Mon, Jul 22, 2024
Volume 33, Issue 4 (9-2023)
JHNM 2023, 33(4): 250-258 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Faraji Dehsorkhi H, Azizi Shamami M, Hayat A A, Rokni J. Predicting Training Transfer of Oxygen Therapy During COVID-19: Theory of Planned Behavior Application. JHNM 2023; 33 (4) :250-258
URL: http://hnmj.gums.ac.ir/article-1-2196-en.html
URL: http://hnmj.gums.ac.ir/article-1-2196-en.html
1- Assistant Professor, Department of Education, Faculty of Literature and Humanities, Shahid Bahonar University, Kerman, Iran.
2- Assistant Professor, Department of Education, Faculty of Humanities and Social Sciences, University of Mazandaran, Babolsar, Iran. ,mazizi@umz.ac.ir
3- Assistant Professor, Department of Medical Education, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
4- General Psychology (PhD), Imam Hossein Hospital, Shahid Beheshti University, Tehran, Iran.
2- Assistant Professor, Department of Education, Faculty of Humanities and Social Sciences, University of Mazandaran, Babolsar, Iran. ,
3- Assistant Professor, Department of Medical Education, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
4- General Psychology (PhD), Imam Hossein Hospital, Shahid Beheshti University, Tehran, Iran.
Full-Text [PDF 557 kb]
(176 Downloads)
| Abstract (HTML) (568 Views)
Full-Text: (114 Views)
Introduction
Since the onset of the COVID-19 pandemic in December 2019, the disease has dramatically affected millions worldwide [1]. Studies show that about 14% of patients must be hospitalized since they show severe symptoms such as pneumonia, respiratory failure, and even death [2-4]. Reports suggest that mortality due to COVID-19 results from alveolar damage and respiratory loss [5]. Guan et al. reported that about 90% of the patients need oxygen therapy [6]. Therefore, respiratory support, or oxygen therapy, is critical for treating patients with severe symptoms [7]; oxygen therapy is recommended as the first step in treating hypoxemic patients such as COVID-19 [8, 9]. Empirical studies have also demonstrated oxygen therapy’s efficiency in treating COVID patients [10, 11]. In this line, Shen et al. argued that oxygen therapy was instrumental in suppressing the pathogen by disrupting its replication cycle and boosting the immune system [12].
Owing to the paramount importance of oxygen therapy in treating COVID-19 patients, 5 courses of oxygen therapy were held in a hospital in Tehran City, Iran, in 2021 to improve the nurses’ knowledge and skills of oxygen therapy; 164 nurses participated in these courses. Because of the high cost of implementing such courses, the main question is whether nurses use this training in the workplace. Hence, the issue of training transfer, defined as the maintenance and use of learned attitudes, knowledge, and skills in the workplace [13-15], is considered the main criterion of training effectiveness [16, 17]. Training transfer is of the utmost importance to nurses because it allows them to meet the growing and changing demands of the workplace and improve the quality of healthcare services [17, 18].
However, the healthcare sector is lacking in training transfer research [17, 19, 20], and a majority of the training transfer research has been conducted in other settings [17], showing that training transfer is confronted with difficulties in organizations [21]. Hutchins also states that learners use less than 40% of the knowledge and skills learned from the courses [22]. Similarly, Wexley and Latham found that the training transfer rate is about 40% immediately after training, which drops to 25% after 6 months and 15% after 12 months [23]. In the nursing profession, also, the “transfer problem” exists [17]. The reports indicate that in health and hygiene, only a small part of the knowledge and skills acquired in training courses is used in the workplace [24].
Various models have been developed to understand the process of training transfer, among which the systematic model of training transfer is a reference and framework for understanding the training transfer process [15]. Based on this model, various research studies have been conducted and published in training transfer [14, 25, 26]. However, the existing models of training transfer do not emphasize the learners’ intention to transfer their knowledge and skills as a predictor of training transfer behavior [27, 28]. Factoring this element in the theory of planned behavior (TPB) suggests that intention can be the most effective variable in predicting human behavior in all contexts, including the context of training transfer [29].
According to the TPB, training transfer intention and its antecedents, i.e. attitude, subjective norms (SN), and perceived behavioral control (PBC), are the main predictors of behavior. This theory posits that behavior (training transfer) is shaped by intention, which is, in turn, determined by the perception that the behavior is desirable (positive attitude), people who are important to the individual approve of the behavior (SN), and the behavior is feasible that show perceived behavioral control [30]. Therefore, the present study uses the TPB as the main research framework to investigate training transfer behavior among nurses.
Material and Methods
This study used a cross-sectional, correlational research design to answer the research hypotheses. The target population included all nurses working in one of the educational hospitals affiliated with the Shahid Beheshti University, Tehran, Iran (n=722), who participated in 5 oxygen therapy workshops in 2021 (n=283). Of whom a random sample was selected using the formula proposed by Hair et al. [31]. According to this formula, the minimum sample size required to obtain a statistical power of 95% and an R2 value of 0.10 was 103 individuals. However, 143 questionnaires were distributed among the nurses participating in the workshops to compensate for the sample loss.
To collect data, the following two measurement tools were used. TPB questionnaire that was previously validated by researchers [32-35]. This questionnaire with 17 items has 4 constructs: Attitude toward training transfer (5 items), SN regarding training transfer (3 items), PBC over training transfer (4 items), and training transfer intention (5 items). To rank the answers, a 5-point Likert scale was used (1=strongly disagree, 2=disagree, 3=neutral, 4=agree, and 5=strongly agree). Another tool was the oxygen therapy checklist, a 5-item checklist used to assess nurses’ actual training transfer behavior in the field of oxygen therapy. To rank the answers, a scale with 5 options was used (1=very low, 2=low, 3=medium, 4=high, 5=very high). Finally, for both measurement tools, the score of each structure was determined based on the mean score of the items.
Before implementing the survey, the psychometric properties of the scales were examined in terms of face, content, and construct validity. Three medical practitioners assessed the face validity of the scales in terms of readability, comprehensibility, and wording. Some minor modifications were made to the survey based on the expert’s inputs. Afterward, the content validity of the survey was explored. Assessment of content validity involved empirical methods to determine the content validity ratio (CVR), which represents the essentiality of each item, and the content validity index (CVI), which measures the relevance of each item to the underlying construct. In this regard, 6 academicians with publications on TPB and 4 medical practitioners with knowledge and experience in oxygen therapy were selected. The panelists were then asked to rate each item regarding CVR and CVI. A 3-point scale (1=essential, 2=useful but not essential, and 3=not essential) was used to measure CVR. In addition, a 4-point scale (1=not relevant, 2=somewhat relevant, 3=quite relevant, and 4=highly relevant) was used to quantify CVI. Judged by a panel of 10 experts, the minimum values of CVR [36, 37] and CVI [38] must be at least 0.62 and 0.78, respectively. CVR analysis of the oxygen therapy checklist revealed that the scores of items 2, 6, and 9 were below the cut-off point. Hence they were removed from the checklist. However, the CVR and CVI values of other items are satisfactory. Accordingly, items are deemed content valid. Additionally, confirmatory factor analysis was run to assess the construct validity of the scales. Moreover, the questionnaire was pilot-tested on 32 nurses, and the reliability test showed all the scales possess acceptable α values above 70%.
The TPB survey was implemented immediately after the workshops, and 2 weeks after the workshops, the head nurses of the same participants were asked to fill out the oxygen therapy checklist. Head nurses are in direct contact with nurses, hence a good source to rate participants’ oxygen therapy behavior. In this way, head nurses rated participants’ oxygen therapy behavior.
To analyze the data, structural equation modeling was applied using Smart-PLS3 software.
Results
Out of 143 questionnaires, 127 were returned, yielding a response rate of 89%. The results of the descriptive analysis of the samples are given in Table 1.

Structural equation modeling is a two-step process. In the first step, measurement models/factorial structure of the measures are examined to assess the construct validity of the scales. Since all of the measurement models in the present study are reflective, composite reliability and Cronbach α are used to assess internal consistency. Also, factor loading and average variance extracted (AVE) are used to assess convergent validity, and Heterotrait-Monotrait ratio of correlations (HTMT) and Fornell and Larcker to assess divergent validity. After validating the measurement models, the structural model was examined to test the research hypotheses in The second stage. For this purpose, 3 metrics are used: Path coefficient (its value should be significant), determination coefficient (R2), and predictive relevance (Q2); its value should be greater than 0 [31].
A preliminary assessment of the measurement models showed that item 6 of the attitude scale, item 2 of the SN scale, and item 6 of the oxygen therapy checklist had a factor loading below the threshold value. Hence, these items were removed from the model. The clipped measurement models were then re-evaluated. CVR and CVI metrics demonstrate that the measures are valid regarding content validity. Results also show that factor loadings of the items and AVEs of the measures are above the threshold values, indicating that the measurement tools possess convergent validity. Composite reliability and Cronbach α values of the measures surpass the acceptable cut-off points, proving the questionnaires are reliable (Table 2).

The results showed that all measurement models/tools had the desired validity and reliability (Table 3).
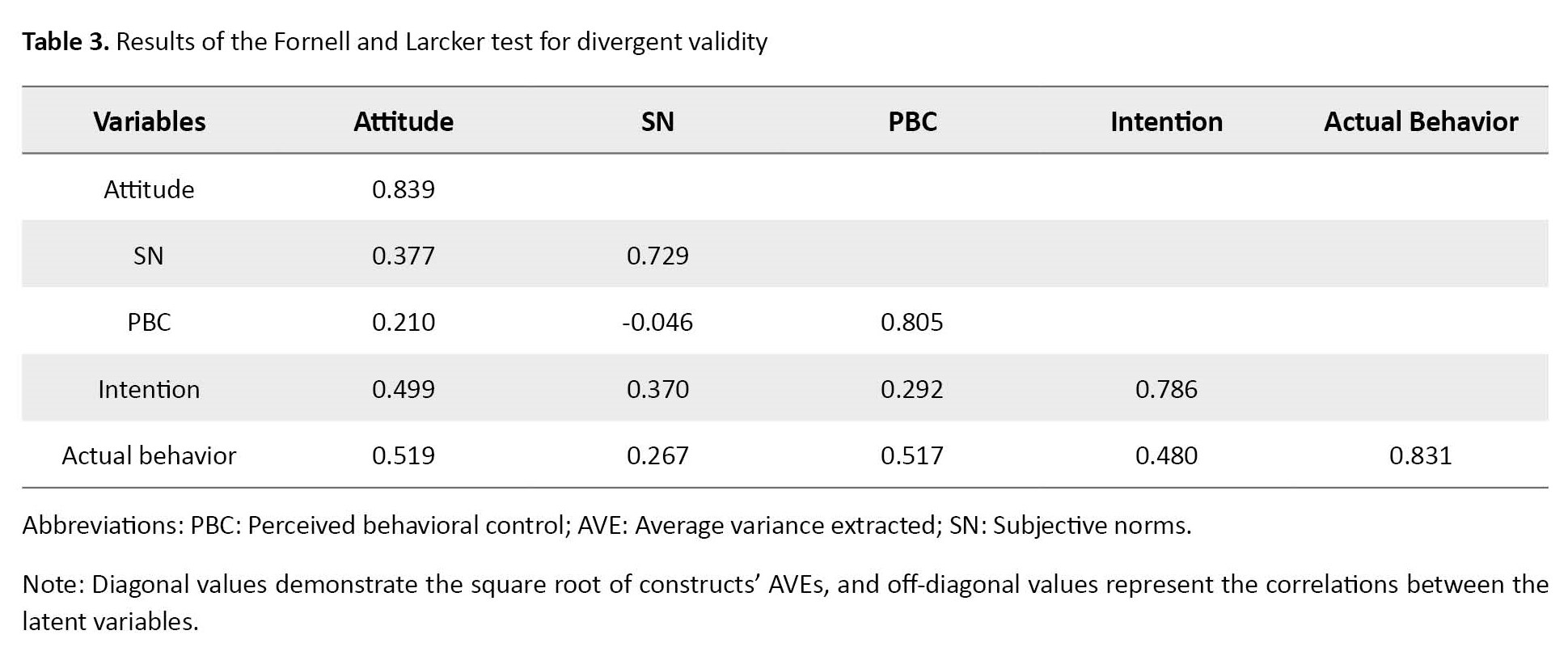
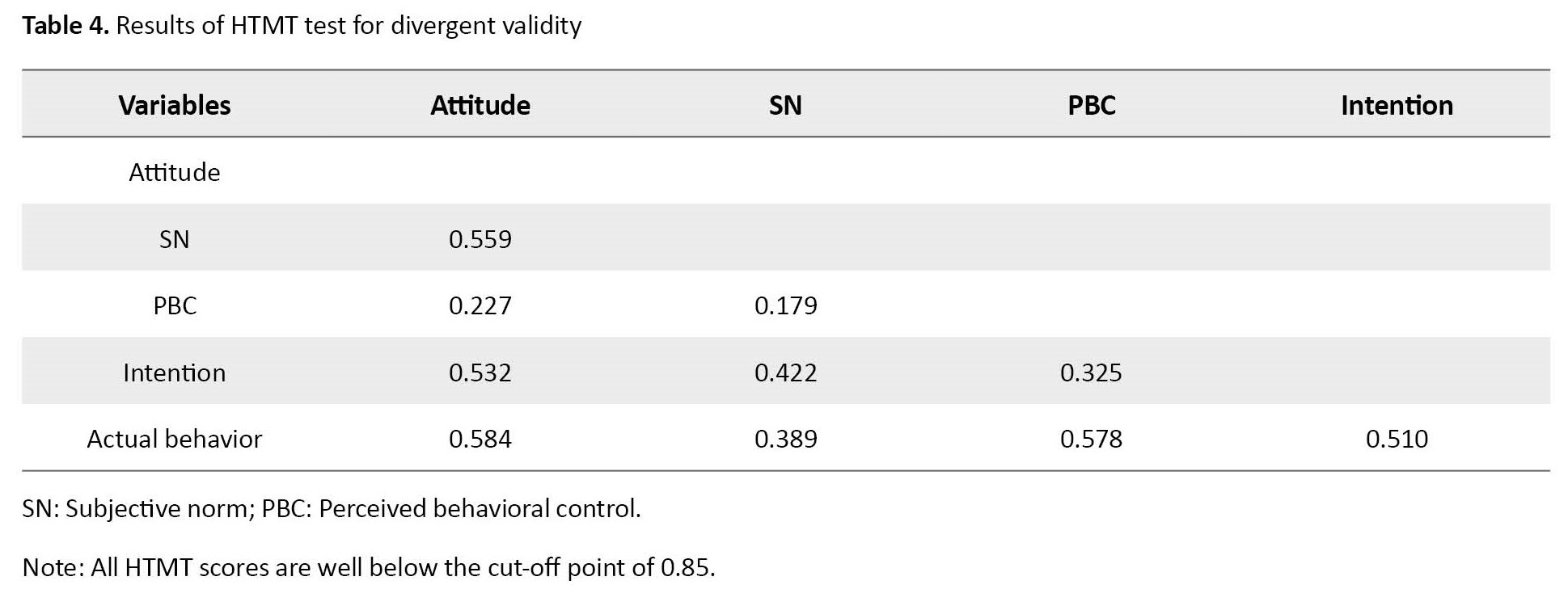
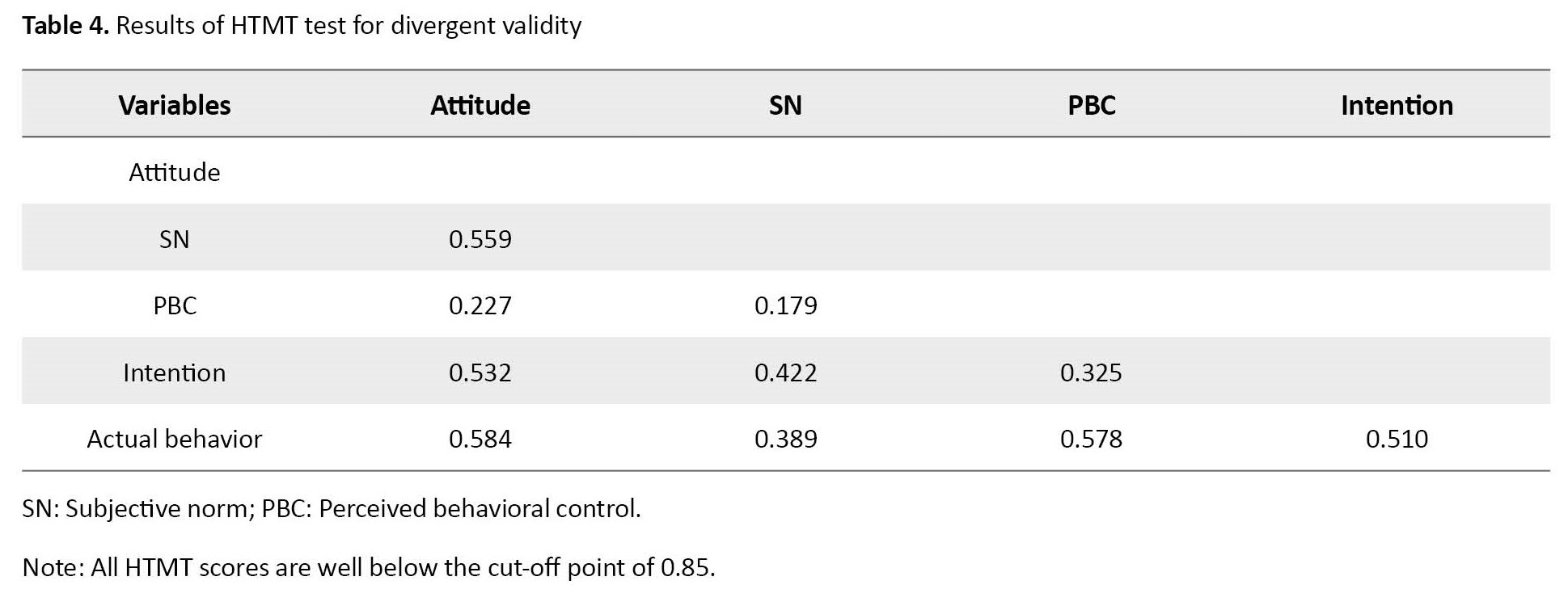
Besides, the results of the Fornell and Larcker test and HTMT, as indicated in Table 4, demonstrate that the measures have divergent validity.
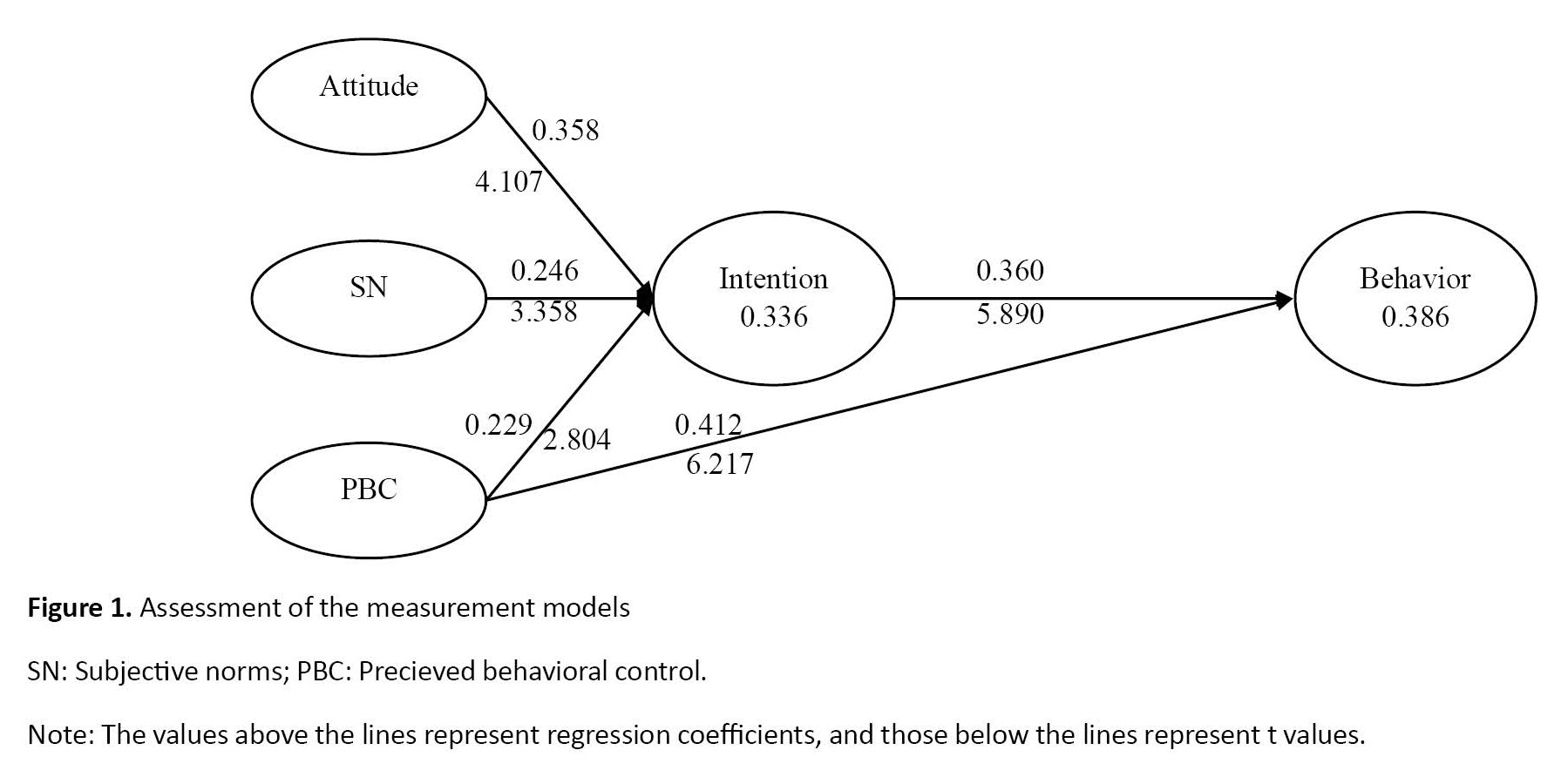
After establishing the validity and reliability of the measures, the structural model assessment was done. The first criterion in evaluating the structural model is the path coefficient. Based on the t-test statistics scores (bootstrapping procedure), the 3 variables of attitude toward training transfer (β=0.358, P=0.001), subjective norms regarding training transfer (β=0.246, P=0.001), and perceived behavioral control over training transfer (β=0.229, P=0.001) have a positive and significant effect on nurses’ training transfer intention. Moreover, two variables of perceived behavioral control (β=0.412, P=0.001) and intention (β=0.360, P=0.001) positively and significantly affect nurses’ actual training transfer behavior. The second criterion in assessing the structural model is the determination coefficient, indicating how the model can predict endogenous variable(s). The TPB predicts approximately 34% of changes in training transfer intention and 39% of actual training transfer behavior, which is considered moderate. The third criterion in evaluating the structural model is Q2 (Figure 1).
Since the onset of the COVID-19 pandemic in December 2019, the disease has dramatically affected millions worldwide [1]. Studies show that about 14% of patients must be hospitalized since they show severe symptoms such as pneumonia, respiratory failure, and even death [2-4]. Reports suggest that mortality due to COVID-19 results from alveolar damage and respiratory loss [5]. Guan et al. reported that about 90% of the patients need oxygen therapy [6]. Therefore, respiratory support, or oxygen therapy, is critical for treating patients with severe symptoms [7]; oxygen therapy is recommended as the first step in treating hypoxemic patients such as COVID-19 [8, 9]. Empirical studies have also demonstrated oxygen therapy’s efficiency in treating COVID patients [10, 11]. In this line, Shen et al. argued that oxygen therapy was instrumental in suppressing the pathogen by disrupting its replication cycle and boosting the immune system [12].
Owing to the paramount importance of oxygen therapy in treating COVID-19 patients, 5 courses of oxygen therapy were held in a hospital in Tehran City, Iran, in 2021 to improve the nurses’ knowledge and skills of oxygen therapy; 164 nurses participated in these courses. Because of the high cost of implementing such courses, the main question is whether nurses use this training in the workplace. Hence, the issue of training transfer, defined as the maintenance and use of learned attitudes, knowledge, and skills in the workplace [13-15], is considered the main criterion of training effectiveness [16, 17]. Training transfer is of the utmost importance to nurses because it allows them to meet the growing and changing demands of the workplace and improve the quality of healthcare services [17, 18].
However, the healthcare sector is lacking in training transfer research [17, 19, 20], and a majority of the training transfer research has been conducted in other settings [17], showing that training transfer is confronted with difficulties in organizations [21]. Hutchins also states that learners use less than 40% of the knowledge and skills learned from the courses [22]. Similarly, Wexley and Latham found that the training transfer rate is about 40% immediately after training, which drops to 25% after 6 months and 15% after 12 months [23]. In the nursing profession, also, the “transfer problem” exists [17]. The reports indicate that in health and hygiene, only a small part of the knowledge and skills acquired in training courses is used in the workplace [24].
Various models have been developed to understand the process of training transfer, among which the systematic model of training transfer is a reference and framework for understanding the training transfer process [15]. Based on this model, various research studies have been conducted and published in training transfer [14, 25, 26]. However, the existing models of training transfer do not emphasize the learners’ intention to transfer their knowledge and skills as a predictor of training transfer behavior [27, 28]. Factoring this element in the theory of planned behavior (TPB) suggests that intention can be the most effective variable in predicting human behavior in all contexts, including the context of training transfer [29].
According to the TPB, training transfer intention and its antecedents, i.e. attitude, subjective norms (SN), and perceived behavioral control (PBC), are the main predictors of behavior. This theory posits that behavior (training transfer) is shaped by intention, which is, in turn, determined by the perception that the behavior is desirable (positive attitude), people who are important to the individual approve of the behavior (SN), and the behavior is feasible that show perceived behavioral control [30]. Therefore, the present study uses the TPB as the main research framework to investigate training transfer behavior among nurses.
Material and Methods
This study used a cross-sectional, correlational research design to answer the research hypotheses. The target population included all nurses working in one of the educational hospitals affiliated with the Shahid Beheshti University, Tehran, Iran (n=722), who participated in 5 oxygen therapy workshops in 2021 (n=283). Of whom a random sample was selected using the formula proposed by Hair et al. [31]. According to this formula, the minimum sample size required to obtain a statistical power of 95% and an R2 value of 0.10 was 103 individuals. However, 143 questionnaires were distributed among the nurses participating in the workshops to compensate for the sample loss.
To collect data, the following two measurement tools were used. TPB questionnaire that was previously validated by researchers [32-35]. This questionnaire with 17 items has 4 constructs: Attitude toward training transfer (5 items), SN regarding training transfer (3 items), PBC over training transfer (4 items), and training transfer intention (5 items). To rank the answers, a 5-point Likert scale was used (1=strongly disagree, 2=disagree, 3=neutral, 4=agree, and 5=strongly agree). Another tool was the oxygen therapy checklist, a 5-item checklist used to assess nurses’ actual training transfer behavior in the field of oxygen therapy. To rank the answers, a scale with 5 options was used (1=very low, 2=low, 3=medium, 4=high, 5=very high). Finally, for both measurement tools, the score of each structure was determined based on the mean score of the items.
Before implementing the survey, the psychometric properties of the scales were examined in terms of face, content, and construct validity. Three medical practitioners assessed the face validity of the scales in terms of readability, comprehensibility, and wording. Some minor modifications were made to the survey based on the expert’s inputs. Afterward, the content validity of the survey was explored. Assessment of content validity involved empirical methods to determine the content validity ratio (CVR), which represents the essentiality of each item, and the content validity index (CVI), which measures the relevance of each item to the underlying construct. In this regard, 6 academicians with publications on TPB and 4 medical practitioners with knowledge and experience in oxygen therapy were selected. The panelists were then asked to rate each item regarding CVR and CVI. A 3-point scale (1=essential, 2=useful but not essential, and 3=not essential) was used to measure CVR. In addition, a 4-point scale (1=not relevant, 2=somewhat relevant, 3=quite relevant, and 4=highly relevant) was used to quantify CVI. Judged by a panel of 10 experts, the minimum values of CVR [36, 37] and CVI [38] must be at least 0.62 and 0.78, respectively. CVR analysis of the oxygen therapy checklist revealed that the scores of items 2, 6, and 9 were below the cut-off point. Hence they were removed from the checklist. However, the CVR and CVI values of other items are satisfactory. Accordingly, items are deemed content valid. Additionally, confirmatory factor analysis was run to assess the construct validity of the scales. Moreover, the questionnaire was pilot-tested on 32 nurses, and the reliability test showed all the scales possess acceptable α values above 70%.
The TPB survey was implemented immediately after the workshops, and 2 weeks after the workshops, the head nurses of the same participants were asked to fill out the oxygen therapy checklist. Head nurses are in direct contact with nurses, hence a good source to rate participants’ oxygen therapy behavior. In this way, head nurses rated participants’ oxygen therapy behavior.
To analyze the data, structural equation modeling was applied using Smart-PLS3 software.
Results
Out of 143 questionnaires, 127 were returned, yielding a response rate of 89%. The results of the descriptive analysis of the samples are given in Table 1.

Structural equation modeling is a two-step process. In the first step, measurement models/factorial structure of the measures are examined to assess the construct validity of the scales. Since all of the measurement models in the present study are reflective, composite reliability and Cronbach α are used to assess internal consistency. Also, factor loading and average variance extracted (AVE) are used to assess convergent validity, and Heterotrait-Monotrait ratio of correlations (HTMT) and Fornell and Larcker to assess divergent validity. After validating the measurement models, the structural model was examined to test the research hypotheses in The second stage. For this purpose, 3 metrics are used: Path coefficient (its value should be significant), determination coefficient (R2), and predictive relevance (Q2); its value should be greater than 0 [31].
A preliminary assessment of the measurement models showed that item 6 of the attitude scale, item 2 of the SN scale, and item 6 of the oxygen therapy checklist had a factor loading below the threshold value. Hence, these items were removed from the model. The clipped measurement models were then re-evaluated. CVR and CVI metrics demonstrate that the measures are valid regarding content validity. Results also show that factor loadings of the items and AVEs of the measures are above the threshold values, indicating that the measurement tools possess convergent validity. Composite reliability and Cronbach α values of the measures surpass the acceptable cut-off points, proving the questionnaires are reliable (Table 2).

The results showed that all measurement models/tools had the desired validity and reliability (Table 3).
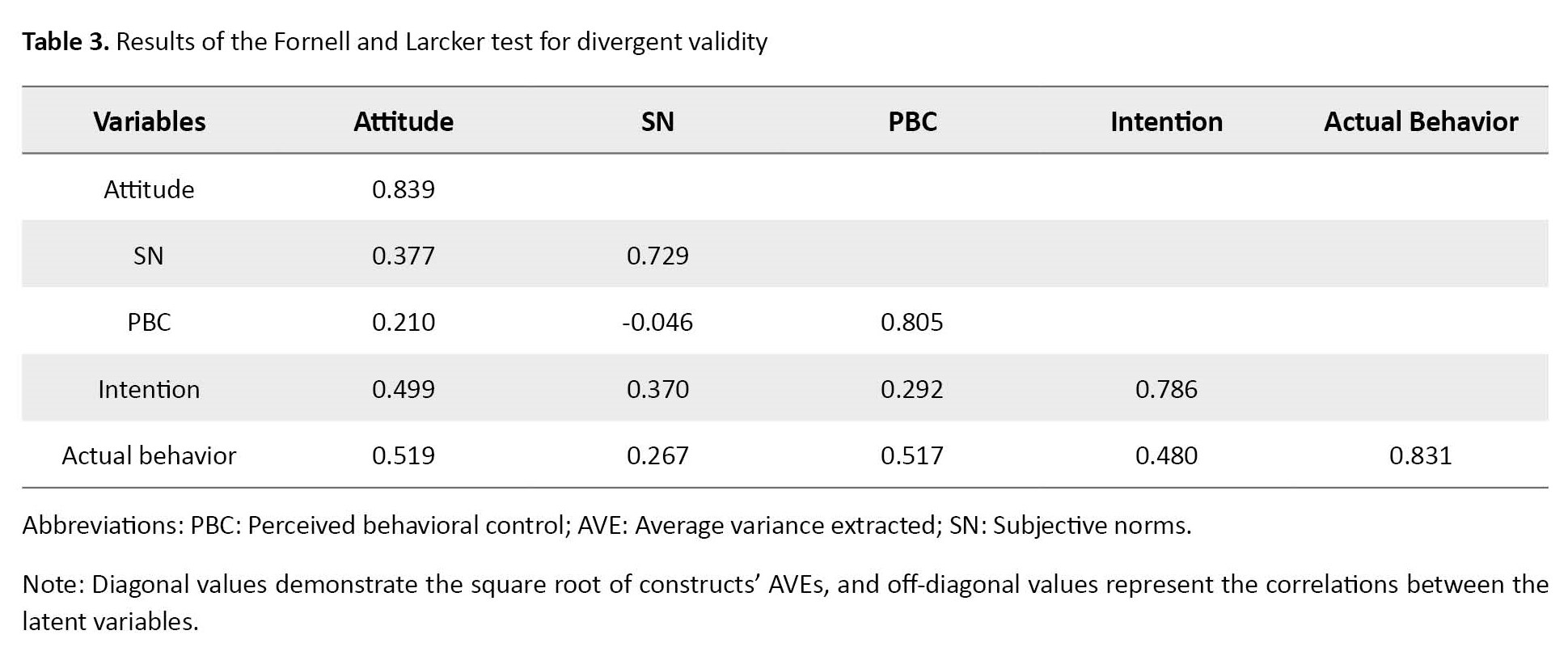
Besides, the results of the Fornell and Larcker test and HTMT, as indicated in Table 4, demonstrate that the measures have divergent validity.
After establishing the validity and reliability of the measures, the structural model assessment was done. The first criterion in evaluating the structural model is the path coefficient. Based on the t-test statistics scores (bootstrapping procedure), the 3 variables of attitude toward training transfer (β=0.358, P=0.001), subjective norms regarding training transfer (β=0.246, P=0.001), and perceived behavioral control over training transfer (β=0.229, P=0.001) have a positive and significant effect on nurses’ training transfer intention. Moreover, two variables of perceived behavioral control (β=0.412, P=0.001) and intention (β=0.360, P=0.001) positively and significantly affect nurses’ actual training transfer behavior. The second criterion in assessing the structural model is the determination coefficient, indicating how the model can predict endogenous variable(s). The TPB predicts approximately 34% of changes in training transfer intention and 39% of actual training transfer behavior, which is considered moderate. The third criterion in evaluating the structural model is Q2 (Figure 1).
According to the results, the value of this index for the endogenous variables of intention and actual behavior is 0.177 and 0.228, respectively, which is greater than 0.
Discussion
This study used the TPB to predict the nurses’ training transfer behavior. Overall, the results showed that the TPB could predict the nurses’ actual use of oxygen therapy techniques. In the following, the results are discussed one by one.
The first research hypothesis states that the nurses’ positive attitude toward oxygen therapy use predicts their intention toward oxygen therapy use. The results of this study showed that the nurses’ attitude has a positive and significant effect on their intention toward oxygen therapy use. This result aligns with the TPB and the previous empirical studies [39, 40]. Previous research has shown that attitude is the most consistent predictor of behavioral intention. Attitude reflects how much the nurse attributes positive consequences to training transfer. Therefore, if nurses think oxygen therapy improves patients’ health, their desire and motivation will increase.
The second research hypothesis states that the nurses’ SN regarding oxygen therapy use predicts their intention toward oxygen therapy use. Examining this hypothesis shows that the nurses’ SN positively and significantly affects their intention toward oxygen therapy use. This result conflicts with the research by Cheng et al. [39], Lumpe et al. [40], Saleh and Albion [41], and in line of Shiue et al results [42]. SN indicates the extent to which nurses expect their co-workers to apply what they have learned from attending workshops. Regarding this result, Iran is a collectivist society, and in such societies, social pressure makes individuals comply with collective norms and cooperate with the group. That is why SN has a significant positive effect on nurses’ training transfer.
The third research hypothesis states that the nurses’ PBC over training transfer predicts their intention toward oxygen therapy use. The results show that the nurses’ PBC positively and significantly affects their intention toward oxygen therapy use. This result is in line with the TPB and the results of the previous empirical studies [39, 40, 43, 44, 45, 46]. However, they conflict with the research results by Salleh and Albion [41] and Shiue [42]. PBC indicates that the nurses’ possession of the knowledge, skills, time, and equipment of using oxygen therapy strengthens their motivation to use it.
The fourth study hypothesis states that the nurses’ PBC over oxygen therapy predicts their actual use of oxygen therapy. The results showed that the nurses’ PBC positively and significantly affects their actual use of oxygen therapy. This result aligns with the TPB and the results of the previous empirical studies by Cheng et al. [39] and Gegenfurtner and Testers [46].
The fifth research hypothesis states that the nurses’ intention toward oxygen therapy use predicts their actual use. Examining this hypothesis shows that the nurses’ oxygen therapy training transfer intention positively and significantly affects their actual use of oxygen therapy. This result is in line with the TPB and the previous empirical studies [39, 42, 46, 47]. According to the TPB, intention resembles motivation and desire. If the nurses are eager to use oxygen therapy, they will likely step in that direction.
The contribution of our study to the existing knowledge is twofold. From a theoretical standpoint, the present research is among a few studies that explore the TPB and shows that the TPB can predict the training transfer of oxygen therapy to the workplace. From a practical standpoint, this study can guide managers and officials in health and hygiene. As shown, attitude is the strongest variable affecting behavioral intention. Therefore, managers need to strengthen the nurses’ attitudes toward using oxygen therapy. In this regard, managers can produce educational content on oxygen therapy and its application and importance. Furthermore, the present study showed that PBC affects behavioral intention and actual behavior. In this regard, hospital officials can empower nursing staff through training workshops. In addition, managers can enhance nurses’ sense of control over oxygen therapy by equipping the hospital with the tools and equipment needed to perform oxygen therapy. Given SN’s positive and significant effect on oxygen therapy transfer intention, managers can also set and communicate expectations about oxygen therapy to nursing staff.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Mazandaran (No.: IR.UMZ.REC.1400.014). Before conducting the study, the participants were informed about the study’s objectives to participate with full knowledge and consent, and written informed consent was obtained from all participants. They were allowed to withdraw from the study at any stage. Participants were also assured that their data and identities would remain confidential. In addition, we confirmed that all methods were performed following the relevant guidelines and regulations (Declaration of Helsinki).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design, preparing the first draft of the manuscript and final approval: All authors; Data collection: Javad Rokni and Hatam Faraji Dehsorkhi; Data analysis, data interpretation: Ali Asghar Hayat, Hatam Faraji Dehsorkhi, and Mostafa Azizi Shamami.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Hereby, the nursing staff participating in the study are fully thanked and appreciated.
References
Discussion
This study used the TPB to predict the nurses’ training transfer behavior. Overall, the results showed that the TPB could predict the nurses’ actual use of oxygen therapy techniques. In the following, the results are discussed one by one.
The first research hypothesis states that the nurses’ positive attitude toward oxygen therapy use predicts their intention toward oxygen therapy use. The results of this study showed that the nurses’ attitude has a positive and significant effect on their intention toward oxygen therapy use. This result aligns with the TPB and the previous empirical studies [39, 40]. Previous research has shown that attitude is the most consistent predictor of behavioral intention. Attitude reflects how much the nurse attributes positive consequences to training transfer. Therefore, if nurses think oxygen therapy improves patients’ health, their desire and motivation will increase.
The second research hypothesis states that the nurses’ SN regarding oxygen therapy use predicts their intention toward oxygen therapy use. Examining this hypothesis shows that the nurses’ SN positively and significantly affects their intention toward oxygen therapy use. This result conflicts with the research by Cheng et al. [39], Lumpe et al. [40], Saleh and Albion [41], and in line of Shiue et al results [42]. SN indicates the extent to which nurses expect their co-workers to apply what they have learned from attending workshops. Regarding this result, Iran is a collectivist society, and in such societies, social pressure makes individuals comply with collective norms and cooperate with the group. That is why SN has a significant positive effect on nurses’ training transfer.
The third research hypothesis states that the nurses’ PBC over training transfer predicts their intention toward oxygen therapy use. The results show that the nurses’ PBC positively and significantly affects their intention toward oxygen therapy use. This result is in line with the TPB and the results of the previous empirical studies [39, 40, 43, 44, 45, 46]. However, they conflict with the research results by Salleh and Albion [41] and Shiue [42]. PBC indicates that the nurses’ possession of the knowledge, skills, time, and equipment of using oxygen therapy strengthens their motivation to use it.
The fourth study hypothesis states that the nurses’ PBC over oxygen therapy predicts their actual use of oxygen therapy. The results showed that the nurses’ PBC positively and significantly affects their actual use of oxygen therapy. This result aligns with the TPB and the results of the previous empirical studies by Cheng et al. [39] and Gegenfurtner and Testers [46].
The fifth research hypothesis states that the nurses’ intention toward oxygen therapy use predicts their actual use. Examining this hypothesis shows that the nurses’ oxygen therapy training transfer intention positively and significantly affects their actual use of oxygen therapy. This result is in line with the TPB and the previous empirical studies [39, 42, 46, 47]. According to the TPB, intention resembles motivation and desire. If the nurses are eager to use oxygen therapy, they will likely step in that direction.
The contribution of our study to the existing knowledge is twofold. From a theoretical standpoint, the present research is among a few studies that explore the TPB and shows that the TPB can predict the training transfer of oxygen therapy to the workplace. From a practical standpoint, this study can guide managers and officials in health and hygiene. As shown, attitude is the strongest variable affecting behavioral intention. Therefore, managers need to strengthen the nurses’ attitudes toward using oxygen therapy. In this regard, managers can produce educational content on oxygen therapy and its application and importance. Furthermore, the present study showed that PBC affects behavioral intention and actual behavior. In this regard, hospital officials can empower nursing staff through training workshops. In addition, managers can enhance nurses’ sense of control over oxygen therapy by equipping the hospital with the tools and equipment needed to perform oxygen therapy. Given SN’s positive and significant effect on oxygen therapy transfer intention, managers can also set and communicate expectations about oxygen therapy to nursing staff.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Mazandaran (No.: IR.UMZ.REC.1400.014). Before conducting the study, the participants were informed about the study’s objectives to participate with full knowledge and consent, and written informed consent was obtained from all participants. They were allowed to withdraw from the study at any stage. Participants were also assured that their data and identities would remain confidential. In addition, we confirmed that all methods were performed following the relevant guidelines and regulations (Declaration of Helsinki).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design, preparing the first draft of the manuscript and final approval: All authors; Data collection: Javad Rokni and Hatam Faraji Dehsorkhi; Data analysis, data interpretation: Ali Asghar Hayat, Hatam Faraji Dehsorkhi, and Mostafa Azizi Shamami.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Hereby, the nursing staff participating in the study are fully thanked and appreciated.
References
- Lee M, Kang BA, You M. Knowledge, attitudes, and practices (KAP) toward COVID-19: A cross-sectional study in South Korea. BMC Public Health. 2021; 21(1):295. [DOI:10.1186/s12889-021-10285-y] [PMID]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497-506. [DOI:10.1016/S0140-6736(20)30183-5] [PMID]
- Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 2020; 133(09):1025-31. [DOI:10.1097/CM9.0000000000000744] [PMID]
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061-9. [DOI:10.1001/jama.2020.1585] [PMID]
- Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: Experience from Jiangsu Province. Ann Intensive Care. 2020; 10(1):33. [DOI:10.1186/s13613-020-00650-2] [PMID]
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708-20. [DOI:10.1056/NEJMoa2002032] [PMID]
- Tabashi S, Mirkheshti A, Dahi M, Abtahi D, Vosoughian M, Sayyadi S, et al. Supplemental oxygen therapy and non-invasive ventilation in corona virus disease (COVID-19). J Cell Mol Anesth. 2020; 5(1):27-31. [DOI:10.22037/jcma.v5i1.29689]
- Greenland JR, Michelow MD, Wang L, London MJ. COVID-19 infection: Implications for perioperative and critical care physicians. Anesthesiology. 2020; 132(6):1346-61. [DOI:10.1097/ALN.0000000000003303] [PMID]
- Jiang B, Wei H. Oxygen therapy strategies and techniques to treat hypoxia in COVID-19 patients. Eur Rev Med Pharmacol Sci. 2020; 24(19):10239-46. [DOI:10.26355%2Feurrev_202010_23248]
- Thibodeaux K, Speyrer M, Raza A, Yaakov R, Serena TE. Hyperbaric oxygen therapy in preventing mechanical ventilation in COVID-19 patients: A retrospective case series. J Wound Care. 2020; 29(Sup5a):S4-8. [DOI:10.12968/jowc.2020.29.Sup5a.S4] [PMID]
- Ospina-Tascón GA, Calderón-Tapia LE, García AF, Zarama V, Gómez-Álvarez F, Álvarez-Saa T, et al. Effect of high-flow oxygen therapy vs conventional oxygen therapy on invasive mechanical ventilation and clinical recovery in patients with severe COVID-19: A randomized clinical trial. JAMA. 2022; 326(21):2161-71. [PMID]
- Shen C, Yue X, Wang J, Shi C, Li W. Nocturnal oxygen therapy as an option for early COVID-19. Int J Infect Dis. 2020; 98:176-9. [DOI:10.1016/j.ijid.2020.06.080] [PMID]
- Bates R, Holton III EF, Hatala JP. A revised learning transfer system inventory: Factorial replication and validation. Hum Resour Dev Int. 2012; 15(5):549-69. [DOI:10.1080/13678868.2012.726872]
- Blume BD, Ford JK, Baldwin TT, Huang JL. Transfer of training: A meta-analytic review. J Manage 2010; 36(4):1065-105. [DOI:10.1177/0149206309352880]
- Baldwin TT, Ford JK. Transfer of training: A review and directions for future research. Pers Psychol. 1988; 41(1):63-105. [DOI:10.1111/j.1744-6570.1988.tb00632.x]
- Abbad G, Andrade JE, Sallorenzo LH. Self-assessment of training impact at work: Validation of a measurement scale. Interam J Psychol. 2004; 38(2):277-84. [Link]
- Ma F, Bai Y, Bai Y, Ma W, Yang X, Li J. Factors influencing training transfer in nursing profession: A qualitative study. BMC Med Educ. 2018; 18(1):44. [DOI:10.1186/s12909-018-1149-7] [PMID]
- Lauder W, Reynolds W, Angus N. Transfer of knowledge and skills: Some implications for nursing and nurse education. Nurse Educ Today. 1999; 19(6):480-7. [DOI:10.1054/nedt.1999.0338] [PMID]
- Clarke N. 14 The limitations of in-service training in social services. In: Sambrook S, Stewart J, editors. Human resource development in the public sector. Oxfordshire: Routledge; 2007. [Link]
- Conway J, McMillan M, Becker J. Implementing workforce development in health care: A conceptual framework to guide and evaluate health service reform. Hum Resour Dev Int. 2006; 9(1):129-39. [DOI:10.1080/13678860500522975]
- Broad ML, Newstrom JW. Transfer of training: Action-packed strategies to ensure high payoff from training investments. New York: Basic Books; 2000. [Link]
- Hutchins HM. In the trainer’s voice: A study of training transfer practices. Perform Improv Quart. 2009; 22(1):69-93. [DOI:10.1002/piq.20046]
- Wexley KN, Latham GP. Developing and training human resources in organizations. New York: Harper Collins; 1991. [Link]
- Gordon LJ, Rees CE, Ker JS, Cleland J. Dimensions, discourses and differences: Trainees conceptualising health care leadership and followership. Med Educ. 2015; 49(12):1248-62. [DOI:10.1111/medu.12832] [PMID]
- Burke LA, Hutchins HM. A study of best practices in training transfer and proposed model of transfer. Hum Resour Dev Quart. 2008; 19(2):107-28. [DOI:10.1002/hrdq.1230]
- Liebermann S, Hoffmann S. The impact of practical relevance on training transfer: Evidence from a service quality training program for German bank clerks. Int J Train Dev. 2008; 12(2):74-86. [DOI:10.1111/j.1468-2419.2008.00296.x]
- Cheng EW, Hampson I. Transfer of training: A review and new insights. Int J Manag Rev. 2008; 10(4):327-41. [DOI:10.1111/j.1468-2370.2007.00230.x]
- Gegenfurtner A, Knogler M, Schwab S. Transfer interest: Measuring interest in training content and interest in training transfer. Hum Resour Dev Int. 2020; 23(2):146-67. [DOI:10.1080/13678868.2019.1644002]
- Ajzen I. The theory of planned behavior: Frequently asked questions. Hum Behav Emerg Tech. 2020; 2:314-24. [DOI:10.1002/hbe2.195]
- Dorce LC, da Silva MC, Mauad JR, de Faria Domingues CH, Borges JA. Extending the theory of planned behavior to understand consumer purchase behavior for organic vegetables in Brazil: The role of perceived health benefits, perceived sustainability benefits and perceived price. Food Qual Prefer. 2021; 91:104191. [DOI:10.1016/j.foodqual.2021.104191]
- Hair Jr JF, Hult GTM, Ringle CM, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM). California: Sage Publications; 2021. [DOI:10.1080/1743727X.2015.1005806]
- Shoham A. Predicting trainees’ intentions to transfer training: An application of the theory of planned behaviour. Montreal: University of Montreal; 2008. [Link]
- Cheng WL. Transfer of training: Using the theory of planned behavior [PhD dissertation]. Sydney: Australian School of Business; 2013. [DOI:10.26190/unsworks/2525]
- Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: A comparison of two theoretical models. Manag Sci. 1989; 35(8):903-1028. [DOI:10.1287/mnsc.35.8.982]
- Thompson RL, Higgins CA, Howell JM. Personal computing: Toward a conceptual model of utilization. MIS Q. 1991; 15(1):125-43. [DOI:10.2307/249443]
- Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975; 28(4):563-75. [DOI:10.1111/j.1744-6570.1975.tb01393.x]
- Burns J, Yates R. An examination of the reliability and validity of the recovery capital questionnaire (RCQ). Drug Alcohol Depend. 2022; 232:109329. [DOI:10.1016/j.drugalcdep.2022.109329] [PMID]
- Lynn MR. Determination and quantification of content validity. Nurs Res. 1986; 35(6):382-5. [DOI:10.1097/00006199-198611000-00017] [PMID]
- Cheng EW, Sanders K, Hampson I. An intention-based model of transfer of training. Manage Res Rev. 2015; 38(8):908-28. [DOI:10.1108/MRR-05-2014-0107]
- Lumpe AT, Haney JJ, Czerniak CM. Science teacher beliefs and intentions to implement science-technology-society (STS) in the classroom. J Sci Teacher Educ. 1998; 9(1):1-24. [DOI:10.1023/A:1009438021848]
- Salleh S, Albion P Using the theory of planned behaviour to predict Bruneian teachers’ intentions to use ICT in teaching. Proceedings of SITE 2004--Society for Information Technology & Teacher Education International Conference. 2004; 1389-96. [Link]
- Shiue YM. Investigating the sources of teachers’ instructional technology use through the decomposed theory of planned behavior. J Educ Comput Res. 2007; 36(4):425-53. [DOI:10.2190/A407-22RR-50X6-2830]
- Lee J, Cerreto FA, Lee J. Theory of planned behavior and teachers’ decisions regarding use of educational technology. J Educ Techno Soc. 2010; 13(1):152-64. [Link]
- Teo T, Zhou M, Noyes J. Teachers and technology: Development of an extended theory of planned behavior. Educ Technol Res Dev. 2016; 64(6):1033-52. [DOI:10.1007/s11423-016-9446-5]
- Jacot A, Raemdonck I, Frenay M. Intra-individual differences in offenders’ motivation and behavioral change after a driver rehabilitation program. Traffic Psychol Behav. 2018; 58:302-18. [DOI:10.1016/j.trf.2018.05.026]
- Gegenfurtner A, Testers L. Transfer of training among non-traditional students in higher education: Testing the theory of planned behavior. Front Educ. 2022; 7:1-7. [DOI:10.3389/feduc.2022.928996]
- Lingappa AK, Kiran KK, Oommen Mathew A. Safety training transfer in chemical manufacturing: The role of personality traits and learning motivation. Cogent Bus Manag. 2020; 7(1):1835335. [DOI:10.1080/23311975.2020.1835335]
Article Type : Research |
Subject:
Special
Received: 2023/07/3 | Accepted: 2023/06/29 | Published: 2023/06/29
Received: 2023/07/3 | Accepted: 2023/06/29 | Published: 2023/06/29
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |