Mon, Dec 1, 2025
Volume 35, Issue 1 (1-2025)
JHNM 2025, 35(1): 27-34 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abdi A, Rahmani S, Rahmati M. Judgmental Care Contexts in Emergency Departments: A Qualitative Study in Iran. JHNM 2025; 35 (1) :27-34
URL: http://hnmj.gums.ac.ir/article-1-2114-en.html
URL: http://hnmj.gums.ac.ir/article-1-2114-en.html
1- Professor of Nursing Education, Department of Emergency and Critical Care Nursing, School of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran.
2- Master of Emergency Nursing, Student Research Committee, School of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran. ,shamsodin97rahmani@gmail.com
3- Psychiatric Nursing Instructors, Department of Psychiatric Nursing, School of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran.
2- Master of Emergency Nursing, Student Research Committee, School of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran. ,
3- Psychiatric Nursing Instructors, Department of Psychiatric Nursing, School of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran.
Full-Text [PDF 483 kb]
(287 Downloads)
| Abstract (HTML) (707 Views)
Full-Text: (198 Views)
Introduction
Judgment refers to the assessment of actions based on certain values, rules, moral principles and preferences [1], and is a hidden process that can result from logical or intuitive thoughts [2]. A functional imaging study has shown that the frontal lobe of the brain in humans is responsible for judgment [3]. In nurses, providing non-judgmental care (NJC) is an important mission. Comprehensive and NJC can help improve patients’ well-being and physical and mental health [4]. Clinical judgment by nurses can have physical and psychological consequences [5]. Judgmental care (JC) and bias can be intensified or reduced under the influence of factors related to the nurse, the patient and the work environment. In a clinical environment, some labels and stereotypes can force health professionals to presuppose the values, ethics, and beliefs of their patients, which can affect their clinical decision-making [6]. The disrespectful behaviors of patients can cause JC [4]. People with higher social status who are more aware of their rights are less judged in a clinical environment [7]. Furthermore, limited equipment and improper allocation of resources can cause nurses to make unfair decisions and can affect their moral judgments [8]. Judgment affects nursing care [9]. The judgment of patients causes them to be neglected and psychologically damaged, which induces a lack of trust in medical personnel and patient dissatisfaction [7, 10].
Considering that NJC is affected by cultural issues, it should emanate from people’s subjective experiences. Also, to our knowledge, there is a lack of information about the effect of NJC on patients` clinical outcomes in emergency departments (EDs). In this regard, we used descriptive phenomenology as a qualitative research approach [11] to find the factors affecting the JC by ED nurses in Iran.
Materials and Methods
This is a qualitative study using a descriptive phenomenological approach. The participants were 14 nurses working in the EDs of hospitals in Kermanshah, Iran. Sampling was done purposefully, until data saturation was reached through interviews [12]. The inclusion criteria were willingness to participate in the study and a history of providing JC to patients (based on self-report).
After obtaining the necessary permits, explaining the study objectives to the participants, and obtaining their written informed consent, semi-structured face-to-face interviews were conducted to collect data.
The interviews were conducted at a time and place convenient to participants and the interviewers. The interview started using open-ended questions such as: “What is your experience of JC?” and “In your opinion, what are the factors affecting JC?” and probing questions such as “Can you explain more?” or “Can you give an example ?” Notes were taken during interviews and the conversations were recorded with the consent of the participants.
The collected data were analyzed based on Colaizzi’s approach, which included seven steps: 1) Familiarization with the data, 2) Identification of significant statements, 3) Formulation of meaning, 4) Grouping the identifying meaning into themes, 5) Developing an exhaustive description of the phenomenon based on themes, 6) Identifying the fundamental structure of phenomena and 7) Verifying the findings.
The trustworthiness of the data was determined based on the four criteria of credibility, transferability, dependability, and confirmability [13]. The researcher who works in an ED tried to have a long-term engagement with the phenomenon and participants’ statements. The interviews, data coding, and analysis were done by the researcher and his co-workers (peer checking) and reviewed by participants (member checking). The researcher tried to choose participants with various ages, genders and backgrounds. A detailed description of the steps and how to collect and analyze data was used, which would be audited by external observers. The researcher tried to avoid personal biases in the research by writing down his thoughts and setting them aside.
Results
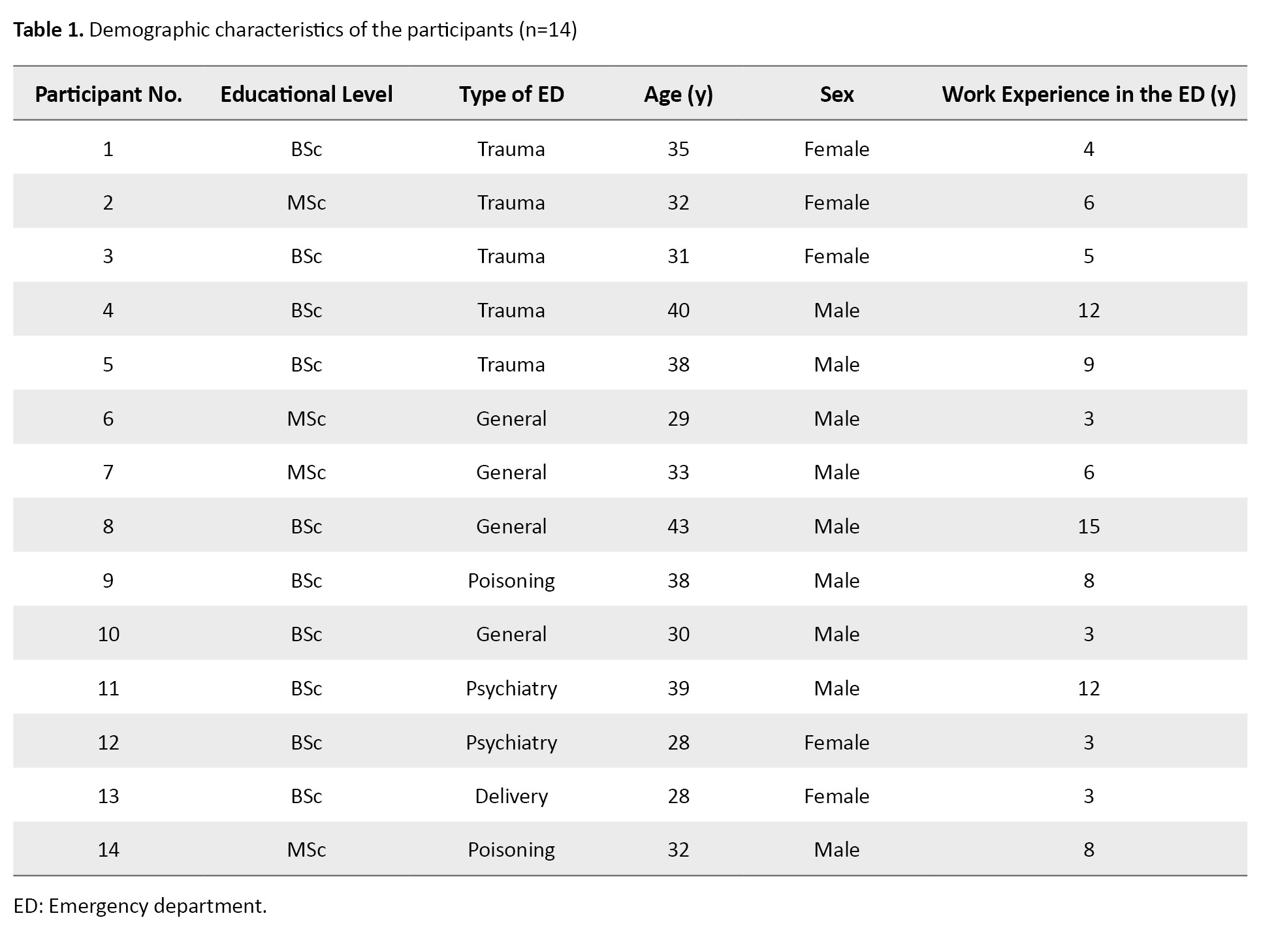
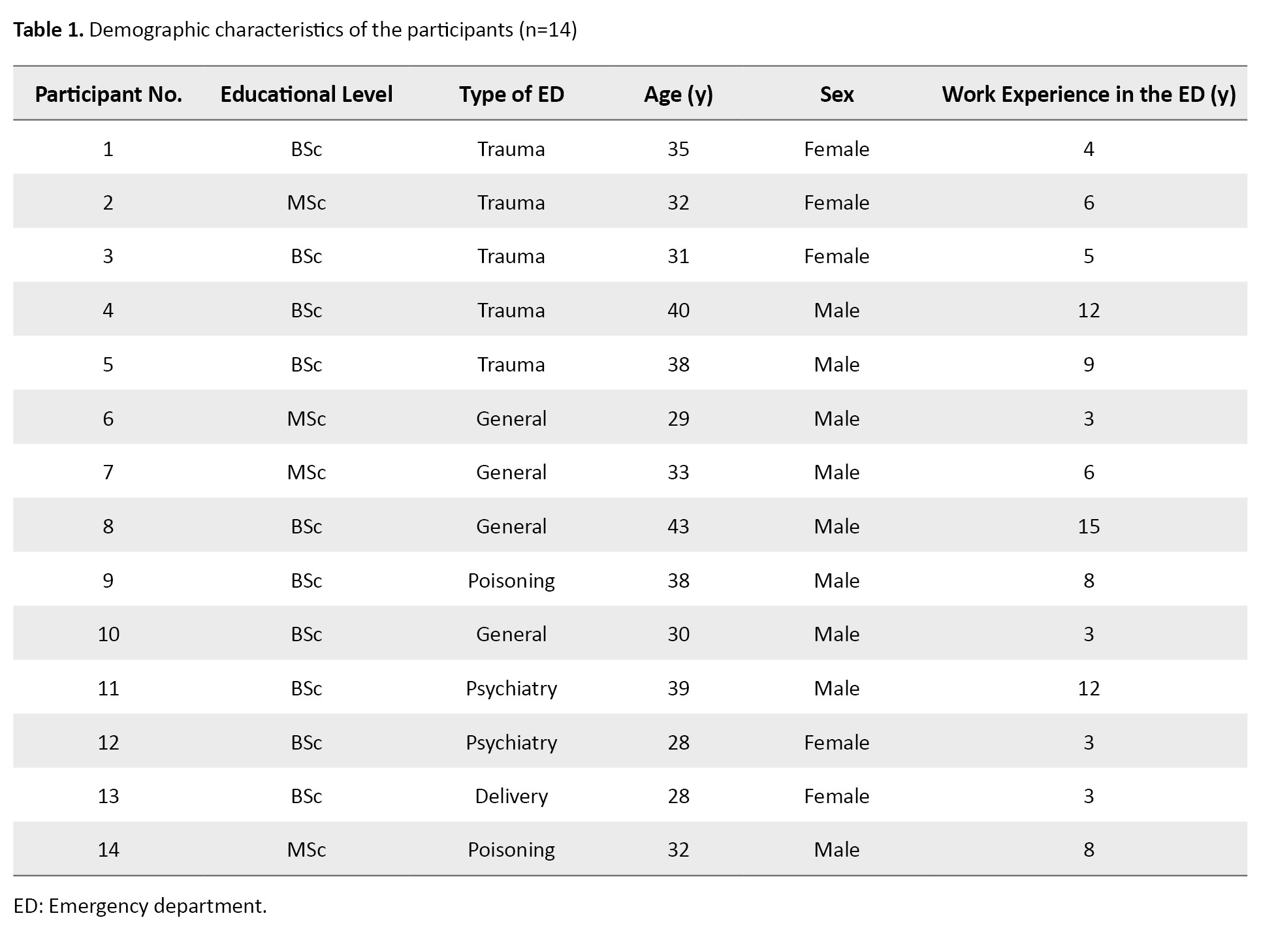
In this study, 14 nurses participated; 9 were males and 7 were single. Table 1 shows the demographic characteristics of each participant.
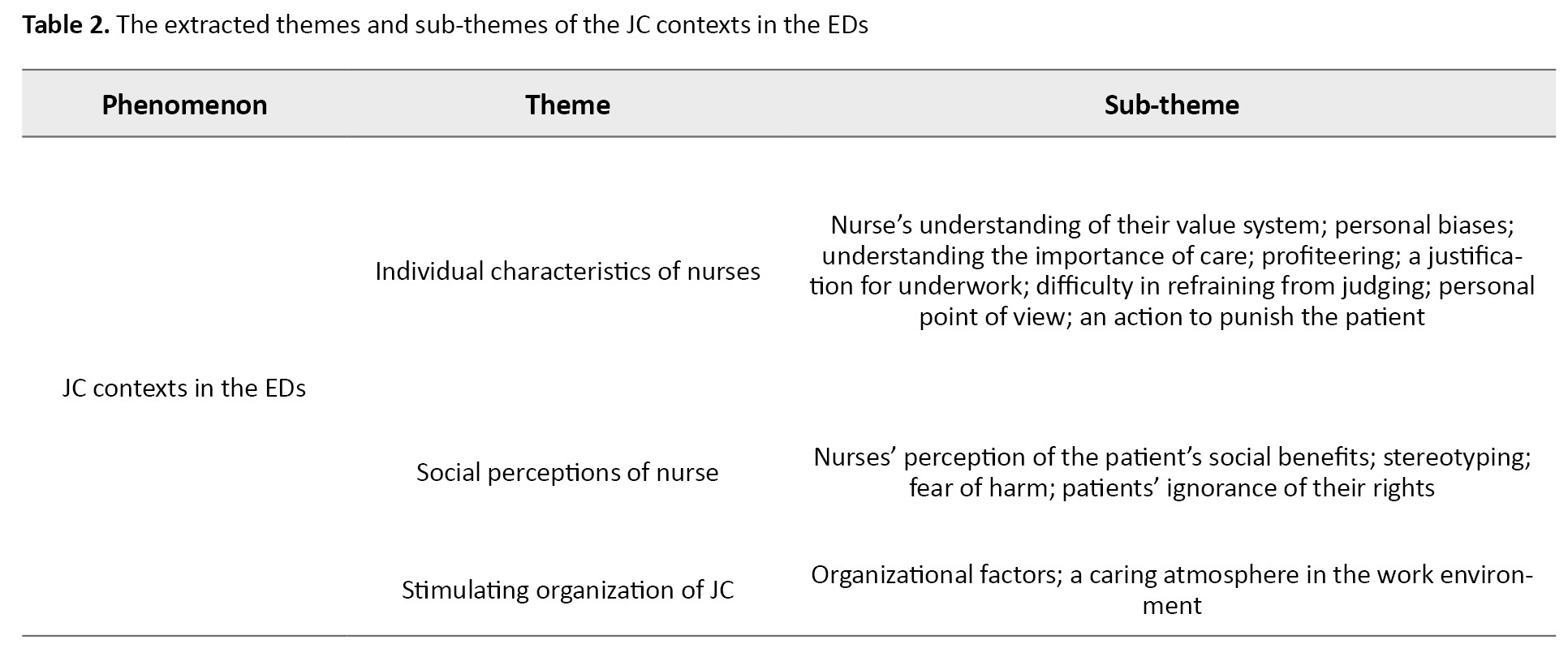
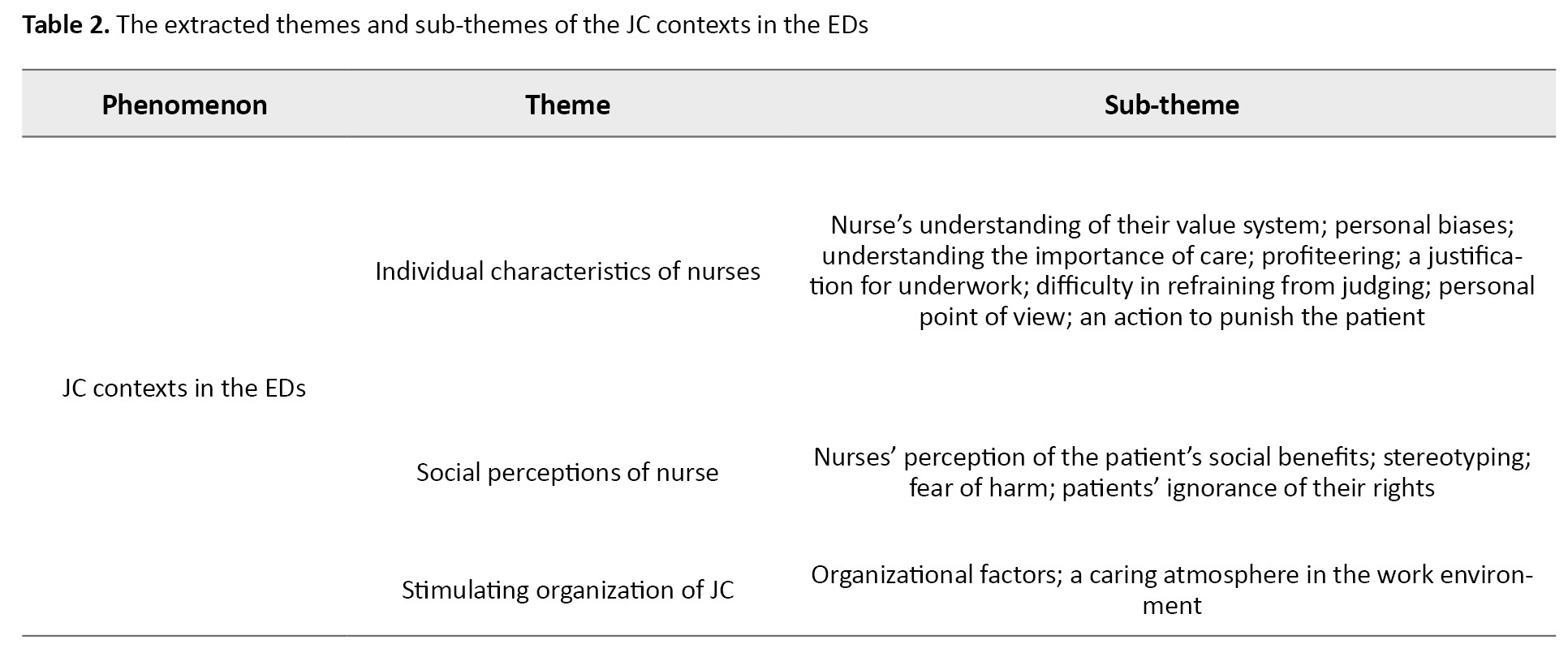
By continuously analyzing the interviews about nurses’ JC experiences, 346 codes, 14 sub-themes and three main themes were extracted (Table 2).
Individual characteristics of nurses
One of the main themes was the “individual characteristics of the nurses”, noted by all 14 participants and had eight subthemes.
Nurses’ understanding of their value system
It was found that the religious beliefs, care habits, experience, and patience of the nurse were effective in providing NJC. Participant No.6 stated: “Well, a person who believes in Allah does not care what happens. She/he [the patient] is a human and I must take care of him/her.” The participants found the effect of previous experience on providing NJC was positive. Participant No.1 said, “The more experience you have, the better you can treat patients non-judgmentally.”
Personal biases
Sometimes, personal experiences and opinions intensify JC and may cause nurses to decide based on personal experiences and biases in patient care. Participant No.1 stated: “I hate Iraqis because of having eight years of war with them! My uncle was martyred [during the war]. It was very difficult for me to take care of them”. Also, participant No. 3 said: “One day, when my daughter was at the hospital, I expected the nurse to treat her well and patiently take care of her. When we had a sick child [in the hospital], I remembered that day. I took care of the child very well and patiently and believed that the child’s mother expected me the same.”
Understanding the importance of care
One of the most important factors influencing JC, as mentioned by all participants, was the nurses’ understanding of the importance of the provided care as well as the clinical conditions and the conditions after the patient’s recovery. Nurses try to provide complete care to patients in critical condition and at high risk despite judging them. However, when the importance of care decreases or the patient’s condition becomes stable, they can easily have JC and cope with reduced patient care. Participant No. 13 said: “In pregnant mothers, since the situation is sensitive and there is high supervision over pregnant mothers, we are less likely to judge or not to do something.” Nurses may not provide care that is less important in their opinions or that is not in the best interest of the patient or society. “When code 99 is called for an incurable patient, we don’t hesitate long; if he [the patient] survives, he will suffer more” (Participant No. 3).
Profiteering
Nurses take care of some patients more than usual because of their interests. This unusual care can be for the benefit of a particular person or for the fear of being reprimanded by a supervisor. Participant No. 5 said: “I saw a colleague gave his phone number to the patient who needed care at home, but he (the nurse) didn’t tell others (other patients) what to do after discharge and even didn’t ask if they had any question.” Participant No. 1 said, “One day, we had a patient in the CPR room. After one hour, when we found out that he was the deputy governor, we all rushed to the room so that the patient’s work could be done sooner. For other patient who had been neglected, the work was done immediately and was sent to the ICU.”
A justification for underwork
The JC is sometimes a justification for the underwork, and nurses justify themselves by judging the patient, which is more related to nurses who are negligent in performing their other duties. Participant No. 10 stated: “Sometimes the staff is really lazy in treating the patients and they justify themselves by judging (the patients)”. Participant No. 7 also stated: “We should not be affected by the ward atmosphere. For example, if we say that there is no cure for pancreatic cancer, what will happen after we inject the albumin (for the survival of the patient) and have to inform the homeless patient (who does not have a good life) that he is going to stay alive? these are what you (nurse) use to justify your underwork.”
Difficulty in refraining from judging
According to the participants, controlling the effect of judgment on patient care was difficult or sometimes impossible. Some participants also considered it unfair to provide NJC to some patients. Participant No. 8 said, “Sometimes it JC is done unintentionally! you may not even realize that your judgment has affected you!” Sometimes, nurses find NJC not only harsh but also unfair.
Personal point of view
The perspective or character of nurses is another effective factor in JC. Some nurses are not judgmental in their personal lives and take this characteristic to the workplace. Some nurses are more sensitive to social issues or pay more attention to details, which can intensify JC. Participant No. 8 stated: “The character of a person is important! Nurses who are more emotional and pay more attention to details are more judgmental than cool-headed and calm nurses”. Participant No. 8 also said: “(To work non-judgmentally), it is essential to adopt a comprehensive attitude (allowing for suspending personal biases). If you consider your personal biases, you may bring and integrate them into your practice”. Participant No. 1 stated: “I am not a judge. My job is something else! I am not supposed to punish or reward the patient”.
An action to punish the patient
The participants stated that sometimes, depending on the patient’s behavior and the reason for admission (e.g. suicide or hysteria), the nurse deliberately performs more painful procedures so that the patient does not repeat those actions. Participant No. 6 said: “For patients with suicide attempts to seek attention, we may opt to use a larger nasogastric tube as a deterrent to prevent future incidents”. Sometimes, this punishment was for relieving anger or emotional relief. “If the patient’s life is in danger, we should do something without judgment, but for the case whose care is not acute, e.g. the patient with a stitch, we have to remove it by applying force [bothering the patient] which causes a psychological relief in me” (Participant No. 4).
Social perceptions of nurses
The second main theme was the “social perception of the nurses”, which had four subthemes. The cultural and social factors of the society in which the nurse was educated or trained affect the provision of JC by nurses. The nurse’s judgment less affects the care for patients with higher social status or who are aware of their rights. Also, when providing JC, the nurse considers the patient’s benefits or harms to society.
Patients’ ignorance of their rights
The more ignorant the patients are about their rights, or the more they are not accompanied by a person or followed by an organization, the easier it is for the nurse to ignore them and influence his/her judgment in the care. Participant No. 9 stated, “For the patients who are accompanied (by family or friend), less JC is provided because they see they have a companion and follow-up the patient’s treatment”. However, for patients who do not have a companion or who have an uninformed companion, the nurse is less afraid of providing JC.
Nurses’ perception of the patient’s social benefit
Nurses may be saddened by the death of patients who, based on their perceptions, have more social benefits and thus show more compassion to them. Therefore, they make more efforts to take care of them. Moreover, nurses with age discrimination were more upset about the death of a young patient than an elderly patient. Participant No. 1 argued: “We had a patient who was an elite student. he had committed suicide and all the staff were sad about it. I tried to help him more. I took care of him by being at his bedside more often”. Participant No. 9 stated: “When we were in a CPR room, we had a patient who was a doctor! There was also a homeless addict patient. We spend more time to take care of the doctor. This patient was more useful to society! He was my coworker.” Nurses consider young patients more useful and give them better care.
Stereotyping
According to the nurses’ experiences, nurses judged some patients under the influence of cultural norms. Participant No. 5 said, “When a patient is handcuffed, he is the first person who is judged. The nurse may think that the patient has a viral disease or is a bad person“. Participant No. 6 stated: “We see some fight-related patients show violent behavior and say curses and bad words! We perceive that all fight-related patients have the same behaviors.”
Fear of harm
Depending on the patient’s appearance and whether she/he is homeless or imprisoned, nurses may perceive that the patient may have a viral disease or be aggressive. As a result, they may have less communication with them and take less time to take care of them. They prefer to stay away from the risk of contracting infectious or viral diseases. Participant No. 6 stated that nurses try not to accept patients suspected or infected with viral diseases: “I see my colleagues that refuse to accept patients with a viral disease and try to run away from them and pass them to other nurses.”
Stimulating organization of JC
Sometimes, the conditions governing the work environment, such as crowdedness, high workload, lack of supervision, low salaries and benefits and the caring atmosphere pave the way for JC.
The caring atmosphere of the work environment
In case of the existence of a caring atmosphere in the EDs and a non-judgmental culture among the personnel, the new personnel will also tend towards NJC. Participant No. 9 said: “Judgement is related to culture! when the prevailing culture of the society or colleagues is less judgmental, it affects the rest.” Another effective factor was the type of patients or frequency of encountering patients such as psychiatric or poisoned patients. Participant No. 8 stated: “In the emergency management of poisoned cases, we encounter patients with drug or alcohol overdose. Thus, when we deal with these patients, we should judge.”
Organizational factors
Organizational factors, including supervision, salaries and benefits, training, wards’ crowdedness, and nurses’ fatigue, are effective in nurses’ JC. Participant No. 6 said: “When a homeless patient was admitted, and I was not busy, and it (the ward) was quiet, I did everything (for the patient); but when I was busy, I paid less attention to the patient! The time you (nurse) spend depends on your workload and energy.” The staff training was also very effective in providing NJC. Participant No. 11 said: “Here (in the hospital), the psychiatric nurses provide training and briefing classes for the nurses. It is very effective. For example, we learned that we should treat all patients equally and understand them if they did something wrong.” Supervision, either internally by supervisors or the patients’ companion or externally by another organization, was also reported to be effective in controlling the effect of judgment on the care.
Discussion
In this study, it was discovered that the perspectives, characters, and experiences of the ED nurses had an impact on JC. Nurses with higher religious beliefs are less likely to ignore the care for the patient they have judged due to the fear of retribution in the afterlife. Moreover, experienced nurses judge patients less. Spiritual beliefs can improve the quality of patient care [14]. Nurses’ emotional experiences and patience can improve their normalizing practice and provided care [15].
Some nurses provided better care to the family members, relatives, coworkers, or the patients with a same ethnicity (personal bias). A mindfulness practice can reduce the effect of clinical biases on patient care [16]. Some nurses with a character that is less inclined to judge people had less JC issues in their workplace and focused on their tasks. Ellershaw et al. [17] and Dapaah [18] also stated that nurses’ personality traits such as extroversion as well as their attitudes and perspectives are effective in nursing work.
Understanding the importance of care was another identified factor. Some nurses tried to provide full care to patients in critical condition despite judging them. Suhonen et al. also reported that the prioritization of nursing care is based on the importance of the patient’s condition and needs [8]. Ghanbari et al. also suggested that medical need is the most important factor in patient prioritization [19].
The difficulty in refraining from judging was another factor. Some nurses perceived that it is unfair to deliver NJC to some patients such as rapists and murderers. It has been stated that impartiality is very difficult and each person has his/her own experiences and attitudes [20]. In this study, nurses were more upset after the death of patients who had more social benefits, such as athletes, elite people, and young people, and made more efforts to treat them. In a study by Skirbekk and Nortvedt, nurses were also more upset about the death of younger patients than elderly patients, and used more facilities and spent more energy to treat them [21].
For patients with a lack of awareness of their rights or who do not have a companion and coverage by an organization, ED nurses were more likely to have JC without the fear of consequences. In a study, nurses declared that patients’ awareness of their rights and their active participation in self-care improve the quality of care [22, 23].
Organizational factors can also facilitate JC. The hospitals, by not supervising the behavior of nurses, not allocating the personnel based on the workload in the ED, and not paying proper salaries and benefits to the nurses, can provide a context for JC. Studies have shown that the lack of respect for the basic rights of nurses and the crowdedness of the EDs can reduce patient care quality [24, 25]. A caring atmosphere in the work environment is another organizational factor. In the case of an NJC atmosphere in the ED, the nurses will have less JC, but if the atmosphere is a whole of moral judgment, it will affect the nurses. A positive intergroup interaction can reduce implicit bias during care [26]. In a professional practice environment, missed nursing care can be reduced by improving staff relationships, teamwork, and cultural sensitivity [27].
The reluctance of some nurses to express all their experiences due to the fear of disclosure and not answering some questions were among the limitations of this study. To reduce these problems, the researcher tried to establish proper communication by providing the necessary explanations and ensuring that their information would be kept confidential.
Overall, it can be concluded that JC in the EDs is affected by the individual characteristics of nurses, the conditions of the hospital, and the social perceptions of nurses regarding the patients’ social benefits or harms, stereotyped behaviors, social status and awareness of their rights. The hospitals can reduce the possibility of JC in the EDs by providing financial incentives for nurses, proper allocation of personnel based on the workload, recruiting experienced and committed nurses to work in the ED, and training personnel about JC, as well as defining legal implications for JC, and monitoring the stigmatized patients. Further studies should be conducted on the impact of individual, social, or organizational factors on JC in hospitals.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of Kermanshah University of Medical Sciences, Kermanshah, Iran (Code: IR.KUMS.REC.1399.473). All methods were in accordance with the guidelines and regulations of the Declaration of Helsinki. Written informed consent was obtained from all participants before the interviews.
Funding
This article was extracted from a master’s thesis, approved by the Research and Technology Deputy of Kermanshah University of Medical Sciences, Kermanshah, Iran. This study was financially supported by Kermanshah University of Medical Sciences, Kermanshah, Iran.
Authors' contributions
Study design, writing, review and editing: Shamsodin Rahmani and Alireza Abdi; Data collection: Shamsodin Rahmani; Data analysis and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the nurses from the EDs of selected hospitals in Kermanshah for their cooperation and the Vice-Chancellor for Research and Technology of Kermanshah University of Medical Sciences Kermanshah, Iran for the financial support.
Judgment refers to the assessment of actions based on certain values, rules, moral principles and preferences [1], and is a hidden process that can result from logical or intuitive thoughts [2]. A functional imaging study has shown that the frontal lobe of the brain in humans is responsible for judgment [3]. In nurses, providing non-judgmental care (NJC) is an important mission. Comprehensive and NJC can help improve patients’ well-being and physical and mental health [4]. Clinical judgment by nurses can have physical and psychological consequences [5]. Judgmental care (JC) and bias can be intensified or reduced under the influence of factors related to the nurse, the patient and the work environment. In a clinical environment, some labels and stereotypes can force health professionals to presuppose the values, ethics, and beliefs of their patients, which can affect their clinical decision-making [6]. The disrespectful behaviors of patients can cause JC [4]. People with higher social status who are more aware of their rights are less judged in a clinical environment [7]. Furthermore, limited equipment and improper allocation of resources can cause nurses to make unfair decisions and can affect their moral judgments [8]. Judgment affects nursing care [9]. The judgment of patients causes them to be neglected and psychologically damaged, which induces a lack of trust in medical personnel and patient dissatisfaction [7, 10].
Considering that NJC is affected by cultural issues, it should emanate from people’s subjective experiences. Also, to our knowledge, there is a lack of information about the effect of NJC on patients` clinical outcomes in emergency departments (EDs). In this regard, we used descriptive phenomenology as a qualitative research approach [11] to find the factors affecting the JC by ED nurses in Iran.
Materials and Methods
This is a qualitative study using a descriptive phenomenological approach. The participants were 14 nurses working in the EDs of hospitals in Kermanshah, Iran. Sampling was done purposefully, until data saturation was reached through interviews [12]. The inclusion criteria were willingness to participate in the study and a history of providing JC to patients (based on self-report).
After obtaining the necessary permits, explaining the study objectives to the participants, and obtaining their written informed consent, semi-structured face-to-face interviews were conducted to collect data.
The interviews were conducted at a time and place convenient to participants and the interviewers. The interview started using open-ended questions such as: “What is your experience of JC?” and “In your opinion, what are the factors affecting JC?” and probing questions such as “Can you explain more?” or “Can you give an example ?” Notes were taken during interviews and the conversations were recorded with the consent of the participants.
The collected data were analyzed based on Colaizzi’s approach, which included seven steps: 1) Familiarization with the data, 2) Identification of significant statements, 3) Formulation of meaning, 4) Grouping the identifying meaning into themes, 5) Developing an exhaustive description of the phenomenon based on themes, 6) Identifying the fundamental structure of phenomena and 7) Verifying the findings.
The trustworthiness of the data was determined based on the four criteria of credibility, transferability, dependability, and confirmability [13]. The researcher who works in an ED tried to have a long-term engagement with the phenomenon and participants’ statements. The interviews, data coding, and analysis were done by the researcher and his co-workers (peer checking) and reviewed by participants (member checking). The researcher tried to choose participants with various ages, genders and backgrounds. A detailed description of the steps and how to collect and analyze data was used, which would be audited by external observers. The researcher tried to avoid personal biases in the research by writing down his thoughts and setting them aside.
Results
In this study, 14 nurses participated; 9 were males and 7 were single. Table 1 shows the demographic characteristics of each participant.
By continuously analyzing the interviews about nurses’ JC experiences, 346 codes, 14 sub-themes and three main themes were extracted (Table 2).
Individual characteristics of nurses
One of the main themes was the “individual characteristics of the nurses”, noted by all 14 participants and had eight subthemes.
Nurses’ understanding of their value system
It was found that the religious beliefs, care habits, experience, and patience of the nurse were effective in providing NJC. Participant No.6 stated: “Well, a person who believes in Allah does not care what happens. She/he [the patient] is a human and I must take care of him/her.” The participants found the effect of previous experience on providing NJC was positive. Participant No.1 said, “The more experience you have, the better you can treat patients non-judgmentally.”
Personal biases
Sometimes, personal experiences and opinions intensify JC and may cause nurses to decide based on personal experiences and biases in patient care. Participant No.1 stated: “I hate Iraqis because of having eight years of war with them! My uncle was martyred [during the war]. It was very difficult for me to take care of them”. Also, participant No. 3 said: “One day, when my daughter was at the hospital, I expected the nurse to treat her well and patiently take care of her. When we had a sick child [in the hospital], I remembered that day. I took care of the child very well and patiently and believed that the child’s mother expected me the same.”
Understanding the importance of care
One of the most important factors influencing JC, as mentioned by all participants, was the nurses’ understanding of the importance of the provided care as well as the clinical conditions and the conditions after the patient’s recovery. Nurses try to provide complete care to patients in critical condition and at high risk despite judging them. However, when the importance of care decreases or the patient’s condition becomes stable, they can easily have JC and cope with reduced patient care. Participant No. 13 said: “In pregnant mothers, since the situation is sensitive and there is high supervision over pregnant mothers, we are less likely to judge or not to do something.” Nurses may not provide care that is less important in their opinions or that is not in the best interest of the patient or society. “When code 99 is called for an incurable patient, we don’t hesitate long; if he [the patient] survives, he will suffer more” (Participant No. 3).
Profiteering
Nurses take care of some patients more than usual because of their interests. This unusual care can be for the benefit of a particular person or for the fear of being reprimanded by a supervisor. Participant No. 5 said: “I saw a colleague gave his phone number to the patient who needed care at home, but he (the nurse) didn’t tell others (other patients) what to do after discharge and even didn’t ask if they had any question.” Participant No. 1 said, “One day, we had a patient in the CPR room. After one hour, when we found out that he was the deputy governor, we all rushed to the room so that the patient’s work could be done sooner. For other patient who had been neglected, the work was done immediately and was sent to the ICU.”
A justification for underwork
The JC is sometimes a justification for the underwork, and nurses justify themselves by judging the patient, which is more related to nurses who are negligent in performing their other duties. Participant No. 10 stated: “Sometimes the staff is really lazy in treating the patients and they justify themselves by judging (the patients)”. Participant No. 7 also stated: “We should not be affected by the ward atmosphere. For example, if we say that there is no cure for pancreatic cancer, what will happen after we inject the albumin (for the survival of the patient) and have to inform the homeless patient (who does not have a good life) that he is going to stay alive? these are what you (nurse) use to justify your underwork.”
Difficulty in refraining from judging
According to the participants, controlling the effect of judgment on patient care was difficult or sometimes impossible. Some participants also considered it unfair to provide NJC to some patients. Participant No. 8 said, “Sometimes it JC is done unintentionally! you may not even realize that your judgment has affected you!” Sometimes, nurses find NJC not only harsh but also unfair.
Personal point of view
The perspective or character of nurses is another effective factor in JC. Some nurses are not judgmental in their personal lives and take this characteristic to the workplace. Some nurses are more sensitive to social issues or pay more attention to details, which can intensify JC. Participant No. 8 stated: “The character of a person is important! Nurses who are more emotional and pay more attention to details are more judgmental than cool-headed and calm nurses”. Participant No. 8 also said: “(To work non-judgmentally), it is essential to adopt a comprehensive attitude (allowing for suspending personal biases). If you consider your personal biases, you may bring and integrate them into your practice”. Participant No. 1 stated: “I am not a judge. My job is something else! I am not supposed to punish or reward the patient”.
An action to punish the patient
The participants stated that sometimes, depending on the patient’s behavior and the reason for admission (e.g. suicide or hysteria), the nurse deliberately performs more painful procedures so that the patient does not repeat those actions. Participant No. 6 said: “For patients with suicide attempts to seek attention, we may opt to use a larger nasogastric tube as a deterrent to prevent future incidents”. Sometimes, this punishment was for relieving anger or emotional relief. “If the patient’s life is in danger, we should do something without judgment, but for the case whose care is not acute, e.g. the patient with a stitch, we have to remove it by applying force [bothering the patient] which causes a psychological relief in me” (Participant No. 4).
Social perceptions of nurses
The second main theme was the “social perception of the nurses”, which had four subthemes. The cultural and social factors of the society in which the nurse was educated or trained affect the provision of JC by nurses. The nurse’s judgment less affects the care for patients with higher social status or who are aware of their rights. Also, when providing JC, the nurse considers the patient’s benefits or harms to society.
Patients’ ignorance of their rights
The more ignorant the patients are about their rights, or the more they are not accompanied by a person or followed by an organization, the easier it is for the nurse to ignore them and influence his/her judgment in the care. Participant No. 9 stated, “For the patients who are accompanied (by family or friend), less JC is provided because they see they have a companion and follow-up the patient’s treatment”. However, for patients who do not have a companion or who have an uninformed companion, the nurse is less afraid of providing JC.
Nurses’ perception of the patient’s social benefit
Nurses may be saddened by the death of patients who, based on their perceptions, have more social benefits and thus show more compassion to them. Therefore, they make more efforts to take care of them. Moreover, nurses with age discrimination were more upset about the death of a young patient than an elderly patient. Participant No. 1 argued: “We had a patient who was an elite student. he had committed suicide and all the staff were sad about it. I tried to help him more. I took care of him by being at his bedside more often”. Participant No. 9 stated: “When we were in a CPR room, we had a patient who was a doctor! There was also a homeless addict patient. We spend more time to take care of the doctor. This patient was more useful to society! He was my coworker.” Nurses consider young patients more useful and give them better care.
Stereotyping
According to the nurses’ experiences, nurses judged some patients under the influence of cultural norms. Participant No. 5 said, “When a patient is handcuffed, he is the first person who is judged. The nurse may think that the patient has a viral disease or is a bad person“. Participant No. 6 stated: “We see some fight-related patients show violent behavior and say curses and bad words! We perceive that all fight-related patients have the same behaviors.”
Fear of harm
Depending on the patient’s appearance and whether she/he is homeless or imprisoned, nurses may perceive that the patient may have a viral disease or be aggressive. As a result, they may have less communication with them and take less time to take care of them. They prefer to stay away from the risk of contracting infectious or viral diseases. Participant No. 6 stated that nurses try not to accept patients suspected or infected with viral diseases: “I see my colleagues that refuse to accept patients with a viral disease and try to run away from them and pass them to other nurses.”
Stimulating organization of JC
Sometimes, the conditions governing the work environment, such as crowdedness, high workload, lack of supervision, low salaries and benefits and the caring atmosphere pave the way for JC.
The caring atmosphere of the work environment
In case of the existence of a caring atmosphere in the EDs and a non-judgmental culture among the personnel, the new personnel will also tend towards NJC. Participant No. 9 said: “Judgement is related to culture! when the prevailing culture of the society or colleagues is less judgmental, it affects the rest.” Another effective factor was the type of patients or frequency of encountering patients such as psychiatric or poisoned patients. Participant No. 8 stated: “In the emergency management of poisoned cases, we encounter patients with drug or alcohol overdose. Thus, when we deal with these patients, we should judge.”
Organizational factors
Organizational factors, including supervision, salaries and benefits, training, wards’ crowdedness, and nurses’ fatigue, are effective in nurses’ JC. Participant No. 6 said: “When a homeless patient was admitted, and I was not busy, and it (the ward) was quiet, I did everything (for the patient); but when I was busy, I paid less attention to the patient! The time you (nurse) spend depends on your workload and energy.” The staff training was also very effective in providing NJC. Participant No. 11 said: “Here (in the hospital), the psychiatric nurses provide training and briefing classes for the nurses. It is very effective. For example, we learned that we should treat all patients equally and understand them if they did something wrong.” Supervision, either internally by supervisors or the patients’ companion or externally by another organization, was also reported to be effective in controlling the effect of judgment on the care.
Discussion
In this study, it was discovered that the perspectives, characters, and experiences of the ED nurses had an impact on JC. Nurses with higher religious beliefs are less likely to ignore the care for the patient they have judged due to the fear of retribution in the afterlife. Moreover, experienced nurses judge patients less. Spiritual beliefs can improve the quality of patient care [14]. Nurses’ emotional experiences and patience can improve their normalizing practice and provided care [15].
Some nurses provided better care to the family members, relatives, coworkers, or the patients with a same ethnicity (personal bias). A mindfulness practice can reduce the effect of clinical biases on patient care [16]. Some nurses with a character that is less inclined to judge people had less JC issues in their workplace and focused on their tasks. Ellershaw et al. [17] and Dapaah [18] also stated that nurses’ personality traits such as extroversion as well as their attitudes and perspectives are effective in nursing work.
Understanding the importance of care was another identified factor. Some nurses tried to provide full care to patients in critical condition despite judging them. Suhonen et al. also reported that the prioritization of nursing care is based on the importance of the patient’s condition and needs [8]. Ghanbari et al. also suggested that medical need is the most important factor in patient prioritization [19].
The difficulty in refraining from judging was another factor. Some nurses perceived that it is unfair to deliver NJC to some patients such as rapists and murderers. It has been stated that impartiality is very difficult and each person has his/her own experiences and attitudes [20]. In this study, nurses were more upset after the death of patients who had more social benefits, such as athletes, elite people, and young people, and made more efforts to treat them. In a study by Skirbekk and Nortvedt, nurses were also more upset about the death of younger patients than elderly patients, and used more facilities and spent more energy to treat them [21].
For patients with a lack of awareness of their rights or who do not have a companion and coverage by an organization, ED nurses were more likely to have JC without the fear of consequences. In a study, nurses declared that patients’ awareness of their rights and their active participation in self-care improve the quality of care [22, 23].
Organizational factors can also facilitate JC. The hospitals, by not supervising the behavior of nurses, not allocating the personnel based on the workload in the ED, and not paying proper salaries and benefits to the nurses, can provide a context for JC. Studies have shown that the lack of respect for the basic rights of nurses and the crowdedness of the EDs can reduce patient care quality [24, 25]. A caring atmosphere in the work environment is another organizational factor. In the case of an NJC atmosphere in the ED, the nurses will have less JC, but if the atmosphere is a whole of moral judgment, it will affect the nurses. A positive intergroup interaction can reduce implicit bias during care [26]. In a professional practice environment, missed nursing care can be reduced by improving staff relationships, teamwork, and cultural sensitivity [27].
The reluctance of some nurses to express all their experiences due to the fear of disclosure and not answering some questions were among the limitations of this study. To reduce these problems, the researcher tried to establish proper communication by providing the necessary explanations and ensuring that their information would be kept confidential.
Overall, it can be concluded that JC in the EDs is affected by the individual characteristics of nurses, the conditions of the hospital, and the social perceptions of nurses regarding the patients’ social benefits or harms, stereotyped behaviors, social status and awareness of their rights. The hospitals can reduce the possibility of JC in the EDs by providing financial incentives for nurses, proper allocation of personnel based on the workload, recruiting experienced and committed nurses to work in the ED, and training personnel about JC, as well as defining legal implications for JC, and monitoring the stigmatized patients. Further studies should be conducted on the impact of individual, social, or organizational factors on JC in hospitals.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of Kermanshah University of Medical Sciences, Kermanshah, Iran (Code: IR.KUMS.REC.1399.473). All methods were in accordance with the guidelines and regulations of the Declaration of Helsinki. Written informed consent was obtained from all participants before the interviews.
Funding
This article was extracted from a master’s thesis, approved by the Research and Technology Deputy of Kermanshah University of Medical Sciences, Kermanshah, Iran. This study was financially supported by Kermanshah University of Medical Sciences, Kermanshah, Iran.
Authors' contributions
Study design, writing, review and editing: Shamsodin Rahmani and Alireza Abdi; Data collection: Shamsodin Rahmani; Data analysis and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the nurses from the EDs of selected hospitals in Kermanshah for their cooperation and the Vice-Chancellor for Research and Technology of Kermanshah University of Medical Sciences Kermanshah, Iran for the financial support.
References
- Cointe N, Bonnet G, Boissier O. Ethical judgment of Agents’ behaviors in multi-agent systems. AAMAS. 2016; 1106-14. [Link]
- Brooks V. Marking as judgment. Res Pap Educ. 2012; 27(1):63-80. [DOI:10.1080/02671520903331008]
- Schneider B, Koenigs M. Human lesion studies of ventromedial prefrontal cortex. Neuropsychologia. 2017; 107:84-93. [DOI:10.1016/j.neuropsychologia.2017.09.035] [PMID]
- Hill TE. How clinicians make (or avoid) moral judgments of patients: Implications of the evidence for relationships and research. Philos Ethics Humanit Med. 2010; 5:11. [DOI:10.1186/1747-5341-5-11] [PMID]
- Corley MC, Goren S. The dark side of nursing: Impact of stigmatizing responses on patients. Sch Inq Nurs Pract. 1998; 12(2):99-118; discussion 119-22. [PMID]
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: A systematic review. BMC Med Ethics. 2017; 18(1):19. [DOI:10.1186/s12910-017-0179-8] [PMID]
- Spencer KL, Grace M. Social foundations of health care inequality and treatment bias. Annu Rev Soc. 2016; 42(1):101-20. [DOI:10.1146/annurev-soc-081715-074226]
- Suhonen R, Stolt M, Habermann M, Hjaltadottir I, Vryonides S, Tonnessen S, et al. Ethical elements in priority setting in nursing care: A scoping review. Int J Nurs Stud. 2018; 88:25-42. [DOI:10.1016/j.ijnurstu.2018.08.006] [PMID]
- Lipp A. Conceding and concealing judgement in termination of pregnancy; a grounded theory study. J Res Nurs. 2010; 15(4):365-78. [DOI:10.1177/1744987109347031]
- Muiruri PN, Brewer G, Khan R. “If It Wasn’t for Ethics, I Wouldn’t Go Near Him: An interpretative phenomenological analysis of caring for patient-prisoners in Kenya. Int J Offender Ther Comp Criminol. 2019; 63(14):2440-52. [DOI:10.1177/0306624X19849556] [PMID]
- Gallagher S. What is phenomenology? In: Phenomenology. Palgrave Philosophy Today. Cham: Palgrave Macmillan; 2022. [DOI:10.1007/978-3-031-11586-8_1]
- Boddy CR. Sample size for qualitative research. Qual Mark Res. 2016; 19(4):426-32. [DOI:10.1108/QMR-06-2016-0053]
- Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf. 2004; 22(2):63-75. [DOI:10.3233/EFI-2004-22201]
- Ravari A, Vanaki Z, Houmann H, Kazemnejad A. Spiritual job satisfaction in an Iranian nursing context. Nurs Ethics. 2009; 16(1):19-30. [DOI:10.1177/0969733008097987] [PMID]
- Roitenberg N. Managing (im) patience of nurses and nurse’s aides: Emotional labour and normalizing practices at geriatric facilities. Sociol Health Illn. 2021; 43(4):995-1011. [DOI:10.1111/1467-9566.13281] [PMID]
- Burgess DJ, Beach MC, Saha S. Mindfulness practice: A promising approach to reducing the effects of clinician implicit bias on patients. Patient Educ Couns. 2017; 100(2):372-6. [DOI:10.1016/j.pec.2016.09.005] [PMID]
- Ellershaw J, Fullarton C, Rodwell J, Mcwilliams J. Conscientiousness, openness to experience and extraversion as predictors of nursing work performance: A facet-level analysis. J Nurs Manag. 2016; 24(2):244-52. [DOI:10.1111/jonm.12306] [PMID]
- Dapaah JM. Attitudes and behaviours of health workers and the use of HIV/AIDS health care services. Nurs Res Pract. 2016; 2016:5172497. [DOI:10.1155/2016/5172497] [PMID]
- Ghanbari V, Ardalan A, Zareiyan A, Nejati A, Hanfling D, Bagheri A, et al. Perceptions on principle of priority setting in disaster triage: A Q-method study. Int Emerg Nurs. 2021; 59:101064. [DOI:10.1016/j.ienj.2021.101064] [PMID]
- Dominicé Dao M. Vulnerability in the clinic: Case study of a transcultural consultation. J Med Ethics. 2018; 44(3):167-70.[DOI:10.1136/medethics-2015-103337] [PMID]
- Skirbekk H, Nortvedt P. Inadequate treatment for elderly patients: Professional norms and tight budgets could cause “ageism” in hospitals. Health Care Anal. 2014; 22(2):192-201. [DOI:10.1007/s10728-012-0207-2] [PMID]
- Renedo A, Marston C. Developing patient-centred care: An ethnographic study of patient perceptions and influence on quality improvement. BMC Health Serv Res. 2015; 15:122. [DOI:10.1186/s12913-015-0770-y] [PMID]
- Mastaneh Z, Mouseli L. Patients’ awareness of their rights: Insight from a developing country. Int J Health Policy Manag. 2013; 1(2):143-6. [DOI:10.15171/ijhpm.2013.26] [PMID]
- Khademi M, Mohammadi E, Vanaki Z. A grounded theory of humanistic nursing in acute care work environments. Nurs Ethics. 2017; 24(8):908-21. [DOI:10.1177/0969733016638140] [PMID]
- Kim KJ, Yoo MS, Seo EJ. Exploring the influence of nursing work environment and patient safety culture on missed nursing care in Korea. Asian Nurs Res (Korean Soc Nurs Sci). 2018; S1976-1317(17)30683-7. [DOI:10.1016/j.anr.2018.04.003] [PMID]
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit bias in health care: A narrative review. Group Process Intergroup Relat. 2016; 19(4):528-42. [DOI:10.1177/1368430216642029] [PMID]
- Zeleníková R, Jarošová D, Plevová I, Janíková E. Nurses’ perceptions of professional practice environment and its relation to missed nursing care and nurse satisfaction. Int J Environ Res Public Health. 2020; 17(11):3805. [DOI:10.3390/ijerph17113805] [PMID]
Article Type : Research |
Subject:
Special
Received: 2023/03/21 | Accepted: 2023/09/30 | Published: 2025/01/12
Received: 2023/03/21 | Accepted: 2023/09/30 | Published: 2025/01/12
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |