Thu, Apr 25, 2024
Volume 32, Issue 2 (3-2022)
JHNM 2022, 32(2): 124-134 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nazarpour P, Jafaraghaee F, Moghadamnia M T, Maroufizadeh S. Predictors of Long-Term Survival after Cardiopulmonary Resuscitation. JHNM 2022; 32 (2) :124-134
URL: http://hnmj.gums.ac.ir/article-1-1833-en.html
URL: http://hnmj.gums.ac.ir/article-1-1833-en.html
1- Nursing (MSN), Department of Nursing, School of Nursing and Midwifery, Guilan University of medical sciences, Rasht, Iran
2- Associate professor of Nursing, Department of Nursing, School of Nursing and Midwifery, Guilan University of medical sciences, Rasht, Iran , fja_a80@yahoo.com
3- Assistant Professor, Department of Nursing, School of Nursing and Midwifery, Guilan University of medical sciences, Rasht, Iran
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran
2- Associate professor of Nursing, Department of Nursing, School of Nursing and Midwifery, Guilan University of medical sciences, Rasht, Iran , fja_a80@yahoo.com
3- Assistant Professor, Department of Nursing, School of Nursing and Midwifery, Guilan University of medical sciences, Rasht, Iran
4- Assistant Professor, Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran
Full-Text [PDF 742 kb]
(401 Downloads)
| Abstract (HTML) (1169 Views)
Full-Text: (432 Views)
Introduction
Sudden cardiac arrest is the third leading cause of death in industrialized countries [1]. Each year, over 630000 cases of Cardiac Arrest (CA) are reported in the United States, of whom 12% are Out-of-Hospital Cardiac Arrest (OHCA) patients and 24.8% In-Hospital Cardiac Arrest (IHCA) patients who survive and discharge from the hospitals [2]. In one of the teaching and medical hospitals of Guilan Province, Iran, among those who survived from IHCA, 30% had short-term survival, and 11% of patients were discharged with good brain conditions [3]. Survived people may experience Post-Cardiac Arrest Syndrome (PCAS), which is a pathological process caused by the Restoration of Spontaneous Circulation (ROSC) [4]. This syndrome can be accompanied by brain injury, heart disorders, recurrent ischemic injuries of the nervous system, and inflammatory responses [5]. Survival after CA is one of the most important issues related to the patients’ safety and quality of care, and unanticipated events such as failure to follow guidelines may endanger patients’ safety [6].
The relationship between guideline-based post-resuscitation care and the survival and functional status of patients after CA has already been emphasized [7]. As CA affects multiple systems, successful post-cardiac arrest care is one of the most effective treatment programs [8].
Post-resuscitation care is an important link in the resuscitation chain and plays a prominent role in prolonging patients’ 24-hour survival. The care should be tailored to the patient’s needs and include (a) identification and treatment of the cause of CA, (b) airway and ventilation management, (c) hemodynamic management, (d) targeted temperature management or therapeutic hypothermia, (e) glycemic control, and (f) seizure management [9]. Studies reveal that initial treatments for hypertension, oxygen saturation, carbon dioxide pressure, glucose level, and temperature are associated with good clinical outcomes in patients with PCAS. The inadequate level of each indicator reduces the patient’s survival or leads to adverse outcomes [4, 7]. Hypertension has been identified as an independent and predictive factor for survival among patients who survived CA [10]. Also, hyperglycemia in CA survivors is associated with increased mortality and poor neurological outcomes [11]. However, a comparative study with precise-matched control group - (4-6 mmol / L or 72-108 mg/L) with (6-8 mmol / L or 108-144 mg/dL) - on OHCA resuscitated patients reported no deaths within 30 days [12].
In many countries, post-resuscitation care is not provided in specialized hospitals, and there are many differences between hospitals in terms of availability and type of post-resuscitation care as well as clinical outcomes [13]. A study in Australia identified some of the shortcomings in post-resuscitation care provided by healthcare staff in comparison to the guideline-recommended care, the most important of which were deficiencies of oxygenation, temperature management, and blood pressure control [7]. Also, Ford et al. reported that post-resuscitation care was an influencing factor in patients’ survival. When the healthcare providers do not follow guidelines, it may lead to significant complications after resuscitation [14].
This study aimed to determine the long-term survival after cardiopulmonary resuscitation and its predictors in patients with cardiac arrest in a specialized heart center, which is the referral center of the Province.
Materials and Methods
This analytic study is based on a retrospective survey of the records of all patients who successfully resuscitated after CA in a large referral heart center in Rasht City, Iran, between 2016 and 2019.
Patients over 18 years with long-term survival (long-term survival means the patient survived for at least 24 hours or more after CPR [15]) and patients who survived at least three days after cardiac arrest and were discharged alive were selected as the samples of this study and examined in terms of clinical and demographic characteristics and the follow-ups within three days of resuscitation. The patients who died in the hospital after three days and were not discharged were not included in the study sample.
The data collection instrument consisted of two parts. The first part collected the demographic information and clinical data, which were extracted from patients’ records. These data included date of admission, date of cardiac arrest, date of discharge, sex, and location of CA, pre-arrest consciousness, CPR duration, initial rhythm, and history of CA during the same hospitalization, history of an underlying disease, final diagnosis, and connection to a mechanical ventilator, death after discharge, and survival period after discharge. The second part of the extracted data comprised the information about the time between post-resuscitation monitoring and discharge in 4 areas of blood pressure monitoring, temperature monitoring, blood glucose monitoring, and oxygenation index. Care measures in four areas of post-resuscitation care guidelines of blood pressure monitoring status (Systolic Blood Pressure [SBP] and Mean Arterial Blood Pressure [MAP]), pulse oximetry saturation (SpO2), Blood Sugar (BS), and temperature were extracted from care guidelines [8, 16] and recorded in a prepared checklist.
To determine the instrument validity, 5 faculty members of the country’s medical universities examined the instrument. They were experienced in cardiopulmonary resuscitation. Afterward, the instrument was given back to two experienced professors in the field of cardiopulmonary resuscitation. Also, to ensure the recording of the variables in the file, 60 CPR files were randomly reviewed for the preliminary study.
Initially, we reviewed the medical records of 1565 patients who received CPR between 2016 and 2019. Cases with a successful CPR were separated from the failed ones, which were 667 cases. In this retrospective study, individual, disease-related, and 3-day follow-up-related factors were monitored after the CPR in all patients with long-term survival after CA. After reviewing the medical records of these patients, their contact numbers were noted from the medical records and followed up by telephone interviews. Their survival time after discharge was assessed. If the patient died after discharge, the date of death was asked of their family, and the duration of survival until the date of death was calculated.
In this study, continuous variables were expressed as Mean±SD and categorical variables as frequency (percentage). The survival probability was calculated using the Kaplan-Meier test and compared with the log-rank test. Furthermore, simple and multiple Cox proportional hazard models were performed to estimate the crude and adjusted Hazard Ratios (HR) and their 95% confidence intervals. Statistical analysis was done with SPSS software v. 16 for Windows (SPSS Inc., Chicago, IL, USA), and the level of significance was set at 0.05.
Results
Among 667 successful CPRs, 156 were patients with long-term survival (8 patients died in the hospital despite having more than 24 hours of survival and were not included in the study). One patient was also not included due to a distorted contact number. Successful telephone calls were made to 147 patients, and the research instrument was completed.
The Mean±SD and median survival times of the patients were 30.98±1.78 and 34.70 months (Figure 1). One-, two-, and three-year survival rates were 72.1%, 61.4%, and 49.9%, respectively. A total of 67 patients (45.6%) died after discharge, and 80 patients (54.4%) survived to the end of the study.
Of 147 patients with cardiac arrest who survived to discharge, 89 (60.5%) were men, and 58 (39.5%) were women. The Mean±SD age of the patients was 66.13±14.26. Of them, 47 patients (32%) were under 60 years old (Table 1).
.jpg)
Most samples (98%) had a temperature above 36°C, and the number of patients with abnormal blood sugar was higher than the number of patients with normal blood sugar. During the first, second, and third days after resuscitation, 27.9%, 32%, and 32% of the samples, respectively, had normal blood sugar levels (80-140 mg/dL). Systolic blood pressure was above 90 mm Hg in the majority of patients. About 16.3%, 15.6%, and 10.2% of the samples had systolic blood pressure lower than 90 mm Hg in the first, second, and third days after resuscitation, respectively. Also, 40.8%, 44.2%, and 46.9% of the samples had normal mean arterial blood pressure (65-80 mm Hg) in the first, second, and third days after resuscitation, respectively. Finally, 58.5%, 78.2%, and 85.7% of the samples had normal SpO2 (94%-98%) in the first, second, and third days after resuscitation, respectively.
The Mean±SD values of temperature, blood sugar, systolic blood pressure, diastolic blood pressure, mean arterial pressure, and pulse oximetry saturation during the three days after resuscitation were estimated respectively at 36.82±0.17°C, 179.58±73.43 mg/dL, 114.37±18.27 mm Hg, 69.34±9.68 mm Hg, 84.29±12.11 mm Hg, and 94.47±2.85%.
The log-rank test revealed that the survival time of patients under 60 years was significantly longer than those over 60 years (P=0.039, log-rank statistics=4.269) (Figure 2). Survival time was significantly longer in patients with an initial Ventricalar Fibrilation rhythm than those with an initial Ventricular Tachycardia (VT) or asystole rhythm (P=0.001, log-rank statistics=19.878) (Figure 3). Subjects who were not connected to a mechanical ventilator after CPR had a significantly longer survival time than those connected to a mechanical ventilator (P=0.004, log-rank statistics=8.191) (Figure 4). People without cardiovascular disease had significantly longer survival than people with cardiovascular disease (P=0.015, log-rank statistics=5.923) (Figure 5). The mean survival time was longer in people without hypertension and diabetes, but the difference was not significant.
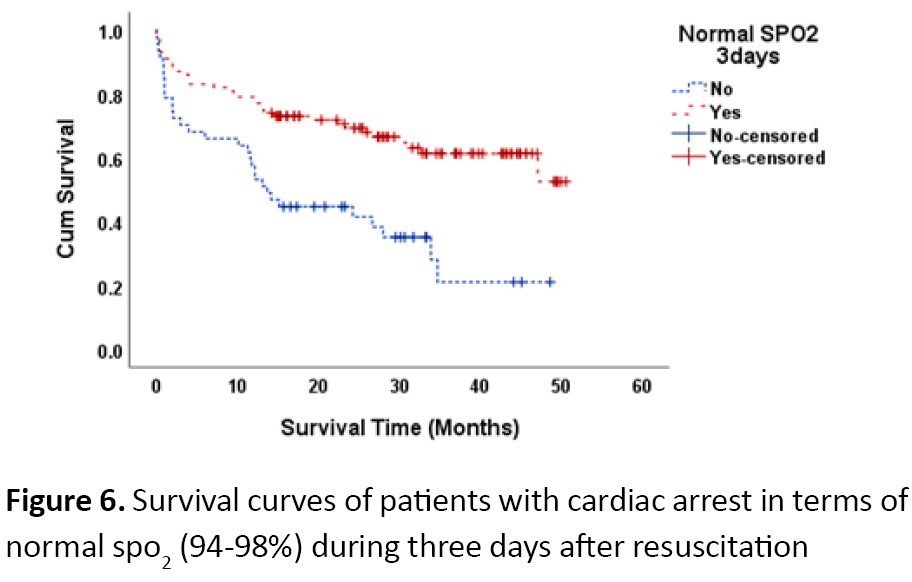
Although the monitored blood glucose and blood pressure showed relationships with long-term survival, the associations were not statistically significant. Regarding SpO2 monitoring (Figure 6), results showed that the patients with normal SPO2 (94-98%) within three days after resuscitation had significantly longer survival than those with abnormal (P=0.001, log rank statistics=14.090) Comparison mean of survival time based on study variables showed in Table 2.
.jpg)
The analysis of Cox proportional hazards model showed that age (>60 y) (HR=1.811, 95%CI; 1.019-3.218, P=0.043), initial asystole rhythm (HR=4.199, 95%CI; 2.129-8.282, P=0.001), VT (HR=2.315, 95%CI; 1.171-4.576, P=0.016), connection to a mechanical ventilator (HR=1.992, 95%CI; 1.229-3.229, P=0.005), and abnormal SpO2 (HR=2.447, 95%CI; 1.507-3.972, P=0.001) had significant relationships with patients’ survival. So that the older age, initial asystole rhythm, VT, connection to a mechanical ventilator and abnormal SpO2 were associated with lower long-term survival.
Multivariate analysis showed that asystole rhythm (HR=5.128, 95%CI; 1.917-13.716, P=0.001), VT (HR=2.728 , 95%CI; 0.991-7.509, P=0.052), and the duration of resuscitation (>20 min) (HR=3.168, 95%CI; 1.037-9.683, P=0.043) had significant relationships with patients’ survival (Table 3).
.jpg)
Discussion
In our study, most of the samples were men over 60 years old. Many studies have considered old age a significant factor in long-term survival [2, 17]. A systematic review reported that the risk of death after CA was lower in women than men [18]. A study provided a justification for the observed differences. It stated that in the event of an OHCA, women are less likely to be resuscitated by their companions than men, which may lead to lower survival rates for women [19].
Our study showed that a systole heart rhythm is associated with patients’ survival. The initial rhythm was the best predictor of patients’ survival. Also, compared to VF, pulseless electrical activity was associated with shorter survival times [20]. Another study reported that a lower probability of survival at discharge was associated with the recurrence of CA [21].
Our study revealed that CPR duration (>20 min) was a risk factor for patients’ survival. Another study in Iran demonstrated that CPR is an influential factor in a patient’s survival [22]. In another study, CPR duration between 10 and 15 minutes was considered a significant factor in patients’ survival. However, the effect of CPR duration on survival was challenging to evaluate due to its variability from patient to patient [23].
Our observations align with other investigators who reported that underlying diseases such as diabetes, cardiovascular diseases, and hypertension were effective in patients’ survival [24, 25]. Of note, a study evaluated the association of hypertension with survival rate after CA in adults and identified its changes according to the patient’s age [26]. However, a study showed that even though patients with cardiovascular diseases are a high-risk group, there was no significant difference in the survival rate between the patients with and without heart disease [27]. It seems that factors such as biological differences, access to health care, or other factors may affect the survival of patients in the long term.
Temperature above 36°C was reported in most of our study samples. A recent meta-analysis reported that temperature management reduces mortality and significantly reduces poor neurological outcomes [28]. Due to observed consistency in our study, the temperature variable was omitted in the Kaplan Meier, log-rank, and Cox regression analyses.
We considered a blood sugar range of 80-140 mg/dL based on care guidelines [8, 16]. The data showed that the number of patients who lacked normal blood sugar was higher than those with normal blood sugar. Following CPR, a cascade of metabolic disorders frequently occurs, which requires careful monitoring and management. Hence, diagnosis and appropriate response to severe metabolic disorders, especially the prevention of hypoglycemia and hyperglycemia, are essential [29]. Some reports have described the relationships between the increase in mean blood sugar during the first 96 hours after admission and mortality rates and neurological dysfunctions [11, 30].
A search on care guidelines reveals that systolic pressure below 90 mm Hg is an influential factor in recovery after CA [8, 16]. But in our study, most subjects had a systolic pressure above 90 mm Hg. Our study is in line with a systematic review on the association between blood pressure and patients’ outcomes following CA. By examining 13150 patients, the researchers suggested that higher blood pressure ameliorated neurological outcomes after CA [31]. Our results were in contrast to Roberts’ finding [32]. However, another study reported no association between MAP above 90 mm Hg and neurological outcomes at the time of discharge [33]. Patients are often hemodynamically unstable after ROSC, and their management could be a challenge. Following CPR, an optimal hemodynamic should maintain adequate cerebral and coronary perfusion pressure and blood flow to the other vital organs. Based on the current guidelines, the main goal of hemodynamic management is to prevent hypotension and maintain a systolic blood pressure of at least 90 mm Hg or a mean arterial pressure of 65 mm Hg after resuscitation [9].
One systematic review study concluded that hyperoxia in adults with CA was associated with lower mortality rates during CA but higher mortality rates after CA [34]. Another study reported that high or low SpO2 might be associated with poor outcomes after CA [35]. After ROSC, hyperoxemia during the reperfusion phase with 100% oxygen increases brain lipid peroxidation and may cause metabolic dysfunction and neurological degeneration [9]. Besides, excess oxygen leads to increased damage to the myocardium, recurrent myocardial infarction, and larger infarctions within 6 months, as hypocapnia induces cerebral vasoconstriction and reduces cerebral blood flow [16].
Conclusion
Our results showed that different factors are influential in the long-term survival of patients after CA. We believe that differences in the observed results and factors predicting long-term survival may stem from differences in demographic, disease-related factors, the complex nature of CA and its affecting factors, various care services provided by healthcare providers, differences in healthcare providers’ knowledge on the subject of post-resuscitation care, treatment policies in different countries, ethnic and demographic differences, and sample size. Therefore, raising sufficient awareness, including the necessary training for medical staff in post-resuscitation care, especially in the field of hypothermia, maintaining this knowledge, and establishing a recovery ward for patients after cardiac arrest and further investigating in this topic can be effective.
The generalization of our results is limited in two respects. First, the research was a retrospective study, and data were extracted from medical records, so the personnel recording the information might make mistakes. Besides, although the study was performed in a referral center, multicenter studies could be more helpful.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the Research Ethics Committee of Guilan University of Medical Sciences (ID: IR.GUMS.REC.2019.496). Official permission of the hospital administration was acquired for accessing patients’ medical files. The study purpose was explained to the subjects at the beginning of the telephone interview, and the patient’s oral consent was obtained.
Funding
This study was extracted from the Master thesis of the first author, Department of Nursing, School of Nursing and Midwifery, , Guilan University of Medical Sciences, Rasht, Iran (registration number: 97283).
Authors' contributions
Conceptualization and supervision: Fatemeh Jafaraghaee; Investigation: Parivash Nazarpour and Fatemeh Jafaraghaei; Formal analysis: Parivash Nazarpour and Saman Maroufizadeh; Methodology, funding acquisition, resources, and writing - original draft: All authors; Writing - review, and editing: Fatemeh Jafaraghaee and Mohammad Taghi Moghadamnia.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors gratefully thank all patients for their participation in this study. This study was supported by the Research Deputy of Guilan University of Medical Sciences. We would like to express our sincere gratitude to this center.
References
Sudden cardiac arrest is the third leading cause of death in industrialized countries [1]. Each year, over 630000 cases of Cardiac Arrest (CA) are reported in the United States, of whom 12% are Out-of-Hospital Cardiac Arrest (OHCA) patients and 24.8% In-Hospital Cardiac Arrest (IHCA) patients who survive and discharge from the hospitals [2]. In one of the teaching and medical hospitals of Guilan Province, Iran, among those who survived from IHCA, 30% had short-term survival, and 11% of patients were discharged with good brain conditions [3]. Survived people may experience Post-Cardiac Arrest Syndrome (PCAS), which is a pathological process caused by the Restoration of Spontaneous Circulation (ROSC) [4]. This syndrome can be accompanied by brain injury, heart disorders, recurrent ischemic injuries of the nervous system, and inflammatory responses [5]. Survival after CA is one of the most important issues related to the patients’ safety and quality of care, and unanticipated events such as failure to follow guidelines may endanger patients’ safety [6].
The relationship between guideline-based post-resuscitation care and the survival and functional status of patients after CA has already been emphasized [7]. As CA affects multiple systems, successful post-cardiac arrest care is one of the most effective treatment programs [8].
Post-resuscitation care is an important link in the resuscitation chain and plays a prominent role in prolonging patients’ 24-hour survival. The care should be tailored to the patient’s needs and include (a) identification and treatment of the cause of CA, (b) airway and ventilation management, (c) hemodynamic management, (d) targeted temperature management or therapeutic hypothermia, (e) glycemic control, and (f) seizure management [9]. Studies reveal that initial treatments for hypertension, oxygen saturation, carbon dioxide pressure, glucose level, and temperature are associated with good clinical outcomes in patients with PCAS. The inadequate level of each indicator reduces the patient’s survival or leads to adverse outcomes [4, 7]. Hypertension has been identified as an independent and predictive factor for survival among patients who survived CA [10]. Also, hyperglycemia in CA survivors is associated with increased mortality and poor neurological outcomes [11]. However, a comparative study with precise-matched control group - (4-6 mmol / L or 72-108 mg/L) with (6-8 mmol / L or 108-144 mg/dL) - on OHCA resuscitated patients reported no deaths within 30 days [12].
In many countries, post-resuscitation care is not provided in specialized hospitals, and there are many differences between hospitals in terms of availability and type of post-resuscitation care as well as clinical outcomes [13]. A study in Australia identified some of the shortcomings in post-resuscitation care provided by healthcare staff in comparison to the guideline-recommended care, the most important of which were deficiencies of oxygenation, temperature management, and blood pressure control [7]. Also, Ford et al. reported that post-resuscitation care was an influencing factor in patients’ survival. When the healthcare providers do not follow guidelines, it may lead to significant complications after resuscitation [14].
This study aimed to determine the long-term survival after cardiopulmonary resuscitation and its predictors in patients with cardiac arrest in a specialized heart center, which is the referral center of the Province.
Materials and Methods
This analytic study is based on a retrospective survey of the records of all patients who successfully resuscitated after CA in a large referral heart center in Rasht City, Iran, between 2016 and 2019.
Patients over 18 years with long-term survival (long-term survival means the patient survived for at least 24 hours or more after CPR [15]) and patients who survived at least three days after cardiac arrest and were discharged alive were selected as the samples of this study and examined in terms of clinical and demographic characteristics and the follow-ups within three days of resuscitation. The patients who died in the hospital after three days and were not discharged were not included in the study sample.
The data collection instrument consisted of two parts. The first part collected the demographic information and clinical data, which were extracted from patients’ records. These data included date of admission, date of cardiac arrest, date of discharge, sex, and location of CA, pre-arrest consciousness, CPR duration, initial rhythm, and history of CA during the same hospitalization, history of an underlying disease, final diagnosis, and connection to a mechanical ventilator, death after discharge, and survival period after discharge. The second part of the extracted data comprised the information about the time between post-resuscitation monitoring and discharge in 4 areas of blood pressure monitoring, temperature monitoring, blood glucose monitoring, and oxygenation index. Care measures in four areas of post-resuscitation care guidelines of blood pressure monitoring status (Systolic Blood Pressure [SBP] and Mean Arterial Blood Pressure [MAP]), pulse oximetry saturation (SpO2), Blood Sugar (BS), and temperature were extracted from care guidelines [8, 16] and recorded in a prepared checklist.
To determine the instrument validity, 5 faculty members of the country’s medical universities examined the instrument. They were experienced in cardiopulmonary resuscitation. Afterward, the instrument was given back to two experienced professors in the field of cardiopulmonary resuscitation. Also, to ensure the recording of the variables in the file, 60 CPR files were randomly reviewed for the preliminary study.
Initially, we reviewed the medical records of 1565 patients who received CPR between 2016 and 2019. Cases with a successful CPR were separated from the failed ones, which were 667 cases. In this retrospective study, individual, disease-related, and 3-day follow-up-related factors were monitored after the CPR in all patients with long-term survival after CA. After reviewing the medical records of these patients, their contact numbers were noted from the medical records and followed up by telephone interviews. Their survival time after discharge was assessed. If the patient died after discharge, the date of death was asked of their family, and the duration of survival until the date of death was calculated.
In this study, continuous variables were expressed as Mean±SD and categorical variables as frequency (percentage). The survival probability was calculated using the Kaplan-Meier test and compared with the log-rank test. Furthermore, simple and multiple Cox proportional hazard models were performed to estimate the crude and adjusted Hazard Ratios (HR) and their 95% confidence intervals. Statistical analysis was done with SPSS software v. 16 for Windows (SPSS Inc., Chicago, IL, USA), and the level of significance was set at 0.05.
Results
Among 667 successful CPRs, 156 were patients with long-term survival (8 patients died in the hospital despite having more than 24 hours of survival and were not included in the study). One patient was also not included due to a distorted contact number. Successful telephone calls were made to 147 patients, and the research instrument was completed.
The Mean±SD and median survival times of the patients were 30.98±1.78 and 34.70 months (Figure 1). One-, two-, and three-year survival rates were 72.1%, 61.4%, and 49.9%, respectively. A total of 67 patients (45.6%) died after discharge, and 80 patients (54.4%) survived to the end of the study.
Of 147 patients with cardiac arrest who survived to discharge, 89 (60.5%) were men, and 58 (39.5%) were women. The Mean±SD age of the patients was 66.13±14.26. Of them, 47 patients (32%) were under 60 years old (Table 1).
.jpg)
Most samples (98%) had a temperature above 36°C, and the number of patients with abnormal blood sugar was higher than the number of patients with normal blood sugar. During the first, second, and third days after resuscitation, 27.9%, 32%, and 32% of the samples, respectively, had normal blood sugar levels (80-140 mg/dL). Systolic blood pressure was above 90 mm Hg in the majority of patients. About 16.3%, 15.6%, and 10.2% of the samples had systolic blood pressure lower than 90 mm Hg in the first, second, and third days after resuscitation, respectively. Also, 40.8%, 44.2%, and 46.9% of the samples had normal mean arterial blood pressure (65-80 mm Hg) in the first, second, and third days after resuscitation, respectively. Finally, 58.5%, 78.2%, and 85.7% of the samples had normal SpO2 (94%-98%) in the first, second, and third days after resuscitation, respectively.
The Mean±SD values of temperature, blood sugar, systolic blood pressure, diastolic blood pressure, mean arterial pressure, and pulse oximetry saturation during the three days after resuscitation were estimated respectively at 36.82±0.17°C, 179.58±73.43 mg/dL, 114.37±18.27 mm Hg, 69.34±9.68 mm Hg, 84.29±12.11 mm Hg, and 94.47±2.85%.
The log-rank test revealed that the survival time of patients under 60 years was significantly longer than those over 60 years (P=0.039, log-rank statistics=4.269) (Figure 2). Survival time was significantly longer in patients with an initial Ventricalar Fibrilation rhythm than those with an initial Ventricular Tachycardia (VT) or asystole rhythm (P=0.001, log-rank statistics=19.878) (Figure 3). Subjects who were not connected to a mechanical ventilator after CPR had a significantly longer survival time than those connected to a mechanical ventilator (P=0.004, log-rank statistics=8.191) (Figure 4). People without cardiovascular disease had significantly longer survival than people with cardiovascular disease (P=0.015, log-rank statistics=5.923) (Figure 5). The mean survival time was longer in people without hypertension and diabetes, but the difference was not significant.
Although the monitored blood glucose and blood pressure showed relationships with long-term survival, the associations were not statistically significant. Regarding SpO2 monitoring (Figure 6), results showed that the patients with normal SPO2 (94-98%) within three days after resuscitation had significantly longer survival than those with abnormal (P=0.001, log rank statistics=14.090) Comparison mean of survival time based on study variables showed in Table 2.
.jpg)
The analysis of Cox proportional hazards model showed that age (>60 y) (HR=1.811, 95%CI; 1.019-3.218, P=0.043), initial asystole rhythm (HR=4.199, 95%CI; 2.129-8.282, P=0.001), VT (HR=2.315, 95%CI; 1.171-4.576, P=0.016), connection to a mechanical ventilator (HR=1.992, 95%CI; 1.229-3.229, P=0.005), and abnormal SpO2 (HR=2.447, 95%CI; 1.507-3.972, P=0.001) had significant relationships with patients’ survival. So that the older age, initial asystole rhythm, VT, connection to a mechanical ventilator and abnormal SpO2 were associated with lower long-term survival.
Multivariate analysis showed that asystole rhythm (HR=5.128, 95%CI; 1.917-13.716, P=0.001), VT (HR=2.728 , 95%CI; 0.991-7.509, P=0.052), and the duration of resuscitation (>20 min) (HR=3.168, 95%CI; 1.037-9.683, P=0.043) had significant relationships with patients’ survival (Table 3).
.jpg)
Discussion
In our study, most of the samples were men over 60 years old. Many studies have considered old age a significant factor in long-term survival [2, 17]. A systematic review reported that the risk of death after CA was lower in women than men [18]. A study provided a justification for the observed differences. It stated that in the event of an OHCA, women are less likely to be resuscitated by their companions than men, which may lead to lower survival rates for women [19].
Our study showed that a systole heart rhythm is associated with patients’ survival. The initial rhythm was the best predictor of patients’ survival. Also, compared to VF, pulseless electrical activity was associated with shorter survival times [20]. Another study reported that a lower probability of survival at discharge was associated with the recurrence of CA [21].
Our study revealed that CPR duration (>20 min) was a risk factor for patients’ survival. Another study in Iran demonstrated that CPR is an influential factor in a patient’s survival [22]. In another study, CPR duration between 10 and 15 minutes was considered a significant factor in patients’ survival. However, the effect of CPR duration on survival was challenging to evaluate due to its variability from patient to patient [23].
Our observations align with other investigators who reported that underlying diseases such as diabetes, cardiovascular diseases, and hypertension were effective in patients’ survival [24, 25]. Of note, a study evaluated the association of hypertension with survival rate after CA in adults and identified its changes according to the patient’s age [26]. However, a study showed that even though patients with cardiovascular diseases are a high-risk group, there was no significant difference in the survival rate between the patients with and without heart disease [27]. It seems that factors such as biological differences, access to health care, or other factors may affect the survival of patients in the long term.
Temperature above 36°C was reported in most of our study samples. A recent meta-analysis reported that temperature management reduces mortality and significantly reduces poor neurological outcomes [28]. Due to observed consistency in our study, the temperature variable was omitted in the Kaplan Meier, log-rank, and Cox regression analyses.
We considered a blood sugar range of 80-140 mg/dL based on care guidelines [8, 16]. The data showed that the number of patients who lacked normal blood sugar was higher than those with normal blood sugar. Following CPR, a cascade of metabolic disorders frequently occurs, which requires careful monitoring and management. Hence, diagnosis and appropriate response to severe metabolic disorders, especially the prevention of hypoglycemia and hyperglycemia, are essential [29]. Some reports have described the relationships between the increase in mean blood sugar during the first 96 hours after admission and mortality rates and neurological dysfunctions [11, 30].
A search on care guidelines reveals that systolic pressure below 90 mm Hg is an influential factor in recovery after CA [8, 16]. But in our study, most subjects had a systolic pressure above 90 mm Hg. Our study is in line with a systematic review on the association between blood pressure and patients’ outcomes following CA. By examining 13150 patients, the researchers suggested that higher blood pressure ameliorated neurological outcomes after CA [31]. Our results were in contrast to Roberts’ finding [32]. However, another study reported no association between MAP above 90 mm Hg and neurological outcomes at the time of discharge [33]. Patients are often hemodynamically unstable after ROSC, and their management could be a challenge. Following CPR, an optimal hemodynamic should maintain adequate cerebral and coronary perfusion pressure and blood flow to the other vital organs. Based on the current guidelines, the main goal of hemodynamic management is to prevent hypotension and maintain a systolic blood pressure of at least 90 mm Hg or a mean arterial pressure of 65 mm Hg after resuscitation [9].
One systematic review study concluded that hyperoxia in adults with CA was associated with lower mortality rates during CA but higher mortality rates after CA [34]. Another study reported that high or low SpO2 might be associated with poor outcomes after CA [35]. After ROSC, hyperoxemia during the reperfusion phase with 100% oxygen increases brain lipid peroxidation and may cause metabolic dysfunction and neurological degeneration [9]. Besides, excess oxygen leads to increased damage to the myocardium, recurrent myocardial infarction, and larger infarctions within 6 months, as hypocapnia induces cerebral vasoconstriction and reduces cerebral blood flow [16].
Conclusion
Our results showed that different factors are influential in the long-term survival of patients after CA. We believe that differences in the observed results and factors predicting long-term survival may stem from differences in demographic, disease-related factors, the complex nature of CA and its affecting factors, various care services provided by healthcare providers, differences in healthcare providers’ knowledge on the subject of post-resuscitation care, treatment policies in different countries, ethnic and demographic differences, and sample size. Therefore, raising sufficient awareness, including the necessary training for medical staff in post-resuscitation care, especially in the field of hypothermia, maintaining this knowledge, and establishing a recovery ward for patients after cardiac arrest and further investigating in this topic can be effective.
The generalization of our results is limited in two respects. First, the research was a retrospective study, and data were extracted from medical records, so the personnel recording the information might make mistakes. Besides, although the study was performed in a referral center, multicenter studies could be more helpful.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the Research Ethics Committee of Guilan University of Medical Sciences (ID: IR.GUMS.REC.2019.496). Official permission of the hospital administration was acquired for accessing patients’ medical files. The study purpose was explained to the subjects at the beginning of the telephone interview, and the patient’s oral consent was obtained.
Funding
This study was extracted from the Master thesis of the first author, Department of Nursing, School of Nursing and Midwifery, , Guilan University of Medical Sciences, Rasht, Iran (registration number: 97283).
Authors' contributions
Conceptualization and supervision: Fatemeh Jafaraghaee; Investigation: Parivash Nazarpour and Fatemeh Jafaraghaei; Formal analysis: Parivash Nazarpour and Saman Maroufizadeh; Methodology, funding acquisition, resources, and writing - original draft: All authors; Writing - review, and editing: Fatemeh Jafaraghaee and Mohammad Taghi Moghadamnia.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors gratefully thank all patients for their participation in this study. This study was supported by the Research Deputy of Guilan University of Medical Sciences. We would like to express our sincere gratitude to this center.
References
- Coute RA, Nathanson BH, Mader TJ, McNally B, Kurz MC. Trend analysis of disability-adjusted life years following adult out-of-hospital cardiac arrest in the United States: A study from the CARES Surveillance Group. Resuscitation. 2021; 163:124-9. [DOI:10.1016/j.resuscitation.2020.10.048] [PMID]
- Agarwal S, Presciutti A, Roth W, Matthews E, Rodriguez A, Roh DJ, et al. Determinants of long-term neurological recovery patterns relative to hospital discharge among cardiac arrest survivors. Critical Care Medicine. 2018; 46(2):e141-50. [DOI:10.1097/CCM.0000000000002846] [PMID] [PMCID]
- Amini S, Moghadamnia MT, Paryad E, Kazem Nezhad Leyli E. Factors associated with survival rate after cardiopulmonary resuscitation. Journal of Holistic Nursing and Midwifery. 2017; 27(3):1-7. http://hnmj.gums.ac.ir/article-1-911-en.html
- Lu J, Liu L, Zhu J, Guo X. Factors influencing the quality of standardized treatment for patients with post-cardiac arrest syndrome. Korean Circulation Journal. 2017; 47(4):455-61. [DOI:10.4070/kcj.2016.0437] [PMID] [PMCID]
- Tsai MS, Chuang PY, Huang CH, Tang CH, Yu PH, Chang WT, et al. Postarrest steroid use may improve outcomes of cardiac arrest survivors. Critical Care Medicine. 2019; 47(2):167-75. [DOI:10.1097/CCM.0000000000003468] [PMID]
- Kim Y, Kim J, Shin SA. Relationship between the legal nurse staffing standard and patient survival after perioperative cardiac arrest: A cross-sectional analysis of Korean administrative data. International Journal of Nursing Studies. 2019; 89:104-11. [DOI:10.1016/j.ijnurstu.2018.09.012] [PMID]
- Milonas A, Hutchinson A, Charlesworth D, Doric A, Green J, Considine J. Post resuscitation management of cardiac arrest patients in the critical care environment: A retrospective audit of compliance with evidence based guidelines. Australian Critical Care. 2017; 30(6):299-305. [DOI:10.1016/j.aucc.2016.12.001] [PMID]
- Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: Post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(18 Suppl 2):S465-82. [DOI:10.1161/CIR.0000000000000262] [PMID] [PMCID]
- Pothiawala S. Post-resuscitation care. Singapore Medical Journal. 2017; 58(7):404-7. [DOI:10.11622/smedj.2017060] [PMID] [PMCID]
- Maryam Y, Sutton RM, Friess SH, Bratinov G, Bhalala U, Kilbaugh TJ, et al. Blood pressure and coronary perfusion pressure targeted cardiopulmonary resuscitation improves 24-hour survival from ventricular fibrillation cardiac arrest. Critical Care Medicine. 2016; 44(11):e1111. [DOI:10.1097/CCM.0000000000001859] [PMID] [PMCID]
- Russo JJ, James TE, Hibbert B, Ramirez FD, Simard T, Osborne C, et al. Hyperglycaemia in comatose survivors of out-of-hospital cardiac arrest. European Heart Journal: Acute Cardiovascular Care. 2018; 7(5):442-9. [DOI:10.1177/2048872616684685] [PMID]
- Todi S, Bhalchandra S, Zirpe K, Mehta Y. Critical care update. New Delhi: Jaypee Brothers Medical Publishers Pvt. Limited; 2019. https://www.google.com/books/edition/_Care__2019/c=frontcover
- Yeung J, Matsuyama T, Bray J, Reynolds J, Skrifvars M. Does care at a cardiac arrest centre improve outcome after out-of-hospital cardiac arrest? A systematic review. Resuscitation. 2019; 137:102-15. [DOI:10.1016/j.resuscitation.2019.02.006] [PMID]
- Ford A, Clark T, Reynolds E, Ross C, Shelley K, Simmonds L, et al. Management of cardiac arrest survivors in UK intensive care units: A survey of practice. Journal of the Intensive Care Society. 2016; 17(2):117-21. [DOI:10.1177/1751143715615151] [PMID] [PMCID]
- Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in-hospital cardiac arrest. New England Journal of Medicine. 2012; 367(20):1912-20. [DOI:10.1056/NEJMoa1109148] [PMID] [PMCID]
- Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VR, Deakin CD, et al. European resuscitation council and European society of intensive care medicine 2015 guidelines for post-resuscitation care. Intensive Care Medicine. 2015; 41(12):2039-56. [DOI:10.1016/j.resuscitation.2015.07.018] [PMID]
- Hiemstra B, Bergman R, Absalom AR, van der Naalt J, van der Harst P, de Vos R, et al. Long-term outcome of elderly out-of-hospital cardiac arrest survivors as compared with their younger counterparts and the general population. Therapeutic Advances in Cardiovascular Disease. 2018; 12(12):341-9. [DOI:10.1177/1753944718792420] [PMID] [PMCID]
- Bougouin W, Mustafic H, Marijon E, Murad MH, Dumas F, Barbouttis A, et al. Gender and survival after sudden cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2015; 94:55-60. [DOI:10.1016/j.resuscitation.2015.06.018] [PMID]
- Blom MT, Oving I, Berdowski J, van Valkengoed IG, Bardai A, Tan HL. Women have lower chances than men to be resuscitated and survive out-of-hospital cardiac arrest. European Heart Journal. 2019; 40(47):3824-34. [DOI:10.1093/eurheartj/ehz297] [PMID] [PMCID]
- Vancini-Campanharo CR, Vancini RL, Lira CABd, Andrade MdS, Góis AFTd, Atallah ÁN. Cohort study on the factors associated with survival post-cardiac arrest. Sao Paulo Medical Journal. 2015; 133(6):495-501. [DOI:10.1590/1516-3180.2015.00472607] [PMID]
- Bhardwaj A, Ikeda DJ, Grossestreuer AV, Sheak KR, Delfin G, Layden T, et al. Factors associated with re-arrest following initial resuscitation from cardiac arrest. Resuscitation. 2017; 111:90-5. [DOI:10.1016/j.resuscitation.2016.12.007] [PMID]
- Arhami Dolatabadi A, Memari E, Shojaee M, Alimohammadi H, Kariman H, Shahrami A, et al. Survival and outcomes following cardiopulmonary resuscitation: A descriptive study in Iran. Journal of Emergency Practice and Trauma. 2017; 3(1):22-5. [DOI:10.15171/jept.2017.09]
- Cheema MA, Ullah W, Abdullah HMA, Haq S, Ahmad A, Balaratna A. Duration of in-hospital cardiopulmonary resuscitation and its effect on survival. Indian Heart Journal. 2019; 71(4):314-9. [DOI:10.1016/j.ihj.2019.09.002] [PMID] [PMCID]
- Parry M, Danielson K, Brennenstuhl S, Drennan IR, Morrison LJ. The association between diabetes status and survival following an out-of-hospital cardiac arrest: A retrospective cohort study. Resuscitation. 2017; 113:21-6. [DOI:10.1016/j.resuscitation.2017.01.011] [PMID]
- Movahedi A, Mirhafez SR, Behnam-Voshani H, Reihani H, Ferns GA, Malekzadeh J. 24-Hour survival after cardiopulmonary resuscitation is reduced in patients with diabetes mellitus. Journal of Cardiovascular and Thoracic Research. 2017; 9(3):175-8. [DOI:10.15171/jcvtr.2017.30] [PMID] [PMCID]
- Jung E, Park JH, Ro YS, Song KJ, Ryu HH, Lee SC, et al. Effect of hypertension across the age group on survival outcomes in out-of-hospital cardiac arrest. The American Journal of Emergency Medicine. 2019; 37(4):608-14. [DOI:10.1016/j.ajem.2018.06.049] [PMID]
- Lee MH, Fook-Chong S, Wah W, Shin SD, Nishiuchi T, Ko PCI, et al. Effect of known history of heart disease on survival outcomes after out-of-hospital cardiac arrests. Emergency Medicine Australasia. 2018; 30(1):67-76. [DOI:10.1111/1742-6723.12809] [PMID]
- Abdalla M, Mohamed A, Mohamed W, Khtab K, Cattoni H, Salih M. Targeted temperature management after cardiac arrest: Updated meta-analysis of all-cause mortality and neurological outcomes. International Journal of Cardiology. Heart & Vasculature. 2019; 24:100400. [DOI:10.1016/j.ijcha.2019.100400] [PMID] [PMCID]
- Bellomo R, Märtensson J, Eastwood GM. Metabolic and electrolyte disturbance after cardiac arrest: How to deal with it. Best Practice & Research Clinical Anaesthesiology. 2015; 29(4):471-84. [DOI:10.1016/j.bpa.2015.10.003] [PMID]
- Borgquist O, Wise MP, Nielsen N, Al-Subaie N, Cranshaw J, Cronberg T, et al. Dysglycemia, glycemic variability, and outcome after cardiac arrest and temperature management at 33° C and 36° C. Critical Care Medicine. 2017; 45(8):1337-43. [DOI:10.1097/CCM.0000000000002367] [PMID]
- Bhate TD, McDonald B, Sekhon MS, Griesdale DE. Association between blood pressure and outcomes in patients after cardiac arrest: A systematic review. Resuscitation. 2015; 97:1-6. [DOI:10.1016/j.resuscitation.2015.08.023] [PMID]
- Roberts BW, Kilgannon JH, Hunter BR, Puskarich MA, Shea L, Donnino M, et al. Association between elevated mean arterial blood pressure and neurological outcome after resuscitation from cardiac arrest: Results from a multicenter prospective cohort study. Critical Care Medicine. 2019; 47(1):93-100. [DOI:10.1097/CCM.0000000000003474] [PMID] [PMCID]
- Young MN, Hollenbeck RD, Pollock JS, Giuseffi JL, Wang L, Harrell FE, et al. Higher achieved mean arterial pressure during therapeutic hypothermia is not associated with neurologically intact survival following cardiac arrest. Resuscitation. 2015; 88:158-64. [DOI:10.1016/j.resuscitation.2014.12.008] [PMID] [PMCID]
- Patel JK, Kataya A, Parikh PB. Association between intra-and post-arrest hyperoxia on mortality in adults with cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2018; 127:83-8. [DOI:10.1016/j.resuscitation.2018.04.008] [PMID]
- Zhou DW, Li ZM, Zhang SL, Wu L, Li YY, Zhou JX, et al. The optimal peripheral oxygen saturation may be 95-97% for post-cardiac arrest patients: A retrospective observational study. The American Journal of Emergency Medicine. 2021; 40:120-6. [DOI:10.1016/j.ajem.2020.01.038] [PMID]
Article Type : Research |
Subject:
Special
Received: 2021/11/26 | Accepted: 2022/01/2 | Published: 2022/04/1
Received: 2021/11/26 | Accepted: 2022/01/2 | Published: 2022/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





.jpg)
.jpg)
.jpg)
.jpg)
.jpg)