Mon, Jul 22, 2024
Volume 33, Issue 4 (9-2023)
JHNM 2023, 33(4): 288-296 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Feizi Mangoodehi N, Mirhadyan L, Mosaffa Khomami H, Kazemnezhad Leili E. Understanding Family-centered Care and Related Factors From the Perspective of Mothers of Children With Autism Spectrum Disorder. JHNM 2023; 33 (4) :288-296
URL: http://hnmj.gums.ac.ir/article-1-2195-en.html
URL: http://hnmj.gums.ac.ir/article-1-2195-en.html
1- Nursing (MSN), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,Lm30075@yahoo.com
3- Assistant Professor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatistics, Social Determinants of Health Research Center (SDHRC), Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Assistant Professor, Department of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Associate Professor, Department of Biostatistics, Social Determinants of Health Research Center (SDHRC), Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 498 kb]
(211 Downloads)
| Abstract (HTML) (505 Views)
Full-Text: (139 Views)
Introduction
Autism spectrum disorder (ASD) is a developmental disorder that typically manifests in childhood and is characterized by stereotyped behaviors, excitability, destructive behaviors, and challenges in social communication, often occurring before age 3 [1, 2]. This disorder affects brain function, and the severity of symptoms may vary across 3 areas: Social interaction, communication, and repetitive behaviors [3]. Approximately 6 out of every 1000 children are affected by some form of autism spectrum disorder [4]. In Iran, the prevalence was reported as 2.95 per 10000 children in 2014 [5].
The challenges of an ASD child’s growth and development significantly impact the family system [6, 7]. Thus, besides focusing on the child with special needs, attention should be directed toward families with such needs. The family-centered approach emerges as promising to improve medical services and enhance satisfaction among families with children with autism spectrum disorder. This approach emphasizes mutual respect, acceptance of family choices, service exclusivity, and flexibility, family participation in decision-making, provision of necessary information and knowledge, and efforts to empower family cooperation and communication between the family and therapists [8].
Family-centered care comprises services tailored to children with special needs and their families. This approach underscores family involvement in decision-making, cooperation, and communication between the family and therapists, as well as mutual respect, acceptance of family choices, family support, service flexibility, and efforts to empower families. It has become a cornerstone of many early intervention and rehabilitation programs [9]. Family-centered care reduces anxiety and tension associated with treatment, shortens recovery time, and improves patient cooperation in care implementation. Moreover, it enhances the ability to address clients’ problems and issues, reduces situational anxiety in mothers, and leads to better clinical decision-making and follow-up in child nursing. Family-centered care fosters family cooperation with therapists, recognizes the family’s capacity and capability, and enhances communication among care team members [10, 11, 12, 13].
The perception of family-centered care can be influenced by factors such as an individual’s experiences, beliefs, convictions, and care standards [10]. Mothers’ individual and social factors are also linked to their perception of family-centered care [2, 10, 14, 15]. Variables like age, parents’ education, economic status, insurance adequacy, understanding of the disease and its severity in the family, the health status of family members, presence of healthy or chronically-ill siblings alongside the child with ASD, government financial support for care services, and government policies related to receiving family-centered care can all impact the quality of care received [12, 16].
Given their scope of work, community health nurses can improve the receipt of family-centered care by playing diverse roles within families with special needs, including those with ASD children. However, this effort requires a thorough understanding of the existing situation and surrounding factors. Therefore, due to the scarcity of research conducted in Iran, particularly in Guilan Province, we aimed to explore the understanding of family-centered care and its related factors among the mothers of children with ASD in Rasht City, Iran.
Materials and Methods
This research is a cross-sectional analytical study conducted in educational and rehabilitation centers covered by the Welfare Organization in Rasht during 2020. The research population comprised all mothers with children under 18 years diagnosed with ASD in Rasht, receiving care at the centers under the Rasht Welfare Organization. The inclusion criteria for the study included having a child under 18 with ASD, caring for the child at home, living with a husband, and providing consent to participate. The exclusion criteria comprised incomplete questionnaire responses or confusion in completing the questionnaire. The sampling method employed was a census, and out of the total research population of 264 people, 183 individuals (69.31%) willingly participated in the study.
The study data were collected using a two-part questionnaire. The first part assessed individual-family characteristics and factors related to understanding family-centered care. They included the age of the mother and father, the age of the child with ASD, the number of children in the family, the age at which ASD was diagnosed, the family’s monthly income and its sufficiency, the mother’s and father’s occupations and education levels, sex and rank of the child with ASD, the severity of ASD, type of health insurance and its sufficiency, family residence, and supplementary insurance for the child with ASD. The second part included the 20-item questionnaire of measure of processes of care, which was used to investigate the understanding of family-centered care from the perspective of mothers of children with ASD.
The questionnaire consists of 20 questions in 5 aspects: Empowerment and participation, providing general information, providing specific information about the child, comprehensiveness and coordination of services for the child and family, and respectful and supportive care. This tool has been translated and validated in several countries to assess the understanding of family-centered care by parents of children with chronic diseases and various care team members (e.g. doctors, nurses, psychologists, therapists, and social workers) [17, 18]. Given that this tool effectively covers the concepts of family-oriented care, it has been used in numerous similar studies [2, 19, 20].
The questionnaire is rated on a 7-point Likert scale, ranging from “never” with a score of 1 to “very much” with a score of 7. The Persian version of this instrument was used in the present study [9]. Due to the COVID-19 pandemic, data collection was conducted either in person by adhering to health protocols or via telephone with the research participants, following coordination with the Guilan Welfare Province and identifying the care centers covered by the Welfare Organization. The inclusion criteria were completed within 3 months. Of the participants, 30(16.39%) completed the questionnaire in person, and 153(83.61%) completed it by telephone due to the pandemic. Each questionnaire took approximately 15 to 20 minutes to complete.
The collected data were analyzed using SPSS software, version 24 at a significance level of 0.05. Quantitative variables were presented as Mean±SD, while qualitative variables were expressed as percentage frequency. To determine the correlation of study variables, the Pearson correlation, independent t-test, and analyses of variance were employed. Additionally, the multiple linear regression model was utilized to identify factors related to the perception score of family-centered care while controlling for individual-family factors.
Result
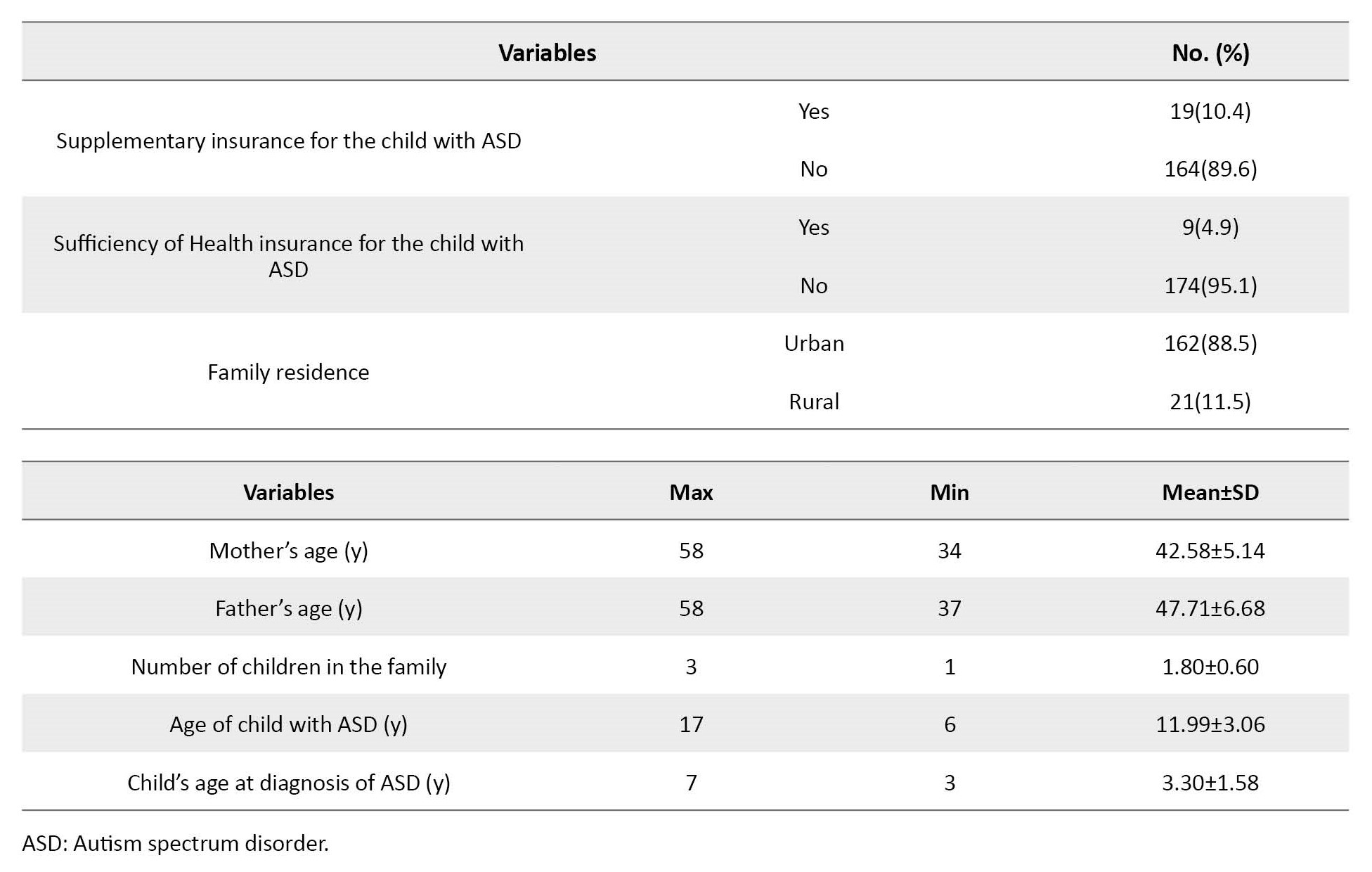
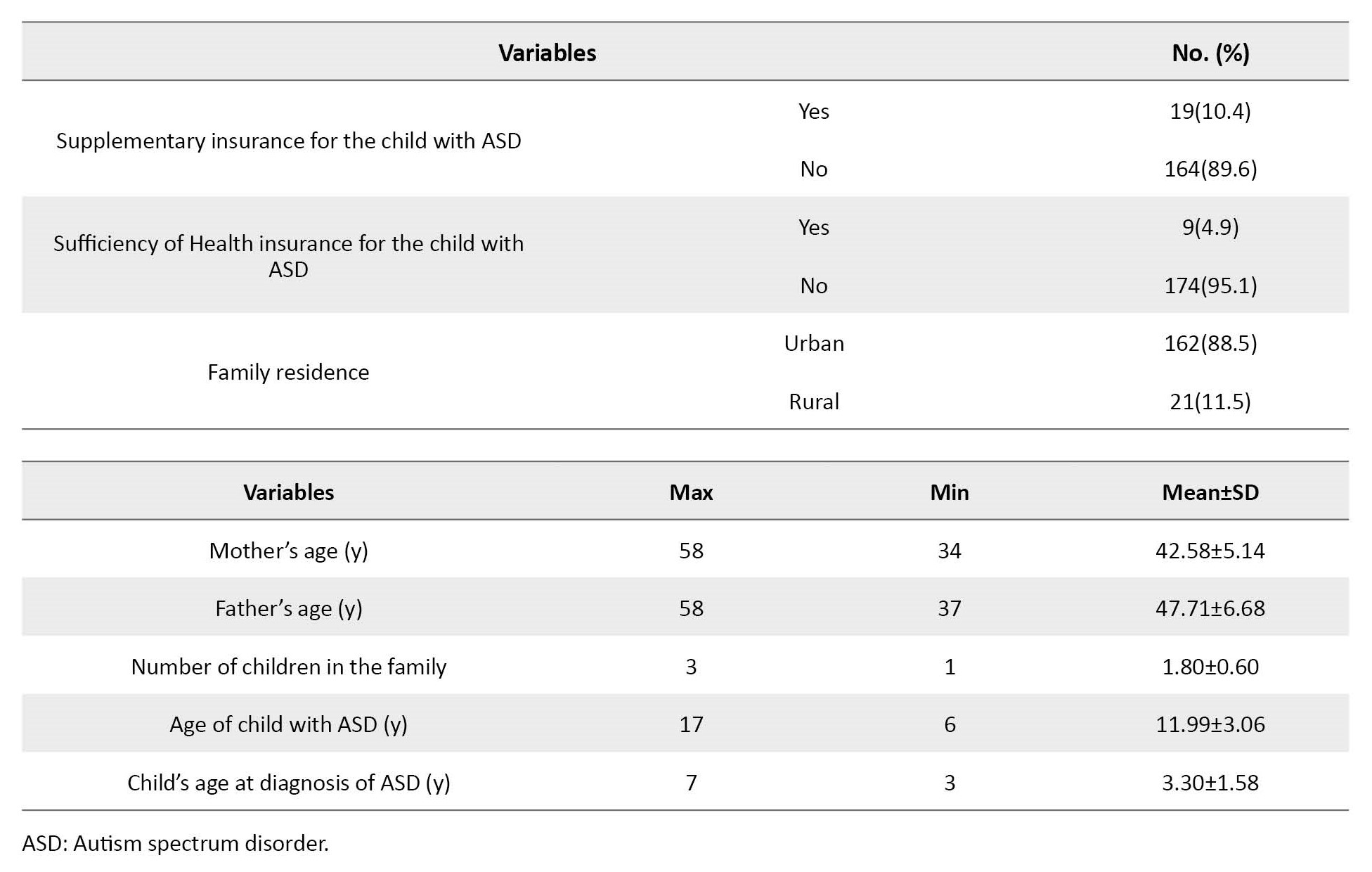
The research findings indicate that 183 participants (69.31%) met the study criteria, with an Mean±SD age of 58.42±14.5 years. Most mothers (41%) had a high school diploma. Many participants (54.6%) had children diagnosed with severe ASD, a male gender predominance (82%), and an Mean±SD age of 11.99±3.06. Additional personal and social information can be found in Table 1.

The Mean±SD of the scores obtained in the family-centered care aspects, from the highest to lowest, were as follows: “Specific information”, 4.55±2.06; “respect and support”, 4.08±1.82; “comprehensiveness and coordination” of services, 4.03±1.99; “empowerment and participation”, 3.77±1.87; and “general information”, 3.45±1.88. Among the quantitative variables, the number of children in the family showed significant correlations with empowerment and participation (P=0.002, r=0.226), general information (P=0.001, r=0.322), specific information (P=0.001, r=0.327), comprehensiveness and coordination (P=0.001, r=0.370), and respect and support (P=0.001, r=0.200). Additionally, the age of the child at the time of ASD diagnosis exhibited significant correlations with empowerment and participation (P=0.001, r=-0.214), general information (P=0.001, r=0.441), specific information (P=0.001, r=0.462), comprehensiveness and coordination (P=0.001, r=-0.404), and respect and support (P=0.001, r=-0.378). Moreover, the father’s age showed statistically significant correlations with general information (P=0.001, r=-0.201), specific information (P=0.028, r=-0.162), comprehensiveness and coordination (P=0.001, r=-0.233), and respect and support (P=0.01, r=-0.191).
The independent t-test and chi-square test revealed significant differences in scores obtained across all 5 aspects according to certain studied variables. Notably, the score of empowerment and participation differed significantly based on the mother’s occupation (P=0.001) and the gender of the child with ASD (P<0.05). The score of general information significantly differed based on the rank of the child with ASD (P=0.009) and the family’s place of residence (P=0.001). Additionally, the score of comprehensiveness and coordination significantly differed based on insurance sufficiency (P=0.001) and supplementary insurance (P=0.001), and the score of respect and support aspect significantly differed based on the family’s place of residence (P=0.001).
One-way analysis of the variance indicated significant differences in scores obtained across all 5 aspects according to certain studied variables. For instance, the score of empowerment and participation differed based on the father’s education level (sub-diploma and diploma, P=0.001; university graduate and diploma, P=0.001) and occupation (retired and freelance, P=0.01). The score of general information significantly differed based on the mother’s education level (undergraduate and university education, P=0.01) and the father’s occupation (retired and freelance, P=0.01). Additionally, the score of specific information aspects significantly differed based on the severity of ASD (mild and moderate, P=0.01; mild and severe, P=0.01). The score of comprehensiveness and coordination significantly differed based on the severity of ASD (mild and moderate, P=0.001; mild and severe, P=0.001) and the type of child’s health insurance (medical service insurance and social security insurance, P=0.001). Finally, the mean score in the aspect of respect and support significantly differed based on the severity of ASD (mild and moderate, P=0.001; mild and severe, P=0.001) and the type of health insurance (medical service insurance and social security insurance, P=0.001; medical services insurance and no insurance, P=0.02).
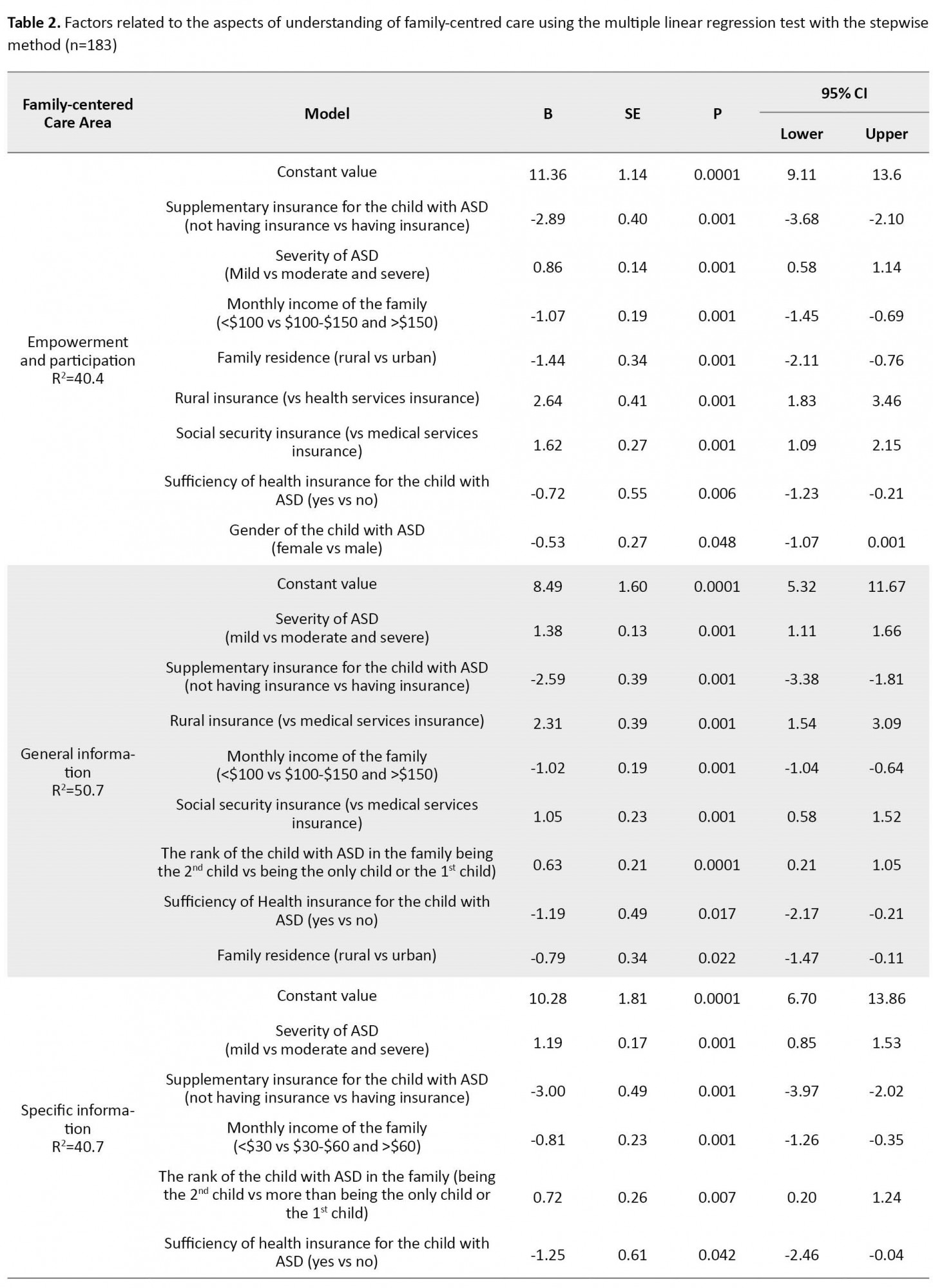
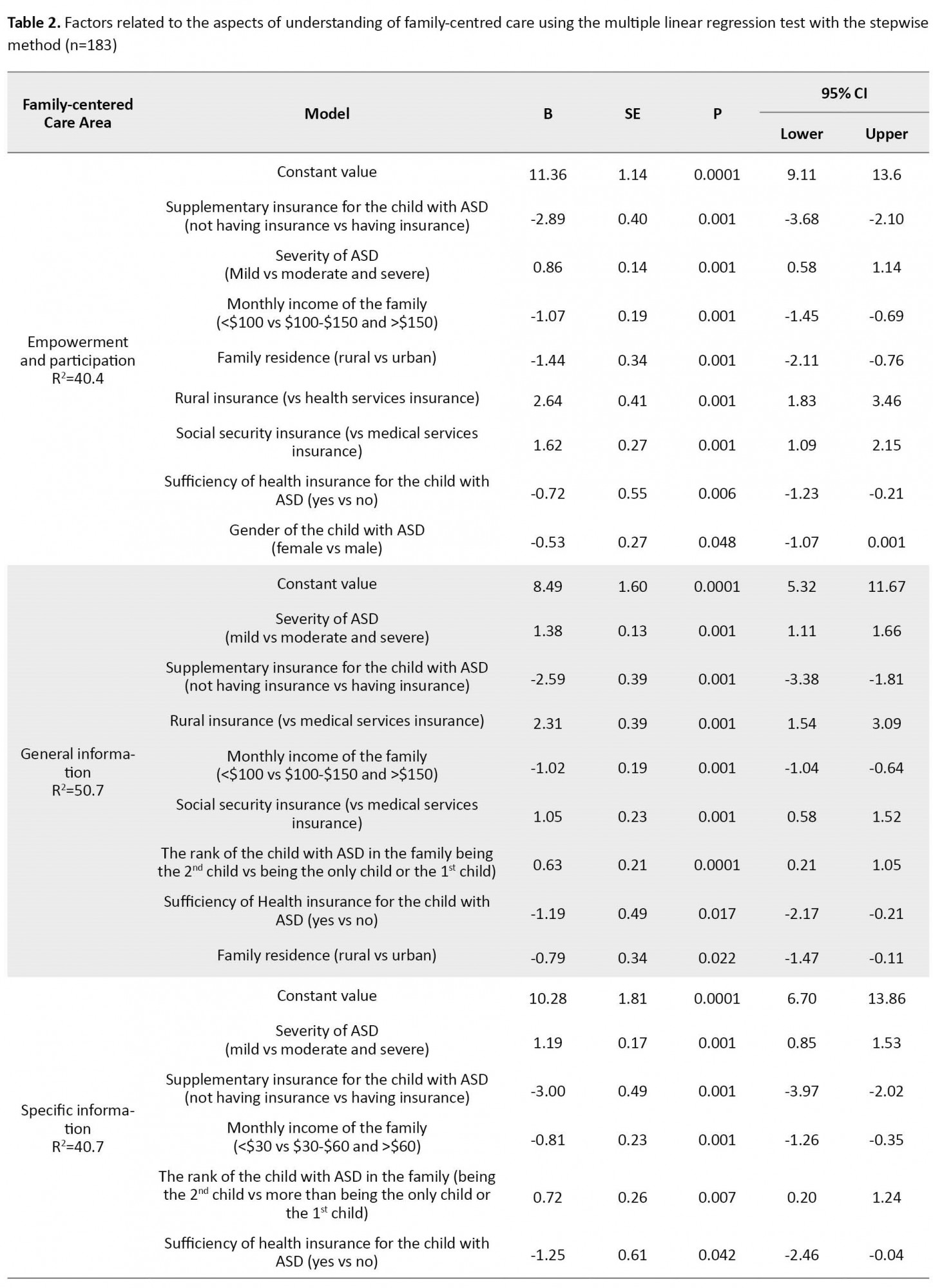
The stepwise multiple linear regression test results demonstrate that in the final model, most of the demographic variables significantly influenced the scores obtained in all 5 aspects. Specifically, the gender of the child with ASD (B=-0.58, 95% CI, -1.07% to 0.001%, P=0.001), general information (B=-1.19, 95% CI, -2.17% to -0.21%, P=0.017), specific information (B=-1.25, 95% CI, -2.46% to -0.04%, P=0.042), the sufficiency of health insurance, comprehensiveness and coordination of services (B=0.87, 95% CI, 1.17% to 0.57%, P=0.001), and family residence in the aspects of respect and support (B=-1.24, 95% CI, -1.94% to 0.54%, P=0.001) are significantly related to the perception of family-centered care from the perspective of mothers. More details can be found in Table 2.

Discussion
The findings of this research, aimed at determining family-centered care from the perspective of mothers with children having ASD in Rasht City, Iran, revealed that the scores obtained in the aspects of “empowerment/participation” and “general information” were lower than the average, while the aspects of “specific information”, “comprehensiveness and coordination” of care, and “respect and support” scored higher than the mean. These results differ from a study by Russell et al. using the same tool, where research samples scored medium to high in all aspects except for “general information” [21]. The difference might be attributed to societal differences and distinct care policies.
In this study, the aspect of “specific information” had the highest mean score, while “general information” had the lowest, consistent with Fontil’s study on Canadian and immigrant families of children with ASD in elementary school [22], Russell’s study in New York [21], Myrhaug’s study on parents of preschool children with brain paralysis [23], Wang’s study [24], and Stefánsdóttir’s study on parents of children under 5 needing rehabilitation services [25]. Care providers may prioritize providing “specific information” to families with children with ASD, potentially neglecting the importance of providing general information.
Regression test analysis demonstrated a significant relationship between understanding family-centered care and certain studied variables. Myrhaug’s study also found a positive correlation between greater financial support and higher scores in comprehensiveness and coordination of medical services [23]. Although direct financial support was not mentioned in the current study, the relationship between having supplementary insurance and family-centered care areas might be due to the high cost of rehabilitation care for children with ASD and limiting access to welfare centers only. Consequently, the quality of care provided may not fully meet family-centered care requirements. Stefánsdóttir’s study on parents’ and therapists’ understanding of family-centered care found age, performance, and type of disability of the sick child to be relevant factors. Younger children received more family-centered care, and parents of children with ASD scored lower in general information than other disabilities [25].
In this study, mothers with male children, except for the aspects of general information and specific information, scored higher in understanding family-centered care. Additionally, higher severity of the disease was associated with lower scores in family-centered care areas. Molinaro’s study similarly revealed that single and unemployed parents and families with lower socioeconomic status scored lower in family-oriented care aspects [26]. The findings suggest that employment status, father’s education, and father’s occupation, apart from general information, influenced higher scores in family-centered care aspects. However, having medical service insurance obtained a lower family-centered care understanding score compared to other insurance types, potentially due to less coverage of medical service insurance compared to social security insurance and rural insurance.
Overall, the mothers’ understanding of family-centered care for children with ASD was mean in three aspects and below mean in two aspects, indicating a need for improvement in the quality-of-care services. This research has limitations, such as using a questionnaire to assess mothers’ understanding, excluding 30% of research samples due to non-inclusion criteria, and conducting a large part of the questionnaire via telephone during the COVID-19 pandemic, potentially affecting respondents’ psychological state.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.238). Ethical principles were fully observed in this study. Informed consent was obtained from all study participants, who were aware of the research process. They were also assured that their information would be kept confidential.
Funding
This study was funded by Guilan University of Medical Sciences.
Authors' contributions
Data collection: Neda Feizi Mangoodehi; Statistical analysis of data: Neda Feizi Mangoodehi and Ehsan Kazemnejad Lieli; Writing the original draft: Leila Mirhadyan and Neda Feizi Mangoodehi; Conceptualization and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Researchers are grateful to the Research Vice-Chancellor of Guilan University of Medical Sciences and Welfare Organization of Rasht for supporting this project and the people participating in the study.
References
Autism spectrum disorder (ASD) is a developmental disorder that typically manifests in childhood and is characterized by stereotyped behaviors, excitability, destructive behaviors, and challenges in social communication, often occurring before age 3 [1, 2]. This disorder affects brain function, and the severity of symptoms may vary across 3 areas: Social interaction, communication, and repetitive behaviors [3]. Approximately 6 out of every 1000 children are affected by some form of autism spectrum disorder [4]. In Iran, the prevalence was reported as 2.95 per 10000 children in 2014 [5].
The challenges of an ASD child’s growth and development significantly impact the family system [6, 7]. Thus, besides focusing on the child with special needs, attention should be directed toward families with such needs. The family-centered approach emerges as promising to improve medical services and enhance satisfaction among families with children with autism spectrum disorder. This approach emphasizes mutual respect, acceptance of family choices, service exclusivity, and flexibility, family participation in decision-making, provision of necessary information and knowledge, and efforts to empower family cooperation and communication between the family and therapists [8].
Family-centered care comprises services tailored to children with special needs and their families. This approach underscores family involvement in decision-making, cooperation, and communication between the family and therapists, as well as mutual respect, acceptance of family choices, family support, service flexibility, and efforts to empower families. It has become a cornerstone of many early intervention and rehabilitation programs [9]. Family-centered care reduces anxiety and tension associated with treatment, shortens recovery time, and improves patient cooperation in care implementation. Moreover, it enhances the ability to address clients’ problems and issues, reduces situational anxiety in mothers, and leads to better clinical decision-making and follow-up in child nursing. Family-centered care fosters family cooperation with therapists, recognizes the family’s capacity and capability, and enhances communication among care team members [10, 11, 12, 13].
The perception of family-centered care can be influenced by factors such as an individual’s experiences, beliefs, convictions, and care standards [10]. Mothers’ individual and social factors are also linked to their perception of family-centered care [2, 10, 14, 15]. Variables like age, parents’ education, economic status, insurance adequacy, understanding of the disease and its severity in the family, the health status of family members, presence of healthy or chronically-ill siblings alongside the child with ASD, government financial support for care services, and government policies related to receiving family-centered care can all impact the quality of care received [12, 16].
Given their scope of work, community health nurses can improve the receipt of family-centered care by playing diverse roles within families with special needs, including those with ASD children. However, this effort requires a thorough understanding of the existing situation and surrounding factors. Therefore, due to the scarcity of research conducted in Iran, particularly in Guilan Province, we aimed to explore the understanding of family-centered care and its related factors among the mothers of children with ASD in Rasht City, Iran.
Materials and Methods
This research is a cross-sectional analytical study conducted in educational and rehabilitation centers covered by the Welfare Organization in Rasht during 2020. The research population comprised all mothers with children under 18 years diagnosed with ASD in Rasht, receiving care at the centers under the Rasht Welfare Organization. The inclusion criteria for the study included having a child under 18 with ASD, caring for the child at home, living with a husband, and providing consent to participate. The exclusion criteria comprised incomplete questionnaire responses or confusion in completing the questionnaire. The sampling method employed was a census, and out of the total research population of 264 people, 183 individuals (69.31%) willingly participated in the study.
The study data were collected using a two-part questionnaire. The first part assessed individual-family characteristics and factors related to understanding family-centered care. They included the age of the mother and father, the age of the child with ASD, the number of children in the family, the age at which ASD was diagnosed, the family’s monthly income and its sufficiency, the mother’s and father’s occupations and education levels, sex and rank of the child with ASD, the severity of ASD, type of health insurance and its sufficiency, family residence, and supplementary insurance for the child with ASD. The second part included the 20-item questionnaire of measure of processes of care, which was used to investigate the understanding of family-centered care from the perspective of mothers of children with ASD.
The questionnaire consists of 20 questions in 5 aspects: Empowerment and participation, providing general information, providing specific information about the child, comprehensiveness and coordination of services for the child and family, and respectful and supportive care. This tool has been translated and validated in several countries to assess the understanding of family-centered care by parents of children with chronic diseases and various care team members (e.g. doctors, nurses, psychologists, therapists, and social workers) [17, 18]. Given that this tool effectively covers the concepts of family-oriented care, it has been used in numerous similar studies [2, 19, 20].
The questionnaire is rated on a 7-point Likert scale, ranging from “never” with a score of 1 to “very much” with a score of 7. The Persian version of this instrument was used in the present study [9]. Due to the COVID-19 pandemic, data collection was conducted either in person by adhering to health protocols or via telephone with the research participants, following coordination with the Guilan Welfare Province and identifying the care centers covered by the Welfare Organization. The inclusion criteria were completed within 3 months. Of the participants, 30(16.39%) completed the questionnaire in person, and 153(83.61%) completed it by telephone due to the pandemic. Each questionnaire took approximately 15 to 20 minutes to complete.
The collected data were analyzed using SPSS software, version 24 at a significance level of 0.05. Quantitative variables were presented as Mean±SD, while qualitative variables were expressed as percentage frequency. To determine the correlation of study variables, the Pearson correlation, independent t-test, and analyses of variance were employed. Additionally, the multiple linear regression model was utilized to identify factors related to the perception score of family-centered care while controlling for individual-family factors.
Result
The research findings indicate that 183 participants (69.31%) met the study criteria, with an Mean±SD age of 58.42±14.5 years. Most mothers (41%) had a high school diploma. Many participants (54.6%) had children diagnosed with severe ASD, a male gender predominance (82%), and an Mean±SD age of 11.99±3.06. Additional personal and social information can be found in Table 1.

The Mean±SD of the scores obtained in the family-centered care aspects, from the highest to lowest, were as follows: “Specific information”, 4.55±2.06; “respect and support”, 4.08±1.82; “comprehensiveness and coordination” of services, 4.03±1.99; “empowerment and participation”, 3.77±1.87; and “general information”, 3.45±1.88. Among the quantitative variables, the number of children in the family showed significant correlations with empowerment and participation (P=0.002, r=0.226), general information (P=0.001, r=0.322), specific information (P=0.001, r=0.327), comprehensiveness and coordination (P=0.001, r=0.370), and respect and support (P=0.001, r=0.200). Additionally, the age of the child at the time of ASD diagnosis exhibited significant correlations with empowerment and participation (P=0.001, r=-0.214), general information (P=0.001, r=0.441), specific information (P=0.001, r=0.462), comprehensiveness and coordination (P=0.001, r=-0.404), and respect and support (P=0.001, r=-0.378). Moreover, the father’s age showed statistically significant correlations with general information (P=0.001, r=-0.201), specific information (P=0.028, r=-0.162), comprehensiveness and coordination (P=0.001, r=-0.233), and respect and support (P=0.01, r=-0.191).
The independent t-test and chi-square test revealed significant differences in scores obtained across all 5 aspects according to certain studied variables. Notably, the score of empowerment and participation differed significantly based on the mother’s occupation (P=0.001) and the gender of the child with ASD (P<0.05). The score of general information significantly differed based on the rank of the child with ASD (P=0.009) and the family’s place of residence (P=0.001). Additionally, the score of comprehensiveness and coordination significantly differed based on insurance sufficiency (P=0.001) and supplementary insurance (P=0.001), and the score of respect and support aspect significantly differed based on the family’s place of residence (P=0.001).
One-way analysis of the variance indicated significant differences in scores obtained across all 5 aspects according to certain studied variables. For instance, the score of empowerment and participation differed based on the father’s education level (sub-diploma and diploma, P=0.001; university graduate and diploma, P=0.001) and occupation (retired and freelance, P=0.01). The score of general information significantly differed based on the mother’s education level (undergraduate and university education, P=0.01) and the father’s occupation (retired and freelance, P=0.01). Additionally, the score of specific information aspects significantly differed based on the severity of ASD (mild and moderate, P=0.01; mild and severe, P=0.01). The score of comprehensiveness and coordination significantly differed based on the severity of ASD (mild and moderate, P=0.001; mild and severe, P=0.001) and the type of child’s health insurance (medical service insurance and social security insurance, P=0.001). Finally, the mean score in the aspect of respect and support significantly differed based on the severity of ASD (mild and moderate, P=0.001; mild and severe, P=0.001) and the type of health insurance (medical service insurance and social security insurance, P=0.001; medical services insurance and no insurance, P=0.02).
The stepwise multiple linear regression test results demonstrate that in the final model, most of the demographic variables significantly influenced the scores obtained in all 5 aspects. Specifically, the gender of the child with ASD (B=-0.58, 95% CI, -1.07% to 0.001%, P=0.001), general information (B=-1.19, 95% CI, -2.17% to -0.21%, P=0.017), specific information (B=-1.25, 95% CI, -2.46% to -0.04%, P=0.042), the sufficiency of health insurance, comprehensiveness and coordination of services (B=0.87, 95% CI, 1.17% to 0.57%, P=0.001), and family residence in the aspects of respect and support (B=-1.24, 95% CI, -1.94% to 0.54%, P=0.001) are significantly related to the perception of family-centered care from the perspective of mothers. More details can be found in Table 2.

Discussion
The findings of this research, aimed at determining family-centered care from the perspective of mothers with children having ASD in Rasht City, Iran, revealed that the scores obtained in the aspects of “empowerment/participation” and “general information” were lower than the average, while the aspects of “specific information”, “comprehensiveness and coordination” of care, and “respect and support” scored higher than the mean. These results differ from a study by Russell et al. using the same tool, where research samples scored medium to high in all aspects except for “general information” [21]. The difference might be attributed to societal differences and distinct care policies.
In this study, the aspect of “specific information” had the highest mean score, while “general information” had the lowest, consistent with Fontil’s study on Canadian and immigrant families of children with ASD in elementary school [22], Russell’s study in New York [21], Myrhaug’s study on parents of preschool children with brain paralysis [23], Wang’s study [24], and Stefánsdóttir’s study on parents of children under 5 needing rehabilitation services [25]. Care providers may prioritize providing “specific information” to families with children with ASD, potentially neglecting the importance of providing general information.
Regression test analysis demonstrated a significant relationship between understanding family-centered care and certain studied variables. Myrhaug’s study also found a positive correlation between greater financial support and higher scores in comprehensiveness and coordination of medical services [23]. Although direct financial support was not mentioned in the current study, the relationship between having supplementary insurance and family-centered care areas might be due to the high cost of rehabilitation care for children with ASD and limiting access to welfare centers only. Consequently, the quality of care provided may not fully meet family-centered care requirements. Stefánsdóttir’s study on parents’ and therapists’ understanding of family-centered care found age, performance, and type of disability of the sick child to be relevant factors. Younger children received more family-centered care, and parents of children with ASD scored lower in general information than other disabilities [25].
In this study, mothers with male children, except for the aspects of general information and specific information, scored higher in understanding family-centered care. Additionally, higher severity of the disease was associated with lower scores in family-centered care areas. Molinaro’s study similarly revealed that single and unemployed parents and families with lower socioeconomic status scored lower in family-oriented care aspects [26]. The findings suggest that employment status, father’s education, and father’s occupation, apart from general information, influenced higher scores in family-centered care aspects. However, having medical service insurance obtained a lower family-centered care understanding score compared to other insurance types, potentially due to less coverage of medical service insurance compared to social security insurance and rural insurance.
Overall, the mothers’ understanding of family-centered care for children with ASD was mean in three aspects and below mean in two aspects, indicating a need for improvement in the quality-of-care services. This research has limitations, such as using a questionnaire to assess mothers’ understanding, excluding 30% of research samples due to non-inclusion criteria, and conducting a large part of the questionnaire via telephone during the COVID-19 pandemic, potentially affecting respondents’ psychological state.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.238). Ethical principles were fully observed in this study. Informed consent was obtained from all study participants, who were aware of the research process. They were also assured that their information would be kept confidential.
Funding
This study was funded by Guilan University of Medical Sciences.
Authors' contributions
Data collection: Neda Feizi Mangoodehi; Statistical analysis of data: Neda Feizi Mangoodehi and Ehsan Kazemnejad Lieli; Writing the original draft: Leila Mirhadyan and Neda Feizi Mangoodehi; Conceptualization and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Researchers are grateful to the Research Vice-Chancellor of Guilan University of Medical Sciences and Welfare Organization of Rasht for supporting this project and the people participating in the study.
References
- Karimzadeh M, Baneshi AR, Dehghan Tezerjani M, Tayyebi Sough Z. [Normalization of pervasive developmental disorder screening test (Persian)]. Arch Rehabil. 2018; 19(2):116-25. [DOI:10.32598/rj.19.2.116]
- Akbari A, Ahmadi F, Zandi H, Talebi-Ghane E, Yadollahifar S, Jalili E. [The effect of family-centered empowerment model on anxiety of mothers of children with cancer (Persian)]. J Health Care. 2021; 22(4):295-305. [DOI:10.52547/jhc.22.4.295]
- Saeedi C. [Investigation of dysfunction in the neural systems underlying social perception, action observation and theory of mind in autism spectrum disorders. (Persian)]. Neurosci JShefaye Khatam. 2018; 6(2):82-93. [DOI:10.29252/shefa.6.2.82]
- Movahhed T, Asadi M, Eslami N. [Comparison of dental caries experience and associated treatment needs between autistic and healthy children (Persian)]. J Mashhad Dent Sch. 2017; 41(3):281-8. [DOI: 10.22038/JMDS.2017.9229]
- Salar S, Daneshmandi H. [Relationship between lumbar-pelvic function and static and dynamic balance in children with autism spectrum disorders. (Persian)]. Sci J Rehabil Med. 2017; 6(2):168-79. [Link]
- Rahimi S, Amin Yazdi S A, Afrooz G. [Comparison of developmental family functioning, personality traits, and parenting stress in mothers with autism spectrum disorder and peers with normal counterparts (Persian)]. Iran J Pediatr Nurs. 2020; 6(3):14-21. [Link]
- Ahangar AA, Salarifar MH, Mojahedi Rezaeian S, Imanverdi A. [Comparing certain time representation features in high-functioning autistic children with normal children’s narrative discourse (Persian)]. Sci J Rehabil Med. 2021; 10(5):948-63. [DOI:10.32598/SJRM.10.5.10]
- Hill C, Knafl KA, Santacroce SJ. Family-centered care from the perspective of parents of children cared for in a pediatric intensive care unit: An integrative review. J Pediatr Nurs. 2018; 41:22-33. [DOI:10.1016/j.pedn.2017.11.007] [PMID]
- Kaviani Broujeni R, Rezaee M, Pashazadeh Azar Z, Tabatabae M, Gerivani H. [The measure of processes of care 20-item (MPOC-20): Validity and reliability of the Persian version (Persian)]. Arch Rehabil 2021; 22(1):102-17. [DOI:10.32598/RJ.22.1.3213.1]
- Aran A, Abazari F, Farokhzadian J, Azizzadeh Forouzi M. [Comparing the perception of family-centered care from the perspectives of nursing staff and mothers of hospitalized children in children’s wards (Persian)]. J Hayat. 2018; 24(1):48-58. [Link]
- Biranvand H, Birjandi M, Goudarzi F, Heydari H. [The impact of family-center interventions on anxiety and depression of low-conscious patient’s family hospitalized in the intensive care units: A randomized clinical trial study (Persian)]. Iran J Nurs Res. 2020; 15(4):93-101. [Link]
- Jalili F, Borimnejad L. [The effect of family-centered care on the parental anxiety of children with febrile seizure (Persian)]. Nurs Midwifery J. 2020; 18(9):732-40. [Link]
- Verklan MT, Walden M, Forest S. Core curriculum for neonatal intensive care nursing e-book. Amsterdam: Elsevier Health Sciences; 2020. [Link]
- Akbari V, Asayesh H, Haji Mohammad Hoseini M, Sharififard F, Shahidi M, Goudarzi M. [Needs of family with hospitalized infant in neonatal intensive care unit: A comparison between mothers’ and nurses’ viewpoint (Persian)]. Qom Univ Med Sci J. 2020; 14(3):10-8. [DOI:10.29252/qums.14.3.10]
- Razeghi Nasrabad HB, Hosseini Z. [The experience of combination of work and family in employed mothers with younger children (Persian)]. J Appl Soci 2019; 30(3):109-34. [DOI:10.22108/JAS.2019.113958.1549]
- Bernier RA, Dawson G, Nigg JT. What science tells us about autism spectrum disorder: Making the right choices for your child. New York: Guilford Publications; 2020. [Link]
- King SM, Rosenbaum PL, King GA. Parents ‘perceptions of caregiving: development and validation of a measure of processes. Dev Med Child Neurol. 1996; 38(9):757-72. [DOI:10.1111/j.1469-8749.1996.tb15110.x] [PMID]
- Gill FJ, Pascoe E, Monterosso L, Young J, Burr C, Tanner A, et al. Parent and staff perceptions of family-centered care in two Australian children’s hospitals. Eur J Pers Cent Healthcare. 2014; 1(2):317-25. [Link]
- Khoshakhlagh H. [The effect of early family-centered psychological and educational interventions on the cognition and social skills development of children with autism disorder (Persian)]. Knowl Res Appl Psychol. 2018; 18(4):102-14. [Link]
- Ramshini M, Hasanzadeh S, Afroz GA, Hashemi Razini H. [The effect of family-centered nature therapy on children with autism spectrum disorder (Persian)]. Arch Rehabil. 2018; 19(2):150-9. [DOI:10.32598/rj.19.2.150]
- Russell S, McCloskey CR. Parent perceptions of care received by children with an autism spectrum disorder. J Pediatr Nurs. 2016; 31(1):21-31. [DOI:10.1016/j.pedn.2015.11.002] [PMID]
- Fontil L, Petrakos HH. Transition to school: The experiences of Canadian and immigrant families of children with autism spectrum disorders. Psychol Sch. 2015; 52(8):773-88. [DOI:10.1002/pits.21859]
- Myrhaug HT, Jahnsen R, Østensjø S. Family-centred practices in the provision of interventions and services in primary health care: A survey of parents of preschool children with cerebral palsy. J Child Health Care. 2016; 20(1):109-19. [DOI:10.1177/1367493514551312] [PMID]
- Wang M, Petrini M, Guan Q. Evaluation of family-centred services from parents of Chinese children with cerebral palsy with the Measure of Processes of Care. Child Care Health Dev. 2015; 41(3):408-15. [DOI:10.1111/cch.12183] [PMID]
- Stefánsdóttir S, Thóra Egilson S. Diverging perspectives on children’s rehabilitation services: A mixed-methods study. Scand J Occup Ther. 2016; 23(5):374-82. [DOI:10.3109/11038128.2015.1105292] [PMID]
- Molinaro A, Fedrizzi E, Calza S, Pagliano E, Jessica G, Fazzi E, et al. Family-centred care for children and young people with cerebral palsy: Results from an Italian multicenter observational study. Child Care Health Dev. 2017; 43(4):588-97. [DOI:10.1111/cch.12449] [PMID]
Article Type : Research |
Subject:
General
Received: 2023/07/2 | Accepted: 2023/06/29 | Published: 2023/06/29
Received: 2023/07/2 | Accepted: 2023/06/29 | Published: 2023/06/29
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






