Fri, Jan 30, 2026
Volume 34, Issue 4 (9-2024)
JHNM 2024, 34(4): 316-325 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kadkhodaei F, Niknami M, Bostani Khalesi Z, Maroufizadeh S. Relationship Between Perceived Social Support and Anxiety in Pregnant Women With a History of Abortion. JHNM 2024; 34 (4) :316-325
URL: http://hnmj.gums.ac.ir/article-1-2132-en.html
URL: http://hnmj.gums.ac.ir/article-1-2132-en.html
1- Midwifery (MsN), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,niknami@gums.ac.ir
3- Associate Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
2- Instructor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Associate Professor, Department of Midwifery, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 518 kb]
(377 Downloads)
| Abstract (HTML) (914 Views)
Full-Text: (452 Views)
Introduction
Abortion is one of the most common complications during pregnancy [1, 2]. Each year, about 140 million pregnancies occur worldwide, of which about 25% end in spontaneous or induced abortion [3]. In Iran, although accurate information on abortion is not available [3], it is estimated that about 80,000 abortions occur annually [2]. Approximately 15-20% of all clinically recognized pregnancies result in spontaneous abortions [4]. Abortion is a harmful experience both physically and psychologically [5], which leads to many complications such as loss of self-confidence, initiation, or increase of alcohol or drug consumption [6], and can increase the risk of developing psychological disorders, such as anxiety [7, 8]. A significant percentage of women show high anxiety up to 6 months after abortion and are at high risk of post-traumatic stress disorder and obsessive-compulsive disorder [5, 9, 10]. Côté-Arsenault et al. reported that anxiety is higher in pregnant women with a history of perinatal loss [11]. Another study showed that the pregnant women with a history of spontaneous abortion have higher anxiety levels in the first trimester than women without a history of abortion [12].
Symptoms of anxiety caused by abortion may continue until the subsequent pregnancy [13] and cause complications such as vomiting, nausea, fatigue, preeclampsia [14], increased levels of cortisol hormones and stimulation of the adrenal gland and sympathetic system [15], preeclampsia [16], spontaneous abortion [17], and weight loss of the infant [16]. Therefore, there is a need to reduce anxiety in pregnant women. Since the medication therapy used to reduce the symptoms of anxiety during pregnancy may be associated with possible side effects such as premature delivery, many women may not want to take medications. In addition, previous studies have shown the mothers’ higher satisfaction with non-pharmacological methods or treatments [18-20]. Social support is one of the non-pharmacological solutions to reduce anxiety [21] and one of the most effective tools to deal with challenging life events [22]. It refers to mental access to care and support received from a social network. It is characterized by emotional, informational, and instrumental support that can be provided by different sources, such as friends or family [23]. Social support indirectly (through increasing social adaptation) reduces people’s reactions to stressful factors and ultimately improves their physical and mental health [24-26].
Despite the wide range of studies on the relationship between anxiety and perceived social support in pregnant women [22, 24, 26, 27], fewer studies have addressed the relationship between abortion-related anxiety and perceived social support [6, 28, 29], and there are contradictory results. The present study aims to determine the relationship between perceived social support and anxiety in pregnant women with a history of abortion.
Materials and Methods
In this analytical cross-sectional study, 193 pregnant women referred to a maternity hospital in Rasht, north of Iran, were selected by using a convenience sampling method. The sample size was determined by considering a correlation coefficient of 0.2 (relatively small effect size) as the appropriate value of correlation between the studied variables, an 80% test power, a two-tailed alpha level of 0.05, and a 10% sample dropout rate. The inclusion criteria were: A history of abortion, positive pregnancy test, no fetal abnormality or child disability in the current and previous pregnancies, no mental illness or psychiatric disorders, no use of sedatives, narcotics or psychotropic drugs, no history of smoking and alcohol consumptions, and willingness to participate in the study.
Data were collected from May to July 2022 in a specialized women’s hospital in Rasht, north of Iran in morning shifts. Before data collection, we explained the study objectives to the participants, ensured their confidentiality, and obtained their informed consent. Data was collected by a three-part questionnaire including a demographic form, Spielberger’s state-trait anxiety inventory- form Y (STAI-Y), and the multidimensional scale of perceived social support (MSPSS).
The following sociodemographicobstetric information was first recorded: Age, educational level, spouse’s education, employment status, spouse’s occupation, family income, gestational age, number of pregnancies, number of children, number of previous abortions, cause and type of abortion, the interval between the current pregnancy and the previous abortion, number of prenatal care visits, history of infertility, history of receiving prenatal care, and history of participation in childbirth preparation classes.
The STAI-Y was used to determine women’s anxiety. It is a self-report tool with 40 items rated on a 4-point Likert scale from 1 to 4. This questionnaire has two subscales to measure state and trait anxiety. The state anxiety subscale has 20 items that assess a person’s feelings at the moment and at the time of responding. The trait anxiety scale also has 20 items that measure a person’s general and normal emotions [30]. The total STAI-Y score ranges from 40 to 160, with higher scores indicating higher anxiety. In this study, the Persian version was used [31].
The MSPSS was used to measure women’s perceived adequacy of social support. It is a 12-item tool rated on a 5-point Likert scale from 0 (strongly disagree) to 5 (strongly agree) measuring social support from three sources: Family, friends, & significant others. The total score ranges from 12 to 84, where a higher score indicates more social support [32]. In this study, the Persian version was used [33].
Statistical analyses were performed in SPSS software, version 16 (SPSS Inc, Chicago, IL, USA) using the Mann-Whitney U test, Kruskal-Wallis test, Spearman’s correlation test, and multiple linear regression analysis. P<0.05 was considered statistically significant.
Results
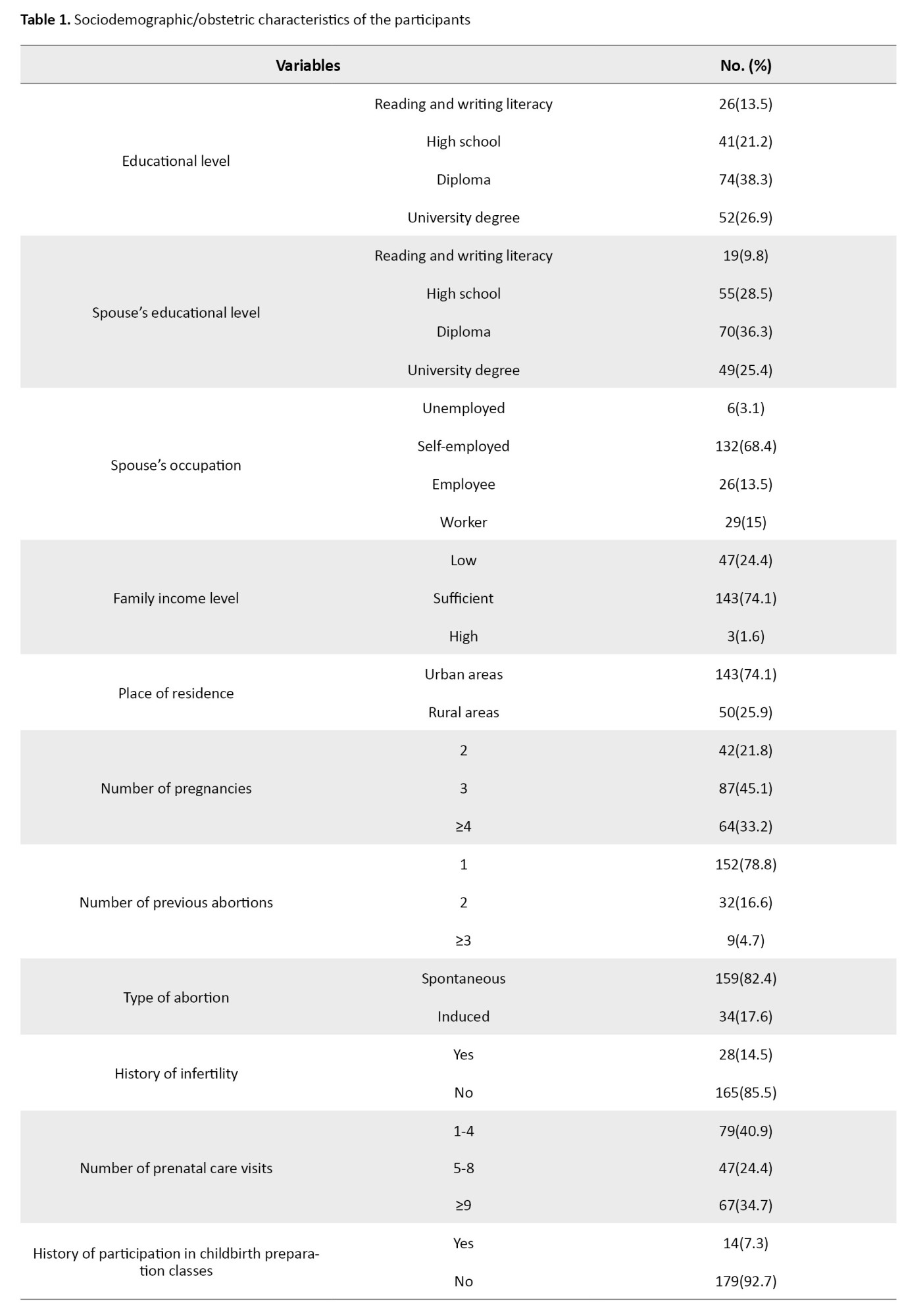
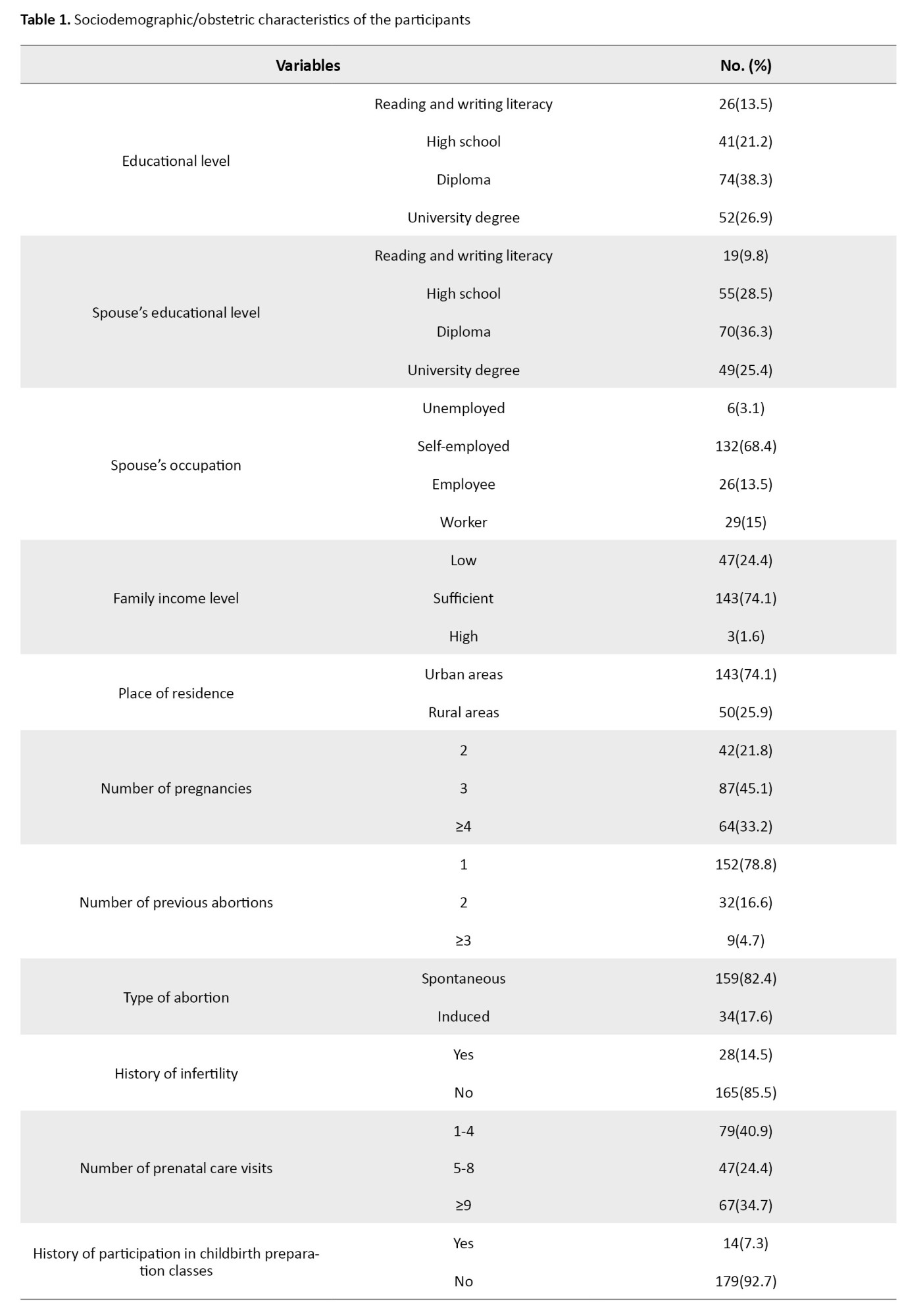
The participants’ mean age was 32.1±5.6, and their mean gestational age was 24.6±10.9 weeks. The interval between the current pregnancy and abortion was 46.4±47.8 months. The majority of women had a high school diploma (38.3%) and were housewives (87.6%) from urban areas (74.1%), with a sufficient family income (74.1%). Most of them (78.8%) had one abortion, most of which (82.4%) were spontaneous. Also, the majority of them were pregnant with previous planning (59.6%) but did not receive prenatal care (62.7%). Other characteristics are presented in Table 1.
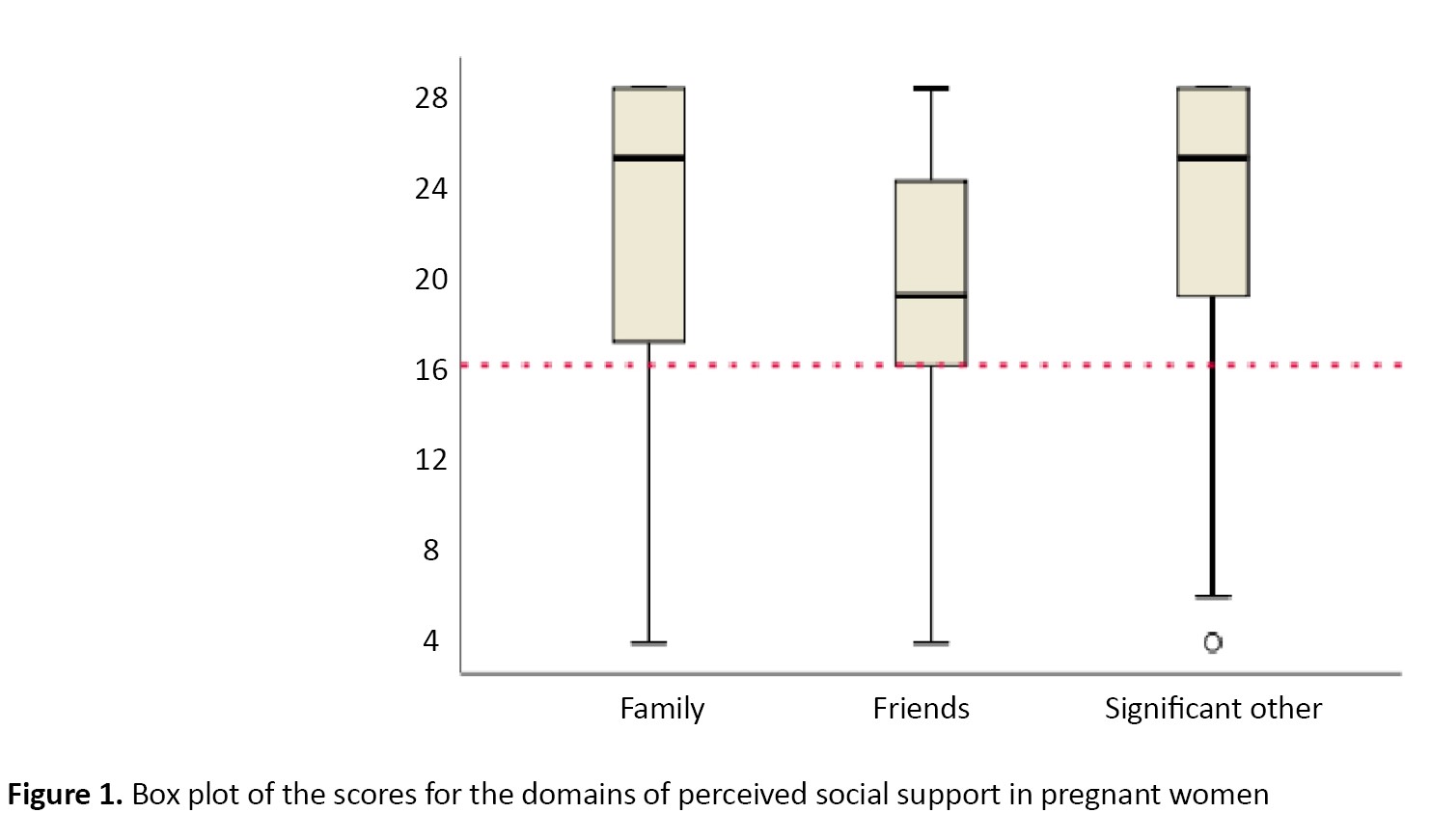
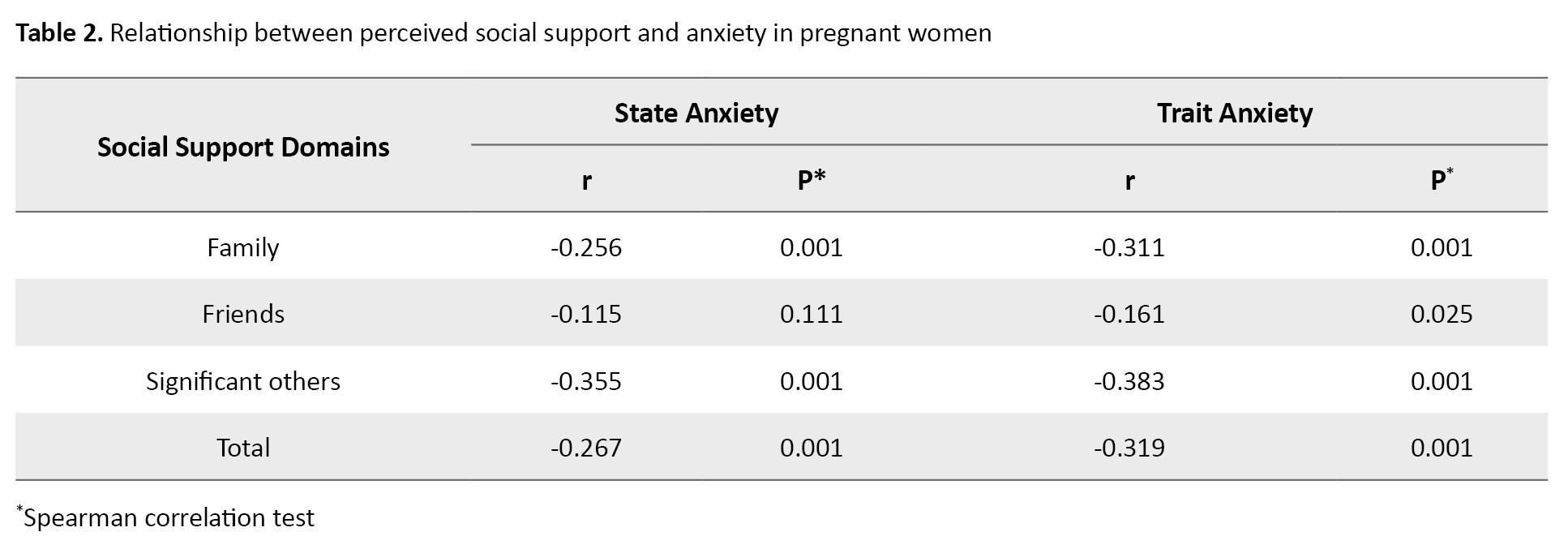
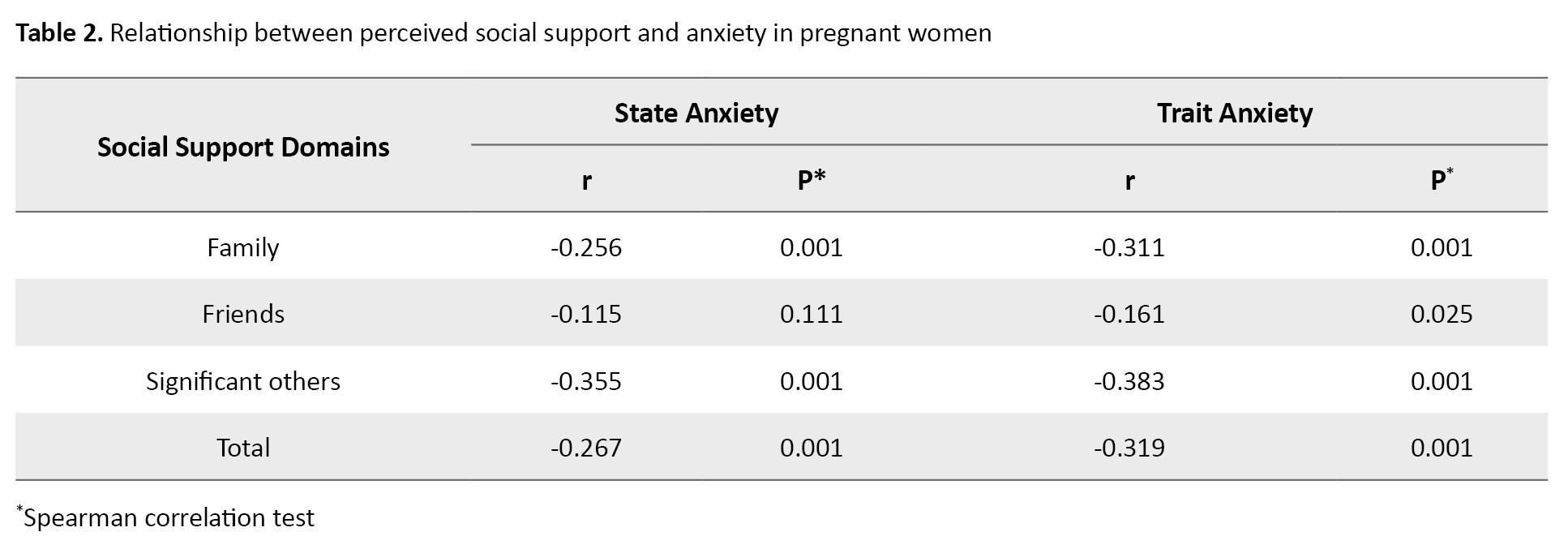
The perceived social support scores are plotted in Figure 1. The mean total score was 64.2±4.9. The mean scores for the support from family and significant others were significantly higher than the score for the support from friends (P=0.001). The mean score of trait anxiety was 38.5±12.2, and the mean score of state anxiety was 40.8±11.9. A significant negative correlation was observed between the scores of state anxiety (r=-0.267, P=0.001) and trait anxiety (r=-0.319, P=0.001) and the total score of perceived social support in pregnant women based on Spearman’s correlation test results (Table 2).
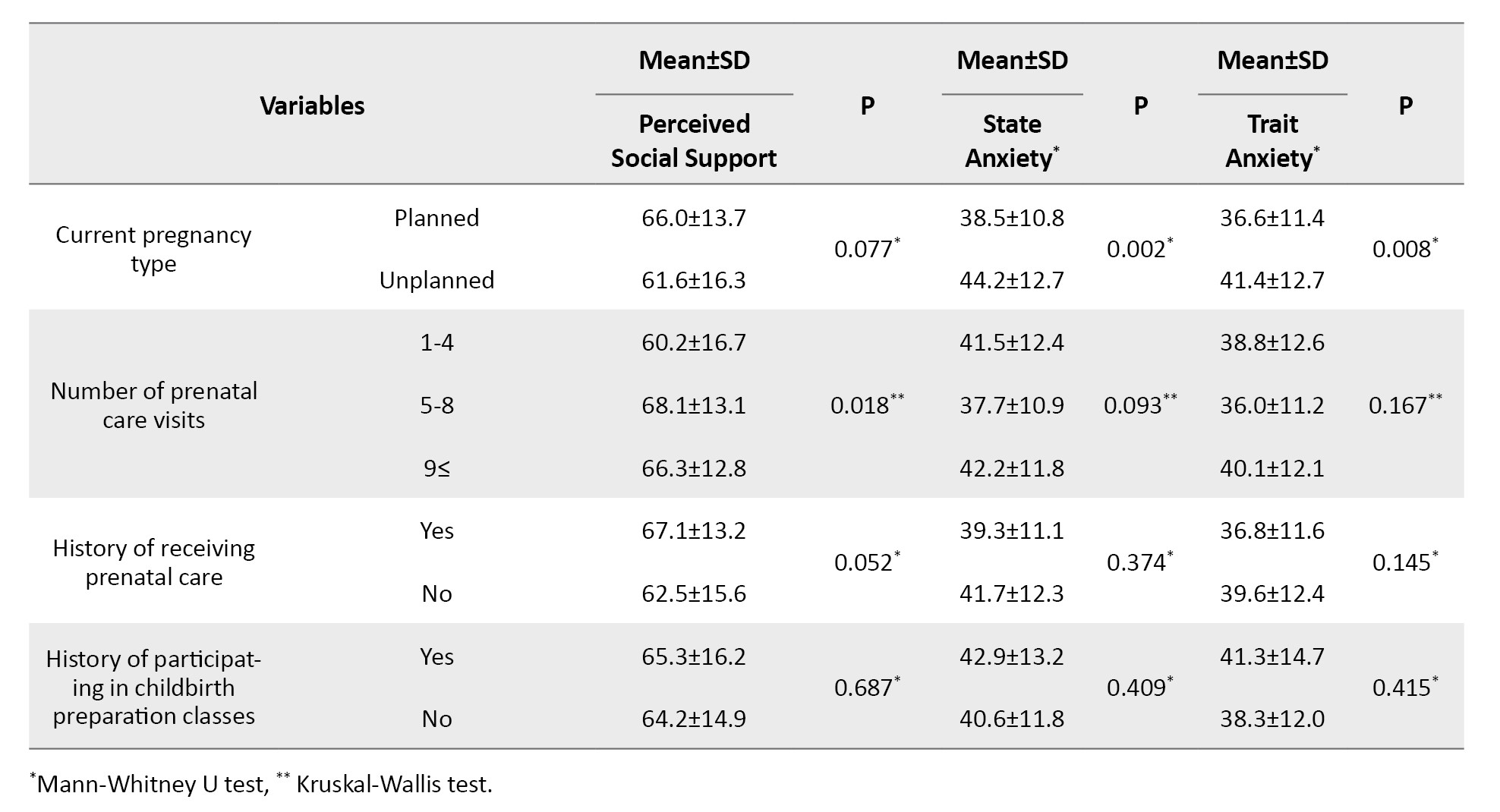
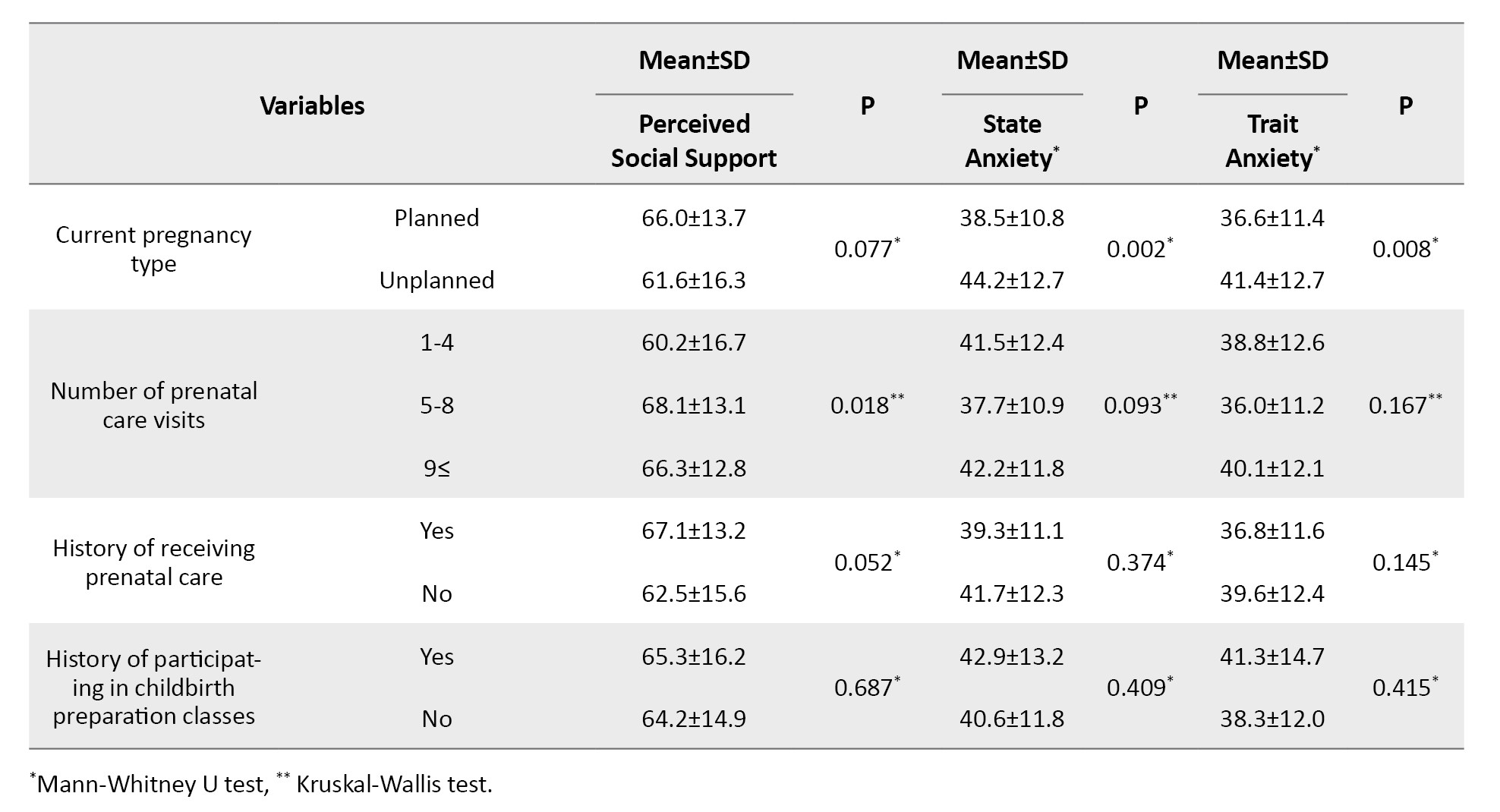
The perceived social support was significantly different based on the husband’s job, family income, number of prenatal care visits, and gestational age (P=0.001). Women’s state anxiety was significantly different based on the interval between current pregnancy and previous abortion, level of education, family income level, unplanned pregnancy, and number of prenatal care visits. Women’s trait anxiety was significantly different based on family income level, type of pregnancy, and the interval between the current pregnancy and the previous abortion (P<0.05) (Table 3).

To find the predictors of perceived social support in pregnant women, multiple linear regression analysis was used, whose results are shown in Table 4.
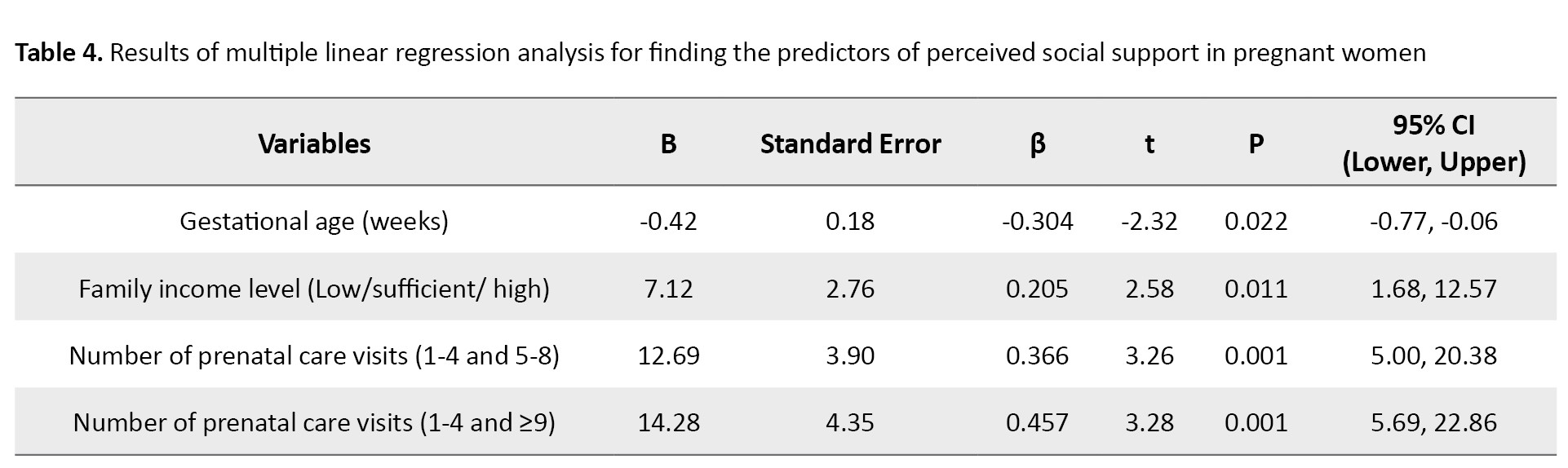
The results showed that family income level, number of prenatal care visits, and gestational age were significantly related to perceived social support. For every one week increase in the gestational age, the perceived social support score decreased by 0.42 (B=-0.42, 95% CI; -0.77%, -0.06%, P=0.022). The likelihood of having a higher perceived social support was 7.12 units higher in women with a sufficient or high family income level than those with a poor income level (B=7.12, 95% CI; 1.68%, 12.57%, P=0.011). Compared to those with 1-4 prenatal care visits, the likelihood of having a higher perceived social support was 12.69 units higher in women with 5-8 prenatal care visits (B=12.69, 95% CI; 5%, 20.38%, P=0.001) and 14.28 units higher in women with ≥9 visits (B=14.28, 95% CI; 5.69%, 22.86%, P=0.001). The coefficient of determination (R²) was 0.260, indicating that these variables explained 26% of the variation in perceived social support.
In finding the predictors of state and trait anxiety, various factors, such as the interval between the current pregnancy and the previous abortion, family income level, type of pregnancy, number of prenatal care visits, and perceived social support, showed a significant relationship with state and trait anxiety (Table 5).
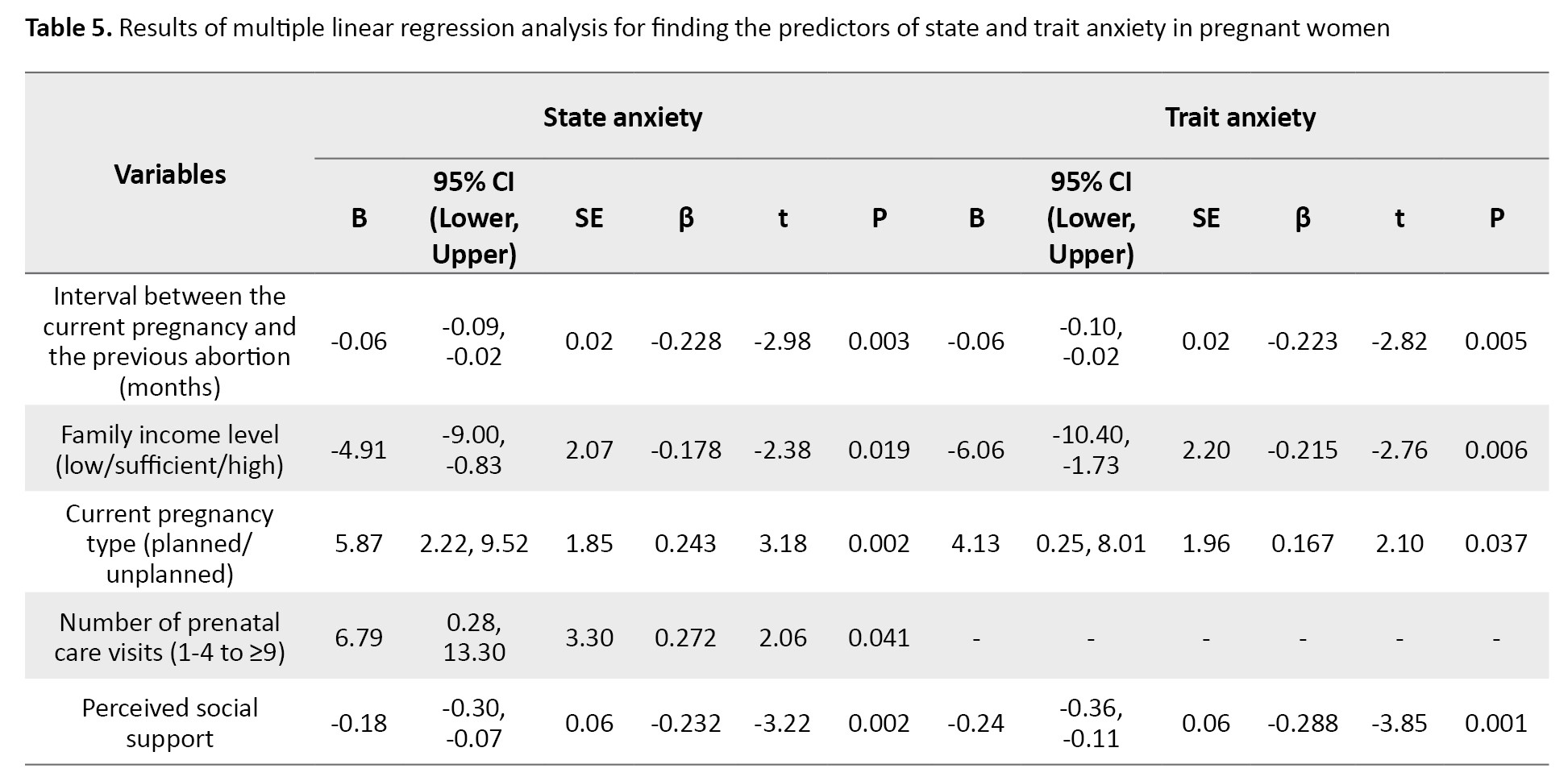
For every one month increase in the interval between the current pregnancy and the previous abortion, the state anxiety decreased by 0.06 units (B=-0.06, 95% CI; -0.09%, -0.02%, P=0.003). Women with a sufficient or high family income level were 4.91 units more likely to have low state anxiety than those with a low income level (B=-4.91, 95% CI; -9.00%, -0.83%, P=0.019). Women with unplanned pregnancies were 5.87 units more likely to have high state anxiety compared to those with planned pregnancies (B=5.87, 95% CI; 2.22%, 9.52% P=0.002). Women with ≥9 prenatal care visits were 6.79 units more likely to have high state anxiety compared to those with 1-4 visits (B=6.79, 95% CI; 0.28%, 13.30%, P=0.040). For every one unit increase in perceived social support, the state anxiety decreased by 0.18 units (B=-0.18, 95% CI; -0.30%, -0.07%, P=0.002). The R² value was 0.378, indicating that these variables explained 37.8% of the variation in state anxiety.
For every one month increase in the interval between the current pregnancy and the previous abortion, the trait anxiety decreased by 0.06 units (B=-0.06, 95% CI; -0.10%, -0.02%, P=0.005). Women with a sufficient or high family income level were 6.06 units more likely to have low trait anxiety (B=-6.06, 95% CI; 10.40%, -1.73%, P=0.006). Women with unplanned pregnancies were 4.13 units more likely to have high trait anxiety compared to those with planned pregnancies (B=4.13, 95% CI; 0.25%, 8.01%, P=0.037). For every one unit increase in perceived social support, trait anxiety decreased by 0.24 units (B=-0.24, 95% CI; -0.36%, -0.11%, P=0.001).
Discussion
The purpose of this study was to determine the relationship between perceived social support and anxiety in pregnant women with a history of abortion. According to the results, the perceived social support of women participating was at a favorable level, which is consistent with the previous studies [6, 34, 35]. However, in Gao’s study, women had a moderate level of social support [10]. The higher level of social support in the present study can be due to cultural differences. Pregnant women are important and valued in Iran and often receive good social support from family, friends, and society.
State and trait anxiety in pregnant women were at the moderate range. This is similar to Chen et al. ‘s results [34]. Another study reported that pregnant women with a history of abortion had moderate anxiety. The prevalence of anxiety in the first trimester of pregnancy in their study was 46.7% [35]. The findings of Kolte et al. also confirmed that women with a history of abortion are at a higher risk of suffering from anxiety in the subsequent pregnancy [36]. In the study by Gao et al., 47.6% of pregnant women with a history of abortion had severe anxiety [10]. The prevalence of trait anxiety in pregnant women in the present study may be due to traumatic memories from the previous pregnancy and fear of repeated abortion. Trait anxiety indicates a person’s personality anxiety [37]. We found out that women’s trait anxiety was lower than their state anxiety; as a result, their anxiety may be influenced by external factors such as abortion.
The results of the present study showed a significant relationship between perceived social support and anxiety in pregnant women. With the increase in perceived social support, their state of anxiety decreased. These findings are consistent with the results of other studies [6, 29, 38]. In Gao et al.’s study, pregnant women with low and moderate levels of social support were reported to be at higher risk of developing anxiety [10]. However, Neisani Samani et al. showed no significant relationship between pregnant women’s social support and anxiety [28].
Studies acknowledge that prenatal anxiety symptoms affect 1 in 4 women and are more common among women at risk of abortion [6, 39]. Social support is a positive factor in preventing psychological distress [28]. Obtaining social support from family, husband, and friends has been stated as one of the essential factors in preventing women from suffering from anxiety [6]. Perceived social support in pregnant women helped them to meet their psychological needs and led to less anxiety, because favorable social support can create a stronger emotional bond between the pregnant woman and the social support providers, bring peace to the women, and reduce the pressures caused by abortion on them. For every one week increase in women’s gestational age, their perceived social support increased by 0.42 units. A study in Iran also reported that gestational age had a significant relationship with perceived social support [40]. On the contrary, Sadeghi et al. did not find a significant relationship between gestational age and social support [41]. Due to reaching the final moments of pregnancy and problematic conditions of childbirth, higher gestational age leads to receiving more attention and support from family, friends, and significant others, ultimately leading to an increase in perceived social support in pregnant women.
In the present study, women with a lower level of education had more anxiety symptoms. Lower state anxiety was seen in women with a university degree. This is consistent with previous studies [10, 42], but is against the results of Neisani Samani et al.’s study [28]. Women with lower education have less knowledge about their condition and the possibility of repeated abortion, leading to more anxiety. The present study also showed that with the increase in family income, the state anxiety of pregnant women decreased. Glazier et al. also report that family income significantly affects pregnant women’s anxiety [43]. Higher income leads to receiving better quality health care services and reduce the worries and anxiety of pregnant mothers.
Perceived social support can affect the state and trait anxiety of pregnant women with a history of abortion. Therefore, healthcare providers should consider the high level of anxiety in these pregnant women and provide counseling to their husbands or families to strengthen their social support for the women and improve their mental health. In this study, we used self-report questionnaires, which may affect the responses. Moreover, the generalizability of the findings to all pregnant women in Iran should be done with caution.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.047). After explaining the study objectives to all participants, they were given informed written consent. They were free to leave the study at any time.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Maryam Niknami and Zahra Bostani Khalesi; Data collection: Fateme Kadkhodaei; Methodology and data analysis: Saman Maroofizade; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants and the staff of Al-Zahra Maternity Hospital in Rasht for their cooperation in this study.
References
Abortion is one of the most common complications during pregnancy [1, 2]. Each year, about 140 million pregnancies occur worldwide, of which about 25% end in spontaneous or induced abortion [3]. In Iran, although accurate information on abortion is not available [3], it is estimated that about 80,000 abortions occur annually [2]. Approximately 15-20% of all clinically recognized pregnancies result in spontaneous abortions [4]. Abortion is a harmful experience both physically and psychologically [5], which leads to many complications such as loss of self-confidence, initiation, or increase of alcohol or drug consumption [6], and can increase the risk of developing psychological disorders, such as anxiety [7, 8]. A significant percentage of women show high anxiety up to 6 months after abortion and are at high risk of post-traumatic stress disorder and obsessive-compulsive disorder [5, 9, 10]. Côté-Arsenault et al. reported that anxiety is higher in pregnant women with a history of perinatal loss [11]. Another study showed that the pregnant women with a history of spontaneous abortion have higher anxiety levels in the first trimester than women without a history of abortion [12].
Symptoms of anxiety caused by abortion may continue until the subsequent pregnancy [13] and cause complications such as vomiting, nausea, fatigue, preeclampsia [14], increased levels of cortisol hormones and stimulation of the adrenal gland and sympathetic system [15], preeclampsia [16], spontaneous abortion [17], and weight loss of the infant [16]. Therefore, there is a need to reduce anxiety in pregnant women. Since the medication therapy used to reduce the symptoms of anxiety during pregnancy may be associated with possible side effects such as premature delivery, many women may not want to take medications. In addition, previous studies have shown the mothers’ higher satisfaction with non-pharmacological methods or treatments [18-20]. Social support is one of the non-pharmacological solutions to reduce anxiety [21] and one of the most effective tools to deal with challenging life events [22]. It refers to mental access to care and support received from a social network. It is characterized by emotional, informational, and instrumental support that can be provided by different sources, such as friends or family [23]. Social support indirectly (through increasing social adaptation) reduces people’s reactions to stressful factors and ultimately improves their physical and mental health [24-26].
Despite the wide range of studies on the relationship between anxiety and perceived social support in pregnant women [22, 24, 26, 27], fewer studies have addressed the relationship between abortion-related anxiety and perceived social support [6, 28, 29], and there are contradictory results. The present study aims to determine the relationship between perceived social support and anxiety in pregnant women with a history of abortion.
Materials and Methods
In this analytical cross-sectional study, 193 pregnant women referred to a maternity hospital in Rasht, north of Iran, were selected by using a convenience sampling method. The sample size was determined by considering a correlation coefficient of 0.2 (relatively small effect size) as the appropriate value of correlation between the studied variables, an 80% test power, a two-tailed alpha level of 0.05, and a 10% sample dropout rate. The inclusion criteria were: A history of abortion, positive pregnancy test, no fetal abnormality or child disability in the current and previous pregnancies, no mental illness or psychiatric disorders, no use of sedatives, narcotics or psychotropic drugs, no history of smoking and alcohol consumptions, and willingness to participate in the study.
Data were collected from May to July 2022 in a specialized women’s hospital in Rasht, north of Iran in morning shifts. Before data collection, we explained the study objectives to the participants, ensured their confidentiality, and obtained their informed consent. Data was collected by a three-part questionnaire including a demographic form, Spielberger’s state-trait anxiety inventory- form Y (STAI-Y), and the multidimensional scale of perceived social support (MSPSS).
The following sociodemographicobstetric information was first recorded: Age, educational level, spouse’s education, employment status, spouse’s occupation, family income, gestational age, number of pregnancies, number of children, number of previous abortions, cause and type of abortion, the interval between the current pregnancy and the previous abortion, number of prenatal care visits, history of infertility, history of receiving prenatal care, and history of participation in childbirth preparation classes.
The STAI-Y was used to determine women’s anxiety. It is a self-report tool with 40 items rated on a 4-point Likert scale from 1 to 4. This questionnaire has two subscales to measure state and trait anxiety. The state anxiety subscale has 20 items that assess a person’s feelings at the moment and at the time of responding. The trait anxiety scale also has 20 items that measure a person’s general and normal emotions [30]. The total STAI-Y score ranges from 40 to 160, with higher scores indicating higher anxiety. In this study, the Persian version was used [31].
The MSPSS was used to measure women’s perceived adequacy of social support. It is a 12-item tool rated on a 5-point Likert scale from 0 (strongly disagree) to 5 (strongly agree) measuring social support from three sources: Family, friends, & significant others. The total score ranges from 12 to 84, where a higher score indicates more social support [32]. In this study, the Persian version was used [33].
Statistical analyses were performed in SPSS software, version 16 (SPSS Inc, Chicago, IL, USA) using the Mann-Whitney U test, Kruskal-Wallis test, Spearman’s correlation test, and multiple linear regression analysis. P<0.05 was considered statistically significant.
Results
The participants’ mean age was 32.1±5.6, and their mean gestational age was 24.6±10.9 weeks. The interval between the current pregnancy and abortion was 46.4±47.8 months. The majority of women had a high school diploma (38.3%) and were housewives (87.6%) from urban areas (74.1%), with a sufficient family income (74.1%). Most of them (78.8%) had one abortion, most of which (82.4%) were spontaneous. Also, the majority of them were pregnant with previous planning (59.6%) but did not receive prenatal care (62.7%). Other characteristics are presented in Table 1.
The perceived social support scores are plotted in Figure 1. The mean total score was 64.2±4.9. The mean scores for the support from family and significant others were significantly higher than the score for the support from friends (P=0.001). The mean score of trait anxiety was 38.5±12.2, and the mean score of state anxiety was 40.8±11.9. A significant negative correlation was observed between the scores of state anxiety (r=-0.267, P=0.001) and trait anxiety (r=-0.319, P=0.001) and the total score of perceived social support in pregnant women based on Spearman’s correlation test results (Table 2).
The perceived social support was significantly different based on the husband’s job, family income, number of prenatal care visits, and gestational age (P=0.001). Women’s state anxiety was significantly different based on the interval between current pregnancy and previous abortion, level of education, family income level, unplanned pregnancy, and number of prenatal care visits. Women’s trait anxiety was significantly different based on family income level, type of pregnancy, and the interval between the current pregnancy and the previous abortion (P<0.05) (Table 3).

To find the predictors of perceived social support in pregnant women, multiple linear regression analysis was used, whose results are shown in Table 4.
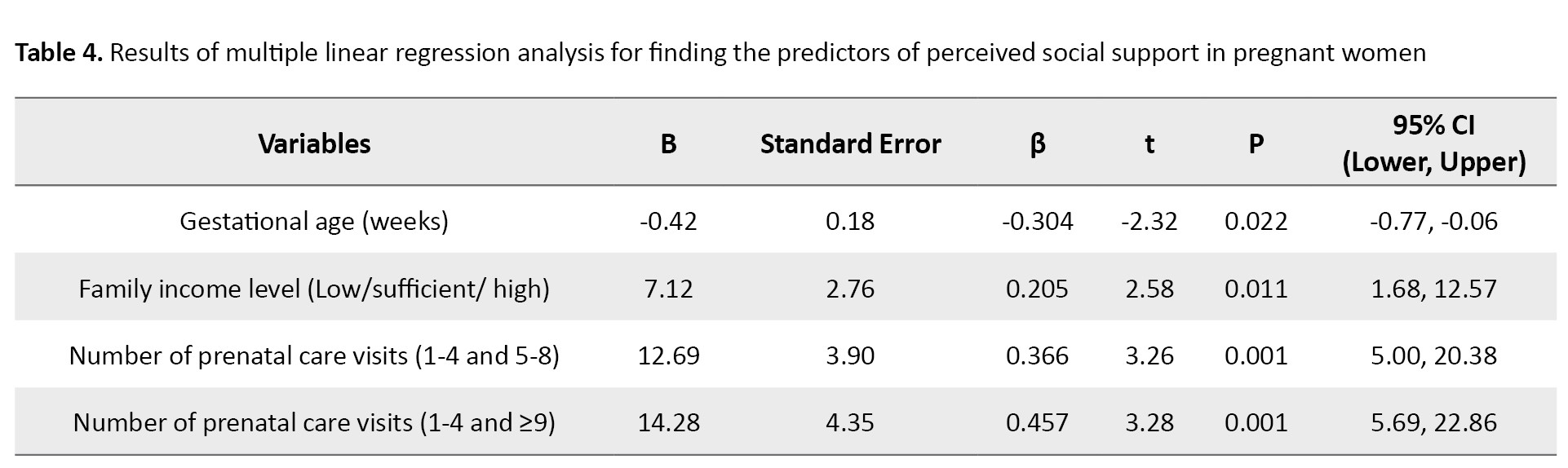
The results showed that family income level, number of prenatal care visits, and gestational age were significantly related to perceived social support. For every one week increase in the gestational age, the perceived social support score decreased by 0.42 (B=-0.42, 95% CI; -0.77%, -0.06%, P=0.022). The likelihood of having a higher perceived social support was 7.12 units higher in women with a sufficient or high family income level than those with a poor income level (B=7.12, 95% CI; 1.68%, 12.57%, P=0.011). Compared to those with 1-4 prenatal care visits, the likelihood of having a higher perceived social support was 12.69 units higher in women with 5-8 prenatal care visits (B=12.69, 95% CI; 5%, 20.38%, P=0.001) and 14.28 units higher in women with ≥9 visits (B=14.28, 95% CI; 5.69%, 22.86%, P=0.001). The coefficient of determination (R²) was 0.260, indicating that these variables explained 26% of the variation in perceived social support.
In finding the predictors of state and trait anxiety, various factors, such as the interval between the current pregnancy and the previous abortion, family income level, type of pregnancy, number of prenatal care visits, and perceived social support, showed a significant relationship with state and trait anxiety (Table 5).
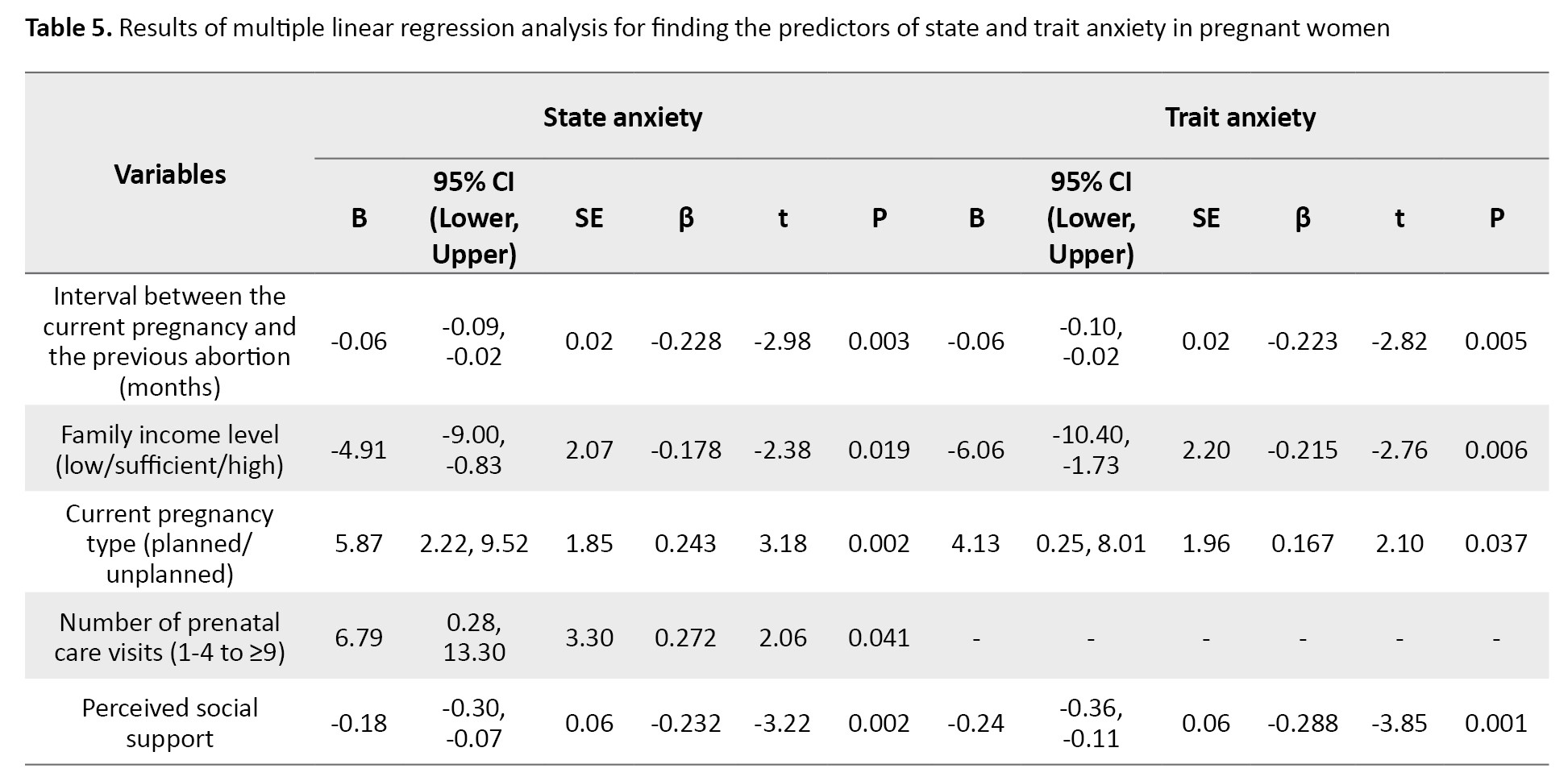
For every one month increase in the interval between the current pregnancy and the previous abortion, the state anxiety decreased by 0.06 units (B=-0.06, 95% CI; -0.09%, -0.02%, P=0.003). Women with a sufficient or high family income level were 4.91 units more likely to have low state anxiety than those with a low income level (B=-4.91, 95% CI; -9.00%, -0.83%, P=0.019). Women with unplanned pregnancies were 5.87 units more likely to have high state anxiety compared to those with planned pregnancies (B=5.87, 95% CI; 2.22%, 9.52% P=0.002). Women with ≥9 prenatal care visits were 6.79 units more likely to have high state anxiety compared to those with 1-4 visits (B=6.79, 95% CI; 0.28%, 13.30%, P=0.040). For every one unit increase in perceived social support, the state anxiety decreased by 0.18 units (B=-0.18, 95% CI; -0.30%, -0.07%, P=0.002). The R² value was 0.378, indicating that these variables explained 37.8% of the variation in state anxiety.
For every one month increase in the interval between the current pregnancy and the previous abortion, the trait anxiety decreased by 0.06 units (B=-0.06, 95% CI; -0.10%, -0.02%, P=0.005). Women with a sufficient or high family income level were 6.06 units more likely to have low trait anxiety (B=-6.06, 95% CI; 10.40%, -1.73%, P=0.006). Women with unplanned pregnancies were 4.13 units more likely to have high trait anxiety compared to those with planned pregnancies (B=4.13, 95% CI; 0.25%, 8.01%, P=0.037). For every one unit increase in perceived social support, trait anxiety decreased by 0.24 units (B=-0.24, 95% CI; -0.36%, -0.11%, P=0.001).
Discussion
The purpose of this study was to determine the relationship between perceived social support and anxiety in pregnant women with a history of abortion. According to the results, the perceived social support of women participating was at a favorable level, which is consistent with the previous studies [6, 34, 35]. However, in Gao’s study, women had a moderate level of social support [10]. The higher level of social support in the present study can be due to cultural differences. Pregnant women are important and valued in Iran and often receive good social support from family, friends, and society.
State and trait anxiety in pregnant women were at the moderate range. This is similar to Chen et al. ‘s results [34]. Another study reported that pregnant women with a history of abortion had moderate anxiety. The prevalence of anxiety in the first trimester of pregnancy in their study was 46.7% [35]. The findings of Kolte et al. also confirmed that women with a history of abortion are at a higher risk of suffering from anxiety in the subsequent pregnancy [36]. In the study by Gao et al., 47.6% of pregnant women with a history of abortion had severe anxiety [10]. The prevalence of trait anxiety in pregnant women in the present study may be due to traumatic memories from the previous pregnancy and fear of repeated abortion. Trait anxiety indicates a person’s personality anxiety [37]. We found out that women’s trait anxiety was lower than their state anxiety; as a result, their anxiety may be influenced by external factors such as abortion.
The results of the present study showed a significant relationship between perceived social support and anxiety in pregnant women. With the increase in perceived social support, their state of anxiety decreased. These findings are consistent with the results of other studies [6, 29, 38]. In Gao et al.’s study, pregnant women with low and moderate levels of social support were reported to be at higher risk of developing anxiety [10]. However, Neisani Samani et al. showed no significant relationship between pregnant women’s social support and anxiety [28].
Studies acknowledge that prenatal anxiety symptoms affect 1 in 4 women and are more common among women at risk of abortion [6, 39]. Social support is a positive factor in preventing psychological distress [28]. Obtaining social support from family, husband, and friends has been stated as one of the essential factors in preventing women from suffering from anxiety [6]. Perceived social support in pregnant women helped them to meet their psychological needs and led to less anxiety, because favorable social support can create a stronger emotional bond between the pregnant woman and the social support providers, bring peace to the women, and reduce the pressures caused by abortion on them. For every one week increase in women’s gestational age, their perceived social support increased by 0.42 units. A study in Iran also reported that gestational age had a significant relationship with perceived social support [40]. On the contrary, Sadeghi et al. did not find a significant relationship between gestational age and social support [41]. Due to reaching the final moments of pregnancy and problematic conditions of childbirth, higher gestational age leads to receiving more attention and support from family, friends, and significant others, ultimately leading to an increase in perceived social support in pregnant women.
In the present study, women with a lower level of education had more anxiety symptoms. Lower state anxiety was seen in women with a university degree. This is consistent with previous studies [10, 42], but is against the results of Neisani Samani et al.’s study [28]. Women with lower education have less knowledge about their condition and the possibility of repeated abortion, leading to more anxiety. The present study also showed that with the increase in family income, the state anxiety of pregnant women decreased. Glazier et al. also report that family income significantly affects pregnant women’s anxiety [43]. Higher income leads to receiving better quality health care services and reduce the worries and anxiety of pregnant mothers.
Perceived social support can affect the state and trait anxiety of pregnant women with a history of abortion. Therefore, healthcare providers should consider the high level of anxiety in these pregnant women and provide counseling to their husbands or families to strengthen their social support for the women and improve their mental health. In this study, we used self-report questionnaires, which may affect the responses. Moreover, the generalizability of the findings to all pregnant women in Iran should be done with caution.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.047). After explaining the study objectives to all participants, they were given informed written consent. They were free to leave the study at any time.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Maryam Niknami and Zahra Bostani Khalesi; Data collection: Fateme Kadkhodaei; Methodology and data analysis: Saman Maroofizade; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants and the staff of Al-Zahra Maternity Hospital in Rasht for their cooperation in this study.
References
- Leveno KJ, Spong CY, Dashe JS, Casey BM, Hoffman BL, Cunningham FG, et al. Williams Obstetrics, 25th Edition. New York: McGraw-Hill Education; 2018. [Link]
- Rahmani R, Yaghoobi Moghadam F, Rasooli M, Heydarian Node Z. [Relation between Couples’ Blood Group and RH with Abortions in women of reproductive age: A case-control study (Persian)]. Iran J Obstet Gynecol Infertil. 2020; 23(9):17-26. [DOI:10.22038/ijogi.2020.17371]
- Mahdavi SA, Jafari A, Azimi K, Dehghanizadeh N, Barzegar A. Therapeutic abortion in Iran: An epidemiologic study of legal abortion in 2 years. BMC Res Notes. 2020; 13(1):1-6. [DOI:10.1186/s13104-020-05098-y]
- Mohammadi M, Shirazi SR, Derogar P, Dadashi A, Mohammadi S, Moharrami T. [Evaluation of factors involved in Recurrent Miscarriages (Persian)]. Sarem J Med Res. 2021; 6(3):185-98. [DOI:10.52547/sjrm.6.3.185]
- Khodakarami B, Shobeiri F, Mefakheri B, Soltanian A, Mohagheghi H. [The effect of counseling based on fordyce’s pattern of happiness on the anxiety of women with spontaneous abortion (Persian)]. Avicenna J Nurs Midwifery Care. 2019; 26(6):377-88. [DOI:10.30699/sjhnmf.26.6.377]
- GÜMÜŞSOY S, Dönmez S, Çiçek Ö. Anxiety, depression, hopelessness and perceived social support levels of women with and without threatened miscarriage. J Clin Obstet Gynecol. 2020; 30(2):43-51. [DOI:10.5336/jcog.2019-72381]
- Knight LK, Depue BE. New frontiers in anxiety research: The translational potential of the bed nucleus of the stria terminalis. Front Psychiatry. 2019; 10:510. [DOI:10.3389/fpsyt.2019.00510]
- Sinesi A, Maxwell M, O’Carroll R, Cheyne H. Anxiety scales used in pregnancy: Systematic review.BJPsych Open. 2019; 5(1):e5.[DOI:10.1192/bjo.2018.75]
- Blackmore ER, Côté-Arsenault D, Tang W, Glover V, Evans J, Golding J, et al. Previous prenatal loss as a predictor of perinatal depression and anxiety. Br J Psychiatry Suppl. 2011; 198(5):373-8. [DOI:10.1192/bjp.bp.110.083105]
- Gao L, Qu J, Wang AY. Anxiety, depression and social support in pregnant women with a history of recurrent miscarriage: A cross-sectional study. J Reprod Infant Psychol. 2020; 38(5):497-508. [DOI:10.1080/02646838.2019.1652730]
- Côté-Arsenault D. The influence of perinatal loss on anxiety in multigravidas. J Obstet Gynecol Neonatal Nurs. 2003; 32(5):623-9. [DOI:10.1177/0884217503257140] [PMID]
- Fertl KI, Bergner A, Beyer R, Klapp BF, Rauchfuss M. Levels and effects of different forms of anxiety during pregnancy after a prior miscarriage. Eur J Obstet Gynecol Reprod Biol. 2009; 142(1):23-9. [DOI:10.1016/j.ejogrb.2008.09.009]
- Haghparast E, Faramarzi M, Hassanzadeh R. Psychiatric symptoms and pregnancy distress in subsequent pregnancy after spontaneous abortion history. Pak J Med Sci. 2016; 32(5):1097-101. [DOI:10.12669/pjms.325.10909]
- Ertekin Pinar S, Duran Aksoy O, Daglar G, Yurtsal ZB, Cesur B. Effect of stress management training on depression, stress and coping strategies in pregnant women: A randomised controlled trial. J Psychosom Obstet Gynecol. 2018; 39(3):203-10. [DOI:10.1080/0167482X.2017.1321632]
- Campillo IS, Meaney S, McNamara K, O’Donoghue K. Psychological and support interventions to reduce levels of stress, anxiety or depression on women’s subsequent pregnancy with a history of miscarriage: An empty systematic review. BMJ Open. 2017; 7(9):e017802. [DOI:10.1136/bmjopen-2017-017802]
- Mohammadpour M, Mohammad-Alizadeh Charandabi S, Malakouti J, Mohammadi MN, Mirghafourvand M. The effect of counseling on fathers’ stress and anxiety during pregnancy: A randomized controlled clinical trial. BMC Psychiatry. 2021; 21(1):1-8. [DOI:10.1186/s12888-021-03217-y]
- Boryri T, Navidian A, Zehi FH. Assessing the effect of self-care education on anxiety and depression among pregnant women with a history of spontaneous abortion. J Educ Health Promot. 2020; 9(1):347. [DOI:10.4103/jehp.jehp_465_20]
- Domínguez-Solís E, Lima-Serrano M, Lima-Rodriguez JS. Non-pharmacological interventions to reduce anxiety in pregnancy, labour and postpartum: A systematic review. Midwifery. 2021; 102:103126. [DOI:10.1016/j.midw.2021.103126]
- Bodaghi E, Alipour F, Bodaghi M, Nori R, Peiman N, Saeidpour S. [The role of spirituality and social support in pregnant women’s anxiety, depression and stress symptoms (Persian)]. J Community Health. 2016; 10(2):72-82. [Link]
- Henrique AJ, Gabrielloni MC, Rodney P, Barbieri M. Non-pharmacological interventions during childbirth for pain relief, anxiety, and neuroendocrine stress parameters: A randomized controlled trial. Int J Nurs Pract. 2018; 24(3):e12642. [DOI:10.1111/ijn.12642]
- Evans K, Spiby H, Morrell JC. Non-pharmacological interventions to reduce the symptoms of mild to moderate anxiety in pregnant women. A systematic review and narrative synthesis of women’s views on the acceptability of and satisfaction with interventions. Arch Womens Ment Health. 2020; 23(1):11-28. [DOI:10.1007/s00737-018-0936-9]
- Yu M, Qiu T, Liu C, Cui Q, Wu H. The mediating role of perceived social support between anxiety symptoms and life satisfaction in pregnant women: A cross-sectional study. Health Qual Life Outcomes. 2020; 18(1):1-8. [DOI:10.1186/s12955-020-01479-w]
- Scardera S, Perret LC, Ouellet-Morin I, Gariépy G, Juster RP, Boivin M, et al. Association of social support during adolescence with depression, anxiety, and suicidal ideation in young adults. JAMA Netw Open. 2020; 3(12):e2027491. [DOI:10.1001/jamanetworkopen.2020.27491]
- Fayazi S, Ghasemi F, Ghobadian M, Zenoozian S, Kharaghani R. [Relationship between social support with anxiety, depression, and stress in pregnant women attending to health care centers in Zanjan-Iran in 2015-2016 (Persian)]. Prev Care Nurs Midwifery J. 2017; 7(2):41-8. [Link]
- Bedaso A, Adams J, Peng W, Sibbritt D. The relationship between social support and mental health problems during pregnancy: A systematic review and meta-analysis. Reprod Health. 2021; 18:62. [DOI:10.1186/s12978-021-01209-5]
- Basharpoor S, Heydarirad H, Daryadel SJ, Heydari F, Ghamari Givi H, Kishore J. The role of perceived stress and social support among predicting anxiety in pregnant women. J Holistic Nurs Midwifery. 2017; 27(2):9-16. [DOI:10.18869/acadpub.hnmj.27.2.9]
- Peter PJ, de Mola CL, de Matos MB, Coelho FM, Pinheiro KA, da Silva RA, et al. Association between perceived social support and anxiety in pregnant adolescents. Braz J Psychiatry. 2016; 39:21-7. [DOI:10.1590/1516-4446-2015-1806]
- Neisani Samani L, Chereh H, Seted Fatemi N, Hosseini F, Karmelahi Z. [Relationship between perceived social support and Anxiety in Pregnant Women Conceived through Assisted Reproductive Technologies (ARTs) (Persian)]. Iran J Nurs. 2016; 29(103):51-9. [DOI:10.29252/ijn.29.103.51]
- Agostini F, Neri E, Salvatori P, Dellabartola S, Bozicevic L, Monti F. Antenatal depressive symptoms associated with specific life events and sources of social support among Italian women. Matern Child Health J. 2015; 19(5):1131-41. [DOI:10.1007/s10995-014-1613-x]
- Spielberger CD, Gorsuch RL. Manual for the State-trait Anxiety Inventory (form Y) (“self-evaluation Questionnaire”). California: Consulting Psychologists Press; 1983. [Link]
- Mahram B. [Standardization of spielberger anxiety test in Mashhad (Persian)] [MA thesis]. Mashhad: Allameh Tabataba’i University; 1994.
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988; 52(1):30-41. [DOI:10.1207/s15327752jpa5201_2]
- Bagherian-Sararoudi R, Hajian A, Ehsan HB, Sarafraz MR, Zimet GD. Psychometric properties of the Persian version of the multidimensional scale of perceived social support in Iran. Int J Prev Med. 2013; 4(11):1277-82. [PMID]
- Chen SL, Chang SM, Kuo PL, Chen CH. Stress, anxiety and depression perceived by couples with recurrent miscarriage. Int J Nurs Pract. 2020; 26(2):e12796. [DOI:10.1111/ijn.12796]
- Qu J, Weng XL, Gao LL. Anxiety, depression and social support across pregnancy in women with a history of recurrent miscarriage: A prospective study. Int J Nurs Pract. 2021; 27(5):e12997. [DOI:10.1111/ijn.12997]
- Kolte AM, Olsen LR, Christiansen OB, Schmidt L, Nielsen HS. Pregnancy outcomes after recurrent pregnancy loss: a longitudinal cohort study on stress and depression. Reprod Biomed Online. 2019; 38(4):599-605. [DOI:10.1016/j.rbmo.2018.12.006]
- Tahmasebi H, Hasani S, Akbarzadeh H, Darvishi H. [Trait anxiety and state anxiety before coronary angiography (Persian)]. Fam Health. 2012. 1(1):41-6. [Link]
- Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord. 2016; 191:62-77. [DOI:10.1016/j.jad.2015.11.014] [PMID]
- Dagklis T, Tsakiridis I, Chouliara F, Mamopoulos A, Rousso D, Athanasiadis A, et al. Antenatal depression among women hospitalized due to threatened preterm labor in a high-risk pregnancy unit in Greece. J Matern Fetal Neonatal Med. 2018; 31(7):919-25. [DOI:10.1080/14767058.2017.1301926] [PMID]
- Iranifard E, Akbari N, Montazeri A. [Perceived social support and pregnancy outcomes in vulnerable women (Persian)]. Payesh. 2019; 18(5):517-24. [Link]
- Sadeghi AS, Moosavi Sahebalzamani SS, Jahdi F, Neisani Samani I, Haghani H. [Relationship between perceived social support in first pregnancy with birth satisfaction in primigravid women referred to Shahid Akbar Abadi Hospital (Persian)]. Prev Care Nurs Midwifery J. 2014; 4(1):54-64. [Link]
- Furtado M, Chow CH, Owais S, Frey BN, Van Lieshout RJ. Risk factors of new onset anxiety and anxiety exacerbation in the perinatal period: A systematic review and meta-analysis. J Affect Disord. 2018; 238:626-35. [DOI:10.1016/j.jad.2018.05.073]
- Glazier RH, Elgar FJ, Goel V, Holzapfel S. Stress, social support, and emotional distress in a community sample of pregnant women. J Psychosom Obstet Gynecol. 2004; 25(3-4):247-55. [DOI:10.1080/01674820400024406]
Article Type : Research |
Subject:
Special
Received: 2023/04/18 | Accepted: 2024/03/11 | Published: 2024/10/1
Received: 2023/04/18 | Accepted: 2024/03/11 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |