Mon, Dec 1, 2025
Volume 35, Issue 2 (3-2025)
JHNM 2025, 35(2): 98-108 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Misaghi M, Jahani S, Haghighi S B, Maraghi E, Sayadi N. Relationship of the Alternative Communication Methods by Nurse With Work Environment and Patient Safety Culture in Intensive Care Units. JHNM 2025; 35 (2) :98-108
URL: http://hnmj.gums.ac.ir/article-1-2183-en.html
URL: http://hnmj.gums.ac.ir/article-1-2183-en.html
1- Nursing (Msc), Department of Nursing, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
2- Associated Professor, Department of Nursing and Midwifery, Nursing Care Research Center in Chronic Disease, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
3- Assistant Professor, Department of English Language, School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
4- Assistant Professor, Department of Biostatistics and Epidemiology, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
5- Associated Professor, Department of Nursing and Midwifery, Nursing Care Research Center in Chronic Disease, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,sayadi_neda@yahoo.com
2- Associated Professor, Department of Nursing and Midwifery, Nursing Care Research Center in Chronic Disease, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
3- Assistant Professor, Department of English Language, School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
4- Assistant Professor, Department of Biostatistics and Epidemiology, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
5- Associated Professor, Department of Nursing and Midwifery, Nursing Care Research Center in Chronic Disease, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,
Full-Text [PDF 491 kb]
(303 Downloads)
| Abstract (HTML) (874 Views)
Full-Text: (190 Views)
Introduction
Effective communication enables healthcare personnel to establish rapport with their patients, obtain crucial health information and work effectively with all healthcare team members. Nurses are always expected to maintain good communication and approach every patient with the intention to understand their concerns [1]. Good communication between nurses and patients is more important in intensive care units (ICUs) as it helps patients perceive their illnesses more positively. According to the statistics of the Iranian Society of Anesthesiology and Critical Care, 1.5-2 million people annually refer to hospitals due to road accidents, strokes and other reasons, of whom 30% need to be hospitalized in the ICU [2]. When normal ways of speaking and writing are restricted in patients, augmentative and alternative communication (AAC) is employed [1]. It refers to the use of strategies or auxiliary tools to support, enhance or replace normal spoken communication [3].The scope of AAC systems varies from simple level that does not require electronic devices (e.g. pen and paper, symbols, communication boards, or books) to high technology levels that include speech generating devices or electronic equipments [4].
Studies have confirmed that nurse-patient communication affects the quality of patient care and safety [5]. Patient safety refers to an environment free of harm in which patients and caregivers apply safety standards, thereby reducing the risks of an unnecessary action [6]. Evaluation of safety culture in hospitals is generally encouraged by policymakers and healthcare managers [7]. Nurses are the key members of a healthcare team, and their role in care-giving and protection and promotion of the healthcare system has been globally established [8]. Among the key factors that affect patient safety is the nursing work environment. According to the American Nurses Association, the nursing work environment includes all effective factors and indicators of nursing performance, including skilled communication, true collaboration, and effective decision-making [9]. Relationship with colleagues, nurse-to-patient staffing ratio, and management and leadership methods, along with the tools and facilities available in the department, are factors related to nursing work environment that can significantly affect the provision of safe patient care [10]. The results of the studies have shown that the cause of almost all accidents in the work environment is the lack of proper communication between caregivers and patients; 75% of medical errors and 65% of accidents during work shifts are due to improper communication [11-15].
Overall, the literature review revealed that safety culture is affected by factors such as communication and work environment; however, there are few studies on the relationship between patient safety and AAC. In this regard, this study aims to determine the usage rate of AAC by ICU nurses in Ahvaz, southwest of Iran, and assess its relationship with nursing work environment and patient safety culture.
Materials and Methods
This is a correlational study with a cross-sectional design. The study population comprised all permanent and contractual nurses working in the ICUs of selected hospitals in Ahvaz, southwest of Iran. They all were included in study using a census method. The inclusion criteria were at least 6 months of work experience in the ICU, at least a bachelor’s degree, willingness to participate in the study, and complete responses to the questionnaires. Of the 378 nurses, 249 were eligible to participate in this research. Data were collected from May to June 2022 using three questionnaires, including the hospital survey on patient safety culture (HSOPSC), the nursing work index (NWI), and the AAC scale.
The HSOPSC is a field questionnaire designed by the agency for healthcare research and quality [16]. It has 42 items and 12 dimensions of patient safety culture. Each item is rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The dimensions include overall perception of continuous improvement/organizational learning, frequency of reported events, overall perception of patient safety, employees/manager expectations and actions promoting patient safety, communication openness, teamwork within the department, feedback and communication about errors, non-punitive response to errors, staffing, teamwork across hospital departments, hospital management support for patient safety, and hospital handoff and transitions. Those with a positive response >75% are considered as areas of strength, and those with a positive response <50% are considered as areas of weakness that require intervention. Those with a positive response between 50-70% are the areas with potential for improvement. In this study, the Persian version of the HSOPSC was used [17].
The NWI is a standard tool designed by Lake et al. It has 34 items rated on a 4-point Likert scale as: 1) Completely disagree, 2) Somewhat disagree, 3) Somewhat agree and 4) Completely agree. This questionnaire has five domains: Nurse participation in hospital affairs (11 items), nursing foundations for quality of care (9 items), nurse/manager ability (7 items), adequacy of resources and staffing (4 items), and collegial nurse-physician relations (3 items). A score above 2.5 in each domain indicates the favorable level of work environment, and a score <2.5 indicates a poor level of work environment [18]. In this study, the Persian version of NWI was used [19].
The AAC scale was used to rate nurses’ use of AAC methods. It was developed by Jansson et al. [8] and has 16 items, measuring demographic information (items 1-10), care needs of special people, such as disabled patients (items 11 and 12 each with four options), communication methods and obtaining information from the patient (items 13 and 14 rated on a Likert scale from 4 [always] to 0 [never]) and the types of AAC methods (items 15 and 16 answered by yes or no). The total score is not calculated. The forward-backward translation method was used to translate the scale from English to Persian, performed by two experts with PhD in English Language Teaching. To confirm the validity of the tool, the content validity was checked by 10 experts with experience working in ICU, including 6 nurses and 4 anesthesiologists. Next, the content validity index (CVI) was calculated for each item and the subscales. The acceptable CVI score for each item is 0.8 or higher, and the acceptable CVI score for each subscale is 0.9 or higher [20]. To examine the reliability of the Persian AAC scale, Cronbach’s α coefficient was calculated, and the acceptable value of 0.74 was obtained.
Before data collection, the study objectives were explained to the participants and their informed consent was obtained. After collection, continuous data were reported as Mean±SD and categorical data as number (percentage). The normality of continuous data was assessed using the Shapiro-Wilks test. The association between the frequency of using each AAC method and the scores of HSOPSC and NWI was assessed using Spearman’s correlation test. P<0.05 were considered statistically significant. All analyses were done in SPSS software, version 22 (IBM Corp., Armonk, NY).
Results
Th mean age of participants was 30.96±6.63 years, and most of them were female (87.1%). Table 1 presents other characteristics of participants.
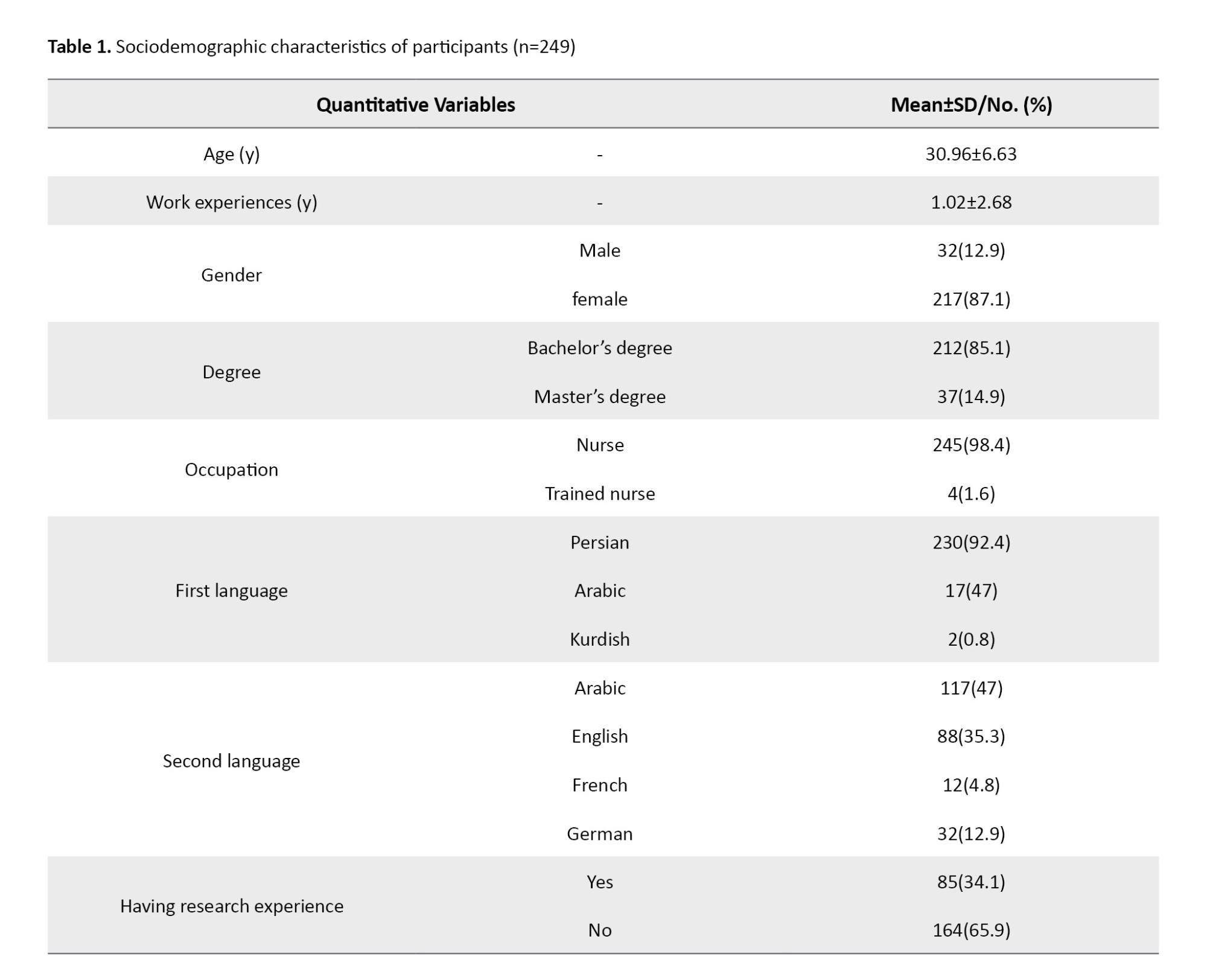
Table 2 presents the frequency of using AAC methods by nurses. The most common method of communication with patients was verbal method as 61(24.5%) nurses had always used verbal communication method.
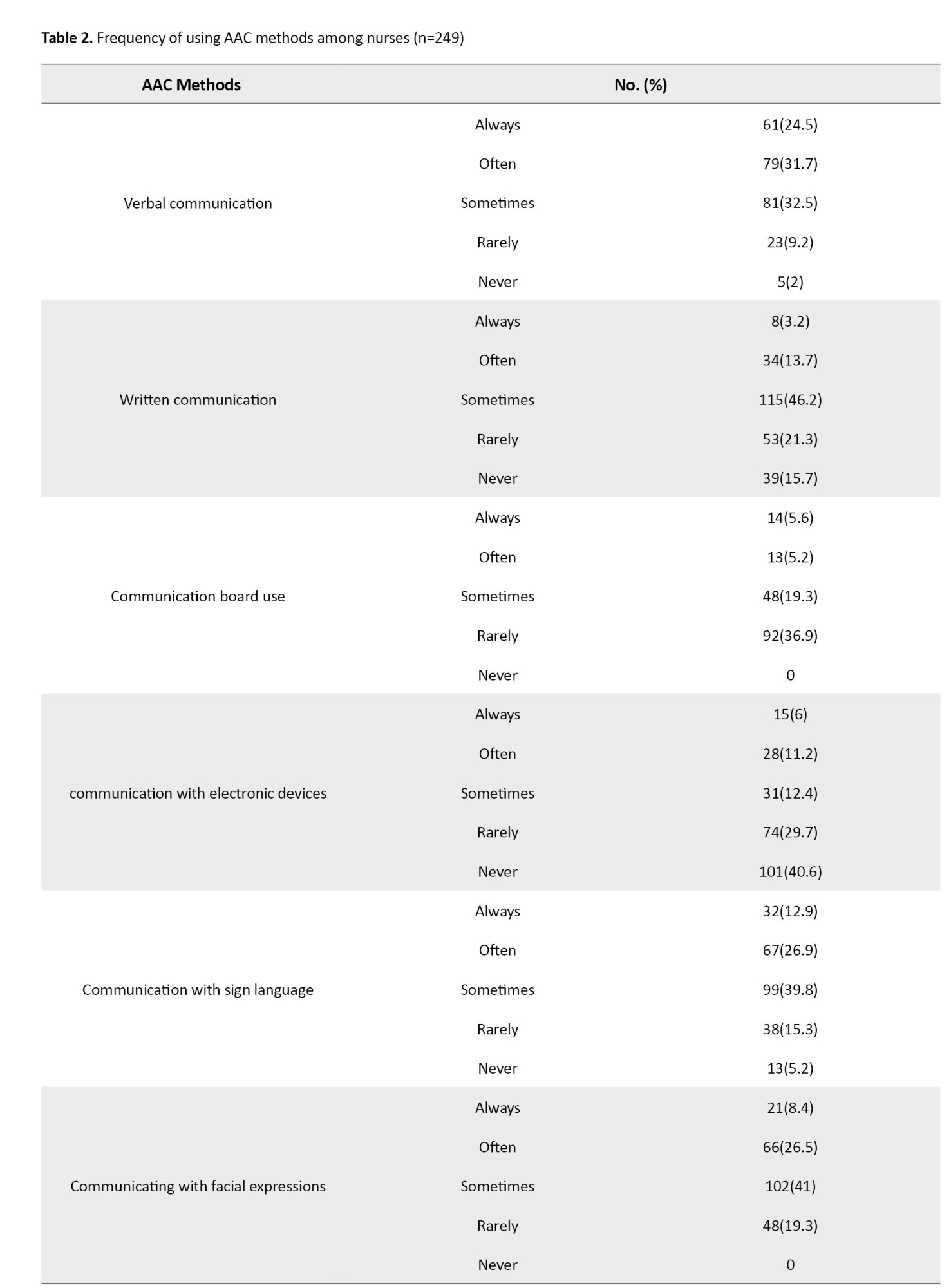
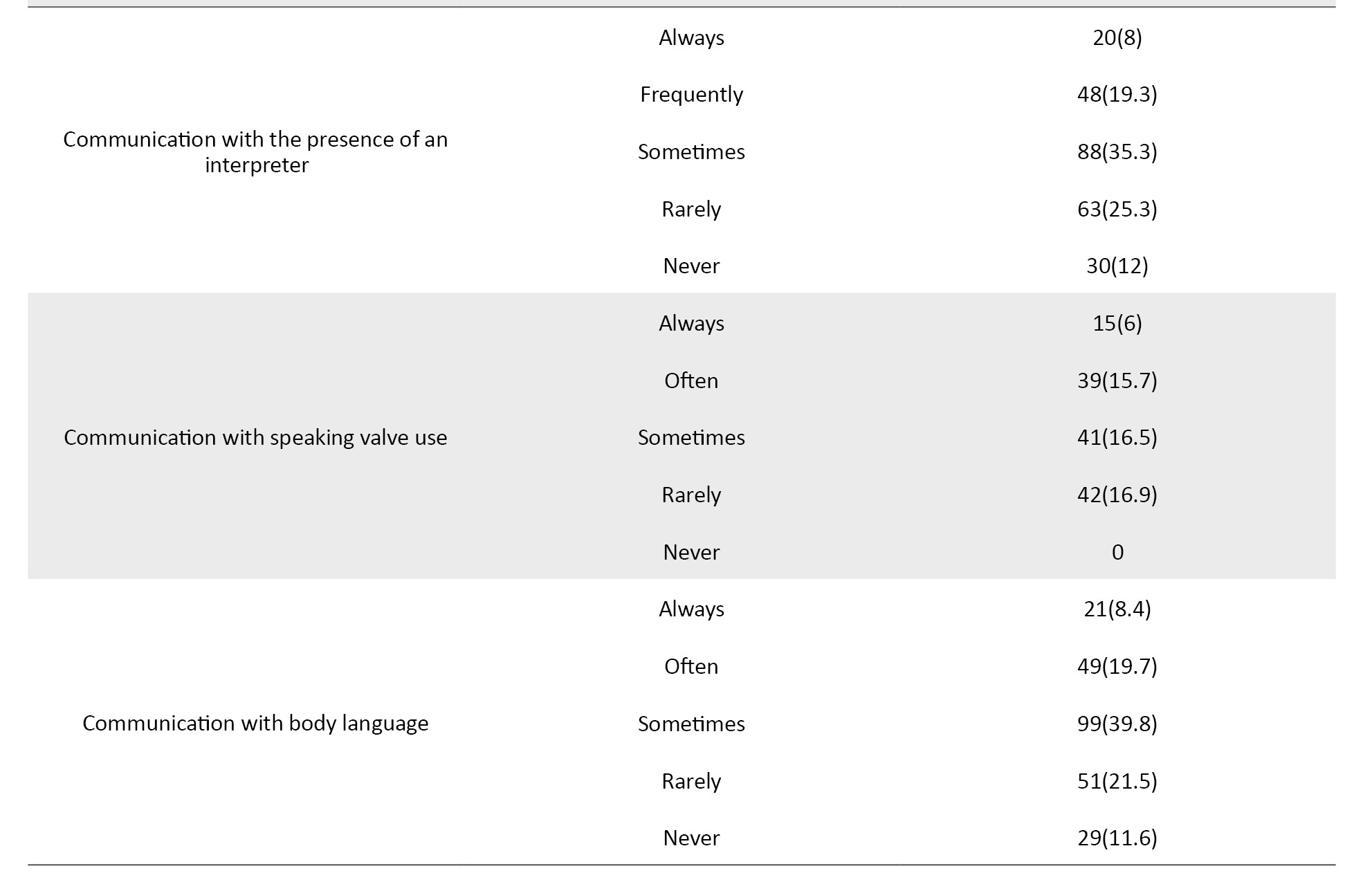
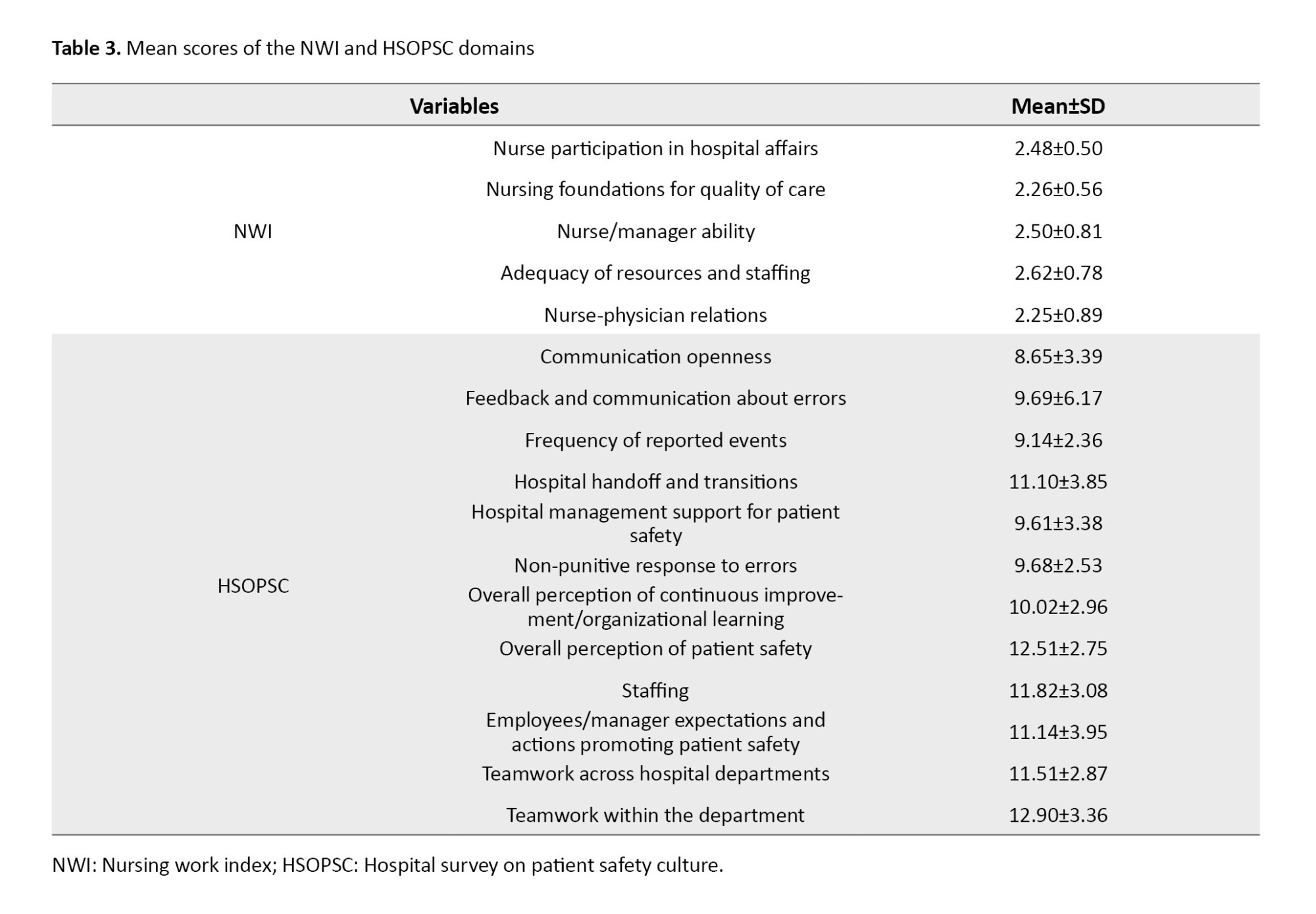
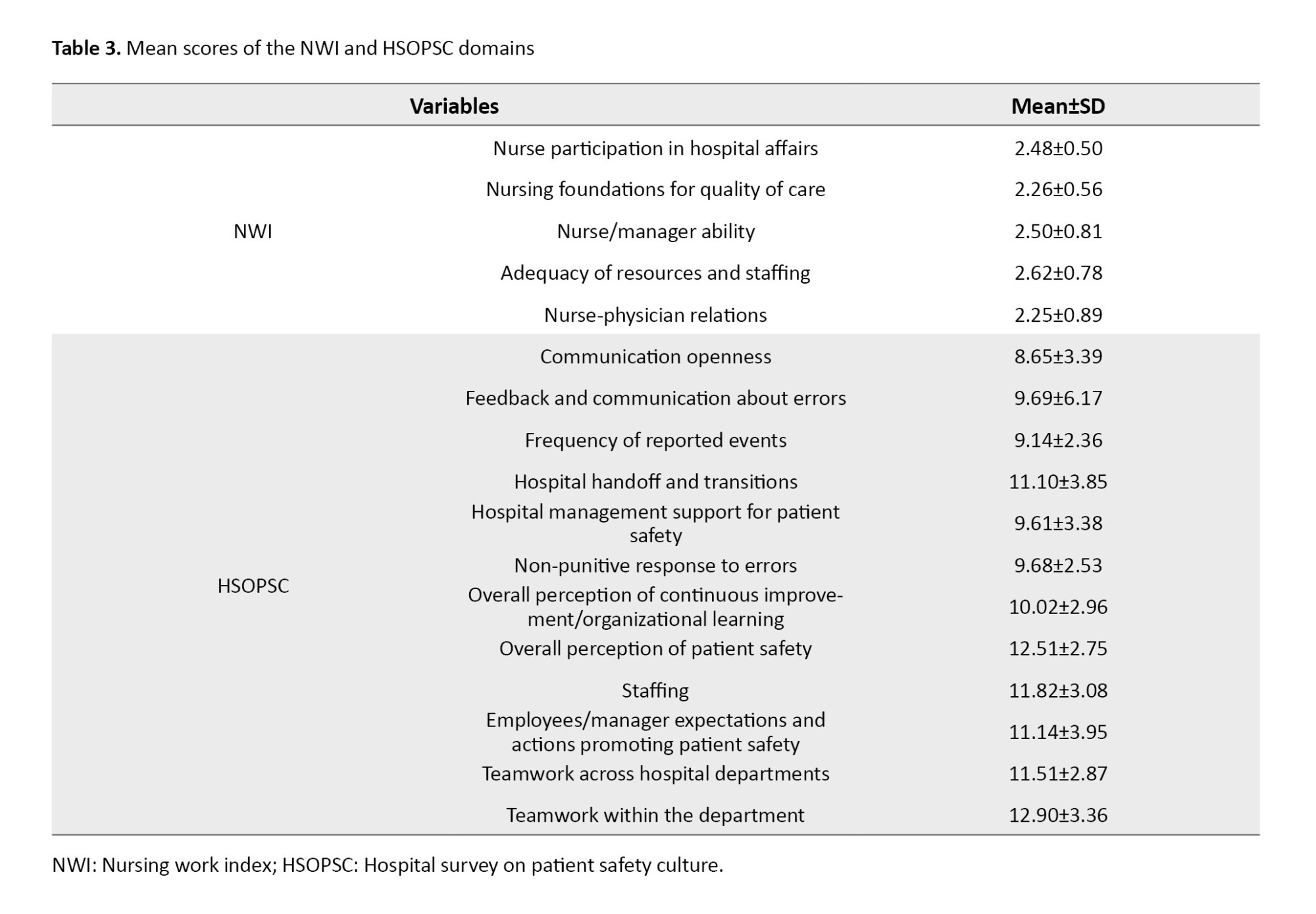
The least commonly used AAC method (n=15, 6%) was communication with electronic devices. Concerning the tools for communication with ICU patients, the call bell was the most common tool (n=93, 37.3%), while the least used communication tool was the speech production tool (n=13, 2.5%). The mean scores of NWI and HSOPSC domains are shown in Table 3.
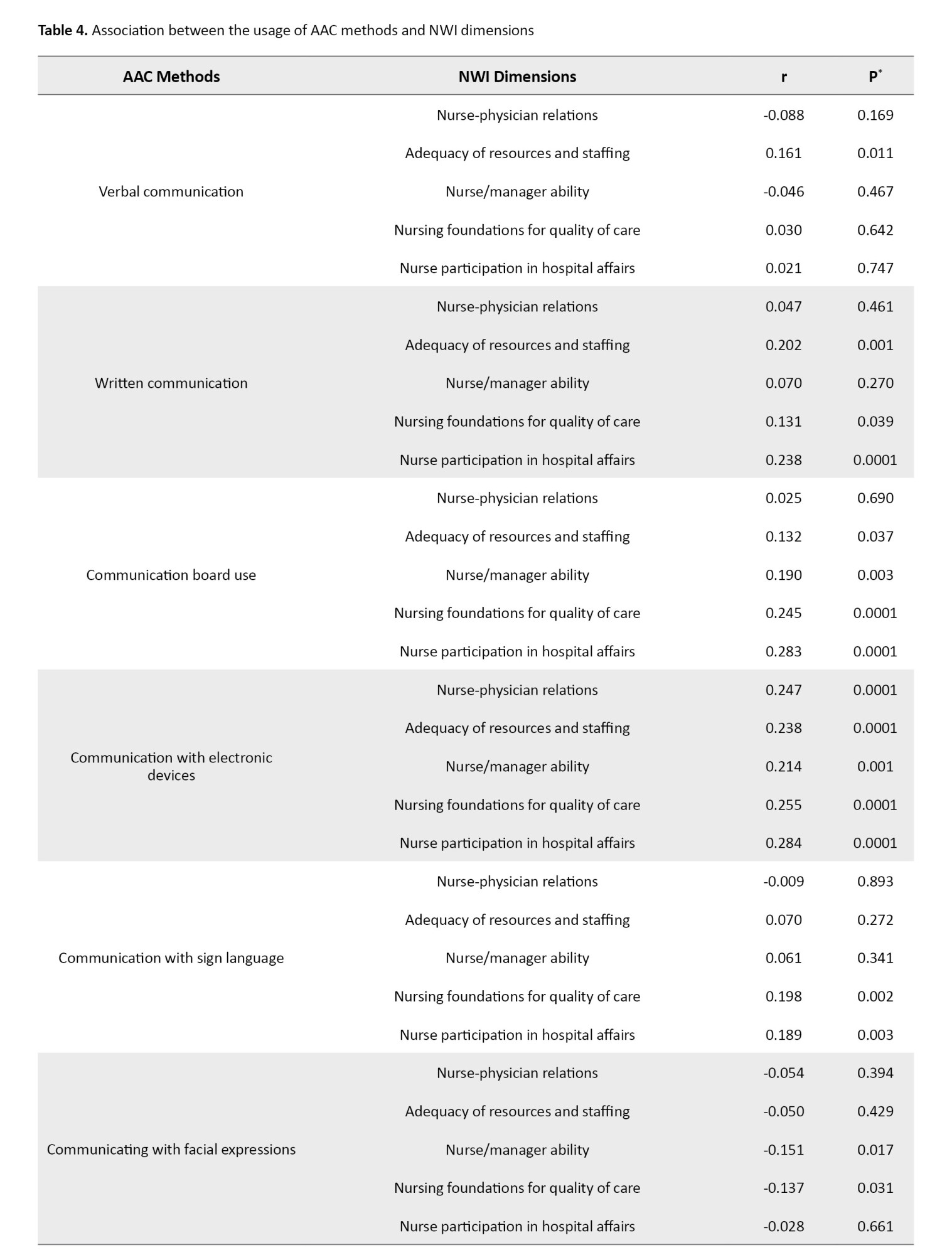
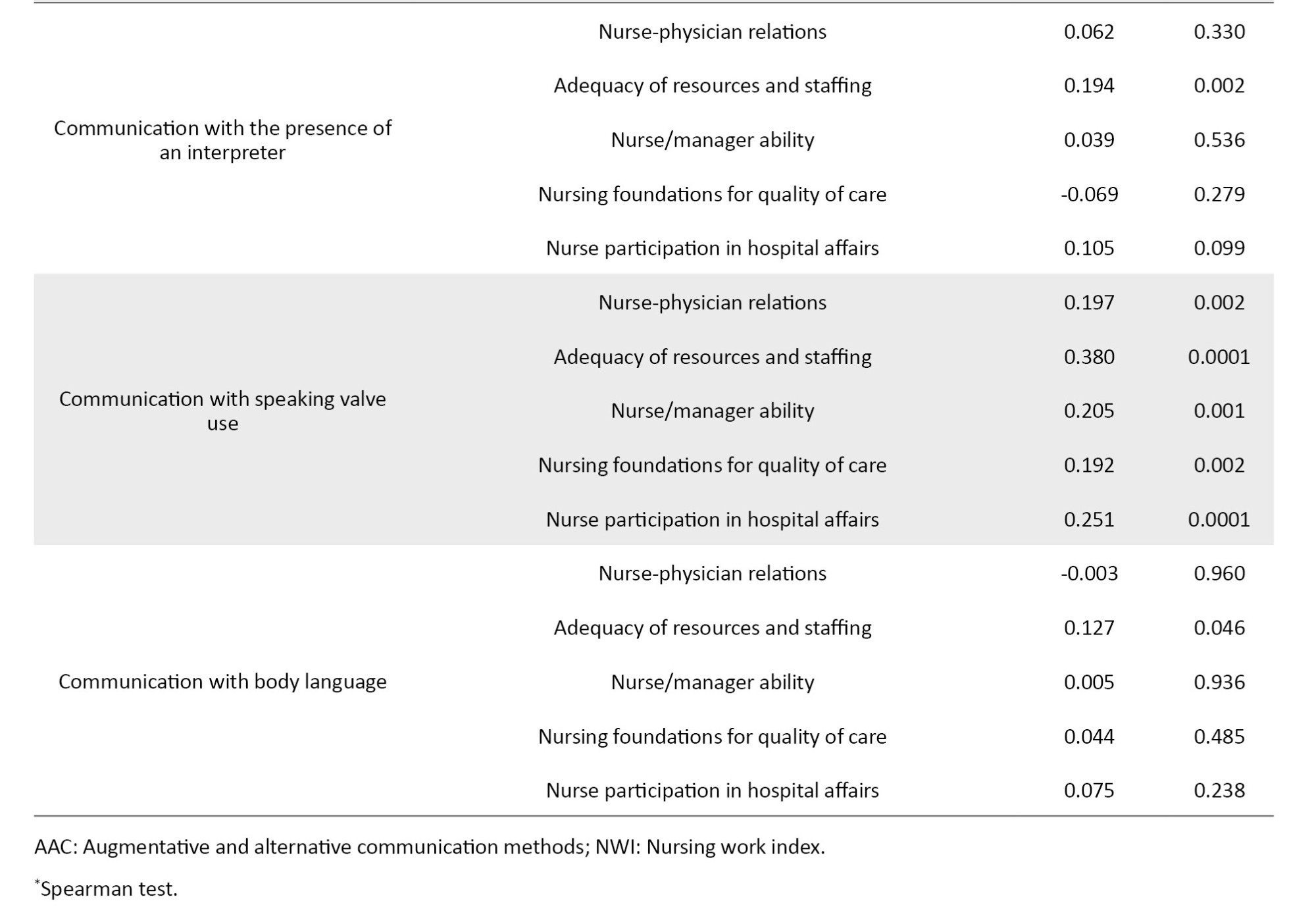
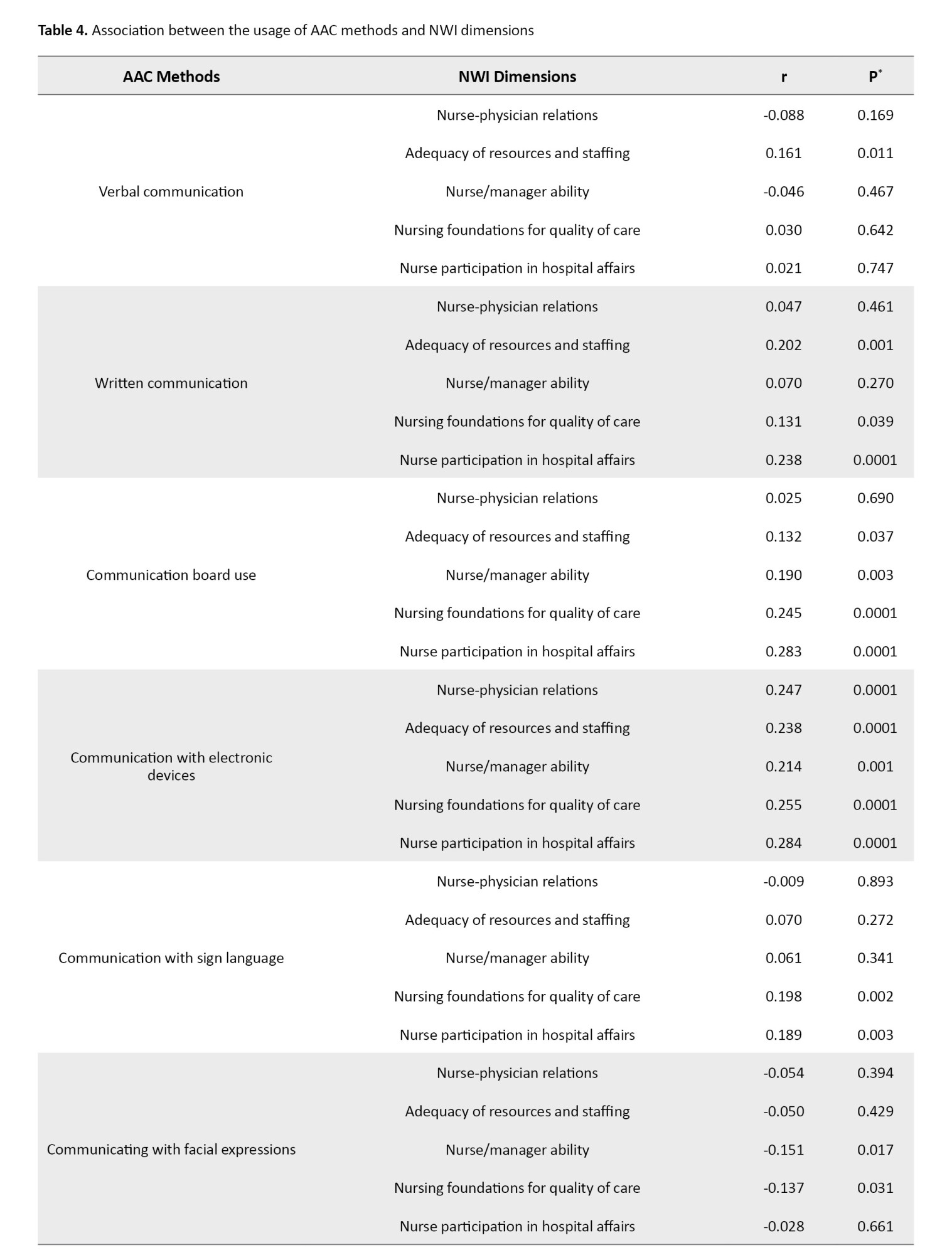
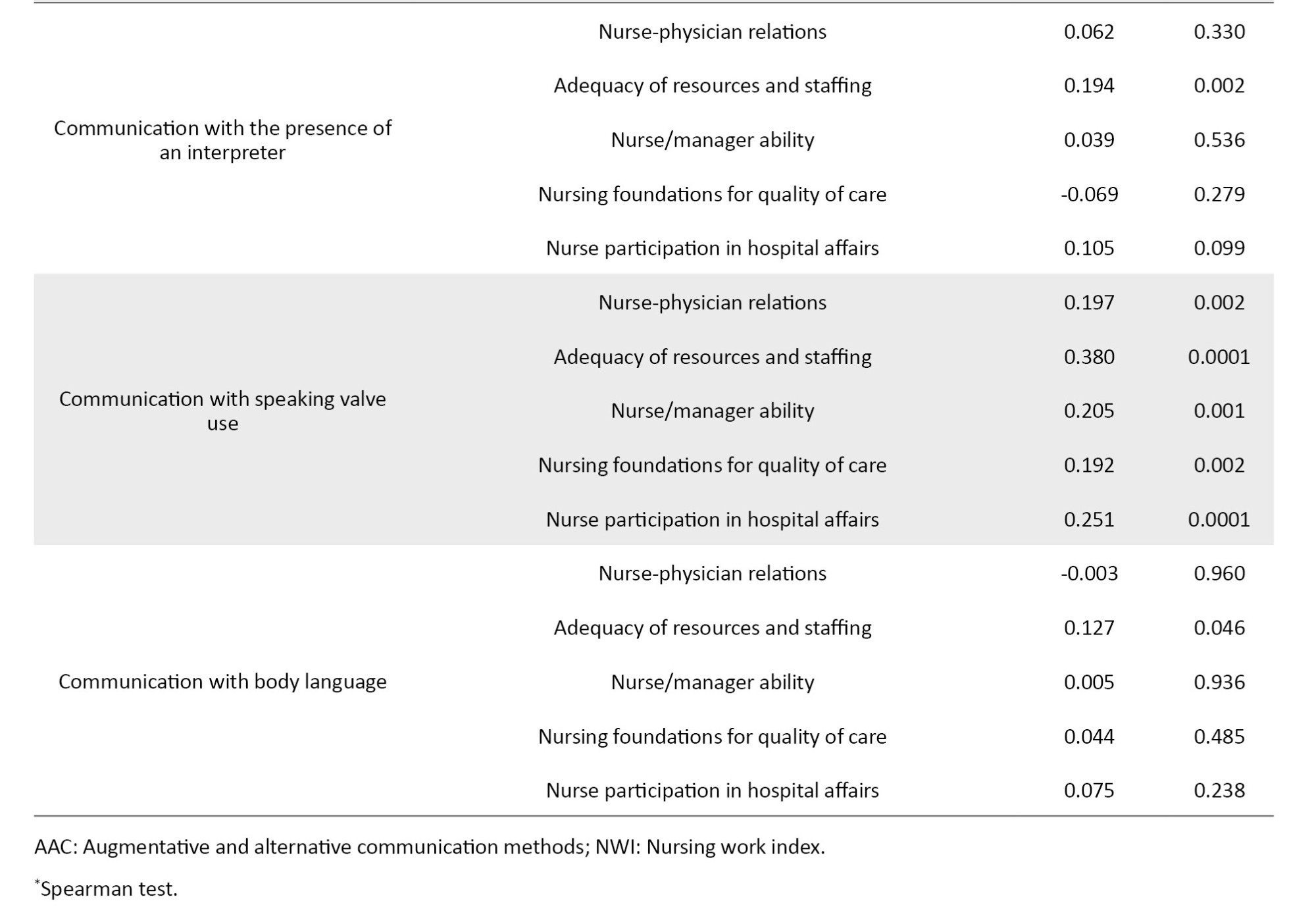
To assess the relationship between the usage of AAC methods and NWI dimensions, Spearman’s test was used. The results are presented in Table 4. There was a significant relationship between communication board use and nurse participation in hospital affairs (r=0.283, P=0.001), between communication with electronic devices and nurse participation in hospital affairs (r=0.284, P=0.001), and between speaking valve use and adequacy of resources and staffing (r=0.380, P=0.001).
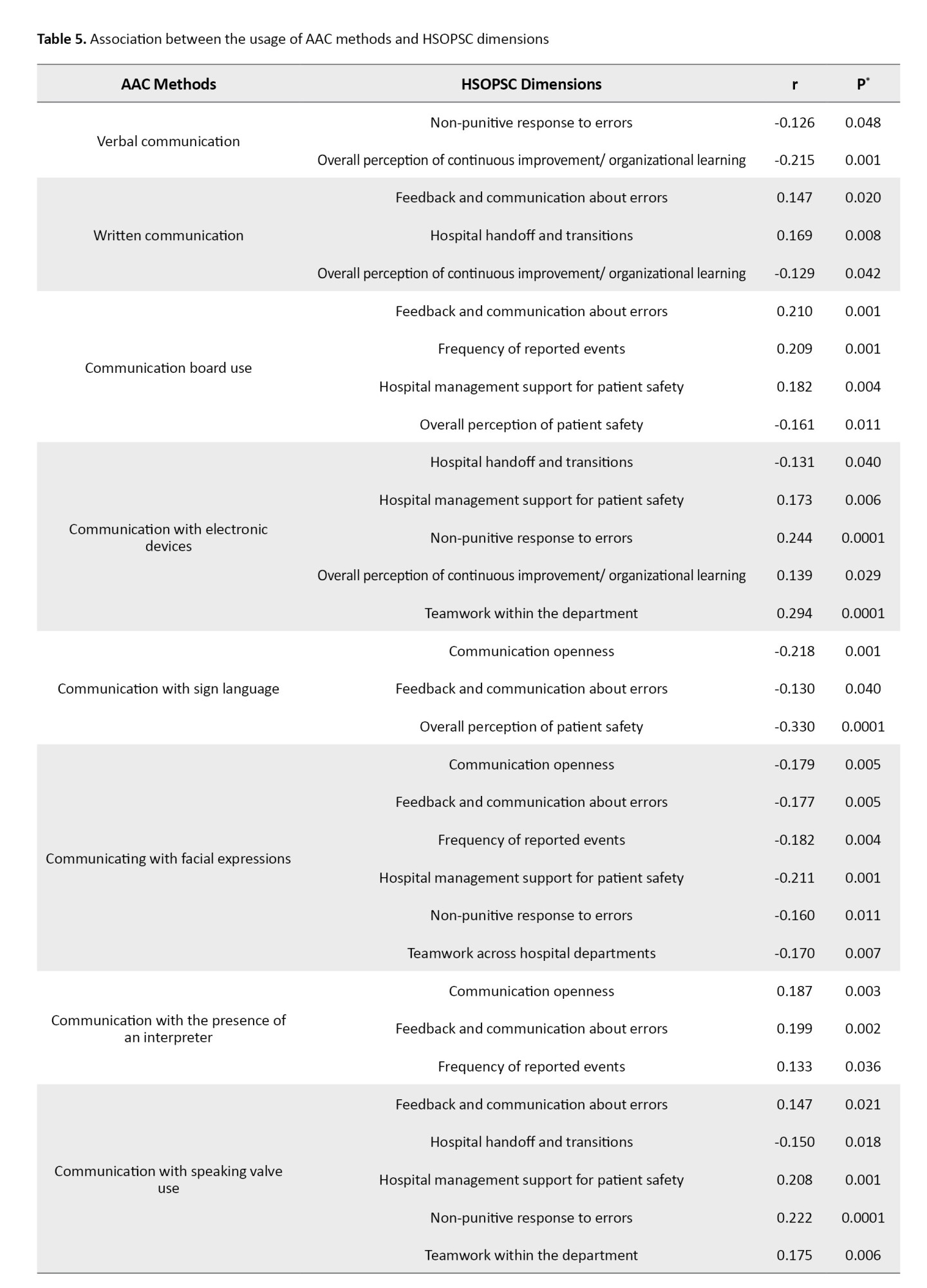
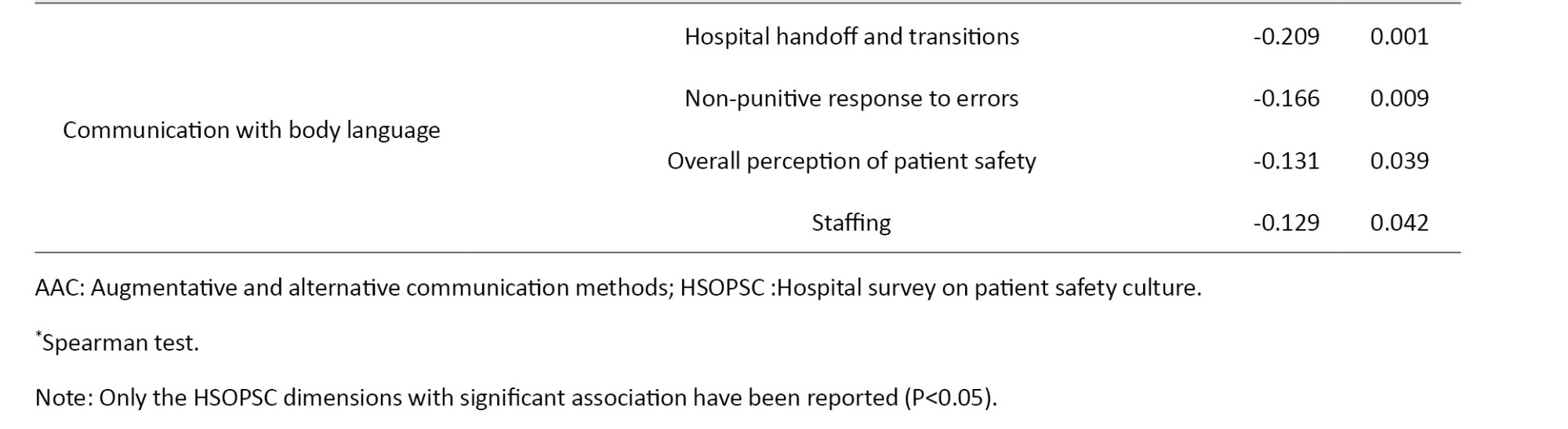
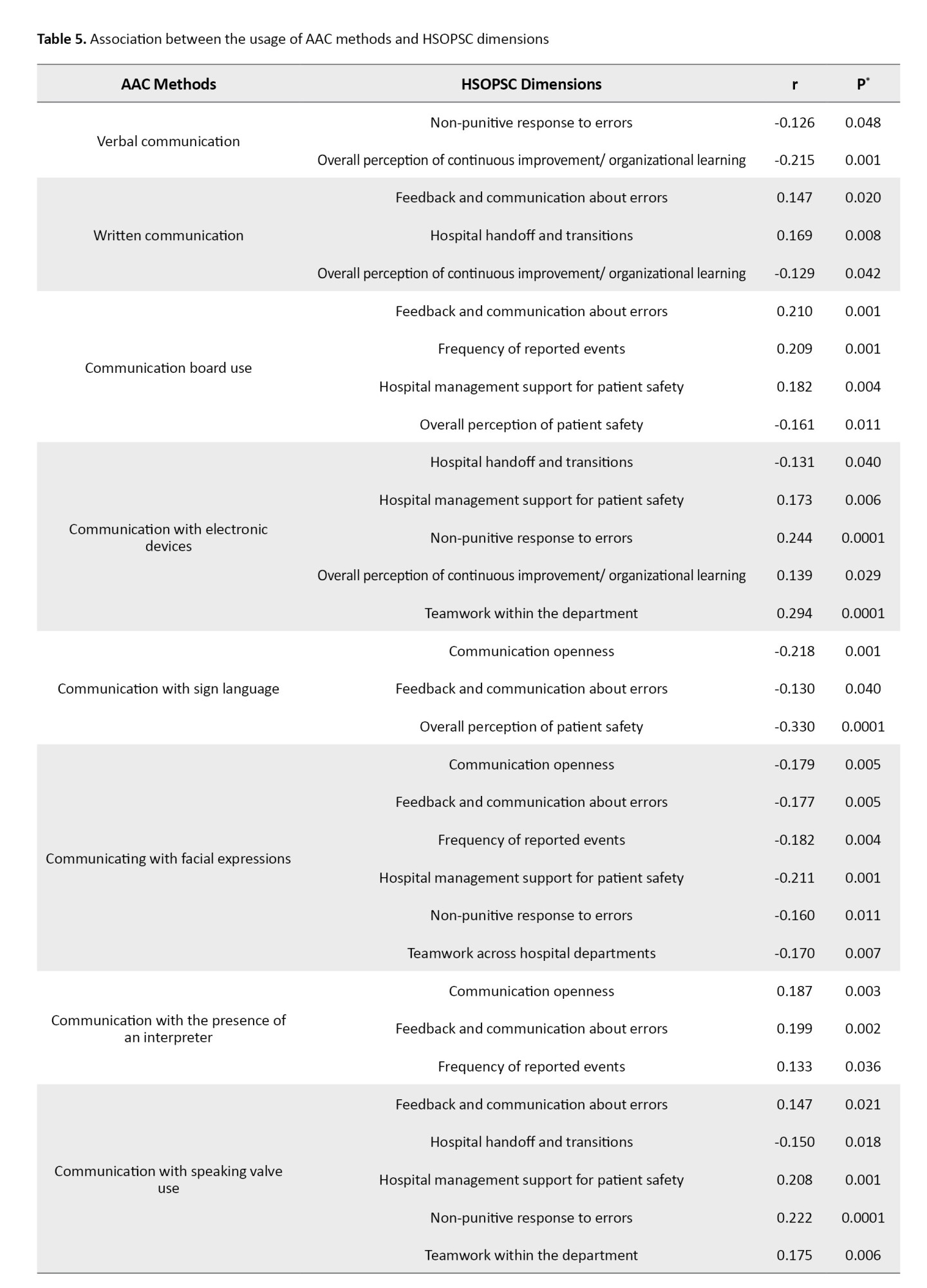
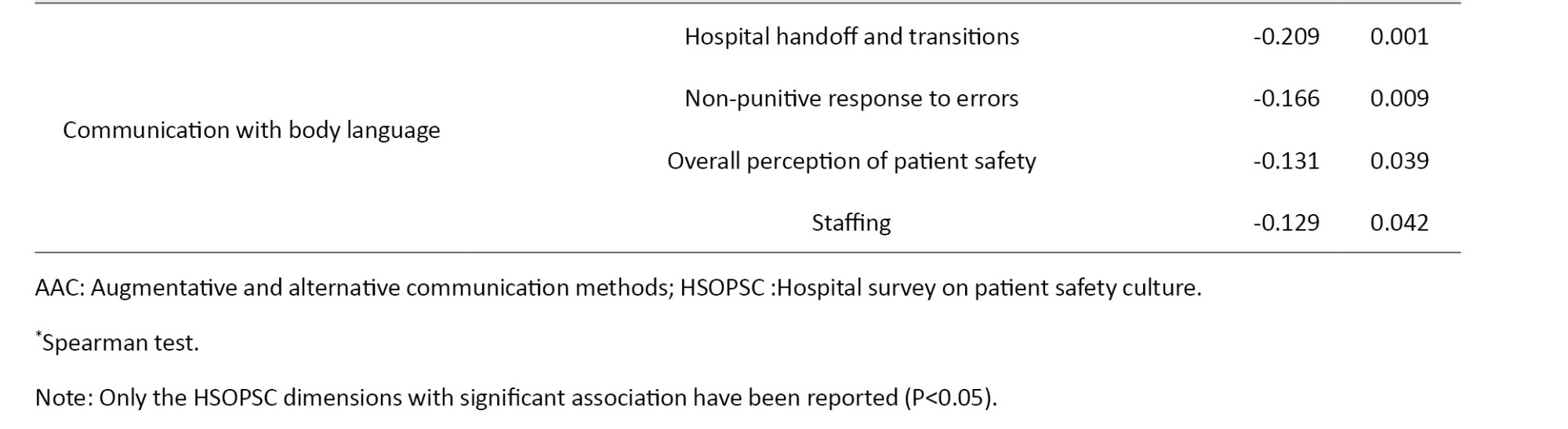
All significant relationships between the usage of AAC methods and HSOPSC are shown in Table 5. There was a significant relationship between communication with sign language and overall perception of patient safety (r= -0.330, P=0.001).
Discussion
The results of this study showed that verbal communication was the most common method of nurse-patient communication in the ICUs of hospitals in Ahvaz, and the use of electronic communication devices was the least common. The most common tool for communication was the nurse call bell, and the least common tool was the speech production tool.
A study in Iran on speech-language pathologists (SLP) showed that a few numbers of them were familiar with the concept of AAC. Most of them were familiar with low-tech AAC devices (e.g. paper and pen, communication board, sign language) and a few were familiar with high-tech AAC devices [21]. In another study, it was found that anesthesiologists had less knowledge about modified call buttons, communication boards, and alphabet boards than nurses [8]. Their study is similar to the present study in terms of examining the use of AAC methods. In their study, the level of patient satisfaction with the AAC methods was examined, while our study investigated the nurses’ usage of AAC methods.
Despite recent developments in different communication modes, most ICU nurses in our study tended to use traditional methods, such as verbal communication. Although ICU patients are limited to communicate verbally due to their lower level of consciousness, this method is still widely preferred by many patients due to its ease of use. By attending educational workshops, ICU nurses can learn about AAC methods and health managers can play an important role in this field by providing them with various communication tools [22].
Research has shown that in hospitals with a continuous positive work environment, nurses have lower burnout, lower desire to leave their positions, and lower job dissatisfaction. Better work environments also correlate with the overall quality of patient care [23]. Given the significant relationship between the dimensions of the work environment and the use of AAC methods in our study, attention to nurses’ environment should be recognized as a priority. Joolaee et al. reported a weak but statistically significant relationship between patients’ falls and the nurses’ working environment [24]. Although the purpose of our study and their study are different, both studies emphasize the safety of the nursing work environment.
Furthermore, the results of our study confirmed that patient safety culture correlated significantly with the use of AAC methods. Consistently, the result of another study showed that there was a significant relationship between the nurses’ communication skills and the patient safety in ICUs [25]. A study showed that the use of communication boards can reduce the anxiety of conscious patients under mechanical ventilation [1]. In a hospital with a favorable patient safety culture, nurses can express their opinions freely, and in cases where an accident is probable to occur due to system problems or human factors, the risks can be reported in time [25]. Research has proved that the problems caused by low patient safety culture among the medical staff caused hospital-acquired infections, medication errors, and patient falling from the bed [26] and nurse withdrawal from the healthcare system [27].
According to the results of the present study regarding the significant relationship between many variables of patient safety culture and the use of AAC methods by nurses, and concerning the role of patient safety culture in increasing safety and improving the quality of nursing care, it seems necessary to increase the focus on establishing correct communication to improve patient safety in the ICUs. However, these findings should be further studied. One of the most important limitations of this study was that nurses’ heavy workloads in ICUs and their psychological states, which could not be controlled, might have influenced their responses while completing the questionnaire.
Necessary training programs regarding AAC methods should be provided to the ICU nurses in Ahvaz city to foster principled and patient-centered manners in them. Moreover, it is recommended to develop applicable and updated solutions for improving the work environment and patient safety culture in hospitals of Ahvaz city. Further studies using larger sample sizes in other hospital departments are commended to gain a better understanding regarding the use of AAC methods by staff for communication with different patients.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Ahvaz jundishapur University of Medical Sciences, Ahvaz, Iran (Code: IR.AJUMS.REC.1400.277). Written informed consent was obtained from all samples prior to participation in the study.
Funding
This paper was extracted from the master’s thesis of Maedeh Misaghi, approved by Ahvaz jundishapur University of Medical Sciences, Ahvaz, Iran and funded by the Ahvaz jundishapur University of Medical Sciences, Ahvaz, Iran (Grant No.: U_00134).
Authors' contributions
Conceptualization and study design: Maedeh Misaghi, Neda Sayadi and Simin Jahani; Data collection: Maedeh Misaghi; Data analysis: Elham Maraghi; Data interpretation: Maedeh Misaghi, Neda Sayadi, Simin Jahani and Elham Maraghi; Writing the original draft: Somayeh Biparva Haghighi, Maedeh Misaghi and Neda Sayadi; Review & editing: Somayeh Biparva Haghighi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all nurses and hospitals for their cooperation in this research.
References
Effective communication enables healthcare personnel to establish rapport with their patients, obtain crucial health information and work effectively with all healthcare team members. Nurses are always expected to maintain good communication and approach every patient with the intention to understand their concerns [1]. Good communication between nurses and patients is more important in intensive care units (ICUs) as it helps patients perceive their illnesses more positively. According to the statistics of the Iranian Society of Anesthesiology and Critical Care, 1.5-2 million people annually refer to hospitals due to road accidents, strokes and other reasons, of whom 30% need to be hospitalized in the ICU [2]. When normal ways of speaking and writing are restricted in patients, augmentative and alternative communication (AAC) is employed [1]. It refers to the use of strategies or auxiliary tools to support, enhance or replace normal spoken communication [3].The scope of AAC systems varies from simple level that does not require electronic devices (e.g. pen and paper, symbols, communication boards, or books) to high technology levels that include speech generating devices or electronic equipments [4].
Studies have confirmed that nurse-patient communication affects the quality of patient care and safety [5]. Patient safety refers to an environment free of harm in which patients and caregivers apply safety standards, thereby reducing the risks of an unnecessary action [6]. Evaluation of safety culture in hospitals is generally encouraged by policymakers and healthcare managers [7]. Nurses are the key members of a healthcare team, and their role in care-giving and protection and promotion of the healthcare system has been globally established [8]. Among the key factors that affect patient safety is the nursing work environment. According to the American Nurses Association, the nursing work environment includes all effective factors and indicators of nursing performance, including skilled communication, true collaboration, and effective decision-making [9]. Relationship with colleagues, nurse-to-patient staffing ratio, and management and leadership methods, along with the tools and facilities available in the department, are factors related to nursing work environment that can significantly affect the provision of safe patient care [10]. The results of the studies have shown that the cause of almost all accidents in the work environment is the lack of proper communication between caregivers and patients; 75% of medical errors and 65% of accidents during work shifts are due to improper communication [11-15].
Overall, the literature review revealed that safety culture is affected by factors such as communication and work environment; however, there are few studies on the relationship between patient safety and AAC. In this regard, this study aims to determine the usage rate of AAC by ICU nurses in Ahvaz, southwest of Iran, and assess its relationship with nursing work environment and patient safety culture.
Materials and Methods
This is a correlational study with a cross-sectional design. The study population comprised all permanent and contractual nurses working in the ICUs of selected hospitals in Ahvaz, southwest of Iran. They all were included in study using a census method. The inclusion criteria were at least 6 months of work experience in the ICU, at least a bachelor’s degree, willingness to participate in the study, and complete responses to the questionnaires. Of the 378 nurses, 249 were eligible to participate in this research. Data were collected from May to June 2022 using three questionnaires, including the hospital survey on patient safety culture (HSOPSC), the nursing work index (NWI), and the AAC scale.
The HSOPSC is a field questionnaire designed by the agency for healthcare research and quality [16]. It has 42 items and 12 dimensions of patient safety culture. Each item is rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The dimensions include overall perception of continuous improvement/organizational learning, frequency of reported events, overall perception of patient safety, employees/manager expectations and actions promoting patient safety, communication openness, teamwork within the department, feedback and communication about errors, non-punitive response to errors, staffing, teamwork across hospital departments, hospital management support for patient safety, and hospital handoff and transitions. Those with a positive response >75% are considered as areas of strength, and those with a positive response <50% are considered as areas of weakness that require intervention. Those with a positive response between 50-70% are the areas with potential for improvement. In this study, the Persian version of the HSOPSC was used [17].
The NWI is a standard tool designed by Lake et al. It has 34 items rated on a 4-point Likert scale as: 1) Completely disagree, 2) Somewhat disagree, 3) Somewhat agree and 4) Completely agree. This questionnaire has five domains: Nurse participation in hospital affairs (11 items), nursing foundations for quality of care (9 items), nurse/manager ability (7 items), adequacy of resources and staffing (4 items), and collegial nurse-physician relations (3 items). A score above 2.5 in each domain indicates the favorable level of work environment, and a score <2.5 indicates a poor level of work environment [18]. In this study, the Persian version of NWI was used [19].
The AAC scale was used to rate nurses’ use of AAC methods. It was developed by Jansson et al. [8] and has 16 items, measuring demographic information (items 1-10), care needs of special people, such as disabled patients (items 11 and 12 each with four options), communication methods and obtaining information from the patient (items 13 and 14 rated on a Likert scale from 4 [always] to 0 [never]) and the types of AAC methods (items 15 and 16 answered by yes or no). The total score is not calculated. The forward-backward translation method was used to translate the scale from English to Persian, performed by two experts with PhD in English Language Teaching. To confirm the validity of the tool, the content validity was checked by 10 experts with experience working in ICU, including 6 nurses and 4 anesthesiologists. Next, the content validity index (CVI) was calculated for each item and the subscales. The acceptable CVI score for each item is 0.8 or higher, and the acceptable CVI score for each subscale is 0.9 or higher [20]. To examine the reliability of the Persian AAC scale, Cronbach’s α coefficient was calculated, and the acceptable value of 0.74 was obtained.
Before data collection, the study objectives were explained to the participants and their informed consent was obtained. After collection, continuous data were reported as Mean±SD and categorical data as number (percentage). The normality of continuous data was assessed using the Shapiro-Wilks test. The association between the frequency of using each AAC method and the scores of HSOPSC and NWI was assessed using Spearman’s correlation test. P<0.05 were considered statistically significant. All analyses were done in SPSS software, version 22 (IBM Corp., Armonk, NY).
Results
Th mean age of participants was 30.96±6.63 years, and most of them were female (87.1%). Table 1 presents other characteristics of participants.
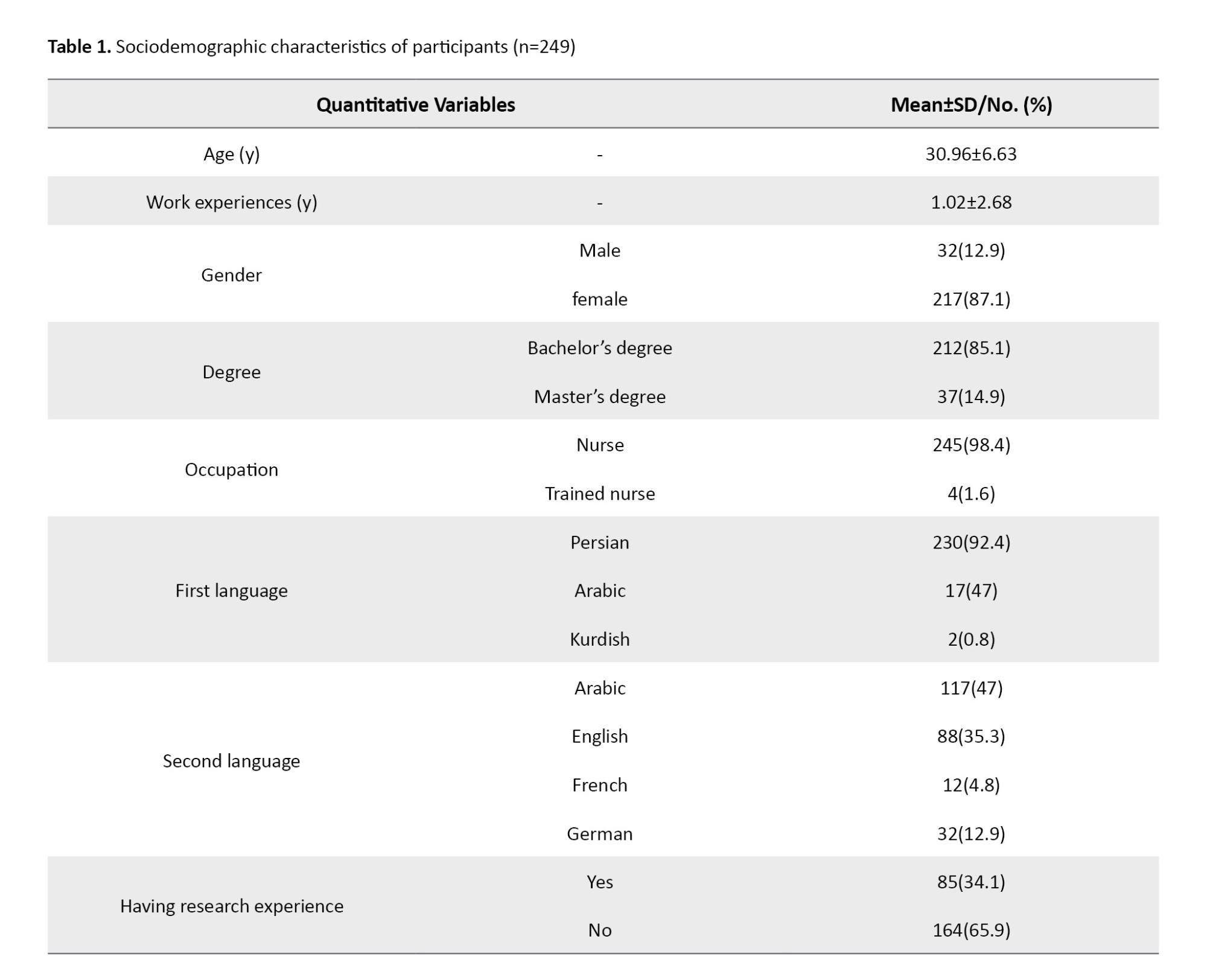
Table 2 presents the frequency of using AAC methods by nurses. The most common method of communication with patients was verbal method as 61(24.5%) nurses had always used verbal communication method.
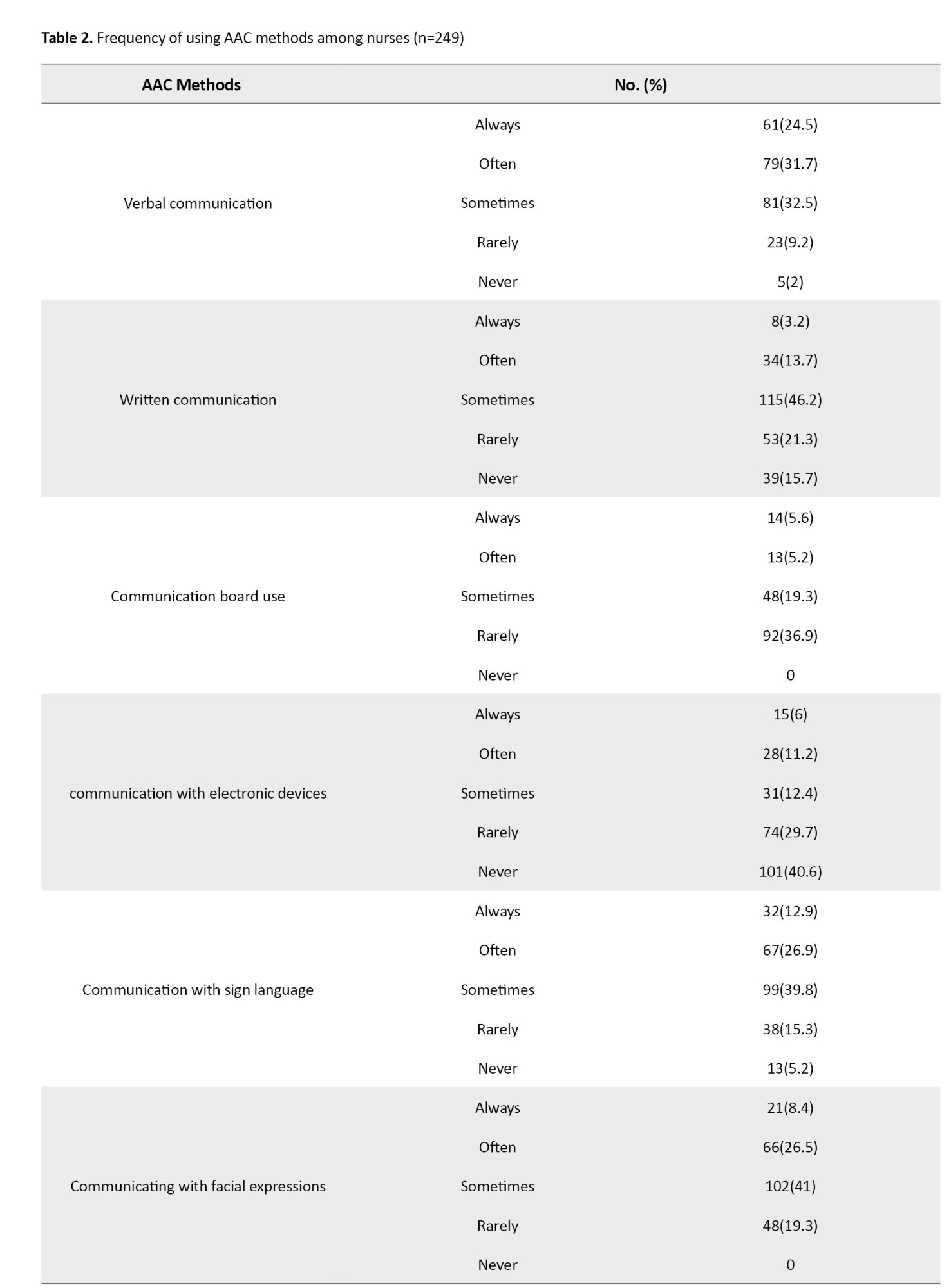
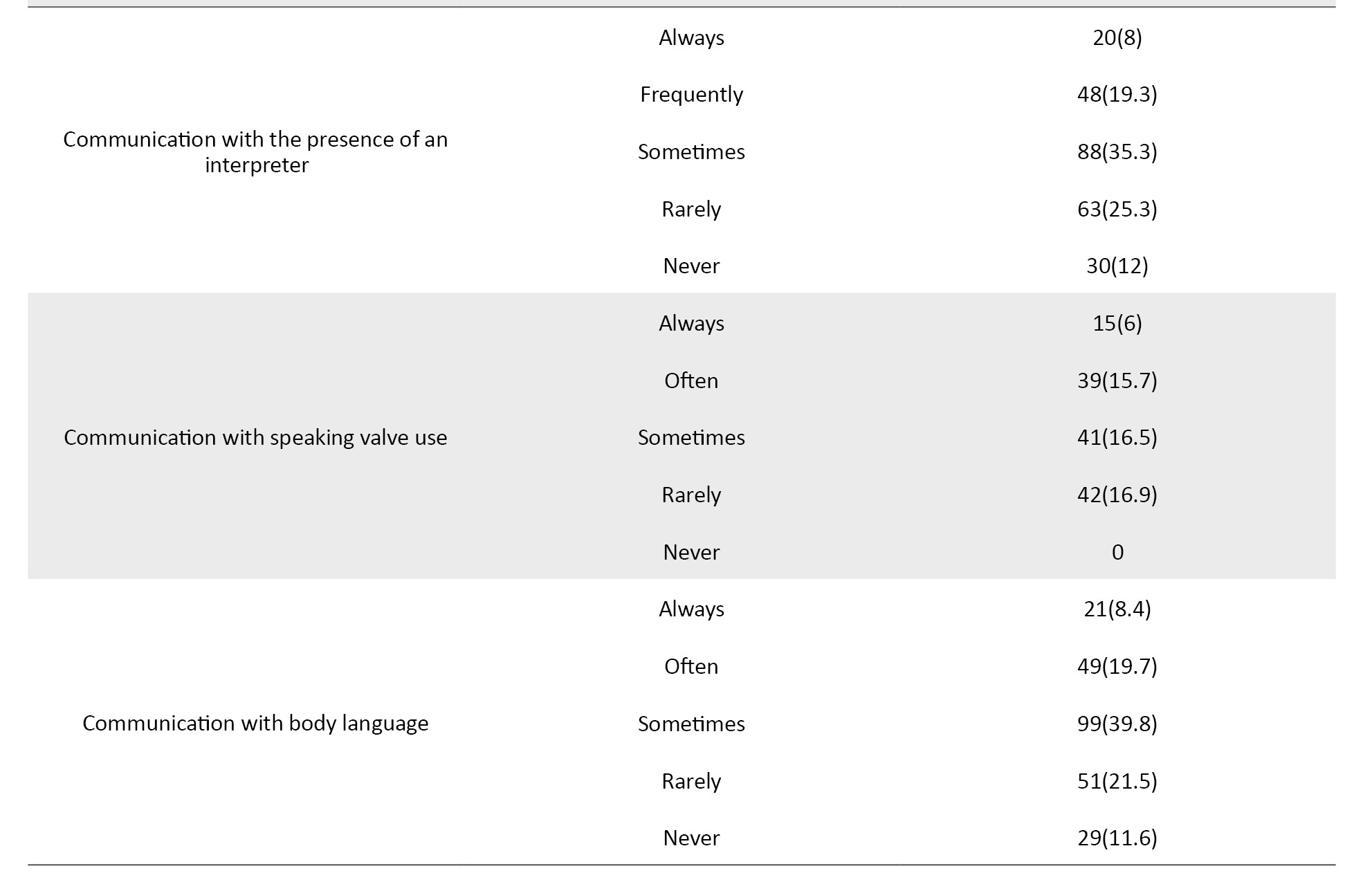
The least commonly used AAC method (n=15, 6%) was communication with electronic devices. Concerning the tools for communication with ICU patients, the call bell was the most common tool (n=93, 37.3%), while the least used communication tool was the speech production tool (n=13, 2.5%). The mean scores of NWI and HSOPSC domains are shown in Table 3.
To assess the relationship between the usage of AAC methods and NWI dimensions, Spearman’s test was used. The results are presented in Table 4. There was a significant relationship between communication board use and nurse participation in hospital affairs (r=0.283, P=0.001), between communication with electronic devices and nurse participation in hospital affairs (r=0.284, P=0.001), and between speaking valve use and adequacy of resources and staffing (r=0.380, P=0.001).
All significant relationships between the usage of AAC methods and HSOPSC are shown in Table 5. There was a significant relationship between communication with sign language and overall perception of patient safety (r= -0.330, P=0.001).
Discussion
The results of this study showed that verbal communication was the most common method of nurse-patient communication in the ICUs of hospitals in Ahvaz, and the use of electronic communication devices was the least common. The most common tool for communication was the nurse call bell, and the least common tool was the speech production tool.
A study in Iran on speech-language pathologists (SLP) showed that a few numbers of them were familiar with the concept of AAC. Most of them were familiar with low-tech AAC devices (e.g. paper and pen, communication board, sign language) and a few were familiar with high-tech AAC devices [21]. In another study, it was found that anesthesiologists had less knowledge about modified call buttons, communication boards, and alphabet boards than nurses [8]. Their study is similar to the present study in terms of examining the use of AAC methods. In their study, the level of patient satisfaction with the AAC methods was examined, while our study investigated the nurses’ usage of AAC methods.
Despite recent developments in different communication modes, most ICU nurses in our study tended to use traditional methods, such as verbal communication. Although ICU patients are limited to communicate verbally due to their lower level of consciousness, this method is still widely preferred by many patients due to its ease of use. By attending educational workshops, ICU nurses can learn about AAC methods and health managers can play an important role in this field by providing them with various communication tools [22].
Research has shown that in hospitals with a continuous positive work environment, nurses have lower burnout, lower desire to leave their positions, and lower job dissatisfaction. Better work environments also correlate with the overall quality of patient care [23]. Given the significant relationship between the dimensions of the work environment and the use of AAC methods in our study, attention to nurses’ environment should be recognized as a priority. Joolaee et al. reported a weak but statistically significant relationship between patients’ falls and the nurses’ working environment [24]. Although the purpose of our study and their study are different, both studies emphasize the safety of the nursing work environment.
Furthermore, the results of our study confirmed that patient safety culture correlated significantly with the use of AAC methods. Consistently, the result of another study showed that there was a significant relationship between the nurses’ communication skills and the patient safety in ICUs [25]. A study showed that the use of communication boards can reduce the anxiety of conscious patients under mechanical ventilation [1]. In a hospital with a favorable patient safety culture, nurses can express their opinions freely, and in cases where an accident is probable to occur due to system problems or human factors, the risks can be reported in time [25]. Research has proved that the problems caused by low patient safety culture among the medical staff caused hospital-acquired infections, medication errors, and patient falling from the bed [26] and nurse withdrawal from the healthcare system [27].
According to the results of the present study regarding the significant relationship between many variables of patient safety culture and the use of AAC methods by nurses, and concerning the role of patient safety culture in increasing safety and improving the quality of nursing care, it seems necessary to increase the focus on establishing correct communication to improve patient safety in the ICUs. However, these findings should be further studied. One of the most important limitations of this study was that nurses’ heavy workloads in ICUs and their psychological states, which could not be controlled, might have influenced their responses while completing the questionnaire.
Necessary training programs regarding AAC methods should be provided to the ICU nurses in Ahvaz city to foster principled and patient-centered manners in them. Moreover, it is recommended to develop applicable and updated solutions for improving the work environment and patient safety culture in hospitals of Ahvaz city. Further studies using larger sample sizes in other hospital departments are commended to gain a better understanding regarding the use of AAC methods by staff for communication with different patients.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Ahvaz jundishapur University of Medical Sciences, Ahvaz, Iran (Code: IR.AJUMS.REC.1400.277). Written informed consent was obtained from all samples prior to participation in the study.
Funding
This paper was extracted from the master’s thesis of Maedeh Misaghi, approved by Ahvaz jundishapur University of Medical Sciences, Ahvaz, Iran and funded by the Ahvaz jundishapur University of Medical Sciences, Ahvaz, Iran (Grant No.: U_00134).
Authors' contributions
Conceptualization and study design: Maedeh Misaghi, Neda Sayadi and Simin Jahani; Data collection: Maedeh Misaghi; Data analysis: Elham Maraghi; Data interpretation: Maedeh Misaghi, Neda Sayadi, Simin Jahani and Elham Maraghi; Writing the original draft: Somayeh Biparva Haghighi, Maedeh Misaghi and Neda Sayadi; Review & editing: Somayeh Biparva Haghighi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all nurses and hospitals for their cooperation in this research.
References
- Holm A, Viftrup A, Karlsson V, Nikolajsen L, Dreyer P. Nurses' communication with mechanically ventilated patients in the intensive care unit: Umbrella review. J Adv Nurs. 2020; 76(11):2909-20. [DOI:10.1111/jan.14524] [PMID]
- Hosseini SR, Valizad-Hasanloei MA, Feizi A. The effect of using communication boards on ease of communication and anxiety in mechanically ventilated conscious patients admitted to intensive care units. Iran J Nurs Midwifery Res. 2018; 23(5):358-62. [DOI:10.4103/ijnmr.IJNMR_68_17] [PMID]
- Patak L, Wilson-Stronks A, Costello J, Kleinpell RM, Henneman EA, Person C, et al. Improving patient-provider communication: A call to action. J Nurs Adm. 2009; 39(9):372-6. [DOI:10.1097/NNA.0b013e3181b414ca] [PMID]
- Khatri Chhetri I, Thulung B. Perception of nurses on needs of family members of patient admitted to critical care units of teaching hospital, Chitwan Nepal: A cross-sectional institutional based study. Nurs Res Pract. 2018; 2018:1369164.[DOI:10.1155/2018/1369164] [PMID]
- Mello JF, Barbosa SFF. Patient safety culture in an intensive care unit: The perspective of the nursing team. Rev Eletr Enf. 2017; 19:a07. [DOI:10.5216/ree.v19.38760]
- Mohammadi M, Naseri Jahromi R, Rasekh Jahromi A, Mokhtari Z, AllameZade M, Tanasan M, et al. [The effects of comfort education on nurses' attitude towards communication skills (Persian)]. Res Med Educ. 2019; 10(4):23-30. [DOI:10.29252/rme.10.4.23]
- Ashori M. [Effect of cognitive rehabilitation program based on memory on executive functions and cognitive emotion regulation in children with hearing impairment (Persian)]. Psychol Except Individ. 2019; 9(34):197-217. [doi:10.22054/jpe.2019.42397.1994]
- Jansson S, Martin TRS, Johnson E, Nilsson S. Healthcare professionals' use of augmentative and alternative communication in an intensive care unit: A survey study. Intensive Crit Care Nurs. 2019; 54:64-70. [DOI:10.1016/j.iccn.2019.04.002] [PMID]
- Janikova E, Zelenikova R, Jarošova D, Plevova I, Mynařikova E. Work environment assessment Instruments used in nursing. Kontakt. 2021; 23(4):263-73. [DOI:10.32725/kont.2021.041]
- Blendon RJ, DesRoches CM, Brodie M, Benson JM, Rosen AB, Schneider E, et al. Views of practicing physicians and the public on medical errors. N Engl J Med. 2002; 347(24):1933-40. [DOI:10.1056/NEJMsa022151] [PMID]
- Wieke Noviyanti L, Ahsan A, Sudartya TS. Exploring the relationship between nurses' communication satisfaction and patient safety culture. J Public Health Res. 2021; 10(2):2225. [DOI:10.4081/jphr.2021.2225]
- Mahvar T, Mohammadi N, Seyedfatemi N, Vedadhir A. Interpersonal communication among critical care nurses: An ethnographic study. J Caring Sci. 2020; 9(1):57-64. [DOI:10.34172/jcs.2020.009] [PMID]
- Karlsen MW, Holm A, Kvande ME, Dreyer P, Tate JA, Heyn LG, et al. Communication with mechanically ventilated patients in intensive care units: A concept analysis. J Adv Nurs. 2023; 79(2):563-80. [DOI:10.1111/jan.15501] [PMID]
- Pooyanfard F, Razban F, Asadi N, Haji-Maghsoudi S. Correlation between nurses' attitude and practice toward communication with patients of decreased level of consciousness and its relationship with ethical care in ICU: A cross-sectional study. Health Sci Rep. 2023; 6(8):e1484. [DOI:10.1002/hsr2.1484] [PMID]
- Schwartz JM, Nelson KL, Saliski M, Hunt EA, Pronovost PJ. The daily goals communication sheet: A simple and novel tool for improved communication and care. Jt Comm J Qual Patient Saf. 2008; 34(10):608-13. [DOI:10.1016/S1553-7250(08)34076-8] [PMID]
- Agency for Healthcare Research and Quality. SOPS hospital survey [Internet]. 2017 [Updated July 2024]. Available from: [Link]
- Moghri J, Ghanbarnezhad A, Moghri M, Rahimi Forooshani A, Akbari Sari A, Arab M. [Validation of Farsi version of hospital survey on patient Safety culture questionnaire, using confirmatory factor analysis method (Persian)]. j Hosp. 2012; 11(2):19-30. [Link]
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002; 25(3):176-88. [DOI:10.1002/nur.10032] [PMID]
- Elmi S, Hassankhani H, Abdollahzadeh F, Jafar Abadi MA, Scott J, Nahamin M. Validity and reliability of the Persian practice environment scale of nursing work index. Iran J Nurs Midwifery Res. 2017; 22(2):106-11. [DOI:10.4103/1735-9066.205953] [PMID]
- Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007; 30(4):459-67. [DOI:10.1002/nur.20199]
- Zarifian T, Malekian M, Azimi T. Iranian speech-language pathologists’ awareness of alternative and augmentative communication methods. Iran Rehabil J. 2021; 19(1):41-50. [DOI:10.32598/irj.19.1.991.1]
- Shaker MR, Momennasab M, Dehghanrad F, Dokoohaki R, Dakhesh R, Jaberi A. [The effect of using augmentative and alternative communication strategies on the quality of nurses’ communication with patients with endotracheal intubation in the cardiac surgery intensive care unit (Persian)]. J Hayat. 2022; 28(1):102-16. [Link]
- Gómez-García T, Ruzafa-Martínez M, Fuentelsaz-Gallego C, Madrid JA, Rol MA, Martínez-Madrid MJ, et al. Nurses' sleep quality, work environment and quality of care in the Spanish National Health System: observational study among different shifts. BMJ Open. 2016; 6(8):e012073. [DOI:10.1136/bmjopen-2016-012073] [PMID]
- Joolaee S, Shali M, Harati Khalilabad T, Haghani H, Vaezi A, Sepehrinia M. [Association of the incidence of patient falls and work environment of nurses (Persian)]. Iran J Nurs. 2018; 31(114):38-48. [DOI:10.29252/ijn.31.114.38]
- Hemmati-Maslakpak M, Sheikhbaglu M, Baghaie R. [Relationship between the communication skill of nurse-patient with patient safety in the critical care units (Persian)]. J Multidiscip Care. 2014; 3(2):77-84. [Link]
- Khan RM, Aljuaid M, Aqeel H, Aboudeif MM, Elatwey S, Shehab R, et al. Introducing the Comprehensive Unit based Safety Program for mechanically ventilated patients in Saudi Arabian Intensive Care Units. Ann Thorac Med. 2017; 12(2):132. [DOI:10.4103/atm.ATM_49_17] [PMID]
- Farzi S, Irajpour A, Saghaei M, Ravaghi H. Causes of medication errors in intensive care units from the perspective of healthcare professionals. J Res Pharm Pract. 2017; 6(3):158-65. [DOI:10.4103/jrpp.JRPP_17_47] [PMID]
Article Type : Research |
Subject:
Special
Received: 2023/06/13 | Accepted: 2024/02/10 | Published: 2025/04/1
Received: 2023/06/13 | Accepted: 2024/02/10 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |