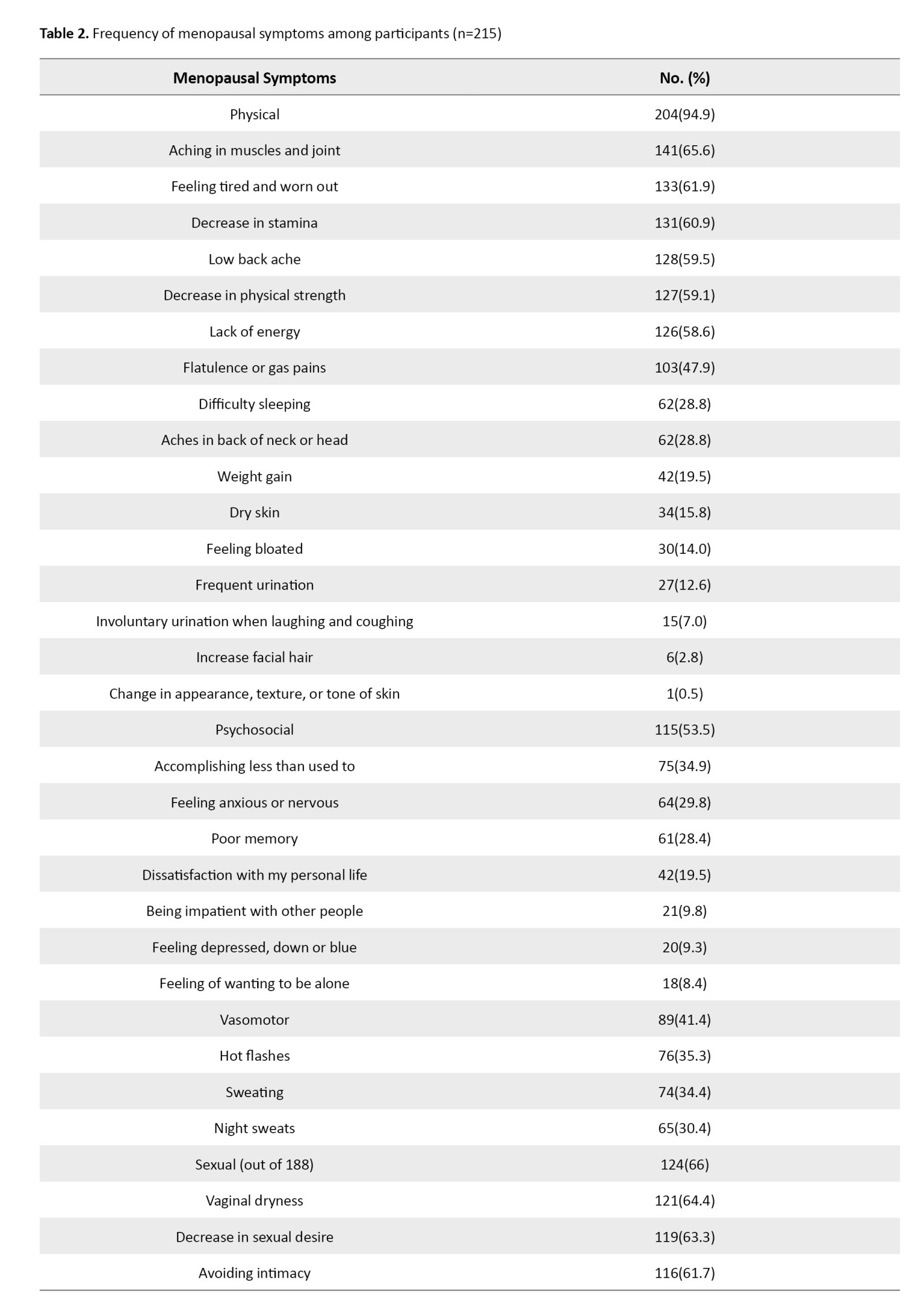
The menopause-related physical symptoms were most prevalent among women (94.9%). More than half of them had experienced physical symptoms such as muscle and joint pain (65.6%), feeling tired or worn out (61.9%), decrease in stamina (60.9%), low back pain (59.5%), decrease in physical strength (59.1%), and lack of energy (58.6%). The menopause-related psychosocial and vasomotor symptoms were prevalent among 53.5% and 41.4% of the participants, respectively. Out of 188 married women, 66% had experienced menopause-related sexual symptoms. Furthermore, among psychosocial symptoms, most of women reported accomplishing less than they used to (34.9%). More than one-third (35.3%) of women had experienced vasomotor symptoms such as hot flashes, sweating (34.4%), and night sweats (30.4%). These results were shown in Table 2.
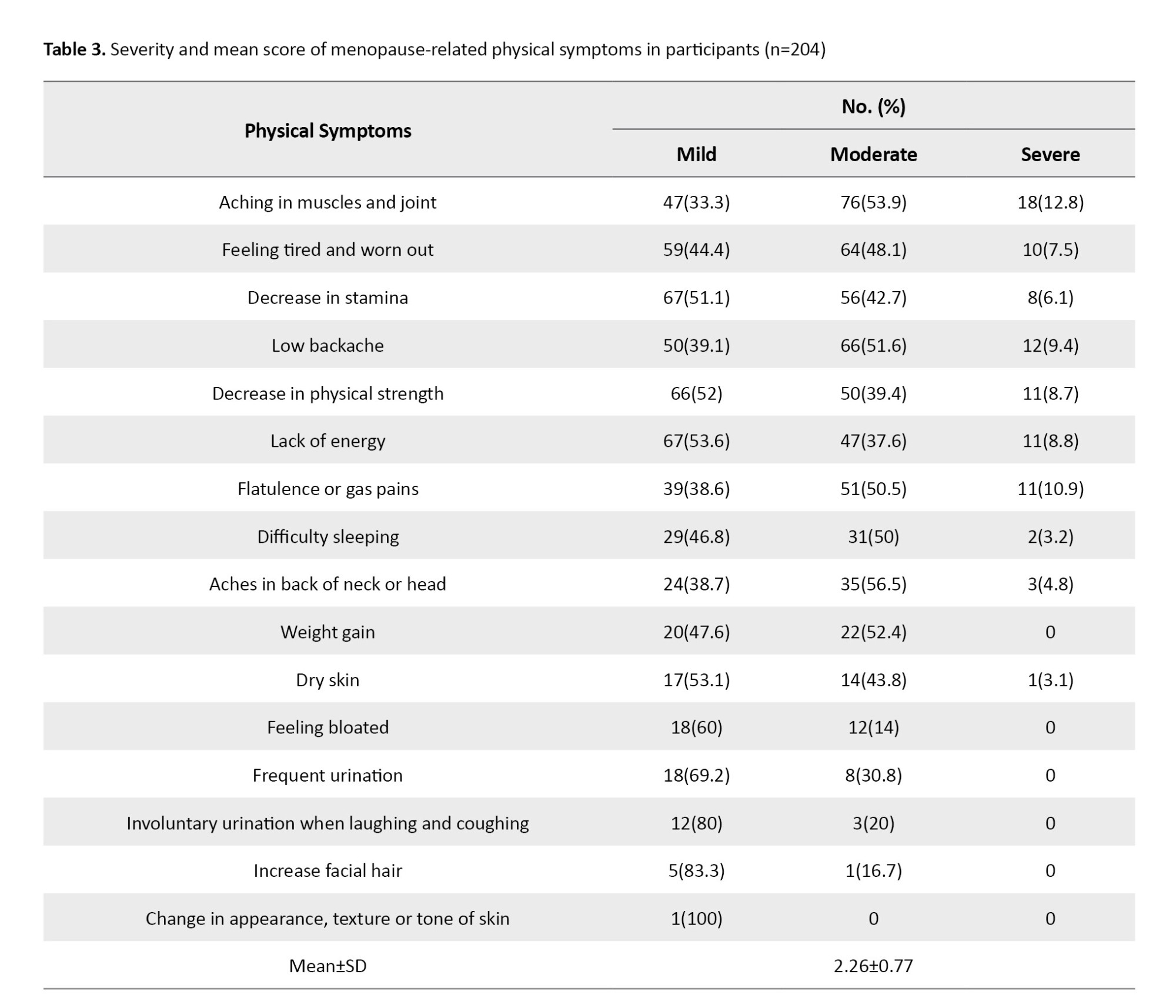
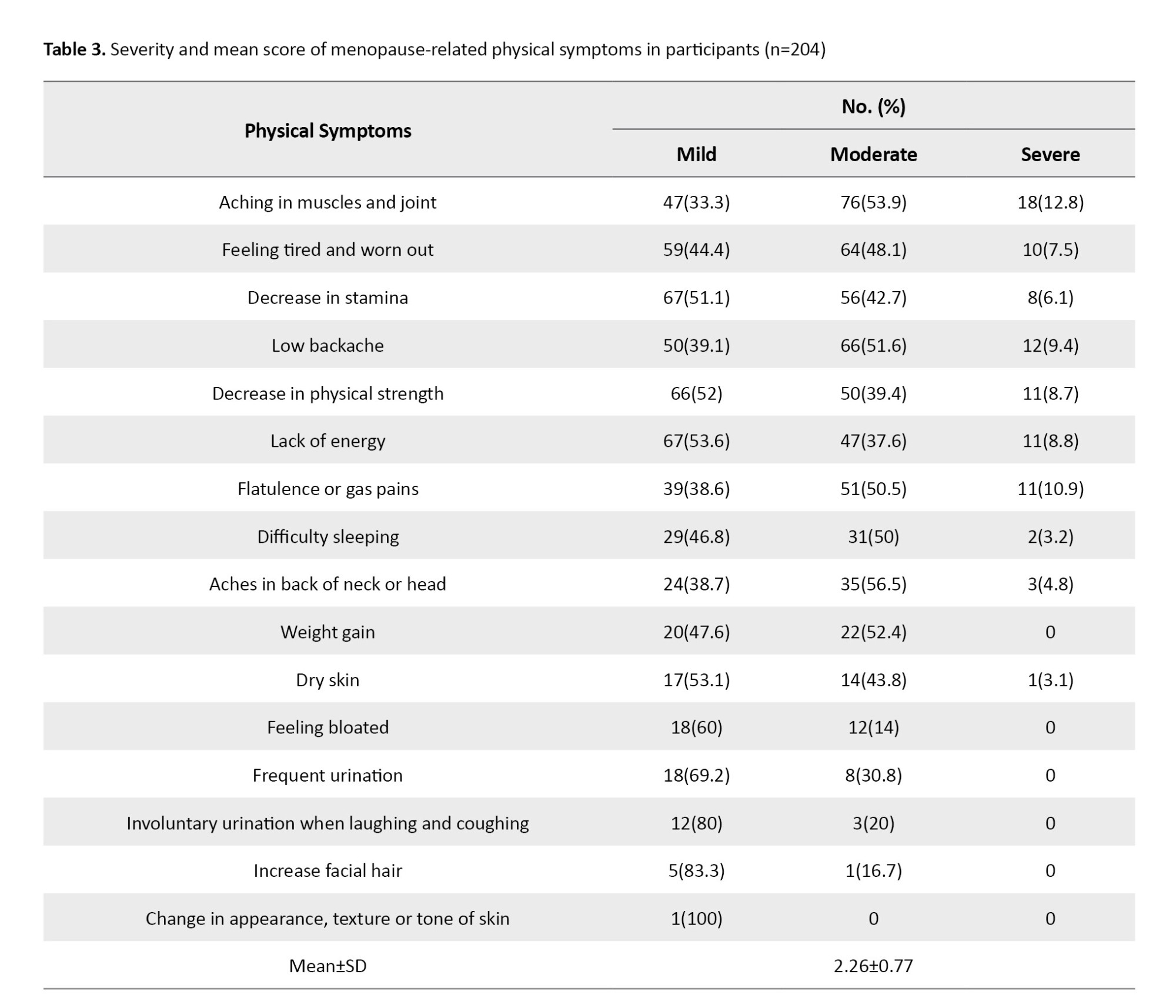
Regarding physical symptoms, more than half of the women had rated the muscle and joint aches as moderate (53.9%), followed by 33.3% as mild and 12.8% as severe. The mean score of the physical domain of the MENQOL was 2.26±0.77 (Table 3).
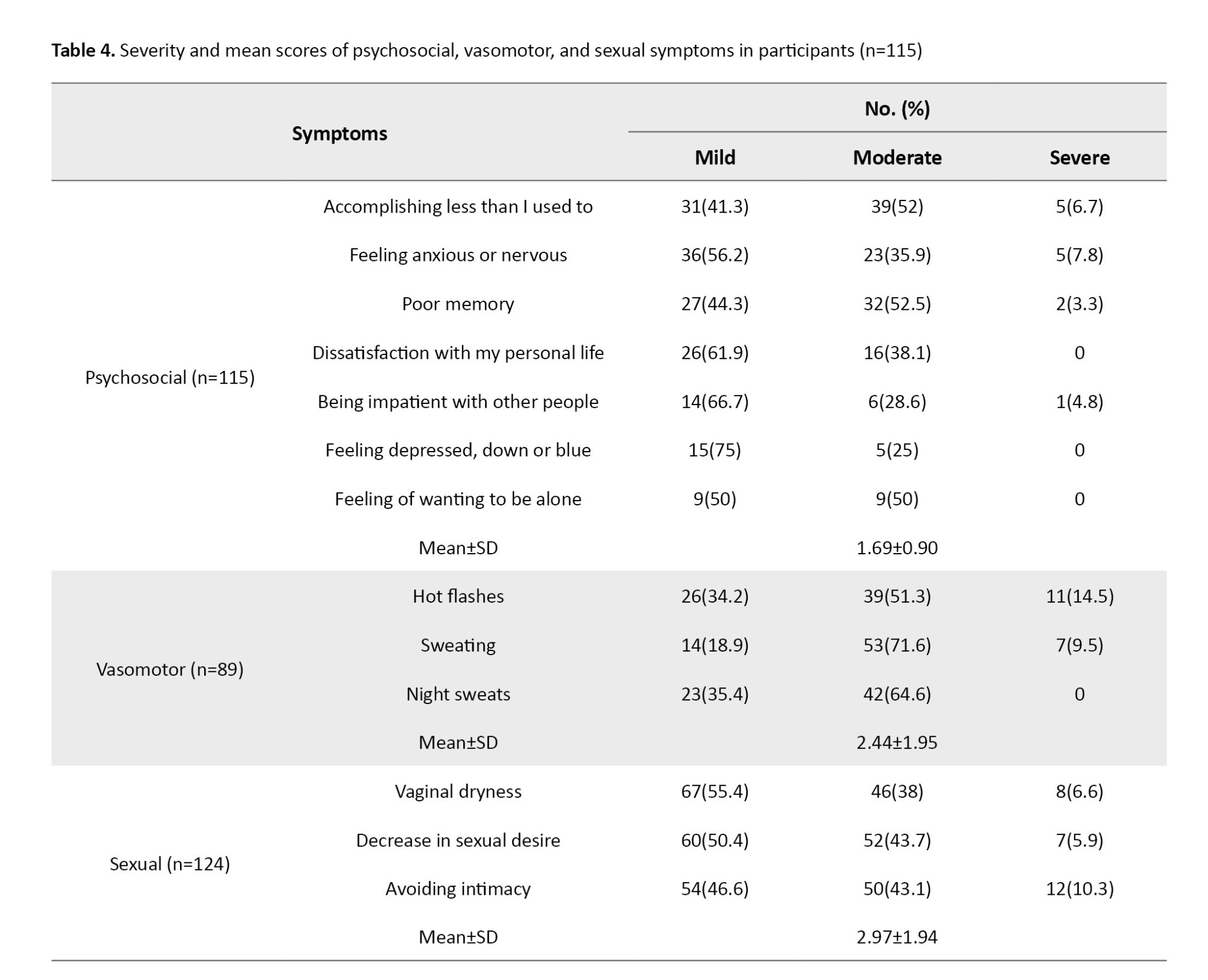
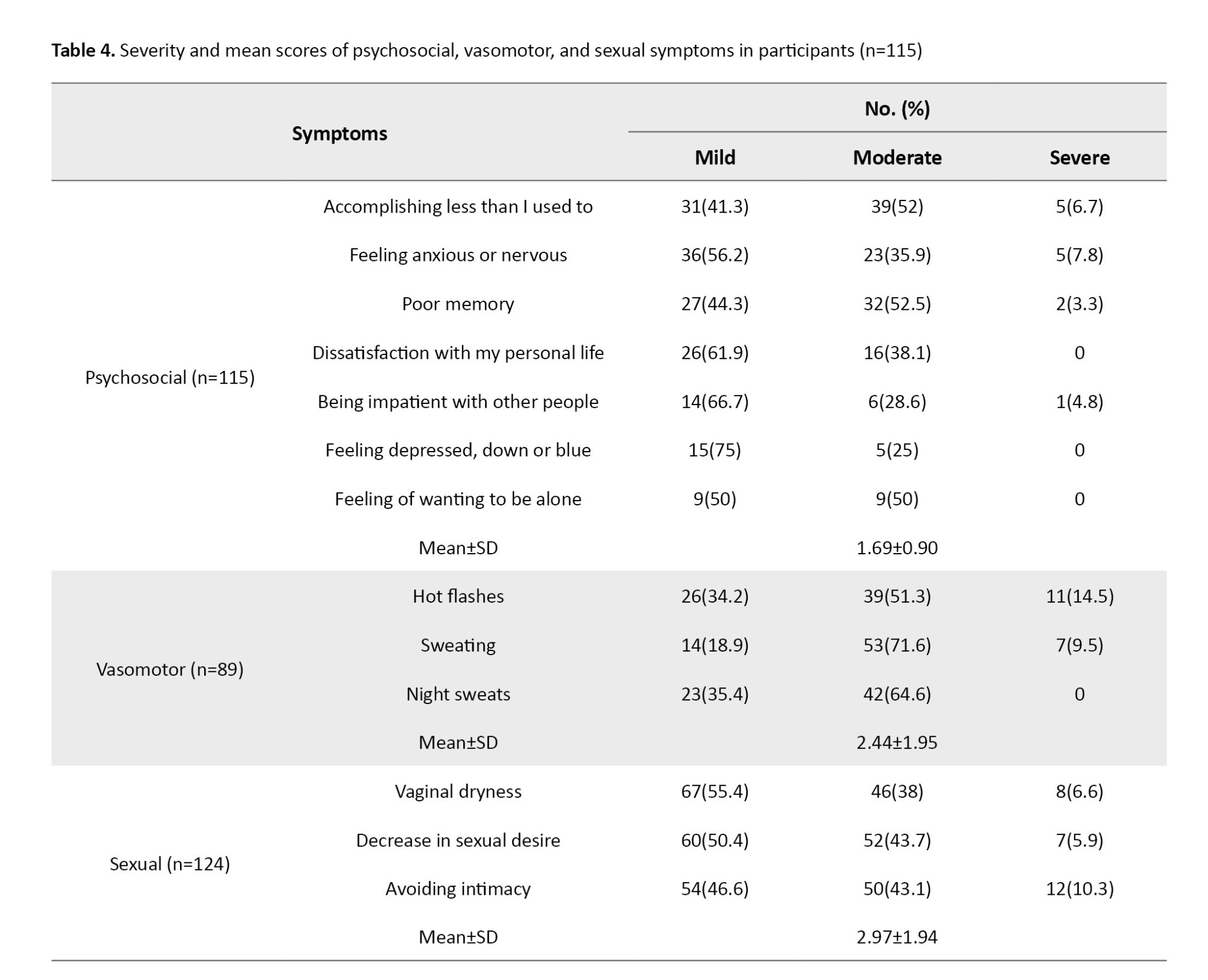
The mean score of the sexual domain (2.97±1.94) was higher than the mean scores of the psychosocial (1.69±0.90) and vasomotor (2.44±1.95) domains. The majority (52.5%) of the women had a moderate level of poor memory, followed by 44.3% with a mild level and 3.3% with a severe level. Severe levels of hot flashes and sweating were reported in 14.5% and 9.5% of the participants. Sexual symptoms such as avoiding intimacy, vaginal dryness and decrease in sexual desire were found to be severe in 10.3%, 6.6%, and 5.9% of the participants, respectively (Table 4).
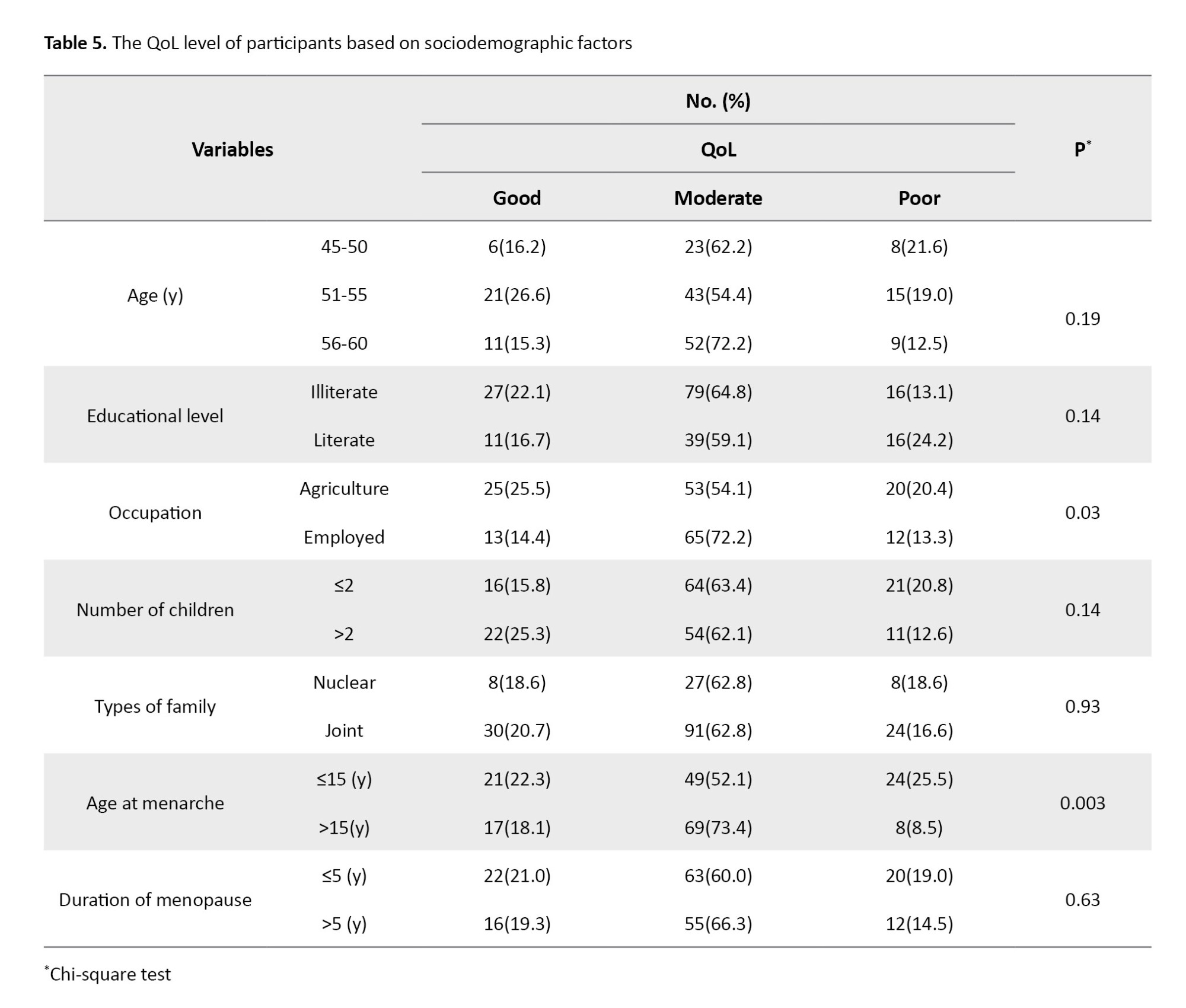
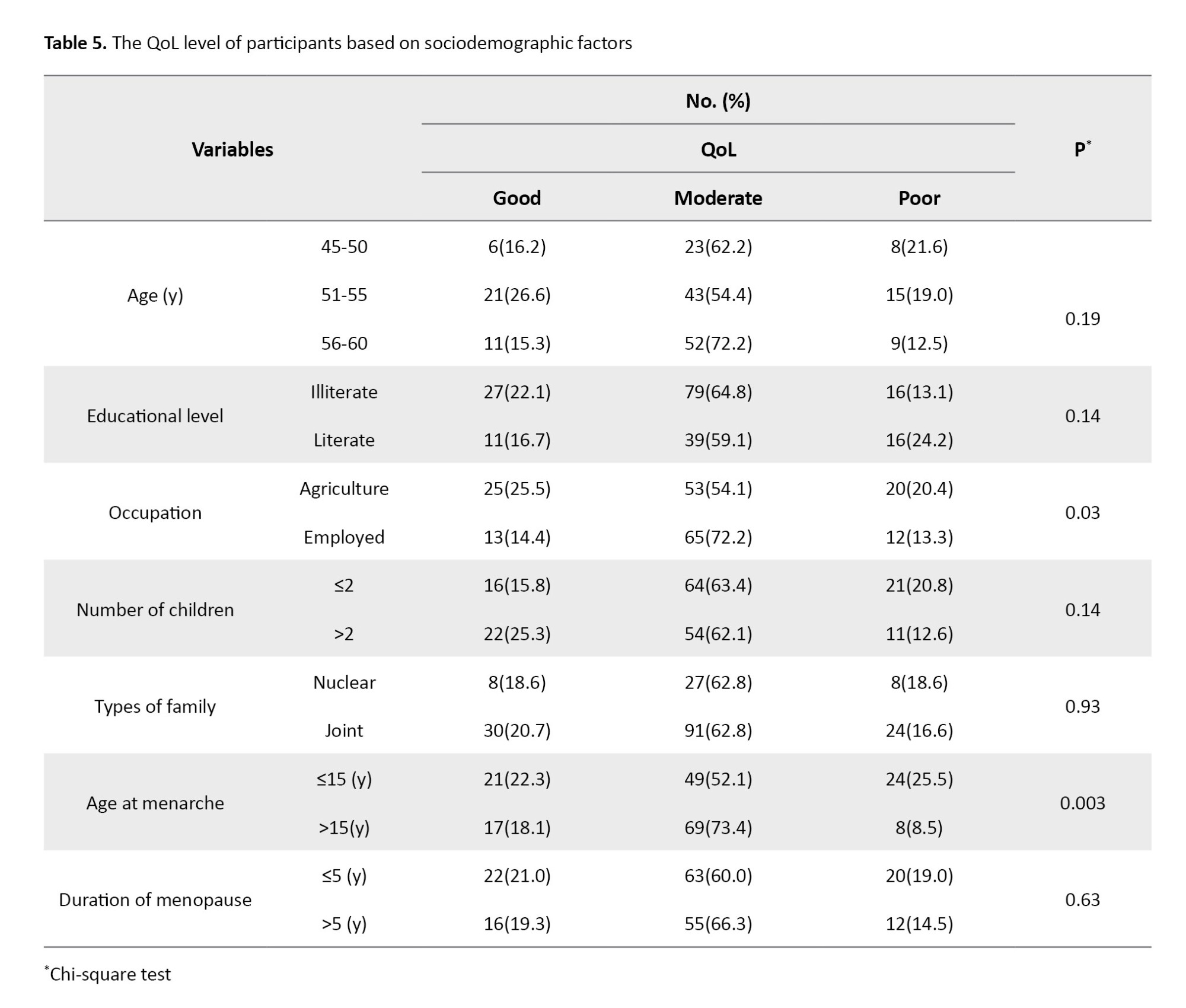
Based on the results, 62.8% of the women had moderate QoL, whereas only 20.2% had good QoL. As shown in Table 5, the level of QoL among postmenopausal women was significantly different based on occupation (P=0.03) and age at menarche (P=0.003).
Discussion
This research aimed to determine the prevalence of menopausal symptoms and the QOL in Nepali postmenopausal women and examine the difference in their QOL according to their sociodemographic characteristics. The results showed that almost all women had experienced at least one menopausal symptom based on the MENQOL domains. A consistent finding was observed in a previous study conducted on women aged 40-60 years in Nepal, which showed that 92% of the women had experienced at least one menopausal symptom [10]. A community-based study on postmenopausal women in Morang district, Nepal also demonstrated that majority of the women had at least one menopausal symptom according to the MENQOL [16]. Our results are also consistent with the results of Ghimire et al. [17].
Most prevalent menopausal symptoms among women in our study were physical symptoms followed by sexual, psychosocial, and vasomotor symptoms. A previous study on postmenopausal women from Nepal also showed that the overall mean score of MENQOL was higher in the physical domain, followed by psychosocial, sexual, and vasomotor domains [13], which the results of this study is consistent with them. Another study in Nepal reported that 100% of the postmenopausal women had physical symptoms [10]. Similarly, a previous study found that vasomotor symptoms were the least prevalent symptoms among postmenopausal women [13]. Conversely, a study conducted in Nepal showed that menopausal symptoms were highly prevalent [17]. The possible reasons for this discrepancy may be due to differences in comorbidities, dietary habits, environmental conditions, economic factors and ethnicity [16, 18].
The top four most common menopause-related physical symptoms in our study were muscle and joint aches, feeling tired and worn out, decrease in stamina, and low backache. This is in line with the results of a study in India [19]. However, it is against the finding of a study conducted in East Delhi, where the most common physical symptom was a decrease in physical strength [20]. The top four most common psychosocial symptoms in women who participated in this study were accomplishing less than before, feeling anxious and nervous, poor memory, and dissatisfaction with personal life. A cross-sectional study on postmenopausal women of 45-60 years from Nepal also reported that accomplishing less than before was the main symptom [21]. However, a study in India reported that poor memory was the most common psychosocial symptom [22]. In a study in Iran, anxiety was found to be the major psychosocial symptom [23]. These discrepancy may be due to differences in the sociodemographic status of women.
In the current study, women’s most common vasomotor symptoms were hot flashes, sweating, and night sweats. Similar to the current study, Prajapati et al. found that hot flashes were the major vasomotor symptom among postmenopausal women in Nepal [21]. Another study reported a similar finding regarding the higher frequency of hot flashes as a vasomotor symptom among postmenopausal women [23]. However, sweating was a common vasomotor symptom among postmenopausal women in Thapa and Thebe’s study in a rural area of Nepal [8]. This discrepancy can be due to differences in the temperature of the study environment and the varied experiences of women.
Regarding the sexual symptoms, the majority of married women in our study had experienced at least one symptom. The most common sexual symptoms were vaginal dryness, decrease in sexual desire, and avoid intimacy. In contrast to our finding, a study on postmenopausal women in rural and urban areas of Sikkim, India, reported that the most common sexual symptom was the avoidance of intimacy [24]. A study in Nepal reported avoiding intimacy as the most common sexual symptom, followed by a decrease in sexual desire and vaginal dryness [8]. The possible reasons for this discrepancy may be the cultural difference and the difference in the subjective nature of participants. Several parts of Nepal, especially the rural areas, still have a culture of silence and do not have the intention to talk freely with others about sexual matters.
The current study reported that the majority of the postmenopausal women had moderate QoL. This is similar to the results of Parsa et al.’s study [25]. A meta-analysis conducted in 2020 reported a similar finding, where the QoL of postmenopausal women in Iran was greater than the moderate level [26]. A study in India also demonstrated a similar result since a low number of postmenopausal women had poor QoL [27]. However, a previous study in Nepal reported a contradictory result, where the majority of the postmenopausal women had poor QoL [28]. The majority of women in postmenopausal women from Malaysia had poor QoL [29]. Moreover, a study in India on middle-aged women (40-60 years) found that most of the women were experiencing poor QoL [30]. These discrepancies may be due to different categorizations of symptoms for a particular domain, different study settings, and the use of different tools to assess QoL.
The current study observed that the overall MENQOL score of postmenopausal women was significantly different in terms of occupation and age at menarche. A systemic review and meta-analysis supported that age at menarche was associated with QoL of women [31]. Conversely, a study found no association between age at menarche and health QoL [32]. Findings of Thapa and Thebe in Nepal showed that occupational status and QoL were significantly related [8]. Meanwhile, Senthilvel et al. found no association between occupational status and QoL of postmenopausal women [33].
The strength of this study is its community-based cross-sectional design used to assess the menopausal symptoms and QoL of postmenopausal women. The findings provide gross information about the QoL of postmenopausal women in Nepal, which can help local authorities address the related problems and pave the way for future studies. However, this study was limited to only one district of Nepal. Therefore, the results cannot be generalized to all postmenopausal women in Nepal. Thus, further studies in other provinces and districts of Nepal are recommended to determine the QoL level of postmenopausal women.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Patan Academy of Health Sciences, Lalitpur, Nepal (Code: PNC2206241646). Written informed consent was obtained from all participants prior to data collection. The participants were informed about their right to leave the study at any time. Confidentiality of participants was maintained throughout the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Data collection, data analysis and interpretation: Prakash Ghimire, Lalita Bhatt and Alisha Khadka; Preparation of draft and review: Prakash Ghimire, Lalita Bhatt, Tina Gurung, Laxmi Gurung and Min Raj Joshi; Conceptualization, study design and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
References
Menopause is an event in women’s lives accounting for decreased reproductive hormone levels, particularly at the age of 45-55 years [1-3]. Inadequacy of these hormones results in the experience of vasomotor, somatic, psychological, and sexual symptoms that could hinder the quality of life (QoL) of post-menopausal women [4]. It has been estimated that the number of postmenopausal women aged ≥50 worldwide will reach more than 1 billion by 2025 [5]. In developing countries, due to not giving proper attention to the health of menopausal women, these women are suffering from various menopause-related health problems and are at risk for osteoporosis and cardiovascular diseases [6]. The type, severity, and duration of menopausal symptoms are varied in women. The most prevalent symptom in Egyptian women was reported to be low back pain (86%) [3]. Asian women were found to experience mostly somatic symptoms followed by vasomotor, sexual, and psychological symptoms [7]. In Nepal, the majority of postmenopausal women had a feeling of tiredness followed by a decline in stamina, decreased physical strength and lack of energy [8].
Previous studies have indicated the prevalence of menopausal complaints in postmenopausal women and its association with their QoL [9]. Menopausal symptoms have a substantial influence on women’s work, social activities, sexual fulfilment, quality of sleep, temperament, and concentration [10]. Some studies found that older age, marital status, health-seeking behaviours, physical inactivity, hand working, lesser economic status, educational level, occupation and number of children were predictors of QoL in postmenopausal women [3, 8, 11]. In Nepal, the patriarchal dominance and the ignorance of menopausal symptoms have made women have poor QoL after menopause. There are limited community-based studies on the QoL of postmenopausal women in Kathmandu Valley, Nepal. Therefore, to fill this research gap, this study aimed to assess the QoL of postmenopausal women in the Lalitpur District, Nepal. This study can be helpful for identifying Nepali postmenopausal women’s healthcare requirements for having an ideal QoL.
Material and Methods
This is a community-based analytical study with a cross-sectional design that was conducted on postmenopausal women aged 45-60 years residing in Mahalaxmi municipality, Lalitpur district located in the central part of Nepal in August 2022. Using the Cochran formula [12], the required sample size was obtained as 215 after considering a 10% sample dropout rate. Samples were selected using a systematic random sampling technique. The total population size of women aged 45-60 years was obtained from the records of the ward office. Then, the sampling interval (kth) was calculated by dividing the total population by the sample size. The first sample was randomly selected followed by consecutive sampling at every kth interval until reaching the required sample size. The inclusion criteria were age 45-60 years, a history of menopause for at least one year, willingness to participate in the study, no history of hysterectomy, being on hormone therapy, and no history of diabetes mellitus, thyroid disorders, hypertension, and cardiac disease based on women’s health records.
The instrument used in this study had two parts. The first part included questions related to sociodemographic characteristics, and the second part was the Menopause-specific QoL (MENQOL) questionnaire, which included items measuring the QoL of postmenopausal women. In this study, the Nepali version of this tool was used, which was translated using the forward-backward translation method and with the help of experts. The MENQOL has also been previously used in a study in Nepal [13]. The MENQOL is a valid tool developed by Hilditch and Lewis [14]. It assesses the impact of menopausal symptoms experienced in the past 30 days. It consists of 29 items and four domains of vasomotor symptoms (3 items), psychosocial symptoms (7 items), physical symptoms (16 items) and sexual symptoms (3 items). The scoring for each domain is identical. Each item is scored from 0 (not bothersome) to 6 (extremely bothersome). The total score is obtained by summing up the four domains’ overall scores. The higher total score indicates a lower QoL. Menopausal symptoms’ severity was categorized as mild (score 2-4), moderate (score 5-6), and severe (score 7-8). The QoL level was classified asgood (scores≤ Mean-1 SD), moderate (scores between Mean-1 SD and Mean+1 SD), and poor (scores ≥ Mean+1 SD) based on the mean and standard deviation of the MENQOL total score [15]. In our study, internal consistency of the MENQOL was tested on 22 samples and a Cronbach’s α of 0.87 was obtained.
Data analysis was done in the SPSS software, version 20. Descriptive statistics such as frequency, percentage, mean, median, and standard deviation were used to describe the data. Inferential statistics, including the chi-square test, was used to examine the difference in QoL based on the sociodemographic variables.
Results
A total of 215 postmenopausal women were included in the study (100% response rate). More than one-third of them (41.9%) had age 55-60 years. The mean age of the women was 54.51±3.83 years. The majority of them (87.4%) were married. Almost two-thirds (74%) were living in a joint family. Most of the women (66%) had no formal or informal education and were illiterate. Also, 48.4% of the participants had 1-2 children. More than half of the participants (52%) had their menarche after the age of 15 (Table 1). The occupation of about half of them (45.58%) was agriculture. Also, the majority (54.4%) had their menopause for ≤5 years.

The menopause-related physical symptoms were most prevalent among women (94.9%). More than half of them had experienced physical symptoms such as muscle and joint pain (65.6%), feeling tired or worn out (61.9%), decrease in stamina (60.9%), low back pain (59.5%), decrease in physical strength (59.1%), and lack of energy (58.6%). The menopause-related psychosocial and vasomotor symptoms were prevalent among 53.5% and 41.4% of the participants, respectively. Out of 188 married women, 66% had experienced menopause-related sexual symptoms. Furthermore, among psychosocial symptoms, most of women reported accomplishing less than they used to (34.9%). More than one-third (35.3%) of women had experienced vasomotor symptoms such as hot flashes, sweating (34.4%), and night sweats (30.4%). These results were shown in Table 2.
Regarding physical symptoms, more than half of the women had rated the muscle and joint aches as moderate (53.9%), followed by 33.3% as mild and 12.8% as severe. The mean score of the physical domain of the MENQOL was 2.26±0.77 (Table 3).
The mean score of the sexual domain (2.97±1.94) was higher than the mean scores of the psychosocial (1.69±0.90) and vasomotor (2.44±1.95) domains. The majority (52.5%) of the women had a moderate level of poor memory, followed by 44.3% with a mild level and 3.3% with a severe level. Severe levels of hot flashes and sweating were reported in 14.5% and 9.5% of the participants. Sexual symptoms such as avoiding intimacy, vaginal dryness and decrease in sexual desire were found to be severe in 10.3%, 6.6%, and 5.9% of the participants, respectively (Table 4).
Based on the results, 62.8% of the women had moderate QoL, whereas only 20.2% had good QoL. As shown in Table 5, the level of QoL among postmenopausal women was significantly different based on occupation (P=0.03) and age at menarche (P=0.003).
Discussion
This research aimed to determine the prevalence of menopausal symptoms and the QOL in Nepali postmenopausal women and examine the difference in their QOL according to their sociodemographic characteristics. The results showed that almost all women had experienced at least one menopausal symptom based on the MENQOL domains. A consistent finding was observed in a previous study conducted on women aged 40-60 years in Nepal, which showed that 92% of the women had experienced at least one menopausal symptom [10]. A community-based study on postmenopausal women in Morang district, Nepal also demonstrated that majority of the women had at least one menopausal symptom according to the MENQOL [16]. Our results are also consistent with the results of Ghimire et al. [17].
Most prevalent menopausal symptoms among women in our study were physical symptoms followed by sexual, psychosocial, and vasomotor symptoms. A previous study on postmenopausal women from Nepal also showed that the overall mean score of MENQOL was higher in the physical domain, followed by psychosocial, sexual, and vasomotor domains [13], which the results of this study is consistent with them. Another study in Nepal reported that 100% of the postmenopausal women had physical symptoms [10]. Similarly, a previous study found that vasomotor symptoms were the least prevalent symptoms among postmenopausal women [13]. Conversely, a study conducted in Nepal showed that menopausal symptoms were highly prevalent [17]. The possible reasons for this discrepancy may be due to differences in comorbidities, dietary habits, environmental conditions, economic factors and ethnicity [16, 18].
The top four most common menopause-related physical symptoms in our study were muscle and joint aches, feeling tired and worn out, decrease in stamina, and low backache. This is in line with the results of a study in India [19]. However, it is against the finding of a study conducted in East Delhi, where the most common physical symptom was a decrease in physical strength [20]. The top four most common psychosocial symptoms in women who participated in this study were accomplishing less than before, feeling anxious and nervous, poor memory, and dissatisfaction with personal life. A cross-sectional study on postmenopausal women of 45-60 years from Nepal also reported that accomplishing less than before was the main symptom [21]. However, a study in India reported that poor memory was the most common psychosocial symptom [22]. In a study in Iran, anxiety was found to be the major psychosocial symptom [23]. These discrepancy may be due to differences in the sociodemographic status of women.
In the current study, women’s most common vasomotor symptoms were hot flashes, sweating, and night sweats. Similar to the current study, Prajapati et al. found that hot flashes were the major vasomotor symptom among postmenopausal women in Nepal [21]. Another study reported a similar finding regarding the higher frequency of hot flashes as a vasomotor symptom among postmenopausal women [23]. However, sweating was a common vasomotor symptom among postmenopausal women in Thapa and Thebe’s study in a rural area of Nepal [8]. This discrepancy can be due to differences in the temperature of the study environment and the varied experiences of women.
Regarding the sexual symptoms, the majority of married women in our study had experienced at least one symptom. The most common sexual symptoms were vaginal dryness, decrease in sexual desire, and avoid intimacy. In contrast to our finding, a study on postmenopausal women in rural and urban areas of Sikkim, India, reported that the most common sexual symptom was the avoidance of intimacy [24]. A study in Nepal reported avoiding intimacy as the most common sexual symptom, followed by a decrease in sexual desire and vaginal dryness [8]. The possible reasons for this discrepancy may be the cultural difference and the difference in the subjective nature of participants. Several parts of Nepal, especially the rural areas, still have a culture of silence and do not have the intention to talk freely with others about sexual matters.
The current study reported that the majority of the postmenopausal women had moderate QoL. This is similar to the results of Parsa et al.’s study [25]. A meta-analysis conducted in 2020 reported a similar finding, where the QoL of postmenopausal women in Iran was greater than the moderate level [26]. A study in India also demonstrated a similar result since a low number of postmenopausal women had poor QoL [27]. However, a previous study in Nepal reported a contradictory result, where the majority of the postmenopausal women had poor QoL [28]. The majority of women in postmenopausal women from Malaysia had poor QoL [29]. Moreover, a study in India on middle-aged women (40-60 years) found that most of the women were experiencing poor QoL [30]. These discrepancies may be due to different categorizations of symptoms for a particular domain, different study settings, and the use of different tools to assess QoL.
The current study observed that the overall MENQOL score of postmenopausal women was significantly different in terms of occupation and age at menarche. A systemic review and meta-analysis supported that age at menarche was associated with QoL of women [31]. Conversely, a study found no association between age at menarche and health QoL [32]. Findings of Thapa and Thebe in Nepal showed that occupational status and QoL were significantly related [8]. Meanwhile, Senthilvel et al. found no association between occupational status and QoL of postmenopausal women [33].
The strength of this study is its community-based cross-sectional design used to assess the menopausal symptoms and QoL of postmenopausal women. The findings provide gross information about the QoL of postmenopausal women in Nepal, which can help local authorities address the related problems and pave the way for future studies. However, this study was limited to only one district of Nepal. Therefore, the results cannot be generalized to all postmenopausal women in Nepal. Thus, further studies in other provinces and districts of Nepal are recommended to determine the QoL level of postmenopausal women.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Patan Academy of Health Sciences, Lalitpur, Nepal (Code: PNC2206241646). Written informed consent was obtained from all participants prior to data collection. The participants were informed about their right to leave the study at any time. Confidentiality of participants was maintained throughout the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Data collection, data analysis and interpretation: Prakash Ghimire, Lalita Bhatt and Alisha Khadka; Preparation of draft and review: Prakash Ghimire, Lalita Bhatt, Tina Gurung, Laxmi Gurung and Min Raj Joshi; Conceptualization, study design and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
References
- NHS. Overview Menopause [Internet]. 2022. Available from: [Link]
- Heinemann LA, Potthoff P, Schneider HP. International versions of the Menopause Rating Scale (MRS). Health Qual Life Outcomes. 2003; 1:28. [DOI:10.1186/1477-7525-1-28] [PMID]
- Gobbens RJ, Remmen R. The effects of sociodemographic factors on quality of life among people aged 50 years or older are not unequivocal: Comparing SF-12, WHOQOL-BREF, and WHOQOL-OLD. Clin Interv Aging. 2019; 14:231-9. [DOI:10.2147/CIA.S189560] [PMID]
- Yim G, Ahn Y, Chang Y, Ryu S, Lim JY, Kang D, et al. Prevalence and severity of menopause symptoms and associated factors across menopause status in Korean women. Menopause. 2015; 22(10):1108-16. [DOI:10.1097/GME.0000000000000438] [PMID]
- Panay N, Ang SB, Cheshire R, Goldstein SR, Maki P, Nappi RE, et al. Menopause and MHT in 2024: Addressing the key controversies–an International Menopause Society White Paper. Climacteric. 2024; 27(5):441-57. [DOI:10.1080/13697137.2024.2394950] [PMID]
- Sharma S, Adhikari L, Karmacharya I, Kaphle M. Menopausal symptoms among postmenopausal women of a selected municipality: a cross-sectional survey. JNMA J Nepal Med Assoc. 2021; 59(243):1155-60. [DOI:10.31729/jnma.7052] [PMID]
- Islam MR, Gartoulla P, Bell RJ, Fradkin P, Davis SR. Prevalence of menopausal symptoms in Asian midlife women: A systematic review. Climacteric. 2015; 18(2):157-76. [DOI:10.3109/13697137.2014.937689] [PMID]
- Thapa P, Thebe P. Quality of life of postmenopausal women in rural area, Nepal. Post Reprod Health. 2021; 27(3):151-7. [DOI:10.1177/20533691211014741] [PMID]
- Schneider HPG, Birkhäuser M. Quality of life in climacteric women. Climacteric. 2017; 20(3):187-94. [DOI:10.1080/13697137.2017.1279599] [PMID]
- Thapa A, Shrestha M, Pokharel N, Basnet T. Quality of life of menopausal women Residing Dharan sub-metropolitan city, Nepal. Research Square.2021. [DOI:10.21203/rs.3.rs-568976/v1]
- Ibrahim ZM, Ghoneim HM, Madny EH, Kishk EA, Lotfy M, Bahaa A, et al. The effect of menopausal symptoms on the quality of life among postmenopausal Egyptian women. Climacteric. 2020; 23(1):9-16. [DOI:10.1080/13697137.2019.1656185] [PMID]
- Kasiulevičius V, Šapoka V, Filipavičiūtė R. Sample size calculation in epidemiological studies. Gerontologija. 2006; 7(4):225-31. [Link]
- Koirala D, Thapa N, Shrestha S. Quality of life of postmenopausal women of Kaski district. Nepal J Obstet Gynecol. 2020; 15(1):43-9. [DOI:10.3126/njog.v15i1.29340]
- Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire: Development and psychometric properties. Maturitas. 1996; 24(3):161-75. [DOI:10.1016/S0378-5122(96)82006-8] [PMID]
- Rothman KJ, Lash TL, Haneuse S, VanderWeele TJ. The scope of epidemiology. In: Lash TL, Rothman KJ, VanderWeele TJ, Haneuse S, editors. Modern epidemiology. 4th ed. Alphen aan den Rijn: Wolters Kluwer; 2021. [Link]
- Parajuli SB, KC H, Mishra SK, Luitel A. Quality of life among postmenopausal women: A community-based cross-sectional study. J BP Koirala Inst Health Sci. 2021; 4(2):35-40. [DOI:10.3126/jbpkihs.v4i2.40843]
- Ghimire N, Dhakal P, Norrish D, Dangal G, Sharma D, Dhimal M, et al. Menopausal health status of women of Kapilvastu district of Nepal. J Nepal Health Res Counc. 2015; 13(31):182-7. [PMID]
- Ghazanfarpour M, Kaviani M, Abdolahian S, Bonakchi H, Najmabadi Khadijeh M, Naghavi M, et al. The relationship between women's attitude towards menopause and menopausal symptoms among postmenopausal women. Gynecol Endocrinol. 2015; 31(11):860-5. [DOI:10.3109/09513590.2015.1056138] [PMID]
- Sagdeo MM, Arora D. Menopausal symptoms: A comparative study in rural and urban women. Jk Sci. 2011; 13(1):23-6. [Link]
- Madan U, Chhabra P, Gupta G, Madan J. Menopausal symptoms and quality of life in women above 40 years in an urban resettlement colony of East Delhi. Int J Med Sci Public Health. 2019; 8(7):514-9. [DOI:10.5455/ijmsph.2019.0203012052019]
- Prajapati LM , Shrestha GK , Sanjel S . Quality of life of menopausal women in Majhifeda VDC, Kavrepalanchok, Nepal. Kathmandu Univ Med J. 2018; 16(64):311-6. [PMID]
- Nayak G, Kamath A, Kumar P, Rao A. A study of quality of life among perimenopausal women in selected coastal areas of Karnataka, India. J Midlife Health. 2012; 3(2):71-5. [DOI:10.4103/0976-7800.104456] [PMID]
- Barati M, Akbari-Heidari H, Samadi-Yaghin E, Jenabi E, Jormand H, Kamyari N. The factors associated with the quality of life among postmenopausal women. BMC Womens Health. 2021; 21(1):208. [DOI:10.1186/s12905-021-01361-x] [PMID]
- Devi B, Karki P, Chhetry R, Sharma N, Niroula M, Lepcha PC, et al. Quality of life of post-menopausal women residing in rural and urban areas of Sikkim, India. Int J Reprod Contracept Obstet Gynecol. 2018; 7(12):5125-33. [DOI:10.18203/2320-1770.ijrcog20184979]
- Parsa P, Tabesh RA, Soltani F, Karami M. Effect of group counseling on quality of life among postmenopausal women in Hamadan, Iran. J Menopausal Med. 2017; 23(1):49-55. [DOI:10.6118/jmm.2017.23.1.49] [PMID]
- Sharifi K, Tagharrobi Z, Sooki Z. Quality of life among Iranian Postmenopausal Women: A systematic review and meta-analysis. Galen Med J. 2020; 9:e1649. [DOI:10.31661/gmj.v9i0.1649]
- Krishnamoorthy Y, Sarveswaran G, Jayaseelan V, Sakthivel M, Arivarasan Y, Bharathnag N. Assessment of quality of life based on psychological, somatovegetative, and urogenital health problems among postmenopausal women in Urban Puducherry, South India: A cross-sectional observational study. J Midlife Health. 2018; 9(4):173-9. [DOI:10.4103/jmh.JMH_61_18] [PMID]
- Koirala S, Manandhar N. Quality of life of peri and postmenopausal women attending outpatient department of obstretics and gynecology of a tertiary care hospital. J Nepal Health Res Counc. 2018; 16(1):32-5. [DOI:10.3126/jnhrc.v16i1.19360] [PMID]
- Abdullah B, Moize B, Ismail BA, Zamri M, Mohd Nasir NF. Prevalence of menopausal symptoms, its effect to quality of life among Malaysian women and their treatment seeking behaviour. Med J Malaysia. 2017; 72(2):94-9. [PMID]
- Kalhan M, Singhania K, Choudhary P, Verma S, Kaushal P, Singh T. Prevalence of menopausal symptoms and its effect on quality of life among rural middle aged women (40–60 Years) of Haryana, India. Int J Appl Basic Med Res. 2020; 10(3):183-8. [DOI:10.4103/ijabmr.IJABMR_428_19] [PMID]
- Charalampopoulos D, McLoughlin A, Elks CE, Ong KK. Age at menarche and risks of all-cause and cardiovascular death: A systematic review and meta-analysis. Am J Epidemiol. 2014; 180(1):29-40.[DOI:10.1093/aje/kwu113] [PMID]
- Baral S, Kaphle HP. Health-related quality of life among menopausal women: A cross-sectional study from Pokhara, Nepal. PLoS One. 2023; 18(1):e0280632. [DOI:10.1371/journal.pone.0280632] [PMID]
- Senthilvel S, Vasudevan S, Anju PS, Sukumaran A, Sureshbabu J. Assessment of symptoms and quality of life among postmenopausal women in a tertiary care hospital in Kochi, South India: A hospital-based descriptive study. J Midlife Health. 2018; 9(4):185-90. [DOI:10.4103/jmh.JMH_98_18] [PMID]
Article Type : Research |
Subject:
General
Received: 2023/11/6 | Accepted: 2024/01/27 | Published: 2025/04/1
Received: 2023/11/6 | Accepted: 2024/01/27 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |