Sat, Jan 31, 2026
Volume 34, Issue 4 (9-2024)
JHNM 2024, 34(4): 326-334 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Roshani Tabrizi A, Sharami S H, Sabetghadam S, Mansour Ghanaei M, Sharafi R, Dalil Heirati S F et al . Factors Related to Neonatal Mortality at Discharge Among Premature Neonates in a Tertiary Care Hospital in North of Iran. JHNM 2024; 34 (4) :326-334
URL: http://hnmj.gums.ac.ir/article-1-2209-en.html
URL: http://hnmj.gums.ac.ir/article-1-2209-en.html
Ali Roshani Tabrizi1 

 , Seyedeh Hajar Sharami *2
, Seyedeh Hajar Sharami *2 

 , Shadi Sabetghadam3
, Shadi Sabetghadam3 

 , Mandana Mansour Ghanaei4
, Mandana Mansour Ghanaei4 

 , Reza Sharafi5
, Reza Sharafi5 

 , Seyedeh Fatemeh Dalil Heirati6
, Seyedeh Fatemeh Dalil Heirati6 

 , Habib Eslami-Kenarsari7
, Habib Eslami-Kenarsari7 




 , Seyedeh Hajar Sharami *2
, Seyedeh Hajar Sharami *2 

 , Shadi Sabetghadam3
, Shadi Sabetghadam3 

 , Mandana Mansour Ghanaei4
, Mandana Mansour Ghanaei4 

 , Reza Sharafi5
, Reza Sharafi5 

 , Seyedeh Fatemeh Dalil Heirati6
, Seyedeh Fatemeh Dalil Heirati6 

 , Habib Eslami-Kenarsari7
, Habib Eslami-Kenarsari7 


1- Pediatrician, Reproductive Health Research Center, Al-zahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Professor, Reproductive Health Research Center, Department of Obstetrics & Gynecology, Al-zahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,sharami@gums.ac.ir
3- Assistant Professor, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Professor, Reproductive Health Research Center, Department of Obstetrics & Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
5- Pediatric Diseases Research Center, Guilan University of Medical Sciences, Rasht, Iran.
6- Midwifery (MSc), Reproductive Health Research Center, Al-zahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
7- Biostatistics (MSc), Vice-chancellor for Research and Technology, Guilan University of Medical Sciences, Rasht, Iran.
2- Professor, Reproductive Health Research Center, Department of Obstetrics & Gynecology, Al-zahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Assistant Professor, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Professor, Reproductive Health Research Center, Department of Obstetrics & Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
5- Pediatric Diseases Research Center, Guilan University of Medical Sciences, Rasht, Iran.
6- Midwifery (MSc), Reproductive Health Research Center, Al-zahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
7- Biostatistics (MSc), Vice-chancellor for Research and Technology, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 491 kb]
(341 Downloads)
| Abstract (HTML) (914 Views)
Full-Text: (311 Views)
Introduction
Premature birth is one of the most critical and challenging problems faced by obstetricians and gynecologists. It is associated with the neonatal death and lifelong complications, such as learning disabilities and visual, hearing, and cognitive problems, and is considered as a public health problem [1-4]. Premature birth also affects the economy, health care system, and society [5]. There is a clinical challenge in dealing with premature birth and reducing its complications due to problems in identifying preventable or modifiable factors. The overall prevalence of preterm birth is increasing worldwide, with about 15 million cases reported annually, leading to the deaths of about 1.1 million children [6]. Perinatal deaths account for about 7% of the global burden of disease [7]. It is estimated that globally four million neonatal deaths and stillbirths occur every year. Almost all these deaths occur in developing countries [8, 9] The neonatal death rate in Iran has been declined in past decades, but the decline has been slowed down, recently [10, 11].
Knowing the causes and predisposing factors of neonatal death can help identify, control, or reduce the death rate. Prematurity is a critical predisposing factor for neonatal death, which, despite the vast advances in midwifery science, is still a serious problem and requires extensive planning before birth and during pregnancy. Complications of prematurity, such as infection, respiratory distress syndrome, and intraventricular hemorrhage, are important causes of neonatal death [12]. Due to the progress in midwifery and quality of services dedicated to newborns, the survival rate of premature neonates has increased dramatically. Today, more than 95% of premature neonates who born before 28 weeks of pregnancy survive [13].
Many studies in Iran have reported the predictors of neonatal death [14, 15]. To the best of our knowledge, neonatal death rate and its associated factors in the tertiary hospitals are poorly documented, particularly at the institutional level. The ability of a premature neonate to survive is different among countries depending on hospital facilities. Therefore, the health centers that accept the admission of premature neonates should plan according to their conditions and decide whether these neonates survive or not, especially in the settings with limited beds in the neonatal intensive care units (NICUs). This study aims to investigate the factors related to death among premature neonates admitted to a tertiary care hospital in Rasht, north of Iran.
Materials and Methods
This is a retrospective cross-sectional study that was conducted at a tertiary care hospital in Rasht, north of Iran, from April to October 2022. The Pediatrics Department of this hospital has two major wards: Premature neonates unit and NICU. There are 50 beds in the two wards, where the NICU has 10 beds. Premature neonates in good general conditions receive care beside their mothers. The minimum sample size was determined 1126, by considering the premature birth prevalence of 7.1% According to the results of Rezaeian et al. [16], an error rate of 0.05, a test power of 0.80, and acceptable error rate of 0.015. All medical records of neonates admitted from May 2017 to March 2022 were examined. All neonates reach gestational age of 25-37 weeks whose information was registered by the neonatal registry form from May 2017 to March 2022 in the hospital were included. The newborns older than 28 days, out-of-hospital birth cases, and revisits were excluded.
The data were collected by two trained midwives and one experienced intern who had undergone the necessary training before the study. A data collection form was used to extract the demographic and maternal/fetal and treatment-related factors. The maternal/fetal factors included the mother’s age, obstetric history, mode of delivery, cause of preterm birth, pregnancy and childbirth complications, gestational age, birth weight, the admission unit, neonate’s sex, congenital malformation, and neonatal complications during hospitalization such as electrolyte disorder, hyperglycemia (blood glucose >200 mg/dL), hypoglycemia (blood glucose <47 mg/dL), sepsis, and abnormal brain ultrasound findings (e.g. germinal matrix hemorrhage, intraventricular hemorrhage, cerebral parenchymal hemorrhage, periventricular leukomalacia, hydrocephalus). The treatment-related factors included respiratory support, breastfeeding, the given treatment, and length of hospitalization.
The collected data entered into SPSS software, version 25 and were expressed as Mean±SD and number (percentage). Chi-square test and Fisher’s exact test were used to analyze the relationships between nominal variables. The factors related to fetal death were analyzed using multivariate logistic regression.
Results
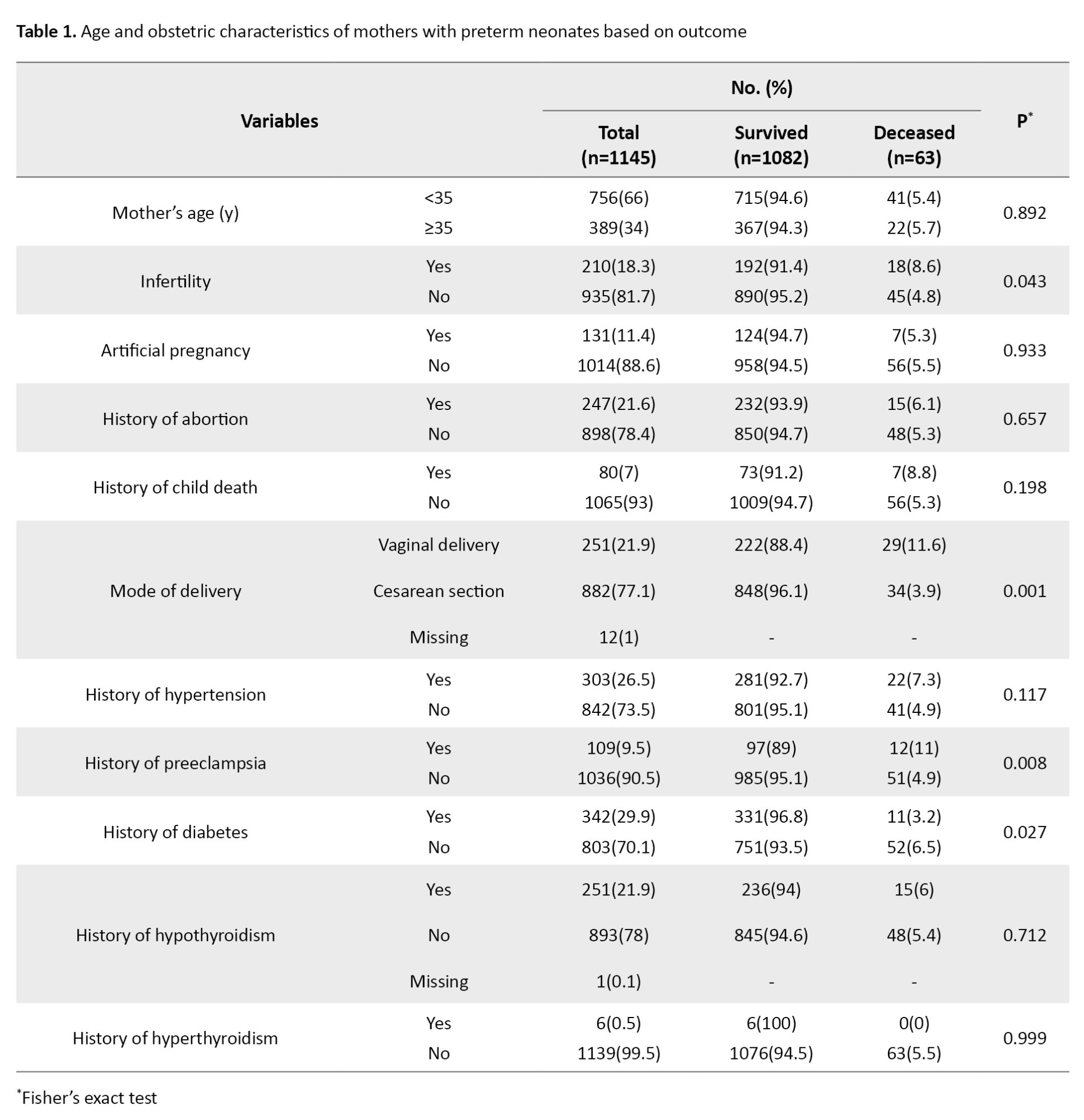
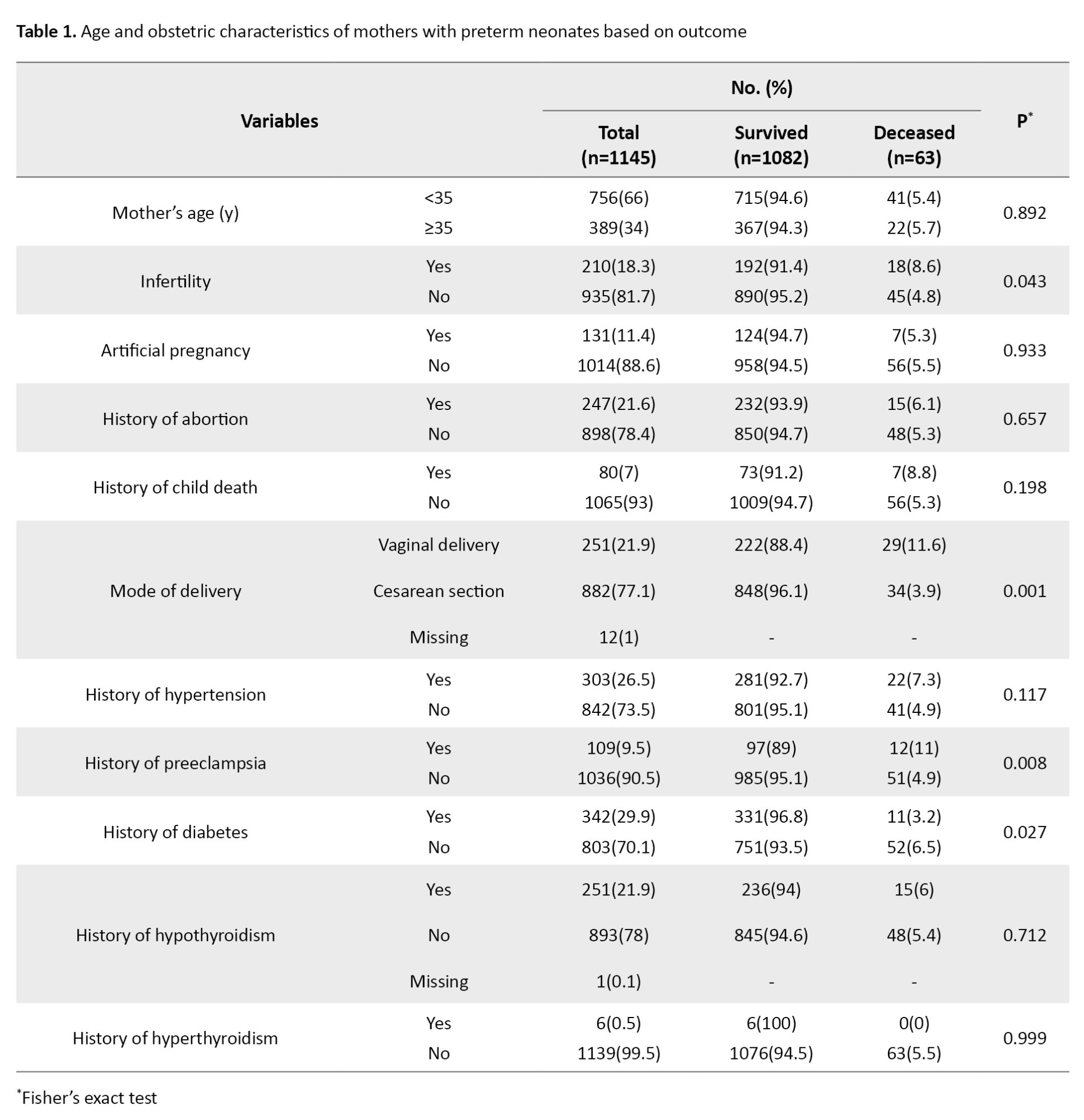
There were 1161 premature neonates registered in the NICU and Premature Neonates Unit’s database, of whom 16 were excluded (five due to revisit, and 11 due to birth outside the hospital). Finally, the data of 1145 neonates were analyzed. Most of the neonates were 33 weeks and older (71.9%). The birth weight of most of them were above 2500 g (94.1%). In most cases, the preterm births happened spontaneously (74.2%). The mean age of mothers was 30.90±6.24 years. In most cases, the mode of delivery was cesarean section (77%), and in one-third of cases, the cause was repeated cesarean section (Table 1).
There were 63(5.5%) deaths during the study period. Among the deceased neonates, 27.7% died during the first 24 hours and 69.8% died during 48 hours. The youngest survived neonate was a 750-g female with a gestational age of 25 weeks. The mean gestational age of survived and dead neonates was about 34 and 28 weeks, respectively. The average time between birth and admission to the NICU was 23 hours (ranged from 22 min to 90 hours). Among neonates, 676(59%) were hospitalized for more than seven days. Eleven neonates had retinopathy of prematurity that needed treatment, 7 had grade-1 necrotizing enterocolitis (NEC), one had grade-2 NEC, and 73(6.4%) had abnormal brain ultrasound findings. Moreover, 346(30.2%) used mechanical ventilation, and 5.2% did not receive breastfeeding and were discharged with infant formula packs. Of all neonates, 212(18.5%) were admitted to NICU, of whom 19(9%) died (Table 2).
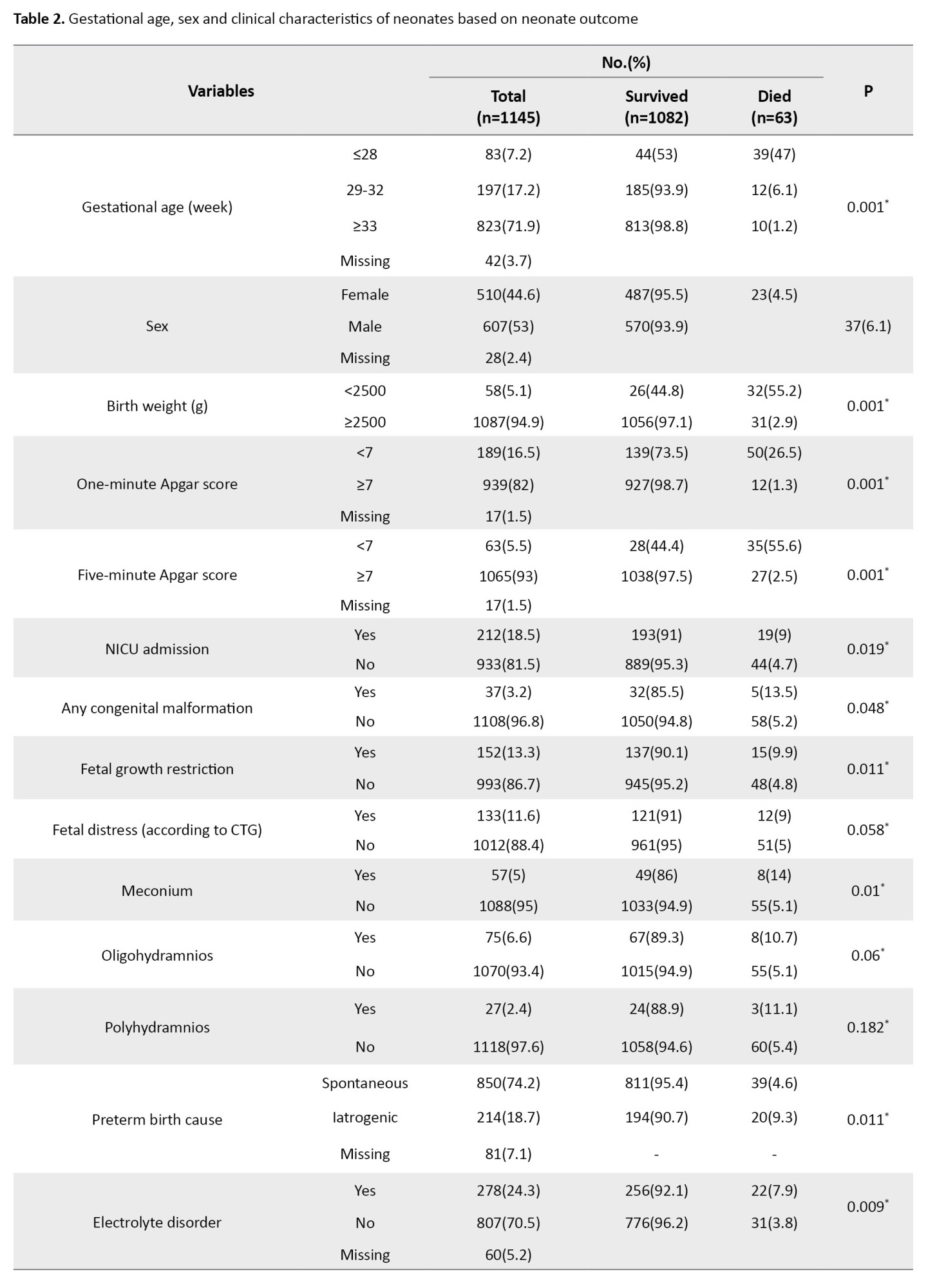
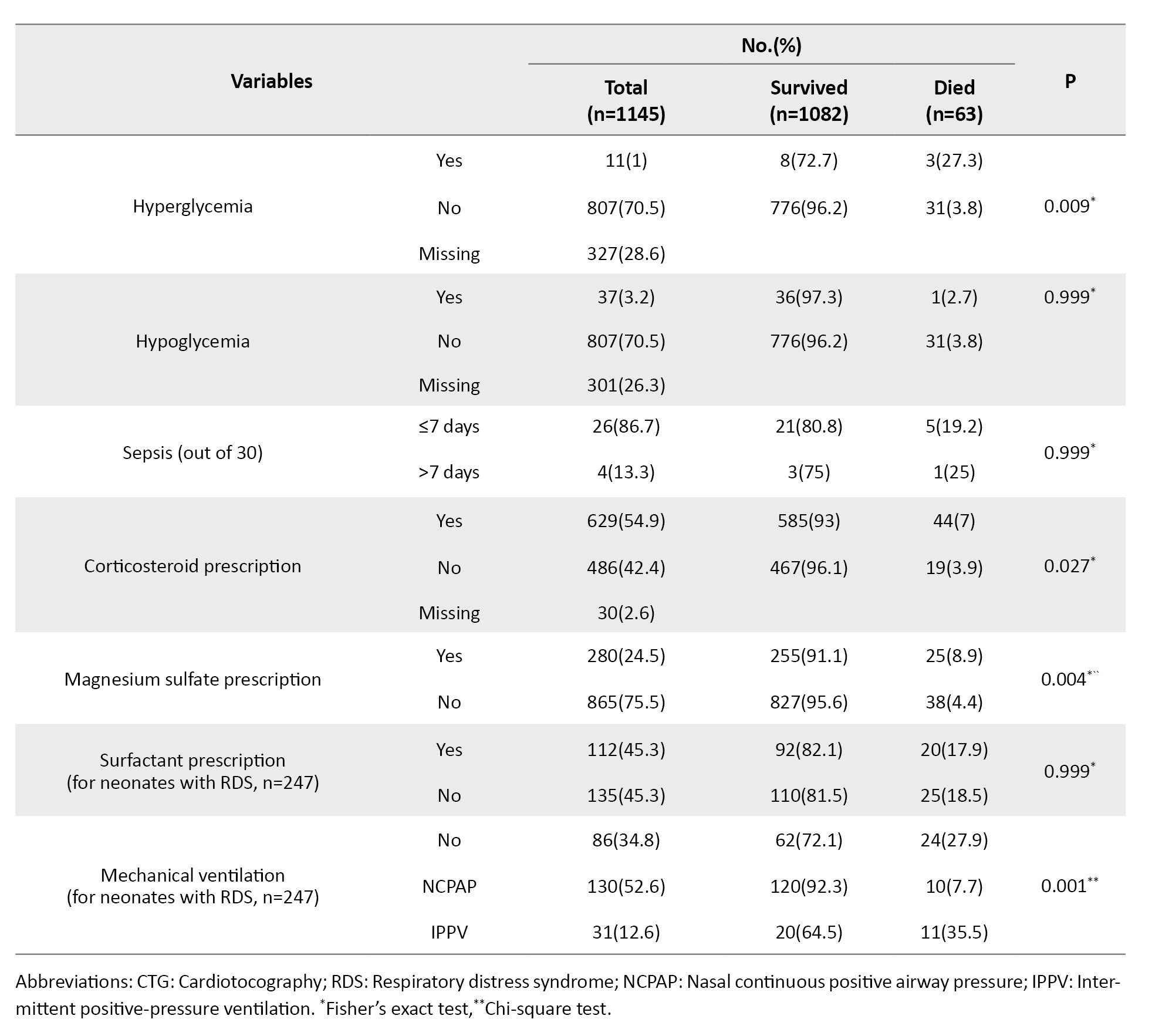
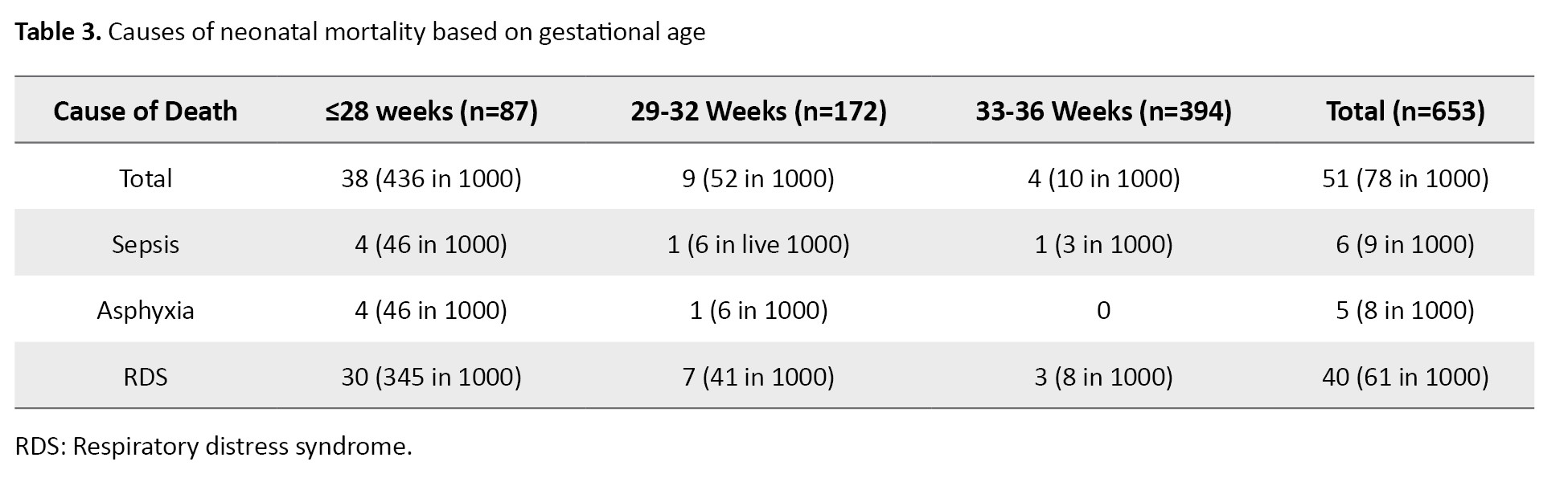
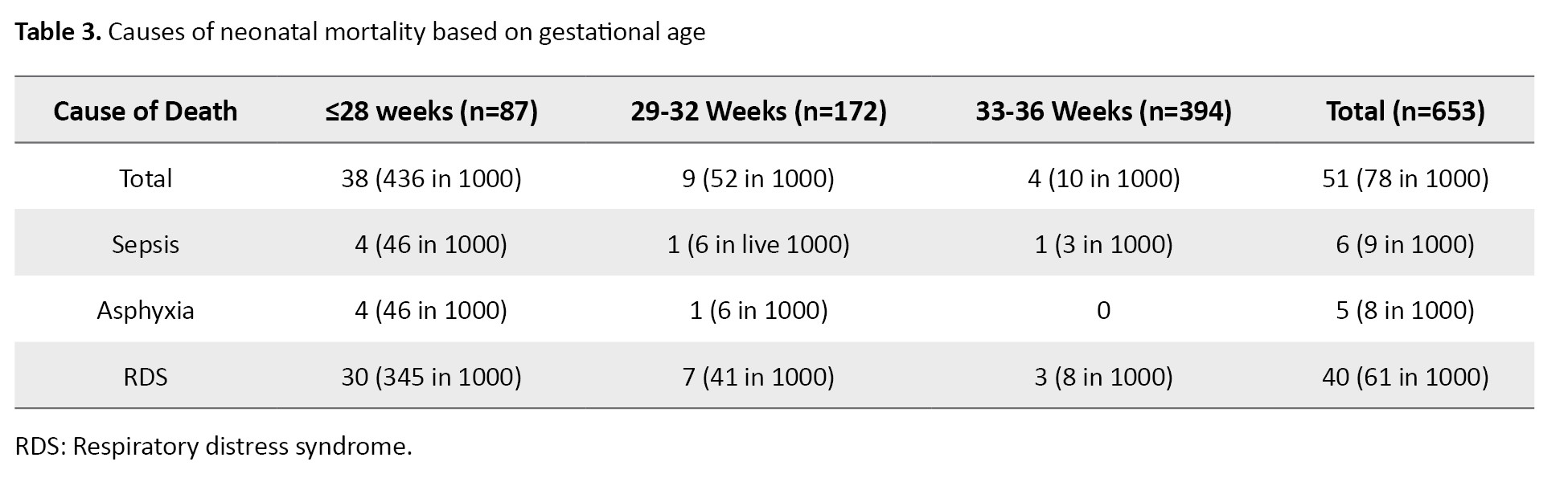
Of neonates who were admitted to the NICU, 83(39%) aged ≤28 weeks, and most of them (63.8%) were primarily admitted to the NICU. Of those who received NICU care, 20.8% died, while 93.3% of neonates who did not receive NICU care died. The most common diagnosis for neonates admitted to the premature neonates unit was icter (73%), while respiratory distress (72.2%) was the most common diagnosis for neonates admitted to NICU. The final diagnosis of 247(21.57%) neonates was respiratory distress (Table 3).
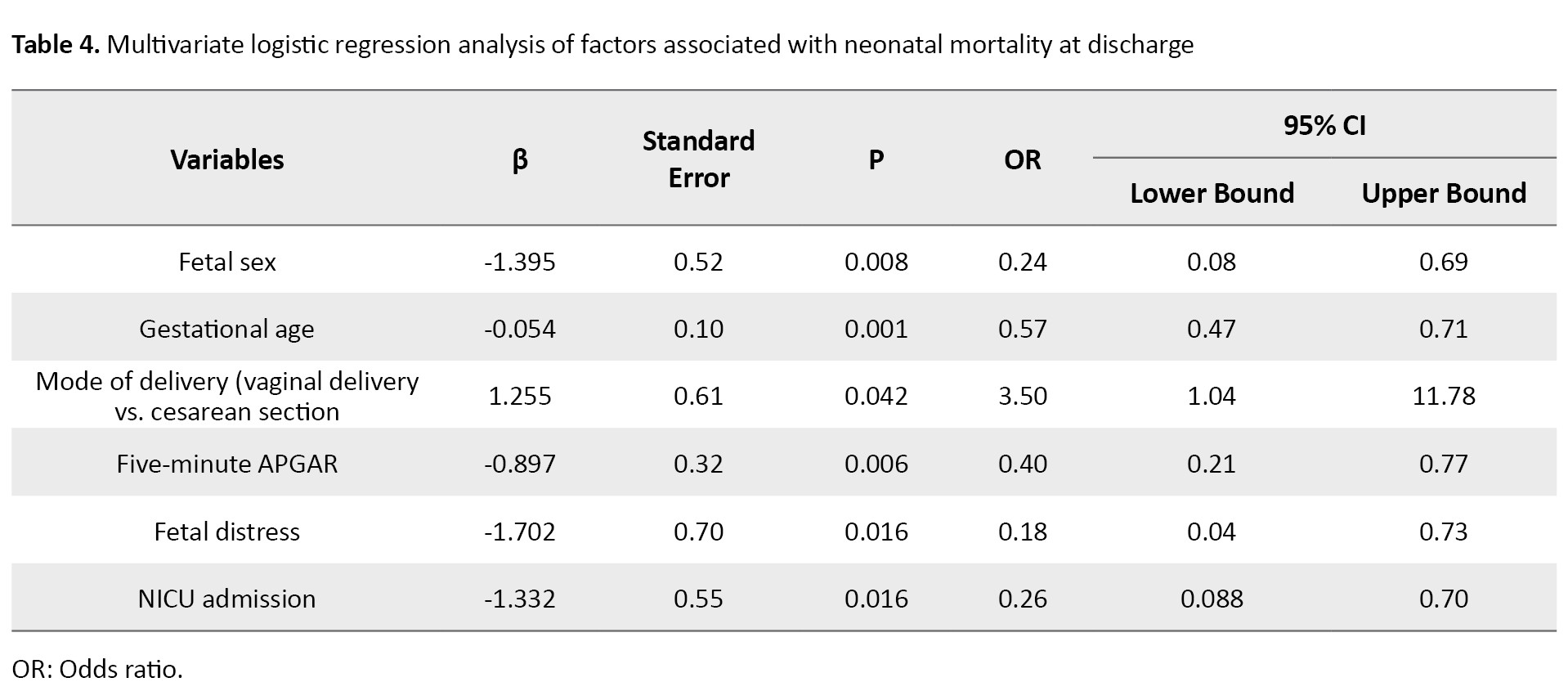
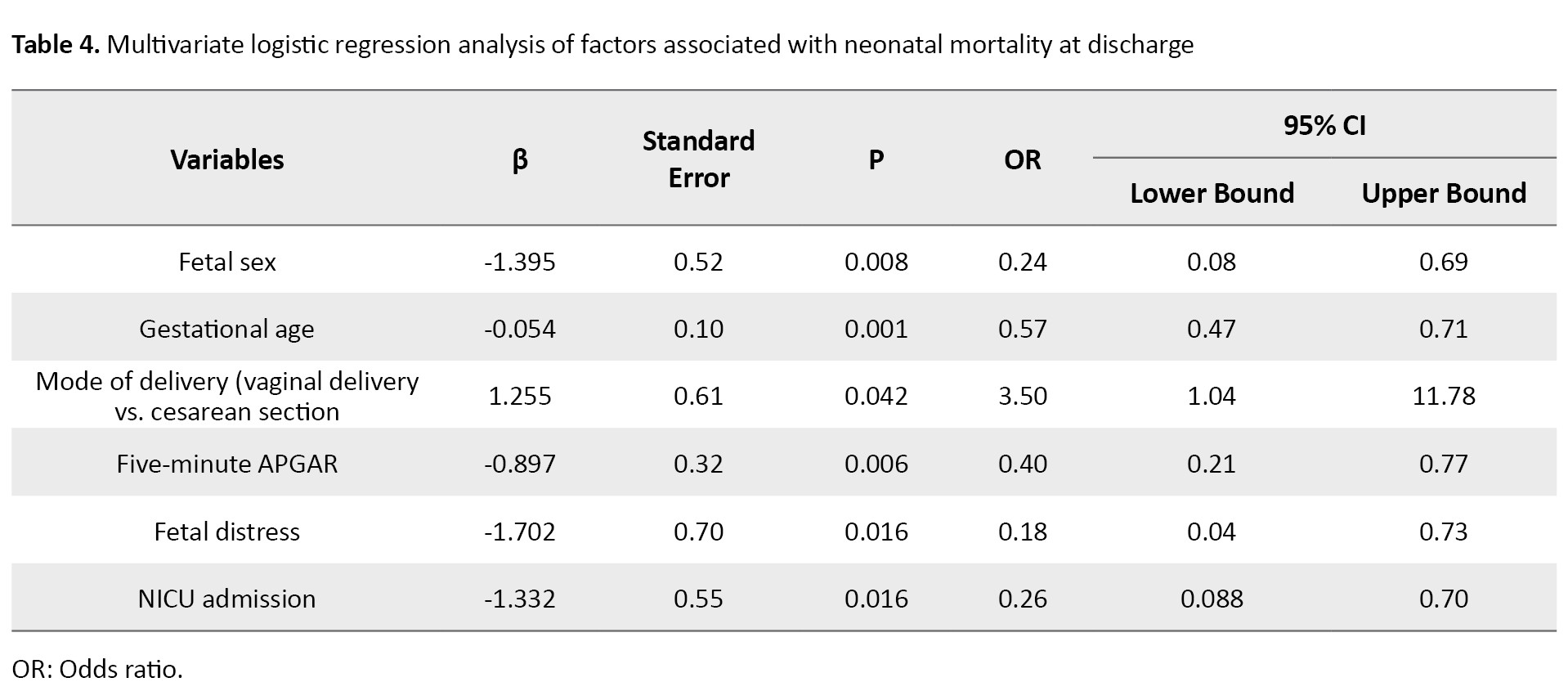
Variables with a P<0.2 in the univariate analysis were included in the logistic regression model. The results of analysis (Table 4) showed the significant association of fetal sex (OR=0.24, 95% CI; 0.08%, 0.69%, P=0.008), gestational age (OR=0.57, 95% CI; 0.47%, 0.71%, P=0.001), mode of delivery (OR= 3.50, 95% CI; 1.04%, 11.78%, P=0.042), five-minute Apgar score (OR= 0.40, 95% CI; 0.21%, 0.77%, P=0.006), fetal distress (OR=0.18, 95% CI; 0.04%, 0.73%, P=0.016), and NICU admission (OR=0.26, 95% CI; 0.08%, 0.78%, P=0.016) with neonatal mortality.
Discussion
In this study, we aimed to determine the factors related to neonatal mortality at discharge among neonates admitted to a tertiary care hospital in Rasht, north of Iran. We found the significant association of fetal sex, gestational age, mode of delivery, five-minute Apgar scores, fetal distress, and NICU admission with neonatal mortality at discharge.
The prevalence of neonatal mortality was 5.5% in premature neonates born during the study. A retrospective study in Ethiopia found a neonatal mortality rate of 5.7% in NICU neonates [17]. Considering that the neonatal mortality rate in our study among NICU neonates was 9%, it can be said that it is higher in our study than in Ethiopia, which can be due to the difference in facilities and conditions.
We found that male neonates died more than female neonates. Haghighi et al. did not find a significant difference between the male and female neonates concerning short-term mortality rates [18]. Aghai et al. reported that under the age of 7 days, the risks of stillbirths and mortality were higher among male infants than among female counterparts [19]. A recent systematic review suggested that few studies maintain a null association between fetal sex and neonatal mortality rate, suggesting that premature male neonates are at a higher risk of mortality after discharge than premature females [20], which should be taken into account by clinical managers in the NICU. In our study, for every one week increase in gestational age, the risk of neonatal mortality decreased. A recent study in Uganda showed that as birth weight increased, the mortality before discharge decreased [21].
We found that cesarean section reduced the risk of neonatal death; however, it may increase maternal deaths. Based on some studies, vaginal childbirth serves As a potential risk for neonatal mortality, and cesarean section serves as a preventive strategy for reducing neonatal mortality [22, 23]. However, a systematic review showed contradictory results [19]. In our study, it can be due to the effect of the gynecologists’ decision based on the probability of saving the neonate. In the study center, the risk of a cesarean section was imposed on mothers whose neonates had a higher chance of survival.
Our study demonstrated that higher five-minute Apgar score was associated with neonate survival. This finding is consistent with the findings of Cnattingius et al. [24]. Another study reported that reduced Apgar score may be better predictor of neonatal mortality in very young preterm infants than in older ones [25]. Since in the hospitals of Iran the Apgar score is calculated routinely for all newborns, those with low Apgar scores can be easily identified.
Our results indicated that neonates diagnosed with fetal distress were at higher risk of death compared to neonates without fetal distress. Hussain et al. found that more than two-thirds of patients had normal neonates with an Apgar score of 7 or more, indicating that abnormal cardiotocography alone should not be considered as an indication for cesarean section [26]. Moreover, our results showed that with admission to NICU, the chances of neonatal survival decreases. The fact that very sick neonates are admitted to the NICU can justifies this finding. However, we found that 20.8% of neonates younger than 28 weeks who received NICU care died, while the death rate for those who did not receive NICU care, was 93.3%. In the study center, not all neonates needing intensive care are admitted to the NICU due to the lack of sufficient NICU beds. Perinatal mortality possibly depends on the presence of a NICU, not on the population size or density. The number of NICU beds in Iran is below 500, far from international standards. In addition, there is unequal distribution of NICU beds nationwide [27]. Thus, resources need to be allocated to preventing mortality in premature neonates.
The neonatal mortality rate in our study was higher in neonates with iatrogenic preterm birth than in those with spontaneous preterm birth. This outcome is against the results of Chen et al., who found no difference in mortality between the two groups [28]. This discrepancy may be due to the difference in the ages of neonates. One unexpected finding in our study was that the neonatal mortality rate in neonates of mothers with diabetes was lower than in non-diabetic mothers. However, the effect of this variable was not significant in the regression model. A recent study found that pregestational diabetes was associated with higher odds of neonatal mortality [29].
This study had some limitations. Due to the lack of time, we could not follow the condition of the neonates until 28 days. Therefore, the findings about neonatal mortality rate may not be precise. In addition, some important predictors of neonatal mortality were not explored because of missing data and lack of information. Further studies, such as prospective studies, should be conducted to explore more maternal, neonatal, and treatment-related factors for neonatal mortality.
The present study showed that the frequency of neonatal mortality at discharge among preterm neonates in the study hospital in northern Iran is considerable, indicating a long way to increase child survival rate in Iran and reduce it to a minimum of 12 per 1,000 live births. Clinicians and policymakers in Iran should give special attention to the reported risk factors. The number of NICU beds is key to ensure that all mothers and infants have reasonable access to NICU services in case of emergency. Resources need to be allocated equally to prevent mortality in premature neonates.
Ethical Considerations
Compliance with ethical guidelines
Ethics approval was obtained from the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1399.302). Written informed consent for the use of medical data was signed by the neonates’ parents.
Funding
The study was funded by Guilan University of Medical Sciences, Rasht, Iran.
Authors' contributions
Conceptualization: Ali Roshani Tabrizi and Reza Sharafi; Methodology: Seyedeh Hajar Sharami and Mandana Mansour Ghanaei; Formal analysis and investigation: Seyedeh Fatemeh Dalil Heirati and Habib Eslami-Kenarsari; Original draft preparation: Shadi Sabetghadam; Review and editing: Shadi Sabetghadam and Seyedeh Hajar Sharami; Funding acquisition: Seyedeh Hajar Sharami; Supervision: Ali Roshani Tabrizi and Seyedeh Hajar Sharami. Final approval: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgments
The authors would like to thank the Deputy for Research of Guilan University of Medical Sciences for their financial and administrative support.
References
Premature birth is one of the most critical and challenging problems faced by obstetricians and gynecologists. It is associated with the neonatal death and lifelong complications, such as learning disabilities and visual, hearing, and cognitive problems, and is considered as a public health problem [1-4]. Premature birth also affects the economy, health care system, and society [5]. There is a clinical challenge in dealing with premature birth and reducing its complications due to problems in identifying preventable or modifiable factors. The overall prevalence of preterm birth is increasing worldwide, with about 15 million cases reported annually, leading to the deaths of about 1.1 million children [6]. Perinatal deaths account for about 7% of the global burden of disease [7]. It is estimated that globally four million neonatal deaths and stillbirths occur every year. Almost all these deaths occur in developing countries [8, 9] The neonatal death rate in Iran has been declined in past decades, but the decline has been slowed down, recently [10, 11].
Knowing the causes and predisposing factors of neonatal death can help identify, control, or reduce the death rate. Prematurity is a critical predisposing factor for neonatal death, which, despite the vast advances in midwifery science, is still a serious problem and requires extensive planning before birth and during pregnancy. Complications of prematurity, such as infection, respiratory distress syndrome, and intraventricular hemorrhage, are important causes of neonatal death [12]. Due to the progress in midwifery and quality of services dedicated to newborns, the survival rate of premature neonates has increased dramatically. Today, more than 95% of premature neonates who born before 28 weeks of pregnancy survive [13].
Many studies in Iran have reported the predictors of neonatal death [14, 15]. To the best of our knowledge, neonatal death rate and its associated factors in the tertiary hospitals are poorly documented, particularly at the institutional level. The ability of a premature neonate to survive is different among countries depending on hospital facilities. Therefore, the health centers that accept the admission of premature neonates should plan according to their conditions and decide whether these neonates survive or not, especially in the settings with limited beds in the neonatal intensive care units (NICUs). This study aims to investigate the factors related to death among premature neonates admitted to a tertiary care hospital in Rasht, north of Iran.
Materials and Methods
This is a retrospective cross-sectional study that was conducted at a tertiary care hospital in Rasht, north of Iran, from April to October 2022. The Pediatrics Department of this hospital has two major wards: Premature neonates unit and NICU. There are 50 beds in the two wards, where the NICU has 10 beds. Premature neonates in good general conditions receive care beside their mothers. The minimum sample size was determined 1126, by considering the premature birth prevalence of 7.1% According to the results of Rezaeian et al. [16], an error rate of 0.05, a test power of 0.80, and acceptable error rate of 0.015. All medical records of neonates admitted from May 2017 to March 2022 were examined. All neonates reach gestational age of 25-37 weeks whose information was registered by the neonatal registry form from May 2017 to March 2022 in the hospital were included. The newborns older than 28 days, out-of-hospital birth cases, and revisits were excluded.
The data were collected by two trained midwives and one experienced intern who had undergone the necessary training before the study. A data collection form was used to extract the demographic and maternal/fetal and treatment-related factors. The maternal/fetal factors included the mother’s age, obstetric history, mode of delivery, cause of preterm birth, pregnancy and childbirth complications, gestational age, birth weight, the admission unit, neonate’s sex, congenital malformation, and neonatal complications during hospitalization such as electrolyte disorder, hyperglycemia (blood glucose >200 mg/dL), hypoglycemia (blood glucose <47 mg/dL), sepsis, and abnormal brain ultrasound findings (e.g. germinal matrix hemorrhage, intraventricular hemorrhage, cerebral parenchymal hemorrhage, periventricular leukomalacia, hydrocephalus). The treatment-related factors included respiratory support, breastfeeding, the given treatment, and length of hospitalization.
The collected data entered into SPSS software, version 25 and were expressed as Mean±SD and number (percentage). Chi-square test and Fisher’s exact test were used to analyze the relationships between nominal variables. The factors related to fetal death were analyzed using multivariate logistic regression.
Results
There were 1161 premature neonates registered in the NICU and Premature Neonates Unit’s database, of whom 16 were excluded (five due to revisit, and 11 due to birth outside the hospital). Finally, the data of 1145 neonates were analyzed. Most of the neonates were 33 weeks and older (71.9%). The birth weight of most of them were above 2500 g (94.1%). In most cases, the preterm births happened spontaneously (74.2%). The mean age of mothers was 30.90±6.24 years. In most cases, the mode of delivery was cesarean section (77%), and in one-third of cases, the cause was repeated cesarean section (Table 1).
There were 63(5.5%) deaths during the study period. Among the deceased neonates, 27.7% died during the first 24 hours and 69.8% died during 48 hours. The youngest survived neonate was a 750-g female with a gestational age of 25 weeks. The mean gestational age of survived and dead neonates was about 34 and 28 weeks, respectively. The average time between birth and admission to the NICU was 23 hours (ranged from 22 min to 90 hours). Among neonates, 676(59%) were hospitalized for more than seven days. Eleven neonates had retinopathy of prematurity that needed treatment, 7 had grade-1 necrotizing enterocolitis (NEC), one had grade-2 NEC, and 73(6.4%) had abnormal brain ultrasound findings. Moreover, 346(30.2%) used mechanical ventilation, and 5.2% did not receive breastfeeding and were discharged with infant formula packs. Of all neonates, 212(18.5%) were admitted to NICU, of whom 19(9%) died (Table 2).
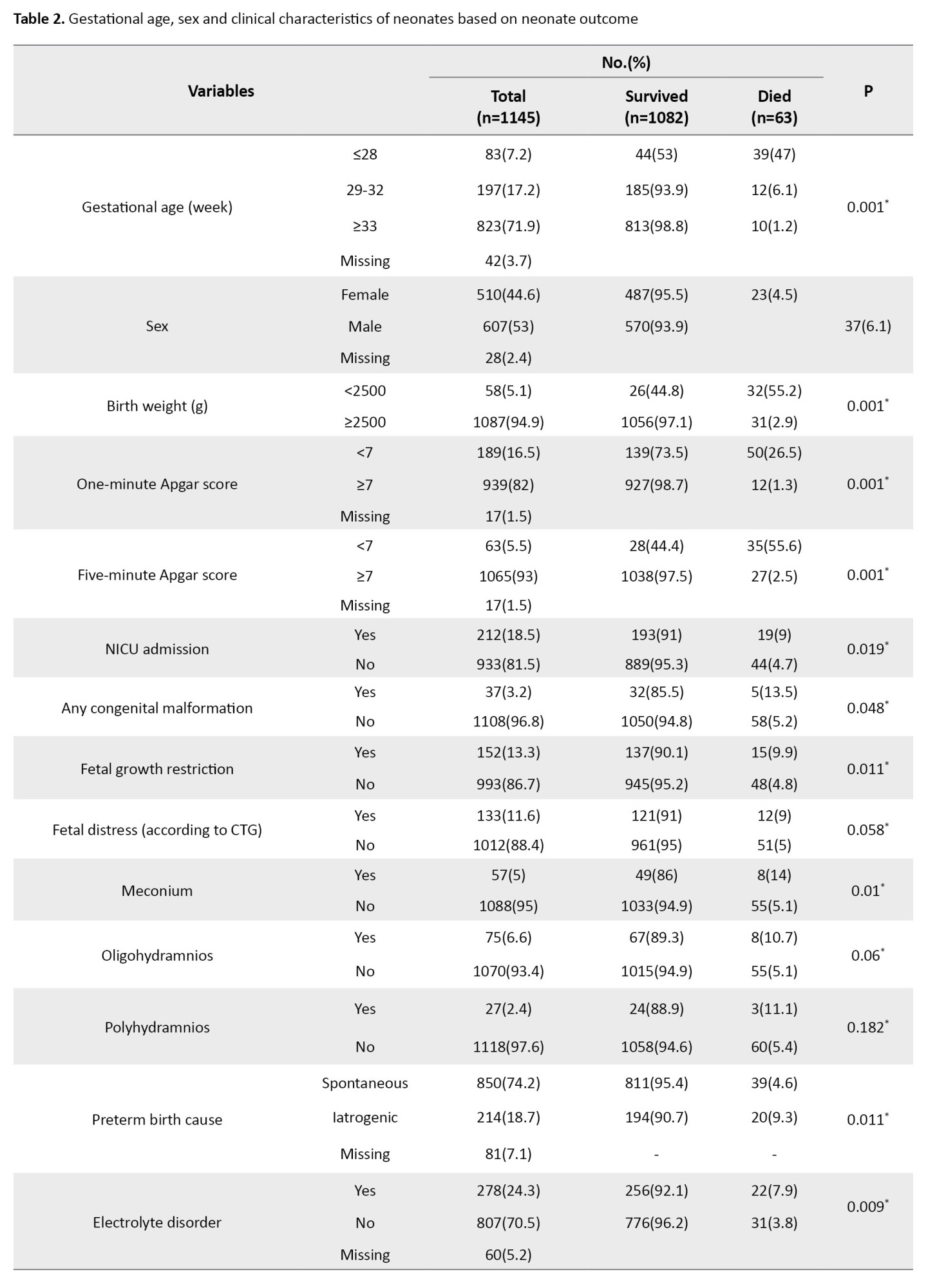
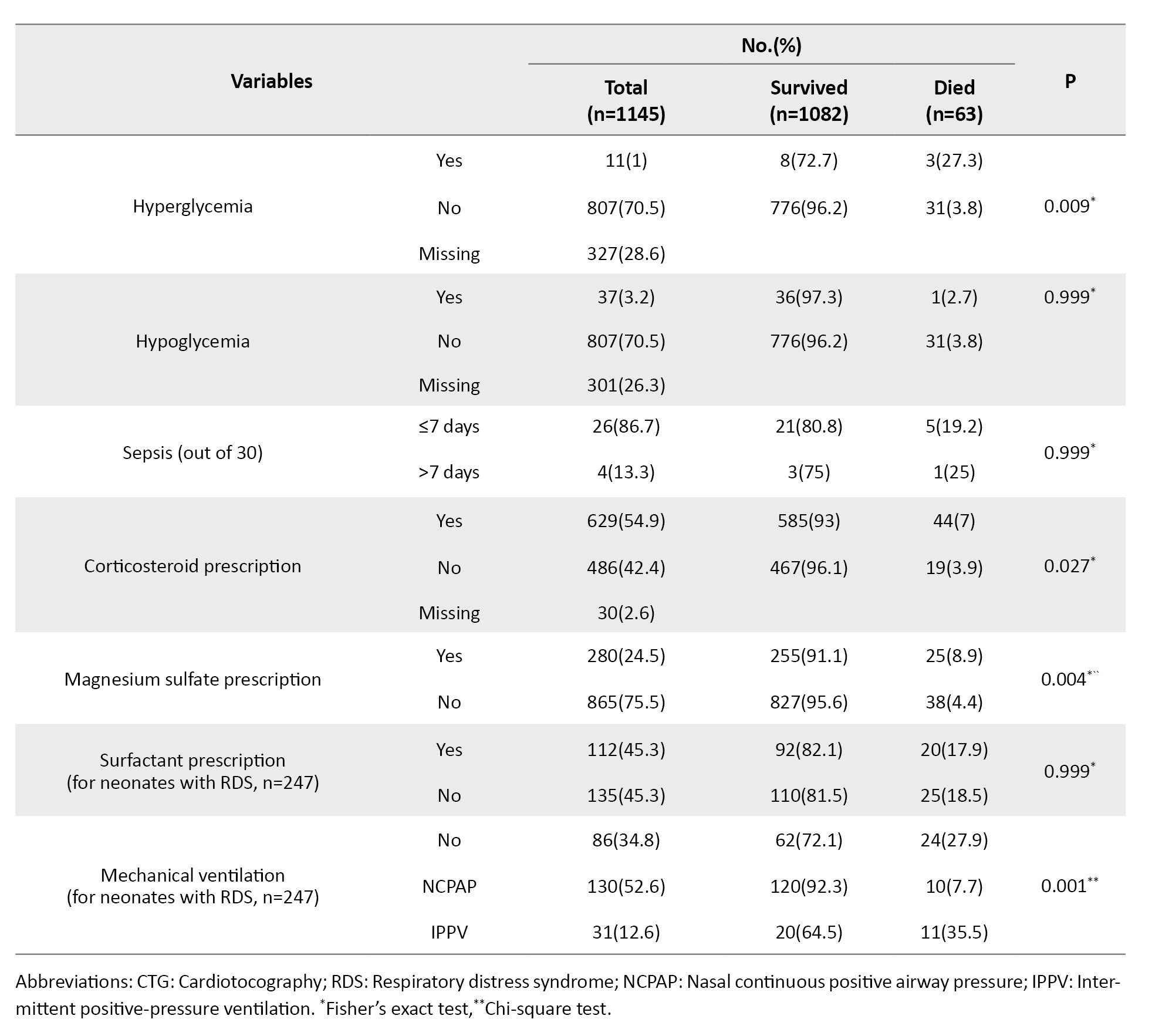
Of neonates who were admitted to the NICU, 83(39%) aged ≤28 weeks, and most of them (63.8%) were primarily admitted to the NICU. Of those who received NICU care, 20.8% died, while 93.3% of neonates who did not receive NICU care died. The most common diagnosis for neonates admitted to the premature neonates unit was icter (73%), while respiratory distress (72.2%) was the most common diagnosis for neonates admitted to NICU. The final diagnosis of 247(21.57%) neonates was respiratory distress (Table 3).
Variables with a P<0.2 in the univariate analysis were included in the logistic regression model. The results of analysis (Table 4) showed the significant association of fetal sex (OR=0.24, 95% CI; 0.08%, 0.69%, P=0.008), gestational age (OR=0.57, 95% CI; 0.47%, 0.71%, P=0.001), mode of delivery (OR= 3.50, 95% CI; 1.04%, 11.78%, P=0.042), five-minute Apgar score (OR= 0.40, 95% CI; 0.21%, 0.77%, P=0.006), fetal distress (OR=0.18, 95% CI; 0.04%, 0.73%, P=0.016), and NICU admission (OR=0.26, 95% CI; 0.08%, 0.78%, P=0.016) with neonatal mortality.
Discussion
In this study, we aimed to determine the factors related to neonatal mortality at discharge among neonates admitted to a tertiary care hospital in Rasht, north of Iran. We found the significant association of fetal sex, gestational age, mode of delivery, five-minute Apgar scores, fetal distress, and NICU admission with neonatal mortality at discharge.
The prevalence of neonatal mortality was 5.5% in premature neonates born during the study. A retrospective study in Ethiopia found a neonatal mortality rate of 5.7% in NICU neonates [17]. Considering that the neonatal mortality rate in our study among NICU neonates was 9%, it can be said that it is higher in our study than in Ethiopia, which can be due to the difference in facilities and conditions.
We found that male neonates died more than female neonates. Haghighi et al. did not find a significant difference between the male and female neonates concerning short-term mortality rates [18]. Aghai et al. reported that under the age of 7 days, the risks of stillbirths and mortality were higher among male infants than among female counterparts [19]. A recent systematic review suggested that few studies maintain a null association between fetal sex and neonatal mortality rate, suggesting that premature male neonates are at a higher risk of mortality after discharge than premature females [20], which should be taken into account by clinical managers in the NICU. In our study, for every one week increase in gestational age, the risk of neonatal mortality decreased. A recent study in Uganda showed that as birth weight increased, the mortality before discharge decreased [21].
We found that cesarean section reduced the risk of neonatal death; however, it may increase maternal deaths. Based on some studies, vaginal childbirth serves As a potential risk for neonatal mortality, and cesarean section serves as a preventive strategy for reducing neonatal mortality [22, 23]. However, a systematic review showed contradictory results [19]. In our study, it can be due to the effect of the gynecologists’ decision based on the probability of saving the neonate. In the study center, the risk of a cesarean section was imposed on mothers whose neonates had a higher chance of survival.
Our study demonstrated that higher five-minute Apgar score was associated with neonate survival. This finding is consistent with the findings of Cnattingius et al. [24]. Another study reported that reduced Apgar score may be better predictor of neonatal mortality in very young preterm infants than in older ones [25]. Since in the hospitals of Iran the Apgar score is calculated routinely for all newborns, those with low Apgar scores can be easily identified.
Our results indicated that neonates diagnosed with fetal distress were at higher risk of death compared to neonates without fetal distress. Hussain et al. found that more than two-thirds of patients had normal neonates with an Apgar score of 7 or more, indicating that abnormal cardiotocography alone should not be considered as an indication for cesarean section [26]. Moreover, our results showed that with admission to NICU, the chances of neonatal survival decreases. The fact that very sick neonates are admitted to the NICU can justifies this finding. However, we found that 20.8% of neonates younger than 28 weeks who received NICU care died, while the death rate for those who did not receive NICU care, was 93.3%. In the study center, not all neonates needing intensive care are admitted to the NICU due to the lack of sufficient NICU beds. Perinatal mortality possibly depends on the presence of a NICU, not on the population size or density. The number of NICU beds in Iran is below 500, far from international standards. In addition, there is unequal distribution of NICU beds nationwide [27]. Thus, resources need to be allocated to preventing mortality in premature neonates.
The neonatal mortality rate in our study was higher in neonates with iatrogenic preterm birth than in those with spontaneous preterm birth. This outcome is against the results of Chen et al., who found no difference in mortality between the two groups [28]. This discrepancy may be due to the difference in the ages of neonates. One unexpected finding in our study was that the neonatal mortality rate in neonates of mothers with diabetes was lower than in non-diabetic mothers. However, the effect of this variable was not significant in the regression model. A recent study found that pregestational diabetes was associated with higher odds of neonatal mortality [29].
This study had some limitations. Due to the lack of time, we could not follow the condition of the neonates until 28 days. Therefore, the findings about neonatal mortality rate may not be precise. In addition, some important predictors of neonatal mortality were not explored because of missing data and lack of information. Further studies, such as prospective studies, should be conducted to explore more maternal, neonatal, and treatment-related factors for neonatal mortality.
The present study showed that the frequency of neonatal mortality at discharge among preterm neonates in the study hospital in northern Iran is considerable, indicating a long way to increase child survival rate in Iran and reduce it to a minimum of 12 per 1,000 live births. Clinicians and policymakers in Iran should give special attention to the reported risk factors. The number of NICU beds is key to ensure that all mothers and infants have reasonable access to NICU services in case of emergency. Resources need to be allocated equally to prevent mortality in premature neonates.
Ethical Considerations
Compliance with ethical guidelines
Ethics approval was obtained from the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1399.302). Written informed consent for the use of medical data was signed by the neonates’ parents.
Funding
The study was funded by Guilan University of Medical Sciences, Rasht, Iran.
Authors' contributions
Conceptualization: Ali Roshani Tabrizi and Reza Sharafi; Methodology: Seyedeh Hajar Sharami and Mandana Mansour Ghanaei; Formal analysis and investigation: Seyedeh Fatemeh Dalil Heirati and Habib Eslami-Kenarsari; Original draft preparation: Shadi Sabetghadam; Review and editing: Shadi Sabetghadam and Seyedeh Hajar Sharami; Funding acquisition: Seyedeh Hajar Sharami; Supervision: Ali Roshani Tabrizi and Seyedeh Hajar Sharami. Final approval: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgments
The authors would like to thank the Deputy for Research of Guilan University of Medical Sciences for their financial and administrative support.
References
- Kvalvik LG, Wilcox AJ, Skjærven R, Østbye T, Harmon QE. Term complications and subsequent risk of preterm birth: Registry based study. BMJ. 2020; 369:m1007 [DOI:10.1136/bmj.m1007]
- Siffel C, Hirst AK, Sarda SP, Chen H, Ferber J, Kuzniewicz MW, Li DK. The clinical burden of extremely preterm birth in a large medical records database in the United States: Complications, medication use, and healthcare resource utilization. J Matern Fetal Neonatal Med. 2022; 35(26):10271-8. [DOI:10.1080/14767058.2022.2122035]
- Tso WW, Ho FK, Coghill D, Lee TM, Wang Y, Lee SL, et al. Preterm postnatal complications and risk of attention-deficit/hyperactivity disorder. Dev Med Child Neurol. 2023; 65(3):358-66. [Link]
- de Paula Eduardo JAF, de Rezende MG, Menezes PR, Del-Ben CM. Preterm birth as a risk factor for postpartum depression: A systematic review and meta-analysis. J Affect Disord. 2019; 259:392-403. [DOI:10.1016/j.jad.2019.08.069]
- Ahmadzadeh N, Rezapour A, Ghanavatinejad Z, Nouhi M, Karimi S, Saravani A, et al. Estimation of economic burden of preterm and premature births in Iran. Med J Islam Repub Iran. 2017; 31(1):78. [DOI:10.14196/mjiri.31.78]
- Althabe F, March of Dimes Birth Defects Foundation. Born too soon: The global action report on preterm birth. Geneva: World Health Organization. 2012. [Link]
- Scott J. Stillbirths: Breaking the silence of a hidden grief. The Lancet. 2011; 377(9775):1386-8. [DOI:10.1016/S0140-6736(11)60107-4]
- Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every Newborn: Progress, priorities, and potential beyond survival. The lancet. 2014; 384(9938):189-205. [DOI:10.1016/S0140-6736(14)60496-7]
- Lincetto O, Banerjee A. World prematurity day: Improving survival and quality of life for millions of babies born preterm around the world. Am J Physiol Lung Cell Mol Physiol. 2020; 319(5):L871-4. [DOI:101152/ajplung004792020]
- Habibelahi A, Heidarzadeh M, Abdollahi L, Taheri M, Ghaffari-Fam S, Vakilian R, et al. Clinical cause of neonatal mortality in Iran: Analysis of the national Iranian maternal and neonatal network. BMJ Paediatrics Open. 2024; 8(1):1-7. [DOI:10.1136%2Fbmjpo-2023-002315]
- Khazaei S, Najafi F, Armanmehr V, Hajipour M, Karami M, Rezaeian S. Trend analysis of mortality rates for leading causes of death among under-five children in Iran, 2000-2015. J Compr Pediatr. 2019; 10(2):e86902. [DOI:10.5812/compreped.86902]
- de Paula Fiod Costa H, de Paula Fiod Costa E. Neonatal complications of prematurity. In: Augusto Moreira de Sá R, Borges da Fonseca E, editors. Perinatology: Evidence-based best practices in perinatal medicine. Berlin: Springer; 2022. [DOI:10.1007/978-3-030-83434-0_58]
- Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Mortality, in-hospital morbidity, care practices, and 2-year outcomes for extremely preterm infants in the US, 2013-2018. Obstetric Anesthesia Digest. 2022; 42(4):184-5. [DOI:10.1097/01.aoa.0000891644.03402.e8]
- Valadbeigi T, Dara N, Tabatabaee H, Tajalli S, Etemad K, Hosseini A, et al. Maternal risk factors of neonatal mortality in iran: a case-control study. Int J Pediatr. 2020; 8(2):10865-74. [DOI:10.22038/ijp.2019.44502.3683]
- Daemi A, Ravaghi H, Jafari M. Risk factors of neonatal mortality in Iran: A systematic review. Med J Islam Repub Iran. 2019; 33:87. [DOI:10.34171%2Fmjiri.33.87] [PMID]
- Rezaeian M, Goujani R, Sheikh Fathollahi M, Vaziri Nejad R, Manshori A, Razi S. [A comparative study on prevalence of preterm birth and low birth weight in Iranians and Afghans races in Rafsanjan Nik-nafs hospital in 2011-2012 (Persian)]. J Rafsanjan Univ Med Sci. 2014; 13(1):67-82. 22. [Link]
- Belay DM, Worku WZ, Wondim A, Hailemeskel HS, Bayih WA. Predictors of survival among preterm neonates admitted to Felege Hiwot comprehensive specialized Hospital, Northwest Ethiopia. Front Pediatr. 2022; 10:800300. [DOI:10.3389/fped.2022.800300]
- Haghighi L, Nojomi M, Mohabbatian B, Najmi Z. Survival predictors of preterm neonates: Hospital based study in Iran (2010-2011). Iran J Reprod Med. 2013; 11(12):957. [PMID] [PMCID]
- Aghai ZH, Goudar SS, Patel A, Saleem S, Dhaded SM, Kavi A, et al. Gender variations in neonatal and early infant mortality in India and Pakistan: A secondary analysis from the global network maternal newborn health registry. Reprod Health. 2020; 17(3):1-11. [DOI:10.1186/s12978-020-01028-0]
- Vu HD, Dickinson C, Kandasamy Y. Sex difference in mortality for premature and low birth weight neonates: A systematic review. Am J Perinatol. 2018;35(08):707-15. [DOI:10.1055/s-0037-1608876]
- Nsubuga R, Rujumba J, Nyende S, Kisaka S, Idro R, Nankunda J. Predictors of mortality among low birth weight neonates after hospital discharge in a low-resource setting: A case study in Uganda. Plos one. 2024; 19(6):e0303454. [DOI:10.1371/journal.pone.0303454]
- Gahlawat V, Chellani H, Saini I, Gupta S. Predictors of mortality in premature babies with respiratory distress syndrome treated by early rescue surfactant therapy. J Neonatal Perinatal Med. 2021; 14(4):547-52. [DOI:10.3233/NPM-190244]
- Iyanda AE, Osayomi T. Association between childbirth modes and neonatal and maternal deaths using a negative binomial model. Womens Reprod Health. 2019; 6(2):128-40. [DOI:10.1080/23293691.2019.1601905]
- Cnattingius S, Johansson S, Razaz N. Apgar score and risk of neonatal death among preterm infants. New Eng J Med. 2020; 383(1):49-57. [DOI:10.1056/NEJMoa1915075]
- Cnattingius S, Norman M, Granath F, Petersson G, Stephansson O, Frisell T. Apgar score components at 5 minutes: Risks and prediction of neonatal mortality. Paediatr Perinat Epidemiol. 2017; 31(4):328-37. [DOI:10.1111/ppe.12360]
- Hussain SS, Fatima SS, Shafqat T, Qazi Q. Fetal outcome after cesarean section preformed for fetal distress based on abnormal cardiotocography. J Med Sci. 2021; 29(01):13-6. [DOI:10.52764/jms.21.29.1.04]
- Meskarpour-Amiri M, Mehdizadeh P, Barouni M, Dopeykar N, Ramezanian M. Assessment the trend of inequality in the distribution of intensive care beds in Iran: Using GINI index. Glob J Health Sci. 2014; 6(6):28. [DOI:10.5539/gjhs.v6n6p28]
- Chen X, Zhang X, Li W, Li W, Wang Y, Zhang S, et al. Iatrogenic vs. spontaneous preterm birth: A retrospective study of neonatal outcome among very preterm infants. Front Neurol. 2021; 12:649749. [DOI:10.3389/fneur.2021.649749]
- Battarbee AN, Venkatesh KK, Aliaga S, Boggess KA. The association of pregestational and gestational diabetes with severe neonatal morbidity and mortality. J Perinatol. 2020; 40(2):232-9. [DOI:10.1038/s41372-019-0516-5]
Article Type : Research |
Subject:
Special
Received: 2023/08/6 | Accepted: 2024/05/11 | Published: 2024/10/1
Received: 2023/08/6 | Accepted: 2024/05/11 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |