Fri, Jan 30, 2026
Volume 34, Issue 4 (9-2024)
JHNM 2024, 34(4): 301-308 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Akbari Z, Jesmi A A, Mahdavifar N, Taj A, Mozari S. Relationship of the Critical Care Pain Observation Tool Score With the APACHE II Score, Sedation Level, and Ventilation Parameters in Critically Ill Patients Under Mechanical Ventilation. JHNM 2024; 34 (4) :301-308
URL: http://hnmj.gums.ac.ir/article-1-2088-en.html
URL: http://hnmj.gums.ac.ir/article-1-2088-en.html
1- MSc Student of Critical Care Nursing, Student Research Committee, Sabzevar University of Medical Sciences, Sabzevar, Iran.
2- Assistant Professor, Department of Nursing Education, Iranian Research Centre on Healthy Aging, Sabzevar University of Medical Sciences, Sabzevar, Iran. ,jesmiaa@gmail.com
3- Instructor, Department of Epidemiology and Biostatistics, Sabzevar University of Medical Sciences, Sabzevar, Iran.
4- Assistant Professor, Department of Para Medicine, Non-Communicable Diseases Research Center, Sabzevar University of Medical Sciences, Sabzevar, Iran.
5- Assistant Professor of Critical Care Medicine, Department of Anesthesiology, School of Medicine, Sabzevar University of Medical Sciences, Sabzevar, Iran.
2- Assistant Professor, Department of Nursing Education, Iranian Research Centre on Healthy Aging, Sabzevar University of Medical Sciences, Sabzevar, Iran. ,
3- Instructor, Department of Epidemiology and Biostatistics, Sabzevar University of Medical Sciences, Sabzevar, Iran.
4- Assistant Professor, Department of Para Medicine, Non-Communicable Diseases Research Center, Sabzevar University of Medical Sciences, Sabzevar, Iran.
5- Assistant Professor of Critical Care Medicine, Department of Anesthesiology, School of Medicine, Sabzevar University of Medical Sciences, Sabzevar, Iran.
Keywords: Pain, Critical care, Ventilation, ICU, Acute physiology and chronic health evaluation (APACHE II)
Full-Text [PDF 478 kb]
(457 Downloads)
| Abstract (HTML) (1018 Views)
Full-Text: (423 Views)
Introduction
Pain is a persistent concern and a common symptom in critically ill patients [1]. Majority of patients admitted to the intensive care units (ICUs), especially those receiving mechanical ventilation, suffer from pain [2]. Pain is described as an unpleasant sensory and emotional experience that is called the “fifth vital sign” by the American Pain Society (APS) [3]. It has been reported that 50-71% of patients admitted to the ICUs experience undiagnosed or untreated pain, and annual statistics suggest that 71% of these patients recall this pain after discharge [4]. Moreover, it is estimated at 30% of patients experience pain while resting, and this rate increases to 50% during nursing procedures. According to the literature, more than 82% of the patients who are discharged from the ICU recall the pain and discomfort caused by the endotracheal intubation [5]. Individuals who have frightening memories of pain are at a higher risk of posttraumatic stress disorder, which affects 34-38% of patients discharged from the ICU [6]. Critically ill patients are often unable to communicate effectively due to their severe condition, mechanical ventilation, sedative/analgesic drug prescription, and decreased consciousness [7].
Inability to report pain is a major challenge for proper pain assessment or management, which is associated with a risk of underrated and untreated pain [8]. Pain assessment and management in critically ill patients are unique challenges for physicians and nurses [9]. The ICU nurses are mostly unaware of proper and objective pain assessment [10], such that 35-55% of nurses estimate patients’ pain less than the real rate. Management of analgesia and sedation in the ICU requires evaluation and monitoring of key parameters in order to detect pain and agitation, and quantify sedation [11]. Unfortunately, 64% of patients do not receive any medication before and during painful procedures [12]. Ineffective pain control is caused by several factors, such as improper measure of pain, inadequate professional training, and pain control not based on evidence [13]. Determining the possible influential factors in pain is a reliable approach to pain measurement in patients who are unable to report pain [14]. According to the guidelines of the American Society for Pain Management Nursing (ASPMN) and the Society of Critical Care Medicine (SCCM), behavioral indicators are can help with the diagnosis of pain in patients who are unable to express pain. Some of these behavioral indicators recommended by the SCCM are the behavioural pain scale (BPS) and critical-care pain observation tool (CPOT) [15]. The value of using each of these scales in patients with different clinical conditions should be carefully evaluated; some clinical experts have even criticized the applicability and ease of implementation of these tools [16].
Effective and adequate pain control in ICUs is associated with a reduction in mechanical ventilation time, shorter length of stay, and lower morbidity and mortality rates. In some health centers that provide care to critically ill patients, pain assessment is performed inadequately or is not performed, making it difficult to manage pain in these patients adequately [17]. Pain management still poses a significant challenge for doctors, nurses, and other medical staff [18]. Considering that pain management is a multidimensional process and pain assessment tools are one-dimensional, it is necessary to check the correlation of these tools with some scales that predict the patient’s condition and affect the pain level. The present study aimed to evaluate the correlation of the scores of the CPOT, the acute physiology and chronic health evaluation (APACHE II) scale, and the Ramsay sedation scale (RSS) with ventilation parameters to provide insight to healthcare professionals for the effective diagnosis and treatment of pain in patients undergoing mechanical ventilation.
Materials and Methods
This cross-sectional study was conducted on 40 intubated patients under mechanical ventilation at the trauma ICU of a hospital in Sabzevar, Iran. Data collection was performed using an observational approach from November 2020 to May 2021. The samples were selected using a convenience sampling method. The minimum sample size was determined 26, according to a pilot study, and considering the correlation coefficient of 0.74 between pain and APACHE II scores and β=80% at a confidence interval of 0.95. Due to the possibility of 50% sample dropout, the sample size was increased to 40. The inclusion criteria were age ≥18 years, a Glasgow coma scale (GCS) score of 5-8, having an artificial airway, and undergoing mechanical ventilation for more than 48 hours. The exclusion criteria were death in the first 24 hours, extubation, and transferring to other wards.
A demographic questionnaire was used to collect patient demographics and health information from the medical records. The recorded information included age, gender, level of education, place of residence, history of addiction, surgical diagnosis, underlying disease, use of sedative drugs one hour before painful procedures, use of narcotics one hour before painful procedures, and the information related to the respiratory status (ventilation mode, minute ventilation, peak inspiratory pressure, and Spo2/Fio2 ratio). After obtaining written informed consent from the legal guardians of the patients, the demographic form was completed by the researcher who was not a part of the treatment team.
The APACHE II scale was also used for data collection, which is a scoring system for ICU mortality rate calculated within the first 24 hours of admission to the ICU. This scale consists of three components. The first component is the acute physiology score (APS) which is obtained from 12 clinical measures in the first 24 hours of admission to the ICU. These measures included: internal temperature, heart rate, mean arterial pressure, respiratory rate, oxygenation, arterial pH, serum sodium, serum potassium, creatinine, hematocrit, white blood cell (WBC) and GCS. The second component is the age point, ranged from 1 to 6 for patients older than 44 years. The third component is the chronic health point for patients with severe and chronic disorders such as the heart, lung, kidney, liver, and immune system disorders. The APACHE score ranges from 0 to 71, with higher scores indicating more severe disease and a higher risk of mortality. Validity and reliability of the Persian version of this tool have been confirmed in Bahtouee et al.’s study [19].
The RSS was another tool used in this study, which measures the level of sedation on a scale from 1 to 6 as 1=anxious and agitated, restless or both; 2= cooperative, alert and calm; 3= confused but responding to commands; 4= rapid and intense response to stimuli; 5= slow response to stimuli; and 6= No responsive. The validity and reliability of the Persian version of this tool have been confirmed by Tabrizi et al in Iran [20].
The CPOT was used to assess pain intensity. It consists of four dimensions, including facial expression, body movement, muscle tension, and compliance with ventilator (in patients with an endotracheal tube) or vocalization (in patients without an endotracheal tube). Each item is scored from 0 to 2. The total CPOT score ranges from 0 (no pain) to 8 (maximum pain). In the present study, the Persian version of this tool was used [21], before the painful interventions. Pain intensity was measured twice in the morning shift and on the first, second and third days of admission to the ICU (6 times in total). The rest interval was one minute before painful procedures of positioning and intratracheal suctioning (T1 or rest time) and during the painful procedure (T2). By summing up the scores of the items, the final T1 and T2 values were determined. In this study, the selected procedures were endotracheal intubation, endotracheal suctioning, and changing position. During the pain intensity assessment, the ventilation parameters were recorded according to ventilator settings for each patient.
Data analysis was performed in SPSS software, version 24 using descriptive statistics to describe the data and Spearman’s correlation test to assess the correlation between the study variables, and the Mann-Whitney U test. The significance level was set at 0.05.
Results
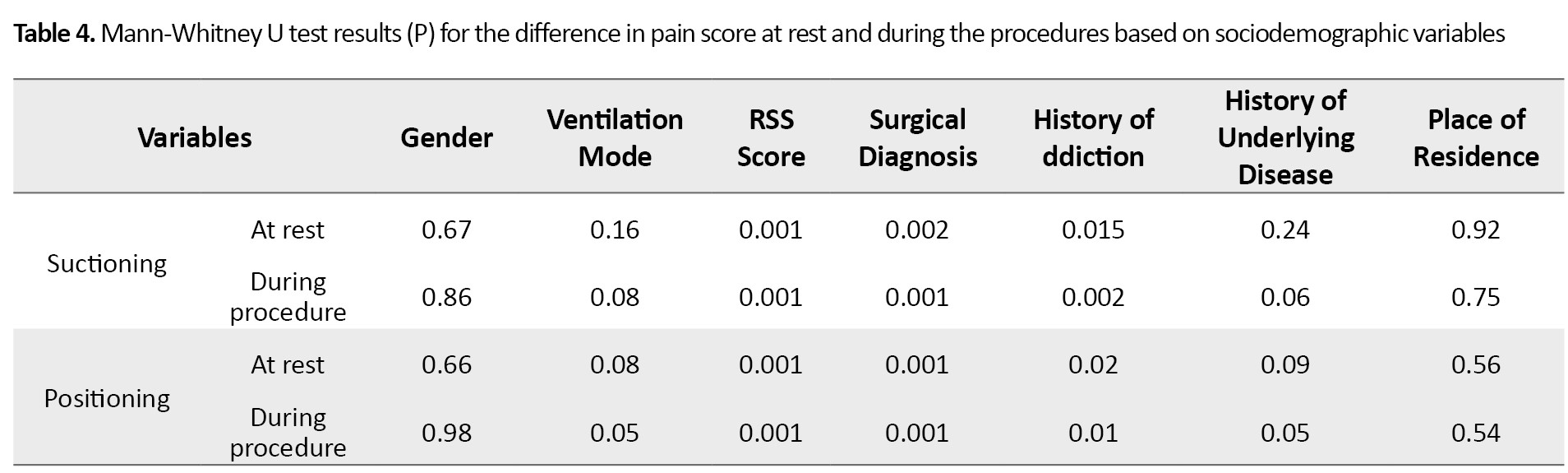
Participants included 87.5% males (n=35) and 12.5% females (n=5). Their mean age was 42.80±17.12 years. In addition, 80% were married, and 62.5% were urban residents. Table 1 shows the demographic characteristics of the patients.
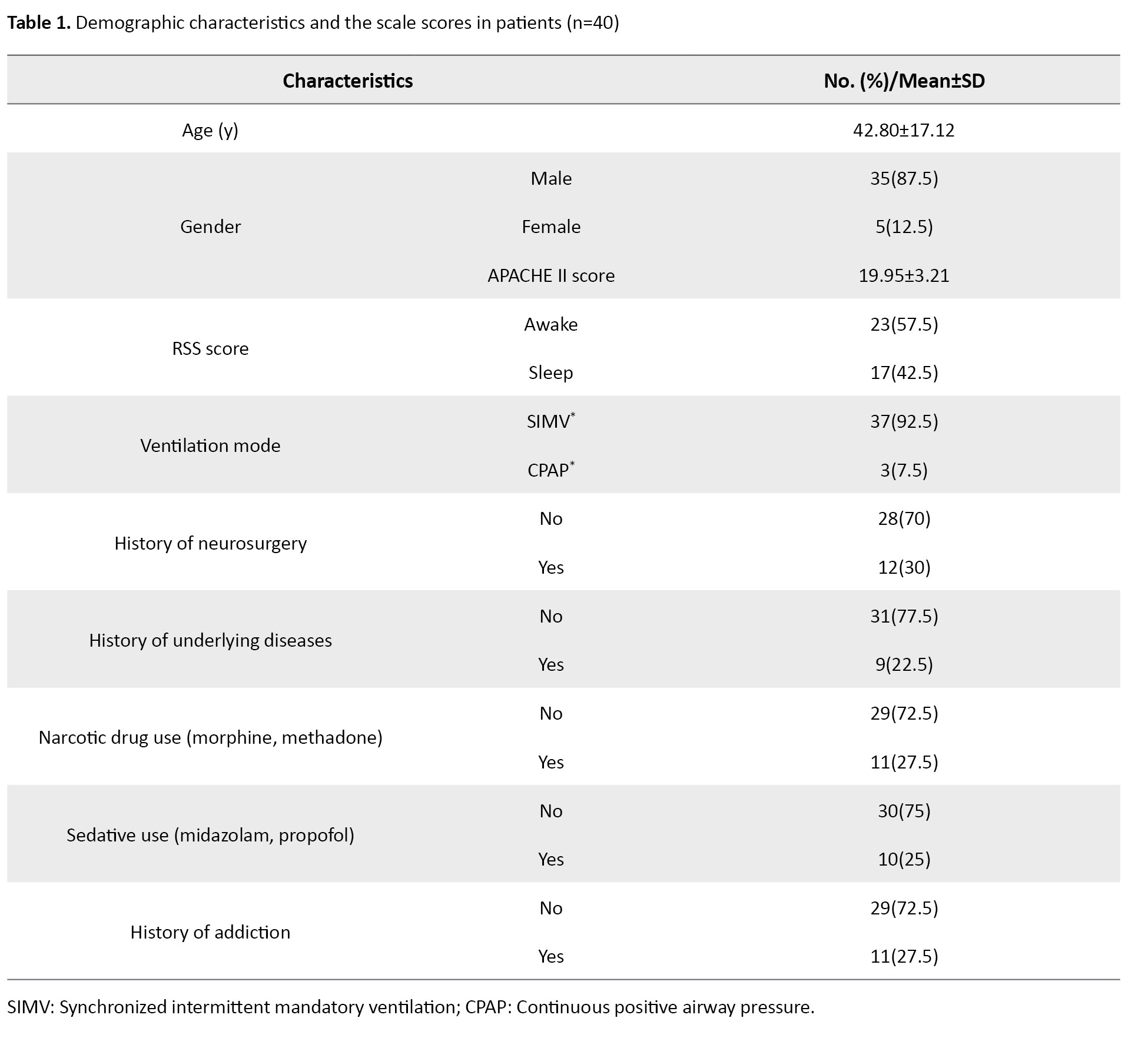
The mean score of APACHE II was 19.95±3.21. According to the RSS score, 42.5 % (n=17) of patients were sedated, while 57.5% (n=23) were not sedated. Before the suctioning at T1, 45% of the patients (n=18) had no pain, while 55% (n=22) experienced pain. At T2, all of the patients had pain. Before changing position (T1), 57.5% of the patients (n=23) were in the pain-free zone, while 100% experienced pain while their position was changing (T2). The mean CPOT score were 2.35 (at rest) and 4.56 (during suctioning). The mean CPOT score were 2.34±1 (at rest) and 4.55±1.33 (during position change).
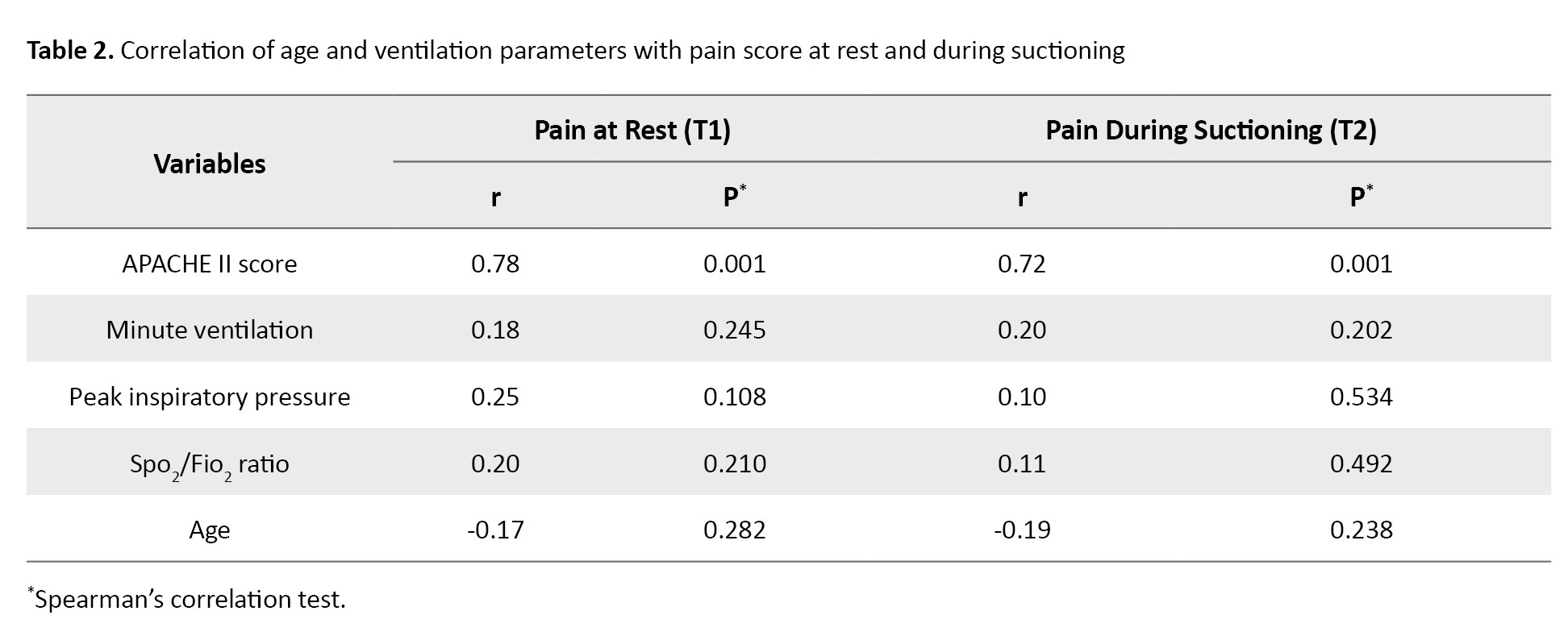
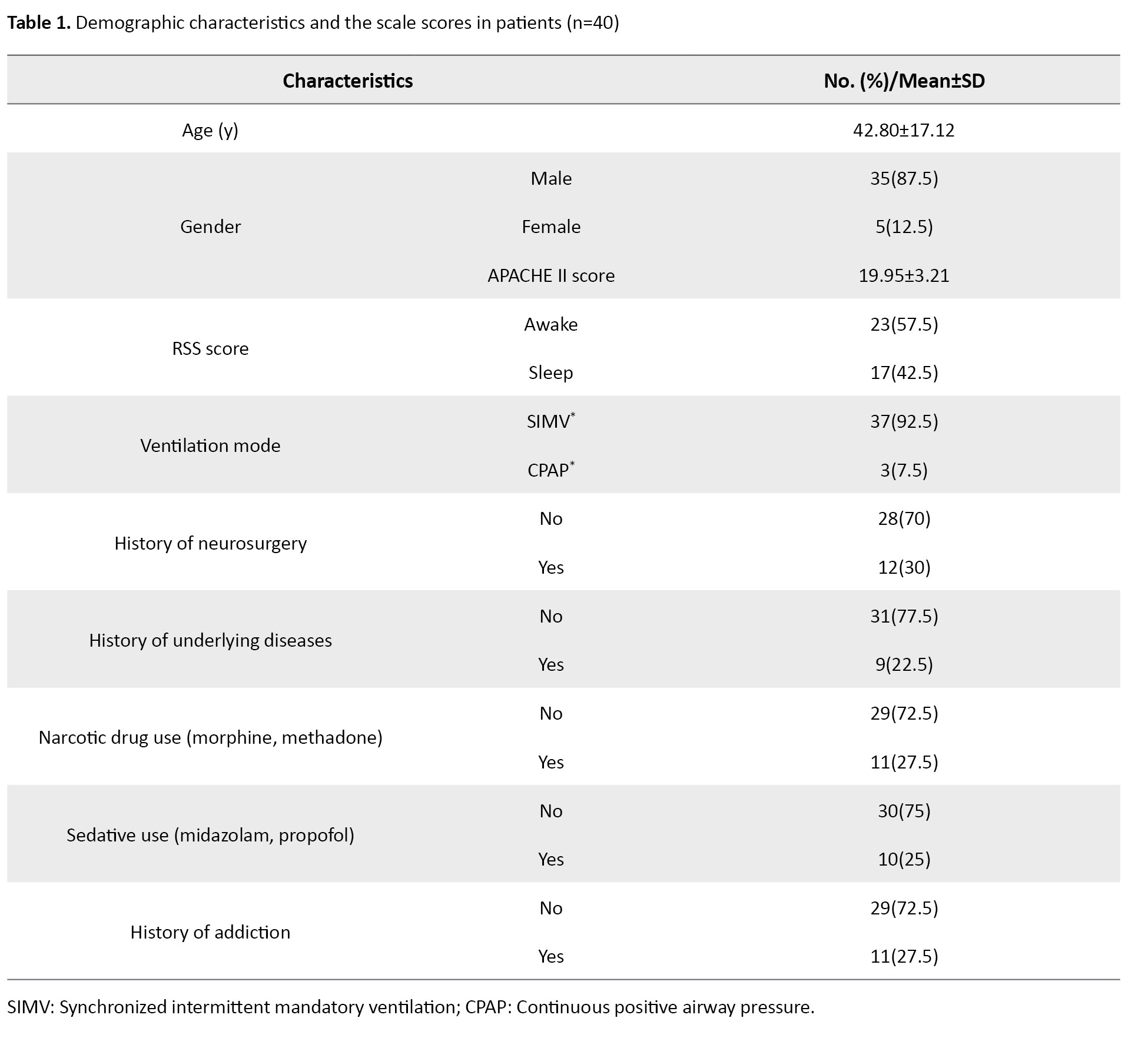
The Spearman correlation test results (Table 2) indicated a significant correlation between the APACHE II scores at T1 (r=0.78) and during suctioning or at T2 (r= 0.72, P=0.001).
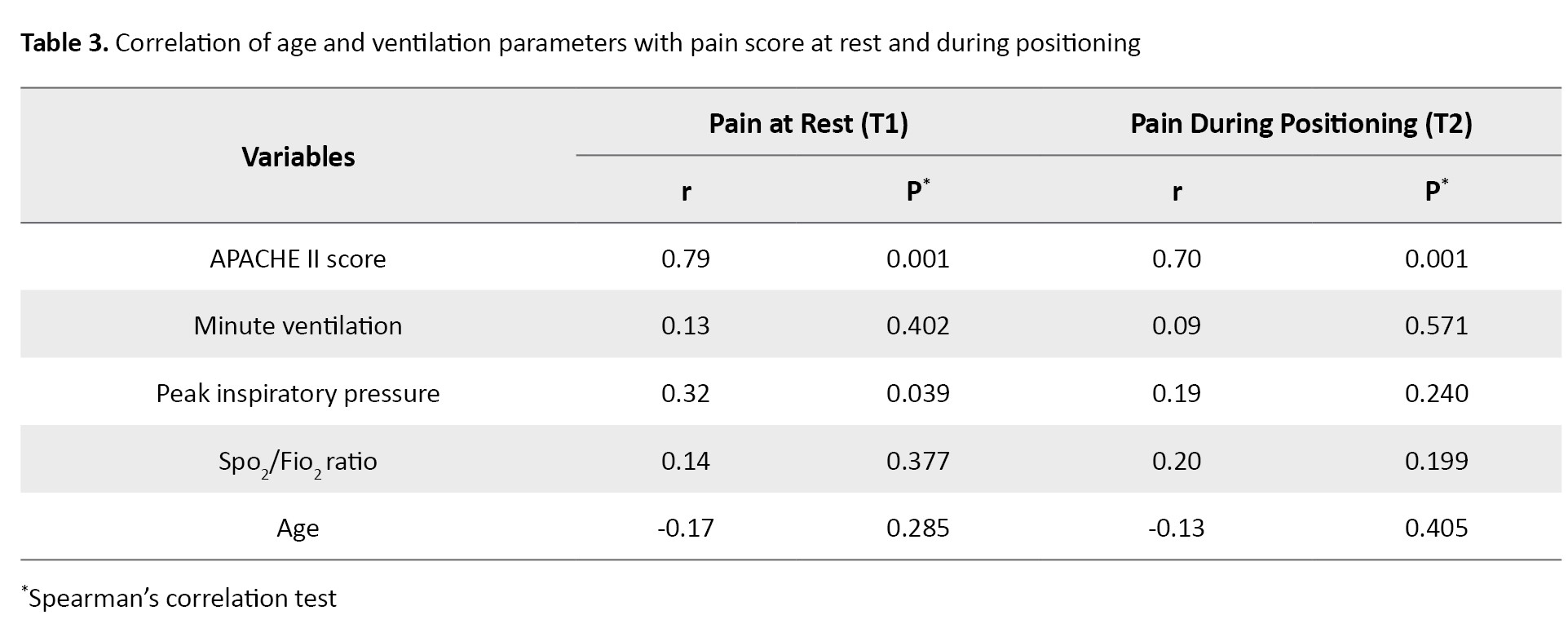
The results showed no significant correlation between pain score and ventilation parameters (Table 3).
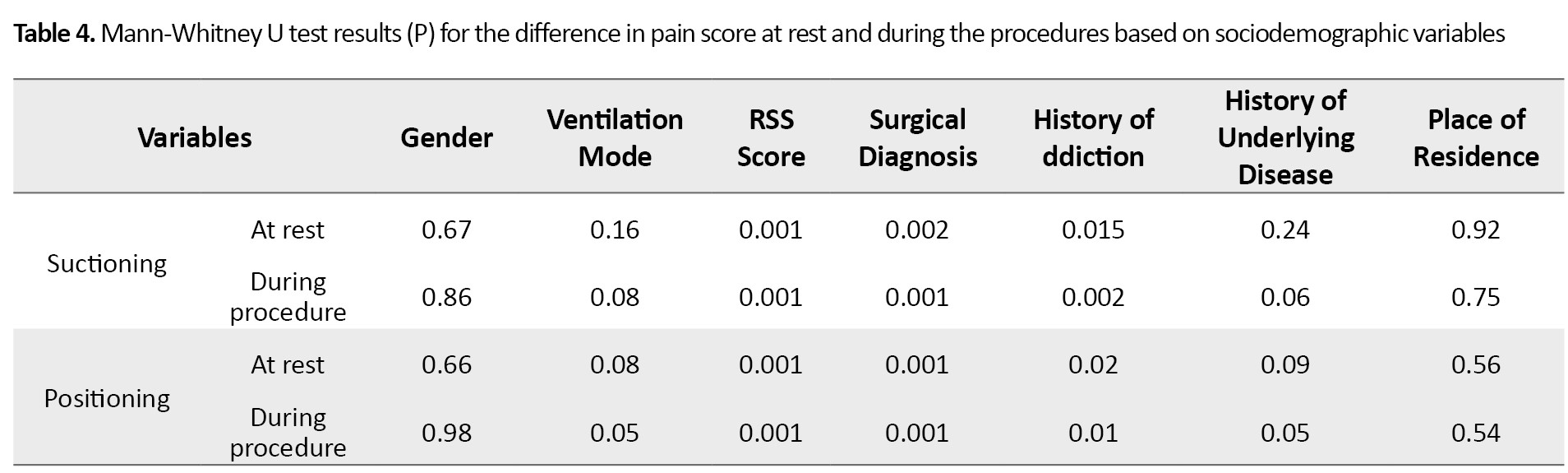
A significant association was observed between pain score and surgical diagnosis (P=0.002 at rest, P=0.001 during the procedure). The patients with surgical diagnosis showed more pain. Pain intensity and history of addiction were significantly correlated with each other (r=0.68, P=0.015 at rest; P=0.002 during the procedure). The patients with a history of addiction reported a higher pain. In terms of demographic characteristics (e.g. age, gender, marital status, education level, place of residence, history of psychoactive drug use), no significant association was found at T1 or T2 (Table 4).
In addition, the Mann-Whitney U test showed that patients with lower sedation scores experienced higher pain levels (P1=0.001, P2=0.001). Ten patients received sedation before the painful procedures of suctioning and position change, and their mean scores during the procedures were 4.56±1.3 and 4.55±1.33, respectively, while 30 patients did not receive sedation and their scores were 24.48 and 24.58. In total, 25% of the patients (n=10) were sedated one hour before undergoing painful procedures, and 27.5% (n=11) were administered with narcotic drugs one hour before undergoing painful procedures. No significant correlation was observed between narcotics use and pain intensity at T1 and T2. However, the Mann-Whitney U test results showed that the pain levels before (P<0.001) and during (P<0.001) procedures were significantly lower in the patients administered with sedatives.
Discussion
The results of this study showed a significant relationship between the pain intensity (CPOT score) and the APACHE score, which is a measure of the severity of the disease. Thus, the pain intensity can be increased with the increase in the severity of the disease. Our findings are consistent with other studies. For example, Ito et al. evaluated the effects of the respiratory status and other aspects of disease on the pain intensity of 20 patients admitted to the ICU. According to their findings, The BPS score was significantly associated with the APACHE II score; the BPS score increased with the increase of APACHE II score. On the other hand, the sequential organ failure assessment (SOFA) score had no significant association with the BPS score [14]. In another study, Ito et al. investigated 34 patients receiving mechanical ventilation after cardiovascular surgery to assess the correlation of the CPOT score with the respiratory and hemodynamic status and disease severity. Their results indicated the reduction in the CPOT score with the increase in the APACHE II score [22].
The results of the present study indicated no significant correlation between the pain intensity and ventilation parameters. This can be due to the fact that the majority of the patients were receiving the synchronized intermittent mandatory ventilation, and they were only monitored on the first three days of ICU admission. In this short period, the patients did not experience diminished respiratory capacities. Moreover, respiratory indicators such as minute ventilation and Spo2/Fio2 ratio showed that the severity of respiratory failure was mild. These findings are consistent with the results of Wojnar-Gruszka et al. They concluded that there is no relationship between ventilator parameters and the CPOT score [23]. Our findings are also in line with the results of Zubrzycki et al. In their study, the patients undergoing cardiovascular surgery were evaluated and the findings indicated that, despite the association of pain scores with PCO2 and HCO3, other respiratory indicators such as minute ventilation, peak inspiratory pressure, Pao2/Fio2 ratio, and respiratory rate, had no association with the CPOT score [24]. The significant difference in the amount of carbon dioxide and bicarbonate may be the reason. The patients in the mentioned study underwent cardiovascular surgery, and the majority had spontaneous breathing and received respiratory support by the biphasic positive airway pressure mode and were inclined to hyperventilation.
Our results also showed that patients who received sedative drugs one hour before painful procedures had lower pain scores than those who did not receive sedation, and no correlation was observed between pain intensity and narcotic drug use before and during procedures. In Mascarenhas et al.’s study, it was found that patients who received narcotics an hour before or during tracheal suctioning experienced more pain during tracheal suctioning than those who did not receive narcotics. In the narcotic drug group, those received sedatives and non-steroidal anti-inflammatory drugs had a higher pain intensity than the non-drug group during and after tracheal suctioning [25]. These results may be due to the dose of narcotics, or maybe the drugs have not reached their peak effect, developing tolerance to these drugs.
The findings of the current study showed that the patients with a history of addiction, surgery, and lower sedation scores experienced more pain compared to others. In this regard, Ayasrah et al. also reported that patients with a history of surgery and lower sedation scores during the rest period obtained higher CPOT scores [8]. In addition, Ito et al. observed that in the light sedation state, the CPOT scores of patients were significantly higher before and after procedures [14]. In the present study, no significant correlation was observed between the pain intensity and age, which is consistent with the findings of Puntillo et al. [22]. The association between pain intensity and age is a matter of debate. According to Ayasrah et al., younger patients experienced higher pain intensity at rest and during painful procedures [8].
According to the results of this study, the patients undergoing mechanical ventilation experience pain at rest and during painful nursing procedures. There is significant correlations between the CPOT score and the APACHE II and RSS scores. It can be concluded that effective pain assessment and management should be based on the disease severity and specific condition of patients as pain perception varies in different individuals. By clarifying pain assessment methods based on patients’ conditions, and teaching nurses about them in the form of in-service training programs in hospitals, the quality of care and effective pain management in critically ill patients under mechanical ventilation can be improved and may prevent the pain complications and shorten the length of stay in the ICU. One of the limitations of this study was that we only included the patients admitted due to trauma ICU, and different results may be obtained in other wards. Furthermore, the patients were monitored for a short period, and the generalization of the findings should be done with caution. It is recommended that further studies be conducted on other patients with different conditions using longer periods of monitoring
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (Code: IR.MEDSAB.REC.1399.097). Informed consent was obtained from all participants, and they were assured of the confidentiality of their information.
Funding
This study was extracted from the master’s thesis of Zohreh Akbari approved by the Department of Nursing, Sabzevar University of Medical Sciences. The study was funded by the Sabzevar University of Medical Sciences (Grant No.: 97148/141).
Authors' contributions
Conceptualization and study design: All authors; Data analysis: Neda Mahdavifar; Drafting of the manuscript: Ali Asghar Jesmi, and Zohreh Akbari; Review, editing and project administration: Ali Taj; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the physicians and nurses of the ICU of Emdad (Shahid Beheshti) Hospital of Sabzevar, and the patients and their families for their cooperation in this study. The authors also thank the Deputy for Research of Sabzevar University of Medical Sciences for financial support.
References
Pain is a persistent concern and a common symptom in critically ill patients [1]. Majority of patients admitted to the intensive care units (ICUs), especially those receiving mechanical ventilation, suffer from pain [2]. Pain is described as an unpleasant sensory and emotional experience that is called the “fifth vital sign” by the American Pain Society (APS) [3]. It has been reported that 50-71% of patients admitted to the ICUs experience undiagnosed or untreated pain, and annual statistics suggest that 71% of these patients recall this pain after discharge [4]. Moreover, it is estimated at 30% of patients experience pain while resting, and this rate increases to 50% during nursing procedures. According to the literature, more than 82% of the patients who are discharged from the ICU recall the pain and discomfort caused by the endotracheal intubation [5]. Individuals who have frightening memories of pain are at a higher risk of posttraumatic stress disorder, which affects 34-38% of patients discharged from the ICU [6]. Critically ill patients are often unable to communicate effectively due to their severe condition, mechanical ventilation, sedative/analgesic drug prescription, and decreased consciousness [7].
Inability to report pain is a major challenge for proper pain assessment or management, which is associated with a risk of underrated and untreated pain [8]. Pain assessment and management in critically ill patients are unique challenges for physicians and nurses [9]. The ICU nurses are mostly unaware of proper and objective pain assessment [10], such that 35-55% of nurses estimate patients’ pain less than the real rate. Management of analgesia and sedation in the ICU requires evaluation and monitoring of key parameters in order to detect pain and agitation, and quantify sedation [11]. Unfortunately, 64% of patients do not receive any medication before and during painful procedures [12]. Ineffective pain control is caused by several factors, such as improper measure of pain, inadequate professional training, and pain control not based on evidence [13]. Determining the possible influential factors in pain is a reliable approach to pain measurement in patients who are unable to report pain [14]. According to the guidelines of the American Society for Pain Management Nursing (ASPMN) and the Society of Critical Care Medicine (SCCM), behavioral indicators are can help with the diagnosis of pain in patients who are unable to express pain. Some of these behavioral indicators recommended by the SCCM are the behavioural pain scale (BPS) and critical-care pain observation tool (CPOT) [15]. The value of using each of these scales in patients with different clinical conditions should be carefully evaluated; some clinical experts have even criticized the applicability and ease of implementation of these tools [16].
Effective and adequate pain control in ICUs is associated with a reduction in mechanical ventilation time, shorter length of stay, and lower morbidity and mortality rates. In some health centers that provide care to critically ill patients, pain assessment is performed inadequately or is not performed, making it difficult to manage pain in these patients adequately [17]. Pain management still poses a significant challenge for doctors, nurses, and other medical staff [18]. Considering that pain management is a multidimensional process and pain assessment tools are one-dimensional, it is necessary to check the correlation of these tools with some scales that predict the patient’s condition and affect the pain level. The present study aimed to evaluate the correlation of the scores of the CPOT, the acute physiology and chronic health evaluation (APACHE II) scale, and the Ramsay sedation scale (RSS) with ventilation parameters to provide insight to healthcare professionals for the effective diagnosis and treatment of pain in patients undergoing mechanical ventilation.
Materials and Methods
This cross-sectional study was conducted on 40 intubated patients under mechanical ventilation at the trauma ICU of a hospital in Sabzevar, Iran. Data collection was performed using an observational approach from November 2020 to May 2021. The samples were selected using a convenience sampling method. The minimum sample size was determined 26, according to a pilot study, and considering the correlation coefficient of 0.74 between pain and APACHE II scores and β=80% at a confidence interval of 0.95. Due to the possibility of 50% sample dropout, the sample size was increased to 40. The inclusion criteria were age ≥18 years, a Glasgow coma scale (GCS) score of 5-8, having an artificial airway, and undergoing mechanical ventilation for more than 48 hours. The exclusion criteria were death in the first 24 hours, extubation, and transferring to other wards.
A demographic questionnaire was used to collect patient demographics and health information from the medical records. The recorded information included age, gender, level of education, place of residence, history of addiction, surgical diagnosis, underlying disease, use of sedative drugs one hour before painful procedures, use of narcotics one hour before painful procedures, and the information related to the respiratory status (ventilation mode, minute ventilation, peak inspiratory pressure, and Spo2/Fio2 ratio). After obtaining written informed consent from the legal guardians of the patients, the demographic form was completed by the researcher who was not a part of the treatment team.
The APACHE II scale was also used for data collection, which is a scoring system for ICU mortality rate calculated within the first 24 hours of admission to the ICU. This scale consists of three components. The first component is the acute physiology score (APS) which is obtained from 12 clinical measures in the first 24 hours of admission to the ICU. These measures included: internal temperature, heart rate, mean arterial pressure, respiratory rate, oxygenation, arterial pH, serum sodium, serum potassium, creatinine, hematocrit, white blood cell (WBC) and GCS. The second component is the age point, ranged from 1 to 6 for patients older than 44 years. The third component is the chronic health point for patients with severe and chronic disorders such as the heart, lung, kidney, liver, and immune system disorders. The APACHE score ranges from 0 to 71, with higher scores indicating more severe disease and a higher risk of mortality. Validity and reliability of the Persian version of this tool have been confirmed in Bahtouee et al.’s study [19].
The RSS was another tool used in this study, which measures the level of sedation on a scale from 1 to 6 as 1=anxious and agitated, restless or both; 2= cooperative, alert and calm; 3= confused but responding to commands; 4= rapid and intense response to stimuli; 5= slow response to stimuli; and 6= No responsive. The validity and reliability of the Persian version of this tool have been confirmed by Tabrizi et al in Iran [20].
The CPOT was used to assess pain intensity. It consists of four dimensions, including facial expression, body movement, muscle tension, and compliance with ventilator (in patients with an endotracheal tube) or vocalization (in patients without an endotracheal tube). Each item is scored from 0 to 2. The total CPOT score ranges from 0 (no pain) to 8 (maximum pain). In the present study, the Persian version of this tool was used [21], before the painful interventions. Pain intensity was measured twice in the morning shift and on the first, second and third days of admission to the ICU (6 times in total). The rest interval was one minute before painful procedures of positioning and intratracheal suctioning (T1 or rest time) and during the painful procedure (T2). By summing up the scores of the items, the final T1 and T2 values were determined. In this study, the selected procedures were endotracheal intubation, endotracheal suctioning, and changing position. During the pain intensity assessment, the ventilation parameters were recorded according to ventilator settings for each patient.
Data analysis was performed in SPSS software, version 24 using descriptive statistics to describe the data and Spearman’s correlation test to assess the correlation between the study variables, and the Mann-Whitney U test. The significance level was set at 0.05.
Results
Participants included 87.5% males (n=35) and 12.5% females (n=5). Their mean age was 42.80±17.12 years. In addition, 80% were married, and 62.5% were urban residents. Table 1 shows the demographic characteristics of the patients.
The mean score of APACHE II was 19.95±3.21. According to the RSS score, 42.5 % (n=17) of patients were sedated, while 57.5% (n=23) were not sedated. Before the suctioning at T1, 45% of the patients (n=18) had no pain, while 55% (n=22) experienced pain. At T2, all of the patients had pain. Before changing position (T1), 57.5% of the patients (n=23) were in the pain-free zone, while 100% experienced pain while their position was changing (T2). The mean CPOT score were 2.35 (at rest) and 4.56 (during suctioning). The mean CPOT score were 2.34±1 (at rest) and 4.55±1.33 (during position change).
The Spearman correlation test results (Table 2) indicated a significant correlation between the APACHE II scores at T1 (r=0.78) and during suctioning or at T2 (r= 0.72, P=0.001).
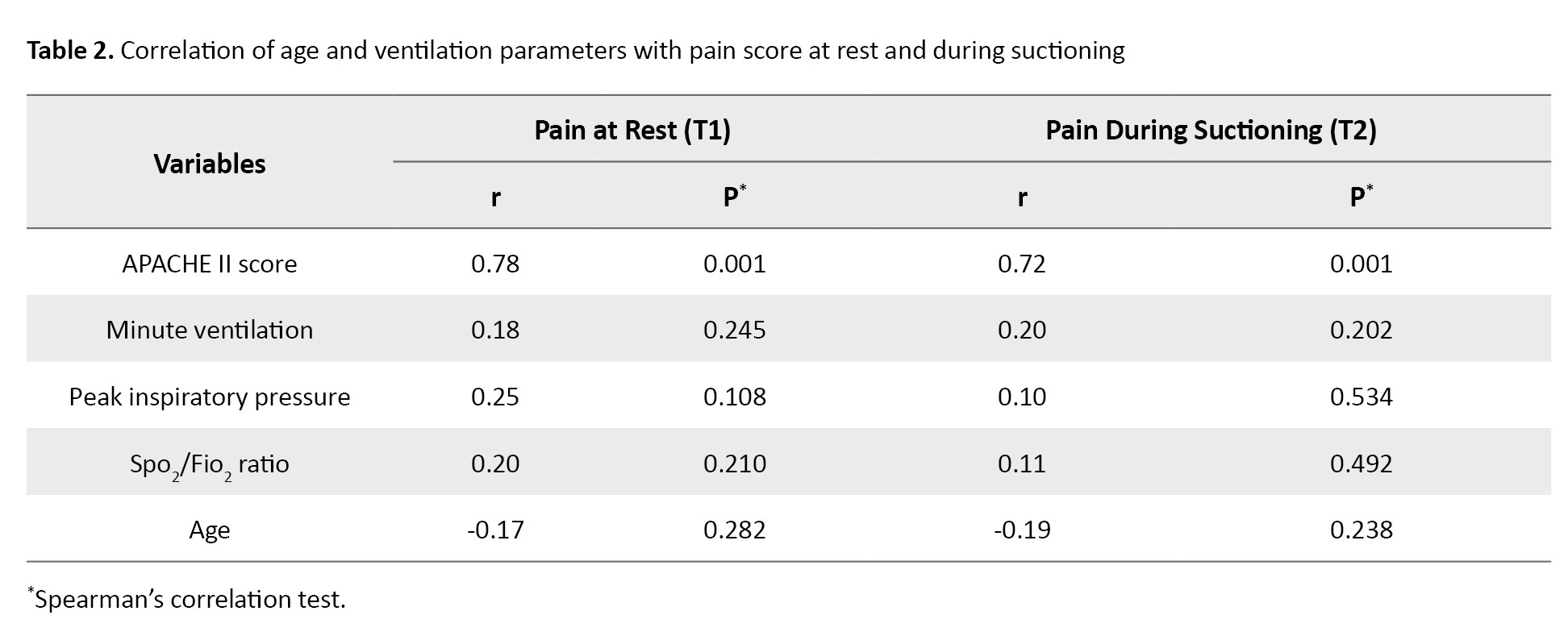
The results showed no significant correlation between pain score and ventilation parameters (Table 3).
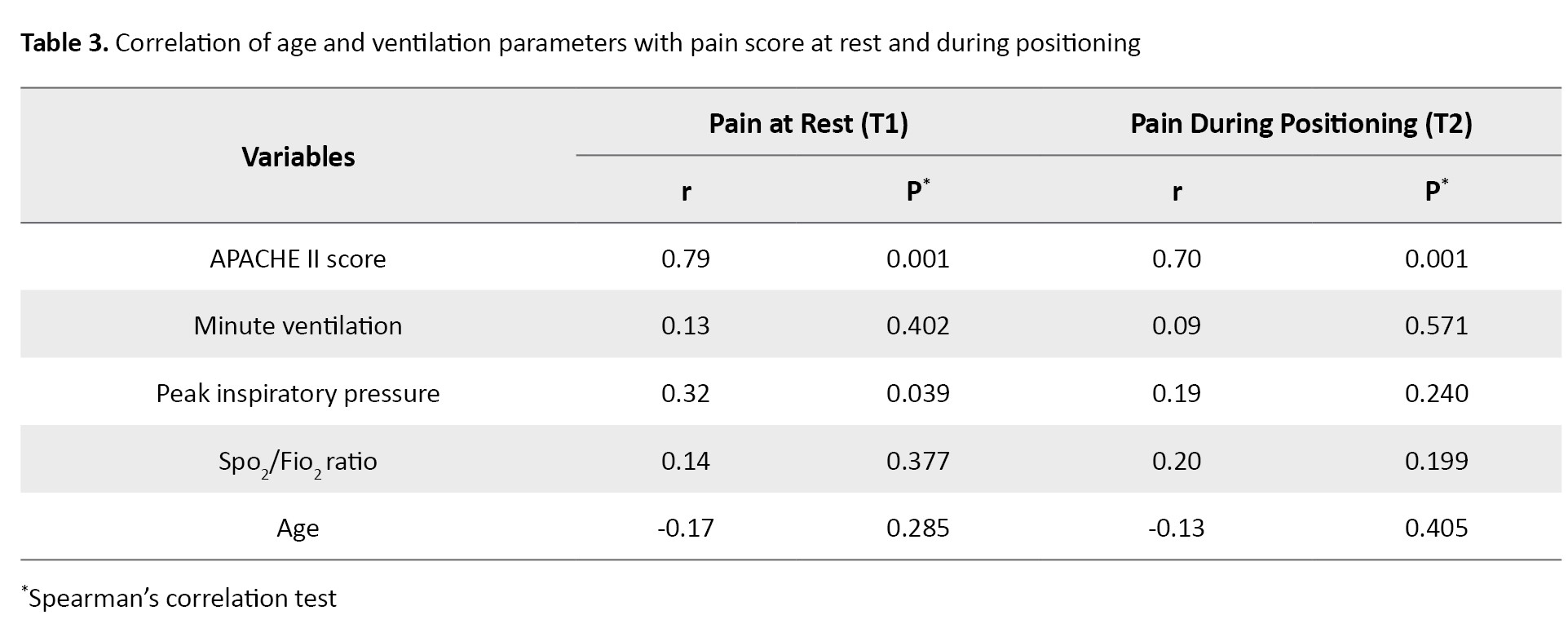
A significant association was observed between pain score and surgical diagnosis (P=0.002 at rest, P=0.001 during the procedure). The patients with surgical diagnosis showed more pain. Pain intensity and history of addiction were significantly correlated with each other (r=0.68, P=0.015 at rest; P=0.002 during the procedure). The patients with a history of addiction reported a higher pain. In terms of demographic characteristics (e.g. age, gender, marital status, education level, place of residence, history of psychoactive drug use), no significant association was found at T1 or T2 (Table 4).
In addition, the Mann-Whitney U test showed that patients with lower sedation scores experienced higher pain levels (P1=0.001, P2=0.001). Ten patients received sedation before the painful procedures of suctioning and position change, and their mean scores during the procedures were 4.56±1.3 and 4.55±1.33, respectively, while 30 patients did not receive sedation and their scores were 24.48 and 24.58. In total, 25% of the patients (n=10) were sedated one hour before undergoing painful procedures, and 27.5% (n=11) were administered with narcotic drugs one hour before undergoing painful procedures. No significant correlation was observed between narcotics use and pain intensity at T1 and T2. However, the Mann-Whitney U test results showed that the pain levels before (P<0.001) and during (P<0.001) procedures were significantly lower in the patients administered with sedatives.
Discussion
The results of this study showed a significant relationship between the pain intensity (CPOT score) and the APACHE score, which is a measure of the severity of the disease. Thus, the pain intensity can be increased with the increase in the severity of the disease. Our findings are consistent with other studies. For example, Ito et al. evaluated the effects of the respiratory status and other aspects of disease on the pain intensity of 20 patients admitted to the ICU. According to their findings, The BPS score was significantly associated with the APACHE II score; the BPS score increased with the increase of APACHE II score. On the other hand, the sequential organ failure assessment (SOFA) score had no significant association with the BPS score [14]. In another study, Ito et al. investigated 34 patients receiving mechanical ventilation after cardiovascular surgery to assess the correlation of the CPOT score with the respiratory and hemodynamic status and disease severity. Their results indicated the reduction in the CPOT score with the increase in the APACHE II score [22].
The results of the present study indicated no significant correlation between the pain intensity and ventilation parameters. This can be due to the fact that the majority of the patients were receiving the synchronized intermittent mandatory ventilation, and they were only monitored on the first three days of ICU admission. In this short period, the patients did not experience diminished respiratory capacities. Moreover, respiratory indicators such as minute ventilation and Spo2/Fio2 ratio showed that the severity of respiratory failure was mild. These findings are consistent with the results of Wojnar-Gruszka et al. They concluded that there is no relationship between ventilator parameters and the CPOT score [23]. Our findings are also in line with the results of Zubrzycki et al. In their study, the patients undergoing cardiovascular surgery were evaluated and the findings indicated that, despite the association of pain scores with PCO2 and HCO3, other respiratory indicators such as minute ventilation, peak inspiratory pressure, Pao2/Fio2 ratio, and respiratory rate, had no association with the CPOT score [24]. The significant difference in the amount of carbon dioxide and bicarbonate may be the reason. The patients in the mentioned study underwent cardiovascular surgery, and the majority had spontaneous breathing and received respiratory support by the biphasic positive airway pressure mode and were inclined to hyperventilation.
Our results also showed that patients who received sedative drugs one hour before painful procedures had lower pain scores than those who did not receive sedation, and no correlation was observed between pain intensity and narcotic drug use before and during procedures. In Mascarenhas et al.’s study, it was found that patients who received narcotics an hour before or during tracheal suctioning experienced more pain during tracheal suctioning than those who did not receive narcotics. In the narcotic drug group, those received sedatives and non-steroidal anti-inflammatory drugs had a higher pain intensity than the non-drug group during and after tracheal suctioning [25]. These results may be due to the dose of narcotics, or maybe the drugs have not reached their peak effect, developing tolerance to these drugs.
The findings of the current study showed that the patients with a history of addiction, surgery, and lower sedation scores experienced more pain compared to others. In this regard, Ayasrah et al. also reported that patients with a history of surgery and lower sedation scores during the rest period obtained higher CPOT scores [8]. In addition, Ito et al. observed that in the light sedation state, the CPOT scores of patients were significantly higher before and after procedures [14]. In the present study, no significant correlation was observed between the pain intensity and age, which is consistent with the findings of Puntillo et al. [22]. The association between pain intensity and age is a matter of debate. According to Ayasrah et al., younger patients experienced higher pain intensity at rest and during painful procedures [8].
According to the results of this study, the patients undergoing mechanical ventilation experience pain at rest and during painful nursing procedures. There is significant correlations between the CPOT score and the APACHE II and RSS scores. It can be concluded that effective pain assessment and management should be based on the disease severity and specific condition of patients as pain perception varies in different individuals. By clarifying pain assessment methods based on patients’ conditions, and teaching nurses about them in the form of in-service training programs in hospitals, the quality of care and effective pain management in critically ill patients under mechanical ventilation can be improved and may prevent the pain complications and shorten the length of stay in the ICU. One of the limitations of this study was that we only included the patients admitted due to trauma ICU, and different results may be obtained in other wards. Furthermore, the patients were monitored for a short period, and the generalization of the findings should be done with caution. It is recommended that further studies be conducted on other patients with different conditions using longer periods of monitoring
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (Code: IR.MEDSAB.REC.1399.097). Informed consent was obtained from all participants, and they were assured of the confidentiality of their information.
Funding
This study was extracted from the master’s thesis of Zohreh Akbari approved by the Department of Nursing, Sabzevar University of Medical Sciences. The study was funded by the Sabzevar University of Medical Sciences (Grant No.: 97148/141).
Authors' contributions
Conceptualization and study design: All authors; Data analysis: Neda Mahdavifar; Drafting of the manuscript: Ali Asghar Jesmi, and Zohreh Akbari; Review, editing and project administration: Ali Taj; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the physicians and nurses of the ICU of Emdad (Shahid Beheshti) Hospital of Sabzevar, and the patients and their families for their cooperation in this study. The authors also thank the Deputy for Research of Sabzevar University of Medical Sciences for financial support.
References
- Havaldar AA. Pain assessment in Intensive Care Unit: A forgotten entity or a quality indicator? Indian J Crit Care Med. 2022; 26(4):421-2. [DOI:10.5005/jp-journals-10071-24191]
- Basiri R, Lari SM, Hejazi S, Rad AV, Ghelichli M. The critical-care pain observation tool: A useful tool for pain assessment in intensive care units. J Cardio-Thoracic Med. 2018; 6(3):329-31. [Link]
- Hoseini MS, Hoseini SB, Mohamadzadeh Tabrizi Z, Rastaghi S, Davarinia Motlagh Quchan A. Comparison of the effect of lidocaine spray and acupressure on the severity of intramuscular injection pain. Evid Based Care. 2022; 11(4):26-32. [DOI:10.22038/ebcj.2021.61629.2601]
- Erden S, Demir N, Ugras GA, Arslan U, Arslan S. Vital signs: Valid indicators to assess pain in intensive care unit patients? An observational, descriptive study. Nurs Health Sci. 2018; 20(4):502-8. [DOI:10.1111/nhs.12543]
- Kotfis K, Zegan-Barańska M, Szydłowski Ł, Żukowski M, Ely EW. Methods of pain assessment in adult intensive care unit patients-Polish version of the CPOT (Critical Care Pain Observation Tool) and BPS (Behavioral Pain Scale). Anaesthesiol Intensive Ther. 2017; 49(1):66-72. [DOI:10.5603/AIT.2017.0010] [PMID]
- Czernicki M, Kunnumpurath S, Park W, Kunnumpurath A, Kodumudi G, Tao J, et al. Perioperative pain management in the critically Ill Patient. Curr Pain Headache Rep. 2019; 23(5):34. [DOI:10.1007/s11916-019-0771-3]
- Talebi F, Jesmi AA, Rakhshani MH, Tajabadi A. Effects of telenursing on the management of self-care behaviors in patients with chronic hypertension. J Res Health. 2023; 13(4):273-80. [DOI:10.32598/JRH.13.4.2118.1]
- Ayasrah SM. Pain among non-verbal critically Ill mechanically ventilated patients: Prevalence, correlates and predictors. J Crit Care. 2019; 49:14-20. [DOI:10.1016/j.jcrc.2018.10.002] [PMID]
- Shahbazi H, Mahdavifar N, Jesmi AA. Effects of COVID-19 pandemic on the treatment management of ST-elevation myocardial infarction. Evid Based Care. 2022; 12(1):7-13. [DOI:10.22038/ebcj.2022.60740.2581]
- Chen HJ, Chen YM. Pain assessment: Validation of the physiologic indicators in the ventilated adult patient. Pain Manag Nurs. 2015; 16(2):105-11. [DOI:10.1016/j.pmn.2014.05.012]
- Gorzin K, Sanagoo A, Jouybari L, Pahlavanzadeh B, Jesmi AA. The effect of education on function and communication skill of nurse with intubated patient in intensive care unit. J Nurs Midwifery Sci. 2020; 7(2):84-7. [Link]
- Akhond M, Froutan R, Malekzadeh J, Mazlom SR. The effect of implementation of a pain monitoring protocol on the pain intensity in the intensive care unit semiconscious patients. Evid Based Care J. 2017; 7(2):37-45. [DOI:10.22038/ebcj.2017.23797.1504]
- Oliveira LS, Macedo MP, Silva SAMd, Oliveira APdF, Santos VS. Pain assessment in critical patients using the Behavioral Pain Scale. BrJP. 2019; 2(2):112-6. [DOI:10.5935/2595-0118.20190021]
- Ito Y, Teruya K, Nakajima E. Evaluation of pain severity in critically ill patients on mechanical ventilation. Intensive Crit Care Nurs. 2022; 68:103118. [DOI:10.1016/j.iccn.2021.103118]
- University of Virginia School of Nursing, Eleanor Crowder Bjoring Center for Nursing Historical Inquiry. American Society for Pain Management Nursing Collection. Charlottesville: School of Nursing -University of Virginia; 2016. [Link]
- Rijkenberg S, Willemke S, Bosman R, Meer N, Voort P. Pain measurement in mechanically ventilated patients after cardiac surgery: Comparison of the Behavioral Pain Scale (BPS) and the Critical-Care Pain Observation Tool (CPOT). J Cardiothorac Vasc Anesth. 2017; 31(4):1227-34. [DOI:10.1053/j.jvca.2017.03.013]
- Loadsman JA, Craigie MJ. Clinical assessment of pain and its measurement and reporting for research: A state of discomfort. Anaesth Intensive Care. 2019; 47(5):411-2. [DOI:10.1177/0310057X19888611]
- Olisarova V, Tothova V, Cerveny M, Dvorakova V, Sadilek P. Pain assessment: Benefits of Using Pain Scales for surgical patients in South Bohemian Hospitals. Healthcare. 2021; 9(2):171. [DOI:10.3390/healthcare9020171]
- Bahtouee M, Eghbali SS, Maleki N, Rastgou V, Motamed N. Use of the APACHE II Score for the assessment of outcome and mortality prediction in an Iranian Medical-Surgical Intensive Care Unit. Arch Anesth Crit Care. 2018; 4(4):521-6. [Link]
- Tabrizi EM, Tadrissi S, Yari AM, Ebadi A, Mirhashemi S. [Validity and reliability of Ramsay sedation scale in intensive care unit adult patients (Persian)]. Iran J Crit Care Nurs. 2010; 3(1):39-44. [Link]
- Rafiei M, Ghadami A, Irajpour A, Feizi A. Validation of critical care pain observation tool in patients hospitalized in surgical wards. Iran J Nurs Midwifery Res. 2016; 21(5):464-9. [DOI:10.4103/1735-9066.193391]
- Puntillo KA, Max A, Timsit JF, Vignoud L, Chanques G, Robleda G, et al. Determinants of procedural pain intensity in the intensive care unit. The Europain® study. Am J Respir Crit Care Med. 2014; 189(1):39-47. [DOI:10.1164/rccm.201306-1174OC]
- Wojnar-Gruszka K, Sega A, Płaszewska-Żywko L, Wojtan S, Potocka M, Kózka M. Pain Assessment with the BPS and CCPOT Behavioral Pain Scales in mechanically ventilated patients requiring analgesia and sedation. Int J Environ Res Public Health. 2022; 19(17):10894. [DOI:10.3390/ijerph191710894]
- Zubrzycki M, Liebold A, Skrabal C, Reinelt H, Ziegler M, Perdas E, et al. Assessment and pathophysiology of pain in cardiac surgery. J Pain Res. 2018; 11:1599-611. [DOI:10.2147/JPR.S162067]
- Mascarenhas M, Beattie M, Roxburgh M, MacKintosh J, Clarke N, et al. Using the model for improvement to implement the critical-care pain observation tool in an adult intensive care unit. BMJ Qual Improv Rep. 2018; 7(4):e000304. [DOI:10.1136/bmjoq-2017-000304]
Article Type : Research |
Subject:
General
Received: 2023/02/14 | Accepted: 2024/04/27 | Published: 2024/10/1
Received: 2023/02/14 | Accepted: 2024/04/27 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |