Wed, Jul 3, 2024
Volume 33, Issue 4 (9-2023)
JHNM 2023, 33(4): 297-305 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Özbudak G, Yıldırım Y. Nonpharmacological Methods Used for Dyspnea Management by Individuals With Lung Cancer. JHNM 2023; 33 (4) :297-305
URL: http://hnmj.gums.ac.ir/article-1-2194-en.html
URL: http://hnmj.gums.ac.ir/article-1-2194-en.html
1- Lecturer, Department of Nursing, School of Health, Trakya University Kesan Hakkı Yörük, Edirne, Turkey. , gizem-ozbudak@hotmail.com
2- Professor, Internal Medicine Nursing, School of Nursing, Ege University Izmir, Turkey.
2- Professor, Internal Medicine Nursing, School of Nursing, Ege University Izmir, Turkey.
Full-Text [PDF 515 kb]
(291 Downloads)
| Abstract (HTML) (485 Views)
Full-Text: (316 Views)
Introduction
Lung cancer is the most common cancer globally and the leading cause of cancer-related death. The World Health Organization (WHO) reported that lung cancer constituted 11.6% of all cancers in 2018, with a total of 2.09 million new cases [1]. According to the 2018 data from the Ministry of Health statistics yearbook, lung cancer is the most common type of cancer in the entire population and males in Turkey and is the fifth most common type in females [2]. Patients with lung cancer have symptoms that can devastate their physical and emotional health [3]. The most common symptoms include dyspnea, cough, weight loss, fatigue, pain, chest pain, anxiety, and depression [4]. Dyspnea is one of the most common and distressing symptoms that limit the daily life activities of individuals and cause a deterioration in the quality of life [5, 6].
Dyspnea is defined as respiratory distress and the sensation of difficulty in breathing. Patients describe this symptom as shortness of breath and an inability to breathe adequately. The prevalence of dyspnea in lung cancer patients has been reported to be between 20% and 90% [7, 8]. Dyspnea harms the quality of life, daily activities, and physical and psychosocial functioning [9]. It is important to identify and eliminate the underlying causes of dyspnea, such as comorbid diseases, and try to relieve the patient [10].
Due to its multidimensional nature, dyspnea management requires pharmacological and nonpharmacological methods [9]. In pharmacological management, medications such as oxygen therapy, opioids, benzodiazepines, phenothiazines, corticosteroids, and inhaler furosemide treat anxiety, agitation, and air hunger accompanying dyspnea [7, 11]. But, because of the troublesome side-effects and costs of pharmaceutical methods, nonpharmaceutical methods are preferable to pharmaceutical methods [8].
Nonpharmacological interventions have been recommended to improve breathing efficiency, manage shortness of breath, and reduce psychological distress, as well as pharmacological interventions to manage dyspnea [11-13]. Nonpharmacological methods alleviate symptoms by creating a holistic approach to cancer care [14]. Physical, behavioral, psychosocial, and environmental changes benefit dyspnea management [12]. In the literature, interventions such as energy conservation techniques, use of fans, staying in a cold room, walking exercises, non-invasive mechanical ventilation, anxiety reduction techniques, Qi therapy, acupuncture, relaxing music, supporting family/caregivers, and training have been reported as nonpharmacological methods used in dyspnea management [11, 15, 16].
Its use, along with pharmacological techniques, increases the effectiveness of the treatments, producing benefits to the patient regarding dyspnea control. It also proves to be beneficial in controlling anxiety and fatigue [17]. We need to determine the nonpharmacological methods patients use for dyspnea and how to apply them [18]. While there is information on what nonpharmacological methods are available in the management of dyspnea, data on the use of these methods by patients are missing [19].
In line with this information, defining the nonpharmacological methods patients use for dyspnea management is important. The study aimed to examine the nonpharmacological methods used by lung cancer patients for dyspnea management and to evaluate the patients’ opinions and their needs and preferences regarding these methods.
Materials and Methods
This cross-sectional study was conducted between June 2018 and September 2018, employing an interview method in an outpatient chemotherapy unit of a university hospital in Izmir, Turkey. All 60 patients of the unit who could communicate, agreed to participate, and could complete the survey form were included. They were at least 18 years old, diagnosed with lung cancer, able to communicate, and described dyspnea during daily activities and agreed to participate. The exclusion criterion was incomplete in filling out the study questionnaires.
In the data collection process, the “patient self-description form”, “verbal rating scale (VRS)”, “dyspnea frequency determination form”, and “dyspnea management form” were prepared by the researchers to evaluate nonpharmacological methods used by patients for the management of dyspnea.
The patient self-description form collected the demographic information. The researchers designed the form, and it consists of two sections: The sociodemographic characteristics (age, gender, height, and weight, body mass index, occupation, current employment, social security, income status, educational status, marital status, with whom they live, and smoking status) and questions concerning the disease (disease diagnosis, time since diagnosis, presence of metastasis, presence of any other chronic disease) [6, 16].
The verbal rating scale (VRS) requires patients to rate their dyspnea from 0 to 10, with 0 indicating no dyspnea and 10 the worst possible level of dyspnea [20, 21].
Determination of dyspnea frequency was created to determine how often patients experience dyspnea, with 5 options: Every day, a few times every day, a few times a week, once a week, and less than once a week [21, 22].
The “dyspnea management form” was designed by the researchers based on the current literature and studies on dyspnea in lung cancer [10, 12]. The form includes a question to ascertain where the patients had access to information about dyspnea management, nonpharmacological applications, and methods, such as slowing down, resting, not overexerting, relaxation-anxiety reduction exercises, getting help in daily life activities, proper sitting position, walking with an assistive device, elevating the head of the bed, physical rehabilitation, walking, opening window, using a room or face fan, nutritional support, not worrying, positive thinking, listening to music, daydreaming, breathing exercises, acupuncture.
Gathering data in the study was done in the outpatient chemotherapy unit. The obtained data were analyzed in SPSS software, version 16. Descriptive statistics were used in the evaluation of the data. The inferential statistics, such as the chi-square and Kruskal-Wallis tests, were used to analyze the obtained data. P<0.05 was considered statistically significant.
Results
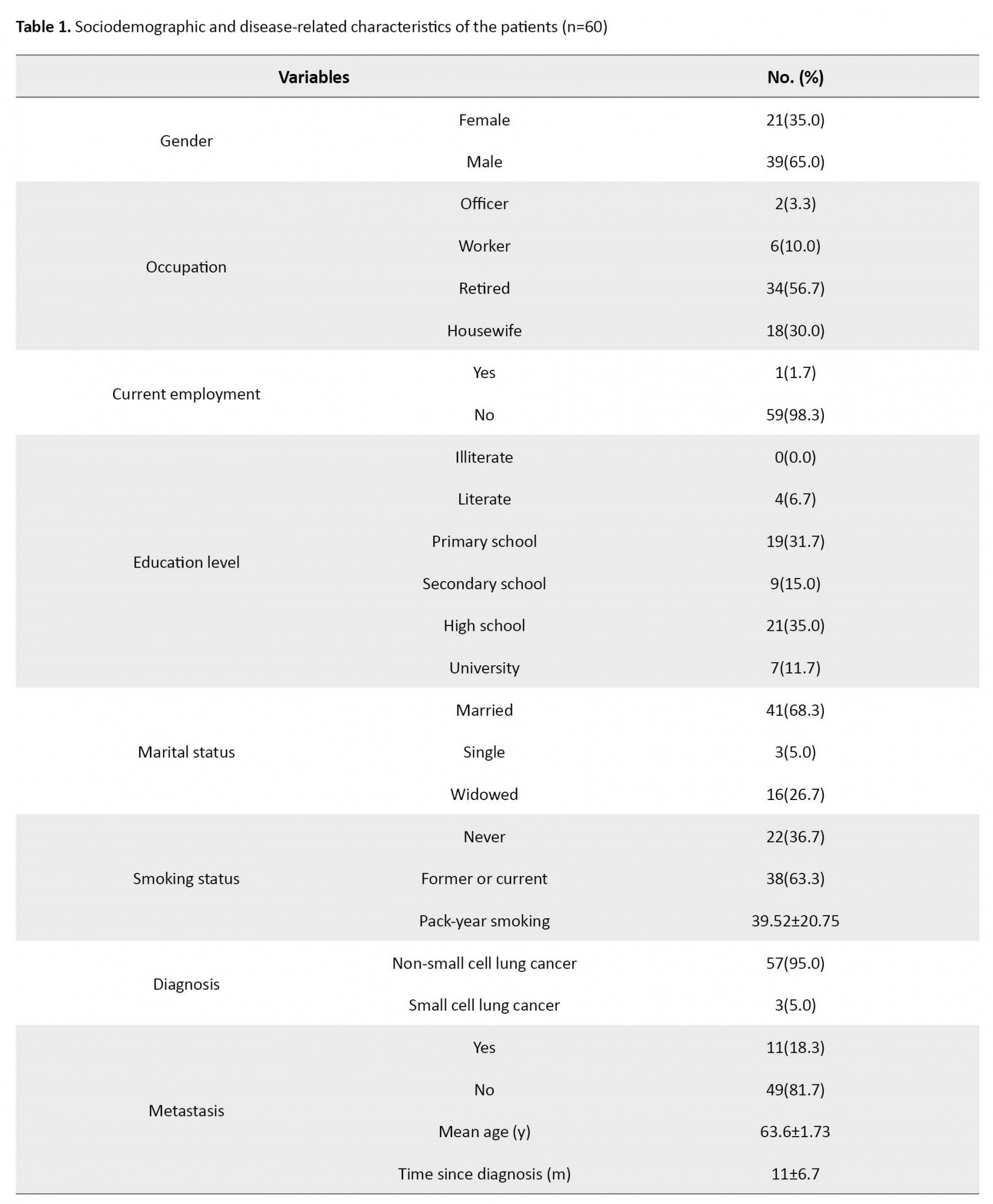
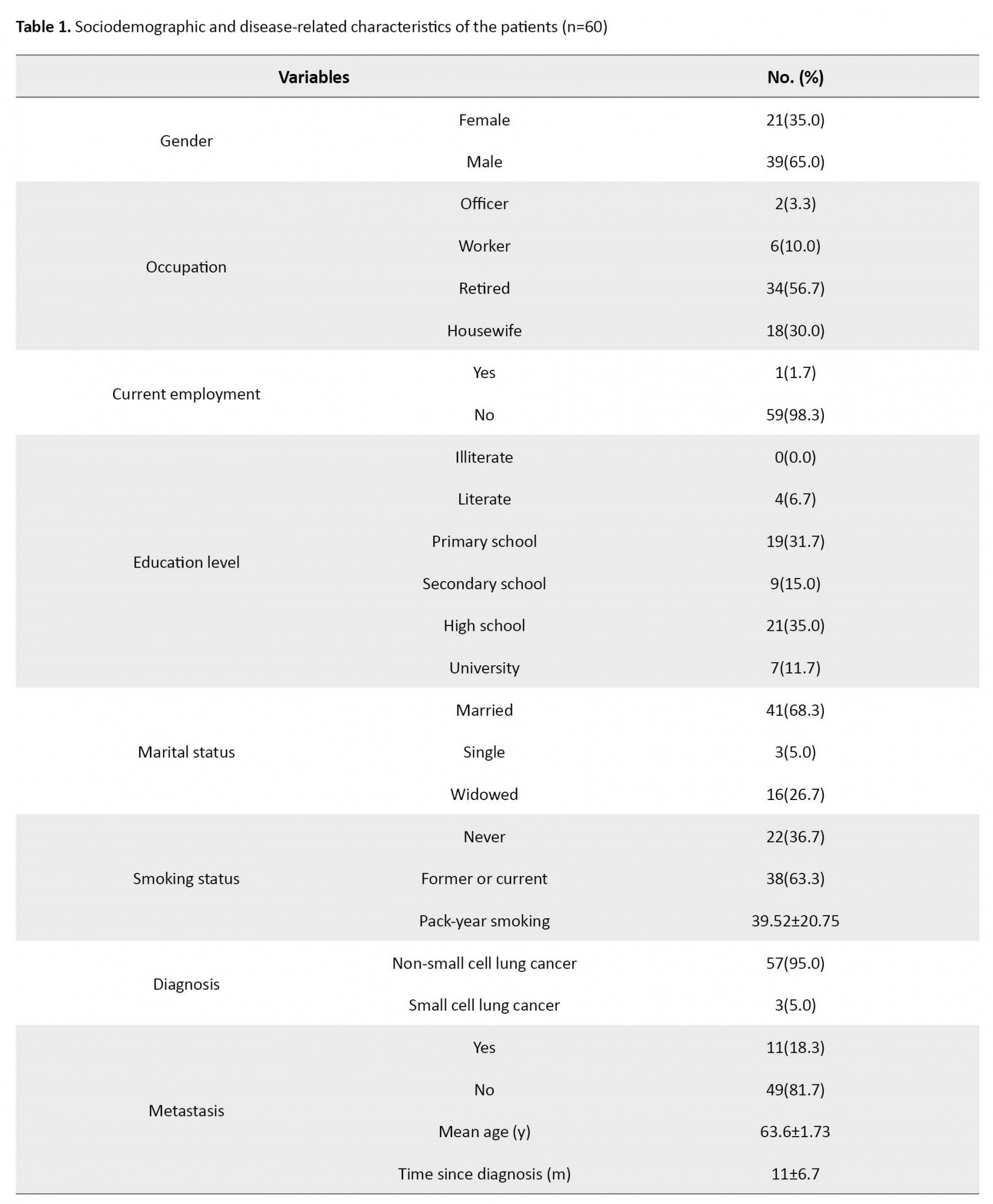
The study samples comprised 65% males and 35% females with a Mean±SD age of 63.6±1.73 years; 56.7% were retired, 35% had an education level of high school, 41% were married, and 63% had a smoking history. In terms of the disease characteristics of the patients, 85% were diagnosed with non-small cell lung cancer, the Mean±SD time since diagnosis was 11±6.7 months, and 81.7% did not have metastasis (Table 1).
The Mean±SD VRS score of the patients was 5.2±2.6 (from 0 to 10), and the frequency rates of dyspnea were 48.3% “a few times a week”, 26.7% “a few times every day”, 10% “less than once a week”, 8.3% “once a week”, and 6.7% “all the time”. Of the study sample, 55% stated they had no information about nonpharmacological methods in dyspnea management.
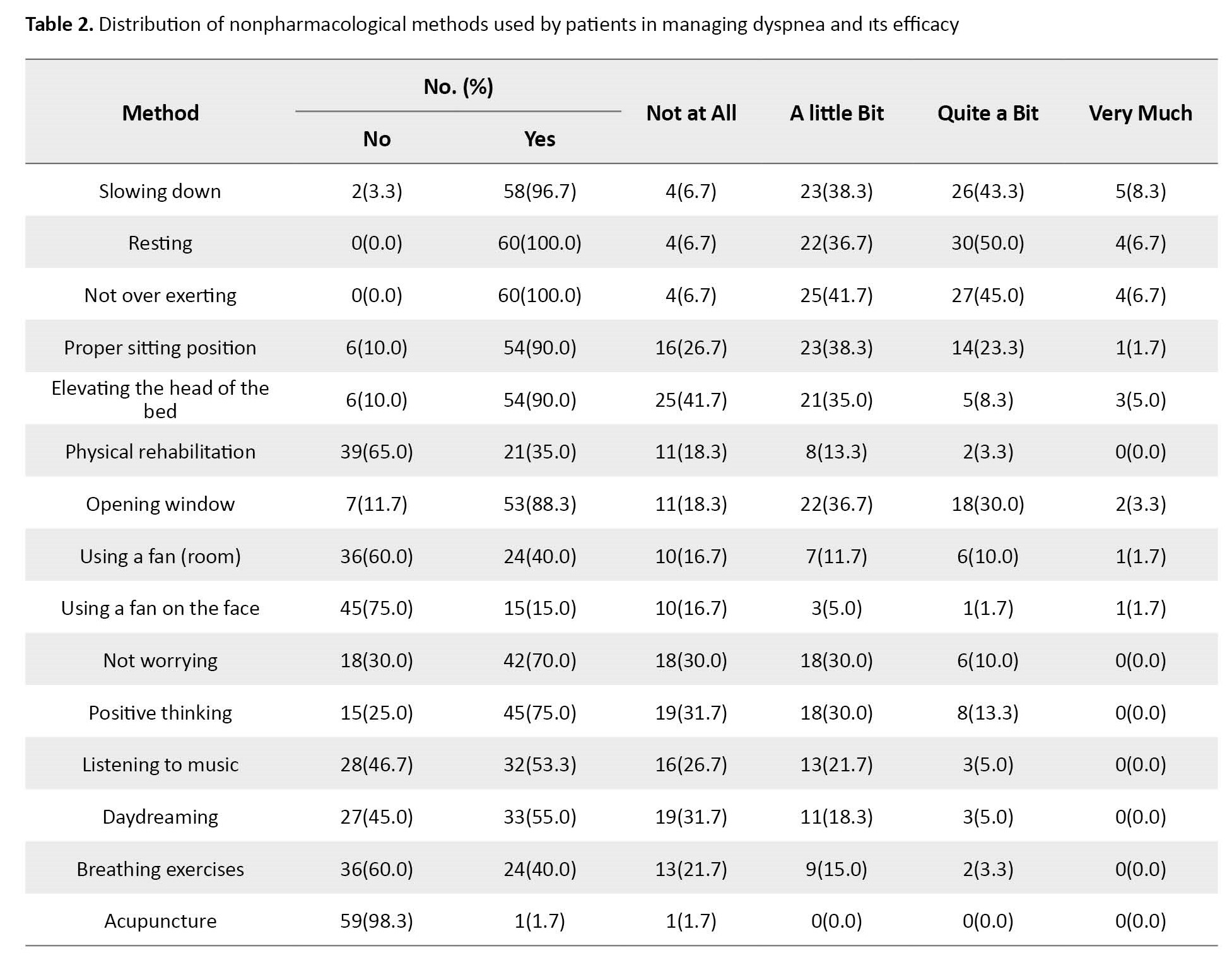
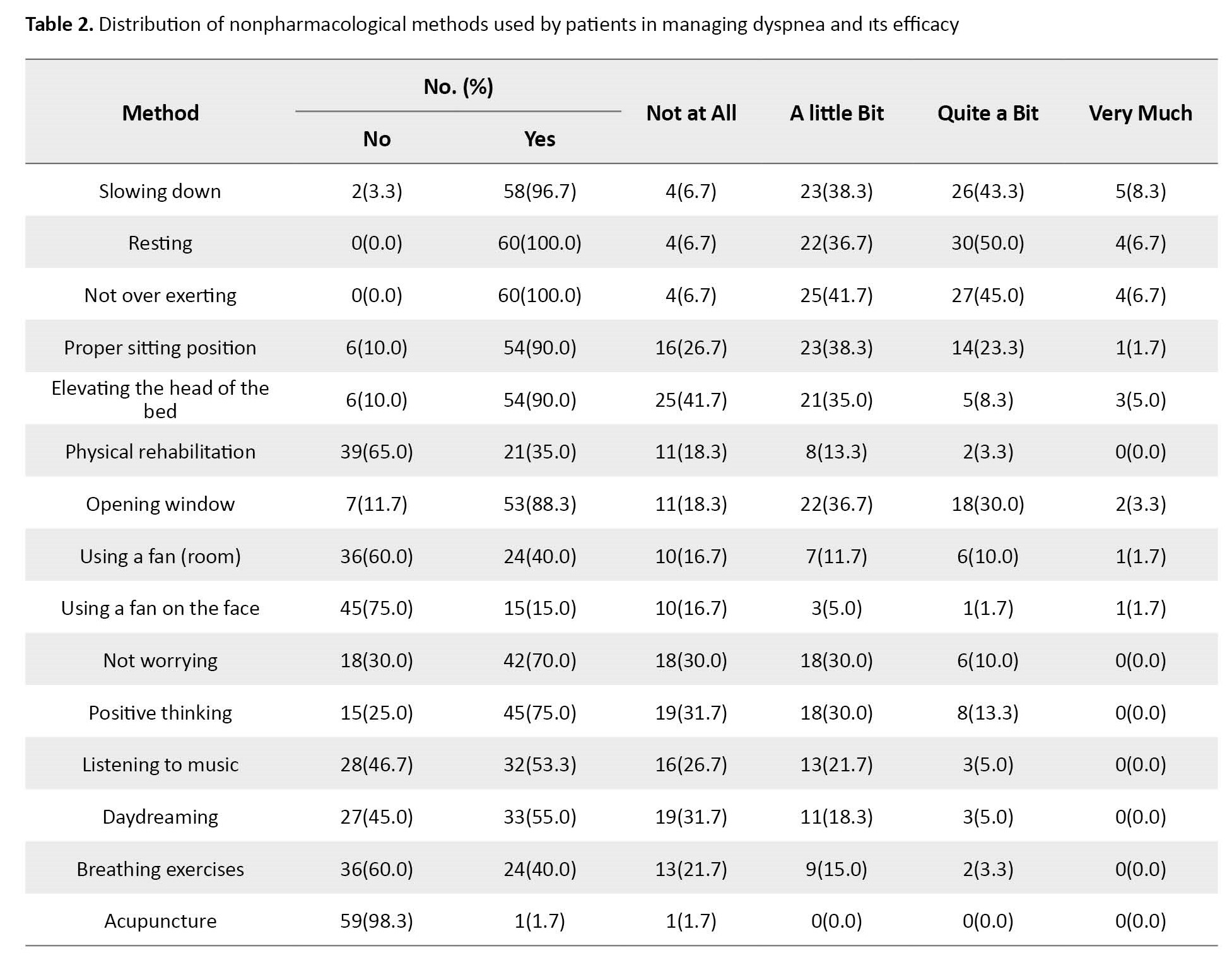
The nonpharmacological methods most used by the patients for the management of dyspnea were slowing down (96.7%), resting and not over-exerting (93.3%), proper sitting position (90%), elevating the head of the bed (90%) and opening windows (88.3). Using a fan in the room (40%), using a fan on the face (25%), breathing exercises (40%), and acupuncture (1.7%) were used less frequently. Patients reported that the frequently used nonpharmacological methods of slowing down, resting, and not overexerting were mostly beneficial. More than half of the patients did not use physical rehabilitation, a room fan, a fan on the face, or breathing exercises, and those who used these methods reported little benefit (Table 2).
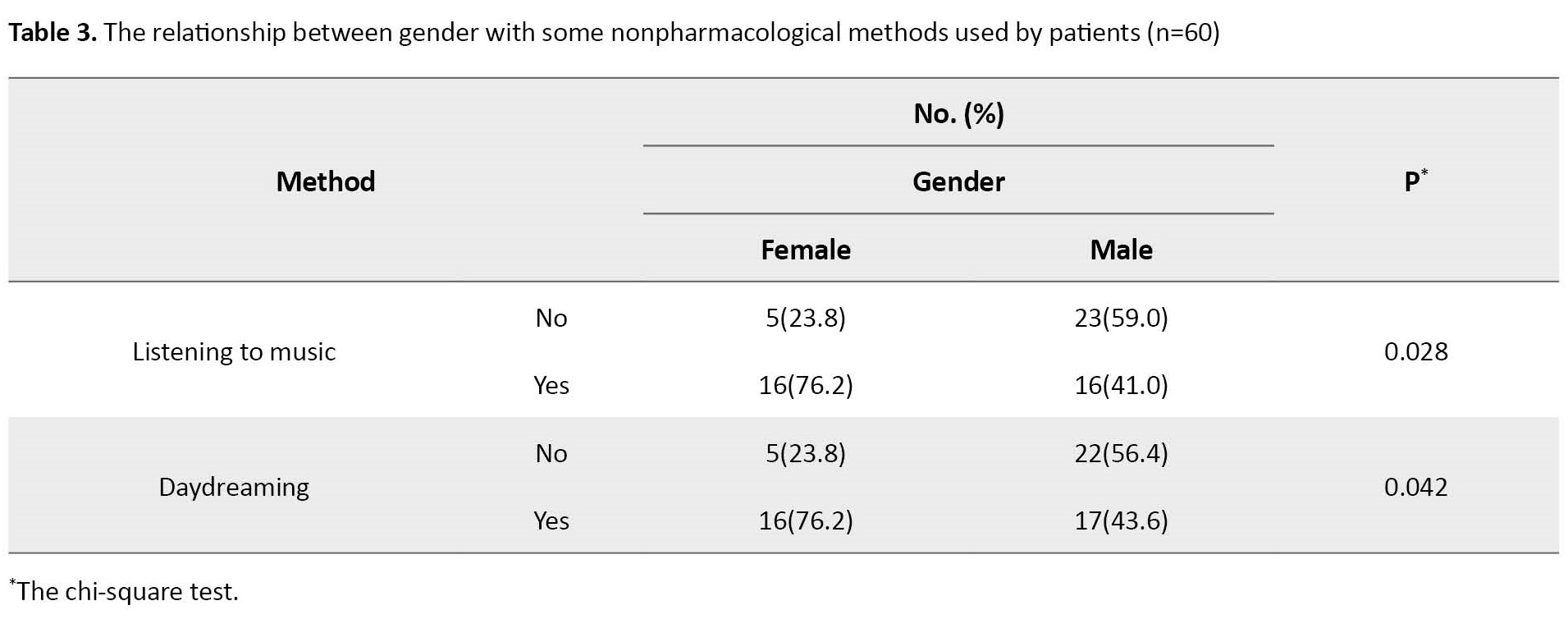
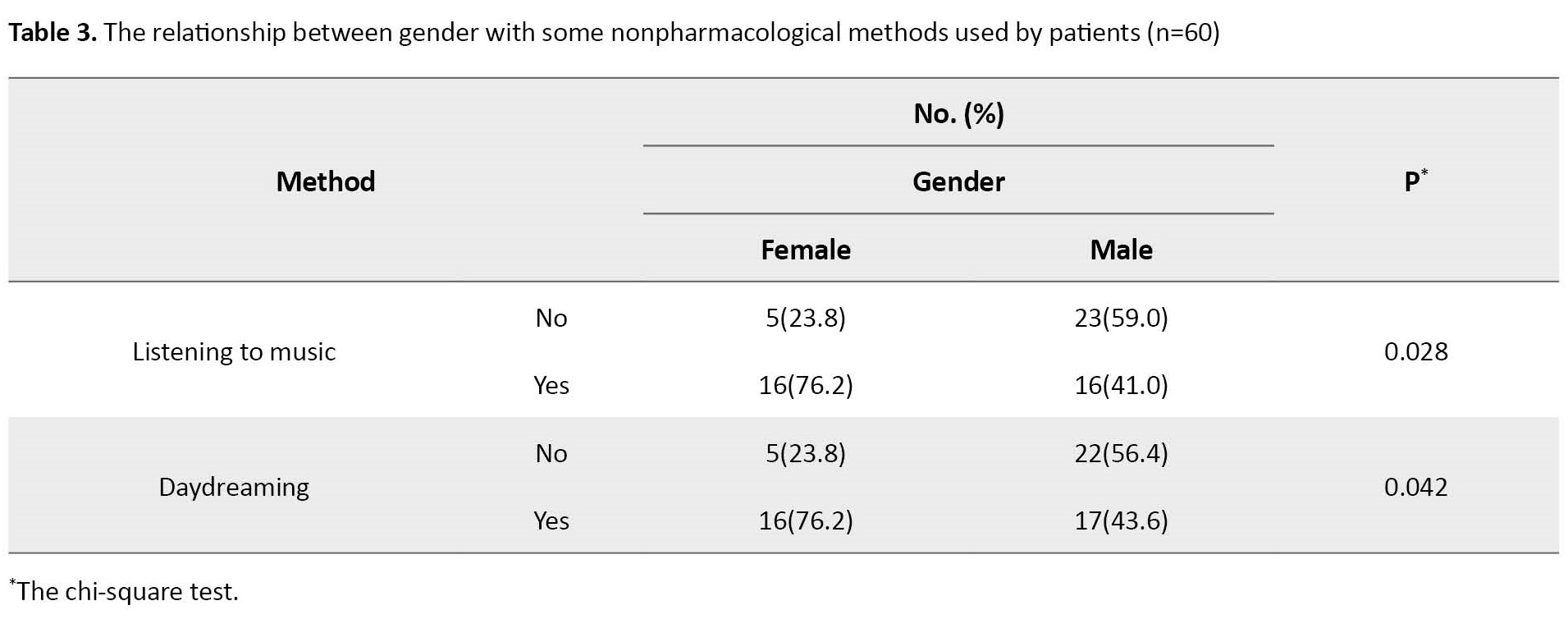
The chi-square test showed that the use of nonpharmacological methods was significant in terms of some variables. Female patients used listening to music (P=0.028) and daydreaming (P=0.042) methods more than male patients (Table 3).
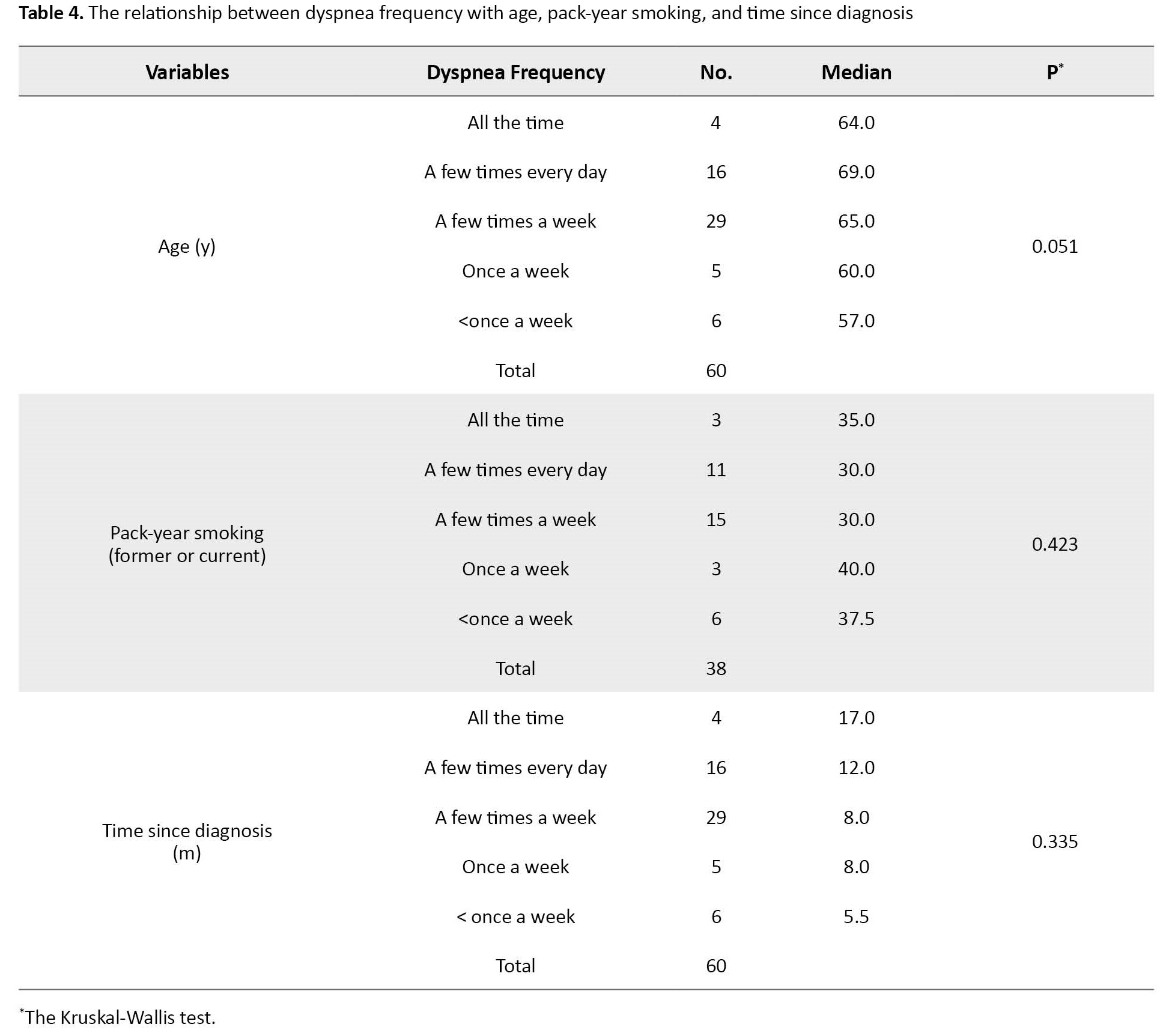
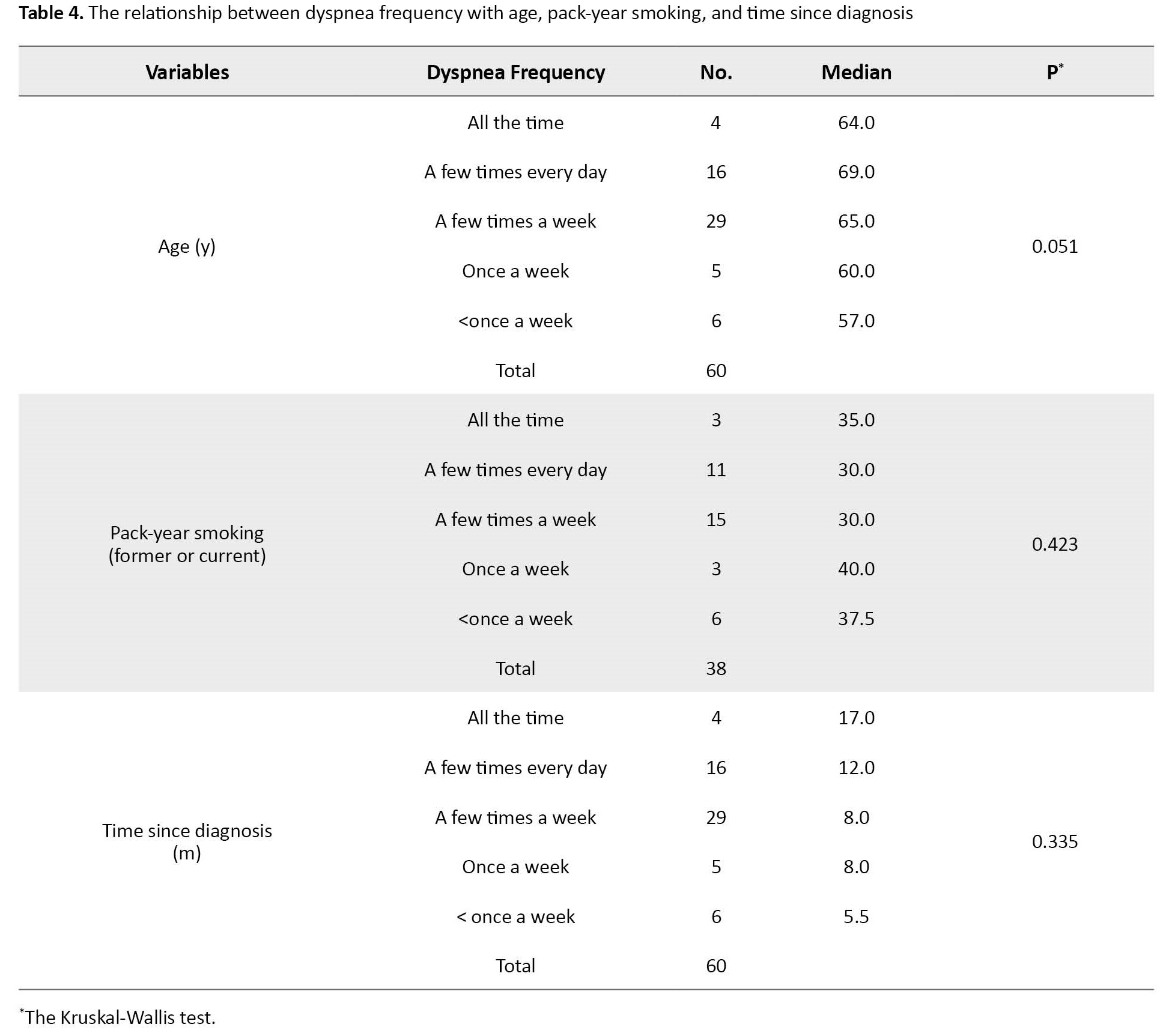
There was not any relationship between the frequency of dyspnea based on age, pack-year of smoking, and the time since diagnosis (Table 4).
Discussion
The current study results showed that the frequency of dyspnea was a few times a week. This result indicated that they experienced dyspnea with an average frequency (not very often and not very rarely). Although there are many review articles on this subject, comparable research findings are limited. Similar to the results of the current study, Weingärtner et al. evaluated patients diagnosed with chronic obstructive pulmonary disease and lung cancer and reported that those with lung cancer described the frequency of dyspnea as 1-3 times a week, and most of them had a history of smoking [23]. Another study reported that the incidence of dyspnea is higher (several times a day) in patients receiving lung cancer treatment [22]. In studies in the relevant literature, the prevalence of dyspnea in patients with lung cancer has been reported to vary between 21% and 90% [7, 8].
Over half of the current study patients had no information about nonpharmacological methods for managing dyspnea. There is, therefore, a clear need for these patients to be informed about nonpharmacological methods.
In the study, nonpharmacological methods most used by the patients to manage dyspnea were slowing down, resting and not over-exerting, proper sitting position, elevating the head of the bed, and opening windows. Using a fan (room), a fan on the face, breathing exercises, and acupuncture were used less frequently. This result shows that physiological methods are used more, and psychological support methods are less preferred or unknown.
In a qualitative study by Simon et al., lung cancer patients said they reduced physical activity, rested, and lay in bed to relieve dyspnea. The patients stated that resting and not overexerting strategies were the most effective. Also, calming down, relaxing, and showing a positive attitude were beneficial as cognitive and psychological strategies. Most patients reported using several pillows to raise the upper body and sleep upright. It has been determined that using a fan is not common, but fresh and cold air makes the patient feel better [24]. Similarly, Yates et al. reported that the dyspnea methods used most frequently by lung cancer patients were slowing down, resting, positive thinking, and not overexerting or worrying. The less frequently used strategies were comfortable positioning, window opening, and using a fan on the face [12]. In a qualitative study by Linde et al., it was determined that patients with lung cancer motivated themselves with an affirmation of “calm down, everything will be better”, most of the patients stated that they relaxed with breathing exercises and appropriate positioning [25].
In the current study, methods developed by individuals based on their own experience were used more frequently, and methods requiring the knowledge and support of health professionals less frequently. The often-used methods by patients can be attributed to reasons such as no cost, personal experience, and few or no side effects.
The orthopnea position, which is a forward bending position with the patient extending his hands and arms towards his legs or raising them towards an object such as a table, is a suitable sitting position, improves oxygenation and reduces inspiratory effort, thereby allowing the patient to breathe more comfortably [26].
The current study showed that more than half of the individuals do not use a room fan, a fan on the face, or breathing exercises. Also, the individuals who use these methods have reported insignificant benefits from these methods. This finding may be due to the low awareness of individuals about evidence-based nonpharmacological methods and or application errors in the management of dyspnea. The stimulation of mechanoreceptors in the face area or cooling of the skin with a hand fan application to the face creates central inhibition of dyspnea and decreases the feeling of dyspnea by stimulating the second and third branches of the trigeminal nerve. A face fan is recommended to be used for about 5 minutes at a distance of 15-30 cm from the lip and mouth area [10, 27]. Breathing exercises have been reported to improve the perception of dyspnea, lung function, exercise capacity, and health-related quality of life parameters [28]. Teaching respiratory exercises to reduce shortness of breath is another important component of the approach to patients [29].
Patients have not used acupuncture, a widely used traditional Chinese therapy to manage dyspnea. The clinical efficacy of acupuncture has been evaluated with numerous randomized controlled studies [30, 31]. Acupuncture has been reported to provide control of dyspnea by providing endogenous opioid release and limbic system stimulation [28]. In Turkey, acupuncture practice may be limited for reasons such as not being part of traditional Turkish culture, being unable to easily adopt new applications, having health concerns, and lacking information [30].
The current study showed that mostly female patients used the methods of listening to music and daydreaming. This result can be related to the fact that females have a greater psychological ability to divert attention. Methods such as relaxation exercises, listening to music, and not worrying positively affect dyspnea and reduce anxiety and distress [12]. A sense of control over dyspnea can be achieved by drawing attention to a pleasurable experience or feeling. However, no study has evaluated the factors affecting nonpharmacological methods used by lung cancer patients.
In conclusion, the studies on nonpharmacological methods for dyspnea management are limited, and the frequency and awareness of evidence-based nonpharmacological methods for dyspnea management are low. Due to the lack of studies in this field and weak evidence to determine the value and acceptability of nonpharmacological methods used in dyspnea caused by lung cancer, studies such as this are significant. It is also the nurse’s responsibility within the multidisciplinary team to provide training for all these methods for patients with lung cancer.
Dyspnea is a common symptom in individuals with lung cancer, but its management is still inadequate, and there is no information about effective coping strategies [24].
This research revealed that the patients need training on current strategies to manage dyspnea and use nonpharmacological methods. With nonpharmacological methods, the feeling of shortness of breath experienced by the individual during dyspnea decreases both psychologically and physiologically, and respiratory control is provided [17]. An increase in nonpharmacological methods, which have an important place in the management of dyspnea, will provide greater benefit. In particular, patients should be guided and encouraged to perform breathing exercises and use a fan on the face with the correct method and technique [32]. The small number of samples that meet the criteria for entering the research and the use of one questionnaire to determine the performance of patients in dyspnea relief are the limitations of the present research.
Ethical Considerations
Compliance with ethical guidelines
Approval for the study was granted by the Ege University Local Ethics Committee (No.: 2018-5.1/31), and the necessary permits were obtained from the Ege University Medical Hospital, Chest Diseases Department. The written informed consent was obtained from all patients. The questionnaires were anonymous, and participants were assured that their information would be confidential.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, designing, writing the article and final approval: The both authors; Data collection and statistical analysis: Gizem Özbudak.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors gratefully acknowledge the contribution of the participants.
References
Lung cancer is the most common cancer globally and the leading cause of cancer-related death. The World Health Organization (WHO) reported that lung cancer constituted 11.6% of all cancers in 2018, with a total of 2.09 million new cases [1]. According to the 2018 data from the Ministry of Health statistics yearbook, lung cancer is the most common type of cancer in the entire population and males in Turkey and is the fifth most common type in females [2]. Patients with lung cancer have symptoms that can devastate their physical and emotional health [3]. The most common symptoms include dyspnea, cough, weight loss, fatigue, pain, chest pain, anxiety, and depression [4]. Dyspnea is one of the most common and distressing symptoms that limit the daily life activities of individuals and cause a deterioration in the quality of life [5, 6].
Dyspnea is defined as respiratory distress and the sensation of difficulty in breathing. Patients describe this symptom as shortness of breath and an inability to breathe adequately. The prevalence of dyspnea in lung cancer patients has been reported to be between 20% and 90% [7, 8]. Dyspnea harms the quality of life, daily activities, and physical and psychosocial functioning [9]. It is important to identify and eliminate the underlying causes of dyspnea, such as comorbid diseases, and try to relieve the patient [10].
Due to its multidimensional nature, dyspnea management requires pharmacological and nonpharmacological methods [9]. In pharmacological management, medications such as oxygen therapy, opioids, benzodiazepines, phenothiazines, corticosteroids, and inhaler furosemide treat anxiety, agitation, and air hunger accompanying dyspnea [7, 11]. But, because of the troublesome side-effects and costs of pharmaceutical methods, nonpharmaceutical methods are preferable to pharmaceutical methods [8].
Nonpharmacological interventions have been recommended to improve breathing efficiency, manage shortness of breath, and reduce psychological distress, as well as pharmacological interventions to manage dyspnea [11-13]. Nonpharmacological methods alleviate symptoms by creating a holistic approach to cancer care [14]. Physical, behavioral, psychosocial, and environmental changes benefit dyspnea management [12]. In the literature, interventions such as energy conservation techniques, use of fans, staying in a cold room, walking exercises, non-invasive mechanical ventilation, anxiety reduction techniques, Qi therapy, acupuncture, relaxing music, supporting family/caregivers, and training have been reported as nonpharmacological methods used in dyspnea management [11, 15, 16].
Its use, along with pharmacological techniques, increases the effectiveness of the treatments, producing benefits to the patient regarding dyspnea control. It also proves to be beneficial in controlling anxiety and fatigue [17]. We need to determine the nonpharmacological methods patients use for dyspnea and how to apply them [18]. While there is information on what nonpharmacological methods are available in the management of dyspnea, data on the use of these methods by patients are missing [19].
In line with this information, defining the nonpharmacological methods patients use for dyspnea management is important. The study aimed to examine the nonpharmacological methods used by lung cancer patients for dyspnea management and to evaluate the patients’ opinions and their needs and preferences regarding these methods.
Materials and Methods
This cross-sectional study was conducted between June 2018 and September 2018, employing an interview method in an outpatient chemotherapy unit of a university hospital in Izmir, Turkey. All 60 patients of the unit who could communicate, agreed to participate, and could complete the survey form were included. They were at least 18 years old, diagnosed with lung cancer, able to communicate, and described dyspnea during daily activities and agreed to participate. The exclusion criterion was incomplete in filling out the study questionnaires.
In the data collection process, the “patient self-description form”, “verbal rating scale (VRS)”, “dyspnea frequency determination form”, and “dyspnea management form” were prepared by the researchers to evaluate nonpharmacological methods used by patients for the management of dyspnea.
The patient self-description form collected the demographic information. The researchers designed the form, and it consists of two sections: The sociodemographic characteristics (age, gender, height, and weight, body mass index, occupation, current employment, social security, income status, educational status, marital status, with whom they live, and smoking status) and questions concerning the disease (disease diagnosis, time since diagnosis, presence of metastasis, presence of any other chronic disease) [6, 16].
The verbal rating scale (VRS) requires patients to rate their dyspnea from 0 to 10, with 0 indicating no dyspnea and 10 the worst possible level of dyspnea [20, 21].
Determination of dyspnea frequency was created to determine how often patients experience dyspnea, with 5 options: Every day, a few times every day, a few times a week, once a week, and less than once a week [21, 22].
The “dyspnea management form” was designed by the researchers based on the current literature and studies on dyspnea in lung cancer [10, 12]. The form includes a question to ascertain where the patients had access to information about dyspnea management, nonpharmacological applications, and methods, such as slowing down, resting, not overexerting, relaxation-anxiety reduction exercises, getting help in daily life activities, proper sitting position, walking with an assistive device, elevating the head of the bed, physical rehabilitation, walking, opening window, using a room or face fan, nutritional support, not worrying, positive thinking, listening to music, daydreaming, breathing exercises, acupuncture.
Gathering data in the study was done in the outpatient chemotherapy unit. The obtained data were analyzed in SPSS software, version 16. Descriptive statistics were used in the evaluation of the data. The inferential statistics, such as the chi-square and Kruskal-Wallis tests, were used to analyze the obtained data. P<0.05 was considered statistically significant.
Results
The study samples comprised 65% males and 35% females with a Mean±SD age of 63.6±1.73 years; 56.7% were retired, 35% had an education level of high school, 41% were married, and 63% had a smoking history. In terms of the disease characteristics of the patients, 85% were diagnosed with non-small cell lung cancer, the Mean±SD time since diagnosis was 11±6.7 months, and 81.7% did not have metastasis (Table 1).
The Mean±SD VRS score of the patients was 5.2±2.6 (from 0 to 10), and the frequency rates of dyspnea were 48.3% “a few times a week”, 26.7% “a few times every day”, 10% “less than once a week”, 8.3% “once a week”, and 6.7% “all the time”. Of the study sample, 55% stated they had no information about nonpharmacological methods in dyspnea management.
The nonpharmacological methods most used by the patients for the management of dyspnea were slowing down (96.7%), resting and not over-exerting (93.3%), proper sitting position (90%), elevating the head of the bed (90%) and opening windows (88.3). Using a fan in the room (40%), using a fan on the face (25%), breathing exercises (40%), and acupuncture (1.7%) were used less frequently. Patients reported that the frequently used nonpharmacological methods of slowing down, resting, and not overexerting were mostly beneficial. More than half of the patients did not use physical rehabilitation, a room fan, a fan on the face, or breathing exercises, and those who used these methods reported little benefit (Table 2).
The chi-square test showed that the use of nonpharmacological methods was significant in terms of some variables. Female patients used listening to music (P=0.028) and daydreaming (P=0.042) methods more than male patients (Table 3).
There was not any relationship between the frequency of dyspnea based on age, pack-year of smoking, and the time since diagnosis (Table 4).
Discussion
The current study results showed that the frequency of dyspnea was a few times a week. This result indicated that they experienced dyspnea with an average frequency (not very often and not very rarely). Although there are many review articles on this subject, comparable research findings are limited. Similar to the results of the current study, Weingärtner et al. evaluated patients diagnosed with chronic obstructive pulmonary disease and lung cancer and reported that those with lung cancer described the frequency of dyspnea as 1-3 times a week, and most of them had a history of smoking [23]. Another study reported that the incidence of dyspnea is higher (several times a day) in patients receiving lung cancer treatment [22]. In studies in the relevant literature, the prevalence of dyspnea in patients with lung cancer has been reported to vary between 21% and 90% [7, 8].
Over half of the current study patients had no information about nonpharmacological methods for managing dyspnea. There is, therefore, a clear need for these patients to be informed about nonpharmacological methods.
In the study, nonpharmacological methods most used by the patients to manage dyspnea were slowing down, resting and not over-exerting, proper sitting position, elevating the head of the bed, and opening windows. Using a fan (room), a fan on the face, breathing exercises, and acupuncture were used less frequently. This result shows that physiological methods are used more, and psychological support methods are less preferred or unknown.
In a qualitative study by Simon et al., lung cancer patients said they reduced physical activity, rested, and lay in bed to relieve dyspnea. The patients stated that resting and not overexerting strategies were the most effective. Also, calming down, relaxing, and showing a positive attitude were beneficial as cognitive and psychological strategies. Most patients reported using several pillows to raise the upper body and sleep upright. It has been determined that using a fan is not common, but fresh and cold air makes the patient feel better [24]. Similarly, Yates et al. reported that the dyspnea methods used most frequently by lung cancer patients were slowing down, resting, positive thinking, and not overexerting or worrying. The less frequently used strategies were comfortable positioning, window opening, and using a fan on the face [12]. In a qualitative study by Linde et al., it was determined that patients with lung cancer motivated themselves with an affirmation of “calm down, everything will be better”, most of the patients stated that they relaxed with breathing exercises and appropriate positioning [25].
In the current study, methods developed by individuals based on their own experience were used more frequently, and methods requiring the knowledge and support of health professionals less frequently. The often-used methods by patients can be attributed to reasons such as no cost, personal experience, and few or no side effects.
The orthopnea position, which is a forward bending position with the patient extending his hands and arms towards his legs or raising them towards an object such as a table, is a suitable sitting position, improves oxygenation and reduces inspiratory effort, thereby allowing the patient to breathe more comfortably [26].
The current study showed that more than half of the individuals do not use a room fan, a fan on the face, or breathing exercises. Also, the individuals who use these methods have reported insignificant benefits from these methods. This finding may be due to the low awareness of individuals about evidence-based nonpharmacological methods and or application errors in the management of dyspnea. The stimulation of mechanoreceptors in the face area or cooling of the skin with a hand fan application to the face creates central inhibition of dyspnea and decreases the feeling of dyspnea by stimulating the second and third branches of the trigeminal nerve. A face fan is recommended to be used for about 5 minutes at a distance of 15-30 cm from the lip and mouth area [10, 27]. Breathing exercises have been reported to improve the perception of dyspnea, lung function, exercise capacity, and health-related quality of life parameters [28]. Teaching respiratory exercises to reduce shortness of breath is another important component of the approach to patients [29].
Patients have not used acupuncture, a widely used traditional Chinese therapy to manage dyspnea. The clinical efficacy of acupuncture has been evaluated with numerous randomized controlled studies [30, 31]. Acupuncture has been reported to provide control of dyspnea by providing endogenous opioid release and limbic system stimulation [28]. In Turkey, acupuncture practice may be limited for reasons such as not being part of traditional Turkish culture, being unable to easily adopt new applications, having health concerns, and lacking information [30].
The current study showed that mostly female patients used the methods of listening to music and daydreaming. This result can be related to the fact that females have a greater psychological ability to divert attention. Methods such as relaxation exercises, listening to music, and not worrying positively affect dyspnea and reduce anxiety and distress [12]. A sense of control over dyspnea can be achieved by drawing attention to a pleasurable experience or feeling. However, no study has evaluated the factors affecting nonpharmacological methods used by lung cancer patients.
In conclusion, the studies on nonpharmacological methods for dyspnea management are limited, and the frequency and awareness of evidence-based nonpharmacological methods for dyspnea management are low. Due to the lack of studies in this field and weak evidence to determine the value and acceptability of nonpharmacological methods used in dyspnea caused by lung cancer, studies such as this are significant. It is also the nurse’s responsibility within the multidisciplinary team to provide training for all these methods for patients with lung cancer.
Dyspnea is a common symptom in individuals with lung cancer, but its management is still inadequate, and there is no information about effective coping strategies [24].
This research revealed that the patients need training on current strategies to manage dyspnea and use nonpharmacological methods. With nonpharmacological methods, the feeling of shortness of breath experienced by the individual during dyspnea decreases both psychologically and physiologically, and respiratory control is provided [17]. An increase in nonpharmacological methods, which have an important place in the management of dyspnea, will provide greater benefit. In particular, patients should be guided and encouraged to perform breathing exercises and use a fan on the face with the correct method and technique [32]. The small number of samples that meet the criteria for entering the research and the use of one questionnaire to determine the performance of patients in dyspnea relief are the limitations of the present research.
Ethical Considerations
Compliance with ethical guidelines
Approval for the study was granted by the Ege University Local Ethics Committee (No.: 2018-5.1/31), and the necessary permits were obtained from the Ege University Medical Hospital, Chest Diseases Department. The written informed consent was obtained from all patients. The questionnaires were anonymous, and participants were assured that their information would be confidential.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, designing, writing the article and final approval: The both authors; Data collection and statistical analysis: Gizem Özbudak.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors gratefully acknowledge the contribution of the participants.
References
- World Health Organization. International agency for research on cancer. Geneva: World Health Organization; 2020. [Link]
- Başara BB, Çağlar IS, Aygün A, Özdemir TA, Kulali B, Uzun SB, et al. TC. The Ministry of Health of Turkey Health Statistics Yearbook 2018. Ankara: Ministry of Health Publication; 2019. [Link]
- Choi S, Ryu E. Effects of symptom clusters and depression on the quality of life in patients with advanced lung cancer. Eur J Cancer Care (Engl). 2018; 27(1):e12508. [DOI:10.1111/ecc.12508] [PMID]
- Polański J, Jankowska-Polańska B, Mazur G. Relationship between nutritional status and quality of life in patients with lung cancer. Cancer Manag. Res. 2021; 13:1407-16. [DOI:10.2147/CMAR.S287551] [PMID]
- Kocatepe V, Can G, Oruç Ö. Lung cancer-related dyspnea: The effects of a handheld fan on management of symptoms. Clin J Oncol Nurs. 2021; 25(6):655-61. [DOI:10.1188/21.CJON.655-661] [PMID]
- Garratt AM, Nerheim EM, Einvik G, Stavem K, Edvardsen A. Evaluation of the norwegian version of the dyspnoea-12 questionnaire in patients with COPD. BMJ Open Respir Res. 2022; 9(1):e001262.[DOI:10.1136/bmjresp-2022-001262] [PMID]
- Metin ZG, Dönmez A. Dyspnea management in patients with cancer. Turk J Oncol. 2016; 31(2):61-7. [DOI:10.5505/tjo.2016.1366]
- Yodang Y. Non-pharmacological breathlessness management in older patients: A review study. J Client-Cent Nurs Care. 2019; 5(1):1-14. [DOI:10.32598/jccnc.5.1.1]
- Hui D, Maddocks M, Johnson MJ, Ekström M, Simon ST, Ogliari AC, et al. Management of breathlessness in patients with cancer: ESMO clinical practice guidelines. ESMO Open. 2020; 5(6):e001038. [DOI:10.1136/esmoopen-2020-001038] [PMID]
- Kamal AH, Maguire JM, Wheeler JL, Currow DC, Abernethy AP. Dyspnea review for the palliative care professional: Treatment goals and therapeutic options. J Palliat Med. 2012; 15(1):106-14. [DOI:10.1089/jpm.2011.0110] [PMID]
- Ambrosino N, Fracchia C. Strategies to relieve dyspnoea in patients with advanced chronic respiratory diseases. A narrative review. Pulmonology. 2019; 25(5):289-98. [DOI:10.1016/j.pulmoe.2019.04.002] [PMID]
- Yates P, Zhao I. Update on complex nonpharmacological interventions for breathlessness. Curr Opin Support Palliat Care. 2012; 6(2):144-52. [DOI:10.1097/SPC.0b013e3283536413] [PMID]
- Zemel RA. Pharmacologic and non- pharmacologic dyspnea management in advanced cancer patients. Am J Hosp Palliat Care. 2022; 39(7):847-55. [DOI:10.1177/10499091211040436] [PMID]
- Swan F, Newey A, Bland M, Allgar V, Booth S, Bausewein C, et al. Airflow relieves chronic breathlessness in people with advanced disease: An exploratory systematic review and meta-analyses. Palliat Med. 2019; 33(6):618-33. [DOI:10.1177/0269216319835393] [PMID]
- Joyce A, Fair N, Fongeh T. An overview of the non-pharmacological and non-surgical management of chronic obstructive pulmonary disease. Med Ress Arch. 2020; 8(6). [DOI:10.18103/mra.v8i6.2178]
- Smith TA, Roberts MM, Cho JG, Klimkeit E, Luckett T, McCaffrey N, et al. Protocol for a single-blind, randomized, parallel-group study of a nonpharmacological integrated care intervention to reduce the impact of breathlessness in patients with chronic obstructive pulmonary disease. Palliat Med Rep. 2020; 1(1):296-306. [DOI:10.1089/pmr.2020.0081] [PMID]
- Ramos A, Tavares AP, Lopes M, Mendes P, Parreira P, Fonseca C, et al. Control of pain and dyspnea in patients with oncologic disease in acute care: Non-pharmacological interventions. Nurs Care Open Access J. 2017;2(3):71-5. [DOI:10.15406/ncoaj.2017.02.00036]
- Wangsom A, Matchim Y. Dyspnea management in patients with COPD: Non-pharmacological strategies. J Res Nurs Midwifery Health Sci. 2017; 37(4):108-17. [Link]
- Lutter JI, Lukas M, Schwarzkopf L, Jörres RA, Studnicka M, Kahnert K, et al. Utilization and determinants of use of non-pharmacological interventions in COPD: Results of the COSYCONET cohort. Respir Med. 2020; 171:106087. [DOI:10.1016/j.rmed.2020.106087] [PMID]
- Biber Ç. Assessment of dyspnea in pulmonary rehabilitation [Turkish]. Updates On Pulmonary Diseases. 2019; 7(1):19-25. [Link]
- Zhuang Q, Yang GM, Neo SH, Cheung YB. Validity, reliability, and diagnostic accuracy of the Respiratory Distress Observation Scale for assessment of dyspnea in adult palliative care patients. J Pain Symptom Manage. 2019; 57(2):304-10. [DOI:10.1016/j.jpainsymman.2018.10.506] [PMID]
- Hately J, Laurence V, Scott A, Baker R, Thomas P. Breathlessness clinics within specialist palliative care settings can improve the quality of life and functional capacity of patients with lung cancer.Palliat Med. 2003; 17(5):410-17. [DOI:10.1191/0269216303pm752oa] [PMID]
- Weingärtner V, Scheve C, Gerdes V, Schwarz-Eywill M, Prenzel R, Otremba B, et al. Characteristics of episodic breathlessness as reported by patients with advanced chronic obstructive pulmonary disease and lung cancer: Results of a descriptive cohort study. Palliat Med. 2015; 29(5):420-8. [DOI:10.1177/0269216314563428] [PMID]
- Simon ST, Weingärtner V, Higginson IJ, Benalia H, Gysels M, Murtagh FE, et al. I Can Breathe Again!’’ patients’ self-management strategies for episodic breathlessness in advanced disease, derived from qualitative interviews.J Pain Symptom Manage. 2016; 52(2):228-34. [DOI:10.1016/j.jpainsymman.2016.02.016] [PMID]
- Linde P, Hanke G, Voltz R, Simon ST. Unpredictable episodic breathlessness in patients with advanced chronic obstructive pulmonary disease and lung cancer: A qualitative study. Support Care Cancer. 2018; 26(4):1097-104. [DOI:10.1007/s00520-017-3928-9] [PMID]
- Cambell ML. Dyspnea. Crit Care Nurs Clin North Am. 2017; 29(4):461-70. [DOI:10.1016/j.cnc.2017.08.006] [PMID]
- Kako J, Kobayashi M, Oosono Y, Kajiwara K, Miyashita M. Immediate effect of fan therapy in terminal cancer with dyspnea at rest: A meta-analysis.Am J Hosp Palliat Care. 2020; 37(4):294-9. [DOI:10.1177/1049909119873626] [PMID]
- Yun R, Bai Y, Lu Y, Wu X, Lee SD. How breathing exercises influence on respiratory muscles and quality of life among patients with COPD? A systematic review and meta-analysis. Can Respir J. 2021; 2021:1904231. [DOI:10.1155/2021/1904231] [PMID]
- Yılmaz Ü. [Palliative approaches in dyspnea treatment (Turkish)]. Palliat Care Assoc. 2018; 1-13. [Link]
- Pehlivan S, Süner A, Yıldırım Y, Fadıloğlu Ç. Investigation into complementary and ıntegrative health approaches for Turkish patients with gastrointestinal cancer. J Relig Health. 2018; 57(4):1497-508. [DOI:10.1007/s10943-017-0546-2] [PMID]
- Maekura T, Miki K, Miki M, Kitada S, Maekura R. Clinical effects of acupuncture on the pathophysiological mechanism of chronic obstructive pulmonary disease during exercise. Int J Chron Obstruct Pulmon Dis. 2019; 14:2787-98. [DOI:10.2147/COPD.S225694] [PMID]
- von Trott P, Oei SL, Ramsenthaler C. Acupuncture for breathlessness in advanced diseases: A systematic review and meta-analysis. J Pain Symptom Manage. 2020; 59(2):327-38. [DOI:10.1016/j.jpainsymman.2019.09.007] [PMID]
Article Type : Research |
Subject:
Special
Received: 2023/06/28 | Accepted: 2023/06/29 | Published: 2023/06/29
Received: 2023/06/28 | Accepted: 2023/06/29 | Published: 2023/06/29
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |