Wed, Jul 3, 2024
Volume 33, Issue 4 (9-2023)
JHNM 2023, 33(4): 316-324 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fouly H, M. Davidson P. Clinical Learning Environment of the "Nursing of Childbearing Family" Course from the Students' Perspectives: An Observational Prospective Study. JHNM 2023; 33 (4) :316-324
URL: http://hnmj.gums.ac.ir/article-1-2228-en.html
URL: http://hnmj.gums.ac.ir/article-1-2228-en.html
1- Assistant professor of Obstetric, Gynecology & Midwifery Nursing, Health Sciences - Nursing, Higher Colleges of Technology, RAKWC, UAE. , hfouly@hct.ac.ae
2- Professor, Cardiovascular and Chronic Care, Dean of the Johns Hopkins School of Nursing, Vice-Chancellor and President University of Wollongong, Northfields Ave, Wollongong, United States of America.
2- Professor, Cardiovascular and Chronic Care, Dean of the Johns Hopkins School of Nursing, Vice-Chancellor and President University of Wollongong, Northfields Ave, Wollongong, United States of America.
Full-Text [PDF 466 kb]
(145 Downloads)
| Abstract (HTML) (294 Views)
Full-Text: (118 Views)
Introduction
The clinical learning environment includes students, educators, clinical staff, patients, various experiences, perspectives, and aspects of interactions. These myriad components must interact as students are expected to be socialized in the professional community, a journey affected by individual characteristics such as personality and preferences. Consequently, students’ viewpoints are crucial for the qualified and safe patient care and security of the trainee learning and familiarizing with the career to achieve an effective clinical learning environment [1, 2].
Clinical simulation training is a teaching method to help students acquire nursing knowledge and competencies. This objective is achieved through debriefing after reproducing clinical scenarios using a simulator. Hence, nursing educators should familiarize themselves with the required instruments to integrate simulation skills into their core curriculum. Although nursing research confirmed the widespread adoption of simulation-based education within nursing and midwifery education, the scope of the practice, setup, and evidence for simulation-based training and education is still under investigation [3].
The simulation positively influences the students, educators, and, consequently, the broader community due to replicating a clinical environment similar to natural settings. It enables nursing practice in a safe, simulated environment, elevating the quality of care and imbuing ethical perspectives with actual patients during their training stage. Also, it ensures the protection and respect of human rights via following professionalism in the learning process [4].
During simulations, students are divided into small groups to practice and gain training in nursing and midwifery. The active pedagogical strategy helps students translate their acquired knowledge into technical skills and practice rules through critical thinking. In addition to enhancing their competence, professional level, and quality of care, simulations reduce errors or harm to patients [5, 6, 7, 8].
During simulation, managing critical obstetric conditions will develop professional skills in a real-life environment that provides students with the required qualifications [9]. Despite the mentioned benefits of simulation education, it still needs a periodic evaluation from students’ perspectives to pick up any shortages and make it up-to-date with the advanced technology [10].
The significance of the study lies in its contribution to improving childbearing nursing education. National leaders have underscored the need for more efficient and practical instruction, emphasizing the importance of learning environment outcomes to address these educational needs through innovative approaches and adaptability to changing circumstances [11, 12, 13]. Simulation acts as a bridge between academic and clinical performance. Therefore, students’ perspectives regarding simulation and clinical experience can help educators rectify future concerns. This study aimed to evaluate the clinical learning environment in the context of the “nursing the childbearing family” course at an advanced level of education in a developed country through these questions.
From students ‘perspectives, is there a relationship between the university and the clinical site?
Are students’ perspectives different before and after receiving clinical training?
Materials and Methods
This study employed an observational prospective design and was conducted at simulation labs at the School of Nursing, Johns Hopkins University, Baltimore, Maryland, USA.
A convenient sample included all students who agreed to participate in the study. All students from this course were invited, of whom 62(84.93%) participated. They were enrolled in the childbearing family course at the School of Nursing at Johns Hopkins University in Spring 2017. The students were between 23 and 35 years old, lived in Baltimore, Maryland, and agreed to participate in the investigation.
A structured questionnaire assessed students’ perspectives on the clinical learning environment. The questionnaire comprised 54 questions (50 multiple-choice and 4 open-ended questions). The questions were designed to explore four aspects: The first is about students’ clinical sites. It contained 17 questions; 16 were graded on a 5-point Likert scale (5=almost always, 4=often, 3=sometimes, 2=seldom, and 1=never), and one question was open-ended, exploring students’ suggestions for clinical sites. The second aspect was about the students’ perspectives of their clinical instructor. It contained 14 questions, 13 of which are graded with a Likert scale, and the last one is an open-ended question for students’ suggestions. The third aspect asks about the effective working relationships between the university and the clinical site. It contained 9 questions; 8 were graded on a Likert scale, and the last was an open-ended question for students’ suggestions. The fourth aspect included 14 questions about students’ perspectives of the simulation labs (before and after the clinical training); 4 of them were multiple-choice questions about before the training and 10 questions after receiving the lab training, 9 of them were graded as 1=strongly disagree, 2=disagree, 3=agree, and 4=strongly agree. The tenth and the last one is an open-ended question.
The study questionnaire was adopted from the audit of the clinical environment: Student questionnaire version 2010 [14] School of Nursing and Midwifery, University College Cork. Our version was modified to be marked on the Likert scale and multiple-choice questions instead of “yes” or “no” ones in the questionnaire. Three maternity, childbearing, and nursing education experts reviewed the questionnaire, and all their comments reflected that the questionnaire was transparent and relevant to what it is supposed to measure. Also, its reliability was tested, and the Cronbach α was found to be 0.932, which is of high reliability based on standardized items.
The study evaluated the clinical learning environment of the course (NR.120.520 nursing the childbearing family), one of the undergraduate courses offered at Johns Hopkins University. In this course, students build and develop assessment, care planning, communication, and leadership skills in the context of caring for childbearing families. During the preparation phase, the researcher focused on the simulation labs’ facilities for clinical training, assisting students with clinical materials, guided practice, and immediate feedback to students. He supervised the actual performance of the skill in the clinical laboratory, clinical learning environment, utilization of clinical learning opportunities, and techniques of using scenarios in simulation labs in compliance with the International Nursing Association for Clinical Simulation and Learning (INACSL) principles. The methods of filling in student progress reports per placement area, supervisor consultation with students, and communication skills were used during simulation lab training and recording students’ responses in dealing with conflicting situations.
In the simulation session, the researcher attended a postpartum hemorrhage simulation lasting 20 minutes. The scene showed students sitting in a debriefing room to receive instructions about the simulation lab. Before that, they had received the simulation scenario on their blackboard to be prepared. The students were divided into two groups. One group was to be role players in the simulation scenario, and the other group was observed during their role-playing through a big screen that permitted the last group to observe without distracting their colleagues as they were unseen. The procedure started with a conversation between the students in the “nurse role” and the clinical instructor in the “patient role.” In contrast, the student spoke in a highly simulated form. Then, the “simulated nurse” asked the “simulated patient” about her health and pain history and took blood pressure, which was 120/80 mm Hg. During the assessment of the uterus, the simulated nurse felt it was boggy and asked the patient if he would make a uterine massage to check her bleeding status; he also asked about the time of changing her perineal pad. Then, he asked her if she needed any breastfeeding concerns and if she fed her newborn.
For data gathering, the researcher uploaded the questionnaire with the consent form on the Qualtrics survey, available on the School of Nursing at Johns Hopkins University blackboard for students’ responses. Simultaneously, the researcher sent a message to each student, including the questionnaire link, to notify them about the study. Later, the researcher followed up the students’ responses daily until they finished within 9 months.
The SPSS software, version 22 was used for statistical analysis based on the proposed objectives and variables. Descriptive statistics were used to sort out the obtained information, as frequency, percentage, Mean±SD. Inferential statistics such as the Pearson test were used to determine the correlation between the students’ perspectives regarding the clinical site and clinical instructors, and the paired t-test to compare the mean scores of the students’ performances before and after receiving the simulation training labs. P<0.05 were considered statistically significant. There was no missing data as the online questionnaire design required the responder to answer the question in order to move to the next question.
Results
The study participants were 62 BSc nursing students with a 100% response rate. They were enrolled in childbearing and family nursing course in the academic year. The participants’ Mean±SD age was 20.75±0.97 years, and all live in Baltimore, near the Johns Hopkins University School of Nursing campus. Two-thirds of the participants were female (61.3%), and the remaining (38.7%) were male. A majority (88.7%) of the participants were US citizens.
Table 1 presents the distribution of students’ perspectives regarding the first aspect of the clinical site according to the childbearing family course.
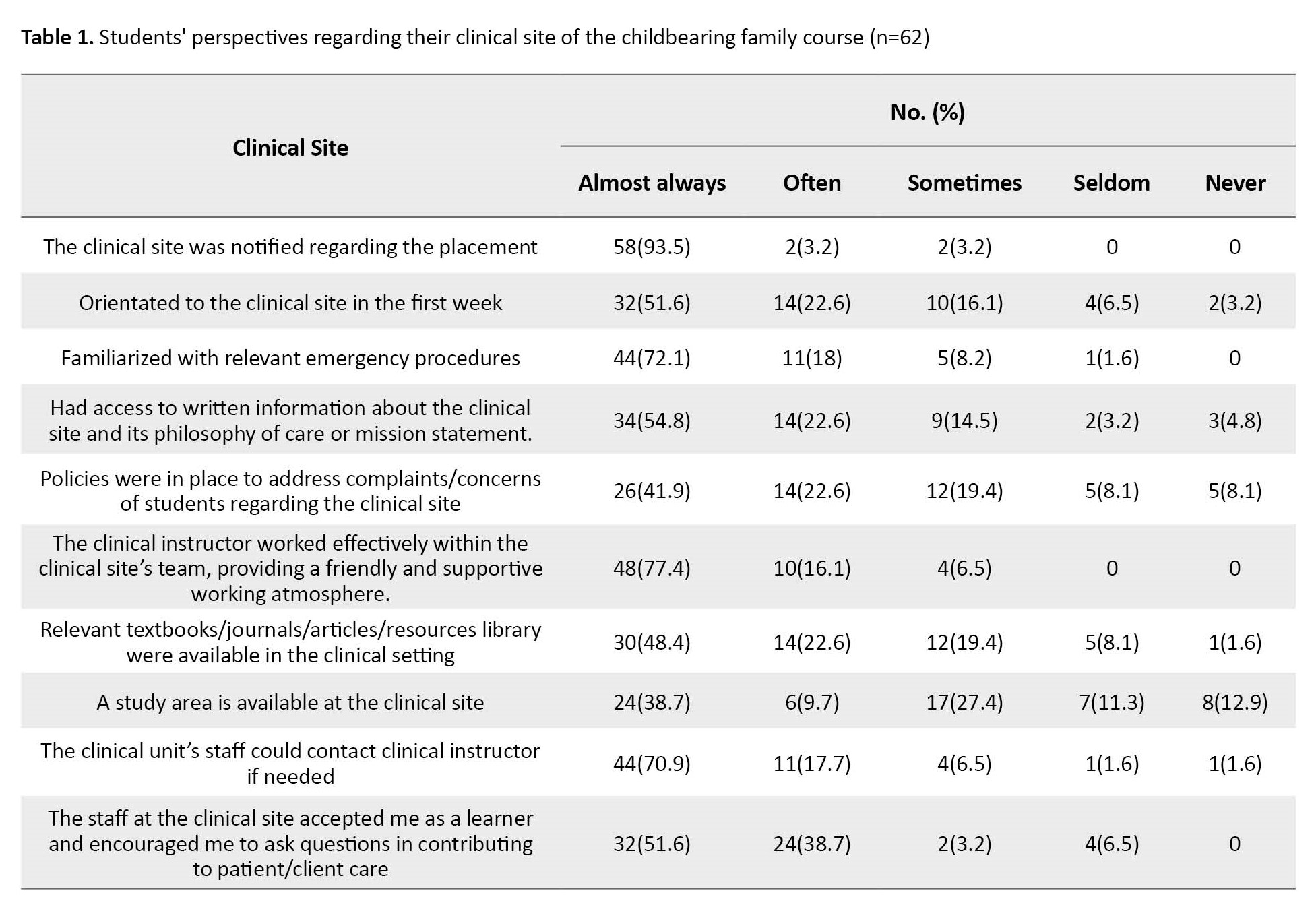
The views displayed that the vast majority of students (93.5%) answered that they “almost always” receive notification about the clinical site placement, while 38.7% mentioned the availability of study areas to students at the clinical site.
Table 2 presents the distribution of the second 2, i.e.
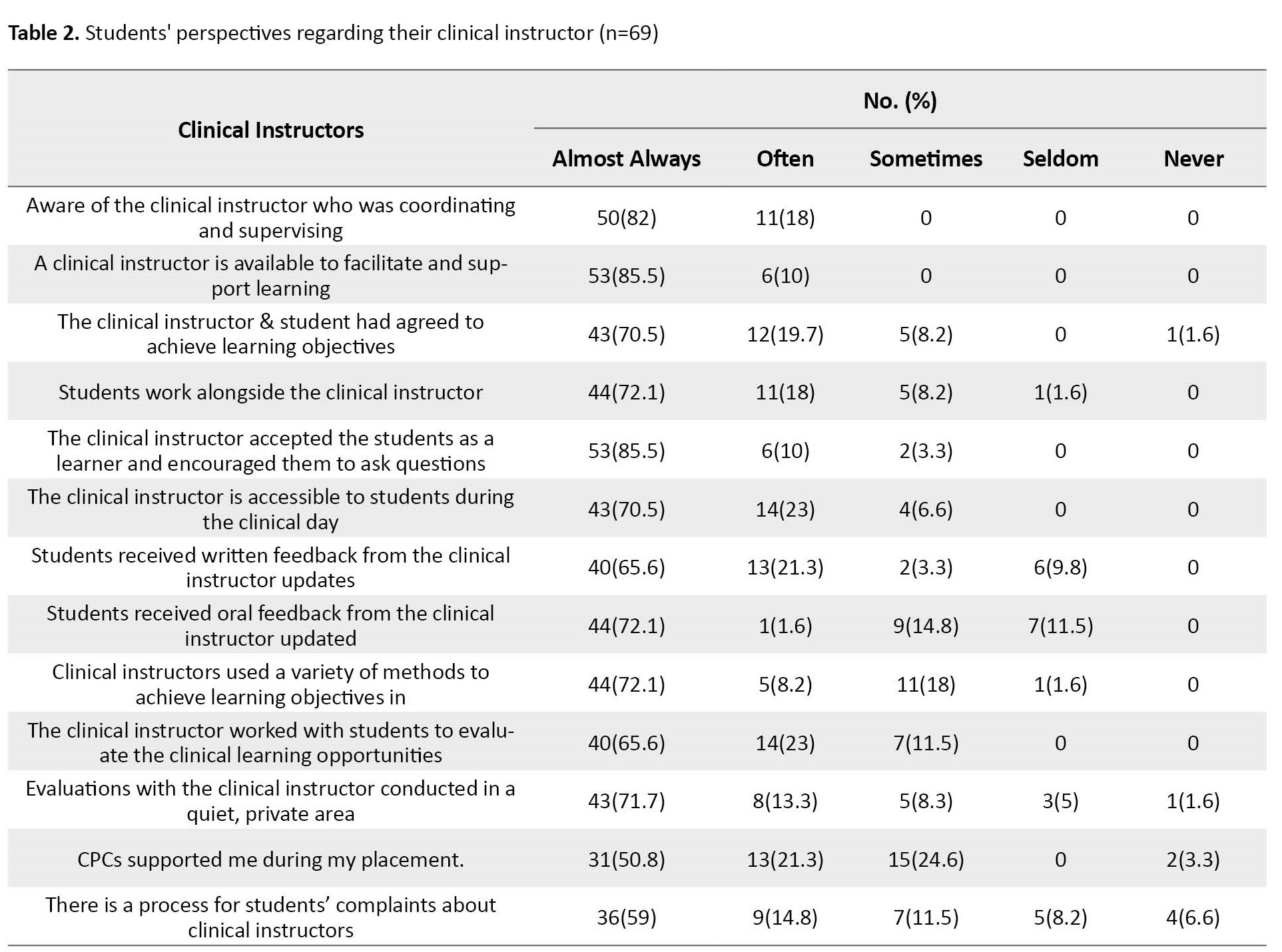
students’ perspectives regarding their clinical instructor. It reflects that the highest degree (almost always) achieved 85.5% in clinical instructor availability to facilitate and support learning and clinical instructor acceptance to learners and encourage them to ask questions. Simultaneously, to the slightest degree, 50.8% of clinical course coordinators (CPCs) support students during the placement process. Of the 10th percentage range, the highest percentage ranged from 23% in the statement about the clinical instructor who works with students to evaluate their clinical learning opportunities to 8.2% of clinical instructors who used various methods to achieve learning objectives.
Table 3 presents the distribution of students’ perspectives regarding the high quality of the childbearing family nursing practice indicators.
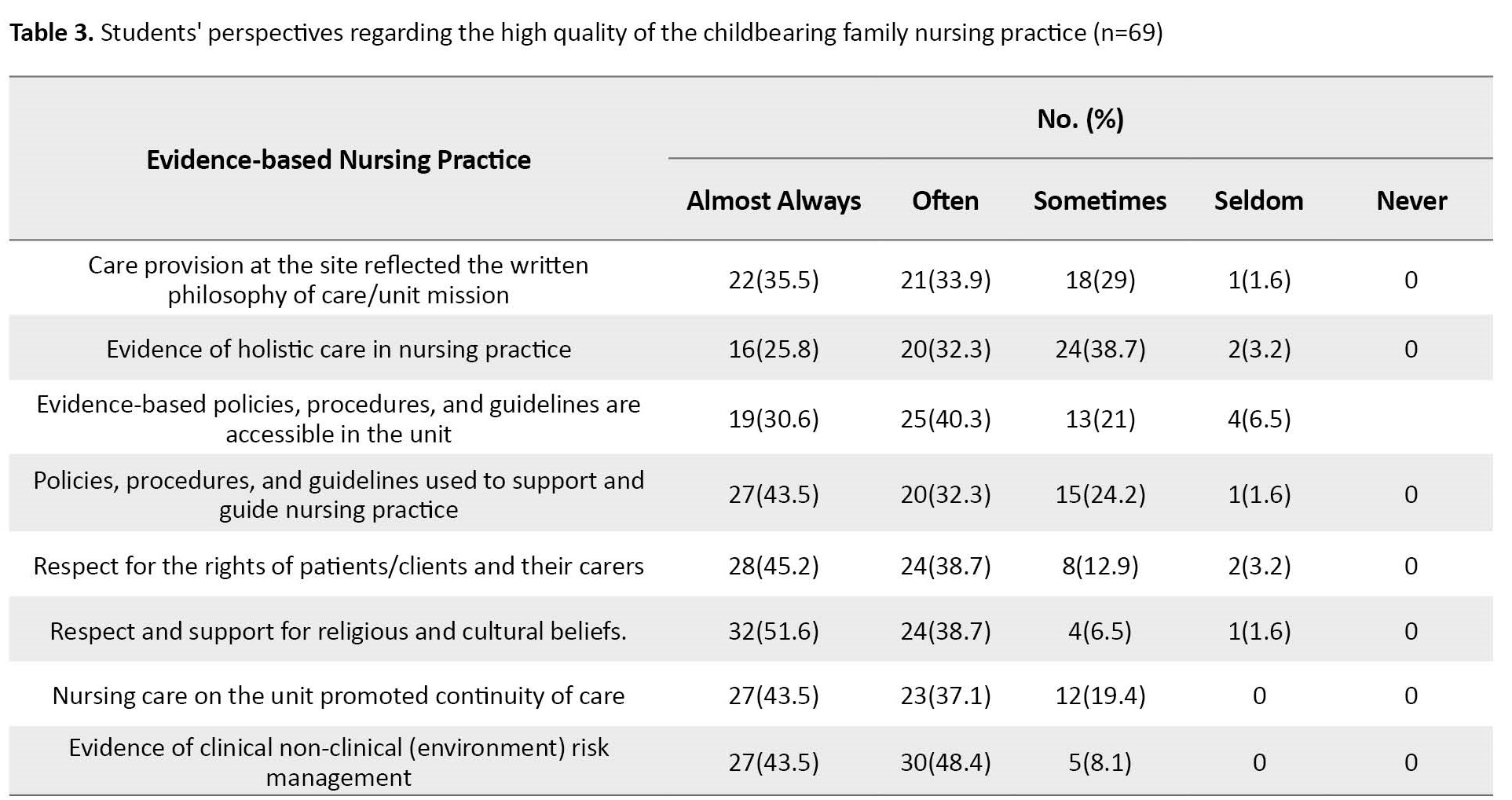
It reflects that the highest degree (almost always) achieved 45.2% regarding patients/clients and their carers’ rights. While the smallest percentage, i.e. 25.8%, was achieved in evidence of holistic care in nursing practice.
Table 4 indicates that two-thirds of students (64.5%) almost always complete the required preparation activities before simulations, 16.1% said often, while 4.8% said sometimes.
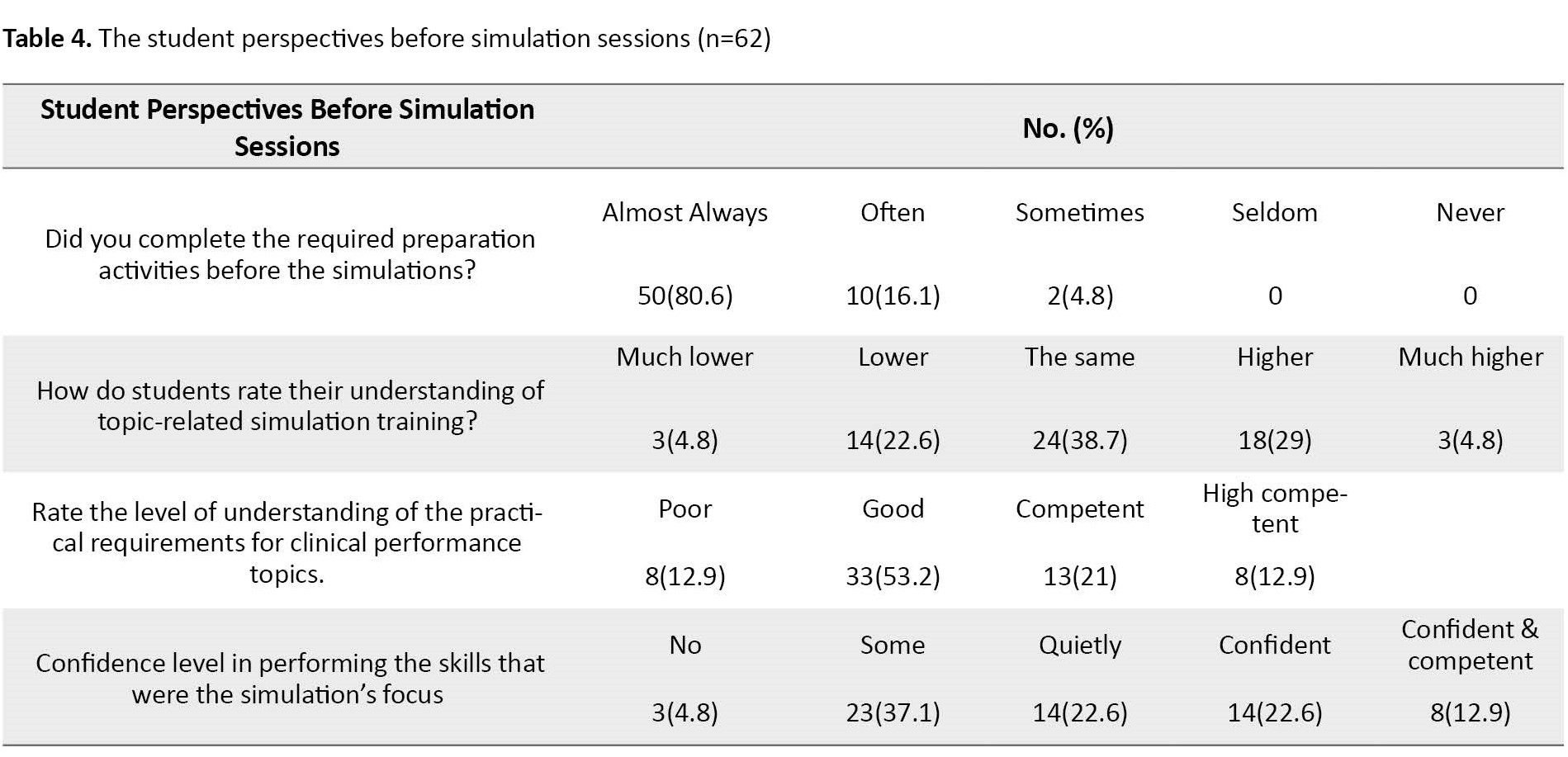
Regarding students’ rating of their understanding of a topic related to simulation training, 38.7% reported the same level, 29% confirmed a higher level, and only 4.8% a much higher level. In addition, more than one-third (37.1%) verified some confidence level in performing the skills that were the simulation’s focus.
Table 5 presents students’ perspectives after taking part in the clinical simulation labs.
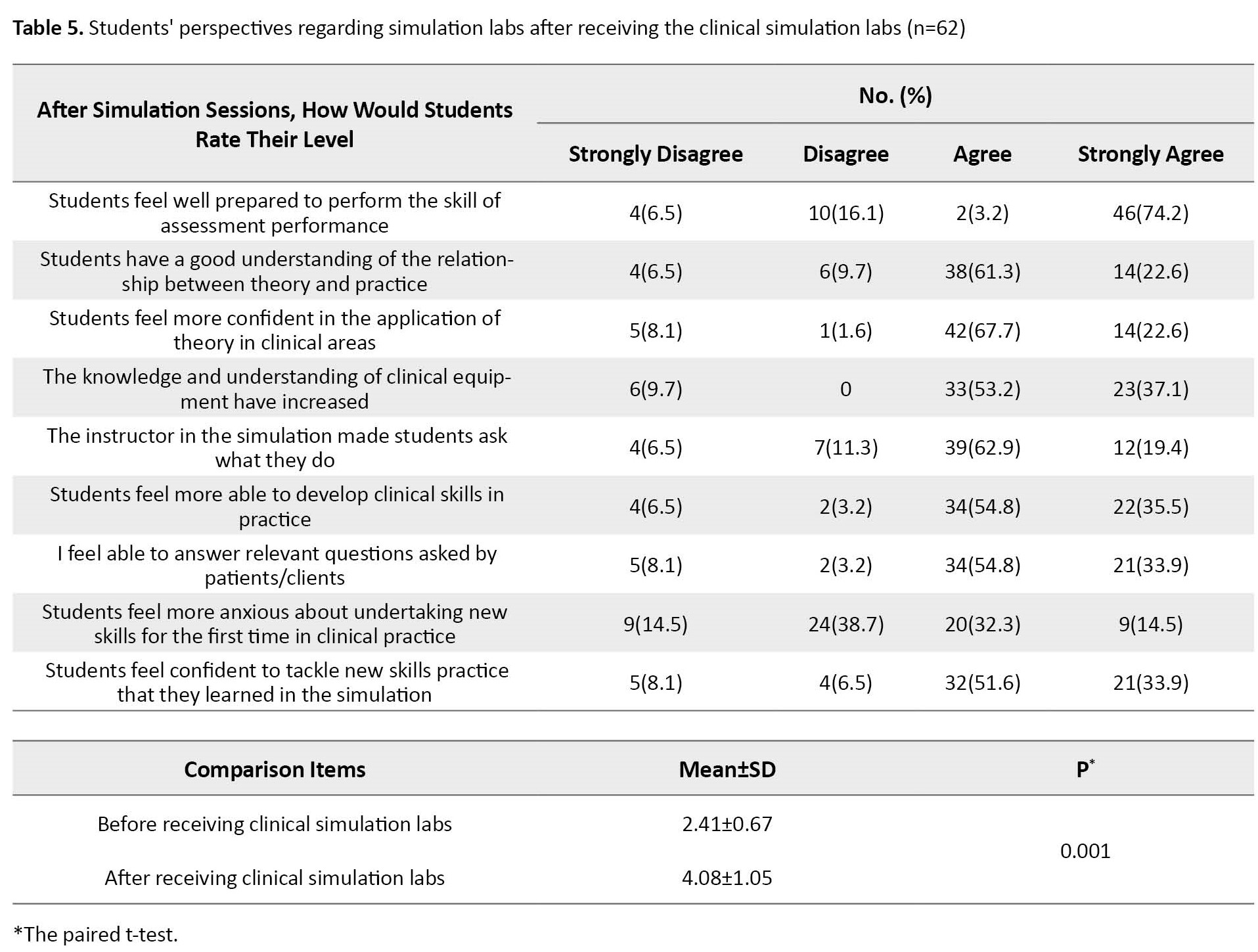
It confirms that about three-quarters (74.2%) strongly agree to feel prepared to perform an assessment. However, two-thirds (61.3%) agreed they understand the relationship between theory and practice well. More than two-thirds (67.7%) felt more confident applying theory in clinical areas. Regarding anxiety about undertaking new skills for the first time in clinical practice, 32.3% confirmed, and 51.6% felt confident in tackling new skills in training, skills that students learned in simulation. Comparison between students’ perspectives about simulation labs (before and after receiving the clinical simulation labs shows a highly significant difference (P=0.001).
Describing simulation preparation materials (theory) is part of students’ perspectives. The participants showed that 1.6% suggested more emergent cases at the bedside than normal childbirth care, such as late decelerations, breech position, and amniotic fluid embolism. While 4.83% reported that simulation reinforced what they had learned in theory, 3.2% reported that the discussion in the simulation section was helpful. Also, 1.6% said the information before and after review theories was helpful. Another 1.6% said that simulation offered the opportunity to observe critical cases that not everyone could see in reality on the unit. The last two students (3.6%) added that more details about the material should have been given before the simulation to help understand the theory.
The correlation between the students’ perspective regarding the clinical site and clinical instructors is shown in Table 6.
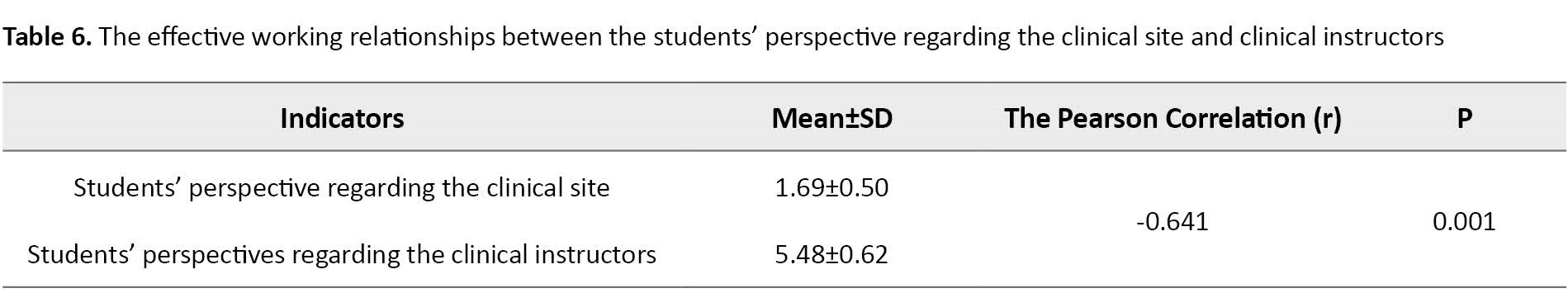
The Pearson test showed a negative significant correlation between the first and second aspects (r=-0.641, P=0.001).
Discussion
This study aimed to evaluate the clinical learning environment in the context of the nursing the childbearing family course at an advanced level of education by assessing the students’ perspectives about their clinical site, clinical instructor, and the effective working relationships between the university and the clinical site. Similarly, a Turkish study [15] confirms that the clinical learning environment is essential for enhancing students’ competencies in laboratory settings before practicing in a real patient care environment.
Regarding the students’ perspectives about the first aspect (the clinical site) of the childbearing family course, the findings of this study showed that the vast majority answered that they “almost always” received a notification about the clinical site placement, and one-fourth found the reflective practice was facilitated during the placement.
Students’ perspectives regarding their clinical instructor reflected that the majority responded as “almost always.” It means the availability of the clinical instructor to facilitate support, accept learners, and encourage them to ask questions. The vast majority would access relevant information relating to the course in the clinical setting. The students’ answers showed that the briefing section of the simulation was helpful. These findings, supported by a similar study [10], reported that the students also said that simulation training should be pre-requisite and obligatory before starting the clinical practice of midwifery practice in the real environment.
Most students confirmed that the clinical instructor accepted them as learners and encouraged them to ask questions. This finding supported that the faculty instructors should adhere to their learning objectives to achieve the learning outcomes. Likewise, another study [16] reported that a faculty member should follow the best practice model through simulation sections to provide practical clinical training.
Our findings showed that most students completed the required preparation activities before the simulations. In the same way, another study [17] confirmed that the simulation practices improved the students’ clinical practice skills and were satisfactory with their education. After receiving the clinical simulation labs, many students demonstrated that they strongly felt well-prepared to perform the skill of assessment performance. These findings match another study [9], which reported that simulation and skills education supported the development of midwifery skills and facilitated students’ learning capacity in transition from theory to practice. Similarly, an integrative review [13] was conducted to evaluate the use of simulation in nursing education. It demonstrated that simulation practices contributed to developing critical thinking and self-confidence and helped students be competent in clinical skills. Similarly, another study [18] revealed that students’ simulation experience significantly helped them. Another study in Sweden [19] reported that participants could describe their feelings and confirmed their preparedness for having challenges in care and communicating with patients in the future.
Moreover, in the open questions, students reported needing more training on topics like breech position and amniotic fluid embolism. However, other views confirmed that their confidence level had increased since attending the birth process. Consistent with the study’s findings, the results of a study [20] demonstrated that improving students’ confidence during simulation encourages them to learn more about obstetric emergencies, which would eventually enhance patient care.
Our study explored anxiety levels regarding undertaking new skills for the first time in clinical practice. However, the anxiety level was replaced by a confident feeling regarding these new skills when practicing what they learned in simulation. This finding was confirmed by a Turkish study [10], which revealed that simulation would reduce anxiety during practice and improve the profession accordingly. Moreover, in the current study, the students’ perspectives improved, reflecting the importance of simulation labs. The difference was significant before and after receiving the clinical simulation labs. Likewise, the findings of another study [21] show that students’ post-test scores following simulation application with a simulated patient were significantly higher than their pret-est scores.
The current study was an inspection study to evaluate the clinical learning environment in the context of the childbearing family course based on the students’ perspectives at the Johns Hopkins School of Nursing. The findings reflected that the students’ perspectives are positively high toward the four standards of the clinical site, clinical instructor, effective working relationships between the university and the clinical site, and simulation labs. However, some students underscored the need for more education topics such as obstetric emergencies, breech position, and amniotic fluid embolism. This finding confirms that the clinical environment gives the students more confidence to go beyond the course procedures and ask for more complicated scenarios.
Based on the results of this study, we recommend periodic monitoring for the clinical environment development, synchronizing with the advanced education level, and developing an appropriate plan in the low-middle setting to establish the clinical environment in nursing schools. Further studies are needed to focus on universal guidelines for a productive learning environment for undergraduate and postgraduate midwifery and maternity nursing courses and updating curricula in developing countries to include more real simulation labs.
This study was done to evaluate nursing in the childbearing family course at John Hopkins University at the School of Nursing. As a result, the study findings’ generalizability is limited to a specific department. However, the study highlighted the importance of students’ perspectives for a more advanced level of the clinical environment.
Ethical Considerations
Compliance with ethical guidelines
The required study permissions were received from the School of Nursing at John Hopkins University and the Institutional Review Board (Code: IRB00137384) in June 2017. The study was carried out per relevant guidelines and regulations. Informed consent was obtained from all participants. The students received a written consent form regarding the study, including voluntary participation and withdrawal at any time without further explanation.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Data collection and statistical analysis: Howieda Fouly; Drafting the manuscript: Patricia M Davidson; Conceptualization and final approval: The both authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Nicole Warran at School of Nursing John Hopkins University for all the support and help introduced during the study.
References
The clinical learning environment includes students, educators, clinical staff, patients, various experiences, perspectives, and aspects of interactions. These myriad components must interact as students are expected to be socialized in the professional community, a journey affected by individual characteristics such as personality and preferences. Consequently, students’ viewpoints are crucial for the qualified and safe patient care and security of the trainee learning and familiarizing with the career to achieve an effective clinical learning environment [1, 2].
Clinical simulation training is a teaching method to help students acquire nursing knowledge and competencies. This objective is achieved through debriefing after reproducing clinical scenarios using a simulator. Hence, nursing educators should familiarize themselves with the required instruments to integrate simulation skills into their core curriculum. Although nursing research confirmed the widespread adoption of simulation-based education within nursing and midwifery education, the scope of the practice, setup, and evidence for simulation-based training and education is still under investigation [3].
The simulation positively influences the students, educators, and, consequently, the broader community due to replicating a clinical environment similar to natural settings. It enables nursing practice in a safe, simulated environment, elevating the quality of care and imbuing ethical perspectives with actual patients during their training stage. Also, it ensures the protection and respect of human rights via following professionalism in the learning process [4].
During simulations, students are divided into small groups to practice and gain training in nursing and midwifery. The active pedagogical strategy helps students translate their acquired knowledge into technical skills and practice rules through critical thinking. In addition to enhancing their competence, professional level, and quality of care, simulations reduce errors or harm to patients [5, 6, 7, 8].
During simulation, managing critical obstetric conditions will develop professional skills in a real-life environment that provides students with the required qualifications [9]. Despite the mentioned benefits of simulation education, it still needs a periodic evaluation from students’ perspectives to pick up any shortages and make it up-to-date with the advanced technology [10].
The significance of the study lies in its contribution to improving childbearing nursing education. National leaders have underscored the need for more efficient and practical instruction, emphasizing the importance of learning environment outcomes to address these educational needs through innovative approaches and adaptability to changing circumstances [11, 12, 13]. Simulation acts as a bridge between academic and clinical performance. Therefore, students’ perspectives regarding simulation and clinical experience can help educators rectify future concerns. This study aimed to evaluate the clinical learning environment in the context of the “nursing the childbearing family” course at an advanced level of education in a developed country through these questions.
From students ‘perspectives, is there a relationship between the university and the clinical site?
Are students’ perspectives different before and after receiving clinical training?
Materials and Methods
This study employed an observational prospective design and was conducted at simulation labs at the School of Nursing, Johns Hopkins University, Baltimore, Maryland, USA.
A convenient sample included all students who agreed to participate in the study. All students from this course were invited, of whom 62(84.93%) participated. They were enrolled in the childbearing family course at the School of Nursing at Johns Hopkins University in Spring 2017. The students were between 23 and 35 years old, lived in Baltimore, Maryland, and agreed to participate in the investigation.
A structured questionnaire assessed students’ perspectives on the clinical learning environment. The questionnaire comprised 54 questions (50 multiple-choice and 4 open-ended questions). The questions were designed to explore four aspects: The first is about students’ clinical sites. It contained 17 questions; 16 were graded on a 5-point Likert scale (5=almost always, 4=often, 3=sometimes, 2=seldom, and 1=never), and one question was open-ended, exploring students’ suggestions for clinical sites. The second aspect was about the students’ perspectives of their clinical instructor. It contained 14 questions, 13 of which are graded with a Likert scale, and the last one is an open-ended question for students’ suggestions. The third aspect asks about the effective working relationships between the university and the clinical site. It contained 9 questions; 8 were graded on a Likert scale, and the last was an open-ended question for students’ suggestions. The fourth aspect included 14 questions about students’ perspectives of the simulation labs (before and after the clinical training); 4 of them were multiple-choice questions about before the training and 10 questions after receiving the lab training, 9 of them were graded as 1=strongly disagree, 2=disagree, 3=agree, and 4=strongly agree. The tenth and the last one is an open-ended question.
The study questionnaire was adopted from the audit of the clinical environment: Student questionnaire version 2010 [14] School of Nursing and Midwifery, University College Cork. Our version was modified to be marked on the Likert scale and multiple-choice questions instead of “yes” or “no” ones in the questionnaire. Three maternity, childbearing, and nursing education experts reviewed the questionnaire, and all their comments reflected that the questionnaire was transparent and relevant to what it is supposed to measure. Also, its reliability was tested, and the Cronbach α was found to be 0.932, which is of high reliability based on standardized items.
The study evaluated the clinical learning environment of the course (NR.120.520 nursing the childbearing family), one of the undergraduate courses offered at Johns Hopkins University. In this course, students build and develop assessment, care planning, communication, and leadership skills in the context of caring for childbearing families. During the preparation phase, the researcher focused on the simulation labs’ facilities for clinical training, assisting students with clinical materials, guided practice, and immediate feedback to students. He supervised the actual performance of the skill in the clinical laboratory, clinical learning environment, utilization of clinical learning opportunities, and techniques of using scenarios in simulation labs in compliance with the International Nursing Association for Clinical Simulation and Learning (INACSL) principles. The methods of filling in student progress reports per placement area, supervisor consultation with students, and communication skills were used during simulation lab training and recording students’ responses in dealing with conflicting situations.
In the simulation session, the researcher attended a postpartum hemorrhage simulation lasting 20 minutes. The scene showed students sitting in a debriefing room to receive instructions about the simulation lab. Before that, they had received the simulation scenario on their blackboard to be prepared. The students were divided into two groups. One group was to be role players in the simulation scenario, and the other group was observed during their role-playing through a big screen that permitted the last group to observe without distracting their colleagues as they were unseen. The procedure started with a conversation between the students in the “nurse role” and the clinical instructor in the “patient role.” In contrast, the student spoke in a highly simulated form. Then, the “simulated nurse” asked the “simulated patient” about her health and pain history and took blood pressure, which was 120/80 mm Hg. During the assessment of the uterus, the simulated nurse felt it was boggy and asked the patient if he would make a uterine massage to check her bleeding status; he also asked about the time of changing her perineal pad. Then, he asked her if she needed any breastfeeding concerns and if she fed her newborn.
For data gathering, the researcher uploaded the questionnaire with the consent form on the Qualtrics survey, available on the School of Nursing at Johns Hopkins University blackboard for students’ responses. Simultaneously, the researcher sent a message to each student, including the questionnaire link, to notify them about the study. Later, the researcher followed up the students’ responses daily until they finished within 9 months.
The SPSS software, version 22 was used for statistical analysis based on the proposed objectives and variables. Descriptive statistics were used to sort out the obtained information, as frequency, percentage, Mean±SD. Inferential statistics such as the Pearson test were used to determine the correlation between the students’ perspectives regarding the clinical site and clinical instructors, and the paired t-test to compare the mean scores of the students’ performances before and after receiving the simulation training labs. P<0.05 were considered statistically significant. There was no missing data as the online questionnaire design required the responder to answer the question in order to move to the next question.
Results
The study participants were 62 BSc nursing students with a 100% response rate. They were enrolled in childbearing and family nursing course in the academic year. The participants’ Mean±SD age was 20.75±0.97 years, and all live in Baltimore, near the Johns Hopkins University School of Nursing campus. Two-thirds of the participants were female (61.3%), and the remaining (38.7%) were male. A majority (88.7%) of the participants were US citizens.
Table 1 presents the distribution of students’ perspectives regarding the first aspect of the clinical site according to the childbearing family course.
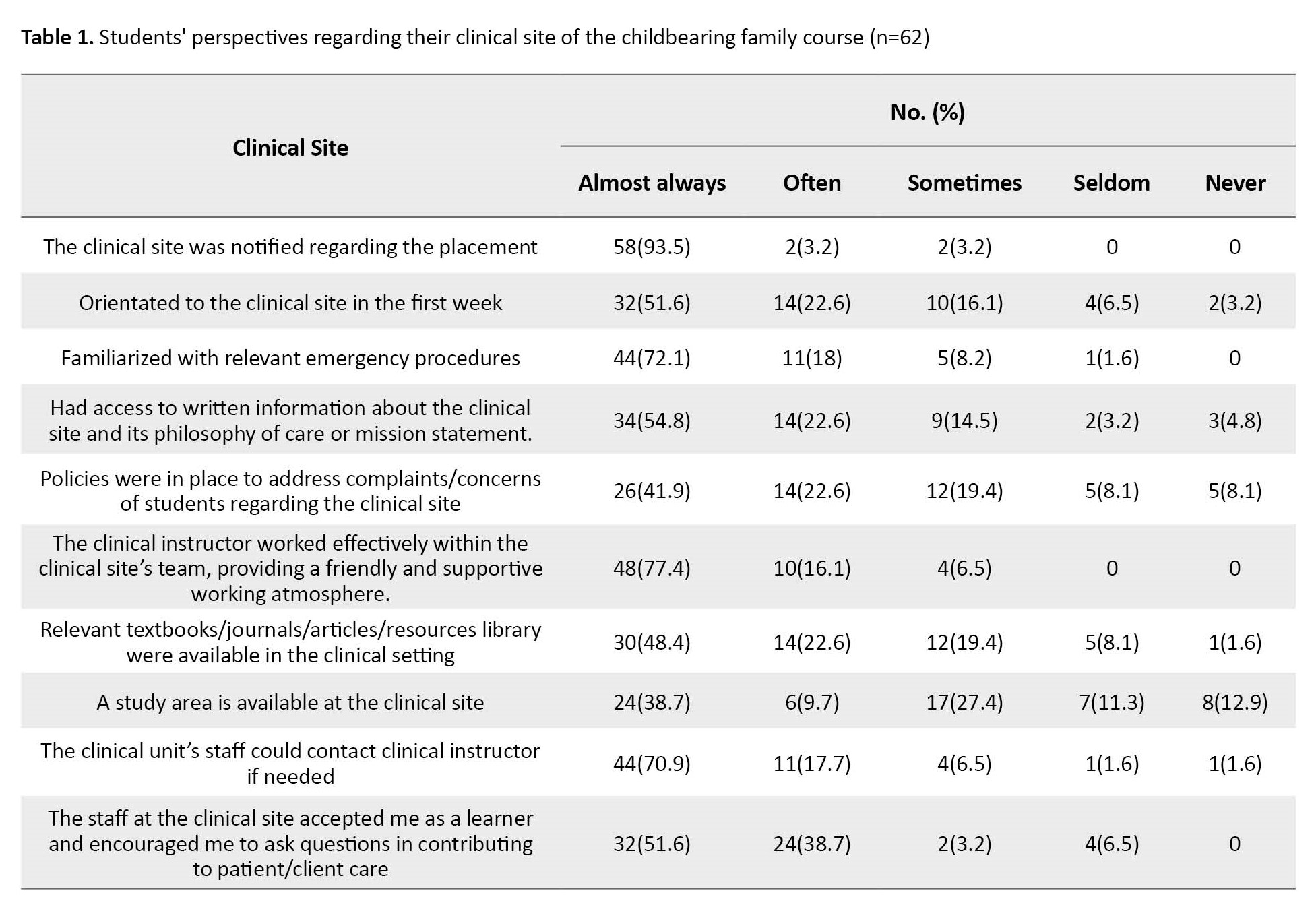
The views displayed that the vast majority of students (93.5%) answered that they “almost always” receive notification about the clinical site placement, while 38.7% mentioned the availability of study areas to students at the clinical site.
Table 2 presents the distribution of the second 2, i.e.
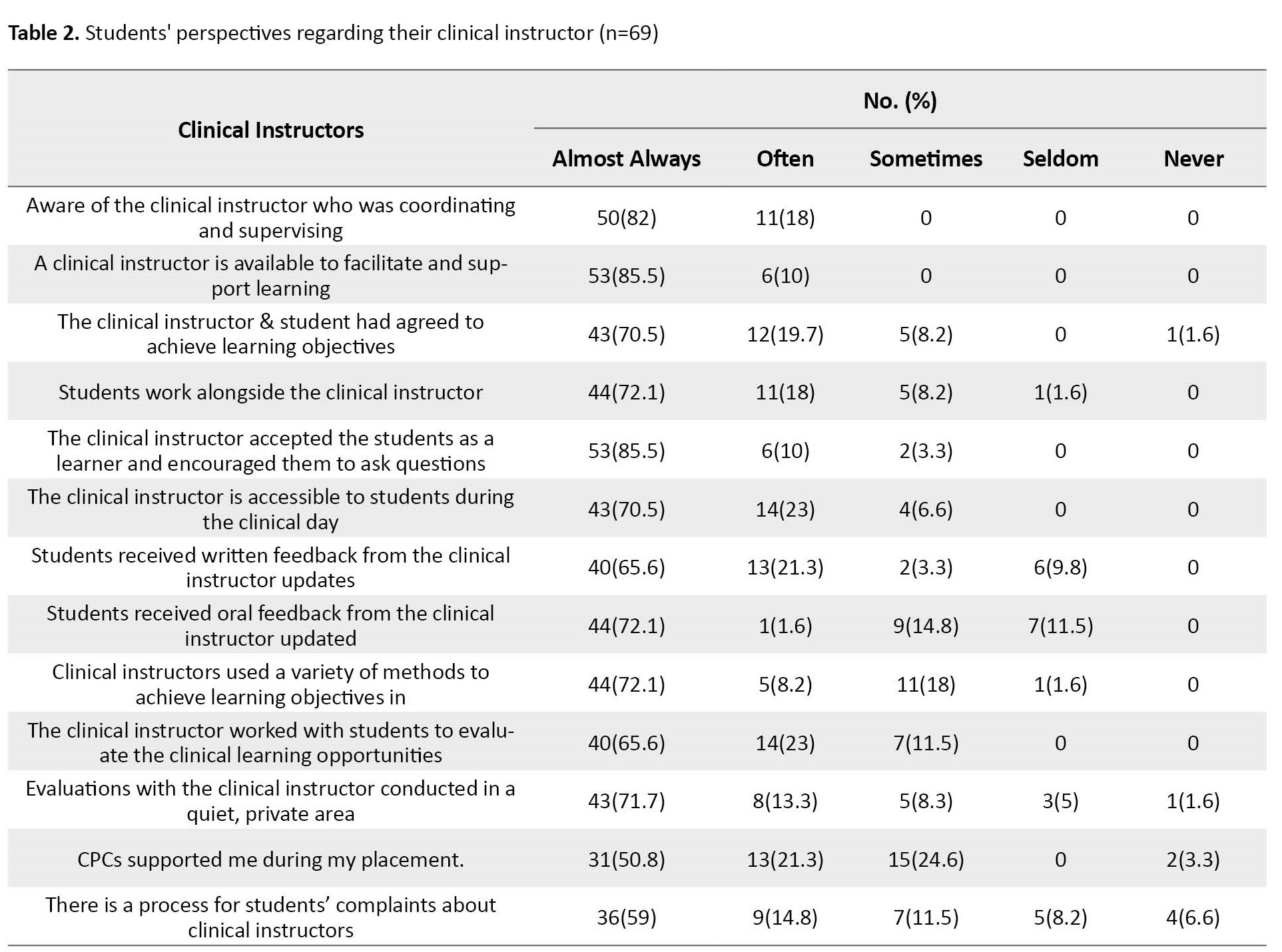
students’ perspectives regarding their clinical instructor. It reflects that the highest degree (almost always) achieved 85.5% in clinical instructor availability to facilitate and support learning and clinical instructor acceptance to learners and encourage them to ask questions. Simultaneously, to the slightest degree, 50.8% of clinical course coordinators (CPCs) support students during the placement process. Of the 10th percentage range, the highest percentage ranged from 23% in the statement about the clinical instructor who works with students to evaluate their clinical learning opportunities to 8.2% of clinical instructors who used various methods to achieve learning objectives.
Table 3 presents the distribution of students’ perspectives regarding the high quality of the childbearing family nursing practice indicators.
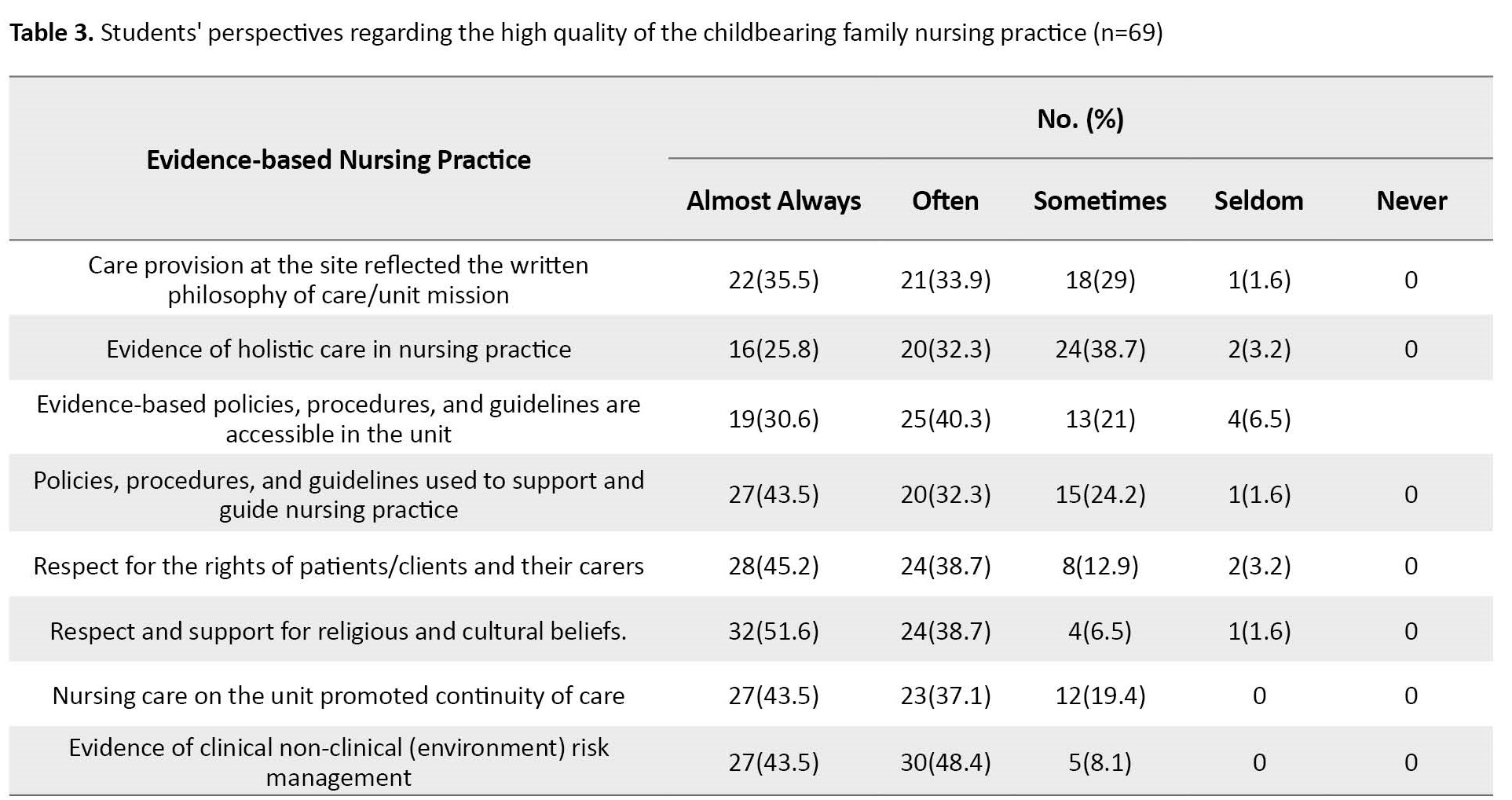
It reflects that the highest degree (almost always) achieved 45.2% regarding patients/clients and their carers’ rights. While the smallest percentage, i.e. 25.8%, was achieved in evidence of holistic care in nursing practice.
Table 4 indicates that two-thirds of students (64.5%) almost always complete the required preparation activities before simulations, 16.1% said often, while 4.8% said sometimes.
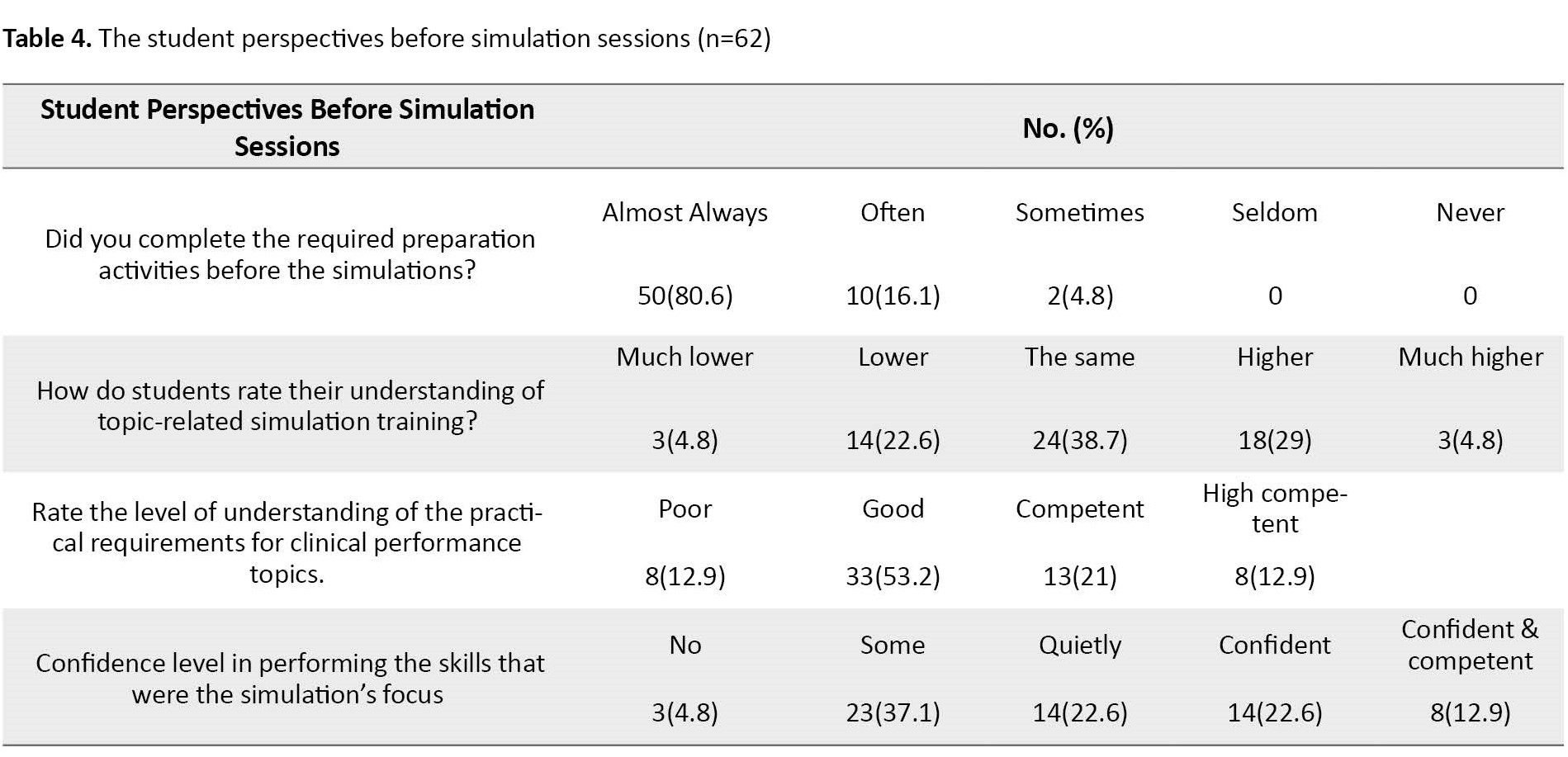
Regarding students’ rating of their understanding of a topic related to simulation training, 38.7% reported the same level, 29% confirmed a higher level, and only 4.8% a much higher level. In addition, more than one-third (37.1%) verified some confidence level in performing the skills that were the simulation’s focus.
Table 5 presents students’ perspectives after taking part in the clinical simulation labs.
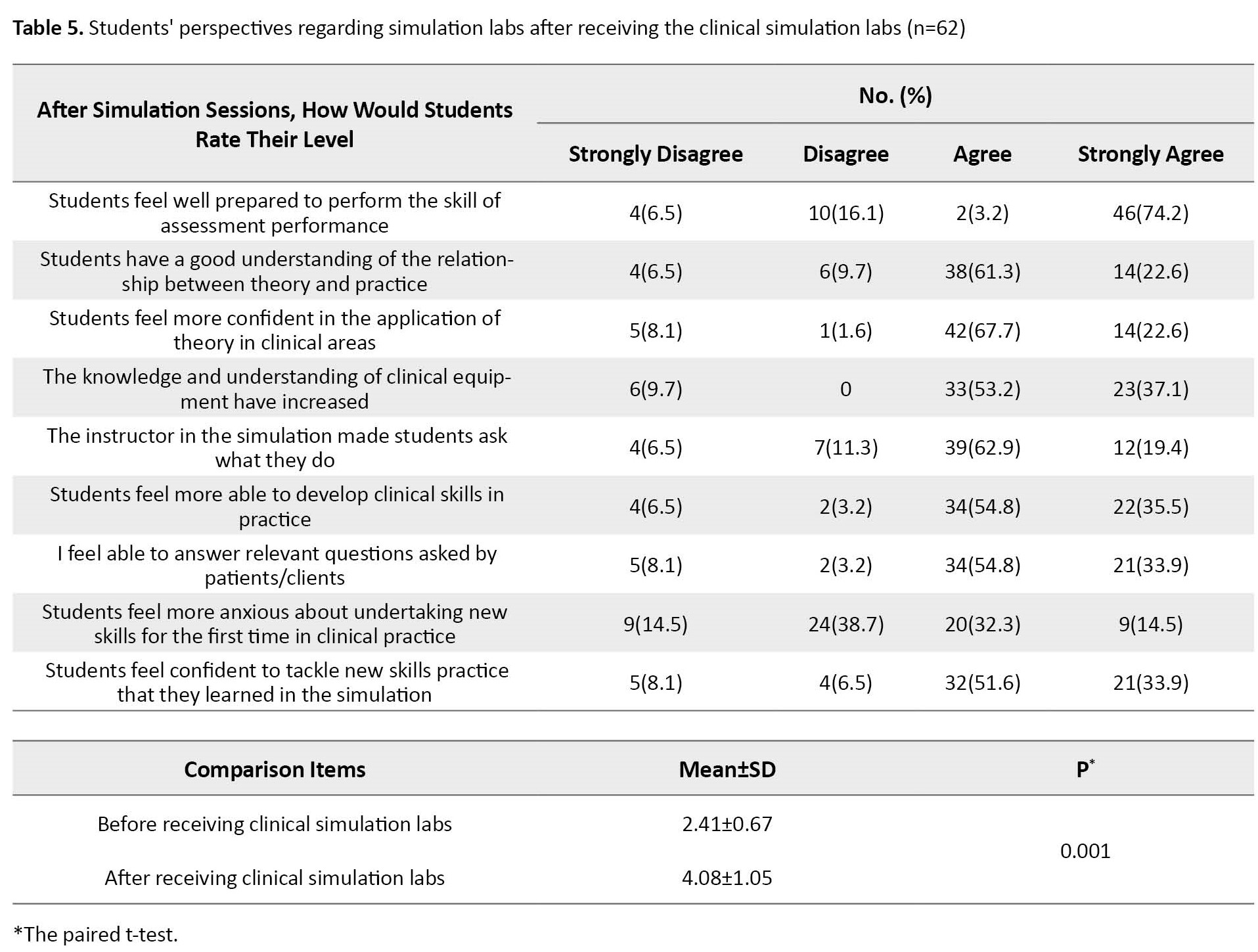
It confirms that about three-quarters (74.2%) strongly agree to feel prepared to perform an assessment. However, two-thirds (61.3%) agreed they understand the relationship between theory and practice well. More than two-thirds (67.7%) felt more confident applying theory in clinical areas. Regarding anxiety about undertaking new skills for the first time in clinical practice, 32.3% confirmed, and 51.6% felt confident in tackling new skills in training, skills that students learned in simulation. Comparison between students’ perspectives about simulation labs (before and after receiving the clinical simulation labs shows a highly significant difference (P=0.001).
Describing simulation preparation materials (theory) is part of students’ perspectives. The participants showed that 1.6% suggested more emergent cases at the bedside than normal childbirth care, such as late decelerations, breech position, and amniotic fluid embolism. While 4.83% reported that simulation reinforced what they had learned in theory, 3.2% reported that the discussion in the simulation section was helpful. Also, 1.6% said the information before and after review theories was helpful. Another 1.6% said that simulation offered the opportunity to observe critical cases that not everyone could see in reality on the unit. The last two students (3.6%) added that more details about the material should have been given before the simulation to help understand the theory.
The correlation between the students’ perspective regarding the clinical site and clinical instructors is shown in Table 6.
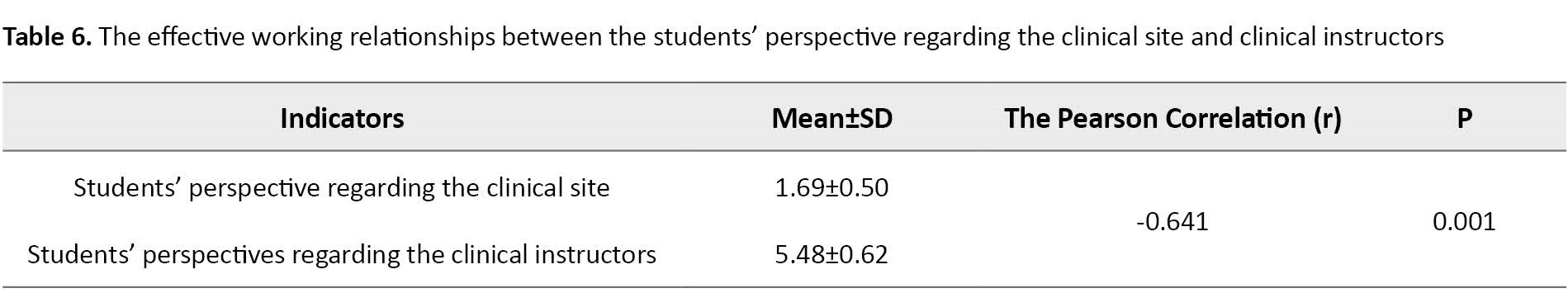
The Pearson test showed a negative significant correlation between the first and second aspects (r=-0.641, P=0.001).
Discussion
This study aimed to evaluate the clinical learning environment in the context of the nursing the childbearing family course at an advanced level of education by assessing the students’ perspectives about their clinical site, clinical instructor, and the effective working relationships between the university and the clinical site. Similarly, a Turkish study [15] confirms that the clinical learning environment is essential for enhancing students’ competencies in laboratory settings before practicing in a real patient care environment.
Regarding the students’ perspectives about the first aspect (the clinical site) of the childbearing family course, the findings of this study showed that the vast majority answered that they “almost always” received a notification about the clinical site placement, and one-fourth found the reflective practice was facilitated during the placement.
Students’ perspectives regarding their clinical instructor reflected that the majority responded as “almost always.” It means the availability of the clinical instructor to facilitate support, accept learners, and encourage them to ask questions. The vast majority would access relevant information relating to the course in the clinical setting. The students’ answers showed that the briefing section of the simulation was helpful. These findings, supported by a similar study [10], reported that the students also said that simulation training should be pre-requisite and obligatory before starting the clinical practice of midwifery practice in the real environment.
Most students confirmed that the clinical instructor accepted them as learners and encouraged them to ask questions. This finding supported that the faculty instructors should adhere to their learning objectives to achieve the learning outcomes. Likewise, another study [16] reported that a faculty member should follow the best practice model through simulation sections to provide practical clinical training.
Our findings showed that most students completed the required preparation activities before the simulations. In the same way, another study [17] confirmed that the simulation practices improved the students’ clinical practice skills and were satisfactory with their education. After receiving the clinical simulation labs, many students demonstrated that they strongly felt well-prepared to perform the skill of assessment performance. These findings match another study [9], which reported that simulation and skills education supported the development of midwifery skills and facilitated students’ learning capacity in transition from theory to practice. Similarly, an integrative review [13] was conducted to evaluate the use of simulation in nursing education. It demonstrated that simulation practices contributed to developing critical thinking and self-confidence and helped students be competent in clinical skills. Similarly, another study [18] revealed that students’ simulation experience significantly helped them. Another study in Sweden [19] reported that participants could describe their feelings and confirmed their preparedness for having challenges in care and communicating with patients in the future.
Moreover, in the open questions, students reported needing more training on topics like breech position and amniotic fluid embolism. However, other views confirmed that their confidence level had increased since attending the birth process. Consistent with the study’s findings, the results of a study [20] demonstrated that improving students’ confidence during simulation encourages them to learn more about obstetric emergencies, which would eventually enhance patient care.
Our study explored anxiety levels regarding undertaking new skills for the first time in clinical practice. However, the anxiety level was replaced by a confident feeling regarding these new skills when practicing what they learned in simulation. This finding was confirmed by a Turkish study [10], which revealed that simulation would reduce anxiety during practice and improve the profession accordingly. Moreover, in the current study, the students’ perspectives improved, reflecting the importance of simulation labs. The difference was significant before and after receiving the clinical simulation labs. Likewise, the findings of another study [21] show that students’ post-test scores following simulation application with a simulated patient were significantly higher than their pret-est scores.
The current study was an inspection study to evaluate the clinical learning environment in the context of the childbearing family course based on the students’ perspectives at the Johns Hopkins School of Nursing. The findings reflected that the students’ perspectives are positively high toward the four standards of the clinical site, clinical instructor, effective working relationships between the university and the clinical site, and simulation labs. However, some students underscored the need for more education topics such as obstetric emergencies, breech position, and amniotic fluid embolism. This finding confirms that the clinical environment gives the students more confidence to go beyond the course procedures and ask for more complicated scenarios.
Based on the results of this study, we recommend periodic monitoring for the clinical environment development, synchronizing with the advanced education level, and developing an appropriate plan in the low-middle setting to establish the clinical environment in nursing schools. Further studies are needed to focus on universal guidelines for a productive learning environment for undergraduate and postgraduate midwifery and maternity nursing courses and updating curricula in developing countries to include more real simulation labs.
This study was done to evaluate nursing in the childbearing family course at John Hopkins University at the School of Nursing. As a result, the study findings’ generalizability is limited to a specific department. However, the study highlighted the importance of students’ perspectives for a more advanced level of the clinical environment.
Ethical Considerations
Compliance with ethical guidelines
The required study permissions were received from the School of Nursing at John Hopkins University and the Institutional Review Board (Code: IRB00137384) in June 2017. The study was carried out per relevant guidelines and regulations. Informed consent was obtained from all participants. The students received a written consent form regarding the study, including voluntary participation and withdrawal at any time without further explanation.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Data collection and statistical analysis: Howieda Fouly; Drafting the manuscript: Patricia M Davidson; Conceptualization and final approval: The both authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Nicole Warran at School of Nursing John Hopkins University for all the support and help introduced during the study.
References
- Ackerman-Barger K, Boatright D, Gonzalez-Colaso R, Orozco R, Latimore D. Seeking inclusion excellence: Understanding racial microaggressions as experienced by underrepresented medical and nursing students. Acad Med. 2020; 95(5):758-63. [DOI:10.1097/ACM.0000000000003077] [PMID]
- Nordquist J, Hall J, Caverzagie K, Snell L, Chan MK, Thoma B, et al. The clinical learning environment. Med Teach. 2019; 41(4):366-72. [DOI:10.1080/0142159X.2019.1566601] [PMID]
- McTague K, Smith V. Simulation-based education for nurse and midwife advanced practitioner education: A scoping review protocol.JBI Evid Synth. 2023; 21(7):1453-60. [DOI:10.11124/JBIES-22-00111] [PMID]
- World Health Organization. Simulation in nursing and midwifery education. Geneva: WHO; 2018. [Link]
- Mehdipour-Rabori R, Bagherian B, Nematollahi M. Simulation-based mastery improves nursing skills in BSc nursing students: A quasi-experimental study. BMC Nurs. 2021; 20(1):10. [DOI:10.1186/s12912-020-00532-9] [PMID]
- Martins J. Learning and development in simulated practice environments. Rev Enferm Ref. 2017; IV Série(12):155-62. [DOI:10.12707/RIV16074]
- Jones F, Passos-Neto CE, Melro Braghiroli OF. Simulation in medical education: Brief history and methodology. Princ Pract Clin Res. 2015; 1(2):56-63. [DOI:10.21801/ppcrj.2015.12.8]
- Chacko TV. Simulation-based medical education: Using best practices and curriculum mapping to maximize educational benefits in the context of shift toward competency-based medical education. Arch Med Health Sci. 2017; 5(1):9-15. [DOI:10.4103/2321-4848.208217]
- Lendahls L, Oscarsson MG. Midwifery students’ experiences of simulation- and skills training. Nurse Educ Today. 2017; 50:12-6. [DOI:10.1016/j.nedt.2016.12.005] [PMID]
- Reyhan F, Mete A, Sayiner FD, Celik N. Evaluating the views of midwifery students about simulation education. Int J Car Sci. 2018; 11(1):239-45. [Link]
- Klein-Collins R. Strategies to produce new nurses for a changing profession: A policy brief on innovation in nursing education. Chicago: Council for Adult and Experiential Learning, 2011. [Link]
- Koukourikos K, Tsaloglidou A, Kourkouta L, Papathanasiou IV, Iliadias C, Fratazana A, et al. Simulation in clinical nursing education. Acta Inform Med. 2021; 29(1):15-20. [DOI:10.5455/aim.2021.29.15-20] [PMID]
- Al Gharibi M, Arulappan MS. Repeated simulation experience on self-confidence, critical thinking, and competence of nurses and nursing students-an integrative review. SAGE Open Nurs. 2020; 6:2377960820927377. [DOI:10.1177/2377960820927377] [PMID]
- Student questionnaire nursing [Internet]. 2016 [Updated 2022 November 24]. Available from: [Link]
- Gürol A, Akpinar RB, Apay SE. [Simulasyon uygulamalarının öğrencilerin beceri düzeylerine etkisi (Turkish)]. Kocatepe Med J. 2016; 17(3):99-104. [Link]
- Kelly S. Evaluation methods used in simulation: A survey of faculty and student perceptions in an undergraduate nursing program [PhD dissertation]. Pittsburgh: University of Pittsburgh; 2015. [Link]
- Gönenç İM, Yılmaz Sezer N. Evaluation of the effectiveness of four different training techniques in the development of non-stress testing application skills: A randomised controlled trial. Nurse Educ Today. 2019; 76:118-24. [DOI:10.1016/j.nedt.2019.01.030] [PMID]
- Omer T. Nursing students’ perceptions of satisfaction and self-confidence with clinical simulation experience. J Educ Pract. 2016; 7(5):131-8. [Link]
- Isaksson J, Krabbe J, Ramklint M. Medical students’ experiences of working with simulated patients in challenging communication training. Adv Simul. 2022; 7(1):32. [DOI:10.1186/s41077-022-00230-3] [PMID]
- Brady S, Bogossian F, Gibbons K. The effectiveness of varied levels of simulation fidelity on integrated performance of technical skills in midwifery students--a randomised intervention trial. Nurse Educ Today. 2015; 35(3):524-9. [DOI:10.1016/j.nedt.2014.11.005] [PMID]
- Martin CT, Chanda N. Mental health clinical simulation: Therapeutic communication. Clin Simul Nurs. 2016; 12(6):209-14. [DOI:10.1016/j.ecns.2016.02.007]
Article Type : Research |
Subject:
General
Received: 2023/09/18 | Accepted: 2023/09/3 | Published: 2023/09/3
Received: 2023/09/18 | Accepted: 2023/09/3 | Published: 2023/09/3
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |