Mon, Dec 1, 2025
Volume 35, Issue 1 (1-2025)
JHNM 2025, 35(1): 1-10 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Afshar F, Pakseresht S, Jafarzadeh-Kenarsari F, Maroufizadeh S. Comparison of Childbirth Experience and Related Factors in Primiparous Women With Normal Vaginal Delivery and Cesarean Section From Northern Iran. JHNM 2025; 35 (1) :1-10
URL: http://hnmj.gums.ac.ir/article-1-2200-en.html
URL: http://hnmj.gums.ac.ir/article-1-2200-en.html
1- Midwifery (MSc), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Professor, Department of Midwifery, Social Determinants of Health Research Center (SDHRC), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,paksersht@yahoo.com
3- Associate Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
2- Professor, Department of Midwifery, Social Determinants of Health Research Center (SDHRC), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Associate Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 525 kb]
(480 Downloads)
| Abstract (HTML) (779 Views)
Full-Text: (423 Views)
Introduction
Childbirth is one of the most challenging physiological and psychological events in a woman’s life [1]. A positive childbirth experience has benefits such as improved mother-infant bonding, self-esteem, and quality of life [2, 3]. In contrast, a negative childbirth experience has consequences, including post-traumatic stress disorder, decreased breastfeeding rates, impaired mother-infant relationships, fear of childbirth, and an increased tendency to have elective Cesarean sections (CSs) in future pregnancies [4, 5, 6]. Therefore, one of the important factors for deciding on subsequent pregnancies is the type of experience gained from previous childbirth [7]. A systematic review conducted in different countries showed that 10-33% of women reported childbirth as a negative experience [8].
Today, the childbirth experience has become an important factor in assessments of health care delivery for mothers, emphasizing the active role of childbirth in this process [9]. Previous studies have shown that several factors affect mothers’ experiences of the postpartum period, including sociodemographic characteristics (race, age, social status), maternal expectations, prenatal education, maternal awareness, pain perception, type of delivery, unforeseen complications, medical interventions, transfer of the infant to the neonatal intensive care unit, and receiving adequate support during labor and delivery from medical staff [10, 11]. Also, factors such as a sense of security, personal support, midwifery care, information provided to the mother, and her participation in decision-making affect the childbirth experience [12].
Despite the identification of many factors that have a negative or positive effect on the childbirth experience, the impact of these factors on women’s experiences in different situations and societies is still not comprehensively and accurately known [13, 14]. The cultural, economic, and social differences necessitate the need to examine human experiences in each society separately [15]. In Iran, few studies have investigated the childbirth experience and the related factors in mothers. A study in this field was conducted in Rasht City on hospitalized mothers after childbirth and the results showed that effective communication between mothers and healthcare providers and the mother’s right to participate in labor have a positive impact on the birth experience [16]. Other studies in Iran have reported that assessing childbirth experiences immediately after delivery can lead to women’s false reporting of positive childbirth experiences due to the delivery of a healthy baby [12, 17].
Therefore, considering the importance of mothers’ childbirth experience and its outcomes, the impact of childbirth experience on maternal health and child development, and the desire to have children in case of a positive childbirth experience, it seems necessary to conduct a study to compare childbirth experience and related factors in primiparous women with normal vaginal delivery (NVD) and CS.
Materials and Methods
This is an analytical cross-sectional study conducted in 2022. The study population consists of all primiparous women with NVD or CS referring to comprehensive health centers in Rasht, Iran. Inclusion criteria were willingness to participate in the study, singleton pregnancy, uncomplicated and low-risk pregnancy, cephalic presentation, term pregnancy (37 weeks or more), and experiencing all or part of the active phase of labor and painful uterine contractions. Women with elective CS (women who did not go into labor), women who had a stillborn baby, or a baby admitted to the neonatal intensive care unit were not included in the study. A multi-stage sampling method was used. In the first, second, and third stages, stratified sampling, cluster sampling, and convenience sampling methods were used, respectively. In the first stage, Rasht was divided into four regions (north, south, west, and east) and each region was considered as a stratum. In the second stage, the comprehensive health centers (clusters) were selected within each stratum by simple random sampling. Finally, in the third stage, a convenience sampling method was used to choose women from each center. Considering that, in linear regression analyses, at least 20 samples should be selected for each independent variable (predictor) [18, 19] and given that there were 14 independent variables in the present study, at least 300 primiparous women were selected and put in two groups: 150 with NVD and 150 with CS.
The data collection tools were two questionnaires. The first questionnaire surveys socio-demographic information (age, place of residence, woman’s educational level, husband’s educational level, woman’s occupation, husband’s occupation, income level, insurance status, type of hospital) and obstetric characteristics (type of delivery, type of pregnancy, gender of the baby, gestational age with emphasis on sonography and date of last menstrual period, and history of participation in childbirth education classes). This questionnaire was used after determining its face validity based on the opinions of five faculty members of the School of Nursing and Midwifery. The second tool was the childbirth experience questionnaire (CEQ) developed by Dencker et al. [12]. It contains 22 items that measure the childbirth experience of primiparous women up to one month after delivery. This questionnaire includes four domains: Own capacity (8 items), professional support (5 items), perceived safety (6 items), and participation (3 items). Each item is scored using a 4-point Likert scale as 1 (totally agree), 2 (mostly agree), 3 (mostly disagree), and 4 (totally disagree), except for two items from the own capacity domain and one item from the perceived safety domain, referring to perceived pain, sense of control and sense of security, which are assessed using a visual analog scale (VAS), rated as 1 (score 0–40), 2 (score 41–60), 3 (score 61–80), and 4 (score 81–100). The scoring of negatively worded items is reversed. A higher score indicates a better childbirth experience. The Persian version of the CEQ has been validated by Kazemi et al. [20].
After obtaining official permission and receiving the code of ethics from the Ethics Committee of Guilan University of Medical Sciences, informed consent was obtained from the samples after emphasizing the confidentiality of their information and explaining the study objectives to them. The researcher collected data from the women within one month after delivery when women visited comprehensive health centers for postpartum care.
Data analysis was performed using descriptive and inferential statistics. The descriptive statistics included Mean±SD, frequency, and percentage. Inferential statistics included independent t-test, chi-square test, and Cochran-Armitage test (to compare sociodemographic/obstetric characteristics of two NVD and CS groups). The Shapiro-Wilks test was used to examine the assumption of normality of the CEQ score in primiparous women. In univariate analyses, independent t-test, one-way analysis of variance, and Pearson correlation test were used to examine the relationship between the CEQ score and sociodemographic/obstetric characteristics. In multivariate analyses, the multiple linear regression analysis was used to determine factors associated with the total CEQ score. Data were analyzed in SPSS software, version 16, and the significance level was set at 0.05.
Results
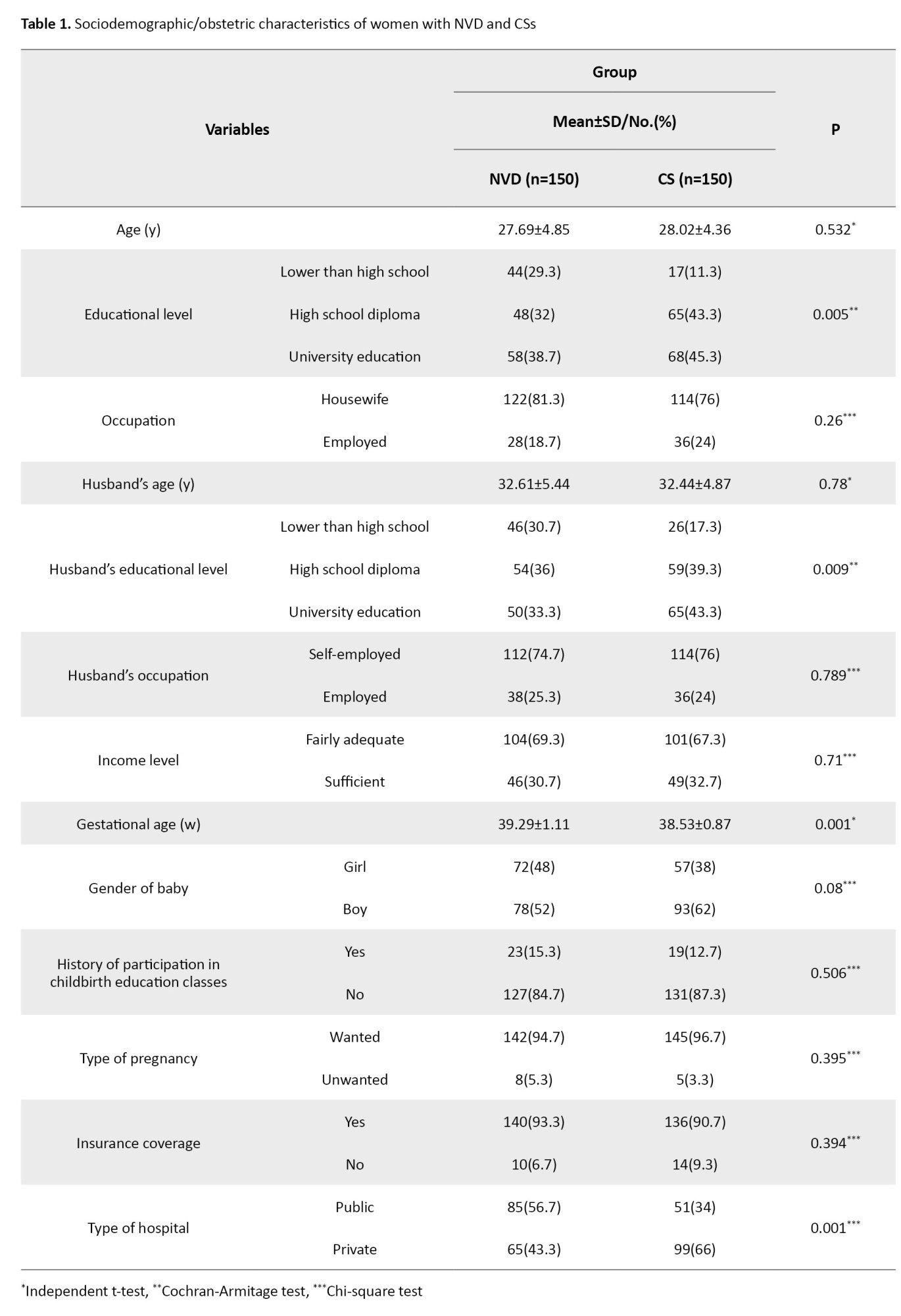
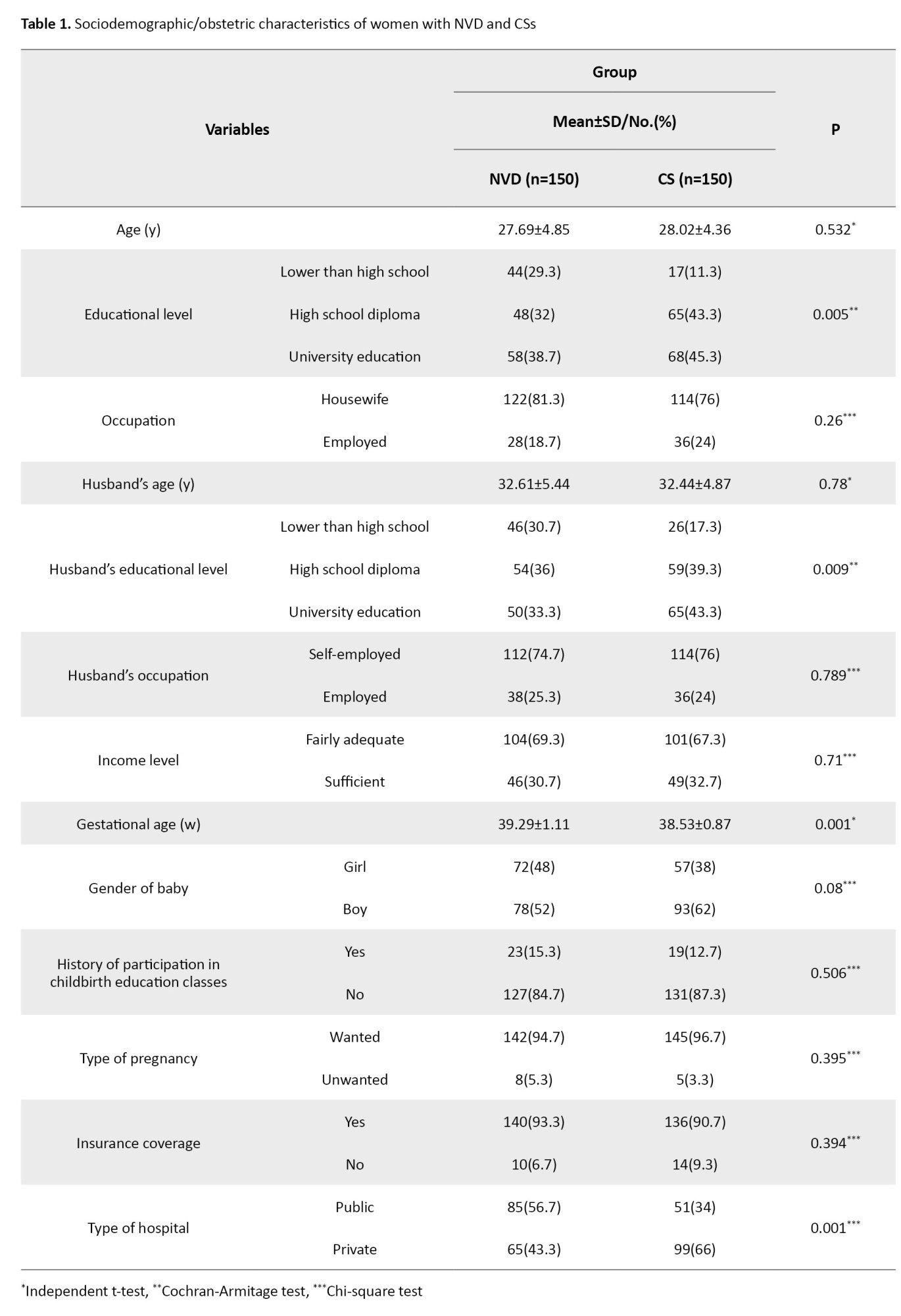
The mean age of women and their husbands was 27.85±4.61 and 32.52±5.15 years, respectively. The level of education of 42% of women and 38.3% of their husbands was university education. Also, 78.7% of women were housewives and 75.3% of their husbands were self-employed. Based on the results, the education of women with CS was significantly higher than that of women with NVD (P=0.005). A similar finding was also observed based on their husbands’ education level (P=0.009). Gestational age in women with CS was significantly lower than in women with NVD (P=0.001). Also, the percentage of deliveries in private hospitals in women with CS was significantly higher than in women with NVD (P=0.001). These results are shown in Table 1.
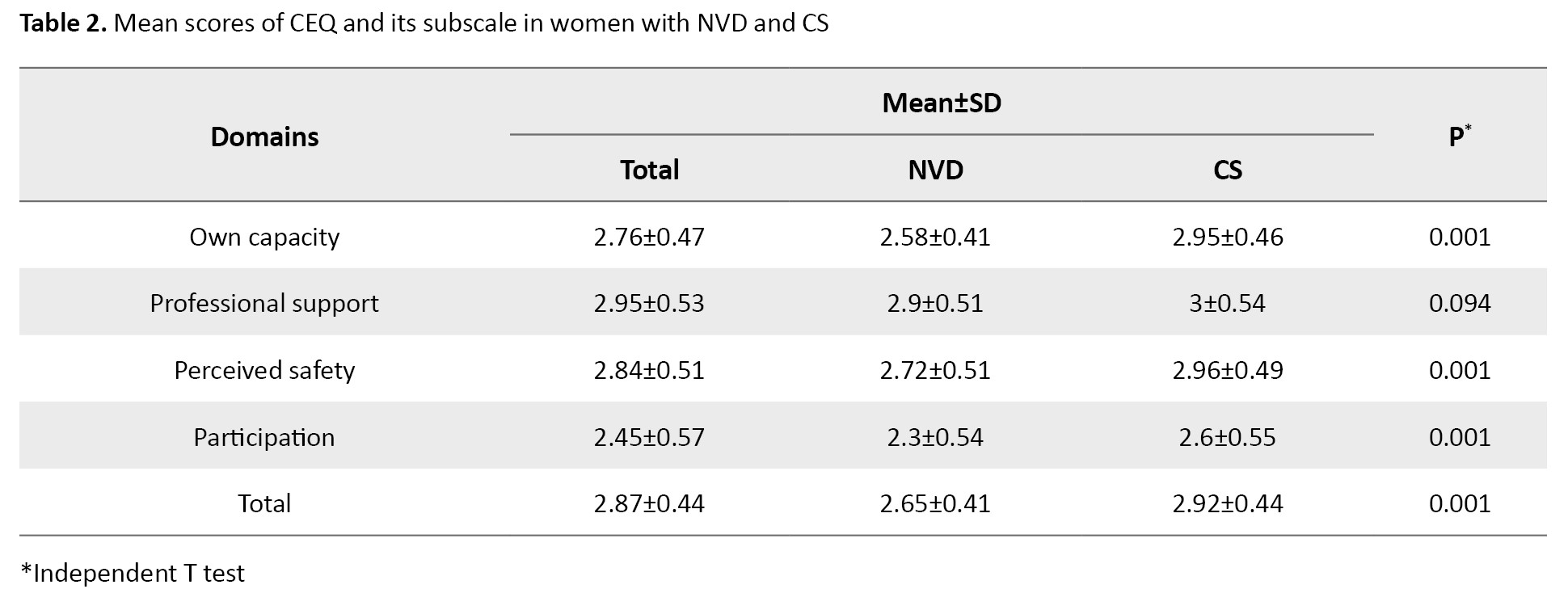
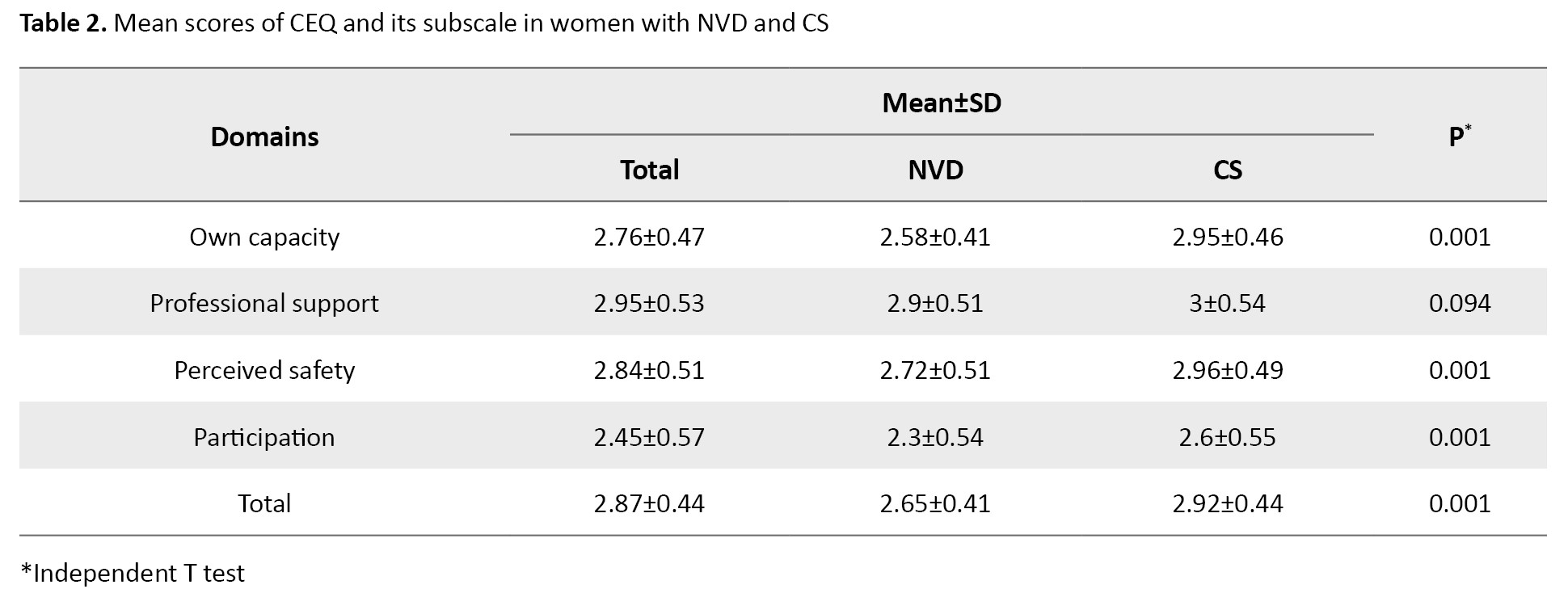
The mean total CEQ score was significantly higher in women with CS than in women with NVD (p=0.001). Also, the mean scores for the domains of own capacity, perceived safety, and participation were significantly higher in women with CS than those with NVD (P=0.001). Although the mean score for the professional support domain was higher in women with CS, the difference was not statistically significant (Table 2).
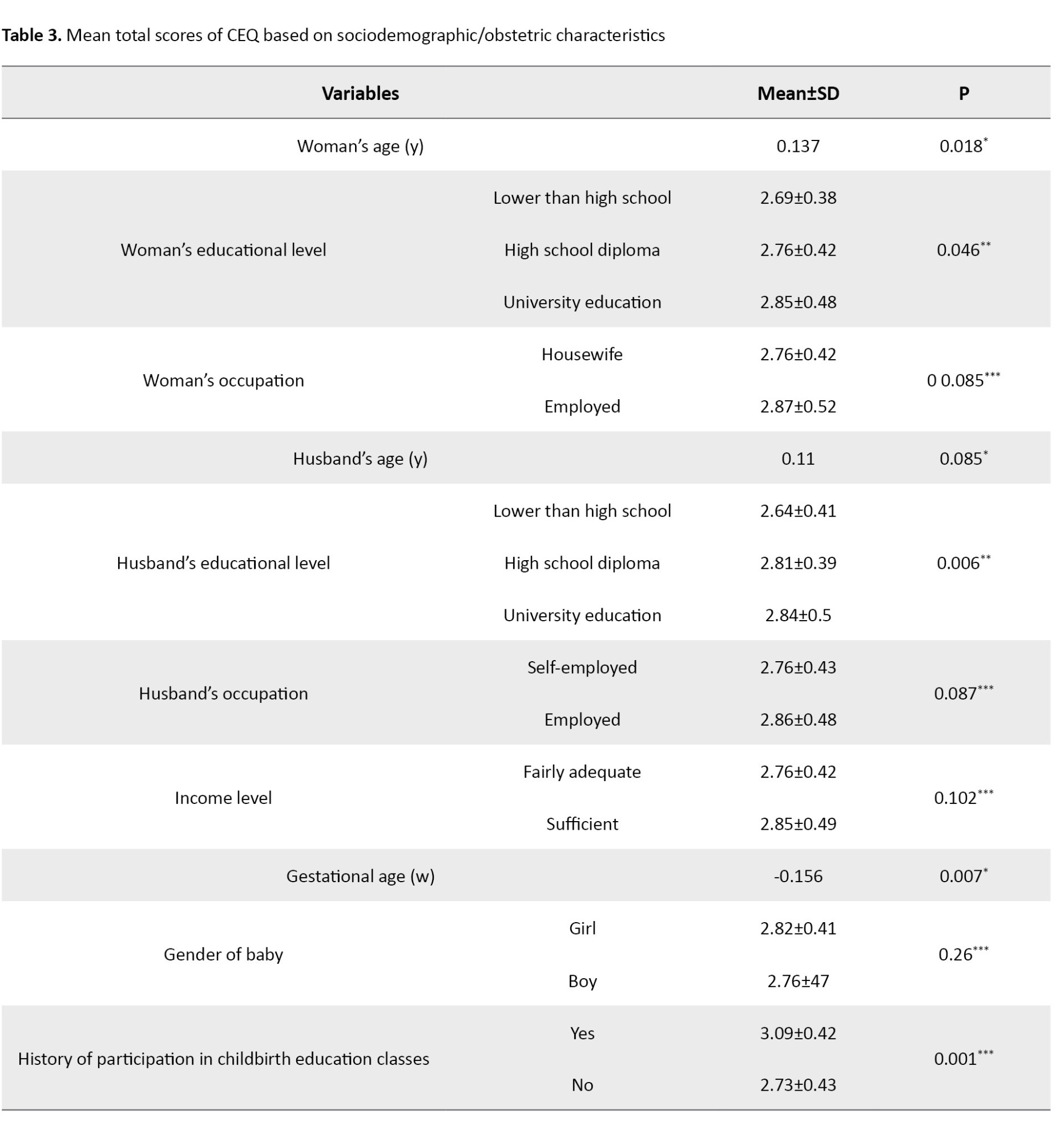
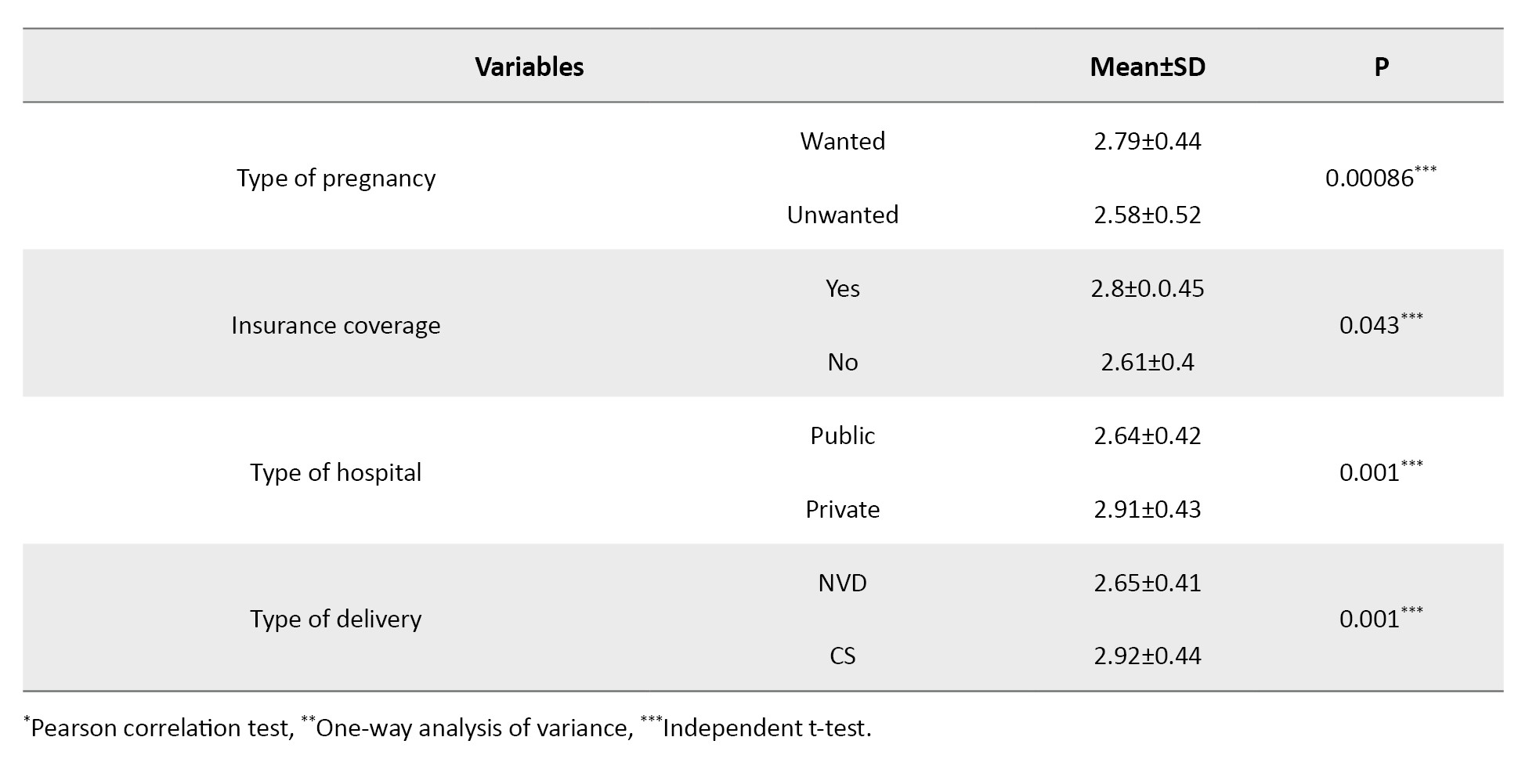
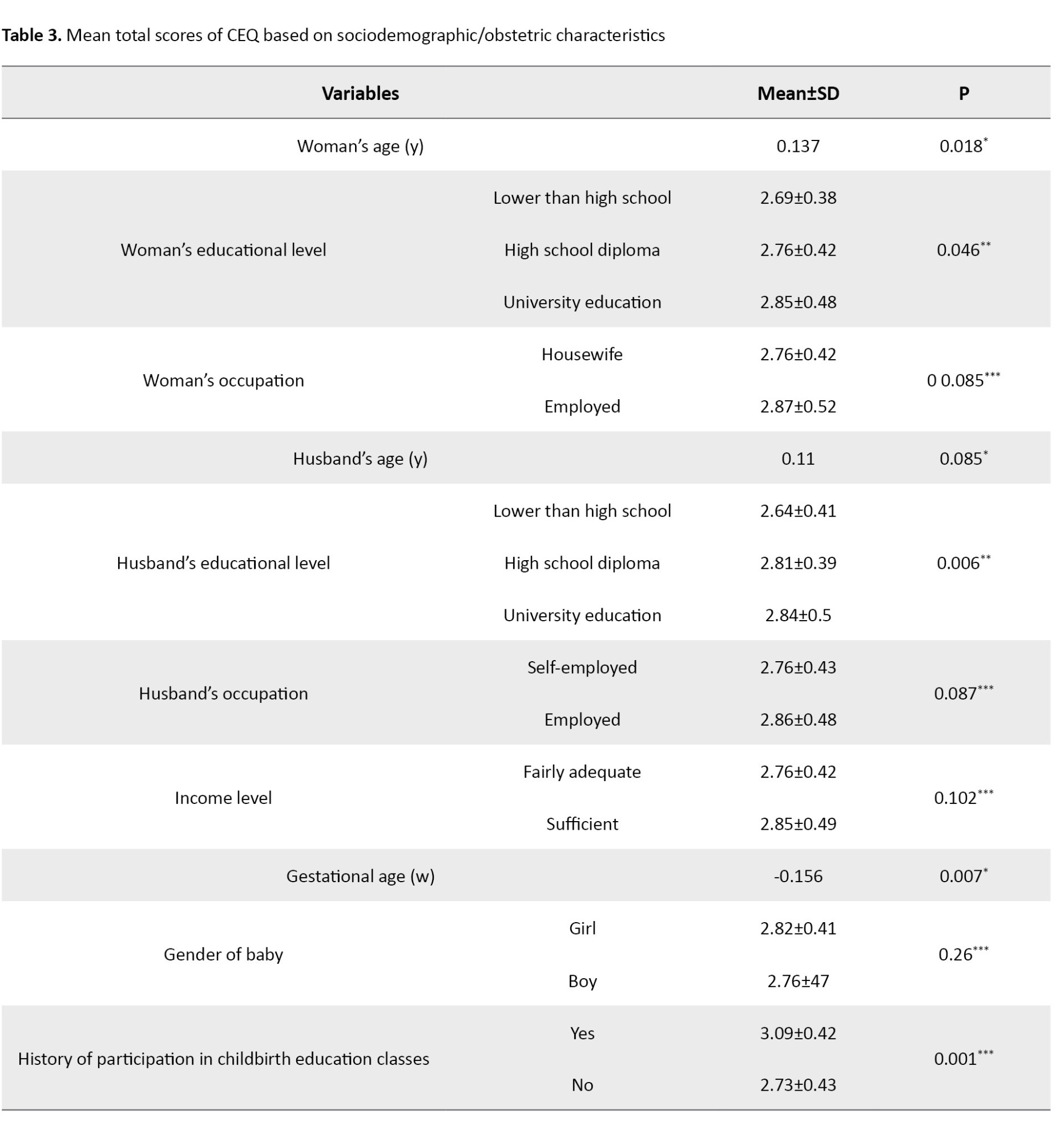
The mean total CEQ score in women with CS was significantly higher than in women with NVD (P=0.001). The results showed a weak significant positive correlation between women’s age and their total CEQ score (r=0.137, P=0.018). In addition, a statistically significant difference was observed in the total CEQ score based on the women’s education level (P=0.046) and their husbands’ educational level (P=0.006); the women with higher education levels had higher total CEQ scores, and the women whose husbands had higher educational level had higher total CEQ scores. A weak, significant negative correlation was observed between women’s gestational age and their total CEQ score (r=-0.156, P=0.007). The mean total CEQ scores of women who had a history of participating in childbirth education classes (P=0.001), insurance (P=0.043), childbirth in a private hospital (P=0.001) were significantly higher than that of women with no history of participation, no insurance, and a history of childbirth in a public hospital, respectively. Other sociodemographic/obstetric characteristics of primiparous women had no statistically significant relationship with their total CEQ score (Table 3).
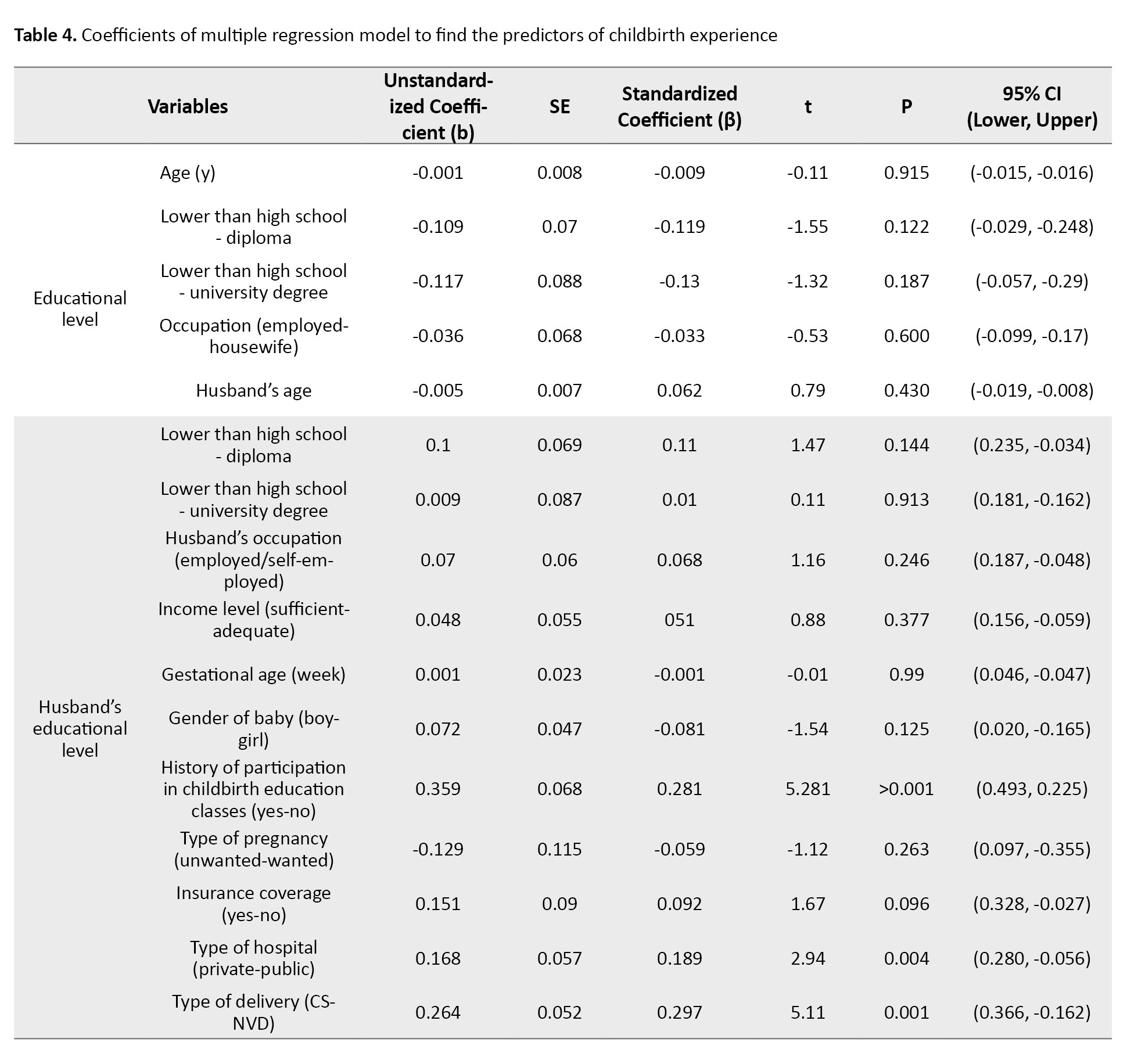
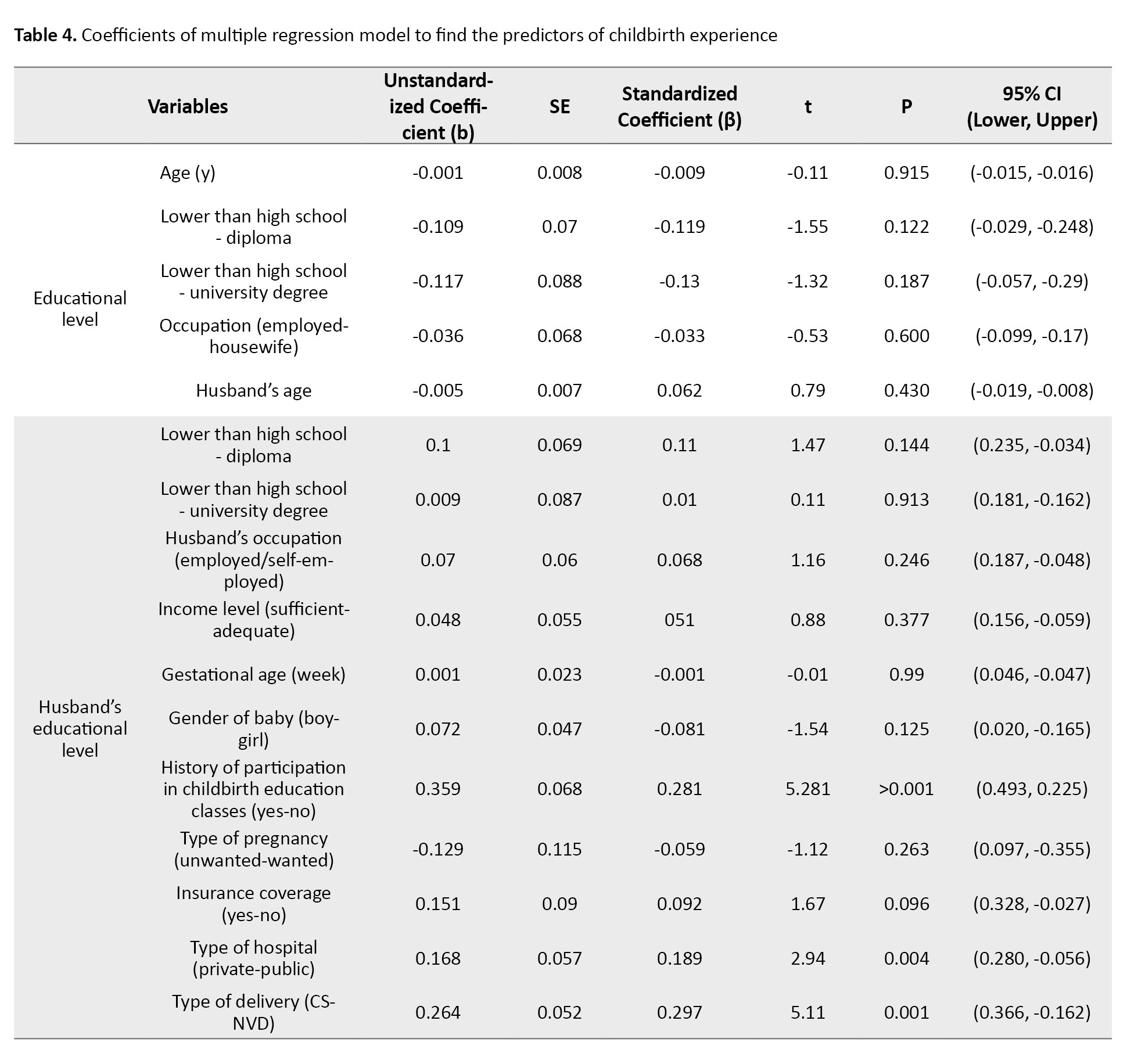
According to the regression coefficients, the total CEQ score in women with a history of attending childbirth education classes was 0.359 units higher than in women without a history of attending classes (b=0.359, 95% CI; 0.225%, 0.493%, P=0.001). Also, the total CEQ score in women who delivered in a private hospital was 0.168 units higher than in women who gave birth in a public hospital (b=0.168, 95% CI; 0.056%, 0.28%, P=0.004). Furthermore, the total CEQ score in women with CS was 0.264 units higher than in women with NVD (b=0.264, 95% CI; 0.162%, 0.366%, P=0.001). The coefficient of determination (R2) was 0.257, indicating that 25.7% of the variation in the total CEQ score was explained by these characteristics. The association of other sociodemographic/obstetric characteristics with the total CEQ score was not statistically significant (Table 4).
Discussion
This study aimed to compare the childbirth experience and related factors in primiparous women with NVD and CS referring to comprehensive health centers in Rasht, Iran, in 2022. It was found that the women with higher educational levels had higher total CEQ scores. Also, the education level of women with CS was significantly higher than that of women with NVD. The findings of Karlström also showed that the level of education significantly affects women’s tendency to choose CS and their childbirth experience [21]. The reasons for the high CS rate among educated women may be the changes in lifestyle and the perceived convenience of surgery, which have been mentioned in some studies [6, 22].
In the present study, the highest mean score was in the professional support domain of CEQ and the lowest score was in the participation domain. The results of Zamani et al. [16] also indicated that women’s professional support (support from maternity hospital staff) had the highest score. A study also showed that women who received continuous and primary midwifery care from midwifery staff had a better overall childbirth experience than the group who only received routine care in the ward [23]. The results of the present study are also consistent other studies [16, 24]. During labor and delivery, women need attention and support from loved ones, relatives, and healthcare providers (including midwives) and active participation, and this can play a key role in having a positive childbirth experience.
The findings of the present study showed that the mean total CEQ score in women with CS was significantly higher than in women with NVD. In other words, women who had CS reported a better childbirth experience than those who had NVD. The results are consistent with other studies [25-27]. Most women prefer to have a CS due to the painful process of NVD and the lack of comprehensive information about the complications of CS. The findings of some studies showed that the childbirth experience of women with NVD was better than that of other women [28, 29]. The reason for this discrepancy may be the fact that, in the present study, women had a low level of participation in the labor stages, which led to their acceptance of CS.
In the present study, the total CEQ score of women who had a history of participating in childbirth preparation classes was significantly higher than that of women with no history of participation. This is consistent with the results of Smarandache [6] but is against the results of Zamani [16]. The provided content, number duration of classes, and type of communication between midwives and pregnant mothers in different centers may have influenced the results. In some cases, meeting the mother’s expectations might lead to a better childbirth experience, while in other cases, it had no such impact. The total CEQ score of women who had an unwanted pregnancy was significantly lower than that of women with a wanted pregnancy. Some studies did not find a significant relationship between women’s childbirth experience, type of delivery, and type of pregnancy (wanted/unwanted) [14, 16]. A study suggested that the pregnancy (wanted or unwanted) may cause maternal anxiety and women may report a lower childbirth experience [8]. Due to this reason, an unwanted pregnancy might lead to a negative experience of childbirth in women who participated in our study. In the present study, employed women and women who delivered in a private hospital had a better childbirth experience, consistent with the results of other studies [26, 30]. The results may be due to the employment and financial independence of women, which may affect their childbirth experience. Also, women who had insurance had a better childbirth experience, may be due to reduced financial concerns and the choice of a private hospital for giving birth.
The history of participating in childbirth education classes was significantly associated with better childbirth experience in primiparous women, consistent with the results of other studies [25, 31]. Also, there was a significant relationship between the total CEQ score and age; the increase in age can increase women’s childbirth experience. This is consistent with the results of Smarandache [6] but is against the results of other studies [22, 32]. The high childbirth experience score at older ages may be because older women deal with pregnancy complications more easily, which leads to a better child birth experience for them.
Overall, it can be concluded that primiparous women with CS in Rasht City have a better childbirth experience than those with NVD. Participating in childbirth education classes has a significant impact on primiparous women’s childbirth experience. Despite only one-sixth of women attended childbirth preparation classes, the childbirth experience was significantly positive in both groups of NVD and CS. Therefore, more attention should be paid to holding childbirth education classes for women to help further improve their experience of natural childbirth. It is recommended that future studies be conducted to investigate practical and interventional methods to improve the childbirth experience of women with NVD. The psychological state of the women could affect their responses to the questions, which can be a limitation of this study.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1400.512).
Funding
This study was taken from a master's thesis, approved by the School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
Authors' contributions
Conceptualization, study design, and resources: Fatemeh Afshar, Sedigheh Pakseresht, and Fatemeh Jafarzadeh Kenarsari; Data collection: Fatemeh Afshar and Saman Maroufizadeh; Data analysis: Fatemeh Afshar, Sedigheh Pakseresht, and Saman Maroufizadeh; Investigation, writing the original draft: Fatemeh Afshar and Sedigheh Pakseresht; Review and editing: Fatemeh Afshar, Sedigheh Pakseresht, and Fatemeh Jafarzadeh Kenarsari.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the postpartum women for their cooperation in this study.
References
Childbirth is one of the most challenging physiological and psychological events in a woman’s life [1]. A positive childbirth experience has benefits such as improved mother-infant bonding, self-esteem, and quality of life [2, 3]. In contrast, a negative childbirth experience has consequences, including post-traumatic stress disorder, decreased breastfeeding rates, impaired mother-infant relationships, fear of childbirth, and an increased tendency to have elective Cesarean sections (CSs) in future pregnancies [4, 5, 6]. Therefore, one of the important factors for deciding on subsequent pregnancies is the type of experience gained from previous childbirth [7]. A systematic review conducted in different countries showed that 10-33% of women reported childbirth as a negative experience [8].
Today, the childbirth experience has become an important factor in assessments of health care delivery for mothers, emphasizing the active role of childbirth in this process [9]. Previous studies have shown that several factors affect mothers’ experiences of the postpartum period, including sociodemographic characteristics (race, age, social status), maternal expectations, prenatal education, maternal awareness, pain perception, type of delivery, unforeseen complications, medical interventions, transfer of the infant to the neonatal intensive care unit, and receiving adequate support during labor and delivery from medical staff [10, 11]. Also, factors such as a sense of security, personal support, midwifery care, information provided to the mother, and her participation in decision-making affect the childbirth experience [12].
Despite the identification of many factors that have a negative or positive effect on the childbirth experience, the impact of these factors on women’s experiences in different situations and societies is still not comprehensively and accurately known [13, 14]. The cultural, economic, and social differences necessitate the need to examine human experiences in each society separately [15]. In Iran, few studies have investigated the childbirth experience and the related factors in mothers. A study in this field was conducted in Rasht City on hospitalized mothers after childbirth and the results showed that effective communication between mothers and healthcare providers and the mother’s right to participate in labor have a positive impact on the birth experience [16]. Other studies in Iran have reported that assessing childbirth experiences immediately after delivery can lead to women’s false reporting of positive childbirth experiences due to the delivery of a healthy baby [12, 17].
Therefore, considering the importance of mothers’ childbirth experience and its outcomes, the impact of childbirth experience on maternal health and child development, and the desire to have children in case of a positive childbirth experience, it seems necessary to conduct a study to compare childbirth experience and related factors in primiparous women with normal vaginal delivery (NVD) and CS.
Materials and Methods
This is an analytical cross-sectional study conducted in 2022. The study population consists of all primiparous women with NVD or CS referring to comprehensive health centers in Rasht, Iran. Inclusion criteria were willingness to participate in the study, singleton pregnancy, uncomplicated and low-risk pregnancy, cephalic presentation, term pregnancy (37 weeks or more), and experiencing all or part of the active phase of labor and painful uterine contractions. Women with elective CS (women who did not go into labor), women who had a stillborn baby, or a baby admitted to the neonatal intensive care unit were not included in the study. A multi-stage sampling method was used. In the first, second, and third stages, stratified sampling, cluster sampling, and convenience sampling methods were used, respectively. In the first stage, Rasht was divided into four regions (north, south, west, and east) and each region was considered as a stratum. In the second stage, the comprehensive health centers (clusters) were selected within each stratum by simple random sampling. Finally, in the third stage, a convenience sampling method was used to choose women from each center. Considering that, in linear regression analyses, at least 20 samples should be selected for each independent variable (predictor) [18, 19] and given that there were 14 independent variables in the present study, at least 300 primiparous women were selected and put in two groups: 150 with NVD and 150 with CS.
The data collection tools were two questionnaires. The first questionnaire surveys socio-demographic information (age, place of residence, woman’s educational level, husband’s educational level, woman’s occupation, husband’s occupation, income level, insurance status, type of hospital) and obstetric characteristics (type of delivery, type of pregnancy, gender of the baby, gestational age with emphasis on sonography and date of last menstrual period, and history of participation in childbirth education classes). This questionnaire was used after determining its face validity based on the opinions of five faculty members of the School of Nursing and Midwifery. The second tool was the childbirth experience questionnaire (CEQ) developed by Dencker et al. [12]. It contains 22 items that measure the childbirth experience of primiparous women up to one month after delivery. This questionnaire includes four domains: Own capacity (8 items), professional support (5 items), perceived safety (6 items), and participation (3 items). Each item is scored using a 4-point Likert scale as 1 (totally agree), 2 (mostly agree), 3 (mostly disagree), and 4 (totally disagree), except for two items from the own capacity domain and one item from the perceived safety domain, referring to perceived pain, sense of control and sense of security, which are assessed using a visual analog scale (VAS), rated as 1 (score 0–40), 2 (score 41–60), 3 (score 61–80), and 4 (score 81–100). The scoring of negatively worded items is reversed. A higher score indicates a better childbirth experience. The Persian version of the CEQ has been validated by Kazemi et al. [20].
After obtaining official permission and receiving the code of ethics from the Ethics Committee of Guilan University of Medical Sciences, informed consent was obtained from the samples after emphasizing the confidentiality of their information and explaining the study objectives to them. The researcher collected data from the women within one month after delivery when women visited comprehensive health centers for postpartum care.
Data analysis was performed using descriptive and inferential statistics. The descriptive statistics included Mean±SD, frequency, and percentage. Inferential statistics included independent t-test, chi-square test, and Cochran-Armitage test (to compare sociodemographic/obstetric characteristics of two NVD and CS groups). The Shapiro-Wilks test was used to examine the assumption of normality of the CEQ score in primiparous women. In univariate analyses, independent t-test, one-way analysis of variance, and Pearson correlation test were used to examine the relationship between the CEQ score and sociodemographic/obstetric characteristics. In multivariate analyses, the multiple linear regression analysis was used to determine factors associated with the total CEQ score. Data were analyzed in SPSS software, version 16, and the significance level was set at 0.05.
Results
The mean age of women and their husbands was 27.85±4.61 and 32.52±5.15 years, respectively. The level of education of 42% of women and 38.3% of their husbands was university education. Also, 78.7% of women were housewives and 75.3% of their husbands were self-employed. Based on the results, the education of women with CS was significantly higher than that of women with NVD (P=0.005). A similar finding was also observed based on their husbands’ education level (P=0.009). Gestational age in women with CS was significantly lower than in women with NVD (P=0.001). Also, the percentage of deliveries in private hospitals in women with CS was significantly higher than in women with NVD (P=0.001). These results are shown in Table 1.
The mean total CEQ score was significantly higher in women with CS than in women with NVD (p=0.001). Also, the mean scores for the domains of own capacity, perceived safety, and participation were significantly higher in women with CS than those with NVD (P=0.001). Although the mean score for the professional support domain was higher in women with CS, the difference was not statistically significant (Table 2).
The mean total CEQ score in women with CS was significantly higher than in women with NVD (P=0.001). The results showed a weak significant positive correlation between women’s age and their total CEQ score (r=0.137, P=0.018). In addition, a statistically significant difference was observed in the total CEQ score based on the women’s education level (P=0.046) and their husbands’ educational level (P=0.006); the women with higher education levels had higher total CEQ scores, and the women whose husbands had higher educational level had higher total CEQ scores. A weak, significant negative correlation was observed between women’s gestational age and their total CEQ score (r=-0.156, P=0.007). The mean total CEQ scores of women who had a history of participating in childbirth education classes (P=0.001), insurance (P=0.043), childbirth in a private hospital (P=0.001) were significantly higher than that of women with no history of participation, no insurance, and a history of childbirth in a public hospital, respectively. Other sociodemographic/obstetric characteristics of primiparous women had no statistically significant relationship with their total CEQ score (Table 3).
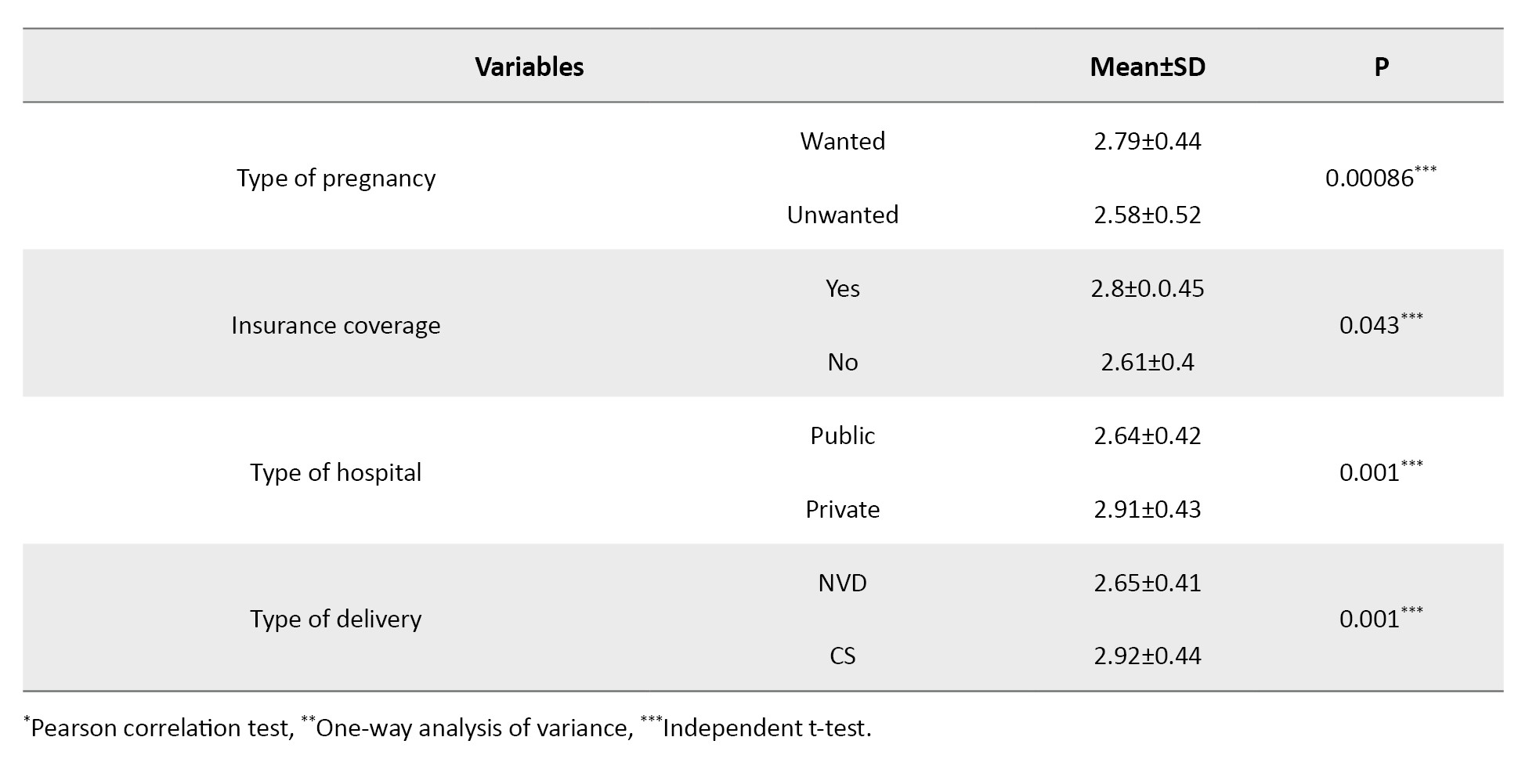
According to the regression coefficients, the total CEQ score in women with a history of attending childbirth education classes was 0.359 units higher than in women without a history of attending classes (b=0.359, 95% CI; 0.225%, 0.493%, P=0.001). Also, the total CEQ score in women who delivered in a private hospital was 0.168 units higher than in women who gave birth in a public hospital (b=0.168, 95% CI; 0.056%, 0.28%, P=0.004). Furthermore, the total CEQ score in women with CS was 0.264 units higher than in women with NVD (b=0.264, 95% CI; 0.162%, 0.366%, P=0.001). The coefficient of determination (R2) was 0.257, indicating that 25.7% of the variation in the total CEQ score was explained by these characteristics. The association of other sociodemographic/obstetric characteristics with the total CEQ score was not statistically significant (Table 4).
Discussion
This study aimed to compare the childbirth experience and related factors in primiparous women with NVD and CS referring to comprehensive health centers in Rasht, Iran, in 2022. It was found that the women with higher educational levels had higher total CEQ scores. Also, the education level of women with CS was significantly higher than that of women with NVD. The findings of Karlström also showed that the level of education significantly affects women’s tendency to choose CS and their childbirth experience [21]. The reasons for the high CS rate among educated women may be the changes in lifestyle and the perceived convenience of surgery, which have been mentioned in some studies [6, 22].
In the present study, the highest mean score was in the professional support domain of CEQ and the lowest score was in the participation domain. The results of Zamani et al. [16] also indicated that women’s professional support (support from maternity hospital staff) had the highest score. A study also showed that women who received continuous and primary midwifery care from midwifery staff had a better overall childbirth experience than the group who only received routine care in the ward [23]. The results of the present study are also consistent other studies [16, 24]. During labor and delivery, women need attention and support from loved ones, relatives, and healthcare providers (including midwives) and active participation, and this can play a key role in having a positive childbirth experience.
The findings of the present study showed that the mean total CEQ score in women with CS was significantly higher than in women with NVD. In other words, women who had CS reported a better childbirth experience than those who had NVD. The results are consistent with other studies [25-27]. Most women prefer to have a CS due to the painful process of NVD and the lack of comprehensive information about the complications of CS. The findings of some studies showed that the childbirth experience of women with NVD was better than that of other women [28, 29]. The reason for this discrepancy may be the fact that, in the present study, women had a low level of participation in the labor stages, which led to their acceptance of CS.
In the present study, the total CEQ score of women who had a history of participating in childbirth preparation classes was significantly higher than that of women with no history of participation. This is consistent with the results of Smarandache [6] but is against the results of Zamani [16]. The provided content, number duration of classes, and type of communication between midwives and pregnant mothers in different centers may have influenced the results. In some cases, meeting the mother’s expectations might lead to a better childbirth experience, while in other cases, it had no such impact. The total CEQ score of women who had an unwanted pregnancy was significantly lower than that of women with a wanted pregnancy. Some studies did not find a significant relationship between women’s childbirth experience, type of delivery, and type of pregnancy (wanted/unwanted) [14, 16]. A study suggested that the pregnancy (wanted or unwanted) may cause maternal anxiety and women may report a lower childbirth experience [8]. Due to this reason, an unwanted pregnancy might lead to a negative experience of childbirth in women who participated in our study. In the present study, employed women and women who delivered in a private hospital had a better childbirth experience, consistent with the results of other studies [26, 30]. The results may be due to the employment and financial independence of women, which may affect their childbirth experience. Also, women who had insurance had a better childbirth experience, may be due to reduced financial concerns and the choice of a private hospital for giving birth.
The history of participating in childbirth education classes was significantly associated with better childbirth experience in primiparous women, consistent with the results of other studies [25, 31]. Also, there was a significant relationship between the total CEQ score and age; the increase in age can increase women’s childbirth experience. This is consistent with the results of Smarandache [6] but is against the results of other studies [22, 32]. The high childbirth experience score at older ages may be because older women deal with pregnancy complications more easily, which leads to a better child birth experience for them.
Overall, it can be concluded that primiparous women with CS in Rasht City have a better childbirth experience than those with NVD. Participating in childbirth education classes has a significant impact on primiparous women’s childbirth experience. Despite only one-sixth of women attended childbirth preparation classes, the childbirth experience was significantly positive in both groups of NVD and CS. Therefore, more attention should be paid to holding childbirth education classes for women to help further improve their experience of natural childbirth. It is recommended that future studies be conducted to investigate practical and interventional methods to improve the childbirth experience of women with NVD. The psychological state of the women could affect their responses to the questions, which can be a limitation of this study.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1400.512).
Funding
This study was taken from a master's thesis, approved by the School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
Authors' contributions
Conceptualization, study design, and resources: Fatemeh Afshar, Sedigheh Pakseresht, and Fatemeh Jafarzadeh Kenarsari; Data collection: Fatemeh Afshar and Saman Maroufizadeh; Data analysis: Fatemeh Afshar, Sedigheh Pakseresht, and Saman Maroufizadeh; Investigation, writing the original draft: Fatemeh Afshar and Sedigheh Pakseresht; Review and editing: Fatemeh Afshar, Sedigheh Pakseresht, and Fatemeh Jafarzadeh Kenarsari.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the postpartum women for their cooperation in this study.
References
- Khamehchian M, Adib-Hajbaghery M, HeydariKhayat N, Rezaei M, Sabery M. Primiparous women’s experiences of normal vaginal delivery in Iran: A qualitative study. BMC Pregnancy Childbirth. 2020; 20(1):259. [DOI:10.1186/s12884-020-02954-4] [PMID]
- Guittier MJ, Cedraschi C, Jamei N, Boulvain M, Guillemin F. Impact of mode of delivery on the birth experience in first-time mothers: A qualitative study. BMC Pregnancy Childbirth. 2014; 14:254.[DOI:10.1186/1471-2393-14-254] [PMID]
- Hildingsson I, Johansson M, Karlström A, Fenwick J. Factors associated with a positive birth experience: An exploration of swedish women’s experiences. Int J Childbirth. 2013; 3(3):153-64. [DOI:10.1891/2156-5287.3.3.153]
- Taheri M, Takian A, Taghizadeh Z, Jafari N, Sarafraz N. Creating a positive perception of childbirth experience: Systematic review and meta-analysis of prenatal and intrapartum interventions. Reprod Health. 2018; 15(1):73. [DOI:10.1186/s12978-018-0511-x] [PMID]
- Nilvér H, Begley C, Berg M. Measuring women’s childbirth experiences: A systematic review for identification and analysis of validated instruments. BMC Pregnancy Childbirth. 2017; 17(1):203.[DOI:10.1186/s12884-017-1356-y] [PMID]
- Smarandache A, Kim TH, Bohr Y, Tamim H. Predictors of a negative labour and birth experience based on a national survey of Canadian women. BMC Pregnancy Childbirth. 2016; 16(1):114. [DOI:10.1186/s12884-016-0903-2] [PMID]
- Gottvall K, Waldenström U. Does a traumatic birth experience have an impact on future reproduction? BJOG. 2002; 109(3):254-60. [DOI:10.1111/j.1471-0528.2002.01200.x] [PMID]
- Chabbert M, Panagiotou D, Wendland J. Predictive factors of women’s subjective perception of childbirth experience: A systematic review of the literature. J Reprod Infant Psychol. 2021; 39(1):43-66. [DOI:10.1080/02646838.2020.1748582] [PMID]
- Place K, Kruit H, Rahkonen L. Comparison of primiparous womenʼs childbirth experience in labor induction with cervical ripening by balloon catheter or oral misoprostol - a prospective study using a validated childbirth experience questionnaire (CEQ) and visual analogue scale (VAS). Acta Obstet Gynecol Scand. 2022; 101(10):1153-62. [DOI:10.1111/aogs.14433] [PMID]
- Ariffin IA, Abd Hamid J, Shukri SM. Mediating role of customer satisfaction on the relationship of demographic factors and customer loyalty. Syst Rev Pharm. 2020; 11(1):1170-6. [Link]
- Baas CI, Wiegers TA, de Cock TP, Erwich JJ, Spelten ER, de Boer MR, et al. Client-related factors associated with a “Less than Good” Experience of midwifery care during childbirth in the Netherlands. Birth. 2017; 44(1):58-67. [DOI:10.1111/birt.12266] [PMID]
- Dencker A, Taft C, Bergqvist L, Lilja H, Berg M. Childbirth experience questionnaire (CEQ): Development and evaluation of a multidimensional instrument. BMC Pregnancy Childbirth. 2010; 10:81.[DOI:10.1186/1471-2393-10-81] [PMID]
- Kalisa R, Rulisa S, van den Akker T, van Roosmalen J. Maternal Near Miss and quality of care in a rural Rwandan hospital. BMC Pregnancy Childbirth. 2016; 16(1):324. [DOI:10.1186/s12884-016-1119-1] [PMID]
- Ghobadi M, Ziaee T, Mirhaghjo N, Pazandeh F, Kazemnejad lili E. [Evaluation of satisfaction with natural delivery experience and its related factors in Rasht Women (Persian)]. J Health Care. 2018; 20(3):215-24. [DOI:10.29252/jhc.20.3.215]
- Vaziri F, Khademian Z, Behbahani BM. [Qualitative investigation of experiences and perception of primiparous women regarding childbirth in women referring to educational hospitals of Shiraz University of Medical Sciences (Persian)]. Mod Care J. 2012; 9(3):226-36. [Link]
- Zamani P, Ziaie T, Mokhtari Lakeh N, Kazemnejad Leili E. [Childbirth experience and its related socio-demographic factors in mothers admitted to postpartum ward of AL Zahra Hospital of Rasht City, (Iran) (Persian)]. Qom Univ Med Sci J. 2019; 12(11):70-8. [DOI:10.29252/qums.12.11.8]
- Waldenström U. Why do some women change their opinion about childbirth over time? Birth. 2004; 31(2):102-7. [DOI:10.1111/j.0730-7659.2004.00287.x] [PMID]
- Pituch KA, Stevens JP. Applied multivariate statistics for the social sciences: Analyses with SAS and IBM’s SPSS. Sixth Edition. Oxfordshire: Taylor & Francis; 2015. [Link]
- Hair J, Black WC, Babin BJ, Anderson R. Multivariate Data Analysis. London: Pearson; 2013. [Link]
- Kazemi S, Dencker A, Pazandeh F, Montazeri A, Sedigh-Mobarakabadi S, Hajian S. Psychometric evaluation of the persian version of the Childbirth Experience Questionnaire (CEQ). Biomed Res Int. 2020; 2020:6879283. [DOI:10.1155/2020/6879283] [PMID]
- Karlström A, Nystedt A, Hildingsson I. A comparative study of the experience of childbirth between women who preferred and had a caesarean section and women who preferred and had a vaginal birth. Sex Reprod Healthc. 2011; 2(3):93-9. [DOI:10.1016/j.srhc.2011.03.002] [PMID]
- Waldenström U, Hildingsson I, Rubertsson C, Rådestad I. A Negative birth experience: Prevalence and risk factors in a national sample. Birth. 2004; 31(1):17-27. [DOI:10.1111/j.0730-7659.2004.0270.x] [PMID]
- McLachlan HL, Forster DA, Davey MA, Farrell T, Flood M, Shafiei T, et al. The effect of primary midwife-led care on women’s experience of childbirth: Results from the COSMOS randomised controlled trial. BJOG. 2016; 123(3):465-74. [DOI:10.1111/1471-0528.13713] [PMID]
- Spaich S, Welzel G, Berlit S, Temerinac D, Tuschy B, Sütterlin M, et al. Mode of delivery and its influence on women’s satisfaction with childbirth. Eur J Obstet Gynecol Reprod Biol. 2013; 170(2):401-6. [DOI:10.1016/j.ejogrb.2013.07.040] [PMID]
- Ozkan SA, Bal MD. Maternal satisfaction in normal and caesarean birth: A cross-sectional study. Int J Caring Sci. 2019; 12(2):1017. [Link]
- Jha P, Larsson M, Christensson K, Skoog Svanberg A. Satisfaction with childbirth services provided in public health facilities: Results from a cross- sectional survey among postnatal women in Chhattisgarh, India. Glob Health Action. 2017; 10(1):1386932. [DOI:10.1080/16549716.2017.1386932] [PMID]
- Blomquist JL, Quiroz LH, MacMillan D, McCullough A, Handa VL. Mothers’ satisfaction with planned vaginal and planned cesarean birth. Am J Perinatol. 2011; 28(5):383-8. [DOI:10.1055/s-0031-1274508] [PMID]
- Sigurdardottir VL, Gamble J, Gudmundsdottir B, Kristjansdottir H, Sveinsdottir H, Gottfredsdottir H. The predictive role of support in the birth experience: A longitudinal cohort study. Women Birth. 2017; 30(6):450-9. [DOI:10.1016/j.wombi.2017.04.003] [PMID]
- Nystedt A, Hildingsson I. Women’s and men’s negative experience of child birth-A cross-sectional survey. Women Birth. 2018; 31(2):103-9. [DOI:10.1016/j.wombi.2017.07.002] [PMID]
- Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J Adv Nurs. 2004; 46(2):212-9. [DOI:10.1111/j.1365-2648.2003.02981.x] [PMID]
- Adeyinka O, Jukic AM, McGarvey ST, Muasau-Howard BT, Faiai M, Hawley NL. Predictors of prenatal care satisfaction among pregnant women in American Samoa. BMC Pregnancy Childbirth. 2017; 17(1):381. [DOI:10.1186/s12884-017-1563-6] [PMID]
- Congdon JL, Adler NE, Epel ES, Laraia BA, Bush NR. A prospective investigation of prenatal mood and childbirth perceptions in an ethnically diverse, low-income sample. Birth. 2016; 43(2):159-66. [DOI:10.1111/birt.12221] [PMID]
Article Type : Research |
Subject:
Special
Received: 2023/07/11 | Accepted: 2023/12/25 | Published: 2025/01/12
Received: 2023/07/11 | Accepted: 2023/12/25 | Published: 2025/01/12
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |