Thu, Jan 1, 2026
Volume 35, Issue 3 (6-2025)
JHNM 2025, 35(3): 161-167 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Meliati L, Sudarmi S, Halimatusyaadiah S. Influence of the First Thousand Days of Life on Stunting Incidence. JHNM 2025; 35 (3) :161-167
URL: http://hnmj.gums.ac.ir/article-1-2091-en.html
URL: http://hnmj.gums.ac.ir/article-1-2091-en.html
1- Associate Professor, Department of Midwifery, Politeknik Kesehatan of the Ministry of Health of Mataram, Mataram City, Indonesia. , lindameliati77@gmail.com
2- Associate Professor, Department of Midwifery, Politeknik Kesehatan of the Ministry of Health of Mataram, Mataram City, Indonesia.
3- Assistant Professor, Department of Midwifery, Politeknik Kesehatan of the Ministry of Health of Mataram, Mataram City, Indonesia.
2- Associate Professor, Department of Midwifery, Politeknik Kesehatan of the Ministry of Health of Mataram, Mataram City, Indonesia.
3- Assistant Professor, Department of Midwifery, Politeknik Kesehatan of the Ministry of Health of Mataram, Mataram City, Indonesia.
Full-Text [PDF 497 kb]
(374 Downloads)
| Abstract (HTML) (585 Views)
Full-Text: (199 Views)
Introduction
Stunting is still a severe public health problem in Indonesia. This condition not only inhibits children’s physical growth but also has an impact on children’s cognitive development, immunity, and productivity in the future. Data from the 2022 Indonesian Nutritional Status Study (SSGI) shows that the national prevalence of stunting is 21.6%, while West Nusa Tenggara (NTB) Province is ranked as one of 12 priority provinces with the highest prevalence nationally, namely 31.4% [1]. This figure shows that the intervention efforts that have been carried out have not effectively addressed the factors that play a role in stunting in the area. One of the most crucial periods in preventing stunting is the first 1000 days of life (1000 HPK), namely from pregnancy to the age of two years. During this period, organs and body systems grow rapidly, so nutritional imbalances or health disorders can have permanent impacts. Various studies have shown that suboptimal breastfeeding practices, mothers who are too young when pregnant, pregnancies that are too close together, and too many children are significant risk factors for stunting [2-4].
Although these factors have been extensively studied, most studies are still unspecific and have not presented a quantitative analysis based on regional aggregate data with a comprehensive approach. In West Nusa Tenggara, local data on the relationship between the 1000 HPK component and stunting incidence is still limited, especially when several variables of mothers and parenting patterns are involved simultaneously. Therefore, this study is here to answer these gaps by leveraging the Riskesdas 2018 data, which allows for multivariate analysis by region, while providing an evidence-based policy basis [5]. This is also in line with the study of Laksono et al. (2020) which shows the existence of regional stunting disparities, as well as the importance of Riskesdas data in supporting the formulation of national strategies [6].
This research is here to provide a more detailed and contextual picture of the stunting problem in West Nusa Tenggara, Indonesia, by utilizing Riskesdas 2018 data [5]. This study aims to analyze the influence of the first 1000 days of life on the incidence of stunting in West Nusa Tenggara Province, Indonesia. The findings of this study are expected to be the basis for formulating specific and evidence-based interventions to support the program in accelerating stunting reduction in high-risk areas.
Materials and Methods
This study is an analytical observational study with a cross-sectional design. The data were archived secondary data from the 2018 Basic Health Research Survey (Riskesdas) organized by the Health Research and Development Agency (Balitbangkes), Ministry of Health of the Republic of Indonesia.
This study’s population comprised all toddlers aged 0–59 months registered in the 2018 Riskesdas data in West Nusa Tenggara Province, with an initial total of 1197 samples. After selecting according to the inclusion and exclusion criteria, a final sample of 1119 samples with complete data eligible for analysis was obtained.
The inclusion criteria in this study included complete toddler data (age, gender, birth weight, body length, weight at the time of measurement), as well as maternal data (maternal age, gestational age at that time, number of living children, pregnancy spacing, breastfeeding status, Antenatal Care (ANC) service visits, consumption of iron tablets, and Hemoglobin (Hb) level examination results during pregnancy. The exclusion criteria were incomplete data on the main variables, such as birth weight, maternal age during pregnancy, pregnancy spacing, breastfeeding practices, and nutritional status data based on height according to age. In addition, children outside the age range of 0–59 months at the time of data collection were not included because this study only focused on the toddler group. Also, we excluded children with a history of chronic diseases, congenital abnormalities, or major congenital disabilities that can significantly affect growth, such as Down syndrome or genetic metabolic diseases, based on information recorded in the child health variables in Riskesdas 2018. Likewise, the final sample did not include mothers who did not have complete information regarding pregnancy (age at pregnancy, number of living children, or pregnancy spacing)—respondents who did not follow the Riskesdas questionnaire filling protocol validly. For example, if the interview was incomplete or there was a coding discrepancy by the enumerator, they were also excluded from the analysis to maintain data validity.
In this study, the dependent variable is the incidence of stunting in toddlers, which is measured based on the standard indicator of height for age (height-for-age Z-score) with a threshold of < -2 SD, according to the World Health Organization (WHO). The independent variables include components in 1000 HPK: Maternal age during pregnancy, distance between pregnancies, number of living children, breastfeeding, ANC visits, consumption of iron tablets, and Hb examination during pregnancy.
This study was conducted from March to July 2022. Data were collected through an official application submission to the Data and Information Center of the Indonesian Ministry of Health via the official email address datin.bkpk@kemkes.go.id. After the application was approved, the researcher Paid Non-tax State Revenue (PNBP), signed a statement of data use (informed consent), and received a data set in digital format and a variable codebook as a reference in data processing. The data received had been archived and verified by government agencies as a valid source of information.
Data were analyzed using the IBM SPSS software, version 25 (IBM Corp., Armonk, NY, USA). The analysis stages include univariate analysis to describe the characteristics of respondents in the form of frequency distribution and bivariate analysis with the chi squared test to determine the relationship between independent variables and the incidence of stunting. Also, we used a multivariate analysis using logistic regression to identify the variables that have the most influence on the incidence of stunting.
Results
Based on the characteristics of the research subjects, of the 1119 toddlers (aged 0-59 months, 814(72.7%) did not experience stunting. The characteristics of the mothers showed that most were aged ≥20 years (66.7%) and aged ≤35 years (99.2%). Only 33.3% of mothers were <20 years old, and 0.8% were aged >35 years. The pregnancy interval was mostly ≥2 years (71.6%), and most mothers had ≤2 living children (71.1%). Most pregnant mothers also showed involvement in pregnancy services, with 99.7% making ANC visits, 87% undergoing Hb level checks, and 62.4% consuming ≥90 iron tablets. However, more than half of the mothers (50.8%) did not provide breast milk to their children. These data describe sociodemographic conditions during pregnancy, which are potential factors for stunting in toddlers, as detailed in Table 1.
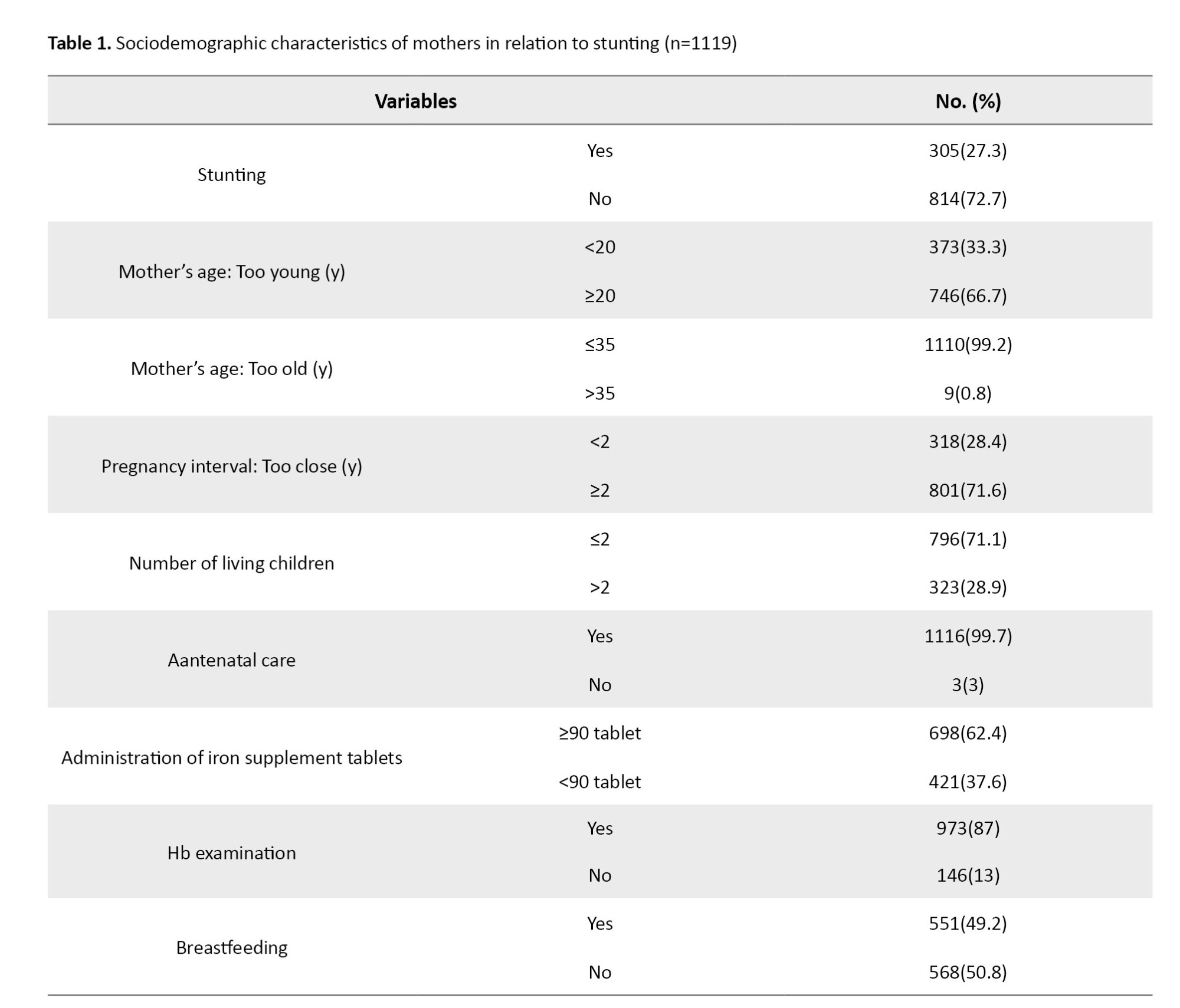
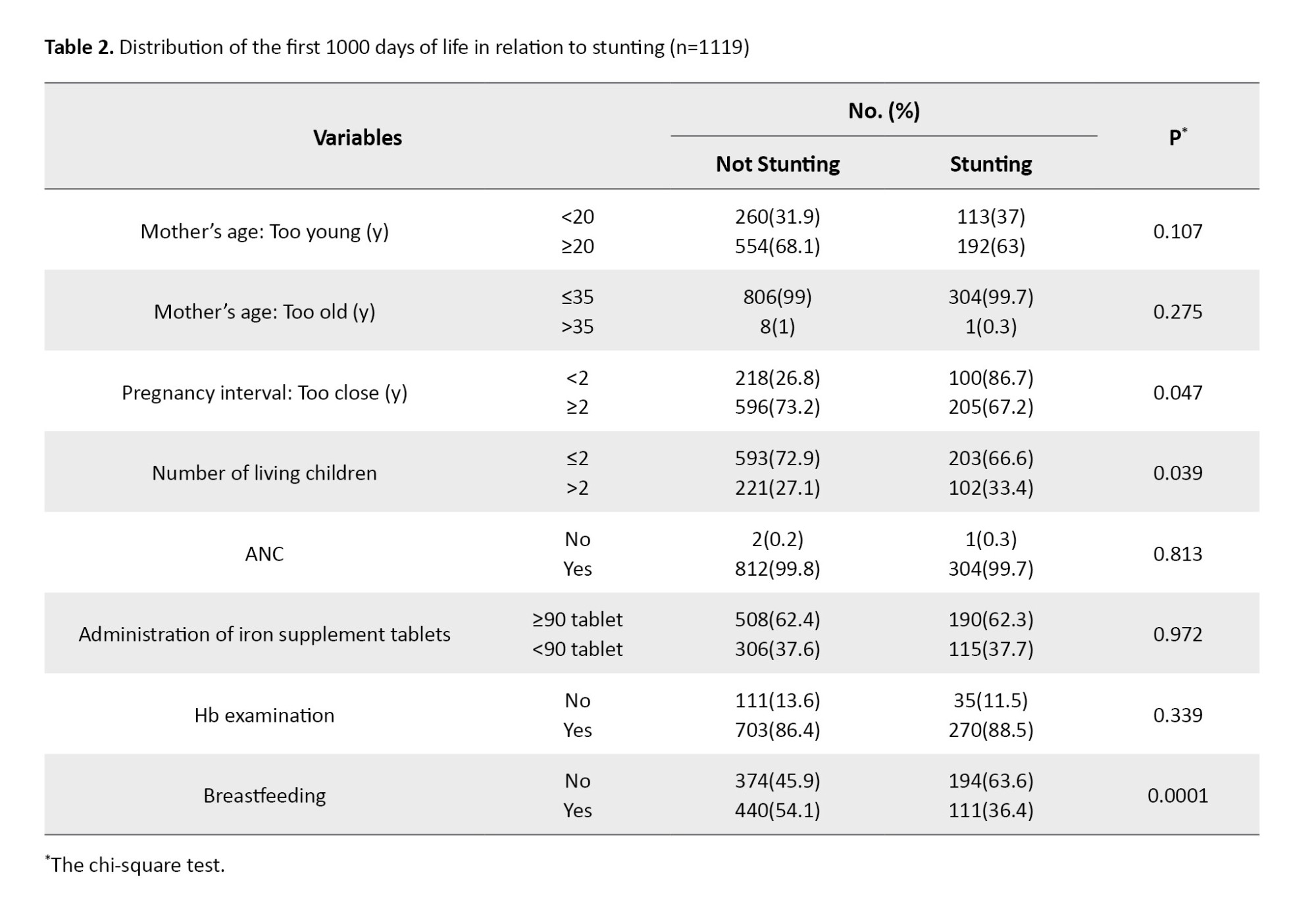
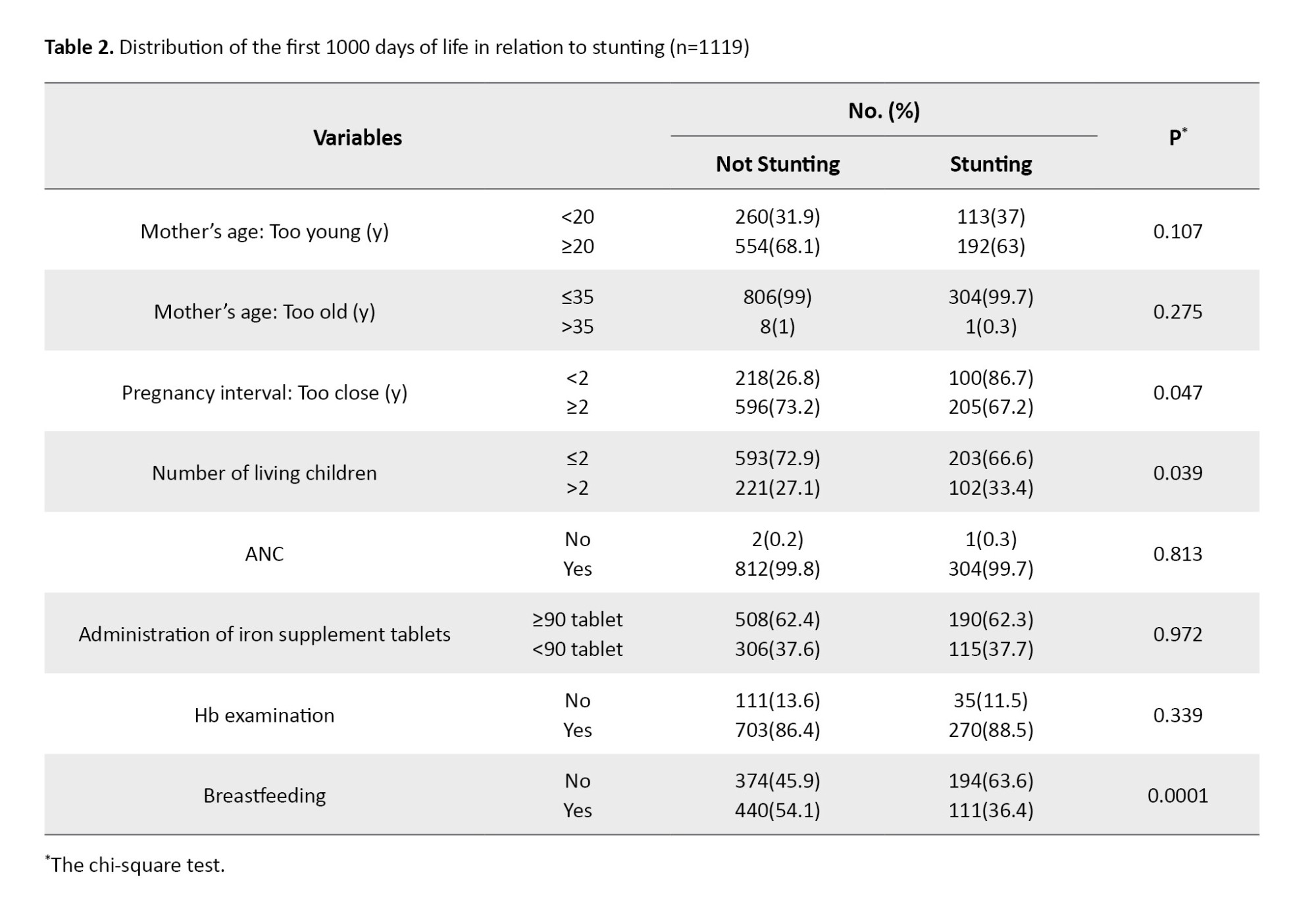
Table 2 shows the frequency distribution of factors in the first 1000 days of life (1000 HPK) related to the incidence of stunting in West Nusa Tenggara Province, Indonesia. Based on the bivariate test with the chi-square test, several variables were obtained that had a significant relationship to the incidence of stunting (P≤0.05), but several others were not significant. The pregnancy spacing variable showed a statistically significant relationship to the incidence of stunting (P=0.047). Children of mothers with a pregnancy spacing of <2 years were more likely to experience stunting (86.7%) compared to mothers with a pregnancy spacing of ≥2 years (67.2%). This finding shows that pregnancies that are too close together can increase the risk of stunting in children. Likewise, the number of living children showed a significant relationship (P=0.039), where mothers with >2 living children had a higher proportion of stunted children (33.4%) compared to mothers who had ≤2 children (27.1%). The most significant variable was breastfeeding (P=0.0001). Children who were not breastfed had a much higher proportion of stunting (63.6%) compared to children who were breastfed (36.4%). This finding confirms that breastfeeding is an important protective factor in preventing stunting. In contrast, other variables such as maternal age being too young (<20 years), maternal age being too old (>35 years), ANC visits, number of iron tablets consumed, and Hb examination did not show a statistically significant relationship with stunting (Table 2).
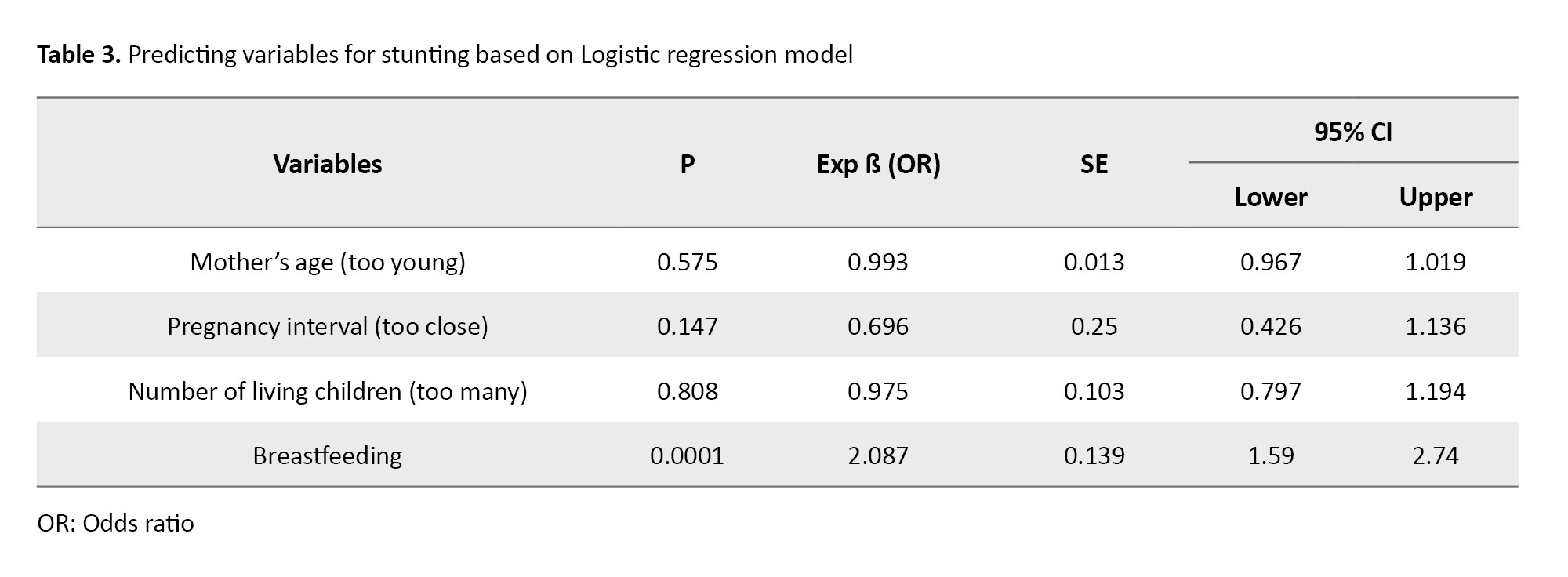
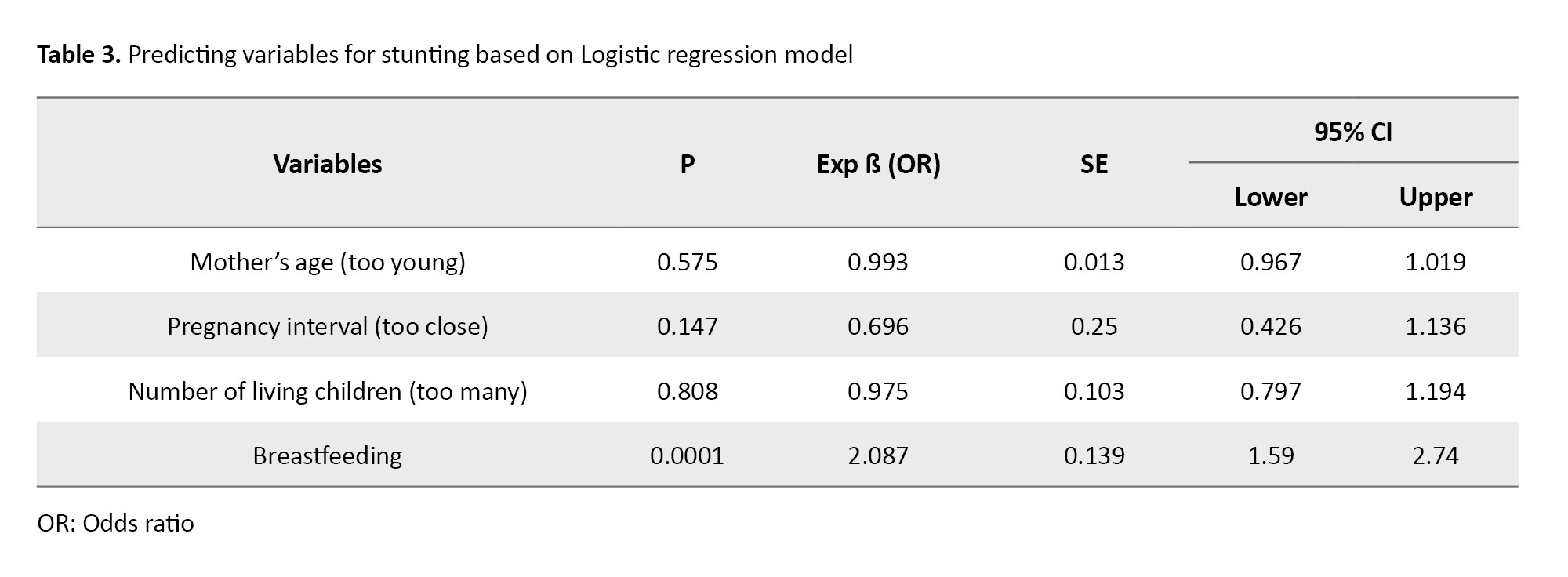
After that, we included variables with P<0.25 in the logistic regression model. Based on the binary logistic regression model (Table 3), the dominant factors in the incidence of stunting show that of the four variables entered into the model, only breastfeeding has a statistically significant effect on the incidence of stunting (P<0.05). The breastfeeding variable shows a statistically significant relationship to the incidence of stunting (OR=2.087, 95% CI; 1.590, 2.740, P=0.0001). This finding shows that toddlers who do not get breast milk are 2.08 times more likely to experience stunting than toddlers given breast milk after being controlled with other variables in the model. Meanwhile, the variable of too-close pregnancy spacing (<2 years) shows that it is not statistically significant in the model. Similarly, the number of living children >2 also indicated that it was not significant.
Discussion
The results of this study confirm that the HPK period is a critical phase in determining the nutritional status and growth of children, especially related to the incidence of stunting in West Nusa Tenggara Province, Indonesia. Maternal factors such as gestational age, spacing between pregnancies, and breastfeeding practices have been shown to contribute significantly to the risk of stunting.
Maternal age at the time of pregnancy was found to be a crucial factor, especially pregnancy at the age of <20 years and >35 years. Adolescent girls who marry and become pregnant too early are at risk or tend to face reproductive health, psychosocial, and economic challenges that impact the health of the fetus and the child they give birth [7]. This finding aligns with another study, which found that adolescent gestational age correlates with low birth weight and infant length, which does not meet WHO standards [8].
Meanwhile, a pregnancy spacing of <24 months increases the risk of stunting due to insufficient maternal nutritional recovery time. Pregnancy that occurs too soon after a previous birth does not give the mother’s body enough time to restore its nutritional reserves, thereby increasing the risk of chronic energy deficiency and growth complications in subsequent children. Several studies have linked short birth intervals to low birth weight and stunting in developing countries [9-11]. Data from other developing countries also support these findings. A multilevel study in Cambodia concluded that short birth intervals significantly determined poor nutritional status, recurrent infections, and limited maternal and child health services [12]. Therefore, postnatal contraceptive practices and family planning education are essential to prevent stunting in the context of the first 1000 days of life program.
Although the coverage of ANC visits and consumption of iron tablets ≥90 tablets have shown an increasing trend, the effectiveness of this program in reducing stunting rates has not been optimal, probably due to the low quality of counseling provided during ANC. Nutritional counseling during ANC has been shown to improve maternal compliance in consuming iron supplements, prevent anemia and low birth weight babies, and ultimately prevent fetal growth disorders [13, 14].
The most dominant factor in this study was the low coverage of exclusive breastfeeding. Breast milk is the primary source of nutrition that not only meets the needs of infants but also provides immunological protection. Exclusive breastfeeding has been proven effective in reducing the risk of stunting globally [15]. On the other hand, giving complementary foods too early increases the risk of digestive infections and disrupts child growth [16, 17].
Infants with a history of low birth weight who do not receive exclusive breastfeeding have a greater risk of stunting [18]. In addition, the lack of maternal knowledge about nutrition and low consumption of animal protein, especially in coastal and remote areas, are also factors that worsen children’s nutritional conditions during the HPK period [19, 20]. Therefore, community-based intervention models such as family assistance based on local culture have been proven effective in reducing stunting rates [21].
Analytically, the findings in this study strengthen the theory that stunting is not only a matter of acute malnutrition but is the result of the accumulation of various structural, social, and biological determinants that occur before pregnancy. Low coverage of exclusive breastfeeding, pregnancy at an inappropriate age, and unpreparedness in early care are the main interrelated risk factors. In other words, preventing stunting requires a multi-sector and multi-system approach from the household level, health services, and cross-sector policies emphasizing maternal education and empowerment.
This study has several limitations, such as using 2018 Riskesdas data, which may not reflect current conditions, and limited variables such as sanitation or maternal employment status. In addition, the study was only conducted in one province, so the results cannot be generalized widely. However, these findings reinforce the importance of interventions during the first 1000 days of life in preventing stunting.
Specific findings indicate that most children do not experience stunting, and exclusive breastfeeding emerged as a dominant factor influencing the incidence of stunting during the 1000 HPK period.
Based on these findings, we recommend strengthening cultural and community-based exclusive breastfeeding education and promotion programs, for example, through pregnancy classes or peer groups for breastfeeding mothers, and the need to strengthen the social system so that breastfeeding practices become part of the community norm. For example, mothers feel ashamed if they do not provide exclusive breastfeeding or are motivated to breastfeed because of awareness, not coercion. Improving the quality of ANC services, monitoring child nutrition, and utilizing information technology are also expected to accelerate the achievement of national stunting reduction targets. A cross-sectoral approach starting from the village is critical to build collective awareness in preventing stunting in infants aged 0-6 months, from family planning to household-based nutrition interventions, which is crucial to ensure the first 1000 days of life. This strategy is expected to strengthen breastfeeding culture as part of sustainable nutrition interventions..
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for this study was obtained from the Health Research Ethics Committee, Faculty of Medicine, University of Mataram, Mataram, Indonesia (Code: 138/UN18.F7/ETIK/2022). The chief researcher signed informed consent for secondary data from the Datin BKPK of the Indonesian Ministry of Health.
Funding
This study was a collaboration between the West Nusa Tenggara (NTB) Province BKKBN and Mataram Health Polytechnic of the Ministry of Health (Poltekkes Kemenkes Mataram). It was funded by the NTB Province BKKBN for the 2022 fiscal year.
Authors' contributions
Conceptualization, study design, data analysis, interpretation, and writing: Linda Meliati; Obtaining funds, collection, and assembly of statistical data expertise: Sudarmi Sudarmi; Administrative, technical, or logistical support: St. Halimatusyaadiah; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors offer thanks to Health Research and Development Agency (Balitbangkes), Ministry of Health of the Republic of Indonesia for their cooperation.
References
Stunting is still a severe public health problem in Indonesia. This condition not only inhibits children’s physical growth but also has an impact on children’s cognitive development, immunity, and productivity in the future. Data from the 2022 Indonesian Nutritional Status Study (SSGI) shows that the national prevalence of stunting is 21.6%, while West Nusa Tenggara (NTB) Province is ranked as one of 12 priority provinces with the highest prevalence nationally, namely 31.4% [1]. This figure shows that the intervention efforts that have been carried out have not effectively addressed the factors that play a role in stunting in the area. One of the most crucial periods in preventing stunting is the first 1000 days of life (1000 HPK), namely from pregnancy to the age of two years. During this period, organs and body systems grow rapidly, so nutritional imbalances or health disorders can have permanent impacts. Various studies have shown that suboptimal breastfeeding practices, mothers who are too young when pregnant, pregnancies that are too close together, and too many children are significant risk factors for stunting [2-4].
Although these factors have been extensively studied, most studies are still unspecific and have not presented a quantitative analysis based on regional aggregate data with a comprehensive approach. In West Nusa Tenggara, local data on the relationship between the 1000 HPK component and stunting incidence is still limited, especially when several variables of mothers and parenting patterns are involved simultaneously. Therefore, this study is here to answer these gaps by leveraging the Riskesdas 2018 data, which allows for multivariate analysis by region, while providing an evidence-based policy basis [5]. This is also in line with the study of Laksono et al. (2020) which shows the existence of regional stunting disparities, as well as the importance of Riskesdas data in supporting the formulation of national strategies [6].
This research is here to provide a more detailed and contextual picture of the stunting problem in West Nusa Tenggara, Indonesia, by utilizing Riskesdas 2018 data [5]. This study aims to analyze the influence of the first 1000 days of life on the incidence of stunting in West Nusa Tenggara Province, Indonesia. The findings of this study are expected to be the basis for formulating specific and evidence-based interventions to support the program in accelerating stunting reduction in high-risk areas.
Materials and Methods
This study is an analytical observational study with a cross-sectional design. The data were archived secondary data from the 2018 Basic Health Research Survey (Riskesdas) organized by the Health Research and Development Agency (Balitbangkes), Ministry of Health of the Republic of Indonesia.
This study’s population comprised all toddlers aged 0–59 months registered in the 2018 Riskesdas data in West Nusa Tenggara Province, with an initial total of 1197 samples. After selecting according to the inclusion and exclusion criteria, a final sample of 1119 samples with complete data eligible for analysis was obtained.
The inclusion criteria in this study included complete toddler data (age, gender, birth weight, body length, weight at the time of measurement), as well as maternal data (maternal age, gestational age at that time, number of living children, pregnancy spacing, breastfeeding status, Antenatal Care (ANC) service visits, consumption of iron tablets, and Hemoglobin (Hb) level examination results during pregnancy. The exclusion criteria were incomplete data on the main variables, such as birth weight, maternal age during pregnancy, pregnancy spacing, breastfeeding practices, and nutritional status data based on height according to age. In addition, children outside the age range of 0–59 months at the time of data collection were not included because this study only focused on the toddler group. Also, we excluded children with a history of chronic diseases, congenital abnormalities, or major congenital disabilities that can significantly affect growth, such as Down syndrome or genetic metabolic diseases, based on information recorded in the child health variables in Riskesdas 2018. Likewise, the final sample did not include mothers who did not have complete information regarding pregnancy (age at pregnancy, number of living children, or pregnancy spacing)—respondents who did not follow the Riskesdas questionnaire filling protocol validly. For example, if the interview was incomplete or there was a coding discrepancy by the enumerator, they were also excluded from the analysis to maintain data validity.
In this study, the dependent variable is the incidence of stunting in toddlers, which is measured based on the standard indicator of height for age (height-for-age Z-score) with a threshold of < -2 SD, according to the World Health Organization (WHO). The independent variables include components in 1000 HPK: Maternal age during pregnancy, distance between pregnancies, number of living children, breastfeeding, ANC visits, consumption of iron tablets, and Hb examination during pregnancy.
This study was conducted from March to July 2022. Data were collected through an official application submission to the Data and Information Center of the Indonesian Ministry of Health via the official email address datin.bkpk@kemkes.go.id. After the application was approved, the researcher Paid Non-tax State Revenue (PNBP), signed a statement of data use (informed consent), and received a data set in digital format and a variable codebook as a reference in data processing. The data received had been archived and verified by government agencies as a valid source of information.
Data were analyzed using the IBM SPSS software, version 25 (IBM Corp., Armonk, NY, USA). The analysis stages include univariate analysis to describe the characteristics of respondents in the form of frequency distribution and bivariate analysis with the chi squared test to determine the relationship between independent variables and the incidence of stunting. Also, we used a multivariate analysis using logistic regression to identify the variables that have the most influence on the incidence of stunting.
Results
Based on the characteristics of the research subjects, of the 1119 toddlers (aged 0-59 months, 814(72.7%) did not experience stunting. The characteristics of the mothers showed that most were aged ≥20 years (66.7%) and aged ≤35 years (99.2%). Only 33.3% of mothers were <20 years old, and 0.8% were aged >35 years. The pregnancy interval was mostly ≥2 years (71.6%), and most mothers had ≤2 living children (71.1%). Most pregnant mothers also showed involvement in pregnancy services, with 99.7% making ANC visits, 87% undergoing Hb level checks, and 62.4% consuming ≥90 iron tablets. However, more than half of the mothers (50.8%) did not provide breast milk to their children. These data describe sociodemographic conditions during pregnancy, which are potential factors for stunting in toddlers, as detailed in Table 1.
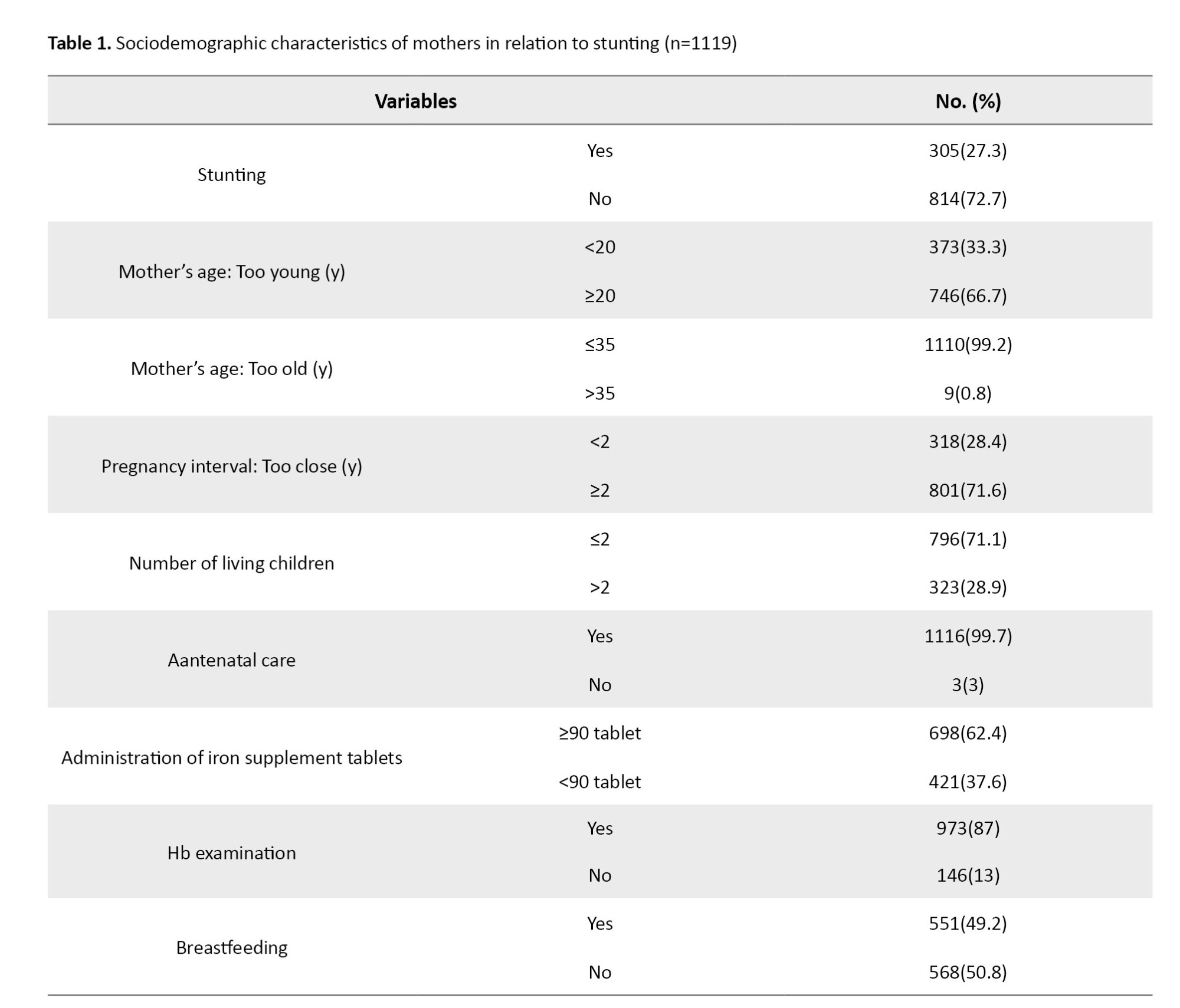
Table 2 shows the frequency distribution of factors in the first 1000 days of life (1000 HPK) related to the incidence of stunting in West Nusa Tenggara Province, Indonesia. Based on the bivariate test with the chi-square test, several variables were obtained that had a significant relationship to the incidence of stunting (P≤0.05), but several others were not significant. The pregnancy spacing variable showed a statistically significant relationship to the incidence of stunting (P=0.047). Children of mothers with a pregnancy spacing of <2 years were more likely to experience stunting (86.7%) compared to mothers with a pregnancy spacing of ≥2 years (67.2%). This finding shows that pregnancies that are too close together can increase the risk of stunting in children. Likewise, the number of living children showed a significant relationship (P=0.039), where mothers with >2 living children had a higher proportion of stunted children (33.4%) compared to mothers who had ≤2 children (27.1%). The most significant variable was breastfeeding (P=0.0001). Children who were not breastfed had a much higher proportion of stunting (63.6%) compared to children who were breastfed (36.4%). This finding confirms that breastfeeding is an important protective factor in preventing stunting. In contrast, other variables such as maternal age being too young (<20 years), maternal age being too old (>35 years), ANC visits, number of iron tablets consumed, and Hb examination did not show a statistically significant relationship with stunting (Table 2).
After that, we included variables with P<0.25 in the logistic regression model. Based on the binary logistic regression model (Table 3), the dominant factors in the incidence of stunting show that of the four variables entered into the model, only breastfeeding has a statistically significant effect on the incidence of stunting (P<0.05). The breastfeeding variable shows a statistically significant relationship to the incidence of stunting (OR=2.087, 95% CI; 1.590, 2.740, P=0.0001). This finding shows that toddlers who do not get breast milk are 2.08 times more likely to experience stunting than toddlers given breast milk after being controlled with other variables in the model. Meanwhile, the variable of too-close pregnancy spacing (<2 years) shows that it is not statistically significant in the model. Similarly, the number of living children >2 also indicated that it was not significant.
Discussion
The results of this study confirm that the HPK period is a critical phase in determining the nutritional status and growth of children, especially related to the incidence of stunting in West Nusa Tenggara Province, Indonesia. Maternal factors such as gestational age, spacing between pregnancies, and breastfeeding practices have been shown to contribute significantly to the risk of stunting.
Maternal age at the time of pregnancy was found to be a crucial factor, especially pregnancy at the age of <20 years and >35 years. Adolescent girls who marry and become pregnant too early are at risk or tend to face reproductive health, psychosocial, and economic challenges that impact the health of the fetus and the child they give birth [7]. This finding aligns with another study, which found that adolescent gestational age correlates with low birth weight and infant length, which does not meet WHO standards [8].
Meanwhile, a pregnancy spacing of <24 months increases the risk of stunting due to insufficient maternal nutritional recovery time. Pregnancy that occurs too soon after a previous birth does not give the mother’s body enough time to restore its nutritional reserves, thereby increasing the risk of chronic energy deficiency and growth complications in subsequent children. Several studies have linked short birth intervals to low birth weight and stunting in developing countries [9-11]. Data from other developing countries also support these findings. A multilevel study in Cambodia concluded that short birth intervals significantly determined poor nutritional status, recurrent infections, and limited maternal and child health services [12]. Therefore, postnatal contraceptive practices and family planning education are essential to prevent stunting in the context of the first 1000 days of life program.
Although the coverage of ANC visits and consumption of iron tablets ≥90 tablets have shown an increasing trend, the effectiveness of this program in reducing stunting rates has not been optimal, probably due to the low quality of counseling provided during ANC. Nutritional counseling during ANC has been shown to improve maternal compliance in consuming iron supplements, prevent anemia and low birth weight babies, and ultimately prevent fetal growth disorders [13, 14].
The most dominant factor in this study was the low coverage of exclusive breastfeeding. Breast milk is the primary source of nutrition that not only meets the needs of infants but also provides immunological protection. Exclusive breastfeeding has been proven effective in reducing the risk of stunting globally [15]. On the other hand, giving complementary foods too early increases the risk of digestive infections and disrupts child growth [16, 17].
Infants with a history of low birth weight who do not receive exclusive breastfeeding have a greater risk of stunting [18]. In addition, the lack of maternal knowledge about nutrition and low consumption of animal protein, especially in coastal and remote areas, are also factors that worsen children’s nutritional conditions during the HPK period [19, 20]. Therefore, community-based intervention models such as family assistance based on local culture have been proven effective in reducing stunting rates [21].
Analytically, the findings in this study strengthen the theory that stunting is not only a matter of acute malnutrition but is the result of the accumulation of various structural, social, and biological determinants that occur before pregnancy. Low coverage of exclusive breastfeeding, pregnancy at an inappropriate age, and unpreparedness in early care are the main interrelated risk factors. In other words, preventing stunting requires a multi-sector and multi-system approach from the household level, health services, and cross-sector policies emphasizing maternal education and empowerment.
This study has several limitations, such as using 2018 Riskesdas data, which may not reflect current conditions, and limited variables such as sanitation or maternal employment status. In addition, the study was only conducted in one province, so the results cannot be generalized widely. However, these findings reinforce the importance of interventions during the first 1000 days of life in preventing stunting.
Specific findings indicate that most children do not experience stunting, and exclusive breastfeeding emerged as a dominant factor influencing the incidence of stunting during the 1000 HPK period.
Based on these findings, we recommend strengthening cultural and community-based exclusive breastfeeding education and promotion programs, for example, through pregnancy classes or peer groups for breastfeeding mothers, and the need to strengthen the social system so that breastfeeding practices become part of the community norm. For example, mothers feel ashamed if they do not provide exclusive breastfeeding or are motivated to breastfeed because of awareness, not coercion. Improving the quality of ANC services, monitoring child nutrition, and utilizing information technology are also expected to accelerate the achievement of national stunting reduction targets. A cross-sectoral approach starting from the village is critical to build collective awareness in preventing stunting in infants aged 0-6 months, from family planning to household-based nutrition interventions, which is crucial to ensure the first 1000 days of life. This strategy is expected to strengthen breastfeeding culture as part of sustainable nutrition interventions..
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for this study was obtained from the Health Research Ethics Committee, Faculty of Medicine, University of Mataram, Mataram, Indonesia (Code: 138/UN18.F7/ETIK/2022). The chief researcher signed informed consent for secondary data from the Datin BKPK of the Indonesian Ministry of Health.
Funding
This study was a collaboration between the West Nusa Tenggara (NTB) Province BKKBN and Mataram Health Polytechnic of the Ministry of Health (Poltekkes Kemenkes Mataram). It was funded by the NTB Province BKKBN for the 2022 fiscal year.
Authors' contributions
Conceptualization, study design, data analysis, interpretation, and writing: Linda Meliati; Obtaining funds, collection, and assembly of statistical data expertise: Sudarmi Sudarmi; Administrative, technical, or logistical support: St. Halimatusyaadiah; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors offer thanks to Health Research and Development Agency (Balitbangkes), Ministry of Health of the Republic of Indonesia for their cooperation.
References
- Ministry of Health of the Republic of Indonesia. [BUKU SAKU Hasil Survei Status Gizi Indonesia (SSGI) 2022 (Indonesian). Jakarta: Ministry of Health of the Republic of Indonesia; 2022. [Link]
- Saleh A, Syahrul S, Hadju V, Andriani I, Restika I. Role of maternal in preventing stunting: A systematic review. Gac Sanit. 2021; 35(Suppl 2):S576-82. [DOI:10.1016/j.gaceta.2021.10.087] [PMID]
- Renyoet BS, Dary D, Nugroho CVR. Literature review: Intervention on adolescent girls in 8000 first days of life (HPK) as stunting prevention in future generations. Amerta Nutr. 2023; 7:295-306. [DOI:10.20473/amnt.v7i2.2023.295-306]
- Aramico B, Huriyati E, Dewi FS. Determinant factors of stunting and effectiveness of nutrition, information, education interventions to prevent stunting in the first 1000 days of life: A systematic review. In: The 7th International Conference On Public Health. 2020; 5(1): 285-300. [DOI: 10.26911/the7thicph-FP.03.30]
- Ministry of Health of the Republic of Indonesia. 2018 National Riskesdas Report. Jakarta: Ministry of Health of the Republic of Indonesia; 2018. [Link]
- Laksono AD, Kusrini I. Regional disparities of stunted toddler in Indonesia. Indian J Forensic Med Toxicol. 2020; 14(3): 1952-6. [DOI: 10.37506/ijfmt.v14i3.10706]
- Angellina S, Putri RY, NR PH, Indraini F. [Evaluation of the implementation of the stunting prevention program in the first 1,000 days of life in Agam regency (Indonesian). J Andalas Medica. 2025; 3(1):63-71. [Link]
- Sri Nurlaily Z, Agustini RD, Nurhidayah. Stunting Among Children Aged 6-59 Months in Gorontalo, Indonesia. J Kesehatan Masyarakat. 2025; 20(3):523-33. [DOI:10.15294/kemas.v20i3.13539]
- Čvorović J. The association between maternal age at childbirth and child nutritional outcomes: A cross-sectional study from Serbian Roma Communities. Glob Pediatr Health. 2024; 11:2333794X241298831. [DOI:10.1177/2333794X241298831] [PMID]
- Mohamoud JH, Mahmoud AA, Adan RA, Mohamed AMS, Adam MH. Magnitude of low birth weight and associated factors among newborns delivered in public hospitals of Benadir Region, Somalia: A facility-based cross-sectional study. Sage Open Pediatr. 2025; 12:30502225251321023. [DOI:10.1177/30502225251321023] [PMID]
- Burki AA. Assessing relative significance of key risk factors for child undernutrition: Evidence from Pakistan [preprint]. 2025. [DOI:10.21203/rs.3.rs-4358901/v1]
- Mohamed Gouda Mohamed Mohamed, A. The state of malnutrition and its determinants among under-five children in Cambodia: A comprehensive multilevel analysis on Cambodian demographic health survey (CDHS-2021/2022). 2024. [Link]
- Mizawati A, Effendi N, Sulastri D, Purna RS. Anemia-free strategies and antenatal care services in stunting prevention. BKM Public Health Community Med. 2024; 40(07):e6806. [DOI:10.22146/bkm.v40i07.6806]
- Palimbo A, Bamegawati IM, Mahdiyah D, Herawati A, Hidayati Rahman L, Fariana VR, et al. Overcoming anemia in prospective brides and grooms as an effort to prevent stunting. Health Sci Int J. 2024; 2(2):115-22. [DOI:10.71357/hsij.v2i2.28]
- Zhang L, Liu HJ, Li P, Liu Y, Zhang T, Zhu JY, et al. Association of early-term birth and breastfeeding practices with nutritional outcomes in singleton term infants: A multicenter cross-sectional study. Int Breastfeed J. 2024; 19(1):46. [DOI:10.1186/s13006-024-00653-w] [PMID]
- Busert-Sebela L, Cortina-Borja M, Paudel V, Devakumar D, Wells JCK, Manandhar DS, et al. Determinants of infant growth in a birth cohort in the Nepal Plains. Matern Child Nutr. 2025; 21(3):e70004. [DOI:10.1111/mcn.70004] [PMID]
- Amjad S, Ashraf S, Mohamed J, Leng SK, Rashid N, Rafiq S, et al. Nutritional assessment of infants in Pakistan: Impact of breastfeeding practices on growth-insights from the Lahore birth cohort study. Rom J Diabetes Nutr Metab Dis. 2024; 31:1048-59. [Link]
- Hurun A, Yuni SA, Ilya K, Nurul P, Sulastyawat, Supono, et al. Determinants of stunting risk factors for toddlers aged 6-36 months in the Malang regency, Indonesia. Afr J Food Agric Nutr Dev. 2024; 24(11):24912-30. [Link]
- Fatiha A, Putri SA, Ramahdani S, Sabrina Z, Zuhra F. [Coastal Communities' Knowledge of Stunting and the Importance of Nutrition for Children (Indonesian)]. J Health Educ Law Inf Humanit. 2025; 1:509-15. [DOI:10.57235/helium.v2i1.5232]
- Retni R, Arfianti M. [Pentingnya protein hewani dalam mencegah stunting pada balita: Systematic review (Indonesian)]. J Ners. 2025; 9(2):1462-70. [Link]
- Muchlashin A. [Community-based stunting reduction: A pilot case study of Sidoluhur Village, Sleman Regency (Indonesian)]. J Community Dev Disaster Manage. 2025, 7.1: 339-351. [Link]
Article Type : Research |
Subject:
General
Received: 2023/02/15 | Accepted: 2024/06/30 | Published: 2025/06/10
Received: 2023/02/15 | Accepted: 2024/06/30 | Published: 2025/06/10
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |