Thu, Jan 29, 2026
Volume 34, Issue 4 (9-2024)
JHNM 2024, 34(4): 309-315 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Suniyadewi N W, Nursalam N, Sufyanti Arief Y, Kurniawati N D, Agustini N L P I B, Rismayanti I D A, et al . Effect of Android-based Mobile Diabetic Foot Early Self-assessment on Diabetic Foot Prevention Behaviors of Indonesian Patients With Type 2 Diabetes. JHNM 2024; 34 (4) :309-315
URL: http://hnmj.gums.ac.ir/article-1-2102-en.html
URL: http://hnmj.gums.ac.ir/article-1-2102-en.html
Ni Wayan Suniyadewi1 

 , Nursalam Nursalam2
, Nursalam Nursalam2 

 , Yuni Sufyanti Arief *3
, Yuni Sufyanti Arief *3 

 , Ninuk Dian Kurniawati4
, Ninuk Dian Kurniawati4 

 , Ni Luh Putu Inca Buntari Agustini5
, Ni Luh Putu Inca Buntari Agustini5 

 , I Dewa Ayu Rismayanti6
, I Dewa Ayu Rismayanti6 

 , Virgianti Nur Farida7
, Virgianti Nur Farida7 

 , Arifal Aris8
, Arifal Aris8 

 , Resti Utami9
, Resti Utami9 




 , Nursalam Nursalam2
, Nursalam Nursalam2 

 , Yuni Sufyanti Arief *3
, Yuni Sufyanti Arief *3 

 , Ninuk Dian Kurniawati4
, Ninuk Dian Kurniawati4 

 , Ni Luh Putu Inca Buntari Agustini5
, Ni Luh Putu Inca Buntari Agustini5 

 , I Dewa Ayu Rismayanti6
, I Dewa Ayu Rismayanti6 

 , Virgianti Nur Farida7
, Virgianti Nur Farida7 

 , Arifal Aris8
, Arifal Aris8 

 , Resti Utami9
, Resti Utami9 


1- PhD Candidate, Department of Nursing Community, Faculty of Nursing, Airlangga University, East Java, Indonesia.
2- Professor, Department of Nursing Management, Faculty of Nursing, Airlangga University, Est Java, Indonesia.
3- Associate Professor, Department of Pediatric Nursing, Faculty of Nursing, Airlangga University, Est Java, Indonesia. ,yuni.sa@fkp.unair.ac.id
4- Associate Professor, Department of Medical Surgical Nursing, Faculty of Nursing, Airlangga University, Est Java, Indonesia.
5- Assistant Professor, Department of Critical Care Nursing, Institute of Technology and Health Bali, Bali Indonesia.
6- Assistant Professor, Department of Medical Surgical Nursing, Nursing Program STIKES Buleleng, Bali, Indonesia.
7- Assistant Professor, Department of Medical Surgical Nursing, Nursing Program, University of Muhammadiyah Lamongan, East Java, Indonesia.
8- Assistant Professor, Department of Nursing Community, Nursing Program, University of Muhammadiyah Lamongan, East Java, Indonesia.
9- Assistant Professor, Department of Pediatric Nursing, Nursing Program, University of Muhammadiyah Jember, East Java, Indonesia.
2- Professor, Department of Nursing Management, Faculty of Nursing, Airlangga University, Est Java, Indonesia.
3- Associate Professor, Department of Pediatric Nursing, Faculty of Nursing, Airlangga University, Est Java, Indonesia. ,
4- Associate Professor, Department of Medical Surgical Nursing, Faculty of Nursing, Airlangga University, Est Java, Indonesia.
5- Assistant Professor, Department of Critical Care Nursing, Institute of Technology and Health Bali, Bali Indonesia.
6- Assistant Professor, Department of Medical Surgical Nursing, Nursing Program STIKES Buleleng, Bali, Indonesia.
7- Assistant Professor, Department of Medical Surgical Nursing, Nursing Program, University of Muhammadiyah Lamongan, East Java, Indonesia.
8- Assistant Professor, Department of Nursing Community, Nursing Program, University of Muhammadiyah Lamongan, East Java, Indonesia.
9- Assistant Professor, Department of Pediatric Nursing, Nursing Program, University of Muhammadiyah Jember, East Java, Indonesia.
Full-Text [PDF 686 kb]
(481 Downloads)
| Abstract (HTML) (970 Views)
Full-Text: (437 Views)
Introduction
Diabetes mellitus (DM) is a chronic silent-killer disease with many complications. The most common complication of DM is diabetic foot, which is the most common cause of hospitalization in DM patients, resulting in increased treatment costs, disability, decreased quality of life, and risk of death [1]. Globally, the incidence of diabetic foot is relatively high and continues to increase along with the increase in the prevalence of DM. Diabetic foot mainly occurs in patients with type 2 DM for more than 10 years, where about 60% experience disability and leg amputation. The risk of amputation occurs every 30 seconds and is 15-40 times more frequent in DM patients worldwide [2]. In DM patients, 85% of amputations began with undetected foot ulceration and late treatment, which can turn into a severe infection [3-6]. Most diabetic foots occur due to late detection and poor management [7]. To prevent acute or chronic complications, early detection and appropriate treatments are needed [3].
Diabetic foot disorder is a preventable complication. Five key elements for diabetic foot prevention, include identifying the at-risk foot, examining the at-risk foot regularly, providing education to patients, families, and health workers, ensuring the use of appropriate footwear, and treating risk factors [8]. The assessment format is not specific for detecting diabetic foot, because it is still combined with the patient's general assessment. In addition, the existing instruments can only be used by health workers when patients visit health centres. They are also not accessible to patients and their families, making the instruments less effective in detecting the occurrence of diabetic foot. Hence, developing an innovative and efficient instrument for early detection of diabetic foot that is easy to use independently by patients and their families is required.
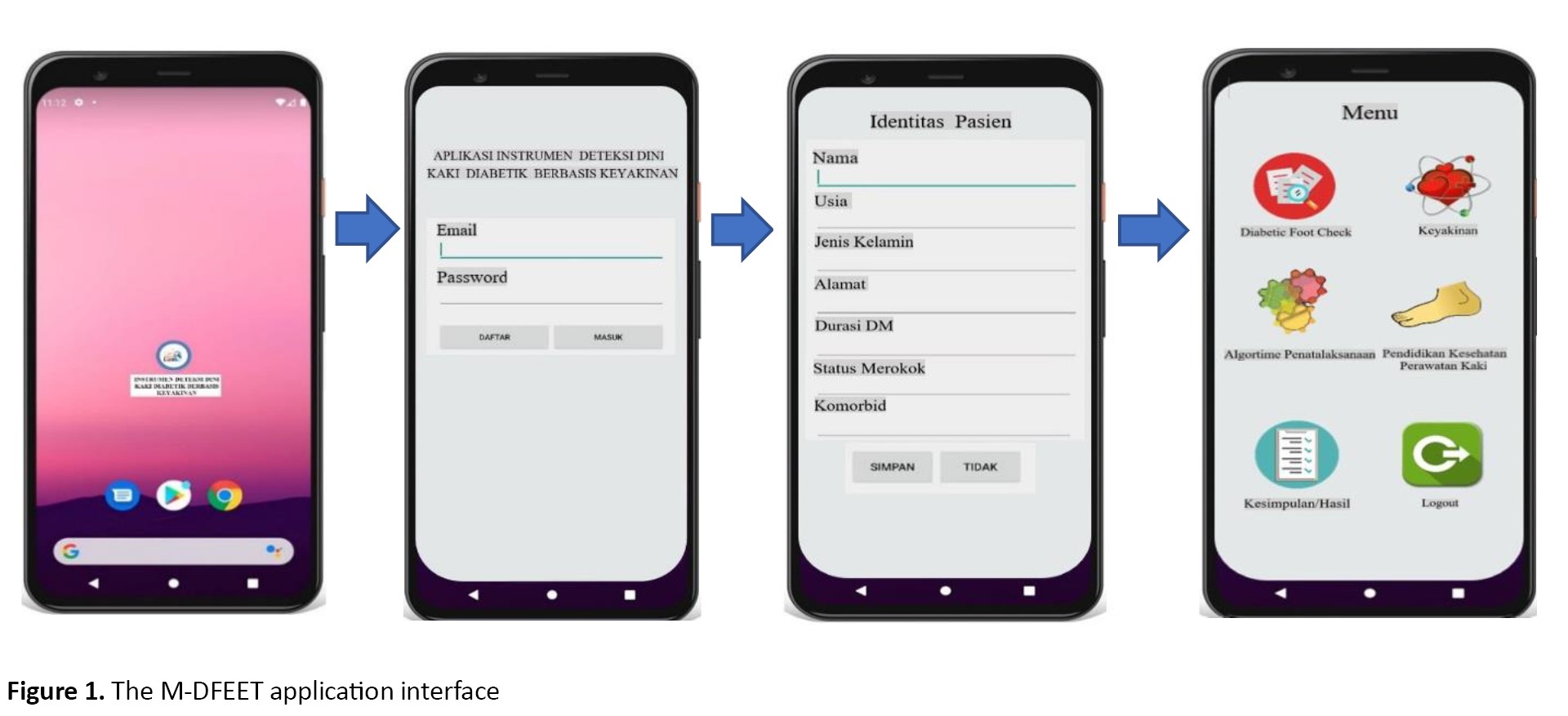
One strategy for developing such instruments is the use of mobile applications. One developed application for the diabetic foot screening is “Inlow’s 60-second diabetic foot screen” [9]. Another mobile application for the early detection of diabetic foot is “android-based mobile diabetic foot early self-assessment” (M-DFEET) which has simple features regarding patient identity, patient confidence in conducting foot examinations, assessment of foot conditions, conclusions on the results of the early detection, recommendations according to the early detection results, health education about foot examination at home, and automatic reminders. The M-DFEET application is in Indonesian language and has promising, valid, and reliable features that enable patients with type 2 diabetes to perform early self-assessment of their feet (Figure 1). It has been developed based on the software development life cycle (SDLC) principle which consists of five phases of inception, design, implementation, maintenance, and audit [10]. The M-DFEET has acceptable content validity (I-CVI=1.00) and good internal consistency (Cronbach's α=0.74). The Android operating system has been chosen because of its widespread use and the accessibility of Android applications from Google Play. A survey in 2022 on the growth of internet users in Indonesia revealed that Android the largest smartphone platform in Indonesia, which is around 91% compared to other platforms [11].
The health belief model (HBM) elucidates the impact of an individual’s perception of disease and health-promoting behavior. According to this model, if individuals perceive themselves as susceptible to severe complications of their disease, they are more likely to believe the benefits of taking necessary health measures and feel exposed to cues from internal or external sources that can trigger action [12, 13]. Based on this theory, this study aimed to assess the effectiveness of the M-DFEET application in Indonesian patients with type 2 DM.
Materials and Methods
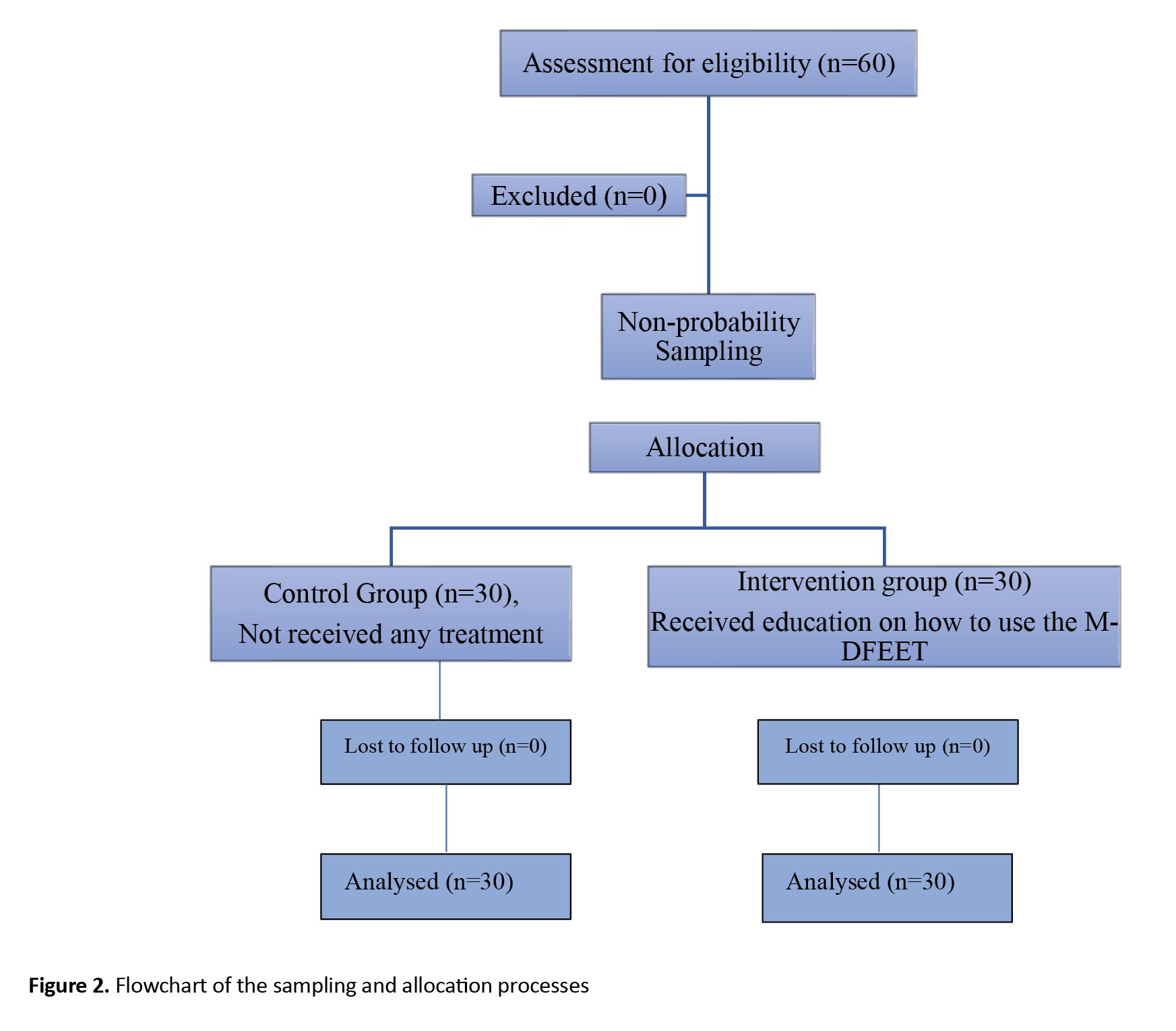
This is a quasi-experimental study with a pre-test/post-test design. The data were conducted from August to October 2021. The sample size was determined 26 per group using DanielSoper’s free sample size calculator, by considering a large effect size of 0.8, a test power of 0.8, and a type 1 error rate of 0.05 [14]. By accounting for a 10% sample dropout rate, the final sample size was 30 per group. In this regard, 60 patients with type 2 DM who met the inclusion criteria were purposively recruited from Puskesmas Blahbatuh Hospital, Gianyar, Bali. The inclusion criteria were a diagnosed type 2 DM, age 30-65 years, no diabetic foot complications, having a smartphone with Android operating system and being able to use these smartphones, attending socialisation and training on the use of the M-DFEET application, and willingness to participate in the study. On the other hand, the patients who already had diabetic foot were excluded. Sample selection was done based on assigning even and odd numbers to patient names. Even numbers were for the inclusion in the control group and odd numbers were for the intervention group. The flowchart of sampling allocation process is shown in Figure 2. A HBM-based questionnaire was used to measure patient’s perceived severity, perceived susceptibility, cues to action, perceived benefits, and perceived barriers. Also, the Inlow’s 60-second diabetic foot screen tool was used for screening and assessing the risk of diabetic ulcers so that appropriate prevention and treatment could be carried out [9]. It is a reliable and valid tool [15]. The diabetic foot prevention behavior was measured using a faith-based early detection instrument for diabetic foot through an Android application that had been developed. The M-DFEET has acceptable content validity (I-CVI=1.00) and good internal consistency (Cronbach’s α 0.74). The Android operating system has been chosen because of its widespread use and the accessibility of Android applications from Google Play. A number of items included about routine foot examinations, routine diabetic foot exercises, routine foot cleaning, nail cutting, foot massage, and selection of appropriate footwear. The items rated on a scale as 0 (never), 1 (sometimes), 2 (often), and 3 (always). Based on the score, the prevention behaviors were categorized into three levels: Poor (≤50%), moderate (51-75%), and good (76-100%).
The research team provided socialization and training to the participants in the intervention group regarding the proper use of the application. They were trained to log in, register and fill the questionnaire. Diabetic foot prevention behaviors were measured before using application and three months after using application. The collected data were analysed using descriptive statistics, paired t-test to compare pre-test and post-test scores and independent t-test to measure the difference in the post-test scores between groups.
Results
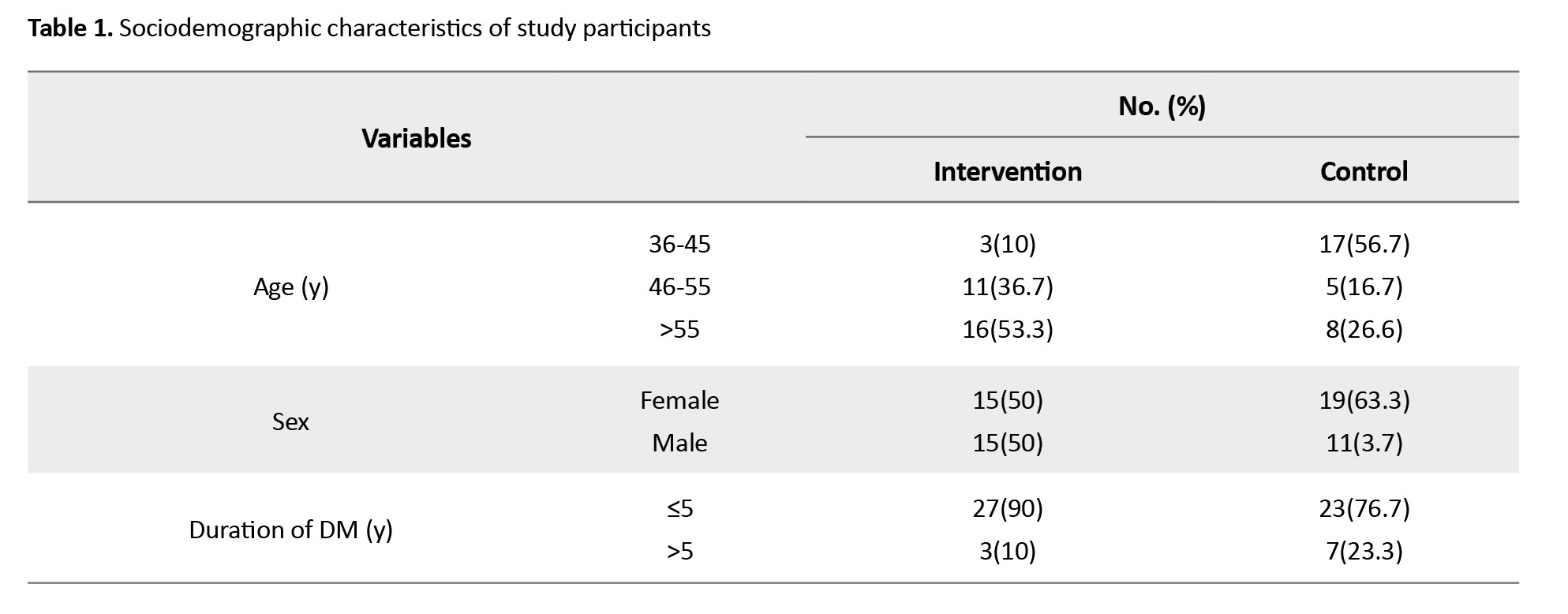
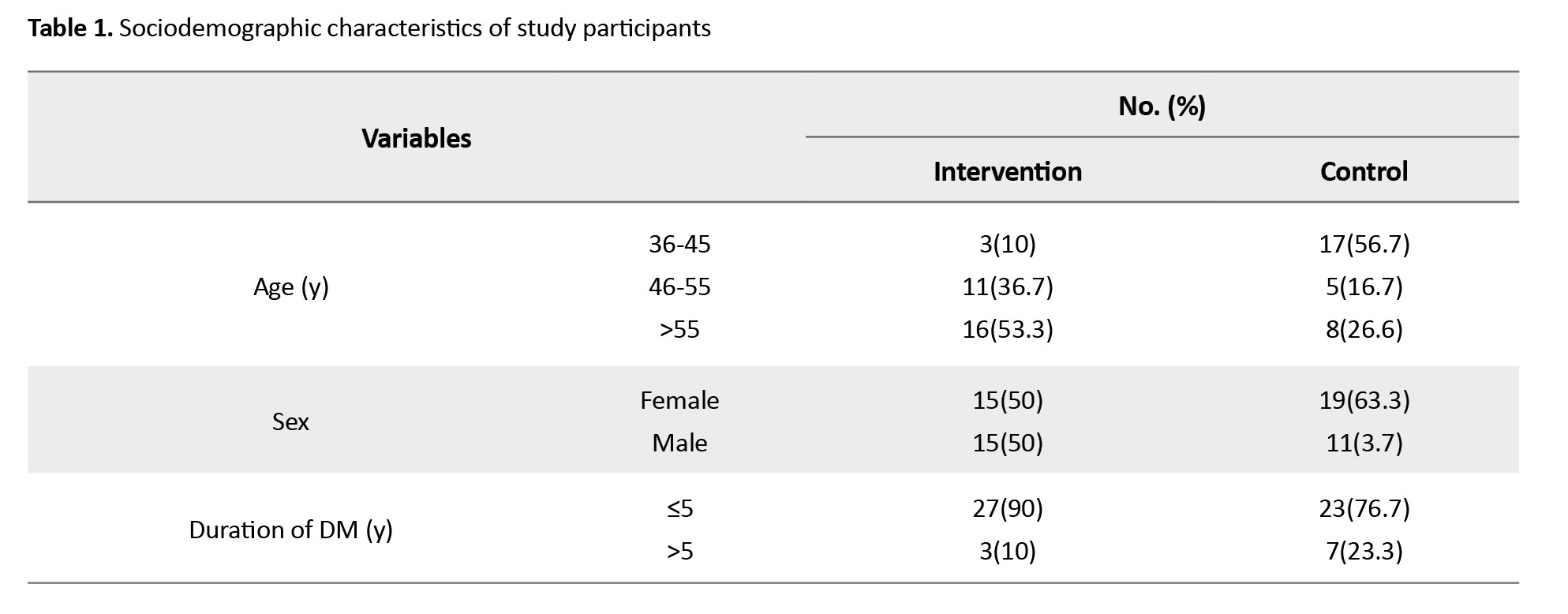
The most of respondents in the intervention group were over 55 years of age (53.3%), while the majority of respondents in the control group aged 36-45 years (56.7%). Regarding gender, the majority of respondents in the control group were female (63.3%) while the percentage of females and males in the intervention group was equal (50%). The majority of respondents had DM for less than 5 years in both intervention (90%) and control (76.7%) group (Table 1).
The levels of ability to use the M-DFEET application in the intervention group are shown in Table 2.
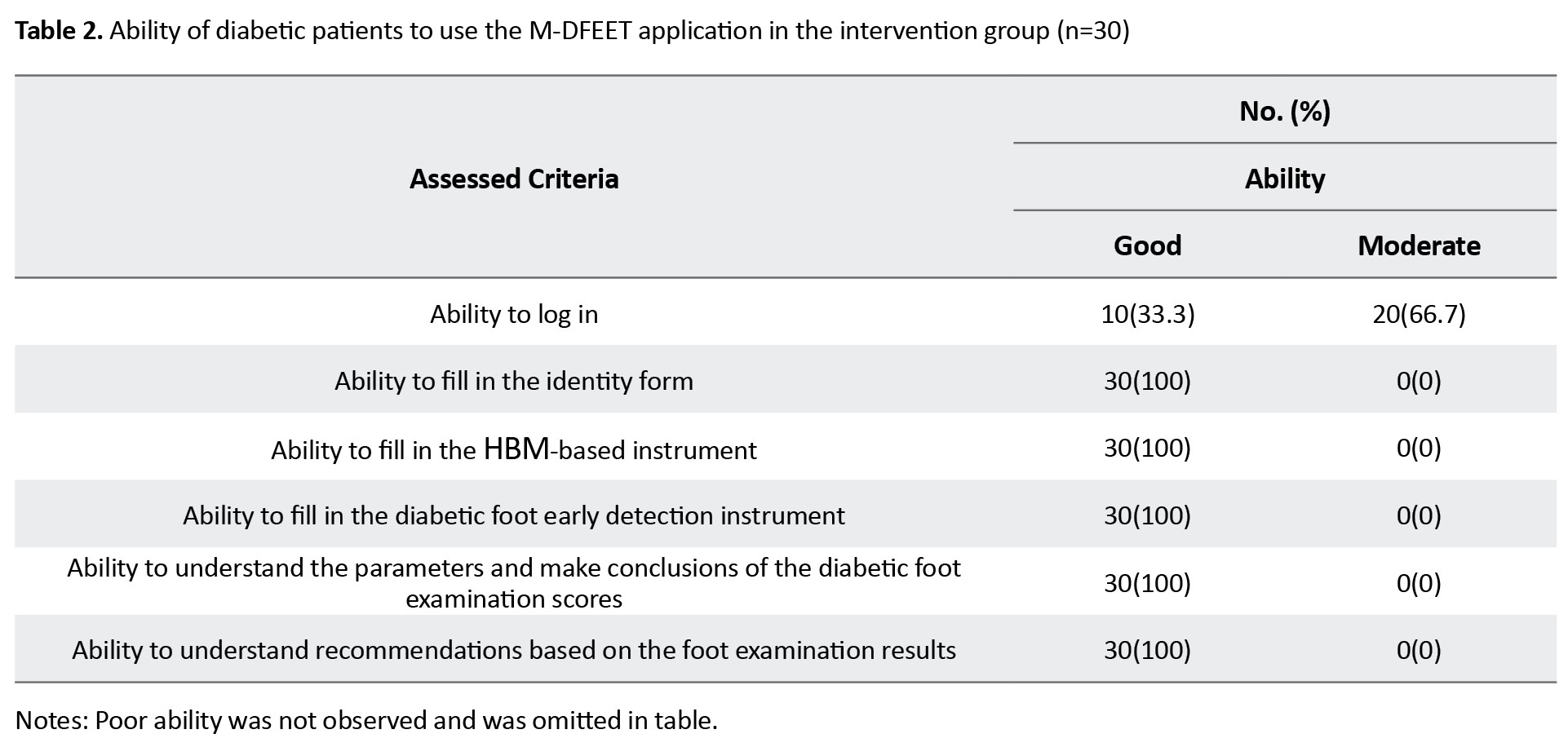
The results showed that one third of participants in the intervention group had a good ability to log into the M-DFEET application, while the rest had a moderate ability to log in.
At baseline, there were 18(60%) participants who had good preventive behaviors in the intervention group, while 12(40%) had moderate behavior. Meanwhile, in the control group, there were 10(33.3%) participants with good preventive behaviors and 20(66.7%) with moderate behavior (Table 3).
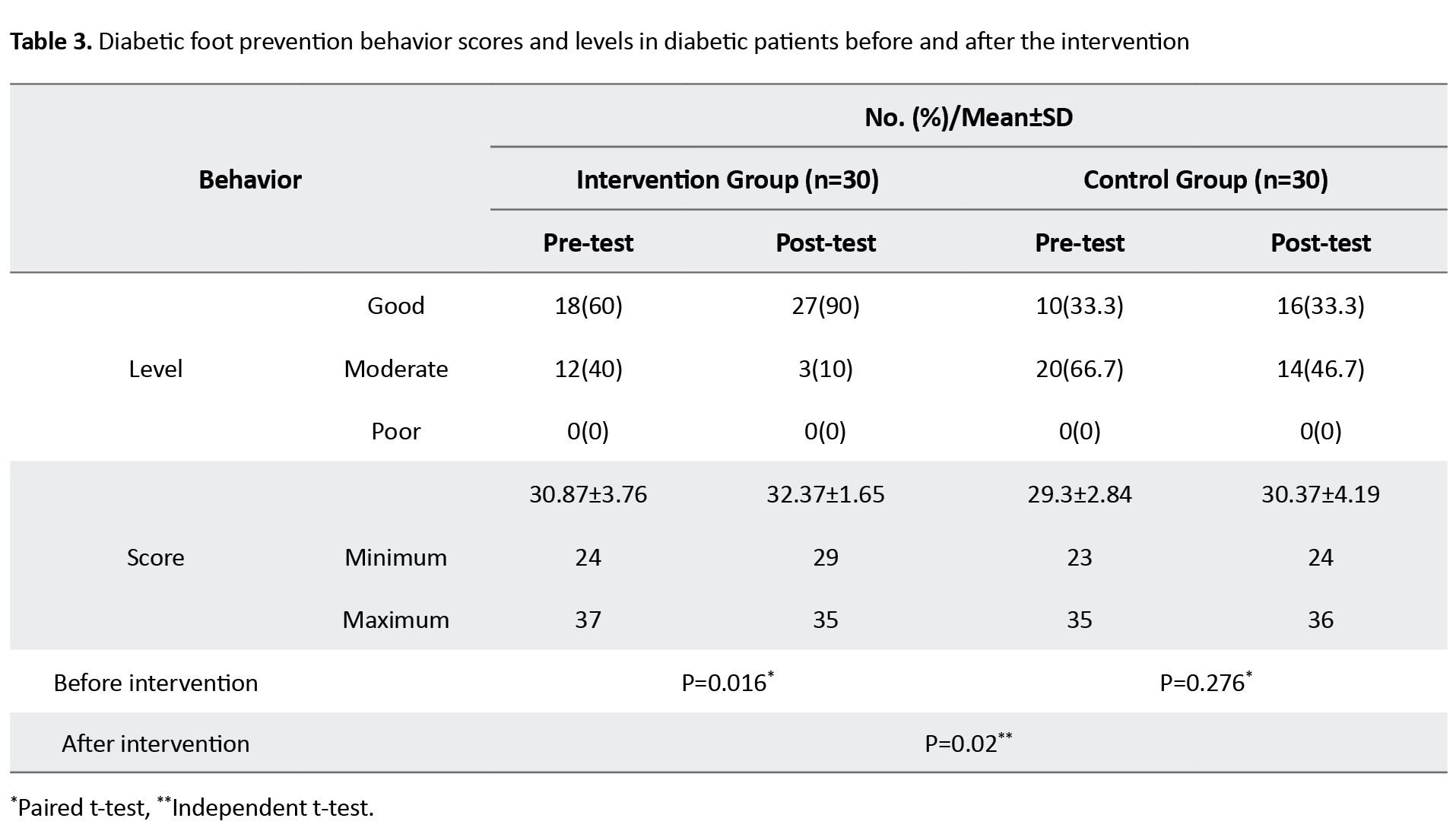
After the intervention, there was an increase in the number of participants with good behavior in the experimental group from 12 to 27(90%), while 3 participants (10%) still had moderate behavior. Meanwhile, in the control group, there were 16 participants (53.3%) with good behavior and 14(46.7%) with had moderate behavior. Additionally, statistical analysis results showed a significance difference between control and experimental groups after intervention (Table 3).
Discussion
The findings showed that the M-DFEET application had a significant impact on diabetic foot prevention behaviors in the experimental group. The application can increase the diabetic patients’ knowledge of foot condition. Two previous studies had similar findings; they also showed that mobile applications can help diabetic patients to maintain their foot conditions [16, 17]. By using mobile applications, patients with DM do not need to go to healthcare centres; they can have easy access to related information anywhere and anytime. Development of the application with remote consultation is beneficial [18]. The M-DFEET is very easy to use. All age groups can use it according to the assessment results. Technology can help diabetic patients to understand their condition [19, 20]. It is very important for diabetic patients to take preventive measures to controlling glucose level and DM complications [21]. A previous study showed that many diabetes-related mobile applications could help diabetic people [22].
We employed the HBM model [23] in this study. This model measures patient’s perceived severity, perceived susceptibility, cues to action, perceived benefits, and perceived barriers. When diabetic patients perceive themselves to be susceptible to serious complications of diabetic foot and have a heightened knowledge of benefits, they are more likely to adopt essential health-related measures [24]. The cues to action from internal or external sources can help patients take health actions, such as early detection of diabetic foot [25].
The M-DFEET application uses a theoretical approach that builds trust in patients with type 2 DM, prevent diabetic foot complications, or reduce deaths. The success of controlling the complications of diabetic foot depends on patients’ self-care behaviors since more than 95% of DM-related treatments are done by the patients themselves based on beliefs, ability, and adherence to health guidelines. By the M-DFEET application, diabetic patients can conduct early diabetic foot detection test independently anywhere and anytime. The application also has proper quality based on functionality, reliability, efficiency, usability, and portability. This application is projected to contribute to evidence-based nursing practice to reduce DM-related disability and death. However, the application, which was developed only for Android users and use the Indonesian language, is highly dependent on the stability of the internet connection. Furthermore, the application has yet to be tested extensively with a larger number of participants. In addition, the application needs to be upgraded to be used offline and save data for online processing when internet is reconnected.
Ethical Considerations
Compliance with ethical guidelines
This study received ethical approval from the Research Ethics Committee of STIKES Buleleng (Code: 085/EC-KEPK-SB/IX/2021) on September 20, 2021.
Funding
This study was financially supported by the Faculty of Nursing, Airlangga Universit and STIKes Wira Medika Bali.
Authors' contributions
Conceptualisation and methodology: Ni Wayan Suniyadewi, Nursalam, Yuni Sufyanti Arief, Ninuk Dian Kurniawati; Data collection: Ni Luh Putu Inca Buntari Agustini, I Dewa Ayu Rismayanti, and Virgianti Nur Farida; Data analysis: Arifal Aris and Resti Utami; Writing the original draft: Ni Wayan Suniyadewi, and Yuni Sufyanti Arief; Final approval: All authors.
Conflict of interest
The authors declared no competing interest.
Acknowledgments
The authors would like to extend their gratitude to the Faculty of Nursing, Airlangga University and STIKes Wira Medika Bali for financial support, and all participants for their cooperation in this study.
References
Diabetes mellitus (DM) is a chronic silent-killer disease with many complications. The most common complication of DM is diabetic foot, which is the most common cause of hospitalization in DM patients, resulting in increased treatment costs, disability, decreased quality of life, and risk of death [1]. Globally, the incidence of diabetic foot is relatively high and continues to increase along with the increase in the prevalence of DM. Diabetic foot mainly occurs in patients with type 2 DM for more than 10 years, where about 60% experience disability and leg amputation. The risk of amputation occurs every 30 seconds and is 15-40 times more frequent in DM patients worldwide [2]. In DM patients, 85% of amputations began with undetected foot ulceration and late treatment, which can turn into a severe infection [3-6]. Most diabetic foots occur due to late detection and poor management [7]. To prevent acute or chronic complications, early detection and appropriate treatments are needed [3].
Diabetic foot disorder is a preventable complication. Five key elements for diabetic foot prevention, include identifying the at-risk foot, examining the at-risk foot regularly, providing education to patients, families, and health workers, ensuring the use of appropriate footwear, and treating risk factors [8]. The assessment format is not specific for detecting diabetic foot, because it is still combined with the patient's general assessment. In addition, the existing instruments can only be used by health workers when patients visit health centres. They are also not accessible to patients and their families, making the instruments less effective in detecting the occurrence of diabetic foot. Hence, developing an innovative and efficient instrument for early detection of diabetic foot that is easy to use independently by patients and their families is required.
One strategy for developing such instruments is the use of mobile applications. One developed application for the diabetic foot screening is “Inlow’s 60-second diabetic foot screen” [9]. Another mobile application for the early detection of diabetic foot is “android-based mobile diabetic foot early self-assessment” (M-DFEET) which has simple features regarding patient identity, patient confidence in conducting foot examinations, assessment of foot conditions, conclusions on the results of the early detection, recommendations according to the early detection results, health education about foot examination at home, and automatic reminders. The M-DFEET application is in Indonesian language and has promising, valid, and reliable features that enable patients with type 2 diabetes to perform early self-assessment of their feet (Figure 1). It has been developed based on the software development life cycle (SDLC) principle which consists of five phases of inception, design, implementation, maintenance, and audit [10]. The M-DFEET has acceptable content validity (I-CVI=1.00) and good internal consistency (Cronbach's α=0.74). The Android operating system has been chosen because of its widespread use and the accessibility of Android applications from Google Play. A survey in 2022 on the growth of internet users in Indonesia revealed that Android the largest smartphone platform in Indonesia, which is around 91% compared to other platforms [11].
The health belief model (HBM) elucidates the impact of an individual’s perception of disease and health-promoting behavior. According to this model, if individuals perceive themselves as susceptible to severe complications of their disease, they are more likely to believe the benefits of taking necessary health measures and feel exposed to cues from internal or external sources that can trigger action [12, 13]. Based on this theory, this study aimed to assess the effectiveness of the M-DFEET application in Indonesian patients with type 2 DM.
Materials and Methods
This is a quasi-experimental study with a pre-test/post-test design. The data were conducted from August to October 2021. The sample size was determined 26 per group using DanielSoper’s free sample size calculator, by considering a large effect size of 0.8, a test power of 0.8, and a type 1 error rate of 0.05 [14]. By accounting for a 10% sample dropout rate, the final sample size was 30 per group. In this regard, 60 patients with type 2 DM who met the inclusion criteria were purposively recruited from Puskesmas Blahbatuh Hospital, Gianyar, Bali. The inclusion criteria were a diagnosed type 2 DM, age 30-65 years, no diabetic foot complications, having a smartphone with Android operating system and being able to use these smartphones, attending socialisation and training on the use of the M-DFEET application, and willingness to participate in the study. On the other hand, the patients who already had diabetic foot were excluded. Sample selection was done based on assigning even and odd numbers to patient names. Even numbers were for the inclusion in the control group and odd numbers were for the intervention group. The flowchart of sampling allocation process is shown in Figure 2. A HBM-based questionnaire was used to measure patient’s perceived severity, perceived susceptibility, cues to action, perceived benefits, and perceived barriers. Also, the Inlow’s 60-second diabetic foot screen tool was used for screening and assessing the risk of diabetic ulcers so that appropriate prevention and treatment could be carried out [9]. It is a reliable and valid tool [15]. The diabetic foot prevention behavior was measured using a faith-based early detection instrument for diabetic foot through an Android application that had been developed. The M-DFEET has acceptable content validity (I-CVI=1.00) and good internal consistency (Cronbach’s α 0.74). The Android operating system has been chosen because of its widespread use and the accessibility of Android applications from Google Play. A number of items included about routine foot examinations, routine diabetic foot exercises, routine foot cleaning, nail cutting, foot massage, and selection of appropriate footwear. The items rated on a scale as 0 (never), 1 (sometimes), 2 (often), and 3 (always). Based on the score, the prevention behaviors were categorized into three levels: Poor (≤50%), moderate (51-75%), and good (76-100%).
The research team provided socialization and training to the participants in the intervention group regarding the proper use of the application. They were trained to log in, register and fill the questionnaire. Diabetic foot prevention behaviors were measured before using application and three months after using application. The collected data were analysed using descriptive statistics, paired t-test to compare pre-test and post-test scores and independent t-test to measure the difference in the post-test scores between groups.
Results
The most of respondents in the intervention group were over 55 years of age (53.3%), while the majority of respondents in the control group aged 36-45 years (56.7%). Regarding gender, the majority of respondents in the control group were female (63.3%) while the percentage of females and males in the intervention group was equal (50%). The majority of respondents had DM for less than 5 years in both intervention (90%) and control (76.7%) group (Table 1).
The levels of ability to use the M-DFEET application in the intervention group are shown in Table 2.
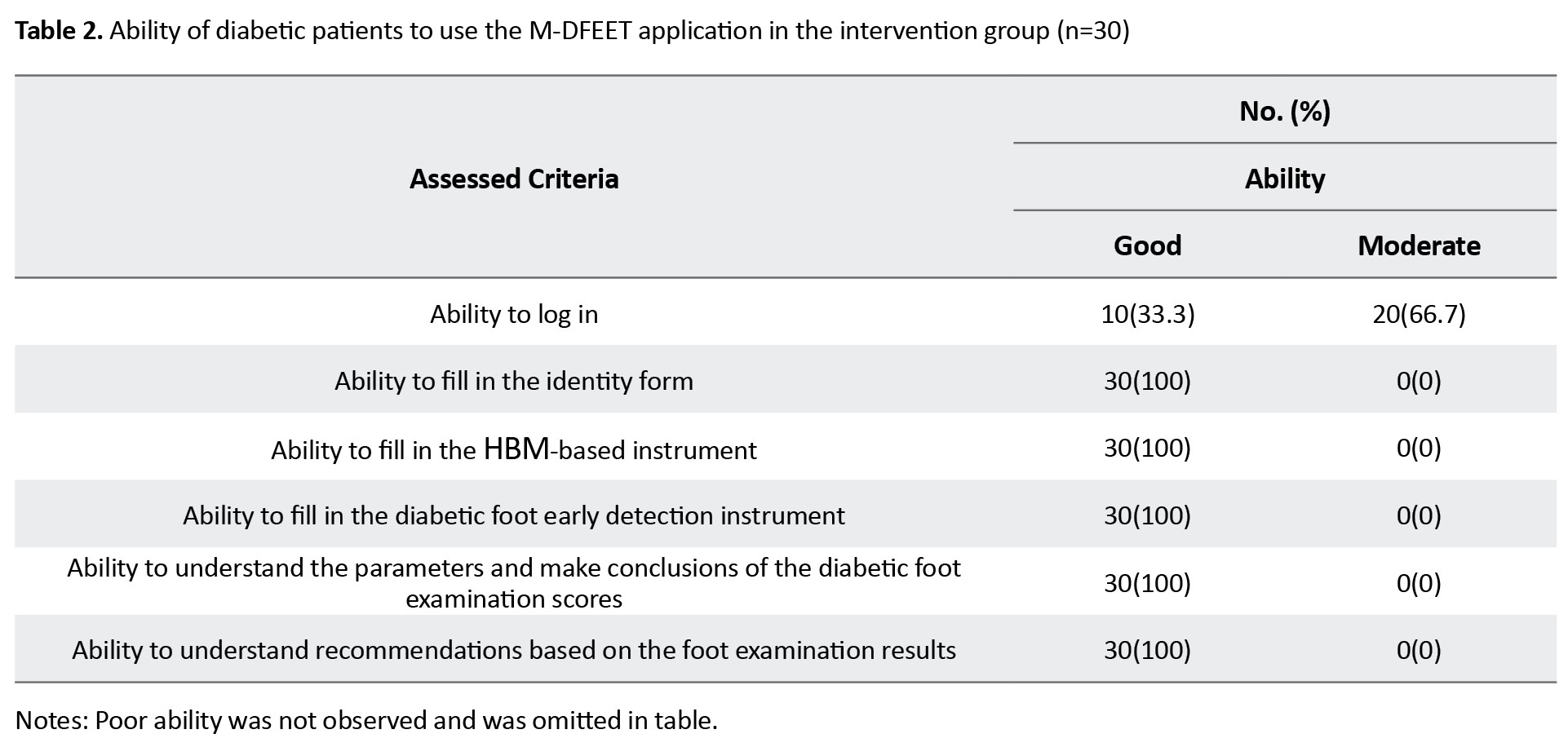
The results showed that one third of participants in the intervention group had a good ability to log into the M-DFEET application, while the rest had a moderate ability to log in.
At baseline, there were 18(60%) participants who had good preventive behaviors in the intervention group, while 12(40%) had moderate behavior. Meanwhile, in the control group, there were 10(33.3%) participants with good preventive behaviors and 20(66.7%) with moderate behavior (Table 3).
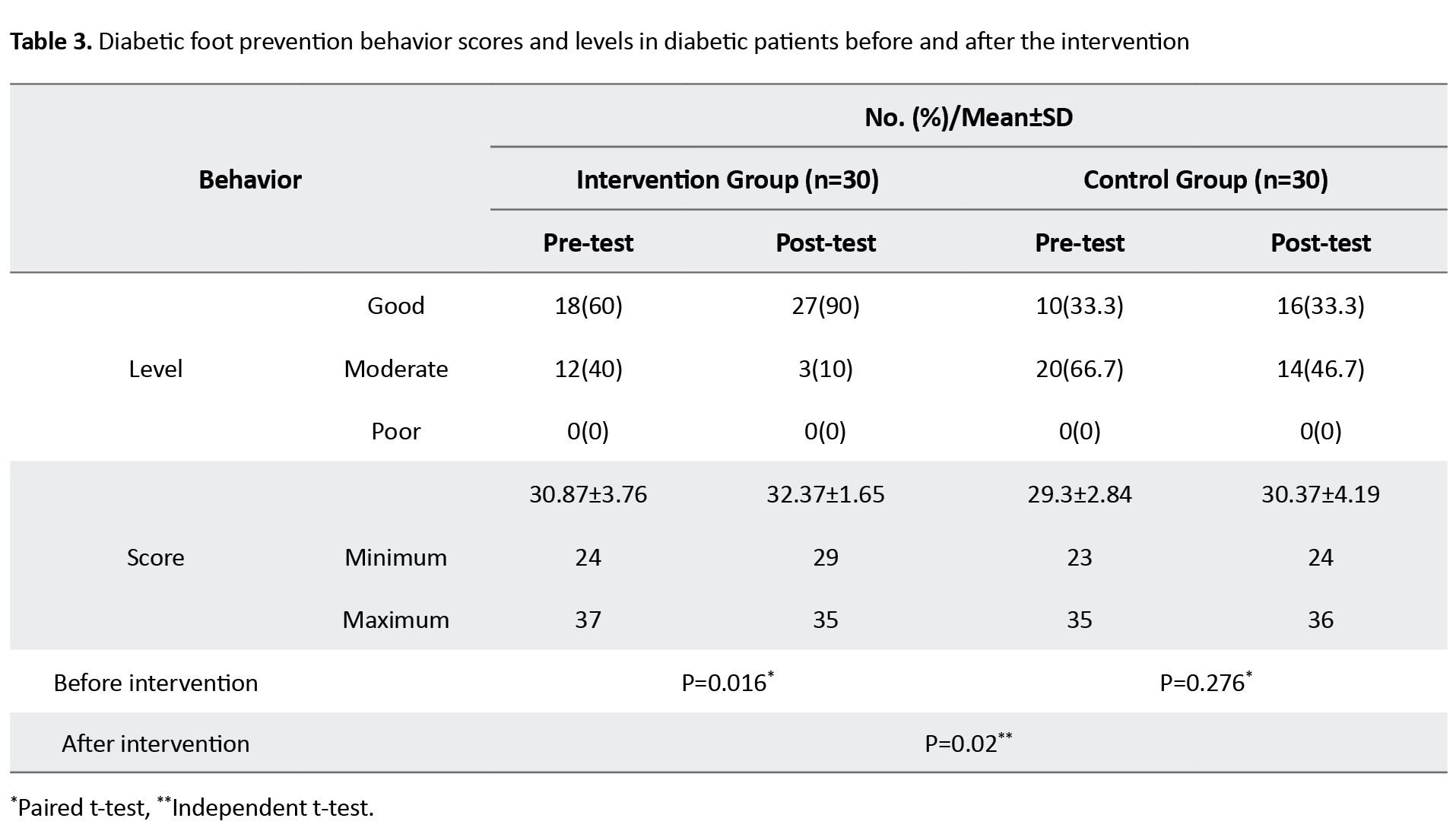
After the intervention, there was an increase in the number of participants with good behavior in the experimental group from 12 to 27(90%), while 3 participants (10%) still had moderate behavior. Meanwhile, in the control group, there were 16 participants (53.3%) with good behavior and 14(46.7%) with had moderate behavior. Additionally, statistical analysis results showed a significance difference between control and experimental groups after intervention (Table 3).
Discussion
The findings showed that the M-DFEET application had a significant impact on diabetic foot prevention behaviors in the experimental group. The application can increase the diabetic patients’ knowledge of foot condition. Two previous studies had similar findings; they also showed that mobile applications can help diabetic patients to maintain their foot conditions [16, 17]. By using mobile applications, patients with DM do not need to go to healthcare centres; they can have easy access to related information anywhere and anytime. Development of the application with remote consultation is beneficial [18]. The M-DFEET is very easy to use. All age groups can use it according to the assessment results. Technology can help diabetic patients to understand their condition [19, 20]. It is very important for diabetic patients to take preventive measures to controlling glucose level and DM complications [21]. A previous study showed that many diabetes-related mobile applications could help diabetic people [22].
We employed the HBM model [23] in this study. This model measures patient’s perceived severity, perceived susceptibility, cues to action, perceived benefits, and perceived barriers. When diabetic patients perceive themselves to be susceptible to serious complications of diabetic foot and have a heightened knowledge of benefits, they are more likely to adopt essential health-related measures [24]. The cues to action from internal or external sources can help patients take health actions, such as early detection of diabetic foot [25].
The M-DFEET application uses a theoretical approach that builds trust in patients with type 2 DM, prevent diabetic foot complications, or reduce deaths. The success of controlling the complications of diabetic foot depends on patients’ self-care behaviors since more than 95% of DM-related treatments are done by the patients themselves based on beliefs, ability, and adherence to health guidelines. By the M-DFEET application, diabetic patients can conduct early diabetic foot detection test independently anywhere and anytime. The application also has proper quality based on functionality, reliability, efficiency, usability, and portability. This application is projected to contribute to evidence-based nursing practice to reduce DM-related disability and death. However, the application, which was developed only for Android users and use the Indonesian language, is highly dependent on the stability of the internet connection. Furthermore, the application has yet to be tested extensively with a larger number of participants. In addition, the application needs to be upgraded to be used offline and save data for online processing when internet is reconnected.
Ethical Considerations
Compliance with ethical guidelines
This study received ethical approval from the Research Ethics Committee of STIKES Buleleng (Code: 085/EC-KEPK-SB/IX/2021) on September 20, 2021.
Funding
This study was financially supported by the Faculty of Nursing, Airlangga Universit and STIKes Wira Medika Bali.
Authors' contributions
Conceptualisation and methodology: Ni Wayan Suniyadewi, Nursalam, Yuni Sufyanti Arief, Ninuk Dian Kurniawati; Data collection: Ni Luh Putu Inca Buntari Agustini, I Dewa Ayu Rismayanti, and Virgianti Nur Farida; Data analysis: Arifal Aris and Resti Utami; Writing the original draft: Ni Wayan Suniyadewi, and Yuni Sufyanti Arief; Final approval: All authors.
Conflict of interest
The authors declared no competing interest.
Acknowledgments
The authors would like to extend their gratitude to the Faculty of Nursing, Airlangga University and STIKes Wira Medika Bali for financial support, and all participants for their cooperation in this study.
References
- Deputy NP, Kim SY, Conrey EJ, Bullard KM. Prevalence and changes in preexisting diabetes and gestational diabetes among women who had a live birth - United States, 2012-2016. MMWR Morb Mortal Wkly Rep. 2018; 67(43):1201-7. [DOI:10.15585/mmwr.mm6743a2] [PMID]
- International Diabetes Federation. Five questions on the IDF Diabetes Atlas. Diabetes Res Clin Pract. 2013; 102(2):147-8. [PMID]
- Shabibi P, Zavareh MSA, Sayehmiri K, Qorbani M, Safari O, Rastegarimehr B, et al. Effect of educational intervention based on the Health Belief Model on promoting self-care behaviors of type-2 diabetes patients. Electron Physician. 2017; 9(12):5960-8. [DOI:10.19082/5960] [PMID]
- Ming A, Walter I, Alhajjar A, Leuckert M, Mertens PR. Study protocol for a randomized controlled trial to test for preventive effects of diabetic foot ulceration by telemedicine that includes sensor-equipped insoles combined with photo documentation. Trials. 2019; 20(1):521. [DOI:10.1186/s13063-019-3623-x] [PMID]
- Asharib Arshad M, Arshad S, Arshad S, Abbas H. The quality of life in patients with diabetic foot Ulcers. J Diabetes Metab. 2020; 11(2):1-2. [Link]
- Cassidy B, Reeves ND, Pappachan JM, Gillespie D, O’Shea C, Rajbhandari S, et al. The DFUC 2020 Dataset: Analysis towards diabetic foot ulcer detection. touchREV Endocrinol. 2021; 17(1):5-11. [DOI:10.17925/EE.2021.17.1.5] [PMID]
- Tolossa T, Mengist B, Mulisa D, Fetensa G, Turi E, Abajobir A. Prevalence and associated factors of foot ulcer among diabetic patients in Ethiopia: A systematic review and meta-analysis. BMC Public Health. 2020; 20(1):41. [DOI:10.1186/s12889-019-8133-y] [PMID]
- Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA, et al. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 2020; 36(Suppl 1):e3266. [DOI:10.1002/dmrr.3266] [PMID]
- Canadian Association of Wound Care. Inlow’s 60-second Diabetic Foot Screen. Wound Care Canada. 2004; 2(2):10-1.
- Gurung G, Shah R, Jaiswal DP. Software Development Life Cycle Models-A comparative study. Int J Sci Res Comput Sci Eng Inf Technol. 2020; 6(4):30-7. [Link]
- Statista. Internet usage in Indonesia - statistics & facts. New York: Hanadian Nurhayati-Wolff; 2024. [Link]
- Ghobadi A, Sarbarzeh PA, Jalilian M, Abdi A, Manouchehri S. Evaluation of factors affecting the severity of diabetic foot ulcer in patients with diabetes referred to a diabetes centre in Kermanshah. Diabetes, Metab Syndr Obes. 2020; 13:693-703. [DOI:10.2147/DMSO.S242431] [PMID]
- Hsieh YL, Lee FH, Chen CL, Chang MF, Han PH. Factors influencing intention to receive examination of diabetes complications. Asian Nurs Res (Korean Soc Nurs Sci). 2016; 10(4):289-94. [DOI:10.1016/j.anr.2016.10.004] [PMID]
- Free Statistics Calculators. A-priori sample size for student t-test [Internet]. 2023 [Updated 20Februaryb 2023]. Available from: [Link]
- Parasuraman M, Giridharan B, Vijayalakshmi G. Reliability and credibility analysis of Inlow’s 60 second diabetic foot screening tool for diabetic foot risk stratification and its feasibility in India: A systematic review. Int Surg J. 2017; 4(9):2878. [Link]
- Marques ADB, Moreira TMM, Carvalho REFL, Chaves EMC, Oliveira SKP, Felipe GF, et al. PEDCARE: Validation of a mobile application on diabetic foot self-care. Rev Bras Enferm. 2021; 74(suppl 5):e20200856. [DOI:10.1590/0034-7167-2020-0856] [PMID]
- Colodetti R, Prado TN do, Bringuente ME de O, Bicudo SDS.Mobile application for the management of diabetic foot ulcers. Acta Paul Enferm. 2021; 34. [DOI:10.37689/acta-ape/2021AO00702]
- Tekale S, Varma A, Tekale S, Kumbhare U. A Review on Newer Interventions for the Prevention of Diabetic Foot Disease. Cureus. 2022; 14(10):e30591. [DOI:10.7759/cureus.30591] [PMID]
- Wang W, Pei X, Zhang L, Chen Z, Lin D, Duan X, et al. Application of new international classification of adult-onset diabetes in Chinese inpatients with diabetes mellitus. Diabetes Metab Res Rev. 2021; 37(7):e3427. [DOI:10.1002/dmrr.3427] [PMID]
- Joshua SR, Abbas W, Lee JH. M-Healthcare Model: An Architecture for a Type 2 Diabetes Mellitus Mobile Application. Appl Sci. 2023; 13(1):8. [DOI:10.3390/app13010008]
- Pourkazemi A, Ghanbari A, Khojamli M, Balo H, Hemmati H, Jafaryparvar Z, et al. Diabetic foot care: Knowledge and practice. BMC Endocr Disord. 2020; 20(1):40. [DOI:10.1186/s12902-020-0512-y] [PMID]
- Doupis J, Festas G, Tsilivigos C, Efthymiou V, Kokkinos A. Smartphone-Based Technology in Diabetes Management. Diabetes Ther. 2020; 11(3):607-19. [DOI:10.1007/s13300-020-00768-3] [PMID]
- Rosenstock IM. Historical Origins of the Health Belief Model. Health Educ Monogr. 1974; 2(4):328-35. [DOI:10.1177/109019817400200403]
- Malik A, Islam T, Ahmad M, Mahmood K. Health information seeking and sharing behavior of young adults on social media in Pakistan. J Librarnf Sci. 2022; 096100062210902. [DOI:10.1177/09610006221090228]
- Khosravizadeh O, Ahadinezhad B, Maleki A, Vosoughi P, Najafpour Z. Applying the health belief model and behavior of diabetic patients: A systematic review and meta-analysis. Clin Diabetol. 2021; 10(2):209-20. [Link]
Article Type : Research |
Subject:
General
Received: 2023/03/9 | Accepted: 2024/02/5 | Published: 2024/10/1
Received: 2023/03/9 | Accepted: 2024/02/5 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |