Sat, Jan 31, 2026
Volume 35, Issue 4 (9-2025)
JHNM 2025, 35(4): 315-322 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahmoodi Z, Hashemnejad M, Yazdkhasti M, Akbari Kamrani M, Mehdizadeh Tourzani Z, Arabi M, et al . The Effect of a Mobile-based Safe Motherhood Education Program on Postpartum Care Knowledge of Marginalized Women. JHNM 2025; 35 (4) :315-322
URL: http://hnmj.gums.ac.ir/article-1-2145-en.html
URL: http://hnmj.gums.ac.ir/article-1-2145-en.html
Zohreh Mahmoodi1 

 , Maryam Hashemnejad2
, Maryam Hashemnejad2 

 , Mansoureh Yazdkhasti1
, Mansoureh Yazdkhasti1 

 , Mahnaz Akbari Kamrani1
, Mahnaz Akbari Kamrani1 

 , Zahra Mehdizadeh Tourzani1
, Zahra Mehdizadeh Tourzani1 

 , Mohsen Arabi3
, Mohsen Arabi3 

 , Kourosh Kabir4
, Kourosh Kabir4 
 , Farima Mohamadi5
, Farima Mohamadi5 

 , Leila Zivdarchegini6
, Leila Zivdarchegini6 

 , Sara Esmaelzadeh Saeieh *7
, Sara Esmaelzadeh Saeieh *7 




 , Maryam Hashemnejad2
, Maryam Hashemnejad2 

 , Mansoureh Yazdkhasti1
, Mansoureh Yazdkhasti1 

 , Mahnaz Akbari Kamrani1
, Mahnaz Akbari Kamrani1 

 , Zahra Mehdizadeh Tourzani1
, Zahra Mehdizadeh Tourzani1 

 , Mohsen Arabi3
, Mohsen Arabi3 

 , Kourosh Kabir4
, Kourosh Kabir4 
 , Farima Mohamadi5
, Farima Mohamadi5 

 , Leila Zivdarchegini6
, Leila Zivdarchegini6 

 , Sara Esmaelzadeh Saeieh *7
, Sara Esmaelzadeh Saeieh *7 


1- Professor, Department of Reproductive Health, Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran.
2- Associated Professor, Department of Obstetrics & Gynaecology, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
3- Associated Professor, Department of Physiology, Pharmacology and Medical Physics, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
4- Associated Professor, Department of Community Medicine and Epidemiology, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
5- Assistant Professor, Social Determinants of Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
6- Ms Student, Department of Midwifery, School of Nursing and Midwifery, Semnan University of Medical sciences, Semnan, Iran.
7- Professor, Department of Reproductive Health, Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran. ,esmaelzadeh1360@gmail.com
2- Associated Professor, Department of Obstetrics & Gynaecology, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
3- Associated Professor, Department of Physiology, Pharmacology and Medical Physics, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
4- Associated Professor, Department of Community Medicine and Epidemiology, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
5- Assistant Professor, Social Determinants of Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
6- Ms Student, Department of Midwifery, School of Nursing and Midwifery, Semnan University of Medical sciences, Semnan, Iran.
7- Professor, Department of Reproductive Health, Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran. ,
Full-Text [PDF 568 kb]
(170 Downloads)
| Abstract (HTML) (369 Views)
Full-Text: (138 Views)
Introduction
The postpartum period is one of the most critical and sensitive periods in a woman’s life. It starts one hour after delivery of the placenta and occurs up to six weeks. During this period, women experience numerous physical, social, and emotional changes that can have adverse maternal and neonatal outcomes if not carefully evaluated and monitored [1]. According to the reports, 292,982 women die annually due to complications related to pregnancy, childbirth, and the postpartum period, and many suffer from long-term disabilities [2]. The risk of maternal mortality is 33 times higher in developing countries than in developed countries [3]. Providing continuous care before and during pregnancy and after childbirth is critical for reducing maternal and neonatal mortality rates worldwide [2].
Several factors contribute to postpartum women’s higher vulnerability and lack of adequate postpartum care [4]. One of these factors is the settlement on the outskirts of cities. Marginalization is a social problem that has drawn the attention of urban sociologists and other experts in urbanization [5]. Marginalized women have lower health indicators than other women [6]. One of the main reasons for this inequality is their lack of access to reproductive health facilities [7]. Studies have also shown that the lack of postpartum care is strongly associated with poor socioeconomic status, large household size, living in non-nuclear families, ethnicity, long distance to healthcare centers, poor physical environment, long waiting times, and insufficient knowledge [8, 9]. Therefore, it is essential to empower these vulnerable women through counseling and training on proper health behaviors and self-care [10]. Currently, women receive such training briefly in verbal form or using educational pamphlets in gynecology clinics, which is usually not adequate or effective due to the existing time constraints and high referral rates of these clinics. Meanwhile, the information provided through mobile applications is more convenient, effective, and accessible for a longer time [11]. In our previous study, a safe motherhood educational application for Iranian postpartum women living in marginalized areas was designed based on the qualitative results, participants’ viewpoints, and the feasibility of service provision, which can be installed on Android phones [8]. In this study, we aim to assess the impact of this mobile-based safe motherhood learning program on the postpartum care knowledge of marginalized women.
Materials and Methods
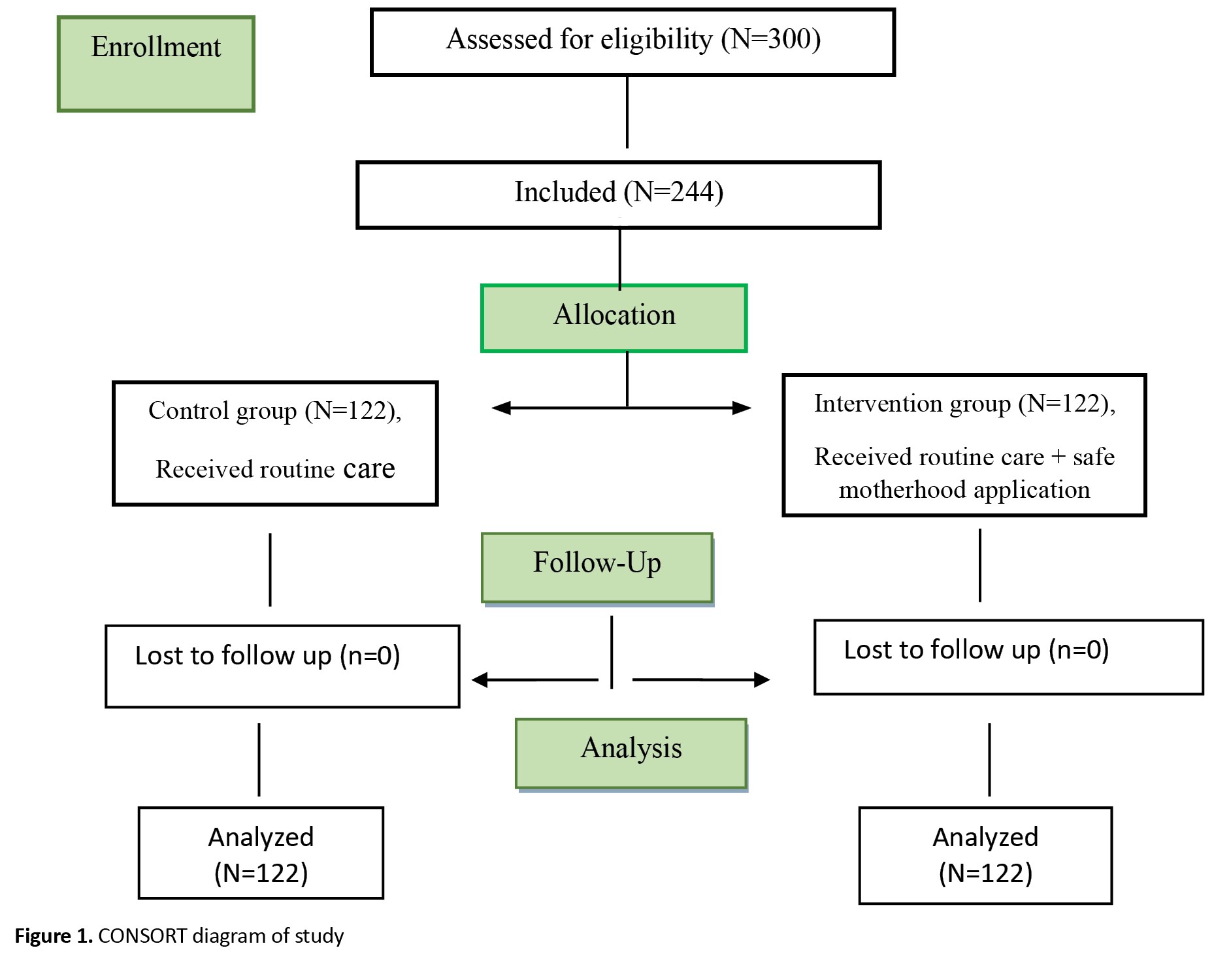
This is a quasi-experimental study conducted on 244 postpartum women referring to comprehensive health centers in Karaj (Mehdi Abad, Kalak No, and Ahmad Abad districts), Alborz Province, Iran, in 2021-2022. The sample size was calculated to be 110 per group (220 in total) using G*power software, version 3.1. Based on the results of Mirmolaei et al. [12], considering an effect size of 0.5, type I error (α) of 0.05, type II error (β) of 0.05, and 95% test power. Taking into account a 10% sample dropout, the sample size increased to 122 per group (244 in total). Participants were selected using a convenience sampling method and randomly assigned to two groups of intervention and control using a random number table. Figure 1 shows the flowchart of sampling and randomization processes. Inclusion criteria for mothers were Iranian nationality, referring to the selected health centers on postpartum days of 3-5, having an Android smartphone, no physical or mental illnesses affecting the interview (based on self-reports or medical records), being fluent in Persian, at the least a reading and writing literacy, and no use of narcotic drugs and psychotropic substances. Inclusion criteria for the newborns were being the first or second full-term (37 weeks of gestation) child of the family, having a healthy appearance, and having no anomalies. The exclusion criterion was immigration during the study.
Data were collected using a sociodemographic checklist, a postpartum care knowledge scale, a postpartum care performance checklist, and a socioeconomic status form. The sociodemographic checklist surveyed age, pre-pregnancy weight, height, and pregnancy details such as gestational age, parity, and weight before pregnancy. The postpartum care knowledge scale consisted of 42 items and three domains, including mothers’ self-care behavior (28 items), infants’ nutritional or breastfeeding status (5 items), and mothers’ infant care behavior (9 items). The items are answered as correct (1 point) or incorrect (0 points). Therefore, the total score ranges from 0 to 42, with higher scores indicating proper postpartum care knowledge. The validity and reliability of this questionnaire were investigated in Iran by Mirmolaei et al. [12]. We examined the reliability of this questionnaire on 45 participants, and a Cronbach’s α value of 0.85 was obtained. The socioeconomic status form, which was developed by Ghodratnama et al. [13], consists of four components (income, economic class, housing status, and education)and used by Eslami et al. [14]. The scoring is based on a Likert scale from 1 (very low) to 5 (very high). The total score ranges from 4 to 20.
After obtaining the necessary permits and ethical approval from the Research Ethics Committee of the National Strategic Research Center for Medical Education, the researcher visited the comprehensive health centers in the marginalized districts of Karaj and selected eligible women. After explaining the study objectives to the participants, their written consent to participate in the study was obtained. Then, the questionnaires were completed by both groups in three phases: Before the intervention (postpartum days 3-5), second week of postpartum (postpartum days 14-15), and sixth week of postpartum (postpartum days 42-45), based on the guidelines for postpartum care developed by the Iranian Ministry of Health and Medical Education [15].
For the intervention group, the safe motherhood application was installed on participants’ Android smartphones by the researcher, and they were trained on how to use it. As mentioned before, it was designed based on the results of our previous study [8]. It consisted of pre-pregnancy training, pregnancy/childbirth training, postpartum training, information about adverse pregnancy outcomes, screening, how to provide care to healthy infants, how to provide care to premature neonates, information about the stages of fetal development, interpretation of tests, and frequently asked questions. The participants in the intervention group received routine care in addition to the educational application. The control group received only routine care. After the interventions, the control group also received access to the educational application to comply with ethical considerations.
Data were analyzed in SPSS software, version 16 using descriptive statistics and analytical tests, including independent t-test, independent t-test, and repeated measures ANOVA. Before testing, the ANOVA assumptions were examined using Box’s M test, Mauchly’s test of sphericity, and Levene’s test. Since Box’s M test results did not show significant results for any variables (P>0.05), the assumption of the homogeneity of the variance-covariance matrices was established. Also, the non-significant results of Levene’s test confirmed the equality of variances between the groups (P>0.05). Mauchly’s sphericity test results were not significant for the study variables (P>0.05), indicating that the equality of variances within the subjects (i.e. the assumption of sphericity) was also met. Therefore, the Greenhouse-Geisser correction was used.
Results
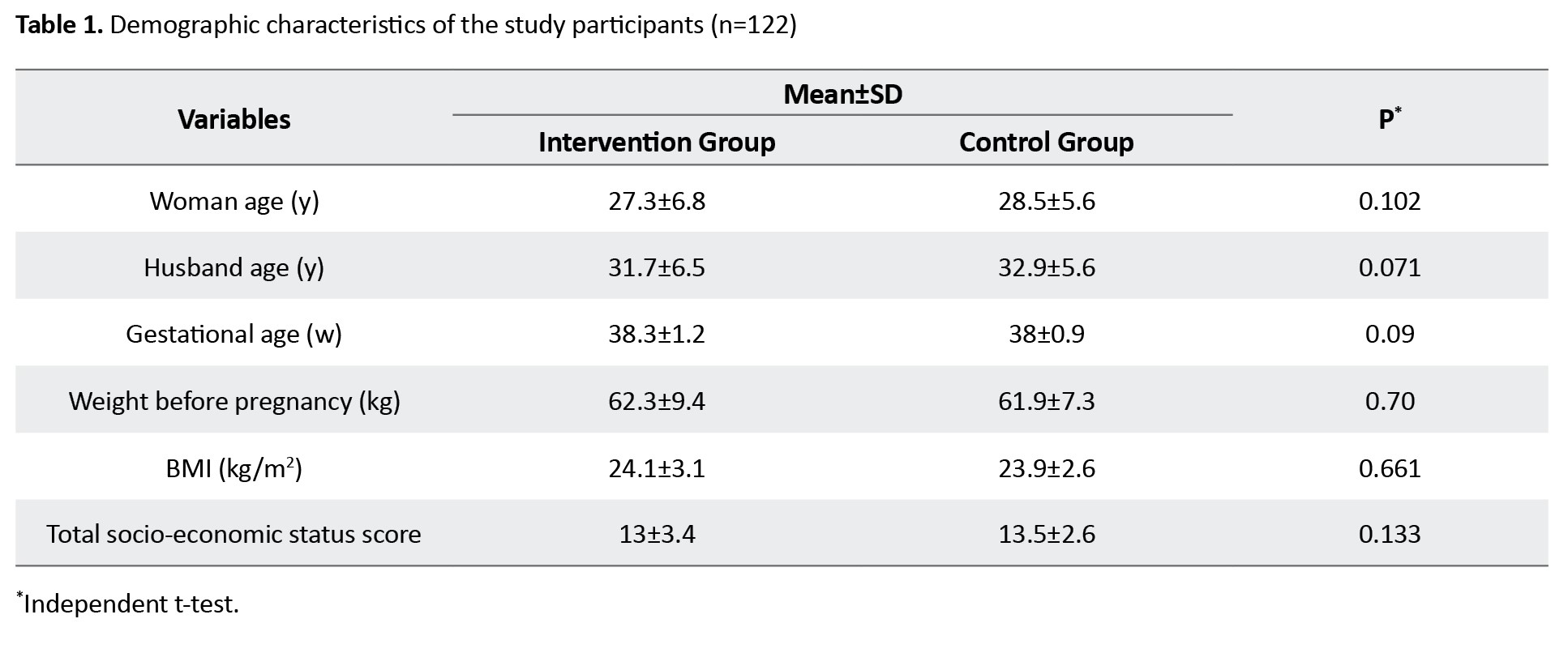
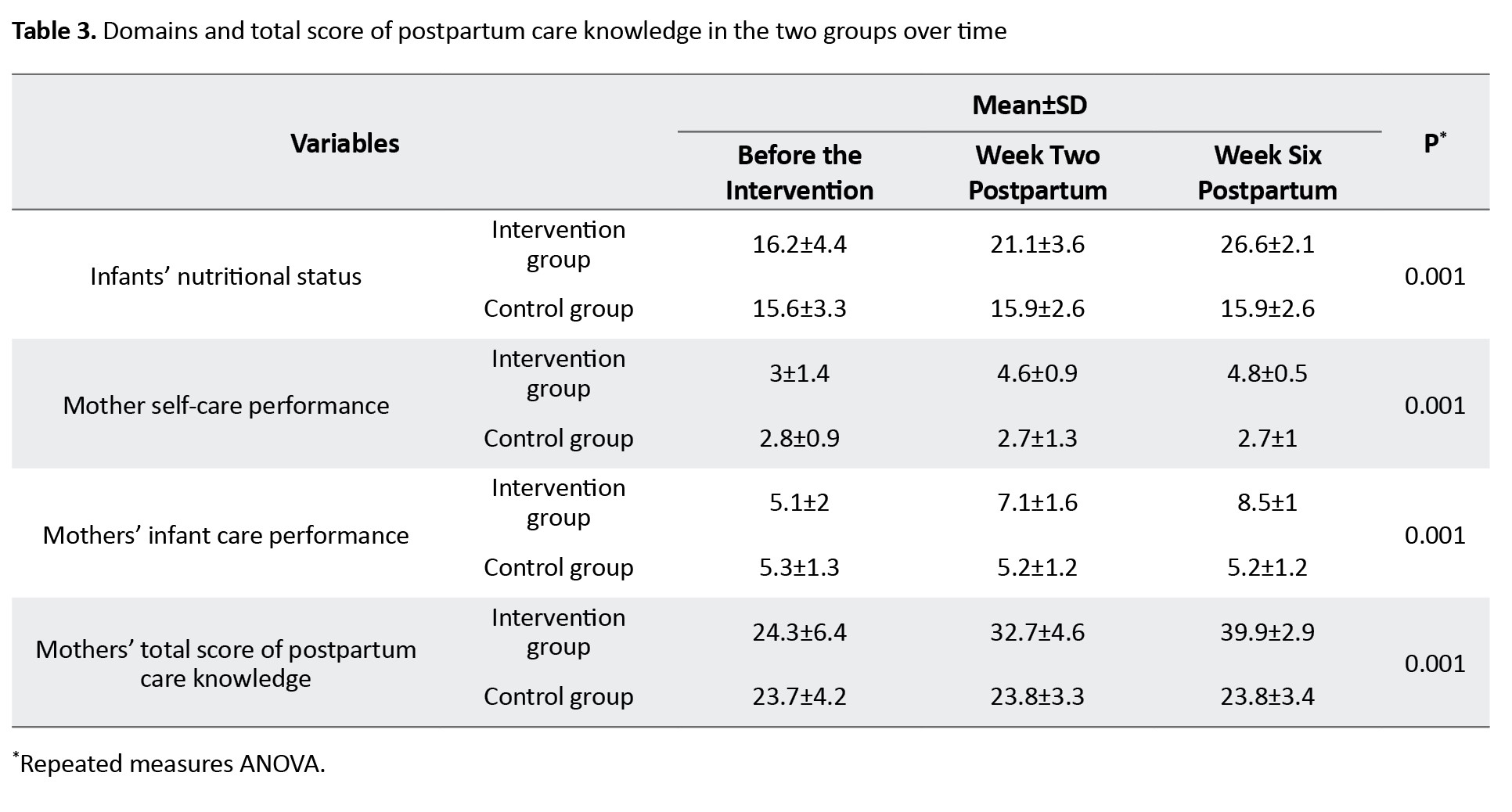
The mean age of the participants was 27.3±6.8 years in the intervention group and 28.5±5.6 years in the control group. Their other characteristics are presented in Table 1.
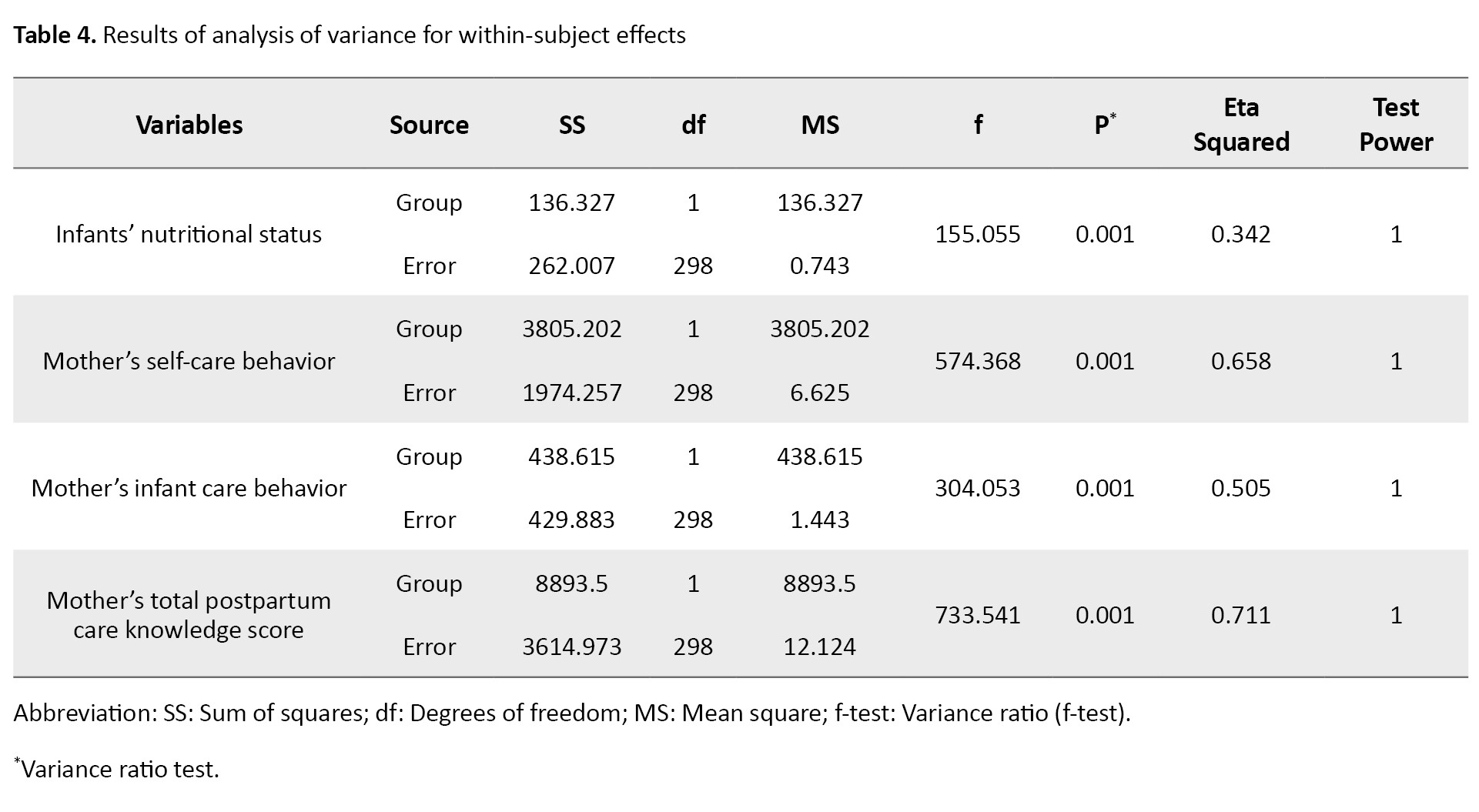
According to the independent t-test results (Table 2), the scores of infants’ nutritional status, mothers’ self-care behavior, mothers’ infant care behavior, and total postpartum care knowledge did not differ significantly between the two groups before the intervention.
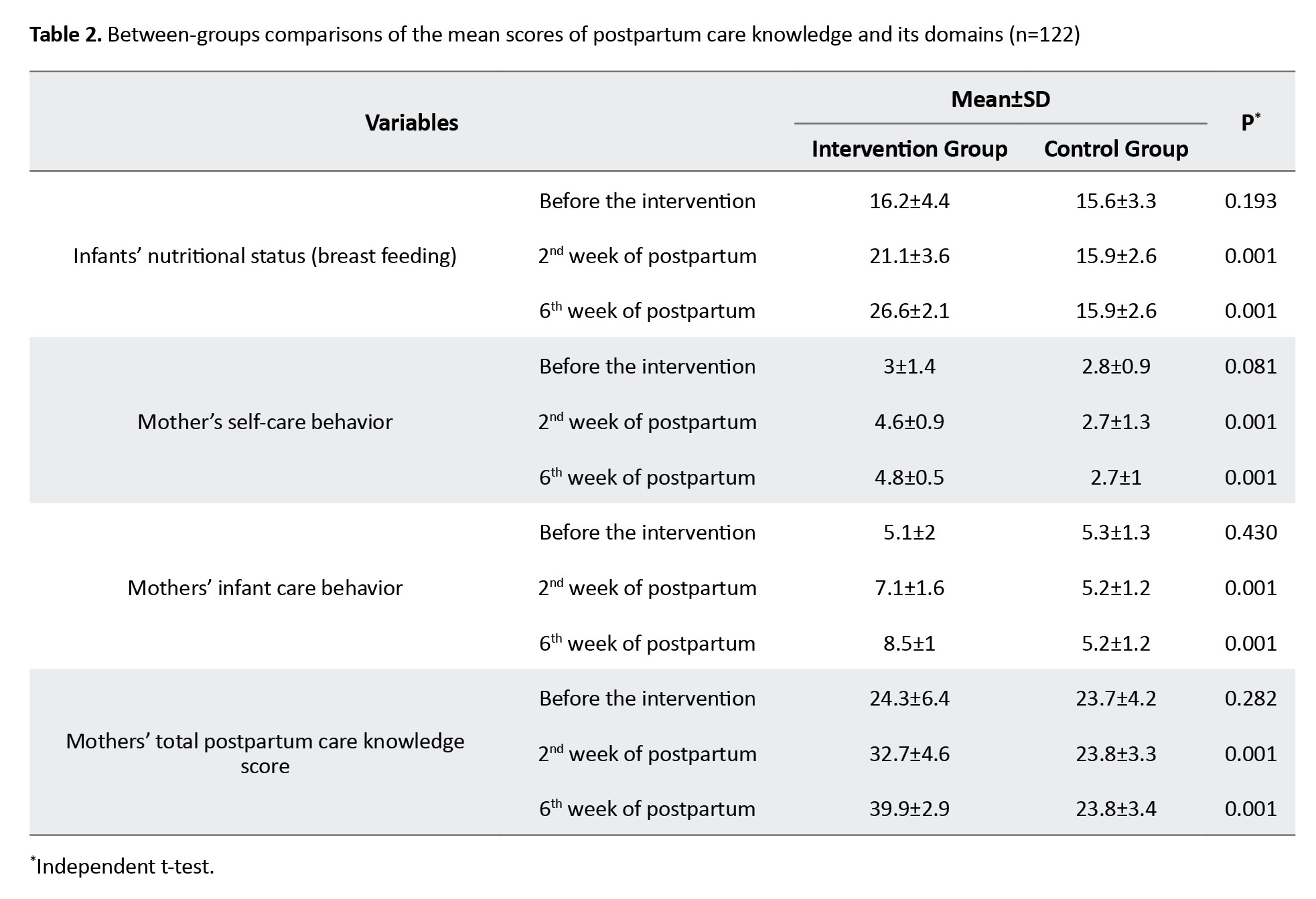
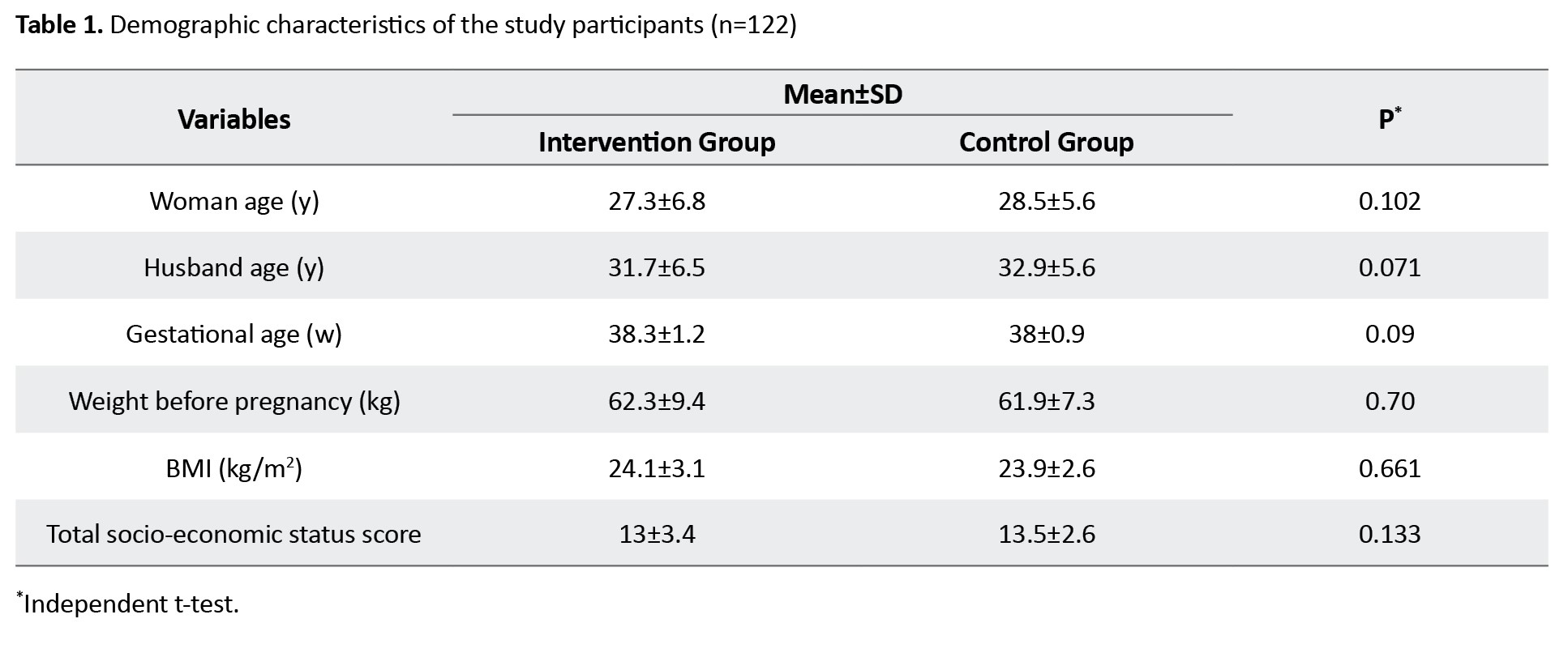
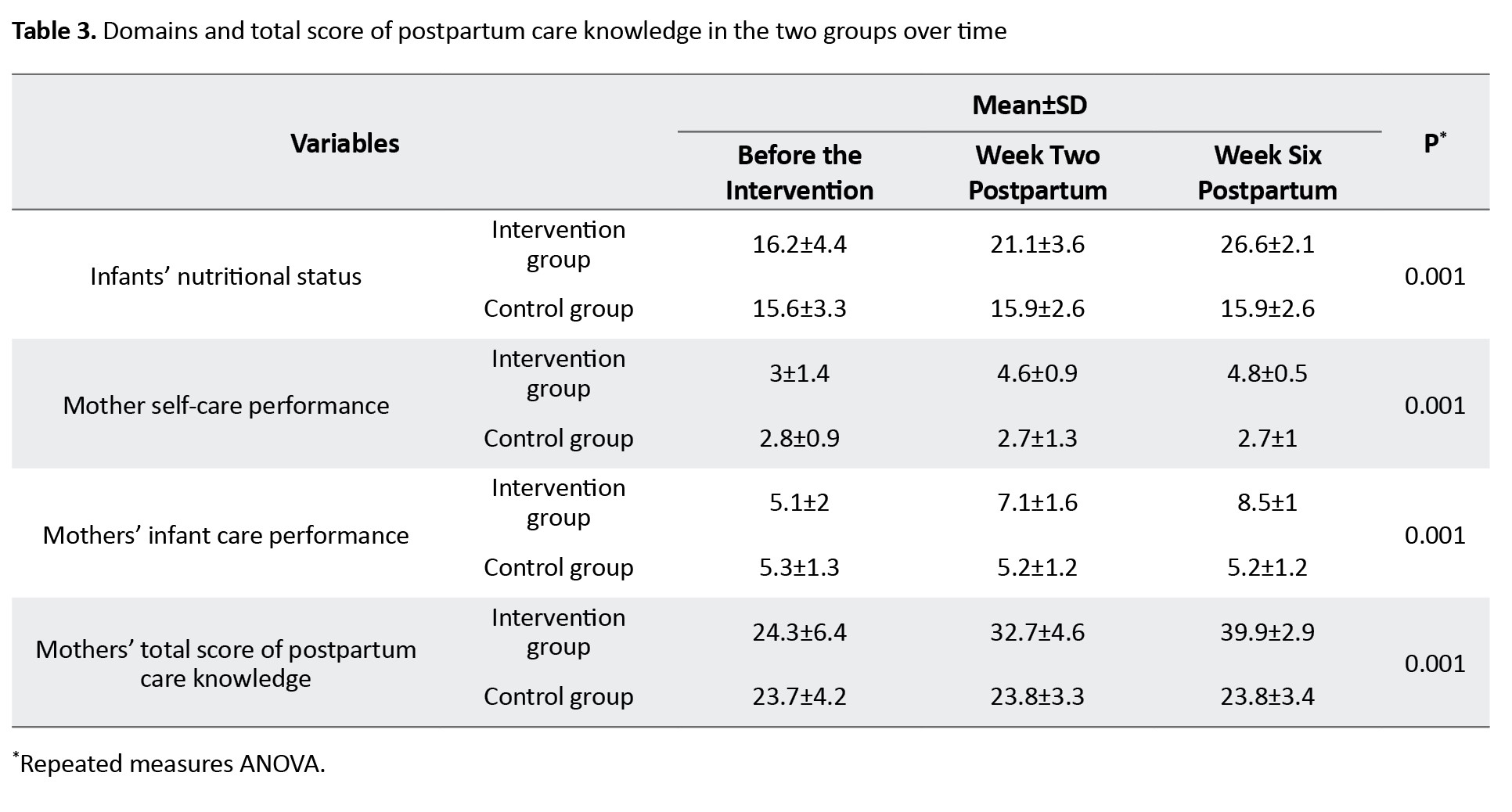
Nevertheless, the scores of these variables in the other two stages (days 14-15 and days 42-45 postpartum) differed significantly between the two groups (P=0.001). The repeated measures ANOVA was used to compare these four variables in the intervention and control groups over time. The results showed a significant increase in the mean scores over time in the intervention group (P=0.001), but the differences were not statistically significant in the control group for any variables. The results of within-group comparison showed that infants’ nutritional status, mothers’ self-care performance, mothers’ infant care performance, and mothers’ total postpartum care knowledge changed over time (P=0.001), as shown in Table 3, with the mean scores of all these variables showing an increase over time in the intervention group.
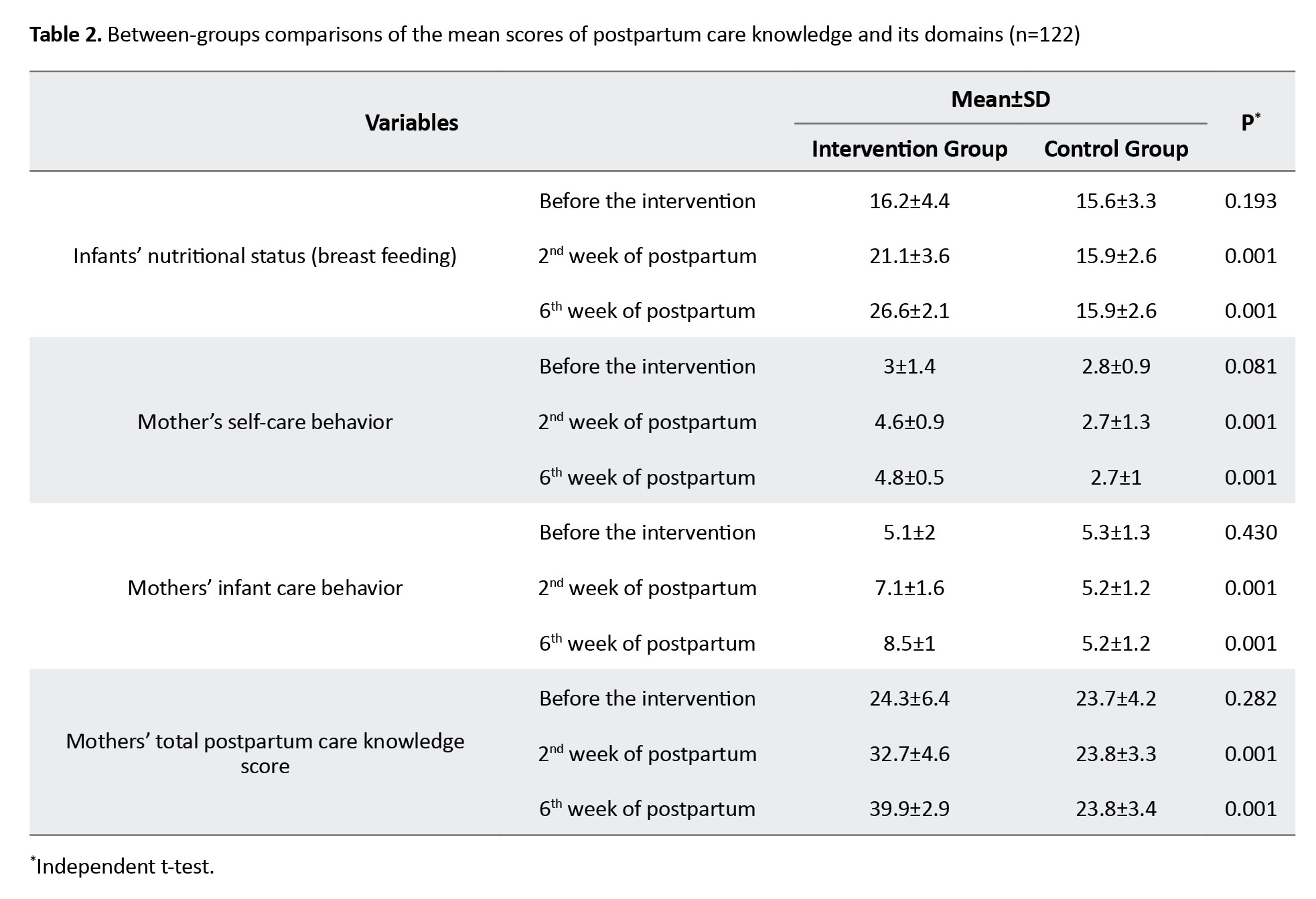
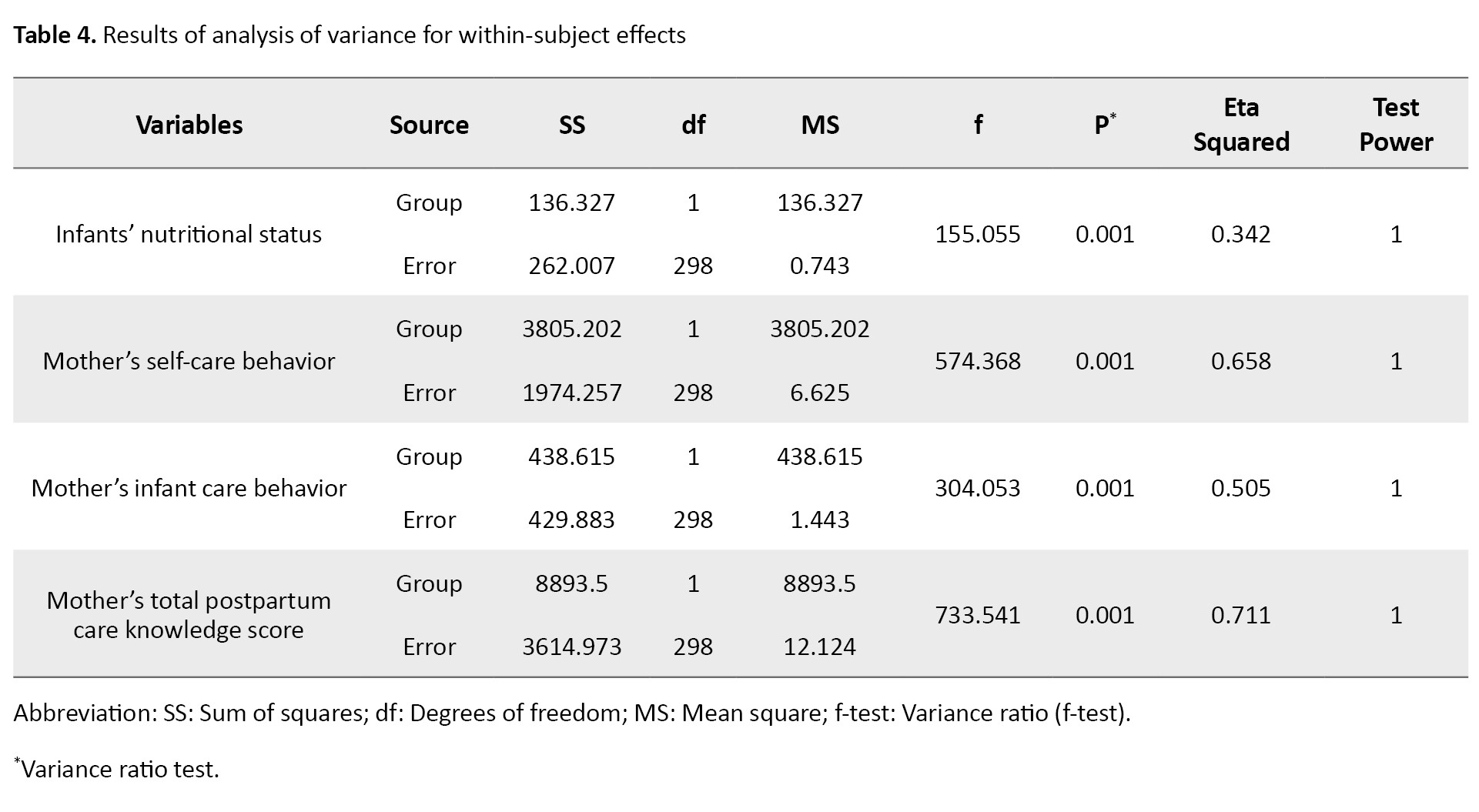
The eta-squared values showed that the use of the educational application accounted for 34.2% of the variance in infants’ nutritional status, 65.8% of the variance in mothers’ self-care performance, 50.5% of the variance in mothers’ infant care performance, and 71.1% of the variance in mothers’ total postpartum care knowledge score (Table 4).
Discussion
The residents of marginalized areas experience more diseases, accidents, and premature death. Environmental hazards and deprivations can decline the health of these residents. In this study, the effect of a safe motherhood educational application on the postpartum care of Iranian postpartum women living in marginalized areas was investigated. According to our findings, the infants’ nutritional status, mothers’ self-care behavior, mothers’ infant care behavior, and their total postpartum care knowledge increased in the intervention group over time, indicating the positive effect of educational application. Nazari et al. reviewed the results of 49 studies on postpartum care education and found that home care can improve mothers’ self-care and infant care behaviors and satisfaction [16]. According to a study by Khayat et al. the most important reasons for marginalized mothers’ failure to receive postpartum care include long waiting times and unaffordable costs of services [5]. The failure to receive postpartum care is strongly associated with socioeconomic status, ethnicity, household size, and place of service provision [17]. Poverty and its associated factors are barriers to receiving safe, accessible, appropriate, and high-quality postpartum care among women living in marginalized areas [18].
In gynecology clinics and centers, especially in marginalized areas, the necessary education is not usually given properly due to time constraints and referral of many patients. In this regard, distance learning is an effective and suitable method of learning related information for marginalized women [8]. In a study by Anto-Ocrah et al. in Malawi villages, education through mobile phones was also found to be one of the key social determinants of health that plays a vital role in reducing postpartum challenges in difficult conditions [1]. In 2014, the World Health Organization (WHO) recommended using cost-effective and practical technologies for low-income and middle-income countries. Their surveys revealed that mobile phones are a key technology for healthcare delivery and improving health outcomes [19].
Self-care education at home, due to receiving education in a safe and calm environment and spending more time on care tasks, is very effective in improving the health of mothers and infants [20]. The use of educational support systems such as mobile applications can help reduce the costs and workload of healthcare professionals. Health care systems should use mobile applications to deliver healthcare services and gain access to the most vulnerable groups living in inaccessible areas [21]. Mobile applications have been well accepted as a communication/educational tool and as a reliable means for delivering healthcare services [22].
To the best of our knowledge, this is the first study that developed a safe motherhood educational application based on needs assessments and feedback from marginalized women in Iran. However, there were some limitations. The data were collected using self-report questionnaires, which may cause response bias.
In conclusion, the designed safe motherhood educational application can improve the postpartum care knowledge of Iranian women living in marginalized areas. Given the limitations of these women, including a lack of access to healthcare services, and the importance of paying attention to the health of mothers and neonates, this educational application is recommended for them.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the National Strategic Research Center for Medical Education and the National Strategic Research Center for Medical Education, Tehran, Iran (Code: IR.NASRME.REC.1400.231).
Funding
This study is a part of prior research project (Code: 971974), and financially supported by the National Strategic Research Center for Medical Education, Tehran, Iran (Grant No.: 994880).
Authors' contributions
Study design and data interpretation: Zohreh Mahmoodi and Sara Esmaelzadeh; Data analysis and experiments: Zohreh Mahmoodi, Sara Esmaelzadeh Kourosh Kabir, Kourosh Kabir, Mohsen Arabi, Zahra Mehdizadeh-Tourzani and Farima Mohamadi; Writing the original draft: Zohreh Mahmoodi, Sara Esmaelzadeh Kourosh Kabir, Mohsen Arabi, Zahra Mehdizadeh-Tourzani, Farima Mohamadi, Mansoureh Yazdkhasti, Mahnaz Akbari Kamrani, Leila zivdarchegini, Maryam Hashmnejad; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the National Strategic Research Center for Medical Education for financial support and all the mothers who participated in this study for their cooperation.
References
The postpartum period is one of the most critical and sensitive periods in a woman’s life. It starts one hour after delivery of the placenta and occurs up to six weeks. During this period, women experience numerous physical, social, and emotional changes that can have adverse maternal and neonatal outcomes if not carefully evaluated and monitored [1]. According to the reports, 292,982 women die annually due to complications related to pregnancy, childbirth, and the postpartum period, and many suffer from long-term disabilities [2]. The risk of maternal mortality is 33 times higher in developing countries than in developed countries [3]. Providing continuous care before and during pregnancy and after childbirth is critical for reducing maternal and neonatal mortality rates worldwide [2].
Several factors contribute to postpartum women’s higher vulnerability and lack of adequate postpartum care [4]. One of these factors is the settlement on the outskirts of cities. Marginalization is a social problem that has drawn the attention of urban sociologists and other experts in urbanization [5]. Marginalized women have lower health indicators than other women [6]. One of the main reasons for this inequality is their lack of access to reproductive health facilities [7]. Studies have also shown that the lack of postpartum care is strongly associated with poor socioeconomic status, large household size, living in non-nuclear families, ethnicity, long distance to healthcare centers, poor physical environment, long waiting times, and insufficient knowledge [8, 9]. Therefore, it is essential to empower these vulnerable women through counseling and training on proper health behaviors and self-care [10]. Currently, women receive such training briefly in verbal form or using educational pamphlets in gynecology clinics, which is usually not adequate or effective due to the existing time constraints and high referral rates of these clinics. Meanwhile, the information provided through mobile applications is more convenient, effective, and accessible for a longer time [11]. In our previous study, a safe motherhood educational application for Iranian postpartum women living in marginalized areas was designed based on the qualitative results, participants’ viewpoints, and the feasibility of service provision, which can be installed on Android phones [8]. In this study, we aim to assess the impact of this mobile-based safe motherhood learning program on the postpartum care knowledge of marginalized women.
Materials and Methods
This is a quasi-experimental study conducted on 244 postpartum women referring to comprehensive health centers in Karaj (Mehdi Abad, Kalak No, and Ahmad Abad districts), Alborz Province, Iran, in 2021-2022. The sample size was calculated to be 110 per group (220 in total) using G*power software, version 3.1. Based on the results of Mirmolaei et al. [12], considering an effect size of 0.5, type I error (α) of 0.05, type II error (β) of 0.05, and 95% test power. Taking into account a 10% sample dropout, the sample size increased to 122 per group (244 in total). Participants were selected using a convenience sampling method and randomly assigned to two groups of intervention and control using a random number table. Figure 1 shows the flowchart of sampling and randomization processes. Inclusion criteria for mothers were Iranian nationality, referring to the selected health centers on postpartum days of 3-5, having an Android smartphone, no physical or mental illnesses affecting the interview (based on self-reports or medical records), being fluent in Persian, at the least a reading and writing literacy, and no use of narcotic drugs and psychotropic substances. Inclusion criteria for the newborns were being the first or second full-term (37 weeks of gestation) child of the family, having a healthy appearance, and having no anomalies. The exclusion criterion was immigration during the study.
Data were collected using a sociodemographic checklist, a postpartum care knowledge scale, a postpartum care performance checklist, and a socioeconomic status form. The sociodemographic checklist surveyed age, pre-pregnancy weight, height, and pregnancy details such as gestational age, parity, and weight before pregnancy. The postpartum care knowledge scale consisted of 42 items and three domains, including mothers’ self-care behavior (28 items), infants’ nutritional or breastfeeding status (5 items), and mothers’ infant care behavior (9 items). The items are answered as correct (1 point) or incorrect (0 points). Therefore, the total score ranges from 0 to 42, with higher scores indicating proper postpartum care knowledge. The validity and reliability of this questionnaire were investigated in Iran by Mirmolaei et al. [12]. We examined the reliability of this questionnaire on 45 participants, and a Cronbach’s α value of 0.85 was obtained. The socioeconomic status form, which was developed by Ghodratnama et al. [13], consists of four components (income, economic class, housing status, and education)and used by Eslami et al. [14]. The scoring is based on a Likert scale from 1 (very low) to 5 (very high). The total score ranges from 4 to 20.
After obtaining the necessary permits and ethical approval from the Research Ethics Committee of the National Strategic Research Center for Medical Education, the researcher visited the comprehensive health centers in the marginalized districts of Karaj and selected eligible women. After explaining the study objectives to the participants, their written consent to participate in the study was obtained. Then, the questionnaires were completed by both groups in three phases: Before the intervention (postpartum days 3-5), second week of postpartum (postpartum days 14-15), and sixth week of postpartum (postpartum days 42-45), based on the guidelines for postpartum care developed by the Iranian Ministry of Health and Medical Education [15].
For the intervention group, the safe motherhood application was installed on participants’ Android smartphones by the researcher, and they were trained on how to use it. As mentioned before, it was designed based on the results of our previous study [8]. It consisted of pre-pregnancy training, pregnancy/childbirth training, postpartum training, information about adverse pregnancy outcomes, screening, how to provide care to healthy infants, how to provide care to premature neonates, information about the stages of fetal development, interpretation of tests, and frequently asked questions. The participants in the intervention group received routine care in addition to the educational application. The control group received only routine care. After the interventions, the control group also received access to the educational application to comply with ethical considerations.
Data were analyzed in SPSS software, version 16 using descriptive statistics and analytical tests, including independent t-test, independent t-test, and repeated measures ANOVA. Before testing, the ANOVA assumptions were examined using Box’s M test, Mauchly’s test of sphericity, and Levene’s test. Since Box’s M test results did not show significant results for any variables (P>0.05), the assumption of the homogeneity of the variance-covariance matrices was established. Also, the non-significant results of Levene’s test confirmed the equality of variances between the groups (P>0.05). Mauchly’s sphericity test results were not significant for the study variables (P>0.05), indicating that the equality of variances within the subjects (i.e. the assumption of sphericity) was also met. Therefore, the Greenhouse-Geisser correction was used.
Results
The mean age of the participants was 27.3±6.8 years in the intervention group and 28.5±5.6 years in the control group. Their other characteristics are presented in Table 1.
According to the independent t-test results (Table 2), the scores of infants’ nutritional status, mothers’ self-care behavior, mothers’ infant care behavior, and total postpartum care knowledge did not differ significantly between the two groups before the intervention.
Nevertheless, the scores of these variables in the other two stages (days 14-15 and days 42-45 postpartum) differed significantly between the two groups (P=0.001). The repeated measures ANOVA was used to compare these four variables in the intervention and control groups over time. The results showed a significant increase in the mean scores over time in the intervention group (P=0.001), but the differences were not statistically significant in the control group for any variables. The results of within-group comparison showed that infants’ nutritional status, mothers’ self-care performance, mothers’ infant care performance, and mothers’ total postpartum care knowledge changed over time (P=0.001), as shown in Table 3, with the mean scores of all these variables showing an increase over time in the intervention group.
The eta-squared values showed that the use of the educational application accounted for 34.2% of the variance in infants’ nutritional status, 65.8% of the variance in mothers’ self-care performance, 50.5% of the variance in mothers’ infant care performance, and 71.1% of the variance in mothers’ total postpartum care knowledge score (Table 4).
Discussion
The residents of marginalized areas experience more diseases, accidents, and premature death. Environmental hazards and deprivations can decline the health of these residents. In this study, the effect of a safe motherhood educational application on the postpartum care of Iranian postpartum women living in marginalized areas was investigated. According to our findings, the infants’ nutritional status, mothers’ self-care behavior, mothers’ infant care behavior, and their total postpartum care knowledge increased in the intervention group over time, indicating the positive effect of educational application. Nazari et al. reviewed the results of 49 studies on postpartum care education and found that home care can improve mothers’ self-care and infant care behaviors and satisfaction [16]. According to a study by Khayat et al. the most important reasons for marginalized mothers’ failure to receive postpartum care include long waiting times and unaffordable costs of services [5]. The failure to receive postpartum care is strongly associated with socioeconomic status, ethnicity, household size, and place of service provision [17]. Poverty and its associated factors are barriers to receiving safe, accessible, appropriate, and high-quality postpartum care among women living in marginalized areas [18].
In gynecology clinics and centers, especially in marginalized areas, the necessary education is not usually given properly due to time constraints and referral of many patients. In this regard, distance learning is an effective and suitable method of learning related information for marginalized women [8]. In a study by Anto-Ocrah et al. in Malawi villages, education through mobile phones was also found to be one of the key social determinants of health that plays a vital role in reducing postpartum challenges in difficult conditions [1]. In 2014, the World Health Organization (WHO) recommended using cost-effective and practical technologies for low-income and middle-income countries. Their surveys revealed that mobile phones are a key technology for healthcare delivery and improving health outcomes [19].
Self-care education at home, due to receiving education in a safe and calm environment and spending more time on care tasks, is very effective in improving the health of mothers and infants [20]. The use of educational support systems such as mobile applications can help reduce the costs and workload of healthcare professionals. Health care systems should use mobile applications to deliver healthcare services and gain access to the most vulnerable groups living in inaccessible areas [21]. Mobile applications have been well accepted as a communication/educational tool and as a reliable means for delivering healthcare services [22].
To the best of our knowledge, this is the first study that developed a safe motherhood educational application based on needs assessments and feedback from marginalized women in Iran. However, there were some limitations. The data were collected using self-report questionnaires, which may cause response bias.
In conclusion, the designed safe motherhood educational application can improve the postpartum care knowledge of Iranian women living in marginalized areas. Given the limitations of these women, including a lack of access to healthcare services, and the importance of paying attention to the health of mothers and neonates, this educational application is recommended for them.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the National Strategic Research Center for Medical Education and the National Strategic Research Center for Medical Education, Tehran, Iran (Code: IR.NASRME.REC.1400.231).
Funding
This study is a part of prior research project (Code: 971974), and financially supported by the National Strategic Research Center for Medical Education, Tehran, Iran (Grant No.: 994880).
Authors' contributions
Study design and data interpretation: Zohreh Mahmoodi and Sara Esmaelzadeh; Data analysis and experiments: Zohreh Mahmoodi, Sara Esmaelzadeh Kourosh Kabir, Kourosh Kabir, Mohsen Arabi, Zahra Mehdizadeh-Tourzani and Farima Mohamadi; Writing the original draft: Zohreh Mahmoodi, Sara Esmaelzadeh Kourosh Kabir, Mohsen Arabi, Zahra Mehdizadeh-Tourzani, Farima Mohamadi, Mansoureh Yazdkhasti, Mahnaz Akbari Kamrani, Leila zivdarchegini, Maryam Hashmnejad; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the National Strategic Research Center for Medical Education for financial support and all the mothers who participated in this study for their cooperation.
References
- Anto-Ocrah M, Latulipe RJ, Mark TE, Adler D, Zaihra T, Lanning JW. Exploring association of mobile phone access with positive health outcomes and behaviors amongst post-partum mothers in rural Malawi. BMC Pregnancy Childbirth. 2022; 22(1):485. [DOI:10.1186/s12884-022-04782-0] [PMID]
- Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. 2016; 387(10017):462-74. [DOI:10.1016/S0140-6736(15)00838-7] [PMID]
- WHO. Maternal mortality: Evidence brief [Internet]. 2019 [Updated 2019 November 11]. Available from: [Link]
- Mi T, Hung P, Li X, McGregor A, He J, Zhou J. Racial and ethnic disparities in postpartum care in the greater boston area during the COVID-19 pandemic. JAMA Netw Open. 2022; 5(6):e2216355. [DOI:10.1001/jamanetworkopen.2022.16355] [PMID]
- Khayat S, Dolatian M, Fanaei H, Navidian A, Mahmoodi Z, Kasaeian A. Women’s reproductive health status in urban slums in Southeast Iran in 2017: A cross-sectional study. J Midwifery Reproduct Health. 2020; 8(1):2069-82. [Link]
- Baah FO, Teitelman AM, Riegel B. Marginalization: Conceptualizing patient vulnerabilities in the framework of social determinants of health-An integrative review. Nurs Inq. 2019; 26(1):e12268. [DOI:10.1111/nin.12268] [PMID]
- Kaviarasu SJ, Xavier G. Status of women’s health in urban sub-standard settlements of Chennai, Tamil Nadu state, India. Eur Acad Res. 2015; 2(1):14473-83. [Link]
- Mahmoodi Z, Arabi M, Kabir K, Yazdkhasti M, Kamrani MA, Tourzani ZM, et al. Educational needs on safe motherhood from the perspective of suburban women: A qualitative study. Heliyon. 2021; 7(3):e06582. [DOI:10.1016/j.heliyon.2021.e06582] [PMID]
- Devasenapathy N, Ghosh Jerath S, Allen E, Sharma S, Shankar AH, Zodpey S. Reproductive healthcare utilization in urban poor settlements of Delhi: Baseline survey of ANCHUL (Ante Natal and Child Health care in Urban Slums) project. BMC Pregnancy Childbirth. 2015; 15:212. [DOI:10.1186/s12884-015-0635-8] [PMID]
- Houshmandpour M, Mahmoodi Z, Lotfi R, Tehranizadeh M, Kabir K. The effect of midwife-oriented group counseling, based on oremâ s model on self-care and empowerment, in primiparous women: A clinical trial. Shiraz E Med J. 2019; 20(3):e70685. [DOI:10.5812/semj.70685]
- Borgen I, Garnweidner-Holme LM, Jacobsen AF, Bjerkan K, Fayyad S, Joranger P,et al. Smartphone application for women with gestational diabetes mellitus: A study protocol for a multicentre randomised controlled trial. BMJ Open. 2017; 7(3):e013117.[DOI:10.1136/bmjopen-2016-013117] [PMID]
- Mirmolaei T, AmelValizadeh M, Mahmoodi M, Tavakol Z. [The effect of postpartum home care on maternal practises in infant care (Persian)]. Nurs Midwifery J. 2012; 10(3):1-9. [Link]
- Ghodratnama A, Heidarinejad S, Davoodi I. [The relationship between socio-Economic status and the rate of physical activity in Shahid Chamran University Students of Ahwaz (Persian)]. Sport Manag J. 2013; 5(16):5-20. [DOI:10.22059/jsm.2013.30410]
- Eslami A, Mahmoudi A, Khabiri M, Najafiyan SM. [The role of socioeconomic conditions in the citiznsmotivation for participating in public sports (Persian)]. Appl Res Sport Manag. 2014; 2(3):89-104. [Link]
- Kharaghani R, Shariati M, Yunesian M, Keramat A, Moghisi A. The Iranian integrated maternal health care guideline based on evidence-based medicine and American guidelines: A comparative study. Mod Care J. 2016; 13(2):e9455. [DOI:10.17795/modernc.9455]
- Nazari S, Hajian S, Abasi Z, Majd HA. [A review of postpartum care education and care interventions in Iran (Persian)]. Sci J Kurdistan Univ Med Sci. 2021; 26(3):86-104. [Link]
- Grand-Guillaume-Perrenoud JA, Origlia P, Cignacco E. Barriers and facilitators of maternal healthcare utilisation in the perinatal period among women with social disadvantage: A theory-guided systematic review. Midwifery. 2022; 105:103237. [DOI:10.1016/j.midw.2021.103237] [PMID]
- Smith M, Benoit C. How social inequities in maternity care impact marginalized groups. In: Sandall J, editor. The continuous textbook of women’s medicine series–Obstetrics module. Volume 1, pregnancy and society. London: King’s College; 2021. [DOI:10.3843/GLOWM.415053]
- WHO. WHO compendium of innovative health technologies for low resource settings, 2011-2014: Assistive devices, eHealth solutions, medical devices, other technologies, technologies for outbreaks. Geneva: WHO; 2015. [Link]
- Moudi A, Tafazoli M, Boskabadi H, Ebrahimzadeh S, Salehiniya H. Comparing the effect of peer support and training by healthcare providers on women’s breastfeeding self-efficacy. J Midwifery Reproduct Health. 2016; 4(1):488-97. [DOI:10.22038/JMRH.2016.5629]
- Healthy People 2030. Social determinants of health. 2020 [Updated 2025 September 14]. Available from: [Link]
- Yazdani M, Mahmoodi Z, Azin SA, Qorbani M. The effect of counseling based on sexual self-concept via social networks on smartphone in infertile women: A randomized controlled trial. Int J Commun Based Nurs Midwifery. 2019; 7(3):231-40. [DOI:10.1016/j.midw.2021.103237] [PMID]
Article Type : Research |
Subject:
Special
Received: 2023/05/2 | Accepted: 2025/05/25 | Published: 2025/09/8
Received: 2023/05/2 | Accepted: 2025/05/25 | Published: 2025/09/8
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |