Thu, Jan 29, 2026
Volume 33, Issue 4 (9-2023)
JHNM 2023, 33(4): 306-315 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Moustafa Ashour H, Rizk Mohammed N, Aziz N I A, Fathallah N F. Effect of Progressive Muscle Relaxation Technique on Signs and Symptoms of Premenstrual Syndrome Among Female Nursing Students. JHNM 2023; 33 (4) :306-315
URL: http://hnmj.gums.ac.ir/article-1-2229-en.html
URL: http://hnmj.gums.ac.ir/article-1-2229-en.html
Hanan Moustafa Ashour1 

 , Niven Rizk Mohammed2
, Niven Rizk Mohammed2 

 , Nemat Ismail Abdel Aziz3
, Nemat Ismail Abdel Aziz3 

 , Naglaa Fathy Fathallah *4
, Naglaa Fathy Fathallah *4 




 , Niven Rizk Mohammed2
, Niven Rizk Mohammed2 

 , Nemat Ismail Abdel Aziz3
, Nemat Ismail Abdel Aziz3 

 , Naglaa Fathy Fathallah *4
, Naglaa Fathy Fathallah *4 


1- Assistant Lecturer, Department of Obstetrics and Gynecologic Nursing, School of Nursing, Damanhur University, Elbeheria, Egypt.
2- Professor, Department of Obstetrics and Gynecologic Nursing, School of Nursing, Alexandria University, Alexandria, Egypt.
3- Assistant Professor, Department of Obstetrics and Gynecologic Nursing, School of Nursing, Damanhur University, Elbeheria, Egypt .
4- Assistant Professor, Department of Obstetrics and Gynecologic Nursing, School of Nursing, Alexandria University, Alexandria, Egypt. ,naglaa.fathalla@alexu.edu.eg
2- Professor, Department of Obstetrics and Gynecologic Nursing, School of Nursing, Alexandria University, Alexandria, Egypt.
3- Assistant Professor, Department of Obstetrics and Gynecologic Nursing, School of Nursing, Damanhur University, Elbeheria, Egypt .
4- Assistant Professor, Department of Obstetrics and Gynecologic Nursing, School of Nursing, Alexandria University, Alexandria, Egypt. ,
Full-Text [PDF 671 kb]
(843 Downloads)
| Abstract (HTML) (1309 Views)
Full-Text: (1069 Views)
Introduction
Premenstrual syndrome (PMS) is one of the most prevalent health issues among women worldwide. More than 90% of women during reproductive age may experience PMS—with prevalence rates spanning from 35.6% to 96.6% [1, 2, 3]. The syndrome is particularly prevalent among female university students and negatively affects their quality of life and academic performance. Reports on the prevalence of PMS among female university students exhibit regional variations; for example, it ranges from 39.4% to 56.9% in Iran and 65% in Egypt [4]. The exact etiology of PMS is unknown; it could possess a complex and multifactorial origin. PMS has been linked to over 200 physical, psychological, and behavioral symptoms. The main symptoms include breast tenderness, abdominal discomfort, mood swings, anxiety, and social isolation [5, 6, 7].
PMS has been seen as an obstacle for female teenagers and young adults as they strive to attain developmental goals. The syndrome may impede work productivity, decrease health-related quality of life, and interfere with interpersonal relationships and daily living activities [4]. Furthermore, it can result in a loss of self-esteem, foster social isolation, prevent academic achievement, and increase accident risk [8]. PMS control is best achieved through a combination of both pharmacological and non-pharmacological therapies. Non-pharmacologic methods empower individuals to control their emotions, decrease the feeling of weakness, improve the activity level, and enhance functional capacity. They also contribute to reducing the needed dosage of analgesic drugs, thus decreasing the side effects of treatment [9]. Cognitive and behavioral therapies, exercises, massage therapy, relaxation techniques, and dietary and nutritional modifications have been proven beneficial for treating premenstrual symptoms [10].
Jacobson’s progressive muscle relaxation technique (JPMRT) represents a valuable relaxing method commonly used in nursing practice. This technique facilitates deep relaxation through a systemic sequential tensing of specific muscle groups (face, hand, shoulder, abdomen, and legs) for 5-7 seconds, followed by relaxing the same muscle group for 10-12 seconds. As a result, the approach serves as a mediator in the stress-response process, moderating emotional and physiological reactions to the stressor events. In addition, the hypothalamic response in Jacobson’s approach reduces sympathetic arousal and muscular tone. Furthermore, this mechanism aids in the reduction of pain, distress, and anxiety, helps to divert attention away from a painful body part, and establishes a sense of control over pain [11, 12].
Sudhadevi et al. reported the positive outcomes of progressive muscle relaxation on PMS [13]. Similarly, Gayathri reported that muscle relaxation therapy would effectively reduce the severity of premenstrual symptoms [14]. Premenstrual syndrome is a growing concern for healthcare providers. The syndrome’s physical, psychological, and behavioral manifestations may impair interpersonal relationships, academic performance, and health-related quality of life, as well as reduced job productivity and a greater demand for specialist healthcare. As a result, it has a high health burden and social-economic cost. PMS management is a problem that can no longer be ignored. However, administering analgesics is not always effective in reducing the severity of PMS; rather, utilization of non-pharmacological interventions like PMS assists in symptom relief and increases individual feelings of pain control. So, there is a need for sparking research to explore these interventions’ impact on PMS. Such knowledge paves the road for nurses to use safe, effective, easy-to-apply, and costless methods to control PMS.
Materials and Methods
This research is a quasi-experimental study employing a pre-test post-test design with two groups. The investigation was conducted at the Faculty of Nursing, Damanhur University in Egypt, at the Obstetrics and Gynecologic Nursing Skills Lab.
A convenience sampling was employed to recruit 80 female nursing students who fulfilled the following inclusion criteria: Suffering from mild or moderate degree of PMS according to the premenstrual syndrome scale (PMSS) and having a history of regular menstrual cycle ranging from 21 to 35 days, lasting from 3-7 days.
To choose the eligible subjects, the researchers interviewed all female nursing students enrolled in the third and fourth academic years during the second semester of 2020-2021. The selected cases were 97 students. Epi info program version 10 was used to estimate the sample size using the following parameters: Population size of 97, a confidence interval of 95%, an expected frequency of 50%, and an acceptable error of 5%. The minimum sample size required was determined as 77.
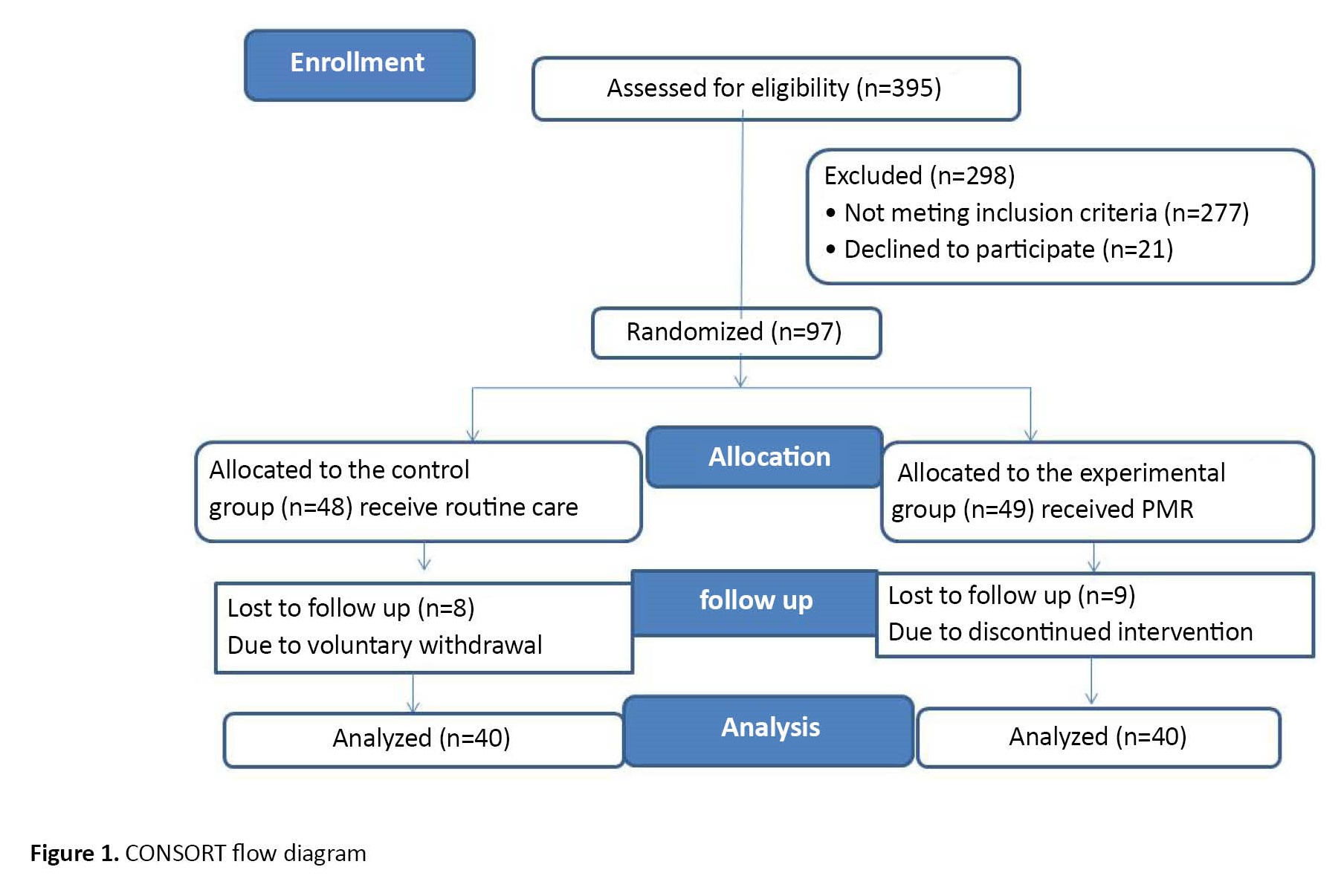
During the study period (from March until the end of July 2021), 80 out of 97 students who agreed to participate in the study were assigned to two Equal groups using a random number generator program: The study group (40 students) and the control group (40 students). Also, 17 students were removed because they did not practice PMS for 4 weeks (Figure 1).
Premenstrual syndrome (PMS) is one of the most prevalent health issues among women worldwide. More than 90% of women during reproductive age may experience PMS—with prevalence rates spanning from 35.6% to 96.6% [1, 2, 3]. The syndrome is particularly prevalent among female university students and negatively affects their quality of life and academic performance. Reports on the prevalence of PMS among female university students exhibit regional variations; for example, it ranges from 39.4% to 56.9% in Iran and 65% in Egypt [4]. The exact etiology of PMS is unknown; it could possess a complex and multifactorial origin. PMS has been linked to over 200 physical, psychological, and behavioral symptoms. The main symptoms include breast tenderness, abdominal discomfort, mood swings, anxiety, and social isolation [5, 6, 7].
PMS has been seen as an obstacle for female teenagers and young adults as they strive to attain developmental goals. The syndrome may impede work productivity, decrease health-related quality of life, and interfere with interpersonal relationships and daily living activities [4]. Furthermore, it can result in a loss of self-esteem, foster social isolation, prevent academic achievement, and increase accident risk [8]. PMS control is best achieved through a combination of both pharmacological and non-pharmacological therapies. Non-pharmacologic methods empower individuals to control their emotions, decrease the feeling of weakness, improve the activity level, and enhance functional capacity. They also contribute to reducing the needed dosage of analgesic drugs, thus decreasing the side effects of treatment [9]. Cognitive and behavioral therapies, exercises, massage therapy, relaxation techniques, and dietary and nutritional modifications have been proven beneficial for treating premenstrual symptoms [10].
Jacobson’s progressive muscle relaxation technique (JPMRT) represents a valuable relaxing method commonly used in nursing practice. This technique facilitates deep relaxation through a systemic sequential tensing of specific muscle groups (face, hand, shoulder, abdomen, and legs) for 5-7 seconds, followed by relaxing the same muscle group for 10-12 seconds. As a result, the approach serves as a mediator in the stress-response process, moderating emotional and physiological reactions to the stressor events. In addition, the hypothalamic response in Jacobson’s approach reduces sympathetic arousal and muscular tone. Furthermore, this mechanism aids in the reduction of pain, distress, and anxiety, helps to divert attention away from a painful body part, and establishes a sense of control over pain [11, 12].
Sudhadevi et al. reported the positive outcomes of progressive muscle relaxation on PMS [13]. Similarly, Gayathri reported that muscle relaxation therapy would effectively reduce the severity of premenstrual symptoms [14]. Premenstrual syndrome is a growing concern for healthcare providers. The syndrome’s physical, psychological, and behavioral manifestations may impair interpersonal relationships, academic performance, and health-related quality of life, as well as reduced job productivity and a greater demand for specialist healthcare. As a result, it has a high health burden and social-economic cost. PMS management is a problem that can no longer be ignored. However, administering analgesics is not always effective in reducing the severity of PMS; rather, utilization of non-pharmacological interventions like PMS assists in symptom relief and increases individual feelings of pain control. So, there is a need for sparking research to explore these interventions’ impact on PMS. Such knowledge paves the road for nurses to use safe, effective, easy-to-apply, and costless methods to control PMS.
Materials and Methods
This research is a quasi-experimental study employing a pre-test post-test design with two groups. The investigation was conducted at the Faculty of Nursing, Damanhur University in Egypt, at the Obstetrics and Gynecologic Nursing Skills Lab.
A convenience sampling was employed to recruit 80 female nursing students who fulfilled the following inclusion criteria: Suffering from mild or moderate degree of PMS according to the premenstrual syndrome scale (PMSS) and having a history of regular menstrual cycle ranging from 21 to 35 days, lasting from 3-7 days.
To choose the eligible subjects, the researchers interviewed all female nursing students enrolled in the third and fourth academic years during the second semester of 2020-2021. The selected cases were 97 students. Epi info program version 10 was used to estimate the sample size using the following parameters: Population size of 97, a confidence interval of 95%, an expected frequency of 50%, and an acceptable error of 5%. The minimum sample size required was determined as 77.
During the study period (from March until the end of July 2021), 80 out of 97 students who agreed to participate in the study were assigned to two Equal groups using a random number generator program: The study group (40 students) and the control group (40 students). Also, 17 students were removed because they did not practice PMS for 4 weeks (Figure 1).
The premenstrual syndrome scale (PMSS) was used in this study. PMSS comprised 40 items with three subscales: Physiological symptoms (16 items), psychological symptoms (12 items), and behavioral symptoms (12 items) as per the original instrument. The students’ responses were rated on a 5-point Likert scale ranging from never=1 to always=5. the total scores ranged from 40 to 200, with higher scores indicating increased PMS severity. The students’ PMS severity was categorized as follows: No symptoms (1-40), mild symptoms (41-80), moderate symptoms (81-120), severe symptoms (121-160), and very severe symptoms (161-200) [15]. We used the main questionnaire (designed in the English language) in this study.
We also used a sociodemographic data form including age, academic year, current residence, and menstrual history (age of menarche, interval, rhythm, duration, and amount of menstrual flow).
Top of form
Initially, the researchers interviewed students of both groups in the nursing skill lab on a weekday before menstruation, established rapport, and collected the sociodemographic data and menstrual history. Moreover, the baseline PMS symptoms severity was assessed.
The researchers explained to the study group how to perform progressive muscle relaxation using videos and pictures and demonstrated each step. The procedure included the following steps.
The student was asked to evacuate her bladder, lose tight clothes, and assume a comfortable position. The researcher instructed the student to inhale deeply through her nose, feel her abdomen rise, and slowly exhale out of her mouth. Then, she repeats 3-5 cycles of deep breathing.
Then, they were asked to tense the muscles of the face, wrinkle the forehead, frown on the nose, close their eyes very tightly, and purse their lips for 5-7 seconds. Then, they were asked to release the hold gradually while counting for 10 seconds. They were also instructed to tense the muscles of the hands, forearms, and biceps muscles. They were asked to clench their fists and hands and move on to the biceps by drawing the forearm up towards the shoulder, slowly bend the elbow using a strong 5-second contraction, then slowly releasing while counting to 10. After that, the researcher instructed the student to tense the shoulders and neck muscles. Hold them for 5 seconds and then slowly release them.
Also, the student was asked to suck and hold the abdomen for 5-7 seconds, then slowly release while counting for 10 seconds. Also, the subject was asked to tense the buttocks by pulling them together, hold for 5-7 seconds, and then slowly release while counting to 10. Finally, the researcher instructed the student to tense the muscles of the legs, lift the leg off the ground, straighten knees, and point toes toward the head. Hold them for 5 seconds and slowly release them while counting for 10 seconds.
After completing the explanation, each female student was asked to re-demonstrate it until the researchers ensured that the student could perform the technique on her own. At the end of the session, students were informed to practice progressive muscle relaxation for 30 minutes per day for 4 weeks. The researchers instructed every student about the importance of compliance with the intervention.
The control group included female students who received routine care such as warm drinks, warm baths, and low salt and fat intake. After 4 weeks, they were interviewed to reassess the severity of PMS symptoms. The intervention group received the intervention plus routine care.
The researchers contacted the students daily to ascertain their cooperation. Participants were also instructed to attend the nursing skills lab after 4 weeks for follow-up when the intensity of PMS symptoms was reassessed.
The SPSS software, version 20 was utilized for data analysis. Descriptive statistics, including frequency, percentages, the Mean±SD, were employed to describe demographic characteristics, menstrual history, and the intensity of PMS. Inferential statistics were used to compare the study groups, including the chi-square test, t-test, Monte Carlo test, and Mann-Whitney test, and Marginal Homogeneity test. All of the statistical analyses were considered significant at P<0.05.
Results
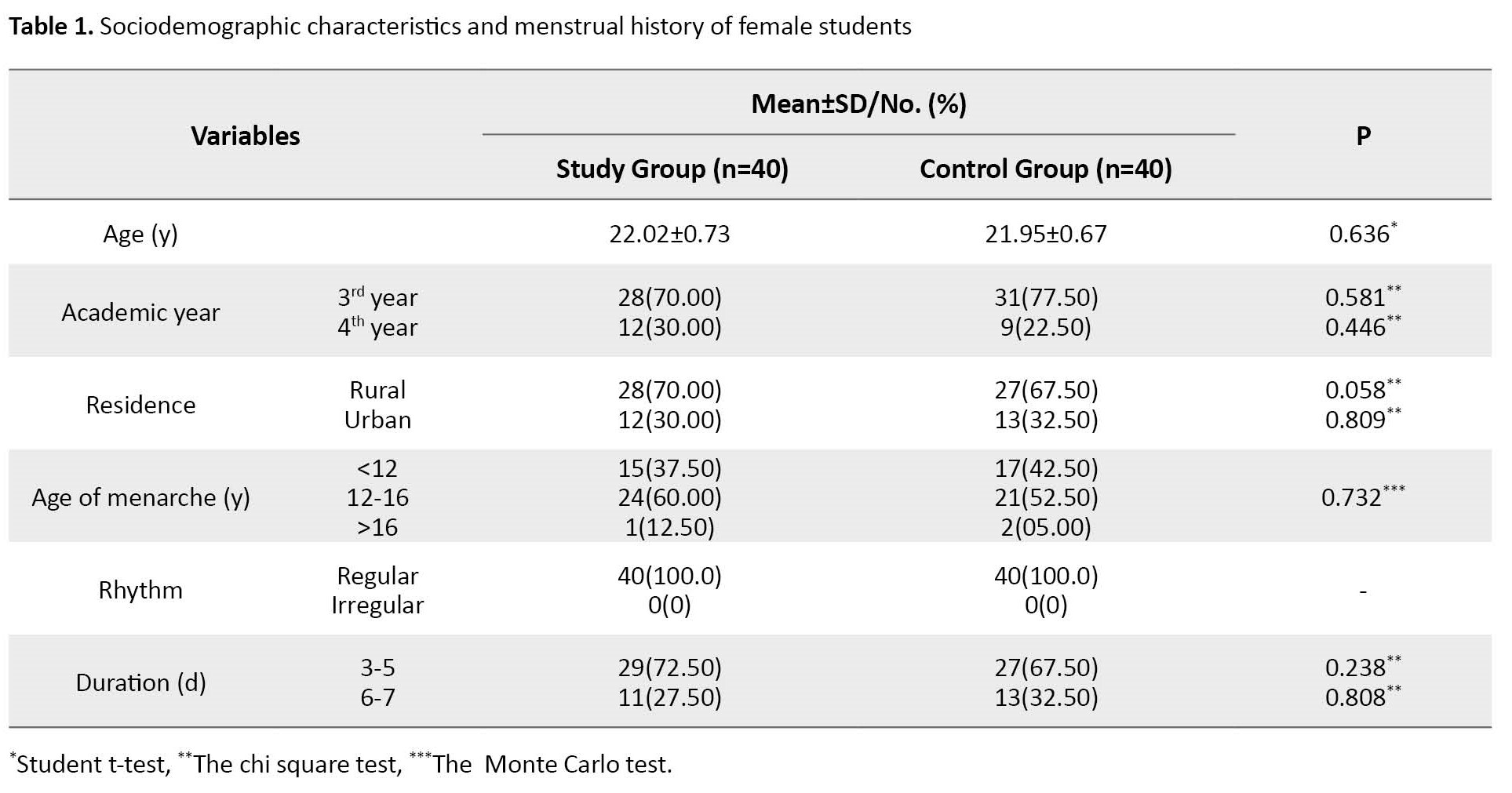
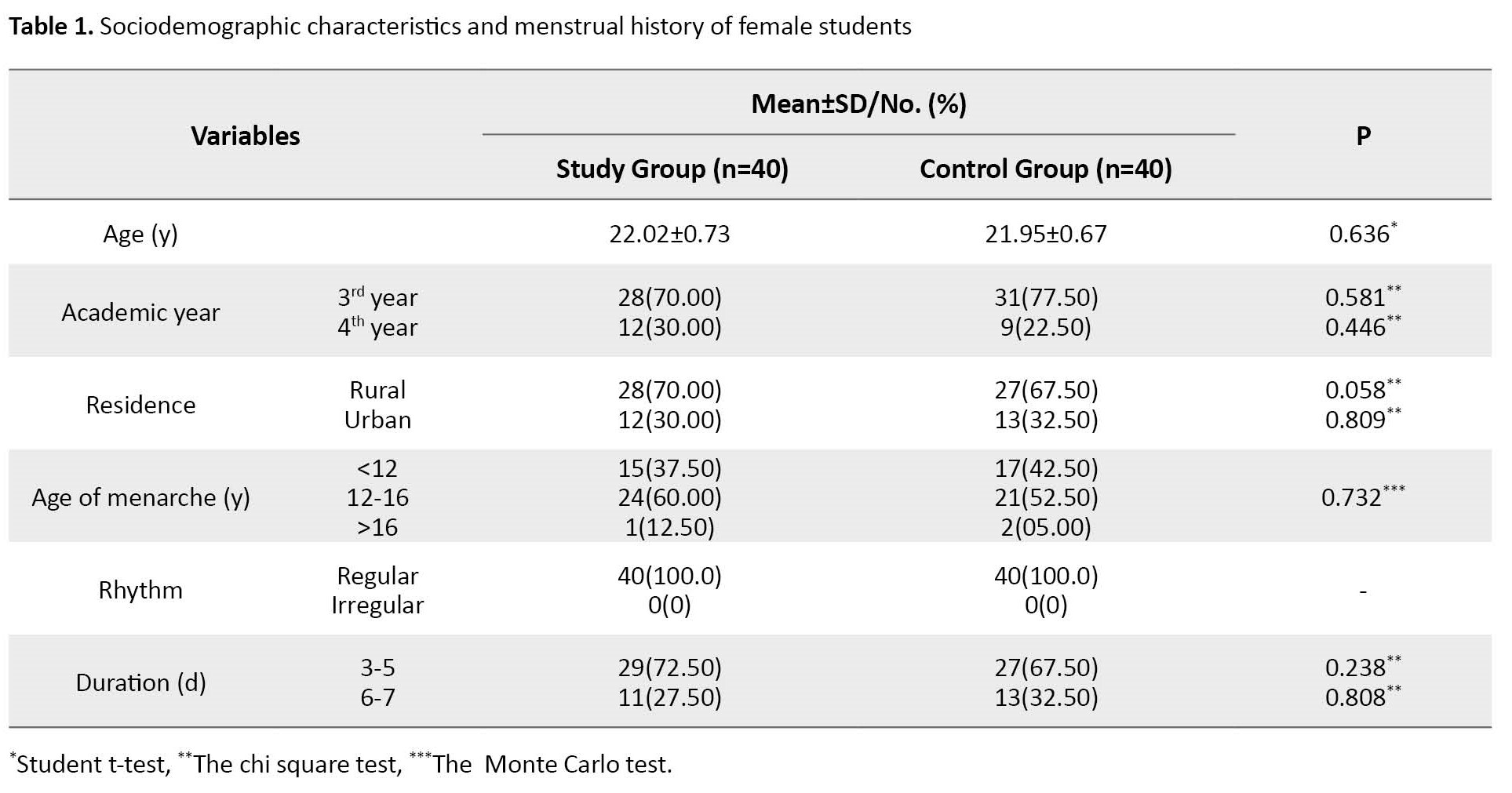
The Mean±SD age among the study and control groups was 22.02±0.73 and 21.95±0.67 years, respectively. Moreover, 70% of the study and 77% of the control groups were in their third academic year. More than 70% and 67.5% of the study and control groups were from rural areas, respectively. Also, 60% of the study group and 52.5% of the control group had their menarche at 12 to 16 years old. All students in both groups had a regular menstrual cycle, with intervals ranging from 21 to 35 days. Moreover, the duration of menstruation spanned 3-5 days among 72.5% of students in the study group and 67.5% of students in the control group (Table 1).
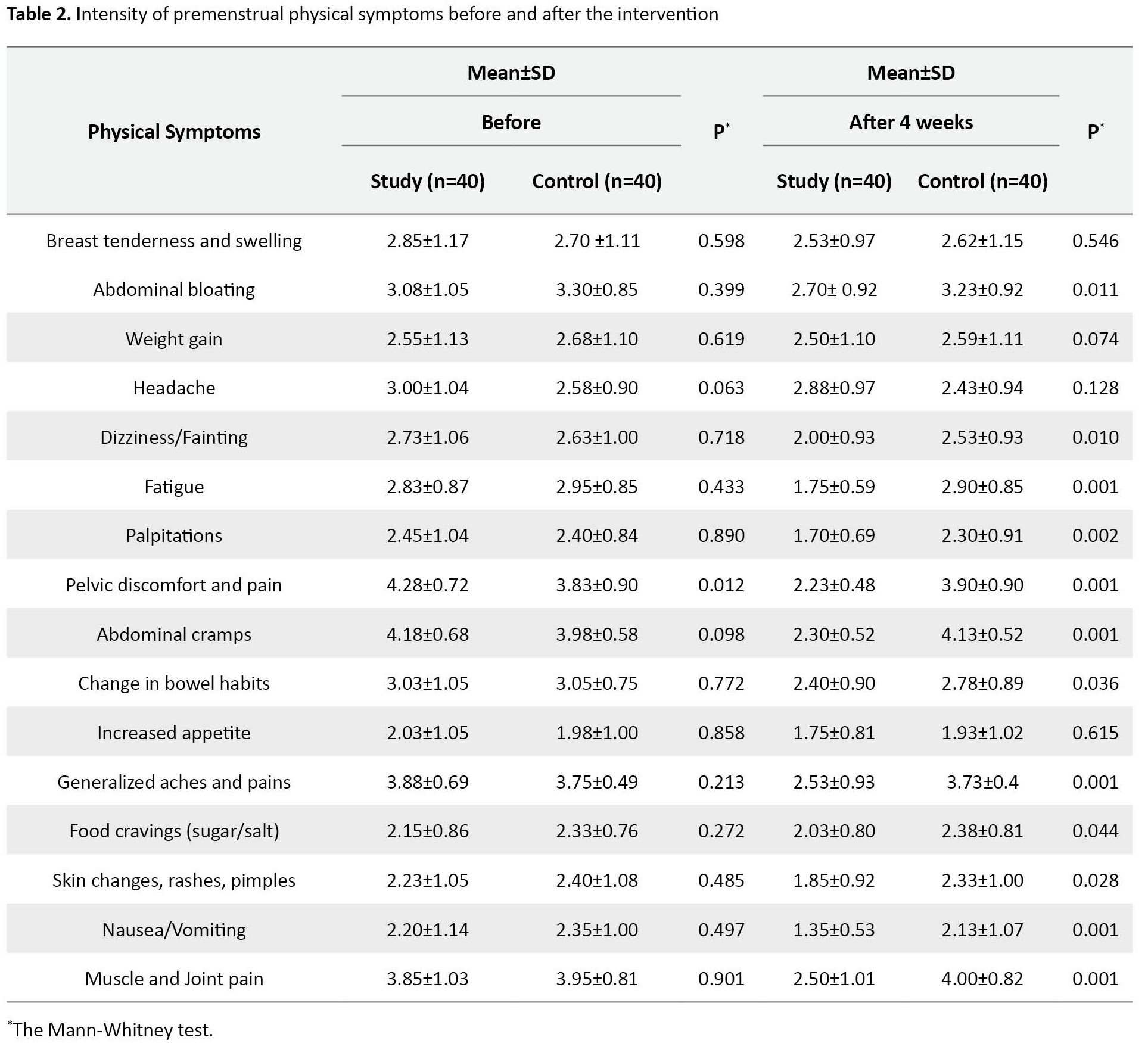
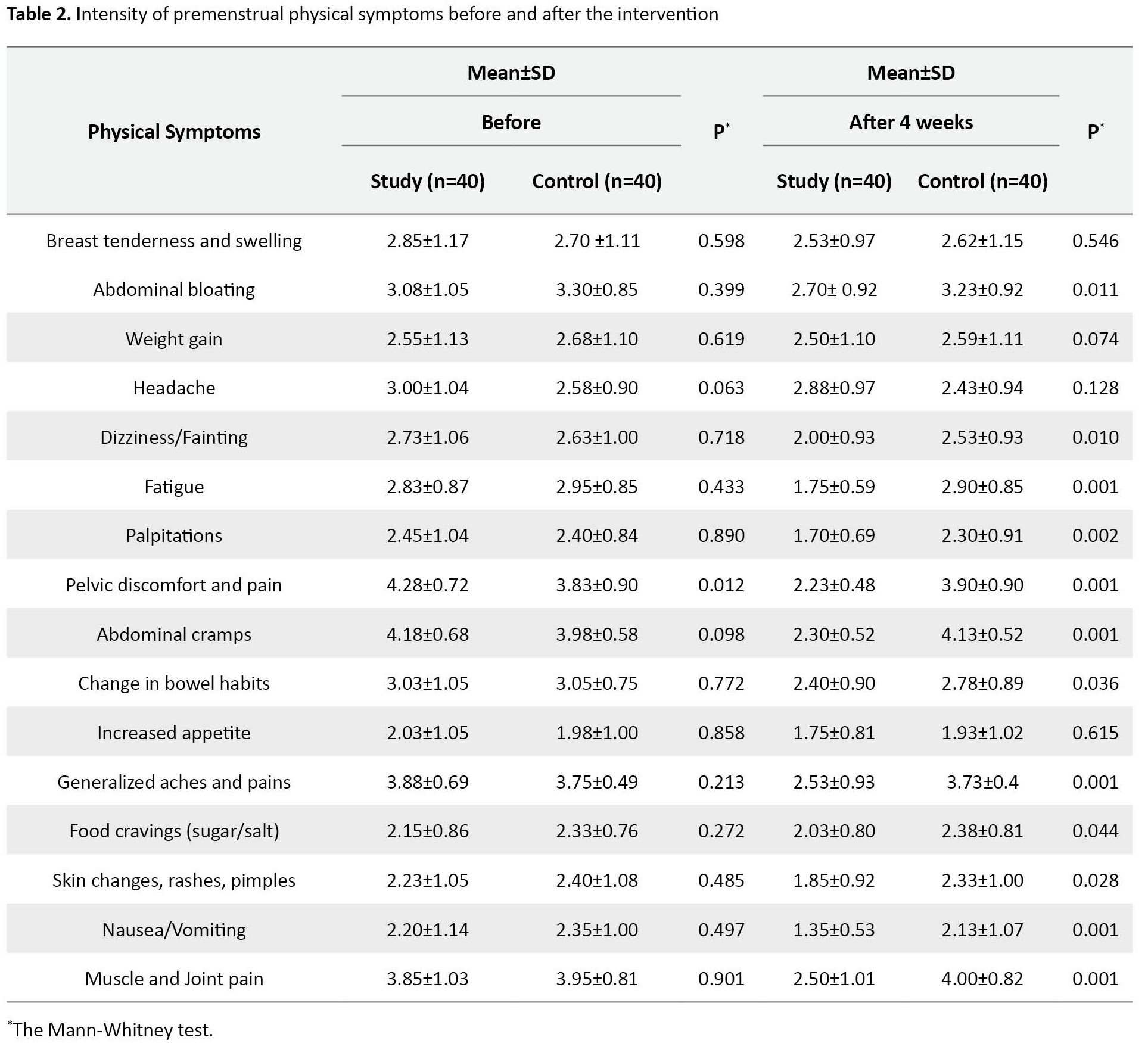
Before Intervention, no statistically significant differences were observed between the study and control groups in the mean intensity scores of all PMS physical symptoms except pelvic discomfort and pain (P=0.012). While after the intervention, there was a statistically significant decrease in the mean score of the intensity of all PMS physical symptoms between the study and control groups in favor of the study group, except for breast tenderness and swelling, weight gain, headache, and increased appetite (Table 2).
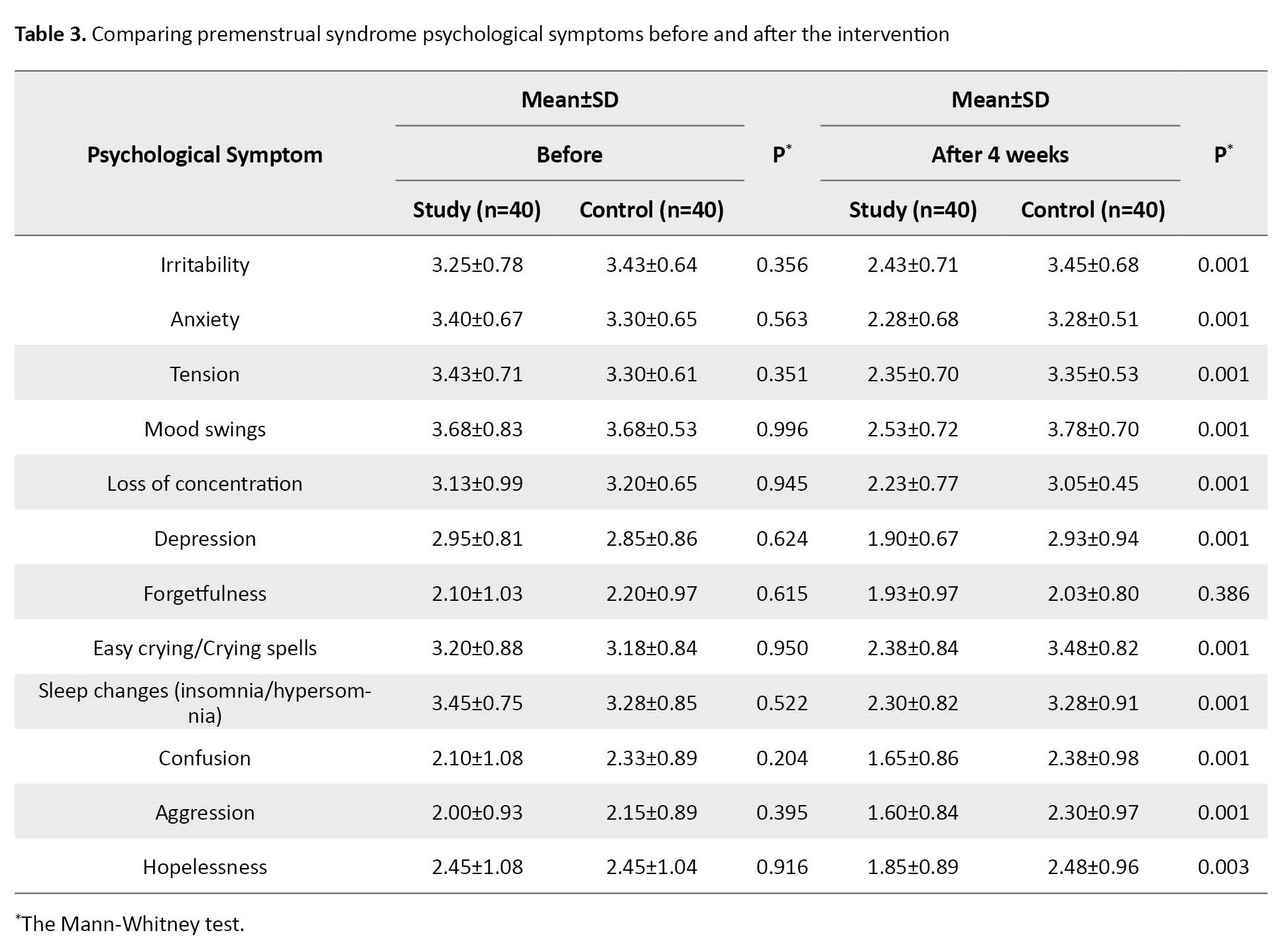
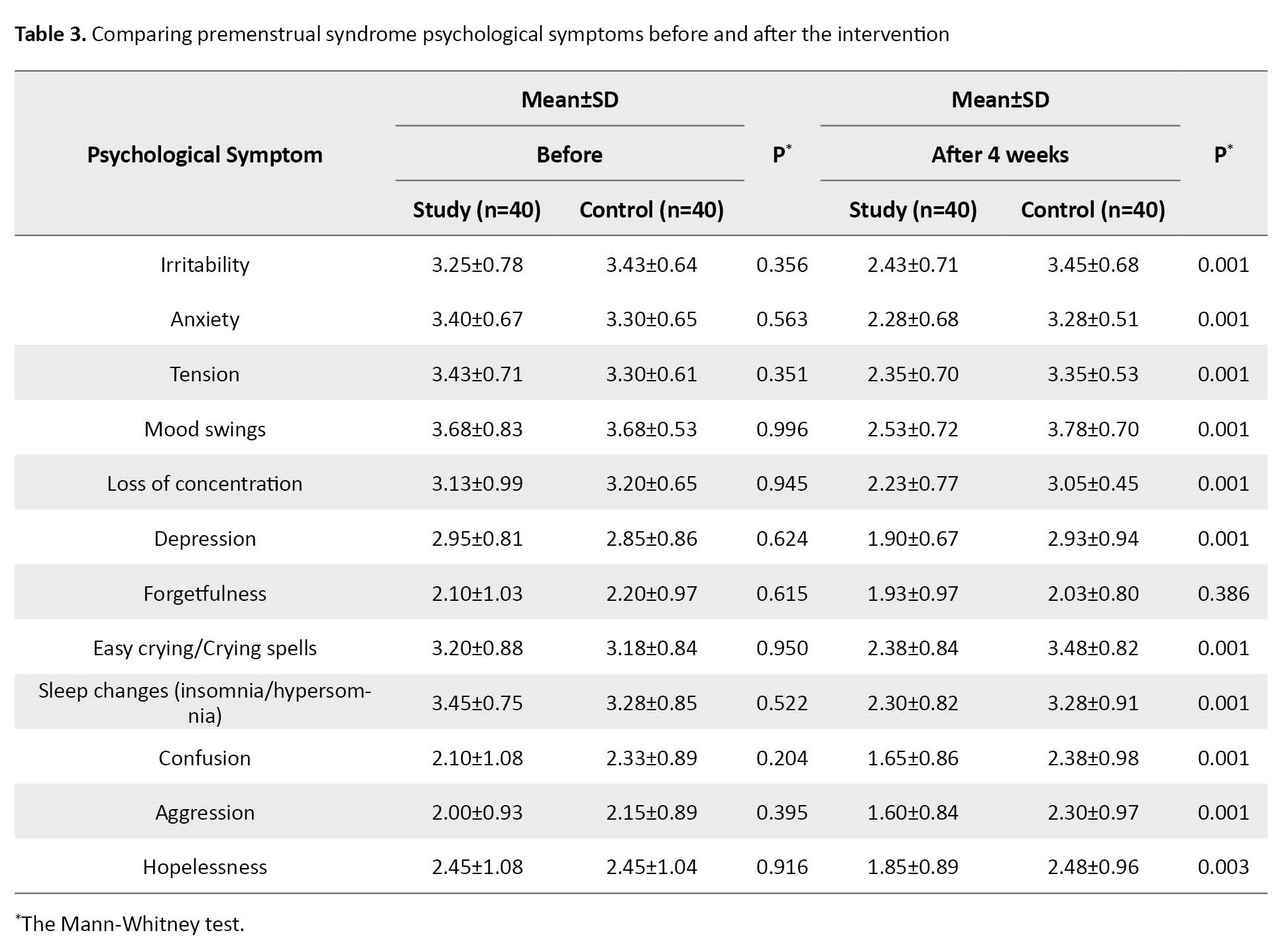
Furthermore, a significant decrease in mean scores of the intensity of all premenstrual psychological symptoms was noted among the study and control groups in favor of the study group after 4 weeks of interventions, except for forgetfulness (Table 3).
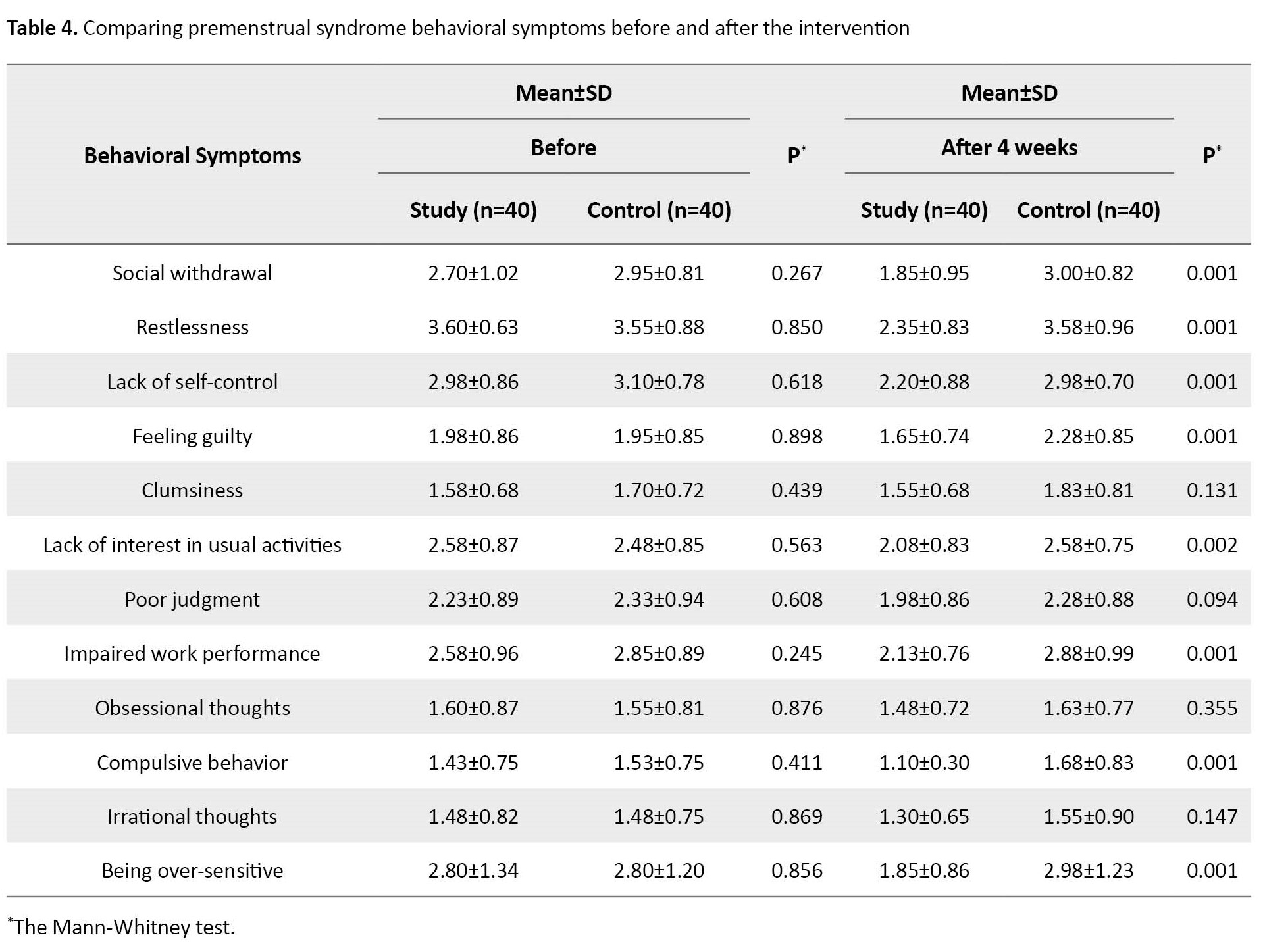
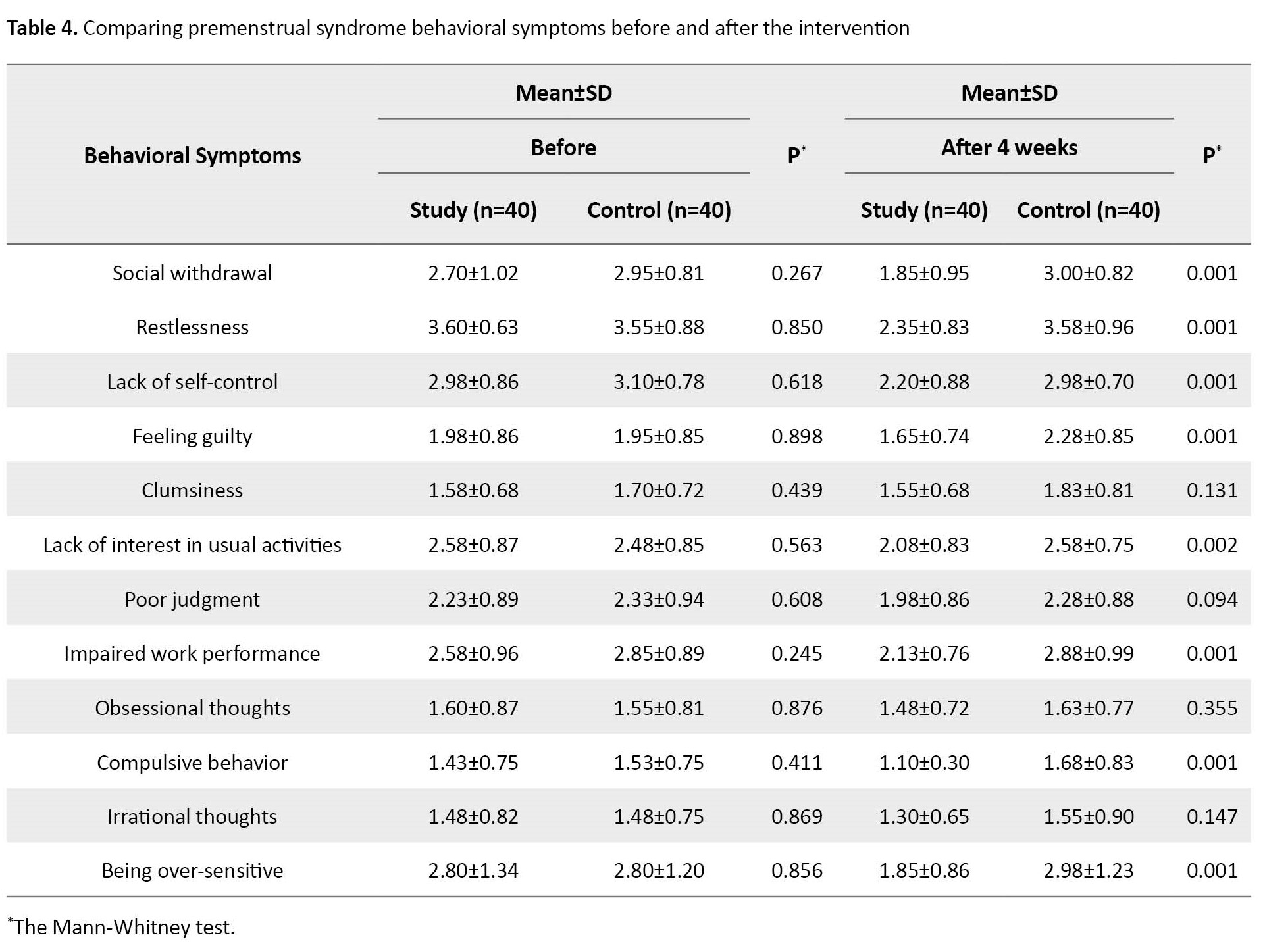
There was no statistically significant difference between the study and control groups in mean intensity scores of all premenstrual behavioral symptoms. On the other hand, after the intervention, there was a statistically significant decrease in mean scores of the intensity of all premenstrual behavioral symptoms between the study and control groups in favor of the study group, except for clumsiness, poor judgment, obsessive and irrational thoughts (Table 4).
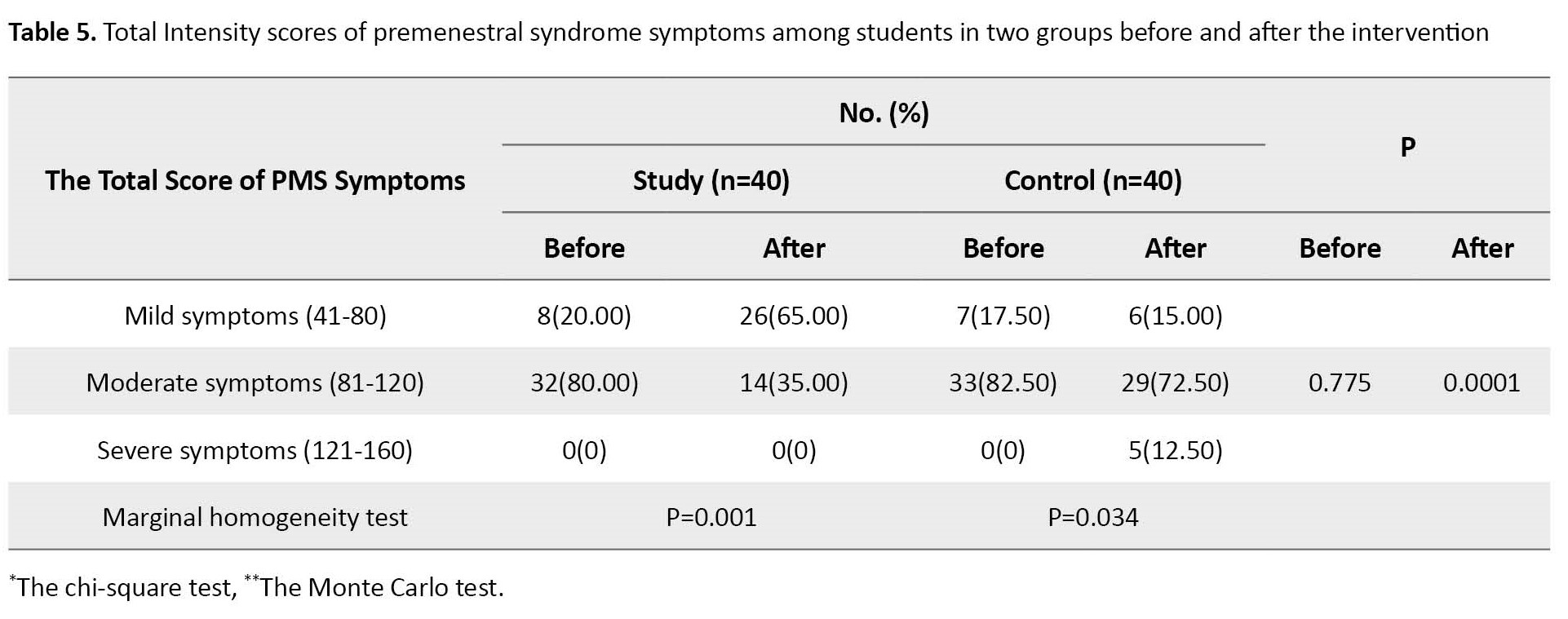
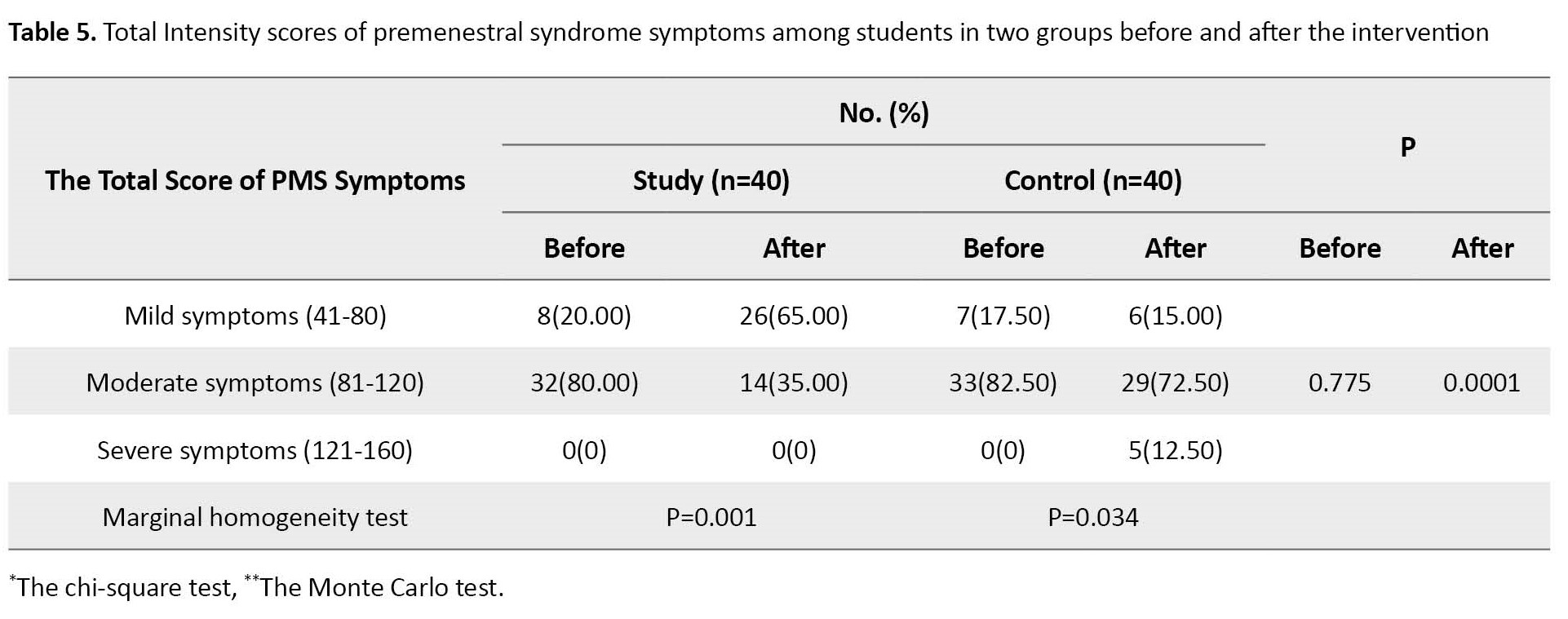
It was found that the intensity of PMS symptoms before intervention was moderate among the majority (80% and 82.5%) of the study and control groups, respectively, with no statistically significant difference between the two groups (P=0.775). Meanwhile, after the intervention, about one-third (35%) of the study group still suffered moderate-intensity PMS compared to about three-quarters (72.5%) of the control group. Consequently, the difference between the two groups was statistically significant (P=0.0001). In addition, the intensity of PMS symptoms among the study group was significantly decreased after the intervention (P=0.001). In contrast, the intensity of PMS symptoms among the control group was significantly increased after the intervention (P=0.034). Finally, the intensity of PMS symptoms became severe among 12.5% of the control group after intervention compared to none before intervention (Table 5).
Discussion
Upon investigating the effect of JPMRT on PMS, the current study revealed that the intensity of PMS physical symptoms significantly decreased after practicing JPMRT in the study group. Meanwhile, no difference was found between the control group after applying routine care. This result suggests a possible positive influence of JPMRT on decreasing the intensity of PMS physical symptoms. Dizziness and fatigue emerged as common PMS physical symptoms in the current study. Both symptoms were significantly reduced in the study group after practicing JPMRT. These results may be attributed to the circulatory enhancement of PMRT, which is instrumental in improving such symptoms. In the study of Ferreira and Kulkarn, the relaxation technique was more effective in reducing the severity of fatigue and headaches in premenstrual syndrome in individuals compared to meditation with visualization [16].
The results of the present study also showed that after practicing PMRT, marked improvement was observed among the study group concerning pelvic discomfort and pain, abdominal cramps, generalized aches and pain, and muscle and joint pain. This result may be attributed to progressive relaxation enhancing pain relief by decreasing muscle tension, lowering anxiety levels, and distracting attention. Moreover, it improves pain relief by aligning with the gate control theory of pain. The theory postulates that changes in pain impulses transmitted from the peripheral nerve receptors to the brain can result in little or no pain perception [17]. The current study’s findings were relatively similar to the results of Naik et al. They reported a highly significant reduction in post-test pain scores for those supplemented with Jacobson’s relaxation technique on dysmenorrhea [18].
The present study observed that PMRT significantly decreased abdominal bloating, bizarre bowel habits, and nausea and vomiting symptoms among the study group after the intervention. According to the relevant literature, prostaglandins may provide a pathophysiological link to understanding the overlap between menstrual pain and gastrointestinal symptoms. Premenstrual uterine prostaglandin production may mediate an inflammatory response characterized by pain. So, during menses, abnormally high levels of prostaglandins in a menstrual fluid may induce abnormal uterine contractions and pain. In the gut, prostaglandins can cause smooth muscle contractions, reduced absorption, and induced secretion of electrolytes in the small bowel, all of which may lead to gastrointestinal pain and diarrhea [19]. Bernstein et al. reported that the occurrence of gastrointestinal symptoms in conjunction with the premenstrual and menses phases is common [20].
Furthermore, skin changes, rashes, and pimples significantly improved among the study group after practicing PMRT. This result agrees with the fact that PMRT decreases salivary cortisol and improves immune system functions, which justifies the improvement of these symptoms [21].
Regarding the effect of PMRT on PMS psychological symptoms, the result of the current study revealed a statistically significant decrease in the intensity of almost all PMS psychological symptoms among the study group after the intervention. In other words, progressive muscle relaxation positively affected PMS psychological symptoms. In this respect, Nasution et al. reported that this emotional response and the soothing effect generated by this relaxation transform the sympathetic dominant physiology into the dominant parasympathetic system. In these circumstances, the secretion of stress hormones such as cortisol and catecholamine (epinephrine and norepinephrine) decreased [22]. The present result is similar to the findings of other studies [23, 24].
The present study noted a statistically significant decrease in the intensity of most PMS behavioral symptoms among the study group after the intervention. This finding may be attributed to those premenstrual behavioral symptoms directly related to premenstrual psychological symptoms. In addition, this means that PMS behavioral symptoms may be triggered by the luteal phase psychological disturbance that results from serotonin deficiency. Consequently, improvement of psychological symptoms may significantly lead to behavioral symptoms improvement.
Regarding the total score of the intensity of PMS symptoms, the intensity of PMS symptoms in the study group was significantly decreased after the intervention. In contrast, the intensity of PMS symptoms in the control group significantly increased after routine care.
This result is incongruent with Sudhadevi et al. They concluded that PMRT exercises effectively reduced premenstrual syndrome symptoms among students [13].
Based on the results of the current study, the progressive muscle relaxation technique appears to have a remarkable effect on reducing the severity of PMS. Therefore, useful, beneficial impacts of non-pharmacological modalities such as PMRT on PMS should be included in curricula of university students in different educational settings, and training programs for nurses in maternity units about the utilization of non-pharmacological interventions such as PMRT in managing PMS are recommended.
This study was limited to students of Nursing School, at Damanhur University in Egypt and does not represent the whole female university student population in Egypt. Since the topic is sensitive to Egyptian culture, some respondents were reluctant to discuss their real personal problems.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the School of Nursing, Alexandria University, for the period 2020- 2021. The researchers also secured permission to conduct the study from the responsible authorities of the study setting. Before implementing the interventions, the researchers approached eligible students and gave them a detailed description of the intervention, its benefits, and any possible risks. Researchers also ascertained that participation in the study is entirely voluntary, and the subjects could refuse to participate or withdraw from the study at any time. Confidentiality of the obtained data, students’ anonymity, and privacy were assured. The study was conducted following the principles of the Declaration of Helsinki, seventh revision.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Study design and manuscript writing the original draft : Naglaa Fathy Fathalla, Niven Rizk Mohmed and Hanan Moustafa Ashour; Data collection: Nemat Ismail Abdel Aziz; Data analysis: Naglaa Fathy Fathalla and Hanan Moustfa Ashour; Final Approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers offer sincere appreciation and thanks to the entire study participants for their cooperation in the successful completion of this study.
References
We also used a sociodemographic data form including age, academic year, current residence, and menstrual history (age of menarche, interval, rhythm, duration, and amount of menstrual flow).
Top of form
Initially, the researchers interviewed students of both groups in the nursing skill lab on a weekday before menstruation, established rapport, and collected the sociodemographic data and menstrual history. Moreover, the baseline PMS symptoms severity was assessed.
The researchers explained to the study group how to perform progressive muscle relaxation using videos and pictures and demonstrated each step. The procedure included the following steps.
The student was asked to evacuate her bladder, lose tight clothes, and assume a comfortable position. The researcher instructed the student to inhale deeply through her nose, feel her abdomen rise, and slowly exhale out of her mouth. Then, she repeats 3-5 cycles of deep breathing.
Then, they were asked to tense the muscles of the face, wrinkle the forehead, frown on the nose, close their eyes very tightly, and purse their lips for 5-7 seconds. Then, they were asked to release the hold gradually while counting for 10 seconds. They were also instructed to tense the muscles of the hands, forearms, and biceps muscles. They were asked to clench their fists and hands and move on to the biceps by drawing the forearm up towards the shoulder, slowly bend the elbow using a strong 5-second contraction, then slowly releasing while counting to 10. After that, the researcher instructed the student to tense the shoulders and neck muscles. Hold them for 5 seconds and then slowly release them.
Also, the student was asked to suck and hold the abdomen for 5-7 seconds, then slowly release while counting for 10 seconds. Also, the subject was asked to tense the buttocks by pulling them together, hold for 5-7 seconds, and then slowly release while counting to 10. Finally, the researcher instructed the student to tense the muscles of the legs, lift the leg off the ground, straighten knees, and point toes toward the head. Hold them for 5 seconds and slowly release them while counting for 10 seconds.
After completing the explanation, each female student was asked to re-demonstrate it until the researchers ensured that the student could perform the technique on her own. At the end of the session, students were informed to practice progressive muscle relaxation for 30 minutes per day for 4 weeks. The researchers instructed every student about the importance of compliance with the intervention.
The control group included female students who received routine care such as warm drinks, warm baths, and low salt and fat intake. After 4 weeks, they were interviewed to reassess the severity of PMS symptoms. The intervention group received the intervention plus routine care.
The researchers contacted the students daily to ascertain their cooperation. Participants were also instructed to attend the nursing skills lab after 4 weeks for follow-up when the intensity of PMS symptoms was reassessed.
The SPSS software, version 20 was utilized for data analysis. Descriptive statistics, including frequency, percentages, the Mean±SD, were employed to describe demographic characteristics, menstrual history, and the intensity of PMS. Inferential statistics were used to compare the study groups, including the chi-square test, t-test, Monte Carlo test, and Mann-Whitney test, and Marginal Homogeneity test. All of the statistical analyses were considered significant at P<0.05.
Results
The Mean±SD age among the study and control groups was 22.02±0.73 and 21.95±0.67 years, respectively. Moreover, 70% of the study and 77% of the control groups were in their third academic year. More than 70% and 67.5% of the study and control groups were from rural areas, respectively. Also, 60% of the study group and 52.5% of the control group had their menarche at 12 to 16 years old. All students in both groups had a regular menstrual cycle, with intervals ranging from 21 to 35 days. Moreover, the duration of menstruation spanned 3-5 days among 72.5% of students in the study group and 67.5% of students in the control group (Table 1).
Before Intervention, no statistically significant differences were observed between the study and control groups in the mean intensity scores of all PMS physical symptoms except pelvic discomfort and pain (P=0.012). While after the intervention, there was a statistically significant decrease in the mean score of the intensity of all PMS physical symptoms between the study and control groups in favor of the study group, except for breast tenderness and swelling, weight gain, headache, and increased appetite (Table 2).
Furthermore, a significant decrease in mean scores of the intensity of all premenstrual psychological symptoms was noted among the study and control groups in favor of the study group after 4 weeks of interventions, except for forgetfulness (Table 3).
There was no statistically significant difference between the study and control groups in mean intensity scores of all premenstrual behavioral symptoms. On the other hand, after the intervention, there was a statistically significant decrease in mean scores of the intensity of all premenstrual behavioral symptoms between the study and control groups in favor of the study group, except for clumsiness, poor judgment, obsessive and irrational thoughts (Table 4).
It was found that the intensity of PMS symptoms before intervention was moderate among the majority (80% and 82.5%) of the study and control groups, respectively, with no statistically significant difference between the two groups (P=0.775). Meanwhile, after the intervention, about one-third (35%) of the study group still suffered moderate-intensity PMS compared to about three-quarters (72.5%) of the control group. Consequently, the difference between the two groups was statistically significant (P=0.0001). In addition, the intensity of PMS symptoms among the study group was significantly decreased after the intervention (P=0.001). In contrast, the intensity of PMS symptoms among the control group was significantly increased after the intervention (P=0.034). Finally, the intensity of PMS symptoms became severe among 12.5% of the control group after intervention compared to none before intervention (Table 5).
Discussion
Upon investigating the effect of JPMRT on PMS, the current study revealed that the intensity of PMS physical symptoms significantly decreased after practicing JPMRT in the study group. Meanwhile, no difference was found between the control group after applying routine care. This result suggests a possible positive influence of JPMRT on decreasing the intensity of PMS physical symptoms. Dizziness and fatigue emerged as common PMS physical symptoms in the current study. Both symptoms were significantly reduced in the study group after practicing JPMRT. These results may be attributed to the circulatory enhancement of PMRT, which is instrumental in improving such symptoms. In the study of Ferreira and Kulkarn, the relaxation technique was more effective in reducing the severity of fatigue and headaches in premenstrual syndrome in individuals compared to meditation with visualization [16].
The results of the present study also showed that after practicing PMRT, marked improvement was observed among the study group concerning pelvic discomfort and pain, abdominal cramps, generalized aches and pain, and muscle and joint pain. This result may be attributed to progressive relaxation enhancing pain relief by decreasing muscle tension, lowering anxiety levels, and distracting attention. Moreover, it improves pain relief by aligning with the gate control theory of pain. The theory postulates that changes in pain impulses transmitted from the peripheral nerve receptors to the brain can result in little or no pain perception [17]. The current study’s findings were relatively similar to the results of Naik et al. They reported a highly significant reduction in post-test pain scores for those supplemented with Jacobson’s relaxation technique on dysmenorrhea [18].
The present study observed that PMRT significantly decreased abdominal bloating, bizarre bowel habits, and nausea and vomiting symptoms among the study group after the intervention. According to the relevant literature, prostaglandins may provide a pathophysiological link to understanding the overlap between menstrual pain and gastrointestinal symptoms. Premenstrual uterine prostaglandin production may mediate an inflammatory response characterized by pain. So, during menses, abnormally high levels of prostaglandins in a menstrual fluid may induce abnormal uterine contractions and pain. In the gut, prostaglandins can cause smooth muscle contractions, reduced absorption, and induced secretion of electrolytes in the small bowel, all of which may lead to gastrointestinal pain and diarrhea [19]. Bernstein et al. reported that the occurrence of gastrointestinal symptoms in conjunction with the premenstrual and menses phases is common [20].
Furthermore, skin changes, rashes, and pimples significantly improved among the study group after practicing PMRT. This result agrees with the fact that PMRT decreases salivary cortisol and improves immune system functions, which justifies the improvement of these symptoms [21].
Regarding the effect of PMRT on PMS psychological symptoms, the result of the current study revealed a statistically significant decrease in the intensity of almost all PMS psychological symptoms among the study group after the intervention. In other words, progressive muscle relaxation positively affected PMS psychological symptoms. In this respect, Nasution et al. reported that this emotional response and the soothing effect generated by this relaxation transform the sympathetic dominant physiology into the dominant parasympathetic system. In these circumstances, the secretion of stress hormones such as cortisol and catecholamine (epinephrine and norepinephrine) decreased [22]. The present result is similar to the findings of other studies [23, 24].
The present study noted a statistically significant decrease in the intensity of most PMS behavioral symptoms among the study group after the intervention. This finding may be attributed to those premenstrual behavioral symptoms directly related to premenstrual psychological symptoms. In addition, this means that PMS behavioral symptoms may be triggered by the luteal phase psychological disturbance that results from serotonin deficiency. Consequently, improvement of psychological symptoms may significantly lead to behavioral symptoms improvement.
Regarding the total score of the intensity of PMS symptoms, the intensity of PMS symptoms in the study group was significantly decreased after the intervention. In contrast, the intensity of PMS symptoms in the control group significantly increased after routine care.
This result is incongruent with Sudhadevi et al. They concluded that PMRT exercises effectively reduced premenstrual syndrome symptoms among students [13].
Based on the results of the current study, the progressive muscle relaxation technique appears to have a remarkable effect on reducing the severity of PMS. Therefore, useful, beneficial impacts of non-pharmacological modalities such as PMRT on PMS should be included in curricula of university students in different educational settings, and training programs for nurses in maternity units about the utilization of non-pharmacological interventions such as PMRT in managing PMS are recommended.
This study was limited to students of Nursing School, at Damanhur University in Egypt and does not represent the whole female university student population in Egypt. Since the topic is sensitive to Egyptian culture, some respondents were reluctant to discuss their real personal problems.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the School of Nursing, Alexandria University, for the period 2020- 2021. The researchers also secured permission to conduct the study from the responsible authorities of the study setting. Before implementing the interventions, the researchers approached eligible students and gave them a detailed description of the intervention, its benefits, and any possible risks. Researchers also ascertained that participation in the study is entirely voluntary, and the subjects could refuse to participate or withdraw from the study at any time. Confidentiality of the obtained data, students’ anonymity, and privacy were assured. The study was conducted following the principles of the Declaration of Helsinki, seventh revision.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Study design and manuscript writing the original draft : Naglaa Fathy Fathalla, Niven Rizk Mohmed and Hanan Moustafa Ashour; Data collection: Nemat Ismail Abdel Aziz; Data analysis: Naglaa Fathy Fathalla and Hanan Moustfa Ashour; Final Approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers offer sincere appreciation and thanks to the entire study participants for their cooperation in the successful completion of this study.
References
- Fatemi M, Allahdadian M, Bahadorani M. Comparison of serum level of some trace elements and vitamin D between patients with premenstrual syndrome and normal controls: A cross-sectional study. Int J Reprod Biomed. 2019; 17(9):647-52. [DOI:10.18502/ijrm.v17i9.5100] [PMID]
- Pizzorno JE, Murray MT. Textbook of natural medicin. Amsterdam: Elsevier Health Sciences; 2020. [Link]
- Abeje A, Berhanu Z. Premenstrual syndrome and factors associated with it among secondary and preparatory school students in Debremarkos town, North-west Ethiopia, 2016. BMC Res Notes. 2019; 12(1):535. [DOI:10.1186/s13104-019-4549-9] [PMID]
- Hashim MS, Obaideen AA, Jahrami HA, Radwan H, Hamad HJ, Owais AA, et al. Premenstrual syndrome is associated with dietary and lifestyle behaviors among university students: A cross-sectional study from Sharjah, UAE. Nutrients. 2019; 11(8):1939. [DOI:10.3390/nu11081939] [PMID]
- Azima S, Bakhshayesh HR, Mousavi S, Ashrafizaveh A. Comparison of the effects of reflexology and massage therapy on primary dysmenorrheal. Biomed Res. 2015; 26(3):471-6. [Link]
- Dilbaz B, Aksan A. Premenstrual syndrome, a common but underrated entity: Review of the clinical literature. J Turk Ger Gynecol Assoc. 2021; 22(2):139-48. [DOI:10.4274/jtgga.galenos.2021.2020.0133] [PMID]
- Salem IMW, Alsamti MY, Murad MA. Predictors of premenstrual syndrome among female students at governmental secondary schools in Jeddah, Saudi Arabia: A cross-sectional study. Egypt J Hosp Med. 2020; 78(2):337-47. [DOI:10.21608/ejhm.2020.76614]
- Abay H, Kaplan S. Evaluation of the effectiveness of a training program for coping with PMS symptoms based on IMB model in university students. Women Health. 2021; 61(6):550-61. [DOI:10.1080/03630242.2021.1927286] [PMID]
- Metawie MAH, Amasha HAR, Abdraboo RA, Ali SE. Effectiveness of aromatherapy with lavender oil in relieving post cesarean incision pain. J Surg. 2015; 3(2-1):8-13. [DOI:10.11648/j.js.s.2015030201.12]
- Abdolrahmi F, Kaboudi M, Kamerzarin H, Kaboudi B, Mohammadi P, Horriat M. The effect of Fordyce happiness training on marital satisfaction and mental health in women with premenstrual syndrome. J Holistic Nurs Midwifery. 2023; 33(1):15-24. [DOI:10.32598/jhnm.33.1.2273]
- Read JR, Perz J, Ussher JM. Ways of coping with premenstrual change: Development and validation of a premenstrual coping measure. BMC Womens Health. 2014; 14:1. [DOI:10.1186/1472-6874-14-1] [PMID]
- Maddineshat M, Keyvanloo S, Lashkardoost H, Arki M, Tabatabaeichehr M. Effectiveness of group cognitive-behavioral therapy on symptoms of premenstrual syndrome (PMS) . Iran J Psychiatry. 2016; 11(1):30-6. [PMID]
- Sudhadevi M, Prabavathi S, Aruna E. Effectiveness of jacobson’s progressive muscle relaxation exercises on premenstrual syndrome among students at selected school, erode, tamilnadu. Asian Pac J Nurs. 2018; 5(01):1-3. [Link]
- Gayathri M. A study to assess the effectiveness of Jacobson muscle relaxation therapy on premenstrual syndrome among adolescent girls in CSI girls Higher Secondary school at Madurai [PhD dissertation]. Madurai: CSI Jeyaraj Annapackiam College of Nursing; 2018. [Link]
- Padmavathi P, Sankar R, Kokilavani N, Dhanapal K, Ashok B. Validity and reliability study of Premenstrual Syndrome Scale (PMSS). Int J Adv Nurs Manag. 2014; 2(1):4-10. [Link]
- Ferreira RL, Kulkarni N. Effect of relaxation techniques on fatigue and headaches in premenstrual syndrome. Int J Yoga Physiother Phy Educ. 2019; 4(3):37-43. [Link]
- Roykulcharoen V, Good M. Systematic relaxation to relieve postoperative pain. J Adv Nurs. 2004; 48(2):140-8. [DOI:10.1111/j.1365-2648.2004.03181.x] [PMID]
- Naik MN, Warulkar MY, Salvi MR. A study to assess the effect of Jacobson’s relaxation technique on dysmenorrhea among adolescent girls in selected schools. Eur. J Mol Clin Med. 2021; 7(11):7445-60. [Link]
- Çelik AS, Apay SE. Effect of progressive relaxation exercises on primary dysmenorrhea in Turkish students: A randomized prospective controlled trial. Complement Ther Clin Pract. 2021; 42:101280. [DOI:10.1016/j.ctcp.2020.101280] [PMID]
- Bernstein MT, Graff LA, Avery L, Palatnick C, Parnerowski K, Targownik LE. Gastrointestinal symptoms before and during menses in healthy women. BMC Women’s Health. 2014; 14:14. [DOI:10.1186/1472-6874-14-14] [PMID]
- Varvogli L, Darviri C. Stress management techniques: Evidence-based procedures that reduce stress and promote health. Health Sci J. 2011; 5(2):74-89. [Link]
- Nasution S, Ariga R. Effects of progressive muscle relaxation technique on decrease pain intensity in woman during the latent phase delivery. Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches. 2018; 1:449-53. [DOI:10.5220/0010072704490453]
- Ismail NIA, Elgzar WTI. The effect of progressive muscle relaxation on post cesarean section pain, quality of sleep and physical activities limitation. Int J Stud Nurs. 2018; 3(3):14-29. [DOI:10.20849/ijsn.v3i3.461]
- Jasuja VV, Makwana J, Thomas E. Effect of PMR on somatic and psychological symptoms of premenstrual syndrome. Depression. 2014; 5:16.7. [Link]
Article Type : Research |
Subject:
General
Received: 2023/09/18 | Accepted: 2023/09/3 | Published: 2023/09/3
Received: 2023/09/18 | Accepted: 2023/09/3 | Published: 2023/09/3
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |